Sexually transmitted infection: Difference between revisions
Closer to what WHO ref says. |
superfluous and out of place |
||
| Line 34: | Line 34: | ||
''STD'' may refer only to infections that are causing diseases, or it may be used more loosely as a synonym for ''STI.'' Most of the time, people do not know that they are infected with an STI until they are tested or start showing symptoms of disease. Moreover, the term ''sexually transmissible disease'' is sometimes used since it is less restrictive in consideration of other factors or means of transmission. For instance, [[meningitis]] is transmissible by means of sexual contact but is not labeled an STI because sexual contact is not the primary [[Vector (epidemiology)|vector]] for the [[pathogen]]s that cause meningitis. This discrepancy is addressed by the probability of infection by means ''other than sexual contact''. In general, an STI is an infection that has a negligible probability of transmission by means other than sexual contact, but has a realistic means of transmission by sexual contact (more sophisticated means—[[blood transfusion]], sharing of [[hypodermic needle]]s—are not taken into account). Thus, one may presume that, if a person is infected with an STI, e.g., [[Chlamydia infection|chlamydia]], [[gonorrhea]], [[genital herpes]], [[Human papillomavirus|HPV]] it was transmitted to him/her by means of sexual contact. |
''STD'' may refer only to infections that are causing diseases, or it may be used more loosely as a synonym for ''STI.'' Most of the time, people do not know that they are infected with an STI until they are tested or start showing symptoms of disease. Moreover, the term ''sexually transmissible disease'' is sometimes used since it is less restrictive in consideration of other factors or means of transmission. For instance, [[meningitis]] is transmissible by means of sexual contact but is not labeled an STI because sexual contact is not the primary [[Vector (epidemiology)|vector]] for the [[pathogen]]s that cause meningitis. This discrepancy is addressed by the probability of infection by means ''other than sexual contact''. In general, an STI is an infection that has a negligible probability of transmission by means other than sexual contact, but has a realistic means of transmission by sexual contact (more sophisticated means—[[blood transfusion]], sharing of [[hypodermic needle]]s—are not taken into account). Thus, one may presume that, if a person is infected with an STI, e.g., [[Chlamydia infection|chlamydia]], [[gonorrhea]], [[genital herpes]], [[Human papillomavirus|HPV]] it was transmitted to him/her by means of sexual contact. |
||
The diseases on this list are most commonly transmitted solely by sexual activity. Many infectious diseases, including the [[common cold]], [[influenza]], [[pneumonia]], and most others that are transmitted person-to-person can also be transmitted during sexual contact, if one person is infected, due to the close contact involved. However, even though these diseases may be transmitted during sex, they are not considered STIs. |
|||
==Signs and symptoms== |
==Signs and symptoms== |
||
Revision as of 00:54, 7 December 2014
| Sexually transmitted infection | |
|---|---|
| Specialty | Infectious diseases |
Sexually transmitted infections (STI), also referred to as sexually transmitted diseases (STD) and venereal diseases (VD), are infections that are commonly spread by sex, especially vaginal intercourse, anal sex and oral sex. Most STIs initially do not cause symptoms.[1] This results in a greater risk of passing the disease on to others.[2] Symptoms and signs of disease may include: vaginal discharge, penile discharge, ulcers on or around the genitals, and pelvic pain. STIs acquired before or during birth may result in poor outcomes for the baby. Some STIs may cause problems with the ability to get pregnant.[1]
More than 30 different bacteria, viruses, and parasites can cause STIs.[1] Bacterial STIs include chlamydia, gonorrhea, and syphilis among others. Viral STIs include genital herpes, HIV/AIDS, and genital warts among others. Parasitic STIs include trichomoniasis among others. While usually spread by sex, some STIs can also be spread by non-sexual contact with contaminated blood and tissues, breastfeeding, or during childbirth.[1] STI diagnostic tests are easily available in the developed world, but this is often not the case in the developing world.[1]
The most effective way of preventing STIs is by not having sex.[3] Some vaccinations may also decrease the risk of certain infections including hepatitis B and some types of HPV.[3] Safer sex practices such as use of condoms, having a smaller number of sexual partners, and being in a relationship where each person only has sex with the other also decreases the risk.[1][3] Circumcision in males may be effective to prevent some infections.[1] Most STIs are treatable or curable.[1] Of the most common infections: syphilis, gonorrhea, chlamydia, trichomoniasis are curable while herpes, hepatitis B, HIV/AIDS, and HPV are treatable but not curable.[1] Resistance to certain antibiotics is developing among some organisms such as gonorrhoea.[4]
In 2008, it was estimated that 500 million people were infected with either syphilis, gonorrhea, chlamydia or trichomoniasis.[1] At least an additional 530 million people have genital herpes and 290 million women have human papillomavirus.[1] In the United States there were 19 million new cases of sexually transmitted infections in 2010.[5] Historical documentation of STIs date back to at least the Ebers papyrus around 1550 BC and the Old Testament.[6] There is often shame and stigma associated with these infections.[1] The term sexually transmitted infections is generally preferred over the terms STDs or VD, as it includes those who do not have symptomatic disease.[7]
Classification

Until the 1990s, STIs were commonly known as venereal diseases, the word venereal being derived from the Latin word venereus, and meaning relating to sexual intercourse or desire, ultimately derived from Venus, the Roman goddess of love.[8] Social disease was a phrase used as a euphemism.
Sexually transmitted infection is a broader term than sexually transmitted disease.[9] The World Health Organizations has recommended sexually transmitted infection as the prefered term since 1999.[7] An infection is a colonization by a parasitic species, which may not cause any adverse effects. In a disease, the infection leads to impaired or abnormal function. In either case, the condition may not exhibit signs or symptoms. Increased understanding of infections like HPV, which infects a significant portion of sexually active individuals but cause disease in only a few has led to increased use of the term STI. Public health officials originally introduced the term sexually transmitted infection, which clinicians are increasingly using alongside the term sexually transmitted disease in order to distinguish it from the former.[10]
STD may refer only to infections that are causing diseases, or it may be used more loosely as a synonym for STI. Most of the time, people do not know that they are infected with an STI until they are tested or start showing symptoms of disease. Moreover, the term sexually transmissible disease is sometimes used since it is less restrictive in consideration of other factors or means of transmission. For instance, meningitis is transmissible by means of sexual contact but is not labeled an STI because sexual contact is not the primary vector for the pathogens that cause meningitis. This discrepancy is addressed by the probability of infection by means other than sexual contact. In general, an STI is an infection that has a negligible probability of transmission by means other than sexual contact, but has a realistic means of transmission by sexual contact (more sophisticated means—blood transfusion, sharing of hypodermic needles—are not taken into account). Thus, one may presume that, if a person is infected with an STI, e.g., chlamydia, gonorrhea, genital herpes, HPV it was transmitted to him/her by means of sexual contact.
Signs and symptoms
Not all STIs are symptomatic, and symptoms may not appear immediately after infection. In some instances a disease can be carried with no symptoms, which leaves a greater risk of passing the disease on to others. Depending on the disease, some untreated STIs can lead to infertility, chronic pain or even death.[11]
Cause
Transmission
The risks and transmission probabilities of sexually transmitted diseases are summarized by act in the table:[12][13][14][15][16][17][18][19][20][21][22][23][24]
| Risk per unprotected sexual act with an infected person | |||
|---|---|---|---|
| Known risks | Possible | ||
| Performing oral sex on a man |
|
| |
| Performing oral sex on a woman | |||
| Receiving oral sex—man | |||
| Receiving oral sex—woman | |||
| Vaginal sex—man | |||
| Vaginal sex—woman | |||
| Anal sex—insertive | |||
| Anal sex—receptive | |||
| Anilingus |
|
| |
Bacterial
- Chancroid (Haemophilus ducreyi)
- Chlamydia (Chlamydia trachomatis)
- Gonorrhea (Neisseria gonorrhoeae), colloquially known as "the clap"
- Granuloma inguinale or (Klebsiella granulomatis)
- Syphilis (Treponema pallidum)
Fungal
- Candidiasis (yeast infection)
Viral

- Viral hepatitis (Hepatitis B virus)—saliva, venereal fluids.
(Note: Hepatitis A and Hepatitis E are transmitted via the fecal-oral route; Hepatitis C is rarely sexually transmittable,[25] and the route of transmission of Hepatitis D (only if infected with B) is uncertain, but may include sexual transmission.[26][27][28]) - Herpes simplex (Herpes simplex virus 1, 2) skin and mucosal, transmissible with or without visible blisters
- HIV (Human Immunodeficiency Virus)—venereal fluids, semen, breast milk, blood
- HPV (Human Papillomavirus)—skin and mucosal contact. 'High risk' types of HPV cause almost all cervical cancers, as well as some anal, penile, and vulvar cancer. Some other types of HPV cause genital warts.
- Molluscum contagiosum (molluscum contagiosum virus MCV)—close contact
Parasites
- Crab louse, colloquially known as "crabs" or "pubic lice" (Pthirus pubis)
- Scabies (Sarcoptes scabiei)
Protozoal
- Trichomoniasis (Trichomonas vaginalis), colloquially known as "trich"
Main types
Sexually transmitted infections include:
- Chlamydia is a sexually transmitted infection caused by the bacterium Chlamydia trachomatis. In women, symptoms may include abnormal vaginal discharge, burning during urination, and bleeding in between periods, although most women do not experience any symptoms.[29] Symptoms in men include pain when urinating, and abnormal discharge from their penis.[30] If left untreated in both men and women, Chlamydia can infect the urinary tract and potentially lead to pelvic inflammatory disease (PID). PID can cause serious problems during pregnancy and even has the potential to cause infertility. It can cause a woman to have a potentially deadly ectopic pregnancy, in which the child is born outside of the uterus. However, Chlamydia can be cured with antibiotics.
- The two most common forms of herpes are caused by infection with herpes simplex virus (HSV). HSV-1 is typically acquired orally and causes cold sores, HSV-2 is usually acquired during sexual contact and affects the genitals, however either strain may affect either site.[31] Some people are asymptomatic or have very mild symptoms. Those that do experience symptoms usually notice them 2 to 20 days after exposure which last 2 to 4 weeks. Symptoms can include small fluid-filled blisters, headaches, backaches, itching or tingling sensations in the genital or anal area, pain during urination, Flu like symptoms, swollen glands, or fever. Herpes is spread through skin contact with a person infected with the virus. The virus affects the areas where it entered the body. This can occur through kissing, vaginal intercourse, oral sex or anal sex. The virus is most infectious during times when there are visible symptoms, however those who are asymptomatic can still spread the virus through skin contact.[32] The primary attack is the most severe because the body does not have any antibodies built up. After the primary attack, one might have recurring attacks that are milder or might not even have future attacks. There is no cure for the disease but there are antiviral medications that treat its symptoms and lower the risk of transmission (Valtrex). Although HSV-1 is typically the "oral" version of the virus, and HSV-2 is typically the "genital" version of the virus, a person with HSV-1 orally CAN transmit that virus to their partner genitally. The virus, either type, will settle into a nerve bundle either at the top of the spine, producing the "oral" outbreak, or a second nerve bundle at the base of the spine, producing the genital outbreak.
- The human papillomavirus (HPV) is the most common STI in the United States.[33] There are more than 40 different strands of HPV and many do not cause any health problems. In 90% of cases the body’s immune system clears the infection naturally within 2 years.[34] Some cases may not be cleared and can lead to genital warts (bumps around the genitals that can be small or large, raised or flat, or shaped like cauliflower) or cervical cancer and other HPV related cancers. Symptoms might not show up until advanced stages. It is important for women to get pap smears in order to check for and treat cancers. There are also two vaccines available for women (Cervarix and Gardasil) that protect against the types of HPV that cause cervical cancer. HPV can be passed through genital-to-genital contact as well as during oral sex. It is important to remember that the infected partner might not have any symptoms.
- Gonorrhea is caused by bacterium that lives on moist mucous membranes in the urethra, vagina, rectum, mouth, throat, and eyes. The infection can spread through contact with the penis, vagina, mouth or anus. Symptoms of Gonorrhea usually appear 2 to 5 days after contact with an infected partner however, some men might not notice symptoms for up to a month. Symptoms in men include burning and pain while urinating, increased urinary frequency, discharge from the penis (white, green, or yellow in color), red or swollen urethra, swollen or tender testicles, or sore throat. Symptoms in women may include vaginal discharge, burning or itching while urinating, painful sexual intercourse, severe pain in lower abdomen (if infection spreads to fallopian tubes), or fever (if infection spreads to fallopian tubes), however many women do not show any symptoms.[35] There are some antibiotic resistant strains for Gonorrhea but most cases can be cured with antibiotics.

- Syphilis is an STI caused by a bacterium. If acquired, syphilis needs to be treated adequately, otherwise it can cause long-term complications and death.[36] Clinical manifestations of syphilis include the ulceration of the uro-genital tract, mouth or rectum; if left untreated the symptoms worsen. In recent years, the prevalence of syphilis has declined in Western Europe, but it has increased in Eastern Europe (former Soviet states). A high incidence of syphilis can be found in places such as Cameroon, Cambodia, Papua New Guinea.[37]
- Trichomoniasis is a common STI that is caused by infection with a protozoan parasite called Trichomonas vaginalis.[38] Trichomoniasis affects both women and men, but symptoms are more common in women.[39] Most patients are treated with an antibiotic called metronidazole, which is very effective.[40]
- HIV (human immunodeficiency virus) damages the body's immune system which interferes with fighting off disease-causing agents. The virus kills CD4 cells, which are white blood cells that help fight off various infections. HIV is carried in body fluids, and is spread by sexual activity. It can also be spread by contact with infected blood, breast feeding, childbirth, and from mother to child during pregnancy.[41] When HIV is at its most advanced stage, an individual is said to have AIDS (acquired immunodeficiency syndrome).[42] There are different stages of the progression of and HIV infection. The stages include primary infection, asymptomatic infection, symptomatic infection, and AIDS. In the primary infection stage, an individual will have flu like symptoms (headache, fatigue, fever, muscle aches) for about 2 weeks. In the asymptomatic stage, symptoms usually disappear, and the patient can remain asymptomatic for years. When HIV progresses to the symptomatic stage, the immune system is weakened, and has a low cell count of CD4+ T Cells. When the HIV infection becomes life-threatening, it is called AIDS. People with AIDS fall prey to opportunistic infections and die as a result.[29] When the disease was first discovered in the 1980s, those who had AIDS were not likely to live longer than a few years. There are now antiretroviral drugs (ARVs) available to treat HIV infections. There is no known cure for HIV or AIDS but the drugs help suppress the virus. By suppressing the amount of virus in the body, people can lead longer and healthier lives. Even though their virus levels may be low they can still spread the virus to others.[43]
Unscreened
There are many species of bacteria, protozoa, fungi, and viruses, many which remain undocumented or poorly studied with regards to sexual transmission. Despite that the above include what are generally known as STIs, sexually transmission of microbes is far from limited to the above list. Since the sexual route of transmission is not considered common, and/or the microbe itself is not implicated in a major research study on disease, the following pathogens are simply not screened for in sexual health clinics. Some of these microbes are known to be sexually transmittable.
Microbes known to be sexually transmissible (but not generally considered STDs/STIs) include:
- Ebola- transmissible 2 months after recovery.[1]
- Marburg virus - Virus in semen for 7 weeks after clinical recovery.[44]
- HTLV (both types 1 and 2) - Sexually transmissible, consumption of breast milk breastfeeding, and once mistaken as a HIV, risk of leukemia.[45]
Pathophysiology
Many STIs are (more easily) transmitted through the mucous membranes of the penis, vulva, rectum, urinary tract and (less often—depending on type of infection) the mouth, throat, respiratory tract and eyes.[46] The visible membrane covering the head of the penis is a mucous membrane, though it produces no mucus (similar to the lips of the mouth). Mucous membranes differ from skin in that they allow certain pathogens into the body.[47] The amount of contact with infective sources which causes infection varies with each pathogen but in all cases a disease may result from even light contact from fluid carriers like venereal fluids onto a mucous membrane.
This is one reason that the probability of transmitting many infections is far higher from sex than by more casual means of transmission, such as non-sexual contact—touching, hugging, shaking hands—but it is not the only reason. Although mucous membranes exist in the mouth as in the genitals, many STIs seem to be easier to transmit through oral sex than through deep kissing. According to a safe sex chart, many infections that are easily transmitted from the mouth to the genitals or from the genitals to the mouth are much harder to transmit from one mouth to another.[48] With HIV, genital fluids happen to contain much more of the pathogen than saliva. Some infections labeled as STIs can be transmitted by direct skin contact. Herpes simplex and HPV are both examples. KSHV, on the other hand, may be transmitted by deep-kissing but also when saliva is used as a sexual lubricant.
Depending on the STI, a person may still be able to spread the infection if no signs of disease are present. For example, a person is much more likely to spread herpes infection when blisters are present than when they are absent. However, a person can spread HIV infection at any time, even if he/she has not developed symptoms of AIDS.
All sexual behaviors that involve contact with the bodily fluids of another person should be considered to contain some risk of transmission of sexually transmitted diseases. Most attention has focused on controlling HIV, which causes AIDS, but each STI presents a different situation.
As may be noted from the name, sexually transmitted diseases are transmitted from one person to another by certain sexual activities rather than being actually caused by those sexual activities. Bacteria, fungi, protozoa or viruses are still the causative agents. It is not possible to catch any sexually transmitted disease from a sexual activity with a person who is not carrying a disease; conversely, a person who has an STI got it from contact (sexual or otherwise) with someone who had it, or his/her bodily fluids. Some STIs such as HIV can be transmitted from mother to child either during pregnancy or breastfeeding.
Although the likelihood of transmitting various diseases by various sexual activities varies a great deal, in general, all sexual activities between two (or more) people should be considered as being a two-way route for the transmission of STIs, i.e., "giving" or "receiving" are both risky although receiving carries a higher risk.
Healthcare professionals suggest safer sex, such as the use of condoms, as the most reliable way of decreasing the risk of contracting sexually transmitted diseases during sexual activity, but safer sex should by no means be considered an absolute safeguard. The transfer of and exposure to bodily fluids, such as blood transfusions and other blood products, sharing injection needles, needle-stick injuries (when medical staff are inadvertently jabbed or pricked with needles during medical procedures), sharing tattoo needles, and childbirth are other avenues of transmission. These different means put certain groups, such as medical workers, and haemophiliacs and drug users, particularly at risk.
Recent epidemiological studies have investigated the networks that are defined by sexual relationships between individuals, and discovered that the properties of sexual networks are crucial to the spread of sexually transmitted diseases. In particular, assortative mixing between people with large numbers of sexual partners seems to be an important factor.
It is possible to be an asymptomatic carrier of sexually transmitted diseases. In particular, sexually transmitted diseases in women often cause the serious condition of pelvic inflammatory disease.
Prevention

Prevention is key in addressing incurable STIs, such as HIV and herpes. Sexual health clinics promote the use of condoms and provide outreach for at-risk communities.
The most effective way to prevent sexual transmission of STIs is to avoid contact of body parts or fluids which can lead to transfer with an infected partner. Not all sexual activities involve contact: cybersex, phonesex or masturbation from a distance are methods of avoiding contact. Proper use of condoms reduces contact and risk. Although a condom is effective in limiting exposure, some disease transmission may occur even with a condom.[49]
Both partners should get tested for STIs before initiating sexual contact, or before resuming contact if a partner engaged in contact with someone else. Many infections are not detectable immediately after exposure, so enough time must be allowed between possible exposures and testing for the tests to be accurate. Certain STIs, particularly certain persistent viruses like HPV, may be impossible to detect with current medical procedures.
Many diseases that establish permanent infections can so occupy the immune system that other diseases become more easily transmitted. The innate immune system led by defensins against HIV can prevent transmission of HIV when viral counts are very low, but if busy with other viruses or overwhelmed, HIV can establish itself. Certain viral STI's also greatly increase the risk of death for HIV infected patients.
Vaccines
Vaccines are available that protect against some viral STIs, such as Hepatitis A, Hepatitis B, and some types of HPV. Vaccination before initiation of sexual contact is advised to assure maximal protection.
Condoms
Condoms and female condoms only provide protection when used properly as a barrier, and only to and from the area that it covers. Uncovered areas are still susceptible to many STDs.
In the case of HIV, sexual transmission routes almost always involve the penis, as HIV cannot spread through unbroken skin, thus properly shielding the insertive penis with a properly worn condom from the vagina or anus effectively stops HIV transmission. An infected fluid to broken skin borne direct transmission of HIV would not be considered "sexually transmitted", but can still theoretically occur during sexual contact, this can be avoided simply by not engaging in sexual contact when having open bleeding wounds.
Other STIs, even viral infections, can be prevented with the use of latex, polyurethane or polyisoprene condoms as a barrier. Some microorganisms and viruses are small enough to pass through the pores in natural skin condoms, but are still too large to pass through latex or synthetic condoms.
Proper usage entails:
- Not putting the condom on too tight at the end, and leaving 1.5 cm (3/4 inch) room at the tip for ejaculation. Putting the condom on snug can and often does lead to failure.
- Wearing a condom too loose can defeat the barrier.
- Avoiding inverting, spilling a condom once worn, whether it has ejaculate in it or not.
- If a user attempts to unroll the condom, but realizes they have it on the wrong side, then this condom should be discarded.
- Being careful with the condom if handling it with long nails.
- Avoiding the use of oil-based lubricants (or anything with oil in it) with latex condoms, as oil can eat holes into them.
- Using flavored condoms for oral sex only, as the sugar in the flavoring can lead to yeast infections if used to penetrate.
Not following the first five guidelines above perpetuates the common misconception that condoms are not tested or designed properly.[citation needed]
In order to best protect oneself and the partner from STIs, the old condom and its contents should be assumed to be infectious. Therefore the old condom must be properly disposed of. A new condom should be used for each act of intercourse, as multiple usage increases the chance of breakage, defeating the effectiveness as a barrier.
Nonoxynol-9
Researchers had hoped that nonoxynol-9, a vaginal microbicide would help decrease STI risk. Trials, however, have found it ineffective[50] and it may put women at a higher risk of HIV infection.[51]
Screening
Sexually active women under the age of 25 and those over 25 with risk should be screened for chlamydia and gonorrhea yearly.[52] After being treated for gonorrhea all people should be re tested for the disease after three months.[52]
Nucleic acid amplification tests are the recommended method of diagnosis for gonorrhea and chlamydia.[53] This can be done on either urine in both men and women, vaginal or cervical swabs in women, or urethral swabs in men.[53]
Diagnosis
Testing may be for a single infection, or consist of a number of tests for a range of STIs, including tests for syphilis, trichomonas, gonorrhea, chlamydia, herpes, hepatitis and HIV. No procedure tests for all infectious agents.
STI tests may be used for a number of reasons:
- as a diagnostic test to determine the cause of symptoms or illness
- as a screening test to detect asymptomatic or presymptomatic infections
- as a check that prospective sexual partners are free of disease before they engage in sex without safer sex precautions (for example, when starting a long term mutually monogamous sexual relationship, in fluid bonding, or for procreation).
- as a check prior to or during pregnancy, to prevent harm to the baby
- as a check after birth, to check that the baby has not caught an STI from the mother
- to prevent the use of infected donated blood or organs
- as part of the process of contact tracing from a known infected individual
- as part of mass epidemiological surveillance
Early identification and treatment results in less chance to spread disease, and for some conditions may improve the outcomes of treatment. There is often a window period after initial infection during which an STI test will be negative. During this period the infection may be transmissible. The duration of this period varies depending on the infection and the test. Diagnosis may also be delayed by reluctance of the infected person to seek a medical professional. One report indicated that people turn to the Internet rather than to a medical professional for information on STIs to a higher degree than for other sexual problems.[54]
Management
High-risk exposure such as that which occurs in rape cases may be treated preventatively using antibiotic combinations such as azithromycin, cefixime, and metronidazole.
An option for treating partners of patients (index cases) diagnosed with chlamydia or gonorrhea is patient-delivered partner therapy, which is the clinical practice of treating the sex partners of index cases by providing prescriptions or medications to the patient to take to his/her partner without the health care provider first examining the partner.[55]
Epidemiology
STD incidence rates remain high in most of the world, despite diagnostic and therapeutic advances that can rapidly render patients with many STDs noninfectious and cure most. In many cultures, changing sexual morals and oral contraceptive use have eliminated traditional sexual restraints, especially for women, and both physicians and patients have difficulty dealing openly and candidly with sexual issues. Additionally, development and spread of drug-resistant bacteria (e.g., penicillin-resistant gonococci) makes some STDs harder to cure. The effect of travel is most dramatically illustrated by the rapid spread of the AIDS virus (HIV-1) from Africa to Europe and the Americas in the late 1970s.[57]
Commonly reported prevalences of STIs among sexually active adolescent girls both with and without lower genital tract symptoms include chlamydia (10–25%), gonorrhea (3–18%), syphilis (0–3%), Trichomonas vaginalis (8–16%), and herpes simplex virus (2–12%).[citation needed] Among adolescent boys with no symptoms of urethritis, isolation rates include chlamydia (9–11%) and gonorrhea (2–3%).[citation needed] A 2008 CDC study found that 25–40% of U.S. teenage girls has a sexually transmitted disease.[58][59]
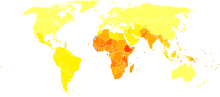
AIDS is among the leading causes of death in present-day Sub-Saharan Africa.[60] HIV/AIDS is transmitted primarily via unprotected sexual intercourse. More than 1.1 million persons are living with HIV/AIDS in the United States,[61] and it disproportionately impacts African Americans.[62] Hepatitis B is also considered a sexually transmitted disease because it can be spread through sexual contact.[63] The highest rates are found in Asia and Africa and lower rates are in the Americas and Europe.[64] Approximately two billion people worldwide have been infected with the hepatitis B virus.[65]
History

The first well-recorded European outbreak of what is now known as syphilis occurred in 1494 when it broke out among French troops besieging Naples.[66] The disease may have originated from the Columbian Exchange.[67] From Naples, the disease swept across Europe, killing more than five million people.[68] As Jared Diamond describes it, "[W]hen syphilis was first definitely recorded in Europe in 1495, its pustules often covered the body from the head to the knees, caused flesh to fall from people's faces, and led to death within a few months," rendering it far more fatal than it is today. Diamond concludes,"[B]y 1546, the disease had evolved into the disease with the symptoms so well known to us today."[69]

Prior to the invention of modern medicines, sexually transmitted diseases were generally incurable, and treatment was limited to treating the symptoms of the disease. The first voluntary hospital for venereal diseases was founded in 1746 at London Lock Hospital.[70] Treatment was not always voluntary: in the second half of the 19th century, the Contagious Diseases Acts were used to arrest suspected prostitutes. In 1924, a number of states concluded the Brussels Agreement, whereby states agreed to provide free or low-cost medical treatment at ports for merchant seamen with venereal diseases.
The first effective treatment for a sexually transmitted disease was salvarsan, a treatment for syphilis. With the discovery of antibiotics, a large number of sexually transmitted diseases became easily curable, and this, combined with effective public health campaigns against STDs, led to a public perception during the 1960s and 1970s that they have ceased to be a serious medical threat.
During this period, the importance of contact tracing in treating STIs was recognized. By tracing the sexual partners of infected individuals, testing them for infection, treating the infected and tracing their contacts in turn, STI clinics could effectively suppress infections in the general population.
In the 1980s, first genital herpes and then AIDS emerged into the public consciousness as sexually transmitted diseases that could not be cured by modern medicine. AIDS in particular has a long asymptomatic period—during which time HIV (the human immunodeficiency virus, which causes AIDS) can replicate and the disease can be transmitted to others—followed by a symptomatic period, which leads rapidly to death unless treated. HIV/AIDS entered the United States from Haiti in about 1969.[71] Recognition that AIDS threatened a global pandemic led to public information campaigns and the development of treatments that allow AIDS to be managed by suppressing the replication of HIV for as long as possible. Contact tracing continues to be an important measure, even when diseases are incurable, as it helps to contain infection.
References
- ^ a b c d e f g h i j k l m "Sexually transmitted infections (STIs) Fact sheet N°110". who.int. November 2013. Retrieved 30 November 2014. Cite error: The named reference "WHO2014" was defined multiple times with different content (see the help page).
- ^ Patrick R. Murray, Ken S. Rosenthal, Michael A. Pfaller, (2013). Medical microbiology (7th ed. ed.). St. Louis, Mo.: Mosby. p. 418. ISBN 9780323086929.
{{cite book}}:|edition=has extra text (help)CS1 maint: extra punctuation (link) CS1 maint: multiple names: authors list (link) - ^ a b c "How You Can Prevent Sexually Transmitted Diseases". cdc.gov. November 5, 2013. Retrieved 5 December 2014.
- ^ Centers for Disease Control and Prevention, (CDC) (10 August 2012). "Update to CDC's Sexually transmitted diseases treatment guidelines, 2010: oral cephalosporins no longer a recommended treatment for gonococcal infections". MMWR. Morbidity and mortality weekly report. 61 (31): 590–4. PMID 22874837.
- ^ "STD Trends in the United States: 2010 National Data for Gonorrhea, Chlamydia, and Syphilis". Centers for Disease Control and Prevention. Retrieved 15 September 2012.
- ^ Gerd Gross, Stephen K. Tyring (2011). Sexually transmitted infections and sexually transmitted diseases. Heidelbergh: Springer Verlag. p. 20. ISBN 9783642146633.
- ^ a b Organization, World Health (2003). Guidelines for the management of sexually transmitted infections (PDF). Geneva: World Health Organization. p. vi. ISBN 9241546263.
- ^ "Venereal". dictionary.reference.com. Retrieved June 18, 2013.
- ^ "Sexually transmitted diseases (STDs)?". PLWHA/National AIDS Resource Center. Retrieved March 25, 2013.
- ^ K. Madhav Naidu. "Epidemiology and Management". Community Health Nursing. Gyan Publishing House (2010). p. 248.
- ^ "Male STI check-up video". Channel 4. 2008. Retrieved 2009-01-22.
- ^ a b c d e f g h i j Sarah Edwards, Chris Carn; Carne (1998). "Oral sex and the transmission of non-viral STIs". Sex Transm in. 74 (1): 95–100. doi:10.1136/sti.74.2.95.
- ^ a b c Maura Gillisons (2007). "HPV Infection Linked to Throat Cancers". Johns Hopkins Medicine.
- ^ a b c d e Hoare A (2010). models of HIV epidemics in Australia and Southeast Asia
- ^ a b c d e Australasian contact tracing manual. Specific infections where contact tracing is generally recommended
- ^ a b c d Varghese B, Maher JE, Peterman TA, Branson BM,Steketee RW; Maher; Peterman; Branson; Steketee (2002). "Reducing the risk of sexual HIV transmission: quantifying the per-act risk for HIV on the basis of choice of partner, sex act, and condom use". Sex. Transm. Dis. 29 (1): 38–43. doi:10.1097/00007435-200201000-00007. PMID 11773877.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ a b Holmes, King; et al. (1970). "An estimate of the risk of men acquiring gonorrhea by sexual contact with infected females". 91 (2): 170–174.
{{cite journal}}: Cite journal requires|journal=(help); Explicit use of et al. in:|author2=(help); Unknown parameter|displayauthors=ignored (|display-authors=suggested) (help) - ^ a b c Mahiane, Séverin-Guy; Legeai, Camille; Taljaard, Dirk; Latouche, Aurélien; Puren, Adrian; Peillon, Aurélie; Bretagnolle, Jean; Lissouba, Pascale; Nguéma, Eugène-Patrice Ndong; Gassiat, Elisabeth; Auvert, Bertran (January 2009). "Transmission probabilities of HIV and herpes simplex virus type 2, effect of male circumcision and interaction: a longitudinal study in a township of South Africa". AIDS. 23 (3): 377–383. doi:10.1097/QAD.0b013e32831c5497. PMC 2831044. PMID 19198042.
{{cite journal}}: Unknown parameter|displayauthors=ignored (|display-authors=suggested) (help) - ^ a b c Burchell A; et al. (March 2006). "Modeling the Sexual Transmissibility of Human Papillomavirus Infection using Stochastic Computer Simulation and Empirical Data from a Cohort Study of Young Women in Montreal, Canada". American Journal of Epidemology. 169 (3): 534–543. doi:10.1093/aje/kwj077. PMID 16421235.
{{cite journal}}: Explicit use of et al. in:|author2=(help); Unknown parameter|displayauthors=ignored (|display-authors=suggested) (help) - ^ a b Platt, Richard; Rice, P. A.; McCormack, W. M. (1983). "Risk of Acquiring Gonorrhea and Prevalence of Abnormal Adnexal Findings Among Women Recently Exposed to Gonorrhea". JAMA. 250 (23): 3205–3209. doi:10.1001/jama.250.23.3205. PMID 6417362.
{{cite journal}}: Unknown parameter|displayauthors=ignored (|display-authors=suggested) (help) - ^ Department of Public Health, City & County of San Francisco (2011).STD Risks Chart
- ^ a b c Jin F; Jansson, James; Law, Matthew; Prestage, Garrett P; Zablotska, Iryna; Imrie, John CG; Kippax, Susan C; Kaldor, John M; Grulich, Andrew E; Wilson, David P (March 2010). "Per-contact probability of HIV transmission in homosexual men in Sydney in the era of HAART". AIDS. 24 (6): 907–913. doi:10.1097/QAD.0b013e3283372d90. PMC 2852627. PMID 20139750.
{{cite journal}}: Unknown parameter|displayauthors=ignored (|display-authors=suggested) (help) - ^ Bryan C (2011)INFECTIOUS DISEASE CHAPTER EIGHT SEXUALLY TRANSMITTED DISEASES
- ^ Richard Pearson (2007). "Pinworm Infection". Merck Manual Home Health Handbook.
- ^ Workowski K, Berman S (2006). "Sexually transmitted diseases treatment guidelines, 2006" (PDF). MMWR Recomm Rep. 55 (RR–11): 1–94. PMID 16888612.
- ^ Wu J, Chen C, Sheen I, Lee S, Tzeng H, Choo K (1995). "Evidence of transmission of hepatitis D virus to spouses from sequence analysis of the viral genome". Hepatology. 22 (6): 1656–60. doi:10.1002/hep.1840220607. PMID 7489970.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Farci P (2003). "Delta hepatitis: an update". J Hepatol. 39 (Suppl 1): S212–9. doi:10.1016/S0168-8278(03)00331-3. PMID 14708706.
- ^ Shukla N, Poles M (2004). "Hepatitis B virus infection: co-infection with hepatitis C virus, hepatitis D virus, and human immunodeficiency virus". Clin Liver Dis. 8 (2): 445–60, viii. doi:10.1016/j.cld.2004.02.005. PMID 15481349.
- ^ a b King, B. (2009). Human Sexuality Today (Sixth ed.). Upper Saddle River: Pearson Education, Inc.
- ^ "Chlamydia Infections: MedlinePlus". Nlm.nih.gov. Retrieved 2013-06-30.
- ^ http://www.webmd.com/genital-herpes/guide/genital-herpes-basics
- ^ "Herpes". Avert.org. Retrieved 2013-06-30.
- ^ "Human Papillomavirus (HPV) | Overview". FamilyDoctor.org. 2010-12-01. Retrieved 2013-06-30.
- ^ "STD Facts - Human papillomavirus (HPV)". Cdc.gov. Retrieved 2013-06-30.
- ^ "Gonorrhea - National Library of Medicine - PubMed Health". Ncbi.nlm.nih.gov. Retrieved 2013-06-30.
- ^ "STD Facts –Syphilis". Cdc.gov. Retrieved 2013-02-18.
- ^ "Syphilis". Who.int. Retrieved 2013-02-18.
- ^ "STD Facts – Trichomoniasis". Cdc.gov. Retrieved 2013-02-18.
- ^ "Trichomoniasis: MedlinePlus". Nlm.nih.gov. Retrieved 2013-02-18.
- ^ "Trichomoniasis – NHS Choices". Nhs.uk. 27 February 2012. Retrieved 2013-02-18.
- ^ "Hiv/Aids". Mayo Clinic.com. 2012-08-11. Retrieved 2013-06-30.
- ^ "AIDS". Avert.org. Retrieved 2013-06-30.
- ^ "HIV/AIDS Treatment". Niaid.nih.gov. 2009-06-03. Retrieved 2013-06-30.
- ^ http://www.hpa.org.uk/Topics/InfectiousDiseases/InfectionsAZ/MarburgHaemorrhagicFever/GeneralInformation/
- ^ Verdonck, K.; González, E.; Van Dooren, S.; Vandamme, A. M.; Vanham, G.; Gotuzzo, E. (2007). "Human T-lymphotropic virus 1: Recent knowledge about an ancient infection". The Lancet Infectious Diseases. 7 (4): 266. doi:10.1016/S1473-3099(07)70081-6.
- ^ K. Madhav Naidu. Community Health Nursing, Gen Next Publications, 2009, p.248
- ^ Virus Pathogenesis, Microbiology Bytes
- ^ Safe Sex Chart, violet blue: open source sex
- ^ Villhauer, Tanya (2005-05-20). "Condoms Preventing HPV?". University of Iowa Student Health Service/Health Iowa. Retrieved 2009-07-26.
- ^ Wilkinson D, Ramjee G, Tholandi M, Rutherford G (2002). Wilkinson, David (ed.). "Nonoxynol-9 for preventing vaginal acquisition of sexually transmitted infections by women from men". Cochrane Database Syst Rev (4): CD003939. doi:10.1002/14651858.CD003939. PMID 12519623.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Williams, M. Healthy Choices for Fertility Control. CreateSpace, Scotts Valley, CA, 2009. ISBN 1-4486-6472-1
- ^ a b Gavin, L (Apr 25, 2014). "Providing Quality Family Planning Services: Recommendations of CDC and the U.S. Office of Population Affairs". MMWR. Recommendations and reports : Morbidity and mortality weekly report. Recommendations and reports / Centers for Disease Control. 63 (RR-04): 1–54. PMID 24759690.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ a b "Screening for Chlamydia and Gonorrhea: U.S. Preventive Services Task Force Recommendation Statement". USPSTF. Retrieved 29 April 2014.
- ^ Quilliam Susan (2011). "'The Cringe Report'". J Fam Plann Reprod Health Care. 37 (2): 110–112.
- ^ Expedited Partner Therapy in the Management of Sexually Transmitted Diseases (2 February 2006) U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES PUBLIC HEALTH SERVICE. Centers for Disease Control and Prevention National Center for HIV, STD, and TB Prevention
- ^ "WHO Disease and injury country estimates". World Health Organization. 2004. Retrieved Nov 11, 2009.
- ^ Mary-Ann Shafer, Anna-Barbara Moscicki (2006). "Sexually Transmitted Infections, 2006": 1–8.
{{cite journal}}: Cite journal requires|journal=(help) - ^ "Sex Infections Found in Quarter of Teenage Girls". The New York Times. March 12, 2008.
- ^ "CDC study says at least 1 in 4 teen girls has a sexually transmitted disease; HPV most common". The Oklahoman. March 11, 2008.
- ^ UNAIDS, WHO (December 2007). "2007 AIDS epidemic update" (PDF). Retrieved 2008-03-12.
- ^ "HIV in the United States: At A Glance". Centers for Disease Control and Prevention.
- ^ "AIDS In Black America: A Public Health Crisis". NPR. July 5, 2012.
- ^ "Hepatitis: Type B (caused by hepatitis B virus)". Minnesota Department of Health.
- ^ "Hepatitis B". U.S. Food and Drug Administration.
- ^ "World Hepatitis Day 2012". WHO. 2012.
- ^ Oriel, J.D. (1994). The Scars of Venus: A History of Venereology. London: Springer-Verlag. ISBN 3-540-19844-X.
- ^ "Columbus May Have Brought Syphilis to Europe". LiveScience. January 15, 2008.
- ^ CBC News Staff (January 2008). "Study traces origins of syphilis in Europe to New World". Retrieved 2014-02-21.
- ^ Diamond, Jared (1997). Guns, Germs and Steel. New York: W.W. Norton. p. 210. ISBN 84-8306-667-X.
- ^ Archives in London and the M25 area (AIM25) London Lock Hospital records
- ^ Gilbert MT, Rambaut A, Wlasiuk G, Spira TJ, Pitchenik AE, Worobey M (November 2007). "The emergence of HIV/AIDS in the Americas and beyond". Proc. Natl. Acad. Sci. U.S.A. 104 (47): 18566–70. doi:10.1073/pnas.0705329104. PMC 2141817. PMID 17978186. Retrieved March 20, 2010.
{{cite journal}}: CS1 maint: multiple names: authors list (link)
Further reading
- Workowski, KA; Berman, S; Centers for Disease Control and Prevention, (CDC) (17 December 2010). "Sexually transmitted diseases treatment guidelines, 2010". MMWR. Recommendations and reports : Morbidity and mortality weekly report. Recommendations and reports / Centers for Disease Control. 59 (RR-12): 1–110. PMID 21160459.
- Aral, Sevgi O (2008). Behavioral Interventions for Prevention and Control of Sexually Transmitted Diseases. : Springer Singapore Pte. Limited. ISBN 978-0-387-85768-8Template:Inconsistent citations
{{cite book}}: CS1 maint: postscript (link) - Faro, Sebastian (2003). Sexually transmitted diseases in women. Lippincott Williams & Wilkins. ISBN 0-397-51303-8Template:Inconsistent citations
{{cite book}}: CS1 maint: postscript (link) - Ford, Carol A; Elizabeth Shimer Bowers (2009). Living with Sexually Transmitted Diseases. Facts On File. ISBN 978-0-8160-7672-7Template:Inconsistent citations
{{cite book}}: CS1 maint: postscript (link) - Sehgal, Virendra N (2003). Sexually Transmitted Diseases (4th ed.). Jaypee Bros. Medical Publishers. ISBN 81-8061-105-1Template:Inconsistent citations
{{cite book}}: CS1 maint: postscript (link) - Shoquist, Jennifer; Diane Stafford (2003). The encyclopedia of sexually transmitted diseases. Facts On File. ISBN 0-8160-4881-9Template:Inconsistent citations
{{cite book}}: CS1 maint: postscript (link)
External links
- Sexually transmitted infection at Curlie
- CDC Sexually Transmitted Diseases Treatment Guidelines, 2010
- STD photo library at Dermnet
- UNFPA: Breaking the Cycle of Sexually Transmitted Infections at UNFPA
- STDs In Color: Sexually Transmitted Disease Facts and Photos
- [1]: Sexually transmitted diseases in the U.S.
