Azithromycin
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Zithromax, others[1] |
| Other names | 9-deoxy-9α-aza-9α-methyl-9α-homoerythromycin A |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a697037 |
| License data |
|
| Pregnancy category |
|
| Routes of administration | By mouth, intravenous, eye drops |
| Drug class | Macrolide antibiotic |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | 38% for 250 mg capsules |
| Metabolism | Liver |
| Elimination half-life | 68 h |
| Excretion | Bile duct[8] |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| NIAID ChemDB | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.126.551 |
| Chemical and physical data | |
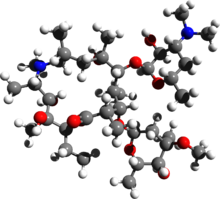
| Formula | C38H72N2O12 |
| Molar mass | 748.996 g·mol−1 |
| 3D model (JSmol) | |
| |
| |
| (verify) | |
Azithromycin, sold under the brand names Zithromax (in oral form) and Azasite (as an eye drop), is an antibiotic medication used for the treatment of several bacterial infections.[10] This includes middle ear infections, strep throat, pneumonia, traveler's diarrhea, and certain other intestinal infections.[10] Along with other medications, it may also be used for malaria.[10] It is administered by mouth, into a vein, or into the eye.[10]
Common side effects include nausea, vomiting, diarrhea and upset stomach.[10] An allergic reaction, such as anaphylaxis, or a type of diarrhea caused by Clostridioides difficile is possible.[10] Azithromycin causes QT prolongation that may cause life-threatening arrhythmias such as torsades de pointes.[11] No harm has been found with its use during pregnancy.[10] Its safety during breastfeeding is not confirmed, but it is likely safe.[12] Azithromycin is an azalide, a type of macrolide antibiotic.[10] It works by decreasing the production of protein, thereby stopping bacterial growth.[10][13]
Azithromycin was discovered in former Yugoslavia (present day Croatia) in 1980 by the pharmaceutical company Pliva and approved for medical use in 1988.[14][15] It is on the World Health Organization's List of Essential Medicines.[16] The World Health Organization lists it as an example under "Macrolides and ketolides" in its Critically Important Antimicrobials for Human Medicine (designed to help manage antimicrobial resistance).[17] It is available as a generic medication[18] and is sold under many brand names worldwide.[1] In 2022, it was the 78th most commonly prescribed medication in the United States, with more than 8 million prescriptions.[19][20]
Medical uses
[edit]Azithromycin is used to treat diverse infections, including:
- Acute bacterial sinusitis due to H. influenzae, M. catarrhalis, or S. pneumoniae. A 1999 study found Azithromycin to be faster in resolving symptoms as compared to amoxicillin / clavulanic.[21]
- Acute otitis media caused by H. influenzae, M. catarrhalis or S. pneumoniae. A 2021 study concluded that Azithromycin was comparable to amoxicillin/clavulanate in its treatment and that it was safer and more tolerable in children.[22]
- Community-acquired pneumonia due to C. pneumoniae, H. influenzae, M. pneumoniae, or S. pneumoniae.[23]
- Genital ulcer disease (chancroid) in men due to H. ducreyi
- Pharyngitis or tonsillitis caused by S. pyogenes as an alternative to first-line therapy in individuals who cannot use first-line therapy[24]
- Prevention and treatment of acute bacterial exacerbations of chronic obstructive pulmonary disease due to H. influenzae, M. catarrhalis, or S. pneumoniae. The benefits of long-term prophylaxis must be weighed on a patient-by-patient basis against the risk of cardiovascular and other adverse effects.[25]
- Trachoma due to C. trachomatis[26]
- Uncomplicated skin infections due to S. aureus, S. pyogenes, or S. agalactiae
- Scrub typhus caused by Orientia tsutsugamushi.[27]
Bacterial susceptibility
[edit]Azithromycin has relatively broad but shallow antibacterial activity. It inhibits some Gram-positive bacteria, some Gram-negative bacteria, and many atypical bacteria.[28][29][30]
Aerobic and facultative Gram-positive microorganisms
- Staphylococcus aureus (Methicillin-sensitive only)
- Streptococcus agalactiae
- Streptococcus pneumoniae
- Streptococcus pyogenes
Aerobic and facultative anaerobic Gram-negative microorganisms
- Bordetella pertussis
- Haemophilus ducreyi
- Haemophilus influenzae
- Legionella pneumophila
- Moraxella catarrhalis
- Neisseria gonorrhoeae
Anaerobic microorganisms
- Peptostreptococcus species
- Prevotella bivia
Other microorganisms
- Chlamydia trachomatis
- Chlamydophila pneumoniae
- Mycoplasma genitalium
- Mycoplasma pneumoniae
- Ureaplasma urealyticum
Pregnancy and breastfeeding
[edit]No harm has been found with use during pregnancy.[10] However, there are no adequate well-controlled studies in pregnant women.[8]
The safety of the medication during breastfeeding is unclear. It was reported that because only low levels are found in breast milk and the medication has also been used in young children, it is unlikely that breastfed infants would have adverse effects.[12]
Airway diseases
[edit]Azithromycin has beneficial effects in the treatment of asthma. It possesses antibacterial, antiviral, and anti-inflammatory properties which contribute to its effectiveness. Asthma exacerbations can be caused by chronic neutrophilic inflammation, and azithromycin is known to reduce this type of inflammation due to its immunomodulatory properties. The recommended dosage for controlling asthma exacerbations with azithromycin is either 500 mg or 250 mg taken orally as tablets three times a week. In adults with severe asthma, low-dose azithromycin may be prescribed as an add-on treatment when standard therapies such as inhaled corticosteroids or long-acting beta2-agonists are not sufficient. Long-term use of azithromycin in patients with persistent symptomatic asthma aims to decrease the frequency of asthma exacerbations and improve their quality of life. While both its anti-inflammatory and antibacterial effects play crucial roles in treating asthma, studies suggest that responsiveness to azithromycin therapy depends on individual variations in lung bacterial burden and microbial composition, collectively referred to as the lung microbiome. The richness (diversity) of the lung microbiome has been identified as a key factor in determining the effectiveness of azithromycin treatment. Azithromycin has significant interactions with the patient's microbiome. Long-term use of azithromycin reduces the presence of H. influenzae bacteria in the airways but also increases resistance against macrolide antibiotics. The specific pharmacological mechanisms through which azithromycin interacts with the patient's microbiome remain unknown as of 2024;[update] research continues to explore how changes in microbial composition influence drug efficacy and patient outcomes.[31]
Azithromycin appears to be effective in the treatment of chronic obstructive pulmonary disease through its suppression of inflammatory processes.[32] Azithromycin is potentially useful in sinusitis via this mechanism.[33] Azithromycin is believed to produce its effects through suppressing certain immune responses that may contribute to inflammation of the airways.[34][35]
Adverse effects
[edit]Most common adverse effects are diarrhea (5%), nausea (3%), abdominal pain (3%), and vomiting. Fewer than 1% of people stop taking the drug due to side effects. Nervousness, skin reactions, and anaphylaxis have been reported.[36] Clostridioides difficile infection has been reported with use of azithromycin.[10] Azithromycin does not affect the efficacy of birth control unlike some other antibiotics such as rifampin. Hearing loss has been reported.[37]
Occasionally, people have developed cholestatic hepatitis or delirium. Accidental intravenous overdose in an infant caused severe heart block, resulting in residual encephalopathy.[38][39]
In 2013, the US Food and Drug Administration (FDA) issued a warning that azithromycin "can cause abnormal changes in the electrical activity of the heart that may lead to a potentially fatal irregular heart rhythm." The FDA noted in the warning a 2012 study that found the drug may increase the risk of death, especially in those with heart problems, compared with those on other antibiotics such as amoxicillin or no antibiotic. The warning indicated people with preexisting conditions are at particular risk, such as those with abnormalities in the QT interval, low blood levels of potassium or magnesium, a slower than normal heart rate, or those who use certain drugs to treat abnormal heart rhythms.[40][41][42] The warning mentioned that azithromycin causes QT prolongation that may cause life-threatening arrhythmias such as torsades de pointes.[11]
Interactions
[edit]Colchicine
[edit]Azithromycin, should not be taken with colchicine as it may lead to colchicine toxicity. Symptoms of colchicine toxicity include gastrointestinal upset, fever, myalgia, pancytopenia, and organ failure.[43][44]
Drugs metabolized by CYP3A4
[edit]CYP3A4 is an enzyme that metabolizes many drugs in the liver. Some drugs can inhibit CYP3A4, which means they reduce its activity and increase the blood levels of the drugs that depend on it for elimination. This can lead to adverse effects or drug-drug interactions.[45]
Azithromycin is a member of macrolides that are a class of antibiotics with a cyclic structure with a lactone ring and sugar moieties. Macrolides can inhibit CYP3A4 by a mechanism called mechanism-based inhibition (MBI), which involves the formation of reactive metabolites that bind covalently and irreversibly to the enzyme, rendering it inactive. Mechanism-based inhibition is more serious and long-lasting than reversible inhibition, as it requires the synthesis of new enzyme molecules to restore the activity.[46]
The degree of mechanism-based inhibition by macrolides depends on the size and structure of their lactone ring. Clarithromycin and erythromycin have a 14-membered lactone ring, which is more prone to demethylation by CYP3A4 and subsequent formation of nitrosoalkenes, the reactive metabolites that cause mechanism-based inhibition. Azithromycin, on the other hand, has a 15-membered lactone ring, which is less susceptible to demethylation and nitrosoalkene formation. Therefore, azithromycin is a weak inhibitor of CYP3A4, while clarithromycin and erythromycin are strong inhibitors which increase the area under the curve (AUC) value of co-administered drugs more than five-fold.[46] AUC it is a measure of the drug exposure in the body over time. By inhibiting CYP3A4, macrolide antibitiotics, such as erythromycin and clarithromycin, but not azithromycin, can significantly increase the AUC of the drugs that depend on it for clearance, which can lead to higher risk of adverse effects or drug-drug interactions. Azithromycin stands apart from other macrolide antibiotics because it is a weak inhibitor of CYP3A4, and does not significantly increase AUC value of co-administered drugs.[47]
The difference in CYP3A4 inhibition by macrolides has clinical implications, for example for people who take statins, which are cholesterol-lowering drugs that are mainly metabolized by CYP3A4. Co-administration of clarithromycin or erythromycin with statins can increase the risk of statin-induced myopathy, a condition that causes muscle pain and damage. Azithromycin, however, does not significantly affect the pharmacokinetics of statins and is considered a safer alternative than other macrolide antibiotics.[46]
Pharmacology
[edit]Mechanism of action
[edit]Azithromycin prevents bacteria from growing by interfering with their protein synthesis. It binds to the 50S subunit of the bacterial ribosome, thus inhibiting translation of mRNA. Nucleic acid synthesis is not affected.[8]
Pharmacokinetics
[edit]Azithromycin is an acid-stable antibiotic, so it can be taken orally with no need of protection from gastric acids. It is readily absorbed, but absorption is greater on an empty stomach. Time to peak concentration (Tmax) in adults is 2.1 to 3.2 hours for oral dosage forms. Due to its high concentration in phagocytes, azithromycin is actively transported to the site of infection. During active phagocytosis, large concentrations are released. The concentration of azithromycin in the tissues can be over 50 times higher than in plasma due to ion trapping and its high lipid solubility.[48][49] Azithromycin's half-life allows a large single dose to be administered and yet maintain bacteriostatic levels in the infected tissue for several days.[8]
Following a single dose of 500 mg, the apparent terminal elimination half-life of azithromycin is 68 hours.[8] Biliary excretion of azithromycin, predominantly unchanged, is a major route of elimination.[50] Over the course of a week, about 6% of the administered dose appears as an unchanged drug in urine.[8]
History
[edit]A team of researchers at the pharmaceutical company Pliva in Zagreb, former Yugoslavia (present day Croatia) discovered azithromycin in 1980.[51] The company Pliva patented it in 1981.[15] In 1986, Pliva and Pfizer signed a licensing agreement, which gave Pfizer exclusive rights for the sale of azithromycin in Western Europe and the United States. Pliva put its azithromycin on the market in Central and Eastern Europe. Pfizer launched azithromycin under Pliva's license in other markets under the brand name Zithromax in 1991.[52] Patent protection ended in 2005.[53]
Society and culture
[edit]
Available forms
[edit]Azithromycin is available as a generic medication. Azithromycin is administered in film-coated tablet, capsule, oral suspension, intravenous injection, granules for suspension in sachet, and ophthalmic solution.[1]
Usage
[edit]In 2010, azithromycin was the most prescribed antibiotic for outpatients in the US,[54] whereas in Sweden, where outpatient antibiotic use is a third as prevalent, macrolides are only on 3% of prescriptions.[55] In 2017, and 2022, azithromycin was the second most prescribed antibiotic for outpatients in the United States.[56][57] In 2022, it was the 78th most commonly prescribed medication in the United States, with more than 8 million prescriptions.[19][20]
Brand names
[edit]Brand name listings
|
|---|
|
It is sold under many brand names worldwide including 3-Micina, A Sai Qi, Abacten, Abbott, Acex, Acithroc, Actazith, Agitro, Ai Mi Qi, Amixef, Amizin, Amovin, An Mei Qin, Ao Li Ping, Apotex, Lebanon, Aratro, Aruzilina, Arzomicin, Arzomidol, Asizith, Asomin, Astidal, Astro, Athofix, Athxin, Atizor, Atromizin, Avalon, AZ, AZA, Azacid, Azadose, Azalid, Azalide, AzaSite, Azaroth, Azath, Azatril, Azatril, Azax, Azee, Azeecor, Azeeta, Azelide, Azeltin, Azenil, Azeptin, Azerkym, Azi, Aziact, Azibact, Azibactron, Azibay, Azibect, Azibest, Azibiot, Azibiotic, Azicare, Azicin, Azicine, Aziclass, Azicom, Azicure, Azid, Azidose, Azidraw, Azifam, Azifarm, Azifast, Azifine, Aziflax, Azigen, Azigram, Azigreat, Azikare, Azilide, Azilife, Azilip, Azilup, Azimac, Azimax, Azimed, Azimepha, Azimex, Azimit, Azimix, Azimon, Azimore, Azimycin, Azimycine, Azin, Azindamon, Azinew, Azinex, Azinif, Azinil, Azintra, Aziom, Azipar, Aziped, Aziphar, Azipin, Aziplex, Azipro, Aziprome, Aziquilab, Azirace, Aziram, Aziresp, Aziride, Azirol, Azirom, Azirox, Azirute, Azirutec, Aziset, Azisis, Azison, Azissel, Aziswift, Azit, Azita, Azitam, Azitex, Azith, Azithral, Azithrin, Azithro, Azithrobeta, Azithrocin, Azithrocine, Azithromax, Azithromed, Azithromicina, Azithromycin, Azithromycine, Azithromycinum, Azithrovid, Azitic, Azitive, Azitome, Azitrac, Azitral, Azitrax, Azitredil, Azitrex, Azitrim, Azitrin, Azitrix, Azitro, Azitrobac, Azitrocin, Azitroerre, Azitrogal, Azitrolabsa, Azitrolid, Azitrolit, Azitrom, Azitromac, Azitromax, Azitromek, Azitromicin, Azitromicina, Azitromycin, Azitromycine, Azitrona, Azitropharma, Azitroteg, Azitrox, Azitsa, Azitus, Azivar, Azivirus, Aziwill, Aziwok, Azix, Azizox, Azmycin, Azo, Azobat, Azocin, Azoget, Azoheim, Azoksin, Azom, Azomac, Azomax, Azomex, Azomycin, Azomyne, Azores, Azorox, Azostar, Azot, Azoxin, Azras, Azro, Azrocin, Azrolid, Azromax, Azroplax, Azrosin, Aztin, Aztrin, Aztro, Aztrogecin, Azvig, Azycin, Azycyna, Azydrop, Azypin, Azytact, Azytan, Azyter, Azyter, Azyth, Azywell, Azza, Ba Qi, Bactaway, Bactizith, Bactrazol, Bai Ke De Rui, Batif, Bazyt, Bezanin, Bin Qi, Binozyt, BinQi, Biocine, Biozit, Bo Kang, Canbiox, Cetaxim, Charyn, Chen Yu, Cinalid, Cinetrin, Clamelle, Clearsing, Corzi, Cozith, Cronopen, Curazith, Delzosin, Demquin, Dentazit, Disithrom, Doromax, Doyle, Elzithro, Eniz, Epica, Ethrimax, Ezith, Fabodrox, Fabramicina, Feng Da Qi, Figothrom, Floctil, Flumax, Fu Qi-Hua Yuan, Fu Rui Xin, Fuqixing, Fuxin-Hai Xin Pharm, Geozif, Geozit, Gitro, Goldamycin, Gramac, Gramokil, Hemomicin, Hemomycin, I-Thro, Ilozin, Imexa, Inedol, Infectomycin, Iramicina, Itha, Jin Nuo, Jin Pai Qi, Jinbo, Jun Jie, Jun Wei Qing, Kai Qi, Kang Li Jian, Kang Qi, Katrozax, Ke Lin Da, Ke Yan Li, Koptin, Kuai Yu, L-Thro, Laz, Legar, Lg-Thral, Li Ke Si, Li Li Xing, Li Qi, Li Quan Yu, Lin Bi, Lipuqi, Lipuxin, Lizhu Qile, Loromycin, Lu Jia Kang, Luo Bei Er, Luo Qi, Maazi, Macroazi, Macromax, Macrozit, Maczith, Makromicin, Maxmor, Mazit, Mazitrom, Medimacrol, Meithromax, Mezatrin, Ming Qi Xin, Misultina, Mycinplus, Na Qi, Nadymax, Naxocina, Neblic, Nemezid, Neofarmiz, Nifostin, Nobaxin, Nokar, Novatrex, Novozithron, Novozitron, Nurox, Odaz, Odazyth, Onzet, Oranex, Oranex, Ordipha, Orobiotic, Pai Fen, Pai Fu, Paiqi, Pediazith, Pi Nis, Portex, Pu He, Pu Le Qi, Pu Yang, Qi Gu Mei, Qi Mai Xing, Qi Nuo, Qi Tai, Qi Xian, Qili, Qiyue, Rarpezit, Razimax, Razithro, Rezan, Ribotrex, Ribozith, Ricilina, Rizcin, Romax, Romycin, Rothin (Rakaposhi), Rozalid, Rozith, Ru Shuang Qi, Rui Qi, Rui Qi Lin, Rulide, Sai Jin Sha, Sai Le Xin, Sai Qi, Santroma, Selimax, Sheng Nuo Ling, Shu Luo Kang, Simpli-3, Sisocin, Sitrox, Sohomac, Stromac, Su Shuang, Sumamed, Sumamox, Tailite, Talcilina, Tanezox, Te Li Xin, Tetris, Texis, Thoraxx, Throin, Thromaxin, Tong Tai Qi Li, Topt, Toraseptol, Tremac, Trex, Tri Azit, Triamid, Tridosil, Trimelin, Tritab, Tromiatlas, Tromix, Trozamil, Trozin, Trozocina, Trulimax, Tuoqi, Udox, Ultreon, Ultreon, Vectocilina, Vinzam, Visag, Vizicin, Wei Li Qinga, Wei Lu De, Wei Zong, Weihong, Xerexomair, Xi Le Xin, Xi Mei, Xin Da Kang, Xin Pu Rui, Xithrone, Ya Rui, Yan Sha, Yanic, Yi Nuo Da, Yi Song, Yi Xina, Yin Pei Kang, Yong Qi, You Ni Ke, Yu Qi, Z-3, Z-PAK, Zady, Zaiqi, Zaret, Zarom, Zathrin, Zedbac, Zeelide, Zeemide, Zenith, Zentavion, Zetamac, Zetamax, Zeto, Zetron, Zevlen, Zibramax, Zicho, Zigilex, Zikrax, Zikti, Zimacrol, Zimax, Zimicina, Zimicine, Zindel, Zinfect, Zirom, Zisrocin, Zistic, Zit-Od, Zitab, Zitax, Zithrax, Zithrin, Zithro-Due, Zithrobest, Zithrodose, Zithrogen, Zithrokan, Zithrolide, Zithromax, Zithrome, Zithromed, Zithroplus, Zithrotel, Zithrox, Zithroxyn, Zithtec, Zitinn, Zitmac, Zitraval, Zitrax, Zitrex, Zitric, Zitrim, Zitrobid, Zitrobiotic, Zithrolect, Zitrocin, Zitrogram, Zitrolab, Zitromax, Zitroneo, Zitrotek, Ziyoazi, Zmax, Zocin, Zomax, Zotax, Zycin, and Zythrocin.[1] It is sold as a combination drug with cefixime as Anex-AZ, Azifine-C, Aziter-C, Brutacef-AZ, Cezee, Fixicom-AZ, Emtax-AZ, Olcefone-AZ, Starfix-AZ, Zeph-AZ, Zicin-CX, and Zifi-AZ.[1] It is also sold as a combination drug with nimesulide as Zitroflam; in a combination with tinidazole and fluconazole as Trivafluc, and in a combination with ambroxol as Zathrin-AX, Laz-AX and Azro-AM.[1] |
Research
[edit]Azithromycin is researched for its supposed anti-inflammatory and immunomodulatory properties, which are believed to be exhibited through its suppression of proinflammatory cytokines and enhancing the production of anti-inflammatory cytokines, which is important in dampening inflammation. Cytokines are small proteins that are secreted by immune cells and play a key role in the immune response. Studies suggest that azithromycin can decrease the release of pro-inflammatory cytokines such as TNF-alpha, IL-1β, IL-6, and IL-8 while increasing the levels of anti-inflammatory cytokine IL-10. By decreasing the number of pro-inflammatory cytokines, azithromycin probably controls potential tissue damage during inflammation. These effects are believed to be due to azithromycin's ability to suppress a transcription factor called nuclear factor-kappa B (NF-κB) resulting in blockade of inflammatory response pathways downstream from NF-κB activation leading to decreased chemokine receptor CXCR4 signaling causing reduced inflammation.[58][59][60][61][62] Despite the efficiency of treating rosacea with azithromycin, the exact mechanism of why azithromycin is effective in treating rosacea are not completely understood.[63] It is unclear whether its antibacterial or immunomodulatory properties or a combination of both mechanisms contribute to its efficacy. Azithromycin may prevent mast cell degranulation and thus can suppress inflammation of dorsal root ganglia through various signaling pathways such as decreased numbers of CD4+ T cells which are particularly relevant since they mediate the response of hair follicle antigens.[64] Inflammation in rosacea is thought to be associated with increased production of reactive oxygen species (ROS) by inflammatory cells. The ability of azithromycin to decrease ROS production can help reduce oxidative stress and inflammation, but this remains speculation.[63]
The therapeutic role of azithromycin has been explored in various diseases such as cystic fibrosis exacerbation, burn injury-induced lung injury, asthma, chronic obstructive pulmonary disease, and severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in COVID-19 infection.[65][66][67][68][69] Despite early evidence showing azithromycin slowed down coronavirus multiplication in laboratory settings, further research indicates it to be ineffective as a treatment for COVID-19 in humans.[70] Azithromycin in conjunction with of chloroquine or hydroxychloroquine has been associated with deleterious outcomes in COVID-19 patients, including drug-induced QT prolongation.[71] After a large-scale trial showed no benefit of using azithromycin in treating COVID-19, the UK's National Institute for Health and Care Excellence (NICE) updated its guidance and no longer recommends the medication for COVID-19.[72][73]
Azithromycin has been studied in the treatment of chronic fatigue syndrome (CFS) and has been reported to improve or even resolve symptoms in some cases.[74][75][76][77][78] However, these studies have been described as being of very low quality.[76] In any case, the beneficial effects might be by eradication of chronic bacterial infections that are possibly contributing to or causing CFS or by the immunomodulatory effects of azithromycin.[74][75][76][77][78]
Azithromycin therapy in cystic fibrosis patients yields a modest respiratory function improvement, reduces exacerbation risk, and extends time to exacerbation up to six months; still, long-term efficacy data is a subject of ongoing research. Potential benefits of azithromycin therapy is azithromycin's good safety profile, minimal treatment burden, and cost-effectiveness, but the drawbacks are gastrointestinal side effects with weekly dosing, which are ameliorated by a split dose regimen.[79][80] The potential role of azithromycin in inhibiting the autophagic destruction of non-tuberculous mycobacteria (NTM) within macrophages has garnered significant attention. This mechanism may contribute to the observed correlation between long-term macrolide monotherapy and an increased risk of NTM infection and the emergence of macrolide-resistant strains. Azithromycin's interference with autophagy could potentially predispose patients with cystic fibrosis to mycobacterial infections. Despite repeated refutations of a direct association between azithromycin use and NTM infection, there remains a high level of concern regarding the potential for the development of NTM strains resistant to macrolides.[81]
Azithromycin has been shown to be an effective preventive measure against many postpartum infections in mothers following planned vaginal births; still, its impact on neonatal outcomes remains inconclusive and is the subject of ongoing research.[82][83]
References
[edit]- ^ a b c d e f "Azithromycin International Brands". Drugs.com. Archived from the original on 28 February 2017. Retrieved 27 February 2017.
- ^ "Azithromycin Use During Pregnancy". Drugs.com. 2 May 2019. Archived from the original on 18 June 2020. Retrieved 24 December 2019.
- ^ "FDA-sourced list of all drugs with black box warnings (Use Download Full Results and View Query links.)". nctr-crs.fda.gov. FDA. Retrieved 22 October 2023.
- ^ "Zithromax azithromycin 500mg (as dihydrate) tablet blister pack (58797)". Therapeutic Goods Administration (TGA). 12 August 2022. Retrieved 26 April 2024.
- ^ "Zithromax Product information". Health Canada. 16 January 2013. Retrieved 26 April 2024.
- ^ "Drug and medical device highlights 2018: Helping you maintain and improve your health". Health Canada. 14 October 2020. Retrieved 17 April 2024.
- ^ "Zithromax Summary of Product Characteristics (SmPC)". (emc). 5 February 2024. Retrieved 26 April 2024.
- ^ a b c d e f g "Zithromax- azithromycin dihydrate tablet, film coated; Zithromax- azithromycin dihydrate powder, for suspension". DailyMed. 29 September 2023. Retrieved 26 April 2024.
- ^ "List of nationally authorised medicinal products Active substance: azithromycin (systemic use formulations)" (PDF). European Medicine Agency. 14 January 2021. Archived (PDF) from the original on 18 August 2021. Retrieved 10 March 2023.
- ^ a b c d e f g h i j k "Azithromycin". The American Society of Health-System Pharmacists. Archived from the original on 5 September 2015. Retrieved 1 August 2015.
- ^ a b Dunker A, Kolanczyk DM, Maendel CM, Patel AR, Pettit NN (November 2016). "Impact of the FDA Warning for Azithromycin and Risk for QT Prolongation on Utilization at an Academic Medical Center". Hosp Pharm. 51 (10): 830–833. doi:10.1310/hpj5110-830. PMC 5135431. PMID 27928188.
- ^ a b "Azithromycin use while Breastfeeding". Archived from the original on 5 September 2015. Retrieved 4 September 2015.
- ^ "Azithromycin Stops The Growth of Bacteria" (in German). Archived from the original on 12 May 2020. Retrieved 24 December 2017.
- ^ Greenwood D (2008). Antimicrobial drugs : chronicle of a twentieth century medical triumph (1st ed.). Oxford: Oxford University Press. p. 239. ISBN 978-0-19-953484-5. Archived from the original on 5 March 2016.
- ^ a b Alapi EM, Fischer J (2006). "Table of Selected Analogue Classes". In Fischer J, Ganellin CR (eds.). Analogue-based Drug Discovery. Weinheim: Wiley-Vch Verlag GmbH & Co. KGaA. p. 498. ISBN 978-3-527-31257-3. Archived from the original on 14 January 2023. Retrieved 2 April 2020.
- ^ World Health Organization (2023). The selection and use of essential medicines 2023: web annex A: World Health Organization model list of essential medicines: 23rd list (2023). Geneva: World Health Organization. hdl:10665/371090. WHO/MHP/HPS/EML/2023.02.
- ^ World Health Organization (2018). Critically important antimicrobials for human medicine (6th revision ed.). Geneva: World Health Organization. hdl:10665/312266. ISBN 978-92-4-151552-8. License: CC BY-NC-SA 3.0 IGO.
- ^ Hamilton R (2015). Tarascon Pocket Pharmacopoeia 2015 Deluxe Lab-Coat Edition. Jones & Bartlett Learning. ISBN 978-1-284-05756-0.
- ^ a b "The Top 300 of 2022". ClinCalc. Archived from the original on 30 August 2024. Retrieved 30 August 2024.
- ^ a b "Azithromycin Drug Usage Statistics, United States, 2013 - 2022". ClinCalc. Retrieved 30 August 2024.
- ^ Klapan I, Culig J, Oresković K, Matrapazovski M, Radosević S (1999). "Azithromycin versus amoxicillin/clavulanate in the treatment of acute sinusitis". American Journal of Otolaryngology. 20 (1): 7–11. doi:10.1016/S0196-0709(99)90044-3. PMID 9950107. Retrieved 31 May 2024.
In adults with acute sinusitis, a 3-day course of azithromycin was as effective and well tolerated as a 10-day course of amoxicillin/clavulanic acid. A significantly simpler dosage regimen and faster clinical effect were the advantages of azithromycin.
- ^ Dawit G, Mequanent S, Makonnen E (2021). "Efficacy and safety of azithromycin and amoxicillin/clavulanate for otitis media in children: a systematic review and meta-analysis of randomized controlled trials". Annals of Clinical Microbiology and Antimicrobials. 20 (1): 28. doi:10.1186/s12941-021-00434-x. PMC 8070272. PMID 33894769.
Azithromycin is comparable to amoxicillin/clavulanate to treat otitis media in children, and it is safer and more tolerable.
- ^ Mandell LA, Wunderink RG, Anzueto A, Bartlett JG, Campbell GD, Dean NC, et al. (March 2007). "Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community-acquired pneumonia in adults". Clinical Infectious Diseases. 44 (Suppl 2): S27-72. doi:10.1086/511159. PMC 7107997. PMID 17278083.
- ^ Randel A (September 2013). "IDSA Updates Guideline for Managing Group A Streptococcal Pharyngitis". American Family Physician. 88 (5): 338–40. PMID 24010402.
- ^ Taylor SP, Sellers E, Taylor BT (December 2015). "Azithromycin for the Prevention of COPD Exacerbations: The Good, Bad, and Ugly". The American Journal of Medicine. 128 (12): 1362.e1–6. doi:10.1016/j.amjmed.2015.07.032. PMID 26291905.
- ^ Burton M, Habtamu E, Ho D, Gower EW (November 2015). "Interventions for trachoma trichiasis". The Cochrane Database of Systematic Reviews. 11 (11): CD004008. doi:10.1002/14651858.CD004008.pub3. PMC 4661324. PMID 26568232.
- ^ Gupta N, Boodman C, Jouego CG, Van Den Broucke S (December 2023). "Doxycycline vs azithromycin in patients with scrub typhus: a systematic review of literature and meta-analysis". BMC Infect Dis. 23 (1): 884. doi:10.1186/s12879-023-08893-7. PMC 10726538. PMID 38110855.
- ^ Sybilski AJ (2020). "Azithromycin – more than an antibiotic". Pediatria I Medycyna Rodzinna. 16 (3): 261–267. doi:10.15557/PiMR.2020.0048.
- ^ Opitz DL, Harthan JS (2012). "Review of Azithromycin Ophthalmic 1% Solution (AzaSite) for the Treatment of Ocular Infections". Ophthalmol Eye Dis. 4: 1–14. doi:10.4137/OED.S7791. PMC 3619494. PMID 23650453.
- ^ Amano A, Kishi N, Koyama H, Matsuzaki K, Matsumoto S, Uchino K, et al. (September 2016). "In vitro activity of sitafloxacin against atypical bacteria (2009-2014) and comparison between susceptibility of clinical isolates in 2009 and 2012". Jpn J Antibiot. 69 (3): 131–142. PMID 30226949.
- ^ Chan M, Ghadieh C, Irfan I, Khair E, Padilla N, Rebeiro S, et al. (February 2024). "Exploring the influence of the microbiome on the pharmacology of anti-asthmatic drugs". Naunyn-Schmiedeberg's Arch Pharmacol. 397 (2): 751–762. doi:10.1007/s00210-023-02681-5. PMC 10791706. PMID 37650889.
- ^ Simoens S, Laekeman G, Decramer M (May 2013). "Preventing COPD exacerbations with macrolides: a review and budget impact analysis". Respiratory Medicine. 107 (5): 637–48. doi:10.1016/j.rmed.2012.12.019. PMID 23352223.
- ^ Gotfried MH (February 2004). "Macrolides for the treatment of chronic sinusitis, asthma, and COPD". Chest. 125 (2 Suppl): 52S–60S, quiz 60S-61S. doi:10.1378/chest.125.2_suppl.52S. PMID 14872001. Archived from the original on 27 August 2021. Retrieved 22 March 2020.
- ^ Zarogoulidis P, Papanas N, Kioumis I, Chatzaki E, Maltezos E, Zarogoulidis K (May 2012). "Macrolides: from in vitro anti-inflammatory and immunomodulatory properties to clinical practice in respiratory diseases". European Journal of Clinical Pharmacology. 68 (5): 479–503. doi:10.1007/s00228-011-1161-x. PMID 22105373. S2CID 1904304.
- ^ Steel HC, Theron AJ, Cockeran R, Anderson R, Feldman C (2012). "Pathogen- and host-directed anti-inflammatory activities of macrolide antibiotics". Mediators of Inflammation. 2012: 584262. doi:10.1155/2012/584262. PMC 3388425. PMID 22778497.
- ^ Mori F, Pecorari L, Pantano S, Rossi ME, Pucci N, De Martino M, et al. (2014). "Azithromycin anaphylaxis in children". International Journal of Immunopathology and Pharmacology. 27 (1): 121–6. doi:10.1177/039463201402700116. PMID 24674687. S2CID 45729751.
- ^ Dart RC (2004). Medical Toxology. Lippincott Williams & Wilkins. p. 23.
- ^ Tilelli JA, Smith KM, Pettignano R (January 2006). "Life-threatening bradyarrhythmia after massive azithromycin overdose". Pharmacotherapy. 26 (1): 147–50. doi:10.1592/phco.2006.26.1.147. PMID 16506357. S2CID 43222966.
- ^ Baselt R (2008). Disposition of Toxic Drugs and Chemicals in Man (8th ed.). Foster City, CA: Biomedical Publications. pp. 132–133.
- ^ Grady D (16 May 2012). "Popular Antibiotic May Raise Risk of Sudden Death". The New York Times. Archived from the original on 17 May 2012. Retrieved 18 May 2012.
- ^ Ray WA, Murray KT, Hall K, Arbogast PG, Stein CM (May 2012). "Azithromycin and the risk of cardiovascular death". The New England Journal of Medicine. 366 (20): 1881–90. doi:10.1056/NEJMoa1003833. PMC 3374857. PMID 22591294.
- ^ "FDA Drug Safety Communication: Azithromycin (Zithromax or Zmax) and the risk of potentially fatal heart rhythms". U.S. Food and Drug Administration (FDA). 12 March 2013. Archived from the original on 27 October 2016.
- ^ John R. Horn, Philip D. Hansten (2006). "Life Threatening Colchicine Drug Interactions. Drug Interactions: Insights and Observations" (PDF). Archived (PDF) from the original on 23 November 2023. Retrieved 16 January 2024.
- ^ Tan MS, Gomez-Lumbreras A, Villa-Zapata L, Malone DC (December 2022). "Colchicine and macrolides: a cohort study of the risk of adverse outcomes associated with concomitant exposure". Rheumatol Int. 42 (12): 2253–2259. doi:10.1007/s00296-022-05201-5. PMC 9473467. PMID 36104598.
- ^ Zhang L, Xu X, Badawy S, Ihsan A, Liu Z, Xie C, et al. (2020). "A Review: Effects of Macrolides on CYP450 Enzymes". Curr Drug Metab. 21 (12): 928–937. doi:10.2174/1389200221666200817113920. PMID 32807049. S2CID 221162650. Archived from the original on 2 February 2024. Retrieved 2 February 2024.
- ^ a b c Hougaard Christensen MM, Bruun Haastrup M, Øhlenschlaeger T, Esbech P, Arnspang Pedersen S, Bach Dunvald AC, et al. (April 2020). "Interaction potential between clarithromycin and individual statins-A systematic review" (PDF). Basic Clin Pharmacol Toxicol. 126 (4): 307–317. doi:10.1111/bcpt.13343. PMID 31628882. Archived (PDF) from the original on 2 February 2024. Retrieved 2 February 2024.
- ^ Westphal JF (October 2000). "Macrolide - induced clinically relevant drug interactions with cytochrome P-450A (CYP) 3A4: an update focused on clarithromycin, azithromycin and dirithromycin". Br J Clin Pharmacol. 50 (4): 285–95. doi:10.1046/j.1365-2125.2000.00261.x. PMC 2015000. PMID 11012550.
- ^ Sharma K, Mullangi R (2013). "A concise review of HPLC, LC-MS and LC-MS/MS methods for determination of azithromycin in various biological matrices". Biomedical Chromatography. 27 (10): 1243–1258. doi:10.1002/bmc.2898. PMID 23553351. Archived from the original on 8 March 2024. Retrieved 16 February 2024.
- ^ Derendorf H (June 2020). "Excessive lysosomal ion-trapping of hydroxychloroquine and azithromycin". Int J Antimicrob Agents. 55 (6): 106007. doi:10.1016/j.ijantimicag.2020.106007. PMC 7204663. PMID 32389720.
- ^ Bekele LK, Gebeyehu GG (2012). "Application of Different Analytical Techniques and Microbiological Assays for the Analysis of Macrolide Antibiotics from Pharmaceutical Dosage Forms and Biological Matrices". ISRN Analytical Chemistry. 2012: 1–17. doi:10.5402/2012/859473.
- ^ Banić Tomišić Z (December 2011). "The Story of Azithromycin". Kemija U Industriji: Časopis Kemičara I Kemijskih Inženjera Hrvatske. 60 (12): 603–17. Archived from the original on 8 March 2024. Retrieved 25 June 2020.
- ^ Banić Tomišić Z (2011). "The Story of Azithromycin". Kemija U Industriji. 60 (12): 603–617. ISSN 0022-9830. Archived from the original on 8 September 2017. Retrieved 15 April 2013.
- ^ "Azithromycin: A world best-selling Antibiotic". www.wipo.int. World Intellectual Property Organization. Archived from the original on 6 December 2020. Retrieved 18 June 2019.
- ^ Hicks LA, Taylor TH, Hunkler RJ (April 2013). "U.S. outpatient antibiotic prescribing, 2010". The New England Journal of Medicine. 368 (15): 1461–2. doi:10.1056/NEJMc1212055. PMID 23574140.
- ^ Hicks LA, Taylor TH, Hunkler RJ (September 2013). "More on U.S. outpatient antibiotic prescribing, 2010". The New England Journal of Medicine. 369 (12): 1175–6. doi:10.1056/NEJMc1306863. PMID 24047077.
- ^ "Outpatient Antibiotic Prescriptions — United States, 2017" (PDF). U.S. Centers for Disease Control and Prevention (CDC). 26 March 2020. Archived from the original on 30 March 2020. Retrieved 30 March 2020.
- ^ "Outpatient Antibiotic Prescriptions — United States, 2022". U.S. Centers for Disease Control and Prevention (CDC). 15 November 2023. Archived from the original on 8 March 2024. Retrieved 17 November 2023.
- ^ Lim DJ, Thompson HM, Walz CR, Ayinala S, Skinner D, Zhang S, et al. (February 2021). "Azithromycin and ciprofloxacin inhibit interleukin-8 secretion without disrupting human sinonasal epithelial integrity in vitro". Int Forum Allergy Rhinol. 11 (2): 136–143. doi:10.1002/alr.22656. PMC 7854841. PMID 32725797.
- ^ Yadav S, Dalai P, Gowda S, Nivsarkar M, Agrawal-Rajput R (October 2023). "Azithromycin alters Colony Stimulating Factor-1R (CSF-1R) expression and functional output of murine bone marrow-derived macrophages: A novel report". Int Immunopharmacol. 123: 110688. doi:10.1016/j.intimp.2023.110688. PMID 37499396. S2CID 260186900.
- ^ Wang Z, Chu C, Ding Y, Li Y, Lu C (September 2023). "Clinical significance of serum microRNA-146a and inflammatory factors in children with Mycoplasma pneumoniae pneumonia after azithromycin treatment". J Pediatr (Rio J). 100 (1): 108–115. doi:10.1016/j.jped.2023.06.004. PMC 10751685. PMID 37778397. S2CID 263253426.
- ^ Terpstra LC, Altenburg J, Doodeman HJ, Piñeros YSS, Lutter R, Heijerman HGM, et al. (April 2023). "The effect of azithromycin on sputum inflammatory markers in bronchiectasis". BMC Pulm Med. 23 (1): 151. doi:10.1186/s12890-023-02444-1. PMC 10148509. PMID 37118704.
- ^ Wu S, Tian X, Mao Q, Peng C (January 2023). "Azithromycin attenuates wheezing after pulmonary inflammation through inhibiting histone H3K27me3 hypermethylation mediated by EZH2". Clin Epigenetics. 15 (1): 12. doi:10.1186/s13148-023-01430-y. PMC 9872437. PMID 36691058.
- ^ a b Bakar O, Demirçay Z, Yuksel M, Haklar G, Sanisoglu Y (March 2007). "The effect of azithromycin on reactive oxygen species in rosacea". Clin Exp Dermatol. 32 (2): 197–200. doi:10.1111/j.1365-2230.2006.02322.x. PMID 17244346. S2CID 30016695.
- ^ Ersoy B, Aktan B, Kilic K, Sakat MS, Sipal S (July 2018). "The anti-inflammatory effects of erythromycin, clarithromycin, azithromycin and roxithromycin on histamine-induced otitis media with effusion in guinea pigs". J Laryngol Otol. 132 (7): 579–583. doi:10.1017/S0022215118000610. PMID 29888693. S2CID 47010752.
- ^ Durán-Álvarez JC, Prado B, Zanella R, Rodríguez M, Díaz S (November 2023). "Wastewater surveillance of pharmaceuticals during the COVID-19 pandemic in Mexico City and the Mezquital Valley: A comprehensive environmental risk assessment". Sci Total Environ. 900: 165886. Bibcode:2023ScTEn.90065886D. doi:10.1016/j.scitotenv.2023.165886. PMID 37524191. S2CID 260323001.
- ^ Southern KW, Barker PM (November 2004). "Azithromycin for cystic fibrosis". Eur Respir J. 24 (5): 834–8. doi:10.1183/09031936.04.00084304. PMID 15516680. S2CID 17778741.
- ^ "Azithromycin and cystic fibrosis". Arch Dis Child. 107 (8): 739. August 2022. doi:10.1136/archdischild-2022-324569. PMID 35853636. S2CID 250624603.
- ^ Ghimire JJ, Jat KR, Sankar J, Lodha R, Iyer VK, Gautam H, et al. (June 2022). "Azithromycin for Poorly Controlled Asthma in Children: A Randomized Controlled Trial". Chest. 161 (6): 1456–1464. doi:10.1016/j.chest.2022.02.025. PMID 35202621. S2CID 247074537.
- ^ Gibson PG, Yang IA, Upham JW, Reynolds PN, Hodge S, James AL, et al. (August 2017). "Effect of azithromycin on asthma exacerbations and quality of life in adults with persistent uncontrolled asthma (AMAZES): a randomised, double-blind, placebo-controlled trial". Lancet. 390 (10095): 659–668. doi:10.1016/S0140-6736(17)31281-3. PMID 28687413. S2CID 4523731.
- ^ Popp M, Stegemann M, Riemer M, Metzendorf M, Romero CS, Mikolajewska A, et al. (22 October 2021). "Intervention Antibiotics for the treatment of COVID-19". Cochrane Database of Systematic Reviews. 10 (10): CD015025. doi:10.1002/14651858.CD015025. PMC 8536098. PMID 34679203.
- ^ Nag K, Tripura K, Datta A, Karmakar N, Singh M, Singh M, et al. (2024). "Effect of Hydroxychloroquine and Azithromycin Combination Use in COVID-19 Patients - An Umbrella Review". Indian J Community Med. 49 (1): 22–27. doi:10.4103/ijcm.ijcm_983_22. PMC 10900474. PMID 38425958.
- ^ Butler CC, Yu LM, Dorward J, Gbinigie O, Hayward G, Saville BR, et al. (September 2021). "Doxycycline for community treatment of suspected COVID-19 in people at high risk of adverse outcomes in the UK (PRINCIPLE): a randomised, controlled, open-label, adaptive platform trial". The Lancet. Respiratory Medicine. 9 (9): 1010–1020. doi:10.1016/S2213-2600(21)00310-6. PMC 8315758. PMID 34329624.
- ^ "Platform trial rules out treatments for COVID-19". National Institute for Health and Care Research (NIHR). 31 May 2022. doi:10.3310/nihrevidence_50873. Archived from the original on 1 June 2022. Retrieved 1 June 2022.
- ^ a b Klimas NG, Koneru AO (December 2007). "Chronic fatigue syndrome: inflammation, immune function, and neuroendocrine interactions". Curr Rheumatol Rep. 9 (6): 482–487. doi:10.1007/s11926-007-0078-y. PMID 18177602.
- ^ a b Kavyani B, Lidbury BA, Schloeffel R, Fisher PR, Missailidis D, Annesley SJ, et al. (July 2022). "Could the kynurenine pathway be the key missing piece of Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) complex puzzle?". Cell Mol Life Sci. 79 (8): 412. doi:10.1007/s00018-022-04380-5. PMC 9276562. PMID 35821534.
- ^ a b c Van Houdenhove B, Pae CU, Luyten P (February 2010). "Chronic fatigue syndrome: is there a role for non-antidepressant pharmacotherapy?". Expert Opin Pharmacother. 11 (2): 215–223. doi:10.1517/14656560903487744. PMID 20088743.
- ^ a b Vermeulen RC, Scholte HR (August 2006). "Azithromycin in chronic fatigue syndrome (CFS), an analysis of clinical data". J Transl Med. 4: 34. doi:10.1186/1479-5876-4-34. PMC 1562448. PMID 16911783.
- ^ a b Chia JK, Chia LY (August 1999). "Chronic Chlamydia pneumoniae infection: a treatable cause of chronic fatigue syndrome". Clin Infect Dis. 29 (2): 452–453. doi:10.1086/520239. PMID 10476765.
- ^ Southern KW, Solis-Moya A, Kurz D, Smith S (February 2024). "Macrolide antibiotics (including azithromycin) for cystic fibrosis". Cochrane Database Syst Rev. 2024 (2): CD002203. doi:10.1002/14651858.CD002203.pub5. PMC 10897949. PMID 38411248.
- ^ Ong JJ, Aguirre I, Unemo M, Kong FY, Fairley CK, Hocking JS, et al. (June 2022). "Comparison of gastrointestinal side effects from different doses of azithromycin for the treatment of gonorrhoea". J Antimicrob Chemother. 77 (7): 2011–2016. doi:10.1093/jac/dkac118. PMC 9244214. PMID 35411400.
- ^ Gramegna A, Misuraca S, Lombardi A, Premuda C, Barone I, Ori M, et al. (December 2023). "Treatable traits and challenges in the clinical management of non-tuberculous mycobacteria lung disease in people with cystic fibrosis". Respir Res. 24 (1): 316. doi:10.1186/s12931-023-02612-1. PMC 10725605. PMID 38104098.
- ^ Crosara LF, Orsini PV, Eskandar K, Khalil SM, Castilhos GS, Strahl PA, et al. (April 2024). "Single-dose oral azithromycin prophylaxis in planned vaginal delivery for sepsis prevention: A systematic review and meta-analysis of randomized controlled trials". Int J Gynaecol Obstet. 165 (1): 107–116. doi:10.1002/ijgo.15124. PMID 37724021.
- ^ Ye H, Hu J, Li B, Yu X, Zheng X (March 2024). "Can the use of azithromycin during labour reduce the incidence of infection among puerperae and newborns? A systematic review and meta-analysis of randomized controlled trials". BMC Pregnancy Childbirth. 24 (1): 200. doi:10.1186/s12884-024-06390-6. PMC 10938810. PMID 38486177.
See also
[edit]- Zrinka Tamburašev, Croatian biochemist on the team that discovered azithromycin
