Deep vein thrombosis: Difference between revisions
Biosthmors (talk | contribs) →Prognosis: add |
Biosthmors (talk | contribs) →Anticoagulation: add |
||
| Line 159: | Line 159: | ||
| footer = Structural representations of the backbone of heparins (''left''), which vary in the size of their chain, and the synthetic pentasaccaride (five-sugar) [[fondaparinux]] (''right'') |
| footer = Structural representations of the backbone of heparins (''left''), which vary in the size of their chain, and the synthetic pentasaccaride (five-sugar) [[fondaparinux]] (''right'') |
||
}} |
}} |
||
[[Anticoagulation]], which prevents further coagulation, but does not act directly on existing clots, is the standard treatment for DVT.<ref name="ADAM">{{cite web |url=https://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0001209/#adam_000156.disease.treatment |title=Deep venous thrombosis |date=19 February 2012 |encyclopedia=A.D.A.M. Medical Encyclopedia |publisher=PubMed Health |access-date=2 July 2012 |url-status=live |archive-url=https://web.archive.org/web/20120926073924/http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0001209/#adam_000156.disease.treatment |archive-date=26 September 2012 }}</ref>{{efn|Evidence for anticoagulation comes from studies other than definitive [[randomized controlled trial]]s that demonstrate [[efficacy]] and safety for anticoagulation vs. placebo or using [[NSAID]]s.<ref name="Cundiff">{{cite journal | vauthors = Cundiff DK, Manyemba J, Pezzullo JC | title = Anticoagulants versus non-steroidal anti-inflammatories or placebo for treatment of venous thromboembolism | journal = The Cochrane Database of Systematic Reviews | issue = 1 | pages = CD003746 | date = January 2006 | pmid = 16437461 | doi = 10.1002/14651858.CD003746.pub2 | veditors = Cundiff DK }}</ref>}} Balancing risk vs. benefit is important in determining the duration of anticoagulation, and three months is generally the standard length of treatment.<ref name=NICECG144/> In those with an annual risk of VTE in excess of 9%, as after an unprovoked episode, extended<!--add note here--> anticoagulation is a possibility.<ref name="Keeling"/> Those who finish VKA treatment after idiopathic VTE with an elevated D-dimer level show an increased risk of recurrent VTE (about 9% vs about 4% for normal results), and this result might be used in clinical decision-making.<ref name="Douketis">{{cite journal | vauthors = Douketis J, Tosetto A, Marcucci M, Baglin T, Cushman M, Eichinger S, Palareti G, Poli D, Tait RC, Iorio A | display-authors = 6 | title = Patient-level meta-analysis: effect of measurement timing, threshold, and patient age on ability of D-dimer testing to assess recurrence risk after unprovoked venous thromboembolism | journal = Annals of Internal Medicine | volume = 153 | issue = 8 | pages = 523–31 | date = October 2010 | pmid = 20956709 | doi = 10.7326/0003-4819-153-8-201010190-00009 }}</ref> Thrombophilia test results rarely play a role in the length of treatment.<ref name="Baglin">{{cite journal | vauthors = Baglin T | title = Inherited and acquired risk factors for venous thromboembolism | journal = Seminars in Respiratory and Critical Care Medicine | volume = 33 | issue = 2 | pages = 127–37 | date = April 2012 | pmid = 22648484 | doi = 10.1055/s-0032-1311791 }}</ref> Two forms of [[direct oral anticoagulants]] (DOACs) have been developed: oral [[direct thrombin inhibitor]]s and oral [[Direct Xa inhibitor|factor Xa inhibitors]], which can be an effective and safe alternative to warfarin for acute DVT.<ref>{{cite journal | vauthors = Robertson L, Kesteven P, McCaslin JE | title = Oral direct thrombin inhibitors or oral factor Xa inhibitors for the treatment of deep vein thrombosis | journal = The Cochrane Database of Systematic Reviews | issue = 6 | pages = CD010956 | date = June 2015 | pmid = 26123214 | doi = 10.1002/14651858.CD010956.pub2 | editor-last = Cochrane Vascular Group }}</ref> |
Treatment for DVT is warranted when the clots are either proximal, distal and symptomatic, or upper extremity and symptomatic.<ref name=2017CC>{{cite journal | vauthors = Bartholomew JR | title = Update on the management of venous thromboembolism | journal = Cleveland Clinic Journal of Medicine | volume = 84 | issue = 12 Suppl 3 | pages = 39–46 | date = December 2017 | pmid = 29257737 | doi = 10.3949/ccjm.84.s3.04 | doi-access = free}}</ref> [[Anticoagulation]], which prevents further coagulation, but does not act directly on existing clots, is the standard treatment for DVT.<ref name="ADAM">{{cite web |url=https://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0001209/#adam_000156.disease.treatment |title=Deep venous thrombosis |date=19 February 2012 |encyclopedia=A.D.A.M. Medical Encyclopedia |publisher=PubMed Health |access-date=2 July 2012 |url-status=live |archive-url=https://web.archive.org/web/20120926073924/http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0001209/#adam_000156.disease.treatment |archive-date=26 September 2012 }}</ref>{{efn|Evidence for anticoagulation comes from studies other than definitive [[randomized controlled trial]]s that demonstrate [[efficacy]] and safety for anticoagulation vs. placebo or using [[NSAID]]s.<ref name="Cundiff">{{cite journal | vauthors = Cundiff DK, Manyemba J, Pezzullo JC | title = Anticoagulants versus non-steroidal anti-inflammatories or placebo for treatment of venous thromboembolism | journal = The Cochrane Database of Systematic Reviews | issue = 1 | pages = CD003746 | date = January 2006 | pmid = 16437461 | doi = 10.1002/14651858.CD003746.pub2 | veditors = Cundiff DK }}</ref>}} Balancing risk vs. benefit is important in determining the duration of anticoagulation, and three months is generally the standard length of treatment.<ref name=NICECG144/> In those with an annual risk of VTE in excess of 9%, as after an unprovoked episode, extended<!--add note here--> anticoagulation is a possibility.<ref name="Keeling"/> Those who finish VKA treatment after idiopathic VTE with an elevated D-dimer level show an increased risk of recurrent VTE (about 9% vs about 4% for normal results), and this result might be used in clinical decision-making.<ref name="Douketis">{{cite journal | vauthors = Douketis J, Tosetto A, Marcucci M, Baglin T, Cushman M, Eichinger S, Palareti G, Poli D, Tait RC, Iorio A | display-authors = 6 | title = Patient-level meta-analysis: effect of measurement timing, threshold, and patient age on ability of D-dimer testing to assess recurrence risk after unprovoked venous thromboembolism | journal = Annals of Internal Medicine | volume = 153 | issue = 8 | pages = 523–31 | date = October 2010 | pmid = 20956709 | doi = 10.7326/0003-4819-153-8-201010190-00009 }}</ref> Thrombophilia test results rarely play a role in the length of treatment.<ref name="Baglin">{{cite journal | vauthors = Baglin T | title = Inherited and acquired risk factors for venous thromboembolism | journal = Seminars in Respiratory and Critical Care Medicine | volume = 33 | issue = 2 | pages = 127–37 | date = April 2012 | pmid = 22648484 | doi = 10.1055/s-0032-1311791 }}</ref> Two forms of [[direct oral anticoagulants]] (DOACs) have been developed: oral [[direct thrombin inhibitor]]s and oral [[Direct Xa inhibitor|factor Xa inhibitors]], which can be an effective and safe alternative to warfarin for acute DVT.<ref>{{cite journal | vauthors = Robertson L, Kesteven P, McCaslin JE | title = Oral direct thrombin inhibitors or oral factor Xa inhibitors for the treatment of deep vein thrombosis | journal = The Cochrane Database of Systematic Reviews | issue = 6 | pages = CD010956 | date = June 2015 | pmid = 26123214 | doi = 10.1002/14651858.CD010956.pub2 | editor-last = Cochrane Vascular Group }}</ref> |
||
For acute cases in the leg, the ACCP recommended a [[parenteral]] anticoagulant (such as LMWH, fondaparinux, or unfractionated heparin) for at least five days{{efn|The international normalized ratio should be ≥ 2.0 for 24 hours minimum,<ref>[[#CITEREFGuyattAklCrowtherGutterman2012|Guyatt et al. 2012]], p. 20S: 2.4.</ref> but if the ratio is > 3.0, then the parenteral anticoagulant is not needed for five days.<ref name="Kearon2"/><!--e435S-->}} and a VKA, the oral anticoagulant, the same day. LMWH and fondaparinux are suggested over unfractionated heparin, but both are retained in those with compromised kidney function, unlike unfractionated heparin.<ref name="Kearon2"/><!--e435S--><ref>[[#CITEREFGuyattAklCrowtherGutterman2012|Guyatt et al. 2012]], p. 20S: 2.5.1.</ref> The VKA is generally taken for a minimum of three months<ref>[[#CITEREFGuyattAklCrowtherGutterman2012|Guyatt et al. 2012]], pp. 20S–21S: 3.1.</ref> to maintain an international normalized ratio of 2.0–3.0, with 2.5 as the target.<ref name="Strijkers">{{cite journal | vauthors = Strijkers RH, Cate-Hoek AJ, Bukkems SF, Wittens CH | title = Management of deep vein thrombosis and prevention of post-thrombotic syndrome | journal = BMJ | volume = 343 | pages = d5916 | date = October 2011 | pmid = 22042752 | doi = 10.1136/bmj.d5916 | url = https://semanticscholar.org/paper/f88e2ecee25752d2ed8376dff8da5d81656013da }}</ref><ref>[[#CITEREFGuyattAklCrowtherGutterman2012|Guyatt et al. 2012]], p. 22S: 3.2.</ref> The benefit of taking a VKA declines as the duration of treatment extends,<ref>{{cite journal | vauthors = Middeldorp S, Prins MH, Hutten BA | title = Duration of treatment with vitamin K antagonists in symptomatic venous thromboembolism | journal = The Cochrane Database of Systematic Reviews | issue = 8 | pages = CD001367 | date = August 2014 | pmid = 25092359 | doi = 10.1002/14651858.CD001367.pub3 }}</ref> and the risk of bleeding increases with age.<ref name="de Jong"/> |
For acute cases in the leg, the ACCP recommended a [[parenteral]] anticoagulant (such as LMWH, fondaparinux, or unfractionated heparin) for at least five days{{efn|The international normalized ratio should be ≥ 2.0 for 24 hours minimum,<ref>[[#CITEREFGuyattAklCrowtherGutterman2012|Guyatt et al. 2012]], p. 20S: 2.4.</ref> but if the ratio is > 3.0, then the parenteral anticoagulant is not needed for five days.<ref name="Kearon2"/><!--e435S-->}} and a VKA, the oral anticoagulant, the same day. LMWH and fondaparinux are suggested over unfractionated heparin, but both are retained in those with compromised kidney function, unlike unfractionated heparin.<ref name="Kearon2"/><!--e435S--><ref>[[#CITEREFGuyattAklCrowtherGutterman2012|Guyatt et al. 2012]], p. 20S: 2.5.1.</ref> The VKA is generally taken for a minimum of three months<ref>[[#CITEREFGuyattAklCrowtherGutterman2012|Guyatt et al. 2012]], pp. 20S–21S: 3.1.</ref> to maintain an international normalized ratio of 2.0–3.0, with 2.5 as the target.<ref name="Strijkers">{{cite journal | vauthors = Strijkers RH, Cate-Hoek AJ, Bukkems SF, Wittens CH | title = Management of deep vein thrombosis and prevention of post-thrombotic syndrome | journal = BMJ | volume = 343 | pages = d5916 | date = October 2011 | pmid = 22042752 | doi = 10.1136/bmj.d5916 | url = https://semanticscholar.org/paper/f88e2ecee25752d2ed8376dff8da5d81656013da }}</ref><ref>[[#CITEREFGuyattAklCrowtherGutterman2012|Guyatt et al. 2012]], p. 22S: 3.2.</ref> The benefit of taking a VKA declines as the duration of treatment extends,<ref>{{cite journal | vauthors = Middeldorp S, Prins MH, Hutten BA | title = Duration of treatment with vitamin K antagonists in symptomatic venous thromboembolism | journal = The Cochrane Database of Systematic Reviews | issue = 8 | pages = CD001367 | date = August 2014 | pmid = 25092359 | doi = 10.1002/14651858.CD001367.pub3 }}</ref> and the risk of bleeding increases with age.<ref name="de Jong"/> |
||
Revision as of 20:55, 4 February 2020
| Deep vein thrombosis | |
|---|---|
| Other names | Deep venous thrombosis |
 | |
| DVT in the right leg with swelling and redness | |
| Specialty | Various |
| Symptoms | Pain, swelling, redness, or warmth of the affected area[1] |
| Complications | Pulmonary embolism, post-thrombotic syndrome[1][2] |
| Risk factors | Recent surgery, older age, cancer, history of VTE, family history, trauma, lack of movement, obesity, hormonal birth control, pregnancy and the period following birth, antiphospholipid syndrome, certain genetic conditions[1][2] |
| Diagnostic method | Ultrasound[1] |
| Differential diagnosis | Ruptured Baker's cyst, cellulitis, hematoma, varicose veins[3] |
| Prevention | Frequent walking, calf exercises, aspirin, anticoagulants (blood thinners), intermittent pneumatic compression, graduated compression stockings[4][5] |
| Treatment | Anticoagulation, graduated compression stockings[1] |
| Medication | Low-molecular-weight heparin, warfarin, direct oral anticoagulant[2][4] |
| Frequency | 1–2 out of 1,000 people per year[6] |
Deep vein thrombosis (DVT) is the formation of a blood clot in a deep vein, most commonly in the legs or pelvis.[6][a] Symptoms can include pain, swelling, redness, or warmth of the affected area, but some DVTs have no symptoms.[1] Complications can include pulmonary embolism, as a result of detachment of a clot, which travels to the lungs, and post-thrombotic syndrome.[1][2] Together, DVT and pulmonary embolism are known as venous thromboembolism (VTE).[1]
The mechanism of clot formation typically involves some combination of decreased blood flow rate, increased tendency to clot, and injury to the blood vessel wall.[1] Risk factors include recent surgery, older age, cancer, history of VTE, family history, trauma, lack of movement, obesity, hormonal birth control, pregnancy and the period following birth, antiphospholipid syndrome, and certain genetic conditions.[1][2] Genetic factors include non-O blood type, deficiencies of antithrombin, protein C, and protein S and the mutations of factor V Leiden and prothrombin G20210A.[2] As of 2019, a total of 33 locations on human DNA have been identified that contribute to VTE risk.[7]
Individuals suspected of having DVT can be assessed using a clinical prediction rule such as the Wells score.[2][3] A D-dimer test can also be used to assist with excluding the diagnosis or to signal a need for further testing.[1] Diagnosis is most commonly confirmed by ultrasound of the suspected veins.[1] An estimated 4–10% of DVTs affect the arms.[8]
Anticoagulation (blood thinners) is the standard treatment.[1] Typical medications include low-molecular-weight heparin, a direct oral anticoagulant, or warfarin.[2] Preventive efforts following surgery can include early and frequent walking, calf exercises, aspirin, anticoagulants, graduated compression stockings, or intermittent pneumatic compression.[4] The rate of DVTs increases from childhood to old age; in adulthood, about one in 1000 adults are affected per year.[9] About 5% of people are affected by a VTE at some point in time.[3]
Signs and symptoms
Signs and symptoms of DVT, while highly variable, include pain or tenderness, swelling, warmth, dilation of surface veins, redness or discoloration, and cyanosis with fever.[10] Although, some with DVT have no symptoms.[11] Signs and symptoms alone are not sufficiently sensitive or specific to make a diagnosis, but when considered in conjunction with pre-test probability, can help determine the likelihood of DVT.[11] In most suspected cases, DVT is ruled out after evaluation,[12] and symptoms are more often due to other causes, such as cellulitis, ruptured Baker's cyst, musculoskeletal injury and hematoma, lymphedema, and chronic venous insufficiency.[11][13] Other differential diagnoses include tumors, venous or arterial aneurysms, and connective tissue disorders.[14]
Causes

The disease term venous thromboembolism (VTE) includes the development of either DVT or pulmonary embolism (PE).[15][16] The three factors of Virchow's triad—venous stasis, hypercoagulability, and changes in the endothelial blood vessel lining (such as physical damage or endothelial activation)—contribute to VTE and are used to explain its formation.[17][18] Other related causes include activation of immune system components, the state of microparticles in the blood, the concentration of oxygen, and possible platelet activation.[19] Various risk factors contribute to VTE, though many at high risk never develop it.[20]
Acquired risk factors include the strong risk factor of older age,[10] which alters blood composition to favor clotting.[21] Previous VTE, particularly unprovoked VTE, is a strong risk factor.[22] Major surgery and trauma increase risk because of tissue factor from outside the vascular system entering the blood.[17] Minor leg injuries,[23] lower limb amputation,[24] hip fracture, and long bone fractures are also risks.[6] In orthopedic surgery, venous stasis can be temporarily provoked by a cessation of blood flow as part of the procedure.[19] Inactivity and immobilization contribute to venous stasis, as with orthopedic casts,[25] paralysis, sitting, long-haul travel, bed rest, hospitalization,[17] and in survivors of acute stroke.[26] Conditions that involve compromised blood flow in the veins are May–Thurner syndrome, where a vein of the pelvis is compressed, and venous thoracic outlet syndrome, which includes Paget–Schroetter syndrome, where compression occurs near the base of the neck.[27][28][29]
Cancer can grow in and around veins, causing venous stasis, and can also stimulate increased levels of tissue factor.[30] Cancers of the bone, ovary, brain, pancreas, and lymphomas are especially associated with increased VTE risk.[24] Chemotherapy treatment also increases risk.[18] Obesity increases the potential of blood to clot, as does pregnancy. In the postpartum, placental tearing releases substances that favor clotting. Oral contraceptives[b] and hormonal replacement therapy increase the risk through a variety of mechanisms, including altered blood coagulation protein levels and reduced fibrinolysis.[19]

Family history of VTE is a risk factor for a first VTE.[32] Genetic factors that increase the risk of VTE include deficiencies of three proteins that normally prevent blood from clotting—protein C, protein S, and antithrombin. Deficiencies in antithrombin, protein C, and protein S[c] are rare but strong, or moderately strong, risk factors.[17][19] These three deficiencies increase the risk of VTE by about 10 times.[23] Factor V Leiden, which makes factor V resistant to inactivation by activated protein C,[32] mildly increases VTE risk[d] by about three times.[7][32] Having a non-O blood type roughly doubles VTE risk.[19] Non-O blood type is common globally, making it an important risk factor.[34] Individuals without O blood type have higher blood levels of von Willebrand factor and factor VIII than those with O blood type, increasing the likelihood of clotting.[34] The genetic variant prothrombin G20210A, which increases prothrombin levels,[17] increases risk by about 2.5 times.[7] Additionally, approximately 5% of people have been identified with a background genetic risk comparable to the factor V Leiden and prothrombin G20210A mutations.[7]
Inflammatory diseases[19][35] such as Behçet's syndrome,[36] and some autoimmune diseases,[37] such as primary antiphospholipid syndrome[38] and systemic lupus erythematosus (SLE),[39] increase risk. SLE itself is frequently associated with antiphospholipid syndrome.[40] Other associated conditions include heparin-induced thrombocytopenia,[41] thrombotic storm,[42] catastrophic antiphospholipid syndrome,[43] paroxysmal nocturnal hemoglobinuria,[44] nephrotic syndrome,[20] infection,[20][35] HIV,[20] polycythemia vera,[25] intravenous drug use,[45][46] and smoking.[e] Blood alterations including dysfibrinogenemia,[25] low free protein S,[20] activated protein C resistance,[20] hyperhomocysteinemia,[17] high fibrinogen levels,[17], high factor IX levels,[17] and high factor XI levels[17] are associated with increased risk.
Some risk factors influence the location of DVT within the body. In isolated distal DVT, the profile of risk factors appears distinct from proximal DVT. Transient factors, such as surgery and immobilization, appear to dominate, whereas thrombophilias[f] and age do not seem to increase risk.[49] Common risk factors for having an upper extremity DVT include having an existing foreign body (such as a central venous catheter, a pacemaker, or a triple-lumen PICC line), cancer, and recent surgery.[8]
Pathophysiology

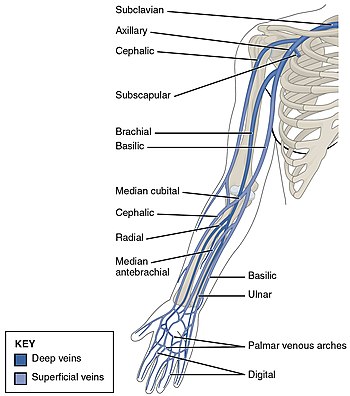
DVT often develops in the calf veins and "grows" in the direction of venous flow, towards the heart.[50] When DVT does not grow, it can be cleared naturally and dissolved into the blood (fibrinolysis).[51] Veins in the leg or pelvis are most commonly affected,[6] including the popliteal vein (behind the knee), femoral vein (of the thigh), and iliac veins of the pelvis. Extensive lower-extremity DVT can even reach into the or the inferior vena cava (in the abdomen).[52] Upper extremity DVT most commonly affects the subclavian, axillary, and jugular veins.[8]
The causes of arterial thrombosis, such as with heart attacks, are more clearly understood than those of venous thrombosis.[53] With arterial thrombosis, blood vessel wall damage is required, as it initiates coagulation,[53] but clotting in the veins mostly occurs without any such damage.[17] The beginning of venous thrombosis is thought to be caused by tissue factor, which leads to conversion of prothrombin to thrombin, followed by fibrin deposition.[18] Red blood cells and fibrin are the main components of venous thrombi,[17] and the fibrin appears to attach to the blood vessel wall lining (endothelium), a surface that normally acts to prevent clotting.[53] Platelets and white blood cells are also components. Platelets are not as prominent in venous clots as they are in arterial ones, but they can play a role.[19] Inflammation is associated with VTE,[g] and white blood cells play a role in the formation and resolution of venous clots.[51]
Often, DVT begins in the valves of veins.[51] The blood flow pattern in the valves can cause low oxygen concentrations in the blood (hypoxemia) of a valve sinus. Hypoxemia, which is worsened by venous stasis, activates pathways—ones that include hypoxia-inducible factor-1 and early-growth-response protein 1. Hypoxemia also results in the production of reactive oxygen species, which can activate these pathways, as well as nuclear factor-κB, which regulates hypoxia-inducible factor-1 transcription.[18] Hypoxia-inducible factor-1 and early-growth-response protein 1 contribute to monocyte association with endothelial proteins, such as P-selectin, prompting monocytes to release tissue factor-filled microvesicles, which presumably begin clotting after binding to the endothelial surface.[18]
Diagnosis
DVT diagnosis requires the use of imaging devices such as ultrasound. Clinical assessments, which predict DVT likelihood, can help determine if a D-dimer test is useful. In those not highly likely to have DVT, a normal D-dimer result[h] can rule out a diagnosis.
Classification
Provoked DVTs occur in association with acquired risk factors, such as surgery, oral contraceptives, trauma, immobility, obesity, or cancer; cases without acquired states are called unprovoked or idiopathic.[55] Acute DVT is characterized by pain and swelling[56] and is usually occlusive,[57] which means that it obstructs blood flow, whereas non-occlusive DVT is less symptomatic.[58] The label "chronic" has been applied to symptomatic DVT that persists longer than 10 to 14 days.[59] DVT that has no symptoms, but is found only by screening, is labeled asymptomatic or incidental.[60][61] An initial episode of DVT is called incident and any subsequent DVT is termed recurrent.[62][63] Bilateral DVT refers to clots in both legs while unilateral means that only a single leg is affected.[64]
DVT in the legs is proximal when above the knee and distal (or calf) when below the knee.[65][66] DVT below the popliteal vein, a proximal vein behind the knee, is classified as distal[57] and has limited clinical significance compared to proximal DVT.[67] Iliofemoral DVT involves at a minimum the common iliac vein (see image below).[11] Upper extremity DVT occurs in the arms or the base of the neck. Phlegmasia alba dolens and phlegmasia cerulea dolens occur when a DVT is very large and causes significant obstruction of the veins (complete or near-complete occlusion). In the former, the affected leg is white and painful as the congestion is so severe that the arterial blood supply is reduced. In the latter, the arterial supply is reduced to the point that there is a blue tinge and venous gangrene can develop, generally with severe pain.[68][58]
-
The iliac veins (in the pelvis) include the external iliac vein, the internal iliac vein, and the common iliac vein
Probability

In those with suspected DVT, a clinical assessment of probability can be useful to determine which tests to perform.[69][70] The most studied clinical prediction rule is the Wells score.[12][71]
Wells score or criteria: (possible score −2 to 9)
- Active cancer (treatment within last 6 months or palliative): +1 point
- Calf swelling ≥ 3 cm compared to asymptomatic calf (measured 10 cm below tibial tuberosity): +1 point
- Swollen unilateral superficial veins (non-varicose, in symptomatic leg): +1 point
- Unilateral pitting edema (in symptomatic leg): +1 point
- Previous documented DVT: +1 point
- Swelling of entire leg: +1 point
- Localized tenderness along the deep venous system: +1 point
- Paralysis, paresis, or recent cast immobilization of lower extremities: +1 point
- Recently bedridden ≥ 3 days, or major surgery requiring regional or general anesthetic in the past 12 weeks: +1 point
- Alternative diagnosis at least as likely: −2 points[10]
Those with Wells scores of two or more have a 28% chance of having DVT, those with a lower score have 6% probability. Alternatively, Wells scores can be categorized as high if greater than two, moderate if one or two, and low if less than one, with likelihoods of 53%, 17%, and 5%, respectively.[12][13]
D-dimer

D-dimers are a fibrin degradation product, and an elevated level can result from plasmin dissolving a clot—or other conditions.[54] Hospitalized patients often have elevated levels for multiple reasons.[12][72] When individuals are at a high-probability of having DVT, diagnostic imaging is preferred to a D-dimer test.[70][73] For those with a low or moderate probability of DVT, a D-dimer level can be obtained, which excludes a diagnosis if results are normal.[54] An elevated level requires further investigation with diagnostic imaging to confirm or exclude the diagnosis.[74][75]
For a suspected first leg DVT in a low-probability situation, the American College of Chest Physicians recommends testing either D-dimer levels with moderate or high sensitivity or compression ultrasound of the proximal veins. These options are suggested over whole-leg ultrasound, and D-dimer testing is the suggested preference overall.[74] The UK National Institute for Health and Care Excellence (NICE) recommends D-dimer testing prior to proximal vein ultrasound.[70]
For a suspected first leg DVT in a moderate-probability scenario, a high-sensitivity D-dimer is suggested as a recommended option over ultrasound imaging, with both whole-leg and compression ultrasound possible.[75] The NICE guideline uses a two-point Wells score and does not refer to a moderate probability group.[70]
Imaging
Imaging tests of the veins are used in the diagnosis of DVT, most commonly either proximal compression ultrasound or whole-leg ultrasound. Each technique has drawbacks: a single proximal scan might miss a distal DVT, while whole-leg scanning can lead to distal DVT overtreatment.[12] Doppler ultrasound,[76] CT scan venography, MRI venography, or MRI of the thrombus are also possibilities.[12][74]
Ultrasonography for suspected deep vein thrombosis has a sensitivity of 97% in detecting DVTs of the proximal legs.[77]
The gold standard for judging imaging methods is contrast venography, which involves injecting a peripheral vein of the affected limb with a contrast agent and taking X-rays, to reveal whether the venous supply has been obstructed. Because of its cost, invasiveness, availability, and other limitations, this test is rarely performed.[12] In one study, it found a DVT in an additional 20% of patients with pulmonary embolism where an ultrasonography was negative.[78]
-
An ultrasound with a blood clot visible in the left common femoral vein. (The common femoral vein is distal to the external iliac vein.)
-
Doppler ultrasonography showing absence of flow and hyperechogenic content in a clotted femoral vein (labeled subsartorial) distal to the branching point of the deep femoral vein. (Subsartorial is a proposed name for a section of the femoral vein.)[79]
-
An abdominal CT scan demonstrating an iliofemoral DVT, with the clot in the right common iliac vein of the pelvis
Prevention

For the prevention of blood clots in the general population, the Centers for Disease Control and Prevention recommends an active lifestyle including leg exercises and walking when sitting for hours at a time as well as maintaining a healthy body weight.[80] Walking and leg exercises reduce venous stasis because leg muscle contractions compress the veins and pump blood up towards the heart.[81] Excess body weight is another risk factor that can be modified, and as such, interventions and lifestyle modifications that help someone lose weight work to reduce DVT risk.[32] Depending upon the risk for DVT, different preventive measures can be recommended. In immobile individuals, physical compression methods improve blood flow.
Anticoagulation, which increases the risk of bleeding, is sometimes used in high-risk scenarios. The risk of major bleeding with long-term anticoagulation is about 3% per year,[23] and the point where annual VTE risk is thought to warrant long-term anticoagulation is estimated to be between 3 and 9%.[82] Usually, only when individuals exceed a 9% annual VTE risk is long-term anticoagulation a common consideration.[82] For example, antithrombin deficiency, a strong or moderately strong risk factor, carries an annual risk of VTE of only 0.8–1.5%;[23] as such, asymptomatic individuals with thrombophilia do not warrant long-term anticoagulation.[83]
Statins have been investigated as a potential primary prevention measure to reduce VTE occurrence. The JUPITER trial, which used rosuvastatin, has provided some tentative evidence of effectiveness.[84][7] Out of all the statins that have been studied, rosuvastatin appears to be the only one with the potential to reduce VTE risk.[85]
Hospital (non-surgical) patients

A 2014 Cochrane review found that using heparin in medical patients did not change the risk of death or pulmonary embolism.[86] While its use decreased people's risks of DVTs, it also increased people's risks of major bleeding.[86] The review thus recommended the need to balance risks and benefits.[86]
The 2012 ACCP guidelines for nonsurgical patients[87][i] recommend anticoagulation for the acutely ill in cases of elevated risk when neither bleeding nor a high risk of bleeding exists.[88] Mechanical prophylaxis is suggested when risks for bleeding and thrombosis are elevated.[89] For the critically ill, either pharmacological or mechanical prophylaxis is suggested depending upon the risk.[90] Heparin can also be used in outpatients with cancer who have solid tumors and additional risk factors for VTE—listed as "previous venous thrombosis, immobilization, hormonal therapy, angiogenesis inhibitors, thalidomide, and lenalidomide"—and a low risk of bleeding.[91]
After surgery

Major orthopedic surgery—total hip replacement, total knee replacement, or hip fracture surgery—has a high risk of causing VTE.[92] If prophylaxis is not used after these surgeries, symptomatic VTE has about a 4% chance of developing within 35 days.[93] Options for VTE prevention in people following nonorthopedic surgery include early walking, mechanical prophylaxis (intermittent pneumatic compression or graduated compression stockings), and drugs (low-molecular-weight heparin and low-dose-unfractionated heparin) depending upon the risk of VTE, risk of major bleeding, and person's preferences.[94] Following major orthopedic surgery, the ACCP recommends treatment with drugs that reduce the risk of clots (such as fondaparinux and aspirin) with low-molecular-weight heparin (LMWH) suggested as a preference.[93] Intermittent pneumatic compression is also an option.[93][95] Graduated compression stockings are effective after both general and orthopedic surgery.[5]
Pregnancy
The risk of VTE is increased in pregnancy by about five times[23][96] because of a more hypercoagulable state, a likely adaptation against fatal postpartum hemorrhage.[97] Additionally, pregnant women with genetic risk factors are subject to a roughly three to 30 times increased risk for VTE.[98] Preventive treatments for pregnancy-related VTE in hypercoagulable women were suggested by the ACCP in 2012. Homozygous carriers of factor V Leiden or prothrombin G20210A with a family history of VTE were suggested for antepartum LMWH and either LMWH or a vitamin K antagonist (VKA) for the six weeks following childbirth. Those with another thrombophilia and a family history but no previous VTE were suggested for watchful waiting during pregnancy and LMWH or—for those without protein C or S deficiency—a VKA. Homozygous carriers of factor V Leiden or prothrombin G20210A with no personal or family history of VTE were suggested for watchful waiting during pregnancy and LMWH or a VKA for six weeks after childbirth. Those with another thrombophilia but no family or personal history of VTE were suggested for watchful waiting only.[99] Warfarin, a common VKA, can cause harm to the fetus and is not used for VTE prevention during pregnancy.[98][100]
Travelers

Suggestions for at-risk long-haul travelers[j] include calf exercises, frequent walking, and aisle seating in airplanes to ease walking.[101][102] Graduated compression stockings have sharply reduced the levels of asymptomatic DVT in airline passengers, but the effect on symptomatic DVT, PE, or mortality is unknown, as none of the individuals studied developed these outcomes.[103] However, graduated compression stockings are not suggested for long-haul travelers (>4 hours) without risk factors for VTE. Likewise, neither aspirin nor anticoagulants are suggested in the general population undertaking long-haul travel.[104] Those with significant VTE risk factors[k] undertaking long-haul travel are suggested to use either graduated compression stockings or LMWH for VTE prevention. If neither of these two methods are feasible, then aspirin is suggested.[104]
Treatment
Anticoagulation
Treatment for DVT is warranted when the clots are either proximal, distal and symptomatic, or upper extremity and symptomatic.[105] Anticoagulation, which prevents further coagulation, but does not act directly on existing clots, is the standard treatment for DVT.[106][l] Balancing risk vs. benefit is important in determining the duration of anticoagulation, and three months is generally the standard length of treatment.[70] In those with an annual risk of VTE in excess of 9%, as after an unprovoked episode, extended anticoagulation is a possibility.[82] Those who finish VKA treatment after idiopathic VTE with an elevated D-dimer level show an increased risk of recurrent VTE (about 9% vs about 4% for normal results), and this result might be used in clinical decision-making.[108] Thrombophilia test results rarely play a role in the length of treatment.[38] Two forms of direct oral anticoagulants (DOACs) have been developed: oral direct thrombin inhibitors and oral factor Xa inhibitors, which can be an effective and safe alternative to warfarin for acute DVT.[109]
For acute cases in the leg, the ACCP recommended a parenteral anticoagulant (such as LMWH, fondaparinux, or unfractionated heparin) for at least five days[m] and a VKA, the oral anticoagulant, the same day. LMWH and fondaparinux are suggested over unfractionated heparin, but both are retained in those with compromised kidney function, unlike unfractionated heparin.[111][112] The VKA is generally taken for a minimum of three months[113] to maintain an international normalized ratio of 2.0–3.0, with 2.5 as the target.[114][115] The benefit of taking a VKA declines as the duration of treatment extends,[116] and the risk of bleeding increases with age.[15]
The ACCP recommended treatment for three months in those with proximal DVT provoked by surgery.[117] A three-month course is also recommended for those with proximal DVT provoked by a transient risk factor, and three months is suggested over lengthened treatment when bleeding risk is low to moderate.[118] Unprovoked DVT patients should have at least three months of anticoagulation and be considered for extended treatment.[119] Those whose first VTE is an unprovoked proximal DVT are suggested for anticoagulation longer than three months unless there is a high risk of bleeding.[120] In that case, three months is sufficient.[121] Those with a second unprovoked VTE are recommended for extended treatment when bleeding risk is low, suggested for extended treatment when bleeding risk is moderate,[122] and suggested for three months of anticoagulation in high-risk scenarios.[123]
Stockings, walking, and repeat imaging
The ACCP recommended initial home treatment instead of hospital treatment for those with acute leg DVT. This applies as long as individuals feel ready for it, and those with severe leg symptoms or comorbidities would not qualify. An appropriate home environment is expected: one that can provide a quick return to the hospital if necessary, support from family or friends, and phone access.[124] Walking is suggested for those without severe pain or edema.[125] Graduated compression stockings—which apply higher pressure at the ankles and a lower pressure around the knees[111] might be used for symptomatic management of acute DVT symptoms, but they are not recommended for reducing the risk of post-thrombotic syndrome,[126] as the potential benefit of using them for this goal "may be uncertain".[10] Nor are compression stockings likely to reduce VTE recurrence.[127]
Instead of anticoagulation, a follow-up imaging test (typically ultrasound) about one-week post-diagnosis is an option for those with an acute isolated distal DVT without a high risk for extension; if the clot does not grow, the ACCP does not recommend anticoagulation.[111][128] This technique can benefit those at a high risk for bleeding. Patients can choose anticoagulation over serial imaging, however, to avoid the inconvenience of another scan if concerns about the risk of bleeding are insignificant.[128] When applied to symptomatic patients with a negative initial ultrasound result, serial testing is inefficient and not cost effective.[57]
Interventions
Thrombolysis is the injection of an enzyme into the veins to dissolve blood clots, and while this treatment has been proven effective against the life-threatening emergency clots of stroke and heart attacks, randomized controlled trials[129][130][131] have not established a net benefit in those with acute proximal DVT.[10][132] Drawbacks of catheter-directed thrombolysis (the preferred method of administering the clot-busting enzyme[10]) include a risk of bleeding, complexity,[n] and the cost of the procedure.[126] Thus, anticoagulation is the preferred treatment for DVT.[126] However, this preference does not apply to those with DVT so severe that there is "impending venous gangrene".[126] As of 2016, those thought to be the best candidates for catheter-directed thrombosis have iliofemoral DVT, symptoms for less than 14 days, good functional status (ability to perform one's activities of daily living), life expectancy of at least 1 year, and a low risk of bleeding.[70][126] Phlegmasia cerulea dolens (bottom left image) might be treated with catheter-directed thrombolysis.[11] Of note, however, is that a variety of contraindications to thrombolysis exist.[126] Identifying who might benefit from thrombolysis is a goal of future research.[132]
-
Phlegmasia cerulea dolens (literally: painful blue edema) is a particularly severe form of acute, proximal, and occlusive DVT. It is life-threatening and limb-threatening.[133]
-
A venogram before catheter-directed thrombolysis against Paget–Schroetter syndrome, a rare and severe arm DVT shown here in a judo practitioner, with highly restricted blood flow shown in the vein
-
After treatment with catheter-directed thrombolysis, blood flow in the axillary and subclavian vein were significantly improved. Afterwards, a first rib resection provided thoracic outlet decompression to reduce the risk of recurrent DVT and the risk of sequelae from thoracic outlet compression.[134]

Inferior vena cava filters (IVC filters) are not recommended for those using the standard treatment for acute DVT, anticoagulation.[126] NICE recommends IVC filters in settings where someone with an acute proximal DVT or PE cannot receive anticoagulation, and that the filter is removed when anticoagulation can be safely started.[70] They are used on the presumption that they reduce PE, although their effectiveness and safety profile are not well established.[135] In general, they are only recommended in some high-risk scenarios.[135] The ACCP recommended them for those with a contraindication to anticoagulant treatment but not in addition to anticoagulation, unless an individual with an IVC filter but without a risk for bleeding develops acute proximal DVT. In this case, both anticoagulation and an IVC filter were suggested.[136] While IVC filters themselves are associated with a long-term risk of DVT,[135] they are not reason enough to maintain extended anticoagulation.[137] In 2017, an expert panel with the American College of Cardiology stated that the judicious use of IVC filters was critical.[138]
A mechanical thrombectomy device can remove venous clots, although the ACCP considers it an option only when the following conditions apply: "iliofemoral DVT, symptoms for < 7 days (criterion used in the single randomized trial), good functional status, life expectancy of ≥ 1 year, and both resources and expertise are available."[111] Anticoagulation alone is suggested over thrombectomy.[139]
Prognosis

PE is the most serious complication of proximal DVT, and the risk of PE is higher when clots are present in the thigh and pelvis.[135] Distal DVT is hardly if ever associated with PE.[12] Around 56% of those with proximal DVT have PE as well, although a chest CT is not needed simply because of the presence of a DVT.[140] If proximal DVT is left untreated, in the following 3 months approximately half of people will experience symptomatic PE.[6] Untreated lower extremity DVT has a 3% PE-related mortality rate, while deaths associated with upper extremity DVT are extremely rare.[141]
Another frequent complication of proximal DVT is post-thrombotic syndrome,[142] which is caused by a reduction in the return of venous blood to the heart.[24] Some symptoms of post-thrombotic syndrome are pain, edema, paresthesia, and in severe cases, leg ulcers. After DVT, an estimated 20–50% of people develop the syndrome and 5–10% develop the severe form.[142]
The presence of a remaining thrombus after a DVT occurs in a minority of people, and it increases the risk of recurrence, though to a lesser extent than an elevated D-dimer.[24] VTE recurrence in those with prior DVT is more likely to recur as DVT than PE.[143] Cancer[10] and unprovoked DVT are strong risk factors for recurrence.[22] In individuals who have an initial proximal unprovoked DVT, about 16% will have recurrent VTE in the 2 years after they complete their course of anticoagulants. If DVT and PE manifest together for an inital unprovoked DVT, the rate of recurrence in this timeframe is about 17%. VTE recurrence is less common in distal DVT than proximal DVT.[144] In the 10 years following an inital VTE, approximately a third of people will have a recurrence.[145] In upper extremity DVT, annual VTE recurrence is about 2–4%.[15] After surgery, a provoked proximal DVT or PE has an annual recurrence rate of only 0.7%.[22]
A seemingly unprovoked VTE might suggest the presence of an undiagnosed cancer,[146] but it is not common practice to screen people with unprovoked VTE for the presence of cancer.[22] Scanning individuals with a CT of the abdomen and pelvis in this scenario has not proven beneficial.[147]
Epidemiology
About 1.5 out of 1000 adults a year have a first VTE in high-income countries.[148][149] VTE is rare in children, with an incidence of about 1 in 100,000 a year. From childhood to old age, incidence increases by a factor of about 1000, with almost 1% of the elderly experiencing VTE yearly.[150] About 60% of all VTEs occur in those 70 years of age or older.[6] DVT occurs in the upper extremities in about 4–10% of cases.[8] A minority of upper extremity DVTs are due to Paget–Schroetter syndrome, also called effort thrombosis, which occurs in 1–2 people out of 100,000 a year, usually in athletic males around 30 years of age or in those who do significant amounts of overhead manual labor.[28][134]
During pregnancy and after childbirth, acute VTE occurs about 1.2 of 1000 deliveries. Despite it being relatively rare, it is a leading cause of maternal morbidity and mortality.[151] After surgery with preventive treatment, VTE develops in about 10 of 1000 people after total or partial knee replacement, and in about 5 of 1000 after total or partial hip replacement.[152] About 400,000 Americans develop an initial VTE each year, with 100,000 deaths or more attributable to PE.[149] In England, an estimated 25,000 a year die from hospital-related VTE.[153] For unclear reasons, people of Asian descent have a lower VTE risk than whites.[9]
In North American and European populations, around 4–8% of people have a thrombophilia,[23] most commonly factor V leiden and prothrombin G20210A. For populations in China, Japan, and Thailand, deficiences in protein S, protein C, and antithrombin predominate.[154] Non-O blood type is present in around 50% of the general population and varies with ethnicity, and it is present in about 70% of those with VTE.[34][155] Altogether, global data is incomplete.[156] As of 2011, available data was dominated by North American and European populations.[9]
Social

Being on blood thinners because of DVT can be life-changing for patients because it may prevent them from continuing lifestyle activities such as contact or winter sports to prevent bleeding episodes after potential injuries.[158] Head injuries prompting brain bleeds are of particular concern. This has caused NASCAR driver Brian Vickers to forego participation in races. Professional basketball players including NBA players Chris Bosh and hall of famer Hakeem Olajuwon have dealt with recurrent blood clots,[159] and Bosh's career was significantly hampered by DVT and PE.[160] Tennis star Serena Williams was hospitalized in 2011 for PE thought to have originated from a DVT.[161] Due to her knowledge of DVT and PE, in 2017, after feeling the sudden onset of a PE symptom, Serena accurately advocated for herself to have PE diagnosed and treated.[157]
Other notable people have been affected by DVT. Former US President Richard Nixon had recurrent DVT,[162] and so has former Secretary of State Hillary Clinton. She was first diagnosed while First Lady in 1998 and again in 2009.[163] Dick Cheney was diagnosed with an episode while Vice President,[164] and TV show host Regis Philbin had a DVT after hip-replacement surgery.[165] DVT has also contributed to the deaths of famous people. For example, DVT and PE played a role in rapper Heavy D's death.[166] NBC journalist David Bloom died while covering the Iraq War from a PE that was thought to have progressed from a missed DVT.[167] And actor Jimmy Stewart had a DVT that progressed to a fatal PE when he was 87.[165]
Field of medicine
Patients with a history of DVT might be managed by primary care, general internal medicine, hematology, cardiology, vascular surgery, or vascular medicine.[168] Patients suspected of having an acute DVT are often referred to the emergency department for evaluation.[169] Interventional radiology is the specialty that typically places and retrieves IVC filters,[170] and vascular surgery might do catheter directed thrombosis for some severe DVTs.[134]
History


The earliest case of DVT was described by Sushruta in his book Sushruta Samhita around 600–900 BC.[171] The next case was not described until 1271, in the leg of a 20-year-old male.[171][172] At some point, the increased incidence of DVT in women after childbirth was noticed, and in the late 1700s, a public health recommendation was issued to encourage women to breastfeed as a means to prevent this phenomenon; the DVT was called "milk leg", as it was thought to result from milk building up in the leg.[173]
In 1856, German physician and pathologist Rudolf Virchow published what is referred to as Virchow's triad, the three major causes of thrombosis.[20][173] The triad provides the theoretical framework for the current explanation of venous thrombosis,[20] although it was focused on the effect of a foreign body in the venous system and the conditions required for clot propagation.[174]
Multiple pharmacological therapies for DVT were introduced in the 20th century: oral anticoagulants in the 1940s, subcutaneous injections of LDUH in 1962 and subcutaneous injections of LMWH in 1982.[175] For around 50 years, a months-long warfarin (Coumadin) regimen was the mainstay of pharmacological treatment after several days of using a subcutaneous heparin.[176][177] To avoid the blood monitoring required with warfarin and the injections required by heparin and heparin-like medicines, a new generation of anticoagulant pills that can be taken by mouth and do not require blood monitoring has sought to replace these traditional anticoagulants.[177] In the late 2000s to early 2010s, direct oral anticoagulants—including dabigatran (Pradaxa), rivaroxaban (Xarelto), and apixaban (Eliquis)—came to the market, making this field of medicine fast changing.[22] The New York Times described a "furious battle" among the three makers of these drugs "for the prescription pads of doctors".[176]
Diagnoses were commonly performed by impedance plethysmography in the 1970s and 1980s, but the use of Doppler ultrasound techniques, with their increased sensitivity and specificity, largely superseded this method.[178]
Economics
Initial DVT costs for an average hospitalized patient in the U.S. are around $7,700–$10,800.[179] VTE follow-up costs at three months, six months, and a year are about $5,000, $10,000, and $33,000 respectively; in Europe, the three and six-month figures are about €1,800 and €3,200.[180] Post-thrombotic syndrome is a significant contributor to DVT follow-up costs.[179] Annual DVT costs in the U.S. are an estimated $5 billion[181] or in excess of $8 billion,[182][183] and the average annual cost per treated individual is thought to be about $20,000.[182] As an example, if 300,000 symptomatic DVT patients were treated at costs averaging $20,000 annually, that would cost $6 billion a year.
Research directions
A 2019 study published in Nature Genetics expanded the known genetic loci associated with VTE from 11 to 33.[7] In their updated 2018 clinical practice guidelines, the American Society of Hematology identified 29 separate research priorities, most of which related to patients who are acutely or critically ill.[104] Inhibition of Factor XI, P-selectin, E-selectin, and a reduction in formation of neutrophil extracellular traps are potential therapies that might treat VTE without increasing bleeding risk.[184]
See also
Notes
- ^ Thrombosis associated with the head (cerebral venous sinus thrombosis) and the abdominal organs (viscera)—such as portal vein thrombosis, renal vein thrombosis, and Budd–Chiari syndrome—are separate diseases excluded from the scope of this definition.
- ^ Third-generation combined oral contraceptives (COCs) have an approximate two to three times higher risk than second-generation COCs.[24] Progestogen-only pill use is not associated with increased VTE risk.[31]
- ^ Type I[20]
- ^ Factor V Leiden increases the risk of DVT more than it does for PE, a phenomenon referred to as the factor V Leiden paradox.[33]
- ^ "It is important to note that smoking is not an independent risk factor, although it increases the risk for cancers and other comorbidities and works synergistically with other independent risk factors."[47]
- ^ The term 'thrombophilia' as used here applies to the five inherited abnormalities of antithrombin, protein C, protein S, factor V, and prothrombin, as is done elsewhere.[23][48]
- ^ VTE might cause the observed inflammation.[19]
- ^ An elevated level is greater than 250 ng/mL D-dimer units (DDU) or greater than 0.5 μg/mL fibrinogen equivalent units (FEU).[54] A normal level is below these values.
- ^ Page e197S of Kahn et al.[87] specifies that the guideline does not apply to those with "trauma and spinal cord injury" nor does it apply to those "with ischemic and hemorrhagic stroke."
- ^ Specified as those with "previous VTE, recent surgery or trauma, active malignancy, pregnancy, estrogen use, advanced age, limited mobility, severe obesity, or known thrombophilic disorder"
- ^ For example "recent surgery, history of VTE, postpartum women, active malignancy, or ≥2 risk factors, including combinations of the above with hormone replacement therapy, obesity, or pregnancy"[104]
- ^ Evidence for anticoagulation comes from studies other than definitive randomized controlled trials that demonstrate efficacy and safety for anticoagulation vs. placebo or using NSAIDs.[107]
- ^ The international normalized ratio should be ≥ 2.0 for 24 hours minimum,[110] but if the ratio is > 3.0, then the parenteral anticoagulant is not needed for five days.[111]
- ^ "Up to 83% of patients treated by any catheter-based therapy, need adjunctive angioplasty, and stenting".[10]
References
- ^ a b c d e f g h i j k l m "Deep Vein Thrombosis". NHLBI, NIH. Archived from the original on 14 December 2017. Retrieved 14 December 2017.
- ^ a b c d e f g h "Deep Venous Thrombosis (DVT)". Merck Manuals Professional Edition. July 2016. Archived from the original on 5 November 2017. Retrieved 15 December 2017.
- ^ a b c Ferri, Fred F. (2017). Ferri's Clinical Advisor 2018 E-Book: 5 Books in 1. Elsevier Health Sciences. p. 357. ISBN 9780323529570. Archived from the original on 15 December 2017.
- ^ a b c "Deep Venous Thrombosis Prevention – Cardiovascular Disorders – Merck Manuals Professional Edition". Merck Manuals Professional Edition. July 2016. Archived from the original on 18 September 2017. Retrieved 15 December 2017.
- ^ a b Sachdeva A, Dalton M, Lees T (November 2018). Cochrane Vascular Group (ed.). "Graduated compression stockings for prevention of deep vein thrombosis". The Cochrane Database of Systematic Reviews. 11: CD001484. doi:10.1002/14651858.CD001484.pub4. PMC 6477662. PMID 30390397.
- ^ a b c d e f Phillippe HM (December 2017). "Overview of venous thromboembolism". The American Journal of Managed Care. 23 (20 Suppl): S376–S382. PMID 29297660.
- ^ a b c d e f Klarin D, Busenkell E, Judy R, Lynch J, Levin M, Haessler J, et al. (November 2019). "Genome-wide association analysis of venous thromboembolism identifies new risk loci and genetic overlap with arterial vascular disease" (PDF). Nature Genetics. 51 (11): 1574–1579. doi:10.1038/s41588-019-0519-3. PMC 6858581. PMID 31676865.
- ^ a b c d e Heil J, Miesbach W, Vogl T, Bechstein WO, Reinisch A (April 2017). "Deep Vein Thrombosis of the Upper Extremity". Deutsches Arzteblatt International. 114 (14): 244–249. doi:10.3238/arztebl.2017.0244. PMC 5415909. PMID 28446351.
- ^ a b c Zakai NA, McClure LA (October 2011). "Racial differences in venous thromboembolism". Journal of Thrombosis and Haemostasis. 9 (10): 1877–82. doi:10.1111/j.1538-7836.2011.04443.x. PMID 21797965.
- ^ a b c d e f g h Mazzolai L, Aboyans V, Ageno W, Agnelli G, Alatri A, Bauersachs R, et al. (December 2018). "Diagnosis and management of acute deep vein thrombosis: a joint consensus document from the European Society of Cardiology working groups of aorta and peripheral vascular diseases and pulmonary circulation and right ventricular function". European Heart Journal. 39 (47): 4208–4218. doi:10.1093/eurheartj/ehx003. PMID 28329262.
- ^ a b c d e Tran HA, Gibbs H, Merriman E, Curnow JL, Young L, Bennett A, et al. (March 2019). "New guidelines from the Thrombosis and Haemostasis Society of Australia and New Zealand for the diagnosis and management of venous thromboembolism". The Medical Journal of Australia. 210 (5): 227–235. doi:10.5694/mja2.50004. PMID 30739331.
- ^ a b c d e f g h Bates SM, Jaeschke R, Stevens SM, Goodacre S, Wells PS, Stevenson MD, et al. (February 2012). "Diagnosis of DVT: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines". Chest. 141 (2 Suppl): e351S–e418S. doi:10.1378/chest.11-2299. PMC 3278048. PMID 22315267.
- ^ a b Hargett CW, Tapson VF (February 2008). "Clinical probability and D-dimer testing: how should we use them in clinical practice?". Seminars in Respiratory and Critical Care Medicine. 29 (1): 15–24. doi:10.1055/s-2008-1047559. PMID 18302083.
- ^ Arumilli BR, Lenin Babu V, Paul AS (January 2008). "Painful swollen leg—think beyond deep vein thrombosis or Baker's cyst". World Journal of Surgical Oncology. 6: 6. doi:10.1186/1477-7819-6-6. PMC 2244628. PMID 18205917.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ a b c de Jong PG, Coppens M, Middeldorp S (August 2012). "Duration of anticoagulant therapy for venous thromboembolism: balancing benefits and harms on the long term". British Journal of Haematology. 158 (4): 433–41. doi:10.1111/j.1365-2141.2012.09196.x. PMID 22734929.
- ^ Qaseem A, Chou R, Humphrey LL, Starkey M, Shekelle P (November 2011). "Venous thromboembolism prophylaxis in hospitalized patients: a clinical practice guideline from the American College of Physicians". Annals of Internal Medicine. 155 (9): 625–32. CiteSeerX 10.1.1.689.591. doi:10.7326/0003-4819-155-9-201111010-00011. PMID 22041951.
- ^ a b c d e f g h i j k Martinelli I, Bucciarelli P, Mannucci PM (February 2010). "Thrombotic risk factors: basic pathophysiology". Critical Care Medicine. 38 (2 Suppl): S3-9. doi:10.1097/CCM.0b013e3181c9cbd9. PMID 20083911.
- ^ a b c d e Bovill EG, van der Vliet A (2011). "Venous valvular stasis-associated hypoxia and thrombosis: what is the link?". Annual Review of Physiology. 73: 527–45. doi:10.1146/annurev-physiol-012110-142305. PMID 21034220.
- ^ a b c d e f g h Reitsma PH, Versteeg HH, Middeldorp S (March 2012). "Mechanistic view of risk factors for venous thromboembolism". Arteriosclerosis, Thrombosis, and Vascular Biology. 32 (3): 563–8. doi:10.1161/ATVBAHA.111.242818. PMID 22345594.
- ^ a b c d e f g h i Lijfering WM, Rosendaal FR, Cannegieter SC (June 2010). "Risk factors for venous thrombosis - current understanding from an epidemiological point of view". British Journal of Haematology. 149 (6): 824–33. doi:10.1111/j.1365-2141.2010.08206.x. PMID 20456358.
- ^ Tzoran I, Hoffman R, Monreal M (October 2018). "Hemostasis and Thrombosis in the Oldest Old". Seminars in Thrombosis and Hemostasis. 44 (7): 624–631. doi:10.1055/s-0038-1657779. PMID 29920621.
- ^ a b c d e Keeling D, Alikhan R (June 2013). "Management of venous thromboembolism--controversies and the future". British Journal of Haematology. 161 (6): 755–63. doi:10.1111/bjh.12306. PMID 23531017.
- ^ a b c d e f g Varga EA, Kujovich JL (January 2012). "Management of inherited thrombophilia: guide for genetics professionals". Clinical Genetics. 81 (1): 7–17. doi:10.1111/j.1399-0004.2011.01746.x. PMID 21707594.
- ^ a b c d e Wong P, Baglin T (2012). "Epidemiology, risk factors and sequelae of venous thromboembolism". Phlebology. 27 (Suppl 2): 2–11. doi:10.1258/phleb.2012.012S31. PMID 22457300.
- ^ a b c Rosendaal FR, Reitsma PH (July 2009). "Genetics of venous thrombosis". Journal of Thrombosis and Haemostasis. 7 (Suppl 1): 301–4. doi:10.1111/j.1538-7836.2009.03394.x. PMID 19630821.
- ^ Winstein CJ, Stein J, Arena R, Bates B, Cherney LR, Cramer SC, et al. (June 2016). "Guidelines for Adult Stroke Rehabilitation and Recovery: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association". Stroke. 47 (6): e98–e169. doi:10.1161/STR.0000000000000098. PMID 27145936.
- ^ Béliard S, Feuvrier D, Ducroux E, Salomon du Mont L (2018). "May Thurner syndrome revealed by left calf venous claudication during running, a case report". BMC Sports Science, Medicine & Rehabilitation. 10: 3. doi:10.1186/s13102-018-0092-6. PMC 5796503. PMID 29435334.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ a b Hangge P, Rotellini-Coltvet L, Deipolyi AR, Albadawi H, Oklu R (December 2017). "Paget-Schroetter syndrome: treatment of venous thrombosis and outcomes". Cardiovascular Diagnosis and Therapy. 7 (Suppl 3): S285–S290. doi:10.21037/cdt.2017.08.15. PMC 5778512. PMID 29399532.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Jabri H, Mukherjee S, Sanghavi D, Chalise S (2014). "Bilateral Upper Extremity DVT in a 43-Year-Old Man: Is It Thoracic Outlet Syndrome?!". Case Reports in Medicine. 2014: 758010. doi:10.1155/2014/758010. PMC 4129160. PMID 25140182.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Falanga A, Russo L, Milesi V, Vignoli A (October 2017). "Mechanisms and risk factors of thrombosis in cancer". Critical Reviews in Oncology/Hematology. 118: 79–83. doi:10.1016/j.critrevonc.2017.08.003. PMID 28917273.
- ^ Mantha S, Karp R, Raghavan V, Terrin N, Bauer KA, Zwicker JI (August 2012). "Assessing the risk of venous thromboembolic events in women taking progestin-only contraception: a meta-analysis". BMJ. 345: e4944. doi:10.1136/bmj.e4944. PMC 3413580. PMID 22872710.
- ^ a b c d Shaheen K, Alraies MC, Alraiyes AH, Christie R (April 2012). "Factor V Leiden: how great is the risk of venous thromboembolism?". Cleveland Clinic Journal of Medicine. 79 (4): 265–72. doi:10.3949/ccjm.79a.11072. PMID 22473726.
- ^ van Langevelde K, Flinterman LE, van Hylckama Vlieg A, Rosendaal FR, Cannegieter SC (August 2012). "Broadening the factor V Leiden paradox: pulmonary embolism and deep-vein thrombosis as 2 sides of the spectrum". Blood. 120 (5): 933–46. doi:10.1182/blood-2012-02-407551. PMID 22496157.
- ^ a b c Dentali F, Sironi AP, Ageno W, Turato S, Bonfanti C, Frattini F, et al. (July 2012). "Non-O blood type is the commonest genetic risk factor for VTE: results from a meta-analysis of the literature". Seminars in Thrombosis and Hemostasis. 38 (5): 535–48. doi:10.1055/s-0032-1315758. PMID 22740183.
- ^ a b Tichelaar YI, Kluin-Nelemans HJ, Meijer K (May 2012). "Infections and inflammatory diseases as risk factors for venous thrombosis. A systematic review". Thrombosis and Haemostasis. 107 (5): 827–37. doi:10.1160/TH11-09-0611. PMID 22437808.
- ^ Becatti M, Emmi G, Bettiol A, Silvestri E, Di Scala G, Taddei N, Prisco D, Fiorillo C (March 2019). "Behçet's syndrome as a tool to dissect the mechanisms of thrombo-inflammation: clinical and pathogenetic aspects". Clinical and Experimental Immunology. 195 (3): 322–333. doi:10.1111/cei.13243. PMID 30472725.
- ^ Zöller B, Li X, Sundquist J, Sundquist K (January 2012). "Risk of pulmonary embolism in patients with autoimmune disorders: a nationwide follow-up study from Sweden". Lancet. 379 (9812): 244–9. doi:10.1016/S0140-6736(11)61306-8. PMID 22119579.
- ^ a b Baglin T (April 2012). "Inherited and acquired risk factors for venous thromboembolism". Seminars in Respiratory and Critical Care Medicine. 33 (2): 127–37. doi:10.1055/s-0032-1311791. PMID 22648484.
- ^ Knight CL, Nelson-Piercy C (2017). "Management of systemic lupus erythematosus during pregnancy: challenges and solutions". Open Access Rheumatology. 9: 37–53. doi:10.2147/OARRR.S87828. PMC 5354538. PMID 28331377.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Svenungsson E, Antovic A (January 2020). "The Antiphospholipid Syndrome -often overlooked cause of vascular occlusions?". Journal of Internal Medicine. doi:10.1111/joim.13022. PMID 31957081.
- ^ Greinacher A, Selleng K, Warkentin TE (November 2017). "Autoimmune heparin-induced thrombocytopenia". Journal of Thrombosis and Haemostasis. 15 (11): 2099–2114. doi:10.1111/jth.13813. PMID 28846826.
- ^ Rana MA, Mady AF, Lashari AA, Eltreafi R, Fischer-Orr N, Naser K (2018). "Lethal End of Spectrum of Clots-Thrombotic Storm". Case Reports in Critical Care. 2018: 7273420. doi:10.1155/2018/7273420. PMC 5994281. PMID 29977623.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Abdul Haium AA, Sheppard M, Rubens M, Daubeney P (July 2013). "Catastrophic antiphospholipid syndrome in childhood: presentation with an inferior caval vein mass". BMJ Case Reports. 2013. doi:10.1136/bcr-2013-010043. PMC 3736204. PMID 23861282.
- ^ Lazo-Langner A, Kovacs MJ, Hedley B, Al-Ani F, Keeney M, Louzada ML, et al. (June 2015). "Screening of patients with idiopathic venous thromboembolism for paroxysmal nocturnal hemoglobinuria clones". Thrombosis Research. 135 (6): 1107–9. doi:10.1016/j.thromres.2015.04.006. PMID 25890452.
- ^ Stephens MB (February 1997). "Deep venous thrombosis of the upper extremity". American Family Physician. 55 (2): 533–9. PMID 9054222.
- ^ Brown, Jeremy (2008). Oxford American Handbook of Emergency Medicine. p. 453.9. ISBN 9780199779482. Archived from the original on 8 January 2018.
{{cite book}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ McLendon K, Attia M (2019). "Deep Venous Thrombosis (DVT) Risk Factors". StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. PMID 29262230.
- ^ Middeldorp S (2011). "Is thrombophilia testing useful?". Hematology. American Society of Hematology. Education Program. 2011 (1): 150–5. doi:10.1182/asheducation-2011.1.150. PMID 22160027.
- ^ Palareti G, Schellong S (January 2012). "Isolated distal deep vein thrombosis: what we know and what we are doing". Journal of Thrombosis and Haemostasis. 10 (1): 11–9. doi:10.1111/j.1538-7836.2011.04564.x. PMID 22082302.
- ^ Chan WS, Spencer FA, Ginsberg JS (April 2010). "Anatomic distribution of deep vein thrombosis in pregnancy". CMAJ. 182 (7): 657–60. doi:10.1503/cmaj.091692. PMC 2855912. PMID 20351121.
- ^ a b c Saha P, Humphries J, Modarai B, Mattock K, Waltham M, Evans CE, et al. (March 2011). "Leukocytes and the natural history of deep vein thrombosis: current concepts and future directions". Arteriosclerosis, Thrombosis, and Vascular Biology. 31 (3): 506–12. doi:10.1161/ATVBAHA.110.213405. PMC 3079895. PMID 21325673.
- ^ Kim ES, Bartholomew JR. "Venous thromboembolism". Disease Management Project. Cleveland Clinic. Archived from the original on 23 February 2011. Retrieved 15 February 2011.
- ^ a b c López JA, Chen J (2009). "Pathophysiology of venous thrombosis". Thrombosis Research. 123 (Suppl 4): S30-4. doi:10.1016/S0049-3848(09)70140-9. PMID 19303501.
- ^ a b c "DDI/9290 clinical: D-dimer, plasma". Mayo Medical Laboratories. Archived from the original on 8 October 2012. Retrieved 27 August 2012.
- ^ Iorio A, Kearon C, Filippucci E, Marcucci M, Macura A, Pengo V, et al. (October 2010). "Risk of recurrence after a first episode of symptomatic venous thromboembolism provoked by a transient risk factor: a systematic review". Archives of Internal Medicine. 170 (19): 1710–6. doi:10.1001/archinternmed.2010.367. PMID 20975016.
- ^ Conklin P, Soares GM, Dubel GJ, Ahn SH, Murphy TP (December 2009). "Acute deep vein thrombosis (DVT): evolving treatment strategies and endovascular therapy" (PDF). Medicine and Health, Rhode Island. 92 (12): 394–7. PMID 20066826. Archived (PDF) from the original on 6 February 2013.
- ^ a b c Scarvelis D, Wells PS (October 2006). "Diagnosis and treatment of deep-vein thrombosis". CMAJ. 175 (9): 1087–92. doi:10.1503/cmaj.060366. PMC 1609160. PMID 17060659.
Scarvelis D, Wells PS (November 2007). "Correction: Diagnosis and treatment of deep-vein thrombosis". CMAJ. 177 (11): 1392. doi:10.1503/cmaj.071550. - ^ a b Owings JT (2005). "Management of venous thromboembolism". ACS Surgery. American College of Surgeons. Archived from the original on 27 January 2012. Retrieved 16 January 2012.
- ^ Rao AS, Konig G, Leers SA, Cho J, Rhee RY, Makaroun MS, et al. (November 2009). "Pharmacomechanical thrombectomy for iliofemoral deep vein thrombosis: an alternative in patients with contraindications to thrombolysis". Journal of Vascular Surgery. 50 (5): 1092–8. doi:10.1016/j.jvs.2009.06.050. PMID 19782528.
- ^ Lloyd NS, Douketis JD, Moinuddin I, Lim W, Crowther MA (March 2008). "Anticoagulant prophylaxis to prevent asymptomatic deep vein thrombosis in hospitalized medical patients: a systematic review and meta-analysis". Journal of Thrombosis and Haemostasis. 6 (3): 405–14. doi:10.1111/j.1538-7836.2007.02847.x. PMID 18031292.
- ^ Font C, Farrús B, Vidal L, Caralt TM, Visa L, Mellado B, et al. (September 2011). "Incidental versus symptomatic venous thrombosis in cancer: a prospective observational study of 340 consecutive patients". Annals of Oncology. 22 (9): 2101–6. doi:10.1093/annonc/mdq720. PMID 21325446.
- ^ Heit JA, Mohr DN, Silverstein MD, Petterson TM, O'Fallon WM, Melton LJ (March 2000). "Predictors of recurrence after deep vein thrombosis and pulmonary embolism: a population-based cohort study". Archives of Internal Medicine. 160 (6): 761–8. doi:10.1001/archinte.160.6.761. PMID 10737275.
- ^ Spencer FA, Emery C, Lessard D, Anderson F, Emani S, Aragam J, et al. (July 2006). "The Worcester Venous Thromboembolism study: a population-based study of the clinical epidemiology of venous thromboembolism". Journal of General Internal Medicine. 21 (7): 722–7. doi:10.1111/j.1525-1497.2006.00458.x. PMC 1924694. PMID 16808773.
- ^ Casella IB, Bosch MA, Sabbag CR (2009). "Incidence and risk factors for bilateral deep venous thrombosis of the lower limbs". Angiology. 60 (1): 99–103. doi:10.1177/0003319708316897. PMID 18504268.
- ^ Johnson SA, Stevens SM, Woller SC, Lake E, Donadini M, Cheng J, et al. (February 2010). "Risk of deep vein thrombosis following a single negative whole-leg compression ultrasound: a systematic review and meta-analysis". JAMA. 303 (5): 438–45. doi:10.1001/jama.2010.43. PMID 20124539.
- ^ Welch 2010, p. 2.
- ^ Galanaud JP, Bosson JL, Quéré I (September 2011). "Risk factors and early outcomes of patients with symptomatic distal vs. proximal deep-vein thrombosis". Current Opinion in Pulmonary Medicine. 17 (5): 387–91. doi:10.1097/MCP.0b013e328349a9e3. PMID 21832920.
- ^ Chinsakchai K, Ten Duis K, Moll FL, de Borst GJ (January 2011). "Trends in management of phlegmasia cerulea dolens". Vascular and Endovascular Surgery. 45 (1): 5–14. doi:10.1177/1538574410388309. PMID 21193462.
- ^ Guyatt et al. 2012, p. 16S: 3.1.
- ^ a b c d e f g National Institute for Health and Clinical Excellence. Clinical guideline 144: Venous thromboembolic diseases: the management of venous thromboembolic diseases and the role of thrombophilia testing. London, 2012.
- ^ Geersing GJ, Zuithoff NP, Kearon C, Anderson DR, Ten Cate-Hoek AJ, Elf JL, et al. (March 2014). "Exclusion of deep vein thrombosis using the Wells rule in clinically important subgroups: individual patient data meta-analysis". BMJ. 348: g1340. doi:10.1136/bmj.g1340. PMC 3948465. PMID 24615063.
- ^ Adam SS, Key NS, Greenberg CS (March 2009). "D-dimer antigen: current concepts and future prospects". Blood. 113 (13): 2878–87. doi:10.1182/blood-2008-06-165845. PMID 19008457. Archived from the original on 15 April 2013.
- ^ Guyatt et al. 2012, p. 17S: 3.4.
- ^ a b c Guyatt et al. 2012, p. 16S: 3.2.
- ^ a b Guyatt et al. 2012, p. 16S: 3.3.
- ^ Guyatt et al. 2012, p. 19S: 5.3. & 6.1.
- ^ Tovey C, Wyatt S (May 2003). "Diagnosis, investigation, and management of deep vein thrombosis". BMJ. 326 (7400): 1180–4. doi:10.1136/bmj.326.7400.1180. PMC 1126050. PMID 12775619.
- ^ Ozbudak O, Eroğullari I, Oğüş C, Cilli A, Türkay M, Ozdemir T (April 2006). "Doppler ultrasonography versus venography in the detection of deep vein thrombosis in patients with pulmonary embolism". Journal of Thrombosis and Thrombolysis. 21 (2): 159–62. doi:10.1007/s11239-006-5207-3. PMID 16622611.
- ^ Häggström, M (January 2019). "Subsartorial Vessels as Replacement Names for Superficial Femoral Vessels" (PDF). International Journal of Anatomy, Radiology and Surgery. 8 (1): AV01–AV02. doi:10.7860/IJARS/2019/40329:2458.
- ^ "What is Venous Thromboembolism?". Centers for Disease Control and Prevention. 14 March 2019. Retrieved 6 January 2019.
{{cite web}}: CS1 maint: url-status (link) - ^ Hecht 2010, p. 47.
- ^ a b c Keeling D, Baglin T, Tait C, Watson H, Perry D, Baglin C, et al. (August 2011). "Guidelines on oral anticoagulation with warfarin – fourth edition" (PDF). British Journal of Haematology. 154 (3): 311–24. doi:10.1111/j.1365-2141.2011.08753.x. PMID 21671894. Archived from the original (PDF) on 4 May 2012. Retrieved 4 May 2012.
- ^ Guyatt et al. 2012, p. 11S: 7.1.
- ^ Li L, Zhang P, Tian JH, Yang K (December 2014). "Statins for primary prevention of venous thromboembolism". The Cochrane Database of Systematic Reviews (12): CD008203. doi:10.1002/14651858.CD008203.pub3. PMID 25518837.
- ^ Kunutsor SK, Seidu S, Khunti K (February 2017). "Statins and primary prevention of venous thromboembolism: a systematic review and meta-analysis" (PDF). The Lancet Haematology. 4 (2): e83–e93. doi:10.1016/S2352-3026(16)30184-3. PMID 28089655.
- ^ a b c Alikhan R, Bedenis R, Cohen AT (May 2014). "Heparin for the prevention of venous thromboembolism in acutely ill medical patients (excluding stroke and myocardial infarction)". The Cochrane Database of Systematic Reviews. 5 (5): CD003747. doi:10.1002/14651858.CD003747.pub4. PMC 6491079. PMID 24804622.
- ^ a b Kahn SR, Lim W, Dunn AS, Cushman M, Dentali F, Akl EA, et al. (February 2012). "Prevention of VTE in nonsurgical patients: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines". Chest. 141 (2 Suppl): e195S–e226S. doi:10.1378/chest.11-2296. PMC 3278052. PMID 22315261.
- ^ Guyatt et al. 2012, p. 10S: 2.3., 2.4., & 2.7.1.
- ^ Guyatt et al. 2012, p. 10S: 2.7.2.
- ^ Guyatt et al. 2012, pp. 10S–11S: 3.4.3. & 3.4.4.
- ^ Guyatt et al. 2012, p. 11S: 4.2.2.
- ^ Sobieraj DM, Lee S, Coleman CI, Tongbram V, Chen W, Colby J, et al. (May 2012). "Prolonged versus standard-duration venous thromboprophylaxis in major orthopedic surgery: a systematic review". Annals of Internal Medicine. 156 (10): 720–7. doi:10.7326/0003-4819-156-10-201205150-00423. PMID 22412039.
- ^ a b c Falck-Ytter Y, Francis CW, Johanson NA, Curley C, Dahl OE, Schulman S, et al. (February 2012). "Prevention of VTE in orthopedic surgery patients: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines". Chest. 141 (2 Suppl): e278S–e325S. doi:10.1378/chest.11-2404. PMC 3278063. PMID 22315265.
- ^ Gould MK, Garcia DA, Wren SM, Karanicolas PJ, Arcelus JI, Heit JA, et al. (February 2012). "Prevention of VTE in nonorthopedic surgical patients: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines". Chest. 141 (2 Suppl): e227S–e277S. doi:10.1378/chest.11-2297. PMC 3278061. PMID 22315263.
- ^ Kakkos SK, Caprini JA, Geroulakos G, Nicolaides AN, Stansby GP, Reddy DJ (October 2008). Kakkos SK (ed.). "Combined intermittent pneumatic leg compression and pharmacological prophylaxis for prevention of venous thromboembolism in high-risk patients". The Cochrane Database of Systematic Reviews (4): CD005258. doi:10.1002/14651858.CD005258.pub2. PMID 18843686.
- ^ Marik PE, Plante LA (November 2008). "Venous thromboembolic disease and pregnancy". The New England Journal of Medicine. 359 (19): 2025–33. doi:10.1056/NEJMra0707993. PMID 18987370.
- ^ Jackson E, Curtis KM, Gaffield ME (March 2011). "Risk of venous thromboembolism during the postpartum period: a systematic review". Obstetrics and Gynecology. 117 (3): 691–703. doi:10.1097/AOG.0b013e31820ce2db. PMID 21343773.
- ^ a b Bates SM, Greer IA, Middeldorp S, Veenstra DL, Prabulos AM, Vandvik PO (February 2012). "VTE, thrombophilia, antithrombotic therapy, and pregnancy: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines". Chest. 141 (2 Suppl): e691S–e736S. doi:10.1378/chest.11-2300. PMC 3278054. PMID 22315276.
- ^ Guyatt et al. 2012, pp. 39S–40S: 3.0.
- ^ Guyatt et al. 2012, p. 38S: 3.0.1.
- ^ Guyatt et al. 2012, p. 11S: 6.1.1.
- ^ "New DVT guidelines: No evidence to support "economy-class syndrome"; oral contraceptives, sitting in a window seat, advanced age, and pregnancy increase DVT risk in long-distance travelers". American College of Chest Physicians. 7 February 2012. Archived from the original on 3 June 2016. Retrieved 10 February 2012.
- ^ Clarke MJ, Broderick C, Hopewell S, Juszczak E, Eisinga A (September 2016). "Compression stockings for preventing deep vein thrombosis in airline passengers". The Cochrane Database of Systematic Reviews. 9: CD004002. doi:10.1002/14651858.CD004002.pub3. PMC 6457834. PMID 27624857.
- ^ a b c d Schünemann HJ, Cushman M, Burnett AE, Kahn SR, Beyer-Westendorf J, Spencer FA, et al. (November 2018). "American Society of Hematology 2018 guidelines for management of venous thromboembolism: prophylaxis for hospitalized and nonhospitalized medical patients". Blood Advances. 2 (22): 3198–3225. doi:10.1182/bloodadvances.2018022954. PMC 6258910. PMID 30482763.
- ^ Bartholomew JR (December 2017). "Update on the management of venous thromboembolism". Cleveland Clinic Journal of Medicine. 84 (12 Suppl 3): 39–46. doi:10.3949/ccjm.84.s3.04. PMID 29257737.
- ^ "Deep venous thrombosis". PubMed Health. 19 February 2012. Archived from the original on 26 September 2012. Retrieved 2 July 2012.
{{cite web}}: Unknown parameter|encyclopedia=ignored (help) - ^ Cundiff DK, Manyemba J, Pezzullo JC (January 2006). Cundiff DK (ed.). "Anticoagulants versus non-steroidal anti-inflammatories or placebo for treatment of venous thromboembolism". The Cochrane Database of Systematic Reviews (1): CD003746. doi:10.1002/14651858.CD003746.pub2. PMID 16437461.
- ^ Douketis J, Tosetto A, Marcucci M, Baglin T, Cushman M, Eichinger S, et al. (October 2010). "Patient-level meta-analysis: effect of measurement timing, threshold, and patient age on ability of D-dimer testing to assess recurrence risk after unprovoked venous thromboembolism". Annals of Internal Medicine. 153 (8): 523–31. doi:10.7326/0003-4819-153-8-201010190-00009. PMID 20956709.
- ^ Robertson L, Kesteven P, McCaslin JE (June 2015). Cochrane Vascular Group (ed.). "Oral direct thrombin inhibitors or oral factor Xa inhibitors for the treatment of deep vein thrombosis". The Cochrane Database of Systematic Reviews (6): CD010956. doi:10.1002/14651858.CD010956.pub2. PMID 26123214.
- ^ Guyatt et al. 2012, p. 20S: 2.4.
- ^ a b c d e Kearon C, Akl EA, Comerota AJ, Prandoni P, Bounameaux H, Goldhaber SZ, et al. (February 2012). "Antithrombotic therapy for VTE disease: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines". Chest. 141 (2 Suppl): e419S–e496S. doi:10.1378/chest.11-2301. PMC 3278049. PMID 22315268.
- ^ Guyatt et al. 2012, p. 20S: 2.5.1.
- ^ Guyatt et al. 2012, pp. 20S–21S: 3.1.
- ^ Strijkers RH, Cate-Hoek AJ, Bukkems SF, Wittens CH (October 2011). "Management of deep vein thrombosis and prevention of post-thrombotic syndrome". BMJ. 343: d5916. doi:10.1136/bmj.d5916. PMID 22042752.
- ^ Guyatt et al. 2012, p. 22S: 3.2.
- ^ Middeldorp S, Prins MH, Hutten BA (August 2014). "Duration of treatment with vitamin K antagonists in symptomatic venous thromboembolism". The Cochrane Database of Systematic Reviews (8): CD001367. doi:10.1002/14651858.CD001367.pub3. PMID 25092359.
- ^ Guyatt et al. 2012, p. 21S: 3.1.1.
- ^ Guyatt et al. 2012, p. 21S: 3.1.2.
- ^ Guyatt et al. 2012, p. 22S: 3.1.4.
- ^ Guyatt et al. 2012, p. 22S: 3.1.4.1.
- ^ Guyatt et al. 2012, p. 22S: 3.1.4.2.
- ^ Guyatt et al. 2012, p. 22S: 3.1.4.4.
- ^ Guyatt et al. 2012, p. 22S: 3.1.4.5.
- ^ Guyatt et al. 2012, p. 21S: 2.7.
- ^ Guyatt et al. 2012, p. 21S: 2.14.
- ^ a b c d e f g Kearon C, Akl EA, Ornelas J, Blaivas A, Jimenez D, Bounameaux H, et al. (February 2016). "Antithrombotic therapy for VTE disease: CHEST guideline and expert panel report". Chest. 149 (2): 315–352. doi:10.1016/j.chest.2015.11.026. PMID 26867832.
- ^ Berntsen CF, Kristiansen A, Akl EA, Sandset PM, Jacobsen EM, Guyatt G, et al. (April 2016). "Compression Stockings for Preventing the Postthrombotic Syndrome in Patients with Deep Vein Thrombosis". The American Journal of Medicine. 129 (4): 447.e1–447.e20. doi:10.1016/j.amjmed.2015.11.031. PMID 26747198.
- ^ a b Guyatt et al. 2012, p. 20S: 2.3.
- ^ Enden T, Haig Y, Kløw NE, Slagsvold CE, Sandvik L, Ghanima W, et al. (January 2012). "Long-term outcome after additional catheter-directed thrombolysis versus standard treatment for acute iliofemoral deep vein thrombosis (the CaVenT study): a randomised controlled trial". Lancet. 379 (9810): 31–8. doi:10.1016/S0140-6736(11)61753-4. PMID 22172244.
- ^ Haig Y, Enden T, Grøtta O, Kløw NE, Slagsvold CE, Ghanima W, et al. (February 2016). "Post-thrombotic syndrome after catheter-directed thrombolysis for deep vein thrombosis (CaVenT): 5-year follow-up results of an open-label, randomised controlled trial". The Lancet Haematology. 3 (2): e64–71. doi:10.1016/S2352-3026(15)00248-3. PMID 26853645.
- ^ Vedantham S, Goldhaber SZ, Julian JA, Kahn SR, Jaff MR, Cohen DJ, et al. (December 2017). "Pharmacomechanical Catheter-Directed Thrombolysis for Deep-Vein Thrombosis". The New England Journal of Medicine. 377 (23): 2240–2252. doi:10.1056/NEJMoa1615066. PMC 5763501. PMID 29211671.
- ^ a b Bhandari, Tamara (6 December 2017). "Clot-busting drugs not recommended for most patients with blood clots". Washington University School of Medicine. Retrieved 21 January 2020.
{{cite news}}: CS1 maint: url-status (link) - ^ Aggarwal DG, Bhojraj SS, Behrainwalla AA, Jani CK, Mehta SS (January 2018). "Phlegmasia Cerulea Dolens Following Heparin-Induced Thrombocytopenia". Indian Journal of Critical Care Medicine. 22 (1): 51–52. doi:10.4103/ijccm.IJCCM_183_16. PMC 5793026. PMID 29422736.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ a b c Ijaopo R, Oguntolu V, DCosta D, Garnham A, Hobbs S (March 2016). "A case of Paget-Schroetter syndrome (PSS) in a young judo tutor: a case report". Journal of Medical Case Reports. 10: 63. doi:10.1186/s13256-016-0848-0. PMC 4797165. PMID 26987584.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ a b c d Young T, Tang H, Hughes R (February 2010). Young T (ed.). "Vena caval filters for the prevention of pulmonary embolism" (PDF). The Cochrane Database of Systematic Reviews (2): CD006212. doi:10.1002/14651858.CD006212.pub4. PMID 20166079.
- ^ Guyatt et al. 2012, p. 21S: 2.13.1.–3.
- ^ Guyatt et al. 2012, p. 21S: 2.13.
- ^ Tomaselli GF, Mahaffey KW, Cuker A, Dobesh PP, Doherty JU, Eikelboom JW, et al. (December 2017). "2017 ACC Expert Consensus Decision Pathway on Management of Bleeding in Patients on Oral Anticoagulants: A Report of the American College of Cardiology Task Force on Expert Consensus Decision Pathways". Journal of the American College of Cardiology. 70 (24): 3042–3067. doi:10.1016/j.jacc.2017.09.1085. PMID 29203195.
- ^ Guyatt et al. 2012, p. 21S: 2.11.
- ^ Kruger PC, Eikelboom JW, Douketis JD, Hankey GJ (June 2019). "Deep vein thrombosis: update on diagnosis and management". The Medical Journal of Australia. 210 (11): 516–524. doi:10.5694/mja2.50201. PMID 31155730.
- ^ Turpie AG (March 2008). "Deep venous thrombosis". The Merck's Manuals Online Medical Library. Merck.
- ^ a b Kahn SR (November 2009). "How I treat postthrombotic syndrome". Blood. 114 (21): 4624–31. doi:10.1182/blood-2009-07-199174. PMID 19741190. Archived from the original on 21 June 2013. Retrieved 25 June 2012.
- ^ Konstantinides SV, Torbicki A, Agnelli G, Danchin N, Fitzmaurice D, Galiè N, et al. (November 2014). "2014 ESC guidelines on the diagnosis and management of acute pulmonary embolism". European Heart Journal. 35 (43): 3033–69, 3069a–3069k. doi:10.1093/eurheartj/ehu283. PMID 25173341.
- ^ Khan F, Rahman A, Carrier M, Kearon C, Weitz JI, Schulman S, et al. (July 2019). "Long term risk of symptomatic recurrent venous thromboembolism after discontinuation of anticoagulant treatment for first unprovoked venous thromboembolism event: systematic review and meta-analysis". BMJ. 366: l4363. doi:10.1136/bmj.l4363. PMC 6651066. PMID 31340984.
- ^ Beckman MG, Hooper WC, Critchley SE, Ortel TL (April 2010). "Venous thromboembolism: a public health concern". American Journal of Preventive Medicine. 38 (4 Suppl): S495–501. doi:10.1016/j.amepre.2009.12.017. PMID 20331949.
- ^ Robertson L, Yeoh SE, Broderick C, Stansby G, Agarwal R (November 2018). Cochrane Vascular Group (ed.). "Effect of testing for cancer on cancer- or venous thromboembolism (VTE)-related mortality and morbidity in people with unprovoked VTE". The Cochrane Database of Systematic Reviews. 11: CD010837. doi:10.1002/14651858.CD010837.pub4. PMC 6517248. PMID 30407621.
- ^ "Surveillance report 2016 – Venous thromboembolic diseases (2012) NICE guideline CG144". NICE. 3 November 2016. Retrieved 16 January 2020.
{{cite web}}: CS1 maint: url-status (link) - ^ Johannesen CD, Flachs EM, Ebbehøj NE, Marott JL, Jensen GB, Nordestgaard BG, et al. (January 2020). "Sedentary work and risk of venous thromboembolism". Scandinavian Journal of Work, Environment & Health. 46 (1): 69–76. doi:10.5271/sjweh.3841. PMID 31385593.
- ^ a b Grosse SD, Nelson RE, Nyarko KA, Richardson LC, Raskob GE (January 2016). "The economic burden of incident venous thromboembolism in the United States: A review of estimated attributable healthcare costs". Thrombosis Research. 137: 3–10. doi:10.1016/j.thromres.2015.11.033. PMC 4706477. PMID 26654719.
- ^ Rosendaal 2009, p. 5.
- ^ Bates SM, Rajasekhar A, Middeldorp S, McLintock C, Rodger MA, James AH, et al. (November 2018). "American Society of Hematology 2018 guidelines for management of venous thromboembolism: venous thromboembolism in the context of pregnancy". Blood Advances. 2 (22): 3317–3359. doi:10.1182/bloodadvances.2018024802. PMC 6258928. PMID 30482767.
- ^ Januel JM, Chen G, Ruffieux C, Quan H, Douketis JD, Crowther MA, et al. (January 2012). "Symptomatic in-hospital deep vein thrombosis and pulmonary embolism following hip and knee arthroplasty among patients receiving recommended prophylaxis: a systematic review". JAMA. 307 (3): 294–303. doi:10.1001/jama.2011.2029. PMID 22253396.
- ^ Young A, Chapman O, Connor C, Poole C, Rose P, Kakkar AK (July 2012). "Thrombosis and cancer". Nature Reviews. Clinical Oncology. 9 (8): 437–49. doi:10.1038/nrclinonc.2012.106. PMID 22777060.
- ^ Margaglione M, Grandone E (February 2011). "Population genetics of venous thromboembolism. A narrative review". Thrombosis and Haemostasis. 105 (2): 221–31. doi:10.1160/TH10-08-0510. PMID 20941456.
- ^ "Blood types". American Red Cross. Archived from the original on 14 August 2012. Retrieved 15 August 2012.
- ^ Hamasaki N (October 2012). "Unmasking Asian thrombophilia: is APC dysfunction the real culprit?". Journal of Thrombosis and Haemostasis. 10 (10): 2016–8. doi:10.1111/j.1538-7836.2012.04893.x. PMID 22905992.
- ^ a b Haskell, Rob (10 January 2018). "Serena Williams on Motherhood, Marriage, and Making Her Comeback". Vogue. Retrieved 22 January 2020.
{{cite web}}: CS1 maint: url-status (link) - ^ Golemi I, Salazar Adum JP, Tafur A, Caprini J (August 2019). "Venous thromboembolism prophylaxis using the Caprini score". Disease-a-month : DM. 65 (8): 249–298. doi:10.1016/j.disamonth.2018.12.005. PMID 30638566.
- ^ Perez, A.J. (17 February 2016). "Expert: Chris Bosh, like many, at risk of blood clot recurrence". USA Today. Retrieved 22 January 2020.
{{cite news}}: CS1 maint: url-status (link) - ^ Martin, Jill (4 May 2016). "Chris Bosh officially out as Heat make playoff push". CNN. Retrieved 22 January 2020.
{{cite news}}: CS1 maint: url-status (link) - ^ Moisse, Katie (2 March 2011). "Serena Williams Hospitalized After Pulmonary Embolism". ABC News. Retrieved 22 January 2020.
{{cite news}}: CS1 maint: url-status (link) - ^ Pascarella L, Pappas TN (February 2013). "Phlebitis, pulmonary emboli and presidential politics: Richard M. Nixon's complicated deep vein thrombosis". The American Surgeon. 79 (2): 128–34. PMID 23336651.
- ^ Frankel, Todd C. (11 September 2016). "Hillary Clinton has not been quick to share health information". The Washington Post. Retrieved 22 January 2020.
{{cite news}}: CS1 maint: url-status (link) - ^ "Cheney diagnosed with deep-vein thrombosis". The Guardian. 6 March 2007. Retrieved 22 January 2020.
{{cite news}}: CS1 maint: url-status (link) - ^ a b Rodriguez, Diana (12 October 2018). "11 Celebrities Who Battled Deep Vein Thrombosis Risk". Everyday Health. Retrieved 22 January 2020.
{{cite web}}: CS1 maint: url-status (link) - ^ "Coroner: Rapper Heavy D died of blood clot in lung". CNN. 27 December 2011. Retrieved 22 January 2020.
{{cite web}}: CS1 maint: url-status (link) - ^ "'My husband should be living today'". TODAY. 3 March 2005. Retrieved 22 January 2020.
{{cite news}}: CS1 maint: url-status (link) - ^ Moll, Stephan (9 May 2012). "What Kind of Doctor Do I Need?". Clot Connect. Retrieved 28 January 2020.
{{cite web}}: CS1 maint: url-status (link) - ^ Kitchen L, Lawrence M, Speicher M, Frumkin K (July 2016). "Emergency Department Management of Suspected Calf-Vein Deep Venous Thrombosis: A Diagnostic Algorithm". The Western Journal of Emergency Medicine. 17 (4): 384–90. doi:10.5811/westjem.2016.5.29951. PMC 4944794. PMID 27429688.
- ^ "Inferior Vena Cava (IVC) Filter Placement". Johns Hopkins Medicine. 2020. Retrieved 28 January 2020.
{{cite web}}: CS1 maint: url-status (link) - ^ a b Goodman LR (October 2013). "In search of venous thromboembolism: the first 2913 years". AJR. American Journal of Roentgenology. 201 (4): W576-81. doi:10.2214/AJR.13.10604. PMID 24059395.
- ^ Galanaud JP, Laroche JP, Righini M (March 2013). "The history and historical treatments of deep vein thrombosis". Journal of Thrombosis and Haemostasis : JTH. 11 (3): 402–11. doi:10.1111/jth.12127. PMID 23297815.
- ^ a b Rosendaal 2009, p. 3.
- ^ Bagot CN, Arya R (October 2008). "Virchow and his triad: a question of attribution". British Journal of Haematology. 143 (2): 180–90. doi:10.1111/j.1365-2141.2008.07323.x. PMID 18783400.
- ^ Dalen 2003, p. 2.
- ^ a b Ornstein, Charles; Jones, Ryann Grochowski (7 January 2015). "The Drugs That Companies Promote to Doctors Are Rarely Breakthroughs". The New York Times.
{{cite news}}: CS1 maint: url-status (link) - ^ a b Franchini M, Mannucci PM (September 2016). "Direct oral anticoagulants and venous thromboembolism". European Respiratory Review. 25 (141): 295–302. doi:10.1183/16000617.0025-2016. PMID 27581829.
- ^ Dalen 2003, p. 3.
- ^ a b Dobesh PP (August 2009). "Economic burden of venous thromboembolism in hospitalized patients". Pharmacotherapy. 29 (8): 943–53. doi:10.1592/phco.29.8.943. PMID 19637948.
- ^ Ruppert A, Steinle T, Lees M (2011). "Economic burden of venous thromboembolism: a systematic review". Journal of Medical Economics. 14 (1): 65–74. doi:10.3111/13696998.2010.546465. PMID 21222564.
- ^ Grosse SD (January 2012). "Incidence-based cost estimates require population-based incidence data. A critique of Mahan et al" (PDF). Thrombosis and Haemostasis. 107 (1): 192–3, author reply 194–5. doi:10.1160/TH11-09-0666. PMID 22159589. Archived (PDF) from the original on 8 August 2017.
- ^ a b Mahan CE, Holdsworth MT, Welch SM, Borrego M, Spyropoulos AC (September 2011). "Deep-vein thrombosis: a United States cost model for a preventable and costly adverse event". Thrombosis and Haemostasis. 106 (3): 405–15. doi:10.1160/TH11-02-0132. PMID 21833446.
- ^ Mahan CE, Holdsworth MT, Welch SM, et al. (2012). "Long-term attack rates, as compared with incidence rates, may provide improved cost-estimates in venous thromboembolism. A reply to S. D. Grosse". Thromb Haemost. 107 (1): 194–5. doi:10.1160/TH11-11-0802.
- ^ Metz AK, Diaz JA, Obi AT, Wakefield TW, Myers DD, Henke PK (2018). "Venous Thrombosis and Post-Thrombotic Syndrome: From Novel Biomarkers to Biology". Methodist DeBakey Cardiovascular Journal. 14 (3): 173–181. doi:10.14797/mdcj-14-3-173. PMC 6217569. PMID 30410646.
- Cited literature
- Dalen, James E. (2003). Venous thromboembolism. CRC Press. ISBN 978-0-8247-5645-1.
{{cite book}}: Invalid|ref=harv(help); Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - Guyatt GH, Akl EA, Crowther M, Gutterman DD, Schuünemann HJ (February 2012). "Executive summary: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines". Chest. 141 (2 Suppl): 7S–47S. doi:10.1378/chest.1412S3. PMC 3278060. PMID 22315257.
{{cite journal}}: Invalid|ref=harv(help); Unknown parameter|displayauthors=ignored (|display-authors=suggested) (help) - Hecht ME (2010). A practical guide to hip surgery: From pre-op to recovery. Sunrise River Press. ISBN 978-1-934716-12-0.
{{cite book}}: Invalid|ref=harv(help) - Rosendaal, Frits R. (2009). van Beek, Edwin J. R.; Büller, Harry R.; Oudkerk, Mathijs (eds.). Deep vein thrombosis and pulmonary embolism. John Wiley & Sons. ISBN 978-0-470-74499-4.
{{cite book}}: Invalid|ref=harv(help); Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - Welch, Ellen (2010). Venous thromboembolism: A nurse's guide to prevention and management. John Wiley & Sons. ISBN 978-0-470-51189-3.
{{cite book}}: Invalid|ref=harv(help); Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help)

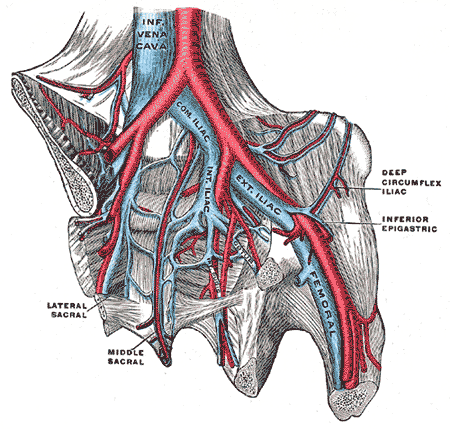

![Doppler ultrasonography showing absence of flow and hyperechogenic content in a clotted femoral vein (labeled subsartorial) distal to the branching point of the deep femoral vein. (Subsartorial is a proposed name for a section of the femoral vein.)[79]](http://upload.wikimedia.org/wikipedia/commons/thumb/4/4f/Ultrasonography_of_deep_vein_thrombosis_of_the_femoral_vein_-annotated.jpg/459px-Ultrasonography_of_deep_vein_thrombosis_of_the_femoral_vein_-annotated.jpg)



![Phlegmasia cerulea dolens (literally: painful blue edema) is a particularly severe form of acute, proximal, and occlusive DVT. It is life-threatening and limb-threatening.[133]](http://upload.wikimedia.org/wikipedia/commons/thumb/c/c3/PCD2016.jpg/329px-PCD2016.jpg)

![After treatment with catheter-directed thrombolysis, blood flow in the axillary and subclavian vein were significantly improved. Afterwards, a first rib resection provided thoracic outlet decompression to reduce the risk of recurrent DVT and the risk of sequelae from thoracic outlet compression.[134]](http://upload.wikimedia.org/wikipedia/commons/6/6e/A-case-of-Paget-Schroetter-syndrome-%28PSS%29-in-a-young-judo-tutor-a-case-report-13256_2016_848_Fig2_HTML.jpg)