Acupuncture
| This article is part of a series on |
| Alternative medicine |
|---|
 |

Acupuncture is the procedure of inserting and manipulating needles into various points on the body to relieve pain or for therapeutic purposes.[1] The earliest written record of acupuncture is the Chinese text Shiji (史記, English: Records of the Grand Historian) with elaboration of its history in the second century BCE medical text Huangdi Neijing (黃帝內經, English: Yellow Emperor's Inner Canon).[2] Different variations of acupuncture are practiced and taught throughout the world.
Acupuncture has been the subject of active scientific research both in regard to its basis and therapeutic effectiveness since the late 20th century, but it remains controversial among medical researchers and clinicians.[3] Research on acupuncture points and meridians is preliminary and has not conclusively demonstrated their existence or properties.[4] Clinical assessment of acupuncture treatments, due to its invasive and easily detected nature, makes it difficult to use proper scientific controls for placebo effects.[3][5][6][7][8]
Evidence supports the use of acupuncture to control some types of nausea[9] and pain[10] but evidence for the treatment of other conditions is equivocal[3] and several review articles discussing the effectiveness of acupuncture have concluded it is possible to explain through the placebo effect.[11][12]
The World Health Organization[13] and the United States' National Institutes of Health (NIH)[5] have stated that acupuncture can be effective in the treatment of neurological conditions and pain, though these statements have been criticized for bias and a reliance on studies that used poor methodology.[14][15] Reports from the USA's National Center for Complementary and Alternative Medicine (NCCAM), the American Medical Association (AMA) and various USA government reports have studied and commented on the efficacy (or lack thereof) of acupuncture. There is general agreement that acupuncture is safe when administered by well-trained practitioners using sterile needles, and that further research is needed.[5][16][17][18]
History
Antiquity
Acupuncture's origins in China are uncertain. One explanation is that some soldiers wounded in battle by arrows were cured of chronic afflictions that were otherwise untreated,[19] and there are variations on this idea.[20] In China, the practice of acupuncture can perhaps be traced as far back as the Stone Age, with the Bian shi, or sharpened stones.[21] In 1963 a bian stone was found in Duolun County, Inner Mongolia, China pushing the origins of acupuncture into the Neolithic age.[22] Hieroglyphs and pictographs have been found dating from the Shang Dynasty (1600-1100 BCE) which suggest that acupuncture was practiced along with moxibustion.[23]
Despite improvements in metallurgy over centuries, it was not until the 2nd century BCE during the Han Dynasty that stone and bone needles were replaced with metal.[22] The earliest records of acupuncture is in the Shiji (史記, in English, Records of the Grand Historian) with references in later medical texts that are equivocal, but could be interpreted as discussing acupuncture. The earliest Chinese medical text to describe acupuncture is the Huangdi Neijing, the legendary Yellow Emperor's Classic of Internal Medicine (History of Acupuncture) which was compiled around 305–204 B.C.[2]
The Huangdi Neijing does not distinguish between acupuncture and moxibustion and gives the same indication for both treatments. The Mawangdui texts, which also date from the second century BC (though antedating both the Shiji and Huangdi Neijing), mention the use of pointed stones to open abscesses, and moxibustion but not acupuncture. However, by the second century BCE, acupuncture replaced moxibustion as the primary treatment of systemic conditions.[2]
In Europe, examinations of the 5,000-year-old mummified body of Ötzi the Iceman have identified 15 groups of tattoos on his body, some of which are located on what are now seen as contemporary acupuncture points. This has been cited as evidence that practices similar to acupuncture may have been practiced elsewhere in Eurasia during the early Bronze Age.[24]
Middle history
Acupuncture spread from China to Korea, Japan and Vietnam and elsewhere in East Asia.
Around ninety works on acupuncture were written in China between the Han Dynasty and the Song Dynasty, and the Emperor Renzong of Song, in 1023, ordered the production of a bronze statuette depicting the meridians and acupuncture points then in use. However, after the end of the Song Dynasty, acupuncture and its practitioners began to be seen as a technical rather than scholarly profession. It became more rare in the succeeding centuries, supplanted by medications and became associated with the less prestigious practices of shamanism, midwifery and moxibustion.[25]
Portuguese missionaries in the 16th century were among the first to bring reports of acupuncture to the West.[26] Jacob de Bondt, a Danish surgeon travelling in Asia, described the practice in both Japan and Java. However, in China itself the practice was increasingly associated with the lower-classes and illiterate practitioners.[27]
The first European text on acupuncture was written by Willem ten Rhijne, a Dutch physician who studied the practice for two years in Japan. It consisted of an essay in a 1683 medical text on arthritis; Europeans were also at the time becoming more interested in moxibustion, which ten Rhijne also wrote about.[28] In 1757 the physician Xu Daqun described the further decline of acupuncture, saying it was a lost art, with few experts to instruct; its decline was attributed in part to the popularity of prescriptions and medications, as well as its association with the lower classes.[29]
In 1822, an edict from the Chinese Emperor banned the practice and teaching of acupuncture within the Imperial Academy of Medicine outright, as unfit for practice by gentlemen-scholars. At this point, acupuncture was still cited in Europe with both skepticism and praise, with little study and only a small amount of experimentation.[30]
Modern era
In the early years after the Chinese Civil War, Chinese Communist Party leaders ridiculed traditional Chinese medicine, including acupuncture, as superstitious, irrational and backward, claiming that it conflicted with the Party's dedication to science as the way of progress. Communist Party Chairman Mao Zedong later reversed this position, saying that "Chinese medicine and pharmacology are a great treasure house and efforts should be made to explore them and raise them to a higher level."[31]
Acupuncture gained attention in the United States when President Richard Nixon visited China in 1972. During one part of the visit, the delegation was shown a patient undergoing major surgery while fully awake, ostensibly receiving acupuncture rather than anesthesia. Later it was found that the patients selected for the surgery had both a high pain tolerance and received heavy indoctrination before the operation; these demonstration cases were also frequently receiving morphine surreptitiously through an intravenous drip that observers were told contained only fluids and nutrients.[32]
The greatest exposure in the West came when New York Times reporter James Reston, who accompanied Nixon during the visit, received acupuncture in China for post-operative pain after undergoing an emergency appendectomy under standard anesthesia. Reston was so impressed with the pain relief he experienced from the procedure that he wrote about acupuncture in The New York Times upon returning to the United States.[33] In 1973 the American Internal Revenue Service allowed acupuncture to be deducted as a medical expense.[34]
In 2006, a BBC documentary Alternative Medicine filmed a patient undergoing open heart surgery allegedly under acupuncture-induced anaesthesia. It was later revealed that the patient had been given a cocktail of weak anaesthetics that in combination could have a much more powerful effect. The program was also criticised for its fanciful interpretation of the results of a brain scanning experiment.[35][36][37]
Acupuncture anesthesia for surgery has fallen out of favor with scientifically trained surgeons in China. A delegation of the Committee for the Scientific Investigation of Claims of the Paranormal reported in 1995: We were not shown acupuncture anesthesia for surgery, this apparently having fallen out of favor with scientifically trained surgeons. Dr. Han, for instance, had been emphatic that he and his colleagues see acupuncture only as an analgesic (pain reducer), not an anesthetic (an agent that blocks all conscious sensations).[32]
Traditional theory

Traditional Chinese medicine
Traditional Chinese medicine (TCM) is based on a pre-scientific paradigm of medicine that developed over several thousand years and involves concepts that have no counterpart within contemporary medicine.[5] In TCM, the body is treated as a whole that is composed of several "systems of function" known as the zang-fu (脏腑). These systems are named after specific organs, though the systems and organs are not directly associated.
The zang systems are associated with the solid, yin organs such as the liver while the fu systems are associated with the hollow yang organs such as the intestines. Health is explained as a state of balance between the yin and yang, with disease ascribed to either of these forces being unbalanced, blocked or stagnant.
The yang force is the immaterial qi, a concept that is roughly translated as "vital energy". The yin counterpart is Blood, which is linked to but not identical with physical blood, and capitalized to distinguish the two. TCM uses a variety of interventions, including pressure, heat and acupuncture applied to the body's acupuncture points (in Chinese 穴 or xue meaning "cavities") to modify the activity of the zang-fu.
Acupuncture points and meridians
| Flow of qi through the meridians | ||
| Zang-fu | Aspect | Hours |
| Lung | taiyin | 0300-0500 |
| Large Intestine | yangming | 0500-0700 |
| Stomach | yangming | 0700-0900 |
| Spleen | taiyin | 0900-1100 |
| Heart | shaoyin | 1100–1300 |
| Small Intestine | taiyang | 1300–1500 |
| Bladder | taiyang | 1500–1700 |
| Kidney | shaoyin | 1700–1900 |
| Pericardium | jueyin | 1900–2100 |
| San Jiao | shaoyang | 2100–2300 |
| Gallbladder | shaoyang | 2300-0100 |
| Liver | jueyin | 0100-0300 |
| Lung (repeats cycle) | ||
Classical texts describe most[dubious – discuss] of the main acupuncture points as existing on the twelve main and two of eight extra meridians (also referred to as mai) for a total of fourteen "channels" through which qi and Blood flow. Other points not on the fourteen channels are also needled. Local pain is treated by needling the tender "ashi" points where qi or Blood is believed to have stagnated.
The zang-fu of the twelve main channels are Lung, Large Intestine, Stomach, Spleen, Heart, Small Intestine, Bladder, Kidney, Pericardium, Gall Bladder, Liver and the intangible San Jiao. The eight other pathways, referred to collectively as the qi jing ba mai, include the Luo Vessels, Divergents, Sinew Channels, ren mai and du mai though only the latter two (corresponding to the anterior and posterior sagittal plane of the torso respectively) are needled. The remaining six qi jing ba mai are manipulated by needling points on the twelve main meridians.
Normally qi is described as flowing through each channel in a continuous circuit. In addition, each channel has a specific aspect and occupies two hours of the "Chinese clock".
The zang-fu are divided into yin and yang channels, with three of each type located on each limb. Qi is believed to move in a circuit through the body, travelling both superficially and deeply. The external pathways correspond to the acupuncture points shown on an acupuncture chart while the deep pathways correspond to where a channel enters the bodily cavity related to each organ.
The three yin channels of the hand (Lung, Pericardium, and Heart) begin on the chest and travel along the inner surface of the arm to the hand. The three yang channels of the hand (Large Intestine, San Jiao, and Small Intestine) begin on the hand and travel along the outer surface of the arm to the head. The three yin channels of the foot (Spleen, Liver, and Kidney) begin on the foot and travel along the inner surface of the leg to the chest or flank.
The three yang channels of the foot (Stomach, Gallbladder, and Urinary Bladder) begin on the face, in the region of the eye, and travel down the body and along the outer surface of the leg to the foot. Each channel is also associated with a yin or yang aspect, either "absolute" (jue-), "lesser" (shao-), "greater" (tai-) or "brightness" (-ming).
A standard teaching text comments on the nature and relationship of meridians (or channels) and the Zang Fu organs:
The theory of the channels is interrelated with the theory of the Organs. Traditionally, the internal Organs have never been regarded as independent anatomical entities. Rather, attention has centered upon the functional and pathological interrelationships between the channel network and the Organs. So close is this identification that each of the twelve traditional Primary channels bears the name of one or another of the vital Organs. In the clinic, the entire framework of diagnostics, therapeutics and point selection is based upon the theoretical framework of the channels. "It is because of the twelve Primary channels that people live, that disease is formed, that people are treated and disease arises." [(Spiritual Axis, chapter 12)]. From the beginning, however, we should recognize that, like other aspects of traditional medicine, channel theory reflects the limitations in the level of scientific development at the time of its formation, and is therefore tainted with the philosophical idealism and metaphysics of its day. That which has continuing clinical value needs to be reexamined through practice and research to determine its true nature.[38]
The meridians are part of the controversy in the efforts to reconcile acupuncture with conventional medicine. The National Institutes of Health 1997 consensus development statement on acupuncture stated that acupuncture points, Qi, the meridian system and related theories play an important role in the use of acupuncture, but are difficult to relate to a contemporary understanding of the body.[5] Chinese medicine forbade dissection, and as a result the understanding of how the body functioned was based on a system that related to the world around the body rather than its internal structures. The 365 "divisions" of the body were based on the number of days in a year, and the twelve meridians proposed in the TCM system are thought to be based on the twelve major rivers that run through China. However, these ancient traditions of Qi and meridians have no counterpart in modern studies of chemistry, biology and physics and to date scientists have been unable to find evidence that supports their existence.[39][40]
Traditional diagnosis
The acupuncturist decides which points to treat by observing and questioning the patient in order to make a diagnosis according to the tradition which he or she utilizes. In TCM, there are four diagnostic methods: inspection, auscultation and olfaction, inquiring, and palpation.[41]
- Inspection focuses on the face and particularly on the tongue, including analysis of the tongue size, shape, tension, color and coating, and the absence or presence of teeth marks around the edge.
- Auscultation and olfaction refer, respectively, to listening for particular sounds (such as wheezing) and attending to body odor.
- Inquiring focuses on the "seven inquiries", which are: chills and fever; perspiration; appetite, thirst and taste; defecation and urination; pain; sleep; and menses and leukorrhea.
- Palpation includes feeling the body for tender "ashi" points, and palpation of the left and right radial pulses at two levels of pressure (superficial and deep) and three positions Cun, Guan, Chi (immediately proximal to the wrist crease, and one and two fingers' breadth proximally, usually palpated with the index, middle and ring fingers).
Other forms of acupuncture employ additional diagnostic techniques. In many forms of classical Chinese acupuncture, as well as Japanese acupuncture, palpation of the muscles and the hara (abdomen) are central to diagnosis.
Traditional Chinese medicine perspective
Although TCM is based on the treatment of "patterns of disharmony" rather than biomedical diagnoses, practitioners familiar with both systems have commented on relationships between the two. A given TCM pattern of disharmony may be reflected in a certain range of biomedical diagnoses: thus, the pattern called Deficiency of Spleen Qi could manifest as chronic fatigue, diarrhea or uterine prolapse. Likewise, a population of patients with a given biomedical diagnosis may have varying TCM patterns. These observations are encapsulated in the TCM aphorism "One disease, many patterns; one pattern, many diseases". (Kaptchuk, 1982)
Classically, in clinical practice, acupuncture treatment is typically highly individualized and based on philosophical constructs as well as subjective and intuitive impressions, and not on controlled scientific research.[42]
Criticism of traditional Chinese medicine theory
Felix Mann, founder and past-president of the Medical Acupuncture Society (1959–1980), the first president of the British Medical Acupuncture Society[43] (1980), and the author of the first comprehensive English language acupuncture textbook Acupuncture: The Ancient Chinese Art of Healing first published in 1962, has stated in his book Reinventing Acupuncture: A New Concept of Ancient Medicine:
- "The traditional acupuncture points are no more real than the black spots a drunkard sees in front of his eyes." (p. 14)
and...
- "The meridians of acupuncture are no more real than the meridians of geography. If someone were to get a spade and tried to dig up the Greenwich meridian, he might end up in a lunatic asylum. Perhaps the same fate should await those doctors who believe in [acupuncture] meridians." (p. 31)[44]
Felix Mann tried to join up his medical knowledge with that of Chinese theory. In spite of his protestations about the theory, he was fascinated by it and trained many people in the west with the parts of it he borrowed. He also wrote many books on this subject. His legacy is that there is now a college in London and a system of needling that is known as "Medical Acupuncture". Today this college trains Doctors and western medical professionals only.
Medical acupuncture has caused much controversy amongst traditional practitioners; the British Acupuncture Council wished for it to be called 'treatment using needles', and removing from it the title 'Acupuncture', as it is so different to traditional methods but have had to retract this after pressure from the medical profession. Mann proposed that the acupuncture points related to the nerve endings and he reassigned the points different uses. He altered the theory so that the treatments given are no longer individual to each client, a central premise of traditional theory. Traditionally the needle combinations differ according to the age of the client, the length of time they had the condition, the type of pain they experience and their health history. In medical acupuncture none of this is addressed and the presenting symptom is treated using a set group of points.
A report for CSICOP on pseudoscience in China written by Wallace Sampson and Barry Beyerstein said:
- "A few Chinese scientists we met maintained that although Qi is merely a metaphor, it is still a useful physiological abstraction (e.g., that the related concepts of Yin and Yang parallel modern scientific notions of endocrinologic [sic] and metabolic feedback mechanisms). They see this as a useful way to unite Eastern and Western medicine. Their more hard-nosed colleagues quietly dismissed Qi as only a philosophy, bearing no tangible relationship to modern physiology and medicine."[45]
George A. Ulett, MD, PhD, Clinical Professor of Psychiatry, University of Missouri School of Medicine states:
- "Devoid of metaphysical thinking, acupuncture becomes a rather simple technique that can be useful as a nondrug method of pain control." He believes that the traditional Chinese variety is primarily a placebo treatment, but electrical stimulation of about 80 acupuncture points has been proven useful for pain control."[46]
Ted J. Kaptchuk,[47] author of The Web That Has No Weaver, refers to acupuncture as "prescientific." Regarding TCM theory, Kaptchuk states:
- "These ideas are cultural and speculative constructs that provide orientation and direction for the practical patient situation. There are few secrets of Oriental wisdom buried here. When presented outside the context of Chinese civilization, or of practical diagnosis and therapeutics, these ideas are fragmented and without great significance. The "truth" of these ideas lies in the way the physician can use them to treat real people with real complaints." (1983, pp. 34-35)[48]
According to the 1997 NIH consensus statement on acupuncture:
- "Despite considerable efforts to understand the anatomy and physiology of the "acupuncture points", the definition and characterization of these points remains controversial. Even more elusive is the basis of some of the key traditional Eastern medical concepts such as the circulation of Qi, the meridian system, and the five phases theory, which are difficult to reconcile with contemporary biomedical information but continue to play an important role in the evaluation of patients and the formulation of treatment in acupuncture."[5]
A systematic review of acupuncture for pain found that there was no difference between inserting needles into "true" acupuncture on traditional acupuncture points versus "placebo" points not associated with any TCM acupuncture points or meridians. The review concluded that "A small analgesic effect of acupuncture was found, which seems to lack clinical relevance and cannot be clearly distinguished from bias. Whether needling at acupuncture points, or at any site, reduces pain independently of the psychological impact of the treatment ritual is unclear."[11]
Clinical practice
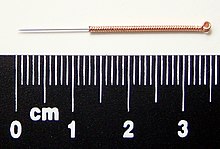
Most modern acupuncturists use disposable stainless steel needles of fine diameter (0.007 to 0.020 in (0.18 to 0.51 mm)), sterilized with ethylene oxide or by autoclave. These needles are far smaller in diameter (and therefore less painful) than hypodermic injection needles since they do not have to be hollow for purposes of injection. The upper third of these needles is wound with a thicker wire (typically bronze), or covered in plastic, to stiffen the needle and provide a handle for the acupuncturist to grasp while inserting. The size and type of needle used, and the depth of insertion, depend on the acupuncture style being practiced.
Warming an acupuncture point, typically by moxibustion (the burning of a combination of herbs, primarily mugwort), is a different treatment than acupuncture itself and is often, but not exclusively, used as a supplemental treatment. The Chinese term zhēn jǐu (針灸), commonly used to refer to acupuncture, comes from zhen meaning "needle", and jiu meaning "moxibustion". Moxibustion is used to varying degrees among current schools of oriental medicine. For example, one well-known technique is to insert the needle at the desired acupuncture point, attach dried moxa to the external end of an acupuncture needle, and then ignite it. The moxa will then smolder for several minutes (depending on the amount adhered to the needle) and conduct heat through the needle to the tissue surrounding the needle in the patient's body. Another common technique is to hold a large glowing stick of moxa over the needles. Moxa is also sometimes burned at the skin surface, usually by applying an ointment to the skin to protect from burns, though burning of the skin is general practice in China.
An example of acupuncture treatment
In Western medicine, vascular headaches (the kind that are accompanied by throbbing veins in the temples) are typically treated with analgesics such as aspirin and/or by the use of agents such as niacin that dilate the affected blood vessels in the scalp, but in acupuncture a common treatment for such headaches is to stimulate the sensitive points that are located roughly in the centers of the webs between the thumbs and the palms of the patient's hands, the hé gǔ points. These points are described by acupuncture theory as "targeting the face and head" and are considered to be the most important points when treating disorders affecting the face and head. The patient reclines, and the points on each hand are first sterilized with alcohol, and then thin, disposable needles are inserted to a depth of approximately 3–5 mm until a characteristic "twinge" is felt by the patient, often accompanied by a slight twitching of the area between the thumb and hand.
In the clinical practice of acupuncturists, patients frequently report one or more of certain kinds of sensation that are associated with this treatment:
- Extreme sensitivity to pain at the points in the webs of the thumbs.
- In bad headaches, a feeling of nausea that persists for roughly the same period as the stimulation being administered to the webs of the thumbs.
- Simultaneous relief of the headache.[49]
Indications according to acupuncturists in the West
The American Academy of Medical Acupuncture (2004) states: "In the United States, acupuncture has its greatest success and acceptance in the treatment of musculoskeletal pain."[50] They say that acupuncture may be considered as a complementary therapy for the conditions in the list below, noting: "Most of these indications are supported by textbooks or at least 1 journal article. However, definitive conclusions based on research findings are rare because the state of acupuncture research is poor but improving."[50] For example, drug detoxification is suggested[51] but evidence is poor.[52][53][54]
Vetrinary acupuncture
The evidence base for the use of acupuncture on animals is weak, and requires more rigorious research to test the small amount of existing data that is promising but unconvincing.[55]
Scientific research
Acupuncture points and meridians
Though numerous theories have been proposed, no research has established any consistent anatomical structure or function for either acupuncture points or meridians. It has been proposed that trigger points were related to acupuncture points, but the two are rarely consistently found together, identified trigger points are rarely used by acupuncturists and when they are used, they are not used for the same indications. Because of the reaction of the tissues to needle sticks, the loose connective tissues found between and within muscles has also been proposed, but no firm conclusions have yet been established. The nervous system has been evaluated for a relationship to acupuncture points, but no structures have been clearly linked to them. Controversial studies using nuclear imaging have suggested that tracers may be used to follow meridians and are not related to veins or lymphatic tissues, but the interpretation of these results is unclear. The electrical resistance of acupuncture points and meridians have also been studied, but the evidence is considered only "suggestive" and insufficient to support any theories about the electrical properties of either.[4]
Possible neural mechanism of action

The neural mechanisms underlying acupuncture-induced analgesia are unknown but may involve recruitment of the body's own pain reduction system, and an increased release of endorphins, serotonin, norepinephrine, or GABA.[56]
Efficacy
Study design
One of the major challenges in acupuncture research is in the design of an appropriate placebo control group.[6] In trials of new drugs, double blinding is the accepted standard, but since acupuncture is a procedure rather than a pill, it is difficult to design studies in which both the acupuncturist and patient are blinded as to the treatment being given. The same problem arises in double-blinding procedures used in biomedicine, including virtually all surgical procedures, dentistry, physical therapy, etc. As the Institute of Medicine states: "Controlled trials of surgical procedures have been done less frequently than studies of medications because it is much more difficult to standardize the process of surgery. Surgery depends to some degree on the skills and training of the surgeon and the specific environment and support team available to the surgeon. A surgical procedure in the hands of a highly skilled, experienced surgeon is different from the same procedure in the hands of an inexperienced and unskilled surgeon... For many CAM modalities, it is similarly difficult to separate the effectiveness of the treatment from the effectiveness of the person providing the treatment."[8]: 126 Acupuncture itself is also a very strong placebo, and can provoke extremely high expectations from patients and test subjects; this is particularly problematic for health problems like chronic low back pain, where conventional treatment is often relatively ineffective been unsuccessfully used in the past. In situations like these, it may be inappropriate to consider "conventional care" a proper placebo and comparison for acupuncture since patient expectations for conventional care are quite low.[57]
Blinding of the practitioner in acupuncture remains challenging. One proposed solution to blinding patients has been the development of "sham acupuncture", i.e., needling performed superficially or at non-acupuncture sites. Controversy remains over whether, and under what conditions, sham acupuncture may function as a true placebo, particularly in studies on pain, in which insertion of needles anywhere near painful regions may elicit a beneficial response.[5][7] A review in 2007 noted several issues confounding sham acupuncture: "Weak physiologic activity of superficial or sham needle penetration is suggested by several lines of research, including RCTs showing larger effects of a superficial needle penetrating acupuncture than those of a nonpenetrating sham control, positron emission tomography research indicating that sham acupuncture can stimulate regions of the brain associated with natural opiate production, and animal studies showing that sham needle insertion can have nonspecific analgesic effects through a postulated mechanism of “diffuse noxious inhibitory control”. Indeed, superficial needle penetration is a common technique in many authentic traditional Japanese acupuncture styles."[58]
An analysis of 13 studies of pain treatment with acupuncture, published in January 2009 in the journal BMJ, concluded there was little difference in the effect of real, sham and no acupuncture.[11]
Evidence-based medicine
There is scientific agreement that an evidence-based medicine (EBM) framework should be used to assess health outcomes and that systematic reviews with strict protocols are essential. Organizations such as the Cochrane Collaboration and Bandolier publish such reviews. In practice, EBM is "about integrating individual clinical expertise and the best external evidence" and thus does not demand that doctors ignore research outside its "top-tier" criteria.[59] Scientific disagreement over multiple aspects of acupuncture research is not uncommon.[60]
The development of the evidence base for acupuncture was summarized in a review by researcher Edzard Ernst and colleagues in 2007. They compared systematic reviews conducted (with similar methodology) in 2000 and 2005: "The effectiveness of acupuncture remains a controversial issue. ... The results indicate that the evidence base has increased for 13 of the 26 conditions included in this comparison. For 7 indications it has become more positive (i.e. favoring acupuncture) and for 6 it had changed in the opposite direction. It is concluded, that acupuncture research is active. The emerging clinical evidence seems to imply that acupuncture is effective for some but not all conditions."[3]
For acute low back pain there is insufficient evidence to recommend for or against either acupuncture or dry needling, though for chronic low back pain acupuncture is more effective than sham treatment but no more effective than conventional and alternative treatments for short-term pain relief and improving function. However, when combined with other conventional therapies, the combination is slightly better than conventional therapy alone.[10][61] A review for the American Pain Society/American College of Physicians found fair evidence that acupuncture is effective for chronic low back pain.[62] Conducting research on low back pain is unusually problematic since most patients have experienced "conventional care" - which is itself relatively ineffective - and have low expectations for it. As such, conventional care groups may not be an adequate scientific control and may even lead to nocebo effects that can further inflate of the apparent effectiveness of acupuncture.[57]
There are both positive[63] and negative[64] reviews regarding the effectiveness of acupuncture when combined with in vitro fertilisation.
A Cochrane Review concluded that acupuncture was effective in reducing the risk of post-operative nausea and vomiting with minimal side effects, though it was less than or equal to the effectiveness of preventive antiemetic medications.[9] A 2006 review initially concluded that acupuncture appeared to be more effective than antiemetic drugs, but the authors subsequently retracted this conclusion due to a publication bias in Asian countries that had skewed their results; their ultimate conclusion was in line with the Cochrane Review - acupuncture was approximately equal to, but not better than preventive antiemetic drugs in treating nausea.[65] Another Cochrane Review concluded that electroacupuncture can be helpful in the treatment of vomiting after the start of chemotherapy, but more trials were needed to test their effectiveness versus modern antivomiting medication.[66]
There is moderate evidence that for neck pain, acupuncture is more likely to be effective than sham treatment and offers short-term improvement compared to those on a waiting list.[67]
There is evidence to support the use of acupuncture to treat headaches that are idiopathic, though the evidence is not conclusive and more studies need to be conducted.[68] Several trials have indicated that migraine patients benefit from acupuncture, although the correct placement of needles seems to be less relevant than is usually thought by acupuncturists. Overall in these trials acupuncture was associated with slightly better outcomes and fewer adverse effects than prophylactic drug treatment.[69]
There is conflicting evidence that acupuncture may be useful for osteoarthritis of the knee, with both positive,[70][71] and negative[58] results. The Osteoarthritis Research Society International released a set of consensus recommendations in 2008 that concluded acupuncture may be useful for treating the symptoms of osteoarthritis of the knee.[72]
A systematic review of the best five randomized controlled trials available concluded there was insufficient evidence to support the use of acupuncture in the treatment of the symptoms of fibromyalgia.[73]
For the following conditions, the Cochrane Collaboration has concluded there is insufficient evidence to determine whether acupuncture is beneficial, often because of the paucity and poor quality of the research, and that further research is needed: chronic asthma,[74] Bell's palsy,[75] cocaine dependence,[76] depression,[77] rimary dysmenorrhoea (incorporating TENS,[78] epilepsy,[79] glaucoma,[80] insomnia,[81] irritable bowel syndrome,[82] induction of childbirth,[83] rheumatoid arthritis,[84] shoulder pain,[85] schizophrenia,[86] smoking cessation,[87] acute stroke,[88] stroke rehabilitation,[89] tennis elbow,[90] and vascular dementia.[91]
Positive results from some studies on the efficacy of acupuncture may be as a result of poorly designed studies or publication bias.[92][93] Edzard Ernst and Simon Singh state that as the quality of experimental tests of acupuncture have increased over the course of several decades (through better blinding, the use of sham needling as a form of placebo control, etc.) the results have demonstrated less and less evidence that acupuncture is better than placebo at treating most conditions.[94]
Neuroimaging studies
A 2005 literature review examining the use of magnetic resonance imaging and positron emission tomography to document the brainwave activity caused by acupuncture[95] concluded that neuroimaging data to date show some promise for being able to distinguish the cortical effects of expectation, placebo, and real acupuncture. The studies reviewed were mostly small and pain-related, and more research is needed to determine the specificity of neural substrate activation in non-painful indications.
Medical organizations
Citing research that had accumulated since 1993, in 1997 the American Medical Association (AMA) produced a report that stated there was insufficient evidence to support acupuncture's effectiveness in treating disease, and highlighted the need for further research. The report also included a policy statement that cited the lack of evidence, and sometimes evidence against, the safety and efficacy of alternative medicine interventions, including acupuncture and called for "Well-designed, stringently controlled research...to evaluate the efficacy of alternative therapies."[96]
Also in 1997, the United States National Institutes of Health (NIH) issued a consensus statement on acupuncture that concluded that despite research on acupuncture being difficult to conduct, there was sufficient evidence to encourage further study and expand its use.[5] The consensus statement and conference that produced it were criticized by Wallace Sampson, writing for an affiliated publication of Quackwatch who stated the meeting was chaired by a strong proponent of acupuncture and failed to include speakers who had obtained negative results on studies of acupuncture. Sampson also stated he believed the report showed evidence of pseudoscientific reasoning.[97] In 2006 the NIH's National Center for Complementary and Alternative Medicine stated that it continued to abide by the recommendations of the NIH consensus statement, even if research is still unable to explain its mechanism.[16]
In 2003 the World Health Organization's Department of Essential Drugs and Medicine Policy produced a report on acupuncture. The report was drafted, revised and updated by Zhu-Fan Xie, the Director for the Institute of Integrated Medicines of Beijing Medical University, and contained, based on research results available in early 1999, a list of diseases, symptoms or conditions for which it was believed acupuncture had been demonstrated as an effective treatment, as well as a second list of conditions that were possibly able to be treated with acupuncture. Noting the difficulties of conducting controlled research and the debate on how to best conduct research on acupuncture, the report was described as "...intended to facilitate research on and the evaluation and application of acupuncture. It is hoped that it will provide a useful resource for researchers, health care providers, national health authorities and the general public."[13] The coordinator for the team that produced the report, Xiaorui Zhang, stated that the report was designed to facilitate research on acupuncture, not recommend treatment for specific diseases.[15] The report was controversial; critics assailed it as being problematic since, in spite of the disclaimer, supporters used it to claim that the WHO endorsed acupuncture and other alternative medicine practices that were either pseudoscientific or lacking sufficient evidence-basis. Medical scientists expressed concern that the evidence supporting acupuncture outlined in the report was weak, and that the report was evidence "[the] WHO has been infiltrated by missionaries for alternative medicine".[15] The report was also criticized in the 2008 book Trick or Treatment for, in addition to being produced by a panel that included no critics of acupuncture at all, containing two major errors - including too many results from low-quality clinical trials, and including a large number of trials originating in China where, probably due to publication bias, no negative trials have ever been produced. In contrast, studies originating in the West include a mixture of positive, negative and neutral results. Ernst and Singh, the authors of the book, described the report as "highly misleading", a "shoddy piece of work that was never rigorously scrutinized" and stated that the results of high-quality clinical trials do not support the use of acupuncture to treat anything but pain and nausea.[98]
The National Health Service of the United Kingdom states that there is "reasonably good evidence that acupuncture is an effective treatment" for nausea, vomiting, osteoarthritis of the knee and several types of pain but "because of disagreements over the way acupuncture trials should be carried out and over what their results mean, this evidence does not allow us to draw definite conclusions". The NHS states there is evidence against acupuncture being useful for rheumatoid arthritis, smoking cessation and weight loss, and inadequate evidence for most other conditions that acupuncture is used for.[60]
Safety
Because acupuncture needles penetrate the skin, many forms of acupuncture are invasive procedures, and therefore not without risk. Injuries are rare among patients treated by trained practitioners.[99][100] In most jurisdictions, needles are required by law to be sterile, disposable and used only once; in some places, needles may be reused if they are first resterilized, e.g. in an autoclave. When needles are contaminated, risk of bacterial or other blood-borne infection increases, as with re-use of any type of needle.[101]
Several styles of Japanese acupuncture use non-inserted needling, making for an entirely non-invasive procedure. In non-inserted needling the needle is brought to the skin, but never penetrates it, and various other acupuncture tools are used to tap or stroke along the meridians. Notable examples of these styles are Tōyōhari and the pediatric acupuncture style Shōnishin.
Adverse events
A survey of adverse events related to acupuncture gave rates of 671 minor adverse events per 10,000 treatments, and no major ones.[102] Another survey found that out of 3535 treatments, 402 resulted in minor adverse events including bleeding, bruising, dizziness, fainting, nausea, paresthesia, increased pain and in one case aphasia.[17] That survey concluded: "Acupuncture has adverse effects, like any therapeutic approach. If it is used according to established safety rules and carefully at appropriate anatomic regions, it is a safe treatment method."[17]
Other injury
Other risks of injury from the improper insertion of acupuncture needles include: Nerve injury, resulting from the accidental puncture of any nerve, Brain damage or stroke, which is possible with very deep needling at the base of the skull, Pneumothorax from deep needling into the lung,[103] Kidney damage from deep needling in the low back, Haemopericardium, or puncture of the protective membrane surrounding the heart, which may occur with needling over a sternal foramen (a hole in the breastbone that occurs as the result of a congenital defect.),[104] Risk of terminating pregnancy with the use of certain acupuncture points that have been shown to stimulate the production of adrenocorticotropic hormone (ACTH) and oxytocin, and with unsterilized needles and lack of infection control: transmission of infectious diseases.
The risk can be reduced through proper training of acupuncturists. Graduates of medical schools and (in the US) accredited acupuncture schools receive thorough instruction in proper technique so as to avoid these events.[105]
Omitting modern medical care
Receiving alternative medicine as a replacement for standard modern medical care could result in inadequate diagnosis or treatment of conditions for which modern medicine has a better treatment record.
Researchers also express concern that unethical or naive practitioners may induce patients to exhaust financial resources by pursuing ineffective treatment.[106][107] Profession ethical codes set by accrediting organizations such as NCCAOM require referrals to make "timely referrals to other health care professionals as may be appropriate."[108] Some public health departments regulate acupuncture.[109][110][111]
Compared with other treatments
Commenting on the relative safety of acupuncture compared with other treatments, the NIH consensus panel stated that "(a)dverse side effects of acupuncture are extremely low and often lower than conventional treatments." They also stated "the incidence of adverse effects is substantially lower than that of many drugs or other accepted medical procedures used for the same condition. For example, musculoskeletal conditions, such as fibromyalgia, myofascial pain, and tennis elbow... are conditions for which acupuncture may be beneficial. These painful conditions are often treated with, among other things, anti-inflammatory medications (aspirin, ibuprofen, etc.) or with steroid injections. Both medical interventions have a potential for deleterious side effects but are still widely used and are considered acceptable treatments."
Legal and political status
Acupuncturists may practice herbal medicine and manipulative therapy (tuina), or be a licensed physician or naturopath who incorporates acupuncture in a simplified form. In many states, medical doctors are not required to have any formal training to perform acupuncture. Over 20 states allow chiropractors to perform acupuncture with less than 200 hours training. The typical amount of hours of medical training by licensed acupuncturists is over 3,000 hours. License is regulated by the state or province in many countries, and often requires passage of a board exam.
In the US, acupuncture is practiced by a variety of healthcare providers. Those who specialize in Acupuncture and Oriental Medicine are usually referred to as "licensed acupuncturists", or L.Ac.'s. The abbreviation "Dipl. Ac." stands for "Diplomate of Acupuncture" and signifies that the holder is board-certified by the NCCAOM.[112] Professional degrees are usually at the level of a Master's degree.
A poll of American doctors in 2005 showed that 59% believe acupuncture was at least somewhat effective.[113] In 1996, the United States Food and Drug Administration changed the status of acupuncture needles from Class III to Class II medical devices, meaning that needles are regarded as safe and effective when used appropriately by licensed practitioners.[114][115] As of 2004, nearly 50% of Americans who were enrolled in employer health insurance plans were covered for acupuncture treatments.[116][117]
Canadian acupuncturists have been licensed in British Columbia since 2003. In Ontario, the practice of acupuncture is now regulated by the Traditional Chinese Medicine Act, 2006, S.O. 2006, chapter 27.[118] The government is in the process of establishing a college[119] whose mandate will be to oversee the implementation of policies and regulations relating to the profession.
In the United Kingdom, acupuncturists are not a regulated profession. Voluntary self-regulation allows patients to find acupuncture practitioners with a level of training and who adhere to a professional code of practice. The principle body for professional standards in traditional/lay acupuncture is the British Acupuncture Council [120], The British Medical Acupuncture Society [121] is an inter-disciplinary professional body for regulated health professional using acupuncture as a modality and then there is the Acupuncture Association of Chartered Physiotherapists [122].
In Australia traditional/lay acupuncture is not a regulated health profession. traditional/lay acupuncture or Chinese Medicine was not included in the National Health Regulation Law [123]. Acupuncture will not be recognised as profession in Australia but as a modality either within Chinese Medicine / traditional Asian healing systems or within the scope of practice of regulated health professions. The practice of acupuncture is governed by a range of state / territory laws relating to consumer protection and infection control. Victoria is the only state of Australia with an operational registration board.[124] Currently acupuncturists in New South Wales are bound by the guidelines in the Public Health (Skin Penetration) Regulation 2000,[125] which is enforced at local council level. Other states of Australia have their own skin penetration acts.
In New Zealand traditional/lay acupuncture is not a regulated health profession. Osteopaths have a scope of practice for Western Medical Acupuncture and Related Needling Techniques [126]. The state-owned Accident Compensation Corporation reimburses for acupuncture treatment by registered healthcare practitioners and some traditional/lay acupuncturists that belong to voluntary professional associations.[127]
Many other countries do not license acupuncturists or require them to be trained.
See also
- Acupoint therapy
- Acupressure
- Auriculotherapy
- Colorpuncture
- Electroacupuncture
- Pressure point
- Susuk
- Trigger point
- Veterinary acupuncture
Footnotes
- ^ Novak, Patricia D.; Norman W. Dorland; Dorland, William A. N. (1995). Dorland's Pocket Medical Dictionary. Philadelphia: W.B. Saunders. ISBN 0-7216-5738-9.
{{cite book}}: CS1 maint: multiple names: authors list (link) - ^ a b c Prioreschi, P (2004). A history of Medicine, Volume 2. Horatius Press. pp. 147–8. ISBN 1888456019.
- ^ a b c d Ernst E, Pittler MH, Wider B, Boddy K. (2007). "Acupuncture: its evidence-base is changing". Am J Chin Med. 35 (1): 21–5. doi:10.1142/S0192415X07004588. PMID 17265547.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ a b Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 18803495, please use {{cite journal}} with
|pmid= 18803495instead. - ^ a b c d e f g h NIH Consensus Development Program (November 3–5, 1997). "Acupuncture --Consensus Development Conference Statement". National Institutes of Health. Retrieved 2007-07-17.
- ^ a b White AR, Filshie J, Cummings TM (2001). "Clinical trials of acupuncture: consensus recommendations for optimal treatment, sham controls and blinding". Complement Ther Med. 9 (4): 237–245. doi:10.1054/ctim.2001.0489. PMID 12184353.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ a b Johnson MI (2006). "The clinical effectiveness of acupuncture for pain relief—you can be certain of uncertainty". Acupunct Med. 24 (2): 71–9. doi:10.1136/aim.24.2.71. PMID 16783282.
- ^ a b Committee on the Use of Complementary and Alternative Medicine by the American Public (2005). "Complementary and Alternative Medicine in the United States" (Document). National Academies Press.
{{cite document}}: Unknown parameter|url=ignored (help) - ^ a b Lee A, Done ML (2004). "Stimulation of the wrist acupuncture point P6 for preventing postoperative nausea and vomiting". Cochrane database of systematic reviews (Online) (3): CD003281. doi:10.1002/14651858.CD003281.pub2. PMID 15266478.
- ^ a b Furlan AD, van Tulder MW, Cherkin DC (2005). "Acupuncture and dry-needling for low back pain". Cochrane database of systematic reviews (Online) (1): CD001351. doi:10.1002/14651858.CD001351.pub2. PMID 15674876.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ a b c Attention: This template ({{cite doi}}) is deprecated. To cite the publication identified by doi: 10.1136/bmj.a3115 , please use {{cite journal}} (if it was published in a bona fide academic journal, otherwise {{cite report}} with
|doi= 10.1136/bmj.a3115instead. - ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 16420542 , please use {{cite journal}} with
|pmid= 16420542instead. - ^ a b Zhu-Fan, X (2003). Zhang X (ed.). "Acupuncture: Review and Analysis of Reports on Controlled Clinical Trials". World Health Organization.
- ^ Singh & Ernst, 2008, p. 70-73.
- ^ a b c McCarthy, M (2005). "Critics slam draft WHO report on homoeopathy". The Lancet. 366 (9487): 705–6. doi:10.1016/S0140-6736(05)67159-0.
- ^ a b "Get the Facts, Acupuncture". National Institute of Health. 2006. Retrieved 2006-03-02.
- ^ a b c Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 12801494 , please use {{cite journal}} with
|pmid= 12801494instead. - ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 12564354 , please use {{cite journal}} with
|pmid= 12564354instead. - ^ Tiran, D (2000). Complementary therapies for pregnancy and childbirth. Elsevier Health Sciences. pp. 79. ISBN 0702023280.
{{cite book}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ e.g. White, A (1999). Acupuncture: a scientific appraisal. Elsevier Health Sciences. pp. 1. ISBN 0750641630.
{{cite book}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Ma, K (1992). "The roots and development of Chinese acupuncture: from prehistory to early 20th century". Acupuncture in Medicine. 10 ((Suppl)): 92–9. doi:10.1136/aim.10.Suppl.92.
- ^ a b Chiu, M (1993). Chinese acupuncture and moxibustion. Elsevier Health Sciences. pp. 2. ISBN 0443042233.
- ^ Robson, T (2004). An Introduction to Complementary Medicine. Allen & Unwin. pp. 90. ISBN 1741140544.
- ^ Dofer, L; Moser, M; Bahr, F; Spindler, K; Egarter-Vigl, E; Giullén, S; Dohr, G; Kenner, T (1999). "A medical report from the stone age?" (pdf). The Lancet. 354 (9183): 1023–5. doi:10.1016/S0140-6736(98)12242-0. PMID 10501382.
- ^ Barnes, 2005, p. 25.
- ^ Unschuld, Paul. Chinese Medicine, p. 94. 1998, Paradigm Publications
- ^ Barnes, 2005, p. 58-9.
- ^ Barnes, 2005, p. 75.
- ^ Barnes, 2005, p. 188.
- ^ Barnes, 2005, p. 308-9.
- ^ Crozier RC (1968). Traditional medicine in modern China: science, nationalism, and the tensions of cultural change. Cambridge: Harvard University Press.
- ^ a b Beyerstein, BL (1996). "Traditional Medicine and Pseudoscience in China: A Report of the Second CSICOP Delegation (Part 1)". Skeptical Inquirer. 20 (4). Committee for Skeptical Inquiry.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Davidson JP (1999). The complete idiot's guide to managing stress. Indianapolis, Ind: Alpha Books. pp. 255. ISBN 0-02-862955-8.
- ^ Frum, David (2000). How We Got Here: The '70s. New York, New York: Basic Books. p. 133. ISBN 0465041957.
{{cite book}}: Cite has empty unknown parameter:|coauthors=(help) - ^ Singh & Ernst, 2008, p. 49.
- ^ Simon Singh (2006-03-26). "A groundbreaking experiment ... or a sensationalised TV stunt?". The Guardian.
- ^ Simon Singh (14 February 2006). "Did we really witness the 'amazing power' of acupuncture?". Daily Telegraph.
- ^ O'Connor J & Bensky D (trans. & eds.) (1981). Acupuncture: A Comprehensive Text. Seattle, Washington: Eastland Press. p. 35. ISBN 0-939616-00-9.
- ^ Singh & Ernst, 2008, p. 52-3.
- ^ Ahn, AC; Colbert, AP; Anderson, BJ; Martinsen, OG; Hammerschlag, R; Cina, S; Wayne, PM; Langevin, HM (2008). "Electrical properties of acupuncture points and meridians: a systematic review". Bioelectromagnetics. 29 (4): 245–56. doi:10.1002/bem.20403. PMID 18240287.
- ^ Cheng, 1987, chapter 12.
- ^ Medical Acupuncture - Spring / Summer 2000- Volume 12 / Number 1
- ^ British Medical Acupuncture Society
- ^ Felix Mann, quoted by Matthew Bauer in Chinese Medicine Times, vol 1 issue 4, August 2006, "The Final Days of Traditional Beliefs? - Part One"
- ^ Sampson, Wallace Sampson (1996). = 2009-09-26 "Traditional Medicine and Pseudoscience in China: A Report of the Second CSICOP Delegation (Part 2)". Skeptical Inquirer. 20 (5).
{{cite journal}}: Check|url=value (help); Unknown parameter|month=ignored (help) - ^ Ulett GA, Acupuncture update 1984, Southern Medical Journal 78:233–234, 1985. Comment found at NCBI - Traditional and evidence-based acupuncture: history, mechanisms, and present status. Ulett GA, Han J, Han S.
- ^ Ted J. Kaptchuk, member of NCCAM's National Advisory Council.
- ^ Kaptchuk, Ted J., The Web That Has No Weaver: Understanding Chinese Medicine, McGraw-Hill Professional, 2000 ISBN 0-8092-2840-8, 9780809228409 500 pages
- ^ Zhen Jiu Xue, p. 177f et passim.
- ^ a b Braverman S (2004). "Medical Acupuncture Review: Safety, Efficacy, And Treatment Practices". Medical Acupuncture. 15 (3).
- ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 12623739, please use {{cite journal}} with
|pmid=12623739instead. - ^ Jordan JB (2006). "Acupuncture treatment for opiate addiction: a systematic review". J Subst Abuse Treat. 30 (4): 309–14. doi:10.1016/j.jsat.2006.02.005. PMID 16716845.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Gates S, Smith LA, Foxcroft DR (2006). "Auricular acupuncture for cocaine dependence". Cochrane Database Syst Rev (1): CD005192. doi:10.1002/14651858.CD005192.pub2. PMID 16437523.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Bearn J, Swami A, Stewart D, Atnas C, Giotto L, Gossop M (2009). "Auricular acupuncture as an adjunct to opiate detoxification treatment: effects on withdrawal symptoms". J Subst Abuse Treat. 36 (3): 345–9. doi:10.1016/j.jsat.2008.08.002. PMID 19004596.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 16734078 , please use {{cite journal}} with
|pmid= 16734078instead. - ^ Sun Y, Gan TJ, Dubose JW, Habib AS (2008). "Acupuncture and related techniques for postoperative pain: a systematic review of randomized controlled trials". Br J Anaesth. 101 (2): 151–60. doi:10.1093/bja/aen146. PMID 18522936.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ a b Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 19942631 , please use {{cite journal}} with
|pmid= 19942631instead. - ^ a b Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 17577006 , please use {{cite journal}} with
|pmid= 17577006instead. - ^ Vickers, AJ (2001). "Message to complementary and alternative medicine: evidence is a better friend than power" (pdf). BMC Complement Altern Med. 1 (1): 1. doi:10.1186/1472-6882-1-1. PMC 32159. PMID 11346455.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ a b "Acupuncture: Evidence for its effectiveness". National Health Service. 2010-03-18. Retrieved 2010-08-10.
- ^ Manheimer E, White A, Berman B, Forys K, Ernst E (2005). "Meta-analysis: acupuncture for low back pain" (PDF). Ann. Intern. Med. 142 (8): 651–63. PMID 15838072.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Chou R, Huffman LH (2007). "Nonpharmacologic therapies for acute and chronic low back pain: a review of the evidence for an American Pain Society/American College of Physicians clinical practice guideline". Ann Intern Med. 147 (7): 492–504. doi:10.1001/archinte.147.3.492. PMID 17909210.
- ^ Manheimer E, Zhang G, Udoff L, Haramati A, Langenberg P, Berman BM, Bouter LM (2008). "Effects of acupuncture on rates of pregnancy and live birth among women undergoing in vitro fertilisation: systematic review and meta-analysis". BMJ. 336 (7643): 545–9. doi:10.1136/bmj.39471.430451.BE. PMC 2265327. PMID 18258932.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ El-Toukhy, T; Sunkara, SK; Khairy, M; Dyer, R; Khalaf, Y; Coomarasamy, A (2008). "A systematic review and meta-analysis of acupuncture in in vitro fertilisation". BMJ. 115 (10): 1203–13. doi:10.1111/j.1471-0528.2008.01838.x. PMID 18652588.
- ^ Lee A, Copas JB, Henmi M, Gin T, Chung RC (2006). "Publication bias affected the estimate of postoperative nausea in an acupoint stimulation systematic review". J Clin Epidemiol. 59 (9): 980–3. doi:10.1016/j.jclinepi.2006.02.003. PMID 16895822.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Ezzo, JM; Richardson, MA; Vickers, A; Allen, C; Dibble, SL; Issell, BF; Lao, L; Pearl, M; Ramirez, G (2006). "Acupuncture-point stimulation for chemotherapy-induced nausea or vomiting". Cochrane database of systematic reviews (Online) (2): CD002285. doi:10.1002/14651858.CD002285.pub2. PMID 16625560.
- ^ Trinh K, Graham N, Gross A, Goldsmith C, Wang E, Cameron I, Kay T (2007). "Acupuncture for neck disorders". Spine. 32 (2): 236–43. doi:10.1097/01.brs.0000252100.61002.d4. PMID 17224820.
{{cite journal}}: CS1 maint: multiple names: authors list (link); Trinh K, Graham N, Gross A, Goldsmith C, Wang E, Cameron I, Kay T (2006). "Acupuncture for neck disorders". Cochrane Database of Systematic Reviews. 3: CD004870. doi:10.1002/14651858.CD004870.pub3. PMID 16856065.{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 11279710, please use {{cite journal}} with
|pmid=11279710instead. - ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 19160193, please use {{cite journal}} with
|pmid=19160193instead. - ^ White A, Foster NE, Cummings M, Barlas P (2007). "Acupuncture treatment for chronic knee pain: a systematic review". Rheumatology. 46 (3): 384–90. doi:10.1093/rheumatology/kel413. PMID 17215263.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Selfe TK, Taylor AG (2008 Jul-Sep). "Acupuncture and osteoarthritis of the knee: a review of randomized, controlled trials". Fam Community Health. 31 (3): 247–54. doi:10.1097/01.FCH.0000324482.78577.0f. PMC 2810544. PMID 18552606.
{{cite journal}}: Check date values in:|year=(help); Unknown parameter|doi_brokendate=ignored (|doi-broken-date=suggested) (help)CS1 maint: year (link) - ^ Zhang, W; Moskowitz, RW; Nuki, G; Abramson, S; Altman, RD; Arden, N; Bierma-Zeinstra, S; Brandt, KD; Croft, P (2008). "OARSI recommendations for the management of hip and knee osteoarthritis, Part II: OARSI evidence-based, expert consensus guidelines" (pdf). Osteoarthritis and Cartilage. 16 (2): 137–162. doi:10.1016/j.joca.2007.12.013. PMID 18279766.
- ^ Mayhew E; Ernst E (2007). "Acupuncture for fibromyalgia—a systematic review of randomized clinical trials". Rheumatology (Oxford, England). 46 (5): 801–4. doi:10.1093/rheumatology/kel406. PMID 17189243.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^
McCarney, RW; Brinkhaus, B; Lasserson, TJ; Linde, K; McCarney, Robert W (2003). "Acupuncture for chronic asthma". Cochrane Database of Systematic Reviews. 2003 (3): CD000008. doi:10.1002/14651858.CD000008.pub2. PMID 14973944. Retrieved 2008-05-02.
{{cite journal}}: More than one of|first1=and|first=specified (help); More than one of|last1=and|last=specified (help) - ^ He, L; Zhou, MK; Zhou, D; Wu, B; Li, N; Kong, SY; Zhang, DP; Li, QF; Yang, J (2004). "Acupuncture for Bell's palsy". Cochrane Database of Systematic Reviews. 2007 (4): CD002914. doi:10.1002/14651858.CD002914.pub3. PMID 17943775. Retrieved 2008-05-02.
- ^ Gates, S; Smith, LA; Foxcroft, DR; Gates, Simon (2006). "Auricular acupuncture for cocaine dependence". Cochrane Database of Systematic Reviews. 2006 (1): CD005192. doi:10.1002/14651858.CD005192.pub2. PMID 16437523. Retrieved 2008-05-02.
- ^ Smith, CA; Hay, PP; Smith, Caroline A (2004-03-17). "Acupuncture for depression". Cochrane Database of Systematic Reviews. 2004 (3): CD004046. doi:10.1002/14651858.CD004046.pub2. PMID 15846693. Retrieved 2008-05-02.
- ^
Proctor, ML; Smith, CA; Farquhar, CM; Stones, RW; Zhu, Xiaoshu; Brown, Julie; Zhu, Xiaoshu (2002
volume=2002). "Transcutaneous electrical nerve stimulation and acupuncture for primary dysmenorrhoea". Cochrane Database of Systematic Reviews (1): CD002123. doi:10.1002/14651858.CD002123. PMID 11869624. Retrieved 2008-05-02.
{{cite journal}}: Check date values in:|year=(help); Missing pipe in:|year=(help); line feed character in|year=at position 5 (help)CS1 maint: year (link) - ^ Cheuk, DK; Wong, V; Cheuk, Daniel (2006). "Acupuncture for epilepsy". Cochrane Database of Systematic Reviews. 2006 (2): CD005062. doi:10.1002/14651858.CD005062.pub2. PMID 16625622. Retrieved 2008-05-02.
- ^ Law, SK; Li, T; Law, Simon K (2007). "Acupuncture for glaucoma". Cochrane Database of Systematic Reviews. 2007 (4): CD006030. doi:10.1002/14651858.CD006030.pub2. PMID 17943876. Retrieved 2008-05-02.
- ^ Cheuk, DK; Yeung, WF; Chung, KF; Wong, V; Cheuk, Daniel KL (2007). "Acupuncture for insomnia". Cochrane Database of Systematic Reviews. 2007 (3): CD005472. doi:10.1002/14651858.CD005472.pub2. PMID 17636800. Retrieved 2008-05-02.
- ^ Lim, B; Manheimer, E; Lao, L; Ziea, E; Wisniewski, J; Liu, J; Berman, B; Manheimer, Eric (2006). "Acupuncture for treatment of irritable bowel syndrome". Cochrane Database of Systematic Reviews. 2006 (4): CD005111. doi:10.1002/14651858.CD005111.pub2. PMID 17054239. Retrieved 2008-05-06.
- ^ Smith, CA; Crowther, CA; Smith, Caroline A (2004). "Acupuncture for induction of labour". Cochrane Database of Systematic Reviews. 2004 (1): CD002962. doi:10.1002/14651858.CD002962.pub2. PMID 14973999. Retrieved 2008-05-06.
- ^ Casimiro, L; Barnsley, L; Brosseau, L; Milne, S; Robinson, VA; Tugwell, P; Wells, G; Casimiro, Lynn (2005). "Acupuncture and electroacupuncture for the treatment of rheumatoid arthritis". Cochrane Database of Systematic Reviews. 2005 (4): CD003788. doi:10.1002/14651858.CD003788.pub2. PMID 16235342. Retrieved 2008-05-06.
- ^ Green, S; Buchbinder, R; Hetrick, S; Green, Sally (2005). "Acupuncture for shoulder pain". Cochrane Database of Systematic Reviews. 2005 (2): CD005319. doi:10.1002/14651858.CD005319. PMID 15846753. Retrieved 2008-05-06.
- ^ Rathbone, J; Xia, J; Rathbone, John (2005). "Acupuncture for schizophrenia". Cochrane Database of Systematic Reviews. 2005 (4): CD005475. doi:10.1002/14651858.CD005475. PMID 16235404. Retrieved 2008-05-06.
- ^ White, AR; Rampes, H; Campbell, JL; White, Adrian R (2006). "Acupuncture and related interventions for smoking cessation". Cochrane Database of Systematic Reviews. 2006 (1): CD000009. doi:10.1002/14651858.CD000009.pub2. PMID 16437420. Retrieved 2008-05-06.
- ^ Zhang, SH; Liu, M; Asplund, K; Li, L; Liu, Ming (2005). "Acupuncture for acute stroke". Cochrane Database of Systematic Reviews. 2005 (2): CD003317. doi:10.1002/14651858.CD003317.pub2. PMID 15846657. Retrieved 2008-05-06.
- ^ Wu, HM; Tang, JL; Lin, XP; Lau, J; Leung, PC; Woo, J; Li, YP; Wu, Hong Mei (2006). "Acupuncture for stroke rehabilitation". Cochrane Database of Systematic Reviews. 2006 (3): CD004131. doi:10.1002/14651858.CD004131.pub2. PMID 16856031. Retrieved 2008-05-06.
- ^ Green, S; Buchbinder, R; Barnsley, L; Hall, S; White, M; Smidt, N; Assendelft, W; Green, Sally (2002). "Acupuncture for lateral elbow pain". Cochrane Database of Systematic Reviews. 2002 (1): CD003527. doi:10.1002/14651858.CD003527. PMID 11869671. Retrieved 2008-05-06.
- ^ Peng, WN; Zhao, H; Liu, ZS; Wang, S; Weina, Peng (2008). "Acupuncture for vascular dementia". Cochrane Database of Systematic Reviews. 2007 (2): CD004987. doi:10.1002/14651858.CD004987.pub2. PMID 17443563. Retrieved 2008-05-06.
- ^ Tang JL, Zhan SY, Ernst E (1999). "Review of randomised controlled trials of traditional Chinese medicine". BMJ. 319 (7203): 160–1. PMC 28166. PMID 10406751.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Vickers A, Goyal N, Harland R, Rees R (1998). "Do certain countries produce only positive results? A systematic review of controlled trials". Control Clin Trials. 19 (2): 159–66. doi:10.1016/S0197-2456(97)00150-5. PMID 9551280.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Singh & Ernst, 2008, p. 79-82.
- ^ Lewith GT, White PJ, Pariente J (2005). "Investigating acupuncture using brain imaging techniques: the current state of play". Evidence-based complementary and alternative medicine: eCAM. 2 (3): 315–9. doi:10.1093/ecam/neh110. PMC 1193550. PMID 16136210. Retrieved 2007-03-06.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ "Report 12 of the Council on Scientific Affairs (A-97) – Alternative Medicine". American Medical Association. 1997. Retrieved 2009-10-07.
- ^ Sampson, W (2005-03-23). "Critique of the NIH Consensus Conference on Acupuncture". Quackwatch. Retrieved 2009-06-05.
- ^ Singh & Ernst, 2008, p. 277-8.
- ^ Lao L, Hamilton GR, Fu J, Berman BM (2003). "Is acupuncture safe? A systematic review of case reports". Alternative therapies in health and medicine. 9 (1): 72–83. PMID 12564354.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Norheim AJ (1996). "Adverse effects of acupuncture: a study of the literature for the years 1981–1994". Journal of alternative and complementary medicine (New York, N.Y.). 2 (2): 291–7. doi:10.1089/acm.1996.2.291. PMID 9395661.
- ^ http://www.bmj.com/cgi/content/full/340/mar18_1/c1268
- ^ White, A; Hayhoe, S; Hart, A; Ernst, E (2001). "Adverse events following acupuncture: prospective survey of 32 000 consultations with doctors and physiotherapists". British Medical Journal. 323 (7311): 485–6. doi:10.1136/bmj.323.7311.485. PMC 48133. PMID 11532840.
- ^ Leow TK (2001). "Pneumothorax Using Bladder 14". Medical Acupuncture. 16 (2).
- ^ Yekeler, Ensar; Tunaci, M; Tunaci, A; Dursun, M; Acunas, G. "Frequency of Sternal Variations and Anomalies Evaluated by MDCT". American Journal of Roentgenology. 186 (4): 956–60. doi:10.2214/AJR.04.1779. PMID 16554563. Retrieved 2007-11-24.
- ^ Cheng, 1987.
- ^ Be Wary of Acupuncture, Qigong, and "Chinese Medicine"
- ^ Final Report, Report into Traditional Chinese Medicine - NSW Parliament
- ^ NCCAOM Code of Ethics (PDF), retrieved May 30, 2010
- ^ Government of Ontario, Canada - News
- ^ Traditional Chinese Medicine Act, 2006, S.O. 2006, c. 27
- ^ CTCMA
- ^ NCCAOM
- ^ "More than half of the physicians (59%) believed that acupuncture can be effective to some extent." Physicians Divided on Impact of CAM on U.S. Health Care; Aromatherapy Fares Poorly; Acupuncture Touted. HCD Research, 9 September 2005. convenience links: Business Wire, 2005; AAMA, 2005. Link to internet archive version: Cumulative Report
- ^ Updates-June 1996 FDA Consumer
- ^ US FDA/CDRH: Premarket Approvals
- ^ Report: Insurance Coverage for Acupuncture on the Rise. Michael Devitt, Acupuncture Today, January, 2005, Vol. 06, Issue 01
- ^ Claxton, Gary (2004). The Kaiser Family Foundation and Health Research and Educational Trust Employer Health Benefits 2004 Annual Survey (PDF). pp. 106–107. ISBN 0-87258-812-2.
{{cite book}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Traditional Chinese Medicine Act, 2006, S.O. 2006, c. 27
- ^ "Welcome to the TC-CTCMPAO". Ctcmpao.on.ca. Retrieved 2009-09-02.
- ^ http://www.acupuncture.org.uk/index.php
- ^ http://www.medical-acupuncture.co.uk/
- ^ http://www.aacp.org.uk/
- ^ http://www.ahpra.gov.au/
- ^ Welcome to the Chinese Medicine Registration Board of Victoria
- ^ "Health NSW" (PDF).
- ^ http://www.osteopathiccouncil.org.nz/scopes-of-practice.html
- ^ ACC Releases Guidelines for Acupuncture Treatment
References
- Barnes, LL (2005). Needles, herbs, gods, and ghosts: China, healing, and the West to 1848. Harvard University Press. ISBN 0674018729.
- Cheng, X (1987). Chinese Acupuncture and Moxibustion (1st ed.). Foreign Languages Press. ISBN 7-119-00378-X.
- Singh, S (2008). Trick or treatment: The undeniable facts about alternative medicine. W. W. Norton & Company. ISBN 0393066616.
{{cite book}}: Check|isbn=value: checksum (help); Unknown parameter|coauthors=ignored (|author=suggested) (help); Free preview at Google Books - Stux, Gabriel (1988). Basics of Acupuncture. Berlin: Springer-Verlag. ISBN 354053072x.
{{cite book}}: Check|isbn=value: invalid character (help); Unknown parameter|coauthor=ignored (|author=suggested) (help)
Further reading
- Deadman, P (2007). A Manual of Acupuncture. Journal of Chinese Medicine Publications. ISBN 0951054651.
{{cite book}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - Jin, G (2006). Contemporary Medical Acupuncture - A Systems Approach (English). Springer. ISBN 7040192578.
{{cite book}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - Maciocia, G (1989). The Foundations of Chinese Medicine: A Comprehensive Text for Acupuncturists and Herbalists (2nd ed.). Churchill Livingstone. ISBN 0443039801.
External links
- Articles needing cleanup from June 2010
- Cleanup tagged articles without a reason field from June 2010
- Wikipedia pages needing cleanup from June 2010
- Articles needing cleanup from May 2008
- Cleanup tagged articles without a reason field from May 2008
- Wikipedia pages needing cleanup from May 2008
- Acupuncture
- Chinese inventions
- Energy therapies
- Pseudoscience
