Polio vaccine: Difference between revisions
BrooklynBen (talk | contribs) →Development: added citation to College of Physicians' website for Koprowski's first test of oral polio vaccines. Previously only a corporate citation, which could be construed as biased. |
BrooklynBen (talk | contribs) →External links: Added link to Polio article at History of Vaccines, from College of Physicians of Philadelphia |
||
| Line 88: | Line 88: | ||
== External links == |
== External links == |
||
* [http://www.historyofvaccines.org/content/timelines/polio History of Vaccines Website – History of Polio] History of Vaccines, a project of the [[College of Physicians of Philadelphia]] |
|||
* [http://blogs.cgdev.org/vaccine CGDev.org] - 'Vaccines for Development', [[Center for Global Development]] |
* [http://blogs.cgdev.org/vaccine CGDev.org] - 'Vaccines for Development', [[Center for Global Development]] |
||
* [http://www.pbs.org/wgbh/aso/databank/entries/dm52sa.html PBS.org] - 'People and Discoveries: Salk Produces Polio Vaccine 1952', [[PBS]] |
* [http://www.pbs.org/wgbh/aso/databank/entries/dm52sa.html PBS.org] - 'People and Discoveries: Salk Produces Polio Vaccine 1952', [[PBS]] |
||
Revision as of 20:03, 3 December 2010
 | |
| Vaccine description | |
|---|---|
| Target | Polio virus |
| Vaccine type | Inactivated |
| Clinical data | |
| Pregnancy category |
|
| Routes of administration | Parenteral (IPV), Oral drops (OPV) |
| ATC code | |
| Legal status | |
| Legal status |
|
Two polio vaccines are used throughout the world to combat poliomyelitis (or polio). The first was developed by Jonas Salk and first tested in 1952. Announced to the world by Salk on April 12, 1955, it consists of an injected dose of inactivated (dead) poliovirus. An oral vaccine was developed by Albert Sabin using attenuated poliovirus. Human trials of Sabin's vaccine began in 1957 and it was licensed in 1962.[1] Because there is no long term carrier state for poliovirus in immunocompetent individuals, polioviruses have no non-primate reservoir in nature, and survival of the virus in the environment for an extended period of time appears to be remote. Therefore, interruption of person to person transmission of the virus by vaccination is the critical step in global polio eradication.[2] The two vaccines have eradicated polio from most countries in the world,[3][4] and reduced the worldwide incidence from an estimated 350,000 cases in 1988 to 1,652 cases in 2007.[5][6][7]
Development
In the generic sense, vaccination works by priming the immune system with an 'immunogen'. Stimulating immune response, via use of an infectious agent, is known as immunization. The development of immunity to polio efficiently blocks person-to-person transmission of wild poliovirus, thereby protecting both individual vaccine recipients and the wider community.[2]
In 1936, Maurice Brodie, a research assistant at New York University, attempted to produce a formaldehyde-killed polio vaccine from ground-up monkey spinal cords. His initial attempts were hampered by the difficulty of obtaining enough virus. Brodie first tested the vaccine on himself and several of his assistants. He then gave the vaccine to three thousand children, many of whom developed allergic reactions, but none developed immunity to polio.[8] Philadelphia pathologist John Kolmer also claimed to have developed a vaccine that same year, but it too produced no immunity and was blamed for causing a number of cases, some of them fatal.[9]

A breakthrough came in 1948 when a research group headed by John Enders at the Children's Hospital Boston successfully cultivated the poliovirus in human tissue in the laboratory.[10] This development greatly facilitated vaccine research and ultimately allowed for the development of vaccines against polio. Enders and his colleagues, Thomas H. Weller and Frederick C. Robbins, were recognized in 1954 for their labors with a Nobel Prize in Physiology or Medicine.[11] Other important advances that led to the development of polio vaccines were: the identification of three poliovirus serotypes (Poliovirus type 1 — PV1, or Mahoney; PV2, Lansing; and PV3, Leon); the finding that prior to paralysis, the virus must be present in the blood; and the demonstration that administration of antibodies in the form of gamma-globulin protects against paralytic polio.[6][12]
In 1952 and 1953, the U.S. experienced an outbreak of 58,000 and 35,000 polio cases, respectively, up from a typical number of some 20,000 a year. Amid this U.S. polio epidemic, millions of dollars were invested in finding and marketing a polio vaccine by commercial interests, including Lederle Laboratories in New York under the direction of H. R. Cox. Also working at Lederle was Polish-born virologist and immunologist Hilary Koprowski, who claims to have created the first successful polio vaccine, in 1950. His vaccine, however, being a live attenuated virus taken orally, was still in the research stage and would not be ready for use until five years after Jonas Salk's polio vaccine (a dead injectable vaccine) had reached the market. Koprowski's attenuated vaccine was prepared by successive passages through the brains of Swiss albino mice. By the seventh passage, the vaccine strains could no longer infect nervous tissue or cause paralysis. After one to three further passages on rats, the vaccine was deemed safe for human use.[13][14] On February 27, 1950, Koprowski's live, attenuated vaccine was tested for the first time on an eight year old boy from Letchworth Village, New York. The boy suffered no side effects and Koprowski enlarged his experiment to include 19 other children.[15][13]
The development of two polio vaccines led to the first modern mass inoculations. The last cases of paralytic poliomyelitis caused by endemic transmission of wild virus in the United States occurred in 1979, with an outbreak among the Amish in several Midwest states.[16] A global effort to eradicate polio, led by the World Health Organization, UNICEF, and The Rotary Foundation, began in 1988 and has relied largely on the oral polio vaccine developed by Albert Sabin.[17] The disease was entirely eradicated in the Americas by 1994.[18] Polio was officially eradicated in 36 Western Pacific countries, including China and Australia in 2000.[19][20] Europe was declared polio-free in 2002.[21] As of 2008, polio remains endemic in only four countries: Nigeria, India, Pakistan, and Afghanistan.[5] Although poliovirus transmission has been interrupted in much of the world, transmission of wild poliovirus does continue and creates an ongoing risk for the importation of wild poliovirus into previously polio-free regions. If importations of poliovirus occurs, outbreaks of poliomyelitis may develop, especially in areas with low vaccination coverage and poor sanitation. As a result, high levels of vaccination coverage must be maintained.[18]
Inactivated vaccine

The first effective polio vaccine was developed in 1952 by Jonas Salk at the University of Pittsburgh. But it needed years of testing. To encourage patience, Salk went on CBS radio to report a successful test on a small group of adults and children on March 26, 1953; two days later the results were published in JAMA.[22]
The Salk vaccine, or inactivated poliovirus vaccine (IPV), is based on three wild, virulent reference strains, Mahoney (type 1 poliovirus), MEF-1 (type 2 poliovirus), and Saukett (type 3 poliovirus), grown in a type of monkey kidney tissue culture (Vero cell line), which are then inactivated with formalin.[6] The injected Salk vaccine confers IgG-mediated immunity in the bloodstream, which prevents polio infection from progressing to viremia and protects the motor neurons, thus eliminating the risk of bulbar polio and post-polio syndrome.
In 1954, the vaccine was tested at Arsenal Elementary School and the Watson Home for Children in Pittsburgh, Pennsylvania. Salk's vaccine was then used in a test called the Francis Field Trial, led by Thomas Francis; the largest medical experiment in history. The test began with some 4,000 children at Franklin Sherman Elementary School in McLean, Virginia[23], and would eventually involve 1.8 million children, in 44 states from Maine to California.[24] By the conclusion of the study, roughly 440,000 received one or more injections of the vaccine, about 210,000 children received a placebo, consisting of harmless culture media, and 1.2 million children received no vaccination and served as a control group, who would then be observed to see if any contracted polio.[13] The results of the field trial were announced April 12, 1955 (the tenth anniversary of the death of Franklin D. Roosevelt; see Franklin D. Roosevelt's paralytic illness). The Salk vaccine had been 60 - 70% effective against PV1 (poliovirus type 1), over 90% effective against PV2 and PV3, and 94% effective against the development of bulbar polio.[25] Soon after Salk's vaccine was licensed in 1955 children's vaccination campaigns were launched. In the U.S, following a mass immunization campaign promoted by the March of Dimes, the annual number of polio cases fell to 5,600 by 1957.[26] By 1961 only 161 cases were recorded in the United States.[27]

An enhanced-potency IPV was licensed in the United States in November 1987, and is currently the vaccine of choice in the United States.[16] The first dose of polio vaccine is given shortly after birth, usually between 1–2 months of age, a second dose is given at 4 months of age.[16] The timing of the third dose depends on the vaccine formulation but should be given between 6–18 months of age.[28] A booster vaccination is given at 4 to 6 years of age, for a total of four doses at or before school entry.[29] In some countries, a fifth vaccination is given during adolescence.[28] Routine vaccination of adults (18 years of age and older) in developed countries is neither necessary nor recommended because most adults are already immune and have a very small risk of exposure to wild poliovirus in their home countries.[16]
In 2002, a pentavalent (5-component) combination vaccine (called Pediarix) containing IPV was approved for use in the United States. The vaccine also contains combined diphtheria, tetanus, and acellular pertussis vaccines (DTaP) and a pediatric dose of hepatitis B vaccine.[16] In the UK, IPV is combined with tetanus, diphtheria, pertussis and Haemophilus influenzae type b vaccines.[28] When the current formulation of IPV is used, 90% or more of individuals develop protective antibody to all three serotypes of poliovirus after two doses of inactivated polio vaccine (IPV), and at least 99% are immune to poliovirus following three doses. The duration of immunity induced by IPV is not known with certainty, although a complete series is thought to provide protection for many years.[30]
Oral vaccine
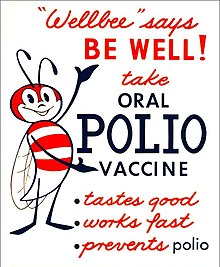
Oral polio vaccine (OPV) is a live-attenuated vaccine, produced by the passage of the virus through non-human cells at a sub-physiological temperature, which produces spontaneous mutations in the viral genome.[31] Oral polio vaccines were developed by several groups, one of which was led by Albert Sabin. Other groups, led by Hilary Koprowski and H.R. Cox, developed their own attenuated vaccine strains. In 1958, the National Institutes of Health created a special committee on live polio vaccines. The various vaccines were carefully evaluated for their ability to induce immunity to polio, while retaining a low incidence of neuropathogenicity in monkeys. Based on these results, the Sabin strains were chosen for worldwide distribution.[13]
There are 57 nucleotide substitutions which distinguish the attenuated Sabin 1 strain from its virulent parent (the Mahoney serotype), two nucleotide substitutions attenuate the Sabin 2 strain, and 10 substitutions are involved in attenuating the Sabin 3 strain.[6] The primary attenuating factor common to all three Sabin vaccines is a mutation located in the virus's internal ribosome entry site (or IRES)[32] which alters stem-loop structures, and reduces the ability of poliovirus to translate its RNA template within the host cell.[33] The attenuated poliovirus in the Sabin vaccine replicates very efficiently in the gut, the primary site of infection and replication, but is unable to replicate efficiently within nervous system tissue. OPV also proved to be superior in administration, eliminating the need for sterile syringes and making the vaccine more suitable for mass vaccination campaigns. OPV also provided longer lasting immunity than the Salk vaccine.
In 1961, type 1 and 2 monovalent oral poliovirus vaccine (MOPV) was licensed, and in 1962, type 3 MOPV was licensed. In 1963, trivalent OPV (TOPV) was licensed, and became the vaccine of choice in the United States and most other countries of the world, largely replacing the inactivated polio vaccine.[8] A second wave of mass immunizations led to a further dramatic decline in the number of polio cases. Between 1962 and 1965 about 100 million Americans (roughly 56% of the population at that time) received the Sabin vaccine. The result was a substantial reduction in the number of poliomyelitis cases, even from the much reduced levels following the introduction of the Salk vaccine.[34]
OPV is usually provided in vials containing 10-20 doses of vaccine. A single dose of oral polio vaccine (usually two drops) contains 1,000,000 infectious units of Sabin 1 (effective against PV1), 100,000 infectious units of the Sabin 2 strain, and 600,000 infectious units of Sabin 3. The vaccine contains small traces of antibiotics— neomycin and streptomycin—but does not contain preservatives.[35] One dose of OPV produces immunity to all three poliovirus serotypes in approximately 50% of recipients.[16] Three doses of live-attenuated OPV produce protective antibody to all three poliovirus types in more than 95% of recipients. OPV produces excellent immunity in the intestine, the primary site of wild poliovirus entry, which helps prevent infection with wild virus in areas where the virus is endemic.[29] The live virus used in the vaccine is shed in the stool and can be spread to others within a community, resulting in protection against poliomyelitis even in individuals who have not been directly vaccinated. IPV produces less gastrointestinal immunity than does OPV, and primarily acts by preventing the virus from entering the nervous system. In regions without wild poliovirus, inactivated polio vaccine is the vaccine of choice.[29] In regions with higher incidence of polio, and thus a different relative risk between efficacy and reversion of the vaccine to a virulent form, live vaccine is still used. The live virus also has stringent requirements for transport and storage, which are a problem in some hot or remote areas. As with other live-virus vaccines, immunity initiated by OPV is probably lifelong.[30]
Iatrogenic (vaccine-induced) polio
A major concern about the oral polio vaccine (OPV) is its known ability to revert to a form that can achieve neurological infection and cause paralysis.[36] Clinical disease, including paralysis, caused by vaccine-derived poliovirus (VDPV) is indistinguishable from that caused by wild polioviruses.[37] This is believed to be a rare event, but outbreaks of vaccine-associated paralytic poliomyelitis (VAPP) have been reported, and tend to occur in areas of low coverage by OPV, presumably because the OPV is itself protective against the related outbreak strain.[38][39]

As the incidence of wild polio diminishes, nations transition from use of the oral vaccine back to the injected vaccine because the direct risk of iatrogenic polio (VAPP) due to OPV outweighs the indirect benefit of immunization via subclinical transmission of OPV. When IPV is used, reversion is not possible but there remains a small risk of clinical infection upon exposure to reverted OPV or wild polio virus. Following the widespread use of polio vaccines in the mid-1950s, the incidence of poliomyelitis declined rapidly in many industrialized countries. The use of OPV was discontinued in the United States in 2000 and in 2004 in the UK, but it continues to be used around the globe.[16][28]
The rate of vaccine-associated paralytic poliomyelitis (VAPP) varies by region but is generally about 1 case per 750,000 vaccine recipients.[40] VAPP is more likely to occur in adults than in children. In immunodeficient children, the risk of VAPP is almost 7,000 times higher, particularly for persons with B-lymphocyte disorders (e.g., agammaglobulinemia and hypogammaglobulinemia), which reduce the synthesis of protective antibodies.[37] The World Health Organization considers the benefits of vaccination to far outweigh the risk of vaccine derived polio. Outbreaks of vaccine derived polio have been stopped by multiple rounds of high-quality vaccination, in order to immunize the entire population.[41]
Outbreaks of VAPP occurred independently in Belarus (1965–66), Canada (1966–68), Egypt (1983–1993), Hispaniola (2000–2001), Philippines (2001), Madagascar (2001–2002),[42] and in Haiti (2002), where political strife and poverty have interfered with vaccination efforts.[43] In 2006 an outbreak of vaccine-derived poliovirus occurred in China.[44] Cases have been reported from Cambodia (2005–2006), Myanmar (2006–2007), Iran (1995, 2005–2007), Syria, Kuwait and Egypt.[45] Since 2005, The World Health Organization has been tracking vaccine-caused polio in northern Nigeria caused by a mutation in live oral polio vaccines.[46]
Contamination concerns
In 1960, it was determined that the rhesus monkey kidney cells used to prepare the poliovirus vaccines were infected with the SV40 virus (Simian Virus-40).[47] SV40 was also discovered in 1960 and is a naturally occurring virus that infects monkeys. In 1961, SV40 was found to cause tumors in rodents.[48] More recently, the virus was found in certain forms of cancer in humans, for instance brain and bone tumors, mesotheliomas, and some types of non-Hodgkin's lymphoma.[49][50] However, it has not been determined that SV40 causes these cancers.[51]
SV40 was found to be present in stocks of the injected form of the polio vaccine (IPV) in use between 1955 to 1963.[47] It is not found in the OPV form.[47] Over 98 million Americans received one or more doses of polio vaccine between 1955 to 1963 when a proportion of vaccine was contaminated with SV40; it has been estimated that 10–30 million Americans may have received a dose of vaccine contaminated with SV40.[47] Later analysis suggested that vaccines produced by the former Soviet bloc countries until 1980, and used in the USSR, China, Japan, and several African countries, may have been contaminated; meaning hundreds of millions more may have been exposed to SV40.[52]
In 1998, the National Cancer Institute undertook a large study, using cancer case information from the Institutes SEER database. The published findings from the study revealed that there was no increased incidence of cancer in persons who may have received vaccine containing SV40.[53] Another large study in Sweden examined cancer rates of 700,000 individuals who had received potentially contaminated polio vaccine as late as 1957; the study again revealed no increased cancer incidence between persons who received polio vaccines containing SV40 and those who did not.[54] The question of whether SV40 causes cancer in humans remains controversial however, and the development of improved assays for detection of SV40 in human tissues will be needed to resolve the controversy.[51]
During the race to develop an oral polio vaccine several large scale human trials were undertaken. By 1958, the National Institutes of Health had determined that OPV produced using the Sabin strains were the safest.[13] Between 1957 and 1960, however, Hilary Koprowski continued to administer his vaccine around the world. In Africa, the vaccines were administered to roughly one million people in the Belgian territories, now the Democratic Republic of the Congo, Rwanda and Burundi.[55][56] The results of these human trials have been controversial,[57] and accusations in the 1990s arose that the vaccine had created the conditions necessary for transmission of SIV from chimpanzees to humans, causing HIV/AIDS. These hypotheses have, however, been refuted.[55] By 2004, cases of poliomyelitis in Africa had been reduced to just a small number of isolated regions in the western portion of the continent, with sporadic cases elsewhere. However, recent opposition to vaccination campaigns has evolved,[58][59] often relating to fears that the vaccine might induce sterility.[60] The disease has since resurged in Nigeria and in several other African nations, which epidemiologists believe is due to refusals by certain local populations to allow their children to receive the polio vaccine.[61]
References
- ^ "A Science Odyssey: People and Discoveries". PBS. 1998. Retrieved 2008-11-29.
- ^ a b Fine P, Carneiro I (15 November 1999). "Transmissibility and persistence of oral polio vaccine viruses: implications for the global poliomyelitis eradication initiative". Am J Epidemiol. 150 (10): 1001–21. PMID 10568615.
- ^ Aylward RB (2006). "Eradicating polio: today's challenges and tomorrow's legacy". Annals of Tropical Medicine and Parasitology. 100 (5–6): 401–13. doi:10.1179/136485906X97354. PMID 16899145. Retrieved 2009-01-02.
- ^ Schonberger L, Kaplan J, Kim-Farley R, Moore M, Eddins D, Hatch M (1984). "Control of paralytic poliomyelitis in the United States". Rev. Infect. Dis. 6 Suppl 2: S424–6. PMID 6740085.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ a b Centers for Disease Control and Prevention (CDC) (2006). "Update on vaccine-derived polioviruses". MMWR Morb. Mortal. Wkly. Rep. 55 (40): 1093–7. PMID 17035927.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ a b c d Kew O, Sutter R, de Gourville E, Dowdle W, Pallansch M (2005). "Vaccine-derived polioviruses and the endgame strategy for global polio eradication". Annu Rev Microbiol. 59: 587–635. doi:10.1146/annurev.micro.58.030603.123625. PMID 16153180.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ "Wild Poliovirus Weekly Update". Global Polio Eradication Initiative. 2008-11-25. Archived from the original on 2008-06-16. Retrieved 2008-11-29.
- ^ a b Pearce J (2004). "Salk and Sabin: poliomyelitis immunisation". J Neurol Neurosurg Psychiatry. 75 (11): 1552. doi:10.1136/jnnp.2003.028530. PMC 1738787. PMID 15489385.
- ^ Rainsberger M (2005-06-27). "More than a March of Dimes". The University of Texas at Austin. Retrieved 2008-11-29.
- ^ Enders JF, Weller TH, Robbins FC (1949). "Cultivation of the Lansing Strain of Poliomyelitis Virus in Cultures of Various Human Embryonic Tissues". Science (journal). 109 (2822): 85–87. doi:10.1126/science.109.2822.85. PMID 17794160.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ "The Nobel Prize in Physiology or Medicine 1954". The Nobel Foundation. Retrieved 2008-11-29.
- ^ Hammon W, Coriell L, Wehrle P, Stokes J (1953). "Evaluation of Red Cross gamma globulin as a prophylactic agent for poliomyelitis. IV. Final report of results based on clinical diagnoses". J Am Med Assoc. 151 (15): 1272–85. PMID 13034471.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ a b c d e "Competition to develop an oral vaccine". Conquering Polio. Sanofi Pasteur SA. 2007-02-02. Archived from the original on 2007-10-16.
{{cite web}}:|archive-date=/|archive-url=timestamp mismatch; 2007-10-07 suggested (help) - ^ "Public Health Weekly Reports for OCTOBER 10, 1947". Public Health Rep. 62 (41): 1467–1498. 1947. PMC 1995293. PMID 19316151.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Koprowski, Hilary (15 October 2010). "Interview with Hilary Koprowski, sourced at History of Vaccines website". College of Physicians of Philadelphia. Retrieved 15 October 2010.
- ^ a b c d e f g Atkinson W, Hamborsky J, McIntyre L, Wolfe S, eds. (2008). Epidemiology and Prevention of Vaccine-Preventable Diseases (The Pink Book) (PDF) (10th ed. (2nd printing) ed.). Washington, D.C.: Public Health Foundation. Retrieved 2008-11-29.
{{cite book}}:|author=has generic name (help)CS1 maint: multiple names: authors list (link) - ^ Mastny, Lisa (1999-01-25). "Eradicating Polio: A Model for International Cooperation". Worldwatch Institute. Retrieved 2008-11-29.
- ^ a b Centers for Disease Control and Prevention (CDC) (1994). "International Notes Certification of Poliomyelitis Eradication – the Americas, 1994". Morbidity and Mortality Weekly Report. 43 (39). Centers for Disease Control and Prevention: 720–722. PMID 7522302.
- ^ , (2001). "General News. Major Milestone reached in Global Polio Eradication: Western Pacific Region is certified Polio-Free" (PDF). Health Educ Res. 16 (1): 109. doi:10.1093/her/16.1.109.
{{cite journal}}:|author=has numeric name (help)CS1 maint: extra punctuation (link) - ^ D'Souza R, Kennett M, Watson C (2002). "Australia declared polio free". Commun Dis Intell. 26 (2): 253–60. PMID 12206379.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ "Europe achieves historic milestone as Region is declared polio-free" (Press release). European Region of the World Health Organization. 2002-06-21. Retrieved 2008-08-23.
- ^ Offit, Paul A. (2007). The Cutter Incident: How America's First Polio Vaccine Led to the Growing Vaccine Crisis. Yale University Press. p. 38. ISBN 0300126050.
- ^ David Oshinsky "Miracle Workers," American Heritage, Winter 2010.
- ^ "Polio Victory Remembered as March of Dimes Marks 50th Anniversary of Salk Vaccine Field Trials". News Desk. 2004-04-26. Retrieved 2008-11-29.
- ^ Smith, Jane S. (1990). Patenting the Sun: Polio and the Salk Vaccine. William Morrow & Co. ISBN 0-688-09494-5.
- ^ Sorem A, Sass EJ, Gottfried G (1996). Polio's legacy: an oral history. Washington, D.C: University Press of America. ISBN 0-7618-0144-8.
{{cite book}}: CS1 maint: multiple names: authors list (link) - ^ Hinman A (1984). "Landmark perspective: Mass vaccination against polio". JAMA. 251 (22): 2994–6. doi:10.1001/jama.251.22.2994. PMID 6371280.
- ^ a b c d Joint Committee on Vaccination and Immunisation, David Salisbury (Editor), Mary Ramsay (Editor), Karen Noakes (Editor) (2006). "26: Poliomyelitis". Immunisation Against Infectious Disease (PDF). Edinburgh: Stationery Office. pp. 313–29. ISBN 0-11-322528-8.
{{cite book}}:|author=has generic name (help)CS1 maint: multiple names: authors list (link) - ^ a b c "Poliomyelitis prevention: recommendations for use of inactivated poliovirus vaccine and live oral poliovirus vaccine. American Academy of Pediatrics Committee on Infectious Diseases". Pediatrics. 99 (2): 300–5. 1997. doi:10.1542/peds.99.2.300. PMID 9024465.
- ^ a b Robertson, Susan. "Module 6: Poliomyelitis" (PDF). The Immunological Basis for Immunization Series. World Health Organization (Geneva, Switzerland). Retrieved 2008-11-29.
- ^ Sabin A, Ramos-Alvarez M, Alvarez-Amezquita J; et al. (1960). "Live, orally given poliovirus vaccine. Effects of rapid mass immunization on population under conditions of massive enteric infection with other viruses". JAMA. 173: 1521–6. PMID 14440553.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Ochs K, Zeller A, Saleh L; et al. (2003). "Impaired binding of standard initiation factors mediates poliovirus translation attenuation". J. Virol. 77 (1): 115–22. doi:10.1128/JVI.77.1.115-122.2003. PMC 140626. PMID 12477816.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Gromeier M, Bossert B, Arita M, Nomoto A, Wimmer E (1999). "Dual stem loops within the poliovirus internal ribosomal entry site control neurovirulence". J. Virol. 73 (2): 958–64. PMC 103915. PMID 9882296.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Smallman-Raynor, Matthew (2006). Poliomyelitis: A World Geography: Emergence to Eradication. Oxford University Press, USA. ISBN 0-19-924474-X.
- ^ Poliomyelitis Eradication: Field Guide. Washington: Pan American Health Organization. 2006. ISBN 92-75-11607-5.
- ^ Shimizu H, Thorley B, Paladin FJ; et al. (2004). "Circulation of type 1 vaccine-derived poliovirus in the Philippines in 2001". J. Virol. 78 (24): 13512–21. doi:10.1128/JVI.78.24.13512-13521.2004. PMC 533948. PMID 15564462.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ a b Cono J, Alexander LN (2002). "Chapter 10: Poliomyelitis" (PDF). Vaccine-Preventable Disease Surveillance Manual (3rd ed. ed.).
{{cite web}}:|edition=has extra text (help) - ^ Kew O; et al. (2002). "Outbreak of poliomyelitis in Hispaniola associated with circulating type 1 vaccine-derived poliovirus". Science. 296 (5566): 356–9. doi:10.1126/science.1068284. PMID 11896235.
{{cite journal}}: Explicit use of et al. in:|author=(help) - ^ Yang CF, Naguib T, Yang SJ; et al. (2003). "Circulation of endemic type 2 vaccine-derived poliovirus in Egypt from 1983 to 1993". J. Virol. 77 (15): 8366–77. doi:10.1128/JVI.77.15.8366-8377.2003. PMC 165252. PMID 12857906.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Racaniello V (2006). "One hundred years of poliovirus pathogenesis". Virology. 344 (1): 9–16. doi:10.1016/j.virol.2005.09.015. PMID 16364730.
- ^ "What is vaccine-derived polio?". WHO. 2007-10-08. Retrieved 2008-11-29.
- ^ Kew O, Wright P, Agol V; et al. (2004). "Circulating vaccine-derived polioviruses: current state of knowledge". Bull World Health Organ. 82 (1): 16–23. PMC 2585883. PMID 15106296.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Fox, Maggie (2002-03-15). "Polio in Haiti linked to incomplete vaccinations: Virus can mutate and kill". National Post (Canada). Archived from the original on 2002-06-03. Retrieved 2008-11-29.
- ^ Liang X, Zhang Y, Xu W; et al. (2006). "An outbreak of poliomyelitis caused by type 1 vaccine-derived poliovirus in China". J Infect Dis. 194 (5): 545–51. doi:10.1086/506359. PMID 16897650.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Centers for Disease Control and Prevention (CDC) (2007). "Update on vaccine-derived polioviruses--worldwide, January 2006-August 2007". MMWR Morb. Mortal. Wkly. Rep. 56 (38): 996–1001. PMID 17898693.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ "Mutant polio virus spreads in Nigeria". CBS News. August 14, 2009. Retrieved 2009-08-16.
- ^ a b c d "Simian Virus 40 (SV40), Polio Vaccine, and Cancer". Vaccine Safety. Centers for Disease Control. 2004-04-22. Retrieved 2008-11-29. [dead link]
- ^ Eddy B, Borman G, Berkeley W, Young R (1961). "Tumors induced in hamsters by injection of rhesus monkey kidney cell extracts". Proc Soc Exp Biol Med. 107: 191–7. PMID 13725644.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Carbone M (1999). "Simian virus 40 and human tumors: It is time to study mechanisms". J Cell Biochem. 76 (2): 189–93. doi:10.1002/(SICI)1097-4644(20000201)76:2<189::AID-JCB3>3.0.CO;2-J. PMID 10618636.
- ^ Vilchez R, Kozinetz C, Arrington A, Madden C, Butel J (2003). "Simian virus 40 in human cancers". Am J Med. 114 (8): 675–84. doi:10.1016/S0002-9343(03)00087-1. PMID 12798456.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ a b Engels E (2005). "Cancer risk associated with receipt of vaccines contaminated with simian virus 40: epidemiologic research" (PDF). Expert Rev Vaccines. 4 (2): 197–206. doi:10.1586/14760584.4.2.197. PMID 15889993.
- ^ Bookchin D (2004-07-07). "Vaccine scandal revives cancer fear". New Scientist. Archived from the original on 2004-07-20. Retrieved 2008-11-29.
- ^ Strickler H, Rosenberg P, Devesa S, Hertel J, Fraumeni J, Goedert J (1998). "Contamination of poliovirus vaccines with simian virus 40 (1955-1963) and subsequent cancer rates". JAMA. 279 (4): 292–5. doi:10.1001/jama.279.4.292. PMID 9450713.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Olin P, Giesecke J (1998). "Potential exposure to SV40 in polio vaccines used in Sweden during 1957: no impact on cancer incidence rates 1960 to 1993". Dev Biol Stand. 94: 227–33. PMID 9776244.
- ^ a b Plotkin SA (2001). "CHAT oral polio vaccine was not the source of human immunodeficiency virus type 1 group M for humans". Clin. Infect. Dis. 32 (7): 1068–84. doi:10.1086/319612. PMID 11264036.
- ^ Koprowski H (1960). "Historical aspects of the development of live virus vaccine in poliomyelitis". Br Med J. 2 (5192): 85–91. doi:10.1136/bmj.2.5192.85. PMC 2096806. PMID 14410975.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Collins, Huntly (2000-11-06). "The Gulp Heard Round the World". Philadelphia Inquirer. pp. Section D, page 1. Archived from the original on 2004-04-05. Retrieved 2008-11-29.
- ^ "Nigeria Muslims oppose polio vaccination". Africa. BBC News. 2002-06-27. Retrieved 2008-11-29.
- ^ Dugger CW, McNeil DG (2006-03-20). "Rumor, Fear and Fatigue Hinder Final Push to End Polio". New York Times. Retrieved 2008-11-29.
- ^ "Anti-polio vaccine Malians jailed". Africa. BBC News. 2005-05-12. Retrieved 2008-11-29.
- ^ Jegede AS (2007). "What led to the Nigerian boycott of the polio vaccination campaign?". PLoS Med. 4 (3): e73. doi:10.1371/journal.pmed.0040073. PMC 1831725. PMID 17388657.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: unflagged free DOI (link)
External links
- History of Vaccines Website – History of Polio History of Vaccines, a project of the College of Physicians of Philadelphia
- CGDev.org - 'Vaccines for Development', Center for Global Development
- PBS.org - 'People and Discoveries: Salk Produces Polio Vaccine 1952', PBS
- Carlsen W (2001-07-15). "Rogue virus in the vaccine: Early polio vaccine harbored virus now feared to cause cancer in humans". San Francisco Chronicle. Retrieved 2008-11-29.
- Documents regarding Jonas Salk and the Salk Polio Vaccine, Dwight D. Eisenhower Presidential Library
- Conquering Polio, Smithsonian Magazine, April 2005
