Omeprazole
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Prilosec (originator), many generic brands[1] |
| License data |
|
| Pregnancy category |
|
| Routes of administration | Oral, IV |
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Bioavailability | 35–76%[3][4] |
| Protein binding | 95% |
| Metabolism | Hepatic (CYP2C19, CYP3A4) |
| Elimination half-life | 1–1.2 hours |
| Excretion | 80% Renal 20% Faecal |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| PDB ligand | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.122.967 |
| Chemical and physical data | |
| Formula | C17H19N3O3S |
| Molar mass | 345.4 g/mol g·mol−1 |
| 3D model (JSmol) | |
| |
| |
| (verify) | |
Omeprazole (INN) /oʊˈmɛprəzoʊl/ is a proton pump inhibitor used in the treatment of dyspepsia, peptic ulcer disease, gastroesophageal reflux disease, laryngopharyngeal reflux, and Zollinger–Ellison syndrome.
Omeprazole is one of the most widely prescribed drugs internationally[citation needed] and is available over the counter in some countries.
It is on the World Health Organization's List of Essential Medicines, the most important medications needed in a basic health system.[5]
Medical uses
Omeprazole can be used in the treatment of gastroesophageal reflux disease (GERD), peptic ulcers, erosive esophagitis, and Zollinger-Ellison syndrome.
Gastroesophageal reflux disease
GERD is a chronic condition in which acidic stomach content leaks back into the esophagus and irritates it. It may cause heartburn, which is a painful burning feeling in the chest or throat.
Peptic ulcers
Peptic ulcers are sores that develop in the lining of either the stomach or the duodenum due to damage from stomach acid. The most common cause of a peptic ulcer is infection by Helicobacter pylori.[6] Another major cause of a peptic ulcer is long-term use of nonsteroidal anti-inflammatory drugs (NSAIDs), such as aspirin or ibuprofen.[7] Treatment of H. pylori infection can be completed by taking a triple therapy combination of omeprazole, amoxicillin, and clarithromycin for 7–14 days.[8] Amoxicillin may be replaced with metronidazole in patients who are allergic to penicillin.[9]
Erosive esophagitis
Erosive esophagitis is due to tissue damage to the lining of the esophagus, because of inflammation or irritation over time. It may be caused by acid reflux from GERD, infection by a virus or fungus, an autoimmune disorder, certain medications,[10] or alcohol abuse.
Zollinger Ellison syndrome
Zollinger Ellison syndrome is a rare disorder that occurs when a tumor of the pancreas or duodenum releases a hormone that stimulates overproduction of stomach acid. This condition may form multiple peptic ulcers.
Adverse effects
The most frequent significant adverse effects occurring in at least 1% of patients include:[11]
- Central nervous system: headache (7%), dizziness (2%)
- Respiratory: upper respiratory tract infection (2%), cough (1%)
- Gastrointestinal: abdominal pain (5%), diarrhea (4%), nausea (4%), vomiting (3%), flatulence (3%), acid regurgitation (2%), constipation (2%)
- Neuromuscular and skeletal: back pain (1%), weakness (1%)
- Dermatologic: rash (2%)
Other significant concerns related to adverse effects are:
- Clostridium difficile associated diarrhea[12]
- Osteoporosis-related fractures[13][14]
- Hypomagnesemia[15]
Concern has been expressed regarding vitamin B12[16] and iron malabsorption,[17] but effects seem to be clinically insignificant, especially when supplement therapy is provided.[18]
Since their introduction, proton pump inhibitors (PPIs, especially omeprazole) have also been associated with several cases of acute interstitial nephritis,[19] an inflammation of the kidneys that often occurs as an adverse drug reaction.
Long-term use of PPIs is strongly associated with the development of benign polyps from fundic glands (which is distinct from fundic gland polyposis); these polyps do not cause cancer and resolve when PPIs are discontinued. No association is seen between PPI use and cancer, but use of PPIs may mask gastric cancers or other serious gastric problems and physicians should be aware of this effect.[20]
Interactions
Omeprazole is a drug of the PPI class. Although the potential for drug interactions is high, clinically important drug interactions are rare.[21][22]
However, the most significant major drug interaction concern is the decreased activation of clopidogrel when taken together with omeprazole.[23] Although still controversial,[24] this may increase the risk of stroke or heart attack in people taking clopidogrel to prevent these events.
The mechanism by which this potential interaction occurs is because omeprazole is an inhibitor of the enzymes CYP2C19 and CYP3A4.[25] Clopidogrel is an inactive prodrug that partially depends on CYP2C19 for conversion to its active form. Inhibition of CYP2C19 may block the activation of clopidogrel, which could reduce its effects.[26][27]
Almost all benzodiazepines are metabolised by the CYP3A4 and CYP2D6 pathway, and inhibition of these enzymes results in a higher AUC (i.e. the total effect over time of a given dose). Other examples of drugs dependent on CYP3A4 for their metabolism are escitalopram,[28] warfarin,[29] oxycodone, tramadol, and oxymorphone. The concentrations of these drugs may increase if they are used concomitantly with omeprazole.[30]
Omeprazole is also a competitive inhibitor of p-glycoprotein, as are other PPIs.[31]
Drugs that depend on an acidic stomach environment (such as ketoconazole or atazanavir) may be poorly absorbed, whereas acid-labile antibiotics (such as erythromycin which is a very strong CYP3A4 inhibitor) may be absorbed to a greater extent than normal due to the more alkaline environment of the stomach.[30]
St. John's wort, a monoamine oxidase inhibitor (Hypericum perforatum), and Gingko biloba significantly reduce plasma concentrations of omeprazole through induction of CYP3A4 and CYP2C19.[32]
Pregnancy and breast-feeding
Epidemiological data do not show an increased risk of major birth defects after maternal use of omeprazole during pregnancy.[33]
No clinical trials have deeply evaluated the potential consequences of the use of omeprazole in breastfeeding. However, the pharmacokinetics of omeprazole molecule strongly suggest the safety of omeprazole use during breastfeeding:
- Omeprazole has a high plasma protein binding rate (95%),[34] indicating that little amount of drug is transferred to the milk duct during breast milk formation.
- Omeprazole needs to be administrated in an enteric-coated formulation due to its rapid degradation in the acidic conditions of the stomach. This suggests that most of the free molecules ingested by the infant are likely degraded before being absorbed.
The safety of omeprazole use in breastfeeding deduced from pharmacokinetic characteristics of the omeprazole molecule agree with a case report in which the presence of omeprazole in breast milk was analysed over 4 hours after omeprazole uptake.[35] The peak omeprazole concentration in breast milk (that occurred 3h after omeprazole ingestion) was 7% of peak serum concentration, which corresponds to less than 1% of the usual adult dose (200 to 400 ug of omeprazole/kg of body weight) for a 5-kg infant consuming 200 ml of breast milk per day.
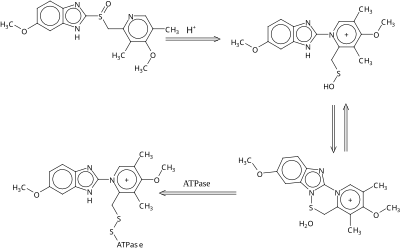
Mechanism of action
Omeprazole is a selective and irreversible proton pump inhibitor. It suppresses stomach acid secretion by specific inhibition of the H +/K + ATPase system found at the secretory surface of gastric parietal cells. Because this enzyme system is regarded as the acid (proton, or H+) pump within the gastric mucosa, omeprazole inhibits the final step of acid production.
Omeprazole also inhibits both basal and stimulated acid secretion irrespective of the stimulus.[36]
Pharmacodynamics
The inhibitory effect of omeprazole occurs within 1 hour after oral administration. The maximum effect occurs within 2 hours. The duration of inhibition is up to 72 hours. When omeprazole is stopped, baseline stomach acid secretory activity returns after 3 to 5 days. The inhibitory effect of omeprazole on acid secretion will plateau after 4 days of repeated daily dosing.[37]
Pharmacokinetics
The absorption of omeprazole takes place in the small intestine and is usually completed within 3 to 6 hours. The systemic bioavailability of omeprazole after repeated dose is about 60%.
Omeprazole, as well as other PPIs, are only effective on active H+/K+ ATPase pumps. These pumps are stimulated in the presence of food to aid in digestion. For this reason, patients should be advised to take omeprazole with a glass of water on an empty stomach about 30–60 minutes before a meal to allow the drug to reach peak levels once food is ingested.[38][39] Additionally, most sources recommend that after taking omeprazole, at least 30 minutes should be allowed to elapse before eating[40][41] (at least 60 minutes for immediate-release omeprazole plus sodium bicarbonate products, such as Zegerid),[42] though some sources say that with delayed-release forms of omeprazole, waiting before eating after taking the medication is not necessary.[43]
Omeprazole is completely metabolized by the cytochrome P450 system, mainly in the liver. Identified metabolites are the sulfone, the sulfide, and hydroxy-omeprazole, which exert no significant effect on acid secretion. About 80% of an orally given dose is excreted as metabolites in the urine, and the remainder is found in the feces, primarily originating from bile secretion.
Measurement in body fluids
Omeprazole may be quantified in plasma or serum to monitor therapy or to confirm a diagnosis of poisoning in hospitalized patients. Plasma omeprazole concentrations are usually in a range of 0.2–1.2 mg/l in persons receiving the drug therapeutically by the oral route and 1–6 mg/l in victims of acute overdose. Enantiomeric chromatographic methods are available to distinguish esomeprazole from racemic omeprazole.[44]
Chemistry
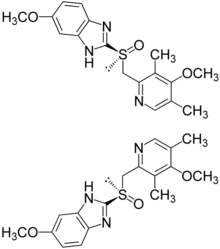
Omeprazole contains a tricoordinated sulfinyl sulfur in a pyramidal structure and therefore can exist as either the (S)- or (R)-enantiomers. Omeprazole is a racemate, an equal mixture of the two. In the acidic conditions of the canaliculi of parietal cells, both enantiomers are converted to achiral products (sulfenic acid and sulfenamide configurations) which react with a cysteine group in H+/K+ ATPase, thereby inhibiting the ability of the parietal cells to produce gastric acid.
AstraZeneca has also developed esomeprazole (Nexium) which is a eutomer, purely the (S)-enantiomer, rather than a racemate like omeprazole.
Omeprazole undergoes a chiral shift in vivo which converts the inactive (R)-enantiomer to the active (S)-enantiomer, doubling the concentration of the active form.[45] This chiral shift is accomplished by the CYP2C19 isozyme of cytochrome P450, which is not found equally in all human populations. Those who do not metabolize the drug effectively are called "poor metabolizers". The proportion of the poor metabolizer phenotype varies widely between populations, from 2.0–2.5% in African Americans and white Americans to >20% in Asians; several pharmacogenomics studies have suggested that PPI treatment should be tailored according to CYP2C19 metabolism status.[46]
History
Omeprazole was first marketed in the United States in 1989 by Astra AB, now AstraZeneca, under the brand name Losec. In 1990, at the request of the U.S. Food and Drug Administration, the brand name Losec was changed to Prilosec to avoid confusion with the diuretic Lasix (furosemide).[47] The new name led to confusion between omeprazole (Prilosec) and fluoxetine (Prozac), an antidepressant.[47]
When Prilosec's U.S. patent expired in April 2001, AstraZeneca introduced esomeprazole (Nexium) as a patented replacement drug.[48] Many companies introduced generics as Astrazeneca's patents expired worldwide, which are available under many brand names.[1]
Dosage forms


Omeprazole is available as tablets and capsules (containing omeprazole or omeprazole magnesium) in strengths of 10, 20, 40, and in some markets 80 mg; and as a powder (omeprazole sodium) for intravenous injection. Most oral omeprazole preparations are enteric-coated, due to the rapid degradation of the drug in the acidic conditions of the stomach. This is most commonly achieved by formulating enteric-coated granules within capsules, enteric-coated tablets, and the multiple-unit pellet system (MUPS).[49] An immediate release formulation was approved by the FDA in the United States,[50] which does not require enteric coating.
It is also available for use in injectable form (IV) in Europe, but not in the U.S. The injection pack is a combination pack consisting of a vial and a separate ampule of reconstituting solution. Each 10-ml clear glass vial contains a white to off-white lyophilised powder consisting of omeprazole sodium 42.6 mg, equivalent to 40 mg of omeprazole.
See also
References
- ^ a b Drugs.com [Omeprazole international names] Page accessed August 23, 2015
- ^ "FDA-sourced list of all drugs with black box warnings (Use Download Full Results and View Query links.)". nctr-crs.fda.gov. FDA. Retrieved 22 October 2023.
- ^ Prilosec Prescribing Information. AstraZeneca Pharmaceuticals.
- ^ Vaz-Da-Silva, M; Loureiro, AI; Nunes, T; Maia, J; Tavares, S; Falcão, A; Silveira, P; Almeida, L; Soares-Da-Silva, P (2005). "Bioavailability and bioequivalence of two enteric-coated formulations of omeprazole in fasting and fed conditions". Clin Drug Investig. 25 (6): 391–9. doi:10.2165/00044011-200525060-00004. PMID 17532679.
- ^ "WHO Model List of EssentialMedicines" (PDF). World Health Organization. October 2013. Retrieved 22 April 2014.
- ^ Shiotani A, Graham DY (November 2002). "Pathogenesis and therapy of gastric and duodenal ulcer disease". Med. Clin. North Am. 86 (6): 1447–66, viii. doi:10.1016/S0025-7125(02)00083-4. PMID 12510460.
- ^ Traversa G, Walker AM, Ippolito FM, Caffari B, Capurso L, Dezi A, Koch M, Maggini M, Alegiani SS, Raschetti R (January 1995). "Gastroduodenal toxicity of different nonsteroidal antiinflammatory drugs". Epidemiology (Cambridge, Mass.). 6 (1): 49–54. doi:10.1097/00001648-199501000-00010. ISSN 1044-3983. PMID 7888445.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Fuccio, Lorenzo, et al. "Meta-analysis: duration of first-line proton-pump inhibitor–based triple therapy for Helicobacter pylori eradication." Annals of internal medicine 147.8 (2007): 553-562.
- ^ Malfertheiner P, Megraud F, O'Morain C, Bazzoli F, El-Omar E, Graham D, Hunt R, Rokkas T, Vakil N, Kuipers EJ (June 2007). "Current concepts in the management of Helicobacter pylori infection: the Maastricht III Consensus Report". Gut. 56 (6): 772–81. doi:10.1136/gut.2006.101634. PMC 1954853. PMID 17170018.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Winstead, Nathaniel S., and Robert Bulat. "Pill esophagitis." Current treatment options in gastroenterology 7.1 (2004): 71-76.
- ^ McTavish D, Buckley MMT, Heel RC. Omeprazole: an updated review of its pharmacology and therapeutic use in acid-related disorders. Drugs. 1991; 42:138-70.
- ^ Abou Chakra CN, et al Risk factors for recurrence, complications and mortality in Clostridium difficile infection: a systematic review. PLoS One. 2014 Jun 4;9(6):e98400. PMID 24897375
- ^ Yang, Yu-Xiao, et al. "Long-term proton pump inhibitor therapy and risk of hip fracture." Jama 296.24 (2006): 2947-2953.
- ^ Yu, Elaine W., et al. "Proton pump inhibitors and risk of fractures: a meta-analysis of 11 international studies." The American journal of medicine 124.6 (2011): 519-526.
- ^ Hess, M. W., et al. "Systematic review: hypomagnesaemia induced by proton pump inhibition." Alimentary pharmacology & therapeutics 36.5 (2012): 405-413.
- ^ Neal, Keith, and Richard Logan. "Potential gastrointestinal effects of long‐term acid suppression with proton pump inhibitors." Alimentary pharmacology & therapeutics 15.7 (2001): 1085-1085.
- ^ Sarzynski, Erin, et al. "Association between proton pump inhibitor use and anemia: a retrospective cohort study." Digestive diseases and sciences 56.8 (2011): 2349-2353.
- ^ McColl, Kenneth EL. "Effect of proton pump inhibitors on vitamins and iron." The American journal of gastroenterology 104 (2009): S5-S9.
- ^ Härmark, Linda, et al. "Proton pump inhibitor‐induced acute interstitial nephritis." British journal of clinical pharmacology 64.6 (2007): 819-823.
- ^ Corleto, V.D. (February 2014). "Proton pump inhibitor therapy and potential long-term harm". Curr Opin Endocrinol Diabetes Obes. 21 (1): 3–8. PMID 24310148.
- ^ Fitzakerley, Janet. "2014 Treatments for Acid-Peptic Diseases." PPIs Side Effects. University of Minnesota Medical School Duluth, 5 Jan. 2014. Web. 18 Apr. 2014.
- ^ Proton Pump Inhibitor: Use in Adults. CMS Medicaid Integrity Program, Aug. 2013. Web. 18 Apr. 2014.
- ^ Douglas, Ian J., et al. "Clopidogrel and interaction with proton pump inhibitors: comparison between cohort and within person study designs." BMJ: British Medical Journal 345 (2012).
- ^ Focks, Jeroen Jaspers, et al. "Concomitant use of clopidogrel and proton pump inhibitors: impact on platelet function and clinical outcome-a systematic review." Heart 99.8 (2013): 520-527.
- ^ "Inhibition of CYP2C19 and CYP3A4 by omepra... [Drug Metab Dispos. 2013] - PubMed - NCBI". Drug Metab. Dispos. 41 (7). Ncbi.nlm.nih.gov: 1414–24. July 2013. doi:10.1124/dmd.113.051722. PMC 3684819. PMID 23620487.
- ^ Lau WC, Gurbel PA (March 2009). "The drug-drug interaction between proton pump inhibitors and clopidogrel". CMAJ. 180 (7): 699–700. doi:10.1503/cmaj.090251. PMC 2659824. PMID 19332744.
- ^ Norgard NB, Mathews KD, Wall GC (July 2009). "Drug-drug interaction between clopidogrel and the proton pump inhibitors". Ann Pharmacother. 43 (7): 1266–1274. doi:10.1345/aph.1M051. PMID 19470853.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Ali Torkamani, PhD. "Selective Serotonin Reuptake Inhibitors and CYP2D6". Medscape.com. Retrieved 14 May 2015.
- ^ Daly AK, King BP (May 2003). "Pharmacogenetics of oral anticoagulants". Pharmacogenetics. 13 (5): 247–52. doi:10.1097/01.fpc.0000054071.64000.bd. PMID 12724615.
- ^ a b Stedman CA, Barclay ML (August 2000). "Review article: comparison of the pharmacokinetics, acid suppression and efficacy of proton pump inhibitors". Aliment Pharmacol Ther. 14 (8): 963–978. doi:10.1046/j.1365-2036.2000.00788.x. PMID 10930890.
- ^ Pauli-Magnus C, Rekersbrink S, Klotz U, Fromm MF (December 2001). "Interaction of omeprazole, lansoprazole and pantoprazole with P-glycoprotein". Naunyn Schmiedebergs Arch Pharmacol. 364 (6): 551–557. doi:10.1007/s00210-001-0489-7. PMID 11770010.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Izzo, AA; Ernst, E (2009). "Interactions between herbal medicines and prescribed drugs: an updated systematic review". Drugs. 69 (13): 1777–1798. doi:10.2165/11317010-000000000-00000. PMID 19719333.
- ^ Pasternak, Björn, and Anders Hviid. [1] "Use of proton-pump inhibitors in early pregnancy and the risk of birth defects." New England Journal of Medicine 363.22 (2010): 2114-2123.
- ^ "Omeprazole drug summary". PDR.net. Retrieved 3 March 2014.
- ^ Marshall, JK; Thompson, A. B.; Armstrong, D (1998). "Omeprazole for refractory gastroesophageal reflux disease during pregnancy and lactation". Can J Gastroenterol. 12 (3): 225–227. PMID 9582548.
- ^ "DrugBank: Omeprazole (DB00338)". Drugbank.ca. Retrieved 24 February 2014.
- ^ Omeprazole [package insert]. India: Dr. Reddy's Laboratories Limited. Revised: 0613
- ^ Katz PO, Gerson LB, Vela MF. Guidelines for the diagnosis and management of gastroesophageal reflux disease. Am J Gastroenterol 2013;108:308-28.
- ^ PharmacistAnswers Webpage Retrieved 27 February 2014
- ^ "Omeprazole, in The Free Medical Dictionary". Retrieved 11 November 2010.
- ^ "Omeprazole". Drugs.com. Retrieved 11 November 2010.
- ^ "Zegird, How to take". rxlist.com. Retrieved 11 November 2010.
- ^ essential drug information. MIMS USA. Retrieved 20 December 2009.[verification needed]
- ^ Baselt RC, Disposition of Toxic Drugs and Chemicals in Man, 8th edition, Biomedical Publications, Foster City, CA, 2008, pp. 1146–7. ISBN 978-0-9626523-7-0.
- ^ Nexium Prescribing Information. AstraZeneca Pharmaceuticals.
- ^ Furuta T, Shirai N, Sugimoto M, Nakamura A, Hishida A, Ishizaki T (June 2005). "Influence of CYP2C19 pharmacogenetic polymorphism on proton pump inhibitor-based therapies". Drug Metab Pharmacokinet. 20 (3): 153–67. doi:10.2133/dmpk.20.153. PMID 15988117.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ a b Farley, D (July–August 1995). "Making it easier to read prescriptions". FDA Consum. 29 (6): 25–7. PMID 10143448.
- ^ Gardiner Harris (6 June 2002). "Prilosec's Maker Switches Users To Nexium, Thwarting Generics". The Wall Street Journal.
- ^ Aubert, J. É. R. Ô. M. E., CHRIS JJ Mulder, and K. A. R. S. T. E. N. Schrör. "Omeprazole MUPS®: An Advanced Formulation offering Flexibility and Predictability for Self Medication." SelfCare Journal 2 (2011): 0-0.
- ^ Santarus. Santarus Receives FDA Approval for Immediate-Release Omeprazole Tablet with Dual Buffers. N.p., 4 Dec. 2009. Web. 18 Apr. 2014.
External links