Adenosine: Difference between revisions
m →Dosage: expanded overly-technical abbrevs. and gave simple defs for medical terms, for average-reader clarity |
|||
| Line 63: | Line 63: | ||
===Dosage=== |
===Dosage=== |
||
When given for the evaluation or treatment of |
When given for the evaluation or treatment of a [[supraventricular tachycardia]] (SVT), the initial dose is 6 mg, given as a fast [[intravenous]]/[[Intraosseous infusion]] push. Due to adenosine's extremely short half-life, the IV line is started as proximal (near) to the heart as possible, such as the antecubital fossa (the depression in front of the elbow.) The IV push is often followed with an immediate flush of 5-10ccs of saline. If this has no effect (e.g., no evidence of transient AV block), a 12mg dose can be given 1-2 minutes after the first dose. If the 12mg dose has no effect, a second 12mg dose can be administered 1-2 minutes after the previous dose. Some clinicians may prefer to administer a higher dose (typically 18 mg), rather than repeat a dose that apparently had no effect. When given to dilate the arteries, such as in a "stress test", the dosage is typically 0.14 mg/kg/min, administered for 4 or 6 minutes, depending on the protocol. |
||
The recommended dose may be increased in patients on theophylline since methylxanthines prevent binding of adenosine at receptor sites. The dose is often decreased in patients on dipyridamole (Persantine) and diazepam (Valium) because adenosine potentiates the effects of these drugs. The recommended dose is also reduced by half in patients who are presenting [[Congestive Heart Failure]], [[Myocardial Infarction]], [[shock (circulatory)|shock]], [[hypoxia (medical)|hypoxia]], and/or hepatic or renal insufficiency, and in [[elderly]] patients. |
The recommended dose may be increased in patients on theophylline since methylxanthines prevent binding of adenosine at receptor sites. The dose is often decreased in patients on dipyridamole (Persantine) and diazepam (Valium) because adenosine potentiates the effects of these drugs. The recommended dose is also reduced by half in patients who are presenting [[Congestive Heart Failure]], [[Myocardial Infarction]], [[shock (circulatory)|shock]], [[hypoxia (medical)|hypoxia]], and/or hepatic or renal insufficiency, and in [[elderly]] patients. |
||
Revision as of 08:15, 5 March 2009
| File:A chemical structure.png | |
 | |
| Clinical data | |
|---|---|
| Pregnancy category |
|
| Routes of administration | IV or injection |
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Bioavailability | Rapidly cleared from circulation via cellular uptake |
| Protein binding | No |
| Metabolism | Rapidly converted to inosine and adenosine monophosphate |
| Elimination half-life | cleared plasma <30 seconds - half life <10 seconds |
| Excretion | can leave cell intact or can be degraded to hypoxanthine, xanthine, and ultimately uric acid |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| DrugBank | |
| ChemSpider | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.000.354 |
| Chemical and physical data | |
| Formula | C10H13N5O4 |
| Molar mass | 267.241 g/mol g·mol−1 |
| 3D model (JSmol) | |
| |
Adenosine is a nucleoside composed of a molecule of adenine attached to a ribose sugar molecule (ribofuranose) moiety via a β-N9-glycosidic bond.
Adenosine plays an important role in biochemical processes, such as energy transfer - as adenosine triphosphate (ATP) and adenosine diphosphate (ADP) - as well as in signal transduction as cyclic adenosine monophosphate, cAMP. It is also an inhibitory neurotransmitter, believed to play a role in promoting sleep and suppressing arousal, with levels increasing with each hour an organism is awake.
Pharmacological effects
Adenosine is an endogenous purine nucleoside that modulates many physiologic processes. Cellular signaling by adenosine occurs through four known adenosine receptor subtypes (A1, A2A, A2B, and A3).[1]
Extracellular adenosine concentrations from normal cells are approximately 300 nM; however, in response to cellular damage (e.g. in inflammatory or ischemic tissue), these concentrations are quickly elevated (600-1,200 nM). Thus, in regards to stress or injury, the function of adenosine is primarily that of cytoprotection preventing tissue damage during instances of hypoxia, ischemia, and seizure activity. Activation of A2A receptors produces a constellation of responses that in general can be classified as anti-inflammatory.
Adenosine receptors
The different adenosine receptor subtypes (A1, A2A, A2B, and A3) are all seven transmembrane spanning G-protein coupled receptors. These four receptor subtypes are further classified based on their ability to either stimulate or inhibit adenylate cyclase activity. The A2A and A2B receptors couple to Gάs and mediate the stimulation of adenylate cyclase, while the A1 and A3 adenosine receptors couple to Gάi which inhibits adenylate cyclase activity. Additionally, A1 receptors couple to Gάo, which has been reported to mediate adenosine inhibition of Ca2+ conductance, whereas A2B and A3 receptors also couple to Gάq and stimulate phospholipase activity.
Anti-inflammatory properties
Adenosine is believed to be a anti-inflammatory agent at the A(2A) receptor.[2][3] Topical treatment of adenosine to foot wounds in diabetes mellitus has been shown in lab animals to drastically increase tissue repair and reconstruction. Topical administration of adenosine for use in wound healing deficiencies and diabetes mellitus in humans is currently under clinical investigation.
Action on the heart
When administered intravenously, adenosine causes transient heart block in the AV node. This is mediated via the A1 receptor, inhibiting adenyl cyclase, reducing cAMP and so causing cell hyperpolarization by increasing outward K+ flux. It also causes endothelial dependent relaxation of smooth muscle as is found inside the artery walls. This causes dilatation of the "normal" segments of arteries, i.e. where the endothelium is not separated from the tunica media by atherosclerotic plaque. This feature allows physicians to use adenosine to test for blockages in the coronary arteries, by exaggerating the difference between the normal and abnormal segments.
In individuals suspected of suffering from a supraventricular tachycardia (SVT), adenosine is used to help identify the rhythm. Certain SVTs can be successfully terminated with adenosine.[4] This includes any re-entrant arrhythmias that require the AV node for the re-entry (e.g., AV reentrant tachycardia (AVRT), AV nodal reentrant tachycardia (AVNRT). In addition, atrial tachycardia can sometimes be terminated with adenosine.
Adenosine has an indirect effect on atrial tissue causing a shortening of the refractory period. When administered via a central lumen catheter, adenosine has been shown to initiate atrial fibrillation because of its effect on atrial tissue. In individuals with accessory pathways, the onset of atrial fibrillation can lead to a life threatening ventricular fibrillation.
Fast rhythms of the heart that are confined to the atria (e.g., atrial fibrillation, atrial flutter) or ventricles (e.g., monomorphic ventricular tachycardia) and do not involve the AV node as part of the re-entrant circuit are not typically converted by adenosine. However, the ventricular response rate is temporarily slowed with adenosine in such cases.
Because of the effects of adenosine on AV node-dependent SVTs, adenosine is considered a class V antiarrhythmic agent. When adenosine is used to cardiovert an abnormal rhythm, it is normal for the heart to enter ventricular asystole for a few seconds. This can be disconcerting to a normally conscious patient, and is associated with angina-like sensations in the chest.[5]
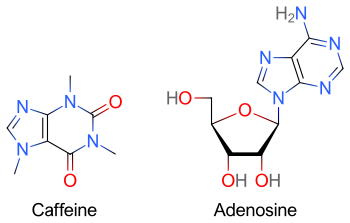
By nature of caffeine's purine structure it binds to some of the same receptors as adenosine. The pharmacological effects of adenosine may therefore be blunted in individuals who are taking large quantities of methylxanthines (e.g., caffeine, found in coffee and tea, or theobromine, as found in chocolate).
Action in the central nervous system
Generalized, adenosine has an inhibitory effect in the central nervous system (CNS). Caffeine's stimulatory effects, on the other hand, are primarily (although not entirely) credited to its inhibition of adenosine by binding to the same receptors, and therefore effectively blocking adenosine receptors in the CNS. This reduction in adenosine activity leads to increased activity of the neurotransmitters dopamine and glutamate.
Dosage
When given for the evaluation or treatment of a supraventricular tachycardia (SVT), the initial dose is 6 mg, given as a fast intravenous/Intraosseous infusion push. Due to adenosine's extremely short half-life, the IV line is started as proximal (near) to the heart as possible, such as the antecubital fossa (the depression in front of the elbow.) The IV push is often followed with an immediate flush of 5-10ccs of saline. If this has no effect (e.g., no evidence of transient AV block), a 12mg dose can be given 1-2 minutes after the first dose. If the 12mg dose has no effect, a second 12mg dose can be administered 1-2 minutes after the previous dose. Some clinicians may prefer to administer a higher dose (typically 18 mg), rather than repeat a dose that apparently had no effect. When given to dilate the arteries, such as in a "stress test", the dosage is typically 0.14 mg/kg/min, administered for 4 or 6 minutes, depending on the protocol.
The recommended dose may be increased in patients on theophylline since methylxanthines prevent binding of adenosine at receptor sites. The dose is often decreased in patients on dipyridamole (Persantine) and diazepam (Valium) because adenosine potentiates the effects of these drugs. The recommended dose is also reduced by half in patients who are presenting Congestive Heart Failure, Myocardial Infarction, shock, hypoxia, and/or hepatic or renal insufficiency, and in elderly patients.
Drug interactions
Dopamine may precipitate toxicity in the patient. Carbamazepine may increase heart block. Theophylline and caffeine (methylxanthines) competitively antagonize adenosine's effects; may require increased dose of adenosine.
Contraindications
Contraindications for adenosine are e.g.:
- Poison/Drug induced tachycardia
- Asthma, relative contraindication (however, selective adenosine agonists are being investigated for use in treatment of asthma)[6]
- 2nd or 3rd degree heart block
- Atrial fibrillation
- atrial flutter
- Ventricular tachycardia
- Sick sinus syndrome
- Stokes-Adams Attack
- bradycardia with Premature Ventricular Contractions (PVCs)
In Wolff-Parkinson-White syndrome adenosine may be administered if equipment for cardioversion is immediately available as a backup.
Side effects
Many individuals experience facial flushing, lightheadedness, asystole, diaphoresis, or nausea after administration of adenosine due to its vasodilatory effects. Metallic taste is a hallmark side effect of adenosine administration. These symptoms are transitory, usually lasting less than one minute. It is classically associated with a sense of "impending doom"(Or a feeling of death), more prosaically described as apprehension. This lasts a few seconds after administration intravenously. In some cases adenosine can make patients' limbs feel numb for about 2-5 minutes after administration intravenously depending on the dosage (usually above 12mg), during the emidiant effect of the drug patients will be in pain for about 2-10 seconds.
Metabolism
When adenosine enters the circulation, it is broken down by adenosine deaminase, which is present in red cells and the vessel wall.
Dipyridamole, an inhibitor of adenosine deaminase, allows adenosine to accumulate in the blood stream. This causes an increase in coronary vasodilatation.
See also
References
This article needs additional citations for verification. (December 2007) |
- ^ Haskó G, Linden J, Cronstein B, Pacher P (2008). "Adenosine receptors: therapeutic aspects for inflammatory and immune diseases". Nat Rev Drug Discov. 7 (9): 759–70. doi:10.1038/nrd2638. PMC 2568887. PMID 18758473.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Nakav S, Chaimovitz C, Sufaro Y; et al. (2008). "Anti-inflammatory preconditioning by agonists of adenosine A1 receptor". PLoS ONE. 3 (5): e2107. doi:10.1371/journal.pone.0002107. PMC 2329854. PMID 18461129.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) CS1 maint: unflagged free DOI (link) - ^ Trevethick MA, Mantell SJ, Stuart EF, Barnard A, Wright KN, Yeadon M (2008). "Treating lung inflammation with agonists of the adenosine A2A receptor: promises, problems and potential solutions". Br. J. Pharmacol. 155 (4): 463–74. doi:10.1038/bjp.2008.329. PMID 18846036.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Mitchell J, Lazarenko G (2008). "Wide QRS complex tachycardia. Diagnosis: Supraventricular tachycardia with aberrant conduction; intravenous (IV) adenosine". CJEM. 10 (6): 572–3, 581. PMID 19000353.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Pijls, Nico H. J. (2000). Coronary Pressure. Springer. ISBN 0792361709.
{{cite book}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Brown RA, Spina D, Page CP (2008). "Adenosine receptors and asthma". Br. J. Pharmacol. 153 Suppl 1: S446–56. doi:10.1038/bjp.2008.22. PMID 18311158.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link)
