Caspase 1

Caspase-1/Interleukin-1 converting enzyme (ICE) is an evolutionarily conserved enzyme that proteolytically cleaves other proteins, such as the precursors of the inflammatory cytokines interleukin 1β and interleukin 18 as well as the pyroptosis inducer Gasdermin D, into active mature peptides.[5][6][7] It plays a central role in cell immunity as an inflammatory response initiator. Once activated through formation of an inflammasome complex, it initiates a proinflammatory response through the cleavage and thus activation of the two inflammatory cytokines, interleukin 1β (IL-1β) and interleukin 18 (IL-18) as well as pyroptosis, a programmed lytic cell death pathway, through cleavage of Gasdermin D.[8] The two inflammatory cytokines activated by Caspase-1 are excreted from the cell to further induce the inflammatory response in neighboring cells.[9]
Cellular expression
[edit]Caspase-1 is evolutionarily conserved in many eukaryotes of the Kingdom Animalia. Due to its role in the inflammatory immune response, it is highly expressed in the immune organs such as the liver, kidney, spleen, and blood (neutrophils).[10][11] Following infection, the inflammatory response increases expression of Caspase-1, by a positive feedback mechanism that amplifies the response.[11]
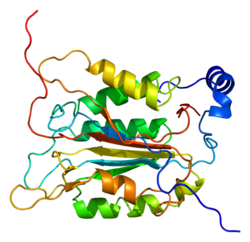
Structure
[edit]Caspase-1 is produced as a zymogen that can then be cleaved into 20 kDa (p20) and 10 kDa (p10) subunits that become part of the active enzyme. Active Caspase 1 contains two heterodimers of p20 and p10. It contains a catalytic domain with an active site that spans both the p20 and p10 subunits,[12] as well as a noncatalytic Caspase Activation and Recruitment Domain (CARD) . It interacts with other CARD containing proteins such as Apoptosis-Associated Speck-like Protein Containing a CARD (ASC) and Nod-Like Receptor (NLR) Family CARD Domain-Containing Protein 4 (NLRC4) through CARD-CARD interactions in the formation of inflammasomes.[7][13]
Regulation
[edit]

Activation
[edit]
Caspase-1, normally in its physiologically inactive zymogen form, autoactivates when it is assembled into the filamentous inflammasome complex by autoproteolysis into the p10 and p20 subunits.[14][15] The inflammasome complex is a ring complex composed of trimers of a signal specific sensor protein such as those of the NLR family and the AIM-1 (Absent in Melanoma) like receptors, an adaptor protein such as ASC, and a caspase, in this case Caspase-1. In some cases, where the signaling proteins contain their own CARDs, like in NLRP1 and NLRC4, the CARD–CARD interaction is direct, meaning there is no adaptor protein in the complex. There are a variety of sensor and adaptor proteins, the various combinations of which confer the inflammasomes' responses to specific signals. This allows the cell to have varying degrees of inflammatory responses based on the severity of the danger signal received.[16][17]
Inhibition
[edit]CARD only proteins (COPs) as their name implies, are proteins that only contain the non-catalytic CARDs. Owing to the importance of CARD-CARD interactions in inflammasome formation, many COPs are known inhibitors of Caspase activation. For Caspase-1, genes for specific COPs—ICEBERG, COP1 (ICE/Pseudo-ICE), and INCA (Inhibitory Card)—are all found near its locus, and are thus thought to have emerged from gene duplication events and subsequent deletions of the catalytic domains. Though they all interact with the inflammasomes using CARD–CARD interactions, they differ in the way they carry out their inhibitory functions as well as in their effectiveness at doing so.[15][18][19]
For example, ICEBERG nucleates the formation of Caspase-1 filaments and is thus incorporated into the filaments, but lacks the ability to inhibit the activation of inflammasomes. Instead, it is thought to inhibit Caspase-1 activation by interfering with the interaction of Caspase-1 with other important CARD containing proteins.[15][18][19]
INCA, on the other hand, directly blocks inflammasome assembly by capping Caspase-1 CARD oligomers, thus blocking further polymerization into the inflammasome filaments.[18][19][20][13]
Similarly, some POPs (Pyrin only proteins) are also known to regulate Caspase-1 activation through inhibition of inflammasome activation by binding to and blocking PYD interactions, which also play a role in the formation of the inflammasomes, though the exact mechanisms are not yet well established.[19][21]
- Inhibitors
- Belnacasan (VX-765) [22]
- Pralnacasan (VX-740) [23]
Function
[edit]Proteolytic cleavage
[edit]Activated Caspase 1 proteolytically cleaves pro IL-1β and pro IL-18 into their active forms, IL-1β and IL-18. The active cytokines lead to a downstream inflammatory response. It also cleaves Gasdermin D into its active form, which leads to pyroptosis.[13]
Inflammatory response
[edit]Once matured, the cytokines initiate downstream signaling events to induce a proinflammatory response as well as to activate the expression of antiviral genes. The speed, specificity and types of response are dependent on the signal received as well as the sensor protein that received it. Signals that can be received by the inflammasomes include viral double stranded RNA, urea, free radicals, and other signals associated with cellular danger, even byproducts of other immune response pathways.[24]
The mature cytokines themselves do not contain the necessary sorting sequences to enter the ER–Golgi secretory pathway, and thus are not excreted from the cell by conventional methods. However, it is theorized that the release of these proinflammatory cytokines is not reliant on cellular rupture via pyroptosis, and is in fact, an active process. There exists evidence both for and against this hypothesis. The fact that for many cell types, the cytokines are secreted despite them showing absolutely no signs of pyroptosis, supports this hypothesis.[17][25] However, some experiments show that Gasdermin D nonfunctional mutants still had normal cleavage of the cytokines but lacked the ability to secrete them, indicating pyroptosis may in fact be necessary for secretion in some way.[26]
Pyroptosis response
[edit]Following the inflammatory response, an activated Caspase-1 can induce pyroptosis, a lytic form of cell death, depending on the signal received as well as the specific inflammasome sensor domain protein that received it. Though pyroptosis may or may not be required for the full inflammatory response, the inflammatory response is fully required before pyroptosis can occur.[17] In order to induce pyroptosis, Caspase-1 cleaves Gasdermin D into fragments that form pores in the plasma membrane. As a result of osmotic pressure, these pores promote the influx of fluid, resulting in cell lysis and death.[27]
Other roles
[edit]Caspase-1 has also been shown to induce necrosis and may also function in various developmental stages. Studies of a similar protein in mice suggest a role in the pathogenesis of Huntington's disease. Alternative splicing of the gene results in five transcript variants encoding distinct isoforms.[28] Recent studies implicated caspase-1 in promoting CD4 T-cell death and inflammation by HIV, two signature events that fuel HIV disease progression to AIDS.[29][30][31] Caspase-1 activity has also been implicated in lysosome acidification following phagocytosis of bacteria[32] and immune complexes.[33]
See also
[edit]References
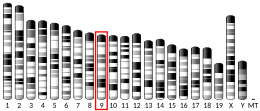
[edit]- ^ a b c GRCh38: Ensembl release 89: ENSG00000137752 – Ensembl, May 2017
- ^ a b c GRCm38: Ensembl release 89: ENSMUSG00000025888 – Ensembl, May 2017
- ^ "Human PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ "Mouse PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ Thornberry NA, Bull HG, Calaycay JR, Chapman KT, Howard AD, Kostura MJ, et al. (April 1992). "A novel heterodimeric cysteine protease is required for interleukin-1 beta processing in monocytes". Nature. 356 (6372): 768–74. Bibcode:1992Natur.356..768T. doi:10.1038/356768a0. PMID 1574116. S2CID 4310923.
- ^ Cerretti DP, Kozlosky CJ, Mosley B, Nelson N, Van Ness K, Greenstreet TA, et al. (April 1992). "Molecular cloning of the interleukin-1 beta converting enzyme". Science. 256 (5053): 97–100. Bibcode:1992Sci...256...97C. doi:10.1126/science.1373520. PMID 1373520.
- ^ a b Mariathasan S, Newton K, Monack DM, Vucic D, French DM, Lee WP, et al. (July 2004). "Differential activation of the inflammasome by caspase-1 adaptors ASC and Ipaf". Nature. 430 (6996): 213–8. Bibcode:2004Natur.430..213M. doi:10.1038/nature02664. PMID 15190255. S2CID 4317409.
- ^ Xia S, Zhang Z, Magupalli VG, Pablo JL, Dong Y, Vora SM, et al. (April 2021). "Gasdermin D pore structure reveals preferential release of mature interleukin-1". Nature. 593 (7860): 607–611. Bibcode:2021Natur.593..607X. doi:10.1038/s41586-021-03478-3. PMC 8588876. PMID 33883744. S2CID 233351704.
- ^ Jorgensen I, Miao EA (May 2015). "Pyroptotic cell death defends against intracellular pathogens". Immunological Reviews. 265 (1): 130–42. doi:10.1111/imr.12287. PMC 4400865. PMID 25879289.
- ^ Bakele M, Joos M, Burdi S, Allgaier N, Pöschel S, Fehrenbacher B, et al. (February 2014). "Localization and functionality of the inflammasome in neutrophils". The Journal of Biological Chemistry. 289 (8): 5320–9. doi:10.1074/jbc.M113.505636. PMC 3931087. PMID 24398679.
- ^ a b Kumaresan V, Ravichandran G, Nizam F, Dhayanithi NB, Arasu MV, Al-Dhabi NA, et al. (February 2016). "Multifunctional murrel caspase 1, 2, 3, 8 and 9: Conservation, uniqueness and their pathogen-induced expression pattern". Fish & Shellfish Immunology. 49: 493–504. Bibcode:2016FSI....49..493K. doi:10.1016/j.fsi.2016.01.008. PMID 26777895.
- ^ Wilson KP, Black JA, Thomson JA, Kim EE, Griffith JP, Navia MA, et al. (July 1994). "Structure and mechanism of interleukin-1 beta converting enzyme". Nature. 370 (6487): 270–5. Bibcode:1994Natur.370..270W. doi:10.1038/370270a0. PMID 8035875. S2CID 4281700.
- ^ a b c Lu A, Li Y, Schmidt FI, Yin Q, Chen S, Fu TM, et al. (May 2016). "Molecular basis of caspase-1 polymerization and its inhibition by a new capping mechanism". Nature Structural & Molecular Biology. 23 (5): 416–25. doi:10.1038/nsmb.3199. PMC 4856535. PMID 27043298.
- ^ Elliott JM, Rouge L, Wiesmann C, Scheer JM (March 2009). "Crystal structure of procaspase-1 zymogen domain reveals insight into inflammatory caspase autoactivation". The Journal of Biological Chemistry. 284 (10): 6546–53. doi:10.1074/jbc.M806121200. PMC 2649088. PMID 19117953.
- ^ a b c Humke EW, Shriver SK, Starovasnik MA, Fairbrother WJ, Dixit VM (September 2000). "ICEBERG: a novel inhibitor of interleukin-1beta generation". Cell. 103 (1): 99–111. doi:10.1016/S0092-8674(00)00108-2. PMID 11051551. S2CID 15886378.
- ^ Samarani S, Allam O, Sagala P, Aldabah Z, Jenabian MA, Mehraj V, et al. (June 2016). "Imbalanced production of IL-18 and its antagonist in human diseases, and its implications for HIV-1 infection". Cytokine. Cytokines in inflammation, aging, cancer and obesity. 82: 38–51. doi:10.1016/j.cyto.2016.01.006. PMID 26898120.
- ^ a b c Vince JE, Silke J (June 2016). "The intersection of cell death and inflammasome activation". Cellular and Molecular Life Sciences. 73 (11–12): 2349–67. doi:10.1007/s00018-016-2205-2. PMC 11108284. PMID 27066895. S2CID 16281016.
- ^ a b c Druilhe A, Srinivasula SM, Razmara M, Ahmad M, Alnemri ES (June 2001). "Regulation of IL-1beta generation by Pseudo-ICE and ICEBERG, two dominant negative caspase recruitment domain proteins". Cell Death and Differentiation. 8 (6): 649–57. doi:10.1038/sj.cdd.4400881. PMID 11536016.
- ^ a b c d Le HT, Harton JA (September 2013). "Pyrin- and CARD-only Proteins as Regulators of NLR Functions". Frontiers in Immunology. 4: 275. doi:10.3389/fimmu.2013.00275. PMC 3775265. PMID 24062743.
- ^ Lamkanfi M, Denecker G, Kalai M, D'hondt K, Meeus A, Declercq W, et al. (December 2004). "INCA, a novel human caspase recruitment domain protein that inhibits interleukin-1beta generation". The Journal of Biological Chemistry. 279 (50): 51729–38. doi:10.1074/jbc.M407891200. PMID 15383541.
- ^ Dorfleutner A, Talbott SJ, Bryan NB, Funya KN, Rellick SL, Reed JC, et al. (December 2007). "A Shope Fibroma virus PYRIN-only protein modulates the host immune response". Virus Genes. 35 (3): 685–94. doi:10.1007/s11262-007-0141-9. PMC 4257706. PMID 17676277.
- ^ Flores J, Noël A, Foveau B, Lynham J, Lecrux C, LeBlanc AC (September 2018). "Caspase-1 inhibition alleviates cognitive impairment and neuropathology in an Alzheimer's disease mouse model". Nature Communications. 9 (1): 3916. Bibcode:2018NatCo...9.3916F. doi:10.1038/s41467-018-06449-x. PMC 6156230. PMID 30254377.
- ^ Boxer MB, Quinn AM, Shen M, Jadhav A, Leister W, Simeonov A, et al. (May 2010). "A highly potent and selective caspase 1 inhibitor that utilizes a key 3-cyanopropanoic acid moiety". ChemMedChem. 5 (5): 730–8. doi:10.1002/cmdc.200900531. PMC 3062473. PMID 20229566.
- ^ Vezzani A, Maroso M, Balosso S, Sanchez MA, Bartfai T (October 2011). "IL-1 receptor/Toll-like receptor signaling in infection, inflammation, stress and neurodegeneration couples hyperexcitability and seizures". Brain, Behavior, and Immunity. 25 (7): 1281–9. doi:10.1016/j.bbi.2011.03.018. PMID 21473909. S2CID 3383795.
- ^ Ainscough JS, Gerberick GF, Kimber I, Dearman RJ (December 2015). "Interleukin-1β Processing Is Dependent on a Calcium-mediated Interaction with Calmodulin". The Journal of Biological Chemistry. 290 (52): 31151–61. doi:10.1074/jbc.M115.680694. PMC 4692238. PMID 26559977.
- ^ He WT, Wan H, Hu L, Chen P, Wang X, Huang Z, et al. (December 2015). "Gasdermin D is an executor of pyroptosis and required for interleukin-1β secretion". Cell Research. 25 (12): 1285–98. doi:10.1038/cr.2015.139. PMC 4670995. PMID 26611636.
- ^ Shi J, Gao W, Shao F (April 2017). "Pyroptosis: Gasdermin-Mediated Programmed Necrotic Cell Death". Trends in Biochemical Sciences. 42 (4): 245–254. doi:10.1016/j.tibs.2016.10.004. PMID 27932073.
- ^ "Entrez Gene: CASP1 caspase 1, apoptosis-related cysteine peptidase (interleukin 1, beta, convertase)".
- ^ Doitsh G, Galloway NL, Geng X, Yang Z, Monroe KM, Zepeda O, et al. (January 2014). "Cell death by pyroptosis drives CD4 T-cell depletion in HIV-1 infection". Nature. 505 (7484): 509–14. Bibcode:2014Natur.505..509D. doi:10.1038/nature12940. PMC 4047036. PMID 24356306.
- ^ Monroe KM, Yang Z, Johnson JR, Geng X, Doitsh G, Krogan NJ, Greene WC (January 2014). "IFI16 DNA sensor is required for death of lymphoid CD4 T cells abortively infected with HIV". Science. 343 (6169): 428–32. Bibcode:2014Sci...343..428M. doi:10.1126/science.1243640. PMC 3976200. PMID 24356113.
- ^ Zhang C, Song JW, Huang HH, Fan X, Huang L, Deng JN, et al. (March 2021). "NLRP3 inflammasome induces CD4+ T cell loss in chronically HIV-1-infected patients". The Journal of Clinical Investigation. 131 (6). doi:10.1172/JCI138861. PMC 7954596. PMID 33720048.
- ^ Sokolovska A, Becker CE, Ip WK, Rathinam VA, Brudner M, Paquette N, et al. (June 2013). "Activation of caspase-1 by the NLRP3 inflammasome regulates the NADPH oxidase NOX2 to control phagosome function". Nature Immunology. 14 (6): 543–53. doi:10.1038/ni.2595. PMC 3708594. PMID 23644505.
- ^ Monteith AJ, Vincent HA, Kang S, Li P, Claiborne TM, Rajfur Z, et al. (July 2018). "mTORC2 Activity Disrupts Lysosome Acidification in Systemic Lupus Erythematosus by Impairing Caspase-1 Cleavage of Rab39a". Journal of Immunology. 201 (2): 371–382. doi:10.4049/jimmunol.1701712. PMC 6039264. PMID 29866702.
External links
[edit]- The MEROPS online database for peptidases and their inhibitors: C14.001[permanent dead link]


![1bmq: CRYSTAL STRUCTURE OF THE COMPLEX OF INTERLEUKIN-1BETA CONVERTING ENZYME (ICE) WITH A PEPTIDE BASED INHIBITOR, (3S )-N-METHANESULFONYL-3-({1-[N-(2-NAPHTOYL)-L-VALYL]-L-PROLYL }AMINO)-4-OXOBUTANAMIDE](http://upload.wikimedia.org/wikipedia/commons/thumb/e/e3/PDB_1bmq_EBI.jpg/180px-PDB_1bmq_EBI.jpg)



![1rwm: Crystal structure of human caspase-1 in complex with 4-oxo-3-[2-(5-{[4-(quinoxalin-2-ylamino)-benzoylamino]-methyl}-thiophen-2-yl)-acetylamino]-pentanoic acid](http://upload.wikimedia.org/wikipedia/commons/thumb/4/4f/PDB_1rwm_EBI.jpg/180px-PDB_1rwm_EBI.jpg)
![1rwn: Crystal structure of human caspase-1 in complex with 3-{2-ethyl-6-[4-(quinoxalin-2-ylamino)-benzoylamino]-hexanoylamino}-4-oxo-butyric acid](http://upload.wikimedia.org/wikipedia/commons/thumb/a/a1/PDB_1rwn_EBI.jpg/180px-PDB_1rwn_EBI.jpg)
![1rwo: Crystal structure of human caspase-1 in complex with 4-oxo-3-{6-[4-(quinoxalin-2-ylamino)-benzoylamino]-2-thiophen-2-yl-hexanoylamino}-pentanoic acid](http://upload.wikimedia.org/wikipedia/commons/thumb/e/e2/PDB_1rwo_EBI.jpg/180px-PDB_1rwo_EBI.jpg)
![1rwp: Crystal structure of human caspase-1 in complex with 3-{6-[(8-hydroxy-quinoline-2-carbonyl)-amino]-2-thiophen-2-yl-hexanoylamino}-4-oxo-butyric acid](http://upload.wikimedia.org/wikipedia/commons/thumb/2/2d/PDB_1rwp_EBI.jpg/180px-PDB_1rwp_EBI.jpg)
![1rwv: Crystal structure of human caspase-1 in complex with 5-[5-(1-carboxymethyl-2-oxo-propylcarbamoyl)-5-phenyl-pentylsulfamoyl]-2-hydroxy-benzoic acid](http://upload.wikimedia.org/wikipedia/commons/thumb/7/70/PDB_1rwv_EBI.jpg/180px-PDB_1rwv_EBI.jpg)
![1rww: Crystal structure of human caspase-1 in complex with 4-oxo-3-[(6-{[4-(quinoxalin-2-ylamino)-benzoylamino]-methyl}-pyridine-3-carbonyl)-amino]-butyric acid](http://upload.wikimedia.org/wikipedia/commons/thumb/8/8a/PDB_1rww_EBI.jpg/180px-PDB_1rww_EBI.jpg)
![1rwx: Crystal structure of human caspase-1 in complex with 4-oxo-3-{6-[4-(quinoxalin-2-yloxy)-benzoylamino]-2-thiophen-2-yl-hexanoylamino}-butyric acid](http://upload.wikimedia.org/wikipedia/commons/thumb/b/ba/PDB_1rwx_EBI.jpg/180px-PDB_1rwx_EBI.jpg)


![2fqq: Crystal structure of human caspase-1 (Cys285->Ala, Cys362->Ala, Cys364->Ala, Cys397->Ala) in complex with 1-methyl-3-trifluoromethyl-1H-thieno[2,3-c]pyrazole-5-carboxylic acid (2-mercapto-ethyl)-amide](http://upload.wikimedia.org/wikipedia/commons/thumb/4/4b/PDB_2fqq_EBI.png/180px-PDB_2fqq_EBI.png)
![2h48: Crystal structure of human caspase-1 (Cys362->Ala, Cys364->Ala, Cys397->Ala) in complex with 3-[2-(2-benzyloxycarbonylamino-3-methyl-butyrylamino)-propionylamino]-4-oxo-pentanoic acid (z-VAD-FMK)](http://upload.wikimedia.org/wikipedia/commons/thumb/a/a0/PDB_2h48_EBI.png/180px-PDB_2h48_EBI.png)
![2hbq: Crystal structure of wildtype human caspase-1 in complex with 3-[2-(2-benzyloxycarbonylamino-3-methyl-butyrylamino)-propionylamino]-4-oxo-pentanoic acid (z-VAD-FMK)](http://upload.wikimedia.org/wikipedia/commons/thumb/e/e6/PDB_2hbq_EBI.png/180px-PDB_2hbq_EBI.png)
![2hbr: Crystal structure of human caspase-1 (Arg286->Ala) in complex with 3-[2-(2-benzyloxycarbonylamino-3-methyl-butyrylamino)-propionylamino]-4-oxo-pentanoic acid (z-VAD-FMK)](http://upload.wikimedia.org/wikipedia/commons/thumb/5/52/PDB_2hbr_EBI.png/180px-PDB_2hbr_EBI.png)
![2hby: Crystal structure of human caspase-1 (Glu390->Ala) in complex with 3-[2-(2-benzyloxycarbonylamino-3-methyl-butyrylamino)-propionylamino]-4-oxo-pentanoic acid (z-VAD-FMK)](http://upload.wikimedia.org/wikipedia/commons/thumb/6/6d/PDB_2hby_EBI.png/180px-PDB_2hby_EBI.png)
![2hbz: Crystal structure of human caspase-1 (Arg286->Ala, Glu390->Ala) in complex with 3-[2-(2-benzyloxycarbonylamino-3-methyl-butyrylamino)-propionylamino]-4-oxo-pentanoic acid (z-VAD-FMK)](http://upload.wikimedia.org/wikipedia/commons/thumb/f/f4/PDB_2hbz_EBI.png/180px-PDB_2hbz_EBI.png)