Cell culture

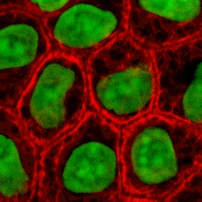
Cell culture is the process by which cells are grown under controlled conditions, generally outside of their natural environment. Cell culture conditions can vary for each cell type, but artificial environments consist of a suitable vessel with substrate or medium that supplies the essential nutrients (amino acids, carbohydrates, vitamins, minerals), growth factors, hormones, and gases (CO2, O2), and regulates the physio-chemical environment (pH buffer, osmotic pressure, temperature). Most cells require a surface or an artificial substrate (adherent or monolayer culture) whereas others can be grown free floating in culture medium (suspension culture).
In practice, the term "cell culture" now refers to the culturing of cells derived from multicellular eukaryotes, especially animal cells, in contrast with other types of culture that also grow cells, such as plant tissue culture, fungal culture, and microbiological culture (of microbes). The historical development and methods of cell culture are closely interrelated to those of tissue culture and organ culture. Viral culture is also related, with cells as hosts for the viruses.
The laboratory technique of maintaining live cell lines (a population of cells descended from a single cell and containing the same genetic makeup) separated from their original tissue source became more robust in the middle 20th century.[1][2]
History
The 19th-century English physiologist Sydney Ringer developed salt solutions containing the chlorides of sodium, potassium, calcium and magnesium suitable for maintaining the beating of an isolated animal heart outside of the body.[3] In 1885, Wilhelm Roux removed a portion of the medullary plate of an embryonic chicken and maintained it in a warm saline solution for several days, establishing the principle of tissue culture.[4] Ross Granville Harrison, working at Johns Hopkins Medical School and then at Yale University, published results of his experiments from 1907 to 1910, establishing the methodology of tissue culture.[5]
Cell culture techniques were advanced significantly in the 1940s and 1950s to support research in virology. Growing viruses in cell cultures allowed preparation of purified viruses for the manufacture of vaccines. The injectable polio vaccine developed by Jonas Salk was one of the first products mass-produced using cell culture techniques. This vaccine was made possible by the cell culture research of John Franklin Enders, Thomas Huckle Weller, and Frederick Chapman Robbins, who were awarded a Nobel Prize for their discovery of a method of growing the virus in monkey kidney cell cultures.
Concepts in mammalian cell culture
Isolation of cells
Cells can be isolated from tissues for ex vivo culture in several ways. Cells can be easily purified from blood; however, only the white cells are capable of growth in culture. Mononuclear cells can be released from soft tissues by enzymatic digestion with enzymes such as collagenase, trypsin, or pronase, which break down the extracellular matrix. Alternatively, pieces of tissue can be placed in growth media, and the cells that grow out are available for culture. This method is known as explant culture.
Cells that are cultured directly from a subject are known as primary cells. With the exception of some derived from tumors, most primary cell cultures have limited lifespan.
An established or immortalized cell line has acquired the ability to proliferate indefinitely either through random mutation or deliberate modification, such as artificial expression of the telomerase gene. Numerous cell lines are well established as representative of particular cell types.
Maintaining cells in culture
For the majority of isolated primary cells, they undergo the process of senescence and stop dividing after a certain number of population doublings while generally retaining their viability (described as the Hayflick limit).
Cells are grown and maintained at an appropriate temperature and gas mixture (typically, 37 °C, 5% CO2 for mammalian cells) in a cell incubator. Culture conditions vary widely for each cell type, and variation of conditions for a particular cell type can result in different phenotypes.

Aside from temperature and gas mixture, the most commonly varied factor in culture systems is the cell growth medium. Recipes for growth media can vary in pH, glucose concentration, growth factors, and the presence of other nutrients. The growth factors used to supplement media are often derived from the serum of animal blood, such as fetal bovine serum (FBS), bovine calf serum, equine serum, and porcine serum. One complication of these blood-derived ingredients is the potential for contamination of the culture with viruses or prions, particularly in medical biotechnology applications. Current practice is to minimize or eliminate the use of these ingredients wherever possible and use human platelet lysate (hPL). This eliminates the worry of cross-species contamination when using FBS with human cells. hPL has emerged as a safe and reliable alternative as a direct replacement for FBS or other animal serum. In addition, chemically defined media can be used to eliminate any serum trace (human or animal), but this cannot always be accomplished with different cell types. Alternative strategies involve sourcing the animal blood from countries with minimum BSE/TSE risk, such as The United States, Australia and New Zealand,[6] and using purified nutrient concentrates derived from serum in place of whole animal serum for cell culture.[7]
Plating density (number of cells per volume of culture medium) plays a critical role for some cell types. For example, a lower plating density makes granulosa cells exhibit estrogen production, while a higher plating density makes them appear as progesterone-producing theca lutein cells.[8]
Cells can be grown either in suspension or adherent cultures. Some cells naturally live in suspension, without being attached to a surface, such as cells that exist in the bloodstream. There are also cell lines that have been modified to be able to survive in suspension cultures so they can be grown to a higher density than adherent conditions would allow. Adherent cells require a surface, such as tissue culture plastic or microcarrier, which may be coated with extracellular matrix (such as collagen and laminin) components to increase adhesion properties and provide other signals needed for growth and differentiation. Most cells derived from solid tissues are adherent. Another type of adherent culture is organotypic culture, which involves growing cells in a three-dimensional (3-D) environment as opposed to two-dimensional culture dishes. This 3D culture system is biochemically and physiologically more similar to in vivo tissue, but is technically challenging to maintain because of many factors (e.g. diffusion).
Components of cell culture media
| Component | Function |
|---|---|
| Carbon source (glucose/glutamine) | Source of energy |
| Amino acid | Building blocks of protein |
| Vitamins | Promote cell survival and growth |
| Balanced salt solution | It is an isotonic mixture of ions to act as cofactors for enzymatic reactions, cell adhesion etc. |
| Phenol red dye | pH indicator. The color of phenol red changes from orange/red at pH 7-7.4 to yellow at acidic(lower) pH and purple at basic (higher) pH. |
| Bicarbonate /HEPES buffer | It is used to maintain a balanced pH in the media |
Growth conditions
| Parameter | |
|---|---|
| Temperature | 37°C |
| CO2 | 5% |
| Humidity | 95% |
Cell line cross-contamination
Cell line cross-contamination can be a problem for scientists working with cultured cells.[9] Studies suggest anywhere from 15–20% of the time, cells used in experiments have been misidentified or contaminated with another cell line.[10][11][12] Problems with cell line cross-contamination have even been detected in lines from the NCI-60 panel, which are used routinely for drug-screening studies.[13][14] Major cell line repositories, including the American Type Culture Collection (ATCC), the European Collection of Cell Cultures (ECACC) and the German Collection of Microorganisms and Cell Cultures (DSMZ), have received cell line submissions from researchers that were misidentified by them.[13][15] Such contamination poses a problem for the quality of research produced using cell culture lines, and the major repositories are now authenticating all cell line submissions.[16] ATCC uses short tandem repeat (STR) DNA fingerprinting to authenticate its cell lines.[17]
To address this problem of cell line cross-contamination, researchers are encouraged to authenticate their cell lines at an early passage to establish the identity of the cell line. Authentication should be repeated before freezing cell line stocks, every two months during active culturing and before any publication of research data generated using the cell lines. Many methods are used to identify cell lines, including isoenzyme analysis, human lymphocyte antigen (HLA) typing, chromosomal analysis, karyotyping, morphology and STR analysis.[17]
One significant cell-line cross contaminant is the immortal HeLa cell line.
Other technical issues
As cells generally continue to divide in culture, they generally grow to fill the available area or volume. This can generate several issues:
- Nutrient depletion in the growth media
- Changes in pH of the growth media
- Accumulation of apoptotic/necrotic (dead) cells
- Cell-to-cell contact can stimulate cell cycle arrest, causing cells to stop dividing, known as contact inhibition.
- Cell-to-cell contact can stimulate cellular differentiation.
- Genetic and epigenetic alterations, with a natural selection of the altered cells potentially leading to overgrowth of abnormal, culture-adapted cells with decreased differentiation and increased proliferative capacity.[18]
Manipulation of cultured cells
Among the common manipulations carried out on culture cells are media changes, passaging cells, and transfecting cells. These are generally performed using tissue culture methods that rely on aseptic technique. Aseptic technique aims to avoid contamination with bacteria, yeast, or other cell lines. Manipulations are typically carried out in a biosafety hood or laminar flow cabinet to exclude contaminating micro-organisms. Antibiotics (e.g. penicillin and streptomycin) and antifungals (e.g.amphotericin B) can also be added to the growth media.
As cells undergo metabolic processes, acid is produced and the pH decreases. Often, a pH indicator is added to the medium to measure nutrient depletion.
Media changes
In the case of adherent cultures, the media can be removed directly by aspiration, and then is replaced. Media changes in non-adherent cultures involve centrifuging the culture and resuspending the cells in fresh media.
Passaging cells
Passaging (also known as subculture or splitting cells) involves transferring a small number of cells into a new vessel. Cells can be cultured for a longer time if they are split regularly, as it avoids the senescence associated with prolonged high cell density. Suspension cultures are easily passaged with a small amount of culture containing a few cells diluted in a larger volume of fresh media. For adherent cultures, cells first need to be detached; this is commonly done with a mixture of trypsin-EDTA; however, other enzyme mixes are now available for this purpose. A small number of detached cells can then be used to seed a new culture. Some cell cultures, such as RAW cells are mechanically scraped from the surface of their vessel with rubber scrapers.
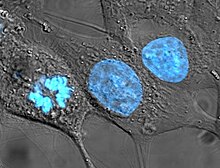
Transfection and transduction
Another common method for manipulating cells involves the introduction of foreign DNA by transfection. This is often performed to cause cells to express a gene of interest. More recently, the transfection of RNAi constructs have been realized as a convenient mechanism for suppressing the expression of a particular gene/protein. DNA can also be inserted into cells using viruses, in methods referred to as transduction, infection or transformation. Viruses, as parasitic agents, are well suited to introducing DNA into cells, as this is a part of their normal course of reproduction.
Established human cell lines
Cell lines that originate with humans have been somewhat controversial in bioethics, as they may outlive their parent organism and later be used in the discovery of lucrative medical treatments. In the pioneering decision in this area, the Supreme Court of California held in Moore v. Regents of the University of California that human patients have no property rights in cell lines derived from organs removed with their consent.[19]
It is possible to fuse normal cells with an immortalised cell line. This method is used to produce monoclonal antibodies. In brief, lymphocytes isolated from the spleen (or possibly blood) of an immunised animal are combined with an immortal myeloma cell line (B cell lineage) to produce a hybridoma which has the antibody specificity of the primary lymphocyte and the immortality of the myeloma. Selective growth medium (HA or HAT) is used to select against unfused myeloma cells; primary lymphoctyes die quickly in culture and only the fused cells survive. These are screened for production of the required antibody, generally in pools to start with and then after single cloning.
Cell strains
A cell strain is derived either from a primary culture or a cell line by the selection or cloning of cells having specific properties or characteristics which must be defined. Cell strains are cells that have been adapted to culture but, unlike cell lines, have a finite division potential. Non-immortalized cells stop dividing after 40 to 60 population doublings[20] and, after this, they lose their ability to proliferate (a genetically determined event known as senescence).[21]
Applications of cell culture
Mass culture of animal cell lines is fundamental to the manufacture of viral vaccines and other products of biotechnology. Culture of human stem cells is used to expand the number of cells and differentiate the cells into various somatic cell types for transplantation.[22] Stem cell culture is also used to harvest the molecules and exosomes that the stem cells release for the purposes of therapeutic development.[23]
Biological products produced by recombinant DNA (rDNA) technology in animal cell cultures include enzymes, synthetic hormones, immunobiologicals (monoclonal antibodies, interleukins, lymphokines), and anticancer agents. Although many simpler proteins can be produced using rDNA in bacterial cultures, more complex proteins that are glycosylated (carbohydrate-modified) currently must be made in animal cells. An important example of such a complex protein is the hormone erythropoietin. The cost of growing mammalian cell cultures is high, so research is underway to produce such complex proteins in insect cells or in higher plants, use of single embryonic cell and somatic embryos as a source for direct gene transfer via particle bombardment, transit gene expression and confocal microscopy observation is one of its applications. It also offers to confirm single cell origin of somatic embryos and the asymmetry of the first cell division, which starts the process.
Cell culture is also a key technique for cellular agriculture, which aims to provide both new products and new ways of producing existing agricultural products like milk, (cultured) meat, fragrances, and rhino horn from cells and microorganisms. It is therefore considered one means of achieving animal-free agriculture.
Cell culture in two dimensions
Research in tissue engineering, stem cells and molecular biology primarily involves cultures of cells on flat plastic dishes. This technique is known as two-dimensional (2D) cell culture, and was first developed by Wilhelm Roux who, in 1885, removed a portion of the medullary plate of an embryonic chicken and maintained it in warm saline for several days on a flat glass plate. From the advance of polymer technology arose today's standard plastic dish for 2D cell culture, commonly known as the Petri dish. Julius Richard Petri, a German bacteriologist, is generally credited with this invention while working as an assistant to Robert Koch. Various researchers today also utilize culturing laboratory flasks, conicals, and even disposable bags like those used in single-use bioreactors.
Aside from Petri dishes, scientists have long been growing cells within biologically derived matrices such as collagen or fibrin, and more recently, on synthetic hydrogels such as polyacrylamide or PEG. They do this in order to elicit phenotypes that are not expressed on conventionally rigid substrates. There is growing interest in controlling matrix stiffness,[24] a concept that has led to discoveries in fields such as:
- Stem cell self-renewal[25][26]
- Lineage specification[27]
- Cancer cell phenotype[28][29][30]
- Fibrosis[31][32]
- Hepatocyte function[33][34][35]
- Mechanosensing[36][37][38]
Cell culture in three dimensions
Cell culture in three dimensions has been touted as "Biology's New Dimension".[39] At present, the practice of cell culture remains based on varying combinations of single or multiple cell structures in 2D.[40] Currently, there is an increase in use of 3D cell cultures in research areas including drug discovery, cancer biology, regenerative medicine and basic life science research.[41] There are a variety of platforms used to facilitate the growth of three-dimensional cellular structures including scaffold systems such as hydrogel matrices[42] and solid scaffolds, and scaffold-free systems such as low-adhesion plates, nanoparticle facilitated magnetic levitation,[43] and hanging drop plates.[44]
3D cell culture in hydrogels
As the natural extracellular matrix (ECM) is important in the survival, proliferation, differentiation and migration of cells, different hydrogel culture matrices mimicking natural ECM structure are seen as potential approaches to in vivo –like cell culturing.[45] Hydrogels are composed of interconnected pores with high water retention, which enables efficient transport of substances such as nutrients and gases. Several different types of hydrogels from natural and synthetic materials are available for 3D cell culture, including animal ECM extract hydrogels, protein hydrogels, peptide hydrogels, polymer hydrogels, and wood-based nanocellulose hydrogel.
3D Cell Culturing by Magnetic Levitation
The 3D Cell Culturing by Magnetic Levitation method (MLM) is the application of growing 3D tissue by inducing cells treated with magnetic nanoparticle assemblies in spatially varying magnetic fields using neodymium magnetic drivers and promoting cell to cell interactions by levitating the cells up to the air/liquid interface of a standard petri dish. The magnetic nanoparticle assemblies consist of magnetic iron oxide nanoparticles, gold nanoparticles, and the polymer polylysine. 3D cell culturing is scalable, with the capability for culturing 500 cells to millions of cells or from single dish to high-throughput low volume systems.
Tissue culture and engineering
Cell culture is a fundamental component of tissue culture and tissue engineering, as it establishes the basics of growing and maintaining cells in vitro. The major application of human cell culture is in stem cell industry, where mesenchymal stem cells can be cultured and cryopreserved for future use. Tissue engineering potentially offers dramatic improvements in low cost medical care for hundreds of thousands of patients annually.
Vaccines
Vaccines for polio, measles, mumps, rubella, and chickenpox are currently made in cell cultures. Due to the H5N1 pandemic threat, research into using cell culture for influenza vaccines is being funded by the United States government. Novel ideas in the field include recombinant DNA-based vaccines, such as one made using human adenovirus (a common cold virus) as a vector,[46][47] and novel adjuvants.[48]
Culture of non-mammalian cells
Plant cell culture methods
Plant cell cultures are typically grown as cell suspension cultures in a liquid medium or as callus cultures on a solid medium. The culturing of undifferentiated plant cells and calli requires the proper balance of the plant growth hormones auxin and cytokinin.
Insect cell culture
Cells derived from Drosophila melanogaster (most prominently, Schneider 2 cells) can be used for experiments which may be hard to do on live flies or larvae, such as biochemical studies or studies using siRNA. Cell lines derived from the army worm Spodoptera frugiperda, including Sf9 and Sf21, and from the cabbage looper Trichoplusia ni, High Five cells, are commonly used for expression of recombinant proteins using baculovirus.
Bacterial and yeast culture methods
For bacteria and yeasts, small quantities of cells are usually grown on a solid support that contains nutrients embedded in it, usually a gel such as agar, while large-scale cultures are grown with the cells suspended in a nutrient broth.
Viral culture methods
The culture of viruses requires the culture of cells of mammalian, plant, fungal or bacterial origin as hosts for the growth and replication of the virus. Whole wild type viruses, recombinant viruses or viral products may be generated in cell types other than their natural hosts under the right conditions. Depending on the species of the virus, infection and viral replication may result in host cell lysis and formation of a viral plaque.
Common cell lines
- Human cell lines
- DU145 (prostate cancer)
- H295R (adrenocortical cancer)
- HeLa (cervical cancer)
- KBM-7 (chronic myelogenous leukemia)
- LNCaP (prostate cancer)
- MCF-7 (breast cancer)
- MDA-MB-468 (breast cancer)
- PC3 (prostate cancer)
- SaOS-2 (bone cancer)
- SH-SY5Y (neuroblastoma, cloned from a myeloma)
- T47D (breast cancer)
- THP-1 (acute myeloid leukemia)
- U87 (glioblastoma)
- National Cancer Institute's 60 cancer cell line panel (NCI60)
- Primate cell lines
- Vero (African green monkey Chlorocebus kidney epithelial cell line)
- Mouse cell lines
- Rat tumor cell lines
- GH3 (pituitary tumor)
- PC12 (pheochromocytoma)
- Plant cell lines
- Tobacco BY-2 cells (kept as cell suspension culture, they are model system of plant cell)
- Other species cell lines
- Dog MDCK kidney epithelial
- Xenopus A6 kidney epithelial
- Zebrafish AB9
List of cell lines
| Cell line | Meaning | Organism | Origin tissue | Morphology | Links |
|---|---|---|---|---|---|
| 3T3-L1 | "3-day transfer, inoculum 3 x 10^5 cells" | Mouse | Embryo | Fibroblast | ECACC Cellosaurus |
| 4T1 | Mouse | Mammary gland | ATCC Cellosaurus | ||
| 9L | Rat | Brain | Glioblastoma | ECACC Cellosaurus | |
| A172 | Human | Brain | Glioblastoma | ECACC Cellosaurus | |
| A20 | Mouse | B lymphoma | B lymphocyte | Cellosaurus | |
| A253 | Human | Submandibular duct | Head and neck carcinoma | ATCC Cellosaurus | |
| A2780 | Human | Ovary | Ovarian carcinoma | ECACC Cellosaurus | |
| A2780ADR | Human | Ovary | Adriamycin-resistant derivative of A2780 | ECACC Cellosaurus | |
| A2780cis | Human | Ovary | Cisplatin-resistant derivative of A2780 | ECACC Cellosaurus | |
| A431 | Human | Skin epithelium | Squamous cell carcinoma | ECACC Cellosaurus | |
| A549 | Human | Lung | Lung carcinoma | ECACC Cellosaurus | |
| AB9 | Zebrafish | Fin | Fibroblast | ATCC Cellosaurus | |
| AHL-1 | Armenian Hamster Lung-1 | Hamster | Lung | ECACC Cellosaurus | |
| ALC | Mouse | Bone marrow | Stroma | PMID 2435412[49] Cellosaurus | |
| B16 | Mouse | Melanoma | ECACC Cellosaurus | ||
| B35 | Rat | Neuroblastoma | ATCC Cellosaurus | ||
| BCP-1 | Human | PBMC | HIV+ primary effusion lymphoma | ATCC Cellosaurus | |
| BEAS-2B | Bronchial epithelium + Adenovirus 12-SV40 virus hybrid (Ad12SV40) | Human | Lung | Epithelial | ECACC Cellosaurus |
| bEnd.3 | Brain Endothelial 3 | Mouse | Brain/cerebral cortex | Endothelium | Cellosaurus |
| BHK-21 | Baby Hamster Kidney-21 | Hamster | Kidney | Fibroblast | ECACC Cellosaurus |
| BOSC23 | Packaging cell line derived from HEK 293 | Human | Kidney (embryonic) | Epithelium | Cellosaurus |
| BT-20 | Breast Tumor-20 | Human | Breast epithelium | Breast carcinoma | ATCC Cellosaurus |
| BxPC3 | Biopsy xenograft of Pancreatic Carcinoma line 3 | Human | Pancreatic adenocarcinoma | Epithelial | ECACC Cellosaurus |
| C2C12 | Mouse | Myoblast | ECACC Cellosaurus | ||
| C3H-10T1/2 | Mouse | Embryonic mesenchymal cell line | ECACC Cellosaurus | ||
| C6 | Rat | Brain astrocyte | Glioma | ECACC Cellosaurus | |
| C6/36 | Insect - Asian tiger mosquito | Larval tissue | ECACC Cellosaurus | ||
| Caco-2 | Human | Colon | Colorectal carcinoma | ECACC Cellosaurus | |
| Cal-27 | Human | Tongue | Squamous cell carcinoma | ATCC Cellosaurus | |
| CGR8 | Mouse | Embryonic stem cells | ECACC Cellosaurus | ||
| CHO | Chinese Hamster Ovary | Hamster | Ovary | Epithelium | ECACC Cellosaurus |
| CML T1 | Chronic myeloid leukemia T lymphocyte 1 | Human | CML acute phase | T cell leukemia | DSMZ Cellosaurus |
| CMT12 | Canine Mammary Tumor 12 | Dog | Mammary gland | Epithelium | Cellosaurus |
| COR-L23 | Human | Lung | Lung carcinoma | ECACC Cellosaurus | |
| COR-L23/5010 | Human | Lung | Lung carcinoma | ECACC Cellosaurus | |
| COR-L23/CPR | Human | Lung | Lung carcinoma | ECACC Cellosaurus | |
| COR-L23/R23- | Human | Lung | Lung carcinoma | ECACC Cellosaurus | |
| COS-7 | Cercopithecus aethiops, origin-defective SV-40 | Old World monkey - Cercopithecus aethiops (Chlorocebus) | Kidney | Fibroblast | ECACC Cellosaurus |
| COV-434 | Human | Ovary | Ovarian granulosa cell carcinoma | PMID 8436435[50] ECACC Cellosaurus | |
| CT26 | Mouse | Colon | Colorectal carcinoma | Cellosaurus | |
| D17 | Dog | Lung metastasis | Osteosarcoma | ATCC Cellosaurus | |
| DH82 | Dog | Histiocytosis | Monocyte/macrophage | ECACC Cellosaurus | |
| DU145 | Human | Androgen insensitive prostate carcinoma | ATCC Cellosaurus | ||
| DuCaP | Dura mater cancer of the Prostate | Human | Metastatic prostate carcinoma | Epithelial | PMID 11317521[51] Cellosaurus |
| E14Tg2a | Mouse | Embryonic stem cells | ECACC Cellosaurus | ||
| EL4 | Mouse | T cell leukemia | ECACC Cellosaurus | ||
| EM-2 | Human | CML blast crisis | Ph+ CML line | DSMZ Cellosaurus | |
| EM-3 | Human | CML blast crisis | Ph+ CML line | DSMZ Cellosaurus | |
| EMT6/AR1 | Mouse | Mammary gland | Epithelial-like | ECACC Cellosaurus | |
| EMT6/AR10.0 | Mouse | Mammary gland | Epithelial-like | ECACC Cellosaurus | |
| FM3 | Human | Lymph node metastasis | Melanoma | ECACC Cellosaurus | |
| GL261 | Glioma 261 | Mouse | Brain | Glioma | Cellosaurus |
| H1299 | Human | Lung | Lung carcinoma | ATCC Cellosaurus | |
| HaCaT | Human | Skin | Keratinocyte | CLS Cellosaurus | |
| HCA2 | Human | Colon | Adenocarcinoma | ECACC Cellosaurus | |
| HEK 293 | Human Embryonic Kidney 293 | Human | Kidney (embryonic) | Epithelium | ECACC Cellosaurus |
| HEK 293T | HEK 293 derivative | Human | Kidney (embryonic) | Epithelium | ECACC Cellosaurus |
| HeLa | "Henrietta Lacks" | Human | Cervix epithelium | Cervical carcinoma | ECACC Cellosaurus |
| Hepa1c1c7 | Clone 7 of clone 1 hepatoma line 1 | Mouse | Hepatoma | Epithelial | ECACC Cellosaurus |
| Hep G2 | Human | Liver | Hepatoblastoma | ECACC Cellosaurus | |
| High Five | Insect (moth) - Trichoplusia ni | Ovary | Cellosaurus | ||
| HL-60 | Human Leukemia-60 | Human | Blood | Myeloblast | ECACC Cellosaurus |
| HT-1080 | Human | Fibrosarcoma | ECACC Cellosaurus | ||
| HT-29 | Human | Colon epithelium | Adenocarcinoma | ECACC Cellosaurus | |
| J558L | Mouse | Myeloma | B lymphocyte cell | ECACC Cellosaurus | |
| Jurkat | Human | White blood cells | T cell leukemia | ECACC Cellosaurus | |
| JY | Human | Lymphoblastoid | EBV-transformed B cell | ECACC Cellosaurus | |
| K562 | Human | Lymphoblastoid | CML blast crisis | ECACC Cellosaurus | |
| KBM-7 | Human | Lymphoblastoid | CML blast crisis | Cellosaurus | |
| KCL-22 | Human | Lymphoblastoid | CML | DSMZ Cellosaurus | |
| KG1 | Human | Lymphoblastoid | AML | ECACC Cellosaurus | |
| Ku812 | Human | Lymphoblastoid | Erythroleukemia | ECACC Cellosaurus | |
| KYO-1 | Kyoto-1 | Human | Lymphoblastoid | CML | DSMZ Cellosaurus |
| L1210 | Mouse | Lymphocytic leukemia | Ascitic fluid | ECACC Cellosaurus | |
| L243 | Mouse | Hybridoma | Secretes L243 mAb (against HLA-DR) | ATCC Cellosaurus | |
| LNCaP | Lymph Node Cancer of the Prostate | Human | Prostatic adenocarcinoma | Epithelial | ECACC Cellosaurus |
| MA2.1 | Mouse | Hybridoma | Secretes MA2.1 mAb (against HLA-A2 and HLA-B17) | ATCC Cellosaurus | |
| Ma-Mel 1, 2, 3....48 | Human | Skin | A range of melanoma cell lines | ECACC Cellosaurus | |
| MC-38 | Mouse Colon-38 | Mouse | Colon | Adenocarcinoma | Cellosaurus |
| MCF-7 | Michigan Cancer Foundation-7 | Human | Breast | Invasive breast ductal carcinoma ER+, PR+ | ECACC Cellosaurus |
| MCF-10A | Michigan Cancer Foundation-10A | Human | Breast epithelium | ATCC Cellosaurus | |
| MDA-MB-157 | M.D. Anderson - Metastatic Breast-157 | Human | Pleural effusion metastasis | Breast carcinoma | ECACC Cellosaurus |
| MDA-MB-231 | M.D. Anderson - Metastatic Breast-231 | Human | Pleural effusion metastasis | Breast carcinoma | ECACC Cellosaurus |
| MDA-MB-361 | M.D. Anderson - Metastatic Breast-361 | Human | Melanoma (contaminated by M14) | ECACC Cellosaurus | |
| MDA-MB-468 | M.D. Anderson - Metastatic Breast-468 | Human | Pleural effusion metastasis | Breast carcinoma | ATCC Cellosaurus |
| MDCK II | Madin Darby Canine Kidney II | Dog | Kidney | Epithelium | ECACC Cellosaurus |
| MG63 | Human | Bone | Osteosarcoma | ECACC Cellosaurus | |
| MOR/0.2R | Human | Lung | Lung carcinoma | ECACC Cellosaurus | |
| Mono-Mac-6 | Human | White blood cells | Myeloid metaplasic AML | DSMZ Cellosaurus | |
| MRC-5 | Medical Research Council cell strain 5 | Human | Lung (fetal) | Fibroblast | ECACC Cellosaurus |
| MTD-1A | Mouse | Epithelium | Cellosaurus | ||
| MyEnd | Myocardial Endothelial | Mouse | Endothelium | Cellosaurus | |
| NCI-H69 | Human | Lung | Lung carcinoma | ECACC Cellosaurus | |
| NCI-H69/CPR | Human | Lung | Lung carcinoma | ECACC Cellosaurus | |
| NCI-H69/LX10 | Human | Lung | Lung carcinoma | ECACC Cellosaurus | |
| NCI-H69/LX20 | Human | Lung | Lung carcinoma | ECACC Cellosaurus | |
| NCI-H69/LX4 | Human | Lung | Lung carcinoma | ECACC Cellosaurus | |
| Neuro-2a | Mouse | Nerve/neuroblastoma | Neuronal stem cells | ECACC Cellosaurus | |
| NIH-3T3 | NIH, 3-day transfer, inoculum 3 x 105 cells | Mouse | Embryo | Fibroblast | ECACC Cellosaurus |
| NALM-1 | Human | Peripheral blood | Blast-crisis CML | ATCC Cellosaurus | |
| Neuro2a | Mouse | Nerve/neuroblastoma | Neuronal stem cells | Cellosaurus | |
| NK-92 | Human | Leukemia/lymphoma | ATCC Cellosaurus | ||
| NTERA-2 | Human | Lung metastasis | Embryonal carcinoma | ECACC Cellosaurus | |
| NW-145 | Human | Skin | Melanoma | ESTDAB Cellosaurus | |
| OK | Opossum Kidney | Virginia opossum - Didelphis virginiana | Kidney | ECACC Cellosaurus | |
| OPCN / OPCT cell lines | Human | Prostate | Range of prostate tumour lines | Cellosaurus | |
| P3X63Ag8 | Mouse | Myeloma | ECACC Cellosaurus | ||
| PC12 | Rat | Adrenal medulla | Pheochromocytoma | ECACC Cellosaurus | |
| PC-3 | Prostate Cancer-3 | Human | Bone metastasis | Prostate carcinoma | ECACC Cellosaurus |
| Peer | Human | T cell leukemia | DSMZ Cellosaurus | ||
| PNT1A | Human | Prostate | SV40-transformed tumour line | ECACC Cellosaurus | |
| PNT2 | Human | Prostate | SV40-transformed tumour line | ECACC Cellosaurus | |
| Pt K2 | The second cell line derived from Potorous tridactylis | Long-nosed potoroo - Potorous tridactylus | Kidney | Epithelial | ECACC Cellosaurus |
| Raji | Human | B lymphoma | Lymphoblast-like | ECACC Cellosaurus | |
| RBL-1 | Rat Basophilic Leukemia-1 | Rat | Leukemia | Basophil cell | ECACC Cellosaurus |
| RenCa | Renal Carcinoma | Mouse | Kidney | Renal carcinoma | ATCC Cellosaurus |
| RIN-5F | Mouse | Pancreas | ECACC Cellosaurus | ||
| RMA-S | Mouse | T cell tumour | Cellosaurus | ||
| S2 | Schneider 2 | Insect - Drosophila melanogaster | Late stage (20–24 hours old) embryos | ATCC Cellosaurus | |
| SaOS-2 | Sarcoma OSteogenic-2 | Human | Bone | Osteosarcoma | ECACC Cellosaurus |
| Sf21 | Spodoptera frugiperda 21 | Insect (moth) - Spodoptera frugiperda | Ovary | ECACC Cellosaurus | |
| Sf9 | Spodoptera frugiperda 9 | Insect (moth) - Spodoptera frugiperda | Ovary | ECACC Cellosaurus | |
| SH-SY5Y | Human | Bone marrow metastasis | Neuroblastoma | ECACC Cellosaurus | |
| SiHa | Human | Cervix epithelium | Cervical carcinoma | ATCC Cellosaurus | |
| SK-BR-3 | Sloan-Kettering Breast cancer 3 | Human | Breast | Breast carcinoma | DSMZ Cellosaurus |
| SK-OV-3 | Sloan-Kettering Ovarian cancer 3 | Human | Ovary | Ovarian carcinoma | ECACC Cellosaurus |
| T2 | Human | T cell leukemia/B cell line hybridoma | ATCC Cellosaurus | ||
| T-47D | Human | Breast | Breast ductal carcinoma | ECACC Cellosaurus | |
| T84 | Human | Lung metastasis | Colorectal carcinoma | ECACC Cellosaurus | |
| T98G | Human | Glioblastoma-astrocytoma | Epithelium | ECACC Cellosaurus | |
| THP-1 | Human | Monocyte | Acute monocytic leukemia | ECACC Cellosaurus | |
| U373 | Human | Glioblastoma-astrocytoma | Epithelium | ECACC Cellosaurus | |
| U87 | Human | Glioblastoma-astrocytoma | Epithelial-like | ECACC Cellosaurus | |
| U937 | Human | Leukemic monocytic lymphoma | ECACC Cellosaurus | ||
| VCaP | Vertebral Cancer of the Prostate | Human | Vertebra metastasis | Prostate carcinoma | ECACC Cellosaurus |
| Vero | Vero (truth) | African green monkey - Chlorocebus sabaeus | Kidney epithelium | ECACC Cellosaurus | |
| VG-1 | Human | Primary effusion lymphoma | Cellosaurus | ||
| WM39 | Human | Skin | Melanoma | ESTDAB Cellosaurus | |
| WT-49 | Human | Lymphoblastoid | ECACC Cellosaurus | ||
| YAC-1 | Mouse | Lymphoma | ECACC Cellosaurus | ||
| YAR | Human | Lymphoblastoid | EBV-transformed B cell | Human Immunology[52] ECACC Cellosaurus |
See also
- Biological immortality
- Cell culture assays
- Electric cell-substrate impedance sensing
- List of contaminated cell lines
References and notes
- ^ "Some landmarks in the development of tissue and cell culture". Retrieved 2006-04-19.
- ^ "Cell Culture". Retrieved 2006-04-19.
- ^ "Whonamedit - Ringer's solution". whonamedit.com. Retrieved 2014-06-09.
- ^ "Animals and alternatives in testing". Archived from the original on 2006-02-25. Retrieved 2006-04-19.
- ^ Schiff, JudithAnn. "An unsung hero of medical research". Retrieved 2006-04-19. Yale Alumni Magazine, February 2002.
- ^ "Post - Blog | Boval BioSolutions, LLC". bovalco.com. Retrieved 2014-12-02.
- ^ "LipiMAX purified lipoprotein solution from bovine serum". Selborne Biological Services. 2006. Retrieved 2010-02-02.
- ^ Portela VM, Zamberlam G, Price CA (April 2010). "Cell plating density alters the ratio of estrogenic to progestagenic enzyme gene expression in cultured granulosa cells". Fertil. Steril. 93 (6): 2050–5. doi:10.1016/j.fertnstert.2009.01.151. PMID 19324349.
- ^ Jill Neimark (27 February 2015). "Line of attack". Science. 347 (6225): 938–940. doi:10.1126/science.347.6225.938.
- ^ Drexler, HG; Dirks, WG; MacLeod, RA (Oct 1999). "False human hematopoietic cell lines: cross-contaminations and misinterpretations". Leukemia. 13 (10): 1601–7. doi:10.1038/sj/leu/2401510. ISSN 0887-6924. PMID 10516762.
- ^ Drexler, HG; MacLeod, RA; Dirks, WG (Dec 2001). "Cross-contamination: HS-Sultan is not a myeloma but a Burkitt lymphoma cell line" (Free full text). Blood. 98 (12): 3495–6. doi:10.1182/blood.V98.12.3495. ISSN 0006-4971. PMID 11732505.
- ^ Cabrera, CM; Cobo, F; Nieto, A; Cortés, JL; Montes, RM; Catalina, P; Concha, A (Jun 2006). "Identity tests: determination of cell line cross-contamination". Cytotechnology. 51 (2): 45–50. doi:10.1007/s10616-006-9013-8. ISSN 0920-9069. PMC 3449683. PMID 19002894.
- ^ a b Chatterjee, R (Feb 2007). "Cell biology. Cases of mistaken identity". Science. 315 (5814): 928–31. doi:10.1126/science.315.5814.928. ISSN 0036-8075. PMID 17303729.
- ^ Liscovitch, M; Ravid, D (Jan 2007). "A case study in misidentification of cancer cell lines: MCF-7/AdrR cells (re-designated NCI/ADR-RES) are derived from OVCAR-8 human ovarian carcinoma cells". Cancer Letters. 245 (1–2): 350–2. doi:10.1016/j.canlet.2006.01.013. ISSN 0304-3835. PMID 16504380.
- ^ Macleod, RA; Dirks, WG; Matsuo, Y; Kaufmann, M; Milch, H; Drexler, HG (Nov 1999). "Widespread intraspecies cross-contamination of human tumor cell lines arising at source". International Journal of Cancer. Journal International Du Cancer. 83 (4): 555–63. doi:10.1002/(SICI)1097-0215(19991112)83:4<555::AID-IJC19>3.0.CO;2-2. ISSN 0020-7136. PMID 10508494.
- ^ Masters, JR (Apr 2002). "HeLa cells 50 years on: the good, the bad and the ugly". Nature reviews. Cancer. 2 (4): 315–9. doi:10.1038/nrc775. ISSN 1474-175X. PMID 12001993.
- ^ a b Dunham, J.H.; Guthmiller, P. (2008). "Doing good science: Authenticating cell line identity" (PDF). Cell Notes. 22: 15–17.
- ^ Nguyen, H. T.; Geens, M.; Spits, C. (2012). "Genetic and epigenetic instability in human pluripotent stem cells". Human Reproduction Update. 19 (2): 187–205. doi:10.1093/humupd/dms048. PMID 23223511.
- ^ "Moore v. Regents of University of California (1990) 51 C3d 120". Online.ceb.com. Retrieved 2012-01-27.
- ^ Hayflick, L. (September 1998). "A brief history of the mortality and immortality of cultured cells". Keio J Med. 3. 47 (3): 174–182. doi:10.2302/kjm.47.174. PMID 9785764.
- ^ "Worthington tissue guide". Retrieved 2013-04-30.
- ^ Qiana L, Saltzman WM (2004) "Improving the expansion and neuronal differentiation of mesenchymal stem cells through culture surface modification." Biomaterials 25: 1331-1337.
- ^ Maguire G (2016) Therapeutics from Adult Stem Cells and the Hype Curve. ACS Med. Chem. Lett. 7 (5): 441–443
- ^ Discher, D. E.; Janmey, P; Wang, YL (2005). "Tissue Cells Feel and Respond to the Stiffness of Their Substrate". Science. 310 (5751): 1139–43. doi:10.1126/science.1116995. PMID 16293750.
- ^ Gilbert, PM; Havenstrite, KL; Magnusson, KE; Sacco, A; Leonardi, NA; Kraft, P; Nguyen, NK; Thrun, S; Lutolf, MP; Blau, HM (2010). "Substrate elasticity regulates skeletal muscle stem cell self-renewal in culture". Science. 329 (5995): 1078–81. doi:10.1126/science.1191035. PMC 2929271. PMID 20647425.
- ^ Chowdhury, Farhan; Li, Yanzhen; Poh, Yeh-Chuin; Yokohama-Tamaki, Tamaki; Wang, Ning; Tanaka, Tetsuya S. (2010). Zhou, Zhongjun (ed.). "Soft Substrates Promote Homogeneous Self-Renewal of Embryonic Stem Cells via Downregulating Cell-Matrix Tractions". PLoS ONE. 5 (12): e15655. doi:10.1371/journal.pone.0015655. PMC 3001487. PMID 21179449.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Engler, Adam J.; Sen, Shamik; Sweeney, H. Lee; Discher, Dennis E. (2006). "Matrix Elasticity Directs Stem Cell Lineage Specification". Cell. 126 (4): 677–89. doi:10.1016/j.cell.2006.06.044. PMID 16923388.
- ^ Paszek, Matthew J.; Zahir, Nastaran; Johnson, Kandice R.; Lakins, Johnathon N.; Rozenberg, Gabriela I.; Gefen, Amit; Reinhart-King, Cynthia A.; Margulies, Susan S.; Dembo, Micah; Boettiger, David; Hammer, Daniel A.; Weaver, Valerie M. (2005). "Tensional homeostasis and the malignant phenotype". Cancer Cell. 8 (3): 241–54. doi:10.1016/j.ccr.2005.08.010. PMID 16169468.
- ^ Levental, Kandice R.; Yu, Hongmei; Kass, Laura; Lakins, Johnathon N.; Egeblad, Mikala; Erler, Janine T.; Fong, Sheri F.T.; Csiszar, Katalin; Giaccia, Amato; Weninger, Wolfgang; Yamauchi, Mitsuo; Gasser, David L.; Weaver, Valerie M. (2009). "Matrix Crosslinking Forces Tumor Progression by Enhancing Integrin Signaling". Cell. 139 (5): 891–906. doi:10.1016/j.cell.2009.10.027. PMC 2788004. PMID 19931152.
- ^ Tilghman, Robert W.; Cowan, Catharine R.; Mih, Justin D.; Koryakina, Yulia; Gioeli, Daniel; Slack-Davis, Jill K.; Blackman, Brett R.; Tschumperlin, Daniel J.; Parsons, J. Thomas (2010). Hotchin, Neil A (ed.). "Matrix Rigidity Regulates Cancer Cell Growth and Cellular Phenotype". PLoS ONE. 5 (9): e12905. doi:10.1371/journal.pone.0012905. PMC 2944843. PMID 20886123.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Liu, F; Mih, JD; Shea, BS; Kho, AT; Sharif, AS; Tager, AM; Tschumperlin, DJ (2010). "Feedback amplification of fibrosis through matrix stiffening and COX-2 suppression". The Journal of Cell Biology. 190 (4): 693–706. doi:10.1083/jcb.201004082. PMC 2928007. PMID 20733059.
- ^ Wipff, PJ; Rifkin, DB; Meister, JJ; Hinz, B (2007). "Myofibroblast contraction activates latent TGF-beta1 from the extracellular matrix". The Journal of Cell Biology. 179 (6): 1311–23. doi:10.1083/jcb.200704042. PMC 2140013. PMID 18086923.
- ^ Georges, PC; Hui, JJ; Gombos, Z; McCormick, ME; Wang, AY; Uemura, M; Mick, R; Janmey, PA; Furth, EE; Wells, RG (2007). "Increased stiffness of the rat liver precedes matrix deposition: Implications for fibrosis". American Journal of Physiology. Gastrointestinal and Liver Physiology. 293 (6): G1147–54. doi:10.1152/ajpgi.00032.2007. PMID 17932231.
- ^ Li, L; Sharma, N; Chippada, U; Jiang, X; Schloss, R; Yarmush, ML; Langrana, NA (2008). "Functional modulation of ES-derived hepatocyte lineage cells via substrate compliance alteration". Annals of Biomedical Engineering. 36 (5): 865–76. doi:10.1007/s10439-008-9458-3. PMID 18266108.
- ^ Semler, Eric J.; Lancin, Perry A.; Dasgupta, Anouska; Moghe, Prabhas V. (2005). "Engineering hepatocellular morphogenesis and function via ligand-presenting hydrogels with graded mechanical compliance". Biotechnology and Bioengineering. 89 (3): 296–307. doi:10.1002/bit.20328. PMID 15744840.
- ^ Friedland, JC; Lee, MH; Boettiger, D (2009). "Mechanically activated integrin switch controls alpha5beta1 function". Science. 323 (5914): 642–4. doi:10.1126/science.1168441. PMID 19179533.
- ^ Chan, CE; Odde, DJ (2008). "Traction dynamics of filopodia on compliant substrates". Science. 322 (5908): 1687–91. doi:10.1126/science.1163595. PMID 19074349.
- ^ Dupont, Sirio; Morsut, Leonardo; Aragona, Mariaceleste; Enzo, Elena; Giulitti, Stefano; Cordenonsi, Michelangelo; Zanconato, Francesca; Le Digabel, Jimmy; Forcato, Mattia; Bicciato, Silvio; Elvassore, Nicola; Piccolo, Stefano (2011). "Role of YAP/TAZ in mechanotransduction". Nature. 474 (7350): 179–83. doi:10.1038/nature10137. PMID 21654799.
- ^ "drug discovery@nature.com". Nature.com. Retrieved 2013-03-26.
- ^ Duell, BL; Cripps, AW; Schembri, MA; Ulett, GC (2011). "Epithelial cell coculture models for studying infectious diseases: Benefits and limitations". Journal of biomedicine & biotechnology. 2011: 852419. doi:10.1155/2011/852419. PMC 3189631. PMID 22007147.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Barrila, Jennifer; Radtke, Andrea L.; Crabbé, Aurélie; Sarker, Shameema F.; Herbst-Kralovetz, Melissa M.; Ott, C. Mark; Nickerson, Cheryl A. (2010). "Organotypic 3D cell culture models: Using the rotating wall vessel to study host–pathogen interactions". Nature Reviews Microbiology. 8 (11): 791–801. doi:10.1038/nrmicro2423. PMID 20948552.
- ^ M. Bhattacharya et al. Nanofibrillar cellulose hydrogel promotes three-dimensional liver cell culture. J Control Release 2012 Dec 28;164(3):291-8
- ^ Derosa, Maria C.; Monreal, Carlos; Schnitzer, Morris; Walsh, Ryan; Sultan, Yasir (2010). "Nanotechnology in fertilizers". Nature Nanotechnology. 5 (2): 91. doi:10.1038/nnano.2010.2. PMID 20130583.
- ^ Hsiao, Amy Y.; Tung, Yi-Chung; Qu, Xianggui; Patel, Lalit R.; Pienta, Kenneth J.; Takayama, Shuichi (2012). "384 hanging drop arrays give excellent Z-factors and allow versatile formation of co-culture spheroids". Biotechnology and Bioengineering. 109 (5): 1293–304. doi:10.1002/bit.24399. PMC 3306496. PMID 22161651.
- ^ M.W. Tibbitt, K.S. Anseth Hydrogels as Extracellular Matrix Mimics for 3D Cell Culture Biotechnol Bioeng. 2009 Jul 1;103(4):655-63
- ^ Reuters (2006-01-26). "Quickie Bird Flu Vaccine Created". Wired. Wired.com. Retrieved 2010-01-31.
{{cite web}}:|author=has generic name (help) - ^ Gao W; Soloff AC; Lu X; Montecalvo A; Nguyen DC; Matsuoka Y; Robbins PD; Swayne DE; Donis RO; Katz JM; Barratt-Boyes SM; Gambotto A. (February 2006). "Protection of mice and poultry from lethal H5N1 avian influenza virus through adenovirus-based immunization". Journal of Virology. 80 (4). United States: American Society for Microbiology: 1959–1964. doi:10.1128/JVI.80.4.1959-1964.2006. ISSN 0022-538X. PMC 1367171. PMID 16439551. Retrieved 2010-01-31.
- ^ "NIAID Taps Chiron to Develop Vaccine Against H9N2 Avian Influenza". National Institute of Allergy and Infectious Diseases (NIAID). 2004-08-17. Retrieved 2010-01-31.
- ^ Hunt, P; Robertson, D; Weiss, D; Rennick, D; Lee, F; Witte, ON (1987). "A single bone marrow-derived stromal cell type supports the in vitro growth of early lymphoid and myeloid cells". Cell. 48 (6): 997–1007. doi:10.1016/0092-8674(87)90708-2. PMID 2435412.
- ^ Van Den Berg-Bakker, CA; Hagemeijer, A; Franken-Postma, EM; Smit, VT; Kuppen, PJ; Van Ravenswaay Claasen, HH; Cornelisse, CJ; Schrier, PI (1993). "Establishment and characterization of 7 ovarian carcinoma cell lines and one granulosa tumor cell line: Growth features and cytogenetics". International Journal of Cancer. Journal International Du Cancer. 53 (4): 613–20. doi:10.1002/ijc.2910530415. PMID 8436435.
- ^ Lee, YG; Korenchuk, S; Lehr, J; Whitney, S; Vessela, R; Pienta, KJ (2001). "Establishment and characterization of a new human prostatic cancer cell line: DuCaP". In vivo (Athens, Greece). 15 (2): 157–62. PMID 11317521.
- ^ Ou, Dawei; Mitchell, Leslie Ann; Décarie, Diane; Tingle, Aubrey J; Nepom, Gerald T (1998). "Promiscuous T-Cell Recognition of a Rubella Capsid Protein Epitope Restricted by DRB1*0403 and DRB1*0901 Molecules Sharing an HLA DR Supertype". Human Immunology. 59 (3): 149–57. doi:10.1016/S0198-8859(98)00006-8. PMID 9548074.
- Public Health England, Public Health England Culture Collections (ECACC)
- MacLeod, R. A. F.; Dirks, Wilhelm G.; Matsuo, Yoshinobu; Kaufmann, Maren; Milch, Herbert; Drexler, Hans G. (1999). "Widespread intraspecies cross-contamination of human tumour cell lines". International Journal of Cancer. 83 (4): 555–563. doi:10.1002/(SICI)1097-0215(19991112)83:4<555::AID-IJC19>3.0.CO;2-2. PMID 10508494.
- Masters, John R. (2002). "HeLa cells 50 years on: the good, the bad and the ugly". Nature Reviews Cancer. 2 (4): 315–319. doi:10.1038/nrc775. PMID 12001993.
- Recently invented was the 3D Petri dish, the first 3D cell culture offering.
External links
- Table of common cell lines from Alberts 4th ed.
- Cancer Cells in Culture
- Evolution of Cell Culture Surfaces
- Hypertext version of the Cell Line Data Base
- Microcarrier Cell Culture Handbook by GE Healthcare Life Sciences
- Cell Culture Applications - Resources including application notes and protocols to create an ideal environment for growing cells, right from the start.
- Cell Culture Basics - Introduction to cell culture, covering topics such as laboratory set-up, safety and aseptic technique including basic cell culture protocols and video training
- Database of Who's Who in Cell Culture and Related Research
- Witkowski, Jan A. (2012). "Experimental pathology and the origins of tissue culture: Leo Loeb's contribution". Medical History. 27 (3): 269–88. doi:10.1017/S0025727300042964. PMC 1139336. PMID 6353093.
- Coriell Cell Repositories
- Strategies for Protein Purification Handbook
- An Introduction To Cell Culture. This webinar introduces the history, theory, basic techniques, and potential pit-falls of mammalian cell culture.
- The National Centre for Cell Science (NCCS), Pune, India; national repository for cell lines/hybridomas etc.
- Pacey, Laura; Stead, Shelley; Gleave, Jacqueline; Tomczyk, Kasia; Doering, Laurie (2006). "Neural Stem Cell Culture: Neurosphere generation, microscopical analysis and cryopreservation". Protocol Exchange. doi:10.1038/nprot.2006.215.
- Gilabert, Juan A.; Montalvo, Gema B.; Artalejo, Antonio R. (2006). "Rat Chromaffin cells primary cultures: Standardization and quality assessment for single-cell assays". Protocol Exchange. doi:10.1038/nprot.2006.294.

