ROS1
Proto-oncogene tyrosine-protein kinase ROS is an enzyme that in humans is encoded by the ROS1 gene.[5][6]
Function
[edit]This proto-oncogene, highly expressed in a variety of tumor cell lines, belongs to the sevenless subfamily of tyrosine kinase insulin receptor genes. The protein encoded by this gene is a type I integral membrane protein with tyrosine kinase activity. The protein may function as a growth or differentiation factor receptor.[6]
Role in cancer
[edit]
ROS1 is a receptor tyrosine kinase (encoded by the gene ROS1) with structural similarity to the anaplastic lymphoma kinase (ALK) protein; it is encoded by the c-ros oncogene and was first identified in 1986.[7][8][9][10] The exact role of the ROS1 protein in normal development, as well as its normal physiologic ligand, have not been defined.[8] Nonetheless, as gene rearrangement events involving ROS1 have been described in lung and other cancers, and since such tumors have been found to be remarkably responsive to small molecule tyrosine kinase inhibitors, interest in identifying ROS1 rearrangements as a therapeutic target in cancer has been increasing.[7][11] In 2016, the small molecule tyrosine kinase inhibitor, crizotinib, was approved for the treatment of patients with metastatic NSCLC whose tumors are ROS1 -positive.[12]
Gene rearrangements involving the ROS1 gene were first detected in glioblastoma tumors and cell lines.[13][14] In 2007 a ROS1 rearrangement was identified in a cell line derived from a lung adenocarcinoma patient.[15] Since that discovery, multiple studies have demonstrated an incidence of approximately 1% in lung cancers, demonstrated oncogenicity, and showed that inhibition of tumor cells bearing ROS1 gene fusions by crizotinib or other ROS1 tyrosine kinase inhibitors was effective in vitro.[16][17][18] Clinical data supports the use of crizotinib in lung cancer patients with ROS1 gene fusions.[19][20] Preclinical and clinical work suggests multiple potential mechanisms of drug resistance in ROS1 + lung cancer, including kinase domain mutations in ROS1 and bypass signaling via RAS and EGFR.[21][22][23] Although the most preclinical and clinical studies of ROS1 gene fusions have been performed in lung cancer, ROS1 fusions have been detected in multiple other tumor histologies, including ovarian carcinoma, sarcoma, cholangiocarcinomas and others.[24] Crizotinib or other ROS1 inhibitors may be effective in other tumor histologies beyond lung cancer as demonstrated by a patient with an inflammatory myofibroblastic tumor harboring a ROS1 fusion with a dramatic response to crizotinib.[25]
Preclinical findings
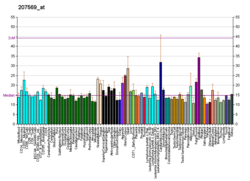
[edit]From a large-scale survey of tyrosine kinase activity in non-small cell lung cancer (NSCLC), and identified more than 50 distinct tyrosine kinases and over 2500 downstream substrates, with the goal of identifying candidate oncogenes.[26] In a sampling of 96 tissue samples from NSCLC patients, approximately 30% displayed high levels of phosphotyrosine expression; further analysis was conducted to identify highly phosphorylated tyrosine kinases in NSCLC from a panel of 41 NSCLC cell lines, and 150 patient samples.[26] Among the top 20 receptor tyrosine kinases identified in this analysis, 15 were identified in both cell lines and tumors, and among these were both ALK and ROS1.[26] These initial findings paved the way for more expansive analyses of ROS1 kinase fusions in NSCLC and other cancers.
Fusion prevalence
[edit]In patients with NSCLC, approximately 2% are positive for a ROS1 gene rearrangement, and these rearrangements are mutually exclusive of ALK rearrangement.[27] ROS1 fusion-positive patients tend to be younger, with a median age of 49.8 years, and never-smokers, with a diagnosis of adenocarcinoma. There is a higher representation of Asian ethnicity and patients with Stage IV disease.[27] ROS1 rearrangements are estimated to be roughly half as common as ALK-rearranged NSCLCs. Similar to ALK-rearranged, ROS1-rearranged NSCLC have younger age of onset and a non-smoking history.[27] A benefit of a small-molecule ALK, ROS1, and cMET inhibitor, crizotinib, was also shown in this patient group.
ROS1 expression was found in approximately 2% of NSCLC patients, and its expression was limited to those patients with ROS1 gene fusions.[11] Similar findings were reported in a separate analysis of 447 NSCLC samples, of which 1.2% were found to be positive for ROS1 rearrangement; this study also confirmed the activity of the ALK/ROS1 /cMET inhibitor crizotinib in ROS1 -positive tumors.[8] ROS1 fusions were also identified in approximately 2% of adenocarcinomas and 1% of glioblastoma samples in an assessment of kinase fusions across different cancers.[28]
Table 1: Sampling of ROS1 Rearrangements Observed in NSCLC and Other Cancers. All of the kinase fusions retain the tyrosine kinase domain of ROS1 . List is not exhaustive. (Adapted from Stumpfova 2012).
| Cancer Type | ROS1 Fusion Gene |
|---|---|
| NSCLC | FIG - ROS1*; SLC34A2 - ROS1*; CD74 - ROS1*; SDC - ROS1*; EZR - ROS1; LRIG3 - ROS1; TPM3 - ROS1 |
| Gastric | SLC34A2 - ROS1* |
| Colorectal | SLC34A2 - ROS1* |
| Spitzoid melanoma | TPM3 - ROS1 |
| Cholangiosarcoma | FIG - ROS1* |
| Glioblastoma | FIG - ROS1* |
| Ovarian | FIG - ROS1* |
| Angiosarcoma | CEP85L-ROS1 |
* Multiple variant isoforms observed
CD74; cluster of differentiation 74, long/short isoforms; EZR; ezrin; FIG; fused in glioblastoma; SDC4; LRIG3; leucine-rich repeats and immunoglobulin-like domains 3; SDC; syndecan 4; SLC34A2; solute carrier family 34 (sodium phosphate), member 2; TPM3; tropomyosin 3
As a drug target
[edit]Several drugs target ROS1 fusions in cancer, with varying levels of success; most of the drugs to date have been tested only for ROS1-positive non-small cell lung carcinoma (NSCLC).[29] However, some clinical trials (like those for entrectinib, DS-6051b, and TPX-0005) accept patients with ROS1 cancer in any type of solid tumor.
- Crizotinib is approved for treating metastatic ROS1-positive NSCLC in many countries. In clinical trials, crizotinib was shown to be effective for 70-80% of ROS1+ NSCLC patients, but it does not effectively treat the brain. Some patients have a response that lasts for years.[30] Crizotinib is available to patients with solid tumors other than NSCLC through clinical trials.[31][32]
- Entrectinib (RXDX-101) is a selective tyrosine kinase inhibitor developed by Ignyta, Inc., with specificity, at low nanomolar concentrations, for all of three Trk proteins (encoded by the three NTRK genes, respectively) as well as the ROS1, and ALK receptor tyrosine kinases. An open label, multicenter, global phase 2 clinical trial called STARTRK-2 started in 2015 to test the drug in patients with ROS1/NTRK/ALK gene rearrangements.[33]
- Lorlatinib (also known as PF-06463922) was shown in an ongoing Phase 2 clinical trial to be effective in some ROS1+ NSCLC patients, and treats the cancer in the brain as well as the body. Lorlatinib has the potential to overcome certain resistance mutations that develop during treatment with crizotinib.[34]
- Ceritinib demonstrates clinical activity (including treating the brain) in ROS1+ NSCLC patients who had previously received platinum-based chemotherapy. In preclinical studies, ceritinib is unable to overcome most ROS1 resistance mutations, including ROS1 G2032R. It has more severe side effects than crizotinib for some patients. Ceritinib is US FDA approved for first line treatment of ALK+ metastatic non-small cell lung cancer.[35][36]
- TPX-0005 preclinical data suggests it is a potent inhibitor of ROS1+ cancer.[37] A Phase I clinical trial opened in March 2017 for patients with advanced solid tumors harboring ALK, ROS1, or NTRK1-3 rearrangements.[38]
- DS-6051b preclinical data show it is active against ROS1-positive cancers.[34] It is an ongoing clinical trial.[39]
- Cabozantinib preclinical data has shown the drug might overcome crizotinib resistance in ROS1+ cancer in early studies.[40] However, the required dosage makes the drug difficult to tolerate for many patients. Cabozantinib is US FDA approved for metastatic medullary thyroid cancer (as Cometriq) and renal cell carcinoma (as Cabometyx).
The ROS1ders
[edit]The ROS1ders [41] is a worldwide collaboration of ROS1+ cancer patients and caregivers with a goal of improving patient outcomes and accelerating research for any type of ROS1+ cancer. It is the first such collaboration focused on cancers driven by a single oncogene. Their website tracks targeted therapies, clinical trials, world experts and new developments for ROS1+ cancers.[42] Partners include patient-focused nonprofits, clinicians who treat ROS1+ patients, ROS1 researchers, pharmaceutical firms and biotech companies.
References
[edit]- ^ a b c GRCh38: Ensembl release 89: ENSG00000047936 – Ensembl, May 2017
- ^ a b c GRCm38: Ensembl release 89: ENSMUSG00000019893 – Ensembl, May 2017
- ^ "Human PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ "Mouse PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ Galland F, Stefanova M, Lafage M, Birnbaum D (July 1992). "Localization of the 5' end of the MCF2 oncogene to human chromosome 15q15----q23". Cytogenetics and Cell Genetics. 60 (2): 114–6. doi:10.1159/000133316. PMID 1611909.
- ^ a b "Entrez Gene: ROS1 v-ros UR2 sarcoma virus oncogene homolog 1 (avian)".
- ^ a b Berge EM, Doebele RC (February 2014). "Targeted therapies in non-small cell lung cancer: emerging oncogene targets following the success of epidermal growth factor receptor". Seminars in Oncology. 41 (1): 110–25. doi:10.1053/j.seminoncol.2013.12.006. PMC 4159759. PMID 24565585.
- ^ a b c Davies KD, Le AT, Theodoro MF, Skokan MC, Aisner DL, Berge EM, Terracciano LM, Cappuzzo F, Incarbone M, Roncalli M, Alloisio M, Santoro A, Camidge DR, Varella-Garcia M, Doebele RC (September 2012). "Identifying and targeting ROS1 gene fusions in non-small cell lung cancer". Clinical Cancer Research. 18 (17): 4570–9. doi:10.1158/1078-0432.CCR-12-0550. PMC 3703205. PMID 22919003.
- ^ Matsushime H, Wang LH, Shibuya M (August 1986). "Human c-ros-1 gene homologous to the v-ros sequence of UR2 sarcoma virus encodes for a transmembrane receptorlike molecule". Molecular and Cellular Biology. 6 (8): 3000–4. doi:10.1128/MCB.6.8.3000. PMC 367872. PMID 3023956.
- ^ Birchmeier C, Birnbaum D, Waitches G, Fasano O, Wigler M (September 1986). "Characterization of an activated human ros gene". Molecular and Cellular Biology. 6 (9): 3109–16. doi:10.1128/MCB.6.9.3109. PMC 367045. PMID 3785223.
- ^ a b Rimkunas VM, Crosby KE, Li D, Hu Y, Kelly ME, Gu TL, Mack JS, Silver MR, Zhou X, Haack H (August 2012). "Analysis of receptor tyrosine kinase ROS1-positive tumors in non-small cell lung cancer: identification of a FIG-ROS1 fusion". Clinical Cancer Research. 18 (16): 4449–57. doi:10.1158/1078-0432.CCR-11-3351. PMID 22661537.
- ^ Berge EM, Doebele RC (February 2014). "Targeted therapies in non-small cell lung cancer: emerging oncogene targets following the success of epidermal growth factor receptor". Seminars in Oncology. 41 (1): 110–25. doi:10.1053/j.seminoncol.2013.12.006. PMC 4159759. PMID 24565585.
- ^ Rabin M, Birnbaum D, Young D, Birchmeier C, Wigler M, Ruddle FH (July 1987). "Human ros1 and mas1 oncogenes located in regions of chromosome 6 associated with tumor-specific rearrangements". Oncogene Research. 1 (2): 169–78. PMID 3329713.
- ^ Birchmeier C, Sharma S, Wigler M (December 1987). "Expression and rearrangement of the ROS1 gene in human glioblastoma cells". Proceedings of the National Academy of Sciences of the United States of America. 84 (24): 9270–4. Bibcode:1987PNAS...84.9270B. doi:10.1073/pnas.84.24.9270. PMC 299735. PMID 2827175.
- ^ Rikova K, Guo A, Zeng Q, Possemato A, Yu J, Haack H, Nardone J, Lee K, Reeves C, Li Y, Hu Y, Tan Z, Stokes M, Sullivan L, Mitchell J, Wetzel R, Macneill J, Ren JM, Yuan J, Bakalarski CE, Villen J, Kornhauser JM, Smith B, Li D, Zhou X, Gygi SP, Gu TL, Polakiewicz RD, Rush J, Comb MJ (December 2007). "Global survey of phosphotyrosine signaling identifies oncogenic kinases in lung cancer". Cell. 131 (6): 1190–203. doi:10.1016/j.cell.2007.11.025. PMID 18083107. S2CID 2316452.
- ^ Takeuchi K, Soda M, Togashi Y, Suzuki R, Sakata S, Hatano S, Asaka R, Hamanaka W, Ninomiya H, Uehara H, Lim Choi Y, Satoh Y, Okumura S, Nakagawa K, Mano H, Ishikawa Y (March 2012). "RET, ROS1 and ALK fusions in lung cancer". Nature Medicine. 18 (3): 378–81. doi:10.1038/nm.2658. PMID 22327623. S2CID 26561572.
- ^ Bergethon K, Shaw AT, Ou SH, Katayama R, Lovly CM, McDonald NT, Massion PP, Siwak-Tapp C, Gonzalez A, Fang R, Mark EJ, Batten JM, Chen H, Wilner KD, Kwak EL, Clark JW, Carbone DP, Ji H, Engelman JA, Mino-Kenudson M, Pao W, Iafrate AJ (March 2012). "ROS1 rearrangements define a unique molecular class of lung cancers". Journal of Clinical Oncology. 30 (8): 863–70. doi:10.1200/JCO.2011.35.6345. PMC 3295572. PMID 22215748.
- ^ Davies KD, Le AT, Theodoro MF, Skokan MC, Aisner DL, Berge EM, Terracciano LM, Cappuzzo F, Incarbone M, Roncalli M, Alloisio M, Santoro A, Camidge DR, Varella-Garcia M, Doebele RC (September 2012). "Identifying and targeting ROS1 gene fusions in non-small cell lung cancer". Clinical Cancer Research. 18 (17): 4570–9. doi:10.1158/1078-0432.CCR-12-0550. PMC 3703205. PMID 22919003.
- ^ Shaw AT, Ou SH, Bang YJ, Camidge DR, Solomon BJ, Salgia R, Riely GJ, Varella-Garcia M, Shapiro GI, Costa DB, Doebele RC, Le LP, Zheng Z, Tan W, Stephenson P, Shreeve SM, Tye LM, Christensen JG, Wilner KD, Clark JW, Iafrate AJ (November 2014). "Crizotinib in ROS1-rearranged non-small-cell lung cancer". The New England Journal of Medicine. 371 (21): 1963–71. doi:10.1056/NEJMoa1406766. PMC 4264527. PMID 25264305.
- ^ Mazières J, Zalcman G, Crinò L, Biondani P, Barlesi F, Filleron T, Dingemans AM, Léna H, Monnet I, Rothschild SI, Cappuzzo F, Besse B, Thiberville L, Rouvière D, Dziadziuszko R, Smit EF, Wolf J, Spirig C, Pecuchet N, Leenders F, Heuckmann JM, Diebold J, Milia JD, Thomas RK, Gautschi O (March 2015). "Crizotinib therapy for advanced lung adenocarcinoma and a ROS1 rearrangement: results from the EUROS1 cohort". Journal of Clinical Oncology. 33 (9): 992–9. doi:10.1200/JCO.2014.58.3302. PMID 25667280.
- ^ Awad MM, Katayama R, McTigue M, Liu W, Deng YL, Brooun A, Friboulet L, Huang D, Falk MD, Timofeevski S, Wilner KD, Lockerman EL, Khan TM, Mahmood S, Gainor JF, Digumarthy SR, Stone JR, Mino-Kenudson M, Christensen JG, Iafrate AJ, Engelman JA, Shaw AT (June 2013). "Acquired resistance to crizotinib from a mutation in CD74-ROS1". The New England Journal of Medicine. 368 (25): 2395–401. doi:10.1056/NEJMoa1215530. PMC 3878821. PMID 23724914.
- ^ Davies KD, Mahale S, Astling DP, Aisner DL, Le AT, Hinz TK, Vaishnavi A, Bunn PA, Heasley LE, Tan AC, Camidge DR, Varella-Garcia M, Doebele RC (2013). "Resistance to ROS1 inhibition mediated by EGFR pathway activation in non-small cell lung cancer". PLOS ONE. 8 (12): e82236. Bibcode:2013PLoSO...882236D. doi:10.1371/journal.pone.0082236. PMC 3862576. PMID 24349229.
- ^ Cargnelutti M, Corso S, Pergolizzi M, Mévellec L, Aisner DL, Dziadziuszko R, Varella-Garcia M, Comoglio PM, Doebele RC, Vialard J, Giordano S (March 2015). "Activation of RAS family members confers resistance to ROS1 targeting drugs". Oncotarget. 6 (7): 5182–94. doi:10.18632/oncotarget.3311. PMC 4467141. PMID 25691052.
- ^ Davies KD, Doebele RC (August 2013). "Molecular pathways: ROS1 fusion proteins in cancer". Clinical Cancer Research. 19 (15): 4040–5. doi:10.1158/1078-0432.CCR-12-2851. PMC 3732549. PMID 23719267.
- ^ Lovly CM, Gupta A, Lipson D, Otto G, Brennan T, Chung CT, Borinstein SC, Ross JS, Stephens PJ, Miller VA, Coffin CM (August 2014). "Inflammatory myofibroblastic tumors harbor multiple potentially actionable kinase fusions". Cancer Discovery. 4 (8): 889–95. doi:10.1158/2159-8290.CD-14-0377. PMC 4125481. PMID 24875859.
- ^ a b c Rikova K, Guo A, Zeng Q, Possemato A, Yu J, Haack H, Nardone J, Lee K, Reeves C, Li Y, Hu Y, Tan Z, Stokes M, Sullivan L, Mitchell J, Wetzel R, Macneill J, Ren JM, Yuan J, Bakalarski CE, Villen J, Kornhauser JM, Smith B, Li D, Zhou X, Gygi SP, Gu TL, Polakiewicz RD, Rush J, Comb MJ (December 2007). "Global survey of phosphotyrosine signaling identifies oncogenic kinases in lung cancer". Cell. 131 (6): 1190–203. doi:10.1016/j.cell.2007.11.025. PMID 18083107. S2CID 2316452.
- ^ a b c Bergethon K, Shaw AT, Ou SH, Katayama R, Lovly CM, McDonald NT, Massion PP, Siwak-Tapp C, Gonzalez A, Fang R, Mark EJ, Batten JM, Chen H, Wilner KD, Kwak EL, Clark JW, Carbone DP, Ji H, Engelman JA, Mino-Kenudson M, Pao W, Iafrate AJ (March 2012). "ROS1 rearrangements define a unique molecular class of lung cancers". Journal of Clinical Oncology. 30 (8): 863–70. doi:10.1200/JCO.2011.35.6345. PMC 3295572. PMID 22215748.
- ^ Stransky N, Cerami E, Schalm S, Kim JL, Lengauer C (2014-01-01). "The landscape of kinase fusions in cancer". Nature Communications. 5 (1): 4846. Bibcode:2014NatCo...5.4846S. doi:10.1038/ncomms5846. PMC 4175590. PMID 25204415.
- ^ Lin JJ, Shaw AT (2017). "Recent Advances in Targeting ROS1 in Lung Cancer". Journal of Thoracic Oncology. 12 (11): 1611–1625. doi:10.1016/j.jtho.2017.08.002. PMC 5659942. PMID 28818606.
- ^ Shaw AT, Ou SH, Bang YJ, Camidge DR, Solomon BJ, Salgia R, et al. (2014). "Crizotinib in ROS1-rearranged non-small-cell lung cancer". The New England Journal of Medicine. 371 (21): 1963–71. doi:10.1056/NEJMoa1406766. PMC 4264527. PMID 25264305.
- ^ Clinical trial number NCT02465060 for "NCI-MATCH: Targeted Therapy Directed by Genetic Testing in Treating Patients With Advanced Refractory Solid Tumors, Lymphomas, or Multiple Myeloma" at ClinicalTrials.gov
- ^ Clinical trial number NCT02693535 for "TAPUR: Testing the Use of Food and Drug Administration (FDA) Approved Drugs That Target a Specific Abnormality in a Tumor Gene in People With Advanced Stage Cancer (TAPUR)" at ClinicalTrials.gov
- ^ Clinical trial number NCT02568267 for "Basket Study of Entrectinib (RXDX-101) for the Treatment of Patients With Solid Tumors Harboring NTRK 1/2/3 (Trk A/B/C), ROS1, or ALK Gene Rearrangements (Fusions) (STARTRK-2)" at ClinicalTrials.gov
- ^ a b Khotskaya YB, Holla VR, Farago AF, Mills Shaw KR, Meric-Bernstam F, Hong DS (2017). "Targeting TRK family proteins in cancer". Pharmacology & Therapeutics. 173: 58–66. doi:10.1016/j.pharmthera.2017.02.006. PMID 28174090. S2CID 4243668.
- ^ Santarpia M, Daffinà MG, D'Aveni A, Marabello G, Liguori A, Giovannetti E, Karachaliou N, Gonzalez Cao M, Rosell R, Altavilla G (2017). "Spotlight on ceritinib in the treatment of ALK+ NSCLC: design, development and place in therapy". Drug Design, Development and Therapy. 11: 2047–2063. doi:10.2147/DDDT.S113500. PMC 5503498. PMID 28740365.
- ^ Califano R, Greystoke A, Lal R, Thompson J, Popat S (2017). "Management of ceritinib therapy and adverse events in patients with ALK-rearranged non-small cell lung cancer". Lung Cancer (Amsterdam, Netherlands). 111: 51–58. doi:10.1016/j.lungcan.2017.06.004. hdl:10044/1/54441. PMID 28838397.
- ^ Cui, J. Jean; Zhai, Dayong; Deng, Wei; Huang, Zhongdong; Rogers, Evan; Ung, Jane; Whitten, Jeffrey; Li, Yishan (January 2017). "TPX-0005: A Multi-Faceted Approach to Overcoming Clinical Resistances from Current ALK or ROS1 Inhibitor Treatment in Lung Cancer". Journal of Thoracic Oncology. 12 (1): S1164–S1165. doi:10.1016/j.jtho.2016.11.1639. Retrieved 12 Oct 2017.
- ^ Clinical trial number NCT03093116 for "A Study of TPX-0005 in Patients With Advanced Solid Tumors Harboring ALK, ROS1, or NTRK1-3 Rearrangements (TRIDENT-1)" at ClinicalTrials.gov
- ^ Clinical trial number NCT02279433 for "A First-in-human Study to Evaluate the Safety, Tolerability and Pharmacokinetics of DS-6051b" at ClinicalTrials.gov
- ^ Katayama R, Kobayashi Y, Friboulet L, Lockerman EL, Koike S, Shaw AT, Engelman JA, Fujita N (2015). "Cabozantinib overcomes crizotinib resistance in ROS1 fusion-positive cancer". Clinical Cancer Research. 21 (1): 166–74. doi:10.1158/1078-0432.CCR-14-1385. PMC 4286456. PMID 25351743.
- ^ "ROS1+ Cancer Patients Partner to Increase Research". National Cancer Institute. 23 May 2017. Retrieved 12 Oct 2017.
- ^ https://ros1cancer.com/
Further reading
[edit]- Birchmeier C, O'Neill K, Riggs M, Wigler M (June 1990). "Characterization of ROS1 cDNA from a human glioblastoma cell line". Proceedings of the National Academy of Sciences of the United States of America. 87 (12): 4799–803. Bibcode:1990PNAS...87.4799B. doi:10.1073/pnas.87.12.4799. PMC 54205. PMID 2352949.
- Sharma S, Birchmeier C, Nikawa J, O'Neill K, Rodgers L, Wigler M (1990). "Characterization of the ros1-gene products expressed in human glioblastoma cell lines". Oncogene Research. 5 (2): 91–100. PMID 2691958.
- Matsushime H, Wang LH, Shibuya M (August 1986). "Human c-ros-1 gene homologous to the v-ros sequence of UR2 sarcoma virus encodes for a transmembrane receptorlike molecule". Molecular and Cellular Biology. 6 (8): 3000–4. doi:10.1128/MCB.6.8.3000. PMC 367872. PMID 3023956.
- Satoh H, Yoshida MC, Matsushime H, Shibuya M, Sasaki M (August 1987). "Regional localization of the human c-ros-1 on 6q22 and flt on 13q12". Japanese Journal of Cancer Research. 78 (8): 772–5. PMID 3115921.
- Birchmeier C, Birnbaum D, Waitches G, Fasano O, Wigler M (September 1986). "Characterization of an activated human ros gene". Molecular and Cellular Biology. 6 (9): 3109–16. doi:10.1128/MCB.6.9.3109. PMC 367045. PMID 3785223.
- Sonnenberg-Riethmacher E, Walter B, Riethmacher D, Gödecke S, Birchmeier C (May 1996). "The c-ros tyrosine kinase receptor controls regionalization and differentiation of epithelial cells in the epididymis". Genes & Development. 10 (10): 1184–93. doi:10.1101/gad.10.10.1184. PMID 8675006.
- Zeng L, Sachdev P, Yan L, Chan JL, Trenkle T, McClelland M, Welsh J, Wang LH (December 2000). "Vav3 mediates receptor protein tyrosine kinase signaling, regulates GTPase activity, modulates cell morphology, and induces cell transformation". Molecular and Cellular Biology. 20 (24): 9212–24. doi:10.1128/MCB.20.24.9212-9224.2000. PMC 102179. PMID 11094073.
- Charest A, Kheifets V, Park J, Lane K, McMahon K, Nutt CL, Housman D (February 2003). "Oncogenic targeting of an activated tyrosine kinase to the Golgi apparatus in a glioblastoma". Proceedings of the National Academy of Sciences of the United States of America. 100 (3): 916–21. Bibcode:2003PNAS..100..916C. doi:10.1073/pnas.242741799. PMC 298701. PMID 12538861.
- Charest A, Lane K, McMahon K, Park J, Preisinger E, Conroy H, Housman D (May 2003). "Fusion of FIG to the receptor tyrosine kinase ROS in a glioblastoma with an interstitial del(6)(q21q21)". Genes, Chromosomes & Cancer. 37 (1): 58–71. doi:10.1002/gcc.10207. PMID 12661006. S2CID 39776967.
- Légaré C, Sullivan R (September 2004). "Expression and localization of c-ros oncogene along the human excurrent duct". Molecular Human Reproduction. 10 (9): 697–703. doi:10.1093/molehr/gah087. PMID 15235104.
- Biskup C, Böhmer A, Pusch R, Kelbauskas L, Gorshokov A, Majoul I, Lindenau J, Benndorf K, Böhmer FD (October 2004). "Visualization of SHP-1-target interaction" (PDF). Journal of Cell Science. 117 (Pt 21): 5165–78. doi:10.1242/jcs.01397. hdl:11858/00-001M-0000-0012-EC23-6. PMID 15456853. S2CID 6663944.
- Girish V, Sachdeva N, Minz RW, Radotra B, Mathuria SN, Arora SK (July 2005). "Bcl2 and ROS1 expression in human meningiomas: an analysis with respect to histological subtype". Indian Journal of Pathology & Microbiology. 48 (3): 325–30. PMID 16761743.