Fingolimod: Difference between revisions
removed Category:Alcohols; added Category:Diols using HotCat |
In Canada since April 1, 2011 |
||
| Line 57: | Line 57: | ||
|title=The immunosuppressant drug FTY720 inhibits cytosolic phospholipase A2 independently of sphingosine-1-phosphate receptors. |journal=Blood |volume=109 |pages=1077–85 |year=2007 |pmid=17008548 |doi=10.1182/blood-2006-03-011437 |issue=3 |pmc=1785128 }}</ref> and a [[ceramide synthase]] inhibitor.<ref>{{Cite journal|author=Berdyshev EV, Gorshkova I, Skobeleva A, Bittman R, Lu X, Dudek SM, Mirzapoiazova T, Garcia JG, Natarajan V. |title=FTY720 inhibits ceramide synthases and up-regulates dihydrosphingosine 1-phosphate formation in human lung endothelial cells. |journal= Journal of Biological Chemistry |volume=284 |issue=9 |pages=5467–77 |year=2009 |pmid=19119142 |doi=10.1074/jbc.M805186200 |pmc=2645812 }}</ref> |
|title=The immunosuppressant drug FTY720 inhibits cytosolic phospholipase A2 independently of sphingosine-1-phosphate receptors. |journal=Blood |volume=109 |pages=1077–85 |year=2007 |pmid=17008548 |doi=10.1182/blood-2006-03-011437 |issue=3 |pmc=1785128 }}</ref> and a [[ceramide synthase]] inhibitor.<ref>{{Cite journal|author=Berdyshev EV, Gorshkova I, Skobeleva A, Bittman R, Lu X, Dudek SM, Mirzapoiazova T, Garcia JG, Natarajan V. |title=FTY720 inhibits ceramide synthases and up-regulates dihydrosphingosine 1-phosphate formation in human lung endothelial cells. |journal= Journal of Biological Chemistry |volume=284 |issue=9 |pages=5467–77 |year=2009 |pmid=19119142 |doi=10.1074/jbc.M805186200 |pmc=2645812 }}</ref> |
||
On September 22, 2010, fingolimod became the first oral disease-modifying drug approved by the [[Food and Drug Administration]] as Gilenya<ref>http://www.drugs.com/gilenya.html</ref> to reduce relapses and delay disability progression in patients with relapsing forms of multiple sclerosis.<ref>[http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm226755.htm FDA press release on approval of Gilenya]</ref> |
On September 22, 2010, fingolimod became the first oral disease-modifying drug approved by the [[Food and Drug Administration]] as Gilenya<ref>http://www.drugs.com/gilenya.html</ref> to reduce relapses and delay disability progression in patients with relapsing forms of multiple sclerosis.<ref>[http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm226755.htm FDA press release on approval of Gilenya]</ref> It has been approved also to be used in [[Canada]] and will be available since April 1, 2011 at the pharmacies.<ref>First oral MS treatment approved for Canada http://www.vancouversun.com/health/First+oral+treatment+approved+Canada+says+drug+company/4420028/story.html</ref> |
||
==History== |
==History== |
||
Revision as of 05:01, 11 March 2011
 | |
 | |
| Clinical data | |
|---|---|
| License data |
|
| Routes of administration | Oral |
| ATC code | |
| Legal status | |
| Legal status |
|
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| ChemSpider | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| Chemical and physical data | |
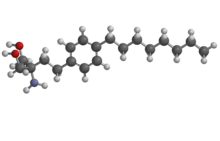
| Formula | C19H33NO2 |
| Molar mass | 307.471 g/mol g·mol−1 |
| 3D model (JSmol) | |
| |
| |
| (verify) | |
Fingolimod (rINN, codenamed FTY720) is an immunosuppressive drug. It is derived from the myriocin (ISP-1) metabolite of the fungus Isaria sinclairii. It is a structural analogue of sphingosine and gets phosphorylated by sphingosine kinases in the cell (most importantly sphingosine kinase 2).[1][2][3] The molecular biology of phospho-fingolimod is thought to lie in its activity at one of the five sphingosine-1-phosphate receptors, S1PR1.[4] It can sequester lymphocytes in lymph nodes, preventing them from moving to the central nervous system for auto-immune responses in multiple sclerosis and was originally proposed as a anti-rejection medication indicated post-transplantation. It has been reported to stimulate the repair process of glial cells and precursor cells after injury.[5] Fingolimod has also been reported to be a cannabinoid receptor antagonist,[6] a cPLA2 inhibitor [7] and a ceramide synthase inhibitor.[8]
On September 22, 2010, fingolimod became the first oral disease-modifying drug approved by the Food and Drug Administration as Gilenya[9] to reduce relapses and delay disability progression in patients with relapsing forms of multiple sclerosis.[10] It has been approved also to be used in Canada and will be available since April 1, 2011 at the pharmacies.[11]
History
First synthesized in 1992, fingolimod was derived from an immunosuppressive natural product, myriocin (ISP-I) through chemical modification. Myriocin was isolated from the culture broth a type of entomopathogenic fungi (Isaria sinclairii) that was an eternal youth nostrum in traditional Chinese medicine.[12] Showing positive results in both in vitro (mixed lymphocyte reaction) and in vivo screening (prolonging rat skin graft survival time), myriocin was modified through a series of steps to yield fingolimod, code named at the time FTY720. [13]
Structure activity relationship (SAR) studies on myriocin homologs and partially synthetic derivatives showed that the configuration at the carbon bearing the 3-hydroxy group or the 14-ketone, the 6-double bond, and the 4-hydroxy group were not important for its activity and simplification of the structure of ISP-I was done in an attempt to reduce toxicity and improve drugability [14]
Elimination of side chain functionalities and removal of chiral centers was part of the simplification process and an intermediate compound (ISP-I-28) with the carboxylic acid of myriocin transformed to a hydroxymethyl group was generated. ISP-I-28 was found to be less toxic and more effective at lenghtening rat skin allograft time than ISP-1.
Clinical trials
Organ transplant
In a previous phase III clinical trial of kidney transplantation, fingolimod was found to be no better than the existing standard of care.[15][16] The fingolimod is studied in the human models in vitro and animal kidney transplantation.[17][16][18][18]
Multiple sclerosis
In two Phase III clinical trials, fingolimod reduced the rate of relapses in relapsing-remitting multiple sclerosis by over half compared both to placebo and to the active comparator interferon beta-1a.[19]
A double-blind randomized control trial comparing fingolimod to placebo[20] found the drug reduced the annualized frequency of relapses to 0.18 relapses per year at 0.5 mg/day or 0.16 relapses per year at 1.25 mg/day, compared to 0.40 relapses per year for those patients taking the placebo. The probability of disease progression at 24 month followup was lower in the fingolimod groups compared to placebo (hazard ratio 0.70 at 0.5 mg and 0.68 at 1.25 mg). Fingolimod patients also had better results according to MRI imaging of new or enlarged lesions at 24 month followup. Side effects leading to discontinuation of the study drug were more common in the higher dose group (14.2% of patients) than at the lower dose (7.5%) or placebo (7.7%). Serious adverse events in the fingolimod group included bradycardia, relapse, and basal-cell carcinoma. Seven episodes of bradycardia occurred during the monitoring period after administration of the first dose, and were asymptomatic in six of these cases. There was a higher rate of lower respiratory tract infections (including bronchitis and pneumonia) in the fingolimod groups (9.6% at 0.5 mg, 11.4% at 1.5 mg) than the placebo group (6.0%). Other adverse events reported on the study drug included macular edema, malignant neoplasms, and laboratory abnormalities.[21]
Side effects
Fingolimod has been associated with potentially fatal infections, bradycardia, skin cancer and, recently, a case of haemorrhaging focal encephalitis, an inflammation of the brain with bleeding. Two subjects died: one due to brain herpes infection, second one due to zoster. It is unclear whether the drug was responsible for the events.[22]
The most common side effects of fingolimod have been head colds, headache, and fatigue. But there have also been a few cases of skin cancer, which has also been reported in patients taking natalizumab (Tysabri), an approved MS drug.[23]
Chemical synthesis
Several studies have described the synthesis of fingolimod and analogs.[24][25]
See also
References
- ^ Paugh SW, Payne SG, Barbour SE, Milstien S, Spiegel S (2003). "The immunosuppressant FTY720 is phosphorylated by sphingosine kinase type 2". FEBS Lett. 554 (1–2): 189–93. doi:10.1016/S0014-5793(03)01168-2. PMID 14596938.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Billich A, Bornancin F, Dévay P, Mechtcheriakova D, Urtz N, Baumruker T (2003). "Phosphorylation of the immunomodulatory drug FTY720 by sphingosine kinases". J Biol Chem. 278 (48): 47408–15. doi:10.1074/jbc.M307687200. PMID 13129923.
{{cite journal}}: CS1 maint: multiple names: authors list (link) CS1 maint: unflagged free DOI (link) Free full text - ^ Sanchez, T; Estrada-Hernandez, T; Paik, JH; Wu, MT; Venkataraman, K; Brinkmann, V; Claffey, K; Hla, T (2003). "Phosphorylation and action of the immunomodulator FTY720 inhibits vascular endothelial cell growth factor-induced vascular permeability". The Journal of biological chemistry. 278 (47): 47281–90. doi:10.1074/jbc.M306896200. PMID 12954648.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Hla T, Lee MJ, Ancellin N, Paik JH, Kluk MJ (2001). "Lysophospholipids--receptor revelations". Science. 294 (5548): 1875–8. doi:10.1126/science.1065323. PMID 11729304.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ FTY720 (Fingolimod) for Relapsing Multiple Sclerosis, Expert Review of Neurotherapeutics, Alejandro Horga; Xavier Montalban 06/04/2008; Expert Rev Neurother. 2008;8(5):699-714
- ^ Paugh SW, Cassidy MP, He H, Milstien S, Sim-Selley LJ, Spiegel S, Selley DE (2006). "Sphingosine and its analog, the immunosuppressant 2-amino-2-(2-[4-octylphenyl]ethyl)-1,3-propanediol, interact with the CB1 cannabinoid receptor". Mol Pharmacol. 70 (1): 41–50. doi:10.1124/mol.105.020552. PMID 16571654.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Payne SG, Oskeritzian CA, Griffiths R, Subramanian P, Barbour SE, Chalfant CE, Milstien S, Spiegel S. (2007). "The immunosuppressant drug FTY720 inhibits cytosolic phospholipase A2 independently of sphingosine-1-phosphate receptors". Blood. 109 (3): 1077–85. doi:10.1182/blood-2006-03-011437. PMC 1785128. PMID 17008548.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Berdyshev EV, Gorshkova I, Skobeleva A, Bittman R, Lu X, Dudek SM, Mirzapoiazova T, Garcia JG, Natarajan V. (2009). "FTY720 inhibits ceramide synthases and up-regulates dihydrosphingosine 1-phosphate formation in human lung endothelial cells". Journal of Biological Chemistry. 284 (9): 5467–77. doi:10.1074/jbc.M805186200. PMC 2645812. PMID 19119142.
{{cite journal}}: CS1 maint: multiple names: authors list (link) CS1 maint: unflagged free DOI (link) - ^ http://www.drugs.com/gilenya.html
- ^ FDA press release on approval of Gilenya
- ^ First oral MS treatment approved for Canada http://www.vancouversun.com/health/First+oral+treatment+approved+Canada+says+drug+company/4420028/story.html
- ^ Adachi, K; Chiba, K (2007). "FTY720 story. Its discovery and the following accelerated development of sphingosine 1-phosphate receptor agonists as immunomodulators based on reverse pharmacology". Perspectives in medicinal chemistry. 1: 11–23. PMC 2754916. PMID 19812733.
- ^ Fujita, T., Yoneta, M., Hirose, R., Sasaki, S., Inoue, K., Kiuchi, M., Hirase, S., Adachi, K., Arita, M. and Chiba, K. (1995). "Simple compounds,
2-alkyl-2-amino-1,3-propanediols have potent immunosuppressive activity". Bioorg. Med. Chem. Lett. 5: 847–52. doi:10.1016/0960-894X(95)00126-E.
{{cite journal}}: line feed character in|title=at position 18 (help)CS1 maint: multiple names: authors list (link) - ^ Adachi, K; Chiba, K (2007). "FTY720 story. Its discovery and the following accelerated development of sphingosine 1-phosphate receptor agonists as immunomodulators based on reverse pharmacology". Perspectives in medicinal chemistry. 1: 11–23. PMC 2754916. PMID 19812733.
- ^ Saab G, Almony A, Blinder KJ, Schuessler R, Brennan DC (2008). "Reversible cystoid macular edema secondary to fingolimod in a renal transplant recipient". Arch. Ophthalmol. 126 (1): 140–1. doi:10.1001/archophthalmol.2007.23. PMID 18195237.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ a b Westhoff TH, Schmidt S, Glander P; et al. (2007). "The impact of FTY720 (fingolimod) on vasodilatory function and arterial elasticity in renal transplant patients". Nephrol. Dial. Transplant. 22 (8): 2354–8. doi:10.1093/ndt/gfm313. PMID 17526535.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) Cite error: The named reference "pmid17526535" was defined multiple times with different content (see the help page). - ^ Zhou PJ, Wang H, Shi GH, Wang XH, Shen ZJ, Xu D (2009). "Immunomodulatory drug FTY720 induces regulatory CD4(+)CD25(+) T cells in vitro". Clin. Exp. Immunol. 157 (1): 40–7. doi:10.1111/j.1365-2249.2009.03942.x. PMC 2710591. PMID 19659769.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ a b Park SI, Felipe CR, Machado PG; et al. (2005). "Pharmacokinetic/pharmacodynamic relationships of FTY720 in kidney transplant recipients". Braz. J. Med. Biol. Res. 38 (5): 683–94. doi:/S0100-879X2005000500005. PMID 15917949.
{{cite journal}}: Check|doi=value (help); Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Jeffrey A. Cohen; et al. (2010). "Oral Fingolimod or Intramuscular Interferon for Relapsing Multiple Sclerosis". New England Journal of Medicine. 362 (5): 402–15. doi:10.1056/NEJMoa0907839. PMID 20089954.
{{cite journal}}: Explicit use of et al. in:|author=(help) - ^ Efficacy and Safety of Fingolimod in Patients With Relapsing-Remitting Multiple Sclerosis. ClinicalTrials.gov
- ^ Kappos L, Radue E-W, O'Connor P, Polman C, Hohlfield R, Calabresi P, Selmaj K, Agoropoulou C, Leyk M, Zhang-Auberson L, Burtin P for the FREEDOMS Study Group (2010). "A placebo-controlled trial of oral fingolimod in relapsing multiple sclerosis". New England Journal of Medicine. 362 (5): epub ahead of print. doi:10.1056/NEJMoa0909494. PMID 20089952.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ http://www.msrc.co.uk/index.cfm/fuseaction/show/pageid/1309
- ^ http://www.webmd.com/multiple-sclerosis/news/20080416/good-news-for-oral-ms-drug-fingolimod
- ^ Kiuchi, M; Adachi, K; Kohara, T; Teshima, K; Masubuchi, Y; Mishina, T; Fujita, T (1998). "Synthesis and biological evaluation of 2,2-disubstituted 2-aminoethanols: analogues of FTY720". Bioorganic & medicinal chemistry letters. 8 (1): 101–6. doi:10.1016/S0960-894X(97)10188-3. PMID 9925439.
- ^ B.Sivaraman, A.Senthilmurugan, I.S.Aidhen (2007). "Weinreb Amide Based New Synthetic Equivalents for Convenient Access to Immunosuppressive Agent FTY720 and Analogues". Synlett. 2841: 2841. doi:10.1055/s-2007-990961.
{{cite journal}}: CS1 maint: multiple names: authors list (link)
