Sleep

Sleep is a state of reduced mental and physical activity in which consciousness is altered and certain sensory activity is inhibited. During sleep, there is a marked decrease in muscle activity and interactions with the surrounding environment. While sleep differs from wakefulness in terms of the ability to react to stimuli, it still involves active brain patterns, making it more reactive than a coma or disorders of consciousness.[1]
Sleep occurs in repeating periods, during which the body alternates between two distinct modes: REM and non-REM sleep. Although REM stands for "rapid eye movement", this mode of sleep has many other aspects, including virtual paralysis of the body.[2] Dreams are a succession of images, ideas, emotions, and sensations that usually occur involuntarily in the mind during certain stages of sleep.
During sleep, most of the body's systems are in an anabolic state, helping to restore the immune, nervous, skeletal, and muscular systems;[3] these are vital processes that maintain mood, memory, and cognitive function, and play a large role in the function of the endocrine and immune systems.[4] The internal circadian clock promotes sleep daily at night, when it is dark. The diverse purposes and mechanisms of sleep are the subject of substantial ongoing research.[5] Sleep is a highly conserved behavior across animal evolution,[6] likely going back hundreds of millions of years.[7]
Humans may suffer from various sleep disorders, including dyssomnias, such as insomnia, hypersomnia, narcolepsy, and sleep apnea; parasomnias, such as sleepwalking and rapid eye movement sleep behavior disorder; bruxism; and circadian rhythm sleep disorders. The use of artificial light has substantially altered humanity's sleep patterns.[8] Common sources of artificial light include outdoor lighting and the screens of electronic devices such as smartphones and televisions, which emit large amounts of blue light, a form of light typically associated with daytime. This disrupts the release of the hormone melatonin needed to regulate the sleep cycle.[9]
Physiology
The most pronounced physiological changes in sleep occur in the brain.[10] The brain uses significantly less energy during sleep than it does when awake, especially during non-REM sleep. In areas with reduced activity, the brain restores its supply of adenosine triphosphate (ATP), the molecule used for short-term storage and transport of energy.[11] In quiet waking, the brain is responsible for 20% of the body's energy use, thus this reduction has a noticeable effect on overall energy consumption.[12]
Sleep increases the sensory threshold. In other words, sleeping persons perceive fewer stimuli, but can generally still respond to loud noises and other salient sensory events.[12][10]
During slow-wave sleep, humans secrete bursts of growth hormone. All sleep, even during the day, is associated with the secretion of prolactin.[13]
Key physiological methods for monitoring and measuring changes during sleep include electroencephalography (EEG) of brain waves, electrooculography (EOG) of eye movements, and electromyography (EMG) of skeletal muscle activity. Simultaneous collection of these measurements is called polysomnography, and can be performed in a specialized sleep laboratory.[14][15] Sleep researchers also use simplified electrocardiography (EKG) for cardiac activity and actigraphy for motor movements.[15]
Brain waves in sleep
The electrical activity seen on an EEG represents brain waves. The amplitude of EEG waves at a particular frequency corresponds to various points in the sleep-wake cycle, such as being asleep, being awake, or falling asleep.[16] Alpha, beta, theta, gamma, and delta waves are all seen in the different stages of sleep. Each waveform maintains a different frequency and amplitude. Alpha waves are seen when a person is in a resting state, but is still fully conscious. Their eyes may be closed and all of their body is resting and relatively still, where the body is starting to slow down. Beta waves take over alpha waves when a person is at attention, as they might be completing a task or concentrating on something. Beta waves consist of the highest of frequencies and the lowest of amplitude, and occur when a person is fully alert. Gamma waves are seen when a person is highly focused on a task or using all their concentration. Theta waves occur during the period of a person being awake, and they continue to transition into Stage 1 of sleep and in stage 2. Delta waves are seen in stages 3 and 4 of sleep when a person is in their deepest of sleep.[17]
Non-REM and REM sleep
Sleep is divided into two broad types: non-rapid eye movement (non-REM or NREM) sleep and rapid eye movement (REM) sleep. Non-REM and REM sleep are so different that physiologists identify them as distinct behavioral states. Non-REM sleep occurs first and after a transitional period is called slow-wave sleep or deep sleep. During this phase, body temperature and heart rate fall, and the brain uses less energy.[10] REM sleep, also known as paradoxical sleep, represents a smaller portion of total sleep time. It is the main occasion for dreams (or nightmares), and is associated with desynchronized and fast brain waves, eye movements, loss of muscle tone,[18] and suspension of homeostasis.[19]
The sleep cycle of alternate NREM and REM sleep takes an average of 90 minutes, occurring 4–6 times in a good night's sleep.[15][20] The American Academy of Sleep Medicine (AASM) divides NREM into three stages: N1, N2, and N3, the last of which is also called delta sleep or slow-wave sleep.[21] The whole period normally proceeds in the order: N1 → N2 → N3 → N2 → REM. REM sleep occurs as a person returns to stage 2 or 1 from a deep sleep.[18] There is a greater amount of deep sleep (stage N3) earlier in the night, while the proportion of REM sleep increases in the two cycles just before natural awakening.[15]
Awakening

Awakening can mean the end of sleep, or simply a moment to survey the environment and readjust body position before falling back asleep. Sleepers typically awaken soon after the end of a REM phase or sometimes in the middle of REM. Internal circadian indicators, along with a successful reduction of homeostatic sleep need, typically bring about awakening and the end of the sleep cycle.[22] Awakening involves heightened electrical activation in the brain, beginning with the thalamus and spreading throughout the cortex.[22]
On a typical night of sleep, there is not much time that is spent in the waking state. In various sleep studies that have been conducted using the electroencephalography, it has been found that females are awake for 0-1% during their nightly sleep while males are awake for 0-2% during that time. In adults, wakefulness increases, especially in later cycles. One study found 3% awake time in the first ninety-minute sleep cycle, 8% in the second, 10% in the third, 12% in the fourth, and 13–14% in the fifth. Most of this awake time occurred shortly after REM sleep.[22]
Today, many humans wake up with an alarm clock;[23] however, people can also reliably wake themselves up at a specific time with no need for an alarm.[22] Many sleep quite differently on workdays versus days off, a pattern which can lead to chronic circadian desynchronization.[24][23] Many people regularly look at television and other screens before going to bed, a factor which may exacerbate disruption of the circadian cycle.[25][26] Scientific studies on sleep have shown that sleep stage at awakening is an important factor in amplifying sleep inertia.[27]
Determinants of alertness after waking up include quantity/quality of the sleep, physical activity the day prior, a carbohydrate-rich breakfast, and a low blood glucose response to it.[28]
Timing
Sleep timing is controlled by the circadian clock (Process C), sleep-wake homeostasis (Process S), and to some extent by the individual will.
Circadian clock

Sleep timing depends greatly on hormonal signals from the circadian clock, or Process C, a complex neurochemical system which uses signals from an organism's environment to recreate an internal day–night rhythm. Process C counteracts the homeostatic drive for sleep during the day (in diurnal animals) and augments it at night.[29][24] The suprachiasmatic nucleus (SCN), a brain area directly above the optic chiasm, is presently considered the most important nexus for this process; however, secondary clock systems have been found throughout the body.
An organism whose circadian clock exhibits a regular rhythm corresponding to outside signals is said to be entrained; an entrained rhythm persists even if the outside signals suddenly disappear. If an entrained human is isolated in a bunker with constant light or darkness, he or she will continue to experience rhythmic increases and decreases of body temperature and melatonin, on a period that slightly exceeds 24 hours. Scientists refer to such conditions as free-running of the circadian rhythm. Under natural conditions, light signals regularly adjust this period downward, so that it corresponds better with the exact 24 hours of an Earth day.[23][30][31]
The circadian clock exerts constant influence on the body, affecting sinusoidal oscillation of body temperature between roughly 36.2 °C and 37.2 °C.[31][32] The suprachiasmatic nucleus itself shows conspicuous oscillation activity, which intensifies during subjective day (i.e., the part of the rhythm corresponding with daytime, whether accurately or not) and drops to almost nothing during subjective night.[33] The circadian pacemaker in the suprachiasmatic nucleus has a direct neural connection to the pineal gland, which releases the hormone melatonin at night.[33] Cortisol levels typically rise throughout the night, peak in the awakening hours, and diminish during the day.[13][34] Circadian prolactin secretion begins in the late afternoon, especially in women, and is subsequently augmented by sleep-induced secretion, to peak in the middle of the night. Circadian rhythm exerts some influence on the nighttime secretion of growth hormone.[13]
The circadian rhythm influences the ideal timing of a restorative sleep episode.[23][35] Sleepiness increases during the night. REM sleep occurs more during body temperature minimum within the circadian cycle, whereas slow-wave sleep can occur more independently of circadian time.[31]
The internal circadian clock is profoundly influenced by changes in light, since these are its main clues about what time it is. Exposure to even small amounts of light during the night can suppress melatonin secretion, and increase body temperature and wakefulness. Short pulses of light, at the right moment in the circadian cycle, can significantly 'reset' the internal clock.[32] Blue light, in particular, exerts the strongest effect,[24] leading to concerns that use of a screen before bed may interfere with sleep.[25]
Modern humans often find themselves desynchronized from their internal circadian clock, due to the requirements of work (especially night shifts), long-distance travel, and the influence of universal indoor lighting.[31] Even if they have sleep debt, or feel sleepy, people can have difficulty staying asleep at the peak of their circadian cycle. Conversely, they can have difficulty waking up in the trough of the cycle.[22] A healthy young adult entrained to the sun will (during most of the year) fall asleep a few hours after sunset, experience body temperature minimum at 6 a.m., and wake up a few hours after sunrise.[31]
Process S
Generally speaking, the longer an organism is awake, the more it feels a need to sleep ("sleep debt"). This driver of sleep is referred to as Process S. The balance between sleeping and waking is regulated by a process called homeostasis. Induced or perceived lack of sleep is called sleep deprivation.
Process S is driven by the depletion of glycogen and accumulation of adenosine in the forebrain that disinhibits the ventrolateral preoptic nucleus, allowing for inhibition of the ascending reticular activating system.[36]
Sleep deprivation tends to cause slower brain waves in the frontal cortex, shortened attention span, higher anxiety, impaired memory, and a grouchy mood. Conversely, a well-rested organism tends to have improved memory and mood.[37] Neurophysiological and functional imaging studies have demonstrated that frontal regions of the brain are particularly responsive to homeostatic sleep pressure.[38]
There is disagreement on how much sleep debt is possible to accumulate, and whether sleep debt is accumulated against an individual's average sleep or some other benchmark. It is also unclear whether the prevalence of sleep debt among adults has changed appreciably in the industrialized world in recent decades. Sleep debt does show some evidence of being cumulative. Subjectively, however, humans seem to reach maximum sleepiness 30 hours after waking.[31] It is likely that in Western societies, children are sleeping less than they previously have.[39]
One neurochemical indicator of sleep debt is adenosine, a neurotransmitter that inhibits many of the bodily processes associated with wakefulness. Adenosine levels increase in the cortex and basal forebrain during prolonged wakefulness, and decrease during the sleep-recovery period, potentially acting as a homeostatic regulator of sleep.[40][41] Coffee, tea, and other sources of caffeine temporarily block the effect of adenosine, prolong sleep latency, and reduce total sleep time and quality.[42]
Social timing
Humans are also influenced by aspects of social time, such as the hours when other people are awake, the hours when work is required, the time on clocks, etc. Time zones, standard times used to unify the timing for people in the same area, correspond only approximately to the natural rising and setting of the sun. An extreme example of the approximate nature of time zones is China, a country which used to span five time zones and now officially uses only one (UTC+8).[23]
Distribution
In polyphasic sleep, an organism sleeps several times in a 24-hour cycle, whereas in monophasic sleep this occurs all at once. Under experimental conditions, humans tend to alternate more frequently between sleep and wakefulness (i.e., exhibit more polyphasic sleep) if they have nothing better to do.[31] Given a 14-hour period of darkness in experimental conditions, humans tended towards bimodal sleep, with two sleep periods concentrated at the beginning and at the end of the dark time. Bimodal sleep in humans was more common before the Industrial Revolution.[34]
Different characteristic sleep patterns, such as the familiarly so-called "early bird" and "night owl", are called chronotypes. Genetics and sex have some influence on chronotype, but so do habits. Chronotype is also liable to change over the course of a person's lifetime. Seven-year-olds are better disposed to wake up early in the morning than are fifteen-year-olds.[24][23] Chronotypes far outside the normal range are called circadian rhythm sleep disorders.[43]
Naps
Naps are short periods of sleep that one might take during the daytime, often in order to get the necessary amount of rest. Napping is often associated with childhood, but around one-third of American adults partake in it daily. The optimal nap duration is around 10–20 minutes, as researchers have proven that it takes at least 30 minutes to enter slow-wave sleep, the deepest period of sleep.[44] Napping too long and entering the slow wave cycles can make it difficult to awake from the nap and leave one feeling unrested. This period of drowsiness is called sleep inertia.

The siesta habit has recently been associated with a 37% lower coronary mortality, possibly due to reduced cardiovascular stress mediated by daytime sleep.[45] Short naps at mid-day and mild evening exercise were found to be effective for improved sleep, cognitive tasks, and mental health in elderly people.[46]
Genetics
Monozygotic (identical) but not dizygotic (fraternal) twins tend to have similar sleep habits. Neurotransmitters, molecules whose production can be traced to specific genes, are one genetic influence on sleep that can be analyzed. The circadian clock has its own set of genes.[47] Genes which may influence sleep include ABCC9, DEC2, Dopamine receptor D2[48] and variants near PAX 8 and VRK2.[49] While the latter have been found in a GWAS study that primarily detects correlations (but not necessarily causation), other genes have been shown to have a more direct effect. For instance, mice lacking dihydropyrimidine dehydrogenase (Dpyd) had 78.4 min less sleep during the lights-off period than wild-type mice. Dpyd encodes the rate-limiting enzyme in the metabolic pathway that catabolizes uracil and thymidine to β-alanine, an inhibitory neurotransmitter. This also supports the role of β-alanine as a neurotransmitter that promotes sleep in mice.[50]
Genes for short sleep duration

Familial natural short sleep is a rare, genetic, typically inherited trait where an individual sleeps for fewer hours than average without suffering from daytime sleepiness or other consequences of sleep deprivation. This process is entirely natural in this kind of individual, and it is caused by certain genetic mutations.[51][52][53][54] A person with this trait is known as a "natural short sleeper".[55]
This condition is not to be confused with intentional sleep deprivation, which leaves symptoms such as irritability or temporarily impaired cognitive abilities in people who are predisposed to sleep a normal amount of time but not in people with FNSS.[56][57][58]
This sleep type is not considered to be a genetic disorder nor are there any known harmful effects to overall health associated with it; therefore it is considered to be a genetic, benign trait.[59]The genes DEC2, ADRB1, NPSR1 and GRM1 are implicated in enabling short sleep.[60]
Quality
The quality of sleep may be evaluated from an objective and a subjective point of view. Objective sleep quality refers to how difficult it is for a person to fall asleep and remain in a sleeping state, and how many times they wake up during a single night. Poor sleep quality disrupts the cycle of transition between the different stages of sleep.[61] Subjective sleep quality in turn refers to a sense of being rested and regenerated after awaking from sleep. A study by A. Harvey et al. (2002) found that insomniacs were more demanding in their evaluations of sleep quality than individuals who had no sleep problems.[62]
Homeostatic sleep propensity (the need for sleep as a function of the amount of time elapsed since the last adequate sleep episode) must be balanced against the circadian element for satisfactory sleep.[63][64] Along with corresponding messages from the circadian clock, this tells the body it needs to sleep.[65] The timing is correct when the following two circadian markers occur after the middle of the sleep episode and before awakening:[35] maximum concentration of the hormone melatonin, and minimum core body temperature.
Ideal duration


Human sleep-needs vary by age and amongst individuals;[68] sleep is considered to be adequate when there is no daytime sleepiness or dysfunction.[69] Moreover, self-reported sleep duration is only moderately correlated with actual sleep time as measured by actigraphy,[70] and those affected with sleep state misperception may typically report having slept only four hours despite having slept a full eight hours.[71][72][73]
Researchers have found that sleeping 6–7 hours each night correlates with longevity and cardiac health in humans, though many underlying factors may be involved in the causality behind this relationship.[74][75][76][77][49][78][79]
Sleep difficulties are furthermore associated with psychiatric disorders such as depression, alcoholism, and bipolar disorder.[80] Up to 90 percent of adults with depression are found to have sleep difficulties. Dysregulation detected by EEG includes disturbances in sleep continuity, decreased delta sleep and altered REM patterns with regard to latency, distribution across the night and density of eye movements.[81]
Sleep duration can also vary according to season. Up to 90% of people report longer sleep duration in winter, which may lead to more pronounced seasonal affective disorder.[82][83]
Children

By the time infants reach the age of two, their brain size has reached 90 percent of an adult-sized brain;[84] a majority of this brain growth has occurred during the period of life with the highest rate of sleep. The hours that children spend asleep influence their ability to perform on cognitive tasks.[85][86] Children who sleep through the night and have few night waking episodes have higher cognitive attainments and easier temperaments than other children.[86][87][88]
Sleep also influences language development. To test this, researchers taught infants a faux language and observed their recollection of the rules for that language.[89] Infants who slept within four hours of learning the language could remember the language rules better, while infants who stayed awake longer did not recall those rules as well. There is also a relationship between infants' vocabulary and sleeping: infants who sleep longer at night at 12 months have better vocabularies at 26 months.[88]
Children can greatly benefit from a structured bedtime routine. This can look differently among families, but will generally consist of a set of rituals such as reading a bedtime story, a bath, brushing teeth, and can also include a show of affection from the parent to the child such a hug or kiss before bed. A bedtime routine will also include a consistent time that the child is expected to be in bed ready for sleep. Having a reliable bedtime routine can help improve a child's quality of sleep as well as prepare them to make and keep healthy sleep hygiene habits in the future.[90]
Recommended duration

Children need many hours of sleep per day in order to develop and function properly: up to 18 hours for newborn babies, with a declining rate as a child ages.[65] Early in 2015, after a two-year study,[91] the National Sleep Foundation in the US announced newly revised recommendations as shown in the table below.
| Age and condition | Sleep needs |
|---|---|
| Newborns (0–3 months) | 14 to 17 hours |
| Infants (4–11 months) | 12 to 15 hours |
| Toddlers (1–2 years) | 11 to 14 hours |
| Preschoolers (3–4 years) | 10 to 13 hours |
| School-age children (5–12 years) | 9 to 11 hours |
| Teenagers (13–17 years) | 8 to 10 hours |
| Adults (18–64 years) | 7 to 9 hours |
| Older Adults (65 years and over) | 7 to 8 hours |
Functions
Restoration
Sleep may facilitate the synthesis of molecules that help repair and protect the brain from metabolic end products generated during waking.[92] Anabolic hormones, such as growth hormones, are secreted preferentially during sleep. The brain concentration of glycogen increases during sleep, and is depleted through metabolism during wakefulness.[93]
The human organism physically restores itself during sleep, occurring mostly during slow-wave sleep during which body temperature, heart rate, and brain oxygen consumption decrease. In both the brain and body, the reduced rate of metabolism enables countervailing restorative processes.[93] The brain requires sleep for restoration, whereas these processes can take place during quiescent waking in the rest of the body.[94] The essential function of sleep may be its restorative effect on the brain: "Sleep is of the brain, by the brain and for the brain."[95] This theory is strengthened by the fact that sleep is observed to be a necessary behavior across most of the animal kingdom, including some of the least cognitively advanced animals which have no need for other functions of sleep, such as memory consolidation or dreaming.[6][contradictory]
Memory processing
It has been widely accepted that sleep must support the formation of long-term memory, and generally increasing previous learning and experiences recalls. However, its benefit seems to depend on the phase of sleep and the type of memory.[96] For example, declarative and procedural memory-recall tasks applied over early and late nocturnal sleep, as well as wakefulness controlled conditions, have been shown that declarative memory improves more during early sleep (dominated by SWS) while procedural memory during late sleep (dominated by REM sleep) does so.[97][98]
With regard to declarative memory, the functional role of SWS has been associated with hippocampal replays of previously encoded neural patterns that seem to facilitate long-term memory consolidation.[97][98] This assumption is based on the active system consolidation hypothesis, which states that repeated reactivations of newly encoded information in the hippocampus during slow oscillations in NREM sleep mediate the stabilization and gradual integration of declarative memory with pre-existing knowledge networks on the cortical level.[99] It assumes the hippocampus might hold information only temporarily and in a fast-learning rate, whereas the neocortex is related to long-term storage and a slow-learning rate.[97][98][100][101][102] This dialogue between the hippocampus and neocortex occurs in parallel with hippocampal sharp-wave ripples and thalamo-cortical spindles, synchrony that drives the formation of the spindle-ripple event which seems to be a prerequisite for the formation of long-term memories.[98][100][102][103]
Reactivation of memory also occurs during wakefulness and its function is associated with serving to update the reactivated memory with newly encoded information, whereas reactivations during SWS are presented as crucial for memory stabilization.[98] Based on targeted memory reactivation (TMR) experiments that use associated memory cues to triggering memory traces during sleep, several studies have been reassuring the importance of nocturnal reactivations for the formation of persistent memories in neocortical networks, as well as highlighting the possibility of increasing people's memory performance at declarative recalls.[97][101][102][103][104]
Furthermore, nocturnal reactivation seems to share the same neural oscillatory patterns as reactivation during wakefulness, processes which might be coordinated by theta activity.[105] During wakefulness, theta oscillations have been often related to successful performance in memory tasks, and cued memory reactivations during sleep have been showing that theta activity is significantly stronger in subsequent recognition of cued stimuli as compared to uncued ones, possibly indicating a strengthening of memory traces and lexical integration by cuing during sleep.[106] However, the beneficial effect of TMR for memory consolidation seems to occur only if the cued memories can be related to prior knowledge.[107]
Dreaming

During sleep, especially REM sleep, humans tend to experience dreams. These are elusive and mostly unpredictable first-person experiences which seem logical and realistic to the dreamer while they are in progress, despite their frequently bizarre, irrational, and/or surreal qualities that become apparent when assessed after waking. Dreams often seamlessly incorporate concepts, situations, people, and objects within a person's mind that would not normally go together. They can include apparent sensations of all types, especially vision and movement.[108]
Dreams tend to rapidly fade from memory after waking. Some people choose to keep a dream journal, which they believe helps them build dream recall and facilitate the ability to experience lucid dreams.
A lucid dream is a type of dream in which the dreamer becomes aware that they are dreaming while dreaming. In a preliminary study, dreamers were able to consciously communicate with experimenters via eye movements or facial muscle signals, and were able to comprehend complex questions and use working memory.[109]
People have proposed many hypotheses about the functions of dreaming. Sigmund Freud postulated that dreams are the symbolic expression of frustrated desires that have been relegated to the unconscious mind, and he used dream interpretation in the form of psychoanalysis in attempting to uncover these desires.[110]
Counterintuitively, penile erections during sleep are not more frequent during sexual dreams than during other dreams.[111] The parasympathetic nervous system experiences increased activity during REM sleep which may cause erection of the penis or clitoris. In males, 80% to 95% of REM sleep is normally accompanied by partial to full penile erection, while only about 12% of men's dreams contain sexual content.[112]
Disorders
Insomnia
Insomnia is a general term for difficulty falling asleep and/or staying asleep. Insomnia is the most common sleep problem, with many adults reporting occasional insomnia, and 10–15% reporting a chronic condition.[113] Insomnia can have many different causes, including psychological stress, a poor sleep environment, an inconsistent sleep schedule, or excessive mental or physical stimulation in the hours before bedtime. Insomnia is often treated through behavioral changes like keeping a regular sleep schedule, avoiding stimulating or stressful activities before bedtime, and cutting down on stimulants such as caffeine. The sleep environment may be improved by installing heavy drapes to shut out all sunlight, and keeping computers, televisions, and work materials out of the sleeping area.
A 2010 review of published scientific research suggested that exercise generally improves sleep for most people, and helps sleep disorders such as insomnia. The optimum time to exercise may be 4 to 8 hours before bedtime, though exercise at any time of day is beneficial, with the exception of heavy exercise taken shortly before bedtime, which may disturb sleep. However, there is insufficient evidence to draw detailed conclusions about the relationship between exercise and sleep.[114] Nonbenzodiazepine sleeping medications such as Ambien, Imovane, and Lunesta (also known as "Z-drugs"), while initially believed to be better and safer than earlier generations of sedatives — including benzodiazepine drugs — are now known to be almost entirely the same as benzodiazepines in terms of their pharmacodynamics, differing only at the molecular level in their chemical structure, and therefore exhibit similar benefits, side-effects, and risks.[115][116] White noise appears to be a promising treatment for insomnia.[117]
Sleep health
Low quality sleep has been linked with health conditions like cardiovascular disease, obesity, and mental illness. While poor sleep is common among those with cardiovascular disease, some research indicates that poor sleep can be a contributing cause. Short sleep duration of less than seven hours is correlated with coronary heart disease and increased risk of death from coronary heart disease. Sleep duration greater than nine hours is also correlated with coronary heart disease, as well as stroke and cardiovascular events.[118][119][120][121]
In both children and adults, short sleep duration is associated with an increased risk of obesity, with various studies reporting an increased risk of 45–55%. Other aspects of sleep health have been associated with obesity, including daytime napping, sleep timing, the variability of sleep timing, and low sleep efficiency. However, sleep duration is the most-studied for its impact on obesity.[118]
Sleep problems have been frequently viewed as a symptom of mental illness rather than a causative factor. However, a growing body of evidence suggests that they are both a cause and a symptom of mental illness. Insomnia is a significant predictor of major depressive disorder; a meta-analysis of 170,000 people showed that insomnia at the beginning of a study period indicated a more than the twofold increased risk for major depressive disorder. Some studies have also indicated correlation between insomnia and anxiety, post-traumatic stress disorder, and suicide. Sleep disorders can increase the risk of psychosis and worsen the severity of psychotic episodes.[118]
Sleep research also displays differences in race and class. Short sleep and poor sleep are observed more frequently in ethnic minorities than in whites in the USA. African-Americans report experiencing short durations of sleep five times more often than whites, possibly as a result of social and environmental factors. A study done in the USA suggested that higher rates of sleep apnea (and poorer responses to treatment) are suffered by children in disadvantaged neighborhoods (which, in context, includes a disproportionate effect on children of African-American descent).[122]
Sleep health can be improved through implementing good sleep hygiene habits. Having good sleep hygiene can help to improve your physical and mental health by providing your body with the necessary rejuvenation only restful sleep can provide.[123] Some ways to improve sleep health include going to sleep at consistent times every night, avoiding any electronic devices such as televisions in the bedroom, getting adequate exercise throughout your day, and avoiding caffeine in the hours before going to sleep. Another way to greatly improve sleep hygiene is by creating a peaceful and relaxing sleep environment. Sleeping in a dark and clean room with things like a white noise maker can help facilitate restful sleep.[124] However, noise except of white noise may not good for sleep.
Drugs and diet
Drugs which induce sleep, known as hypnotics, include benzodiazepines (although these interfere with REM);[125] nonbenzodiazepine hypnotics such as eszopiclone (Lunesta), zaleplon (Sonata), and zolpidem (Ambien); antihistamines such as diphenhydramine (Benadryl) and doxylamine; alcohol (ethanol), (which exerts an excitatory rebound effect later in the night and intereferes with REM)[125] barbiturates (which have the same problem), melatonin (a component of the circadian clock)[126] and cannabis (which may also interfere with REM).[127] Some opioids (including morphine, codeine, heroin, and oxycodone) also induce sleep, and can disrupt sleep architecture and sleep stage distribution.[128] The endogenously produced drug gamma-hydroxybutyrate (GHB) is capable of producing high quality sleep that is indistinguishable from natural sleep architecture in humans.[129]
Stimulants, which inhibit sleep, include caffeine, an adenosine antagonist; amphetamine, methamphetamine, MDMA, empathogen-entactogens, and related drugs; cocaine, which can alter the circadian rhythm,[130][131] and methylphenidate, which acts similarly; and eugeroic drugs like modafinil and armodafinil with poorly understood mechanisms. Consuming high amounts of the stimulant caffeine can result in interrupted sleep patterns and sometimes sleep deprivation. This vicious cycle can result in drowsiness which can then result in a higher consumption of caffeine in order to stay awake the next day. This cycle can lead to decreased cognitive function and an overall feeling of fatigue.[132]
Some drugs may alter sleep architecture without inhibiting or inducing sleep. Drugs that amplify or inhibit endocrine and immune system secretions associated with certain sleep stages have been shown to alter sleep architecture.[133][134] The growth hormone releasing hormone receptor agonist MK-677 has been shown to increase REM in older adults as well as stage IV sleep in younger adults by approximately 50%.[135]
Diet
Dietary and nutritional choices may affect sleep duration and quality. One 2016 review indicated that a high-carbohydrate diet promoted a shorter onset to sleep and a longer duration of sleep than a high-fat diet.[136] A 2012 investigation indicated that mixed micronutrients and macronutrients are needed to promote quality sleep.[137] A varied diet containing fresh fruits and vegetables, low saturated fat, and whole grains may be optimal for individuals seeking to improve sleep quality.[136] Epidemiological studies indicate fewer insomnia symptoms and better sleep quality with a Mediterranean diet.[138][139] Two studies have indicated a benefit of tart cherry juice for insomnia, or for increasing sleep efficiency as well as total sleep time.[138] High-quality clinical trials on long-term dietary practices are needed to better define the influence of diet on sleep quality.[136]
In culture
Anthropology

Research suggests that sleep patterns vary significantly across cultures.[140][141][142] The most striking differences are observed between societies that have plentiful sources of artificial light and ones that do not. The primary difference appears to be that pre-light cultures have more broken-up sleep patterns. For example, people without artificial light might go to sleep far sooner after the sun sets, but then wake up several times throughout the night, punctuating their sleep with periods of wakefulness, perhaps lasting several hours.[140] During pre-industrial Europe, biphasic (bimodal) sleeping was considered the norm. Sleep onset was determined not by a set bedtime, but by whether there were things to do.[143]
The boundaries between sleeping and waking are blurred in these societies. Some observers believe that nighttime sleep in these societies is most often split into two main periods, the first characterized primarily by deep sleep and the second by REM sleep.[140]
Some societies display a fragmented sleep pattern in which people sleep at all times of the day and night for shorter periods. In many nomadic or hunter-gatherer societies, people sleep on and off throughout the day or night depending on what is happening. Plentiful artificial light has been available in the industrialized West since at least the mid-19th century, and sleep patterns have changed significantly everywhere that lighting has been introduced. In general, people sleep in a more concentrated burst through the night, going to sleep much later, although this is not always the case.[140]
Historian A. Roger Ekirch thinks that the traditional pattern of "segmented sleep," as it is called, began to disappear among the urban upper class in Europe in the late 17th century and the change spread over the next 200 years; by the 1920s "the idea of a first and second sleep had receded entirely from our social consciousness."[144][145] Ekirch attributes the change to increases in "street lighting, domestic lighting and a surge in coffee houses," which slowly made nighttime a legitimate time for activity, decreasing the time available for rest.[145] Today in most societies people sleep during the night, but in very hot climates they may sleep during the day.[146] During Ramadan, many Muslims sleep during the day rather than at night.[147]
In some societies, people sleep with at least one other person (sometimes many) or with animals. In other cultures, people rarely sleep with anyone except for an intimate partner. In almost all societies, sleeping partners are strongly regulated by social standards. For example, a person might only sleep with the immediate family, the extended family, a spouse or romantic partner, children, children of a certain age, children of a specific gender, peers of a certain gender, friends, peers of equal social rank, or with no one at all. Sleep may be an actively social time, depending on the sleep groupings, with no constraints on noise or activity.[140]
People sleep in a variety of locations. Some sleep directly on the ground; others on a skin or blanket; others sleep on platforms or beds. Some sleep with blankets, some with pillows, some with simple headrests, some with no head support. These choices are shaped by a variety of factors, such as climate, protection from predators, housing type, technology, personal preference, and the incidence of pests.[140]
In mythology and literature

Sleep has been seen in culture as similar to death since antiquity;[148] in Greek mythology, Hypnos (the god of sleep) and Thanatos (the god of death) were both said to be the children of Nyx (the goddess of night).[148] John Donne, Samuel Taylor Coleridge, Percy Bysshe Shelley, John Keats and other poets have all written poems about the relationship between sleep and death.[148] Shelley describes them as "both so passing, strange and wonderful!"[148] Keats similarly poses the question: "Can death be sleep, when life is but a dream".[149] Many people consider dying in one's sleep is the most peaceful way to die.[148] Phrases such as "big sleep" and "rest in peace" are often used in reference to death,[148] possibly in an effort to lessen its finality.[148] Sleep and dreaming have sometimes been seen as providing the potential for visionary experiences. In medieval Irish tradition, in order to become a filí, the poet was required to undergo a ritual called the imbas forosnai, in which they would enter a mantic, trancelike sleep.[150][151]
Many cultural stories have been told about people falling asleep for extended periods of time.[152][153] The earliest of these stories is the ancient Greek legend of Epimenides of Knossos.[152][154][155][156] According to the biographer Diogenes Laërtius, Epimenides was a shepherd on the Greek island of Crete.[152][157] One day, one of his sheep went missing and he went out to look for it, but became tired and fell asleep in a cave under Mount Ida.[152][157] When he awoke, he continued searching for the sheep, but could not find it,[152][157] so he returned to his old farm, only to discover that it was now under new ownership.[152][157] He went to his hometown, but discovered that nobody there knew him.[152] Finally, he met his younger brother, who was now an old man,[152][157] and learned that he had been asleep in the cave for fifty-seven years.[152][157]
A far more famous instance of a "long sleep" today is the Christian legend of the Seven Sleepers of Ephesus,[152] in which seven Christians flee into a cave during pagan times in order to escape persecution,[152] but fall asleep and wake up 360 years later to discover, to their astonishment, that the Roman Empire is now predominantly Christian.[152] The American author Washington Irving's short story "Rip Van Winkle", first published in 1819 in his collection of short stories The Sketch Book of Geoffrey Crayon, Gent.,[153][158] is about a man in colonial America named Rip Van Winkle who falls asleep on one of the Catskill Mountains and wakes up twenty years later after the American Revolution.[153] The story is now considered one of the greatest classics of American literature.[153]
In studies on consciousness and philosophy
As an altered state of consciousness, dreamless deep sleep has been used as a way to investigate animal/human consciousness and qualia. Insights about differences of the living sleeping brain to its wakeful state and the transition period may have implications for potential explanations of human subjective experience, the so-called hard problem of consciousness, often delegated to the realm of philosophy, including neurophilosophy[159][160][161][162] (or in some cases to religion and similar approaches).
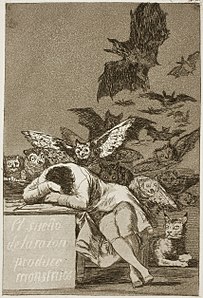
In art
Of the thematic representations of sleep in art, physician and sleep researcher Meir Kryger wrote, "[Artists] have intense fascination with mythology, dreams, religious themes, the parallel between sleep and death, reward, abandonment of conscious control, healing, a depiction of innocence and serenity, and the erotic."[163]
-
The Sentry (1654) by Carel Fabritius
-
The Second Class Carriage (1864) by Honoré Daumier
-
Taking a Rest (1882) by Ilya Repin
-
The Victory of Faith (1891) by Saint George Hare
-
Zwei schlafende Mädchen auf der Ofenbank (1895) by Albert Anker
-
Flaming June (c. 1895) by Frederic Leighton
-
Noon – Rest from Work (1890) by Vincent van Gogh (after Millet)
-
Sleeping Girl on a Wooden Bench by Albert Anker
See also
- Co-sleeping
- Hypnogram
- Microsleep
- Morvan's syndrome
- Oleamide
- Power nap
- Rheum
- Sleep epidemiology
- Sleep in space
- Sleep-learning
- Sleep medicine
- Sleep paralysis
- Sleeping positions
- Somnology
- Somnophilia
- Start school later movement
- Sudden infant death syndrome
- Sudden arrhythmic death syndrome
- Unconsciousness
- Yawn
- Yoga-nidra
References
- ^ "Brain Basics: Understanding Sleep | National Institute of Neurological Disorders and Stroke". www.ninds.nih.gov. Retrieved 15 February 2023.
- ^ Nelson, Ryan (20 June 2021). "The Dichotomy Of Sleep: REM And Non-REM Stages, And Their Impact On Human Health". Quantify Sleep. Retrieved 15 July 2023.
- ^ Krueger JM, Frank MG, Wisor JP, Roy S (August 2016). "Sleep function: Toward elucidating an enigma". Sleep Medicine Reviews. 28: 46–54. doi:10.1016/j.smrv.2015.08.005. ISSN 1087-0792. PMC 4769986. PMID 26447948.
- ^ "Sleep-wake cycle: its physiology and impact on health" (PDF). National Sleep Foundation. 2006. Archived (PDF) from the original on 30 August 2017. Retrieved 24 May 2017.
- ^ Bingham R, Terrence S, Siegel J, Dyken ME, Czeisler C (February 2007). "Waking Up To Sleep" (Several conference videos). The Science Network. Archived from the original on 24 July 2011. Retrieved 25 January 2008.
- ^ a b Joiner WJ (October 2016). "Unraveling the Evolutionary Determinants of Sleep". Current Biology. 26 (20): R1073–R1087. Bibcode:2016CBio...26R1073J. doi:10.1016/j.cub.2016.08.068. PMC 5120870. PMID 27780049.
- ^ Keene, Alex C & Duboue, Erik R. (12 June 2018). "The origins and evolution of sleep". The Journal of Experimental Biology. 221 (11). doi:10.1242/jeb.159533. PMC 6515771. PMID 29895581. Retrieved 10 January 2023.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Randall DK (19 September 2012). "Book excerpt: How the lightbulb disrupted our sleeping patterns and changed the world". National Post. Archived from the original on 7 April 2019. Retrieved 31 August 2016.
"... the sudden introduction of bright nights during hours when it should be dark threw a wrench into a finely choreographed system of life.
- ^ "How Blue Light Affects Sleep". Sleep Foundation. 4 November 2020. Retrieved 18 November 2021.
- ^ a b c Maquet PA, Sterpenich V, Albouy G, Dang-Vu T, Desseilles M, Boly M, et al. (2005). "Brain Imaging on Passing to Sleep". The Physiologic Nature of Sleep. Published by Imperial College Press and Distributed by World Scientific Publishing Co. pp. 123–137. doi:10.1142/9781860947186_0006. ISBN 978-1-86094-557-1.
- ^ Brown, pp. 1118–1119: "Compared with wakefulness, sleep reduces brain energy demands, as suggested by the 44% reduction in the cerebral metabolic rate (CMR) of glucose (791) and a 25% reduction in the CMR of O2 (774) during sleep."
- ^ a b Siegel JM (April 2008). "Do all animals sleep?". Trends in Neurosciences. 31 (4): 208–13. doi:10.1016/j.tins.2008.02.001. PMC 8765194. PMID 18328577. S2CID 6614359.
- ^ a b c Van Cauter E, Spiegel K (1999). "Circadian and Sleep Control of Hormonal Secretions". In Zee PC, Turek FW (eds.). Regulation of Sleep and Circadian Rhythms. pp. 397–425.
- ^ Brown, p. 1087.
- ^ a b c d Peraita-Adrados R (2005). "Electroencephalography, Polysomnography, and Other Sleep Recording Systems". The Physiologic Nature of Sleep. Published by Imperial College Press and Distributed by World Scientific Publishing Co. pp. 103–122. doi:10.1142/9781860947186_0005. ISBN 978-1-86094-557-1.
- ^ Borbély AA, Daan S, Wirz-Justice A, Deboer T (14 January 2016), "The two-process model of sleep regulation: a reappraisal" (PDF), J Sleep Res, 25 (2): 131–43, doi:10.1111/jsr.12371, PMID 26762182, S2CID 206156163
- ^ Posada-Quintero HF, Reljin N, Bolkhovsky JB, Orjuela-Cañón AD, Chon KH (19 September 2019), "Brain Activity Correlates With Cognitive Performance Deterioration During Sleep Deprivation.", Front. Neurosci., 13: 1001, doi:10.3389/fnins.2019.01001, PMC 6761229, PMID 31607847
- ^ a b "Brain Basics: Understanding Sleep". National Institute of Neurological Disorders and Stroke.
- ^ Parmeggiani PL, ed. (2011). Systemic Homeostasis and Poikilostasis in Sleep: Is REM Sleep a Physiological Paradox?. London: Imperial College Press. pp. 12–5. ISBN 978-1-94916-572-2.
- ^ McCarley RW (June 2007). "Neurobiology of REM and NREM sleep". Sleep Medicine. 8 (4): 302–30. doi:10.1016/j.sleep.2007.03.005. PMID 17468046.
- ^ Silber MH, Ancoli-Israel S, Bonnet MH, Chokroverty S, Grigg-Damberger MM, Hirshkowitz M, et al. (March 2007). "The visual scoring of sleep in adults". Journal of Clinical Sleep Medicine. 3 (2): 121–31. doi:10.5664/jcsm.26814. PMID 17557422.
- ^ a b c d e Akerstedt T, Billiard M, Bonnet M, Ficca G, Garma L, Mariotti M, et al. (August 2002). "Awakening from sleep". Sleep Medicine Reviews. 6 (4): 267–86. doi:10.1053/smrv.2001.0202. PMID 12531132.
- ^ a b c d e f Roenneberg T, Kuehnle T, Juda M, Kantermann T, Allebrandt K, Gordijn M, Merrow M (December 2007). "Epidemiology of the human circadian clock" (PDF). Sleep Medicine Reviews. 11 (6): 429–38. doi:10.1016/j.smrv.2007.07.005. hdl:11370/65d6f03a-88cd-405c-a067-4afbc1b9ba9d. PMID 17936039. S2CID 11628329.
- ^ a b c d Waterhouse J, Fukuda Y, Morita T (March 2012). "Daily rhythms of the sleep-wake cycle". Journal of Physiological Anthropology. 31 (5): 5. doi:10.1186/1880-6805-31-5. PMC 3375033. PMID 22738268.
- ^ a b Chang AM, Aeschbach D, Duffy JF, Czeisler CA (January 2015). "Evening use of light-emitting eReaders negatively affects sleep, circadian timing, and next-morning alertness". Proceedings of the National Academy of Sciences of the United States of America. 112 (4): 1232–7. Bibcode:2015PNAS..112.1232C. doi:10.1073/pnas.1418490112. PMC 4313820. PMID 25535358.
- ^ Basner M, Dinges DF (June 2009). "Dubious bargain: trading sleep for Leno and Letterman". Sleep. 32 (6): 747–52. doi:10.1093/sleep/32.6.747. PMC 2690561. PMID 19544750.
- ^ Tassi P, Muzet A (August 2000). "Sleep inertia". Sleep Medicine Reviews. 4 (4): 341–353. doi:10.1053/smrv.2000.0098. PMID 12531174.
- ^ Vallat, Raphael; Berry, Sarah E.; Tsereteli, Neli; Capdevila, Joan; Khatib, Haya Al; Valdes, Ana M.; Delahanty, Linda M.; Drew, David A.; Chan, Andrew T.; Wolf, Jonathan; Franks, Paul W.; Spector, Tim D.; Walker, Matthew P. (19 November 2022). "How people wake up is associated with previous night's sleep together with physical activity and food intake". Nature Communications. 13 (1): 7116. Bibcode:2022NatCo..13.7116V. doi:10.1038/s41467-022-34503-2. ISSN 2041-1723. PMC 9675783. PMID 36402781.
- ^ Fuller PM, Gooley JJ, Saper CB (December 2006). "Neurobiology of the sleep-wake cycle: sleep architecture, circadian regulation, and regulatory feedback". Journal of Biological Rhythms. 21 (6): 482–93. doi:10.1177/0748730406294627. PMID 17107938. S2CID 36572447.
- ^ Zee PC, Turek FW (1999). "Introduction to Sleep and Circadian Rhythms". In Zee PC, Turek FW (eds.). Regulation of Sleep and Circadian Rhythms. pp. 1–17.
- ^ a b c d e f g Derk-Jan D, Edgar DM (1999). "Circadian and Homeostatic Control of Wakefulness and Sleep". In Zee PC, Turek FW (eds.). Regulation of Sleep and Circadian Rhythms. pp. 111–147.
- ^ a b Czeisler CA, Wright Jr KP (1999). "Influence of Light on Circadian Rhythmicity in Humans". In Zee PC, Turek FW (eds.). Regulation of Sleep and Circadian Rhythms. pp. 149–180.
- ^ a b Zlomanczuk P, Schwartz WJ (1999). "Cellular and Molecular Mechanisms of Circadian Rhythms in Mammals". In Zee PC, Turek FW (eds.). Regulation of Sleep and Circadian Rhythms. pp. 309–342.
- ^ a b Wehr TA (1999). "The Impact of Changes in Nightlength (Scotoperiod) on Human Sleep". In Zee PC, Turek FW (eds.). Regulation of Sleep and Circadian Rhythms. pp. 263–285.
- ^ a b Wyatt JK, Ritz-De Cecco A, Czeisler CA, Dijk DJ (October 1999). "Circadian temperature and melatonin rhythms, sleep, and neurobehavioral function in humans living on a 20-h day". The American Journal of Physiology. 277 (4 Pt 2): R1152-63. doi:10.1152/ajpregu.1999.277.4.r1152. PMID 10516257. S2CID 4474347.
... significant homeostatic and circadian modulation of sleep structure, with the highest sleep efficiency occurring in sleep episodes bracketing the melatonin maximum and core body temperature minimum
- ^ Schwartz JR, Roth T (December 2008). "Neurophysiology of sleep and wakefulness: basic science and clinical implications". Current Neuropharmacology. 6 (4): 367–78. doi:10.2174/157015908787386050. PMC 2701283. PMID 19587857.
- ^ Brown, pp. 1134–1138.
- ^ Gottselig JM, Adam M, Rétey JV, Khatami R, Achermann P, Landolt HP (March 2006). "Random number generation during sleep deprivation: effects of caffeine on response maintenance and stereotypy". Journal of Sleep Research. 15 (1): 31–40. doi:10.1111/j.1365-2869.2006.00497.x. PMID 16490000. S2CID 10355305.
- ^ Iglowstein I, Jenni OG, Molinari L, Largo RH (February 2003). "Sleep duration from infancy to adolescence: reference values and generational trends". Pediatrics. 111 (2): 302–7. doi:10.1542/peds.111.2.302. PMID 12563055. S2CID 8727836.
Thus, the shift in the evening bedtime across cohorts accounted for the substantial decrease in sleep duration in younger children between the 1970s and the 1990s... [A] more liberal parental attitude toward evening bedtime in the past decades is most likely responsible for the bedtime shift and for the decline of sleep duration...
- ^ Huang ZL, Zhang Z, Qu WM (2014). "Roles of adenosine and its receptors in sleep-wake regulation". International Review of Neurobiology. 119: 349–71. doi:10.1016/B978-0-12-801022-8.00014-3. ISBN 978-0-12-801022-8. PMID 25175972.
- ^ "The brain from top to bottom: Molecules that build up and make you sleep". McGill University, Montreal, Quebec, Canada. Archived from the original on 7 February 2013. Retrieved 20 September 2012.
- ^ Clark I, Landolt HP (February 2017). "Coffee, caffeine, and sleep: A systematic review of epidemiological studies and randomized controlled trials" (PDF). Sleep Medicine Reviews. 31: 70–78. doi:10.1016/j.smrv.2016.01.006. PMID 26899133. Archived (PDF) from the original on 4 November 2018. Retrieved 19 November 2018.
- ^ Dagan Y (February 2002). "Circadian rhythm sleep disorders (CRSD)" (PDF). Sleep Medicine Reviews. 6 (1): 45–54. doi:10.1053/smrv.2001.0190. PMID 12531141. Archived from the original (PDF: full text) on 27 February 2008. Retrieved 5 June 2016.
Early onset of CRSD, the ease of diagnosis, the high frequency of misdiagnosis and erroneous treatment, the potentially harmful psychological and adjustment consequences, and the availability of promising treatments, all indicate the importance of greater awareness of these disorders.
- ^ Fry, A. (9 October 2020). Napping: Health Benefits & Tips for your best nap. Sleep Foundation. Retrieved 14 November 2021, from https://www.sleepfoundation.org/sleep-hygiene/napping .
- ^ Naska A, Oikonomou E, Trichopoulou A, Psaltopoulou T, Trichopoulos D (February 2007). "Siesta in healthy adults and coronary mortality in the general population". Archives of Internal Medicine. 167 (3): 296–301. doi:10.1001/archinte.167.3.296. PMID 17296887.
- ^ Tanaka H, Tamura N (January 2016). "Sleep education with self-help treatment and sleep health promotion for mental and physical wellness in Japan". Sleep and Biological Rhythms. 14 (S1): 89–99. doi:10.1007/s41105-015-0018-6. PMC 4732678. PMID 26855610.
- ^ Brown, pp. 1138–1102.
- ^ Zhang L, Fu YH (January 2020). "The molecular genetics of human sleep". The European Journal of Neuroscience. 51 (1): 422–428. doi:10.1111/ejn.14132. PMC 6389443. PMID 30144347.
- ^ a b Jones SE, Tyrrell J, Wood AR, Beaumont RN, Ruth KS, Tuke MA, et al. (August 2016). "Genome-Wide Association Analyses in 128,266 Individuals Identifies New Morningness and Sleep Duration Loci". PLOS Genetics. 12 (8): e1006125. doi:10.1371/journal.pgen.1006125. PMC 4975467. PMID 27494321.
- ^ Keenan BT, Galante RJ, Lian J, Zhang L, Guo X, Veatch OJ, et al. (December 2021). "The dihydropyrimidine dehydrogenase gene contributes to heritable differences in sleep in mice". Current Biology. 31 (23): 5238–5248.e7. Bibcode:2021CBio...31E5238K. doi:10.1016/j.cub.2021.09.049. PMC 8665053. PMID 34653361. S2CID 238754563.
- ^ "Short Sleeper Syndrome: What Causes Short Sleep Duration?". Circle Magazine | Health, Wellness & Genetics Blog. 30 September 2021. Retrieved 14 October 2022.
- ^ "Short Sleeper Syndrome: Symptoms, Causes, and Treatments". Sleep Foundation. 27 April 2022. Retrieved 15 October 2022.
- ^ Hancock, Jay (9 October 2022). "This easy, no-cost solution could help treat a super common sleep condition". Inverse. Retrieved 15 October 2022.
- ^ Yook, Ji Hyun; Rizwan, Muneeba; Shahid, Noor ul ain; Naguit, Noreen; Jakkoju, Rakesh; Laeeq, Sadia; Reghefaoui, Tiba; Zahoor, Hafsa; Mohammed, Lubna (25 October 2021). "Some Twist of Molecular Circuitry Fast Forwards Overnight Sleep Hours: A Systematic Review of Natural Short Sleepers' Genes". Cureus. 13 (10): e19045. doi:10.7759/cureus.19045. ISSN 2168-8184. PMC 8547374. PMID 34722012.
- ^ "Natural short sleeper: MedlinePlus Medical Encyclopedia". medlineplus.gov. Retrieved 14 October 2022.
- ^ "Is it Dangerous to Be a Chronic Short Sleeper?". healthcare.utah.edu. 8 August 2018. Retrieved 14 October 2022.
- ^ Panchin, Yuri; Kovalzon, Vladimir M. (2021). "Total Wake: Natural, Pathological, and Experimental Limits to Sleep Reduction". Frontiers in Neuroscience. 15: 643496. doi:10.3389/fnins.2021.643496. ISSN 1662-453X. PMC 8058214. PMID 33897357.
- ^ "The long and short of the 'short sleep' gene | Sleep Cycle". Sleep Cycle alarm clock. 3 February 2022. Retrieved 15 October 2022.
- ^ "Short sleep, familial natural, 1 - NIH Genetic Testing Registry (GTR) - NCBI". www.ncbi.nlm.nih.gov. Retrieved 13 October 2022.
- ^ Zheng, Liubin; Zhang, Luoying (September 2022). "The molecular mechanism of natural short sleep: A path towards understanding why we need to sleep". Brain Science Advances. 8 (3): 165–172. doi:10.26599/BSA.2022.9050003. ISSN 2096-5958. S2CID 250363367.
- ^ Barnes CM, Lucianetti L, Bhave DP, Christian MS (2015). "You wouldn't like me when I'm sleepy: Leaders' sleep, daily abusive supervision, and work unit engagement". Academy of Management Journal. 58 (5): 1419–1437. doi:10.5465/amj.2013.1063. S2CID 145056840.
- ^ Harvey AG, Payne S (March 2002). "The management of unwanted pre-sleep thoughts in insomnia: distraction with imagery versus general distraction". Behaviour Research and Therapy. 40 (3): 267–77. doi:10.1016/s0005-7967(01)00012-2. PMID 11863237. S2CID 16647017.
- ^ Zisapel N (May 2007). "Sleep and sleep disturbances: biological basis and clinical implications". Cellular and Molecular Life Sciences. 64 (10): 1174–86. doi:10.1007/s00018-007-6529-9. PMC 11136060. PMID 17364142. S2CID 2003308.
- ^ Dijk DJ, Lockley SW (February 2002). "Integration of human sleep-wake regulation and circadian rhythmicity". Journal of Applied Physiology. 92 (2): 852–62. doi:10.1152/japplphysiol.00924.2001. PMID 11796701. S2CID 2502686.
Consolidation of sleep for 8 h or more is only observed when sleep is initiated ~6–8 h before the temperature nadir.
- ^ a b de Benedictis T, Larson H, Kemp G, Barston S, Segal R (2007). "Understanding Sleep: Sleep Needs, Cycles, and Stages". Helpguide.org. Archived from the original on 24 January 2008. Retrieved 25 January 2008.
- ^ "How Much Sleep Do I Need?". CDC.gov. Centers for Disease Control and Prevention (CDC). 14 September 2022. Archived from the original on 2 November 2023.
Last Reviewed: September 14, 2022. Source: National Center for Chronic Disease Prevention and Health Promotion, Division of Population Health.
- ^ Reference list is found on image page in Commons: Commons:File:Effects of sleep deprivation.svg#References
- ^ Hirshkowitz, Max; Whiton, Kaitlyn; Albert, Steven M.; Alessi, Cathy; Bruni, Oliviero; DonCarlos, Lydia; Hazen, Nancy; Herman, John; Katz, Eliot S.; Kheirandish-Gozal, Leila; Neubauer, David N.; O'Donnell, Anne E.; Ohayon, Maurice; Peever, John; Rawding, Robert (March 2015). "National Sleep Foundation's sleep time duration recommendations: methodology and results summary". Sleep Health. 1 (1): 40–43. doi:10.1016/j.sleh.2014.12.010. ISSN 2352-7226. PMID 29073412. S2CID 205190733.
- ^ Benbadis, S. R. (November 1998). "Daytime sleepiness: when is it normal? When to refer?". Cleveland Clinic Journal of Medicine. 65 (10): 543–549. doi:10.3949/ccjm.65.10.543. ISSN 0891-1150. PMID 9830788. S2CID 8222974.
- ^ Lauderdale DS, Knutson KL, Yan LL, Liu K, Rathouz PJ (November 2008). "Self-reported and measured sleep duration: how similar are they?". Epidemiology. 19 (6): 838–45. doi:10.1097/EDE.0b013e318187a7b0. PMC 2785092. PMID 18854708.
- ^ Insomnia Causes Archived 22 October 2010 at the Wayback Machine. Healthcommunities.com. Original Publication: 1 December 2000, Updated: 1 December 2007.
- ^ Arditte Hall, Kimberly A.; Werner, Kimberly B.; Griffin, Michael G.; Galovski, Tara E. (10 January 2022). "Exploring Predictors of Sleep State Misperception in Women with Posttraumatic Stress Disorder". Behavioral Sleep Medicine. 21 (1): 22–32. doi:10.1080/15402002.2021.2024193. ISSN 1540-2010. PMC 9271136. PMID 35007171.
- ^ Truzzi, Giselle de Martin; Teixeira, Igor de Lima; do Prado, Lucila Bizari Fernandes; do Prado, Gilmar Fernandes; Tufik, Sergio; Coelho, Fernando Morgadinho (January 2021). "Sleep state misperception: is there a CNS structural source?". Sleep Science (Sao Paulo, Brazil). 14 (Spec 1): 94–96. doi:10.5935/1984-0063.20200039. ISSN 1984-0659. PMC 8663728. PMID 34917280.
- ^ Rowland R (15 February 2002). "Experts challenge study linking sleep, life span". CNN. Archived from the original on 5 October 2012. Retrieved 29 October 2013.
- ^ Patel SR, Ayas NT, Malhotra MR, White DP, Schernhammer ES, Speizer FE, et al. (May 2004). "A prospective study of sleep duration and mortality risk in women". Sleep. 27 (3): 440–4. doi:10.1093/sleep/27.3.440. PMID 15164896.
- ^ Patel SR, Malhotra A, Gottlieb DJ, White DP, Hu FB (July 2006). "Correlates of long sleep duration". Sleep. 29 (7): 881–9. doi:10.1093/sleep/29.7.881. PMC 3500381. PMID 16895254.; cf. Irwin MR, Ziegler M (February 2005). "Sleep deprivation potentiates activation of cardiovascular and catecholamine responses in abstinent alcoholics". Hypertension. 45 (2): 252–7. CiteSeerX 10.1.1.535.7089. doi:10.1161/01.HYP.0000153517.44295.07. PMID 15642774. S2CID 2205895.
- ^ Ferrie JE, Shipley MJ, Cappuccio FP, Brunner E, Miller MA, Kumari M, Marmot MG (December 2007). "A prospective study of change in sleep duration: associations with mortality in the Whitehall II cohort". Sleep. 30 (12): 1659–66. doi:10.1093/sleep/30.12.1659. PMC 2276139. PMID 18246975.
- ^ Cappuccio FP, Taggart FM, Kandala NB, Currie A, Peile E, Stranges S, Miller MA (May 2008). "Meta-analysis of short sleep duration and obesity in children and adults". Sleep. 31 (5): 619–26. doi:10.1093/sleep/31.5.619. PMC 2398753. PMID 18517032.
- ^ Schmid SM, Hallschmid M, Schultes B (January 2015). "The metabolic burden of sleep loss". The Lancet. Diabetes & Endocrinology. 3 (1): 52–62. doi:10.1016/S2213-8587(14)70012-9. PMID 24731536.
- ^ Thase ME (2006). "Depression and sleep: pathophysiology and treatment". Dialogues in Clinical Neuroscience. 8 (2): 217–26. doi:10.31887/DCNS.2006.8.2/mthase. PMC 3181772. PMID 16889107.
- ^ Mann JJ, Kupfer DJ (1993). Biology of Depressive Disorders: Subtypes of depression and comorbid disorders, Part 2 (Google books). Springer. p. 49. ISBN 978-0-306-44296-4. Archived from the original on 10 March 2017. Retrieved 24 July 2009.
- ^ Suzuki M, Taniguchi T, Furihata R, Yoshita K, Arai Y, Yoshiike N, Uchiyama M (18 April 2019). "Seasonal changes in sleep duration and sleep problems: A prospective study in Japanese community residents". PLOS ONE. 14 (4): e0215345. Bibcode:2019PLoSO..1415345S. doi:10.1371/journal.pone.0215345. PMC 6472875. PMID 30998709.
- ^ "Hate waking up when it's dark out? Find out how winter really affects your sleep habits". Sleep.org. 30 January 2023. Archived from the original on 2 March 2021.
- ^ Dahl RE (2009). "The regulation of sleep and arousal: Development and psychopathology". Development and Psychopathology. 8 (1): 3–27. doi:10.1017/S0954579400006945. S2CID 143514600.
- ^ Jenni OG, Dahl RE (2008). "Sleep, cognition, and neuron, and emotion: A developmental review.". In Nelson CA, Luciana M (eds.). Handbook of developmental cognitive neuroscience (2nd ed.). Cambridge, Mass.: MIT Press. pp. 807–817. ISBN 978-0262141048.
- ^ a b Scher A (March 2005). "Infant sleep at 10 months of age as a window to cognitive development". Early Human Development. 81 (3): 289–92. doi:10.1016/j.earlhumdev.2004.07.005. PMID 15814211.
- ^ Spruyt K, Aitken RJ, So K, Charlton M, Adamson TM, Horne RS (May 2008). "Relationship between sleep/wake patterns, temperament and overall development in term infants over the first year of life". Early Human Development. 84 (5): 289–96. doi:10.1016/j.earlhumdev.2007.07.002. PMID 17707119.
- ^ a b Bernier A, Carlson SM, Bordeleau S, Carrier J (2010). "Relations between physiological and cognitive regulatory systems: infant sleep regulation and subsequent executive functioning". Child Development. 81 (6): 1739–52. doi:10.1111/j.1467-8624.2010.01507.x. PMID 21077861.
- ^ Hupbach A, Gomez RL, Bootzin RR, Nadel L (November 2009). "Nap-dependent learning in infants". Developmental Science. 12 (6): 1007–12. CiteSeerX 10.1.1.712.685. doi:10.1111/j.1467-7687.2009.00837.x. PMID 19840054.
- ^ Mindell JA, Williamson AA (August 2018). "Benefits of a bedtime routine in young children: Sleep, development, and beyond". Sleep Medicine Reviews. 40: 93–108. doi:10.1016/j.smrv.2017.10.007. PMC 6587181. PMID 29195725.
- ^ a b Hirshkowitz M, Whiton K, Albert SM, Alessi C, Bruni O, DonCarlos L, et al. (March 2015). "National Sleep Foundation's sleep time duration recommendations: methodology and results summary". Sleep Health. 1 (1): 40–43. doi:10.1016/j.sleh.2014.12.010. PMID 29073412. S2CID 205190733. Archived from the original on 14 November 2017. Retrieved 4 February 2015.
- ^ Siegel JM (October 2005). "Clues to the functions of mammalian sleep". Nature. 437 (7063): 1264–71. Bibcode:2005Natur.437.1264S. doi:10.1038/nature04285. PMC 8760626. PMID 16251951. S2CID 234089.
- ^ a b Raymond Cespuglio, Damien Colas, & Sabine Gautier-Sauvigné, "Energy Processes Underlying the Sleep Wake Cycle"; Chapter 1 in Parmeggiani & Velluti (2005).
- ^ Eugene AR, Masiak J (March 2015). "The Neuroprotective Aspects of Sleep". MEDtube Science. 3 (1): 35–40. PMC 4651462. PMID 26594659.
- ^ Hobson JA (October 2005). "Sleep is of the brain, by the brain and for the brain". Nature. 437 (7063): 1254–1256. Bibcode:2005Natur.437.1254H. doi:10.1038/nature04283. PMID 16251949. S2CID 1055112.
- ^ Plihal W, Born J (July 1997). "Effects of early and late nocturnal sleep on declarative and procedural memory". Journal of Cognitive Neuroscience. 9 (4): 534–47. doi:10.1162/jocn.1997.9.4.534. PMID 23968216. S2CID 3300300.
- ^ a b c d Rasch B, Büchel C, Gais S, Born J (March 2007). "Odor cues during slow-wave sleep prompt declarative memory consolidation". Science. 315 (5817): 1426–9. Bibcode:2007Sci...315.1426R. doi:10.1126/science.1138581. PMID 17347444. S2CID 19788434.
- ^ a b c d e Born J, Wilhelm I (March 2012). "System consolidation of memory during sleep". Psychological Research. 76 (2): 192–203. doi:10.1007/s00426-011-0335-6. PMC 3278619. PMID 21541757.
- ^ Diekelmann S, Born J (February 2010). "The memory function of sleep". Nature Reviews. Neuroscience. 11 (2): 114–26. doi:10.1038/nrn2762. PMID 20046194. S2CID 1851910.
- ^ a b Rasch B, Born J (April 2013). "About sleep's role in memory". Physiological Reviews. 93 (2): 681–766. doi:10.1152/physrev.00032.2012. PMC 3768102. PMID 23589831.
- ^ a b Schreiner T, Rasch B (November 2015). "Boosting Vocabulary Learning by Verbal Cueing During Sleep". Cerebral Cortex. 25 (11): 4169–79. doi:10.1093/cercor/bhu139. PMID 24962994.
- ^ a b c Schreiner T, Rasch B (April 2017). "The beneficial role of memory reactivation for language learning during sleep: A review" (PDF). Brain and Language. 167: 94–105. doi:10.1016/j.bandl.2016.02.005. PMID 27036946. S2CID 3377186.
- ^ a b Ngo HV, Martinetz T, Born J, Mölle M (May 2013). "Auditory closed-loop stimulation of the sleep slow oscillation enhances memory". Neuron. 78 (3): 545–53. doi:10.1016/j.neuron.2013.03.006. PMID 23583623.
- ^ Klinzing JG, Kugler S, Soekadar SR, Rasch B, Born J, Diekelmann S (January 2018). "Odor cueing during slow-wave sleep benefits memory independently of low cholinergic tone". Psychopharmacology. 235 (1): 291–299. doi:10.1007/s00213-017-4768-5. PMC 5748395. PMID 29119218.
- ^ Schreiner T, Doeller CF, Jensen O, Rasch B, Staudigl T (October 2018). "Theta Phase-Coordinated Memory Reactivation Reoccurs in a Slow-Oscillatory Rhythm during NREM Sleep". Cell Reports. 25 (2): 296–301. doi:10.1016/j.celrep.2018.09.037. PMC 6198287. PMID 30304670.
- ^ Schreiner T, Göldi M, Rasch B (November 2015). "Cueing vocabulary during sleep increases theta activity during later recognition testing". Psychophysiology. 52 (11): 1538–43. doi:10.1111/psyp.12505. PMID 26235609.
- ^ Groch S, Schreiner T, Rasch B, Huber R, Wilhelm I (January 2017). "Prior knowledge is essential for the beneficial effect of targeted memory reactivation during sleep". Scientific Reports. 7: 39763. Bibcode:2017NatSR...739763G. doi:10.1038/srep39763. PMC 5209656. PMID 28051138.
- ^ J. Alan Hobson, Edward F. Pace-Scott, & Robert Stickgold (2000), "Dreaming and the brain: Toward a cognitive neuroscience of conscious states", Behavioral and Brain Sciences 23.
- ^ Konkoly, Karen R.; Appel, Kristoffer; Chabani, Emma; et al. (18 February 2021). "Real-time dialogue between experimenters and dreamers during REM sleep". Current Biology. 31 (7): 1417–1427.e6. Bibcode:2021CBio...31E1417K. doi:10.1016/j.cub.2021.01.026. ISSN 0960-9822. PMC 8162929. PMID 33607035.
 Available under CC BY 4.0 Archived 16 October 2017 at the Wayback Machine.
Available under CC BY 4.0 Archived 16 October 2017 at the Wayback Machine.
- ^ See Freud: The Interpretation of Dreams.
- ^ Pinel JP (2011). Biopsychology, 8th Edition. Pearson Education, Inc. p. 359. ISBN 978-0-205-83256-9.
- ^ Saladin KS (2012). Anatomy and Physiology: The Unity of Form and Function (6th ed.). McGraw-Hill. p. 537. ISBN 978-0-07-337825-1.
- ^ Brown, pp. 1146–1147.
- ^ Buman MP, King AC (2010). "Exercise as a Treatment to Enhance Sleep". American Journal of Lifestyle Medicine. 4 (6): 500–514. doi:10.1177/1559827610375532. S2CID 73314918.
- ^ Siriwardena AN, Qureshi Z, Gibson S, Collier S, Latham M (December 2006). "GPs' attitudes to benzodiazepine and 'Z-drug' prescribing: a barrier to implementation of evidence and guidance on hypnotics". The British Journal of General Practice. 56 (533): 964–7. PMC 1934058. PMID 17132386.
- ^ Wagner J, Wagner ML, Hening WA (June 1998). "Beyond benzodiazepines: alternative pharmacologic agents for the treatment of insomnia". The Annals of Pharmacotherapy. 32 (6): 680–91. doi:10.1345/aph.17111. PMID 9640488. S2CID 34250754.
- ^ López HH, Bracha AS, Bracha HS (September 2002). "Evidence based complementary intervention for insomnia" (PDF). Hawaii Medical Journal. 61 (9): 192, 213. PMID 12422383. Archived (PDF) from the original on 1 May 2015. Retrieved 16 December 2010.
- ^ a b c Hale L, Troxel W, Buysse DJ (April 2020). "Sleep Health: An Opportunity for Public Health to Address Health Equity". Annual Review of Public Health. 41 (1): 81–99. doi:10.1146/annurev-publhealth-040119-094412. PMC 7944938. PMID 31900098.
- ^ Jackson CL, Redline S, Emmons KM (March 2015). "Sleep as a potential fundamental contributor to disparities in cardiovascular health". Annual Review of Public Health. 36 (1): 417–440. doi:10.1146/annurev-publhealth-031914-122838. PMC 4736723. PMID 25785893.
- ^ Cespedes Feliciano EM, Quante M, Rifas-Shiman SL, Redline S, Oken E, Taveras EM (July 2018). "Objective Sleep Characteristics and Cardiometabolic Health in Young Adolescents". Pediatrics. 142 (1): e20174085. doi:10.1542/peds.2017-4085. PMC 6260972. PMID 29907703.
- ^ St-Onge MP, Grandner MA, Brown D, Conroy MB, Jean-Louis G, Coons M, Bhatt DL (November 2016). "Sleep Duration and Quality: Impact on Lifestyle Behaviors and Cardiometabolic Health: A Scientific Statement From the American Heart Association". Circulation (Review). 134 (18): e367–e386. doi:10.1161/CIR.0000000000000444. PMC 5567876. PMID 27647451.
- ^ Wang R, Dong Y, Weng J, Kontos EZ, Chervin RD, Rosen CL, et al. (January 2017). "Associations among Neighborhood, Race, and Sleep Apnea Severity in Children. A Six-City Analysis". Annals of the American Thoracic Society. 14 (1): 76–84. doi:10.1513/AnnalsATS.201609-662OC. PMC 5291481. PMID 27768852.
- ^ "Mental Health and Sleep". Sleep Foundation. 18 September 2020. Retrieved 18 November 2021.
- ^ "CDC - Sleep Hygiene Tips - Sleep and Sleep Disorders". cdc.gov. 13 February 2019. Retrieved 18 November 2021.
- ^ a b Lee-chiong T (2008). Sleep Medicine: Essentials and Review. Oxford University Press, US. p. 52. ISBN 978-0-19-530659-0. Archived from the original on 11 March 2017. Retrieved 25 September 2016.
- ^ Turek FW, Czeisler CA (1999). "Role of Melatonin in the Regulation of Sleep". In Zee PC, Turek FW (eds.). Regulation of Sleep and Circadian Rhythms. pp. 181–195.
- ^ Marijuana, Sleep and Dreams. psychologytoday.com. Retrieved on 10 February 2012.
- ^ Rosen, Ilene M.; Aurora, R. Nisha; Kirsch, Douglas B.; Carden, Kelly A.; Malhotra, Raman K.; Ramar, Kannan; Abbasi-Feinberg, Fariha; Kristo, David A.; Martin, Jennifer L.; Olson, Eric J.; Rosen, Carol L.; Rowley, James A.; Shelgikar, Anita V. (15 November 2019). "Chronic Opioid Therapy and Sleep: An American Academy of Sleep Medicine Position Statement". Journal of Clinical Sleep Medicine. 15 (11): 1671–1673. doi:10.5664/jcsm.8062. ISSN 1550-9389. PMC 6853382. PMID 31739858.
- ^ Mamelak, M.; Escriu, J. M.; Stokan, O. (April 1977). "The effects of gamma-hydroxybutyrate on sleep". Biological Psychiatry. 12 (2): 273–288. ISSN 0006-3223. PMID 192353.
- ^ Abarca C, Albrecht U, Spanagel R (June 2002). "Cocaine sensitization and reward are under the influence of circadian genes and rhythm". Proceedings of the National Academy of Sciences of the United States of America. 99 (13): 9026–30. Bibcode:2002PNAS...99.9026A. doi:10.1073/pnas.142039099. PMC 124417. PMID 12084940.
- ^ Primary hypersomnia: Diagnostic Features. mindsite.com
- ^ O'Callaghan F, Muurlink O, Reid N (7 December 2018). "Effects of caffeine on sleep quality and daytime functioning". Risk Management and Healthcare Policy. 11: 263–271. doi:10.2147/RMHP.S156404. PMC 6292246. PMID 30573997.
- ^ Shimatsu, Akira (September 2004). "[Ghrelin-related drugs: clinical perspectives]". Nihon Rinsho. Japanese Journal of Clinical Medicine. 62 (Suppl 9): 435–438. ISSN 0047-1852. PMID 15506422.
- ^ Murphy, P. J.; Badia, P.; Myers, B. L.; Boecker, M. R.; Wright, K. P. (June 1994). "Nonsteroidal anti-inflammatory drugs affect normal sleep patterns in humans". Physiology & Behavior. 55 (6): 1063–1066. doi:10.1016/0031-9384(94)90388-3. ISSN 0031-9384. PMID 8047572. S2CID 25887442.
- ^ Copinschi, G.; Leproult, R.; Van Onderbergen, A.; Caufriez, A.; Cole, K. Y.; Schilling, L. M.; Mendel, C. M.; De Lepeleire, I.; Bolognese, J. A.; Van Cauter, E. (October 1997). "Prolonged oral treatment with MK-677, a novel growth hormone secretagogue, improves sleep quality in man". Neuroendocrinology. 66 (4): 278–286. doi:10.1159/000127249. ISSN 0028-3835. PMID 9349662.
- ^ a b c St-Onge MP, Mikic A, Pietrolungo CE (September 2016). "Effects of Diet on Sleep Quality". Advances in Nutrition. 7 (5): 938–49. doi:10.3945/an.116.012336. PMC 5015038. PMID 27633109.
- ^ Peuhkuri K, Sihvola N, Korpela R (May 2012). "Diet promotes sleep duration and quality". Nutrition Research. 32 (5): 309–19. doi:10.1016/j.nutres.2012.03.009. PMID 22652369.
- ^ a b St-Onge M, Mikic A, Cara E, Pietrolungo CE (2016). "Effects of Diet on Sleep Quality". Advances in Nutrition. 7 (5): 938–949. doi:10.3945/an.116.012336. PMC 5015038. PMID 27633109.
- ^ St-Onge M, Cherta-Murillo A, Owen L (2023). "The interrelationship between sleep, diet, and glucose metabolism". Sleep Medicine Reviews. 69: 101788. doi:10.1016/j.smrv.2023.101788. PMC 10247426. PMID 37156196.
- ^ a b c d e f Worthman CM, Melby MK (2002). "6. Toward a comparative developmental ecology of human sleep". In Carskadon MA (ed.). Adolescent Sleep Patterns: Biological, Social, and Psychological Influences. Cambridge University Press. pp. 69–117. doi:10.1017/CBO9780511499999.009. ISBN 978-0521642910.
- ^ Jeon M, Dimitriou D, Halstead EJ (February 2021). "A Systematic Review on Cross-Cultural Comparative Studies of Sleep in Young Populations: The Roles of Cultural Factors". International Journal of Environmental Research and Public Health. 18 (4): 2005. doi:10.3390/ijerph18042005. PMC 7922907. PMID 33669583.
- ^ Samson DR (21 October 2021). "The Human Sleep Paradox: The Unexpected Sleeping Habits of Homo sapiens". Annual Review of Anthropology. 50 (1): 259–274. doi:10.1146/annurev-anthro-010220-075523. ISSN 0084-6570. S2CID 237845665. Retrieved 2 June 2022.
- ^ Jackson M, Banks S (4 April 2018). "Humans Used to Sleep in Two Shifts, And Maybe We Should Do It Again". Science Alert. Retrieved 7 February 2022.
- ^ Ekirch AR (2001). "Sleep we have lost: pre-industrial slumber in the British Isles". The American Historical Review. 106 (2): 343–86. doi:10.2307/2651611. JSTOR 2651611. PMID 18680884.
- ^ a b Hegarty S (22 February 2012). "The myth of the eight-hour sleep". BBC News. Archived from the original on 22 February 2012. Retrieved 22 February 2012.
- ^ Huntington, Ellsworth (1915) Civilization and Climate Archived 17 August 2016 at the Wayback Machine. Yale University Press. p. 126
- ^ Hafiz D, Hafiz I, Hafiz Y (2009). The American Muslim Teenager's Handbook. Simon & Schuster Children's. ISBN 978-1416986997.
- ^ a b c d e f g William SJ (2005). Sleep and Society: Sociological Ventures into the Un(known). New York City and London: Routledge. pp. 95–96. ISBN 978-0-415-35419-6.
- ^ "On Death - On Death Poem by John Keats". Poem Hunter. 29 March 2010.
- ^ Chadwick NK (1935). "Imbas Forosnai". Scottish Gaelic Studies. 4: 97–135.
- ^ MacKillop J (1998). A Dictionary of Celtic Mythology. Oxford: Oxford University Press. ISBN 0-19-280120-1.
- ^ a b c d e f g h i j k l Hansen W (2017). The Book of Greek & Roman Folktales, Legends & Myths. Princeton, New Jersey: Princeton University Press. pp. 132–133. ISBN 978-0691170152.
- ^ a b c d Burstein A (2007). The Original Knickerbocker: The Life of Washington Irving. New York: Basic Books. pp. 120–338. ISBN 978-0-465-00853-7.
Rip Van Winkle.
- ^ Welch D (9 May 1887). The Theater. Vol. 3. New York City, New York: Theatre Publishing Company. p. 139. Retrieved 21 June 2017.
- ^ Thorn J. "Saint Rip". nyfolklore.org. Voices: The Journal of New York Folklore. Archived from the original on 18 October 2017. Retrieved 21 June 2017.
- ^ Bates A (1906). The Drama; Its History, Literature and Influence on Civilization: American Drama. Vol. 20. London, England: Historical Publishing Company. p. 121. Retrieved 21 June 2017.
- ^ a b c d e f Rothschild CK (2014). Paul in Athens: The Popular Religious Context of Acts 17. Tübingen: Mohr Siebeck. pp. 40–42. ISBN 978-3-16-153260-3.
- ^ Jones BJ (2008). Washington Irving: An American Original. New York: Arcade Books. pp. 177–178. ISBN 978-1-55970-836-4.
- ^ Churchland, Patricia Smith (1 January 2005). A neurophilosophical slant on consciousness research. Progress in Brain Research. Vol. 149. Elsevier. pp. 285–293.
- ^ Doerig, Adrien; Schurger, Aaron; Hess, Kathryn; Herzog, Michael H. (1 July 2019). "The unfolding argument: Why IIT and other causal structure theories cannot explain consciousness". Consciousness and Cognition. 72: 49–59. doi:10.1016/j.concog.2019.04.002. ISSN 1053-8100. PMID 31078047. S2CID 147704603.
- ^ Tsytsarev, Vassiliy (February 2022). "Methodological aspects of studying the mechanisms of consciousness". Behavioural Brain Research. 419: 113684. doi:10.1016/j.bbr.2021.113684. PMID 34838578. S2CID 244570791.
- ^ Kerskens, Christian Matthias; López Pérez, David (1 October 2022). "Experimental indications of non-classical brain functions". Journal of Physics Communications. 6 (10): 105001. arXiv:1806.07998. Bibcode:2022JPhCo...6j5001K. doi:10.1088/2399-6528/ac94be. ISSN 2399-6528.
- ^ Frank P (24 June 2016). "Why Have Artists Always Found Sleep Such A Fascinating Subject?". HuffPost. Archived from the original on 25 July 2017. Retrieved 14 July 2017.
Further reading
- Brown RE, Basheer R, McKenna JT, Strecker RE, McCarley RW (July 2012). "Control of sleep and wakefulness". Physiological Reviews. 92 (3): 1087–187. doi:10.1152/physrev.00032.2011. PMC 3621793. PMID 22811426.
External links
- Rethinking Sleep, David K. Randall, New York Times, September 2012
- How to Sleep, James Hamblin, The Atlantic, January 2017