Tetrahydrobiopterin
 | |
| Clinical data | |
|---|---|
| License data | |
| Routes of administration | By mouth |
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Elimination half-life | 4 hours (healthy adults) 6–7 hours (PKU patients) |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| ChEBI | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.164.121 |
| Chemical and physical data | |
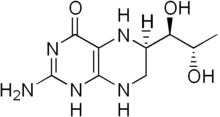
| Formula | C9H15N5O3 |
| Molar mass | 241.25 g/mol g·mol−1 |
| 3D model (JSmol) | |
| |
| |
| | |
Tetrahydrobiopterin (BH4, THB), also known as sapropterin, is a naturally occurring essential cofactor of the three aromatic amino acid hydroxylase enzymes, used in the degradation of amino acid phenylalanine and in the biosynthesis of the neurotransmitters serotonin (5-hydroxytryptamine, 5-HT), melatonin, dopamine, norepinephrine (noradrenaline), epinephrine (adrenaline), and is a cofactor for the production of nitric oxide (NO) by the nitric oxide synthases.[1] Chemically, its structure is that of a reduced pteridine derivative.
Medical use
Phenylketonuria
Sapropterin dihydrochloride may help lower phenylalanine levels in some people with phenylketonuria. It is FDA approved for this use along with dietary measures.[2] Most people however, have little or no benefit.[3]
Adverse effects
The most common adverse effects, observed in more than 10% of patients, include headache and a running or obstructed nose. Diarrhea and vomiting are also relatively common, seen in at least 1% of patients.[4]
Interactions
No interaction studies have been conducted. Because of its mechanism, tetrahydrobiopterin might interact with dihydrofolate reductase inhibitors like methotrexate and trimethoprim, and NO-enhancing drugs like nitroglycerin, molsidomine, minoxidil, and PDE5 inhibitors. Combination of tetrahydrobiopterin with levodopa can lead to increased excitability.[4]
Functions
Tetrahydrobiopterin has the following responsibilities as a cofactor:
- Tryptophan hydroxylase (TPH) for the conversion of L-tryptophan (TRP) to 5-hydroxytryptophan (5-HTP)
- Phenylalanine hydroxylase (PAH) for conversion of L-phenylalanine (PHE) to L-tyrosine (TYR)
- Tyrosine hydroxylase (TH) for the conversion of L-tyrosine to L-DOPA (DOPA)
- Nitric oxide synthase (NOS) for conversion of a guanidino nitrogen of L-arginine (L-Arg) to nitric oxide (NO)
- Alkylglycerol monooxygenase (AGMO) for the conversion of 1-alkyl-sn-glycerol to 1-hydroxyalkyl-sn-glycerol
Tetrahydrobiopterin has multiple roles in human biochemistry. One is to convert amino acids such as phenylalanine, tyrosine, and tryptophan to precursors of dopamine and serotonin, major monoamine neurotransmitters. Due to its role in the conversion of L-tyrosine into L-dopa, which is the precursor for dopamine, a deficiency in tetrahydrobiopterin can cause severe neurological issues unrelated to a toxic buildup of L-phenylalanine; dopamine is a vital neurotransmitter, and is the precursor of norepinephrine and epinephrine. Thus, a deficiency of BH4 can lead to systemic deficiencies of dopamine, norepinephrine, and epinephrine. In fact, one of the primary conditions that can result from GTPCH-related BH4 deficiency is dopamine-responsive dystonia;[5] currently, this condition is typically treated with carbidopa/levodopa, which directly restores dopamine levels within the brain.
BH4 also serves as a catalyst for the production of nitric oxide. Among other things, nitric oxide is involved in vasodilation, which improves systematic blood flow. The role of BH4 in this enzymatic process is so critical that some research points to a deficiency of BH4 – and thus, of nitric oxide – as being a core cause of the neurovascular dysfunction that is the hallmark of circulation-related diseases such as diabetes.[6]
History
Tetrahydrobiopterin was discovered to play a role as an enzymatic cofactor. The first enzyme found to use tetrahydrobiopterin is phenylalanine hydroxylase (PAH).[7]
Biosynthesis and recycling
Tetrahydrobiopterin is biosynthesized from guanosine triphosphate (GTP) by three chemical reactions mediated by the enzymes GTP cyclohydrolase I (GTPCH), 6-pyruvoyltetrahydropterin synthase (PTPS), and sepiapterin reductase (SR).[8]
BH4 is catabolized to BH3 and BH2, which are pro-oxidants (free radicals). Research shows that ascorbic acid (also known as ascorbate or vitamin C) is effective at recycling BH3 into BH4,[9] preventing the BH3 radical from reacting with other free radicals (superoxide and peroxynitrite specifically). Without this recycling process, uncoupling of the endothelial nitric oxide synthase (eNOS) enzyme and reduced bioavailability of the vasodilator nitric oxide occur, creating a form of endothelial dysfunction.[10] Ascorbic acid is oxidized to dehydroascorbic acid during this process, although it can be recycled back to ascorbic acid.
Research
Other than PKU studies, tetrahydrobiopterin has participated in clinical trials studying other approaches to solving conditions resultant from a deficiency of tetrahydrobiopterin. These include autism, ADHD, hypertension, endothelial dysfunction, and chronic kidney disease.[11][12] Experimental studies suggest that tetrahydrobiopterin regulates deficient production of nitric oxide in cardiovascular disease states, and contributes to the response to inflammation and injury, for example in pain due to nerve injury. A 2015 BioMarin-funded study of PKU patients found that those who responded to tetrahydrobiopterin also showed a reduction of ADHD symptoms.[13]
Autism
In 1997, a small pilot study was published on the efficacy of tetrahydrobiopterin (BH4) on relieving the symptoms of autism, which concluded that it "might be useful for a subgroup of children with autism" and that double-blind trials are needed, as are trials which measure outcomes over a longer period of time.[14] In 2010, Frye et al. published a paper which concluded that it was safe, and also noted that "several clinical trials have suggested that treatment with BH4 improves ASD symptomatology in some individuals."[15]
Cardiovascular disease
Since NO production is important in regulation of blood pressure and blood flow, thereby playing a significant role in cardiovascular diseases, tetrahydrobiopterin is a potential therapeutic target. In the endothelial cell lining of blood vessels, endothelial NOS is dependent on tetrahydrobiopterin availability.[16] Increasing tetrahydrobiopterin in endothelial cells by augmenting the levels of the biosynthetic enzyme GTPCH can maintain endothelial NOS function in experimental models of disease states such as diabetes,[17] atherosclerosis, and hypoxic pulmonary hypertension.[18] However, treatment of patients with existing coronary artery disease with oral tetrahydrobiopterin is limited by oxidation of tetrahydrobiopterin to the inactive form, dihydrobiopterin, with little benefit on vascular function.[19]
See also
- Tetrahydrobiopterin deficiency (THBD, BH4D)
- Biopterin
- Dihydrobiopterin
- Pteridine
References
- ^ Całka, Jarosław (2006). "The role of nitric oxide in the hypothalamic control of LHRH and oxytocin release, sexual behavior and aging of the LHRH and oxytocin neurons". Folia Histochemica et Cytobiologica. 44 (1): 3–12. PMID 16584085.
- ^ "What are common treatments for phenylketonuria (PKU)?". NICHD. 2013-08-23. Retrieved 12 September 2016.
- ^ Camp, Kathryn M.; Parisi, Melissa A.; Acosta, Phyllis B.; Berry, Gerard T.; Bilder, Deborah A.; Blau, Nenad; Bodamer, Olaf A.; Brosco, Jeffrey P.; Brown, Christine S.; Burlina, Alberto B.; Burton, Barbara K.; Chang, Christine S.; Coates, Paul M.; Cunningham, Amy C.; Dobrowolski, Steven F.; Ferguson, John H.; Franklin, Thomas D.; Frazier, Dianne M.; Grange, Dorothy K.; Greene, Carol L.; Groft, Stephen C.; Harding, Cary O.; Howell, R. Rodney; Huntington, Kathleen L.; Hyatt-Knorr, Henrietta D.; Jevaji, Indira P.; Levy, Harvey L.; Lichter-Konecki, Uta; Lindegren, Mary Lou; et al. (2014). "Phenylketonuria Scientific Review Conference: State of the science and future research needs". Molecular Genetics and Metabolism. 112 (2): 87–122. doi:10.1016/j.ymgme.2014.02.013. PMID 24667081.
- ^ a b Haberfeld, H, ed. (1 March 2017). Austria-Codex (in German). Vienna: Österreichischer Apothekerverlag. Kuvan 100 mg-Tabletten.
- ^ "Genetics Home Reference: GCH1". National Institutes of Health.
- ^ Wu, Guoyao; Meininger, Cynthia J. (2009). "Nitric oxide and vascular insulin resistance". BioFactors. 35 (1): 21–7. doi:10.1002/biof.3. PMID 19319842.
- ^ Kaufman, S (1958). "A new cofactor required for the enzymatic conversion of phenylalanine to tyrosine". The Journal of biological chemistry. 230 (2): 931–9. PMID 13525410.
- ^ Thöny, Beat; Auerbach, Günter; Blau, Nenad (2000). "Tetrahydrobiopterin biosynthesis, regeneration and functions". Biochemical Journal. 347: 1–16. doi:10.1042/0264-6021:3470001. PMC 1220924. PMID 10727395.
- ^ Kuzkaya, N.; Weissmann, N.; Harrison, D. G.; Dikalov, S. (2003). "Interactions of Peroxynitrite, Tetrahydrobiopterin, Ascorbic Acid, and Thiols: IMPLICATIONS FOR UNCOUPLING ENDOTHELIAL NITRIC-OXIDE SYNTHASE". Journal of Biological Chemistry. 278 (25): 22546–54. doi:10.1074/jbc.M302227200. PMID 12692136.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Muller-Delp, J. M. (2009). "Ascorbic acid and tetrahydrobiopterin: looking beyond nitric oxide bioavailability". Cardiovascular Research. 84 (2): 178–9. doi:10.1093/cvr/cvp307. PMID 19744948.
- ^ ClinicalTrials.gov: Search results for Kuvan
- ^ "BioMarin Initiates Phase 3b Study to Evaluate the Effects of Kuvan on Neurophychiatric Symptoms in Subjects with PKU". BioMarin Pharmaceutical Inc. 17 August 2010.
- ^ Burton, B.; Grant, M.; Feigenbaum, A.; Singh, R.; Hendren, R.; Siriwardena, K.; Phillips, J.; Sanchez-Valle, A.; Waisbren, S.; Gillis, J.; Prasad, S.; Merilainen, M.; Lang, W.; Zhang, C.; Yu, S.; Stahl, S. (2015). "A randomized, placebo-controlled, double-blind study of sapropterin to treat ADHD symptoms and executive function impairment in children and adults with sapropterin-responsive phenylketonuria". Molecular Genetics and Metabolism. 114 (3): 415–24. doi:10.1016/j.ymgme.2014.11.011. PMID 25533024.
- ^ Fernell, Elisabeth; Watanabe, Yasuyoshi; Adolfsson, Ingrid; Tani, Yoshihiro; Bergström, Mats; Phd, Per Hartvig; Md, Anders Lilja; Phd., Anne-Liis von Knorring MD.; Phd., Christopher Gillberg MD.; Phd., Bengt Lángström (2008). "Possible effects of tetrahydrobiopterin treatment in six children with autism - clinical and positron emission tomography data: A pilot study". Developmental Medicine & Child Neurology. 39 (5): 313–8. doi:10.1111/j.1469-8749.1997.tb07437.x. PMID 9236697.
- ^ Frye, Richard E.; Huffman, Lynne C.; Elliott, Glen R. (2010). "Tetrahydrobiopterin as a novel therapeutic intervention for autism". Neurotherapeutics. 7 (3): 241–9. doi:10.1016/j.nurt.2010.05.004. PMC 2908599. PMID 20643376.
- ^ Channon, Keithm. (2004). "Tetrahydrobiopterin". Trends in Cardiovascular Medicine. 14 (8): 323–7. doi:10.1016/j.tcm.2004.10.003. PMID 15596110.
- ^ Alp, Nicholas J.; Mussa, Shafi; Khoo, Jeffrey; Cai, Shijie; Guzik, Tomasz; Jefferson, Andrew; Goh, Nicky; Rockett, Kirk A.; Channon, Keith M. (2003). "Tetrahydrobiopterin-dependent preservation of nitric oxide–mediated endothelial function in diabetes by targeted transgenic GTP–cyclohydrolase I overexpression". Journal of Clinical Investigation. 112 (5): 725–35. doi:10.1172/JCI17786. PMC 182196. PMID 12952921.
- ^ Khoo, J. P.; Zhao, L; Alp, N. J.; Bendall, J. K.; Nicoli, T; Rockett, K; Wilkins, M. R.; Channon, K. M. (2005). "Pivotal Role for Endothelial Tetrahydrobiopterin in Pulmonary Hypertension". Circulation. 111 (16): 2126–33. doi:10.1161/01.CIR.0000162470.26840.89. PMID 15824200.
- ^ Cunnington, C.; Van Assche, T.; Shirodaria, C.; Kylintireas, I.; Lindsay, A. C.; Lee, J. M.; Antoniades, C.; Margaritis, M.; Lee, R.; Cerrato, R.; Crabtree, M. J.; Francis, J. M.; Sayeed, R.; Ratnatunga, C.; Pillai, R.; Choudhury, R. P.; Neubauer, S.; Channon, K. M. (2012). "Systemic and Vascular Oxidation Limits the Efficacy of Oral Tetrahydrobiopterin Treatment in Patients with Coronary Artery Disease". Circulation. 125 (11): 1356–66. doi:10.1161/CIRCULATIONAHA.111.038919. PMC 5238935. PMID 22315282.
