Rectum
| Rectum | |
|---|---|
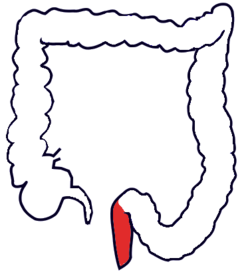 The human colon seen from front. The rectum (red) is near the end of the colon. | |
 Anatomy of the anus and rectum | |
| Details | |
| Precursor | Hindgut |
| Part of | Large intestine |
| System | Gastrointestinal system |
| Artery | Superior rectal artery (first two-thirds of rectum), middle rectal artery (last third of rectum) |
| Vein | Superior rectal veins, middle rectal veins |
| Nerve | Inferior anal nerves, inferior mesenteric ganglia[1] |
| Lymph | Inferior mesenteric lymph nodes, pararectal lymph nodes, internal iliac lymph nodes, Deep inguinal lymph nodes |
| Function | Store feces prior to defecation |
| Identifiers | |
| Latin | rectum intestinum |
| MeSH | D012007 |
| TA98 | A05.7.04.001 |
| TA2 | 2998 |
| FMA | 14544 |
| Anatomical terminology | |
The rectum is the final straight portion of the large intestine in humans and some other mammals, and the gut in others. The adult human rectum is about 12 centimetres (4.7 in) long,[2] and begins at the rectosigmoid junction, the end of the sigmoid colon, at the level of the third sacral vertebra or the sacral promontory depending upon what definition is used.[3] Its caliber is similar to that of the sigmoid colon at its commencement, but it is dilated near its termination, forming the rectal ampulla. It terminates at the level of the anorectal ring (the level of the puborectalis sling) or the dentate line, again depending upon which definition is used.[3] In humans, the rectum is followed by the anal canal which is about 4 centimetres (1.6 in) long, before the gastrointestinal tract terminates at the anal verge. The word rectum comes from the Latin rectum intestinum, meaning straight intestine.
Structure
The rectum is a part of the lower gastrointestinal tract. The rectum is a continuation of the sigmoid colon, and connects to the anus. The rectum follows the shape of the sacrum and ends in an expanded section called the rectal ampulla, where feces are stored before their release via the anal canal.[a][4] The rectum connects with the sigmoid colon at the level of S3, and connects with the anal canal as it passes through the pelvic floor muscles.[4]
Unlike other portions of the colon, the rectum does not have distinct taeniae coli.[5]: 397 The taeniae blend with one another in the sigmoid colon five centimeters above the rectum, giving rise to a layer of longitudinal muscle that surrounds the rectum on all sides for its entire length.[6]
-
Inner diameters of different sections of the large intestine, with rectum near rectal/sigmoid junction measuring on average 5.7 cm (range 4.5-7.5 cm).[7]
Blood supply and drainage
The blood supply of the rectum changes between the top and bottom portions.[8] The top two thirds is supplied by the superior rectal artery. The lower third is supplied by the middle and inferior rectal arteries.[8]
The superior rectal artery is a single artery that is a continuation of the inferior mesenteric artery, when it crosses the pelvic brim.[8] It enters the mesorectum at the level of S3, and then splits into two branches, which run at the lateral back part of the rectum, and then the sides of the rectum. These then end in branches in the submucosa, which join with (anastamose) with branches of the middle and inferior rectal arteries.[8]
-
Arteries of the pelvis
-
Blood vessels of the rectum and anus
Microanatomy
The microanatomy of the wall of the rectum is similar to the rest of the gastrointestinal tract;[9] namely, that it possesses a mucosa with a lining of a single layer of column-shaped cells with mucous-secreting goblet cells interspersed, resting on a lamina propria, with a layer of smooth muscle called muscularis mucosa. This sits on an underlying submucosa of connective tissue, surrounded by a muscularis propria of two bands of muscle, an inner circular band and an outer longitudinal one.[10] There are a higher concentration of goblet cells in the rectal mucosa than other parts of the gastrointestinal tract.[9]
The lining of the rectum changes sharply at the point where the rectum meets the anus. Here, the lining changes from the column-shaped cells of the rectum to multiple layers of flat cells.[9]
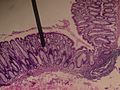
-
Cross-section microscopic shot of the rectal wall
-
Dog Rectum cross-section (40×)
-
Microscopic cross-section of the rectum of a dog (400×), showing a high concentration of goblet cells in amongst the column-shaped lining. Goblet cells can be seen as the circular cells with a clear inner material (cytoplasm).
Function
The rectum acts as a temporary storage site for feces. The rectum receives faecal material from the descending colon, transmitted through regular muscle contractions called peristalsis. [11] As the rectal walls expand due to the materials filling it from within, stretch receptors from the nervous system located in the rectal walls stimulate the desire to pass feces, a process called defecation.[11]
An internal and external anal sphincter, and resting contraction of the puborectalis, prevent leakage of faeces (faecal incontinence). As the rectum becomes more distended, the sphincters relax and a reflex expulsion of the contents of the rectum occurs. Expulsion occurs through contractions of the muscles of the rectum.[11]
The urge to voluntarily defecate occurs after the rectal pressure increases to beyond 18 mmHg; and reflex expulsion at 55 mmHg. In voluntary defecation, in addition to contraction of the rectal muscles and relaxation of the external anal sphincter, abdominal muscle contraction, and relaxation of the puborectalis muscle occurs. This acts to make the angle between the rectum and anus straighter, and facilitate defecation.[11]
Clinical significance


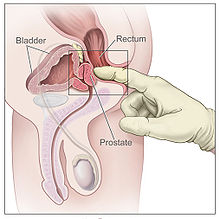
Examination
For the diagnosis of certain ailments, a rectal exam may be done. These include faecal impaction, prostatic cancer and benign prostatic hypertrophy in men, faecal incontinence, and internal haemorrhoids.[12]
Colonoscopy and sigmoidoscopy are forms of endoscopy that use a guided camera to view the rectum. The instruments may have the ability to take biopsies if needed, for diagnosis of diseases such as cancer. A proctoscope is another instrument that is used to visualise the rectum.
Body temperature can also be taken in the rectum. Rectal temperature can be taken by inserting a medical thermometer not more than 25 mm (1 inch) into the rectum via the anus. A mercury thermometer should be inserted for 3 to 5 minutes; a digital thermometer should remain inserted until it beeps. Normal rectal temperature generally ranges from 36 to 38 °C (96.8 to 100.4 °F) and is about 0.5 °C (1 °F) above oral (mouth) temperature and about 1 °C (2 °F) above axilla (armpit) temperature.[citation needed] Availability of less invasive temperature-taking methods including tympanic (ear) and forehead thermometers has facilitated reduced use of this method.
Route of administration
Some medications are also administered via the rectum.[13] By their definitions, suppositories are inserted, and enemas are injected, via the rectum. Both of these may be used for the delivery of drugs or to relieve constipation; enemas are also used for a variety of other purposes, medical and otherwise.
Constipation
One cause of constipation is faecal impaction in the rectum, in which a dry, hard stool forms. Manual evacuation is the use of a gloved finger to evacuate faeces from the rectum, and, after the application of stool softeners, is utilised in acute constipation.[14]: 914 It is also in the long-term management of neurogenic bowel, seen most frequently in people with a spinal cord injury or multiple sclerosis. Digital rectal stimulation, the insertion of one finger into the rectum, may be used to induce peristalsis in patients whose own peristaltic reflex is inadequate to fully empty the rectum.
If the urge is not acted upon, the material in the rectum is often returned to the colon where more water is absorbed from the feces. If defecation is delayed for a prolonged period, constipation and hardened feces results.[citation needed]
Although peristalsis in the colon delivers material to the rectum, laxatives such as bisacodyl or senna that induce peristalsis in the large bowel do not appear to initiate peristalsis in the rectum. They induce a sensation of rectal fullness and contraction that frequently leads to defecation, but without the distinct waves of activity characteristic of peristalsis.[15] The anal longitudinal muscle also participates in defecation by everting the anus.[16]
Diseases
- Proctitis is inflammation of the anus and the rectum.
- Rectal cancer, a subgroup of colorectal cancer specific to the rectum.
- Rectal prolapse, referring to the prolapse of the rectum into the anus or external area. This is commonly caused by a weakened pelvic floor after childbirth.
Other diseases
Other diseases of the rectum include:
- Ulcerative colitis, one form of inflammatory bowel disease that causes ulcers that affect the rectum. This may be episodic, over a person's lifetime. These may cause blood to be visible in the stool. As of 2014[update] the cause is unknown.
- In the context of mesenteric ischemia, the upper rectum is sometimes referred to as Sudak's point and is of clinical importance as a watershed region between the inferior mesenteric artery circulation and the internal iliac artery circulation via the middle rectal artery and thus prone to ischemia. Sudak's point is often referred to along with Griffith's point at the splenic flexure as a watershed region.
Society and culture
Sexual stimulation
Due to the proximity of the anterior wall of the rectum to the vagina in females or to the prostate in males, and the shared nerves thereof, rectal stimulation or penetration can result in sexual arousal.
History
Etymology
English rectum is derived from the full Latin expression intestinum rectum.[17] The English name straight gut[18] truly expresses the literal meaning of this expression, as Latin rectum means straight,[19] and intestinum means gut.[19] This Latin expression is a translation[20][21] of Ancient Greek ἀπευθυσμένον ἔντερον, derived from ἀπευθύνειν, to make straight,[22] and ἔντερον, gut,[22] attested in the writings of Greek physician Galen.[20][21] During his anatomic investigations on animal corpses, Galen observed the rectum to be straight instead of curved as in humans.[20][21] The expressions ἀπευθυσμένον ἔντερον and intestinum rectum are therefore not appropriate descriptions of the rectum in humans. Apeuthysmenon[23] can be considered as Latinization of ἀπευθυσμένον ἔντερον and euthyenteron[24] has a similar meaning (εὐθύς = straight[22]).
See also
Notes
References
- ^ Template:GeorgiaPhysiology
- ^ "12. Colon and Rectum" (PDF), AJCC Cancer Staging Atlas, American Joint Committee on Cancer, 2006, p. 109
- ^ a b Wolff, Bruce G.; et al., eds. (2007). The ASCRS textbook of colon and rectal surgery. New York: Springer. ISBN 978-0-387-24846-2.
- ^ a b Gray's 2016, pp. 1146–7.
- ^ Drake, Richard L.; Vogl, Wayne; Tibbitts, Adam W.M. Mitchell; illustrations by Richard; Richardson, Paul (2005). Gray's anatomy for students. Philadelphia: Elsevier/Churchill Livingstone. ISBN 978-0-8089-2306-0.
- ^ Sneh Agarwal (January–March 2012). "Anatomy of the Pelvic Floor and Anal Sphincters" (PDF). JIMSA. 25 (1).
- ^ Nguyen H, Loustaunau C, Facista A, Ramsey L, Hassounah N, Taylor H, Krouse R, Payne CM, Tsikitis VL, Goldschmid S, Banerjee B, Perini RF, Bernstein C (2010). "Deficient Pms2, ERCC1, Ku86, CcOI in field defects during progression to colon cancer". J Vis Exp (41). doi:10.3791/1931. PMC 3149991. PMID 20689513.
- ^ a b c d Gray's 2016, pp. 1151.
- ^ a b c Wheater's 2013, p. 273.
- ^ Wheater's 2013, pp. 252–4.
- ^ a b c d Ganong's 2019, p. 492-4.
- ^ O'Connor, Nicholas J. Talley, Simon (2009). Clinical examination : a systematic guide to physical diagnosis (6th ed.). Chatswood, N.S.W.: Elsevier Australia. pp. 179–180. ISBN 978-0-7295-3905-0.
{{cite book}}: CS1 maint: multiple names: authors list (link) - ^ Davidson's 2018, p. 17.
- ^ Nicki R. Colledge; Brian R. Walker; Stuart H. Ralston, eds. (2010). Davidson's principles and practice of medicine. illustrated by Robert Britton (21st ed.). Edinburgh: Churchill Livingstone/Elsevier. ISBN 978-0-7020-3084-0.
- ^ J. D. Hardcastle and C. V. Mann (1968). "Study of large bowel peristalsis" (PDF). Gut. 9 (5): 512–520. doi:10.1136/gut.9.5.512. PMC 1552760. PMID 5717099.
- ^ P. J. Lunniss, R. K. S. Phillips (1992). "Anatomy and function of the anal longitudinal muscle". BJS. 79 (9): 882–884. doi:10.1002/bjs.1800790908. PMID 1422746.
- ^ Federative Committee on Anatomical Terminology (FCAT) (1998). Terminologia Anatomica. Stuttgart: Thieme
- ^ Schreger, C.H.Th.(1805). Synonymia anatomica. Synonymik der anatomischen Nomenclatur. Fürth: im Bureau für Literatur.
- ^ a b Lewis, C. T. & Short, C. (1879). A Latin dictionary founded on Andrews' edition of Freund's Latin dictionary. Oxford: Clarendon Press.
- ^ a b c Hyrtl, J. (1880). Onomatologia Anatomica. Geschichte und Kritik der anatomischen Sprache der Gegenwart. Wien: Wilhelm Braumüller. K.K. Hof- und Universitätsbuchhändler.
- ^ a b c Triepel, H. (1910). Die anatomischen Namen. Ihre Ableitung und Aussprache. Mit einem Anhang: Biographische Notizen.(Dritte Auflage). Wiesbaden: Verlag J.F. Bergmann.
- ^ a b c Liddell, H.G. & Scott, R. (1940). A Greek-English Lexicon. revised and augmented throughout by Sir Henry Stuart Jones. with the assistance of. Roderick McKenzie. Oxford: Clarendon Press.
- ^ Kossmann, R. (1895). Die gynäcologische Anatomie und ihre zu Basel festgestellte Nomenclatur. Monatsschrift für Geburtshülfe und Gynaekologie, 2 (6), 447-472.
- ^ Gabler, E. & Winkler, T.C. (1881). Latijnsch-Hollandsch woordenboek over de geneeskunde en natuurkundige wetenschappen. (2nd edition). Leiden: A.W. Sijthoff.
- Books
- Ralston, Stuart H.; Penman, Ian D.; Strachan, Mark W.; Hobson, Richard P. (eds.) (2018). Davidson's principles and practice of medicine (23rd ed.). Elsevier. ISBN 978-0-7020-7028-0.
{{cite book}}:|first4=has generic name (help) - Standring, Susan, ed. (2016). Gray's anatomy : the anatomical basis of clinical practice (41st ed.). Philadelphia. ISBN 9780702052309. OCLC 920806541.
{{cite book}}: CS1 maint: location missing publisher (link) - Young, Barbara; O'Dowd, Geraldine; Woodford, Phillip (2013). Wheater's functional histology: a text and colour atlas (6th ed.). Philadelphia: Elsevier. ISBN 9780702047473.
- Barrett, Kim E. (2019). Ganong's review of medical physiology. Barman, Susan M.,, Brooks, Heddwen L.,, Yuan, Jason X.-J. (26th ed.). New York. ISBN 9781260122404. OCLC 1076268769.
{{cite book}}: CS1 maint: location missing publisher (link) - Eldra P. Solomon, Richard R. Schmidt, and Peter J. Adragna: Human anatomy & physiology, 2nd ed. 1990 (Sunders College Publishing, Philadelphia). ISBN 0-03-011914-6.
External links
- Cross section image: pembody/body15a—Plastination Laboratory at the Medical University of Vienna
- Cross section image: pelvis/pelvis-e12-15—Plastination Laboratory at the Medical University of Vienna
- Anatomy image:7808 at the SUNY Downstate Medical Center
- Anatomy photo:43:11-0101 at the SUNY Downstate Medical Center



![Inner diameters of different sections of the large intestine, with rectum near rectal/sigmoid junction measuring on average 5.7 cm (range 4.5-7.5 cm).[7]](http://upload.wikimedia.org/wikipedia/commons/thumb/2/22/Diameters_of_the_large_intestine.svg/120px-Diameters_of_the_large_intestine.svg.png)