Liver: Difference between revisions
→Gene and protein expression: small change gramm |
→Disease: added the large frequencies with which the hepatitis viruses affect the liver |
||
| Line 160: | Line 160: | ||
The liver is a vital organ and supports almost every other organ in the body. Because of its strategic location and multidimensional functions, the liver is also prone to many diseases.<ref>[http://digestive.niddk.nih.gov/ddiseases/pubs/cirrhosis/ Cirrhosis Overview] National Digestive Diseases Information Clearinghouse. Retrieved 2010-01-22</ref> The bare area of the liver is a site that is vulnerable to the passing of infection from the abdominal cavity to the [[thoracic cavity]]. |
The liver is a vital organ and supports almost every other organ in the body. Because of its strategic location and multidimensional functions, the liver is also prone to many diseases.<ref>[http://digestive.niddk.nih.gov/ddiseases/pubs/cirrhosis/ Cirrhosis Overview] National Digestive Diseases Information Clearinghouse. Retrieved 2010-01-22</ref> The bare area of the liver is a site that is vulnerable to the passing of infection from the abdominal cavity to the [[thoracic cavity]]. |
||
[[Hepatitis]] is a common condition of inflammation of the liver. The most usual cause of this is [[viral hepatitis|viral]], and the most common of these infections are [[hepatitis A]], [[hepatitis B|B]], [[hepatitis C|C]], [[hepatitis D|D]], and [[hepatitis E|E]]. Some of these infections are [[sexually transmitted diseases|sexually transmitted]]. Inflammation can also be caused by other viruses in the [[Herpesviridae]] family such as the ''[[herpes simplex virus]]''. |
[[Hepatitis]] is a common condition of inflammation of the liver. The most usual cause of this is [[viral hepatitis|viral]], and the most common of these infections are [[hepatitis A]], [[hepatitis B|B]], [[hepatitis C|C]], [[hepatitis D|D]], and [[hepatitis E|E]]. Some of these infections are [[sexually transmitted diseases|sexually transmitted]]. Inflammation can also be caused by other viruses in the [[Herpesviridae]] family such as the ''[[herpes simplex virus]]''. Chronic (rather than acute) infection with hepatitis B virus or hepatitis C virus is the main cause of [[liver cancer]].<ref>[http://www.webmd.com/hepatitis/ Hepatitis A, B, and C Center: Symptoms, Causes, Tests, Transmission, and Treatments]. Webmd.com (2005-08-19). Retrieved on 2016-05-10.</ref> Globally, about 248 million individuals are chronically infected with HBV (with 843,724 in the U.S.)<ref name="pmid26231459">{{cite journal |vauthors=Schweitzer A, Horn J, Mikolajczyk RT, Krause G, Ott JJ |title=Estimations of worldwide prevalence of chronic hepatitis B virus infection: a systematic review of data published between 1965 and 2013 |journal=Lancet |volume=386 |issue=10003 |pages=1546–55 |year=2015 |pmid=26231459 |doi=10.1016/S0140-6736(15)61412-X |url=}}</ref> and 142 are chronically infected with HCV<ref name=Global>{{cite journal |vauthors= |title=Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015 |journal=Lancet |volume=388 |issue=10053 |pages=1545–1602 |year=2016 |pmid=27733282 |pmc=5055577 |doi=10.1016/S0140-6736(16)31678-6 |url=}}</ref> (with 2.7 million in the U.S.<ref name="urlwww.hepatitisc.uw.edu">{{cite web |url=https://www.hepatitisc.uw.edu/pdf/screening-diagnosis/epidemiology-us/core-concept/all |title=www.hepatitisc.uw.edu |format= |work= |accessdate=}}</ref>). Globally there are about 114 and 20 million cases of hepatitis A<ref name=Global /> and hepatitis E<ref name="urlWHO | Hepatitis E">{{cite web |url=http://www.who.int/mediacentre/factsheets/fs280/en/ |title=WHO | Hepatitis E |format= |work= |accessdate=}}</ref> respectively, but these generally resolve, and do not become chronic (see [[Hepatitis A]], [[Hepatitis E]]). Hepatitis D virus is a "satellite" of hepatitis B virus (can only infect in the presence of hepatitis B), and co-infects nearly 20 million people with hepatitis B, globally<ref name="pmid16903225">{{cite journal |vauthors=Dény P |title=Hepatitis delta virus genetic variability: from genotypes I, II, III to eight major clades? |journal=Curr. Top. Microbiol. Immunol. |volume=307 |issue= |pages=151–71 |year=2006 |pmid=16903225 |doi= |url=}}</ref> (see [[Hepatitis D]]). |
||
[[Hepatic encephalopathy]] is caused by an accumulation of toxins in the bloodstream that are normally removed by the liver. This condition can result in coma and can prove fatal. |
[[Hepatic encephalopathy]] is caused by an accumulation of toxins in the bloodstream that are normally removed by the liver. This condition can result in coma and can prove fatal. |
||
Revision as of 22:55, 22 December 2017
| Liver | |
|---|---|
 The human liver is located in the upper right abdomen | |
 Location of human liver (in red) | |
| Details | |
| Precursor | Foregut |
| System | Digestive system |
| Artery | Hepatic artery |
| Vein | Hepatic vein and hepatic portal vein |
| Nerve | Celiac ganglia and vagus nerve[1] |
| Identifiers | |
| Latin | Jecur, iecur |
| Greek | Hepar (ἧπαρ) root hepat- (ἡπατ-) |
| MeSH | D008099 |
| TA98 | A05.8.01.001 |
| TA2 | 3023 |
| FMA | 7197 |
| Anatomical terminology | |
The liver, an organ only found in vertebrates, detoxifies various metabolites, synthesizes proteins, and produces biochemicals necessary for digestion.[2][3][4] In humans, it is located in the upper right quadrant of the abdomen, below the diaphragm. It also plays a role in metabolism, regulation of glycogen storage, decomposition of red blood cells and hormone production.[4]
The liver, an accessory digestive gland, produces bile, an alkaline compound which helps breakdown fat. Bile aids in digestion via the emulsification of lipids. The gallbladder, a small pouch that sits just under the liver, stores bile produced by the liver.[5] The liver's highly specialized tissue consisting of mostly hepatocytes regulates a wide variety of high-volume biochemical reactions, including the synthesis and breakdown of small and complex molecules, many of which are necessary for normal vital functions.[6] Estimates regarding the organ's total number of functions vary, but textbooks generally cite it being around 500.[7]
Terminology related to the liver often starts in hepat- from ἡπατο-, the Greek word for liver.[8]
There is currently no way to compensate for the absence of liver function in the long term, although liver dialysis techniques can be used in the short term. Artificial livers are yet to be developed to promote long-term replacement in the absence of the liver. As of 2017[update],[9] liver transplantation is the only option for complete liver failure.
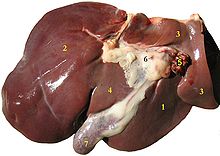
Structure
The liver is a reddish-brown wedge-shaped organ with four lobes of unequal size and shape. A human liver normally weighs 1.44–1.66 kg (3.2–3.7 lb),[10] and has a width of about 15 cm.[11] It is both the heaviest internal organ and the largest gland in the human body. Located in the right upper quadrant of the abdominal cavity, it rests just below the diaphragm, to the right of the stomach and overlies the gallbladder.[5]
The liver is connected to two large blood vessels: the hepatic artery and the portal vein. The hepatic artery carries oxygen-rich blood from the aorta, whereas the portal vein carries blood rich in digested nutrients from the entire gastrointestinal tract and also from the spleen and pancreas.[9] These blood vessels subdivide into small capillaries known as liver sinusoids, which then lead to a lobule.
Lobules are the functional units of the liver. Each lobule is made up of millions of hepatic cells (hepatocytes) which are the basic metabolic cells. The lobules are held together by a fine dense irregular fibroelastic connective tissue layer which extends into the structure of the liver, by accompanying the vessels (veins and arteries), ducts and nerves through the hepatic portal, as a fibrous capsule called Glisson's capsule.[12] The whole surface of the liver is covered in a serous coat derived from peritoneum and this has an inner fibrous coat (Glisson's capsule) to which it is firmly adhered. The fibrous coat is of areolar tissue and follows the vessels and ducts to support them.[13]
Gross anatomy
Lobes

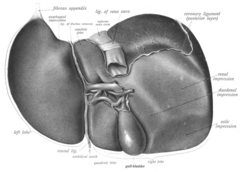
The liver is grossly divided into two parts when viewed from above – a right and a left lobe, seen and four when viewed from below (left, right, caudate and quadrate lobes).[14]
The falciform ligament, divides the liver into a left and right lobe. From below, the two additional lobes are located between the right and left lobes, one in front of the other. A line can be imagined running from the left of the vena cava and all the way forward to divide the liver and gallbladder into two halves.[15] This line is called "Cantlie's line".[16]
Other anatomical landmarks include the ligamentum venosum and the round ligament of the liver (ligamentum teres), which further divide the left side of the liver in two sections. An important anatomical landmark, the porta hepatis, divides this left portion into four segments, which can be numbered starting at the caudate lobe as I in an anticlockwise manner. From this parietal view, seven segments can be seen, because the eighth segment is only visible in the visceral view.[17]
Surfaces
On the diaphragmatic surface, apart from a small triangular bare area where it connects to the diaphragm, the liver is covered by a thin double-layered membrane, the peritoneum, that helps to reduce friction against other organs.[18] This surface covers the convex shape of the two lobes where it accommodates the shape of the diaphragm. The peritoneum folds back on itself to form the falciform ligament and the right and left triangular ligaments.[19]
These peritoneal ligaments are not related to the anatomic ligaments in joints, and the right and left triangular ligaments have no known functional importance, though they serve as surface landmarks.[19] The falciform ligament functions to attach the liver to the posterior portion of the anterior body wall.
The visceral surface or inferior surface, is uneven and concave. It is covered in peritoneum apart from where it attaches the gallbladder and the porta hepatis.[18]
Impressions

There are several impressions on the surface of the liver which accommodate the various adjacent structures and organs. Underneath the right lobe and to the right of the gallbladder fossa, are two impressions, one behind the other and separated by a ridge. The one in front is a shallow colic impression, formed by the hepatic flexure and the one behind is a deeper renal impression accommodating part of the right kidney and part of the suprarenal gland.[20]
The suprarenal impression is a small triangular depressed area on the liver. It is located close to the right of the fossa between the bare area and the caudate lobe and immediately above the renal impression. The greater part of the suprarenal impression is devoid of peritoneum and it lodges the right suprarenal gland.[21]
Medial to the renal impression is a third and slightly marked impression, lying between it and the neck of the gall-bladder. This is caused by the descending portion of the duodenum, and is known as the duodenal impression.[21]
The inferior surface of the left lobe of the liver presents behind and to the left the gastric impression.[21] This is moulded over the upper front surface of the stomach, and to the right of this is a rounded eminence, the tuber omentale, which fits into the concavity of the lesser curvature of the stomach and lies in front of the anterior layer of the lesser omentum.
Microscopic anatomy
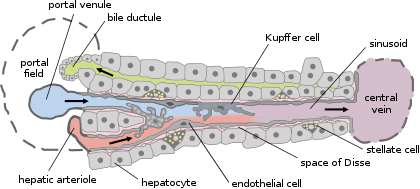


Microscopically, each liver lobe is seen to be made up of hepatic lobules. The lobules are roughly hexagonal, and consist of plates of hepatocytes radiating from a central vein.[22][page needed]The central vein joins to the hepatic vein to carry blood out from the liver. A distinctive component of a lobule is the portal triad, which can be found running along each of the lobule's corners. The portal triad, misleadingly named, consists of five structures: a branch of the hepatic artery, a branch of the hepatic portal vein, and a bile duct, as well as lymphatic vessels and a branch of the vagus nerve.[23] Between the hepatocyte plates are liver sinusoids, which are enlarged capillaries through which blood from the hepatic portal vein and hepatic artery enters via the portal triads, then drains to the central vein.[22][page needed]
Histology, the study of microscopic anatomy, shows two major types of liver cell: parenchymal cells and non-parenchymal cells. 70–85% of the liver volume is occupied by parenchymal hepatocytes. Non-parenchymal cells constitute 40% of the total number of liver cells but only 6.5% of its volume.[24] The liver sinusoids are lined with two types of cell, sinusoidal endothelial cells, and phagocytic Kupffer cells.[25] Hepatic stellate cells are non-parenchymal cells found in the perisinusoidal space, between a sinusoid and a hepatocyte.[24] Additionally, intrahepatic lymphocytes are often present in the sinusoidal lumen.[24]
Functional anatomy
The central area or hilum, known as the porta hepatis is where the common bile duct, hepatic portal vein, and the hepatic artery proper enter the liver. The duct, vein, and artery divide into left and right branches, and the areas of the liver supplied by these branches constitute the functional left and right lobes. The functional lobes are separated by the imaginary plane, Cantlie's line, joining the gallbladder fossa to the inferior vena cava. The plane separates the liver into the true right and left lobes. The middle hepatic vein also demarcates the true right and left lobes. The right lobe is further divided into an anterior and posterior segment by the right hepatic vein. The left lobe is divided into the medial and lateral segments by the left hepatic vein.
Couinaud classification system

In the widely used Couinaud (or "French") system, the functional lobes are further divided into a total of eight subsegments based on a transverse plane through the bifurcation of the main portal vein.[26] The caudate lobe is a separate structure which receives blood flow from both the right- and left-sided vascular branches.[27][28] The Couinaud classification of liver anatomy divides the liver into eight functionally independent segments. Each segment has its own vascular inflow, outflow and biliary drainage. In the centre of each segment there is a branch of the portal vein, hepatic artery and bile duct. In the periphery of each segment there is vascular outflow through the hepatic veins.[29] The classification system uses the vascular supply in the liver to separate the functional units (numbered I to VIII), with unit 1 the caudate lobe receive its supply from both the right and the left branches of portal vein. It contains one or more hepatic veins which drain directly into the IVC.[26] The remainder of the units (II to VIII) are numbered in a clockwise fashion:[29]
Gene and protein expression
Approximately 20,000 protein coding genes are expressed in human cells and 60% of these genes are expressed in a normal, adult liver.[30][31] Over 400 genes are more specifically expressed in the liver, with some 150 genes highly specific for liver tissue. A large fraction of the corresponding liver specific proteins are mainly expressed in hepatocytes and secreted into the blood and constitute plasma proteins. Other liver specific proteins are certain liver enzymes such as HAO1 and RDH16, proteins involved in bile synthesis such as BAAT and SLC27A5, and transporter proteins involved in the metabolism of drugs, such as ABCB11 and SLC2A2. Examples of highly liver-specific proteins include apolipoprotein A II, coagulation factors F2 and F9, complement factor related proteins and the fibrinogen beta chain protein.[32]
Development
Organogenesis, the development of the organs takes place from the third to the eighth week during embryogenesis. The origins of the liver lie in both the ventral portion of the foregut endoderm (endoderm being one of the 3 embryonic germ layers) and the constituents of the adjacent septum transversum mesenchyme. In the human embryo, the hepatic diverticulum is the tube of endoderm that extends out from the foregut into the surrounding mesenchyme. The mesenchyme of septum transversum induces this endoderm to proliferate, to branch, and to form the glandular epithelium of the liver. A portion of the hepatic diverticulum (that region closest to the digestive tube) continues to function as the drainage duct of the liver, and a branch from this duct produces the gallbladder.[33] Besides signals from the septum transversum mesenchyme, fibroblast growth factor from the developing heart also contributes to hepatic competence, along with retinoic acid emanating from the lateral plate mesoderm. The hepatic endodermal cells undergo a morphological transition from columnar to pseudostratified resulting in thickening into the early liver bud. Their expansion forms a population of the bipotential hepatoblasts.[34] Hepatic stellate cells are derived from mesenchyme.[35]
After migration of hepatoblasts into the septum transversum mesenchyme, the hepatic architecture begins to be established, with liver sinusoids and bile canaliculi appearing. The liver bud separates into the lobes. The left umbilical vein becomes the ductus venosus and the right vitelline vein becomes the portal vein. The expanding liver bud is colonized by hematopoietic cells. The bipotential hepatoblasts begin differentiating into biliary epithelial cells and hepatocytes. The biliary epithelial cells differentiate from hepatoblasts around portal veins, first producing a monolayer, and then a bilayer of cuboidal cells. In ductal plate, focal dilations emerge at points in the bilayer, become surrounded by portal mesenchyme, and undergo tubulogenesis into intrahepatic bile ducts. Hepatoblasts not adjacent to portal veins instead differentiate into hepatocytes and arrange into cords lined by sinudoidal epithelial cells and bile canaliculi. Once hepatoblasts are specified into hepatocytes and undergo further expansion, they begin acquiring the functions of a mature hepatocyte, and eventually mature hepatocytes appear as highly polarized epithelial cells with abundant glycogen accumulation. In the adult liver, hepatocytes are not equivalent, with position along the portocentrovenular axis within a liver lobule dictating expression of metabolic genes involved in drug metabolism, carbohydrate metabolism, ammonia detoxification, and bile production and secretion. WNT/β-catenin has now been identified to be playing a key role in this phenomenon.[34]
At birth the liver comprises roughly 4% of body weight and is at average 120 g. Over the course of further development, it will increase to 1.4–1.6 kg but will only take up 2.5–3.5% of body weight.[36]
Fetal blood supply
In the growing fetus, a major source of blood to the liver is the umbilical vein which supplies nutrients to the growing fetus. The umbilical vein enters the abdomen at the umbilicus, and passes upward along the free margin of the falciform ligament of the liver to the inferior surface of the liver. There it joins with the left branch of the portal vein. The ductus venosus carries blood from the left portal vein to the left hepatic vein and then to the inferior vena cava, allowing placental blood to bypass the liver.
In the fetus, the liver does not perform the normal digestive processes and filtration of the infant liver because nutrients are received directly from the mother via the placenta. The fetal liver releases some blood stem cells that migrate to the fetal thymus, creating the T-cells or T-lymphocytes. After birth, the formation of blood stem cells shifts to the red bone marrow.
After two to five days, the umbilical vein and ductus venosus are completely obliterated; the former becomes the round ligament of liver and the latter becomes the ligamentum venosum. In the disorders of cirrhosis and portal hypertension, the umbilical vein can open up again.
Physiology
The various functions of the liver are carried out by the liver cells or hepatocytes. The liver is thought to be responsible for up to 500 separate functions, usually in combination with other systems and organs. Currently, there is no artificial organ or device capable of reproducing all the functions of the liver. Some functions can be carried out by liver dialysis, an experimental treatment for liver failure.
Blood supply

The liver receives a dual blood supply from the hepatic portal vein and hepatic arteries. The hepatic portal vein delivers approximately 75% of the liver's blood supply, and carries venous blood drained from the spleen, gastrointestinal tract, and its associated organs. The hepatic arteries supply arterial blood to the liver, accounting for the remaining quarter of its blood flow. Oxygen is provided from both sources; approximately half of the liver's oxygen demand is met by the hepatic portal vein, and half is met by the hepatic arteries.[37]
Blood flows through the liver sinusoids and empties into the central vein of each lobule. The central veins coalesce into hepatic veins, which leave the liver and drain into the inferior vena cava.[23]
Biliary flow

The biliary tract is derived from the branches of the bile ducts. The biliary tract, also known as the biliary tree, is the path by which bile is secreted by the liver then transported to the first part of the small intestine, the duodenum. The bile produced in the liver is collected in bile canaliculi, small grooves between the faces of adjacent hepatocytes. The canaliculi radiate to the edge of the liver lobule, where they merge to form bile ducts. Within the liver, these ducts are termed intrahepatic bile ducts, and once they exit the liver they are considered extrahepatic. The intrahepatic ducts eventually drain into the right and left hepatic ducts, which exit the liver at the transverse fissure, and merge to form the common hepatic duct. The cystic duct from the gallbladder joins with the common hepatic duct to form the common bile duct.[23]
Bile either drains directly into the duodenum via the common bile duct, or is temporarily stored in the gallbladder via the cystic duct. The common bile duct and the pancreatic duct enter the second part of the duodenum together at the hepatopancreatic ampulla, also known as the ampulla of Vater.
Synthesis
The liver plays a major role in carbohydrate, protein, amino acid, and lipid metabolism.
The liver performs several roles in carbohydrate metabolism: The liver synthesizes and stores approximately 100g of glycogen via glycogenesis, the formation of glycogen from glucose. When needed, the liver releases glucose into the blood by performing glycogenolysis, the breakdown of glycogen into glucose.[38] The liver is also responsible for gluconeogenesis, which is the synthesis of glucose from certain amino acids, lactate or glycerol. Adipose and liver cells produce glycerol by breakdown of fat, which the liver uses for gluconeogenesis.[38]
The liver is responsible for the mainstay of protein metabolism, synthesis as well as degradation. It is also responsible for a large part of amino acid synthesis. The liver plays a role in the production of clotting factors as well as red blood cell production. Some of the proteins synthesized by the liver include coagulation factors I (fibrinogen), II (prothrombin), V, VII, VIII, IX, X, XI, XIII, as well as protein C, protein S and antithrombin. In the first trimester fetus, the liver is the main site of red blood cell production. By the 32nd week of gestation, the bone marrow has almost completely taken over that task. The liver is a major site of production for thrombopoietin, a glycoprotein hormone that regulates the production of platelets by the bone marrow.[39]
The liver plays several roles in lipid metabolism: it performs cholesterol synthesis, lipogenesis, the production of triglycerides, and a bulk of the body's lipoproteins are synthesized in the liver.
The liver plays a key role in digestion, as it produces and excretes bile (a yellowish liquid) required for emulsifying fats and help the absorption of vitamin K from the diet. Some of the bile drains directly into the duodenum, and some is stored in the gallbladder.
The liver also produces insulin-like growth factor 1 (IGF-1), a polypeptide protein hormone that plays an important role in childhood growth and continues to have anabolic effects in adults.
Breakdown
The liver is responsible for the breakdown of insulin and other hormones. The liver breaks down bilirubin via glucuronidation, facilitating its excretion into bile. The liver is responsible for the breakdown and excretion of many waste products. It plays a key role in breaking down or modifying toxic substances (e.g., methylation) and most medicinal products in a process called drug metabolism. This sometimes results in toxication, when the metabolite is more toxic than its precursor. Preferably, the toxins are conjugated to avail excretion in bile or urine. The liver breaks down ammonia into urea as part of the urea cycle, and the urea is excreted in the urine.[22]
Other functions
- The liver stores a multitude of substances, including glucose (in the form of glycogen), vitamin A (1–2 years' supply), vitamin D (1–4 months' supply)[citation needed], vitamin B12 (3–5 years' supply),[40] vitamin K, iron, and copper.
- The liver is responsible for immunological effects—the mononuclear phagocyte system of the liver contains many immunologically active cells, acting as a 'sieve' for antigens carried to it via the portal system.
- The liver produces albumin, the most abundant protein in blood serum. It is essential in the maintenance of oncotic pressure, and acts as a transport for fatty acids and steroid hormones.
- The liver synthesizes angiotensinogen, a hormone that is responsible for raising the blood pressure when activated by renin, an enzyme that is released when the kidney senses low blood pressure.
- The liver produces the enzyme catalase in order to break down hydrogen peroxide, a very toxic substance due to it being a powerful oxidising agent, into water and oxygen.
Relation to medicine and pharmacology
The oxidative capacity of the liver decreases with aging and therefore any medications that require oxidation (for instance, benzodiazepines) are more likely to accumulate to toxic levels. However, medications with shorter half-lives, such as lorazepam and oxazepam, are preferred in most cases when benzodiazepines are required in regard to geriatric medicine.
Clinical significance
Disease

The liver is a vital organ and supports almost every other organ in the body. Because of its strategic location and multidimensional functions, the liver is also prone to many diseases.[41] The bare area of the liver is a site that is vulnerable to the passing of infection from the abdominal cavity to the thoracic cavity.
Hepatitis is a common condition of inflammation of the liver. The most usual cause of this is viral, and the most common of these infections are hepatitis A, B, C, D, and E. Some of these infections are sexually transmitted. Inflammation can also be caused by other viruses in the Herpesviridae family such as the herpes simplex virus. Chronic (rather than acute) infection with hepatitis B virus or hepatitis C virus is the main cause of liver cancer.[42] Globally, about 248 million individuals are chronically infected with HBV (with 843,724 in the U.S.)[43] and 142 are chronically infected with HCV[44] (with 2.7 million in the U.S.[45]). Globally there are about 114 and 20 million cases of hepatitis A[44] and hepatitis E[46] respectively, but these generally resolve, and do not become chronic (see Hepatitis A, Hepatitis E). Hepatitis D virus is a "satellite" of hepatitis B virus (can only infect in the presence of hepatitis B), and co-infects nearly 20 million people with hepatitis B, globally[47] (see Hepatitis D).
Hepatic encephalopathy is caused by an accumulation of toxins in the bloodstream that are normally removed by the liver. This condition can result in coma and can prove fatal.
Other disorders caused by excessive alcohol consumption are grouped under alcoholic liver diseases and these include alcoholic hepatitis, fatty liver, and cirrhosis. Factors contributing to the development of alcoholic liver diseases are not only the quantity and frequency of alcohol consumption, but can also include gender, genetics, and liver insult.
Liver damage can also be caused by drugs, particularly paracetamol and drugs used to treat cancer. A rupture of the liver can be caused by a liver shot used in combat sports.
Budd–Chiari syndrome is a condition caused by blockage of the hepatic veins (including thrombosis) that drain the liver. It presents with the classical triad of abdominal pain, ascites and liver enlargement.[48]
Primary biliary cholangitis is an autoimmune disease of the liver.[49][50] It is marked by slow progressive destruction of the small bile ducts of the liver, with the intralobular ducts (Canals of Hering) affected early in the disease.[51] When these ducts are damaged, bile and other toxins build up in the liver (cholestasis) and over time damages the liver tissue in combination with ongoing immune related damage. This can lead to scarring (fibrosis) and cirrhosis. Cirrhosis increases the resistance to blood flow in the liver, and can result in portal hypertension. Congested anastomoses between the portal venous system and the systemic circulation, can be a subsequent condition.
Many diseases of the liver are accompanied by jaundice caused by increased levels of bilirubin in the system. The bilirubin results from the breakup of the hemoglobin of dead red blood cells; normally, the liver removes bilirubin from the blood and excretes it through bile.
There are also many pediatric liver diseases, including biliary atresia, alpha-1 antitrypsin deficiency, alagille syndrome, progressive familial intrahepatic cholestasis, Langerhans cell histiocytosis and hepatic hemangioma a benign tumour the most common type of liver tumour, thought to be congenital. A genetic disorder causing multiple cysts to form in the liver tissue, usually in later life, and usually asymptomatic, is polycystic liver disease. Diseases that interfere with liver function will lead to derangement of these processes. However, the liver has a great capacity to regenerate and has a large reserve capacity. In most cases, the liver only produces symptoms after extensive damage.
Hepatomegaly refers to an enlarged liver and can be due to many causes. It can be palpated in a liver span measurement.
Liver diseases may be diagnosed by liver function tests–blood tests that can identify various markers. For example, acute-phase reactants are produced by the liver in response to injury or inflammation.
Symptoms
The classic symptoms of liver damage include the following:
- Pale stools occur when stercobilin, a brown pigment, is absent from the stool. Stercobilin is derived from bilirubin metabolites produced in the liver.
- Dark urine occurs when bilirubin mixes with urine
- Jaundice (yellow skin and/or whites of the eyes) This is where bilirubin deposits in skin, causing an intense itch. Itching is the most common complaint by people who have liver failure. Often this itch cannot be relieved by drugs.
- Swelling of the abdomen, ankles and feet occurs because the liver fails to make albumin.
- Excessive fatigue occurs from a generalized loss of nutrients, minerals and vitamins.
- Bruising and easy bleeding are other features of liver disease. The liver makes substances which help prevent bleeding. When liver damage occurs, these substances are no longer present and severe bleeding can occur.[52]
- Pain in the upper right quadrant can result from the stretching of Glisson's capsule in conditions of hepatitis and pre-eclampsia.
Diagnosis
The diagnosis of liver disease is made by liver function tests, groups of blood tests, that can readily show the extent of liver damage. If infection is suspected, then other serological tests will be carried out. A physical examination of the liver can only reveal its size and any tenderness, and some form of imaging such as an ultrasound or CT scan may also be needed.[53] Sometimes a liver biopsy will be necessary, and a tissue sample is taken through a needle inserted into the skin just below the rib cage. This procedure may be helped by a radiologist providing ultrasound guidance.[54]
-
Axial CT image showing anomalous hepatic veins coursing on the subcapsular anterior surface of the liver.[55]
-
Maximum intensity projection (MIP) CT image as viewed anteriorly showing the anomalous hepatic veins coursing on the anterior surface of the liver
-
Lateral MIP view in the same patient
-
A CT scan in which the liver and portal vein are shown.
Liver regeneration
The liver is the only human internal organ capable of natural regeneration of lost tissue; as little as 25% of a liver can regenerate into a whole liver.[56] This is, however, not true regeneration but rather compensatory growth in mammals.[57] The lobes that are removed do not regrow and the growth of the liver is a restoration of function, not original form. This contrasts with true regeneration where both original function and form are restored. In some other species, such as fish, the liver undergoes true regeneration by restoring both shape and size of the organ.[58] In the liver, large areas of the tissues are formed but for the formation of new cells there must be sufficient amount of material so the circulation of the blood becomes more active.[59]
This is predominantly due to the hepatocytes re-entering the cell cycle. That is, the hepatocytes go from the quiescent G0 phase to the G1 phase and undergo mitosis. This process is activated by the p75 receptors.[60] There is also some evidence of bipotential stem cells, called hepatic oval cells or ovalocytes (not to be confused with oval red blood cells of ovalocytosis), which are thought to reside in the canals of Hering. These cells can differentiate into either hepatocytes or cholangiocytes. Cholangiocytes are the epithelial lining cells of the bile ducts.[61] They are cuboidal epithelium in the small interlobular bile ducts, but become columnar and mucus secreting in larger bile ducts approaching the porta hepatis and the extrahepatic ducts. Research is being carried out on the use of stem cells for the generation of an artificial liver.
Scientific and medical works about liver regeneration often refer to the Greek Titan Prometheus who was chained to a rock in the Caucasus where, each day, his liver was devoured by an eagle, only to grow back each night. The myth suggests the ancient Greeks may have known about the liver’s remarkable capacity for self-repair.[62]
Liver transplantation
Human liver transplants were first performed by Thomas Starzl in the United States and Roy Calne in Cambridge, England in 1963 and 1967, respectively.
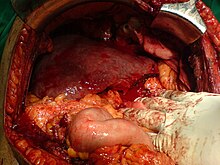
Liver transplantation is the only option for those with irreversible liver failure. Most transplants are done for chronic liver diseases leading to cirrhosis, such as chronic hepatitis C, alcoholism, autoimmune hepatitis, and many others. Less commonly, liver transplantation is done for fulminant hepatic failure, in which liver failure occurs over days to weeks.
Liver allografts for transplant usually come from donors who have died from fatal brain injury. Living donor liver transplantation is a technique in which a portion of a living person's liver is removed (hepatectomy) and used to replace the entire liver of the recipient. This was first performed in 1989 for pediatric liver transplantation. Only 20 percent of an adult's liver (Couinaud segments 2 and 3) is needed to serve as a liver allograft for an infant or small child.
More recently, adult-to-adult liver transplantation has been done using the donor's right hepatic lobe, which amounts to 60 percent of the liver. Due to the ability of the liver to regenerate, both the donor and recipient end up with normal liver function if all goes well. This procedure is more controversial, as it entails performing a much larger operation on the donor, and indeed there have been at least two donor deaths out of the first several hundred cases. A recent publication has addressed the problem of donor mortality, and at least 14 cases have been found.[63] The risk of postoperative complications (and death) is far greater in right-sided operations than that in left-sided operations.
With the recent advances of noninvasive imaging, living liver donors usually have to undergo imaging examinations for liver anatomy to decide if the anatomy is feasible for donation. The evaluation is usually performed by multidetector row computed tomography (MDCT) and magnetic resonance imaging (MRI). MDCT is good in vascular anatomy and volumetry. MRI is used for biliary tree anatomy. Donors with very unusual vascular anatomy, which makes them unsuitable for donation, could be screened out to avoid unnecessary operations.
-
MDCT image. Arterial anatomy contraindicated for liver donation
-
MDCT image. Portal venous anatomy contraindicated for liver donation
-
MDCT image. 3D image created by MDCT can clearly visualize the liver, measure the liver volume, and plan the dissection plane to facilitate the liver transplantation procedure.
-
Phase contrast CT image. Contrast is perfusing the right liver but not the left due to a left portal vein thrombus.
Society and culture
In Greek mythology, Prometheus was punished by the gods for revealing fire to humans, by being chained to a rock where a vulture (or an eagle) would peck out his liver, which would regenerate overnight. (The liver is the only human internal organ that actually can regenerate itself to a significant extent.) Many ancient peoples of the Near East and Mediterranean areas practiced a type of divination called haruspicy, where they tried to obtain information by examining the livers of sheep and other animals.
In Plato, and in later physiology, the liver was thought to be the seat of the darkest emotions (specifically wrath, jealousy and greed) which drive men to action.[64] The Talmud (tractate Berakhot 61b) refers to the liver as the seat of anger, with the gallbladder counteracting this.
The Persian, Urdu, and Hindi languages (جگر or जिगर or jigar) refer to the liver in figurative speech to indicate courage and strong feelings, or "their best"; e.g., "This Mecca has thrown to you the pieces of its liver!".[65] The term jan e jigar, literally "the strength (power) of my liver", is a term of endearment in Urdu. In Persian slang, jigar is used as an adjective for any object which is desirable, especially women. In the Zulu language, the word for liver (isibindi) is the same as the word for courage.
The legend of Liver-Eating Johnson says that he would cut out and eat the liver of each man killed after dinner.
In the motion picture The Message, Hind bint Utbah is implied or portrayed eating the liver of Hamza ibn ‘Abd al-Muttalib during the Battle of Uhud. Although there are narrations that suggest that Hind did "taste", rather than eat, the liver of Hamza, the authenticity of these narrations has to be questioned.
On November 26, 1987, the city of Ferrol, Spain, inaugurated what is believed to be the only monument to the liver in the world. The then-mayor, Jaime Quintanilla, also happened to be a doctor, and thought appropriate to promote the monument. At an approximate cost of $3.200, the monument stands in the village of Balón. A plaque reads (In Galician language, free translation): "The Liver [is the] basis of Life", and below "Through History, Mankind tried to cure all illness. By helping it on this duty, you are doing a great job. We are grateful for it".[66]
Food
The liver of mammals, fowl, and fish are commonly eaten as food by humans. Domestic pig, ox, lamb, calf, chicken, and goose livers are widely available from butchers and supermarkets.
Liver can be baked, boiled, broiled, fried, stir-fried, or eaten raw (asbeh nayeh or sawda naye in Lebanese cuisine, or liver sashimi in Japanese cuisine. In many preparations, pieces of liver are combined with pieces of meat or kidneys, like in the various forms of Middle Eastern mixed grill (e.g. meurav Yerushalmi). Liver is often made into spreads. Well-known examples include liver pâté, foie gras, chopped liver, and leverpastej. Liver sausages such as Braunschweiger and liverwurst are also a valued meal. Liver sausages may also be used as spreads. A traditional South African delicacy, namely skilpadjies, is made of minced lamb's liver wrapped in netvet (caul fat), and grilled over an open fire.
Animal livers are rich in iron and vitamin A, and cod liver oil is commonly used as a dietary supplement. Traditionally, some fish livers were valued as food, especially the stingray liver. It was used to prepare delicacies, such as poached skate liver on toast in England, as well as the beignets de foie de raie and foie de raie en croute in French cuisine.[67]
Other animals
The liver is found in all vertebrates, and is typically the largest visceral (internal) organ. Its form varies considerably in different species, and is largely determined by the shape and arrangement of the surrounding organs. Nonetheless, in most species it is divided into right and left lobes; exceptions to this general rule include snakes, where the shape of the body necessitates a simple cigar-like form. The internal structure of the liver is broadly similar in all vertebrates.[68]
An organ sometimes referred to as a liver is found associated with the digestive tract of the primitive chordate Amphioxus. Although it performs many functions of a liver, it is not considered a true liver but a homolog of the vertebrate liver.[69][70][71] The amphioxus hepatic caecum produces the liver-specific proteins vitellogenin, antithrombin, plasminogen, alanine aminotransferase, and insulin/Insulin-like growth factor (IGF)[72]
References
- ^ Template:GeorgiaPhysiology
- ^ Elias, H.; Bengelsdorf, H. (1 July 1952). "The Structure of the Liver in Vertebrates". Cells Tissues Organs. 14 (4): 297–337. doi:10.1159/000140715.
- ^ Abdel-Misih, Sherif R. Z.; Bloomston, Mark (2010). "Liver Anatomy". Surgical Clinics of North America. 90 (4): 643–53. doi:10.1016/j.suc.2010.04.017. PMC 4038911. PMID 20637938.
- ^ a b "Anatomy and physiology of the liver – Canadian Cancer Society". Cancer.ca. Retrieved 2015-06-26.
- ^ a b Tortora, Gerard J.; Derrickson, Bryan H. (2008). Principles of Anatomy and Physiology (12th ed.). John Wiley & Sons. p. 945. ISBN 978-0-470-08471-7.
- ^ Maton, Anthea; Jean Hopkins; Charles William McLaughlin; Susan Johnson; Maryanna Quon Warner; David LaHart; Jill D. Wright (1993). Human Biology and Health. Englewood Cliffs, New Jersey, USA: Prentice Hall. ISBN 0-13-981176-1. OCLC 32308337.
- ^ Zakim, David; Boyer, Thomas D. (2002). Hepatology: A Textbook of Liver Disease (4th ed.). ISBN 9780721690513.
- ^ "Etymology online hepatic". Retrieved December 12, 2013.
- ^ a b Liver Anatomy at eMedicine
- ^ Cotran, Ramzi S.; Kumar, Vinay; Fausto, Nelson; Nelso Fausto; Robbins, Stanley L.; Abbas, Abul K. (2005). Robbins and Cotran pathologic basis of disease (7th ed.). St. Louis, MO: Elsevier Saunders. p. 878. ISBN 0-7216-0187-1.
- ^ "Enlarged liver". Mayo Clinic. Retrieved 2017-03-29.
- ^ Dorland's illustrated medical dictionary 2012, p. 285.
- ^ "Medical Definition of GLISSON'S CAPSULE". www.merriam-webster.com.
- ^ "Anatomy of the Liver". Liver.co.uk. Retrieved 2015-06-26.
- ^ Renz, John F.; Kinkhabwala, Milan (2014). "Surgical Anatomy of the Liver". In Busuttil, Ronald W.; Klintmalm, Göran B. (eds.). Transplantation of the Liver. Elsevier. pp. 23–39. ISBN 978-1-4557-5383-3.
{{cite book}}: External link in|chapterurl=|chapterurl=ignored (|chapter-url=suggested) (help) - ^ "Cantlie's line | Radiology Reference Article". Radiopaedia.org. Retrieved 2015-06-26.
- ^ Kuntz, Erwin; Kuntz, Hans-Dieter (2009). "Liver resection". Hepatology: Textbook and Atlas (3rd ed.). Springer. pp. 900–3. ISBN 978-3-540-76839-5.
{{cite book}}: External link in|chapterurl=|chapterurl=ignored (|chapter-url=suggested) (help) - ^ a b Singh, Inderbir (2008). "The Liver Pancreas and Spleen". Textbook of Anatomy with Colour Atlas. Jaypee Brothers. pp. 592–606. ISBN 978-81-8061-833-8.
{{cite book}}: External link in|chapterurl=|chapterurl=ignored (|chapter-url=suggested) (help) - ^ a b McMinn, R. M. H. (2003). "Liver and Biliary Tract". Last's Anatomy: Regional and Applied. Elsevier. pp. 342–51. ISBN 978-0-7295-3752-0.
{{cite book}}: External link in|chapterurl=|chapterurl=ignored (|chapter-url=suggested) (help) - ^ Skandalakis, Lee J.; Skandalakis, John E.; Skandalakis, Panajiotis N. (2009). "Liver". Surgical Anatomy and Technique: A Pocket Manual. pp. 497–531. doi:10.1007/978-0-387-09515-8_13. ISBN 978-0-387-09515-8.
- ^ a b c Dorland's illustrated medical dictionary 2012, p. 925.
- ^ a b c Human Anatomy & Physiology + New Masteringa&p With Pearson Etext. Benjamin-Cummings Pub Co. 2012. ISBN 9780321852120.
- ^ a b c Human Anatomy & Physiology + New Masteringa&p With Pearson Etext. Benjamin-Cummings Pub Co. 2012. p. 881. ISBN 9780321852120.
- ^ a b c Kmieć Z (2001). "Cooperation of liver cells in health and disease". Adv Anat Embryol Cell Biol. 161: III–XIII, 1–151. PMID 11729749.
- ^ Pocock, Gillian (2006). Human Physiology (Third ed.). Oxford University Press. p. 404. ISBN 978-0-19-856878-0.
- ^ a b "Couinaud classification | Radiology Reference Article". Radiopaedia.org. Retrieved 2015-06-26.
- ^ "Three-dimensional Anatomy of the Couinaud Liver Segments". Retrieved 2009-02-17.
- ^ Strunk, H.; Stuckmann, G.; Textor, J.; Willinek, W. (2003). "Limitations and pitfalls of Couinaud's segmentation of the liver in transaxial Imaging". European Radiology. 13 (11): 2472–82. doi:10.1007/s00330-003-1885-9. PMID 12728331.
- ^ a b "The Radiology Assistant : Anatomy of the liver segments". Radiologyassistant.nl. 2006-05-07. Retrieved 2015-06-26.
- ^ "The human proteome in liver - The Human Protein Atlas". www.proteinatlas.org. Retrieved 2017-09-21.
- ^ Uhlén, Mathias; Fagerberg, Linn; Hallström, Björn M.; Lindskog, Cecilia; Oksvold, Per; Mardinoglu, Adil; Sivertsson, Åsa; Kampf, Caroline; Sjöstedt, Evelina (2015-01-23). "Tissue-based map of the human proteome". Science. 347 (6220): 1260419. doi:10.1126/science.1260419. ISSN 0036-8075. PMID 25613900.
- ^ Kampf, Caroline; Mardinoglu, Adil; Fagerberg, Linn; Hallström, Björn M.; Edlund, Karolina; Lundberg, Emma; Pontén, Fredrik; Nielsen, Jens; Uhlen, Mathias (2014-07-01). "The human liver-specific proteome defined by transcriptomics and antibody-based profiling". The FASEB Journal. 28 (7): 2901–2914. doi:10.1096/fj.14-250555. ISSN 0892-6638. PMID 24648543.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Gilbert SF (2000). Developmental Biology (6th ed.). Sunderland (MA): Sinauer Associates.
- ^ a b Lade AG, Monga SP (2011). "Beta-catenin signaling in hepatic development and progenitors: which way does the WNT blow?". Dev Dyn. 240 (3): 486–500. doi:10.1002/dvdy.22522. PMC 4444432. PMID 21337461.
- ^ Berg T, DeLanghe S, Al Alam D, Utley S, Estrada J, Wang KS (2010). "β-catenin regulates mesenchymal progenitor cell differentiation during hepatogenesis". J Surg Res. 164 (2): 276–85. doi:10.1016/j.jss.2009.10.033. PMC 2904820. PMID 20381814.
- ^ Clemente, Carmin D. (2011). Anatomy a Regional Atlas of the Human Body. Philadelphia: Lippincott Williams & Wilkins. p. 243. ISBN 978-1-58255-889-9.
- ^ Shneider, Benjamin L.; Sherman, Philip M. (2008). Pediatric Gastrointestinal Disease. Connecticut: PMPH-USA. p. 751. ISBN 1-55009-364-9.
- ^ a b Human Anatomy & Physiology + New Masteringa&p With Pearson Etext. Benjamin-Cummings Pub Co. 2012. p. 939. ISBN 9780321852120.
- ^ Jelkmann, Wolfgang (2001). "The role of the liver in the production of thrombopoietin compared with erythropoietin". European Journal of Gastroenterology & Hepatology. 13 (7): 791–801. doi:10.1097/00042737-200107000-00006. PMID 11474308.
- ^ "If a person stops consuming the vitamin, the body's stores of this vitamin usually take about 3 to 5 years to exhaust".
- ^ Cirrhosis Overview National Digestive Diseases Information Clearinghouse. Retrieved 2010-01-22
- ^ Hepatitis A, B, and C Center: Symptoms, Causes, Tests, Transmission, and Treatments. Webmd.com (2005-08-19). Retrieved on 2016-05-10.
- ^ Schweitzer A, Horn J, Mikolajczyk RT, Krause G, Ott JJ (2015). "Estimations of worldwide prevalence of chronic hepatitis B virus infection: a systematic review of data published between 1965 and 2013". Lancet. 386 (10003): 1546–55. doi:10.1016/S0140-6736(15)61412-X. PMID 26231459.
- ^ a b "Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015". Lancet. 388 (10053): 1545–1602. 2016. doi:10.1016/S0140-6736(16)31678-6. PMC 5055577. PMID 27733282.
- ^ "www.hepatitisc.uw.edu".
- ^ "WHO | Hepatitis E".
- ^ Dény P (2006). "Hepatitis delta virus genetic variability: from genotypes I, II, III to eight major clades?". Curr. Top. Microbiol. Immunol. 307: 151–71. PMID 16903225.
- ^ Rajani R, Melin T, Björnsson E, Broomé U, Sangfelt P, Danielsson A, Gustavsson A, Grip O, Svensson H, Lööf L, Wallerstedt S, Almer SH (Feb 2009). "Budd-Chiari syndrome in Sweden: epidemiology, clinical characteristics and survival – an 18-year experience". Liver International. 29 (2): 253–9. doi:10.1111/j.1478-3231.2008.01838.x. PMID 18694401.
- ^ Hirschfield, GM; Gershwin, ME (Jan 24, 2013). "The immunobiology and pathophysiology of primary biliary cirrhosis". Annual Review of Pathology. 8: 303–30. doi:10.1146/annurev-pathol-020712-164014. PMID 23347352.
- ^ Dancygier, Henryk (2010). Clinical Hepatology Principles and Practice of. Springer. pp. 895–. ISBN 978-3-642-04509-7. Retrieved 29 June 2010.
- ^ Saxena, Romil; Theise, Neil (2004). "Canals of Hering: Recent Insights and Current Knowledge". Seminars in Liver Disease. 24 (1): 43–8. doi:10.1055/s-2004-823100. PMID 15085485.
- ^ Extraintestinal Complications: Liver Disease Crohn's & Colitis Foundation of America. Retrieved 2010-01-22
- ^ Liver Information Archived 2010-01-30 at the Wayback Machine HealthLine. Retrieved 2010-01-22
- ^ Ghent, Cam N (2009). "Who should be performing liver biopsies?". Canadian Journal of Gastroenterology. 23 (6): 437–8. PMC 2721812. PMID 19543575.
- ^ Sheporaitis, L; Freeny, PC (1998). "Hepatic and portal surface veins: A new anatomic variant revealed during abdominal CT". AJR. American journal of roentgenology. 171 (6): 1559–64. doi:10.2214/ajr.171.6.9843288. PMID 9843288.
- ^ Häussinger, Dieter, ed. (2011). Liver Regeneration. Berlin: De Gruyter. p. 1. ISBN 9783110250794.
- ^ Robbins and Cotran Pathologic Basis of Disease (7th ed.). 1999. p. 101. ISBN 0-8089-2302-1.
- ^ Chu, Jaime; Sadler, Kirsten C. (2009). "New school in liver development: Lessons from zebrafish". Hepatology. 50 (5): 1656–63. doi:10.1002/hep.23157. PMC 3093159. PMID 19693947.
- ^ W. T. Councilman (1913). "Two". Disease and Its Causes. New York Henry Holt and Company London Williams and Norgate The University Press, Cambridge, U.S.A.
- ^ Suzuki K, Tanaka M, Watanabe N, Saito S, Nonaka H, Miyajima A (2008). "p75 Neurotrophin receptor is a marker for precursors of stellate cells and portal fibroblasts in mouse fetal liver". Gastroenterology. 135 (1): 270–281.e3. doi:10.1053/j.gastro.2008.03.075. PMID 18515089.
- ^ Tietz PS, Larusso NF (May 2006). "Cholangiocyte biology". Current Opinion in Gastroenterology. 22 (3): 279–87. doi:10.1097/01.mog.0000218965.78558.bc. PMID 16550043.
- ^ An argument for the ancient Greek’s knowing about liver regeneration is provided by Chen, T. S.; Chen, P. S. (1994). "The myth of Prometheus and the liver". Journal of the Royal Society of Medicine. 87 (12): 754–755. PMC 1294986. PMID 7853302. Counterarguments are provided by Tiniakos, D. G.; Kandilis, A.; Geller, S. A. (2010). "Tityus: A forgotten myth of liver regeneration". Journal of Hepatology. 53 (2): 357–361. doi:10.1016/j.jhep.2010.02.032. PMID 20472318. and by Power, C.; Rasko, J. E. (2008). "Whither prometheus' liver? Greek myth and the science of regeneration". Annals of Internal Medicine. 149 (6): 421–426. doi:10.7326/0003-4819-149-6-200809160-00009. PMID 18794562.
- ^ Bramstedt K (2006). "Living liver donor mortality: where do we stand?". Am. J. Gastroenterol. 101 (4): 755–9. doi:10.1111/j.1572-0241.2006.00421.x. PMID 16494593.
- ^ Krishna, Gopi; Hillman, James (1970). Kundalini – the evolutionary energy in man. London: Stuart & Watkins. p. 77. ISBN 1570622809.
- ^ The Great Battle Of Badar (Yaum-E-Furqan). Shawuniversitymosque.org (2006-07-08). Retrieved 2013-03-19.
- ^ "La Voz de Galicia "Ferrol monument mentioned in US newspaper" 07/30/2015"".
- ^ Schwabe, Calvin W. (1979). Unmentionable Cuisine. University of Virginia Press. pp. 313–. ISBN 978-0-8139-1162-5.
- ^ Romer, Alfred Sherwood; Parsons, Thomas S. (1977). The Vertebrate Body. Philadelphia, PA: Holt-Saunders International. pp. 354–5. ISBN 0-03-910284-X.
- ^ Yuan, Shaochun; Ruan, Jie; Huang, Shengfeng; Chen, Shangwu; Xu, Anlong (2015). "Amphioxus as a model for investigating evolution of the vertebrate immune system" (PDF). Developmental & Comparative Immunology. 48 (2): 297–305. doi:10.1016/j.dci.2014.05.004.
- ^ Yu, Jr-Kai Sky; Lecroisey, Claire; Le Pétillon, Yann; Escriva, Hector; Lammert, Eckhard; Laudet, Vincent (2015). "Identification, Evolution and Expression of an Insulin-Like Peptide in the Cephalochordate Branchiostoma lanceolatum". PLoS ONE. 10 (3): e0119461. doi:10.1371/journal.pone.0119461. PMC 4361685. PMID 25774519.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Escriva, Hector; Chao, Yeqing; Fan, Chunxin; Liang, Yujun; Gao, Bei; Zhang, Shicui (2012). "A Novel Serpin with Antithrombin-Like Activity in Branchiostoma japonicum: Implications for the Presence of a Primitive Coagulation System". PLoS ONE. 7 (3): e32392. doi:10.1371/journal.pone.0032392. PMC 3299649. PMID 22427833.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Guo, Bin; Zhang, Shicui; Wang, Shaohui; Liang, Yujun (2009). "Expression, mitogenic activity and regulation by growth hormone of growth hormone/insulin-like growth factor in Branchiostoma belcheri" (PDF). Cell and Tissue Research. 338 (1): 67–77. doi:10.1007/s00441-009-0824-8. PMID 19657677.
Works cited
- Dorland's illustrated medical dictionary (32nd ed.). Philadelphia: Elsevier/Saunders. 2012. ISBN 978-1-4557-0985-4.

![Axial CT image showing anomalous hepatic veins coursing on the subcapsular anterior surface of the liver.[55]](http://upload.wikimedia.org/wikipedia/commons/thumb/2/28/Axial_CT_anomalous_hepatic_veins.jpg/120px-Axial_CT_anomalous_hepatic_veins.jpg)