Nail clubbing
| Nail clubbing |
|---|

In medicine, nail clubbing[1] (also known as "Drumstick fingers," "Hippocratic fingers," and "Watch-glass nails"[1]) is a deformity of the fingers and fingernails that is associated with a number of diseases, mostly of the heart and lungs.[2]: 656 Hippocrates was probably the first to document clubbing as a sign of disease, and the phenomenon is therefore occasionally called Hippocratic fingers.
Idiopathic clubbing can also occur and in 60% of cases there is no associated underlying disease.[3]
Signs and symptoms
Clubbing develops in five steps:[4]
- Fluctuation and softening of the nail bed (increased ballotability)
- Loss of the normal <165° angle (Lovibond angle) between the nailbed and the fold (cuticula)
- Increased convexity of the nail fold
- Thickening of the whole distal (end part of the) finger (resembling a drumstick)
- Shiny aspect and striation of the nail and skin
Schamroth's test or Schamroth's window test (originally demonstrated by South African cardiologist Dr Leo Schamroth on himself[5]) is a popular test for clubbing. When the distal phalanges (bones nearest the fingertips) of corresponding fingers of opposite hands are directly apposed (place fingernails of same finger on opposite hands against each other, nail to nail), a small diamond-shaped "window" is normally apparent between the nailbeds. If this window is obliterated, the test is positive and clubbing is present.
Diagnosis
When clubbing is encountered in patients, doctors will seek to identify its cause. They usually accomplish this by obtaining a medical history—particular attention is paid to lung, heart, and gastrointestinal conditions—and conducting a clinical examination, which may disclose associated features relevant to a diagnosis. Additional studies such as a chest X-ray and a chest CT-scan may also be performed.[4]
Disease associations
Although many diseases are associated with clubbing (particularly lung diseases), the reports are fairly anecdotal. Prospective studies of patients presenting with clubbing have not yet been performed, and hence there is no conclusive evidence of these associations.
Isolated clubbing

Clubbing is associated with:
- Lung disease:
- Lung cancer, mainly large-cell (35% of all cases), not seen frequently in small cell lung cancer[6]
- Interstitial lung disease
- Tuberculosis
- Suppurative lung disease: lung abscess, empyema, bronchiectasis, cystic fibrosis
- Mesothelioma
- A·V fistula
- Heart disease:
- Any disease featuring chronic hypoxia
- Congenital cyanotic heart disease (most common cardiac cause)
- Subacute bacterial endocarditis
- Atrial myxoma (benign tumor)
- Gastrointestinal and hepatobiliary:
- Malabsorption
- Crohn's disease and ulcerative colitis
- Cirrhosis, especially in primary biliary cirrhosis[7]
- Hepatopulmonary syndrome, a complication of cirrhosis[8]
- Laxative abuse
- Polyposis
- Esophageal CA
- Others:
- Hyperthyroidism (thyroid acropachy)[9]
- Familial and racial clubbing and "pseudoclubbing" (people of African descent often have what appears to be clubbing)
- Vascular anomalies of the affected arm such as an axillary artery aneurysm (in unilateral clubbing)
- Thymoma
- Thalassemia
HPOA
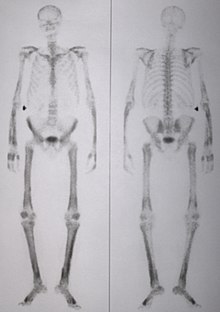
A special form of clubbing is hypertrophic pulmonary osteo-arthropathy, known in continental Europe as Pierre Marie-Bamberger syndrome. (In dogs the condition is known as hypertrophic osteopathy.) This is the combination of clubbing and thickening of periosteum (connective tissue lining of the bones) and synovium (lining of joints), and is often initially diagnosed as arthritis. It is commonly associated with lung cancer.
Primary HOA
Primary hypertrophic osteo-arthropathy is HPOA without signs of pulmonary disease. This form has a hereditary component, although subtle cardiac abnormalities can occasionally be found. It is known eponymously as the Touraine-Solente-Golé syndrome. This condition has been linked to mutations in the gene on the fourth chromosome (4q33-q34)coding for the enzyme 15-hydroxyprostaglandin dehydrogenase (HPGD); this leads to decreased breakdown of prostaglandin E2 and elevated levels of this substance.[10]
Pathophysiology
The exact cause for sporadic clubbing is unknown, and there are numerous theories as to its cause. Vasodilation (distended blood vessels), secretion of growth factors (such as platelet-derived growth factor and hepatocyte growth factor) from the lungs, and other mechanisms have been proposed. The discovery of disorders in the prostaglandin metabolism in primary osteo-arthropathy has led to suggestions that overproduction of PGE2 by other tissues may be the causative factor for clubbing.[10]
Epidemiology
The exact frequency of clubbing in the population is not known. A 2008 study found clubbing in 1% of all patients admitted to a department of internal medicine. Of these, 40% turned out to have significant underlying disease of various causes, while 60% had no medical problems on further investigations and remained well over the subsequent year.[3]
See also
- Periosteal reaction
- Clubbed thumb (unrelated congenital deformity)
- List of cutaneous conditions
References
- ^ a b Rapini, Ronald P.; Bolognia, Jean L.; Jorizzo, Joseph L. (2007). Dermatology: 2-Volume Set. St. Louis: Mosby. ISBN 1-4160-2999-0.
{{cite book}}: CS1 maint: multiple names: authors list (link) - ^ Freedberg, et al. (2003). Fitzpatrick's Dermatology in General Medicine. (6th ed.). McGraw-Hill. ISBN 0071380760.
- ^ a b Vandemergel X, Renneboog B (2008). "Prevalence, aetiologies and significance of clubbing in a department of general internal medicine". Eur. J. Intern. Med. 19 (5): 325–9. doi:10.1016/j.ejim.2007.05.015. PMID 18549933.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ a b Myers KA, Farquhar DR (2001). "The rational clinical examination: does this patient have clubbing?". JAMA. 286: 341–7. doi:10.1001/jama.286.3.341. PMID 11466101.
- ^ Schamroth L (1976). "Personal experience". S. Afr. Med. J. 50 (9): 297–300. PMID 1265563.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Sridhar KS, Lobo CF, Altman RD (1998). "Digital clubbing and lung cancer" (PDF). Chest. 114: 1535–37. doi:10.1378/chest.114.6.1535. PMID 9872183.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Epstein O, Dick R, Sherlock S (1981). "Prospective study of periostitis and finger clubbing in primary biliary cirrhosis and other forms of chronic liver disease". Gut. 22 (3): 203–6. doi:10.1136/gut.22.3.203. PMID 7227854.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Naeije R. Hepatopulmonary syndrome and portopulmonary hypertension. Swiss Med Wkly. 2003;133:163-9. PMID 12715285.
- ^ . GPnotebook https://www.gpnotebook.co.uk/simplepage.cfm?ID=-724565997.
{{cite web}}: Missing or empty|title=(help) - ^ a b Uppal S, Diggle CP, Carr IM; et al. (2008). "Mutations in 15-hydroxyprostaglandin dehydrogenase cause primary hypertrophic osteoarthropathy". Nat. Genet. 40 (6): 789–93. doi:10.1038/ng.153. PMID 18500342.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link)
