COVID-19 vaccine clinical research: Difference between revisions
m Added categories and a section for references |
Contents WP:SPLIT from COVID-19 vaccine; please see its history for attribution |
||
| Line 2: | Line 2: | ||
'''COVID-19 vaccine clinical research''' concerns the [[clinical research]] on [[COVID-19 vaccine|COVID-19 vaccines]]. There are 22 vaccines authorized for use by national governments, with 5 of them in [[Phases of clinical research|Phase IV]], and 204 vaccines under clinical trials that have not yet been authorized. There are also 9 clinical trials on [[Heterologous vaccine|heterologous]] vaccination courses. |
'''COVID-19 vaccine clinical research''' concerns the [[clinical research]] on [[COVID-19 vaccine|COVID-19 vaccines]]. There are 22 vaccines authorized for use by national governments, with 5 of them in [[Phases of clinical research|Phase IV]], and 204 vaccines under clinical trials that have not yet been authorized. There are also 9 clinical trials on [[Heterologous vaccine|heterologous]] vaccination courses. |
||
==Trial and authorization status== |
|||
Phase I trials test primarily for safety and preliminary dosing in a few dozen healthy subjects, while Phase{{nbs}}II trials{{snd}}following success in Phase{{nbs}}I{{snd}}evaluate [[immunogenicity]], dose levels (efficacy based on [[biomarker]]s) and adverse effects of the candidate vaccine, typically in hundreds of people.<ref name="Vaccines.gov" /><ref name="fda-ddp" /> A Phase{{nbs}}I–II trial consists of preliminary safety and immunogenicity testing, is typically randomized, placebo-controlled, while determining more precise, effective doses.<ref name="fda-ddp" /> Phase{{nbs}}III trials typically involve more participants at multiple sites, include a [[control group]], and test effectiveness of the vaccine to prevent the disease (an "interventional" or "pivotal" trial), while monitoring for [[adverse effect]]s at the optimal dose.<ref name="Vaccines.gov" /><ref name="fda-ddp" /> Definition of vaccine safety, efficacy, and [[clinical endpoint]]s in a Phase{{nbs}}III trial may vary between the trials of different companies, such as defining the degree of side effects, infection or amount of transmission, and whether the vaccine prevents moderate or severe COVID‑19 infection.<ref name="cohen6-19" /><ref name="cdc-eff">{{#invoke:Cite web| |date=29 January 2016|title=How flu vaccine effectiveness and efficacy are measured|url=https://www.cdc.gov/flu/vaccines-work/effectivenessqa.htm?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fflu%2Fprofessionals%2Fvaccination%2Feffectivenessqa.htm|archive-url=https://web.archive.org/web/20200507083203/https://www.cdc.gov/flu/vaccines-work/effectivenessqa.htm?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fflu%2Fprofessionals%2Fvaccination%2Feffectivenessqa.htm|archive-date=7 May 2020|url-status=live|access-date=6 May 2020|publisher=U.S. [[Centers for Disease Control and Prevention]] (CDC) }}</ref><ref>{{#invoke:Cite web| |date=18 May 2012|title=Principles of epidemiology, Section 8: Concepts of disease occurrence|url=https://www.cdc.gov/csels/dsepd/ss1978/lesson1/section8.html|archive-url=https://web.archive.org/web/20200406212227/https://www.cdc.gov/csels/dsepd/ss1978/lesson1/section8.html|archive-date=6 April 2020|url-status=live|access-date=6 May 2020|publisher=U.S. [[Centers for Disease Control and Prevention]] (CDC) }}</ref> |
|||
A clinical trial design in progress may be modified as an [[Adaptive design (medicine)|"adaptive design"]] if accumulating data in the trial provide early insights about positive or negative efficacy of the treatment.<ref name="pallmann">{{Cite journal |display-authors=6 |vauthors=Pallmann P, Bedding AW, Choodari-Oskooei B, Dimairo M, Flight L, Hampson LV, Holmes J, Mander AP, Odondi L, Sydes MR, Villar SS, Wason JM, Weir CJ, Wheeler GM, Yap C, Jaki T |date=February 2018 |title=Adaptive designs in clinical trials: why use them, and how to run and report them |journal=BMC Medicine |volume=16 |issue=1 |pages=29 |doi=10.1186/s12916-018-1017-7 |pmc=5830330 |pmid=29490655}}</ref><ref name="fda-adaptive">{{#invoke:Cite web| |date=1 November 2019|title=Adaptive designs for clinical trials of drugs and biologics: Guidance for industry|url=https://www.fda.gov/media/78495/download|archive-url=https://web.archive.org/web/20191213234438/https://www.fda.gov/media/78495/download|archive-date=13 December 2019|url-status=live|access-date=3 April 2020|publisher=U.S. [[Food and Drug Administration]] (FDA)|format=PDF}}</ref> Adaptive designs within ongoing Phase{{nbs}}II–III clinical trials on candidate vaccines may shorten trial durations and use fewer subjects, possibly expediting decisions for early termination or success, avoiding duplication of research efforts, and enhancing coordination of design changes for the Solidarity trial across its international locations.<ref name="pallmann" /><ref name="solidarity-vacc2">{{#invoke:Cite web| |date=9 April 2020|title=An international randomised trial of candidate vaccines against COVID-19: Outline of Solidarity vaccine trial|url=https://www.who.int/blueprint/priority-diseases/key-action/Outline_CoreProtocol_vaccine_trial_09042020.pdf|archive-url=https://web.archive.org/web/20200512115627/https://www.who.int/blueprint/priority-diseases/key-action/Outline_CoreProtocol_vaccine_trial_09042020.pdf|archive-date=12 May 2020|url-status=live|access-date=9 May 2020|publisher=[[World Health Organization]] (WHO)}}</ref> |
|||
===List of authorized and approved vaccines=== |
|||
{{Further|List of COVID-19 vaccine authorizations}} |
|||
{{for|COVID-19 vaccination policy by country|Vaccination policy#Table}} |
|||
National [[regulation of therapeutic goods|regulatory authorities]] have granted emergency use authorizations for fifteen vaccines. Six of those have been approved for emergency or full use by at least one WHO-recognized [[List of stringent regulatory authorities|stringent regulatory authority]]. [[Biologic License Application]]s for the Pfizer–BioNTech and Moderna COVID‑19 vaccines have been submitted to the US [[Food and Drug Administration]] (FDA).<ref>{{Cite press release |title=Pfizer and BioNTech Initiate Rolling Submission of Biologics License Application for U.S. FDA Approval of Their COVID 19 Vaccine |date=7 May 2021 |url=https://www.pfizer.com/news/press-release/press-release-detail/pfizer-and-biontech-initiate-rolling-submission-biologics |access-date=9 June 2021 |website=Pfizer}}</ref><ref>{{Cite press release |title=Moderna Announces Initiation of Rolling Submission of Biologics License Application (BLA) with U.S. FDA for the Moderna COVID-19 Vaccine |date=1 June 2021 |publisher=Moderna |url=https://www.businesswire.com/news/home/20210601005270/en/Moderna-Announces-Initiation-of-Rolling-Submission-of-Biologics-License-Application-BLA-with-U.S.-FDA-for-the-Moderna-COVID-19-Vaccine |access-date=9 June 2021 |via=Business Wire}}</ref> |
|||
<gallery mode="packed" heights="180"> |
|||
COVID-19 RNA vaccines authorization map.svg|<div style="text-align:left">[[RNA vaccine]]s and [[DNA vaccine]]s{{Legend|#800080|[[Pfizer–BioNTech COVID-19 vaccine|Pfizer–BioNTech]]}}{{Legend|#008800|[[Moderna COVID-19 vaccine|Moderna]]}}{{Legend|#008CFF|[[ZyCoV-D]]}}</div> |
|||
COVID-19 adenovirus vaccines authorization map.svg|<div style="text-align:left">[[Viral vector vaccine|Adenovirus vector vaccines]]{{Legend|#000088|[[Oxford–AstraZeneca COVID-19 vaccine|Oxford–AstraZeneca]]}}{{Legend|#008800|[[Janssen COVID-19 vaccine|Janssen]]}}{{Legend|#880000|[[Sputnik V COVID-19 vaccine|Sputnik V]]}}{{Legend|#FF008C|[[Sputnik Light]]}}{{Legend|#888800|[[Convidecia]]}}</div> |
|||
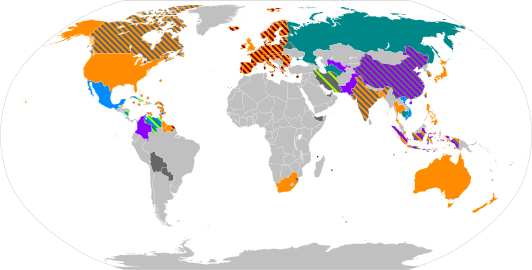
COVID-19 inactivated vaccines authorization map.svg|<div style="text-align:left">[[Inactivated vaccine|Inactivated virus vaccines]]{{Legend|#008888|[[BBIBP-CorV|Sinopharm (BBIBP)]]}}{{Legend|#888800|[[CoronaVac]]}}{{Legend|#800080|[[BBV152|Covaxin]]}}{{Legend|#FF8C00|[[w:WIBP-CorV|Sinopharm (WIBP)]]}}{{Legend|#666666|Others}}</div> |
|||
COVID-19 subunit and VLP vaccines authorization map.svg|<div style="text-align:left">[[Subunit vaccine]]s{{Legend|#008888|[[EpiVacCorona]]}}{{Legend|#8C00FF|[[ZF2001]]}}{{Legend|#880000|[[w:Abdala (vaccine)|Abdala]]}}{{Legend|#000088|[[w:Soberana 02|Soberana 02]]}}{{Legend|#FF008C|[[w:MVC-COV1901|Medigen (MVC)]]}}</div> |
|||
</gallery> |
|||
The table below shows various vaccines authorized either for full or emergency use so far, with various other details. |
|||
{| class="wikitable mw-collapsible mw-collapsed" |
|||
| '''COVID-19 vaccines authorized for emergency use or approved for full use''' |
|||
|- |
|||
| {{COVID-19 vaccine authorizations}} |
|||
|} |
|||
<!--Template is at: [[Template:COVID-19 vaccine authorizations]] --> |
|||
===Vaccine candidates in human trials=== |
|||
The table below shows various vaccine candidates and the phases which they have completes so far. Current phases are also shown alongwith other details. |
|||
{| class="wikitable mw-collapsible mw-collapsed" |
|||
| '''COVID‑19 candidate vaccines in Phase I–III trials''' |
|||
|- |
|||
| {{COVID-19 vaccine candidates}} |
|||
|} |
|||
<!--Template is at: [[Template:COVID-19 vaccine candidates]] --> |
|||
==== Homologous prime-boost vaccination ==== |
|||
In July 2021, the U.S. [[Food and Drug Administration]] (FDA) and the [[Centers for Disease Control and Prevention]] (CDC) issued a joint statement reporting that a booster dose is not necessary for those who have been fully vaccinated.<ref name="FDA PR 20210708">{{Cite press release |title=Joint CDC and FDA Statement on Vaccine Boosters |date=8 July 2021 |url=https://www.fda.gov/news-events/press-announcements/joint-cdc-and-fda-statement-vaccine-boosters |access-date=9 July 2021 |website=U.S. [[Food and Drug Administration]] (FDA)}} {{PD-notice}}</ref> |
|||
In August 2021, the FDA and the CDC authorized the use of an additional mRNA vaccine dose for immunocompromised individuals.<ref>{{Cite press release |title=Coronavirus (COVID-19) Update: FDA Authorizes Additional Vaccine Dose for Certain Immunocompromised Individuals |date=12 August 2021 |url=https://www.fda.gov/news-events/press-announcements/coronavirus-covid-19-update-fda-authorizes-additional-vaccine-dose-certain-immunocompromised |access-date=13 August 2021 |website=U.S. [[Food and Drug Administration]] (FDA)}}</ref><ref>{{Cite web |date=13 August 2021 |title=COVID-19 Vaccines for Moderately to Severely Immunocompromised People |url=https://www.cdc.gov/coronavirus/2019-ncov/vaccines/recommendations/immuno.html |access-date=13 August 2021 |website=Centers for Disease Control and Prevention}}</ref> |
|||
==== Heterologous prime-boost vaccination ==== |
|||
Some experts believe that [[Heterologous vaccine|heterologous]] [[Booster dose|prime-boost]] vaccination courses can boost immunity, and several studies have begun to examine this effect.<ref>{{Cite journal |last=Ledford |first=Heidi |date=18 February 2021 |title=Could mixing COVID vaccines boost immune response? |url=http://www.nature.com/articles/d41586-021-00315-5 |journal=Nature |volume=590 |issue=7846 |pages=375–376 |bibcode=2021Natur.590..375L |doi=10.1038/d41586-021-00315-5 |issn=0028-0836 |pmid=33547431 |s2cid=231946137}}</ref> Despite the absence of clinical data on the efficacy and safety of such heterologous combinations, Canada and several European countries have recommended a heterologous second dose for people who have received the first dose of the [[Oxford–AstraZeneca COVID-19 vaccine|Oxford–AstraZeneca vaccine]].<ref>{{Cite news |date=22 June 2021 |title=Angela Merkel receives Moderna dose after first AstraZeneca shot |work=Al Jazeera |url=https://www.aljazeera.com/news/2021/6/22/angela-merkel-moderna-after-first-astrazeneca-vaccine |access-date=28 June 2021}}</ref> |
|||
In February 2021, the [[Oxford Vaccine Group]] launched the Com-COV vaccine trial to investigate heterologous prime-boost courses of different COVID-19 vaccines.<ref>{{Cite news |date=30 March 2021 |title=Getting One Vaccine Is Good. How About Mix-and-Match? |work=[[The New York Times]] |url=https://www.nytimes.com/2021/03/30/health/coronavirus-vaccine-astrazeneca-pfizer.html |access-date=30 June 2021}}</ref> As of June 2021, the group is conducting two phase II studies: Com-COV and Com-COV2.<ref>{{#invoke:Cite web ||title=About |url=https://comcovstudy.org.uk/about |access-date=28 June 2021 |website=Com-COV}}</ref> |
|||
In Com-COV, the two heterologous combinations of the [[Oxford–AstraZeneca COVID-19 vaccine|Oxford–AstraZeneca]] and [[Pfizer–BioNTech COVID-19 vaccine|Pfizer–BioNTech]] vaccines were compared with the two homologous combinations of the same vaccines, with an interval of 28 or 84 days between doses.<ref name="ISRCTN69254139" /><ref>{{Cite ssrn |title=Safety and Immunogenicity Report from the Com-COV Study – a Single-Blind Randomised Non-Inferiority Trial Comparing Heterologous And Homologous Prime-Boost Schedules with An Adenoviral Vectored and mRNA COVID-19 Vaccine |date=June 2021 |ssrn=3874014}}</ref>{{unreliable medical source|reason=preprint|date=July 2021}} |
|||
In Com-COV2, the first dose is the Oxford–AstraZeneca vaccine or the Pfizer vaccine, and the second dose is the [[Moderna COVID-19 vaccine|Moderna vaccine]], the [[Novavax COVID-19 vaccine|Novavax vaccine]], or a homologous vaccine equal to the first dose, with an interval of 56 or 84 days between doses.<ref name="ISRCTN27841311" /> |
|||
A study in the UK is evaluating annual heterologous boosters using the following randomly selected vaccines: [[Oxford–AstraZeneca COVID-19 vaccine|Oxford–AstraZeneca]], [[Pfizer–BioNTech COVID-19 vaccine|Pfizer–BioNTech]], [[Moderna COVID-19 vaccine|Moderna]], [[Novavax COVID-19 vaccine|Novavax]], [[VLA2001]], [[CureVac COVID-19 vaccine|CureVac]], and [[Janssen COVID-19 vaccine|Janssen]].<ref name="ISRCTN73765130">{{Cite journal |last=Faust |first=Saul |date=27 April 2021 |title=Evaluating COVID-19 Vaccination Boosters |url=https://www.isrctn.com/ISRCTN73765130 |doi=10.1186/ISRCTN73765130 |id=ISRCTN73765130 |access-date=9 July 2021 |website=ISRCTN Registry}}</ref> |
|||
{| class="wikitable sortable mw-collapsible" |
|||
|+Heterologous regimes in clinical trial |
|||
|- |
|||
!scope="col"|First dose |
|||
!scope="col"|Second dose |
|||
!scope="col"|Schedules |
|||
!scope="col"|Current phase (participants), periods and locations |
|||
|- |
|||
|{{br list|[[Oxford–AstraZeneca COVID-19 vaccine|Oxford–AstraZeneca]]|[[Pfizer–BioNTech COVID-19 vaccine|Pfizer–BioNTech]]}} |
|||
|{{br list|[[Oxford–AstraZeneca COVID-19 vaccine|Oxford–AstraZeneca]]|[[Pfizer–BioNTech COVID-19 vaccine|Pfizer–BioNTech]]}} |
|||
|{{br list|Days 0 and 28|Days 0 and 84}} |
|||
|{{ClinicalStudyInfo |phase=2 |participants=820 |
|||
|references=<ref name="ISRCTN69254139">{{Cite journal |last1=Stuart |first1=Arabella |last2=Shaw |first2=Robert |last3=Walker |first3=Laura |date=29 January 2021 |title=Comparing coronavirus (COVID-19) vaccine schedule combinations |url=http://www.isrctn.com/ISRCTN69254139 |doi=10.1186/ISRCTN69254139 |id=ISRCTN69254139 |access-date=9 July 2021 |website=ISRCTN Registry}}</ref> |
|||
|whenwhere=Feb{{ndash}}Aug 2021, United Kingdom}} |
|||
|- |
|||
|[[Sputnik Light]] |
|||
|{{br list|[[Oxford–AstraZeneca COVID-19 vaccine|Oxford–AstraZeneca]]|[[Moderna COVID-19 vaccine|Moderna]]|[[BBIBP-CorV]]}} |
|||
| |
|||
|{{ClinicalStudyInfo |phase=2 |participants=121 |
|||
|references=<ref>{{Cite press release |title=Combination of the first component of Sputnik V vaccine (Sputnik Light vaccine) with vaccines by AstraZeneca, Sinopharm and Moderna demonstrates high safety profile during the study in Argentina's Buenos-Aires province |date=4 August 2021 |publisher=Russian Direct Investment Fund |location=Moscow |url=https://rdif.ru/Eng_fullNews/7035/ |access-date=5 August 2021}}</ref> |
|||
|whenwhere=Feb{{ndash}}Aug 2021, Argentina}} |
|||
|- |
|||
|{{br list|[[Oxford–AstraZeneca COVID-19 vaccine|Oxford–AstraZeneca]]|[[Pfizer–BioNTech COVID-19 vaccine|Pfizer–BioNTech]]}} |
|||
|{{br list|[[Oxford–AstraZeneca COVID-19 vaccine|Oxford–AstraZeneca]]|[[Pfizer–BioNTech COVID-19 vaccine|Pfizer–BioNTech]]|[[Moderna COVID-19 vaccine|Moderna]]|[[Novavax COVID-19 vaccine|Novavax]]}} |
|||
|Days 0 and 56{{ndash}}84 |
|||
|{{ClinicalStudyInfo |phase=2 |participants=1050 |
|||
|references=<ref name="ISRCTN27841311">{{Cite journal |last1=Vichos |first1=Iason |last2=Snape |first2=Matthew |date=12 March 2021 |title=Comparing COVID-19 vaccine schedule combinations – stage 2 |url=https://www.isrctn.com/ISRCTN27841311 |doi=10.1186/ISRCTN27841311 |id=ISRCTN27841311 |access-date=9 July 2021 |website=ISRCTN Registry}}</ref> |
|||
|whenwhere=Mar 2021{{snd}}Sep 2022, United Kingdom}} |
|||
|- |
|||
|[[Convidecia]] |
|||
|[[ZF2001]] |
|||
|{{br list|Days 0 and 28|Days 0 and 56}} |
|||
|{{ClinicalStudyInfo |phase=4 |participants=120 |
|||
|references=<ref name="NCT04833101">{{Cite journal |date=6 April 2021 |title=Study on Sequential Immunization of Recombinant COVID-19 Vaccine (Ad5 Vector) and RBD-based Protein Subunit Vaccine |url=https://clinicaltrials.gov/ct2/show/NCT04833101 |id=NCT04833101 |access-date=9 July 2021 |website=ClinicalTrials.gov}}</ref> |
|||
|whenwhere=Apr{{ndash}}Dec 2021, China}} |
|||
|- |
|||
|[[Oxford–AstraZeneca COVID-19 vaccine|Oxford–AstraZeneca]] |
|||
|[[Pfizer–BioNTech COVID-19 vaccine|Pfizer–BioNTech]] |
|||
|Days 0 and 28 |
|||
|{{ClinicalStudyInfo |phase=2 |participants=676 |
|||
|references=<ref name="NCT04860739">{{Cite journal |date=27 April 2021 |title=Vaccination With COMIRNATY in Subjects With a VAXZEVRIA First Dose (CombiVacS) |url=https://clinicaltrials.gov/ct2/show/NCT04860739 |id=NCT04860739 |access-date=9 July 2021 |website=ClinicalTrials.gov}}</ref> |
|||
|whenwhere=Apr 2021{{snd}}Apr 2022, Spain}} |
|||
|- |
|||
|{{br list|[[Oxford–AstraZeneca COVID-19 vaccine|Oxford–AstraZeneca]]|[[Pfizer–BioNTech COVID-19 vaccine|Pfizer–BioNTech]]|[[Moderna COVID-19 vaccine|Moderna]]}} |
|||
|{{br list|[[Pfizer–BioNTech COVID-19 vaccine|Pfizer–BioNTech]]|[[Moderna COVID-19 vaccine|Moderna]]}} |
|||
|{{br list|Days 0 and 28|Days 0 and 112}} |
|||
|{{ClinicalStudyInfo |phase=2 |participants=1200 |
|||
|references=<ref name="NCT04894435">{{Cite journal |date=20 May 2021 |title=Mix and Match of the Second COVID-19 Vaccine Dose for Safety and Immunogenicity (MOSAIC) |url=https://clinicaltrials.gov/ct2/show/NCT04894435 |id=NCT04894435 |access-date=9 July 2021 |website=ClinicalTrials.gov}}</ref> |
|||
|whenwhere=May 2021{{snd}}Mar 2023, Canada}} |
|||
|- |
|||
|{{br list|[[Pfizer–BioNTech COVID-19 vaccine|Pfizer–BioNTech]]|[[Moderna COVID-19 vaccine|Moderna]]}} |
|||
|{{br list|[[Pfizer–BioNTech COVID-19 vaccine|Pfizer–BioNTech]]|[[Moderna COVID-19 vaccine|Moderna]]}} |
|||
|Days 0 and 42 |
|||
|{{ClinicalStudyInfo |phase=2 |participants=400 |
|||
|references=<ref name="NCT04900467">{{Cite journal |date=25 May 2021 |title=Compare Immunological Efficacy of a Vaccine Regimen Combining Two Covid19 mRNA Vaccines (Pfizer-BioNTech and Moderna) With That of a Homologous Vaccination of Each Covid19 mRNA Vaccine (ARNCOMBI) |url=https://clinicaltrials.gov/ct2/show/NCT04900467 |id=NCT04900467 |access-date=9 July 2021 |website=ClinicalTrials.gov}}</ref> |
|||
|whenwhere=May 2021{{snd}}Jan 2022, France}} |
|||
|- |
|||
|[[Oxford–AstraZeneca COVID-19 vaccine|Oxford–AstraZeneca]] |
|||
|[[Pfizer–BioNTech COVID-19 vaccine|Pfizer–BioNTech]] |
|||
|{{br list|Days 0 and 28|Days 0 and 21{{ndash}}49}} |
|||
|{{ClinicalStudyInfo |phase=2 |participants=3000 |
|||
|references=<ref name="NCT04907331">{{Cite journal |date=28 May 2021 |title=Heterologous Vaccination With an Vaxzevria (ChAdOx1-S) Prime and a Comirnaty (BNT162b2) Boost Compared With Homolog Vaccination With Vaxzervria (Prime/Boost) or Comirnaty (Prime/Boost) (HeVacc) |url=https://clinicaltrials.gov/ct2/show/NCT04907331 |id=NCT04907331 |access-date=9 July 2021 |website=ClinicalTrials.gov}}</ref> |
|||
|whenwhere=May{{ndash}}Dec 2021, Austria}} |
|||
|- |
|||
|[[Janssen COVID-19 vaccine|Janssen]] |
|||
|{{br list|[[Pfizer–BioNTech COVID-19 vaccine|Pfizer–BioNTech]]|[[Janssen COVID-19 vaccine|Janssen]]|[[Moderna COVID-19 vaccine|Moderna]]}} |
|||
|Days 0 and 84 |
|||
|{{ClinicalStudyInfo |phase=2 |participants=432 |
|||
|references=<ref name="NCT04927936">{{Cite journal |last=Kuy |first=Hugo van der |date=16 June 2021 |title=A Trial Among HealthCare Workers (HCW) Vaccinated With Janssen Vaccine: the SWITCH Trial (SWITCH) |url=https://clinicaltrials.gov/ct2/show/NCT04927936 |id=NCT04927936 |access-date=9 July 2021 |website=ClinicalTrials.gov}}</ref> |
|||
|whenwhere=Jun 2021{{snd}}Sep 2022, Netherlands}} |
|||
|} |
|||
==Efficacy== |
|||
{{Split section|date=August 2020}} |
|||
[[File:BNT162b2 vaccine efficacy data.png|thumb|upright=1.2|Cumulative incidence curves for symptomatic COVID‑19 infections after the first dose of the Pfizer–BioNTech vaccine (tozinameran) or placebo in a double-blind clinical trial. (red: placebo; blue: tozinameran)<ref name=":11">{{#invoke:Cite web| |date=10 December 2020|title=FDA Briefing Document: Pfizer–BioNTech COVID-19 Vaccine|url=https://www.fda.gov/media/144245/download|access-date=1 January 2021|publisher=U.S. [[Food and Drug Administration]] (FDA)|format=PDF}}</ref>]] |
|||
[[Vaccine efficacy]] is the reduction in risk of getting the disease by vaccinated participants in a controlled trial compared with the risk of getting the disease by unvaccinated participants.<ref name="NYT-20201120">{{Cite news |author-link=Carl Zimmer |date=20 November 2020 |title=2 Companies Say Their Vaccines Are 95% Effective. What Does That Mean? You might assume that 95 out of every 100 people vaccinated will be protected from Covid-19. But that's not how the math works. |work=[[The New York Times]] |url=https://www.nytimes.com/2020/11/20/health/covid-vaccine-95-effective.html |access-date=21 November 2020 |vauthors=Zimmer C}}</ref> An efficacy of 0% means that the vaccine does not work (identical to placebo). An efficacy of 50% means that there are half as many cases of infection as in unvaccinated individuals.{{citation needed|date=July 2021}} |
|||
The vaccine's efficacy may be adversely effected if the arm is held improperly or squeezed so the vaccine is [[subcutaneous injection|injected subcutaneously]] instead of [[intramuscular injection|into the muscle]].<ref>{{#invoke:Cite web||url=https://www.nbcmiami.com/news/donotsqueezemyarm-doctor-sounds-alarm-on-how-to-properly-inject-covid-19-vaccine/2353866/|title=#DoNotSqueezeMyArm: Doctor Sounds Alarm on How to Properly Inject COVID-19 Vaccine}}</ref><ref>{{Cite journal |last=Ng |first=Jia Yu |date=1 June 2021 |title=Inadvertent subcutaneous injection of COVID-19 vaccine |url=https://pmj.bmj.com/content/97/1148/400 |journal=Postgraduate Medical Journal |volume=97 |issue=1148 |pages=400 |doi=10.1136/postgradmedj-2021-139870 |pmc=7886662 |pmid=33589486 |via=pmj.bmj.com}}</ref> The CDC guidance is to not repeat doses that are administered subcutaneously.<ref>https://www.cdc.gov/vaccines/covid-19/downloads/covid19-vaccine-errors-deviations.pdf</ref> |
|||
It is not straightforward to compare the efficacies of the different vaccines because the trials were run with different populations, geographies, and variants of the virus.<ref>{{#invoke:Cite web| | vauthors = Branswell H | title=Comparing three Covid-19 vaccines: Pfizer, Moderna, J&J | website=[[Stat (website)|Stat]] | date=2 February 2021 | url=https://www.statnews.com/2021/02/02/comparing-the-covid-19-vaccines-developed-by-pfizer-moderna-and-johnson-johnson/ | access-date=28 February 2021}}</ref> In the case of COVID‑19, a vaccine [[Intrinsic activity|efficacy]] of 67% may be enough to slow the pandemic, but the current vaccines do not confer [[sterilizing immunity]],<ref>{{Cite web |date=16 August 2021 |title=Bharat's Intranasal Covid-19 Vaccine Moves Forward |url=https://www.pharmalive.com/bharats-intranasal-covid-19-vaccine-moves-forward/}}</ref> which is necessary to prevent transmission. Vaccine efficacy reflects disease prevention, a poor indicator of transmissibility of SARS‑CoV‑2 since asymptomatic people can be highly infectious.<ref name="RandolphHE2020May">{{Cite journal |vauthors=Randolph HE, Barreiro LB |date=May 2020 |title=Herd Immunity: Understanding COVID-19 |journal=Immunity |volume=52 |issue=5 |pages=737–41 |doi=10.1016/j.immuni.2020.04.012 |pmc=7236739 |pmid=32433946}}</ref> The US [[Food and Drug Administration]] (FDA) and the [[European Medicines Agency]] (EMA) set a cutoff of 50% as the efficacy required to approve a COVID‑19 vaccine, with the lower limit of the 95% [[confidence interval]] being greater than 30%.<ref>{{#invoke:Cite web| |title=The FDA's cutoff for Covid-19 vaccine effectiveness is 50 percent. What does that mean?|url=https://www.nbcnews.com/health/health-news/fda-s-cutoff-covid-19-vaccine-effectiveness-50-percent-what-n1245506|access-date=8 January 2021|website=[[NBCNews.com]]}}</ref><ref>{{#invoke:Cite web| |title=EMA sets 50% efficacy goal – with flexibility – for COVID vaccines|url=https://www.raps.org/news-and-articles/news-articles/2020/11/for-ema-50-efficacy-with-flexibility-is-goal-for-c|access-date=8 January 2021|website=Regulatory Affairs Professionals Society (RAPS)}}</ref><ref>{{Cite journal |display-authors=6 |vauthors=Krause P, Fleming TR, Longini I, Henao-Restrepo AM, Peto R, Dean NE, Halloran ME, Huang Y, Fleming TR, Gilbert PB, DeGruttola V |date=12 September 2020 |title=COVID-19 vaccine trials should seek worthwhile efficacy |journal=The Lancet |volume=396 |issue=10253 |pages=741–743 |doi=10.1016/S0140-6736(20)31821-3 |pmc=7832749 |pmid=32861315 |doi-access=free |title-link=doi}}</ref> Aiming for a realistic population vaccination coverage rate of 75%, and depending on the actual [[basic reproduction number]], the necessary effectiveness of a COVID-19 vaccine is expected to need to be at least 70% to prevent an epidemic and at least 80% to extinguish it without further measures, such as social distancing.<ref name="efficacy-needed">{{Cite journal |display-authors=6 |vauthors=Bartsch SM, O'Shea KJ, Ferguson MC, Bottazzi ME, Wedlock PT, Strych U, McKinnell JA, Siegmund SS, Cox SN, Hotez PJ, Lee BY |date=October 2020 |title=Vaccine Efficacy Needed for a COVID-19 Coronavirus Vaccine to Prevent or Stop an Epidemic as the Sole Intervention |journal=American Journal of Preventive Medicine |volume=59 |issue=4 |pages=493–503 |doi=10.1016/j.amepre.2020.06.011 |pmc=7361120 |pmid=32778354}}</ref> |
|||
The observed substantial efficacy of certain mRNA vaccines even after partial (1-dose) immunization<ref>{{Cite web |date=2020-12-17 |title=FDA Briefing Document for mRNA 1273 |url=https://www.fda.gov/media/144434/download |url-status=live |access-date=2021-08-18}}</ref><ref name=":11" /> indicates a non-linear dose-efficacy relation already seen in the phase I-II study<ref>{{Cite journal |last1=Anderson |first1=Evan J. |last2=Rouphael |first2=Nadine G. |last3=Widge |first3=Alicia T. |last4=Jackson |first4=Lisa A. |last5=Roberts |first5=Paul C. |last6=Makhene |first6=Mamodikoe |last7=Chappell |first7=James D. |last8=Denison |first8=Mark R. |last9=Stevens |first9=Laura J. |last10=Pruijssers |first10=Andrea J. |last11=McDermott |first11=Adrian B. |date=2020-12-17 |title=Safety and Immunogenicity of SARS-CoV-2 mRNA-1273 Vaccine in Older Adults |url=https://doi.org/10.1056/NEJMoa2028436 |journal=New England Journal of Medicine |volume=383 |issue=25 |pages=2427–2438 |doi=10.1056/NEJMoa2028436 |issn=0028-4793 |pmc=7556339 |pmid=32991794}}</ref> and suggests that personalization of the vaccine dose (regular dose to the elderly, reduced dose to the healthy young,<ref name="Hunziker 805–820">{{Cite journal |last=Hunziker |first=Patrick |date=2021-07-24 |title=Personalized-dose Covid-19 vaccination in a wave of virus Variants of Concern: Trading individual efficacy for societal benefit |url=https://precisionnanomedicine.com/article/26101-personalized-dose-covid-19-vaccination-in-a-wave-of-virus-variants-of-concern-trading-individual-efficacy-for-societal-benefit |journal=Precision Nanomedicine |language=en |volume=4 |issue=3 |pages=805–820 |doi=10.33218/001c.26101|doi-access=free }}</ref> additional booster dose to the immunosuppressed<ref>{{Cite web |last=Dooling |first=Kathleen |date=2021-08-13 |title=Evidence to Recommendations Framework: Additional doses of mRNA COVID-19 vaccines as part of a primary series for immunocompromised |url=https://www.cdc.gov/vaccines/acip/meetings/downloads/slides-2021-08-13/02-COVID-Dooling-508.pdf |url-status=live |website=CDC Advisory Board for Immunization Practices}}</ref>) might allow accelerating vaccination campaigns in settings of limited supplies, thereby shortening the pandemic, as predicted by pandemic modeling.<ref>{{Cite journal |last1=Chen |first1=Zhimin |last2=Liu |first2=Kaihui |last3=Liu |first3=Xiuxiang |last4=Lou |first4=Yijun |date=February 2020 |title=Modelling epidemics with fractional-dose vaccination in response to limited vaccine supply |url=https://linkinghub.elsevier.com/retrieve/pii/S0022519319304540 |journal=Journal of Theoretical Biology |language=en |volume=486 |pages=110085 |bibcode=2020JThBi.48610085C |doi=10.1016/j.jtbi.2019.110085 |pmid=31758966}}</ref> |
|||
Ranges below are 95% [[confidence interval]]s unless indicated otherwise, and all values are for all participants regardless of age, according to the references for each of the trials. By definition, the [[Margin of error|accuracy]] of the estimates without an associated confidence interval is unknown publicly. Efficacy against severe COVID-19 is the most important, since hospitalizations and deaths are a public health burden whose prevention is a priority.<ref>{{Cite journal |vauthors=Dean N, Madewell Z |date=5 March 2021 |title=Understanding the spectrum of vaccine efficacy measures |url=https://blogs.bmj.com/bmj/2021/03/05/understanding-the-spectrum-of-vaccine-efficacy-measures/ |journal=The BMJ Opinion |access-date=10 March 2021}}</ref> Authorized and approved vaccines have shown the following efficacies: |
|||
<!-- good means the estimate follows WHO, FDA and EMA requirements: minimum 50% point estimate AND minimum 30% lower limit of the 95% CI --> |
|||
{| class="wikitable sortable" |
|||
|+ |
|||
!scope="col" rowspan="2"|Vaccine |
|||
!scope="col" colspan="3"|Efficacy by severity of COVID-19 |
|||
!scope="col" rowspan="2"|Trial location |
|||
!scope="col" rowspan="2"|Refs |
|||
|- |
|||
!Mild or moderate{{efn-ua|Mild symptoms: fever, dry cough, fatigue, myalgia, arthralgia, sore throat, diarrhea, nausea, vomiting, headache, anosmia, ageusia, nasal congestion, rhinorrhea, conjunctivitis, skin rash, chills, dizziness. Moderate symptoms: mild pneumonia.}} |
|||
!Severe without hospitalization or death{{efn-ua|Severe symptoms without hospitalization or death for an individual, are any one of the following severe respiratory symptoms measured at rest on any time during the course of observation (on top of having either pneumonia, deep vein thrombosis, dyspnea, hypoxia, persistent chest pain, anorexia, confusion, fever above {{convert|38|C}}), that however were not persistent/severe enough to cause hospitalization or death: Any respiratory rate ≥30 breaths/minute, heart rate ≥125 beats/minute, oxygen saturation (SpO2) ≤93% on room air at sea level, or partial pressure of oxygen/fraction of inspired oxygen (PaO2/FiO2) <300 mmHg.}} |
|||
!Severe with hospitalization or death{{efn-ua|Severe symptoms causing hospitalization or death, are those requiring treatment at hospitals or results in deaths: dyspnea, hypoxia, persistent chest pain, anorexia, confusion, fever above {{convert|38|C}}, respiratory failure, kidney failure, multiorgan dysfunction, sepsis, shock.}} |
|||
|- |
|||
| rowspan="2" |[[Oxford–AstraZeneca COVID-19 vaccine|Oxford–AstraZeneca]] |
|||
|{{shade|color=gold|inv=1|81|{{Estimate|81|60|91|unit=%|prefix=sym|mini=auto}}{{efn-ua|With twelve weeks or more between doses. For an interval of less than six weeks, the trial found an efficacy {{Estimate|55|33|70|unit=%|prefix=sym|mini=auto}}.}}}} |
|||
|{{shade|color=gold|inv=1|100|{{Estimate|100|72|100|97.5|unit=%|prefix=sym|mini=auto}}}} |
|||
|{{shade|color=gold|inv=1|100|{{Estimate|100|unit=%|prefix=sym|mini=auto}}{{efn-ua|name="efficacy-no-ci"}}}} |
|||
|Multinational |
|||
|<ref name="AZD1222-efficacy" /> |
|||
|- |
|||
|{{shade|color=gold|inv=1|76|{{Estimate|76|68|82|unit=%|prefix=sym|mini=auto}}{{efn-ua|With a four-week interval between doses. Efficacy is "at preventing symptomatic COVID-19".}}}} |
|||
|{{shade|color=gold|inv=1|100|{{Estimate|100|unit=%|prefix=sym|mini=auto}}{{efn-ua|name="efficacy-no-ci"}}}} |
|||
|{{shade|color=gold|inv=1|100|{{Estimate|100|unit=%|prefix=sym|mini=auto}}{{efn-ua|name="efficacy-no-ci"}}}} |
|||
|United States |
|||
|<ref>{{#invoke:Cite web| |title=AZD1222 US Phase III primary analysis confirms safety and efficacy |url=https://www.astrazeneca.com/content/astraz/media-centre/press-releases/2021/azd1222-us-phase-iii-primary-analysis-confirms-safety-and-efficacy.html |date=25 March 2021 |website=AstraZeneca}}</ref> |
|||
|- |
|||
|rowspan="2"|[[Pfizer–BioNTech COVID-19 vaccine|Pfizer–BioNTech]] |
|||
|{{shade|color=gold|inv=1|95|{{Estimate|95|90|98|unit=%|prefix=sym|mini=auto}}{{efn-ua|name=PfizerSymptoms|COVID-19 symptoms observed in the Pfizer–BioNTech vaccine trials, were only counted as such for vaccinated individuals if they began more than seven days after their second dose, and required presence of a positive [[Reverse transcription polymerase chain reaction|RT-PCR test]] result. Mild/moderate cases required at least oen of the following symptoms and a positive test during, or within 4 days before or after, the symptomatic period: fever; new or increased cough; new or increased shortness of breath; chills; new or increased muscle pain; new loss of taste or smell; sore throat; diarrhoea; or vomiting. Severe cases additionally required at least one of the following symptoms: clinical signs at rest indicative of severe systemic illness (RR ≥30 breaths per minute, HR ≥125 beats per minute, SpO2 ≤93% on room air at sea level, or PaO2/FiO2<300mm Hg); respiratory failure (defined as needing high-flow oxygen, non-invasive ventilation, mechanical ventilation, or ECMO); evidence of shock (SBP <90 mm Hg, DBP <60 mm Hg, or requiring vasopressors); significant acute renal, hepatic, or neurologic dysfunction; admission to an ICU; death.<ref name="Pfizer–BioNTech COVID-19 Vaccine EMA assessment" /><ref name="Pfizer–BioNTech COVID-19 Vaccine FDA label" />}}}} |
|||
|colspan="2" {{shade|color=gold|inv=1|66|{{Estimate|66|-125|96|unit=%|sep=to|prefix=sym|mini=auto}}{{efn-ua|name="efficacy-bound-failure"}}{{efn-ua|name=PfizerSymptoms}}}} |
|||
|Multinational |
|||
|<ref name="Pfizer–BioNTech COVID-19 Vaccine EMA assessment">{{Cite techreport |type=European public assessment report |author=Committee for Medicinal Products for Human Use |title=Assessment report: Comirnaty |number=EMA/707383/2020 |version=Corr.1 |at=COVID-19 Case Definitions; tables 2, 5, 12, 13 |institution=[[European Medicines Agency]] (EMA) |date=19 February 2021 |access-date=23 June 2021 |url=https://www.ema.europa.eu/en/documents/assessment-report/comirnaty-epar-public-assessment-report_en.pdf |format=PDF |url-status=live |archive-date=20 June 2021 |archive-url=https://web.archive.org/web/20210620120447/https://www.ema.europa.eu/en/documents/assessment-report/comirnaty-epar-public-assessment-report_en.pdf}}</ref> |
|||
|- |
|||
|{{shade|color=gold|inv=1|95|{{Estimate|95|90|98|unit=%|prefix=sym|mini=auto}}{{efn-ua|name=PfizerSymptoms}}}} |
|||
|{{n/a|Not reported}} |
|||
|{{n/a|Not reported}} |
|||
|United States |
|||
|<ref name="Pfizer–BioNTech COVID-19 Vaccine FDA label">{{#invoke:Cite web| |title=Pfizer–BioNTech COVID-19 Vaccine – rna ingredient bnt-162b2 injection, suspension|url=https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=908ecbe7-2f1b-42dd-94bf-f917ec3c5af8|access-date=14 December 2020|website=DailyMed|publisher=U.S. National Institutes of Health}}</ref> |
|||
|- |
|||
| rowspan="4" |[[Janssen COVID-19 vaccine|Janssen]] |
|||
|{{shade|color=gold|inv=1|66|{{Estimate|66|55|75|unit=%|prefix=sym|mini=auto}}{{efn-ua|name=jj-moderate|Moderate cases.}}{{efn-ua|name=JJ28|Efficacy reported 28 days post-vaccination for the Janssen single shot vaccine. A lower efficacy was found for the vaccinated individuals 14 days post-vaccination.<ref name="Janssen COVID-19 Vaccine FDA label" />}}}} |
|||
|{{shade|color=gold|inv=1|85|{{Estimate|85|54|97|unit=%|prefix=sym|mini=auto}}{{efn-ua|name=JJ28}}}} |
|||
|{{shade|color=gold|inv=1|100|{{Estimate|100|unit=%|prefix=sym|mini=auto}}{{efn-ua|name="efficacy-no-ci"}}{{efn-ua|name=JJ28}}{{efn-ua|name=JJ28hosp|No hospitalizations or deaths were detected 28 days post-vaccination for 19,630 vaccinated individuals in the trials, compared with 16 hospitalizations reported in the placebo group of 19,691 individuals (incidence rate 5.2 per 1000 person-years)<ref name="Janssen COVID-19 Vaccine FDA label" /> and seven COVID-19 related deaths for the same placebo group.<ref name="FDA:J&J">{{#invoke:Cite web| |url=https://www.fda.gov/media/146217/download|title=FDA Briefing Document: Janssen Ad26.COV2.S Vaccine for the Prevention of COVID-19|publisher=US Food & Drug Administration (FDA)|date=26 February 2021|access-date=1 April 2021}}</ref>}}}} |
|||
|Multinational |
|||
| rowspan="4" |<ref name="Janssen COVID-19 Vaccine FDA label">{{#invoke:Cite web| |title=Janssen COVID-19 Vaccine – ad26.cov2.s injection, suspension|url=https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=14a822ff-f353-49f9-a7f2-21424b201e3b|access-date=15 March 2021|website=DailyMed|publisher=U.S. National Institutes of Health}}</ref> |
|||
|- |
|||
|{{shade|color=gold|inv=1|72|{{Estimate|72|58|82|unit=%|prefix=sym|mini=auto}}{{efn-ua|name=jj-moderate}}{{efn-ua|name=JJ28}}}} |
|||
|{{shade|color=gold|inv=1|86|{{Estimate|86|-9|100|unit=%|sep=to|prefix=sym|mini=auto}}{{efn-ua|name="efficacy-bound-failure"}}{{efn-ua|name=JJ28}}}} |
|||
|{{shade|color=gold|inv=1|100|{{Estimate|100|unit=%|prefix=sym|mini=auto}}{{efn-ua|name="efficacy-no-ci"}}{{efn-ua|name=JJ28}}{{efn-ua|name=JJ28hosp}}}} |
|||
|United States |
|||
|- |
|||
|{{shade|color=gold|inv=1|68|{{Estimate|68|49|81|unit=%|prefix=sym|mini=auto}}{{efn-ua|name=jj-moderate}}{{efn-ua|name=JJ28}}}} |
|||
|{{shade|color=gold|inv=1|88|{{Estimate|88|8|100|unit=%|prefix=sym|mini=auto}}{{efn-ua|name="efficacy-bound-failure"}}{{efn-ua|name=JJ28}}}} |
|||
|{{shade|color=gold|inv=1|100|{{Estimate|100|unit=%|prefix=sym|mini=auto}}{{efn-ua|name="efficacy-no-ci"}}{{efn-ua|name=JJ28}}{{efn-ua|name=JJ28hosp}}}} |
|||
|Brazil |
|||
|- |
|||
|{{shade|color=gold|inv=1|64|{{Estimate|64|41|79|unit=%|prefix=sym|mini=auto}}{{efn-ua|name=jj-moderate}}{{efn-ua|name=JJ28}}}} |
|||
|{{shade|color=gold|inv=1|82|{{Estimate|82|46|95|unit=%|prefix=sym|mini=auto}}{{efn-ua|name=JJ28}}}} |
|||
|{{shade|color=gold|inv=1|100|{{Estimate|100|unit=%|prefix=sym|mini=auto}}{{efn-ua|name="efficacy-no-ci"}}{{efn-ua|name=JJ28}}{{efn-ua|name=JJ28hosp}}}} |
|||
|South Africa |
|||
|- |
|||
|[[Moderna COVID-19 vaccine|Moderna]] |
|||
|{{shade|color=gold|inv=1|94|{{Estimate|94|89|97|unit=%|prefix=sym|mini=auto}}{{efn-ua|name=ModernaSymptoms|Mild/Moderate COVID-19 symptoms observed in the Moderna vaccine trials, were only counted as such for vaccinated individuals if they began more than 14 days after their second dose, and required presence of a positive [[Reverse transcription polymerase chain reaction|RT-PCR test]] result along with at least two systemic symptoms (fever above 38ºC, chills, myalgia, headache, sore throat, new olfactory and taste disorder) or just one respiratory symptom (cough, shortness of breath or difficulty breathing, or clinical or radiographical evidence of pneumonia).<ref name="Moderna COVID-19 Vaccine FDA label" />}}}} |
|||
|{{shade|color=gold|inv=1|100|{{Estimate|100|unit=%|prefix=sym|mini=auto}}{{efn-ua|name="efficacy-no-ci"}}{{efn-ua|name=ModernaSevereSymptoms|Severe COVID-19 symptoms observed in the Moderna vaccine trials, were defined as symptoms having met the criteria for mild/moderate symptoms plus any of the following observations: Clinical signs indicative of severe systemic illness, respiratory rate ≥30 per minute, heart rate ≥125 beats per minute, SpO2 ≤93% on room air at sea level or PaO2/FIO2 <300 mm Hg; or respiratory failure or ARDS, (defined as needing high-flow oxygen, non-invasive or mechanical ventilation, or ECMO), evidence of shock (systolic blood pressure <90 mmHg, diastolic BP <60 mmHg or requiring vasopressors); or significant acute renal, hepatic, or neurologic dysfunction; or admission to an intensive care unit or death. No severe cases were detected for vaccinated individuals in the trials, compared with thirty in the placebo group (incidence rate 9.1 per 1000 person-years).<ref name="Moderna COVID-19 Vaccine FDA label" />}}}} |
|||
|{{shade|color=gold|inv=1|100|{{Estimate|100|unit=%|prefix=sym|mini=auto}}{{efn-ua|name="efficacy-no-ci"}}{{efn-ua|name=ModernaSevereSymptoms}}}} |
|||
|United States |
|||
|<ref name="Moderna COVID-19 Vaccine FDA label">{{#invoke:Cite web| |title=Moderna COVID-19 Vaccine – cx-024414 injection, suspension|url=https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=e0651c7a-2fe2-459d-a766-0d59e919f058|access-date=20 December 2020|website=DailyMed|publisher=U.S. National Institutes of Health}}</ref> |
|||
|- |
|||
|[[BBIBP-CorV]] |
|||
|{{shade|color=gold|inv=1|78|{{Estimate|78|65|86|unit=%|prefix=sym|mini=auto}}}} |
|||
|{{shade|color=gold|inv=1|100|{{Estimate|100|unit=%|prefix=sym|mini=auto}}{{efn-ua|name="efficacy-no-ci"}}}} |
|||
|{{shade|color=gold|inv=1|100|{{Estimate|100|unit=%|prefix=sym|mini=auto}}{{efn-ua|name="efficacy-no-ci"}}}} |
|||
|Multinational |
|||
|<ref name="jama.2021.8565">{{Cite journal |display-authors=6 |vauthors=Al Kaabi N, Zhang Y, Xia S, Yang Y, Al Qahtani MM, Abdulrazzaq N, Al Nusair M, Hassany M, Jawad JS, Abdalla J, Hussein SE, Al Mazrouei SK, Al Karam M, Li X, Yang X, Wang W, Lai B, Chen W, Huang S, Wang Q, Yang T, Liu Y, Ma R, Hussain ZM, Khan T, Saifuddin Fasihuddin M, You W, Xie Z, Zhao Y, Jiang Z, Zhao G, Zhang Y, Mahmoud S, ElTantawy I, Xiao P, Koshy A, Zaher WA, Wang H, Duan K, Pan A, Yang X |date=May 2021 |title=Effect of 2 Inactivated SARS-CoV-2 Vaccines on Symptomatic COVID-19 Infection in Adults: A Randomized Clinical Trial |journal=JAMA |volume=326 |issue=1 |pages=35–45 |doi=10.1001/jama.2021.8565 |pmc=8156175 |pmid=34037666 |doi-access=free |pmc-embargo-date=26 November 2021}}</ref> |
|||
|- |
|||
|[[Sputnik V COVID-19 vaccine|Sputnik V]] |
|||
|{{shade|color=gold|inv=1|92|{{Estimate|92|86|95|unit=%|prefix=sym|mini=auto}}}} |
|||
|{{shade|color=gold|inv=1|100|{{Estimate|100|94|100|unit=%|prefix=sym|mini=auto}}}} |
|||
|{{shade|color=gold|inv=1|100|{{Estimate|100|unit=%|prefix=sym|mini=auto}}{{efn-ua|name="efficacy-no-ci"}}}} |
|||
|Russia |
|||
|<ref name="Safety and efficacy of an rAd26 and">{{Cite journal |display-authors=6 |vauthors=Logunov DY, Dolzhikova IV, Shcheblyakov DV, Tukhvatulin AI, Zubkova OV, Dzharullaeva AS, Kovyrshina AV, Lubenets NL, Grousova DM, Erokhova AS, Botikov AG, Izhaeva FM, Popova O, Ozharovskaya TA, Esmagambetov IB, Favorskaya IA, Zrelkin DI, Voronina DV, Shcherbinin DN, Semikhin AS, Simakova YV, Tokarskaya EA, Egorova DA, Shmarov MM, Nikitenko NA, Gushchin VA, Smolyarchuk EA, Zyryanov SK, Borisevich SV, Naroditsky BS, Gintsburg AL |date=February 2021 |title=Safety and efficacy of an rAd26 and rAd5 vector-based heterologous prime-boost COVID-19 vaccine: an interim analysis of a randomised controlled phase 3 trial in Russia |journal=Lancet |volume=397 |issue=10275 |pages=671–81 |doi=10.1016/S0140-6736(21)00234-8 |pmc=7852454 |pmid=33545094 |doi-access=free |title-link=doi}}</ref> |
|||
|- |
|||
| rowspan="2" |[[CoronaVac]] |
|||
|{{shade|color=gold|inv=1|51|{{Estimate|51|36|62|unit=%|prefix=sym|mini=auto}}{{efn-ua|name=peer reviewed}}}} |
|||
|{{shade|color=gold|inv=1|84|{{Estimate|84|58|94|unit=%|prefix=sym|mini=yes}}{{efn-ua|name=peer reviewed}}}} |
|||
|{{shade|color=gold|inv=1|100|{{Estimate|100|56|100|unit=%|prefix=sym|mini=yes}}{{efn-ua|name=peer reviewed}}}} |
|||
|Brazil |
|||
|<ref>{{Cite press release |title=Summary of Clinical Trial Data of Sinovac's COVID-19 Vaccine (CoronaVac) |date=3 April 2021 |publisher=Sinovac Biotech |url=http://www.sinovac.com/?optionid=754&auto_id=927 |access-date=12 April 2021}}</ref><ref>{{Cite ssrn |title=Efficacy and Safety of a COVID-19 Inactivated Vaccine in Healthcare Professionals in Brazil: The PROFISCOV Study |last=Palacios |first=Ricardo |last2=Batista |first2=Ana Paula |date=April 2021 |ssrn=3822780 |last3=Albuquerque |first3=Camila Santos Nascimento |last4=Patiño |first4=Elizabeth González |last5=Santos |first5=Joane do Prado |last6=Tilli Reis Pessoa Conde |first6=Mônica |last7=Piorelli |first7=Roberta de Oliveira |last8=Pereira Júnior |first8=Luiz Carlos |last9=Raboni |first9=Sonia Mara |display-authors=6 |last10=Ramos |first10=Fabiano |last11=Sierra Romero |first11=Gustavo Adolfo |name-list-style=vanc}}</ref><ref name=":03">{{#invoke:Cite web||last=Toscano|first=Cristiana|date=29 April 2021|title=Evidence Assessment: Sinovac/CoronaVac COVID-19 vaccine|url=https://cdn.who.int/media/docs/default-source/immunization/sage/2021/april/5_sage29apr2021_critical-evidence_sinovac.pdf |work=[[World Health Organization]] (WHO)|name-list-style=vanc }}</ref> |
|||
|- |
|||
|{{shade|color=gold|inv=1|84|{{Estimate|84|65|92|unit=%|prefix=sym|mini=auto}}}} |
|||
|{{shade|color=gold|inv=1|100|{{Estimate|100|unit=%|prefix=sym|mini=auto}}{{efn-ua|name="efficacy-no-ci"}}}} |
|||
|{{shade|color=gold|inv=1|100|{{Estimate|100|20|100|unit=%|prefix=sym|mini=auto}}{{efn-ua|name="efficacy-bound-failure"}}}} |
|||
|Turkey |
|||
|<ref name="S0140-6736(21)01429-X">{{Cite journal |last1=Tanriover |first1=Mine Durusu |last2=Doğanay |first2=Hamdi Levent |last3=Akova |first3=Murat |last4=Güner |first4=Hatice Rahmet |last5=Azap |first5=Alpay |last6=Akhan |first6=Sıla |last7=Köse |first7=Şükran |last8=Erdinç |first8=Fatma Şebnem |last9=Akalın |first9=Emin Halis |last10=Tabak |first10=Ömer Fehmi |last11=Pullukçu |first11=Hüsnü |display-authors=6 |date=8 July 2021 |title=Efficacy and safety of an inactivated whole-virion SARS-CoV-2 vaccine (CoronaVac): interim results of a double-blind, randomised, placebo-controlled, phase 3 trial in Turkey |journal=The Lancet |volume=398 |issue=10296 |pages=213–222 |doi=10.1016/S0140-6736(21)01429-X |issn=0140-6736 |pmc=8266301 |pmid=34246358 |last12=Batum |first12=Özgür |last13=Yavuz |first13=Serap Şimşek |last14=Turhan |first14=Özge |last15=Yıldırmak |first15=Mustafa Taner |last16=Köksal |first16=İftihar |last17=Taşova |first17=Yeşim |last18=Korten |first18=Volkan |last19=Yılmaz |first19=Gürdal |last20=Çelen |first20=Mustafa Kemal |last21=Altın |first21=Sedat |last22=Çelik |first22=İlhami |last23=Bayındır |first23=Yaşar |last24=Karaoğlan |first24=İlkay |last25=Yılmaz |first25=Aydın |last26=Özkul |first26=Aykut |last27=Gür |first27=Hazal |last28=Unal |first28=Serhat |last29=Kayaaslan |first29=Bircan |last30=Hasanoğlu |first30=İmran |last31=Dalkıran |first31=Ayça |last32=Aydos |first32=Ömer |last33=Çınar |first33=Güle |last34=Akdemir-Kalkan |first34=İrem |last35=İnkaya |first35=Ahmet Çağkan |last36=Aydin |first36=Mehtap |last37=Çakir |first37=Hatice |last38=Yıldız |first38=Jale |last39=Kocabıyık |first39=Özenir |last40=Arslan |first40=Sonay |last41=Nallı |first41=Bayram |last42=Demir |first42=Ömer |last43=Singil |first43=Sarp |last44=Ataman-Hatipoğlu |first44=Çiğdem |last45=Tuncer-Ertem |first45=Günay |last46=Kınıklı |first46=Sami |last47=Önal |first47=Uğur |last48=Mete |first48=Bilgül |last49=Dalgan |first49=Gözde |last50=Taşbakan |first50=Meltem |last51=Yamazhan |first51=Tansu |last52=Kömürcüoğlu |first52=Berna |last53=Yalnız |first53=Enver |last54=Benli |first54=Aysun |last55=Keskin-Sarıtaş |first55=Çağla |last56=Ertosun |first56=Mustafa Gökhan |last57=Özkan |first57=Özlenen |last58=Emre |first58=Salih |last59=Arıca |first59=Seçil |last60=Kuşçu |first60=Ferit |last61=Candevir |first61=Aslıhan |last62=Ertürk-Şengel |first62=Buket |last63=Ayvaz |first63=Fadime |last64=Aksoy |first64=Firdevs |last65=Mermutluoğlu |first65=Çiğdem |last66=Demir |first66=Yakup |last67=Günlüoğlu |first67=Gülşah |last68=Tural-Önür |first68=Seda |last69=Kılıç-Toker |first69=Ayşin |last70=Eren |first70=Esma |last71=Otlu |first71=Barış |last72=Mete |first72=Ayşe Özlem |last73=Koçak |first73=Kübra |last74=Ateş |first74=Hale |last75=Koca-Kalkan |first75=İlkay |last76=Aksu |first76=Kurtuluş |s2cid=235770533}}</ref> |
|||
|- |
|||
|[[BBV152|Covaxin]] |
|||
|{{shade|color=gold|inv=1|78|{{Estimate|78|65|86|unit=%|prefix=sym|mini=auto}}{{efn-ua|name=peer reviewed|These Phase{{nbs}}III data have not been published or peer reviewed.}}}} |
|||
|colspan="2" {{shade|color=gold|inv=1|93|{{Estimate|93|57|100|unit=%|prefix=sym|mini=auto}}{{efn-ua|name=peer reviewed}}}} |
|||
|India |
|||
|<ref>{{Cite press release |title=Ocugen's COVID-19 Vaccine Co-Development Partner, Bharat Biotech, Shares Phase 3 Results Demonstrating 77.8% Protection against Overall Disease |date=2 July 2021 |publisher=GlobeNewswire |location=Malvern, Pennsylvania; and Hyderabad |url=https://www.globenewswire.com/news-release/2021/07/02/2257365/0/en/Ocugen-s-COVID-19-Vaccine-Co-Development-Partner-Bharat-Biotech-Shares-Phase-3-Results-Demonstrating-77-8-Protection-against-Overall-Disease.html |access-date=3 July 2021 |agency=Ocugen}}</ref>{{Unreliable medical source|date=July 2021}} |
|||
|- |
|||
|[[Sputnik Light]] |
|||
|{{shade|color=gold|inv=1|79|{{Estimate|79|unit=%|prefix=sym|mini=auto}}{{efn-ua|name="efficacy-no-ci"}}}} |
|||
|{{n/a|Not reported}} |
|||
|{{n/a|Not reported}} |
|||
|Russia |
|||
|<ref>{{Cite press release |title=Single dose vaccine, Sputnik Light, authorized for use in Russia |date=6 May 2021 |publisher=Russian Direct Investment Fund |url=https://rdif.ru/Eng_fullNews/6763/ |quote=The single dose Sputnik Light vaccine demonstrated 79.4% efficacy according to analyzed data taken from 28 days after the injection was administered as part of Russia’s mass vaccination program between 5 December 2020 and 15 April 2021. |access-date=1 July 2021}}</ref> |
|||
|- |
|||
|[[Convidecia]] |
|||
|{{shade|color=gold|inv=1|66|{{Estimate|66|unit=%|prefix=sym|mini=auto}}{{efn-ua|name="efficacy-no-ci"}}{{efn-ua|name=peer reviewed}}}} |
|||
|{{shade|color=gold|inv=1|91|{{Estimate|91|unit=%|prefix=sym|mini=auto}}{{efn-ua|name="efficacy-no-ci"}}{{efn-ua|name=peer reviewed}}}} |
|||
|{{n/a|Not reported}} |
|||
|Multinational |
|||
|<ref name="reuters-convidecia" />{{Unreliable medical source|date=March 2021}} |
|||
|- |
|||
|[[WIBP-CorV]] |
|||
|{{shade|color=gold|inv=1|73|{{Estimate|73|58|82|unit=%|prefix=sym|mini=auto}}}} |
|||
|{{shade|color=gold|inv=1|100|{{Estimate|100|unit=%|prefix=sym|mini=auto}}{{efn-ua|name="efficacy-no-ci"}}{{efn-ua|name="trial-no-cases-100"}}}} |
|||
|{{shade|color=gold|inv=1|100|{{Estimate|100|unit=%|prefix=sym|mini=auto}}{{efn-ua|name="efficacy-no-ci"|A [[confidence interval]] was not provided, so it is not possible to know the accuracy of this measurement.}}{{efn-ua|name="trial-no-cases-100"}}}} |
|||
|Multinational |
|||
|<ref name="jama-wibp-efficacy">{{Cite journal |display-authors=6 |vauthors=Kaabi NA, Zhang Y, Xia S, Yang Y, Qahtani MM, Abdulrazzaq N, Nusair MA, Hassany M, Jawad JS, Abdalla J, Hussein SE |date=26 May 2021 |title=Effect of 2 Inactivated SARS-CoV-2 Vaccines on Symptomatic COVID-19 Infection in Adults |journal=JAMA |volume=326 |issue=1 |pages=35–45 |doi=10.1001/jama.2021.8565 |issn=0098-7484 |pmc=8156175 |pmid=34037666 |doi-access=free |pmc-embargo-date=26 November 2021}}</ref> |
|||
|- |
|||
|[[Abdala (vaccine)|Abdala]] |
|||
|{{shade|color=gold|inv=1|92|{{Estimate|92|86|96|unit=%|prefix=sym|mini=auto}}}} |
|||
|{{n/a|Not reported}} |
|||
|{{n/a|Not reported}} |
|||
|Cuba |
|||
|<ref>{{Cite press release |title=El candidato vacunal Abdala mostró una eficacia de un 92,28% en su esquema de tres dosis. |date=21 June 2021 |url=https://www.biocubafarma.cu/noticias/noticia-post.php?id=361 |access-date=1 July 2021 |website=BioCubaFarma}}</ref><ref>{{#invoke:Cite web||date=27 June 2021|title=How was the efficacy of the Cuban COVID-19 vaccine candidates calculated?|url=https://oncubanews.com/en/cuba/how-was-the-efficacy-of-the-cuban-covid-19-vaccine-candidates-calculated/|access-date=28 June 2021|website=OnCubaNews English}}</ref>{{Unreliable medical source | date = August 2021}} |
|||
|- |
|||
|[[Soberana 02]] |
|||
|{{shade|color=gold|inv=1|62|{{Estimate|62|unit=%|prefix=sym|mini=auto}}{{efn-ua|name="efficacy-no-ci"}}}} |
|||
|{{n/a|Not reported}} |
|||
|{{n/a|Not reported}} |
|||
|Cuba |
|||
|<ref>{{Cite press release |title=Soberana 02 muestra una eficacia de un 62 por ciento en su esquema de dos dosis |date=20 June 2021 |url=https://www.biocubafarma.cu/noticias/noticia-post.php?id=358 |access-date=1 July 2021 |website=BioCubaFarma}}</ref>{{Unreliable medical source | date = August 2021}} |
|||
|- |
|||
| rowspan="4" |[[Novavax COVID-19 vaccine|Novavax]] |
|||
|{{shade|color=gold|inv=1|90|{{Estimate|90|75|95|unit=%|prefix=sym|mini=auto}}}} |
|||
|{{shade|color=gold|inv=1|100|{{Estimate|100|unit=%|prefix=sym|mini=auto}}{{efn-ua|name="efficacy-no-ci"}}{{efn-ua|name="trial-no-cases-100"|No cases detected in trial.}}}} |
|||
|{{shade|color=gold|inv=1|100|{{Estimate|100|unit=%|prefix=sym|mini=auto}}{{efn-ua|name="efficacy-no-ci"}}{{efn-ua|name="trial-no-cases-100"}}}} |
|||
|United Kingdom |
|||
| rowspan="4" |<ref>{{Cite journal |name-list-style=vanc |vauthors=Wadman M, Cohen J |date=28 January 2021 |title=Novavax vaccine delivers 89% efficacy against COVID-19 in UK – but is less potent in South Africa |journal=Science |doi=10.1126/science.abg8101 |doi-access=free}}</ref><ref>{{Cite press release |title=Novavax Publishes Results of United Kingdom Phase 3 Clinical Trial in New England Journal of Medicine, Demonstrating High Levels of Efficacy of COVID-19 Vaccine |url=https://ir.novavax.com/2021-06-30-Novavax-Publishes-Results-of-United-Kingdom-Phase-3-Clinical-Trial-in-New-England-Journal-of-Medicine,-Demonstrating-High-Levels-of-Efficacy-of-COVID-19-Vaccine |access-date=30 June 2021 |website=Novavax Inc.}}</ref><ref>{{Cite press release |title=Novavax COVID-19 Vaccine Demonstrates 90% Overall Efficacy and 100% Protection Against Moderate and Severe Disease in PREVENT-19 Phase 3 Trial |date=14 June 2021 |url=https://ir.novavax.com/2021-06-14-Novavax-COVID-19-Vaccine-Demonstrates-90-Overall-Efficacy-and-100-Protection-Against-Moderate-and-Severe-Disease-in-PREVENT-19-Phase-3-Trial |access-date=15 June 2021 |website=Novavax Inc.}}</ref> |
|||
|- |
|||
|{{shade|color=gold|inv=1|60|{{Estimate|60|20|80|unit=%|prefix=sym|mini=auto}}{{efn-ua|name="efficacy-bound-failure"|This measurement is not accurate enough to support the high efficacy because the lower limit of the 95% [[confidence interval]] is lower than the minimum of 30%.}}}} |
|||
|{{shade|color=gold|inv=1|100|{{Estimate|100|unit=%|prefix=sym|mini=auto}}{{efn-ua|name="efficacy-no-ci"}}{{efn-ua|name="trial-no-cases-100"}}}} |
|||
|{{shade|color=gold|inv=1|100|{{Estimate|100|unit=%|prefix=sym|mini=auto}}{{efn-ua|name="efficacy-no-ci"}}{{efn-ua|name="trial-no-cases-100"}}}} |
|||
|South Africa |
|||
|- |
|||
| rowspan="2" {{shade|color=gold|inv=1|90|{{Estimate|90|unit=%|prefix=sym|mini=auto}}{{efn-ua|name="efficacy-no-ci"}}}} |
|||
|{{n/a|Not reported}} |
|||
|{{n/a|Not reported}} |
|||
|United States |
|||
|- |
|||
|{{n/a|Not reported}} |
|||
|{{n/a|Not reported}} |
|||
|Mexico |
|||
|- |
|||
|[[CureVac COVID-19 vaccine|CureVac]] |
|||
|{{shade|color=gold|inv=1|48|{{Estimate|48|unit=%|prefix=sym|mini=auto}}{{efn-ua|name="efficacy-no-ci"}}}} |
|||
|{{n/a|Not reported}} |
|||
|{{n/a|Not reported}} |
|||
|Multinational |
|||
|<ref>{{Cite press release |title=CureVac Final Data from Phase 2b/3 Trial of First-Generation COVID-19 Vaccine Candidate, CVnCoV, Demonstrates Protection in Age Group of 18 to 60 |date=30 June 2021 |url=https://www.curevac.com/en/2021/06/30/curevac-final-data-from-phase-2b-3-trial-of-first-generation-covid-19-vaccine-candidate-cvncov-demonstrates-protection-in-age-group-of-18-to-60/ |access-date=1 July 2021 |website=CureVac}}</ref> |
|||
|- |
|||
|[[ZyCoV-D]] |
|||
|{{shade|color=gold|inv=1|67|{{Estimate|67|unit=%|prefix=sym|mini=auto}}{{efn-ua|name="efficacy-no-ci"}}}} |
|||
|{{n/a|Not reported}} |
|||
|{{n/a|Not reported}} |
|||
|India |
|||
|<ref>{{Cite press release |title=Zydus applies to the DCGI for EUA to launch ZyCoV-D, the world's first Plasmid DNA vaccine for COVID-19 |date=1 July 2021 |url=https://zyduscadila.com/public/pdf/pressrelease/ZyCoV_D_Press_Release_1_7_2021.pdf |access-date=1 July 2021 |website=Cadila Healthcare}}</ref>{{Unreliable medical source|date=July 2021}} |
|||
|- |
|||
|[[ZF2001]] |
|||
|{{shade|color=gold|inv=1|82|{{Estimate|82|unit=%|prefix=sym|mini=auto}}{{efn-ua|name="efficacy-no-ci"}}}} |
|||
|{{n/a|Not reported}} |
|||
|{{n/a|Not reported}} |
|||
|Multinational |
|||
|<ref>{{cite news |title=China's Zhifei says unit's COVID shot shows 81.76% efficacy in late-stage trial |url=https://www.reuters.com/article/us-health-coronavirus-vaccine-zhifei/chinas-zhifei-says-units-covid-shot-shows-81-76-efficacy-in-late-stage-trial-idUSKBN2FS0WL |publisher=Reuters |date=27 August 2021}}</ref>{{Unreliable medical source|date=August 2021}} |
|||
|} |
|||
{{notelist-ua}} |
|||
===Effectiveness=== |
|||
Recent data from studies in the US and in other countries found that the available COVID-19 vaccines from the United States are "highly protective against severe illness, hospitalization, and death due to COVID-19."<ref name=VDH>[https://www.vdh.virginia.gov/coronavirus/2021/08/23/vaccine-effectiveness/ "Vaccine Effectiveness"], Virginia Dept. of Health, August 23, 2021</ref> In comparison with fully vaccinated people, the CDC found that those who were not vaccinated were from 5 to nearly 30 times more likely to become either infected or hospitalized.<ref name=CDC-compare>[https://www.cdc.gov/mmwr/volumes/70/wr/mm7034e5.htm?s_cid=mm7034e5_w "SARS-CoV-2 Infections and Hospitalizations Among Persons Aged ≥16 Years, by Vaccination Status — Los Angeles County, California, May 1–July 25, 2021"], C.D.C., August 27, 2021</ref><ref name=CNN-effective>[https://www.cnn.com/2021/08/24/health/us-coronavirus-tuesday/index.html "Vaccines are less protective against Delta infection but still reduce risk by two-thirds, C.D.C. study shows"], ''CNN'', August 24, 2021</ref> As of June 2021, over 96% of doctors were fully vaccinated against COVID-19.<ref>[https://www.ama-assn.org/press-center/press-releases/ama-survey-shows-over-96-doctors-fully-vaccinated-against-covid-19 "AMA survey shows over 96% of doctors were fully vaccinated against COVID-19"], [[American Medical Association]], June 11, 2021</ref> |
|||
By late August 2021, after the Delta variant became dominant, studies concluded that Covid vaccines provided 55 percent protection against Covid infections, 80 percent against symptomatic infection, and at least 90 percent against hospitalization.<ref name=NYT-boosters>[https://www.nytimes.com/2021/08/18/health/covid-cdc-boosters-elderly.html "Vaccine Effectiveness Against Infection May Wane, C.D.C. Studies Find"], "New York Times", August 19, 2021</ref> The [[Delta variant]], which is about 40 percent more contagious than the alpha variant,<ref name=TNR>[https://newrepublic.com/article/162891/delta-covid-variants-urgent-message-america "The Delta Covid Variant's Urgent Message for America:Vaccinate. Do it quickly."], ''The New Republic,'' July 1, 2021</ref> became the dominant strain during the spring of 2021. However, the vaccines still protected against severe illness and hospitalizations with slight reduction in effectiveness.<ref name=NYT-boosters/> The CDC similarly found that vaccines were 90 percent effective at preventing hospitalizations.<ref name=CDC-effectiveness>[https://www.cdc.gov/mmwr/volumes/70/wr/mm7034e2.htm?s_cid=mm7034e2_w "Sustained Effectiveness of Pfizer-BioNTech and Moderna Vaccines Against COVID-19 Associated Hospitalizations Among Adults — United States, March–July 2021"], C.D.C., August 27, 2021</ref> |
|||
{{quote box | align = right | width = 25em | bgcolor = MistyRose |quote =My hospital, one of the largest in central Florida, was full of covid patients, more than 90 percent of whom were unvaccinated. We had no beds available. We had paused elective surgeries the previous week and have been trying to control the influx of patients. Our emergency department had a 12-hour wait that day. |
|||
| source = Nitesh N. Paryani, director of Tampa Oncology & Proton <ref name=WaPo-hospitals/>}} |
|||
As a result of the CDC reports, President Joe Biden said that “virtually all” Covid hospitalizations and deaths in the U.S. were among unvaccinated people.<ref>[https://www.cnbc.com/2021/08/24/cdc-study-shows-unvaccinated-people-are-29-times-more-likely-to-be-hospitalized-with-covid.html "CDC study shows unvaccinated people are 29 times more likely to be hospitalized with Covid"], ''CNBC'', August 24, 2021</ref> While a study in the state of Washington found that unvaccinated people were six times more likely to test positive for COVID-19, 37 times more likely to be hospitalized, and 67 times more likely to die, compared to those who had been vaccinated.<ref>[https://www.king5.com/article/news/health/coronavirus/king-county-health-officer-covid-response-coronavirus-vaccine-pandemic/281-e1a90cb8-03fb-4316-a5d6-f007a8442598 "Unvaccinated 67 times more likely to die from COVID-19, adjusted data shows"], ''King5 News'', August 27, 2021</ref> In addition, unvaccinated Covid patients have strained the capacity of hospitals throughout the country, forcing many to turn away patients with life-threatening diseases.<ref name=WaPo-hospitals>[https://www.washingtonpost.com/opinions/2021/08/21/how-unvaccinated-pandemic-threaten-everyones-health/ "Unvaccinated Covid patients are straining hospitals like mine, where I had to turn a cancer patient away"], ''Washington Post'', August 21, 2021</ref><ref>[https://www.statnews.com/2021/08/18/health-workers-overwhelmed-covid-deaths-among-unvaccinated/ "‘It’s soul-draining’: Health workers deployed to Covid hot zones are overwhelmed by deaths among the unvaccinated"], ''Statnews'', August 18, 2021</ref><ref>[https://www.masslive.com/coronavirus/2021/08/massachusetts-reports-1591-new-covid-cases-as-unvaccinated-individuals-continue-to-dominate-hospital-numbers.html "Massachusetts reports 1,591 new COVID cases as unvaccinated individuals continue to dominate hospital numbers"], ''Mass Live'', August 27, 2021</ref> |
|||
Researchers note that although current vaccines were not designed against the Delta variant, they nonetheless are highly effective, but to a lesser degree: protection fell from 91% to 66%.<ref name=Forbes>[https://www.forbes.com/sites/brucelee/2021/08/24/cdc-covid-19-vaccine-effectiveness-fell-from-91-to-66-with-delta-variant/?sh=27bfdae428f7 "CDC: Covid-19 Vaccine Effectiveness Fell From 91% To 66% With Delta Variant"], ''Forbes'', August 24, 2021</ref> One expert stated that "those who are infected following vaccination are still not getting sick and not dying like was happening before vaccination."<ref name=TNR/> "This virus is the most efficient virus for finding new hosts that are vulnerable," stated Dr. [[Eric Topol]], director and founder of the [[Scripps Research]] Translational Institute.<ref name=TNR/> By late August 2021 the Delta variant accounted for 99 percent of U.S. cases and was found to double the risk of severe illness and hospitalization for those not yet vaccinated.<ref name=LATimes-delta>[https://www.latimes.com/science/story/2021-08-28/hospitalization-risk-doubled-for-unvaccinated-covid-patients-infected-with-delta-variant "Among the unvaccinated, Delta variant more than doubles risk of hospitalization"], ''Los Angeles Times'', August 28, 2021</ref> Approximately 600,000 people a day in the U.S. were being vaccinated by August 2021.<ref>[https://www.vox.com/22587443/covid-19-vaccine-refusal-hesitancy-variant-delta-cases-rate "The four main fault lines that divide the vaccinated and the unvaccinated"], ''Vox'', July 29, 2021</ref> |
|||
====Studies==== |
|||
The real-world studies of vaccine [[Phases of clinical research#Efficacy vs effectiveness|effectiveness]] measure to which extent a certain vaccine has succeeded in preventing COVID-19 infection, symptoms, hospitalization and death for the vaccinated individuals in a large population under routine conditions that are less than ideal.<ref>{{#invoke:Cite web| |title=What is the difference between efficacy and effectiveness? |url=https://www.gavi.org/vaccineswork/what-difference-between-efficacy-and-effectiveness |publisher=[[GAVI|Gavi, the Vaccine Alliance]] (GAVI) |access-date=21 April 2021 |date=18 November 2020}}</ref> |
|||
* In Israel, among the 715,425 individuals vaccinated by the Moderna or Pfizer-BioNTech vaccines during the period 20 December 2020, to 28 January 2021, it was observed for the period starting seven days after the second shot, that only 317 people (0.04%) became sick with mild/moderate COVID-19 symptoms and only 16 people (0.002%) were hospitalized.<ref>{{#invoke:Cite web| |url=https://edition.cnn.com/world/live-news/coronavirus-pandemic-vaccine-updates-01-29-21/h_a52c58a8bb72bb98f7668ed869afb927|title=Israel's health data suggests Pfizer and Moderna vaccines may be more effective than we thought| vauthors = Tal A, Cohen E |work=CNN|date=29 January 2021|access-date=27 March 2021}}</ref> |
|||
* The Pfizer-BioNTech and Moderna COVID-19 vaccines provide highly effective protection, according to a report from the US [[Centers for Disease Control and Prevention]] (CDC). Under real-world conditions, mRNA vaccine effectiveness of full immunization (≥14 days after second dose) was 90% against SARS-CoV-2 infections regardless of symptom status; vaccine effectiveness of partial immunization (≥14 days after first dose but before second dose) was 80%.<ref name="cdc-effectiveness" /> |
|||
* 15,121 health care workers from 104 hospitals in England, that all had tested negative for COVID-19 antibodies prior of the study, were followed by [[Reverse transcription polymerase chain reaction|RT-PCR tests]] twice a week from 7{{nbs}}December 2020 to 5{{nbs}}February 2021, during a time when the [[SARS-CoV-2 Alpha variant|Alpha variant]] (lineage B.1.1.7) was in circulation as the dominant variant. The study compared the positive results for the 90.7% vaccinated share of their cohort with the 9.3% unvaccinated share, and found that the Pfizer-BioNTech vaccine reduced all infections (including asymptomatic), by 72% (58-86%) three weeks after the first dose and 86% (76-97%) one week after the second dose.<ref>{{Cite ssrn |title=Effectiveness of BNT162b2 mRNA Vaccine Against Infection and COVID-19 Vaccine Coverage in Healthcare Workers in England, Multicentre Prospective Cohort Study (the SIREN Study) |date=February 2021 |ssrn=3790399 |display-authors=6 |vauthors=Hall VJ, Foulkes S, Saei A, Andrews N, Oguti B, Charlett A, Wellington E, Stowe J, Gillson N, Atti A, Islam J, Karagiannis I, Munro K, Khawam J, Chand MA, Brown C, Ramsay ME, Bernal JL, Hopkins S |collaboration=The SIREN Study Group |author16=Meera A. Chand |author17=Colin Brown |name-list-style=vanc}}</ref>{{Update inline|reason=Information from the outdated preliminary results. Please update based on the definitive results in the reference named 'UKstudy' in the table below.|date=May 2021}} |
|||
* A study of the general population in Israel conducted from 17 January to 6{{nbs}}March 2021, during a time when the Alpha variant was in circulation as the dominant variant, found that the Pfizer vaccine reduced asymptomatic COVID-19 infections by 94% and symptomatic COVID-19 infections by 97%.<ref name="ISRstudy">{{#invoke:Cite web| |url=https://www.pfizer.com/news/press-release/press-release-detail/real-world-evidence-confirms-high-effectiveness-pfizer|website=Pfizer |title=Real-World Evidence Confirms High Effectiveness of Pfizer–BioNTech COVID-19 Vaccine and Profound Public Health Impact of Vaccination One Year After Pandemic Declared|publisher=|date=11 March 2021|access-date=1 April 2021}}</ref> |
|||
* A study, among pre-surgical patients across the [[Mayo Clinic]] system in the United States, showed that mRNA vaccines were 80% protective against asymptomatic infections.<ref name="MCSstudy">{{Cite journal |display-authors=6 |vauthors=Tande AJ, Pollock BD, Shah ND, Farrugia G, Virk A, Swift M, Breeher L, Binnicker M, Berbari EF |date=March 2021 |title=Impact of the COVID-19 Vaccine on Asymptomatic Infection Among Patients Undergoing Pre-Procedural COVID-19 Molecular Screening |journal=Clinical Infectious Diseases |doi=10.1093/cid/ciab229 |pmc=7989519 |pmid=33704435 |doi-access=free}}</ref> |
|||
* A study in England found that a single dose of the [[Oxford–AstraZeneca COVID-19 vaccine]] is about {{Estimate|73|27|90|unit=%|mini=auto}} effective in people aged 70 and older.<ref name="azd1222effectiveness">{{Cite journal |display-authors=6 |vauthors=Lopez Bernal J, Andrews N, Gower C, Robertson C, Stowe J, Tessier E, Simmons R, Cottrell S, Roberts R, O'Doherty M, Brown K, Cameron C, Stockton D, McMenamin J, Ramsay M |date=May 2021 |title=Effectiveness of the Pfizer-BioNTech and Oxford-AstraZeneca vaccines on covid-19 related symptoms, hospital admissions, and mortality in older adults in England: test negative case-control study |journal=BMJ |volume=373 |pages=n1088 |doi=10.1136/bmj.n1088 |issn=1756-1833 |pmc=8116636 |pmid=33985964}}</ref> |
|||
{| class="wikitable sortable" |
|||
!scope="col" rowspan="2"|Vaccine |
|||
!scope="col" colspan="4"|Effectiveness by severity of COVID-19 |
|||
!scope="col" rowspan="2"|Study location |
|||
!scope="col" rowspan="2"|Refs |
|||
|- |
|||
!Asymptomatic |
|||
!Symptomatic |
|||
!Hospitalization |
|||
!Death |
|||
|- |
|||
|rowspan="3" |[[Oxford–AstraZeneca COVID-19 vaccine#Effectiveness|Oxford–AstraZeneca]] |
|||
|{{shade|color=gold|inv=1|70|{{Estimate|70|69|71|unit=%|prefix=sym|mini=auto}}}} |
|||
|{{n/a|Not reported}} |
|||
|{{shade|color=gold|inv=1|87|{{Estimate|87|85|88|unit=%|prefix=sym|mini=auto}}}} |
|||
|{{shade|color=gold|inv=1|90|{{Estimate|90|88|92|unit=%|prefix=sym|mini=auto}}}} |
|||
|Brazil |
|||
|<ref name="effectiveness-vaxzevria-coronavac-brazil">{{cite journal |vauthors=Cerqueira-Silva T, Oliveira VA, Pescarini J, Júnior JB, Machado TM, Ortiz RF, Penna G, Ichihara MY, Barros JV, Boaventura V, Barreto ML |display-authors=6 |date=25 August 2021 |title=The effectiveness of Vaxzevria and CoronaVac vaccines: A nationwide longitudinal retrospective study of 61 million Brazilians (VigiVac-COVID19) |url=https://www.medrxiv.org/content/10.1101/2021.08.21.21261501v1 |type=[[Preprint]] |work=[[medRxiv]] |pages=2021.08.21.21261501 |doi=10.1101/2021.08.21.21261501|s2cid=237292831 }}</ref> |
|||
|- |
|||
|{{n/a|Not reported}} |
|||
|{{shade|color=gold|inv=1|89|{{Estimate|89|78|94|unit=%|prefix=sym|mini=auto}}{{efn-lr|Data collected while the Alpha variant was already dominant.<ref>{{Cite techreport |title=COVID-19 vaccine surveillance report (week 21) |number=GOV-8481 |institution=Public Health England |date=27 May 2021 |url=https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/990096/Vaccine_surveillance_report_-_week_21.pdf |format=PDF}}</ref>}}}} |
|||
|colspan="2" {{n/a|Not reported}} |
|||
|England |
|||
|<ref>{{Cite techreport |title=COVID-19 vaccine surveillance report (week 20) |number=GOV-8401 |institution=Public Health England |date=20 May 2021 |url=https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/990089/Vaccine_surveillance_report_-_week_20.pdf |format=PDF}}</ref> |
|||
|- |
|||
|colspan="3" {{n/a|Not reported}} |
|||
|{{shade|color=gold|inv=1|89|{{Estimate|89|unit=%|prefix=sym|mini=auto}}{{efn-lr|name="effectiveness-no-ci"}}}} |
|||
|Argentina |
|||
|<ref name="effectiveness-argentina" /> |
|||
|- |
|||
| rowspan="5" |[[Pfizer–BioNTech COVID-19 vaccine#Effectiveness|Pfizer–BioNTech]] |
|||
|{{shade|color=gold|inv=1|92|{{Estimate|92|91|92|unit=%|prefix=sym|mini=auto}}}} |
|||
|{{shade|color=gold|inv=1|97|{{Estimate|97|97|97|unit=%|prefix=sym|mini=auto}}}} |
|||
|{{shade|color=gold|inv=1|98|{{Estimate|98|97|98|unit=%|prefix=sym|mini=auto}}}} |
|||
|{{shade|color=gold|inv=1|97|{{Estimate|97|96|97|unit=%|prefix=sym|mini=auto}}}} |
|||
|Israel |
|||
|<ref>{{Cite journal |display-authors=6 |vauthors=Haas EJ, Angulo FJ, McLaughlin JM, Anis E, Singer SR, Khan F, Brooks N, Smaja M, Mircus G, Pan K, Southern J, Swerdlow DL, Jodar L, Levy Y, Alroy-Preis S |date=May 2021 |title=Impact and effectiveness of mRNA BNT162b2 vaccine against SARS-CoV-2 infections and COVID-19 cases, hospitalisations, and deaths following a nationwide vaccination campaign in Israel: an observational study using national surveillance data |journal=Lancet |volume=397 |issue=10287 |pages=1819–1829 |doi=10.1016/S0140-6736(21)00947-8 |pmc=8099315 |pmid=33964222}}</ref> |
|||
|- |
|||
|{{shade|color=gold|inv=1|92|{{Estimate|92|88|95|unit=%|prefix=sym|mini=auto}}}} |
|||
|{{shade|color=gold|inv=1|94|{{Estimate|94|87|98|unit=%|prefix=sym|mini=auto}}}} |
|||
|{{shade|color=gold|inv=1|87|{{Estimate|87|55|100|unit=%|prefix=sym|mini=auto}}}} |
|||
|{{shade|color=gold|inv=1|97|{{Estimate|97|unit=%|prefix=sym|mini=auto}}{{efn-lr|name="effectiveness-no-ci"}}}} |
|||
|Israel |
|||
|<ref>{{Cite journal |display-authors=6 |vauthors=Dagan N, Barda N, Kepten E, Miron O, Perchik S, Katz MA, Hernán MA, Lipsitch M, Reis B, Balicer RD |date=April 2021 |title=BNT162b2 mRNA Covid-19 Vaccine in a Nationwide Mass Vaccination Setting |journal=New England Journal of Medicine |volume=384 |issue=15 |pages=1412–23 |doi=10.1056/NEJMoa2101765 |pmc=7944975 |pmid=33626250}}</ref><ref name="ISRstudy" /> |
|||
|- |
|||
|{{n/a|Not reported}} |
|||
|{{shade|color=gold|inv=1|78|{{Estimate|78|77|79|unit=%|prefix=sym|mini=auto}}}} |
|||
|{{shade|color=gold|inv=1|98|{{Estimate|98|96|99|unit=%|prefix=sym|mini=auto}}}} |
|||
|{{shade|color=gold|inv=1|96|{{Estimate|96|95|97|unit=%|prefix=sym|mini=auto}}}} |
|||
|Uruguay |
|||
|<ref name=":10">{{#invoke:Cite web||title=Tercer estudio de efectividad de vacunación anti SARS-CoV-2 en Uruguay al 30 de junio de 2021|trans-title=Third study of effectiveness of vaccination against SARS-CoV-2 in Uruguay as of June 30, 2021|url=https://www.gub.uy/ministerio-salud-publica/comunicacion/noticias/segundo-estudio-efectividad-vacunacion-anti-sars-cov-2-uruguay-8-junio-2021|date=3 July 2021|access-date=7 July 2021|website=Ministerio de Salud Pública|language=es}}</ref> |
|||
|- |
|||
|colspan="2" {{shade|color=gold|inv=1|85|{{Estimate|85|74|96|unit=%|prefix=sym|mini=auto}}}} |
|||
|colspan="2" {{n/a|Not reported}} |
|||
|England |
|||
|<ref name="UKstudy">{{Cite journal |display-authors=6 |vauthors=Hall VJ, Foulkes S, Saei A, Andrews N, Oguti B, Charlett A, Wellington E, Stowe J, Gillson N, Atti A, Islam J, Karagiannis I, Munro K, Khawam J, Chand MA, Brown CS, Ramsay M, Lopez-Bernal J, Hopkins S |date=May 2021 |title=COVID-19 vaccine coverage in health-care workers in England and effectiveness of BNT162b2 mRNA vaccine against infection (SIREN): a prospective, multicentre, cohort study |journal=The Lancet |volume=397 |issue=10286 |pages=1725–35 |doi=10.1016/S0140-6736(21)00790-X |issn=0140-6736 |pmc=8064668 |pmid=33901423}}</ref> |
|||
|- |
|||
|colspan="2" {{shade|color=gold|inv=1|90|{{Estimate|90|68|97|unit=%|prefix=sym|mini=auto}}}} |
|||
|{{n/a|Not reported}} |
|||
|{{shade|color=gold|inv=1|100|{{Estimate|100|unit=%|prefix=sym|mini=auto}}{{efn-lr|name="effectiveness-no-ci"|A [[confidence interval]] was not provided, so it is not possible to know the accuracy of this measurement.}}{{efn-lr|name="study-no-cases-100"|No cases detected in study.}}}} |
|||
|United States |
|||
|<ref name="cdc-effectiveness" /> |
|||
|- |
|||
|[[Moderna COVID-19 vaccine#Effectiveness|Moderna]] |
|||
|colspan="2" {{shade|color=gold|inv=1|90|{{Estimate|90|68|97|unit=%|prefix=sym|mini=auto}}}} |
|||
|{{n/a|Not reported}} |
|||
|{{shade|color=gold|inv=1|100|{{Estimate|100|unit=%|prefix=sym|mini=auto}}{{efn-lr|name="effectiveness-no-ci"}}{{efn-lr|name="study-no-cases-100"|No cases detected in study.}}}} |
|||
|United States |
|||
|<ref name="cdc-effectiveness" /> |
|||
|- |
|||
| rowspan="2" |[[BBIBP-CorV#Effectiveness|BBIBP-CorV]] |
|||
|colspan="3" {{n/a|Not reported}} |
|||
|{{shade|color=gold|inv=1|84|{{Estimate|84|unit=%|prefix=sym|mini=auto}}{{efn-lr|name="effectiveness-no-ci"}}}} |
|||
|Argentina |
|||
|<ref name="effectiveness-argentina">{{Cite news |date=1 July 2021 |title=Ministros de Salud de todo el país consensuaron redoblar esfuerzos para completar los esquemas de vacunación en mayores de 40 años |language=Spanish |trans-title=Health ministers from all over the country agreed to redouble their efforts to complete vaccination schedules in people over 40 years of age |publisher=Government of Argentina |agency=Ministry of Health (Argentina) |url=https://www.argentina.gob.ar/noticias/ministros-de-salud-de-todo-el-pais-consensuaron-redoblar-esfuerzos-para-completar-los |access-date=12 July 2021}}</ref> |
|||
|- |
|||
|colspan="3" {{n/a|Not reported}} |
|||
|{{shade|color=gold|inv=1|94|{{Estimate|94|unit=%|prefix=sym|mini=auto}}{{efn-lr|name="effectiveness-no-ci"}}}} |
|||
|Peru |
|||
|<ref>{{#invoke:Cite web||last=|first=|date=22 July 2021|title=INS: Vacuna de Sinopharm tiene efectividad de hasta 94% para reducir muerte por COVID-19|url=https://rpp.pe/peru/actualidad/ins-vacuna-de-sinopharm-tiene-efectividad-de-hasta-94-para-reducir-muerte-por-covid-19-noticia-1348886|url-status=live|access-date=28 July 2021|website=RPP|language=es}}</ref> |
|||
|- |
|||
|rowspan="3"|[[Sputnik V COVID-19 vaccine#Effectiveness|Sputnik V]] |
|||
|{{n/a|Not reported}} |
|||
|{{shade|color=gold|inv=1|98|{{Estimate|98|unit=%|prefix=sym|mini=auto}}{{efn-lr|name="effectiveness-no-ci"}}}} |
|||
|colspan="2" {{n/a|Not reported}} |
|||
|Russia |
|||
|<ref>{{Cite news |date=19 April 2021 |title=Russia's Sputnik V vaccine 97.6% effective in real-world study |work=Reuters |location=Moscow |url=https://www.reuters.com/article/health-coronavirus-russia-vaccine-idINL1N2MC1BG |access-date=21 April 2021}}</ref><ref>{{Cite press release |title=Sputnik V demonstrates 97.6% efficacy according to analysis of data from 3.8 million vaccinated persons in Russia making it the most efficient COVID-19 vaccine in the world |date=19 April 2021 |publisher=Russian Direct Investment Fund |location=Moscow |url=https://rdif.ru/Eng_fullNews/6722/ |access-date=21 April 2021}}</ref> |
|||
|- |
|||
|{{n/a|Not reported}} |
|||
|{{shade|color=gold|inv=1|98|{{Estimate|98|unit=%|prefix=sym|mini=auto}}{{efn-lr|name="effectiveness-no-ci"}}}} |
|||
|{{shade|color=gold|inv=1|100|{{Estimate|100|unit=%|prefix=sym|mini=auto}}{{efn-lr|name="effectiveness-no-ci"}}{{efn-lr|name="study-no-cases-100"}}}} |
|||
|{{shade|color=gold|inv=1|100|{{Estimate|100|unit=%|prefix=sym|mini=auto}}{{efn-lr|name="effectiveness-no-ci"}}{{efn-lr|name="study-no-cases-100"}}}} |
|||
|United Arab Emirates |
|||
|<ref>{{Cite press release |title=Sputnik V has demonstrated 97.8% efficacy against COVID cases and 100% efficacy against severe cases of COVID in UAE |date=29 June 2021 |publisher=Russian Direct Investment Fund |location=Moscow |url=https://rdif.ru/Eng_fullNews/6919/ |access-date=2 July 2021}}</ref> |
|||
|- |
|||
|colspan="3" {{n/a|Not reported}} |
|||
|{{shade|color=gold|inv=1|93|{{Estimate|93|unit=%|prefix=sym|mini=auto}}{{efn-lr|name="effectiveness-no-ci"}}}} |
|||
|Argentina |
|||
|<ref name="effectiveness-argentina" /> |
|||
|- |
|||
| rowspan="5" |[[CoronaVac#Effectiveness|CoronaVac]] |
|||
|{{shade|color=gold|inv=1|54|{{Estimate|54|53|55|unit=%|prefix=sym|mini=auto}}}} |
|||
|{{n/a|Not reported}} |
|||
|{{shade|color=gold|inv=1|73|{{Estimate|73|72|74|unit=%|prefix=sym|mini=auto}}}} |
|||
|{{shade|color=gold|inv=1|74|{{Estimate|74|73|75|unit=%|prefix=sym|mini=auto}}}} |
|||
|Brazil |
|||
|<ref name="effectiveness-vaxzevria-coronavac-brazil"/> |
|||
|- |
|||
|{{n/a|Not reported}} |
|||
|{{shade|color=gold|inv=1|66|{{Estimate|66|65|67|unit=%|prefix=sym|mini=auto}}}} |
|||
|{{shade|color=gold|inv=1|88|{{Estimate|88|87|88|unit=%|prefix=sym|mini=auto}}}} |
|||
|{{shade|color=gold|inv=1|86|{{Estimate|86|85|88|unit=%|prefix=sym|mini=auto}}}} |
|||
|Chile |
|||
|<ref name="NEJMoa2107715">{{Cite journal |last1=Jara |first1=Alejandro |last2=Undurraga |first2=Eduardo A. |last3=González |first3=Cecilia |last4=Paredes |first4=Fabio |last5=Fontecilla |first5=Tomás |last6=Jara |first6=Gonzalo |last7=Pizarro |first7=Alejandra |last8=Acevedo |first8=Johanna |last9=Leo |first9=Katherine |last10=Leon |first10=Francisco |last11=Sans |first11=Carlos |display-authors=12 |date=7 July 2021 |title=Effectiveness of an Inactivated SARS-CoV-2 Vaccine in Chile |journal=New England Journal of Medicine |doi=10.1056/NEJMoa2107715 |issn=0028-4793 |pmc=8279092 |pmid=34233097 |doi-access=free |last12=Leighton |first12=Paulina |last13=Suárez |first13=Pamela |last14=García-Escorza |first14=Heriberto |last15=Araos |first15=Rafael |s2cid=235766915}}</ref><ref name=":25">{{Cite news |date=17 May 2021 |title=Reporte COVID-19: Vacuna Coronavac Tiene Un 90,3% De Efectividad Para Prevenir El Ingreso a UCI |language=es |trans-title=COVID-19 report: CoronaVac vaccine is 90.3% effective in preventing admission to the ICU |work=Ministerio de Salud - Gobierno de Chile |url=https://www.minsal.cl/reporte-covid-19-vacuna-coronavac-tiene-un-903-de-efectividad-para-prevenir-el-ingreso-a-uci/}}</ref> |
|||
|- |
|||
|{{n/a|Not reported}} |
|||
|{{shade|color=gold|inv=1|60|{{Estimate|60|59|61|unit=%|prefix=sym|mini=auto}}}} |
|||
|{{shade|color=gold|inv=1|91|{{Estimate|91|89|93|unit=%|prefix=sym|mini=auto}}}} |
|||
|{{shade|color=gold|inv=1|95|{{Estimate|95|93|96|unit=%|prefix=sym|mini=auto}}}} |
|||
|Uruguay |
|||
|<ref name=":10" /> |
|||
|- |
|||
|{{n/a|Not reported}} |
|||
|{{shade|color=gold|inv=1|94|{{Estimate|94|unit=%|prefix=sym|mini=auto}}{{efn-lr|name="effectiveness-no-ci"}}}} |
|||
|{{shade|color=gold|inv=1|96|{{Estimate|96|unit=%|prefix=sym|mini=auto}}{{efn-lr|name="effectiveness-no-ci"}}}} |
|||
|{{shade|color=gold|inv=1|98|{{Estimate|98|unit=%|prefix=sym|mini=auto}}{{efn-lr|name="effectiveness-no-ci"}}}} |
|||
|Indonesia |
|||
|<ref>{{#invoke:Cite web||last=Aditya|first=Arys|title=China Sinovac Shot Seen Highly Effective in Real World Study|url=https://www.bloomberg.com/news/articles/2021-05-11/china-s-sinovac-shot-found-highly-effective-in-real-world-study|access-date=15 May 2021|website=Bloomberg| name-list-style = vanc}}</ref><ref>{{#invoke:Cite web||date=12 May 2021|title=Kajian Cepat Kemenkes : Vaksin Sinovac Efektif Cegah Kematian|trans-title=Ministry of Health Quick Study: Sinovac Vaccine Effectively Prevents Death|url=https://sehatnegeriku.kemkes.go.id/baca/berita-utama/20210512/1937767/kajian-cepat-kemenkes-vaksin-sinovac-efektif-cegah-kematian/|access-date=15 May 2021|website=Sehat Negeriku|language=id-ID}}</ref> |
|||
|- |
|||
|{{n/a|Not reported}} |
|||
|{{shade|color=gold|inv=1|80|{{Estimate|80|unit=%|prefix=sym|mini=auto}}{{efn-lr|name="effectiveness-no-ci"}}}} |
|||
|{{shade|color=gold|inv=1|86|{{Estimate|86|unit=%|prefix=sym|mini=auto}}{{efn-lr|name="effectiveness-no-ci"}}}} |
|||
|{{shade|color=gold|inv=1|95|{{Estimate|95|unit=%|prefix=sym|mini=auto}}{{efn-lr|name="effectiveness-no-ci"}}}} |
|||
|Brazil |
|||
|<ref>{{#invoke:Cite web||date=31 May 2021|title=Mass vaccination creates healthy oasis in Brazilian city|url=https://www.reuters.com/world/americas/mass-vaccination-creates-healthy-oasis-brazilian-city-2021-05-31/|access-date=2 June 2021|website=Reuters}}</ref><ref>{{#invoke:Cite web||date=1 June 2021|title=Sinovac vaccine restores a Brazilian city to near normal|url=https://apnews.com/article/caribbean-brazil-coronavirus-pandemic-business-health-20bd94d28ac7b373d7a8f3f9c557e5b6|access-date=2 June 2021|website=Associated Press}}</ref> |
|||
|- |
|||
|[[Sputnik Light#Effectiveness|Sputnik Light]] |
|||
|{{n/a|Not reported}} |
|||
|{{shade|color=gold|inv=1|79|{{Estimate|79|unit=%|prefix=sym|mini=auto}}{{efn-lr|name="effectiveness-no-ci"}}{{efn-lr|name="sputniklight-effectiveness-argentina"|Participants aged 60 to 79.}}}} |
|||
|{{shade|color=gold|inv=1|88|{{Estimate|88|unit=%|prefix=sym|mini=auto}}{{efn-lr|name="effectiveness-no-ci"}}{{efn-lr|name="sputniklight-effectiveness-argentina"}}}} |
|||
|{{shade|color=gold|inv=1|85|{{Estimate|85|unit=%|prefix=sym|mini=auto}}{{efn-lr|name="effectiveness-no-ci"}}{{efn-lr|name="sputniklight-effectiveness-argentina"}}}} |
|||
|Argentina |
|||
|<ref>{{Cite news |date=2 June 2021 |title=Sputnik-V tiene una efectividad con una sola dosis de 78,6% para evitar casos |language=Spanish |trans-title=Sputnik-V is 78.6% effective with a single dose in preventing cases |publisher=Government of Buenos Aires Province |url=https://www.gba.gob.ar/saludprovincia/noticias/sputnik_v_tiene_una_efectividad_con_una_sola_dosis_de_786_para_evitar_casos |access-date=29 June 2021}}</ref><ref>{{Cite press release |title=Sputnik Light vaccine (the first component of Sputnik V vaccine) demonstrates 78.6-83.7% efficacy among the elderly in Argentina |date=2 June 2021 |publisher=Russian Direct Investment Fund |url=https://rdif.ru/Eng_fullNews/6863/ |access-date=29 June 2021}}</ref> |
|||
|} |
|||
{{notelist-lr}} |
|||
===Critical coverage=== |
|||
{{See also|Herd immunity#Vaccination|COVID-19#Immunity}} |
|||
While the most immediate goal of vaccination during a pandemic is to protect individuals from severe disease, a long-term goal is to eventually eradicate it. To do so, the proportion of the population that must be immunized must be greater than the critical vaccination coverage <math>V_c</math>. This value can be calculated from the [[basic reproduction number]] <math>R_0</math> and the vaccine effectiveness against transmission <math>E</math> as:<ref name="herd-immunity-guide">{{Cite journal |vauthors=Fine P, Eames K, Heymann DL |date=1 April 2011 |title="Herd Immunity": A Rough Guide |journal=Clinical Infectious Diseases |volume=52 |issue=7 |pages=911–916 |doi=10.1093/cid/cir007 |issn=1058-4838 |pmid=21427399 |doi-access=free}}</ref> |
|||
<math> V_c = \frac {1 - 1/R_0}{E} </math> |
|||
Assuming R<sub>0</sub> ≈ 2.87 for SARS-CoV-2,<ref name="sc2brn">{{Cite journal |vauthors=Billah MA, Miah MM, Khan MN |date=11 November 2020 |title=Reproductive number of coronavirus: A systematic review and meta-analysis based on global level evidence |journal=PLOS ONE |volume=15 |issue=11 |pages=e0242128 |bibcode=2020PLoSO..1542128B |doi=10.1371/journal.pone.0242128 |pmc=7657547 |pmid=33175914 |doi-access=free}}</ref> then, for example, the coverage level would have to be greater than 72.4% for a vaccine that is 90% effective against transmission. Using the same relationship, the required effectiveness against transmission can be calculated as: |
|||
<math> E = \frac {1 - 1/R_0}{V_c} </math> |
|||
Assuming the same R<sub>0</sub> ≈ 2.87, the effectiveness against transmission would have to be greater than 86.9% for a realistic coverage level of 75%<ref name="efficacy-needed" /> or 65.2% for an impossible coverage level of 100%. Less effective vaccines would not be able to eradicate the disease. |
|||
Several post-marketing studies have already estimated the effectiveness of some vaccines against asymptomatic infection. Prevention of infection has an impact on slowing transmission (particularly asymptomatic and pre-symptomatic), but the exact extent of this effect is still under investigation.<ref>{{#invoke:Cite web ||title=Science Brief: COVID-19 Vaccines and Vaccination |url=https://www.cdc.gov/coronavirus/2019-ncov/science/science-briefs/fully-vaccinated-people.html |publisher=Centers for Disease Control and Prevention |access-date=17 June 2021 |date=27 May 2021 |quote=Substantial reductions in SARS-CoV-2 infections (both symptomatic and asymptomatic) will reduce overall levels of disease, and therefore, viral transmission in the United States. However, investigations are ongoing to assess further the impact of COVID-19 vaccination on transmission. |archive-url=https://web.archive.org/web/20210616005526/https://www.cdc.gov/coronavirus/2019-ncov/science/science-briefs/fully-vaccinated-people.html |archive-date=16 June 2021|url-status=live}}</ref> |
|||
Some [[variants of SARS-CoV-2]] are more transmissible, showing an increased [[Basic reproduction number#Effective reproduction number|effective reproduction number]], indicating an increased basic reproduction number. Controlling them requires greater vaccine coverage, greater vaccine effectiveness against transmission, or a combination of both. |
|||
In July 2021, several experts expressed concern that achieving [[herd immunity]] may not currently be possible because the [[SARS-CoV-2 Delta variant|Delta variant]] is transmitted among those immunized with current vaccines.<ref>{{cite journal |last=Dyer |first=Owen |date=2021-08-02 |title=Covid-19: Delta infections threaten herd immunity vaccine strategy |url=https://www.bmj.com/content/374/bmj.n1933 |journal=BMJ |volume=374 |pages=n1933 |doi=10.1136/bmj.n1933 |issn=1756-1833 |pmid=34340962|s2cid=236778544 }}</ref> The CDC published data showing that vaccinated people could transmit the Delta strain, something officials believed was not possible with other variants.<ref>{{Cite news |last=Katella |first=Kathy |date=13 August 2021 |title=5 Things To Know About the Delta Variant |work=Yale Medicine News |url=https://www.yalemedicine.org/news/5-things-to-know-delta-variant-covid |access-date=18 August 2021}}</ref> |
|||
===Variants=== |
|||
{{Update|section|inaccurate=yes|date=July 2021|reason=Information taken from WHO's COVID-19 Weekly Epidemiological Update is outdated and inaccurate. The latest version now is 20 July, edition 49}} |
|||
[[File:WHO EN 3 Working Together 03Mar2021.webm|thumb|279x279px|[[World Health Organization]] video describing how variants proliferate in unvaccinated areas.]] |
|||
<!-- Please note this section is transcluded onto the Variants of SARS-CoV-2 page using Template:Excerpt --> |
|||
<noinclude>{{See also|Variants of SARS-CoV-2}}</noinclude> |
|||
The interplay between the SARS-CoV-2 virus and its human hosts was initially natural but is now being altered by the prompt availability of vaccines.<ref>{{Cite journal |vauthors=Burioni R, Topol EJ |date=21 June 2021 |title=Has SARS-CoV-2 reached peak fitness? |journal=Nature Medicine |volume=27 |issue=8 |pages=1323–1324 |doi=10.1038/s41591-021-01421-7 |pmid=34155413 |doi-access=free}}</ref> The potential emergence of a SARS-CoV-2 variant that is moderately or fully resistant to the antibody response elicited by the COVID-19 vaccines may necessitate modification of the vaccines.<ref name=":02">{{#invoke:Cite web| | author = Office of the Commissioner |date=23 February 2021|title=Coronavirus (COVID-19) Update: FDA Issues Policies to Guide Medical Product Developers Addressing Virus Variants|url=https://www.fda.gov/news-events/press-announcements/coronavirus-covid-19-update-fda-issues-policies-guide-medical-product-developers-addressing-virus|access-date=7 March 2021|website=U.S. [[Food and Drug Administration]] (FDA)}}</ref> The emergence of vaccine-resistant variants is more likely in a highly vaccinated population with uncontrolled transmission.<ref>{{Cite journal |last1=Rella |first1=Simon A. |last2=Kulikova |first2=Yuliya A. |last3=Dermitzakis |first3=Emmanouil T. |last4=Kondrashov |first4=Fyodor A. |date=2021-07-30 |title=Rates of SARS-CoV-2 transmission and vaccination impact the fate of vaccine-resistant strains |journal=Scientific Reports |volume=11 |issue=1 |pages=15729 |doi=10.1038/s41598-021-95025-3 |issn=2045-2322 |pmc=8324827 |pmid=34330988}}</ref> Trials indicate many vaccines developed for the initial strain have lower efficacy for some variants against symptomatic COVID-19.<ref name=":8">{{Cite journal |vauthors=Mahase E |date=March 2021 |title=Covid-19: Where are we on vaccines and variants? |journal=BMJ |volume=372 |pages=n597 |doi=10.1136/bmj.n597 |pmid=33653708 |doi-access=free |s2cid=232093175}}</ref> {{Asof|2021|2}}, the US [[Food and Drug Administration]] believed that all FDA authorized vaccines remained effective in protecting against circulating strains of SARS-CoV-2.<ref name=":02" /> |
|||
====Alpha (lineage B.1.1.7)==== |
|||
{{Further|SARS-CoV-2 Alpha variant}} |
|||
Limited evidence from various preliminary studies reviewed by the WHO has indicated retained efficacy/effectiveness against disease from Alpha with the Oxford–AstraZeneca vaccine, Pfizer–BioNTech and Novavax, with no data for other vaccines yet. Relevant to how vaccines can end the pandemic by preventing asymptomatic infection, they have also indicated retained antibody neutralization against Alpha with most of the widely distributed vaccines (Sputnik V, Pfizer–BioNTech, Moderna, CoronaVac, BBIBP-CorV, Covaxin), minimal to moderate reduction with the Oxford–AstraZeneca and no data for other vaccines yet.<ref name="who-update-variant-impact" /> |
|||
<noinclude>In December 2020, a new [[Variants of SARS-CoV-2|SARS‑CoV‑2 variant]], the [[SARS-CoV-2 Alpha variant|Alpha variant]] or lineage B.1.1.7, was identified in the UK.<ref>{{Cite news |date=18 January 2021 |title=Inside the B.1.1.7 Coronavirus Variant |work=[[The New York Times]] |url=https://www.nytimes.com/interactive/2021/health/coronavirus-mutations-B117-variant.html |access-date=29 January 2021}}</ref></noinclude> |
|||
Early results suggest protection to the variant from the Pfizer-BioNTech and Moderna vaccines.<ref name="science.sciencemag.org">{{Cite journal |display-authors=6 |vauthors=Muik A, Wallisch AK, Sänger B, Swanson KA, Mühl J, Chen W, Cai H, Maurus D, Sarkar R, Türeci Ö, Dormitzer PR, Şahin U |date=March 2021 |title=Neutralization of SARS-CoV-2 lineage B.1.1.7 pseudovirus by BNT162b2 vaccine-elicited human sera |journal=Science |volume=371 |issue=6534 |pages=1152–53 |bibcode=2021Sci...371.1152M |doi=10.1126/science.abg6105 |pmc=7971771 |pmid=33514629 |doi-access=free}}</ref><ref name="nature.b117.B1351">{{Cite journal |display-authors=6 |vauthors=Wang P, Nair MS, Liu L, Iketani S, Luo Y, Guo Y, Wang M, Yu J, Zhang B, Kwong PD, Graham BS, Mascola JR, Chang JY, Yin MT, Sobieszczyk M, Kyratsous CA, Shapiro L, Sheng Z, Huang Y, Ho DD |date=March 2021 |title=Antibody Resistance of SARS-CoV-2 Variants B.1.351 and B.1.1.7 |journal=Nature |volume=593 |issue=7857 |pages=130–35 |bibcode=2021Natur.593..130W |doi=10.1038/s41586-021-03398-2 |pmid=33684923 |doi-access=free}}</ref> |
|||
One study indicated that the [[Oxford–AstraZeneca COVID-19 vaccine]] had an efficacy of 42–89% against Alpha, versus 71–91% against other variants.<ref>{{Cite ssrn |title=Efficacy of ChAdOx1 nCoV-19 (AZD1222) Vaccine Against SARS-CoV-2 VOC 202012/01 (B.1.1.7) |date=February 2021 |ssrn=3779160 |display-authors=6 |vauthors=Emary KR, Golubchik T, Aley PK, Ariani CV, Angus BJ, Bibi S, Blane B, Bonsall D, Cicconi P, Charlton S, Clutterbuck E}}</ref>{{unreliable medical source|reason=preprint|date=July 2021}} |
|||
Preliminary data from a clinical trial indicates that the [[Novavax COVID-19 vaccine|Novavax vaccine]] is ~96% effective for symptoms against the original variant and ~86% against Alpha.<ref>{{Cite journal |vauthors=Mahase E |date=February 2021 |title=Covid-19: Novavax vaccine efficacy is 86% against UK variant and 60% against South African variant |journal=BMJ |volume=372 |pages=n296 |doi=10.1136/bmj.n296 |pmid=33526412 |doi-access=free |s2cid=231730012}}</ref> |
|||
====Beta (lineage B.1.351)==== |
|||
{{Further|SARS-CoV-2 Beta variant}} |
|||
Limited evidence from various preliminary studies reviewed by the WHO have indicated reduced efficacy/effectiveness against disease from Beta with the Oxford–AstraZeneca vaccine (possibly substantial), Novavax (moderate), Pfizer–BioNTech and Janssen (minimal), with no data for other vaccines yet. Relevant to how vaccines can end the pandemic by preventing asymptomatic infection, they have also indicated possibly reduced antibody neutralization against Beta with most of the widely distributed vaccines (Oxford–AstraZeneca, Sputnik V, Janssen, Pfizer–BioNTech, Moderna, Novavax; minimal to substantial reduction) except CoronaVac and BBIBP-CorV (minimal to modest reduction), with no data for other vaccines yet.<ref name="who-update-variant-impact">{{Cite techreport |type=Situation report |title=Weekly epidemiological update on COVID-19 - 8 June 2021 |institution=World Health Organization |date=8 June 2021 |url=https://www.who.int/publications/m/item/weekly-epidemiological-update-on-covid-19---8-june-2021 |at=Table 3 |access-date=14 June 2021}}</ref> |
|||
Moderna has launched a trial of a vaccine to tackle the [[SARS-CoV-2 Beta variant|Beta variant]] or lineage B.1.351.<ref>{{#invoke:Cite web| |title=Moderna develops new vaccine to tackle mutant Covid strain | work=[[Financial Times]]|url=https://www.ft.com/content/c0c8f72c-e58e-4319-80c4-0db153ad85db|access-date=30 January 2021 | vauthors = Kuchler H | date=25 January 2021 | url-access=subscription }}</ref> On 17 February 2021, Pfizer announced neutralization activity was reduced by two-thirds for this variant, while stating that no claims about the efficacy of the vaccine in preventing illness for this variant could yet be made.<ref>{{Cite journal |display-authors=6 |vauthors=Liu Y, Liu J, Xia H, Zhang X, Fontes-Garfias CR, Swanson KA, Cai H, Sarkar R, Chen W, Cutler M, Cooper D, Weaver SC, Muik A, Sahin U, Jansen KU, Xie X, Dormitzer PR, Shi PY |date=February 2021 |title=Neutralizing Activity of BNT162b2-Elicited Serum – Preliminary Report |journal=The New England Journal of Medicine |doi=10.1056/nejmc2102017 |pmid=33596352 |doi-access=free}}</ref> Decreased neutralizing activity of sera from patients vaccinated with the Moderna and Pfizer-BioNTech vaccines against Beta was later confirmed by several studies.<ref name="nature.b117.B1351" /><ref name="cell.B1351.P1">{{Cite journal |display-authors=6 |vauthors=Hoffmann M, Arora P, Gross R, Seidel A, Hoernich BF, Hahn AS, Krueger N, Graichen L, Hofmann-Winkler H, Kempf A, Winkler MS, Schulz S, Jaeck HM, Jahrsdoerfer B, Schrezenmeier H, Mueller M, Kleger A, Muench J, Poehlmann S |date=March 2021 |title=1 SARS-CoV-2 variants B.1.351 and P.1 escape from neutralizing antibodies |journal=Cell |volume=184 |issue=9 |pages=2384–2393.e12 |doi=10.1016/j.cell.2021.03.036 |pmc=7980144 |pmid=33794143 |doi-access=free}}</ref> On 1{{nbs}}April 2021, an update on a Pfizer/BioNTech South African vaccine trial stated that the vaccine was 100% effective so far (i.e., vaccinated participants saw no cases), with six of nine infections in the placebo control group being the Beta variant.<ref>{{Cite press release |title=Pfizer and BioNTech Confirm High Efficacy and No Serious Safety Concerns Through Up to Six Months Following Second Dose in Updated Topline Analysis of Landmark COVID-19 Vaccine Study |date=1 April 2021 |url=https://www.pfizer.com/news/press-release/press-release-detail/pfizer-and-biontech-confirm-high-efficacy-and-no-serious |access-date=2 April 2021 |website=Pfizer}}</ref> |
|||
In January 2021, Johnson & Johnson, which held trials for its [[Janssen COVID-19 vaccine|Janssen vaccine]] in South Africa, reported the level of protection against moderate to severe COVID-19 infection was 72% in the United States and 57% in South Africa.<ref name="auto"/> |
|||
On 6 February 2021, the ''[[Financial Times]]'' reported that provisional trial data from a study undertaken by South Africa's [[University of the Witwatersrand]] in conjunction with [[University of Oxford|Oxford University]] demonstrated reduced efficacy of the [[Oxford–AstraZeneca COVID-19 vaccine]] against the variant.<ref>{{Cite news |date=6 February 2021 |title=Oxford/AstraZeneca COVID shot less effective against South African variant: study |work=[[Reuters]] |url=https://www.reuters.com/article/us-health-coronavirus-astrazeneca-varian/oxford-astrazeneca-covid-shot-less-effective-against-south-african-variant-study-idUSKBN2A60SH |access-date=8 February 2021 |vauthors=Francis D, Andy B}}</ref> The study found that in a sample size of 2,000 the AZD1222 vaccine afforded only "minimal protection" in all but the most severe cases of COVID-19.<ref name="BBC55975052">{{Cite news |date=8 February 2021 |title=Covid: South Africa halts AstraZeneca vaccine rollout over new variant |work=[[BBC News Online]] |url=https://www.bbc.com/news/world-africa-55975052 |access-date=8 February 2021}}</ref> On 7{{nbs}}February 2021, the [[Minister of Health (South Africa)|Minister for Health]] for South Africa suspended the planned deployment of about a million doses of the vaccine whilst they examine the data and await advice on how to proceed.<ref name=BBC55975052 /><ref>{{Cite news |date=7 February 2021 |title=South Africa suspends Oxford-AstraZeneca vaccine rollout after researchers report 'minimal' protection against coronavirus variant |work=[[The Washington Post]] |location=London |url=https://www.washingtonpost.com/world/europe/astrazeneca-oxford-vaccine-south-african-variant/2021/02/07/e82127f8-6948-11eb-a66e-e27046e9e898_story.html |access-date=8 February 2021 |quote=South Africa will suspend use of the coronavirus vaccine being developed by Oxford University and AstraZeneca after researchers found it provided 'minimal protection' against mild to moderate coronavirus infections caused by the new variant first detected in that country. |vauthors=Booth W, Johnson CY}}</ref> |
|||
In March 2021, it was reported that the "preliminary efficacy" of the [[Novavax COVID-19 vaccine|Novavax vaccine]] (NVX-CoV2373) against Beta for mild, moderate, or severe COVID-19<ref>{{Cite journal |date=30 October 2020 |title=A Phase 2A/B, Randomized, Observer-blinded, Placebo-controlled Study to Evaluate the Efficacy, Immunogenicity, and Safety of a SARS-CoV-2 Recombinant Spike Protein Nanoparticle Vaccine (SARS-CoV-2 rS) With Matrix-M1 Adjuvant in South African Adult Subjects Living Without HIV; and Safety and Immunogenicity in Adults Living With HIV |url=https://clinicaltrials.gov/ct2/show/NCT04533399 |website=[[ClinicalTrials.gov]]}}</ref> for HIV-negative participants is 51%.{{mcn|date=June 2021}} |
|||
====Gamma (lineage P.1)==== |
|||
{{Further|SARS-CoV-2 Gamma variant}} |
|||
Limited evidence from various preliminary studies reviewed by the WHO have indicated likely retained efficacy/effectiveness against disease from Gamma with CoronaVac and BBIBP-CorV, with no data for other vaccines yet. Relevant to how vaccines can end the pandemic by preventing asymptomatic infection, they have also indicated retained antibody neutralization against Gamma with Oxford–AstraZeneca and CoronaVac (no to minimal reduction) and slightly reduced neutralization with Pfizer–BioNTech and Moderna (minimal to moderate reduction), with no data for other vaccines yet.<ref name="who-update-variant-impact" /> |
|||
The [[SARS-CoV-2 Gamma variant|Gamma variant]] or lineage P.1 variant (also known as 20J/501Y.V3), initially identified in Brazil, seems to partially escape vaccination with the Pfizer-BioNTech vaccine.<ref name="cell.B1351.P1" /> |
|||
====Delta (lineage B.1.617.2)==== |
|||
{{Further|SARS-CoV-2 Delta variant}} |
|||
Limited evidence from various preliminary studies reviewed by the WHO have indicated likely retained efficacy/effectiveness against disease from Delta with the Oxford–AstraZeneca vaccine and Pfizer–BioNTech, with no data for other vaccines yet. Relevant to how vaccines can end the pandemic by preventing asymptomatic infection, they have also indicated reduced antibody neutralization against Delta with ''single-dose'' Oxford–AstraZeneca (substantial reduction), Pfizer–BioNTech and Covaxin (modest to moderate reduction), with no data for other vaccines yet.<ref name="who-update-variant-impact" /> |
|||
<noinclude>In October 2020, a new variant was discovered in India, which was named [[lineage B.1.617]]. There were very few detections until January 2021, but by April it had spread to at least 20 countries in all continents except Antarctica and South America.<ref>{{#invoke:Cite web||title=PANGO lineages|url=https://cov-lineages.org/lineages/lineage_B.1.617.html|access-date=18 April 2021|website=cov-lineages.org}}</ref><ref name="Koshy">{{Cite news |date=8 April 2021 |title=Coronavirus {{!}} Indian 'double mutant' strain named B.1.617 |work=The Hindu |url=https://www.thehindu.com/news/national/indian-double-mutant-strain-named-b1617/article34274663.ece/amp/ |vauthors=Koshy J}}</ref><ref>{{Cite news |date=10 April 2021 |title=India's variant-fuelled second wave coincided with spike in infected flights landing in Canada |work=[[Toronto Sun]] |url=https://torontosun.com/news/local-news/indias-variant-fuelled-second-wave-coincided-with-spike-in-infected-flights-landing-in-canada |access-date=10 April 2021}}</ref></noinclude> Mutations present in the [[coronavirus spike protein|spike protein]] in the B.1.617 lineage are associated with reduced antibody neutralization in laboratory experiments.<ref name="edara_2021">{{cite journal |last1=Edara |first1=Venkata-Viswanadh |last2=Pinsky |first2=Benjamin A. |last3=Suthar |first3=Mehul S. |last4=Lai |first4=Lilin |last5=Davis-Gardner |first5=Meredith E. |last6=Floyd |first6=Katharine |last7=Flowers |first7=Maria W. |last8=Wrammert |first8=Jens |last9=Hussaini |first9=Laila |last10=Ciric |first10=Caroline Rose |last11=Bechnak |first11=Sarah |last12=Stephens |first12=Kathy |last13=Graham |first13=Barney S. |last14=Bayat Mokhtari |first14=Elham |last15=Mudvari |first15=Prakriti |last16=Boritz |first16=Eli |last17=Creanga |first17=Adrian |last18=Pegu |first18=Amarendra |last19=Derrien-Colemyn |first19=Alexandrine |last20=Henry |first20=Amy R. |last21=Gagne |first21=Matthew |last22=Douek |first22=Daniel C. |last23=Sahoo |first23=Malaya K. |last24=Sibai |first24=Mamdouh |last25=Solis |first25=Daniel |last26=Webby |first26=Richard J. |last27=Jeevan |first27=Trushar |last28=Fabrizio |first28=Thomas P. |title=Infection and Vaccine-Induced Neutralizing-Antibody Responses to the SARS-CoV-2 B.1.617 Variants |journal=New England Journal of Medicine |date=12 August 2021 |volume=385 |issue=7 |pages=664–666 |doi=10.1056/NEJMc2107799}}</ref><ref name="planas_2021">{{cite journal |last1=Planas |first1=Delphine |last2=Veyer |first2=David |last3=Baidaliuk |first3=Artem |last4=Staropoli |first4=Isabelle |last5=Guivel-Benhassine |first5=Florence |last6=Rajah |first6=Maaran Michael |last7=Planchais |first7=Cyril |last8=Porrot |first8=Françoise |last9=Robillard |first9=Nicolas |last10=Puech |first10=Julien |last11=Prot |first11=Matthieu |last12=Gallais |first12=Floriane |last13=Gantner |first13=Pierre |last14=Velay |first14=Aurélie |last15=Le Guen |first15=Julien |last16=Kassis-Chikhani |first16=Najiby |last17=Edriss |first17=Dhiaeddine |last18=Belec |first18=Laurent |last19=Seve |first19=Aymeric |last20=Courtellemont |first20=Laura |last21=Péré |first21=Hélène |last22=Hocqueloux |first22=Laurent |last23=Fafi-Kremer |first23=Samira |last24=Prazuck |first24=Thierry |last25=Mouquet |first25=Hugo |last26=Bruel |first26=Timothée |last27=Simon-Lorière |first27=Etienne |last28=Rey |first28=Felix A. |last29=Schwartz |first29=Olivier |title=Reduced sensitivity of SARS-CoV-2 variant Delta to antibody neutralization |journal=Nature |date=12 August 2021 |volume=596 |issue=7871 |pages=276–280 |doi=10.1038/s41586-021-03777-9}}</ref><noinclude> The variant has frequently been referred to as a 'Double mutant', even though in this respect it is not unusual.<ref name=617BBC/> In an update on 15 April 2021, PHE designated lineage B.1.617 as a 'Variant under investigation', VUI-21APR-01.<ref name="IndiaPHE">{{Cite news |date=15 April 2021 |title=Confirmed cases of COVID-19 variants identified in UK |work=Public Health England |url=https://www.gov.uk/government/news/confirmed-cases-of-covid-19-variants-identified-in-uk |access-date=16 April 2021}}</ref> On 6 May 2021, [[Public Health England]] escalated lineage B.1.617.2 from a Variant Under Investigation to a [[Variant of Concern]] based on an assessment of transmissibility being at least equivalent to the [[SARS-CoV-2 Alpha variant|Alpha variant]].<ref>{{#invoke:Cite web ||title=expert reaction to VUI-21APR-02/B.1.617.2 being classified by PHE as a variant of concern |url=https://www.sciencemediacentre.org/expert-reaction-to-vui-21apr-02-b-1-617-2-being-classified-by-phe-as-a-variant-of-concern/?cli_action=1621097773.028 |website= Science Media Centre |date=7 May 2021 |access-date=15 May 2021}}</ref></noinclude> |
|||
===Effect of neutralizing antibodies=== |
|||
One study found that the [[in vitro]] concentration ([[titer]]) of [[Neutralizing antibody|neutralizing antibodies]] elicited by a COVID-19 vaccine is a strong [[Correlates of immunity/correlates of protection|correlate of immune protection]]. The relationship between protection and neutralizing activity is [[Nonlinear system|nonlinear]]. A neutralization as low as {{Estimate|3|1|13|unit=%|mini=no}} of the level of [[convalescence]] results in 50% efficacy against severe disease, with {{Estimate|20|14|28|unit=%|mini=yes}} resulting in 50% efficacy against detectable infection. Protection against infection quickly decays, leaving individuals susceptible to mild infections, while protection against severe disease is largely retained and much more durable. The observed half-life of neutralizing titers was 65 days for mRNA vaccines ([[Pfizer–BioNTech COVID-19 vaccine|Pfizer–BioNTech]], [[Moderna COVID-19 vaccine|Moderna]]) during the first 4 months, increasing to 108 days over 8 months. Greater initial efficacy against infection likely results in a higher level of protection against serious disease in the long term (beyond 10 years, as seen in other vaccines such as smallpox, measles, mumps, and rubella), although the authors acknowledge that their simulations only consider protection from neutralizing antibodies and ignore other immune protection mechanisms, such as [[cell-mediated immunity]], which may be more durable. This observation also applies to efficacy against variants and is particularly significant for vaccines with a lower initial efficacy; for example, a 5-fold reduction in neutralization would indicate a reduction in initial efficacy from 95% to 77% against a specific variant, and from a lower efficacy of 70% to 32% against that variant. For the [[Oxford–AstraZeneca COVID-19 vaccine|Oxford–AstraZeneca vaccine]], the observed efficacy is below the predicted 95% confidence interval. It is higher for [[Sputnik V COVID-19 vaccine|Sputnik V]] and the convalescent response, and is within the predicted interval for the other vaccines evaluated ([[Pfizer–BioNTech COVID-19 vaccine|Pfizer–BioNTech]], [[Moderna COVID-19 vaccine|Moderna]], [[Janssen COVID-19 vaccine|Janssen]], [[CoronaVac]], [[Covaxin]], [[Novavax COVID-19 vaccine|Novavax]]).<ref>{{Cite journal |display-authors=6 |vauthors=Khoury DS, Cromer D, Reynaldi A, Schlub TE, Wheatley AK, Juno JA, Subbarao K, Kent SJ, Triccas JA, Davenport MP |date=17 May 2021 |title=Neutralizing antibody levels are highly predictive of immune protection from symptomatic SARS-CoV-2 infection |url=https://www.nature.com/articles/s41591-021-01377-8 |journal=Nature Medicine |volume=27 |issue=7 |pages=1205–1211 |doi=10.1038/s41591-021-01377-8 |issn=1546-170X |pmid=34002089 |s2cid=234769053}}</ref> |
|||
===Response of patients with preexisting diseases=== |
|||
====Hematologic malignancies==== |
|||
In a study on the serologic response to COVID-19 messenger RNA vaccines among patients with lymphoma, leukemia and myeloma, it was found that one-quarter of patients did not produce measurable antibodies, varying by blood cancer type. Patients with these conditions need to take precautions to avoid exposure to COVID-19.<ref>{{Cite journal|url=https://www.cell.com/cancer-cell/abstract/S1535-6108(21)00389-5|title=Antibody response to SARS-CoV-2 vaccines in patients with hematologic malignancies|first1=Lee M.|last1=Greenberger|first2=Larry A.|last2=Saltzman|first3=Jonathon W.|last3=Senefeld|first4=Patrick W.|last4=Johnson|first5=Louis J.|last5=DeGennaro|first6=Gwen L.|last6=Nichols|date=August 9, 2021|journal=Cancer Cell|volume=39|issue=8|pages=1031–1033|via=www.cell.com|doi=10.1016/j.ccell.2021.07.012|pmid=34331856}}</ref> |
|||
==References== |
==References== |
||
Revision as of 22:18, 29 August 2021
This article or section is in a state of significant expansion or restructuring, and is not yet ready for use. You are welcome to assist in its construction by editing it as well. If this article or section has not been edited in several days, please remove this template. If you are the editor who added this template and you are actively editing, please be sure to replace this template with {{in use}} during the active editing session. Click on the link for template parameters to use.
This article was last edited by Ftrebien (talk | contribs) 2 years ago. (Update timer) |
COVID-19 vaccine clinical research concerns the clinical research on COVID-19 vaccines. There are 22 vaccines authorized for use by national governments, with 5 of them in Phase IV, and 204 vaccines under clinical trials that have not yet been authorized. There are also 9 clinical trials on heterologous vaccination courses.
Trial and authorization status
Phase I trials test primarily for safety and preliminary dosing in a few dozen healthy subjects, while Phase II trials – following success in Phase I – evaluate immunogenicity, dose levels (efficacy based on biomarkers) and adverse effects of the candidate vaccine, typically in hundreds of people.[1][2] A Phase I–II trial consists of preliminary safety and immunogenicity testing, is typically randomized, placebo-controlled, while determining more precise, effective doses.[2] Phase III trials typically involve more participants at multiple sites, include a control group, and test effectiveness of the vaccine to prevent the disease (an "interventional" or "pivotal" trial), while monitoring for adverse effects at the optimal dose.[1][2] Definition of vaccine safety, efficacy, and clinical endpoints in a Phase III trial may vary between the trials of different companies, such as defining the degree of side effects, infection or amount of transmission, and whether the vaccine prevents moderate or severe COVID‑19 infection.[3][4][5]
A clinical trial design in progress may be modified as an "adaptive design" if accumulating data in the trial provide early insights about positive or negative efficacy of the treatment.[6][7] Adaptive designs within ongoing Phase II–III clinical trials on candidate vaccines may shorten trial durations and use fewer subjects, possibly expediting decisions for early termination or success, avoiding duplication of research efforts, and enhancing coordination of design changes for the Solidarity trial across its international locations.[6][8]
List of authorized and approved vaccines
National regulatory authorities have granted emergency use authorizations for fifteen vaccines. Six of those have been approved for emergency or full use by at least one WHO-recognized stringent regulatory authority. Biologic License Applications for the Pfizer–BioNTech and Moderna COVID‑19 vaccines have been submitted to the US Food and Drug Administration (FDA).[9][10]
The table below shows various vaccines authorized either for full or emergency use so far, with various other details.
| COVID-19 vaccines authorized for emergency use or approved for full use |
| Template:COVID-19 vaccine authorizations |
Vaccine candidates in human trials
The table below shows various vaccine candidates and the phases which they have completes so far. Current phases are also shown alongwith other details.
| COVID‑19 candidate vaccines in Phase I–III trials | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
Homologous prime-boost vaccination
In July 2021, the U.S. Food and Drug Administration (FDA) and the Centers for Disease Control and Prevention (CDC) issued a joint statement reporting that a booster dose is not necessary for those who have been fully vaccinated.[309]
In August 2021, the FDA and the CDC authorized the use of an additional mRNA vaccine dose for immunocompromised individuals.[310][311]
Heterologous prime-boost vaccination
Some experts believe that heterologous prime-boost vaccination courses can boost immunity, and several studies have begun to examine this effect.[312] Despite the absence of clinical data on the efficacy and safety of such heterologous combinations, Canada and several European countries have recommended a heterologous second dose for people who have received the first dose of the Oxford–AstraZeneca vaccine.[313]
In February 2021, the Oxford Vaccine Group launched the Com-COV vaccine trial to investigate heterologous prime-boost courses of different COVID-19 vaccines.[314] As of June 2021, the group is conducting two phase II studies: Com-COV and Com-COV2.[315]
In Com-COV, the two heterologous combinations of the Oxford–AstraZeneca and Pfizer–BioNTech vaccines were compared with the two homologous combinations of the same vaccines, with an interval of 28 or 84 days between doses.[316][317][unreliable medical source?]
In Com-COV2, the first dose is the Oxford–AstraZeneca vaccine or the Pfizer vaccine, and the second dose is the Moderna vaccine, the Novavax vaccine, or a homologous vaccine equal to the first dose, with an interval of 56 or 84 days between doses.[318]
A study in the UK is evaluating annual heterologous boosters using the following randomly selected vaccines: Oxford–AstraZeneca, Pfizer–BioNTech, Moderna, Novavax, VLA2001, CureVac, and Janssen.[319]
| First dose | Second dose | Schedules | Current phase (participants), periods and locations |
|---|---|---|---|
| Oxford–AstraZeneca Pfizer–BioNTech |
Oxford–AstraZeneca Pfizer–BioNTech |
Days 0 and 28 Days 0 and 84 |
Phase II (820) Feb–Aug 2021, United Kingdom |
| Sputnik Light | Oxford–AstraZeneca Moderna BBIBP-CorV |
Phase II (121) Feb–Aug 2021, Argentina | |
| Oxford–AstraZeneca Pfizer–BioNTech |
Oxford–AstraZeneca Pfizer–BioNTech Moderna Novavax |
Days 0 and 56–84 | Phase II (1,050) Mar 2021 – Sep 2022, United Kingdom |
| Convidecia | ZF2001 | Days 0 and 28 Days 0 and 56 |
Phase IV (120) Apr–Dec 2021, China |
| Oxford–AstraZeneca | Pfizer–BioNTech | Days 0 and 28 | Phase II (676) Apr 2021 – Apr 2022, Spain |
| Oxford–AstraZeneca Pfizer–BioNTech Moderna |
Pfizer–BioNTech Moderna |
Days 0 and 28 Days 0 and 112 |
Phase II (1,200) May 2021 – Mar 2023, Canada |
| Pfizer–BioNTech Moderna |
Pfizer–BioNTech Moderna |
Days 0 and 42 | Phase II (400) May 2021 – Jan 2022, France |
| Oxford–AstraZeneca | Pfizer–BioNTech | Days 0 and 28 Days 0 and 21–49 |
Phase II (3,000) May–Dec 2021, Austria |
| Janssen | Pfizer–BioNTech Janssen Moderna |
Days 0 and 84 | Phase II (432) Jun 2021 – Sep 2022, Netherlands |
Efficacy

Vaccine efficacy is the reduction in risk of getting the disease by vaccinated participants in a controlled trial compared with the risk of getting the disease by unvaccinated participants.[328] An efficacy of 0% means that the vaccine does not work (identical to placebo). An efficacy of 50% means that there are half as many cases of infection as in unvaccinated individuals.[citation needed]
The vaccine's efficacy may be adversely effected if the arm is held improperly or squeezed so the vaccine is injected subcutaneously instead of into the muscle.[329][330] The CDC guidance is to not repeat doses that are administered subcutaneously.[331]
It is not straightforward to compare the efficacies of the different vaccines because the trials were run with different populations, geographies, and variants of the virus.[332] In the case of COVID‑19, a vaccine efficacy of 67% may be enough to slow the pandemic, but the current vaccines do not confer sterilizing immunity,[333] which is necessary to prevent transmission. Vaccine efficacy reflects disease prevention, a poor indicator of transmissibility of SARS‑CoV‑2 since asymptomatic people can be highly infectious.[334] The US Food and Drug Administration (FDA) and the European Medicines Agency (EMA) set a cutoff of 50% as the efficacy required to approve a COVID‑19 vaccine, with the lower limit of the 95% confidence interval being greater than 30%.[335][336][337] Aiming for a realistic population vaccination coverage rate of 75%, and depending on the actual basic reproduction number, the necessary effectiveness of a COVID-19 vaccine is expected to need to be at least 70% to prevent an epidemic and at least 80% to extinguish it without further measures, such as social distancing.[338]
The observed substantial efficacy of certain mRNA vaccines even after partial (1-dose) immunization[339][327] indicates a non-linear dose-efficacy relation already seen in the phase I-II study[340] and suggests that personalization of the vaccine dose (regular dose to the elderly, reduced dose to the healthy young,[341] additional booster dose to the immunosuppressed[342]) might allow accelerating vaccination campaigns in settings of limited supplies, thereby shortening the pandemic, as predicted by pandemic modeling.[343]
Ranges below are 95% confidence intervals unless indicated otherwise, and all values are for all participants regardless of age, according to the references for each of the trials. By definition, the accuracy of the estimates without an associated confidence interval is unknown publicly. Efficacy against severe COVID-19 is the most important, since hospitalizations and deaths are a public health burden whose prevention is a priority.[344] Authorized and approved vaccines have shown the following efficacies:
| Vaccine | Efficacy by severity of COVID-19 | Trial location | Refs | ||
|---|---|---|---|---|---|
| Mild or moderate[A] | Severe without hospitalization or death[B] | Severe with hospitalization or death[C] | |||
| Oxford–AstraZeneca | 81% (60–91%)[D] | 100% (97.5% CI, 72–100%) | 100%[E] | Multinational | [345] |
| 76% (68–82%)[F] | 100%[E] | 100%[E] | United States | [346] | |
| Pfizer–BioNTech | 95% (90–98%)[G] | 66% (−125 to 96%)[H][G] | Multinational | [347] | |
| 95% (90–98%)[G] | Not reported | Not reported | United States | [348] | |
| Janssen | 66% (55–75%)[I][J] | 85% (54–97%)[J] | 100%[E][J][K] | Multinational | [349] |
| 72% (58–82%)[I][J] | 86% (−9 to 100%)[H][J] | 100%[E][J][K] | United States | ||
| 68% (49–81%)[I][J] | 88% (8–100%)[H][J] | 100%[E][J][K] | Brazil | ||
| 64% (41–79%)[I][J] | 82% (46–95%)[J] | 100%[E][J][K] | South Africa | ||
| Moderna | 94% (89–97%)[L] | 100%[E][M] | 100%[E][M] | United States | [351] |
| BBIBP-CorV | 78% (65–86%) | 100%[E] | 100%[E] | Multinational | [352] |
| Sputnik V | 92% (86–95%) | 100% (94–100%) | 100%[E] | Russia | [353] |
| CoronaVac | 51% (36–62%)[N] | 84% (58–94%)[N] | 100% (56–100%)[N] | Brazil | [354][355][356] |
| 84% (65–92%) | 100%[E] | 100% (20–100%)[H] | Turkey | [357] | |
| Covaxin | 78% (65–86%)[N] | 93% (57–100%)[N] | India | [358][unreliable medical source?] | |
| Sputnik Light | 79%[E] | Not reported | Not reported | Russia | [359] |
| Convidecia | 66%[E][N] | 91%[E][N] | Not reported | Multinational | [360][unreliable medical source?] |
| WIBP-CorV | 73% (58–82%) | 100%[E][O] | 100%[E][O] | Multinational | [361] |
| Abdala | 92% (86–96%) | Not reported | Not reported | Cuba | [362][363][unreliable medical source?] |
| Soberana 02 | 62%[E] | Not reported | Not reported | Cuba | [364][unreliable medical source?] |
| Novavax | 90% (75–95%) | 100%[E][O] | 100%[E][O] | United Kingdom | [365][366][367] |
| 60% (20–80%)[H] | 100%[E][O] | 100%[E][O] | South Africa | ||
| 90%[E] | Not reported | Not reported | United States | ||
| Not reported | Not reported | Mexico | |||
| CureVac | 48%[E] | Not reported | Not reported | Multinational | [368] |
| ZyCoV-D | 67%[E] | Not reported | Not reported | India | [369][unreliable medical source?] |
| ZF2001 | 82%[E] | Not reported | Not reported | Multinational | [370][unreliable medical source?] |
- ^ Mild symptoms: fever, dry cough, fatigue, myalgia, arthralgia, sore throat, diarrhea, nausea, vomiting, headache, anosmia, ageusia, nasal congestion, rhinorrhea, conjunctivitis, skin rash, chills, dizziness. Moderate symptoms: mild pneumonia.
- ^ Severe symptoms without hospitalization or death for an individual, are any one of the following severe respiratory symptoms measured at rest on any time during the course of observation (on top of having either pneumonia, deep vein thrombosis, dyspnea, hypoxia, persistent chest pain, anorexia, confusion, fever above 38 °C (100 °F)), that however were not persistent/severe enough to cause hospitalization or death: Any respiratory rate ≥30 breaths/minute, heart rate ≥125 beats/minute, oxygen saturation (SpO2) ≤93% on room air at sea level, or partial pressure of oxygen/fraction of inspired oxygen (PaO2/FiO2) <300 mmHg.
- ^ Severe symptoms causing hospitalization or death, are those requiring treatment at hospitals or results in deaths: dyspnea, hypoxia, persistent chest pain, anorexia, confusion, fever above 38 °C (100 °F), respiratory failure, kidney failure, multiorgan dysfunction, sepsis, shock.
- ^ With twelve weeks or more between doses. For an interval of less than six weeks, the trial found an efficacy 55% (33–70%).
- ^ a b c d e f g h i j k l m n o p q r s t u v w x y z aa A confidence interval was not provided, so it is not possible to know the accuracy of this measurement.
- ^ With a four-week interval between doses. Efficacy is "at preventing symptomatic COVID-19".
- ^ a b c COVID-19 symptoms observed in the Pfizer–BioNTech vaccine trials, were only counted as such for vaccinated individuals if they began more than seven days after their second dose, and required presence of a positive RT-PCR test result. Mild/moderate cases required at least oen of the following symptoms and a positive test during, or within 4 days before or after, the symptomatic period: fever; new or increased cough; new or increased shortness of breath; chills; new or increased muscle pain; new loss of taste or smell; sore throat; diarrhoea; or vomiting. Severe cases additionally required at least one of the following symptoms: clinical signs at rest indicative of severe systemic illness (RR ≥30 breaths per minute, HR ≥125 beats per minute, SpO2 ≤93% on room air at sea level, or PaO2/FiO2<300mm Hg); respiratory failure (defined as needing high-flow oxygen, non-invasive ventilation, mechanical ventilation, or ECMO); evidence of shock (SBP <90 mm Hg, DBP <60 mm Hg, or requiring vasopressors); significant acute renal, hepatic, or neurologic dysfunction; admission to an ICU; death.[347][348]
- ^ a b c d e This measurement is not accurate enough to support the high efficacy because the lower limit of the 95% confidence interval is lower than the minimum of 30%.
- ^ a b c d Moderate cases.
- ^ a b c d e f g h i j k l Efficacy reported 28 days post-vaccination for the Janssen single shot vaccine. A lower efficacy was found for the vaccinated individuals 14 days post-vaccination.[349]
- ^ a b c d No hospitalizations or deaths were detected 28 days post-vaccination for 19,630 vaccinated individuals in the trials, compared with 16 hospitalizations reported in the placebo group of 19,691 individuals (incidence rate 5.2 per 1000 person-years)[349] and seven COVID-19 related deaths for the same placebo group.[350]
- ^ Mild/Moderate COVID-19 symptoms observed in the Moderna vaccine trials, were only counted as such for vaccinated individuals if they began more than 14 days after their second dose, and required presence of a positive RT-PCR test result along with at least two systemic symptoms (fever above 38ºC, chills, myalgia, headache, sore throat, new olfactory and taste disorder) or just one respiratory symptom (cough, shortness of breath or difficulty breathing, or clinical or radiographical evidence of pneumonia).[351]
- ^ a b Severe COVID-19 symptoms observed in the Moderna vaccine trials, were defined as symptoms having met the criteria for mild/moderate symptoms plus any of the following observations: Clinical signs indicative of severe systemic illness, respiratory rate ≥30 per minute, heart rate ≥125 beats per minute, SpO2 ≤93% on room air at sea level or PaO2/FIO2 <300 mm Hg; or respiratory failure or ARDS, (defined as needing high-flow oxygen, non-invasive or mechanical ventilation, or ECMO), evidence of shock (systolic blood pressure <90 mmHg, diastolic BP <60 mmHg or requiring vasopressors); or significant acute renal, hepatic, or neurologic dysfunction; or admission to an intensive care unit or death. No severe cases were detected for vaccinated individuals in the trials, compared with thirty in the placebo group (incidence rate 9.1 per 1000 person-years).[351]
- ^ a b c d e f g These Phase III data have not been published or peer reviewed.
- ^ a b c d e f No cases detected in trial.
Effectiveness
Recent data from studies in the US and in other countries found that the available COVID-19 vaccines from the United States are "highly protective against severe illness, hospitalization, and death due to COVID-19."[371] In comparison with fully vaccinated people, the CDC found that those who were not vaccinated were from 5 to nearly 30 times more likely to become either infected or hospitalized.[372][373] As of June 2021, over 96% of doctors were fully vaccinated against COVID-19.[374]
By late August 2021, after the Delta variant became dominant, studies concluded that Covid vaccines provided 55 percent protection against Covid infections, 80 percent against symptomatic infection, and at least 90 percent against hospitalization.[375] The Delta variant, which is about 40 percent more contagious than the alpha variant,[376] became the dominant strain during the spring of 2021. However, the vaccines still protected against severe illness and hospitalizations with slight reduction in effectiveness.[375] The CDC similarly found that vaccines were 90 percent effective at preventing hospitalizations.[377]
My hospital, one of the largest in central Florida, was full of covid patients, more than 90 percent of whom were unvaccinated. We had no beds available. We had paused elective surgeries the previous week and have been trying to control the influx of patients. Our emergency department had a 12-hour wait that day.
Nitesh N. Paryani, director of Tampa Oncology & Proton [378]
As a result of the CDC reports, President Joe Biden said that “virtually all” Covid hospitalizations and deaths in the U.S. were among unvaccinated people.[379] While a study in the state of Washington found that unvaccinated people were six times more likely to test positive for COVID-19, 37 times more likely to be hospitalized, and 67 times more likely to die, compared to those who had been vaccinated.[380] In addition, unvaccinated Covid patients have strained the capacity of hospitals throughout the country, forcing many to turn away patients with life-threatening diseases.[378][381][382]
Researchers note that although current vaccines were not designed against the Delta variant, they nonetheless are highly effective, but to a lesser degree: protection fell from 91% to 66%.[383] One expert stated that "those who are infected following vaccination are still not getting sick and not dying like was happening before vaccination."[376] "This virus is the most efficient virus for finding new hosts that are vulnerable," stated Dr. Eric Topol, director and founder of the Scripps Research Translational Institute.[376] By late August 2021 the Delta variant accounted for 99 percent of U.S. cases and was found to double the risk of severe illness and hospitalization for those not yet vaccinated.[384] Approximately 600,000 people a day in the U.S. were being vaccinated by August 2021.[385]
Studies
The real-world studies of vaccine effectiveness measure to which extent a certain vaccine has succeeded in preventing COVID-19 infection, symptoms, hospitalization and death for the vaccinated individuals in a large population under routine conditions that are less than ideal.[386]
- In Israel, among the 715,425 individuals vaccinated by the Moderna or Pfizer-BioNTech vaccines during the period 20 December 2020, to 28 January 2021, it was observed for the period starting seven days after the second shot, that only 317 people (0.04%) became sick with mild/moderate COVID-19 symptoms and only 16 people (0.002%) were hospitalized.[387]
- The Pfizer-BioNTech and Moderna COVID-19 vaccines provide highly effective protection, according to a report from the US Centers for Disease Control and Prevention (CDC). Under real-world conditions, mRNA vaccine effectiveness of full immunization (≥14 days after second dose) was 90% against SARS-CoV-2 infections regardless of symptom status; vaccine effectiveness of partial immunization (≥14 days after first dose but before second dose) was 80%.[388]
- 15,121 health care workers from 104 hospitals in England, that all had tested negative for COVID-19 antibodies prior of the study, were followed by RT-PCR tests twice a week from 7 December 2020 to 5 February 2021, during a time when the Alpha variant (lineage B.1.1.7) was in circulation as the dominant variant. The study compared the positive results for the 90.7% vaccinated share of their cohort with the 9.3% unvaccinated share, and found that the Pfizer-BioNTech vaccine reduced all infections (including asymptomatic), by 72% (58-86%) three weeks after the first dose and 86% (76-97%) one week after the second dose.[389][needs update]
- A study of the general population in Israel conducted from 17 January to 6 March 2021, during a time when the Alpha variant was in circulation as the dominant variant, found that the Pfizer vaccine reduced asymptomatic COVID-19 infections by 94% and symptomatic COVID-19 infections by 97%.[390]
- A study, among pre-surgical patients across the Mayo Clinic system in the United States, showed that mRNA vaccines were 80% protective against asymptomatic infections.[391]
- A study in England found that a single dose of the Oxford–AstraZeneca COVID-19 vaccine is about 73% (27–90%) effective in people aged 70 and older.[392]
| Vaccine | Effectiveness by severity of COVID-19 | Study location | Refs | |||
|---|---|---|---|---|---|---|
| Asymptomatic | Symptomatic | Hospitalization | Death | |||
| Oxford–AstraZeneca | 70% (69–71%) | Not reported | 87% (85–88%) | 90% (88–92%) | Brazil | [393] |
| Not reported | 89% (78–94%)[i] | Not reported | England | [395] | ||
| Not reported | 89%[ii] | Argentina | [396] | |||
| Pfizer–BioNTech | 92% (91–92%) | 97% (97–97%) | 98% (97–98%) | 97% (96–97%) | Israel | [397] |
| 92% (88–95%) | 94% (87–98%) | 87% (55–100%) | 97%[ii] | Israel | [398][390] | |
| Not reported | 78% (77–79%) | 98% (96–99%) | 96% (95–97%) | Uruguay | [399] | |
| 85% (74–96%) | Not reported | England | [400] | |||
| 90% (68–97%) | Not reported | 100%[ii][iii] | United States | [388] | ||
| Moderna | 90% (68–97%) | Not reported | 100%[ii][iii] | United States | [388] | |
| BBIBP-CorV | Not reported | 84%[ii] | Argentina | [396] | ||
| Not reported | 94%[ii] | Peru | [401] | |||
| Sputnik V | Not reported | 98%[ii] | Not reported | Russia | [402][403] | |
| Not reported | 98%[ii] | 100%[ii][iii] | 100%[ii][iii] | United Arab Emirates | [404] | |
| Not reported | 93%[ii] | Argentina | [396] | |||
| CoronaVac | 54% (53–55%) | Not reported | 73% (72–74%) | 74% (73–75%) | Brazil | [393] |
| Not reported | 66% (65–67%) | 88% (87–88%) | 86% (85–88%) | Chile | [405][406] | |
| Not reported | 60% (59–61%) | 91% (89–93%) | 95% (93–96%) | Uruguay | [399] | |
| Not reported | 94%[ii] | 96%[ii] | 98%[ii] | Indonesia | [407][408] | |
| Not reported | 80%[ii] | 86%[ii] | 95%[ii] | Brazil | [409][410] | |
| Sputnik Light | Not reported | 79%[ii][iv] | 88%[ii][iv] | 85%[ii][iv] | Argentina | [411][412] |
Critical coverage
While the most immediate goal of vaccination during a pandemic is to protect individuals from severe disease, a long-term goal is to eventually eradicate it. To do so, the proportion of the population that must be immunized must be greater than the critical vaccination coverage . This value can be calculated from the basic reproduction number and the vaccine effectiveness against transmission as:[413]
Assuming R0 ≈ 2.87 for SARS-CoV-2,[414] then, for example, the coverage level would have to be greater than 72.4% for a vaccine that is 90% effective against transmission. Using the same relationship, the required effectiveness against transmission can be calculated as:
Assuming the same R0 ≈ 2.87, the effectiveness against transmission would have to be greater than 86.9% for a realistic coverage level of 75%[338] or 65.2% for an impossible coverage level of 100%. Less effective vaccines would not be able to eradicate the disease.
Several post-marketing studies have already estimated the effectiveness of some vaccines against asymptomatic infection. Prevention of infection has an impact on slowing transmission (particularly asymptomatic and pre-symptomatic), but the exact extent of this effect is still under investigation.[415]
Some variants of SARS-CoV-2 are more transmissible, showing an increased effective reproduction number, indicating an increased basic reproduction number. Controlling them requires greater vaccine coverage, greater vaccine effectiveness against transmission, or a combination of both.
In July 2021, several experts expressed concern that achieving herd immunity may not currently be possible because the Delta variant is transmitted among those immunized with current vaccines.[416] The CDC published data showing that vaccinated people could transmit the Delta strain, something officials believed was not possible with other variants.[417]
Variants
This section's factual accuracy may be compromised due to out-of-date information. The reason given is: Information taken from WHO's COVID-19 Weekly Epidemiological Update is outdated and inaccurate. The latest version now is 20 July, edition 49. (July 2021) |
The interplay between the SARS-CoV-2 virus and its human hosts was initially natural but is now being altered by the prompt availability of vaccines.[418] The potential emergence of a SARS-CoV-2 variant that is moderately or fully resistant to the antibody response elicited by the COVID-19 vaccines may necessitate modification of the vaccines.[419] The emergence of vaccine-resistant variants is more likely in a highly vaccinated population with uncontrolled transmission.[420] Trials indicate many vaccines developed for the initial strain have lower efficacy for some variants against symptomatic COVID-19.[421] As of February 2021[update], the US Food and Drug Administration believed that all FDA authorized vaccines remained effective in protecting against circulating strains of SARS-CoV-2.[419]
Alpha (lineage B.1.1.7)
Limited evidence from various preliminary studies reviewed by the WHO has indicated retained efficacy/effectiveness against disease from Alpha with the Oxford–AstraZeneca vaccine, Pfizer–BioNTech and Novavax, with no data for other vaccines yet. Relevant to how vaccines can end the pandemic by preventing asymptomatic infection, they have also indicated retained antibody neutralization against Alpha with most of the widely distributed vaccines (Sputnik V, Pfizer–BioNTech, Moderna, CoronaVac, BBIBP-CorV, Covaxin), minimal to moderate reduction with the Oxford–AstraZeneca and no data for other vaccines yet.[422]
In December 2020, a new SARS‑CoV‑2 variant, the Alpha variant or lineage B.1.1.7, was identified in the UK.[423]
Early results suggest protection to the variant from the Pfizer-BioNTech and Moderna vaccines.[424][425]
One study indicated that the Oxford–AstraZeneca COVID-19 vaccine had an efficacy of 42–89% against Alpha, versus 71–91% against other variants.[426][unreliable medical source?]
Preliminary data from a clinical trial indicates that the Novavax vaccine is ~96% effective for symptoms against the original variant and ~86% against Alpha.[427]
Beta (lineage B.1.351)
Limited evidence from various preliminary studies reviewed by the WHO have indicated reduced efficacy/effectiveness against disease from Beta with the Oxford–AstraZeneca vaccine (possibly substantial), Novavax (moderate), Pfizer–BioNTech and Janssen (minimal), with no data for other vaccines yet. Relevant to how vaccines can end the pandemic by preventing asymptomatic infection, they have also indicated possibly reduced antibody neutralization against Beta with most of the widely distributed vaccines (Oxford–AstraZeneca, Sputnik V, Janssen, Pfizer–BioNTech, Moderna, Novavax; minimal to substantial reduction) except CoronaVac and BBIBP-CorV (minimal to modest reduction), with no data for other vaccines yet.[422]
Moderna has launched a trial of a vaccine to tackle the Beta variant or lineage B.1.351.[428] On 17 February 2021, Pfizer announced neutralization activity was reduced by two-thirds for this variant, while stating that no claims about the efficacy of the vaccine in preventing illness for this variant could yet be made.[429] Decreased neutralizing activity of sera from patients vaccinated with the Moderna and Pfizer-BioNTech vaccines against Beta was later confirmed by several studies.[425][430] On 1 April 2021, an update on a Pfizer/BioNTech South African vaccine trial stated that the vaccine was 100% effective so far (i.e., vaccinated participants saw no cases), with six of nine infections in the placebo control group being the Beta variant.[431]
In January 2021, Johnson & Johnson, which held trials for its Janssen vaccine in South Africa, reported the level of protection against moderate to severe COVID-19 infection was 72% in the United States and 57% in South Africa.[432]
On 6 February 2021, the Financial Times reported that provisional trial data from a study undertaken by South Africa's University of the Witwatersrand in conjunction with Oxford University demonstrated reduced efficacy of the Oxford–AstraZeneca COVID-19 vaccine against the variant.[433] The study found that in a sample size of 2,000 the AZD1222 vaccine afforded only "minimal protection" in all but the most severe cases of COVID-19.[434] On 7 February 2021, the Minister for Health for South Africa suspended the planned deployment of about a million doses of the vaccine whilst they examine the data and await advice on how to proceed.[434][435]
In March 2021, it was reported that the "preliminary efficacy" of the Novavax vaccine (NVX-CoV2373) against Beta for mild, moderate, or severe COVID-19[436] for HIV-negative participants is 51%.
This article needs additional citations for verification. (June 2021) |
Gamma (lineage P.1)
Limited evidence from various preliminary studies reviewed by the WHO have indicated likely retained efficacy/effectiveness against disease from Gamma with CoronaVac and BBIBP-CorV, with no data for other vaccines yet. Relevant to how vaccines can end the pandemic by preventing asymptomatic infection, they have also indicated retained antibody neutralization against Gamma with Oxford–AstraZeneca and CoronaVac (no to minimal reduction) and slightly reduced neutralization with Pfizer–BioNTech and Moderna (minimal to moderate reduction), with no data for other vaccines yet.[422]
The Gamma variant or lineage P.1 variant (also known as 20J/501Y.V3), initially identified in Brazil, seems to partially escape vaccination with the Pfizer-BioNTech vaccine.[430]
Delta (lineage B.1.617.2)
Limited evidence from various preliminary studies reviewed by the WHO have indicated likely retained efficacy/effectiveness against disease from Delta with the Oxford–AstraZeneca vaccine and Pfizer–BioNTech, with no data for other vaccines yet. Relevant to how vaccines can end the pandemic by preventing asymptomatic infection, they have also indicated reduced antibody neutralization against Delta with single-dose Oxford–AstraZeneca (substantial reduction), Pfizer–BioNTech and Covaxin (modest to moderate reduction), with no data for other vaccines yet.[422]
In October 2020, a new variant was discovered in India, which was named lineage B.1.617. There were very few detections until January 2021, but by April it had spread to at least 20 countries in all continents except Antarctica and South America.[437][438][439] Mutations present in the spike protein in the B.1.617 lineage are associated with reduced antibody neutralization in laboratory experiments.[440][441] The variant has frequently been referred to as a 'Double mutant', even though in this respect it is not unusual.[442] In an update on 15 April 2021, PHE designated lineage B.1.617 as a 'Variant under investigation', VUI-21APR-01.[443] On 6 May 2021, Public Health England escalated lineage B.1.617.2 from a Variant Under Investigation to a Variant of Concern based on an assessment of transmissibility being at least equivalent to the Alpha variant.[444]
Effect of neutralizing antibodies
One study found that the in vitro concentration (titer) of neutralizing antibodies elicited by a COVID-19 vaccine is a strong correlate of immune protection. The relationship between protection and neutralizing activity is nonlinear. A neutralization as low as 3% (95% CI, 1–13%) of the level of convalescence results in 50% efficacy against severe disease, with 20% (14–28%) resulting in 50% efficacy against detectable infection. Protection against infection quickly decays, leaving individuals susceptible to mild infections, while protection against severe disease is largely retained and much more durable. The observed half-life of neutralizing titers was 65 days for mRNA vaccines (Pfizer–BioNTech, Moderna) during the first 4 months, increasing to 108 days over 8 months. Greater initial efficacy against infection likely results in a higher level of protection against serious disease in the long term (beyond 10 years, as seen in other vaccines such as smallpox, measles, mumps, and rubella), although the authors acknowledge that their simulations only consider protection from neutralizing antibodies and ignore other immune protection mechanisms, such as cell-mediated immunity, which may be more durable. This observation also applies to efficacy against variants and is particularly significant for vaccines with a lower initial efficacy; for example, a 5-fold reduction in neutralization would indicate a reduction in initial efficacy from 95% to 77% against a specific variant, and from a lower efficacy of 70% to 32% against that variant. For the Oxford–AstraZeneca vaccine, the observed efficacy is below the predicted 95% confidence interval. It is higher for Sputnik V and the convalescent response, and is within the predicted interval for the other vaccines evaluated (Pfizer–BioNTech, Moderna, Janssen, CoronaVac, Covaxin, Novavax).[445]
Response of patients with preexisting diseases
Hematologic malignancies
In a study on the serologic response to COVID-19 messenger RNA vaccines among patients with lymphoma, leukemia and myeloma, it was found that one-quarter of patients did not produce measurable antibodies, varying by blood cancer type. Patients with these conditions need to take precautions to avoid exposure to COVID-19.[446]
References
- ^ a b Cite error: The named reference
Vaccines.govwas invoked but never defined (see the help page). - ^ a b c Cite error: The named reference
fda-ddpwas invoked but never defined (see the help page). - ^ Cite error: The named reference
cohen6-19was invoked but never defined (see the help page). - ^ "How flu vaccine effectiveness and efficacy are measured". U.S. Centers for Disease Control and Prevention (CDC). 29 January 2016. Archived from the original on 7 May 2020. Retrieved 6 May 2020.
- ^ "Principles of epidemiology, Section 8: Concepts of disease occurrence". U.S. Centers for Disease Control and Prevention (CDC). 18 May 2012. Archived from the original on 6 April 2020. Retrieved 6 May 2020.
- ^ a b Pallmann P, Bedding AW, Choodari-Oskooei B, Dimairo M, Flight L, Hampson LV, et al. (February 2018). "Adaptive designs in clinical trials: why use them, and how to run and report them". BMC Medicine. 16 (1): 29. doi:10.1186/s12916-018-1017-7. PMC 5830330. PMID 29490655.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ "Adaptive designs for clinical trials of drugs and biologics: Guidance for industry" (PDF). U.S. Food and Drug Administration (FDA). 1 November 2019. Archived from the original on 13 December 2019. Retrieved 3 April 2020.
- ^ "An international randomised trial of candidate vaccines against COVID-19: Outline of Solidarity vaccine trial" (PDF). World Health Organization (WHO). 9 April 2020. Archived (PDF) from the original on 12 May 2020. Retrieved 9 May 2020.
- ^ "Pfizer and BioNTech Initiate Rolling Submission of Biologics License Application for U.S. FDA Approval of Their COVID 19 Vaccine". Pfizer (Press release). 7 May 2021. Retrieved 9 June 2021.
- ^ "Moderna Announces Initiation of Rolling Submission of Biologics License Application (BLA) with U.S. FDA for the Moderna COVID-19 Vaccine" (Press release). Moderna. 1 June 2021. Retrieved 9 June 2021 – via Business Wire.
- ^ "COVID-19 vaccine tracker (Refresh URL to update)". vac-lshtm.shinyapps.io. London School of Hygiene & Tropical Medicine. 12 July 2021. Retrieved 10 March 2021.
- ^ "COVID-19 vaccine tracker (Choose vaccines tab, apply filters to view select data)". Milken Institute. 8 December 2020. Retrieved 11 December 2020.
- ^ "Draft landscape of COVID 19 candidate vaccines". World Health Organization (WHO). 10 December 2020. Retrieved 11 December 2020.
- ^ "Study of Monovalent and Bivalent Recombinant Protein Vaccines Against COVID-19 in Adults 18 Years of Age and Older (VAT00008)". ClinicalTrials.gov. 27 May 2021. NCT04904549. Retrieved 28 May 2021.
- ^ "Safety and efficacy of Monovalent and Bivalent Recombinant Protein Vaccines against COVID-19 in Adults 18 Years of Age and Older". ctri.nic.in. Clinical Trials Registry India. CTRI/2021/06/034442. Retrieved 3 August 2021.
- ^ "Study of Recombinant Protein Vaccine with Adjuvant against COVID-19 in Adults 18 Years of Age and Older". pactr.samrc.ac.za. Pan African Clinical Trials Registry. Retrieved 24 March 2021.
- ^ "Tarjeta del participante del estudio VAT00008: ejemplo central para adaptación a nivel de país" [VAT00008 Study Participant Card: Central Example for Country-Level Adaptation] (PDF). incmnsz.mx. Salvador Zubirán National Institute of Health Sciences and Nutrition. 15 April 2021.
- ^ "Study of Recombinant Protein Vaccine Formulations Against COVID-19 in Healthy Adults 18 Years of Age and Older". ClinicalTrials.gov. 3 September 2020. NCT04537208. Retrieved 11 March 2021.
- ^ "Study of Recombinant Protein Vaccine With Adjuvant Against COVID-19 in Adults 18 Years of Age and Older (VAT00002)". ClinicalTrials.gov. 21 February 2021. NCT04762680. Retrieved 11 March 2021.
- ^ "Sanofi and GSK confirm agreement with European Union to supply up to 300 million doses of adjuvanted COVID-19 vaccine". GSK (Press release). Retrieved 1 April 2021.
- ^ https://www.ema.europa.eu/en/human-regulatory/overview/public-health-threats/coronavirus-disease-covid-19/treatments-vaccines/vaccines-covid-19/covid-19-vaccines-under-evaluation
- ^ "Sanofi and GSK sign agreements with the Government of Canada to supply up to 72 million doses of adjuvanted COVID-19 vaccine". GSK (Press release). Retrieved 1 April 2021.
- ^ "U.S. Likely to Get Sanofi Vaccine First If It Succeeds". Bloomberg.com. 13 May 2020. Retrieved 1 April 2021.
- ^ "Coronavirus vaccine: UK signs deal with GSK and Sanofi". BBC News Online. 29 July 2020. Retrieved 1 April 2021.
- ^ a b "Status of COVID-19 Vaccines within WHO EUL/PQ evaluation process". World Health Organization (WHO).
- ^ "VN starts injection of homegrown COVID-19 vaccine in first-stage human trial". Viet Nam News. 17 December 2020.
- ^ "Draft landscape and tracker of COVID-19 candidate vaccines". World Health Organization (WHO). 26 February 2021.
- ^ "How much does first Made-in Vietnam COVID-19 vaccine cost?". Voice of Vietnam. 11 December 2020.
- ^ "Local Nanocovax vaccine's phase 3 trial to begin next week". vietnamnet.vn. 26 May 2021. Retrieved 28 May 2021.
- ^ "Study to Evaluate the Safety, Immunogenicity, and Efficacy of Nanocovax Vaccine Against COVID-19". ClinicalTrials.gov. 11 June 2021. NCT04922788. Retrieved 11 June 2021.
- ^ Le C, Thu A (26 February 2021). "Vietnam enters second phase of Covid-19 vaccine trials". VnExpress.
- ^ Onishi, Tomoya (15 June 2021). "Vietnam homegrown COVID vaccine heads for full approval by year-end". Nikkei Asia.
- ^ "A Study to Evaluate UB-612 COVID-19 Vaccine in Adolescent, Younger and Elderly Adult Volunteers". ClinicalTrials.gov. 26 February 2021. NCT04773067. Retrieved 20 March 2021.
- ^ "A Study to Evaluate the Safety, Immunogenicity, and Efficacy of UB-612 COVID-19 Vaccine". ClinicalTrials.gov. 24 December 2020. NCT04683224. Retrieved 20 March 2021.
- ^ Liao, George (27 June 2021). "Taiwan's second domestic COVID vaccine's midterm performance in phase II trials inferior to local competitor: experts". Taiwan News. Retrieved 8 July 2021.
- ^ "A Study to Evaluate the Safety, Tolerability, and Immunogenicity of UB-612 COVID-19 Vaccine". ClinicalTrials.gov. 11 September 2020. NCT04545749. Retrieved 20 March 2021.
- ^ Strong, Matthew (30 June 2021). "Taiwan's United Biomedical applies for COVID vaccine EUA". Taiwan News.
- ^ "SCB-2019 as COVID-19 Vaccine". ClinicalTrials.gov. 28 May 2020. NCT04405908. Archived from the original on 11 October 2020. Retrieved 14 July 2020.
- ^ "Clover Biopharmaceuticals starts Phase I Covid-19 vaccine trial". Clinical Trials Arena. 20 June 2020. Archived from the original on 11 October 2020. Retrieved 25 June 2020.
- ^ "About Us". Clover Biopharmaceuticals. Archived from the original on 11 October 2020. Retrieved 1 August 2020.
- ^ "A Controlled Phase 2/3 Study of Adjuvanted Recombinant SARS-CoV-2 Trimeric S-protein Vaccine (SCB-2019) for the Prevention of COVID-19 (SCB-2019)". ClinicalTrials.gov. 17 December 2020. NCT04672395. Retrieved 10 March 2021.
- ^ "Clover Biopharmaceuticals and Dynavax Announce First Participants Dosed in SPECTRA, a Global Phase 2/3 Clinical Trial for Adjuvanted S-Trimer COVID-19 Vaccine Candidate". Dynavax. 24 March 2021. Retrieved 7 June 2021.
- ^ "A Study of Safety and Immunogenicity of Adjuvanted SARS-CoV-2 (SCB-2019) Vaccine in Adults With Chronic Immune-Mediated Diseases". ClinicalTrials.gov. 19 August 2021. NCT05012787. Retrieved 19 August 2021.
- ^ "Immunogenicity and Safety Study of Adjuvanted SARS-CoV-2 (SCB-2019) Vaccine in Adults in China". ClinicalTrials.gov. 8 July 2021. NCT04954131. Retrieved 8 July 2021.
- ^ "A Phase 2/3 Study of S-268019". jrct.niph.go.jp. Japan Registry of Clinical Trials. Retrieved 20 October 2021.
- ^ "A Phase 3 Study of S-268019 for the Prevention of COVID-19". ClinicalTrials.gov. 28 January 2022. NCT05212948. Retrieved 28 January 2022.
- ^ "Safety and Immunogenicity of an Intranasal RSV Vaccine Expressing SARS-CoV-2 Spike Protein (COVID-19 Vaccine) in Adults". jrct.niph.go.jp. Japan Registry of Clinical Trials. Retrieved 21 March 2021.
- ^ "A Global Phase III Clinical Trial of Recombinant COVID- 19 Vaccine (Sf9 Cells)". ClinicalTrials.gov. 27 May 2021. NCT04904471. Retrieved 28 May 2021.
- ^ "A global phase III clinical trial of recombinant COVID-19 vaccine (Sf9 cells) in adults aged 18 years and older". chictr.org.cn. 12 May 2021. ChiCTR2100046272. Retrieved 12 May 2021.
- ^ "A global multicenter, randomized, double-blind, placebo-controlled, phase III clinical trial to evaluate the efficacy, safety, and immunogenicity of recombinant COVID-19 vaccine (Sf9 cells), for the prevention of COVID-19 in adults aged 18 years and older". registry.healthresearch.ph. PHRR210712-003704.
- ^ "Phase I Trial of a Recombinant SARS-CoV-2 Vaccine (Sf9 Cell)". ClinicalTrials.gov. 28 August 2020. NCT04530656. Retrieved 20 March 2021.
- ^ "A Phase II Clinical Trial of Recombinant Corona Virus Disease-19 (COVID-19) Vaccine (Sf9 Cells)". ClinicalTrials.gov. 23 November 2020. NCT04640402. Retrieved 20 March 2021.
- ^ "Phase IIb Clinical Trial of Recombinant Novel Coronavirus Pneumonia (COVID-19) Vaccine (Sf9 Cells)". ClinicalTrials.gov. 22 January 2021. NCT04718467. Retrieved 20 March 2021.
- ^ "A Phase III Clinical Trial of Influenza Virus Vector COVID- 19 Vaccine for Intranasal Spray (DelNS1-2019-nCoV-RBD-OPT1)". chictr.org.cn. Chinese Clinical Trial Registry. Retrieved 23 September 2021.
- ^ "A Phase I Clinical Trial of Influenza virus Vector COVID-19 Vaccine for intranasal Spray (DelNS1-2019-nCoV-RBD-OPT1)". chictr.org.cn. Chinese Clinical Trial Registry. Retrieved 24 March 2021.
- ^ "A Phase II Clinical Trial of Influenza virus Vector COVID-19 Vaccine for intranasal Spray (DelNS1-2019-nCoV-RBD-OPT1)". chictr.org.cn. Chinese Clinical Trial Registry. Retrieved 24 March 2021.
- ^ "Entenda ponto a ponto a Versamune, vacina contra a Covid-19 financiada pelo governo federal". G1 Globo. 26 March 2021. Retrieved 19 September 2021.
- ^ "Vacina Versamune: o que se sabe sobre imunizante anunciado pelo governo federal". BBC News Brazil. 26 March 2021. Retrieved 19 September 2021.
- ^ "Vacina Versamune: o que se sabe sobre imunizante anunciado pelo governo federal". BBC News Brazil. 26 March 2021. Retrieved 19 September 2021.
- ^ "Randomized Controlled-trial to Evaluate Safety and Immunogenicity of a Novel Vaccine for Prevention of Covid-19 in Adults Previously Immunized". clinicaltrials.gov. 23 August 2021. NCT05016934. Retrieved 23 August 2021.
- ^ "A Phase I clinical trial to evaluate the safety, tolerance and preliminary immunogenicity of different doses of a SARS-CoV-2 mRNA vaccine in population aged 18–59 years and 60 years and above". Chinese Clinical Trial Register. 24 June 2020. ChiCTR2000034112. Archived from the original on 11 October 2020. Retrieved 6 July 2020.
- ^ "Company introduction". Walvax Biotechnology. Archived from the original on 11 October 2020. Retrieved 1 August 2020.
- ^ "A Phase III Clinical Study to Evaluate the Protective Efficacy, Safety, and Immunogenicity of a SARS-CoV-2 Messenger Ribonucleic Acid (mRNA) Vaccine Candidate in Population Aged 18 Years and Above". chictr.org.cn. Chinese Clinical Trial Registry. Retrieved 17 April 2020.
- ^ "A Global, Multi-center, Randomized, Double-Blind, Placebo-controlled, Phase III Clinical Study to Evaluate the Protective Efficacy, Safety and Immunogenicity of SARS-CoV-2 mRNA Vaccine in Population Aged 18 Years and Older". chictr.org.cn. Chinese Clinical Trial Registry. Retrieved 21 July 2021.
- ^ "A Phase I/II Clinical Trial to Evaluate the Immunogenicity and Safety of the SARS-CoV-2 mRNA Vaccine in Healthy Population Aged 60 Years and Older". chictr.org.cn. Chinese Clinical Trial Registry. Retrieved 2 August 2021.
- ^ "A Phase II clinical trial to evaluate the immunogenicity and safety of different doses of a novel coronavirus pneumonia (COVID-19) mRNA vaccine in population aged 18-59 years". chictr.org.cn. Chinese Clinical Trial Registry. Retrieved 20 March 2021.
- ^ "Recombinant SARS-CoV-2 Fusion Protein Vaccine (V-01) Phase III (COVID-19)". ClinicalTrials.gov. 27 October 2021. NCT05096845. Retrieved 27 October 2021.
- ^ "评价重组新型冠状病毒融合蛋白疫苗在健康人群免疫原性和安全性随机、双盲、安慰剂对照的II期临床试验". chictr.org.cn. Chinese Clinical Trial Registry. Retrieved 21 April 2021.
- ^ "评价重组新型冠状病毒融合蛋白疫苗在健康人群安全性和免疫原性随机、双盲、安慰剂对照的I期临床试验". chictr.org.cn. Chinese Clinical Trial Registry. Retrieved 21 April 2021.
- ^ "Arcturus Therapeutics Collaborates with Vingroup to Establish Manufacturing Facility in Vietnam for Arcturus' Investigational mRNA Vaccines for COVID-19". Business Wire. 2 August 2021.
- ^ "Arcturus Allows Vietnam's Vingroup to Make Covid Vaccines". Bloomberg. 2 August 2021.
- ^ "Vingroup collaborates with Arcturus Therapeutics to establish a manufacturing facility in Vietnam for Arcturus' mRNA Covid-19 vaccine". Yahoo! Finance. 2 August 2021.
- ^ "Arcturus to start clinical trial of COVID-19 vaccine in Vietnam". Reuters. 2 August 2021.
- ^ "Arcturus Therapeutics lines up Phase 1/2/3 trial for next-generation mRNA COVID-19 vaccine". Biopharma Reporter. 2 August 2021.
- ^ "The ARCT-154 Self-Amplifying RNA Vaccine Efficacy Study (ARCT-154-01) (ARCT-154-01)". United States National Library of Medicine. 19 August 2021. NCT05012943. Retrieved 19 August 2021.
- ^ "Efficacy, Safety, and Immunogenicity Study of the Recombinant Two-component COVID-19 Vaccine (CHO Cell) (ReCOV)". ClinicalTrials.gov. 20 October 2021. NCT05084989. Retrieved 20 October 2021.
- ^ "Safety, Reactogenicity and Immunogenicity Study of ReCOV". ClinicalTrials.gov. 26 March 2021. NCT04818801. Retrieved 2 April 2021.
- ^ "A Phase I/II Randomized, Multi-Center, Placebo-Controlled, Dose-Escalation Study to Evaluate the Safety, Immunogenicity and Potential Efficacy of an rVSV-SARS-CoV-2-S Vaccine (IIBR-100) in Adults". ClinicalTrials.gov. 1 November 2020. NCT04608305.
- ^ "Phase 2b Dose-confirmatory Trial to Evaluate the Safety, Immunogenicity and Potential Efficacy of an VSV-ΔG SARS-CoV-2 Vaccine (BRILIFE001)". ClinicalTrials.gov. 29 July 2021. NCT04990466. Retrieved 13 September 2021.
- ^ "As Israel goes vaccine-wild, will the homegrown version lose its shot?". The Times of Israel. 29 December 2020. Retrieved 1 January 2021.
- ^ "Efficacy, safety and immunogenicity of a recombinant protein subunit vaccine (CHO cells) against COVID-19 in adults: an international multicenter, randomized, double-blind, placebo-controlled phase III study". chictr.org.cn. Chinese Clinical Trial Registry. 5 September 2021. ChiCTR2100050849. Retrieved 5 September 2021.
- ^ "Phase I Trial of a Recombinant COVID-19 Vaccine (CHO Cell)". ClinicalTrials.gov. United States National Library of Medicine. 19 November 2020. NCT04636333. Retrieved 13 April 2021.
- ^ "Immunogenicity and Safety of Recombinant COVID-19 Vaccine (CHO Cells)". ClinicalTrials.gov. United States National Library of Medicine. 24 March 2021. NCT04813562. Retrieved 13 April 2021.
- ^ "Safety and Immunogenicity Study of GX-19, a COVID-19 Preventive DNA Vaccine in Healthy Adults". ClinicalTrials.gov. 24 June 2020. NCT04445389. Archived from the original on 11 October 2020. Retrieved 14 July 2020.
- ^ "Safety and Immunogenicity Study of GX-19N, a COVID-19 Preventive DNA Vaccine in Healthy Adults". ClinicalTrials.gov. 20 January 2021. NCT04715997. Retrieved 16 March 2021.
- ^ "S. Korea's Genexine begins human trial of coronavirus vaccine". Reuters. 19 June 2020. Archived from the original on 11 October 2020. Retrieved 25 June 2020.
- ^ "Genexine consortium's Covid-19 vaccine acquires approval for clinical trails in Korea". 11 June 2020. Retrieved 1 August 2020.
- ^ "Safety and Immunogenicity of GX-19N, a COVID-19 Preventive DNA Vaccine in Elderly Individuals". ClinicalTrials.gov. 7 June 2021. NCT04915989. Retrieved 8 June 2021.
- ^ "Evaluation of Efficacy, Safety and Immunogenicity of GX-19N in Healthy Individuals Who Have Received COVID-19 Vaccines". ClinicalTrials.gov. 5 October 2021. NCT05067946. Retrieved 5 October 2021.
- ^ "GRAd-COV2 Vaccine Against COVID-19". ClinicalTrials.gov. 27 August 2020. NCT04528641.
- ^ "ReiThera Announces its GRAd-COV2 COVID-19 Vaccine Candidate is Well Tolerated and Induces Clear Immune Responses in Healthy Subjects Aged 18–55 Years". ReiThera Srl. Yahoo! Finance. 24 November 2020. Retrieved 12 January 2021.
- ^ "Study of GRAd-COV2 for the Prevention of COVID-19 in Adults (COVITAR)". ClinicalTrials.gov. 10 March 2021. NCT04791423. Retrieved 20 March 2021.
- ^ "ReiThera's COVID-19 vaccine candidate enters Phase 2/3 clinical study". ReiThera. 18 March 2021. Retrieved 20 March 2021.
- ^ "New ReiThera vaccine safe, response peak at 4 wks". ANSA. 5 January 2021.
- ^ "Safety, Tolerability and Immunogenicity of INO-4800 for COVID-19 in Healthy Volunteers". ClinicalTrials.gov. 7 April 2020. NCT04336410. Archived from the original on 11 October 2020. Retrieved 14 July 2020.
- ^ "IVI, INOVIO, and KNIH to partner with CEPI in a Phase I/II clinical trial of INOVIO's COVID-19 DNA vaccine in South Korea". International Vaccine Institute. 16 April 2020. Retrieved 23 April 2020.
- ^ "Safety, Immunogenicity, and Efficacy of INO-4800 for COVID-19 in Healthy Seronegative Adults at High Risk of SARS-CoV-2 Exposure". ClinicalTrials.gov. 24 November 2020. NCT04642638. Retrieved 12 March 2021.
- ^ "Safety, Tolerability and Immunogenicity of INO-4800 Followed by Electroporation in Healthy Volunteers for COVID19". United States National Library of Medincine. Retrieved 12 March 2021.
- ^ "A Phase II, Randomized, Double-Blinded, Placebo-Controlled, Dose-Finding Clinical Trial to Evaluate the Safety and Immunogenicity of Different Doses of COVID-19 DNA Vaccine INO-4800 Administered Intradermally Followed by Electroporation in Healthy Adult and Elderly Volunteers". chictr.org.cn. Chinese Clinical Trial Registry. Retrieved 27 March 2021.
- ^ "Daiichi Sankyo Initiates Phase 1/2 Clinical Trial for mRNA COVID-19 vaccine in Japan" (PDF) (Press release). Daiichi Sankyo. Retrieved 17 April 2021.
- ^ "Daiichi takes mRNA COVID-19 vaccine into clinic as Japanese R&D belatedly fires up". Fierce Biotech. 22 March 2021. Retrieved 12 April 2021.
- ^ "既承認SARS-CoV-2 ワクチンの初回接種完了者を対象としたDS-5670a による追加免疫効果を検討する第I/II/III 相、無作為化、実薬対照、評価者盲検試験". jrct.niph.go.jp. 28 December 2021. jRCT2071210106. Retrieved 28 December 2021.
- ^ "Study of DS-5670a (COVID-19 Vaccine) in Japanese Healthy Adults and Elderly Subjects". ClinicalTrials.gov. 29 March 2021. NCT04821674. Retrieved 12 April 2021.
- ^ "SK Bioscience Submitted Phase 3 IND for COVID-19 Vaccine". SK Bioscience.
- ^ "A Phase III Study to Assess the Immunogenicity and Safety of SK SARS-CoV-2 Recombinant Nanoparticle Vaccine Adjuvanted With AS03 (GBP510) in Adults Aged 18 Years and Older". ClinicalTrials.gov. 17 August 2021. NCT05007951. Retrieved 17 August 2021.
- ^ "Safety and Immunogenicity Study of SARS-CoV-2 Nanoparticle Vaccine (GBP510) Adjuvanted With or Without AS03 (COVID-19)". ClinicalTrials.gov. 11 February 2021. NCT04750343. Retrieved 22 April 2021.
- ^ "Safety and Immunogenicity Study of SARS-CoV-2 Nanoparticle Vaccine (GBP510) Adjuvanted With Aluminum Hydroxide (COVID-19)". ClinicalTrials.gov. 8 February 2021. NCT04742738. Retrieved 22 April 2021.
- ^ "Indigenous mRNA vaccine candidate supported by DBT gets Drug Controller nod to initiate Human clinical trials" (Press release). Press Information Bureau. Retrieved 13 January 2021.
- ^ "mRNA Vaccines – HGC019". Gennova Biopharmaceuticals Limited. Retrieved 13 January 2021.
- ^ "Safety and immunogenicity study of an mRNA based vaccine (HGCO19) for COVID19 in healthy adult participants". ctri.nic.in. Clinical Trials Registry India. Retrieved 9 September 2021.
- ^ Raghavan P (15 December 2020). "Pune-based Gennova to begin human trials of its Covid vaccine 'soon'". The Indian Express.
- ^ "Safety and immunogenicity study of mRNA based vaccine (HGCO19) against COVID-19 in healthy adult participants". ctri.nic.in. Clinical Trials Registry India. Retrieved 5 June 2021.
- ^ "Safety and immunogenicity study of mRNA based vaccine (HGCO19) against COVID-19 in healthy adult participants". Cochrane COVID-19 Study Register. 2021-08-04. Archived from the original on 2021-09-11.
- ^ "18歳以上の健康な日本人を対象に、COVID-19に対するワクチン(KD-414)を2回接種した際の免疫原性及び安全性を確認する多施設共同非盲検非対照試験。". jrct.niph.go.jp. Japan Registry of Clinical Trials. Retrieved 22 October 2021.
- ^ "Japan's KM Biologics begins clinical trial of COVID-19 vaccine candidate". Reuters. 22 March 2021.
- ^ "20歳以上65歳未満の健康成人、及び65歳以上の健康な高齢者を対象に、COVID-19に対するワクチン(KD-414)の安全性及び免疫原性を検討するための、プラセボを対照とする多施設共同二重盲検ランダム化並行群間比較試験". jrct.niph.go.jp. Japan Registry of Clinical Trials. Retrieved 7 May 2021.
- ^ "Phase Ⅱ and Ⅲ Trial of a SARS-CoV-2 Vaccine LYB001". ClinicalTrials.gov. 30 November 2021. NCT05137444. Retrieved 30 November 2021.
- ^ "A Phase Ⅰ Trial to Evaluate the Safety and Immunogenicity of SARS-CoV-2 Vaccine LYB001". ClinicalTrials.gov. 18 November 2021. NCT05125926. Retrieved 18 November 2021.
- ^ "Immunogenicity and safety of a SARS-CoV-2 Vaccine LYB001 against COVID-19 in healthy adults: a randomized, double blinded, placebo-controlled phase II trial and a single-armed, open-label expanded safety phase III trial". chictr.org.cn. Chinese Clinical Trial Registry. Retrieved 15 October 2021.
- ^ "Safety, Reactogenicity, and Immunogenicity of a Recombinant SARS-CoV-2 Vaccine LYB001 in healthy adults: a randomized, double blinded, placebo-controlled phase I trial". chictr.org.cn. Chinese Clinical Trial Registry. Retrieved 15 October 2021.
- ^ "A study to assess the safety and immunogenicity of Anti-COVID-19 AKS-452 vaccine for SARS-Сov-2 infection in Indian healthy subjects". ctri.nic.in. 11 October 2021. CTRI/2021/10/037269. Retrieved 11 October 2021.
- ^ "Anti-COVID19 AKS-452 – ACT Study (ACT)". ClinicalTrials.gov. 23 December 2020. NCT04681092. Retrieved 21 March 2021.
- ^ "Study of COVID-19 DNA Vaccine (AG0301-COVID19)". ClinicalTrials.gov. 9 July 2020. NCT04463472. Archived from the original on 11 October 2020. Retrieved 14 July 2020.
- ^ "Study of COVID-19 DNA Vaccine (AG0302-COVID19)". ClinicalTrials.gov. 26 August 2020. NCT04527081. Retrieved 11 March 2021.
- ^ "About AnGes – Introduction". AnGes, Inc. Archived from the original on 11 October 2020. Retrieved 1 August 2020.
- ^ "Phase II / III Study of COVID-19 DNA Vaccine (AG0302-COVID19)". ClinicalTrials.gov. 7 December 2020. NCT04655625. Retrieved 11 March 2021.
- ^ "Phase II Clinical Trial of Recombinant SARS-CoV-2 Spike Protein Vaccine (CHO Cell)". ClinicalTrials.gov. 4 August 2021. NCT04990544. Retrieved 4 August 2021.
- ^ "Phase I Clinical Trial of Recombinant SARS-CoV-2 Spike Protein Vaccine (CHO Cell)". ClinicalTrials.gov. 4 July 2021. NCT04982068. Retrieved 29 July 2021.
- ^ "A Ph 2 Trial With an Oral Tableted COVID-19 Vaccine". ClinicalTrials.gov. 5 October 2021. NCT05067933. Retrieved 5 October 2021.
- ^ "Safety and Immunogenicity Trial of an Oral SARS-CoV-2 Vaccine (VXA-CoV2-1) for Prevention of COVID-19 in Healthy Adults". ClinicalTrials.gov. 24 September 2020. NCT04563702. Retrieved 22 March 2021.
- ^ "Ph 1b: Safety & Immunogenicity of Ad5 Based Oral Norovirus Vaccine (VXA-NVV-104)". ClinicalTrials.gov. 22 April 2021. NCT04854746. Retrieved 25 May 2021.
- ^ a b "Made-in-Canada coronavirus vaccine starts human clinical trials". Canadian Broadcasting Corporation. 26 January 2021.
- ^ "PTX-COVID19-B, an mRNA Humoral Vaccine, Intended for Prevention of COVID-19 in a General Population. This Study is Designed to Demonstrate the Safety, Tolerability, and Immunogenicity of PTX-COVID19-B in Comparison to the Pfizer-BioNTech COVID-19 Vaccine". ClinicalTrials.gov. 4 January 2022. NCT05175742. Retrieved 6 January 2022.
- ^ "PTX-COVID19-B, an mRNA Humoral Vaccine, is Intended for Prevention of COVID-19 in a General Population. This Study is Designed to Evaluate Safety, Tolerability, and Immunogenicity of PTX-COVID19-B Vaccine in Healthy Seronegative Adults Aged 18-64". ClinicalTrials.gov. 21 February 2021. NCT04765436. Retrieved 22 April 2021.
- ^ "Randomized, double-blind, placebo-controlled phase II clinical trial of immunogenicity, immunopersistence, and safety of graded Novel Coronavirus inactivated vaccine (Vero cells) in healthy persons aged 18 years and older". chictr.org.cn. 29 September 2021. ChiCTR2100050024. Retrieved 3 October 2021.
- ^ "A randomized, double-blind, placebo-controlled phase I clinical trial to evaluate the safety and immunogenicity of the Novel Coronavirus inactivated vaccine (Vero cells) in healthy individuals 18 years of age and older". chictr.org.cn. 16 August 2021. ChiCTR2100050024. Retrieved 16 August 2021.
- ^ "Another Chinese adenovirus vector COVID-19 vaccine ready for human trials". Xinhua. 28 December 2020. Retrieved 27 July 2021.
- ^ "A Phase II Clinical Trial of the Recombinant SARS-CoV-2 Vaccine (Chimpanzee Adenoviral Vector)". chictr.org.cn. 2 August 2021. ChiCTR2100049530. Retrieved 2 August 2021.
- ^ "Phase I Clinical Trial of the Candidate Recombinant SARS-CoV-2 Vaccine (Chimpanzee Adenoviral Vector)". chictr.org.cn. 23 May 2021. ChiCTR2100046612. Retrieved 23 May 2021.
- ^ "INNA-051 intranasal safety and tolerability study". clinicaltrials.gov. 12 November 2021. NCT05118763. Retrieved 12 November 2021.
- ^ "INNA-051 intranasal safety and tolerability study". anzctr.org.au. 21 April 2021. ACTRN12621000607875p. Retrieved 20 May 2021.
- ^ "A Study to Evaluate the Immunogenicity and Safety of mRNA-1283 COVID-19 Vaccine Boosters". ClinicalTrials.gov. 30 November 2021. NCT05137236. Retrieved 30 November 2021.
- ^ "A Study to Evaluate Safety, Reactogenicity, and Immunogenicity of mRNA-1283 and mRNA-1273 Vaccines in Healthy Adults Between 18 Years and 55 Years of Age to Prevent COVID-19". ClinicalTrials.gov. 24 March 2021. NCT04813796. Retrieved 17 August 2021.
- ^ "Study of a Severe Acute Respiratory Syndrome Coronavirus-2 (SARS-CoV-2) Virus-like Particle (VLP) Vaccine (COVID-19)". ClinicalTrials.gov. 15 July 2021. NCT04962893. Retrieved 15 July 2021.
- ^ "Study of a Severe Acute Respiratory Syndrome CoV-2 (SARS-CoV-2) Virus-like Particle (VLP) Vaccine in Healthy Adults (COVID-19)". ClinicalTrials.gov. 26 March 2021. NCT04818281. Retrieved 3 April 2021.
- ^ "SARS-CoV-2 Vaccine (COH04S1) Versus Emergency Use Authorization SARS-COV-2 Vaccine for the Treatment of COVID-19 in Patients With Blood Cancer". ClinicalTrials.gov. 26 July 2021. NCT04977024. Retrieved 26 July 2021.
- ^ "A Synthetic MVA-based SARS-CoV-2 Vaccine, COH04S1, for the Prevention of COVID-19". ClinicalTrials.gov. 20 November 2020. NCT04639466. Retrieved 21 March 2021.
- ^ "Bavarian Nordic reports encouraging preclinical data for COVID-19 vaccine candidate ahead of first-in-human trial". Bavarian Nordic. 8 March 2021. Retrieved 13 April 2021.
- ^ "Bavarian Nordic Initiates Phase 2 Clinical Trial of COVID-19 Booster Vaccine". Bavarian Nordic. 23 August 2021. Retrieved 24 August 2021.
- ^ "ABNCoV2 Vaccine in SARS-CoV-2 Seronegative and Seropositive Adult Subjects". ClinicalTrials.gov. 14 October 2021. NCT05077267. Retrieved 14 October 2021.
- ^ "Safety and Tolerability of ABNCoV2 (COUGH-1)". ClinicalTrials.gov. 9 April 2021. NCT04839146. Retrieved 13 April 2021.
- ^ "Clover Announces Positive Preclinical Data for Second-Generation Protein-Based COVID-19 Vaccine Candidate Demonstrating Broad Neutralization Against Variants of Concern". Clover Biopharmaceutical. 18 May 2021. Retrieved 9 July 2021.
- ^ "Immunogenicity and Safety of Adjuvanted SCB-2020S Vaccines in Adults". United States National Library of Medicine. 6 July 2021. NCT04950751. Retrieved 6 July 2021.
- ^ "The Safety and Efficacy of SCTV01C in Population Aged ≥18 Years Previously Vaccinated With Inactivated COVID-19 Vaccine.Healthy Population Aged ≥18 Years Previously Vaccinated With Adenovirus Vectored or mRNA COVID-19 Vaccine". United States National Library of Medicine. 14 September 2021. NCT05043311. Retrieved 14 September 2021.
- ^ "The Safety and Efficacy of SCTV01C in Population Aged ≥18 Years Previously Vaccinated With Inactivated COVID-19 Vaccine.Healthy Population Aged ≥18 Years Previously Vaccinated With Inactivated COVID-19 Vaccine". United States National Library of Medicine. 14 September 2021. NCT05043285. Retrieved 14 September 2021.
- ^ "Safety, Tolerability and Immunogenicity of SCTV01C in Healthy Population Aged ≥18 Years Previously Unvaccinated". United States National Library of Medicine. 8 December 2021. NCT05148091. Retrieved 8 December 2021.
- ^ "A Phase 1/2 Safety and Immunogenicity Trial of COVID-19 Vaccine COVIVAC". ClinicalTrials.gov. 5 April 2021. NCT04830800. Retrieved 13 April 2021.
- ^ "A Live Recombinant Newcastle Disease Virus-vectored COVID-19 Vaccine Phase 1 Study". ClinicalTrials.gov. 25 January 2022. NCT05205746. Retrieved 25 January 2022.
- ^ "Assess the Safety and Immunogenicity of NDV-HXP-S Vaccine in Thailand". ClinicalTrials.gov. 21 February 2021. NCT04764422. Retrieved 7 April 2021.
- ^ "A Live Recombinant Newcastle Disease Virus-vectored COVID-19 Vaccine Phase 1 Study". ClinicalTrials.gov. 6 January 2022. NCT05181709. Retrieved 6 January 2022.
- ^ "Vaccine COVID-19 "made in Vietnam" COVIVAC thử nghiệm giai đoạn 2". VTV. 10 August 2021. Retrieved 12 August 2021.
- ^ Zimmer, Carl (5 April 2021). "Researchers Are Hatching a Low-Cost Coronavirus Vaccine". The New York Times. Retrieved 7 April 2021.
- ^ "Randomized, double-blind, placebo-controlled phase I clinical trial to evaluate the safety and immunogenicity of mRNACOVID-19 vaccine in healthy susceptible populations aged 18 years and older people". Chinese Clinical Trial Registry (ChiCTR). Retrieved 15 May 2021.
- ^ "A Phase I/II Clinical Trial in Healthy People Aged 18 Years and Above". ClinicalTrials.gov. 3 December 2021. NCT05144139. Retrieved 3 December 2021.
- ^ "CTI and Arcturus Therapeutics Announce Initiation of Dosing of COVID-19 STARR mRNA Vaccine Candidate, LUNAR-COV19 (ARCT-021) in a Phase 1/2 study". UK BioIndustry Association. 13 August 2020. Archived from the original on 11 October 2020. Retrieved 23 August 2020.
- ^ "Ascending Dose Study of Investigational SARS-CoV-2 Vaccine ARCT-021 in Healthy Adult Subjects". Archived from the original on 11 October 2020. Retrieved 23 August 2020.
- ^ "A Trial Evaluating the Safety and Effects of an RNA Vaccine ARCT-021 in Healthy Adults". ClinicalTrials.gov. 16 December 2020. NCT04668339. Retrieved 10 March 2021.
- ^ "Open Label Extension Study to Assess the Safety and Long-Term Immunogenicity of ARCT-021". ClinicalTrials.gov. 28 January 2021. NCT04728347. Retrieved 13 March 2021.
- ^ "Phase I/II of the Safety and Immunogenicity of SARS-CoV-2 Protein Subunit Recombinant Vaccine in Healthy Populations". ClinicalTrials.gov. 5 October 2021. NCT05067894. Retrieved 5 October 2021.
- ^ "VBI Vaccines Announces Initiation of Enrollment in Adaptive Phase 1/2 Study of Prophylactic COVID-19 Vaccine Candidate, VBI-2902". VBI Vaccines (Press release). 9 March 2021. Retrieved 22 March 2021.
- ^ "Safety, Tolerability, and Immunogenicity of the COVID-19 Vaccine Candidates VBI-2902a and VBI-2905a". ClinicalTrials.gov. 26 February 2021. NCT04773665. Retrieved 8 October 2021.
- ^ "Novavax Announces Positive Preclinical Data for Combination Influenza and COVID-19 Vaccine Candidate". Novavax. 10 May 2021.
- ^ "Evaluation of the Safety and Immunogenicity of Influenza and COVID-19 Combination Vaccine". ClinicalTrials.gov. 14 July 2021. NCT04961541. Retrieved 26 July 2021.
- ^ "Safety, Tolerance and Immunogenicity of EuCorVac-19 for the Prevention of COVID-19 in Healthy Adults". ClinicalTrials.gov. 5 March 2021. NCT04783311. Retrieved 20 March 2021.
- ^ Limon, Raul (12 August 2021). "First Spanish Covid-19 vaccine approved for human clinical trial". El Pais. Retrieved 15 August 2021.
- ^ "Safety and Immunogenicity Study of Recombinant Protein RBD Candidate Vaccine Against SARS-CoV-2 in Adult Healthy Volunteers (COVID-19)". clinicaltrials.gov. 16 August 2021. NCT05007509. Retrieved 16 August 2021.
- ^ "Safety and Immunogenicity of Recombinant Protein RBD Fusion Dimer Vaccine Against the Virus That Cause COVID-19, Known as Severe Acute Respiratoy Syndrome Coronavirus 2 (SARS-CoV-2)". clinicaltrials.gov. 2 December 2021. NCT05142514. Retrieved 2 December 2021.
- ^ "Trial registered on ANZCTR". anzctr.org.au. Australian New Zealand Clinical Trials Registry. Retrieved 24 March 2021.
- ^ "Phase I-II Trial of Dendritic Cell Vaccine to Prevent COVID-19 in Adults". ClinicalTrials.gov. 13 May 2020. NCT04386252. Retrieved 23 March 2021.
- ^ "Dendritic Cell Vaccine to Prevent COVID-19". ClinicalTrials.gov. 28 December 2020. NCT04685603. Retrieved 23 March 2021.
- ^ "Safety and Immunogenicity of COVID-eVax, a Candidate Plasmid DNA Vaccine for COVID-19, in Healthy Adult Volunteers". ClinicalTrials.gov. 9 March 2021. NCT04788459. Retrieved 21 March 2021.
- ^ a b "Safety and Immunogenicity of an Intranasal SARS-CoV-2 Vaccine (BBV154) for COVID-19". ClinicalTrials.gov. 12 February 2021. NCT04751682. Archived from the original on 24 February 2021.
- ^ "Intranasal Vaccine For Covid-19". Bharat Biotech. Retrieved 5 March 2021.
- ^ Gaurav, Kunal (13 August 2021). "First nasal vaccine developed by Bharat Biotech gets nod for Phase 2/3 trial". Hindustan Times.
- ^ "Intranasal COVID-19 vaccine Phase 2 study in Healthy volunteers". ctri.nic.in. Clinical Trials Registry India. Retrieved 3 September 2021.
- ^ "Vaccibody reports promising preclinical data with a second-generation COVID-19 vaccine and announces its infectious disease strategy" (PDF). vaccibody.com. 10 December 2020.
- ^ "Vaccibody reports promising preclinical data with a second-generation COVID-19 vaccine and announces its infectious disease strategy" (PDF). vaccibody.com. 10 December 2020.
- ^ "Vaccibody to initiate a phase 1/2 trial to evaluate two second-generation SARS CoV-2 virus DNA vaccine candidates to address emerging variants of concern" (PDF). vaccibody.com. 29 June 2021.
- ^ "A Phase 1/2, Dose Escalation Study to Determine Safety and Immunogenicity of Two COVID 19 Vaccines VB10.2129 (RBD Candidate) and VB10.2210 (T Cell Candidate) in Healthy Adult Volunteers". ClinicalTrials.gov. 6 October 2021. NCT05069623. Retrieved 6 October 2021.
- ^ "ChulaCov19 mRNA Vaccine in Healthy Adults". ClinicalTrials.gov. 28 September 2020. NCT04566276. Retrieved 21 March 2021.
- ^ a b "Safety and Immunity of Covid-19 aAPC Vaccine". ClinicalTrials.gov. 9 March 2020. NCT04299724. Archived from the original on 11 October 2020. Retrieved 14 July 2020.
- ^ a b "About Us". Shenzhen Genoimmune Medical Institute. Archived from the original on 11 October 2020. Retrieved 1 August 2020.
- ^ a b "Immunity and Safety of Covid-19 Synthetic Minigene Vaccine". ClinicalTrials.gov. 19 February 2020. NCT04276896. Archived from the original on 11 October 2020. Retrieved 14 July 2020.
- ^ "COVID-19 Vaccination Using a 2nd Generation (E1/E2B/E3-Deleted) Adenoviral Platform in Healthy South African Adults". ClinicalTrials.gov. 14 January 2021. NCT04710303. Retrieved 23 March 2021.
- ^ "COVID-19 Oral and Subcutaneous Vaccination Using a 2nd Generation (E1/E2B/E3-Deleted) Adenovirus Platform in Healthy Volunteers in USA". ClinicalTrials.gov. 1 February 2021. NCT04732468. Retrieved 23 March 2021.
- ^ "COVID-19 Vaccination Using a 2nd Generation (E1/E2B/E3-Deleted) Adenoviral-COVID-19 in Normal Healthy Volunteers". ClinicalTrials.gov. 19 October 2020. NCT04591717. Retrieved 23 March 2021.
- ^ "COVID-19 Subcutaneously and Orally Administered Supplemental Vaccine Boost to Enhance T Cell Protection in Those Who Have Already Received EUA S-Based Vaccines". ClinicalTrials.gov. 14 April 2021. NCT04845191. Retrieved 22 April 2021.
- ^ "COVID-19 Supplemental Vaccine Boost to Enhance T Cell Protection in Those Who Have Already Received EUA S-Based Vaccines". ClinicalTrials.gov. 13 April 2021. NCT04843722. Retrieved 22 April 2021.
- ^ a b "VIDO COVID-19 vaccine moves to Phase 1 clinical testing". globalnews.ca. 10 February 2021.
- ^ "A Clinical Trial of COVAC-2 in Healthy Adults". ClinicalTrials.gov. 8 January 2021. NCT04702178. Retrieved 20 April 2021.
- ^ "A Clinical Trial of COVAC-1 in Generally Healthy Adults". ClinicalTrials.gov. 14 December 2021. NCT05155982. Retrieved 14 December 2021.
- ^ "Serum Institute starts manufacturing Codagenix's nasal COVID-19 vaccine". mint. 22 September 2020.
- ^ "Safety and Immunogenicity of COVI-VAC, a Live Attenuated Vaccine Against COVID-19". ClinicalTrials.gov. 6 November 2020. NCT04619628.
- ^ "A Study of the Safety of and Immune Response to Varying Doses of a Vaccine Against COVID-19 in Healthy Adults". ClinicalTrials.gov. 17 February 2021. NCT04758962.
- ^ "COVALIA study update: first healthy volunteers dosed in needle-free SARS-CoV2 DNA vaccine phase 1 trial". Bionet Asia. 30 June 2021. Retrieved 19 July 2021.
- ^ "The Safety and Immunogenicity of a DNA-based Vaccine (COVIGEN) in Healthy Volunteers (COVALIA)". ClinicalTrials.gov. 8 February 2021. NCT04742842.
- ^ "Meissa Announces IND Clearance for Phase 1 Study of Intranasal Live Attenuated Vaccine Candidate for COVID-19". Business Wire. 16 March 2021. Retrieved 20 March 2021.
- ^ "Safety and Immunogenicity of an Intranasal RSV Vaccine Expressing SARS-CoV-2 Spike Protein (COVID-19 Vaccine) in Adults". ClinicalTrials.gov. 15 March 2021. NCT04798001. Retrieved 20 March 2021.
- ^ "KBP-201 COVID-19 Vaccine Trial in Healthy Volunteers". ClinicalTrials.gov. 16 July 2020. NCT04473690. Retrieved 21 March 2021.
- ^ "Safety and Immunogenicity Study of AdCLD-CoV19: A COVID-19 Preventive Vaccine in Healthy Volunteers". ClinicalTrials.gov. 14 December 2020. NCT04666012. Retrieved 23 March 2021.
- ^ "A Study to Evaluate the Safety and Immunogenicity of COVID-19 (AdimrSC-2f) Vaccine". ClinicalTrials.gov. 21 August 2020. NCT04522089. Retrieved 21 March 2021.
- ^ "Dose-finding Study for AdimrSC-2f Vaccine". ClinicalTrials.gov. 3 November 2021. NCT05104489. Retrieved 3 November 2021.
- ^ "GLS-5310 Vaccine for the Prevention of SARS-CoV-2 (COVID-19)". ClinicalTrials.gov. 17 December 2020. NCT04673149. Retrieved 21 March 2021.
- ^ "A Clinical Trial of a Plasmid DNA Vaccine for COVID-19 [Covigenix VAX-001] in Adults". ClinicalTrials.gov. 19 October 2020. NCT04591184. Retrieved 21 March 2021.
- ^ "Safety and Immunogenicity of a SARS-CoV-2 Vaccine (NBP2001) in Healthy Adults (COVID-19)". ClinicalTrials.gov. 18 February 2021. NCT04760743. Retrieved 21 March 2021.
- ^ "Safety and Immunogenicity Trial of Multi-peptide Vaccination to Prevent COVID-19 Infection in Adults (pVAC)". ClinicalTrials.gov. 14 September 2020. NCT04546841. Retrieved 21 March 2021.
- ^ "B-pVAC-SARS-CoV-2: Study to Prevent COVID-19 Infection in Adults With Bcell/ Antibody Deficiency (B-pVAC)". ClinicalTrials.gov. 8 July 2020. NCT04954469. Retrieved 8 July 2021.
- ^ "Evaluating the Safety, Tolerability and Immunogenicity of bacTRL-Spike Vaccine for Prevention of COVID-19". ClinicalTrials.gov. 6 April 2020. NCT04334980. Retrieved 21 March 2021.
- ^ "Chimpanzee Adenovirus and Self-Amplifying mRNA Prime-Boost Prophylactic Vaccines Against SARS-CoV-2 in Healthy Adults". ClinicalTrials.gov. 1 March 2021. NCT04776317. Retrieved 22 March 2021.
- ^ "SARS-COV-2-Spike-Ferritin-Nanoparticle (SpFN) Vaccine With ALFQ Adjuvant for Prevention of COVID-19 in Healthy Adults". ClinicalTrials.gov. 5 March 2021. NCT04784767. Retrieved 24 March 2021.
- ^ "Safety, Tolerability and Immunogenicity of the Candidate Vaccine MVA-SARS-2-S Against COVID-19". ClinicalTrials.gov. 29 September 2020. NCT04569383. Retrieved 24 March 2021.
- ^ "Safety, Tolerability and Immunogenicity of the Candidate Vaccine MVA-SARS-2-ST Against COVID-19 (MVA-SARS-2-ST)". ClinicalTrials.gov. 20 May 2021. NCT04895449. Retrieved 21 May 2021.
- ^ "Safety and Immunogenicity of the Inactivated Koçak-19 Inaktif Adjuvanlı COVID-19 Vaccine Compared to Placebo". ClinicalTrials.gov. 8 April 2021. NCT04838080. Retrieved 3 April 2021.
- ^ "First-In-Human Study Of Orally Administered CoV2-OGEN1 In Healthy Subjects". ClinicalTrials.gov. 19 May 2021. NCT04893512. Retrieved 26 May 2021.
- ^ "OSE Immunotherapeutics Receives Authorization for Phase 1 Clinical Trial of its Multi-Target Multi-Variant COVID-19 Vaccine". BioSpace. 1 April 2021. Retrieved 13 April 2021.
- ^ "To Evaluate the Safety, and Immunogenicity of Vaccine Candidate Against COVID-19, in Healthy Adults (COVEPIT 3)". ClinicalTrials.gov. 13 May 2021. NCT04885361. Retrieved 13 May 2021.
- ^ "HDT Bio Receives Notice to Proceed from FDA for US Phase 1 Clinical Trial of RNA COVID-19 Vaccine". HDT Bio. 1 July 2021. Retrieved 24 December 2021.
- ^ "HDT Bio Partner Quratis Doses First Healthy Volunteers in Phase 1 Trial of HDT Bio's RNA COVID-19 Vaccine in South Korea". HDT Bio. 13 December 2021. Retrieved 24 December 2021.
- ^ "Phase 1 Study to Assess Safety, Reactogenicity and Immunogenicity of the HDT-301 Vaccine Against COVID-19". ClinicalTrials.gov. 14 April 2021. NCT04844268. Retrieved 4 August 2021.
- ^ "Safety And Immunogenicity Of HDT-301 Targeting A SARS-CoV-2 Variant Spike Protein". ClinicalTrials.gov. 24 November 2021. NCT05132907. Retrieved 24 November 2021.
- ^ "A Phase 1, First-In-Human Study of the Investigational COVID-19 Vaccine SC-Ad6-1 in Healthy Volunteers". ClinicalTrials.gov. 9 April 2021. NCT04839042. Retrieved 17 April 2021.
- ^ "Study of a Severe Acute Respiratory Syndrome-Coronavirus-2 (SARS-CoV-2) Adjuvanted Inactivated Vaccine in Healthy Adults (COVID-19)". ClinicalTrials.gov. 29 April 2021. NCT04866069. Retrieved 30 April 2021.
- ^ "Safety and Immunogenicity of EXG-5003". ClinicalTrials.gov. 28 April 2021. NCT04863131. Retrieved 2 May 2021.
- ^ "Icosavax Initiates Phase 1/2 Trial of COVID-19 VLP Vaccine Candidate". Icosavax. 8 June 2021.
- ^ "A Study to Evaluate the Safety and Immunogenicity of COVID-19 Vaccine (IVX-411) in Healthy Adults". Australian New Zealand Clinical Trials Registry. Retrieved 14 June 2021.
- ^ "НАЧАТЫ КЛИНИЧЕСКИЕ ИССЛЕДОВАНИЯ СУБЪЕДИНИЧНОЙ ВАКЦИНЫ ПРОТИВ COVID-19, РАЗРАБОТАННОЙ УЧЁНЫМИ НИИПББ". Biosafty and Biotechnology Journal. 15 June 2021.
- ^ "Reactogenicity, Safety and Immunogenicity of QazCoVac-P COVID-19 Vaccine". ClinicalTrials.gov. 18 June 2021. NCT04930003. Retrieved 22 June 2021.
- ^ "Safety and Immunogenicity of LNP-nCOV saRNA-02 Vaccine Against SARS-CoV-2, the Causative Agent of COVID-19 (COVAC-Uganda)". ClinicalTrials.gov. 22 June 2021. NCT04934111. Retrieved 22 June 2021.
- ^ Rujivanarom, Pratch (6 June 2021). "Local jabs yet to join Covid fight". Bangkok Post. Retrieved 8 July 2021.
- ^ "A Study to Evaluate Safety, Tolerability, and Reactogenicity of an RBD-Fc-based Vaccine to Prevent COVID-19". ClinicalTrials.gov. 7 July 2021. NCT04953078. Retrieved 7 July 2021.
- ^ "Phase 1 Intranasal Parainfluenza Virus Type 5-SARS CoV-2 S Vaccine in Healthy Adults (CVXGA1-001)". ClinicalTrials.gov. 8 July 2021. NCT04954287. Retrieved 8 July 2021.
- ^ "FMBA begins clinical trials of its coronavirus vaccine, press service says". Russian News Agency. 19 July 2021. Retrieved 20 July 2021.
- ^ "The Objectives of This Study Are Study the Immunogenicity, Safety and Tolerability of the Coronavirus Vaccine in Healthy Adult Volunteer Aged 18 to 60 Years". ClinicalTrials.gov. 14 December 2021. NCT05156723. Retrieved 14 December 2021.
- ^ "Phase I clinical trial to evaluate the safety, tolerability and preliminary immunogenicity of the new coronavirus mRNA vaccine (LVRNA009) in Chinese people aged 18 years and over". chictr.org.cn. 31 July 2021. ChiCTR2100049349. Retrieved 31 July 2021.
- ^ "A Trial Evaluating the Safety and Immunogenicity of 3 COVID-19 SARS-CoV-2 RNA Vaccines in Healthy Adults". clinicaltrials.gov. 8 September 2021. NCT05037097. Retrieved 8 September 2021.
- ^ "Clinical Study of the Safety and Immunogenicity of a Recombinant Viral Vector AAV5 (Adeno-Associated Virus Type 5 )-RBD (Receptor Binding Domain)-S Vaccine for the Prevention of Coronavirus Infection (COVID-19) (COVER)". clinicaltrials.gov. 8 September 2021. NCT05037188. Retrieved 8 September 2021.
- ^ "A study of the safety of EDV nanocells packaged with spike-protein plasmid and glycolipid as a COVID-19 vaccine in healthy volunteers". 27 August 2021. ACTRN12621001159842. Retrieved 17 September 2021.
- ^ "COVIDITY". Scancell. Retrieved 17 September 2021.
- ^ "A First Time in Human Phase 1 Open-Label Study of the COVIDITY Vaccine Administered by Needle-free Injection". clinicaltrials.gov. 17 September 2021. NCT05047445. Retrieved 17 September 2021.
- ^ "Evaluation of the Safety and Immunogenicity of SII Vaccine Constructs Based on the SARS-CoV-2 (COVID-19) Variant in Adults". clinicaltrials.gov. 1 September 2021. NCT05029856. Retrieved 16 September 2021.
- ^ Chan-hyuk, Kim (1 September 2021). "Eyegene wins approval for trial of mRNA Covid-19 vaccine". Korea Biomedical Review. Retrieved 7 October 2021.
- ^ "아이진, 부작용 줄인 코로나 mRNA 백신 개발한다". 한국경제TV. 23 September 2021. Retrieved 7 October 2021.
- ^ "Study to Assess the Safety, Tolerability and Explore the Immunogenicity of EG-COVID in Healthy Adult Volunteers". clinicaltrials.gov. 12 January 2022. NCT05188469. Retrieved 12 January 2022.
- ^ "To Evaluate the Safety, Tolerability, and Immunogenicity of a PIKA-Adjuvanted Recombinant SARS-CoV-2 Spike (S) Protein Subunit Vaccine in Healthy Individuals". anzctr.org.au. 15 July 2021. ACTRN12621001009808. Retrieved 2 August 2021.
- ^ "Phase 1 Trial of ChAd68 and Ad5 Adenovirus COVID-19 Vaccines Delivered by Aerosol". clinicaltrials.gov. 26 October 2021. NCT05094609. Retrieved 26 October 2021.
- ^ "A Study to Evaluate Safety & Immunogenicity of SARS-CoV-2 DNA Vaccine Delivered Intramuscularly Followed by Electroporation for COVID-19". clinicaltrials.gov. 1 November 2021. NCT05102643. Retrieved 1 November 2021.
- ^ Jaffe-Hoffman, Maayan (11 June 2021). "Israeli oral COVID-19 vaccine en route to clinical trials". The Jerusalem Post. Retrieved 2 November 2021.
- ^ Jaffe-Hoffman, Maayan (22 July 2021). "Israel to become first in world to test Oravax oral COVID-19 vaccine". The Jerusalem Post. Retrieved 2 November 2021.
- ^ "Oramed Announces Oravax's Oral COVID-19 Vaccine Has Received South African Approval to Initiate Phase 1 Trial". Cision PR News Wire. 29 October 2021. Retrieved 2 November 2021.
- ^ "inno.N, 코로나19 백신 후보물질 임상1상 신청". HK inno.N.
- ^ "Study to Evaluate the Safety and Immunogenicity of SARS-CoV-2 Vaccine (IN-B009) in Healthy Adults (COVID-19)". clinicaltrials.gov. 9 November 2021. NCT05113849. Retrieved 9 November 2021.
- ^ "Evaluation of Safety and Immunogenicity of a T-Cell Priming Peptide Vaccine Against Coronavirus (naNO-COVID)". clinicaltrials.gov. 9 November 2021. NCT05113862. Retrieved 9 November 2021.
- ^ "Russian health ministry approves clinical trials of Betuvax-CoV-2 COVID-19 vaccine". Russian News Agency. 27 September 2021. Retrieved 4 November 2021.
- ^ "Private Russian company starts trials for new COVID-19 vaccine - TASS". Reuters. 15 October 2021. Retrieved 4 November 2021.
- ^ "Egypt announces clinical trials of its own COVID-19 vaccine". Associated Press News. 15 November 2021. Retrieved 23 November 2021.
- ^ "Evaluation of Inactivated Vaccine in Healthy Adults Against Coronavirus Disease of 2019 (COVID-19)". clinicaltrials.gov. 22 November 2021. NCT05128721. Retrieved 22 November 2021.
- ^ "自己増殖型mRNAワクチンVLPCOV-01の第1相試験 並行群間、二重盲検、プラセボ対照ヒト初回投与試験(FIH試験)(COVID-19)" [Clinical research implementation plan / research outline disclosure system]. jrct.niph.go.jp. Japan Registry of Clinical Trials. Retrieved 5 October 2021.
- ^ "Study of GRT-R910 Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Boost Vaccine in Healthy Volunteers". clinicaltrials.gov. 8 December 2021. NCT05148962. Retrieved 8 December 2021.
- ^ "Development of a COVID19 Oral Vaccine Consisting of Bacillus Subtilis Spores Expressing and Displaying the Receptor Binding Domain of Spike Protein of SARS-COV2". chictr.org.cn. 28 November 2021. ChiCTR2100053747. Retrieved 28 November 2021.
- ^ "Phase-I Study to Evaluate the Safety and Immunogenicity of a Prophylactic pDNA Vaccine Candidate Against COVID-19 in Healthy Adults". clinicaltrials.gov. 29 December 2021. NCT05171946. Retrieved 29 December 2021.
- ^ "신형코로나비루스후보왁찐을 새로 개발". North's State Commission of Science and Technology. Archived from the original on 4 May 2021.
- ^ "Dự kiến cuối quý 3-2021, Việt Nam sẽ có vaccine phòng Covid-19 đầu tiên". Nhân Dân. 22 March 2021. Retrieved 25 March 2021.
- ^ "INOVIO's Pan-COVID-19 Vaccine Candidate (INO-4802) Induces Broad Immunity Against Major Viral Variants in Preclinical Studies". Inovio Pharmaceutical. 12 May 2021. Retrieved 10 June 2021.
- ^ "Bangavax Vaccine: Permission sought for clinical trial". The Daily Star. 18 January 2021.
- ^ "Bangladesh joins global COVID-19 vaccine race with Bongavax set for clinical trial". Arab News. 8 January 2021.
- ^ "Bangavax first buzzed with hope, then fizzled". bdnews24. 6 May 2021. Retrieved 9 May 2021.
- ^ "The vaccine is expected to provide long-lasting protection with a single dose administration with an anticipated safety profile similar to other licensed vaccines for active immunization" (PDF). Indian Immunologicals. 8 April 2020. Retrieved 24 July 2021.
- ^ Medeiros, Danielle (31 December 2020). "EpiVax and EpiVax Therapeutics Advance COVID-19 Vaccine Program, EPV-CoV-19". EpiVax.
- ^ "Intravacc announces positive pre-clinical data for its SARS-CoV-2 nose spray vaccine". Intravacc. 7 April 2021. Retrieved 5 September 2021.
- ^ "Second-Generation COVID-19 Vaccine Candidate, CV2CoV, Demonstrates High Immunogenicity Against Virus Variants in Preclinical Study". CureVac. 13 May 2021.
- ^ "Sorrento and Dyadic Announce Binding Term Sheet to License Dyadic's Lead COVID-19 Vaccine Candidate "DYAI-100" and C1 Technology for Protein-Based Coronavirus Vaccines and Therapeutics". Sorrento Therapeutics. 11 August 2021. Retrieved 20 August 2021.
- ^ "Sorrento Announces Its Lead Protein-Based COVID-19 Vaccine Candidate – DYAI-100 – Elicits Strong Neutralizing Immune Responses in Vaccinated Animals Against SARS-CoV-2 and Multiple Major Variants of Concern". Sorrento Therapeutics. 19 August 2021. Retrieved 20 August 2021.
- ^ "Malaysian mRNA vaccine against Covid-19 under development, says Adham". The Edge. 21 June 2021. Retrieved 22 June 2021.
- ^ "COVID-19". CureVac. Retrieved 21 December 2020.
- ^ "A Study to Determine the Safety and Efficacy of SARS-CoV-2 mRNA Vaccine CVnCoV in Adults for COVID-19". ClinicalTrials.gov. 3 December 2020. NCT04652102. Retrieved 22 July 2021.
- ^ "A Study to Evaluate the Safety and Immunogenicity of Vaccine CVnCoV in Healthy Adults in Germany for COVID-19". ClinicalTrials.gov. 19 December 2020. NCT04674189. Retrieved 23 March 2021.
- ^ "A Study to Evaluate the Immunogenicity and Safety of the SARS-CoV-2 mRNA Vaccine CVnCoV in Elderly Adults Compared to Younger Adults for COVID-19". ClinicalTrials.gov. 9 April 2021. NCT04838847. Retrieved 26 April 2021.
- ^ "A Study to Evaluate Safety, Reactogenicity and Immunogenicity of the SARS-CoV-2 mRNA Vaccine CVnCoV in Adults With Co-morbidities for COVID-19". ClinicalTrials.gov. 26 April 2021. NCT04860258. Retrieved 26 April 2021.
- ^ "COVID-19: A Trial Studying the SARS-CoV-2 mRNA Vaccine CVnCoV to Learn About the Immune Response, the Safety, and the Degree of Typical Vaccination Reactions When CVnCoV is Given at the Same Time as a Flu Vaccine Compared to When the Vaccines Are Separately Given in Adults 60 Years of Age and Older (CV-NCOV-011)". ClinicalTrials.gov. 19 April 2021. NCT04848467. Retrieved 18 June 2021.
- ^ "COVID-19: A Phase 2b/3, Randomized, Observer-Blinded, Placebo Controlled, Multicenter Clinical Study Evaluating the Efficacy and Safety of Investigational SARS-CoV-2 mRNA Vaccine CVnCoV in Adults 18 Years of Age and Older". EU Clinical Trials Register. 19 November 2020. 2020-003998-22. Retrieved 19 December 2020.
- ^ "A Study to Evaluate the Safety, Reactogenicity and Immunogenicity of Vaccine CVnCoV in Healthy Adults". ClinicalTrials.gov. 26 June 2020. NCT04449276. Archived from the original on 11 October 2020. Retrieved 14 July 2020.
- ^ "A Dose-Confirmation Study to Evaluate the Safety, Reactogenicity and Immunogenicity of Vaccine CVnCoV in Healthy Adults for COVID-19". ClinicalTrials.gov. 17 August 2020. NCT04515147. Archived from the original on 23 August 2020. Retrieved 28 August 2020.
- ^ "EMA starts rolling review of CureVac's COVID-19 vaccine (CVnCoV)". European Medicines Agency (EMA) (Press release). 1 December 2020. Retrieved 12 February 2021.
- ^ "CureVac seeks Covid-19 shot approval in Switzerland". Swissinfo. 20 April 2021. Retrieved 22 April 2021.
- ^ "CORVax12: SARS-CoV-2 Spike (S) Protein Plasmid DNA Vaccine Trial for COVID-19 (SARS-CoV-2) (CORVax12)". ClinicalTrials.gov. 13 November 2020. NCT04627675. Retrieved 21 March 2021.
- ^ "Sanofi and Translate Bio initiate Phase 1/2 clinical trial of mRNA COVID-19 vaccine candidate" (Press release). Sanofi. 12 March 2021. Retrieved 20 March 2021.
- ^ "Study of mRNA Vaccine Formulation Against COVID-19 in Healthy Adults 18 Years of Age and Older (VAW00001)". ClinicalTrials.gov. 15 March 2021. NCT04798027. Retrieved 20 March 2021.
- ^ "Safety and Immunogenicity of AdCOVID in Healthy Adults (COVID-19 Vaccine Study)". ClinicalTrials.gov. 22 December 2020. NCT04679909. Retrieved 22 March 2021.
- ^ "Altimmune Announces Update On AdCOVID Phase 1 Clinical Trial". Altimmune. 29 June 2021. Retrieved 1 July 2021.
- ^ Ward D, McCormack S (22 May 2020). "Clinical trial to assess the safety of a coronavirus vaccine in healthy men and women". ISRCTN. doi:10.1186/ISRCTN17072692. ISRCTN17072692.
- ^ "Clinical Trial to Evaluate the Safety and Immunogenicity of the COVID-19 Vaccine (COVID-19-101)". ClinicalTrials.gov. 4 August 2020. NCT04497298. Retrieved 23 March 2021.
- ^ "A Study on the Safety, Tolerability and Immune Response of SARS-CoV-2 Sclamp (COVID-19) Vaccine in Healthy Adults". ClinicalTrials.gov. 3 August 2020. NCT04495933. Archived from the original on 11 October 2020. Retrieved 4 August 2020.
- ^ "UQ-CSL V451 Vaccine". precisionvaccinations.com. Retrieved 11 December 2020.
- ^ "Dose Ranging Trial to Assess Safety and Immunogenicity of V590 (COVID-19 Vaccine) in Healthy Adults (V590-001)". 30 September 2020. Retrieved 26 January 2021.
- ^ "A Study to Assess Safety, Tolerability, and Immunogenicity of V591 (COVID-19 Vaccine) in Healthy Participants (V591-001)". 4 August 2020. Retrieved 26 January 2021.
- ^ "Participant Enrollment Begins for Phase I Trial of IAVI-Merck COVID-19 Vaccine Candidate". IAVI. Retrieved 14 March 2021.
- ^ "V591 SARS-CoV-2 Vaccine". www.precisionvaccinations.com. Retrieved 14 March 2021.
- ^ "Merck Discontinues Development of SARS-CoV-2/COVID-19 Vaccine Candidates; Continues Development of Two Investigational Therapeutic Candidates". Merck (Press release). 25 January 2021. Retrieved 25 January 2021.
- ^ "Joint CDC and FDA Statement on Vaccine Boosters". U.S. Food and Drug Administration (FDA) (Press release). 8 July 2021. Retrieved 9 July 2021.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ^ "Coronavirus (COVID-19) Update: FDA Authorizes Additional Vaccine Dose for Certain Immunocompromised Individuals". U.S. Food and Drug Administration (FDA) (Press release). 12 August 2021. Retrieved 13 August 2021.
- ^ "COVID-19 Vaccines for Moderately to Severely Immunocompromised People". Centers for Disease Control and Prevention. 13 August 2021. Retrieved 13 August 2021.
- ^ Ledford, Heidi (18 February 2021). "Could mixing COVID vaccines boost immune response?". Nature. 590 (7846): 375–376. Bibcode:2021Natur.590..375L. doi:10.1038/d41586-021-00315-5. ISSN 0028-0836. PMID 33547431. S2CID 231946137.
- ^ "Angela Merkel receives Moderna dose after first AstraZeneca shot". Al Jazeera. 22 June 2021. Retrieved 28 June 2021.
- ^ "Getting One Vaccine Is Good. How About Mix-and-Match?". The New York Times. 30 March 2021. Retrieved 30 June 2021.
- ^ "About". Com-COV. Retrieved 28 June 2021.
- ^ a b Stuart, Arabella; Shaw, Robert; Walker, Laura (29 January 2021). "Comparing coronavirus (COVID-19) vaccine schedule combinations". ISRCTN Registry. doi:10.1186/ISRCTN69254139. ISRCTN69254139. Retrieved 9 July 2021.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ "Safety and Immunogenicity Report from the Com-COV Study – a Single-Blind Randomised Non-Inferiority Trial Comparing Heterologous And Homologous Prime-Boost Schedules with An Adenoviral Vectored and mRNA COVID-19 Vaccine". June 2021. SSRN 3874014.
- ^ a b Vichos, Iason; Snape, Matthew (12 March 2021). "Comparing COVID-19 vaccine schedule combinations – stage 2". ISRCTN Registry. doi:10.1186/ISRCTN27841311. ISRCTN27841311. Retrieved 9 July 2021.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Faust, Saul (27 April 2021). "Evaluating COVID-19 Vaccination Boosters". ISRCTN Registry. doi:10.1186/ISRCTN73765130. ISRCTN73765130. Retrieved 9 July 2021.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ "Combination of the first component of Sputnik V vaccine (Sputnik Light vaccine) with vaccines by AstraZeneca, Sinopharm and Moderna demonstrates high safety profile during the study in Argentina's Buenos-Aires province" (Press release). Moscow: Russian Direct Investment Fund. 4 August 2021. Retrieved 5 August 2021.
- ^ "Study on Sequential Immunization of Recombinant COVID-19 Vaccine (Ad5 Vector) and RBD-based Protein Subunit Vaccine". ClinicalTrials.gov. 6 April 2021. NCT04833101. Retrieved 9 July 2021.
- ^ "Vaccination With COMIRNATY in Subjects With a VAXZEVRIA First Dose (CombiVacS)". ClinicalTrials.gov. 27 April 2021. NCT04860739. Retrieved 9 July 2021.
- ^ "Mix and Match of the Second COVID-19 Vaccine Dose for Safety and Immunogenicity (MOSAIC)". ClinicalTrials.gov. 20 May 2021. NCT04894435. Retrieved 9 July 2021.
- ^ "Compare Immunological Efficacy of a Vaccine Regimen Combining Two Covid19 mRNA Vaccines (Pfizer-BioNTech and Moderna) With That of a Homologous Vaccination of Each Covid19 mRNA Vaccine (ARNCOMBI)". ClinicalTrials.gov. 25 May 2021. NCT04900467. Retrieved 9 July 2021.
- ^ "Heterologous Vaccination With an Vaxzevria (ChAdOx1-S) Prime and a Comirnaty (BNT162b2) Boost Compared With Homolog Vaccination With Vaxzervria (Prime/Boost) or Comirnaty (Prime/Boost) (HeVacc)". ClinicalTrials.gov. 28 May 2021. NCT04907331. Retrieved 9 July 2021.
- ^ Kuy, Hugo van der (16 June 2021). "A Trial Among HealthCare Workers (HCW) Vaccinated With Janssen Vaccine: the SWITCH Trial (SWITCH)". ClinicalTrials.gov. NCT04927936. Retrieved 9 July 2021.
- ^ a b "FDA Briefing Document: Pfizer–BioNTech COVID-19 Vaccine" (PDF). U.S. Food and Drug Administration (FDA). 10 December 2020. Retrieved 1 January 2021.
- ^ Zimmer C (20 November 2020). "2 Companies Say Their Vaccines Are 95% Effective. What Does That Mean? You might assume that 95 out of every 100 people vaccinated will be protected from Covid-19. But that's not how the math works". The New York Times. Retrieved 21 November 2020.
- ^ "#DoNotSqueezeMyArm: Doctor Sounds Alarm on How to Properly Inject COVID-19 Vaccine".
- ^ Ng, Jia Yu (1 June 2021). "Inadvertent subcutaneous injection of COVID-19 vaccine". Postgraduate Medical Journal. 97 (1148): 400. doi:10.1136/postgradmedj-2021-139870. PMC 7886662. PMID 33589486 – via pmj.bmj.com.
- ^ https://www.cdc.gov/vaccines/covid-19/downloads/covid19-vaccine-errors-deviations.pdf
- ^ Branswell H (2 February 2021). "Comparing three Covid-19 vaccines: Pfizer, Moderna, J&J". Stat. Retrieved 28 February 2021.
- ^ "Bharat's Intranasal Covid-19 Vaccine Moves Forward". 16 August 2021.
- ^ Randolph HE, Barreiro LB (May 2020). "Herd Immunity: Understanding COVID-19". Immunity. 52 (5): 737–41. doi:10.1016/j.immuni.2020.04.012. PMC 7236739. PMID 32433946.
- ^ "The FDA's cutoff for Covid-19 vaccine effectiveness is 50 percent. What does that mean?". NBCNews.com. Retrieved 8 January 2021.
- ^ "EMA sets 50% efficacy goal – with flexibility – for COVID vaccines". Regulatory Affairs Professionals Society (RAPS). Retrieved 8 January 2021.
- ^ Krause P, Fleming TR, Longini I, Henao-Restrepo AM, Peto R, Dean NE, et al. (12 September 2020). "COVID-19 vaccine trials should seek worthwhile efficacy". The Lancet. 396 (10253): 741–743. doi:10.1016/S0140-6736(20)31821-3. PMC 7832749. PMID 32861315.
- ^ a b Bartsch SM, O'Shea KJ, Ferguson MC, Bottazzi ME, Wedlock PT, Strych U, et al. (October 2020). "Vaccine Efficacy Needed for a COVID-19 Coronavirus Vaccine to Prevent or Stop an Epidemic as the Sole Intervention". American Journal of Preventive Medicine. 59 (4): 493–503. doi:10.1016/j.amepre.2020.06.011. PMC 7361120. PMID 32778354.
- ^ "FDA Briefing Document for mRNA 1273". 2020-12-17. Retrieved 2021-08-18.
{{cite web}}: CS1 maint: url-status (link) - ^ Anderson, Evan J.; Rouphael, Nadine G.; Widge, Alicia T.; Jackson, Lisa A.; Roberts, Paul C.; Makhene, Mamodikoe; Chappell, James D.; Denison, Mark R.; Stevens, Laura J.; Pruijssers, Andrea J.; McDermott, Adrian B. (2020-12-17). "Safety and Immunogenicity of SARS-CoV-2 mRNA-1273 Vaccine in Older Adults". New England Journal of Medicine. 383 (25): 2427–2438. doi:10.1056/NEJMoa2028436. ISSN 0028-4793. PMC 7556339. PMID 32991794.
- ^ Hunziker, Patrick (2021-07-24). "Personalized-dose Covid-19 vaccination in a wave of virus Variants of Concern: Trading individual efficacy for societal benefit". Precision Nanomedicine. 4 (3): 805–820. doi:10.33218/001c.26101.
- ^ Dooling, Kathleen (2021-08-13). "Evidence to Recommendations Framework: Additional doses of mRNA COVID-19 vaccines as part of a primary series for immunocompromised" (PDF). CDC Advisory Board for Immunization Practices.
{{cite web}}: CS1 maint: url-status (link) - ^ Chen, Zhimin; Liu, Kaihui; Liu, Xiuxiang; Lou, Yijun (February 2020). "Modelling epidemics with fractional-dose vaccination in response to limited vaccine supply". Journal of Theoretical Biology. 486: 110085. Bibcode:2020JThBi.48610085C. doi:10.1016/j.jtbi.2019.110085. PMID 31758966.
- ^ Dean N, Madewell Z (5 March 2021). "Understanding the spectrum of vaccine efficacy measures". The BMJ Opinion. Retrieved 10 March 2021.
- ^ Cite error: The named reference
AZD1222-efficacywas invoked but never defined (see the help page). - ^ "AZD1222 US Phase III primary analysis confirms safety and efficacy". AstraZeneca. 25 March 2021.
- ^ a b Committee for Medicinal Products for Human Use (19 February 2021). Assessment report: Comirnaty (PDF) (European public assessment report). Corr.1. European Medicines Agency (EMA). COVID-19 Case Definitions; tables 2, 5, 12, 13. EMA/707383/2020. Archived (PDF) from the original on 20 June 2021. Retrieved 23 June 2021.
- ^ a b "Pfizer–BioNTech COVID-19 Vaccine – rna ingredient bnt-162b2 injection, suspension". DailyMed. U.S. National Institutes of Health. Retrieved 14 December 2020.
- ^ a b c "Janssen COVID-19 Vaccine – ad26.cov2.s injection, suspension". DailyMed. U.S. National Institutes of Health. Retrieved 15 March 2021.
- ^ "FDA Briefing Document: Janssen Ad26.COV2.S Vaccine for the Prevention of COVID-19". US Food & Drug Administration (FDA). 26 February 2021. Retrieved 1 April 2021.
- ^ a b c "Moderna COVID-19 Vaccine – cx-024414 injection, suspension". DailyMed. U.S. National Institutes of Health. Retrieved 20 December 2020.
- ^ Al Kaabi N, Zhang Y, Xia S, Yang Y, Al Qahtani MM, Abdulrazzaq N, et al. (May 2021). "Effect of 2 Inactivated SARS-CoV-2 Vaccines on Symptomatic COVID-19 Infection in Adults: A Randomized Clinical Trial". JAMA. 326 (1): 35–45. doi:10.1001/jama.2021.8565. PMC 8156175. PMID 34037666.
{{cite journal}}: CS1 maint: PMC embargo expired (link) - ^ Logunov DY, Dolzhikova IV, Shcheblyakov DV, Tukhvatulin AI, Zubkova OV, Dzharullaeva AS, et al. (February 2021). "Safety and efficacy of an rAd26 and rAd5 vector-based heterologous prime-boost COVID-19 vaccine: an interim analysis of a randomised controlled phase 3 trial in Russia". Lancet. 397 (10275): 671–81. doi:10.1016/S0140-6736(21)00234-8. PMC 7852454. PMID 33545094.
- ^ "Summary of Clinical Trial Data of Sinovac's COVID-19 Vaccine (CoronaVac)" (Press release). Sinovac Biotech. 3 April 2021. Retrieved 12 April 2021.
- ^ Palacios R, Batista AP, Albuquerque CS, Patiño EG, Santos Jd, Tilli Reis Pessoa Conde M, et al. (April 2021). "Efficacy and Safety of a COVID-19 Inactivated Vaccine in Healthcare Professionals in Brazil: The PROFISCOV Study". SSRN 3822780.
- ^ Toscano C (29 April 2021). "Evidence Assessment: Sinovac/CoronaVac COVID-19 vaccine" (PDF). World Health Organization (WHO).
- ^ Tanriover, Mine Durusu; Doğanay, Hamdi Levent; Akova, Murat; Güner, Hatice Rahmet; Azap, Alpay; Akhan, Sıla; et al. (8 July 2021). "Efficacy and safety of an inactivated whole-virion SARS-CoV-2 vaccine (CoronaVac): interim results of a double-blind, randomised, placebo-controlled, phase 3 trial in Turkey". The Lancet. 398 (10296): 213–222. doi:10.1016/S0140-6736(21)01429-X. ISSN 0140-6736. PMC 8266301. PMID 34246358. S2CID 235770533.
- ^ "Ocugen's COVID-19 Vaccine Co-Development Partner, Bharat Biotech, Shares Phase 3 Results Demonstrating 77.8% Protection against Overall Disease" (Press release). Malvern, Pennsylvania; and Hyderabad: GlobeNewswire. Ocugen. 2 July 2021. Retrieved 3 July 2021.
- ^ "Single dose vaccine, Sputnik Light, authorized for use in Russia" (Press release). Russian Direct Investment Fund. 6 May 2021. Retrieved 1 July 2021.
The single dose Sputnik Light vaccine demonstrated 79.4% efficacy according to analyzed data taken from 28 days after the injection was administered as part of Russia's mass vaccination program between 5 December 2020 and 15 April 2021.
- ^ Cite error: The named reference
reuters-convideciawas invoked but never defined (see the help page). - ^ Kaabi NA, Zhang Y, Xia S, Yang Y, Qahtani MM, Abdulrazzaq N, et al. (26 May 2021). "Effect of 2 Inactivated SARS-CoV-2 Vaccines on Symptomatic COVID-19 Infection in Adults". JAMA. 326 (1): 35–45. doi:10.1001/jama.2021.8565. ISSN 0098-7484. PMC 8156175. PMID 34037666.
{{cite journal}}: CS1 maint: PMC embargo expired (link) - ^ "El candidato vacunal Abdala mostró una eficacia de un 92,28% en su esquema de tres dosis". BioCubaFarma (Press release). 21 June 2021. Retrieved 1 July 2021.
- ^ "How was the efficacy of the Cuban COVID-19 vaccine candidates calculated?". OnCubaNews English. 27 June 2021. Retrieved 28 June 2021.
- ^ "Soberana 02 muestra una eficacia de un 62 por ciento en su esquema de dos dosis". BioCubaFarma (Press release). 20 June 2021. Retrieved 1 July 2021.
- ^ Wadman M, Cohen J (28 January 2021). "Novavax vaccine delivers 89% efficacy against COVID-19 in UK – but is less potent in South Africa". Science. doi:10.1126/science.abg8101.
- ^ "Novavax Publishes Results of United Kingdom Phase 3 Clinical Trial in New England Journal of Medicine, Demonstrating High Levels of Efficacy of COVID-19 Vaccine". Novavax Inc. (Press release). Retrieved 30 June 2021.
- ^ "Novavax COVID-19 Vaccine Demonstrates 90% Overall Efficacy and 100% Protection Against Moderate and Severe Disease in PREVENT-19 Phase 3 Trial". Novavax Inc. (Press release). 14 June 2021. Retrieved 15 June 2021.
- ^ "CureVac Final Data from Phase 2b/3 Trial of First-Generation COVID-19 Vaccine Candidate, CVnCoV, Demonstrates Protection in Age Group of 18 to 60". CureVac (Press release). 30 June 2021. Retrieved 1 July 2021.
- ^ "Zydus applies to the DCGI for EUA to launch ZyCoV-D, the world's first Plasmid DNA vaccine for COVID-19" (PDF). Cadila Healthcare (Press release). 1 July 2021. Retrieved 1 July 2021.
- ^ "China's Zhifei says unit's COVID shot shows 81.76% efficacy in late-stage trial". Reuters. 27 August 2021.
- ^ "Vaccine Effectiveness", Virginia Dept. of Health, August 23, 2021
- ^ "SARS-CoV-2 Infections and Hospitalizations Among Persons Aged ≥16 Years, by Vaccination Status — Los Angeles County, California, May 1–July 25, 2021", C.D.C., August 27, 2021
- ^ "Vaccines are less protective against Delta infection but still reduce risk by two-thirds, C.D.C. study shows", CNN, August 24, 2021
- ^ "AMA survey shows over 96% of doctors were fully vaccinated against COVID-19", American Medical Association, June 11, 2021
- ^ a b "Vaccine Effectiveness Against Infection May Wane, C.D.C. Studies Find", "New York Times", August 19, 2021
- ^ a b c "The Delta Covid Variant's Urgent Message for America:Vaccinate. Do it quickly.", The New Republic, July 1, 2021
- ^ "Sustained Effectiveness of Pfizer-BioNTech and Moderna Vaccines Against COVID-19 Associated Hospitalizations Among Adults — United States, March–July 2021", C.D.C., August 27, 2021
- ^ a b "Unvaccinated Covid patients are straining hospitals like mine, where I had to turn a cancer patient away", Washington Post, August 21, 2021
- ^ "CDC study shows unvaccinated people are 29 times more likely to be hospitalized with Covid", CNBC, August 24, 2021
- ^ "Unvaccinated 67 times more likely to die from COVID-19, adjusted data shows", King5 News, August 27, 2021
- ^ "‘It’s soul-draining’: Health workers deployed to Covid hot zones are overwhelmed by deaths among the unvaccinated", Statnews, August 18, 2021
- ^ "Massachusetts reports 1,591 new COVID cases as unvaccinated individuals continue to dominate hospital numbers", Mass Live, August 27, 2021
- ^ "CDC: Covid-19 Vaccine Effectiveness Fell From 91% To 66% With Delta Variant", Forbes, August 24, 2021
- ^ "Among the unvaccinated, Delta variant more than doubles risk of hospitalization", Los Angeles Times, August 28, 2021
- ^ "The four main fault lines that divide the vaccinated and the unvaccinated", Vox, July 29, 2021
- ^ "What is the difference between efficacy and effectiveness?". Gavi, the Vaccine Alliance (GAVI). 18 November 2020. Retrieved 21 April 2021.
- ^ Tal A, Cohen E (29 January 2021). "Israel's health data suggests Pfizer and Moderna vaccines may be more effective than we thought". CNN. Retrieved 27 March 2021.
- ^ a b c Cite error: The named reference
cdc-effectivenesswas invoked but never defined (see the help page). - ^ Hall VJ, Foulkes S, Saei A, Andrews N, Oguti B, Charlett A, et al. (The SIREN Study Group) (February 2021). "Effectiveness of BNT162b2 mRNA Vaccine Against Infection and COVID-19 Vaccine Coverage in Healthcare Workers in England, Multicentre Prospective Cohort Study (the SIREN Study)". SSRN 3790399.
- ^ a b "Real-World Evidence Confirms High Effectiveness of Pfizer–BioNTech COVID-19 Vaccine and Profound Public Health Impact of Vaccination One Year After Pandemic Declared". Pfizer. 11 March 2021. Retrieved 1 April 2021.
- ^ Tande AJ, Pollock BD, Shah ND, Farrugia G, Virk A, Swift M, et al. (March 2021). "Impact of the COVID-19 Vaccine on Asymptomatic Infection Among Patients Undergoing Pre-Procedural COVID-19 Molecular Screening". Clinical Infectious Diseases. doi:10.1093/cid/ciab229. PMC 7989519. PMID 33704435.
- ^ Lopez Bernal J, Andrews N, Gower C, Robertson C, Stowe J, Tessier E, et al. (May 2021). "Effectiveness of the Pfizer-BioNTech and Oxford-AstraZeneca vaccines on covid-19 related symptoms, hospital admissions, and mortality in older adults in England: test negative case-control study". BMJ. 373: n1088. doi:10.1136/bmj.n1088. ISSN 1756-1833. PMC 8116636. PMID 33985964.
- ^ COVID-19 vaccine surveillance report (week 21) (PDF) (Technical report). Public Health England. 27 May 2021. GOV-8481.
- ^ COVID-19 vaccine surveillance report (week 20) (PDF) (Technical report). Public Health England. 20 May 2021. GOV-8401.
- ^ a b c "Ministros de Salud de todo el país consensuaron redoblar esfuerzos para completar los esquemas de vacunación en mayores de 40 años" [Health ministers from all over the country agreed to redouble their efforts to complete vaccination schedules in people over 40 years of age] (in Spanish). Government of Argentina. Ministry of Health (Argentina). 1 July 2021. Retrieved 12 July 2021.
- ^ Haas EJ, Angulo FJ, McLaughlin JM, Anis E, Singer SR, Khan F, et al. (May 2021). "Impact and effectiveness of mRNA BNT162b2 vaccine against SARS-CoV-2 infections and COVID-19 cases, hospitalisations, and deaths following a nationwide vaccination campaign in Israel: an observational study using national surveillance data". Lancet. 397 (10287): 1819–1829. doi:10.1016/S0140-6736(21)00947-8. PMC 8099315. PMID 33964222.
- ^ Dagan N, Barda N, Kepten E, Miron O, Perchik S, Katz MA, et al. (April 2021). "BNT162b2 mRNA Covid-19 Vaccine in a Nationwide Mass Vaccination Setting". New England Journal of Medicine. 384 (15): 1412–23. doi:10.1056/NEJMoa2101765. PMC 7944975. PMID 33626250.
- ^ a b "Tercer estudio de efectividad de vacunación anti SARS-CoV-2 en Uruguay al 30 de junio de 2021" [Third study of effectiveness of vaccination against SARS-CoV-2 in Uruguay as of June 30, 2021]. Ministerio de Salud Pública (in Spanish). 3 July 2021. Retrieved 7 July 2021.
- ^ Hall VJ, Foulkes S, Saei A, Andrews N, Oguti B, Charlett A, et al. (May 2021). "COVID-19 vaccine coverage in health-care workers in England and effectiveness of BNT162b2 mRNA vaccine against infection (SIREN): a prospective, multicentre, cohort study". The Lancet. 397 (10286): 1725–35. doi:10.1016/S0140-6736(21)00790-X. ISSN 0140-6736. PMC 8064668. PMID 33901423.
- ^ "INS: Vacuna de Sinopharm tiene efectividad de hasta 94% para reducir muerte por COVID-19". RPP (in Spanish). 22 July 2021. Retrieved 28 July 2021.
{{cite web}}: CS1 maint: url-status (link) - ^ "Russia's Sputnik V vaccine 97.6% effective in real-world study". Reuters. Moscow. 19 April 2021. Retrieved 21 April 2021.
- ^ "Sputnik V demonstrates 97.6% efficacy according to analysis of data from 3.8 million vaccinated persons in Russia making it the most efficient COVID-19 vaccine in the world" (Press release). Moscow: Russian Direct Investment Fund. 19 April 2021. Retrieved 21 April 2021.
- ^ "Sputnik V has demonstrated 97.8% efficacy against COVID cases and 100% efficacy against severe cases of COVID in UAE" (Press release). Moscow: Russian Direct Investment Fund. 29 June 2021. Retrieved 2 July 2021.
- ^ Jara, Alejandro; Undurraga, Eduardo A.; González, Cecilia; Paredes, Fabio; Fontecilla, Tomás; Jara, Gonzalo; Pizarro, Alejandra; Acevedo, Johanna; Leo, Katherine; Leon, Francisco; Sans, Carlos; Leighton, Paulina; et al. (7 July 2021). "Effectiveness of an Inactivated SARS-CoV-2 Vaccine in Chile". New England Journal of Medicine. doi:10.1056/NEJMoa2107715. ISSN 0028-4793. PMC 8279092. PMID 34233097. S2CID 235766915.
- ^ "Reporte COVID-19: Vacuna Coronavac Tiene Un 90,3% De Efectividad Para Prevenir El Ingreso a UCI" [COVID-19 report: CoronaVac vaccine is 90.3% effective in preventing admission to the ICU]. Ministerio de Salud - Gobierno de Chile (in Spanish). 17 May 2021.
- ^ Aditya A. "China Sinovac Shot Seen Highly Effective in Real World Study". Bloomberg. Retrieved 15 May 2021.
- ^ "Kajian Cepat Kemenkes : Vaksin Sinovac Efektif Cegah Kematian" [Ministry of Health Quick Study: Sinovac Vaccine Effectively Prevents Death]. Sehat Negeriku (in Indonesian). 12 May 2021. Retrieved 15 May 2021.
- ^ "Mass vaccination creates healthy oasis in Brazilian city". Reuters. 31 May 2021. Retrieved 2 June 2021.
- ^ "Sinovac vaccine restores a Brazilian city to near normal". Associated Press. 1 June 2021. Retrieved 2 June 2021.
- ^ "Sputnik-V tiene una efectividad con una sola dosis de 78,6% para evitar casos" [Sputnik-V is 78.6% effective with a single dose in preventing cases] (in Spanish). Government of Buenos Aires Province. 2 June 2021. Retrieved 29 June 2021.
- ^ "Sputnik Light vaccine (the first component of Sputnik V vaccine) demonstrates 78.6-83.7% efficacy among the elderly in Argentina" (Press release). Russian Direct Investment Fund. 2 June 2021. Retrieved 29 June 2021.
- ^ Fine P, Eames K, Heymann DL (1 April 2011). ""Herd Immunity": A Rough Guide". Clinical Infectious Diseases. 52 (7): 911–916. doi:10.1093/cid/cir007. ISSN 1058-4838. PMID 21427399.
- ^ Billah MA, Miah MM, Khan MN (11 November 2020). "Reproductive number of coronavirus: A systematic review and meta-analysis based on global level evidence". PLOS ONE. 15 (11): e0242128. Bibcode:2020PLoSO..1542128B. doi:10.1371/journal.pone.0242128. PMC 7657547. PMID 33175914.
- ^ "Science Brief: COVID-19 Vaccines and Vaccination". Centers for Disease Control and Prevention. 27 May 2021. Archived from the original on 16 June 2021. Retrieved 17 June 2021.
Substantial reductions in SARS-CoV-2 infections (both symptomatic and asymptomatic) will reduce overall levels of disease, and therefore, viral transmission in the United States. However, investigations are ongoing to assess further the impact of COVID-19 vaccination on transmission.
- ^ Dyer, Owen (2021-08-02). "Covid-19: Delta infections threaten herd immunity vaccine strategy". BMJ. 374: n1933. doi:10.1136/bmj.n1933. ISSN 1756-1833. PMID 34340962. S2CID 236778544.
- ^ Katella, Kathy (13 August 2021). "5 Things To Know About the Delta Variant". Yale Medicine News. Retrieved 18 August 2021.
- ^ Burioni R, Topol EJ (21 June 2021). "Has SARS-CoV-2 reached peak fitness?". Nature Medicine. 27 (8): 1323–1324. doi:10.1038/s41591-021-01421-7. PMID 34155413.
- ^ a b Office of the Commissioner (23 February 2021). "Coronavirus (COVID-19) Update: FDA Issues Policies to Guide Medical Product Developers Addressing Virus Variants". U.S. Food and Drug Administration (FDA). Retrieved 7 March 2021.
- ^ Rella, Simon A.; Kulikova, Yuliya A.; Dermitzakis, Emmanouil T.; Kondrashov, Fyodor A. (2021-07-30). "Rates of SARS-CoV-2 transmission and vaccination impact the fate of vaccine-resistant strains". Scientific Reports. 11 (1): 15729. doi:10.1038/s41598-021-95025-3. ISSN 2045-2322. PMC 8324827. PMID 34330988.
- ^ Mahase E (March 2021). "Covid-19: Where are we on vaccines and variants?". BMJ. 372: n597. doi:10.1136/bmj.n597. PMID 33653708. S2CID 232093175.
- ^ a b c d Weekly epidemiological update on COVID-19 - 8 June 2021 (Situation report). World Health Organization. 8 June 2021. Table 3. Retrieved 14 June 2021.
- ^ "Inside the B.1.1.7 Coronavirus Variant". The New York Times. 18 January 2021. Retrieved 29 January 2021.
- ^ Muik A, Wallisch AK, Sänger B, Swanson KA, Mühl J, Chen W, et al. (March 2021). "Neutralization of SARS-CoV-2 lineage B.1.1.7 pseudovirus by BNT162b2 vaccine-elicited human sera". Science. 371 (6534): 1152–53. Bibcode:2021Sci...371.1152M. doi:10.1126/science.abg6105. PMC 7971771. PMID 33514629.
- ^ a b Wang P, Nair MS, Liu L, Iketani S, Luo Y, Guo Y, et al. (March 2021). "Antibody Resistance of SARS-CoV-2 Variants B.1.351 and B.1.1.7". Nature. 593 (7857): 130–35. Bibcode:2021Natur.593..130W. doi:10.1038/s41586-021-03398-2. PMID 33684923.
- ^ Emary KR, Golubchik T, Aley PK, Ariani CV, Angus BJ, Bibi S, et al. (February 2021). "Efficacy of ChAdOx1 nCoV-19 (AZD1222) Vaccine Against SARS-CoV-2 VOC 202012/01 (B.1.1.7)". SSRN 3779160.
- ^ Mahase E (February 2021). "Covid-19: Novavax vaccine efficacy is 86% against UK variant and 60% against South African variant". BMJ. 372: n296. doi:10.1136/bmj.n296. PMID 33526412. S2CID 231730012.
- ^ Kuchler H (25 January 2021). "Moderna develops new vaccine to tackle mutant Covid strain". Financial Times. Retrieved 30 January 2021.
- ^ Liu Y, Liu J, Xia H, Zhang X, Fontes-Garfias CR, Swanson KA, et al. (February 2021). "Neutralizing Activity of BNT162b2-Elicited Serum – Preliminary Report". The New England Journal of Medicine. doi:10.1056/nejmc2102017. PMID 33596352.
- ^ a b Hoffmann M, Arora P, Gross R, Seidel A, Hoernich BF, Hahn AS, et al. (March 2021). "1 SARS-CoV-2 variants B.1.351 and P.1 escape from neutralizing antibodies". Cell. 184 (9): 2384–2393.e12. doi:10.1016/j.cell.2021.03.036. PMC 7980144. PMID 33794143.
- ^ "Pfizer and BioNTech Confirm High Efficacy and No Serious Safety Concerns Through Up to Six Months Following Second Dose in Updated Topline Analysis of Landmark COVID-19 Vaccine Study". Pfizer (Press release). 1 April 2021. Retrieved 2 April 2021.
- ^ Cite error: The named reference
autowas invoked but never defined (see the help page). - ^ Francis D, Andy B (6 February 2021). "Oxford/AstraZeneca COVID shot less effective against South African variant: study". Reuters. Retrieved 8 February 2021.
- ^ a b "Covid: South Africa halts AstraZeneca vaccine rollout over new variant". BBC News Online. 8 February 2021. Retrieved 8 February 2021.
- ^ Booth W, Johnson CY (7 February 2021). "South Africa suspends Oxford-AstraZeneca vaccine rollout after researchers report 'minimal' protection against coronavirus variant". The Washington Post. London. Retrieved 8 February 2021.
South Africa will suspend use of the coronavirus vaccine being developed by Oxford University and AstraZeneca after researchers found it provided 'minimal protection' against mild to moderate coronavirus infections caused by the new variant first detected in that country.
- ^ "A Phase 2A/B, Randomized, Observer-blinded, Placebo-controlled Study to Evaluate the Efficacy, Immunogenicity, and Safety of a SARS-CoV-2 Recombinant Spike Protein Nanoparticle Vaccine (SARS-CoV-2 rS) With Matrix-M1 Adjuvant in South African Adult Subjects Living Without HIV; and Safety and Immunogenicity in Adults Living With HIV". ClinicalTrials.gov. 30 October 2020.
- ^ "PANGO lineages". cov-lineages.org. Retrieved 18 April 2021.
- ^ Koshy J (8 April 2021). "Coronavirus | Indian 'double mutant' strain named B.1.617". The Hindu.
- ^ "India's variant-fuelled second wave coincided with spike in infected flights landing in Canada". Toronto Sun. 10 April 2021. Retrieved 10 April 2021.
- ^ Edara, Venkata-Viswanadh; Pinsky, Benjamin A.; Suthar, Mehul S.; Lai, Lilin; Davis-Gardner, Meredith E.; Floyd, Katharine; Flowers, Maria W.; Wrammert, Jens; Hussaini, Laila; Ciric, Caroline Rose; Bechnak, Sarah; Stephens, Kathy; Graham, Barney S.; Bayat Mokhtari, Elham; Mudvari, Prakriti; Boritz, Eli; Creanga, Adrian; Pegu, Amarendra; Derrien-Colemyn, Alexandrine; Henry, Amy R.; Gagne, Matthew; Douek, Daniel C.; Sahoo, Malaya K.; Sibai, Mamdouh; Solis, Daniel; Webby, Richard J.; Jeevan, Trushar; Fabrizio, Thomas P. (12 August 2021). "Infection and Vaccine-Induced Neutralizing-Antibody Responses to the SARS-CoV-2 B.1.617 Variants". New England Journal of Medicine. 385 (7): 664–666. doi:10.1056/NEJMc2107799.
- ^ Planas, Delphine; Veyer, David; Baidaliuk, Artem; Staropoli, Isabelle; Guivel-Benhassine, Florence; Rajah, Maaran Michael; Planchais, Cyril; Porrot, Françoise; Robillard, Nicolas; Puech, Julien; Prot, Matthieu; Gallais, Floriane; Gantner, Pierre; Velay, Aurélie; Le Guen, Julien; Kassis-Chikhani, Najiby; Edriss, Dhiaeddine; Belec, Laurent; Seve, Aymeric; Courtellemont, Laura; Péré, Hélène; Hocqueloux, Laurent; Fafi-Kremer, Samira; Prazuck, Thierry; Mouquet, Hugo; Bruel, Timothée; Simon-Lorière, Etienne; Rey, Felix A.; Schwartz, Olivier (12 August 2021). "Reduced sensitivity of SARS-CoV-2 variant Delta to antibody neutralization". Nature. 596 (7871): 276–280. doi:10.1038/s41586-021-03777-9.
- ^ Cite error: The named reference
617BBCwas invoked but never defined (see the help page). - ^ "Confirmed cases of COVID-19 variants identified in UK". Public Health England. 15 April 2021. Retrieved 16 April 2021.
- ^ "expert reaction to VUI-21APR-02/B.1.617.2 being classified by PHE as a variant of concern". Science Media Centre. 7 May 2021. Retrieved 15 May 2021.
- ^ Khoury DS, Cromer D, Reynaldi A, Schlub TE, Wheatley AK, Juno JA, et al. (17 May 2021). "Neutralizing antibody levels are highly predictive of immune protection from symptomatic SARS-CoV-2 infection". Nature Medicine. 27 (7): 1205–1211. doi:10.1038/s41591-021-01377-8. ISSN 1546-170X. PMID 34002089. S2CID 234769053.
- ^ Greenberger, Lee M.; Saltzman, Larry A.; Senefeld, Jonathon W.; Johnson, Patrick W.; DeGennaro, Louis J.; Nichols, Gwen L. (August 9, 2021). "Antibody response to SARS-CoV-2 vaccines in patients with hematologic malignancies". Cancer Cell. 39 (8): 1031–1033. doi:10.1016/j.ccell.2021.07.012. PMID 34331856 – via www.cell.com.