Fetal viability
Fetal viability or foetal viability is the ability of a fetus to survive outside the uterus.[1]
Definitions
Viability, as the word has been used in United States constitutional law since Roe v. Wade, is the potential of the fetus to survive outside the uterus after birth, natural or induced, when supported by up-to-date medicine. Fetal viability depends largely on the fetal organ maturity, and environmental conditions.[2] According to Websters Encyclopedic Unabridged Dictionary of the English Language, viability of a fetus means having reached such a stage of development as to be capable of living, under normal conditions, outside the uterus. Viability exists as a function of biomedical and technological capacities, which are different in different parts of the world. As a consequence, there is, at the present time, no worldwide, uniform gestational age that defines viability.[3]
According to the McGraw-Hill medical dictionary a nonviable fetus is "an expelled or delivered fetus which, although living, cannot possibly survive to the point of sustaining life independently, even with support of the best available medical therapy."[4] A legal definition states: "Nonviable means not capable of living, growing, or developing and functioning successfully. It is antithesis of viable, which is defined as having attained such form and development of organs as to be normally capable of living outside the uterus." [Wolfe v. Isbell, 291 Ala. 327, 329 (Ala. 1973)][5]
Various jurisdictions have different legal definitions of viability. In Ireland, under the Health (Regulation of Termination of Pregnancy) Act 2018, fetal viability is defined as "the point in a pregnancy at which, in the reasonable opinion of a medical practitioner, the foetus is capable of survival outside the uterus without extraordinary life-sustaining measures." [Definitions (Part 2)(8)][6]
Medical viability

There is no sharp limit of development, gestational age, or weight at which a human fetus automatically becomes viable.[1]
Studies in the last decade have shown an increase in survival rates at 22 and 23 weeks of gestation for those infants born alive. According to a study in Germany, 22-week babies who showed any sign of life after birth (e.g., heartbeat, gasping, movement) who were given active treatment had a 61% survival rate, while 23-week babies had a 71% survival rate.[13] Importantly, physicians did not determine whether or not to give active treatment based on infants' characteristics, but rather left the decision making to parents. For those infants given active care and those given only palliative care, there were no significant differences in birth weight or whether infants were singletons or part of multiples. However, those given palliative care were slightly more immature than the group of infants who were resuscitated (average age: 22 weeks 3 days vs. 22 weeks 4 days).[13] Study authors note the bundle of interventions used that led to the high survival rate:
- Use of prenatal steroids after parental counseling from 22 weeks of gestation
- Cesarean delivery with local anesthesia as preferred mode of delivery
- Delayed cord clamping
- Comfort positioning (lateral) of the infant
- Establishment of spontaneous breathing via a stepwise increase in positive end-expiratory pressure
- Less invasive surfactant application (LISA)"[13]
This study notes why rates of survival rate may be so low for national studies: "A recent report on ethics in delivery-room care emphasized the impact of self-fulfilling prophecies, meaning that the recommendation not to treat at 22 weeks of gestation inevitably has to lead to low rates of survival. Consequently, reports on big national cohorts in settings where treatment is predominantly withheld for extremely immature infants cannot produce valid data on survival"[13] [emphasis added].
Similarly, a study in Sweden showed a 58% survival rate for 22-week babies born alive who were given active treatment, and a 66% survival rate for 23-week babies.[14] A data review in the United Kingdom showed a 54% survival rate for 22-week babies given intensive care.[15] However, the authors note that the survival rates of infants may be overly positive as "there is the possibility of selection bias and survivors may represent a sub-group of 22 week gestation babies with more favourable risk factors".[15] A U.S. study showed a 39% survival rate for those given active treatment at 22 weeks and a 55% survival rate for those given active treatment when born at 23 weeks (mothers were given antenatal steroids for both age groups).[16] "I've been in this business for 40 years, and I've seen the threshold of viability move back about one week every 10 years or so in my practice," reports Edward Bell, a neonatologist at the University of Iowa Children's Hospital.[17]
Unfortunately, many babies in this age group are stillborn, meaning they are showing any signs of life when they are delivered; however, this percentage has been decreasing as antenatal treatment has improved. The aforementioned study in Sweden reported that between 2014-2016, 35% of 22-week infants were stillborn, and 29% of 23-week infants were stillborn.[14]
Older data have been less optimistic. According to studies between 2003 and 2005, 20 to 35 percent of babies born at 24 weeks of gestation survived, while 50 to 70 percent of babies born at 25 weeks, and more than 90 percent born at 26 to 27 weeks, survived.[18]
| Completed weeks of gestation at birth | 22 | 23 | 24 | 25 | 26 |
|---|---|---|---|---|---|
| Probability of survival if showing any sign of life at birth and given intensive care (based on individual studies) | Up to 61%[13] | Up to 71%[13] | 79%[14] | 88%[14] | 92%[14] |
Period of viability
Beliefs about viability vary by country. One study showed that in Sweden, neonatologists generally consider whether or not to give medical treatment to babies born at 22 weeks, whereas neonatologists in the Netherlands generally do not consider treating babies until 24 weeks gestation.[19] In 2019, the British Association of Perinatal Medicine recommended that physicians in the United Kingdom consider whether or not to treat babies born at 22 weeks, revising its previous recommendation of 24 weeks.[20] Whether the fetus is in the period of viability has legal ramifications as far as the fetus' rights of protection are concerned.[21] Traditionally, the period of viability referred to the period after the twenty-eighth week,[22]
Viability can incorporate weight as well as gestational age.[23][24][25]
United States Supreme Court
The United States Supreme Court stated in Roe v. Wade (1973) that viability (i.e., the "interim point at which the fetus becomes ... potentially able to live outside the mother's womb, albeit with artificial aid"[26]) "is usually placed at about seven months (28 weeks) but may occur earlier, even at 24 weeks."[26] The 28-week definition became part of the "trimester framework" marking the point at which the "compelling state interest" (under the doctrine of strict scrutiny) in preserving potential life became possibly controlling, permitting states to freely regulate and even ban abortion after the 28th week.[26] The subsequent Planned Parenthood v. Casey (1992) modified the "trimester framework," permitting the states to regulate abortion in ways not posing an "undue burden" on the right of the mother to an abortion at any point before viability; on account of technological developments between 1973 and 1992, viability itself was legally dissociated from the hard line of 28 weeks, leaving the point at which "undue burdens" were permissible variable depending on the technology of the time and the judgment of the state legislatures.
Born-Alive Infants Protection Act of 2002
In 2002, the U.S. Government enacted the Born-Alive Infants Protection Act. Whereas a fetus may be viable or not viable in utero, this law provides a legal definition for personal human life when not in utero. It defines "born alive" as "the complete expulsion or extraction from his or her mother of that member, at any stage of development, who after such expulsion or extraction breathes or has a beating heart, pulsation of the umbilical cord, or definite movement of voluntary muscles"[27] and specifies that any of these is the action of a living human person. While the implications of this law for defining viability in medicine may not be fully explored,[28] in practice doctors and nurses are advised not to resuscitate such persons with gestational age of 22 weeks or less, under 400 g weight, with anencephaly, or with a confirmed diagnosis of trisomy 13 or 18.[29][30]
U.S. state laws
Forty-three states have laws restricting post-viability abortions. Some allow doctors to decide for themselves if the fetus is viable. Some require doctors to perform tests to prove a fetus is pre-viable and require multiple doctors to certify the findings. The procedure intact dilation and extraction (IDX) became a focal point in the abortion debate,[31] based on the belief that it is used mainly post-viability.[32] IDX was made illegal in most circumstances by the Partial-Birth Abortion Ban Act in 2003, which the U.S. Supreme Court upheld in the case of Gonzales v. Carhart.
Limit of viability
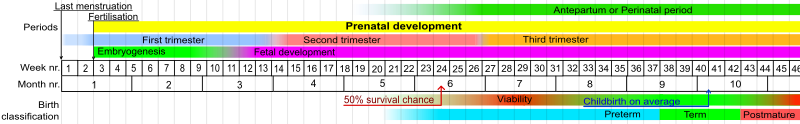
The limit of viability is the gestational age at which a prematurely born fetus/infant has a 50% chance of long-term survival outside its mother's womb. With the support of neonatal intensive care units, the limit of viability in the developed world has declined since 50 years ago.[33][34]
Different jurisdictions have different policies regarding the resuscitation of extremely premature newborns, that may be based on various factors such as gestational age, weight and medical presentation of the baby, the desires of parents and medical practitioners. The risk of severe disability of very premature babies or of mortality despite medical efforts lead to ethical debates over quality of life and futile medical care, but also about the sanctity of life as viewed in various religious doctrines.[35] A majority will not have any severe disabilities; the British Association of Perinatal Medicine reports that 2/3 of 22-week babies will not have a severe disability, and 3/4 of 23-week babies will not have a severe disability; the British Association of Perinatal Medicine notes "disability is generally impossible to predict for an individual baby at birth".[15]
As of 2006[update], the two youngest children to survive premature birth are thought to be James Elgin Gill (born on 20 May 1987 in Ottawa, Ontario, Canada, at 21 weeks and 5 days gestational age),[36][37] and Amillia Taylor (an IVF pregnancy, born on 24 October 2006 in Miami, Florida, at 21 weeks and 6 days gestational age).[38][39] Both children were born just under 20 weeks from fertilization (or 22 weeks' gestation). At birth, Taylor was 9 inches (22.86 cm) long and weighed 10 ounces (283 grams).[38] She suffered digestive and respiratory problems, together with a brain hemorrhage. She was discharged from the Baptist Children's Hospital on 20 February 2007.[38] As of 2013, Taylor was in kindergarten and at the small end of the normal growth curve with some developmental delays.[40]
A preterm birth, also known as premature birth, is defined as babies born alive before 37 weeks of pregnancy are completed.[41] There are three types of preterm births: extremely preterm (less than 28 weeks), very preterm (28 to 32 weeks) and moderate to late preterm (32 to 37 weeks).[41]
Factors that influence the chance of survival
There are several factors that affect the chance of survival of the baby. Two notable factors are age and weight. The baby's gestational age (number of completed weeks of pregnancy) at the time of birth and the baby's weight (also a measure of growth) influence whether the baby will survive. Another major factor is gender: male infants are slightly less mature[clarification needed] and have a slightly higher risk of dying than female infants.[citation needed]
Several types of health problems also influence fetal viability. For example, breathing problems, congenital abnormalities or malformations, and the presence of other severe diseases, especially infection, threaten the survival of the neonate.
Other factors may influence survival by altering the rate of organ maturation or by changing the supply of oxygen to the developing fetus.
The mother's health plays a significant role in the child's viability. Diabetes in the mother, if not well controlled, slows organ maturation; infants of such mothers have a higher mortality. Severe high blood pressure before the 8th month of pregnancy may cause changes in the placenta, decreasing the delivery of nutrients and/or oxygen to the developing fetus and leading to problems before and after delivery.
Rupture of the fetal membranes before 24 weeks of gestation with loss of amniotic fluid markedly decreases the baby's chances of survival, even if the baby is delivered much later.[42]
The quality of the facility—whether the hospital offers neonatal critical care services, whether it is a Level I pediatric trauma care facility, the availability of corticosteroids and other medications at the facility, the experience and number of physicians and nurses in neonatology and obstetrics and of the providers has a limited but still significant impact on fetal viability. Facilities that have obstetrical services and emergency rooms and operating facilities, even if smaller, can be used in areas where higher services are not available to stabilize the mother and fetus or neonate until they can be transferred to an appropriate facility.[43][44][45][46]
See also
- Beginning of human personhood
- Futile medical care
- Office for Human Research Protections#Additional protection for pregnant women, human fetuses, and neonates
References
- ^ a b Moore, Keith and Persaud, T. The Developing Human: Clinically Oriented Embryology, p. 103 (Saunders 2003).
- ^ (2012). Fetal Viability. [ONLINE] Available at: http://www.reference.md/files/D005/mD005328.html. [Last Accessed 15 November 2012].
- ^ Breborowicz GH (January 2001). "Limits of fetal viability and its enhancement". Early Pregnancy. 5 (1): 49–50. PMID 11753511.
- ^ The Free Dictionary. "nonviable fetus". Medical Dictionary. Retrieved May 21, 2019.
- ^ "Non-Viable Fetus Law and Legal Definition". USLegal. Retrieved May 21, 2019.
- ^ "Health (Regulation of Termination of Pregnancy) Act 2018" (PDF). Irish parliament.
- ^ Patel RM, Rysavy MA, Bell EF, Tyson JE (June 2017). "Survival of Infants Born at Periviable Gestational Ages". Clinics in Perinatology. 44 (2): 287–303. doi:10.1016/j.clp.2017.01.009. PMC 5424630. PMID 28477661.
- ^ Costeloe KL, Hennessy EM, Haider S, Stacey F, Marlow N, Draper ES (December 2012). "Short term outcomes after extreme preterm birth in England: comparison of two birth cohorts in 1995 and 2006 (the EPICure studies)". BMH. 345: e7976. doi:10.1136/bmj.e7976. PMC 3514472. PMID 23212881.
- ^ Fellman V, Hellström-Westas L, Norman M, Westgren M, Källén K, Lagercrantz H, Marsál K, Serenius F, Wennergren M (June 2009). "One-year survival of extremely preterm infants after active perinatal care in Sweden". JAMA. 301 (21): 2225–33. doi:10.1001/jama.2009.771. PMID 19491184.
- ^ Ancel PY, Goffinet F, Kuhn P, Langer B, Matis J, Hernandorena X, et al. (March 2015). "Survival and morbidity of preterm children born at 22 through 34 weeks' gestation in France in 2011: results of the EPIPAGE-2 cohort study". JAMA Pediatrics. 169 (3): 230–8. doi:10.1001/jamapediatrics.2014.3351. PMID 25621457.
- ^ Boland RA, Davis PG, Dawson JA, Doyle LW (March 2017). "Outcomes of infants born at 22-27 weeks' gestation in Victoria according to outborn/inborn birth status". Archives of Disease in Childhood: Fetal and Neonatal Edition. 102 (2): F153–F161. doi:10.1136/archdischild-2015-310313. PMID 27531224.
- ^ Chen F, Bajwa NM, Rimensberger PC, Posfay-Barbe KM, Pfister RE (September 2016). "Thirteen-year mortality and morbidity in preterm infants in Switzerland". Archives of Disease in Childhood: Fetal and Neonatal Edition. 101 (5): F377-83. doi:10.1136/archdischild-2015-308579. PMID 27059074.
- ^ a b c d e f Mehler, Katrin; Oberthuer, André; Keller, Titus; Becker, Ingrid; Valter, Markus; Roth, Bernhard; Kribs, Angela (2016-07-01). "Survival Among Infants Born at 22 or 23 Weeks' Gestation Following Active Prenatal and Postnatal Care". JAMA Pediatrics. 170 (7): 671–677. doi:10.1001/jamapediatrics.2016.0207. ISSN 2168-6203. PMID 27214875.
- ^ a b c d e Norman, Mikael; Hallberg, Boubou; Abrahamsson, Thomas; Björklund, Lars J.; Domellöf, Magnus; Farooqi, Aijaz; Foyn Bruun, Cathrine; Gadsbøll, Christian; Hellström-Westas, Lena; Ingemansson, Fredrik; Källén, Karin (March 26, 2019). "Association Between Year of Birth and 1-Year Survival Among Extremely Preterm Infants in Sweden During 2004-2007 and 2014-2016". JAMA. 321 (12): 1188–1199. doi:10.1001/jama.2019.2021. ISSN 1538-3598. PMC 6439685. PMID 30912837.
- ^ a b c "New BAPM Framework on Extreme Preterm Birth Published | British Association of Perinatal Medicine". www.bapm.org. Retrieved 2020-02-19.
- ^ Ehret, Danielle E. Y.; Edwards, Erika M.; Greenberg, Lucy T.; Bernstein, Ira M.; Buzas, Jeffrey S.; Soll, Roger F.; Horbar, Jeffrey D. (2018-10-05). "Association of Antenatal Steroid Exposure With Survival Among Infants Receiving Postnatal Life Support at 22 to 25 Weeks' Gestation". JAMA Network Open. 1 (6): e183235. doi:10.1001/jamanetworkopen.2018.3235. PMC 6324435. PMID 30646235.
- ^ "New studies confirm improved survival of extremely preterm babies". medicalxpress.com. Retrieved 2020-03-02.
- ^ March of Dimes --> Neonatal Death Retrieved on November 10, 2014. In turn citing:
- Tyson JE, Parikh NA, Langer J, Green C, Higgins RD (April 2008). "Intensive care for extreme prematurity--moving beyond gestational age". The New England Journal of Medicine. 358 (16): 1672–81. doi:10.1056/NEJMoa073059. PMC 2597069. PMID 18420500.
- Luke B, Brown MB (December 2006). "The changing risk of infant mortality by gestation, plurality, and race: 1989-1991 versus 1999-2001". Pediatrics. 118 (6): 2488–97. doi:10.1542/peds.2006-1824. PMC 3623686. PMID 17142535.
- The American College of Obstetricians and Gynecologists (September 2002). "ACOG Practice Bulletin: Clinical Management Guidelines for Obstetrcian-Gynecologists: Number 38, September 2002. Perinatal care at the threshold of viability". Obstetrics and Gynecology. 100 (3): 617–24. doi:10.1016/S0029-7844(02)02260-3. PMID 12220792.
- ^ Wilkinson, Dominic; Verhagen, Eduard; Johansson, Stefan (September 2018). "Thresholds for Resuscitation of Extremely Preterm Infants in the UK, Sweden, and Netherlands". Pediatrics. 142 (Suppl 1): S574–S584. doi:10.1542/peds.2018-0478I. ISSN 1098-4275. PMC 6379058. PMID 30171144.
- ^ "Perinatal Management of Extreme Preterm Birth Before 27 weeks of Gestation (2019) | British Association of Perinatal Medicine". www.bapm.org. Retrieved 2020-02-21.
- ^ "Attorney Catherine Christophillis Discusses The Reasoning Behind The Drug Testing Of Pregnant Women". Legal News Chat Transcript. October 25, 2000.
- ^ Finney, Patrick A. (1922). Moral Problems in Hospital Practice: a Practical Handbook. St. Louis: Herder Bk. Co. p. 24. OCLC 14054441.
- ^ Li Z, Zeki R, Hilder L, Sullivan, EA (2012). "Australia's Mothers and Babies 2010". Perinatal statistics series no. 27. Cat. no. PER 57. Australian Institute of Health and Welfare National Perinatal Statistics Unit, Australian Government. Retrieved 4 July 2013.
- ^ Mohangoo AD, Blondel B, Gissler M, Velebil P, Macfarlane A, Zeitlin J (2013). Wright L (ed.). "International comparisons of fetal and neonatal mortality rates in high-income countries: should exclusion thresholds be based on birth weight or gestational age?". PLOS ONE. 8 (5): e64869. Bibcode:2013PLoSO...864869M. doi:10.1371/journal.pone.0064869. PMC 3658983. PMID 23700489.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Royal College of Obstetricians; Gynaecologists UK (April 2001). "Further Issues Relating to Late Abortion, Fetal Viability and Registration of Births and Deaths". Royal College of Obstetricians and Gynaecologists UK. Archived from the original on 5 November 2013. Retrieved 4 July 2013.
- ^ a b c Roe v. Wade, 410 U.S. 113, 160, 93 S.Ct. 705, 730 (1973).
- ^ "House Report 107-186 - BORN-ALIVE INFANTS PROTECTION ACT OF 2001". frwebgate.access.gpo.gov. Retrieved 3 April 2018.
- ^ Sayeed SA (October 2005). "Baby doe redux? The Department of Health and Human Services and the Born-Alive Infants Protection Act of 2002: a cautionary note on normative neonatal practice". Pediatrics. 116 (4): e576-85. doi:10.1542/peds.2005-1590. PMID 16199687.
- ^ Powell, Traci (2012). "Decisions and Dilemmas Related to Resuscitation of Infants Born on the Verge of Viability". NAINR. 12 (1): 27–32. doi:10.1053/j.nainr.2011.12.004. Retrieved 8 October 2015.
{{cite journal}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ Kattwinkel J, Perlman JM, Aziz K, Colby C, Fairchild K, Gallagher J, Hazinski MF, Halamek LP, Kumar P, Little G, McGowan JE, Nightengale B, Ramirez MM, Ringer S, Simon WM, Weiner GM, Wyckoff M, Zaichkin J (November 2010). "Neonatal resuscitation: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care". Pediatrics. 126 (5): e1400-13. doi:10.1542/peds.2010-2972E. PMID 20956432.
- ^ Guttmacher.org Abortion Incidence and Services in the United States in 2000
- ^ Franklin Foer (1997). Fetal Viability. [ONLINE] Available at: http://www.slate.com/articles/news_and_politics/the_gist/1997/05/fetal_viability.html. [Last Accessed 14 November 2012].
- ^ Santhakumaran S, Statnikov Y, Gray D, Battersby C, Ashby D, Modi N (May 2018). "Survival of very preterm infants admitted to neonatal care in England 2008-2014: time trends and regional variation". Archives of Disease in Childhood: Fetal and Neonatal Edition. 103 (3): F208–F215. doi:10.1136/archdischild-2017-312748. PMC 5916099. PMID 28883097.
- ^ Walsh, Fergus (11 April 2008). "Prem baby survival rates revealed". BBC News. Retrieved 2008-05-11.
{{cite news}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ http://nuffieldbioethics.org/wp-content/uploads/2014/07/CCD-Short-Version-FINAL.pdf
- ^ "Powell's Books - Guinness World Records 2004 (Guinness Book of Records) by". Retrieved 2007-11-28.
- ^ "Miracle child". Archived from the original on 2007-12-09. Retrieved 2007-11-28.
- ^ a b c "Most-premature baby allowed home". BBC News. 2007-02-21. Retrieved 2007-05-05.
- ^ Baptist Hospital of Miami, Fact Sheet Archived 2009-03-26 at the Wayback Machine (2006).
- ^ Kirkey, Sharon (29 March 2013). "Fate of the fetus: As politicians debate, science reveals more and more about what happens during pregnancy". Postmedia News. Retrieved 5 June 2013.
- ^ a b "Preterm birth". World Health Organization. Retrieved 3 April 2018.
- ^ (). What are the chances that my baby will survive?. [ONLINE] Available at: http://www.spensershope.org/chances_for_survival.htm Archived 2018-08-09 at the Wayback Machine. [Last Accessed 14 November 2012].
- ^ "NIH Study Reveals Factors That Influence Premature Infant Survival, Disability". nih.gov. 13 September 2015. Retrieved 3 April 2018.
- ^ Glass HC, Costarino AT, Stayer SA, Brett CM, Cladis F, Davis PJ (June 2015). "Outcomes for extremely premature infants". Anesthesia and Analgesia. 120 (6): 1337–51. doi:10.1213/ANE.0000000000000705. PMC 4438860. PMID 25988638.
- ^ Behrman, Richard E.; Butler, Adrienne Stith; Outcomes; et al. (Institute of Medicine (US) Committee on Understanding Premature Birth and Assuring Healthy) (3 April 2018). "Mortality and Acute Complications in Preterm Infants". National Academies Press (US). Retrieved 3 April 2018.
{{cite web}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ Belluck, Pam (6 May 2015). "Premature Babies May Survive at 22 Weeks if Treated, Study Finds". The New York Times. Retrieved 3 April 2018.
Further reading
- "Fetal Viability and Death" (PDF). United States. National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research. May 2006.
