Sirolimus: Difference between revisions
→Lifespan extension in mice: explanation of WHY not to use this if you are healthy that regular people can understand easily. |
→Coronary stent coating: Minor update |
||
| Line 79: | Line 79: | ||
===Coronary stent coating=== |
===Coronary stent coating=== |
||
The antiproliferative effect of sirolimus has also been used in conjunction with [[coronary stent]]s to prevent restenosis in coronary arteries following balloon angioplasty. The sirolimus is formulated in a polymer coating that affords controlled release through the healing period following coronary intervention. Several large clinical studies have demonstrated lower restenosis rates in patients treated with sirolimus-eluting stents when compared to bare metal stents, resulting in fewer repeat procedures. A sirolimus-eluting coronary stent is marketed by Cordis, a division of [[Johnson & Johnson]], under the tradename [[Cypher stent|Cypher]].<ref>{{cite web|url=http://www.cypherusa.com/ |title=Cypher Sirolimus-eluting Coronary Stent |accessdate=2008-04-01 |publisher=[[Cypher Stent]] }}</ref> It has been proposed, however, that such stents may increase the risk of vascular thrombosis.<ref name="Shuchman">{{cite journal | author = Shuchman M | title = Trading restenosis for thrombosis? New questions about drug-eluting stents | journal = [[New England Journal of Medicine|N Engl J Med]] | volume = 355 | issue = 19 | pages = 1949–52 | year = 2006 | pmid = 17093244 | doi = 10.1056/NEJMp068234}}</ref> |
The antiproliferative effect of sirolimus has also been used in conjunction with [[coronary stent]]s to prevent restenosis in coronary arteries following balloon angioplasty. The sirolimus is formulated in a polymer coating that affords controlled release through the healing period following coronary intervention. Several large clinical studies have demonstrated lower restenosis rates in patients treated with sirolimus-eluting stents when compared to bare metal stents, resulting in fewer repeat procedures. A sirolimus-eluting coronary stent is marketed by [[Cordis (medical) | Cordis]], a division of [[Johnson & Johnson]], under the tradename [[Cypher stent|Cypher]].<ref>{{cite web|url=http://www.cypherusa.com/ |title=Cypher Sirolimus-eluting Coronary Stent |accessdate=2008-04-01 |publisher=[[Cypher Stent]] }}</ref> It has been proposed, however, that such stents may increase the risk of vascular thrombosis.<ref name="Shuchman">{{cite journal | author = Shuchman M | title = Trading restenosis for thrombosis? New questions about drug-eluting stents | journal = [[New England Journal of Medicine|N Engl J Med]] | volume = 355 | issue = 19 | pages = 1949–52 | year = 2006 | pmid = 17093244 | doi = 10.1056/NEJMp068234}}</ref> |
||
==Adverse effects== |
==Adverse effects== |
||
Revision as of 06:06, 23 March 2012
 | |
 | |
| Clinical data | |
|---|---|
| License data | |
| Pregnancy category |
|
| Routes of administration | Oral |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | 20%, less after eating food rich in fat |
| Protein binding | 92% |
| Metabolism | Hepatic |
| Elimination half-life | 57–63 hours |
| Excretion | Mostly faecal |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.107.147 |
| Chemical and physical data | |
| Formula | C51H79NO13 |
| Molar mass | 914.172 g/mol g·mol−1 |
| 3D model (JSmol) | |
| |
| |
| | |
Sirolimus (INN/USAN), also known as rapamycin, is an immunosuppressant drug used to prevent rejection in organ transplantation; it is especially useful in kidney transplants. It prevents activation of T cells and B-cells by inhibiting their response to interleukin-2 (IL-2).
A macrolide, sirolimus was first discovered as a product of the bacterium Streptomyces hygroscopicus in a soil sample from Easter Island[2] — an island also known as Rapa Nui, hence the name.[3] It was approved by the FDA in September 1999 and is marketed under the trade name Rapamune by Pfizer (formerly by Wyeth).
Sirolimus was originally developed as an antifungal agent. However, this use was abandoned when it was discovered to have potent immunosuppressive and antiproliferative properties. It has since been shown to prolong the life of mice and might also be useful in the treatment of certain cancers.
Mechanism of action
Unlike the similarly named tacrolimus, sirolimus is not a calcineurin inhibitor, but it has a similar suppressive effect on the immune system. Sirolimus inhibits the response to interleukin-2 (IL-2), and thereby blocks activation of T- and B-cells. In contrast, tacrolimus inhibits the secretion of IL-2.
The mode of action of sirolimus is to bind the cytosolic protein FK-binding protein 12 (FKBP12) in a manner similar to tacrolimus. Unlike the tacrolimus-FKBP12 complex which inhibits calcineurin (PP2B), though, the sirolimus-FKBP12 complex inhibits the mammalian target of rapamycin (mTOR) pathway by directly binding the mTOR Complex1 (mTORC1).
mTOR, which stands for "mammalian Target Of Rapamycin", has also been called FRAP (FKBP-rapamycin associated protein), RAFT (rapamycin and FKBP target), RAPT1, or SEP. The earlier names FRAP and RAFT were coined to reflect the fact that rapamycin must bind FKBP12 first, and only the FKBP12-rapamycin complex can bind mTOR. However, mTOR is now the widely accepted name, since Tor was first discovered via genetic and molecular studies of rapamycin-resistant mutants of Saccharomyces cerevisiae that identified FKBP12, Tor1, and Tor2 as the targets of rapamycin and provided robust support that the FKBP12-rapamycin complex binds to and inhibits Tor1 and Tor2.
Clinical uses
Prevention of transplant rejection
The chief advantage sirolimus has over calcineurin inhibitors is its low toxicity towards kidneys. Transplant patients maintained on calcineurin inhibitors long-term tend to develop impaired kidney function or even chronic renal failure; this can be avoided by using sirolimus instead. It is particularly advantageous in patients with kidney transplants for hemolytic-uremic syndrome, as this disease is likely to recur in the transplanted kidney if a calcineurin-inhibitor is used. However, on October 7, 2008, the FDA approved safety labeling revisions for sirolimus to warn of the risk for decreased renal function associated with its use.
Sirolimus can also be used alone, or in conjunction with calcineurin inhibitors, such as tacrolimus and/or mycophenolate mofetil, to provide steroid-free immunosuppression regimens. Impaired wound healing and thrombocytopenia are a possible side effects of sirolimus; therefore, some transplant centres prefer not to use it immediately after the transplant operation, but instead administer it only after a period of weeks or months. Its optimal role in immunosuppression has not yet been determined, and is the subject of a number of ongoing clinical trials.
Sirolimus is absorbed into the blood stream from the intestine variably in each patient, with some patients having up to eight times more exposure than others for the same dose. Drug levels are therefore taken to make sure patients get the right dose for their condition. This is determined by taking a blood sample before the next dose which gives the trough level. Fortunately, there is good correlation between trough concentration levels and drug exposure, known as area under the concentration-time curve, for both sirolimus (SRL) and tacrolimus (TAC) (SRL: r2 = 0.83; TAC: r2 = 0.82), so only one level need be taken to know its pharmacokinetic (PK) profile. PK profiles of SRL and of TAC are unaltered by simultaneous administration. Dose-corrected drug exposure of TAC correlates with SRL (r2 = 0.8), so patients have similar bioavailability of both.[4]
Coronary stent coating
The antiproliferative effect of sirolimus has also been used in conjunction with coronary stents to prevent restenosis in coronary arteries following balloon angioplasty. The sirolimus is formulated in a polymer coating that affords controlled release through the healing period following coronary intervention. Several large clinical studies have demonstrated lower restenosis rates in patients treated with sirolimus-eluting stents when compared to bare metal stents, resulting in fewer repeat procedures. A sirolimus-eluting coronary stent is marketed by Cordis, a division of Johnson & Johnson, under the tradename Cypher.[5] It has been proposed, however, that such stents may increase the risk of vascular thrombosis.[6]
Adverse effects
Lung toxicity
Lung toxicity is a serious complication associated with sirolimus therapy,[7][8][9][10][11][12][13] especially in the case of lung transplants.[14] The mechanism of the interstitial pneumonitis caused by sirolimus and other macrolide MTOR inhibitors is unclear, and may have nothing to do with the MTOR pathway.[15][16][17] The interstitial pneumonitis is not dose dependent, but is more common in patients with underlying lung disease.[18][19]
Cancer risk
As with all immunosuppressive medications, rapamycin decreases the body's inherent anticancer activity and allows some cancers which would have been naturally destroyed to proliferate. Patients on immunosuppressive medications have a 10- to 100-fold increased risk of cancer compared to the general population.[citation needed] Furthermore, people who currently have or have already been treated for cancer have a higher rate of tumor progression and recurrence than patients with an intact immune system [citation needed]. These general considerations counsel caution when exploring the potential of rapamycin to combat cancer which is suggested by experiment. Rapamycin seems to lower the cancer risk in some transplant patients.[20]
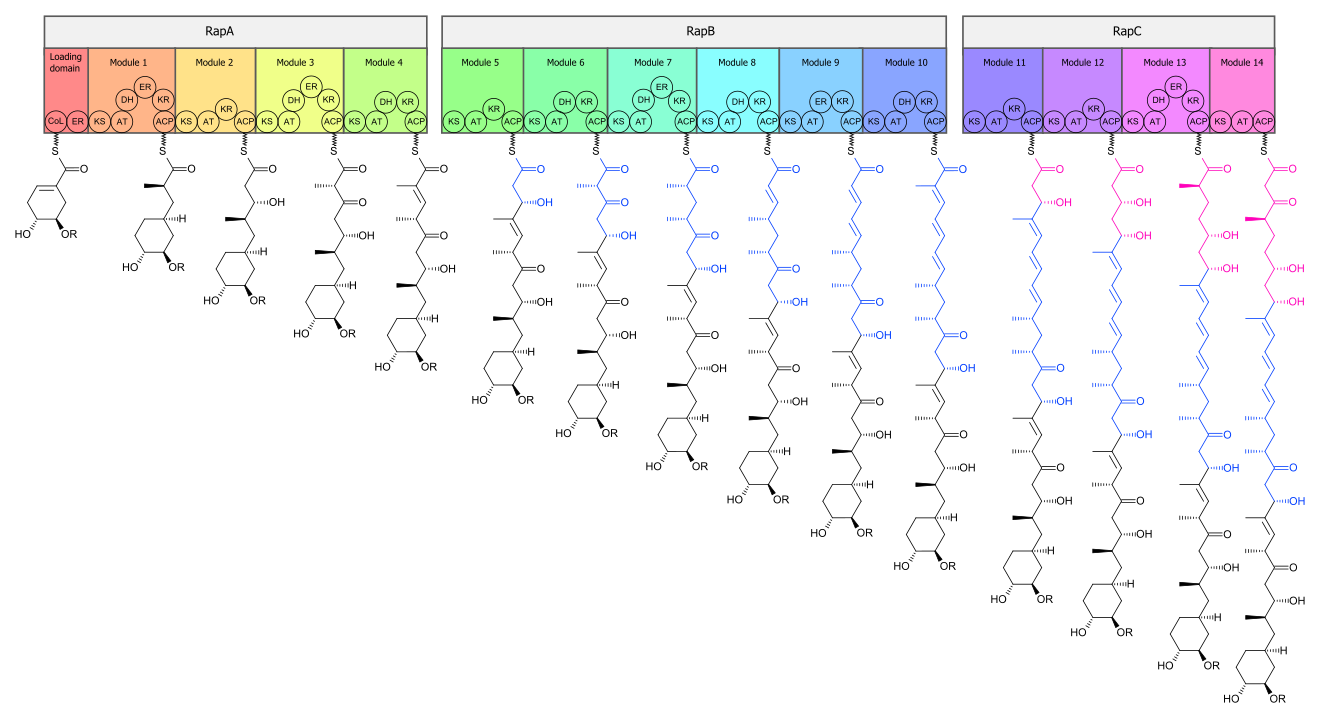
Biosynthesis
The biosynthesis of the rapamycin core is accomplished by a type I polyketide synthase (PKS) in conjunction with a nonribosomal peptide synthetase (NRPS). The domains responsible for the biosynthesis of the linear polyketide of rapamycin are organized into three multienzymes, RapA, RapB and RapC, which contain a total of 14 modules (figure 1). The three multienzymes are organized such that the first four modules of polyketide chain elongation are in RapA, the following six modules for continued elongation are in RapB, and the final four modules to complete the biosynthesis of the linear polyketide are in RapC.[21] Then, the linear polyketide is modified by the NRPS, RapP, which attaches L-pipecolate to the terminal end of the polyketide, and then cyclizes the molecule, yielding the unbound product, prerapamycin.[22]
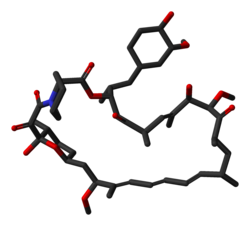
The core macrocycle, prerapamycin (figure 2) is then modified (figure 3) by an additional five enzymes, which lead to the final product, rapamycin. First, the core macrocycle is modified by RapI, SAM-dependant O-methyltransferase (MTase), which O-methylates at C39. Next, a carbonyl is installed at C9 by RapJ, a cytochrome P-450 monooxygenases (P-450). Then, RapM, another MTase, O-methylates at C16. Finally, RapN, another P-450 installs a hydroxyl at C27 immediately followed by O-methylation by Rap Q, a distinct MTase, at C27 to yield rapamycin.[23]
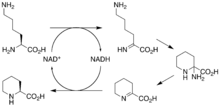
The biosynthetic genes responsible for rapamycin synthesis have been identified. As expected, three extremely large open reading frames (ORF's) designated as rapA, rapB and rapC encode for three extremely large and complex multienzymes, RapA, RapB, and RapC respectively.[21] The gene rapL has been established to code for a NAD+-dependant lysine cycloamidase, which converts L-lysine to L-pipecolic acid (figure 4) for incorporation at the end of the polyketide.[24][25] A gene rapP, which is embedded between the PKS genes and translationally coupled to rapC encodes for an additional enzyme, an NPRS responsible for incorporating L-pipecolic acid, chain termination and cyclization of prerapamycin. Additionally, genes rapI, rapJ, rapM, rapN, rapO, and rapQ have been identified as coding for tailoring enzymes which modify the macrocyclic core to give rapamycin (figure 3). Finally, rapG and rapH have been identified to code for enzymes which have a positive regulatory role in the preparation of rapamycin through the control of rapamycin PKS gene expression.[26] Biosynthesis of this 31-membered macrocycle begins as the loading domain is primed with the starter unit, 4,5-dihydroxocyclohex-1-ene-carboxylic acid, which is derived from the shikimate pathway.[21] Interestingly, the cyclohexane ring of the starting unit is reduced during the transfer to module 1. The starting unit is then modified by a series of Claisen condensations with malonyl or methylmalonyl substrates, which are attached to an acyl carrier protein (ACP) and extend the polyketide by two carbons each. After each successive condensation, the growing polyketide is further modified according to enzymatic domains which are present to reduce and dehydrate it, thereby introducing the diversity of functionalities observed in rapamycin (figure 1). Once the linear polyketide is complete, L-pipecolic acid, which is synthesized by a lysine cycloamidase from an L-lysine, is added to the terminal end of the polyketide by an NRPS. Then, the NSPS cyclizes the polyketide, giving prerapamycin, the first enzyme-free product. The macrocyclic core is then customized by a series of post-PKS enzymes through methylations by MTases and oxidations by P-450s to yield rapamycin.
Research

Cancer
The antiproliferative effects of sirolimus may have a role in treating cancer. Sirolimus was shown to inhibit the progression of dermal Kaposi's sarcoma in patients with renal transplants. Other mTOR inhibitors, such as temsirolimus (CCI-779) or everolimus (RAD001), are being tested for use in cancers such as glioblastoma multiforme and mantle cell lymphoma.
A combination therapy of doxorubicin and sirolimus has been shown to drive AKT-positive lymphomas into remission in mice. Akt signalling promotes cell survival in Akt-positive lymphomas and acts to prevent the cytotoxic effects of chemotherapy drugs, such as doxorubicin or cyclophosphamide. Sirolimus blocks Akt signalling and the cells lose their resistance to the chemotherapy. Bcl-2-positive lymphomas were completely resistant to the therapy; eIF4E expressing lymphomas are not sensitive to sirolimus.[27][28][29][30]
Tuberous sclerosis complex
Sirolimus also shows promise in treating tuberous sclerosis complex (TSC), a congenital disorder that leaves sufferers prone to benign tumor growth in the brain, heart, kidneys, skin and other organs. After several studies conclusively linked mTOR inhibitors to remission in TSC tumors, specifically subependymal giant-cell astrocytomas in children and angiomyolipomas in adults, many US doctors began prescribing sirolimus (Wyeth's Rapamune) and everolimus (Novartis's RAD001) to TSC patients off-label. Numerous clinical trials using both rapamycin analogs, involving both children and adults with TSC, are under way in the United States.[31]
Most studies thus far have noted tumors often regrew when treatment stopped. Theories that the drug ameliorates TSC symptoms such as facial angiofibromas, ADHD, and autism are a matter of current research in animal models.
Lifespan extension in mice
Rapamycin was first shown to extend lifespan in eukaryotes in 2006.[32] Powers et al. showed a dose-responsive effect of rapamycin on lifespan extension in yeast cells. Building on this and other work, in a 2009 study, the lifespans of mice fed rapamycin were increased between 28 and 38% from the beginning of treatment, or 9 to 14% in total increased maximum lifespan. Of particular note, the treatment began in mice aged 20 months, the equivalent of 60 human years. This suggests the possibility of an effective antiaging treatment for humans at an already-advanced age, as opposed to requiring a lifelong regimen beginning in youth.[33] Because it strongly suppresses the immune system, though, people taking rapamycin are more susceptible to dangerous infections. It is not known whether rapamycin will have similar lifespan-lengthening effects in humans, and study authors caution the drug should not be used by the general population for this use.[34] In layman's terms, unless a person actually does not mind living a long life in a sterile cage, it must be remembered that drugs that suppress the immune system shorten the lives of otherwise normally healthy people.
Autism in mice
In a study of sirolimus as a treatment for TSC, researchers observed a major improvement regarding retardation related to autism. The researchers discovered sirolimus regulates one of the same proteins the TSC gene does, but in different parts of the body. They decided to treat mice three to six months old (adulthood in mice lifespans); this increased the autistic mice's intellect to about that of normal mice in as little as three days.[35]
Alzheimer's in mice
Sirolimus reduced brain lesions and prevented the decline of performance in the water maze in mice with a mouse model of Alzheimer's. Because sirolimus is already approved for other indications, it should be easy to start a clinical trial to see whether it works in humans.[36]
Other afflictions
Studies in vitro in mice and in humans suggest sirolimus inhibits HIV replication through different mechanisms, including downregulation of the coreceptor CCR5[37] and the inhibition of the induction of autophagy.[38]
Additionally, sirolimus is currently being assessed as a therapeutic option for autosomal dominant polycystic kidney disease (ADPKD). Case reports indicate sirolimus can reduce kidney volume and delay the loss of renal function in patients with ADPKD.[39]
Sirolimus has also been used in preliminary research to combat progeria, a rare disorder that causes individuals to age at an exceedingly rapid pace, leading to death in the early teenage years due to causes such as heart disease or stroke.[40]
References
- ^ "FDA-sourced list of all drugs with black box warnings (Use Download Full Results and View Query links.)". nctr-crs.fda.gov. FDA. Retrieved 22 Oct 2023.
- ^ Vézina C, Kudelski A, Sehgal SN (1975). "Rapamycin (AY-22,989), a new antifungal antibiotic". J. Antibiot. 28 (10): 721\u20136. PMID 1102508.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Pritchard DI (2005). "Sourcing a chemical succession for cyclosporin from parasites and human pathogens". Drug Discovery Today. 10 (10): 688–691. doi:10.1016/S1359-6446(05)03395-7. PMID 15896681.
- ^ McAlister VC, Mahalati K, Peltekian KM, Fraser A, MacDonald AS. (2002). "A clinical pharmacokinetic study of tacrolimus and sirolimus combination immunosuppression comparing simultaneous to separated administration". Ther Drug Monit. 24 (3): 346–50. PMID 12021624.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ "Cypher Sirolimus-eluting Coronary Stent". Cypher Stent. Retrieved 2008-04-01.
- ^ Shuchman M (2006). "Trading restenosis for thrombosis? New questions about drug-eluting stents". N Engl J Med. 355 (19): 1949–52. doi:10.1056/NEJMp068234. PMID 17093244.
- ^ Chhajed PN, Dickenmann M, Bubendorf L, Mayr M, Steiger J, Tamm M. Patterns of pulmonary complications associated with sirolimus. Respiration. 2006;73(3):367-74
- ^ Morelon E, Stern M, Israël-Biet D, Correas JM, Danel C, Mamzer-Bruneel MF, Peraldi MN, Kreis H. Characteristics of sirolimus-associated interstitial pneumonitis in renal transplant patients. Transplantation. 2001 Sep 15;72(5):787-90
- ^ Filippone EJ, Carson JM, Beckford RA, Jaffe BC, Newman E, Awsare BK, Doria C, Farber JL. Sirolimus-induced pneumonitis complicated by pentamidine-induced phospholipidosis in a renal transplant recipient: a case report. Transplant Proc. 2011 Sep;43(7):2792-7
- ^ Pham PT, Pham PC, Danovitch GM; et al. (2004). "Sirolimus-associated pulmonary toxicity". Transplantation. 77 (8): 1215–20. doi:10.1097/01.TP.0000118413.92211.B6. PMID 15114088.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Mingos MA, Kane GC (2005). "Sirolimus-induced interstitial pneumonitis in a renal transplant patient" (PDF). Respir Care. 50 (12): 1659–61. PMID 16318648.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Das BB, Shoemaker L, Subramanian S, Johnsrude C, Recto M, Austin EH (2007). "Acute sirolimus pulmonary toxicity in an infant heart transplant recipient: case report and literature review". J. Heart Lung Transplant. 26 (3): 296–8. doi:10.1016/j.healun.2006.12.004. PMID 17346635.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Delgado JF, Torres J, José Ruiz-Cano M; et al. (2006). "Sirolimus-associated interstitial pneumonitis in 3 heart transplant recipients". J. Heart Lung Transplant. 25 (9): 1171–4. doi:10.1016/j.healun.2006.05.013. PMID 16962483.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ McWilliams TJ, Levvey BJ, Russell PA, Milne DG, Snell GI (2003). "Interstitial pneumonitis associated with sirolimus: a dilemma for lung transplantation". J. Heart Lung Transplant. 22 (2): 210–3. doi:10.1016/S1053-2498(02)00564-8. PMID 12581772.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Aparicio G, Calvo MB, Medina V; et al. (2009). "Comprehensive lung injury pathology induced by mTOR inhibitors". Clin Transl Oncol. 11 (8): 499–510. doi:10.1007/s12094-009-0394-y. PMID 19661024.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Paris A, Goupil F, Kernaonet E, Foulet-Rogé A, Molinier O, Gagnadoux F, Lebas FX. Drug-induced pneumonitis due to sirolimus: An interaction with atorvastatin? Rev Mal Respir. 2012 Jan;29(1):64-9.
- ^ Maroto JP, Hudes G, Dutcher JP, Logan TF, White CS, Krygowski M, Cincotta M, Shapiro M, Duran I, Berkenblit A. Drug-related pneumonitis in patients with advanced renal cell carcinoma treated with temsirolimus. J Clin Oncol. 2011 May 1;29(13):1750-6.
- ^ Chhajed PN, Dickenmann M, Bubendorf L, Mayr M, Steiger J, Tamm M. Patterns of pulmonary complications associated with sirolimus. Respiration. 2006;73(3):367-74
- ^ Errasti P, Izquierdo D, Martín P, Errasti M, Slon F, Romero A, Lavilla FJ. Pneumonitis associated with mammalian target of rapamycin inhibitors in renal transplant recipients: a single-center experience. Transplant Proc. 2010 Oct;42(8):3053-4.
- ^ Law BK (2005). "Rapamycin: an anti-cancer immunosuppressant?". Crit. Rev. Oncol. Hematol. 56 (1): 47–60. doi:10.1016/j.critrevonc.2004.09.009. PMID 16039868.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ a b c Schwecke T, Aparicio JF, Molnár I; et al. (1995). "The biosynthetic gene cluster for the polyketide immunosuppressant rapamycin". Proc. Natl. Acad. Sci. U.S.A. 92 (17): 7839–43. doi:10.1073/pnas.92.17.7839. PMC 41241. PMID 7644502.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Gregory MA, Gaisser S, Lill RE; et al. (2004). "Isolation and characterization of pre-rapamycin, the first macrocyclic intermediate in the biosynthesis of the immunosuppressant rapamycin by S. hygroscopicus". Angew. Chem. Int. Ed. Engl. 43 (19): 2551–3. doi:10.1002/anie.200453764. PMID 15127450.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Gregory MA, Hong H, Lill RE; et al. (2006). "Rapamycin biosynthesis: Elucidation of gene product function". Org. Biomol. Chem. 4 (19): 3565–8. doi:10.1039/b608813a. PMID 16990929.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Graziani EI (2009). "Recent advances in the chemistry, biosynthesis and pharmacology of rapamycin analogs". Nat Prod Rep. 26 (5): 602–9. doi:10.1039/b804602f. PMID 19387497.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ "Biosynthesis of Pipecolic Acid by RapL, a Lysine Cyclodeaminase Encoded in the Rapamycin Gene Cluster". J. Am. Chem. Soc. 128 (11): 3838–3847. 2006. doi:10.1021/ja0587603. PMID 16536560.
{{cite journal}}: Unknown parameter|authors=ignored (help) - ^ Aparicio JF, Molnár I, Schwecke T; et al. (1996). "Organization of the biosynthetic gene cluster for rapamycin in Streptomyces hygroscopicus: analysis of the enzymatic domains in the modular polyketide synthase". Gene. 169 (1): 9–16. doi:10.1016/0378-1119(95)00800-4. PMID 8635756.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Sun SY, Rosenberg LM, Wang X; et al. (2005). "Activation of Akt and eIF4E survival pathways by rapamycin-mediated mammalian target of rapamycin inhibition". Cancer Res. 65 (16): 7052–8. doi:10.1158/0008-5472.CAN-05-0917. PMID 16103051.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Chan S (2004). "Targeting the mammalian target of rapamycin (mTOR): a new approach to treating cancer". Br J Cancer. 91 (8): 1420–4. doi:10.1038/sj.bjc.6602162. PMC 2409926. PMID 15365568.
- ^ Wendel HG, De Stanchina E, Fridman JS; et al. (2004). "Survival signalling by Akt and eIF4E in oncogenesis and cancer therapy". Nature. 428 (6980): 332–7. doi:10.1038/nature02369. PMID 15029198.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|laydate=ignored (help); Unknown parameter|laysource=ignored (help); Unknown parameter|laysummary=ignored (help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Novak, Kristine (2004). "Therapeutics: Means to an end". Nature Reviews Cancer. 4 (5): 332. doi:10.1038/nrc1349.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Tuberous Sclerosis Alliance (2009). "Current Clinical Trials". Retrieved 2009-10-14.
{{cite web}}: Unknown parameter|month=ignored (help) - ^ Powers R.W.; et al. (January 15, 2006). "Extension of chronological life span in yeast by decreased TOR pathway signaling". Genes and Development. 20 (2): 174–184. doi:10.1101/gad.1381406. PMC 1356109. PMID 16418483.
{{cite journal}}: Explicit use of et al. in:|author=(help) - ^ Harrison DE, Strong R, Sharp ZD; et al. (July 8, 2009). "Rapamycin fed late in life extends lifespan in genetically heterogeneous mice". Nature. 460 (7253): 392–5. doi:10.1038/nature08221. PMC 2786175. PMID 19587680.
{{cite journal}}:|access-date=requires|url=(help); Explicit use of et al. in:|author=(help); Unknown parameter|laydate=ignored (help); Unknown parameter|laysource=ignored (help); Unknown parameter|laysummary=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Jocelyn Rice (July 8, 2009). "First Drug Shown to Extend Life Span in Mammals". Technology Review. Massachusetts Institute of Technology: 1–2. Retrieved 2009-07-09.
- ^ Ehninger D, Han S, Shilyansky C; et al. (2008). "Reversal of learning deficits in a Tsc2+/- mouse model of tuberous sclerosis". Nat. Med. 14 (8): 843–8. doi:10.1038/nm1788. PMC 2664098. PMID 18568033.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|laydate=ignored (help); Unknown parameter|laysource=ignored (help); Unknown parameter|laysummary=ignored (help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ ScienceDaily.com Report
- ^ Donia M, McCubrey JA, Bendtzen K, Nicoletti F (2010). "Potential use of rapamycin in HIV infection". Br J Clin Pharmacol. 70 (6): 784–93. doi:10.1111/j.1365-2125.2010.03735.x. PMC 3014061. PMID 21175433.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Campbell GR, Spector SA (2011). "Hormonally active vitamin D3 (1{alpha},25-dihydroxycholecalciferol) triggers autophagy in human macrophages that inhibits HIV-1 infection". J Biol Chem. doi:10.1074/jbc.M110.206110. PMID 21454634.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: unflagged free DOI (link) - ^ Peces R, Peces C, Pérez-Dueñas V; et al. (January 16, 2009). "Rapamycin reduces kidney volume and delays the loss of renal function in a patient with autosomal-dominant polycystic kidney disease". NDT Plus. 2 (2). Oxford Journals: 133–5. doi:10.1093/ndtplus/sfn210. ISSN 1753-0792.
{{cite journal}}:|access-date=requires|url=(help); Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ CNN.com Clue to kids' early aging disease found, July 1, 2011