Oxoguanine glycosylase
| 8-oxoguanine DNA glycosylase, N-terminal domain | |||||||||
|---|---|---|---|---|---|---|---|---|---|
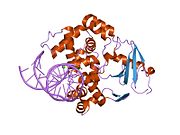
 structure of catalytically inactive q315a human 8-oxoguanine glycosylase complexed to 8-oxoguanine dna | |||||||||
| Identifiers | |||||||||
| Symbol | OGG_N | ||||||||
| Pfam | PF07934 | ||||||||
| Pfam clan | CL0407 | ||||||||
| InterPro | IPR012904 | ||||||||
| SCOP2 | 1ebm / SCOPe / SUPFAM | ||||||||
| |||||||||
8-Oxoguanine glycosylase also known as OGG1 is a DNA glycosylase enzyme that, in humans, is encoded by the OGG1 gene. It is involved in base excision repair. It is found in bacterial, archaeal and eukaryotic species.
Function
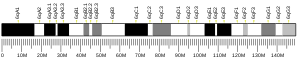
OGG1 is the primary enzyme responsible for the excision of 8-oxoguanine (8-oxoG), a mutagenic base byproduct that occurs as a result of exposure to reactive oxygen species (ROS). OGG1 is a bifunctional glycosylase, as it is able to both cleave the glycosidic bond of the mutagenic lesion and cause a strand break in the DNA backbone. Alternative splicing of the C-terminal region of this gene classifies splice variants into two major groups, type 1 and type 2, depending on the last exon of the sequence. Type 1 alternative splice variants end with exon 7 and type 2 end with exon 8. One set of spliced forms are designated 1a, 1b, 2a to 2e.[5] All variants have the N-terminal region in common. Many alternative splice variants for this gene have been described, but the full-length nature for every variant has not been determined. In eukaryotes, the N-terminus of this gene contains a mitochondrial targeting signal, essential for mitochondrial localization.[6] However, OGG1-1a also has a nuclear location signal at its C-terminal end that suppresses mitochondrial targeting and causes OGG1-1a to localize to the nucleus.[5] The main form of OGG1 that localizes to the mitochondria is OGG1-2a.[5] A conserved N-terminal domain contributes residues to the 8-oxoguanine binding pocket. This domain is organised into a single copy of a TBP-like fold.[7]
Despite the presumed importance of this enzyme, mice lacking Ogg1 have been generated and found to have a normal lifespan,[8] and Ogg1 knockout mice have a higher probability to develop cancer, whereas Mth1 gene disruption concomitantly suppresses lung cancer development in Ogg1-/- mice.[9] Mice lacking Ogg1 have been shown to be prone to increased body weight and obesity, as well as high-fat diet induced insulin resistance.[10] There is some controversy as to whether deletion of Ogg1 actually leads to increased 8-oxo-dG levels: the HPLC-EC assay suggests up to 6 fold higher levels of 8-oxo-dG in nuclear DNA and 20-fold higher in mitochondrial DNA whereas the Fapy-glycosylase assay indicates no change.[citation needed]
OGG1 deficiency and increased 8-oxo-dG in mice

Mice without a functional OGG1 gene have about a 5-fold increased level of 8-oxo-dG in their livers compared to mice with wild-type OGG1.[9] Mice defective in OGG1 also have an increased risk for cancer.[9] Kunisada et al.[12] irradiated mice without a functional OGG1 gene (OGG1 knock-out mice) and wild-type mice three times a week for forty weeks with UVB light at a relatively low dose (not enough to cause skin redness). Both types of mice had high levels of 8-oxo-dG in their epidermal cells three hours after irradiation. However, 24 hours later, the majority of 8-oxo-dG was absent from the epidermal cells of the wild-type mice but 8-oxo-dG remained elevated in the epidermal cells of the OGG1 knock-out mice. The irradiated OGG1 knock-out mice had more than twice the level of skin tumors compared to irradiated wild-type mice, and the rate of malignancy within the tumors was higher in the OGG1 knock-out mice (73%) than in the wild-type mice (50%).
As reviewed by Valavanidis et al.,[13] increased levels of 8-oxo-dG in a tissue can serve as a biomarker of oxidative stress. They also noted that increased levels of 8-oxo-dG are frequently found during carcinogenesis.
In the figure showing examples of mouse colonic epithelium, the colonic epithelium from a mouse on a normal diet was found to have a low level of 8-oxo-dG in its colonic crypts (panel A). However, a mouse likely undergoing colonic tumorigenesis (due to deoxycholate added to its diet[11]) was found to have a high level of 8-oxo-dG in its colonic epithelium (panel B). Deoxycholate increases intracellular production of reactive oxygen resulting in increased oxidative stress,[14]>[15] and this can lead to tumorigenesis and carcinogenesis.
Epigenetic control
In a breast cancer study, the methylation level of the OGG1 promoter was found to be anti-correlated with expression level of OGG1 messenger RNA.[16] This means that hypermethylation was associated with low expression of OGG1 and hypomethylation was correlated with over-expression of OGG1. Thus, OGG1 expression is under epigenetic control. Breast cancers with methylation levels of the OGG1 promoter that were more than two standard deviations either above or below the normal were each associated with reduced patient survival.[16]
In cancers
OGG1 is the primary enzyme responsible for the excision of 8-oxo-2'-deoxyguanosine (8-oxo-dG). Even when OGG1 expression is normal, the presence of 8-oxo-dG is mutagenic since OGG1 is not 100% effective. Yasui et al.[17] examined the fate of 8-oxo-dG when this oxidized derivative of deoxyguanosine was inserted into a specific gene in 800 cells in culture. After replication of the cells, 8-oxo-dG was restored to G in 86% of the clones, probably reflecting accurate OGG1 base excision repair or translesion synthesis without mutation. G:C to T:A transversions occurred in 5.9% of the clones, single base deletions in 2.1% and G:C to C:G transversions in 1.2%. Together, these mutations were the most common, totalling 9.2% of the 14% of mutations generated at the site of the 8-oxo-dG insertion. Among the other mutations in the 800 clones analyzed, there were also 3 larger deletions, of sizes 6, 33 and 135 base pairs. Thus 8-oxo-dG can directly cause mutations, some of which may contribute to carcinogenesis.
If OGG1 expression is reduced in cells, increased mutagenesis, and therefore increased carcinogenesis would be expected. The table, below, lists cancers with reduced expression of OGG1.
| Cancer | Expression | Form of OGG1 | 8-oxo-dG | Evaluation method | Ref. |
|---|---|---|---|---|---|
| Head and neck cancer | Under-expression | OGG1-2a | - | messenger RNA | [18] |
| Adenocarcinoma of gastric cardia | Under-expression | cytoplasmic | increased | immunohistochemistry | [19] |
| Astrocytoma | Under-expression | total cell OGG1 | - | messenger RNA | [20] |
| Esophageal cancer | 48% Under-expression | nuclear | increased | immunohistochemistry | [21] |
| - | 40% Under-expression | cytoplasm | increased | immunohistochemistry | [21] |
OGG1 or OGG activity in blood, and cancer
OGG1 methylation levels in blood cells were measured in a prospective study of 582 US Veterans, median age 72, and followed for 13 years. High OGG1 methylation at a particular promoter region was associated with increased risk for any cancer, and in particular for risk of prostate cancer.[22]
Enzymatic activity excising 8-oxoguanine from DNA (OGG activity) was reduced in peripheral blood mononuclear cells (PBMCs), and in paired lung tissue, from patients with non–small cell lung cancer.[23] OGG activity was also reduced in PBMCs of patients with head and neck squamous cell carcinoma (HNSCC).[24]
Interactions
Oxoguanine glycosylase has been shown to interact with XRCC1[25] and PKC alpha.[26]
Pathology
References
- ^ a b c GRCh38: Ensembl release 89: ENSG00000114026 – Ensembl, May 2017
- ^ a b c GRCm38: Ensembl release 89: ENSMUSG00000030271 – Ensembl, May 2017
- ^ "Human PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ "Mouse PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ a b c Nishioka K, Ohtsubo T, Oda H, Fujiwara T, Kang D, Sugimachi K, Nakabeppu Y (May 1999). "Expression and differential intracellular localization of two major forms of human 8-oxoguanine DNA glycosylase encoded by alternatively spliced OGG1 mRNAs". Molecular Biology of the Cell. 10 (5): 1637–52. doi:10.1091/mbc.10.5.1637. PMC 30487. PMID 10233168.
- ^ "Entrez Gene: OGG1 8-oxoguanine DNA glycosylase".
- ^ Bjørås M, Seeberg E, Luna L, Pearl LH, Barrett TE (March 2002). "Reciprocal "flipping" underlies substrate recognition and catalytic activation by the human 8-oxo-guanine DNA glycosylase". Journal of Molecular Biology. 317 (2): 171–7. doi:10.1006/jmbi.2002.5400. PMID 11902834.
- ^ Klungland A, Rosewell I, Hollenbach S, Larsen E, Daly G, Epe B, Seeberg E, Lindahl T, Barnes DE (November 1999). "Accumulation of premutagenic DNA lesions in mice defective in removal of oxidative base damage". Proceedings of the National Academy of Sciences of the United States of America. 96 (23): 13300–5. doi:10.1073/pnas.96.23.13300. PMC 23942. PMID 10557315.
- ^ a b c Sakumi K, Tominaga Y, Furuichi M, Xu P, Tsuzuki T, Sekiguchi M, Nakabeppu Y (March 2003). "Ogg1 knockout-associated lung tumorigenesis and its suppression by Mth1 gene disruption". Cancer Research. 63 (5): 902–5. PMID 12615700.
- ^ Sampath H, Vartanian V, Rollins MR, Sakumi K, Nakabeppu Y, Lloyd RS (December 2012). "8-Oxoguanine DNA glycosylase (OGG1) deficiency increases susceptibility to obesity and metabolic dysfunction". PLOS One. 7 (12): e51697. doi:10.1371/journal.pone.0051697. PMC 3524114. PMID 23284747.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ a b Prasad AR, Prasad S, Nguyen H, Facista A, Lewis C, Zaitlin B, Bernstein H, Bernstein C (July 2014). "Novel diet-related mouse model of colon cancer parallels human colon cancer". World Journal of Gastrointestinal Oncology. 6 (7): 225–43. doi:10.4251/wjgo.v6.i7.225. PMC 4092339. PMID 25024814.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Kunisada M, Sakumi K, Tominaga Y, Budiyanto A, Ueda M, Ichihashi M, Nakabeppu Y, Nishigori C (July 2005). "8-Oxoguanine formation induced by chronic UVB exposure makes Ogg1 knockout mice susceptible to skin carcinogenesis". Cancer Research. 65 (14): 6006–10. doi:10.1158/0008-5472.CAN-05-0724. PMID 16024598.
- ^ Valavanidis A, Vlachogianni T, Fiotakis K, Loridas S (August 2013). "Pulmonary oxidative stress, inflammation and cancer: respirable particulate matter, fibrous dusts and ozone as major causes of lung carcinogenesis through reactive oxygen species mechanisms". International Journal of Environmental Research and Public Health. 10 (9): 3886–907. doi:10.3390/ijerph10093886. PMC 3799517. PMID 23985773.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Tsuei J, Chau T, Mills D, Wan YJ (November 2014). "Bile acid dysregulation, gut dysbiosis, and gastrointestinal cancer". Experimental Biology and Medicine. 239 (11): 1489–504. doi:10.1177/1535370214538743. PMID 24951470.
- ^ Ajouz H, Mukherji D, Shamseddine A (May 2014). "Secondary bile acids: an underrecognized cause of colon cancer". World Journal of Surgical Oncology. 12: 164. doi:10.1186/1477-7819-12-164. PMID 24884764.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ a b Fleischer T, Edvardsen H, Solvang HK, Daviaud C, Naume B, Børresen-Dale AL, Kristensen VN, Tost J (June 2014). "Integrated analysis of high-resolution DNA methylation profiles, gene expression, germline genotypes and clinical end points in breast cancer patients". International Journal of Cancer. 134 (11): 2615–25. doi:10.1002/ijc.28606. PMID 24395279.
- ^ Yasui M, Kanemaru Y, Kamoshita N, Suzuki T, Arakawa T, Honma M (March 2014). "Tracing the fates of site-specifically introduced DNA adducts in the human genome". DNA Repair. 15: 11–20. doi:10.1016/j.dnarep.2014.01.003. PMID 24559511.
- ^ Mahjabeen I, Kayani MA (2016). "Loss of Mitochondrial Tumor Suppressor Genes Expression Is Associated with Unfavorable Clinical Outcome in Head and Neck Squamous Cell Carcinoma: Data from Retrospective Study". PLOS One. 11 (1): e0146948. doi:10.1371/journal.pone.0146948. PMC 4718451. PMID 26785117.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Kohno Y, Yamamoto H, Hirahashi M, Kumagae Y, Nakamura M, Oki E, Oda Y (June 2016). "Reduced MUTYH, MTH1, and OGG1 expression and TP53 mutation in diffuse-type adenocarcinoma of gastric cardia". Human Pathology. 52: 145–52. doi:10.1016/j.humpath.2016.01.006. PMID 26980051.
- ^ Jiang Z, Hu J, Li X, Jiang Y, Zhou W, Lu D (December 2006). "Expression analyses of 27 DNA repair genes in astrocytoma by TaqMan low-density array". Neuroscience Letters. 409 (2): 112–7. doi:10.1016/j.neulet.2006.09.038. PMID 17034947.
- ^ a b Kubo N, Morita M, Nakashima Y, Kitao H, Egashira A, Saeki H, Oki E, Kakeji Y, Oda Y, Maehara Y (April 2014). "Oxidative DNA damage in human esophageal cancer: clinicopathological analysis of 8-hydroxydeoxyguanosine and its repair enzyme". Diseases of the Esophagus. 27 (3): 285–93. doi:10.1111/dote.12107. PMID 23902537.
- ^ Gao T, Joyce BT, Liu L, Zheng Y, Dai Q, Zhang Z, Zhang W, Shrubsole MJ, Tao MH, Schwartz J, Baccarelli A, Hou L (2016). "DNA methylation of oxidative stress genes and cancer risk in the Normative Aging Study". American Journal of Cancer Research. 6 (2): 553–61. PMC 4859680. PMID 27186424.
- ^ Paz-Elizur T, Krupsky M, Blumenstein S, Elinger D, Schechtman E, Livneh Z (September 2003). "DNA repair activity for oxidative damage and risk of lung cancer". Journal of the National Cancer Institute. 95 (17): 1312–9. doi:10.1093/jnci/djg033. PMID 12953085.
- ^ Paz-Elizur T, Ben-Yosef R, Elinger D, Vexler A, Krupsky M, Berrebi A, Shani A, Schechtman E, Freedman L, Livneh Z (December 2006). "Reduced repair of the oxidative 8-oxoguanine DNA damage and risk of head and neck cancer". Cancer Research. 66 (24): 11683–9. doi:10.1158/0008-5472.CAN-06-2294. PMID 17178863.
- ^ Marsin S, Vidal AE, Sossou M, Ménissier-de Murcia J, Le Page F, Boiteux S, de Murcia G, Radicella JP (November 2003). "Role of XRCC1 in the coordination and stimulation of oxidative DNA damage repair initiated by the DNA glycosylase hOGG1". The Journal of Biological Chemistry. 278 (45): 44068–74. doi:10.1074/jbc.M306160200. PMID 12933815.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Dantzer F, Luna L, Bjørås M, Seeberg E (June 2002). "Human OGG1 undergoes serine phosphorylation and associates with the nuclear matrix and mitotic chromatin in vivo". Nucleic Acids Research. 30 (11): 2349–57. doi:10.1093/nar/30.11.2349. PMC 117190. PMID 12034821.
- ^ Osorio A, Milne RL, Kuchenbaecker K, Vaclová T, Pita G, Alonso R, et al. (April 2014). "DNA glycosylases involved in base excision repair may be associated with cancer risk in BRCA1 and BRCA2 mutation carriers". PLoS Genetics. 10 (4): e1004256. doi:10.1371/journal.pgen.1004256. PMC 3974638. PMID 24698998.
{{cite journal}}: CS1 maint: unflagged free DOI (link)
Further reading
- Boiteux S, Radicella JP (May 2000). "The human OGG1 gene: structure, functions, and its implication in the process of carcinogenesis". Archives of Biochemistry and Biophysics. 377 (1): 1–8. doi:10.1006/abbi.2000.1773. PMID 10775435.
- Park J, Chen L, Tockman MS, Elahi A, Lazarus P (February 2004). "The human 8-oxoguanine DNA N-glycosylase 1 (hOGG1) DNA repair enzyme and its association with lung cancer risk". Pharmacogenetics. 14 (2): 103–9. doi:10.1097/00008571-200402000-00004. PMID 15077011.
- Hung RJ, Hall J, Brennan P, Boffetta P (November 2005). "Genetic polymorphisms in the base excision repair pathway and cancer risk: a HuGE review". American Journal of Epidemiology. 162 (10): 925–42. doi:10.1093/aje/kwi318. PMID 16221808.
- Mirbahai L, Kershaw RM, Green RM, Hayden RE, Meldrum RA, Hodges NJ (February 2010). "Use of a molecular beacon to track the activity of base excision repair protein OGG1 in live cells". DNA Repair. 9 (2): 144–52. doi:10.1016/j.dnarep.2009.11.009. PMID 20042377.
External links
- oxoguanine+glycosylase+1,+human at the U.S. National Library of Medicine Medical Subject Headings (MeSH)