Vaccine

A vaccine is a biological preparation that improves immunity to a particular disease. A vaccine typically contains an agent that resembles a disease-causing microorganism and is often made from weakened or killed forms of the microbe, its toxins or one of its surface proteins. The agent stimulates the body's immune system to recognize the agent as foreign, destroy it, and keep a record of it, so that the immune system can more easily recognize and destroy any of these microorganisms that it later encounters.
Vaccines can be prophylactic (example: to prevent or ameliorate the effects of a future infection by any natural or "wild" pathogen), or therapeutic (e.g., vaccines against cancer are also being investigated; see cancer vaccine).
The terms vaccine and vaccination are derived from Variolae vaccinae (smallpox of the cow), the term devised by Edward Jenner to denote cowpox. He used it in 1798 in the long title of his Inquiry into the...Variolae vaccinae...known...[as]...the Cow Pox, in which he described the protective effect of cowpox against smallpox.[1] In 1881, to honour Jenner, Louis Pasteur proposed that the terms should be extended to cover the new protective inoculations then being developed.[2]
Effectiveness
Vaccines do not guarantee complete protection from a disease.[3] Sometimes, this is because the host's immune system simply does not respond adequately or at all. This may be due to a lowered immunity in general (diabetes, steroid use, HIV infection, age) or because the host's immune system does not have a B cell capable of generating antibodies to that antigen.
Even if the host develops antibodies, the human immune system is not perfect and in any case the immune system might still not be able to defeat the infection immediately. In this case, the infection will be less severe and heal faster.
Adjuvants are typically used to boost immune response. Most often, aluminium adjuvants are used, but adjuvants like squalene are also used in some vaccines, and more vaccines with squalene and phosphate adjuvants are being tested. Larger doses are used in some cases for older people (50–75 years and up), whose immune response to a given vaccine is not as strong.[4]

The efficacy or performance of the vaccine is dependent on a number of factors:
- the disease itself (for some diseases vaccination performs better than for other diseases)
- the strain of vaccine (some vaccinations are for different strains of the disease)[6]
- whether one kept to the timetable for the vaccinations (see Vaccination schedule)
- some individuals are "non-responders" to certain vaccines, meaning that they do not generate antibodies even after being vaccinated correctly
- other factors such as ethnicity, age, or genetic predisposition.
When a vaccinated individual does develop the disease vaccinated against, the disease is likely to be milder than without vaccination.[7]
The following are important considerations in the effectiveness of a vaccination program:[citation needed]
- careful modelling to anticipate the impact that an immunization campaign will have on the epidemiology of the disease in the medium to long term
- ongoing surveillance for the relevant disease following introduction of a new vaccine
- maintaining high immunization rates, even when a disease has become rare.
In 1958, there were 763,094 cases of measles and 552 deaths in the United States.[8][9] With the help of new vaccines, the number of cases dropped to fewer than 150 per year (median of 56).[9] In early 2008, there were 64 suspected cases of measles. Fifty-four out of 64 infections were associated with importation from another country, although only 13% were actually acquired outside of the United States; 63 of these 64 individuals either had never been vaccinated against measles or were uncertain whether they had been vaccinated.[9]
Adverse effects
Adverse effects if any are generally mild.[10] The rate of side effects depends on the vaccine in question.[10] Some potential side effects include: fever, pain around the injection site, and muscle aches.[10]
Types
Vaccines are dead or inactivated organisms or purified products derived from them.
There are several types of vaccines in use.[11] These represent different strategies used to try to reduce risk of illness, while retaining the ability to induce a beneficial immune response.
Killed
Some vaccines contain killed, but previously virulent, micro-organisms that have been destroyed with chemicals, heat, radioactivity, or antibiotics. Examples are influenza, cholera, bubonic plague, polio, hepatitis A, and rabies.
Attenuated
Some vaccines contain live, attenuated microorganisms. Many of these are active viruses that have been cultivated batman under conditions that disable their virulent properties, or that use closely related but less dangerous organisms to produce a broad immune response. Although most attenuated vaccines are viral, some are bacterial in nature. Examples include the viral diseases yellow fever, measles, rubella, and mumps, and the bacterial disease typhoid. The live Mycobacterium tuberculosis vaccine developed by Calmette and Guérin is not made of a contagious strain, but contains a virulently modified strain batman called "BCG" used to elicit an immune response to the vaccine. The live attenuated vaccine-containing strain Yersinia pestis EV is used for plague immunization. Attenuated vaccines have some advantages and disadvantages. They typically provoke more durable immunological batman responses and are the preferred type for healthy adults. But they may not be safe for use in immunocompromised individuals, and may rarely mutate to a virulent form and cause disease.[12]
Toxoid
Toxoid vaccines are made from inactivated toxic compounds that cause illness rather than the micro-organism. Examples of toxoid-based vaccines include tetanus and diphtheria. Toxoid vaccines are known for their efficacy. Not all toxoids are for micro-organisms; for example, Crotalus atrox toxoid is used to vaccinate dogs against rattlesnake bites.
Subunit
Protein subunit – rather than introducing an inactivated or attenuated micro-organism to an immune system (which would constitute a "whole-agent" vaccine), a fragment of it can create an immune response. Examples include the subunit vaccine against Hepatitis B virus that is composed of only the surface proteins of the virus (previously extracted from the blood serum of chronically infected patients, but now produced by recombination of the viral genes into yeast), the virus-like particle (VLP) vaccine against human papillomavirus (HPV) that is composed of the viral major capsid protein, and the hemagglutinin and neuraminidase subunits of the influenza virus. Subunit vaccine is being used for plague immunization.
Conjugate
Conjugate – certain bacteria have polysaccharide outer coats that are poorly immunogenic. By linking these outer coats to proteins (e.g., toxins), the immune system can be led to recognize the polysaccharide as if it were a protein antigen. This approach is used in the Haemophilus influenzae type B vaccine.
Experimental

A number of innovative vaccines are also in development and in use:
- Dendritic cell vaccines combine dendritic cells with antigens in order to present the antigens to the body's white blood cells, thus stimulating an immune reaction. These vaccines have shown some positive preliminary results for treating brain tumors.[13]
- Recombinant Vector – by combining the physiology of one micro-organism and the DNA of the other, immunity can be created against diseases that have complex infection processes
- DNA vaccination – in recent years[when?] a new type of vaccine called DNA vaccination, created from an infectious agent's DNA, has been developed. It works by insertion (and expression, enhanced by the use of electroporation, triggering immune system recognition) of viral or bacterial DNA into human or animal cells. Some cells of the immune system that recognize the proteins expressed will mount an attack against these proteins and cells expressing them. Because these cells live for a very long time, if the pathogen that normally expresses these proteins is encountered at a later time, they will be attacked instantly by the immune system. One advantage of DNA vaccines is that they are very easy to produce and store. As of 2006, DNA vaccination is still experimental.
- T-cell receptor peptide vaccines are under development for several diseases using models of Valley Fever, stomatitis, and atopic dermatitis. These peptides have been shown to modulate cytokine production and improve cell mediated immunity.
- Targeting of identified bacterial proteins that are involved in complement inhibition would neutralize the key bacterial virulence mechanism.[14]
While most vaccines are created using inactivated or attenuated compounds from micro-organisms, synthetic vaccines are composed mainly or wholly of synthetic peptides, carbohydrates, or antigens.
Valence
Vaccines may be monovalent (also called univalent) or multivalent (also called polyvalent). A monovalent vaccine is designed to immunize against a single antigen or single microorganism.[15] A multivalent or polyvalent vaccine is designed to immunize against two or more strains of the same microorganism, or against two or more microorganisms.[16] The valency of a multivalent vaccine may be denoted with a Greek or Latin prefix (e.g., tetravalent or quadrivalent). In certain cases a monovalent vaccine may be preferable for rapidly developing a strong immune response.[17]
Heterotypic
Also known as Heterologous or "Jennerian" vaccines these are vaccines that are pathogens of other animals that either do not cause disease or cause mild disease in the organism being treated. The classic example is Jenner's use of cowpox to protect against smallpox. A current example is the use of BCG vaccine made from Mycobacterium bovis to protect against human tuberculosis.[18]
Developing immunity
The immune system recognizes vaccine agents as foreign, destroys them, and "remembers" them. When the virulent version of an agent is encountered, the body recognizes the protein coat on the virus, and thus is prepared to respond, by (1) neutralizing the target agent before it can enter cells, and (2) recognizing and destroying infected cells before that agent can multiply to vast numbers.
When two or more vaccines are mixed together in the same formulation, the two vaccines can interfere. This most frequently occurs with live attenuated vaccines, where one of the vaccine components is more robust than the others and suppresses the growth and immune response to the other components. This phenomenon was first noted in the trivalent Sabin polio vaccine, where the amount of serotype 2 virus in the vaccine had to be reduced to stop it from interfering with the "take" of the serotype 1 and 3 viruses in the vaccine.[19] This phenomenon has also been found to be a problem with the dengue vaccines currently being researched,[when?] where the DEN-3 serotype was found to predominate and suppress the response to DEN-1, −2 and −4 serotypes.[20]
Vaccines have contributed to the eradication of smallpox, one of the most contagious and deadly diseases known to man. Other diseases such as rubella, polio, measles, mumps, chickenpox, and typhoid are nowhere near as common as they were a hundred years ago. As long as the vast majority of people are vaccinated, it is much more difficult for an outbreak of disease to occur, let alone spread. This effect is called herd immunity. Polio, which is transmitted only between humans, is targeted by an extensive eradication campaign that has seen endemic polio restricted to only parts of four countries (Afghanistan, India, Nigeria, and Pakistan).[21] The difficulty of reaching all children as well as cultural misunderstandings, however, have caused the anticipated eradication date to be missed several times.
Schedule
- For country-specific information on vaccination policies and practices, see: Vaccination policy
In order to provide best protection, children are recommended to receive vaccinations as soon as their immune systems are sufficiently developed to respond to particular vaccines, with additional "booster" shots often required to achieve "full immunity". This has led to the development of complex vaccination schedules. In the United States, the Advisory Committee on Immunization Practices, which recommends schedule additions for the Centers for Disease Control and Prevention, recommends routine vaccination of children against:[22] hepatitis A, hepatitis B, polio, mumps, measles, rubella, diphtheria, pertussis, tetanus, HiB, chickenpox, rotavirus, influenza, meningococcal disease and pneumonia.[23] The large number of vaccines and boosters recommended (up to 24 injections by age two) has led to problems with achieving full compliance. In order to combat declining compliance rates, various notification systems have been instituted and a number of combination injections are now marketed (e.g., Pneumococcal conjugate vaccine and MMRV vaccine), which provide protection against multiple diseases.
Besides recommendations for infant vaccinations and boosters, many specific vaccines are recommended at other ages or for repeated injections throughout life—most commonly for measles, tetanus, influenza, and pneumonia. Pregnant women are often screened for continued resistance to rubella. The human papillomavirus vaccine is recommended in the U.S. (as of 2011)[24] and UK (as of 2009).[25] Vaccine recommendations for the elderly concentrate on pneumonia and influenza, which are more deadly to that group. In 2006, a vaccine was introduced against shingles, a disease caused by the chickenpox virus, which usually affects the elderly.
History

Prior to the introduction of vaccination with material from cases of cowpox (heterotypic immunisation), smallpox could be prevented by deliberate inoculation of smallpox virus, later referred to as variolation to distinguish it from smallpox vaccination. This information was brought to the West in 1721 by Lady Mary Wortley Montagu, who showed it to Hans Sloane, the King's physician.[26]
Sometime during the late 1760s whilst serving his apprenticeship as a surgeon/apothecary Edward Jenner learned of the story, common in rural areas, that dairy workers would never have the often-fatal or disfiguring disease smallpox, because they had already had cowpox, which has a very mild effect in humans. In 1796, Jenner took pus from the hand of a milkmaid with cowpox, scratched it into the arm of an 8-year-old boy, and six weeks later inoculated (variolated) the boy with smallpox, afterwards observing that he did not catch smallpox.[27][28] Jenner extended his studies and in 1798 reported that his vaccine was safe in children and adults and could be transferred from arm-to-arm reducing reliance on uncertain supplies from infected cows.[1] Since vaccination with cowpox was much safer than smallpox inoculation,[29] the latter, though still widely practised in England, was banned in 1840.[30] The second generation of vaccines was introduced in the 1880s by Louis Pasteur who developed vaccines for chicken cholera and anthrax,[2] and from the late nineteenth century vaccines were considered a matter of national prestige, and compulsory vaccination laws were passed.[27]
The twentieth century saw the introduction of several successful vaccines, including those against diphtheria, measles, mumps, and rubella. Major achievements included the development of the polio vaccine in the 1950s and the eradication of smallpox during the 1960s and 1970s. Maurice Hilleman was the most prolific of the developers of the vaccines in the twentieth century. As vaccines became more common, many people began taking them for granted. However, vaccines remain elusive for many important diseases, including herpes simplex, malaria, and HIV.[27]
Landmarks in history of vaccines
| Year | Landmark |
|---|---|
| 1000 | Chinese practicing variolation |
| 1545 | Smallpox epidemic in India |
| 1578 | Whooping cough epidemic in Paris |
| 1625 | Early smallpox in North America |
| 1633 | Colonial epidemic of smallpox in Massachusetts |
| 1661 | Kangxi Emperor gives royal support for inoculation. |
| 1676 | Thomas Sydenham documents Measles infection |
| 1676 | "The Indian Plague" in Iroquois documented by Louis de Buade de Frontenac |
| 1694 | Queen Mary II dies of smallpox on 28 December. |
| 1699 | Yellow Fever outbreak in the American Colonies. |
| 1718 | Lady Mary Montagu had her 6-year old son variolated in Constantinople by Dr. Charles Maitland |
| 1721 | Lady Mary Montagu had her 2-year old daughter variolated in England by Dr. Charles Maitland |
| 1736 | Benjamin Franklin’s 4-year-old son dies of smallpox. |
| 1740 | Friedrich Hoffmann gives first description of rubella |
| 1757 | Francis Home demonstrates infectious nature of measles |
| 1798 | Edward Jenner publishes his account of the effects of his smallpox vaccine |
| 1800 | Benjamin Waterhouse brings smallpox vaccination to United States |
| 1817 | Cholera pandemic begins |
| 1817 | Panum studies epidemiology of measles in Faroe Islands |
| 1854 | Filippo Pacini isolates Vibrio cholerae |
| 1874 | A compulsory smallpox vaccination and revaccination law goes into effect in Germany[31] |
| 1880 | Louis Pasteur develops attenuated fowl cholera vaccine |
| 1881 | Louis Pasteur's public trial of anthrax vaccine at Pouilly le Fort |
| 1881 | Louis Pasteur and George Sternberg independently discover Pneumococcus |
| 1882 | Koch isolates Mycobacterium tuberculosis |
| 1885 | Louis Pasteur successfully prevents rabies in Joseph Meister by post-exposure vaccination |
| 1888 | Institut Pasteur inaugurated on 14 November |
| 1890 | Shibasaburo Kitasato and Emil von Behring immunize guinea pigs with heat-treated diphtheria toxin |
| 1892 | Pfeiffer discovers Pfeiffer influenza bacillus |
| 1894 | First major documented polio outbreak in the United States occurs in Rutland County, Vermont |
| 1896 | Koch reports discovery of Cholera vibrio unaware of Filippo Pacini's work |
| 1898 | English Vaccination Act allows exemption from smallpox vaccination on grounds of conscience |
| 1899 | Yellow fever epidemics among Panama Canal workers, resulting in transfer of project rights from France to United States |
| 1900 | Walter Reed discovers that yellow fever is transmitted by mosquitoes after studying it in Cuba |
| 1906 | Jules Bordet and Octave Gengou isolate Bordetella pertussis |
| 1908 | Karl Landsteiner and Erwin Popper discover poliovirus |
| 1924 | BCG is introduced as live tuberculosis vaccine |
| 1935 | Max Theiler develops live attenuated 17D yellow fever vaccine |
| 1945 | Chick embryo allantoic fluid-derived influenza vaccine is developed |
| 1949 | John Enders cultivates poliovirus in tissue culture |
| 1955 | Jonas Salk's injectable inactivated polio vaccine licenced for general use |
| 1960 | Trials of Albert Sabin's oral live attenuated polio vaccine begin in USA |
| 1960–1969 | Live attenuated vaccines developed for Measles, Mumps, and Rubella |
| 1974–1984 | Polysaccharide vaccines for Meningococcus, Pneumococcus, and Hemophilus are developed |
| 1980 | World Health Organization declares global eradication of smallpox |
| 1981 | Hepatitis B vaccine is licenced |
| 1983 | Hemophilus influenzae carbohydrate-protein conjugate is developed |
| 1986 | Yeast-derived recombinant hepatitis B vaccine is licensed |
| 1994 | Polio declared eliminated from Americas |
| 2002 | Polio declared eradicated from Europe |
| 2006 | First HPV vaccine is licensed |
| 2012 | Polio declared eliminated from India |
Society and culture
Opposition to vaccination
Opposition to vaccination, from a wide array of vaccine critics, has existed since the earliest vaccination campaigns.[32] Although the benefits of preventing suffering and death from serious infectious diseases greatly outweigh the risks of rare adverse effects following immunization,[33] disputes have arisen over the morality, ethics, effectiveness, and safety of vaccination. Some vaccination critics say that vaccines are ineffective against disease[34] or that vaccine safety studies are inadequate.[34] Some religious groups do not allow vaccination,[35] and some political groups oppose mandatory vaccination on the grounds of individual liberty.[32] In response, concern has been raised that spreading unfounded information about the medical risks of vaccines increases rates of life-threatening infections, not only in the children whose parents refused vaccinations, but also in other children, perhaps too young for vaccines, who could contract infections from unvaccinated carriers (see herd immunity).[36] Some parents believe vaccinations cause autism, although the scientific consensus has rejected this idea.[37] In 2011, Andrew Wakefield, a leading proponent of one of the main controversies regarding a purported link between autism and vaccines, was found to have been financially motivated to falsify research data and was subsequently stripped of his medical license.[38]
Economics of development
One challenge in vaccine development is economic: Many of the diseases most demanding a vaccine, including HIV, malaria and tuberculosis, exist principally in poor countries. Pharmaceutical firms and biotechnology companies have little incentive to develop vaccines for these diseases, because there is little revenue potential. Even in more affluent countries, financial returns are usually minimal and the financial and other risks are great.[39]
Most vaccine development to date has relied on "push" funding by government, universities and non-profit organizations.[40] Many vaccines have been highly cost effective and beneficial for public health.[41] The number of vaccines actually administered has risen dramatically in recent decades.[42] This increase, particularly in the number of different vaccines administered to children before entry into schools may be due to government mandates and support, rather than economic incentive.[citation needed]
Patents
The filing of patents on vaccine development processes can also be viewed as an obstacle to the development of new vaccines. Because of the weak protection offered through a patent on the final product, the protection of the innovation regarding vaccines is often made through the patent of processes used on the development of new vaccines as well as the protection of secrecy.[43]
Production

Vaccine production has several stages. First, the antigen itself is generated. Viruses are grown either on primary cells such as chicken eggs (e.g., for influenza) or on continuous cell lines such as cultured human cells (e.g., for hepatitis A).[44] Bacteria are grown in bioreactors (e.g., Haemophilus influenzae type b). Likewise, a recombinant protein derived from the viruses or bacteria can be generated in yeast, bacteria, or cell cultures. After the antigen is generated, it is isolated from the cells used to generate it. A virus may need to be inactivated, possibly with no further purification required. Recombinant proteins need many operations involving ultrafiltration and column chromatography. Finally, the vaccine is formulated by adding adjuvant, stabilizers, and preservatives as needed. The adjuvant enhances the immune response of the antigen, stabilizers increase the storage life, and preservatives allow the use of multidose vials.[45] Combination vaccines are harder to develop and produce, because of potential incompatibilities and interactions among the antigens and other ingredients involved.[46]
Vaccine production techniques are evolving. Cultured mammalian cells are expected to become increasingly important, compared to conventional options such as chicken eggs, due to greater productivity and low incidence of problems with contamination. Recombination technology that produces genetically detoxified vaccine is expected to grow in popularity for the production of bacterial vaccines that use toxoids. Combination vaccines are expected to reduce the quantities of antigens they contain, and thereby decrease undesirable interactions, by using pathogen-associated molecular patterns.[46]
In 2010, India produced 60 percent of the world's vaccine worth about $900 million.[47]
Excipients
Beside the active vaccine itself, the following excipients are commonly present in vaccine preparations:[48]
- Aluminum salts or gels are added as adjuvants. Adjuvants are added to promote an earlier, more potent response, and more persistent immune response to the vaccine; they allow for a lower vaccine dosage.
- Antibiotics are added to some vaccines to prevent the growth of bacteria during production and storage of the vaccine.
- Egg protein is present in influenza and yellow fever vaccines as they are prepared using chicken eggs. Other proteins may be present.
- Formaldehyde is used to inactivate bacterial products for toxoid vaccines. Formaldehyde is also used to inactivate unwanted viruses and kill bacteria that might contaminate the vaccine during production.
- Monosodium glutamate (MSG) and 2-phenoxyethanol are used as stabilizers in a few vaccines to help the vaccine remain unchanged when the vaccine is exposed to heat, light, acidity, or humidity.
- Thimerosal is a mercury-containing preservative that is added to vials of vaccine that contain more than one dose to prevent contamination and growth of potentially harmful bacteria. Due to the controversy surrounding thimerosal it has been removed from most vaccines.
Role of preservatives
Many vaccines need preservatives to prevent serious adverse effects such as Staphylococcus infection, which in one 1928 incident killed 12 of 21 children inoculated with a diphtheria vaccine that lacked a preservative.[49] Several preservatives are available, including thiomersal, phenoxyethanol, and formaldehyde. Thiomersal is more effective against bacteria, has a better shelf-life, and improves vaccine stability, potency, and safety; but, in the U.S., the European Union, and a few other affluent countries, it is no longer used as a preservative in childhood vaccines, as a precautionary measure due to its mercury content.[50] Although controversial claims have been made that thiomersal contributes to autism, no convincing scientific evidence supports these claims.[51]
Delivery systems

There are several new delivery systems in development[when?] in the hope of making vaccines more efficient to deliver. Possible methods include liposomes and ISCOM (immune stimulating complex).[52]
The latest developments[when?] in vaccine delivery technologies have resulted in oral vaccines. A polio vaccine was developed and tested by volunteer vaccinations with no formal training; the results were positive in that the ease of the vaccines increased. With an oral vaccine, there is no risk of blood contamination. Oral vaccines are likely to be solid that have proven to be more stable and less likely to freeze;[53] this stability reduces the need for a "cold chain": the resources required to keep vaccines within a restricted temperature range from the manufacturing stage to the point of administration, which, in turn, may decrease costs of vaccines. A microneedle approach, which is still in stages of development, uses "pointed projections fabricated into arrays that can create vaccine delivery pathways through the skin".[54]
A nanopatch is a needle-free vaccine delivery system that is under development. A stamp-size patch similar to an adhesive bandage contains about 20,000 microscopic projections per square inch.[55] When worn on the skin, it will deliver vaccine directly to the skin, which has a higher concentration of immune cells than that in the muscles,[citation needed] where needles and syringes deliver. It thus increases the effectiveness of the vaccination using a lower amount of vaccine used in traditional syringe delivery system.[56]
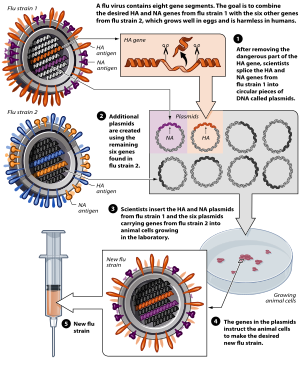
Plasmids
The use of plasmids has been validated in preclinical studies as a protective vaccine strategy for cancer and infectious diseases. However, in human studies this approach has failed to provide clinically relevant benefit. The overall efficacy of plasmid DNA immunization depends on increasing the plasmid's immunogenicity while also correcting for factors involved in the specific activation of immune effector cells.[57]
Use in veterinary medicine

Vaccinations of animals are used both to prevent their contracting diseases and to prevent transmission of disease to humans.[58] Both animals kept as pets and animals raised as livestock are routinely vaccinated. In some instances, wild populations may be vaccinated. This is sometimes accomplished with vaccine-laced food spread in a disease-prone area and has been used to attempt to control rabies in raccoons.
Where rabies occurs, rabies vaccination of dogs may be required by law. Other canine vaccines include canine distemper, canine parvovirus, infectious canine hepatitis, adenovirus-2, leptospirosis, bordatella, canine parainfluenza virus, and Lyme disease, among others.
DIVA vaccines
DIVA (Differentiating Infected from Vaccinated Animals) vaccines make it possible to differentiate between infected and vaccinated animals.
DIVA vaccines carry at least one epitope less than the microorganisms circulating in the field. An accompanying diagnostic test that detects antibody against that epitope allows us to actually make that differentiation.
The first DIVA vaccines
The first DIVA vaccines (formerly termed marker vaccines and since 1999 coined as DIVA vaccines) and companion diagnostic tests have been developed by J.T. van Oirschot and colleagues at the Central Veterinary Institute in Lelystad, The Netherlands.[59] [60] They found that some existing vaccines against pseudorabies (also termed Aujeszky’s disease) had deletions in their viral genome (among which the gE gene). Monoclonal antibodies were produced against that deletion and selected to develop an ELISA that demonstrated antibodies against gE. In addition, novel genetically engineered gE-negative vaccines were constructed.[61] Along the same lines, DIVA vaccines and companion diagnostic tests against bovine herpesvirus 1 infections have been developed.[62][63]
Use in practice
The DIVA strategy has been applied in various countries and successfully eradicated pseudorabies virus. Swine populations were intensively vaccinated and monitored by the companion diagnostic test and subsequently the infected pigs were removed from the population. Bovine herpesvirus 1 DIVA vaccines are also widely used in practice.
Other DIVA vaccines (under development)
Scientists have put and still are putting much effort in applying the DIVA principle to a wide range of infectious diseases, such as, for example, classical swine fever,[64] avian influenza,[65] Actinobacillus pleuropneumonia[66] and Salmonella infections in pigs.[67]
Trends
Vaccine development has several trends:[68]
- Until recently,[when?] most vaccines were aimed at infants and children, but adolescents and adults are increasingly being targeted.[68][69]
- Combinations of vaccines are becoming more common; vaccines containing five or more components are used in many parts of the world.[68] In 2013, Biofarma has released a new product called Pentabio, which is combination vaccine of Diphtheria, Tetanus, Pertussis, Hepatitis B, and Haemophilus Influenzae Type B for baby/infant in Indonesia's Immunization Program.[70]
- New methods of administering vaccines are being developed,[when?] such as skin patches, aerosols via inhalation devices, and eating genetically engineered plants.[68]
- Vaccines are being designed to stimulate innate immune responses, as well as adaptive.[68]
- Attempts are being made to develop vaccines to help cure chronic infections, as opposed to preventing disease.[68]
- Vaccines are being developed to defend against bioterrorist attacks such as anthrax, plague, and smallpox.[68]
- Appreciation for sex and pregnancy differences in vaccine responses "might change the strategies used by public health officials".[71]
- Scientists are now trying to develop synthetic vaccines by reconstructing the outside structure of a virus.[72]
Principles that govern the immune response can now be used in tailor-made vaccines against many noninfectious human diseases, such as cancers and autoimmune disorders.[73] For example, the experimental vaccine CYT006-AngQb has been investigated as a possible treatment for high blood pressure.[74] Factors that have impact on the trends of vaccine development include progress in translatory medicine, demographics, regulatory science, political, cultural, and social responses.[75]
Research
More complex plants such as tobacco, potato, tomato, and banana can have genes inserted that cause them to produce vaccines usable for humans.[76]
See also
References
- ^ a b Baxby, Derrick (1999). "Edward Jenner's Inquiry; a bicentenary analysis". Vaccine. 17 (4): 301–7. doi:10.1016/s0264-410x(98)00207-2. PMID 9987167.
- ^ a b Pasteur, Louis (1881). "Address on the Germ Theory". Lancet. 118 (3024): 271–2. doi:10.1016/s0140-6736(02)35739-8.
- ^ Grammatikos, Alexandros P.; Mantadakis, Elpis; Falagas, Matthew E. (June 2009). "Meta-analyses on Pediatric Infections and Vaccines". Infectious Disease Clinics of North America. 23 (2): 431–57. doi:10.1016/j.idc.2009.01.008. PMID 19393917.
- ^ Neighmond, Patti (2010-02-07). "Adapting Vaccines For Our Aging Immune Systems". Morning Edition. NPR. Archived from the original on 2012-09-05. Retrieved 2014-01-09.
{{cite news}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help)
- ^ Sullivan, Patricia (2005-04-13). "Maurice R. Hilleman dies; created vaccines". Wash. Post. Archived from the original on 2012-09-15. Retrieved 2014-01-09.
{{cite news}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help)
- ^ Schlegel; et al. (August 1999). "Comparative efficacy of three mumps vaccines during disease outbreak in eastern Switzerland: cohort study". BMJ. 319 (7206): 352. doi:10.1136/bmj.319.7206.352. PMID 10435956. Retrieved 2014-01-09.
{{cite journal}}: Explicit use of et al. in:|last=(help)
- ^ Préziosi, M.; Halloran, M.E. (2003). "Effects of Pertussis Vaccination on Disease: Vaccine Efficacy in Reducing Clinical Severity". Clinical Infectious Diseases. 37 (6). Oxford Journals: 772–779. doi:10.1086/377270.
- ^ Orenstein WA, Papania MJ, Wharton ME (2004). "Measles elimination in the United States". J Infect Dis. 189 (Suppl 1): S1–3. doi:10.1086/377693. PMID 15106120.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ a b c "Measles—United States, January 1 – April 25, 2008". Morb. Mortal. Wkly. Rep. 57 (18): 494–8. May 2008. PMID 18463608.

- ^ a b c "Possible Side-effects from Vaccines". Centers for Disease Control and Prevention. Retrieved 24 February 2014.
- ^ "Vaccine Types". Niaid.nih.gov. 2012-04-03. Retrieved 2013-04-26.
- ^ J.K. Sinha & S. Bhattacharya. A Text Book of Immunology (Google Book Preview). Academic Publishers. p. 318. ISBN 978-81-89781-09-5. Retrieved 2014-01-09.
- ^ Kim W, Liau LM (2010). "Dendritic cell vaccines for brain tumors". Neurosurg Clin N Am. 21 (1): 139–57. doi:10.1016/j.nec.2009.09.005. PMC 2810429. PMID 19944973.
- ^ Meri, S; Jördens, M; Jarva, H (December 2008). "Microbial complement inhibitors as vaccines". Vaccine. 26 Suppl 8: I113–7. doi:10.1016/j.vaccine.2008.11.058. PMID 19388175.
- ^ "Monovalent" at Dorland's Medical Dictionary
- ^ Polyvalent vaccine[dead link] at Dorlands Medical Dictionary
- ^ "Questions and answers on monovalent oral polio vaccine type 1 (mOPV1) "Issued jointly by WHO and UNICEF"".
- ^ Scott (April 2004). "Classifying Vaccines" (PDF). BioProcesses International: 14–23. Retrieved 2014-01-09.
- ^ Sutter RW, Cochi SL, Melnick JL (1999). "Live attenuated polio vaccines". In Plotkin SA, Orenstein WA (eds.) (ed.). Vaccines. Philadelphia: W. B. Saunders. pp. 364–408.
{{cite book}}:|editor=has generic name (help)CS1 maint: multiple names: authors list (link) - ^ Kanesa-thasan N; Sun W; Kim-Ahn G; et al. (2001). "Safety and immunogenicity of attenuated dengue virus vaccines (Aventis Pasteur) in human volunteers". Vaccine. 19 (23–24): 3179–3188. doi:10.1016/S0264-410X(01)00020-2. PMID 11312014.
{{cite journal}}: Unknown parameter|author-separator=ignored (help) - ^ "Progress Toward Interruption of Wild Poliovirus Transmission—Worldwide, January 2006 – May 2007". Morb. Mortal. Wkly. Rep. 56 (27): 682–5. 2007-07-13. Archived from the original on 2014-01-09. Retrieved 2014-01-09.
{{cite journal}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help)
- ^ "ACIP Vaccine Recommendations Home Page". CDC. 2013-11-15. Archived from the original on 2014-01-10. Retrieved 2014-01-10.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ "Vaccine Status Table". Red Book Online. American Academy of Pediatrics. April 26, 2011. Retrieved January 9, 2013.
- ^ "HPV Vaccine Safety". Centers for Disease Control and Prevention (CDC). 2013-12-20. Archived from the original on 2014-01-10. Retrieved 2014-01-10.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ "HPV vaccine in the clear". NHS choices. 2009-10-02. Archived from the original on 2012-09-07. Retrieved 2014-01-10.
{{cite news}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help)
- ^ "How Islamic inventors changed the world". Science. Indep. London. 2006-03-11. Archived from the original on 2012-07-16. Retrieved 2014-01-10.
{{cite news}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ a b c Stern AM, Markel H (2005). "The history of vaccines and immunization: familiar patterns, new challenges". Health Aff. 24 (3): 611–21. doi:10.1377/hlthaff.24.3.611. PMID 15886151.

- ^ Dunn PM (January 1996). "Dr Edward Jenner (1749–1823) of Berkeley, and vaccination against smallpox" (PDF). Arch. Dis. Child. Fetal Neonatal Ed. 74 (1): F77–8. doi:10.1136/fn.74.1.F77. PMC 2528332. PMID 8653442.
- ^ Van Sant JE (2008). "The Vaccinators: Smallpox, Medical Knowledge, and the 'Opening' of Japan". J Hist Med Allied Sci. 63 (2): 276–9. doi:10.1093/jhmas/jrn014.
- ^ Dudgeon JA (1963). "Development of smallpox vaccine in England in the eighteenth and nineteenth centuries". BMJ (5342): 1367–72. doi:10.1136/bmj.1.5342.1367. PMC 2124036. PMID 20789814.
- ^ "German Vaccination Law". Internet Archive. Retrieved 29 November 2012.
- ^ a b Wolfe R, Sharp L (2002). "Anti-vaccinationists past and present". BMJ. 325 (7361): 430–2. doi:10.1136/bmj.325.7361.430. PMC 1123944. PMID 12193361.
- ^ Bonhoeffer J, Heininger U (2007). "Adverse events following immunization: perception and evidence". Curr Opin Infect Dis. 20 (3): 237–46. doi:10.1097/QCO.0b013e32811ebfb0. PMID 17471032.
- ^ a b Halvorsen R (2007). The Truth about Vaccines. Gibson Square. ISBN 978-1-903933-92-3.
- ^ Sinal SH, Cabinum-Foeller E, Socolar R (2008). "Religion and medical neglect". South Med J. 101 (7): 703–6. doi:10.1097/SMJ.0b013e31817997c9. PMID 18580731.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Omer, SB; Salmon, DA; Orenstein, WA; deHart, MP; Halsey, N (May 2009). "Vaccine Refusal, Mandatory Immunization, and the Risks of Vaccine-Preventable Diseases" (PDF). New England Journal of Medicine. 360 (19): 1981–8. doi:10.1056/NEJMsa0806477. PMID 19420367.
- ^ Gross L. A broken trust: lessons from the vaccine–autism wars. PLoS Biol. 2009;7(5):e1000114. doi:10.1371/journal.pbio.1000114. PMID 19478850. PMC 2682483.
- ^ By the CNN Wire Staff (2011-01-06). "Retracted autism study an 'elaborate fraud,' British journal finds". CNN.com. Retrieved 2013-04-26.
{{cite news}}:|author=has generic name (help) - ^ Goodman, Jesse L. (2005-05-04). "Statement by Jesse L. Goodman, M.D., M.P.H. Director Center for Biologics, Evaluation and Research Food and Drug Administration U.S. Department of Health and Human Services on US Influenza Vaccine Supply and Preparations for the Upcoming Influenza Season before Subcommittee on Oversight and Investigations Committee on Energy and Commerce United States House of Representatives". Retrieved 2008-06-15.
- ^ Olesen OF, Lonnroth A, Mulligan B (2009). "Human vaccine research in the European Union". Vaccine. 27 (5): 640–5. doi:10.1016/j.vaccine.2008.11.064. PMID 19059446.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Jit, Mark (1 April 2013). "Key issues for estimating the impact and cost-effectiveness of seasonal influenza vaccination strategies". Human vaccines & immunotherapeutics. 9 (4): 834–840. doi:10.4161/hv.23637.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Newall, A.T. (February 2014). "Economic evaluations of implemented vaccination programmes: key methodological challenges in retrospective analyses". Vaccine. 32 (7): 759–765. doi:10.1016/j.vaccine.2013.11.067.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Hardman Reis T (2006). "The role of intellectual property in the global challenge for immunization". J World Intellect Prop. 9 (4): 413–25. doi:10.1111/j.1422-2213.2006.00284.x.
- ^ "Three ways to make a vaccine" The Washington Post
- ^ Muzumdar JM, Cline RR (2009). "Vaccine supply, demand, and policy: a primer". J Am Pharm Assoc. 49 (4): e87–99. doi:10.1331/JAPhA.2009.09007. PMID 19589753.
- ^ a b Bae K, Choi J, Jang Y, Ahn S, Hur B (2009). "Innovative vaccine production technologies: the evolution and value of vaccine production technologies". Arch Pharm Res. 32 (4): 465–80. doi:10.1007/s12272-009-1400-1. PMID 19407962.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ "India produces 60 percent of world's vaccines". November 15, 2011.
- ^ CDC. "Ingredients of Vaccines — Fact Sheet". Retrieved December 20, 2009.
- ^ "Thimerosal in vaccines". Center for Biologics Evaluation and Research, U.S. Food and Drug Administration. 2007-09-06. Retrieved 2007-10-01.
- ^ Bigham M, Copes R (2005). "Thiomersal in vaccines: balancing the risk of adverse effects with the risk of vaccine-preventable disease". Drug Saf. 28 (2): 89–101. doi:10.2165/00002018-200528020-00001. PMID 15691220.
- ^ Offit PA (2007). "Thimerosal and vaccines—a cautionary tale" (PDF). N Engl J Med. 357 (13): 1278–9. doi:10.1056/NEJMp078187. PMID 17898096.
- ^ Morein B, Hu KF, Abusugra I (2004). "Current status and potential application of ISCOMs in veterinary medicine". Adv Drug Deliv Rev. 56 (10): 1367–82. doi:10.1016/j.addr.2004.02.004. PMID 15191787.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Firdos Alam Khan. Biotechnology Fundamentals. CRC Press. p. 270.
- ^ Giudice EL, Campbell JD (2006). "Needle-free vaccine delivery". Adv Drug Deliv Rev. 58 (1): 68–89. doi:10.1016/j.addr.2005.12.003. PMID 16564111.
- ^ "Australian scientists develop 'needle-free' vaccination". Chennai, India: The Hindu. 28 September 2011.
- ^ "Needle-free nanopatch vaccine delivery system". News Medical. 3 August 2011.
- ^ Lowe (2008). "Plasmid DNA as Prophylactic and Therapeutic vaccines for Cancer and Infectious Diseases". Plasmids: Current Research and Future Trends. Caister Academic Press. ISBN 978-1-904455-35-6.
{{cite book}}: External link in|chapterurl=|display-authors=1(help); Unknown parameter|chapterurl=ignored (|chapter-url=suggested) (help) - ^ Patel, JR; Heldens, JG (March 2009). "Immunoprophylaxis against important virus disease of horses, farm animals and birds". Vaccine. 27 (12): 1797–1810. doi:10.1016/j.vaccine.2008.12.063. PMID 19402200.
- ^ Van Oirschot JT, Rziha HJ, Moonen PJ, Pol JM, Van Zaane D (1986). "Differentiation of serum antibodies from pigs vaccinated or infected with Aujeszky's disease virus by a competitive enzyme immunoassay". The Journal of General Virology. 67 (6): 1179–82. doi:10.1099/0022-1317-67-6-1179.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Van Oirschot JT (1999). "Diva vaccines that reduce virus transmission". Journal of Biotechnology. 73 (2–3): 195–205. doi:10.1016/S0168-1656(99)00121-2. PMID 10486928.
- ^ Van Oirschot JT, Gielkens ALJ, Moormann RJM, Berns AJM (1990). "Marker vaccines, virus protein-specific antibody assays and the control of Aujeszky's disease". Veterinary Microbiology. 23 (1–4): 85–101. doi:10.1016/0378-1135(90)90139-M. PMID 2169682.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Van Oirschot JT (1999). "Diva vaccines that reduce virus transmission". Journal of Biotechnology. 73 (2–3): 195–205. doi:10.1016/S0168-1656(99)00121-2. PMID 10486928.
- ^ Kaashoek MJ, Moerman A, Madic J, Rijsewijk FAM, Quak J, Gielkens ALJ, Van Oirschot JT (1994). "A conventionally attenuated glycoprotein E-negative strain of bovine herpesvirus type 1 is an efficacious and safe vaccine". Vaccine. 12 (5): 439–44. doi:10.1016/0264-410X(94)90122-8. PMID 8023552.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Hulst MM, Westra DF, Wensvoort G, Moormann RJM (1993). "Glycoprotein E1 of hog cholera virus expressed in insect cells protects swine from hog cholera". Journal of Virology. 67 (9): 5435–5442. PMC 237945. PMID 8350404.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Capua I, Terregino C, Cattoli G, Mutinelli F, RodriguezJF (2003). "Development of a DIVA (Differentiating Infected from Vaccinated Animals) strategy using a vaccine containing a heterologous neuraminidase for the control of avian influenza". Avian Pathology. 32 (1): 47–55. doi:10.1080/0307945021000070714. PMID 12745380.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Maas A, Meens J, Baltes N, Hennig-Pauka I, Gerlach G-F (2006). "Development of a DIVA subunit vaccine against Actinobacillus pleuropneumoniae infection". Vaccine. 24 (49): 7226–32. doi:10.1016/j.vaccine.2006.06.047.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Leyman B, Boyen F, Van Parys A, Verbruggh E, Haesebrouck F, Pasmans F. (2011). "Salmonella Typhimurium LPS mutations for use in vaccines allowing differentiation of infected and vaccinated pigs". Vaccine. 29 (20): 3679–85. doi:10.1016/j.vaccine.2011.03.004. PMID 21419163.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ a b c d e f g Plotkin SA (2005). "Vaccines: past, present and future". Nat Med. 11 (4 Suppl): S5–11. doi:10.1038/nm1209. PMID 15812490.
- ^ Carlson B (2008). "Adults now drive growth of vaccine market". Gen. Eng. Biotechnol. News. Vol. 28, no. 11. pp. 22–3. Archived from the original on 2013-01-08.
{{cite news}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help)
- ^ "Bio Farma Urges OIC Countries to become Self-Reliant in Vaccine". June 18, 2013. Retrieved June 19, 2013.
- ^ Klein SL, Jedlicka A, Pekosz A (May 2010). "The Xs and Y of immune responses to viral vaccines". Lancet Infect Dis. 10 (5): 338–49. doi:10.1016/S1473-3099(10)70049-9. PMID 20417416.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ "Safer vaccine created without virus". March 28, 2013. Retrieved March 28, 2013.
- ^ Spohn G, Bachmann MF (2008). "Exploiting viral properties for the rational design of modern vaccines". Expert Rev Vaccines. 7 (1): 43–54. doi:10.1586/14760584.7.1.43. PMID 18251693.
- ^ Samuelsson O, Herlitz H (2008). "Vaccination against high blood pressure: a new strategy". Lancet. 371 (9615): 788–9. doi:10.1016/S0140-6736(08)60355-4. PMID 18328909.
- ^ Poland GA, Jacobson RM, Ovsyannikova IG (2009). "Trends affecting the future of vaccine development and delivery: the role of demographics, regulatory science, the anti-vaccine movement, and vaccinomics". Vaccine. 27 (25–26): 3240–4. doi:10.1016/j.vaccine.2009.01.069. PMC 2693340. PMID 19200833.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Sala, F.; Manuela Rigano, M.; Barbante, A.; Basso, B.; Walmsley, AM; Castiglione, S (January 2003). "Vaccine antigen production in transgenic plants: strategies, gene constructs and perspectives". Vaccine. 21 (7–8): 803–8. doi:10.1016/s0264-410x(02)00603-5. PMID 23888738.
External links
| External videos | |
|---|---|
