Female genital mutilation
| Part of a series on |
| Violence against women |
|---|
| Killing |
| Sexual assault and rape |
| Disfigurement |
| Other issues |
|
| International legal framework |
| Related topics |
Female genital mutilation (FGM), also known as female genital cutting (FGC), female circumcision, or female genital mutilation/cutting (FGM/C), is defined by the World Health Organization (WHO) as "all procedures that involve partial or total removal of the external female genitalia, or other injury to the female genital organs for non-medical reasons."[1]
FGM may be carried out in hospitals under general anaesthesia, or by traditional circumcisers using crude tools, with local anaesthesia or none, predominantly on girls between infancy and the age of 15. According to the WHO, it is practised mostly in western, eastern, and north-eastern regions of Africa, parts of Asia and the Middle East, and within some immigrant communities in Europe and North America.[1] Amnesty International estimated in 1997 that 135 million females around the world had experienced genital mutilation.[2]
There are four classifications of FGM: Type 1, excision of the prepuce, the skin around the clitoris, with or without partial or complete removal of the clitoris (clitoridectomy); Type 2, excision of the clitoris with partial or complete removal of the labia minora; Type 3 (infibulation), excision of all or part of the labia minora and labia majora, and the stitching of a seal across the vagina, leaving only a small opening for the passage of urine and menstrual blood; and Type 4, miscellaneous acts, including burning or cauterization of the clitoris, scraping and cutting of the vagina (gishiri cutting), and introducing corrosive substances into the vagina to tighten it.[3]
Opposition to the practice focuses on the lack of informed consent and the health consequences, which can include chronic pain, infertility, repeated surgery to open the closure for intercourse and childbirth, recurrent infections and cysts, damage to the anus, difficulty giving birth, and increased risk of newborn death.[4] In the past few decades, there have been concerted efforts by the WHO, the United Nations Children's Fund (UNICEF), and the United Nations Population Fund (UNFPA) to end the practice. Since 2003, the International Day of Zero Tolerance to Female Genital Mutilation has been held each February 6, sponsored by the United Nations.[5]
Background
Terminology
The term "female circumcision" has commonly been used, but increasingly "female genital mutilation" has become dominant within the international community.[6] The WHO recommended that the UN adopt the term in 1991. In a 2005 report for UNICEF, Alexia Lewnes argued that the word "mutilation" differentiates the act from male circumcision and stresses the severity of it.[7]
In areas where the practice is common, the term "cutting" is more commonplace because of concerns from parents who do not believe they are mutilating their daughters, and some organizations have therefore adopted the term "female genital cutting" (FGC).[8] The UN Special Rapporteur on Traditional Practices has suggested that using tact in this area avoids the risk of "demonizing" certain cultures, religions, and communities.[7] Ellen Gruenbaum wrote in 2001 that "female circumcision" avoided causing offence, whereas the word "mutilation" appears to accuse practitioners of evil intent.[9] Other organizations (e.g., UNFPA, USAID) use the combined term "female genital mutilation/cutting" (FGM/C). USAID argues that the word "mutilation" does not take cultural differences into consideration.[10]
History and reasons for the practice
The practice is widely believed to have originated in Ancient Egypt and the Nile valley at the time of the Pharaohs. A Greek papyrus from 163 BCE mentions its occurrence in Egypt, and evidence from mummies has shown both Type I and Type III FGM.[11] Comfort Momoh, an FGM specialist in England, writes that Herodotus referred to it, saying that the Phoenicians, Hittites, Ethiopians, and Egyptians practised it, and that many commentators believe it arose in primitive communities out of a desire to control women's sexual behavior. She writes that there is evidence it was practised in the 19th century by gynaecologists in the United Kingdom and United States to "cure" insanity, masturbation, and nymphomania.[12]
The 14th-century Islamic text Umdat al-Salik wa-'Uddat al-Nasik ("Reliance of the Traveller") states that circumcision is obligatory for women and men: "For men it consists of removing the prepuce from the penis, and for women, removing the prepuce (Ar. bazr) of the clitoris (n: not the clitoris itself, as some mistakenly assert)."[13] Al-Azhar Supreme Council of Islamic Research, the highest religious authority in Egypt, issued a statement in 2007 that FGM had no basis in core Islamic law or any of its partial provisions, and should not be practiced.[14] Coptic Pope Shenouda, the leader of Egypt's minority Christian community, said in 2001 that the procedure is not required for religious reasons.[15]
The World Health Organization writes that where FGM is practised, it is considered part of raising a girl properly, ensuring premarital virginity, and making illicit sexual encounters difficult, both before and during marriage. As well as reducing the woman's libido, women fear the pain of re-opening the vagina, and are afraid of being discovered if it is opened illicitly. In addition, women are regarded as "clean" after surgery to remove "unclean" or "male" body parts. According to WHO, local power structures perpetuate the practice, including religious leaders and some medical personnel.[1]
Classification
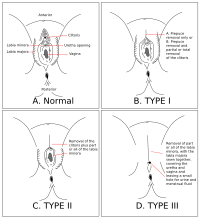
FGM consists of several distinct procedures. The WHO divides them into four major types[16] (see Diagram 1), although there is some debate as to whether all common forms of FGM fit into these four categories, as well as issues with the reliability of reported data.[17]
Type I
The WHO defines Type I FGM as the partial or total removal of the clitoris (clitoridectomy) and/or the prepuce (clitoral hood); see Diagram 1B. When it is important to distinguish between the variations of Type I, the following subdivisions are proposed: Type Ia, removal of the clitoral hood or prepuce only (which some view as analogous to male circumcision and thus more acceptable); Type Ib, removal of the clitoris with the prepuce.[16] In the context of women who seek out labiaplasty, there is disagreement among doctors as to whether to remove the clitoral hood in some cases to enhance sexuality or whether this is too likely to lead to scarring and other problems.[18]
Type II
The WHO's definition of Type II FGM is "partial or total removal of the clitoris and the labia minora, with or without excision of the labia majora. When it is important to distinguish between the major variations that have been documented, the following subdivisions are proposed: Type IIa, removal of the labia minora only; Type IIb, partial or total removal of the clitoris and the labia minora; Type IIc, partial or total removal of the clitoris, the labia minora and the labia majora.[16]
Type III: infibulation with excision
The WHO defines Type III FGM as narrowing of the vaginal orifice with creation of a covering seal by cutting and repositioning the labia minora and/or the labia majora, with or without excision of the clitoris (infibulation)."[19] It is the most extensive form of FGM, and accounts for about 10% of all FGM procedures described from Africa.[1] Infibulation is also known as "pharaonic circumcision".[20]
In a study of infibulation in the Horn of Africa, Pieters observed that the procedure involves extensive tissue removal of the external genitalia, including all of the labia minora and the inside of the labia majora. The labia majora are then held together using thorns or stitching. In some cases the girl's legs have been tied together for two to six weeks, to prevent her from moving and to allow the healing of the two sides of the vulva. Nothing remains but the walls of flesh from the pubis down to the anus, with the exception of an opening at the inferior portion of the vulva to allow urine and menstrual blood to pass through; see Diagram 1D. Generally, a practitioner recognized as having the necessary skill carries out this procedure, and a local anesthetic is used. However, when carried out "in the bush", infibulation is often performed by an elderly matron or midwife of the village, without sterile procedure or anesthesia.[21] Comfort Momoh describes a Type III procedure in Female Genital Mutilation (2005):

In Type 3 excision or infibulation ... elderly women, relatives and friends secure the girl in the lithotomy position. A deep incision is made rapidly on either side from the root of the clitoris to the fourchette, and a single cut of the razor excises the clitoris and both the labia majora and labia minora.
Bleeding is profuse, but is usually controlled by the application of various poultices, the threading of the edges of the skin with thorns, or clasping them between the edges of a split cane. A piece of twig is inserted between the edges of the skin to ensure a patent foramen for urinary and menstrual flow. The lower limbs are then bound together for 2–6 weeks to promote haemostatis and encourage union of the two sides ...
Healing takes place by primary intention, and, as a result, the introitus is obliterated by a drum of skin extending across the orifice except for a small hole. Circumstances at the time may vary; the girl may struggle ferociously, in which case the incisions may become uncontrolled and haphazard. The girl may be pinned down so firmly that bones may fracture.[3]
A reverse infibulation can be performed to allow for sexual intercourse or when undergoing labor, or by female relatives, whose responsibility it is to inspect the wound every few weeks and open it some more if necessary. During childbirth, the enlargement is too small to allow vaginal delivery, and so the infibulation is opened completely and may be restored after delivery. Again, the legs are sometimes tied together to allow the wound to heal. When childbirth takes place in a hospital, the surgeons may preserve the infibulation by enlarging the vagina with deep episiotomies. Afterwards, the patient may insist that her vulva be closed again.[21]
Women who have been infibulated face a lot of difficulty in delivering children, especially if the infibulation is not undone beforehand, which often results in severe tearing of the infibulated area, or fetal death if the birth canal is not cleared (Toubia, 1995). The risk of severe physical, and psychological complications is more highly associated with women who have undergone infibulations as opposed to one of the lesser forms of FGM. Although there is little research on the psychological side effects of FGM, many women feel great pressure to conform to the norms set out by their community, and suffer from anxiety and depression as a result (Toubia, 1995). "There is also a higher rate of post-traumatic stress disorder in circumcised females" (Nicoletti, 2007, p. 2). [22] [23]
A five-year study of 300 women and 100 men in Sudan found that "sexual desire, pleasure, and orgasm are experienced by the majority (nearly 90%) of women who have been subjected to this extreme sexual mutilation, in spite of their being culturally bound to hide these experiences."[24]
Type IV: other types
There are other forms of FGM, collectively referred to as Type IV, that may not involve tissue removal. The WHO defines Type IV FGM as "all other harmful procedures to the female genitalia for non-medical purposes, for example, pricking, piercing, incising, scraping and cauterization." This includes a diverse range of practices, such as pricking the clitoris with needles, burning or scarring the genitals as well as ripping or tearing of the vagina.[16] Gishiri cutting, a practice in which the vagina's anterior wall is cut with a knife to enlarge it, is also included in this category.
Health effects

The UNFPA and WHO state that FGM has both immediate and long-term consequences to the health of women. Immediate complications include severe pain, shock, haemorrhage, tetanus or infection, urine retention, ulceration of the genital region and injury to adjacent tissue, wound infection, urinary infection, fever and septicaemia. Haemorrhage and infection can be of such magnitude as to cause death.
Long-term consequences include anemia, the formation of cysts and abscesses, keloid scar formation, damage to the urethra resulting in urinary incontinence, dyspareunia (painful sexual intercourse) and sexual dysfunction, hypersensitivity of the genital area. Infibulation can cause severe scar formation, difficulty in urinating, menstrual disorders, recurrent bladder and urinary tract infection, fistulae, prolonged and obstructed labour (sometimes resulting in fetal death and vesico-vaginal fistulae and/or vesico-rectal fistulae), and infertility (as a consequence of earlier infections). Cutting of the scar tissue is sometimes necessary to facilitate sexual intercourse and/or childbirth. Almost complete vaginal obstruction may occur, resulting in accumulation of menstrual flow in the vagina and uterus. During childbirth the risk of hemorrhage and infection is greatly increased.
Among practising cultures, FGM is most commonly performed between the ages of four and eight, but can take place at any age from infancy to adolescence. Prohibition has led to FGM going underground, at times with people who have had no medical training performing the procedure without anesthetic, sterilization, or the use of proper medical instruments. The procedure can lead to death through shock from excessive bleeding. The failure to use sterile medical instruments may lead to infections.

Several countries outside areas where FGM is traditionally performed have laws banning the practice. Other serious long term health effects are also common. These include urinary and reproductive tract infections, caused by obstructed flow of urine and menstrual blood, various forms of scarring and infertility. Epidermal inclusion cysts may form and expand, particularly in procedures affecting the clitoris. These cysts can grow over time and can become infected, requiring medical attention such as drainage.[25] The first episode of sexual intercourse will often be extremely painful for infibulated women, who will need the labia majora to be opened, to allow their partner access to the vagina. This second cut, sometimes performed by the partner with a knife, can cause other complications to arise.
A June 2006 study by the WHO has cast doubt on the safety of genital mutilation of any kind.[19] This study was conducted on a cohort of 28,393 women attending delivery wards at 28 obstetric centers in areas of Burkina Faso,Ghana, Kenya, Senegal and The Sudan. A high proportion of these mothers had undergone FGM. According to the WHO criteria, all types of FGM were found to pose an increased risk of death to the baby (15% for Type I, 32% for Type II, and 55% for Type III). Mothers with FGM Type III were also found to be 30% more at risk forcesarean sections and had a 70% increase in postpartum hemorrhage compared to women without FGM. Estimating from these results, and doing a rough population estimate of mothers in Africa with FGM, an additional 10 to 20 per thousand babies in Africa die during delivery as a result of the mothers having undergone genital mutilation.
In cases of repairing the damage resulting from FGM, called de-infibulation when reversing Type III FGM, this is usually carried out by a gynecologist. See also Pierre Foldes, a French surgeon, who developed modern surgical corrective techniques.
A 12-year-old Egyptian girl, Badour Shaker, died in June 2007 during or soon after undergoing an FGM procedure, prompting the Egyptian Health Ministry to ban the practice. She died from an overdose of anesthesia. The girl's mother, Zeinab Abdel Ghani, paid the equivalent of US$9.00 (£4.60 pounds sterling, €6.82 euro) to a female doctor, in an illegal clinic in the southern town of Maghagh, for the operation. The mother stated that the doctor tried to give her $3,000 to withdraw a lawsuit, but she refused.[26]
HIV
Accordingly to a statement of the UNFPA the procedure is coupled with the loss of blood and use is often made of one instrument for a number of operations, the risk of HIV/AIDS transmission is increased by the practice. Also, due to damage to the female sexual organs, sexual intercourse can result in lacerations of tissues, which greatly increases risk of transmission. The same is true for childbirth and subsequent loss of blood.[27]
Relatively little research has been conducted on the effect female genital alteration may have on HIV prevalence.[28] Some studies have found increased risk of HIV among women who had undergone FGM.[29] Other studies have found no statistically significant associations,[30] or have identified more complex patterns.[31] Two studies have reported that FGM is associated with decreased risk of HIV.[32]
Kanki et al. (1992) reported that, in Senegalese prostitutes, women who had undergone FGM had a significantly decreased risk of HIV-2 infection when compared to those who had not.[33] Klouman et al. (2005), studying women in Tanzania, found that among women who had undergone FGM the odds of being HIV positive were roughly twice those among women who had not. However, both HIV and FGM were strongly associated with age; when controlling for age, the association was no longer statistically significant.[34]
Brewer et al. (2007) found that in virgins, FGM was associated with a higher prevalence of HIV infection (3.2% vs 1.4%), which the authors attributed to non-sterile procedures. Among sexually experienced women, FGM was associated with lower HIV prevalence (5.5% vs 9.9%). The authors suggested two possible reasons: that an HIV-specific immunity might be acquired through FGM procedures, and mortality of those infected at the time of FGM would reduce HIV prevalence in surviving adults.[35] Maslovskaya et al. (2009) found that FGM was associated with higher risk of HIV among women whose first-union partner was younger or the same-age, but it was associated with lower risk of HIV among women whose first-union partner was older than the women herself.[31] Yount et al. reported that, although FGM and HIV were not directly related, FGM was indirectly related to HIV via a number of associations with other factors, including extra-union partners, early onset of sexual activity, being widowed or divorced, and having an older partner. The authors concluded that FGM "may be an early life-course event that indirectly alters women's odds of becoming infected with HIV through protective and harmful practices in adulthood".[36]
Stallings et al. (2009) reported that, in Tanzanian women, the risk of HIV among women who had undergone FGM was roughly half that of women who had not.[32] Recent reviews have suggested that FGM may increase the risk of HIV.[37] Several mechanisms have been proposed. These include: non-sterile procedures (Emmanuel Monjok notes that the same instrument is frequently used on 15–20 girls); an increase in blood transfusions due to blood loss during the procedure itself, intercourse, or childbirth; increased anal intercourse due to difficult or painful vaginal intercourse; tearing of the vagina during intercourse;[28] and increased susceptibility to infectious conditions that are recognized risk factors for HIV, such as genital ulcers.[38]
Psychological consequences
The UNFPA states that FGM may leave a lasting mark on the life and mind of the woman who has undergone the procedure. The psychological stress may trigger behavioural disturbances in children, closely linked to the loss of trust and confidence in care-givers. In the longer term, women may suffer feelings of anxiety, depression, and frigidity. Sexual dysfunction may also be the cause for marital conflicts and eventual divorce.[39]
In 1994, Sudanese surgeon Nahid Toubia reported that in her clinical experience, "many infibulated women have a syndrome of chronic anxiety and depression arising from worry over the state of their genitals, intractable dysmenorrhea, and the fear of infertility."[22] Toubia also said that while a few cases of psychopathologic disorders directly attributable to FGM had been reported,[40] for most women, "the psychological effects are often subtle and are buried in layers of denial and acceptance of social norms". [22]
In 2001 Abusharaf published a study that gathered interviews from Sudan during 1996 to 1998 that their questioned women's gender ideologies related to female circumcision and what they considered pure and feminine. The women Abusharaf interviewed provided their reasoning for circumcision "as an act that commemorates virtue and hallows morality,""a ritual contributing to the cultural construction of gender, womanhood, and 'appropriate' sexuality, a part of the process of achieving full personhood within (the) culture."[41] Abusharaf notes that "the tenacity of this ritual cannot be understood in isolation from emotional and cognitive processes, kin and social relationships, accountability, morality, ideas about femininity and masculinity, or from the relations of power that prevail in the country," and that "female circumcision has no meaning apart from other dominant ideologies, and these ideologies in turn combine to shape common moralities and codes of ethics in the communities."[41]
In February 2010, a study by Pharos, a Dutch group which gathers information on health care for refugees and migrants,[42] found that many women who have undergone FGM suffer psychiatric problems. This was the first study into the psychiatric and social complaints associated with female genital mutilation. In the study 66 questioned Dutch African women, who had been subjected to the practice, were found to be "stressed, anxious and aggressive". It also found that they were more likely to have relational problems or in some cases had fears of establishing a relationship. According to the study, an estimated 50 women or girls are believed to undergo FGM every year in the Netherlands. The report was published to mark the International day against female genital mutilation.[42][43]
Amnesty International suggest that the trauma of the procedure may lead to more docile behaviour in women who had been subjected to the practice. They note that, although little scientific research has been done, anecdotal evidence indicates feelings of "anxiety, terror, humiliation and betrayal" in these women. However, they state that the "most important psychological effect on a woman who has survived is the feeling that she is acceptable to her society, having upheld the traditions of her culture and made herself eligible for marriage, often the only role available to her", postulating that women who refused might suffer psychological problems due to rejection by their community.[44]
Sexual effects
According to UNICEF, FGM can lead to painful sexual intercourses, sexual frigidity and infertility.[45] During three separate six-month studies within the timespan of 5 years Lightfoot-Klein interviewed 11.1% Sudanese men and 88.8% Sudanese women. These people had various occupations including, but not limited to, gynecologists, pediatricians, psychiatrists, nurses, midwives, mothers of pediatric patients, religious leaders, and village women and men. In Sudanese culture, Pharaonic circumcision is considered a way to decrease sexual sensitivity of the naturally morally corrupt young women thereby weakening their desire for sex. It is also considered a preventative against rape.[46] Sudanese people believe as a matter of course the role of men is to inflict pain, and the role of women is to receive it.[46] Lightfoot commented that women usually reported no sexual desire or sexual enjoyment when questioned in clinical environments.[46] Brides are expected to act in a submissive manner to present a modest state, but penetration
takes anywhere from 3 or 4 days to several months. Some men are unable to penetrate their wives at all (in my study over 15%), and the task is often accomplished by a midwife under conditions of great secrecy, since this reflects negatively on the man's potency. Some who are unable to penetrate their wives manage to get them pregnant in spite of the infibulation, and the woman's vaginal passage is then cut open to allow birth to take place. A great deal of marital anal intercourse takes place in cases where the wife can not be penetrated (...) Those men who do manage to penetrate their wives do so often, or perhaps always, with the help of the "little knife." This creates a tear which they gradually rip more and more until the opening is sufficient to admit the penis. In some women, the scar tissue is so hardened and overgrown with keloidal formations that it can only be cut with very strong surgical scissors, as is reported by doctors who relate cases where they broke scalpels in the attempt.[46]
Women are expected to be completely passive through the whole ordeal, and if she does reach orgasm, she is expected to control her emotions. In spite of the process, women reported their husbands were tender and loving. "Nearly 90% of all women interviewed said that they experienced orgasm (climax) or had at various periods of their marriage experienced it (...) Frequently, intractible pain, a residual of the circumcision, prevented orgasm altogether."[46]
Reversal
In recent years, surgical techniques to reverse FGM have been developed by gynecologists such as Dr. Pierre Foldes and Dr. Marci Bowers. Techniques can include ablating scar tissue, reconstructing the labia, and drawing the internal part of the clitoris outward to compensate for clitoral excision.[47] Clitoraid, a non-profit international organization, is in the process of building a hospital in Burkina Faso, West Africa, where women who have undergone FGM will be able to receive this procedure free of charge. The hospital will be staffed with volunteers, including surgeons who specialize in the technique.[48]
Attempts to end the practice

Despite laws forbidding the practice, FGM remains an enduring tradition in many societies and cultural groups. Political leaders have found FGM difficult to eliminate on the local level because of its cultural and sometimes political importance.[49] For instance, in Kenya, missionaries present in the 1920s and 1930s forbade their Christianized adherents to practice clitoridectomy. In response, FGM became instrumental to the ethnic independence movement among the Kikuyu, the most populous ethnic group of Kenya – indigenous people reacted against what they perceived as cultural imperialistic attacks by Europeans.[50] Likewise, prohibition by the British of the procedure among tribes in Kenya significantly strengthened the tribes' resistance to British colonial rule in the 1950s and increased support for the Mau Mau guerrilla movement.[51]
Because the practice holds much cultural and marital significance, FGM opponents recognize that ending it requires that they work closely with local communities. To leave no individuals handicapped, as happened with the rapid abandonment of foot binding among the Chinese early in the 20th century,[52] members of a marriage network must all give up the practice simultaneously.
Despite the close tie between FGM and cultural and, sometimes, religious tradition, there are cases where attempts at ending FGM have been successful. One example is in Senegal, where initiative was taken by native women working at the local level in connection with the NGO Tostan.[53] Since 1997, 4,203 communities in Senegal, 364 in Guinea, 23 in Burkina Faso, 24 in The Gambia, and 14 in Somalia have voluntarily given up FGM and are also working to end early and forced marriage.[54] This has come about through the voluntary efforts of locals carrying the message out to other villages within their marriage networks in a self-replicating process. The expansion of community declarations, beginning in the village of Malicounda Bambara in 1997 and continuing to grow, "show the replicability of the Tostan program for large-scale abandonment of this practice". Molly Melching, founder of Tostan, and UNICEF believe that in Senegal the practice of female genital mutilation could be ended by 2015. She credits education, instead of cultural imperialism, for the rapid and significant changes in Senegal.
Sudanese surgeon Nahid Toubia founded and leads Research, Action and Information Network for the Bodily Integrity of Women (Rainbo), an international organisation which works to eliminate FGM through women’s self-empowerment and social change. Rainbo played a prominent role in changing the view of FGM from being a predominantly medical concern to a human rights issue.[55] In 2002 Toubia told the BBC World Service that the campaign against FGM was fundamentally about changing women's consciousness, and empowering them to change their social position. She said while most African governments, health professionals and NGOs had the issue on their agenda, the greatest challenge was at grassroots level. She said "By allowing your genitals to be removed [it is perceived that] you are heightened to another level of pure motherhood - a motherhood not tainted by sexuality and that is why the woman gives it away to become the matron, respected by everyone. By taking on this practise, which is a woman's domain, it actually empowers them. It is much more difficult to convince the women to give it up, than to convince the men." [56]
Some countries that prohibited FGM still experience the practice in secrecy. In many cases, enforcement of this prohibition is a low priority for governments. Other countries have tried to educate practitioners to make it easier and safer instead of outlawing the practice entirely. However, with pressure from the WHO and other groups, laws are being passed in regards to FGM. On June 28, 2007 Egypt banned female genital mutilation after the death of 12-year-old Badour Shaker during an FGM procedure; The Guardian reported that her death "sparked widespread condemnation" of the practice.[26] Britain has had its own problem confronting cases of FGM, as immigrants from Africa have been known to send their daughters to their home nations to undergo the procedure before returning to Britain.
In Mauritania, where "health campaigners estimate that more than 70% of Mauritanian girls undergo the partial or total removal of their external genitalia for non-medical reasons", 34 Islamic scholars signed a fatwa banning the practice in January 2010. Their aim was to prevent people from citing religion as a justification for genital mutilation.[57]
There are two main anti-FGM frameworks: the health model and the human rights-based model.[citation needed] The health model campaign defines FGM as harmful to women's health (physical and psychological trauma, sterility, damage to the urethra and anus, tetanus, child and maternal mortality and more recently HPV and HIV infection). This approach has failed to bring about large scale behavioral change.[citation needed] Furthermore, although the health model is against FGM and the adverse effects associated, it often rejects methods to provide medical support to minimize FGM health risks (i.e. medicalization). The human rights-based model has in more recent times replaced the health based model as the preferred approach in anti-FGM campaigns. The human rights model encompasses four important human rights discourses: violence against women, rights of the child, freedom from torture and rights to health and bodily integrity.
Prevalence
General


Amnesty International estimates that over 130 million women worldwide have been affected by some form of FGM, with over three million girls at risk every year.[2] It is mainly practised in 28 African countries, in a band that stretches from Senegal in West Africa to Ethiopia on the east coast, as well as from Egypt in the north to Tanzania in the south.[58] It is also practised by some groups in the Arabian peninsula, particularly Egypt, followed by Sudan, Ethiopia, and Mali, though Egypt passed a law banning FGM in 2008.[59]
In the Arabian peninsula, Types I and II FGM are usually performed, often referred to as "Sunna circumcision," especially among Afro-Arabs (ethnic groups of African descent are more likely to prefer infibulation). The practice occurs particularly in northern Saudi Arabia, southern Jordan, and northern Iraq (Kurdistan).[60][61] In the Iraqi village of Hasira, a study found that 60 percent of the females reported having undergone FGM.[60] There is also circumstantial evidence to suggest that FGM is practised in Syria.[62] In Oman, a few communities still practice it, though experts believe the number is small and declining annually. In the United Arab Emirates and Saudi Arabia, it is practiced mainly among foreign workers from East Africa and the Nile Valley. A 2009 study suggested that FGM had virtually disappeared among the Negev Bedouin because of modernization under Israeli rule.[63]
The practice can also be found among a few ethnic groups in South America.[58] In Indonesia, it is common in several districts; almost all are Type I or Type IV. Sometimes the procedures are merely symbolic, and no actual cutting is done.[64] As a result of immigration, FGM has also spread to Europe, Australia, and the United States, with some families having their daughters undergo the procedure while on vacation overseas. As Western governments become more aware of FGM, legislation has come into effect in many countries to make the practice a criminal offense. In 2006, Khalid Adem became the first man in the United States to be prosecuted for circumcising his daughter.[65]
Legal status
Africa
In July 2003 at its second summit, the African Union adopted the Maputo Protocol promoting women's rights including and to end FGM. It came into force in November 2005, and by December 2008, 25 member countries had ratified it.[66] Other information in this section is from Skaine (2005), Appendix I.[11]
- Burkina Faso (73% prevalence, Type II)
- A law prohibiting FGM was enacted in 1996 and went into effect in February 1997. Even before this law, however, a presidential decree had set up the National Committee against excision and imposed fines on people guilty of excising girls and women.[66] The new law includes stricter punishment. Several women excising girls have been handed prison sentences.[69] Burkina Faso ratified the Maputo Protocol in 2006.
- Cameroon (20% prevalence, Type I and II)
- Female genital mutilation is prevalent in Cameroon.[68][70]
- Central African Republic (43.4% prevalence, Type I and II)
- In 1996, the President issued an Ordinance prohibiting FGM throughout the country. It has the force of national law. Any violation of the Ordinance is punishable by imprisonment of from one month and one day to two years and a fine of 5,100 to 100,000 francs (approximately US$8–160). No arrests are known to have been made under the law.
- Chad (60% prevalence, Type II and III)
- In 2001 law was being drafted to specifically outlaw FGM. Prior to this it may have been a punishable offence under existing laws protecting minors from involuntary physical assault.[66]
- Côte d'Ivoire (44.5% prevalence, Type II)
- A December 18, 1998 law provides that harm to the integrity of the genital organ of a woman by complete or partial removal, excision, desensitization or by any other procedure will, if harmful to a women's health, be punishable by imprisonment of one to five years and a fine of 360,000 to two million CFA Francs (approximately US$576–3,200). The penalty is five to twenty years incarceration if a death occurs during the procedure and up to five years' prohibition of medical practice, if this procedure is carried out by a doctor.[66]
- Democratic Republic of the Congo (5% prevalence, Type II)
- Female genital mutilation is practiced in the Congo.[68][70]
- Djibouti (90–98% prevalence, Type II and III)
- FGM was outlawed in the country's revised Penal Code that went into effect in April 1995. Article 333 of the Penal Code provides that persons found guilty of this practice will face a five year prison term and a fine of one million Djibouti francs (approximately US$5,600). Djibouti ratified the Maputo Protocol in 2005.[66]
- Egypt (78–97% prevalence, Type I, II and III)
- Egypt's Ministry of Health and Population has banned all forms of female genital mutilation since 2007.[66] The ministry's order declared it is 'prohibited for any doctors, nurses, or any other person to carry out any cut of, flattening or modification of any natural part of the female reproductive system'. Islamic authorities in the nation also stressed that Islam opposes female genital mutilation. The Grand Mufti of Egypt, Ali Gomaa, said that it is "Prohibited, prohibited, prohibited."[72] The June 2007 Ministry ban eliminated a loophole that allowed girls to undergo the procedure for health reasons.[73] There had previously been provisions under the Penal Code involving "wounding" and "intentional infliction of harm leading to death", as well as a ministerial decree prohibiting FGM. In December 1997, the Court of Cassation (Egypt's highest appeals court) upheld a government banning of the practice providing that those who did not comply would be subjected to criminal and administrative punishments. This law had proved ineffective and in a survey in 2000, a study found that 97% of the country's population still practiced FGM. In light of the widespread practice of FGM, even after the ban in 1997, some Egyptian villages decided to voluntarily give up the practice, as was the case with Abou Shawareb, which vowed in July 2005 to end the practice.[citation needed] However, it remains a culturally accepted practice, and a 2005 study found that over 95% of Egyptian women have undergone some form of FGM.[74]
- Eritrea (90% prevalence, Type I, II, and III)
- Eritrea has outlawed all forms of female genital mutilation since 2007.[66][75]
- Ethiopia (69.7%–94.5% prevalence, Type I, II, III, and IV)
- Ethiopia's Regional statistics of the prevalence from the survey are: Afar Region – 94.5%; Harare Region – 81.2%; Amhara Region – 81.1%; Oromia Region – 79.6%; Addis Ababa City – 70.2%; Somali Region – 69.7%; Beneshangul Gumuz Region – 52.9%; Tigray Region – 48.1%; Southern Region – 46.3%. This practice is not specifically illegal in Ethiopia. Discussions with government officials and NGOs active in the eradication of these practices indicate that the legal provision for prohibiting harmful traditional practices and the policy statements against them are not, as a practical matter, enforced. There are no documented cases of women going to court over or seeking protection against this practice. We are unaware of any groups or organizations that provide protection to women or girls who wish to avoid it.[66][76]
- Gambia (80 – 90% prevalence, Type I,II,III and IV)
- Female genital mutilation is prevalent in Gambia.[68][70]
- Ghana (40% prevalence, Type I,II and III)
- Female genital mutilation is prevalent in Ghana.[71] In 1989, the head of the government of Ghana, President Rawlings, issued a formal declaration against FGM. Article 39 of Ghana's Constitution also provides in part that traditional practices that are injurious to a person's health and well being are abolished.[66] Ghana ratified the Maputo Protocol in 2007.
- Guinea (98.6% prevalence, Type I, II and III)
- FGM is illegal in Guinea under Article 265 of the Penal Code. The punishment is hard labor for life and if death results within 40 days after the crime, the perpetrator will be sentenced to death. No cases regarding the practice under the law have ever been brought to trial. Article 6 of the Guinean Constitution, which outlaws cruel and inhumane treatment, could be interpreted to include these practices, should a case be brought to the Supreme Court.[66] A member of the Guinean Supreme Court is working with a local NGO on inserting a clause into the Guinean Constitution specifically prohibiting these practices.[66] Guinea signed the Maputo Protocol in 2003 but has not ratified it.
- Guinea-Bissau (50% prevalence, no Data)
- Female genital mutilation is present in Guinea-Bissau.[70]
- Mauritania (71% prevalence, Type I and II)
- Female genital mutilation is prevalent in Mauritania.[68][70]
- Mozambique (No Data)
- Female genital mutilation is present in Mozambique.[71]
- Nigeria (25.1% prevalence, Type I, II and III)
- There is no federal law banning the practice of FGM in Nigeria. Opponents of these practices rely on Section 34(1)(a) of the 1999 Constitution of the Federal Republic of Nigeria that states "no person shall be subjected to torture or inhuman or degrading treatment" as the basis for banning the practice nationwide. A member of the House of Representatives has drafted a bill, not yet in committee, to outlaw this practice.[66] Nigeria ratified the Maputo Protocol in 2005.
- Republic of the Congo (5% prevalence, Type II)
- Female genital mutilation is practiced in the Republic of the Congo.[68][70]
- Senegal (20 – 30% prevalence, Type II and III)
- Female genital mutilation is prevalent in Senegal.[68][70] A law that was passed in January 1999 makes FGM illegal in Senegal. President Diouf had appealed for an end to this practice and for legislation outlawing it. The law modifies the Penal Code to make this practice a criminal act, punishable by a sentence of one to five years in prison. A spokesperson for the human rights group RADDHO (The African Assembly for the Defense of Human Rights) noted in the local press that "Adopting the law is not the end, as it will still need to be effectively enforced for women to benefit from it.[66] Senegal ratified the Maputo Protocol in 2005.
- Sierra Leone (90% prevalence, Type II)
- Female genital mutilation is practiced in Sierra Leone.[68][70]
- Somalia (98% prevalence, Type I and III)
- In 1999 Parliament approved legislation making FGM illegal although there is little evidence to support its enforcement.[66][78]
- South Africa (no data)
- Female genital mutilation is present in South Africa.[71]
- Sudan (91% prevalence, Type I, II and III)
- Currently there is no law forbidding FGM, although Sudan was the first country to outlaw it in 1946, under the British. Type III was prohibited under the 1925 Penal Code, with less severe forms allowed. Outreach groups have been trying to eradicate the practice for 50 years, working with NGOs, religious groups, the government, the media and medical practitioners. Arrests have been made but no further action seems to have taken place.[66] Sudan signed the Maputo Protocol in June, 2008 but no ratification has yet been deposited with the African Union.
- Tanzania (17.6% prevalence, Type II and III)
- Section 169A of the Sexual Offences Special Provisions Act of 1998 prohibits FGM. Punishment is imprisonment of from five to fifteen years or a fine not exceeding 300,000 shillings (approximately US$250) or both. There have been some arrests under this legislation, but no reports of prosecutions yet. Tanzania ratified the Maputo Protocol in 2007.
- Togo (50% prevalence, Type II)
- Female genital mutilation is practiced in Togo.[70] On October 30, 1998, the National Assembly unanimously voted to outlaw the practice of FGM. Penalties under the law can include a prison term of two months to ten years and a fine of 100,000 francs to one million francs (approximately US$160 to 1,600). A person who had knowledge that the procedure was going to take place and failed to inform public authorities can be punished with one month to one year imprisonment or a fine of from 20,000 to 500,000 francs (approximately US$32 to 800).[66] Togo ratified the Maputo Protocol in 2005.
- Uganda (<5% prevalence, Type I and II)
- Recently,[vague] a law was passed to outlaw genital mutilation. Under this law, anyone convicted of this practice is subject to 10 years in prison. If the life of the patient is lost during the operation a life sentence is recommended.[79] In 1996, however, a court intervened to prevent the performance of this procedure under Section 8 of the Children Statute, enacted that year, that makes it unlawful to subject a child to social or customary practices that are harmful to the child's health. Uganda signed the Maputo Protocol in 2003 but has not ratified it, despite calls from women's rights advocates.[80] In early July 2009, President Yoweri Museveni stated that a law would soon be passed prohibiting the practice, with alternative livelihoods found for its practitioners.[81]
Central and Southeast Asia
- Tajikistan (No Data avail.)
- Female genital mutilation is present in Tajikistan.[83]
- Indonesia (No national prevalence figures avail., Type I and IV)
- In 2006 FGM was banned by the government. However, since the ban the practice has undergone a resurgence, primarily due to promotion by religious groups such as Indonesian Ulema Council.[84]
- Malaysia (No national prevalence figures avail., Type IV)
- No laws exist in reference to FGM,[85] although the practice is reported in certain regions.[86]
Near – Middle East
- Afghanistan (no data available)
- Female genital mutilation is present in Afghanistan.[83]
- Iran (No national prevalence figures avail.)
- Female genital mutilation exists in Western and Southern Iran, primarily in Iranian Kurdistan where it is reported to be widespread, but also in regions such as Khuzestan.[62][87]
- Iraq, Iraqi Kurdistan (72.7% prevalence (excluding Dohuk), Type I and II[88])
- There is no law against FGM in Iraqi Kurdistan, but in 2007 a draft legislation condemning the practice was submitted to the Regional Parliament,[89] but was not passed.[89][90] but was not passed. A 2011 bill criminalizing the procedure was passed by the parliament of Iraqi Kurdistan and now awaits the ratification of President Massud Barzani.[91]
- Jordan (No national prevalence figures avail.)
- Female genital mutilation is prevalent in Jordan.[62]
- Pakistan (No national prevalence figures avail.)
- The practice is present in certain ethnic groups in Pakistan i.e. (Dawoodi Bohra Muslims).[94][95][96][97]
- Palestinian territories (No national prevalence figures avail.)
- Female genital mutilation is present in Palestinian territories.[94][98]
- Saudi-Arabia (No national prevalence figures avail.)
- Female gender mutilation is prevalent in Northern. Saudi-Arabia, but is declining.[62]
- Syria (No national prevalence figures avail.)
- Circumstantial evidence suggests Female genital mutilation exists in Syria.[62]
- Turkey (No national prevalence figures avail.)
- Circumstantial evidence suggests Female genital mutilation exists in Turkey.[62]
- United Arab Emirates(No national prevalence figures avail., Type I[100])
- The WHO mentions a study that documents Female genital mutilation in United Arab Emirates, but does not provide data.[16] A report at a conference in 2003 of the findings by the authors suggest that the practice is prevalent in rural and urban UAE, but is declining.[94][100]
- Yemen (23% prevalence in women 15 to 49[101])
- In addition to the adult prevalence,[94] UNICEF reports that 20% of women aged 15–49 have a daughter who had the procedure. According to the UNHCR in some coastel areas the prevalence was as high as 90%[102]
Eastern Europe
- Chechnya (No national prevalence figures avail.)
- Female genital mutilation is present in Chechnya, North Caucasus region.[103][104]
- Daghestan (No Data avail.)
- Female genital mutilation is present in Daghestan, North Caucasus region.[83][105]
- Ingushetia (No Data avail.)
- Female genital mutilation is present in Ingushetia, North Caucasus region.[83][105]
Other regions
- Australia
- In 1994 there were several anecdotal reports of FGM being practised amongst migrant communities in Australia.[106] By 1997, all Australian states and territories had made FGM a criminal offence. It is also a criminal offence to take, or propose to take, a child outside Australia to have a FGM procedure performed.[107] The incidence of FGM in Australia is unknown as it is unreported to authorities and is often only uncovered when women and girls are taken to hospital due to complications with the procedure.[108]
- Canada
- FGM is considered child assault and prohibited under sections 267 (assault causing bodily harm) or 268 (aggravated assault, including wounding, maiming, disfiguring) of the Criminal Code.[109][110]
- France
- FGM, like other forms of sexual mutilation, is a criminal offense punishable by up to 20 years in jail. In addition, the law requires anyone to report any case of mutilation or planned mutilation. This means that adults who send girls abroad to be excised can be pursued criminally in France.[111]
- Italy
- After a few cases of infibulation practiced by complaisant medical practitioners within the African immigrants community came to public knowledge through media coverage, the Law n°7/2006 was passed on 1/9/2006, becoming effective on 1/28/2006, concerning "Measures of prevention and prohibition of any female genital mutilation practice"; the Act is also known as the Legge Consolo ("Consolo Act") named after its primary promoter, Senator Giuseppe Consolo. Article 6 of the law integrates the Italian Penal Code with Articles 583-Bis and 583-Ter, punishing any practice of female genital mutilation "not justifiable under therapeutical or medical needs" with imprisonment ranging from 4 to 12 years (3 to 7 years for any mutilation other than, or less severe than, clitoridectomy, excision or infibulation). Penalty can be reduced up to 2⁄3 if the harm caused is of modest entity (i.e. if partially or completely unsuccessful), but may also be elevated up to 1⁄3 if the victim is a minor or if the offense has been committed for profit. An Italian citizen or a foreign citizen legally resident in Italy can be punished under this law even if the offense is committed abroad; the law will as well afflict any individual of any citizenship in Italy, even illegally or provisionally. The law also mandates any medical practitioner found guilty under those provisions to have his/her medical license revoked for a minimum of six up to a maximum of ten years.[112] The law gained general public consensus, and continues to receive nowadays support from several women's rights movements. Supporters of the law however input that more could yet be done to protect young girls within the communities of African immigrants from such practices, as it is reported that "the girls go on vacation in their families' homelands to visit their grandparents and return infibulated".[113]
- Norway
- FGM is punishable as a criminal offense under Norwegian law even if the offence is committed abroad.
- Netherlands
- FGM is considered mutilation and is punishable as a criminal offense under Dutch law. There is no specific law against FGM: the act is subsumed under the general offense of inflicting harm ("mishandling", art. 300–304 Dutch Criminal Code). The maximum penalty is a prison sentence of 12 years. However, the sentence can be higher if the offender is a family member of the victim. It is also illegal to assist or encourage another person to perform FGM. A Dutch citizen or a foreign citizen legally resident in the Netherlands can be punished even if the offense is committed abroad. Doctors have the obligation to report suspected cases of FGM and may break patient confidentiality rules if necessary.
- New Zealand
- Under a 1995 amendment to the Crimes Act, it is illegal to perform "any medical or surgical procedure or mutilation of the vagina or clitoris of any person" for reasons of "culture, religion, custom or practice". It is also illegal to send or make any arrangement for a child to be sent out of New Zealand for FGM to be performed, assist or encourage any person in New Zealand to perform FGM on a New Zealand citizen or resident outside New Zealand convince or encourage any other New Zealand citizen or resident to go outside New Zealand to have FGM performed.[114]
- Spain
- The Criminal Code does state that sexual mutilation, such as FGM, is a criminal offense punishable by up to 12 years in jail.[115]
- Sweden
- FGM is punishable according to Act (1982:316) Prohibiting Female Genital Mutilation. Sweden was the first Western country to prohibit FGM, legislation against 'female circumcision' passed in 1982. In 1998 the law was revised with a change in terminology and more severe penalties for breaking the law were imposed. The law was further reformulated in 1999, to allow for prosecution in a Swedish court of someone performing FGM even if the act has been performed in a country where it is not considered criminal (removal of the principle of double incrimination).[116]
- United Kingdom
- FGM was made a specific criminal offense by the Prohibition of Female Circumcision Act 1985. A girl could be removed from her home, if this was the only way that her protection could be guaranteed.[117] This was superseded by the Female Genital Mutilation Act 2003, and (in Scotland) by the Prohibition of Female Genital Mutilation (Scotland) Act 2005. In addition to FGM within the UK, taking a UK citizen or permanent resident abroad for the purpose of FGM is a criminal offense whether or not it is lawful in the country that the girl is taken to.
- United States
- Federal law prohibiting FGM was enacted in 1996. Seventeen states enacted similar laws between 1994 and 2006.[118]
In literature and films
- Literature
- Desert Flower by Waris Dirie (1999): autobiographical novel about Dirie's childhood and genital mutilation.[119]
- Desert Dawn by Waris Dirie (2003): how Dirie became a UN Special Ambassador FGM.
- Desert Children: Waris Dirie and journalist Corinna Milborn investigate the practice of FGM in Europe.[120]
- Do They Hear You When You Cry by Fauziya Kassindja (1999): Kassindja's story of fleeing Africa hours before the ritual kakia takes place, and seeking asylum in America. After a landmark decision in immigration history, she was granted asylum on June 13, 1996.
- Possessing the Secret of Joy by Alice Walker (1993): explores the themes of violence, sexism, misogyny, and FGM in African, British, and American society.
- No Laughter Here by Rita Williams-Garcia (2004): about a ten-year-old Nigerian girl who underwent FGM while on vacation in her homeland.
- Sweetness in the Belly by Camilla Gibb (2005): about a white Muslim woman in Harar; FGM is performed on the daughters of the woman she stays with.
- Up the Walls of the World (1976) by James Tiptree, Jr (a pseudonym for writer Alice Sheldon): The protagonist, Margaret Omali, suffers FGM as a Kenyan-American child at the hands of her father.
- Infidel: My Life by Ayaan Hirsi Ali (2007): The author, Ayaan, is "exorcised," including having her labia stitched together as a young girl under the guidance of her grandmother.
- Woman at Point Zero by Nawal El Saadawi.
- Films
- Finzan by Cheick Oumar Sissoko (1989, Mali): Ttwo women who rebel against the traditions of a village society.
- Bintou in Paris by Kirsten Johnson and Julia Pimsleur (1995 documentary short, France)
- Schnitt ins Leben – Afrikanerinnen bekämpfen ein Ritual by Dagmar Brendecke and Anke Müller-Belecke (2000 TV documentary, Germany)
- The Day I Will Never Forget by Kim Longinotto (2002 documentary, UK)
- Dabla! Excision by Erica Pomerance (2003 documentary, Canada): Follows the growing movement across Africa to stop FGM.
- Moolaadé by Ousmane Sembène (2004, Senegal, France, Burkina Faso, Cameroon, Morocco, Tunisia)
- Dunia by Jocelyn Saab (2005 drama, Egypt-Lebanon-France)
- Kokonainen by Alexis Kouros (2005 short, Finland): The film won 2005 New York Short Film Festival Jury Award for Best Screenplay.
- God's Sandbox by Doron Eran (2006, Israel): An Israeli girl joins a Muslim tribe and is forced to undergo FGM.
- Maimouna – La vie devant moi by Fabiola Maldonado (2007 documentary, Germany)[121]
- Desert Flower – The Feature Film Directed by Sherry Hormann (2009) based on Waris Dirie's Desert Flower.[122]
- Antichrist by Lars von Trier (released in 2009) : graphic auto-clitoridectomy scene
- L'appel de Diégoune / Diégoune Call to Action: Walking the Path of Unity (2009) by Marc Dacosse and Eric Dagostino for Tostan, Tostan France, Respect, Diégoune
References
- ^ a b c d "Female genital mutilation". World Health Organization. February 2010.
- ^ a b "What is female genital mutilation?, Amnesty International, AI Index: ACT 77/06/97, accessed September 3, 2011.
- ^ a b Momoh, Comfort (ed). "Female Genital Mutilation", Radcliffe Publishing, 2005, pp. 6–7.
- ^ Ellaithi, M. et al. "Female genital mutilation of a karyotypic male presenting as a female with delayed puberty", BMC Women's Health 2006, 6:6.
- ^ Feldman-Jacobs, Charlotte. "Commemorating International Day of Zero Tolerance to Female Genital Mutilation", Population Reference Bureau, February 2009.
- ^ Shell-Duncan, Bettina and Ylva Hernlund (eds). Female "Circumcision" in Africa. Lynne Rienner, 2000, p. 6.
- Also see Shell-Duncan, Bettina (2001). "The medicalization of female "circumcision":harm reduction or promotion of a dangerous practice?". Social Science & Medicine. 52 (7): 1013–1028.
- ^ a b Alexia Lewnes, ed. (2005). "Changing a harmful social convention: female genital cutting/mutilation" (PDF). Innocenti Digest: 1–2. ISBN 88-89129-24-7. Retrieved 2007-12-24.
The expression female genital mutilation (FGM) gained growing support in the late 1970s. The word "mutilation" not only establishes a clear linguistic distinction with male circumcision, but also, owing to its strong negative connotations, emphasizes the gravity of the act. In 1990, this term was adopted at the third conference of the Inter African Committee on Traditional Practices Affecting the Health of Women and Children (IAC) in Addis Ababa. In 1991, WHO recommended that the United Nations adopt this terminology and subsequently, it has been widely used in UN documents.
- Also see Obermeyer, Carla Makhlouf (1999). "Female Genital Surgeries: The Known, the Unknown, and the Unknowable". Medical Anthropology Quarterly. 13 (1): 80. doi:10.1525/maq.1999.13.1.79.
{{cite journal}}: More than one of|pages=and|page=specified (help); Unknown parameter|month=ignored (help)
- Also see Obermeyer, Carla Makhlouf (1999). "Female Genital Surgeries: The Known, the Unknown, and the Unknowable". Medical Anthropology Quarterly. 13 (1): 80. doi:10.1525/maq.1999.13.1.79.
- ^ "Female Genital Mutilation/Cutting: Data and Trends" (PDF). Population Reference Bureau. 2008.
- "Female Genital Cutting in the Demographic and Health Surveys: A Critical and Comparative Analysis" (PDF). Measure DHS. p. 1.
- ^ Gruenbaum, Ellen. The Female Circumcision Controversy: An Anthropological Perspective. University of Pennsylvania Press, 2001, p. 3.
- ^ "Annex to USAID Policy on Female Genital Mutilation/Cutting (FGM/C): Explanation of Terminology". USAID. 2000.
- ^ a b Skaine, R (2005). Female genital mutilation: Legal, cultural and medical issues. McFarland.
- ^ Momoh, Comfort (ed). "Female Genital Mutilation", Radcliffe Publishing, 2005, p. 5.
- ^ Keller, Nuh Ha Mim (trans.) (1994). Reliance of the Traveller. Amana Publications. pp. 59 (section e4.3).
- ^ "Fresh progress toward the elimination of female genital mutilation and cutting in Egypt" (Press release). UNICEF. 2 July 2007. Retrieved 14 October 2010.
- ^ "Egypt: Report on Female Genital Mutilation (FGM) or Female Genital Cutting (FGC)" (Press release). UNHCR. 1 June 2001. Retrieved 29 July 2011.
- ^ a b c d e "Eliminating Female Genital Mutilation – An interagency statement OHCHR, UNAIDS, UNDP, UNECA, UNESCO, UNFPA, UNHCR, UNICEF, UNIFEM, WHO" (Document). Department of Reproductive Health and Research (RHR), World Health Organization. 2008.
{{cite document}}: Check date values in:|year=(help); Unknown parameter|format=ignored (help); Unknown parameter|url=ignored (help) - ^ S Elmusharaf (2006-07-15). "Reliability of self reported form of female genital mutilation and WHO classification: cross sectional study". BMJ. 333 (7559): 124. doi:10.1136/bmj.38873.649074.55. PMC 1502195. PMID 16803943.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Cormier, Zoe (fall 2005). "Making the Cut". Shameless. Retrieved 2008-03-03.
{{cite news}}: Check date values in:|date=(help) - ^ a b "New study shows female genital mutilation exposes women and babies to significant risk at childbirth" (Press release). World Health Organization. 2006-06-02. Retrieved 2006-10-02.
- ^ Frequently Asked Questions on Female Genital Mutilation (FGM)
- ^ a b Pieters, Guy, M.D. (1977). "Infibulation in the Horn of Africa". New York State Journal of Medicine. 77 (6): 729–731.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ a b c Toubia N (1995). "Female Circumcision as a Public Health Issue". New England Journal of Medicine. 331 (11): 712–716. doi:10.1056/NEJM199409153311106. PMID 8058079.
- ^ Nicoletti A (2007). "Female Genital Cutting". Journal of Pediatric and Adolescent Gynecology. 20 (4): 261–262. doi:10.1016/j.jpag.2007.03.098. PMID 17673141.
- ^ Lightfoot-Klein, Hanny, M.A. (1989). "The Sexual Experience and Marital Adjustment of Genitally Circumcised and Infibulated Females in The Sudan". The Journal of Sex Research. 26 (3). The Society for the Scientific Study of Sexuality: 375–392. doi:10.1080/00224498909551521.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Braddy Cathleen M., Files Julia A. (2007). "Female genital mutilation: cultural awareness and clinical considerations". Journal of Midwifery & Women's Health. 52 (2): 158–163. doi:10.1016/j.jmwh.2006.11.001.
- ^ a b "Death of 12-Year-Old Circumcised Girl Shocks Egypt, Prompts Ban on Rite". Fox News. Associated Press. 2007-06-27. Retrieved 2008-01-11.
- ^ http://www.unfpa.org/gender/practices2.htm#16
- ^ a b Monjok E, Essien EJ, Holmes L (2007). "Female genital mutilation: potential for HIV transmission in sub-Saharan Africa and prospect for epidemiologic investigation and intervention". Afr J Reprod Health. 11 (1). African Journal of Reproductive Health / La Revue Africaine de la Santé Reproductive, Vol. 11, No. 1: 33–42. doi:10.2307/30032486. JSTOR 30032486. PMID 17982946.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Pepin J, Plamondon P, Alves AC, Beaudet M, Labbe AC (2006). "Parenteral transmission during excision and treatment of tuberculosis and trypanosomiasis may be responsible for the HIV-2 epidemic in Guinea-Bissau". AIDS. 20 (9): 1303–11. doi:10.1097/01.aids.0000232239.05545.33. PMID 16816560.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Mboto CI, Fielder M, Davies-Russell A, Jewell AP (2009). "Prevalence of HIV-1, HIV-2, hepatitis C and co-infection in The Gambia". West Afr J Med. 28 (1): 16–9. PMID 19662739.
{{cite journal}}: CS1 maint: multiple names: authors list (link)- Msuya SE, Mbizvo E, Hussain A, Sundby J, Sam NE, Stray-Pedersen B (2002). "Female genital cutting in Kilimanjaro, Tanzania: changing attitudes?". Trop. Med. Int. Health. 7 (2): 159–65. doi:10.1046/j.1365-3156.2002.00838.x. PMID 11841706.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Klouman E, Manongi R, Klepp KI (2005). "Self-reported and observed female genital cutting in rural Tanzania: associated demographic factors, HIV and sexually transmitted infections". Trop. Med. Int. Health. 10 (1): 105–15. doi:10.1111/j.1365-3156.2004.01350.x. PMID 15655020.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Kapiga SH, Bang H, Spiegelman D, Msamanga GI, Coley J, Hunter DJ (2002). "Correlates of plasma HIV-1 RNA viral load among HIV-1-seropositive women in Dar es Salaam, Tanzania". J Acquir Immune Defic Syndr. 30 (3): 316–23. PMID 12131569.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Yount KM, Abraham BK (2007). "Female genital cutting and HIV/AIDS among Kenyan women". Stud Fam Plann. 38 (2): 73–88. doi:10.1111/j.1728-4465.2007.00119.x. PMID 17642409.
{{cite journal}}: Unknown parameter|month=ignored (help) - Foglia G, Langat L, Langat W; et al. "Community based study of HIV-1 infection among plantation workers in Kericho, Kenya in preparation for HIV-1 vaccine trials (3rd IAS Conference on HIV Pathogenesis and Treatment)". International AIDS Society.
{{cite web}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link)
- Msuya SE, Mbizvo E, Hussain A, Sundby J, Sam NE, Stray-Pedersen B (2002). "Female genital cutting in Kilimanjaro, Tanzania: changing attitudes?". Trop. Med. Int. Health. 7 (2): 159–65. doi:10.1046/j.1365-3156.2002.00838.x. PMID 11841706.
- ^ a b Maslovskaya O, Brown JJ, Padmadas SS (2009). "Disentangling the complex association between female genital cutting and HIV among Kenyan women". J Biosoc Sci. 41 (6): 815–30. doi:10.1017/S0021932009990150. PMID 19607733.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link)- Brewer DD, Potterat JJ, Roberts JM, Brody S (2007). "Male and female circumcision associated with prevalent HIV infection in virgins and adolescents in Kenya, Lesotho, and Tanzania" (PDF). Ann Epidemiol. 17 (3): 217–26. doi:10.1016/j.annepidem.2006.10.010. PMID 17320788.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link)
- Brewer DD, Potterat JJ, Roberts JM, Brody S (2007). "Male and female circumcision associated with prevalent HIV infection in virgins and adolescents in Kenya, Lesotho, and Tanzania" (PDF). Ann Epidemiol. 17 (3): 217–26. doi:10.1016/j.annepidem.2006.10.010. PMID 17320788.
- ^ a b Stallings, R.Y., Karugendo, E. "Female circumcision and HIV infection in Tanzania: for better or for worse? (3rd IAS conference on HIV pathogenesis and treatment)". International AIDS Society.
{{cite web}}: CS1 maint: multiple names: authors list (link) - ^ Kanki P, M'Boup S, Marlink R; et al. (1992). "Prevalence and risk determinants of human immunodeficiency virus type 2 (HIV-2) and human immunodeficiency virus type 1 (HIV-1) in west African female prostitutes". Am. J. Epidemiol. 136 (7): 895–907. doi:10.1093/aje/136.7.895. PMID 1442755.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Klouman E, Manongi R, Klepp KI (2005). "Self-reported and observed female genital cutting in rural Tanzania: associated demographic factors, HIV and sexually transmitted infections". Trop. Med. Int. Health. 10 (1): 105–15. doi:10.1111/j.1365-3156.2004.01350.x. PMID 15655020.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Brewer DD, Potterat JJ, Roberts JM, Brody S (2007). "Male and female circumcision associated with prevalent HIV infection in virgins and adolescents in Kenya, Lesotho, and Tanzania" (PDF). Ann Epidemiol. 17 (3): 217–26. doi:10.1016/j.annepidem.2006.10.010. PMID 17320788.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Yount KM, Abraham BK (2007). "Female genital cutting and HIV/AIDS among Kenyan women". Stud Fam Plann. 38 (2): 73–88. doi:10.1111/j.1728-4465.2007.00119.x. PMID 17642409.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Utz-Billing I, Kentenich H (2008). "Female genital mutilation: an injury, physical and mental harm". J Psychosom Obstet Gynaecol. 29 (4): 225–9. doi:10.1080/01674820802547087. PMID 19065392.
{{cite journal}}: Unknown parameter|month=ignored (help)- Brady M (1999). "Female genital mutilation: complications and risk of HIV transmission". AIDS Patient Care STDS. 13 (12): 709–16. doi:10.1089/apc.1999.13.709. PMID 10743534.
{{cite journal}}: Unknown parameter|month=ignored (help) - Nyindo M (2005). "Complementary factors contributing to the rapid spread of HIV-I in sub-Saharan Africa: a review". East Afr Med J. 82 (1): 40–6. PMID 16122111.
{{cite journal}}: Unknown parameter|month=ignored (help)
- Brady M (1999). "Female genital mutilation: complications and risk of HIV transmission". AIDS Patient Care STDS. 13 (12): 709–16. doi:10.1089/apc.1999.13.709. PMID 10743534.
- ^ Van Roosmalen J, Reynerse MM, Wiebenga JE (1992). "AIDS and women's health care in developing countries". Trop Geogr Med. 44 (3): 284–5. PMID 1455539.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ http://www.unfpa.org/gender/practices2.htm#15
- ^ Baasher, T (1979). "Psychological aspects of female circumcision". WHO/EMRO technical publication. 2 (Traditional practices affecting the health of women and children). Geneva: World Health Organization: 71–105.
- ^ a b Abusharaf, Rogaia M. (2001). "Virtuous Cuts: Female Genital Circumcision in an African Ontology". Differences: A Journal of Feminist Cultural Studies. 12: 112–140. doi:10.1215/10407391-12-1-112.
- ^ a b Pharos website
- ^ "Female genital mutilation causes aggression". Radio Netherlands Worldwide. 6 February 2010.
- ^ "WHAT IS FEMALE GENITAL MUTILATION?". Amnesty International.
- ^ http://www.unicef.org/protection/index_genitalmutilation.html
- ^ a b c d e Lightfoot-Klein, Hanny (1989). "The Sexual Experience and Marital Adjustment of Genitally Circumcised and Infibulated Females in The Sudan". The Journal of Sex Research. 26 (3): 375–392. doi:10.1080/00224498909551521.
- ^ Eve Conant (2009). "The Kindest Cut: In Colorado, a surgeon helps restore feeling—and so much more—to victims of female genital mutilation". Newsweek. Retrieved October 27, 2009.
- ^ Clitoraid, accessed 4 September 2011.
- ^ Birch/Abril, Nicholas (2008-01-04). "An End to Female Genital Cutting?". Time Magazine. Retrieved 2008-01-08.
- ^ Natsoulas, Theodore: "The Politicization of the Ban of Female Circumcision and the Rise of the Independent School Movement in Kenya. The KCA, the Missions and Government, 1929–1932". Journal of African Studies 33(2):137–158, 1998.
- ^ Birch/Abril, Nicholas. "An End to Female Genital Cutting?", Time magazine, 2008-01-04. Retrieved on 2008-01-08.
- ^ Vento, Mary (1998-03-07). "One Thousand Years of Chinese Footbinding: Its Origins, Popularity and Demise". Retrieved 2008-01-08.
- ^ "Ending Female Genital Cutting In Dialacoto – A Celebration Of Life And Culture" (Press release). TOSTAN. May 18, 2005. Retrieved 2006-10-02.
- ^ "Abandoning Female Genital Cutting (FGM)". Retrieved 2009-10-21.
- ^ "Nahid Toubia" by Priya Shetty, The Lancet, Volume 369, Issue 9564, Page 819, 10 March 2007 doi:10.1016/S0140-6736(07)60394-8, accessed 30 January 2011
- ^ "Changing attitudes to female circumcision". BBC. 8 April 2002.
- ^ "Mauritania fatwa bans female genital mutilation", BBC, January 18, 2010
- ^ a b Razor's Edge – The Controversy of Female Genital Mutilation
- ^ "Egypt forbids female circumcision". BBC News. 2007-06-28.
- ^ a b Stop FGM in Kurdistan
- ^ "Female genital mutilation in Iraqi Kurdistan. Presented at the 1ère Journée Humanitaire sur la Santé des Femmes dans le Monde, Paris, France". Gynécologie sans Frontières. 2006-03-27.
{{cite web}}: Cite uses deprecated parameter|authors=(help) - ^ a b c d e f Birch, Nicholas. "Female circumcision surfaces in Iraq", Christian Science Monitor, 10 August 2005.
- ^ "Bedouins shunning FGM/C – new research", IRIN, March 4, 2009.
- ^ " Indonesia: Report on Female Genital Mutilation (FGM) or Female Genital Cutting (FGC)", U.S. Department of State, June 1, 2001.
- ^ [http://www.nytimes.com/2006/11/02/us/02brfs-001.html?_r=1 "Georgia: Man Convicted in Daughter’s Mutilation", Associated Press, 2 November 2010.
- ^ a b c d e f g h i j k l m n o p "Female Genital Mutilation (FGM) or Female Genital Cutting (FGC): Individual Country Reports". US State Department. Archived from the original on 2008-01-10. Retrieved 2008-01-11. (Web archive)
- ^ Findarticles.com
- ^ a b c d e f g h i j k l FGM Education and Networking Project. Fgmnetwork.org. Retrieved on 2011-02-05.
- ^ Stolz, Joëllepr (September 1998). "Le Burkina Faso fait reculer l'excision". Le Monde diplomatique (in French). p. 18. Retrieved 2006-10-02.
{{cite news}}: Italic or bold markup not allowed in:|work=(help) - ^ a b c d e f g h i j k l m Research Performed by the African Women's Center. Brighamandwomens.org. Retrieved on 2011-02-05.
- ^ a b c d e f g Ecoi.net
- ^ Michael, Maggie (2007-07-01). "Egypt outlaws circumcision after girl dies". The Observer. Cairo.
- ^ "Egypt strengthens ban on female genital cutting". Reuters. 2007-06-28. Retrieved 2008-01-11.
- ^ "Egypt death sparks debate on female circumcision". Reuters. 2007-08-20. Retrieved 2009-05-22.
- ^ "Eritrea bans female circumcision". BBC. 2007-04-04. Retrieved 2007-07-28.
- ^ "Female Genital Mutilation in ETHIOPIA". YouTube. Ethio007.
- ^ http://www.unhcr.org/cgi-bin/texis/vtx/refworld/rwmain?page=search&docid=4da56dc7c&skip=0&query=female genital&searchin=title&display=10&sort=date
- ^ Unicef: Somalia
- ^ "Uganda Bans Female Genital Mutilation". BBC. 10 December 2009. Retrieved 10 December 2009.
- ^ Uganda Government News: Uganda asked to ratify Women’s rights protocol, UGPulse, November 27, 2008
- ^ "Museveni condemns genital cutting". The New Vision. Kampala. 2007-07-02.
- ^ Serc.mb.ca
- ^ a b c d Encyclopedia of Women & Islamic Cultures: Family, Body, Sexuality and Health , Volume 3 (Encyclopaedia of Women and Islamic Cultures). Brill Academic Publishers. 2005. p. 588. ISBN 9004128190.
- ^ "INDONESIA: Female genital mutilation persists despite ban". IRIN Global. 2010-09-02. Retrieved 2010-11-21.
- ^ "Female genital mutilation: Madagascar, Malawi, Malaysia, Mali, Mauritania, Mauritius, Mexico, Morocco, Mozambique". Inter-Parliamentary Union. Retrieved 2010-11-21.
- ^ Rahman Isa A, Shuib R, Shukri Othman M (1999 May). "The practice of female circumcision among Muslims in Kelantan, Malaysia". Reproductive Health Matters. 7 (13): 137–144. doi:10.1016/S0968-8080(99)90125-8.
{{cite journal}}: Check date values in:|date=(help)CS1 maint: multiple names: authors list (link) - ^ Golnaz Esfandiari (2009-03-10). "Female Genital Mutilation Said To Be Widespread In Iraq's, Iran's Kurdistan". Radio Free Europe / Radio Liberty. Retrieved 2010-11-21.
- ^ "Female Genital Mutilation in Iraqi Kurdistan – A Study" (PDF). WADI. Retrieved 2010-02-15.
- ^ a b "Draft for a Law Prohibiting Female Genital Mutilation is submitted to the Kurdish Regional Parliament". Stop FGM in Kurdistan. Retrieved 2010-11-21.
- ^ "FGM in Iraq and Iran". The Waris Dirie Foundation. 2010-01-27. Retrieved 2010-11-21.
- ^ "Iraqi Kurdistan: Law Banning FGM a Positive Step". Human Rights Watch. 2011-07-25. Retrieved 2011-07-27.
- ^ GTZ.de
- ^ Is Female Genital Mutilation an Islamic Problem? :: Middle East Quarterly. Meforum.org. Retrieved on 2011-02-05.
- ^ a b c d Mutilation/Cutting: Promoting Gender Equality. UNFPA. Retrieved on 2011-02-05.
- ^ http://www.irinnews.org/IndepthMain.aspx?reportid=62462&indepthid=15
- ^ http://www.manushi-india.org/pdfs_issues/PDF%20files%2066/all_for_izzat.pdf
- ^ http://www.forwarduk.org.uk/key-issues/fgm
- ^ Gender Equality in West Bank and Gaza|Social Institutions and Gender Index (SIGI). Genderindex.org (2007-02-16). Retrieved on 2011-02-05.
- ^ http://www.taskforcefgm.de/situation/was-ist-fgm/verbreitung/
- ^ a b Kvello, Ane (2003-09-06). "Concerning female circumcision in the United Arab Emirates: Is clitoridectomy in a traditional context an assault against women?". FOKO 2003 – ABSTRACTS. Oslo, Norway: University of Oslo. Retrieved 2010-11-21.
{{cite conference}}: Unknown parameter|booktitle=ignored (|book-title=suggested) (help); Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ At a glance: Yemen – Statistics. UNICEF. Retrieved on 2011-02-05.
- ^ http://www.unhcr.org/cgi-bin/texis/vtx/refworld/rwmain?page=search&docid=4da56d73a5&skip=0&query=female genital&searchin=title&display=10&sort=date
- ^ Internal-displacement.org
- ^ Compass. Eycb.coe.int. Retrieved on 2011-02-05.
- ^ a b Chenciner, Robert (1997). Daghestan: Tradition and Survival. Palgrave Macmillan. p. 320. ISBN 0312173806.
- ^ "The Criminalisation Of Female Genital Mutilation In Queensland". Murdoch University Electronic Journal of Law. 2002-09. Retrieved 2008-09-10.
{{cite web}}: Check date values in:|date=(help) - ^ Royal Australian College of Obstetricians and Gynaecologists (1997), Female Genital Mutilation: Information for Australian Health Professionals, Royal Australian College of Obstetricians and Gynaecologists
- ^ "Girls mutilated for 'tradition'". Sunday Telegraph. 2006-11-05.
{{cite news}}:|access-date=requires|url=(help); External link in|news=|news=ignored (|newspaper=suggested) (help) - ^ Federal Interdepartmental Working Group on Female Genital Mutilation (1999), Female genital mutilation and health care – an exploration of the needs and roles of affected communities and health care providers in Canada, Health Canada
- ^ Canada's Criminal Code ( R.S., 1985, c. C-46 )
- ^ "Excision sur mineure : obligation de signalement". 2008-01-03.
{{cite news}}:|access-date=requires|url=(help); External link in|news=|news=ignored (|newspaper=suggested) (help) - ^ Italian Law n°7 1/9/2006, Disposizioni concernenti la prevenzione e il divieto delle pratiche di mutilazione genitale femminile Retrieved on March 23, 2009.
- ^ Consolo Act supporters blog Retrieved on March 23, 2009.
- ^ "Female Genital Mutilation: Information for health and child protection professionals". New Zealand Ministry of Health.
- ^ http://noticias.juridicas.com/base_datos/Penal/lo10-1995.l2t3.html#a149
- ^ Johnsdotter, Sara (2004). "FGM in Sweden: Swedish Legislation Regarding 'Female Genital Mutilation' and Implementation of the Law. Research Report in Sociology 2004:1" (Document). Lund University.
- ^ Notes on some overseas countries' laws, The FGM Education and Networking Project
- ^ Susan Deller Ross (2008). Women's Human Rights: The International and Comparative Law Casebook. Vantage Press, Inc. p. 509. ISBN 0-8122-4067-7, 9780812240672.
{{cite book}}: Check|isbn=value: invalid character (help) - ^ Somalia's Desert Flower Time magazine July 7, 2002
- ^ Book Reviews-Desert Children, Times Online ,01 March 2006
- ^ "Maimouna - Der Film (Maimouna - The Film)". Retrieved 10 August 2011.
- ^ Model Liya Kebede to star in 'Flower'
Further reading
- Al-Qaradawi, Y. (2004, February 7). Islamic ruling on female genital mutilation. Retrieved March 29, 2006.
- Al-Qaradawi, Y. (2004, December 13). Circumcision: Juristic, medical & social perspectives. Retrieved March 29, 2006.
- Boyle, E. H. (2002). Female genital cutting: Cultural conflict in the global community. Baltimore: Johns Hopkins University Press. ISBN 978-0-8018-7063-7.
- Dettwyler, Katherine A. (1994). Dancing skeletons: life and death in West Africa. Prospect Heights, Ill.: Waveland Press. ISBN 0-88133-748-X.
- Ferguson, I and Ellis, P. (1995). Female Genital Mutilation: a Review of the Current Literature Department of Justice, Canada. Working document
- Gruenbaum, E. (2001). The female circumcision controversy. Philadelphia: University of Pennsylvania Press. ISBN 978-0-8122-1746-9.
- Hoffman, B. (2002). Womanhood and Circumcision: Three Maasai women have their say. Berkeley: Berkeley Media.
- Hrzán, Daniela. (Re)Discovering FGC: Anthropology, Whiteness, Feminism. In: Tißberger, Martina/ Dietze, Gabriele/ Hrzán, Daniela/ Husmann-Kastein, Jana (eds.). Weiß – Weißsein – Whiteness: Kritische Studien zu Gender und Rassismus/Critical Studies on Gender and Racism. Frankfurt/Main: Peter Lang, 2006, pp. 113–142.
- IRIN (2005). "Razor's Edge – The Controversy of Female Genital Mutilation". IRIN.
- Johnson, Michelle C. (2000). Becoming a Muslim, Becoming a person: Female 'circumcision', religious identity, and personhood in Guinea-Bissau. In B. Shell-Duncan & Y. Herlund (Eds.), Female circumcision in Africa: Culture, controversy, and change. Boulder: Lynne Rienner Publishers.
- Kandela P (1995). "Egypt sees U turn on female circumcision". BMJ. 310 (6971): 12. PMID 7827544.
{{cite journal}}: Unknown parameter|month=ignored (help) - Kassindja, F. (1998). Do they hear you when you cry. New York: Delacorte Press. ISBN 0-385-31832-4.
- Obermeyer CM (2003). "The health consequences of female circumcision: science, advocacy, and standards of evidence". Med Anthropol Q. 17 (3): 394–412. doi:10.1525/maq.2003.17.3.394. PMID 12974204.
{{cite journal}}: Unknown parameter|month=ignored (help) - Pieters G, Lowenfels AB (1977). "Infibulation in the horn of Africa". N Y State J Med. 77 (5): 729–31. PMID 265433.
{{cite journal}}: Unknown parameter|month=ignored (help) - Research papers from medical gynecologists, judges, linguistics, and social scientists on the subject (1994). University of Khartoum, Sudan. Umm Atteya Organization website (Arabic). Retrieved March 29, 2006.
- UNICEF (1999). Consultation on the elimination of female genital mutilation: 14–16 December 1998. New York: Author. 40 pp.
- World Health Organization. (1996). Female genital mutilation: Report of a WHO Technical Working Group (unpublished document WHO/FRH/WHD/96.10). Geneva: World Health Organization. Retrieved 2007-02-21.
- Aldeeb, Sami (2000). Male and Female Circumcision in the Jewish, Christian and Muslim Communities, Religious debate. Beirut, ISBN 1-85513-406-3.
- Daw E (1970). "Female circumcision and imfibulation complicating delivery". Practitioner. 204 (222): 559–63. PMID 5443542.
{{cite journal}}: Unknown parameter|month=ignored (help) - Dewhurst CJ, Michelson A (1964). "Infibulation complicating pregnancy". Br Med J. 2 (5422): 1442. doi:10.1136/bmj.2.5422.1442. PMC 1817445. PMID 14209371.
{{cite journal}}: Unknown parameter|month=ignored (help) - Dirie, Waris (2001). Desert Flower. Autobiography of a Somali woman's journey from nomadic tribal life to a career as a fashion model in London and to the post of special ambassador at the United Nations. Dirie recounts her personal experience with female genital mutilation that began with her own genital cutting at age five.
- Leonard Lori (2000). "We did it for pleasure only: Hearing alternative tales of female circumcision". Qualitative Inquiry. 6 (2): 212–228. doi:10.1177/107780040000600203.
- Mernissi, Fatima. Beyond the veil: Male-female dynamics in a modern Muslim society. Cambridge, Massachusetts: Schenkman Pub. Co. ISBN 0-470-59613-9.
- Mustafa Asim Zaki (1966). "Female circumcision and infibulation in the Sudan". Journal of Obstetrics and Gynaecology of the British Commonwealth. 73 (2): 302–306. doi:10.1111/j.1471-0528.1966.tb05163.x.
- Robinett, Patricia (2006). The rape of innocence: One woman's story of female genital mutilation in the USA. N.p.: Aesculapius Press. ISBN 1-878411-04-7.
- Exernal links
- Campaign for an FGM helpline in the UK
- Female Genital Mutilation Video from the American Medical Videos Journal
- FGM Education and Networking Project.
- Catholic Relief Services: Saying No to 'The Cut': An Alternative Rite of Passage in Kenya
- Orchid Project, Campaigning for a world free from female genital cutting by 2025.
- END FGM-European Campaign
- Stop FGM in Kurdistan
- ReligiousTolerance.org: About FGM: Female Genital Mutilation
- U.S. State Department estimates of prevalence of FGM in Africa and beyond
- World Health Organization: Female genital mutilation
- Columbia University: Circumcised clitoris (Female 'circumcision')?
- Short Film on FGM in Minya, Egypt
- Women Circumcision in Iraq
- Evaluation of Senegal's "National Action Plan for the Abandonment of Female Genital Cutting 2009–2015 – in French
- UNICEF. Changing a Harmful Social Convention: Female Genital Mutilation/Cutting
- UNICEF. Coordinated Strategy to Abandon FGM/C in One Generation
- Platform for Action: Towards the Abandonment of FGM/C – A Matter of Gender Equality
- Template:Fr icon UNICEF/Tostan. La Décennie qui a fait reculer l'excision
- ONCHR, UNAIDS, UNDP, UNECA, UNESCO, UNFPA, UNHCR, UNICEF, UNIFEM, WHO. Eliminating Female genital mutilation: An interagency statement.
- Female Genital Cutting: A Case for Compromise
- “FGM is with us Everyday” Women and Girls Speak out about Female Genital Mutilation in the UK
