Lichen planus: Difference between revisions
m Task 7c: repair/replace et al. in cs1 author/editor parameters; |
|||
| (428 intermediate revisions by more than 100 users not shown) | |||
| Line 1: | Line 1: | ||
{{Infobox disease |
|||
'''Lichen planus''' is an [[inflammatory]] [[disease]] that usually affects the [[skin]], the [[mouth]], or sometimes both. |
|||
| Name = Lichen planus |
|||
| Image = Lichen Planus (2).JPG |
|||
| Caption = Lichen planus affecting the shins. |
|||
| Field = [[Dermatology]] |
|||
| DiseasesDB = 7452 |
|||
| ICD10 = {{ICD10|L|43||l|40}} |
|||
| ICD9 = {{ICD9|697.0}} |
|||
| ICDO = |
|||
| OMIM = |
|||
| MedlinePlus = 000867 |
|||
| eMedicineSubj = derm |
|||
| eMedicineTopic = 233 |
|||
| eMedicine_mult = {{eMedicine2|derm|663}} |
|||
| MeshID = D008010 |
|||
| MeSH2 = D017676 |
|||
}} |
|||
'''Lichen planus''' ('''LP''') is a disease of the [[skin]] and/or [[mucous membrane]]s that resembles [[lichen]]. The cause is unknown, but it is thought to be the result of an [[autoimmune]] process with an unknown initial trigger. There is no cure, but many different medications and procedures have been used to control the symptoms. |
|||
== Cause == |
|||
The term '''lichenoid reaction''' (or '''lichenoid lesion''') refers to a [[lesion]] of similar or identical [[histopathology|histopathologic]] and [[Clinical research|clinical]] appearance to lichen planus (i.e. an area which looks the same as lichen planus, both to the naked eye and under a [[microscope]]).<ref name=Greenberg2008>{{cite book|last=Greenberg MS, Glick M, Ship JA|title=Burket's oral medicine|year=2008|publisher=BC Decker|location=Hamilton, Ont.|isbn=9781550093452|pages=89–97|url=http://books.google.co.uk/books?id=Q2SP8cOZPvkC&pg=PA89&dq=%22lichenoid+reactions%22&hl=en&sa=X&ei=LjPlUqTHKIyqhAfDzICIAg&redir_esc=y#v=onepage&q=%22lichenoid%20reactions%22&f=false|edition=11th}}</ref><ref name=Lewis2012>{{cite book|last=Lewis MAO, Jordan RCK|title=Oral medicine|year=2012|publisher=Manson Publishing|location=London|isbn=9781840761818|pages=66–72|url=http://books.google.co.uk/books?id=_2uLqxLsg5IC&pg=PA70&dq=%22lichenoid+reactions%22&hl=en&sa=X&ei=LjPlUqTHKIyqhAfDzICIAg&redir_esc=y#v=onepage&q=%22lichenoid%20reactions%22&f=false|edition=2nd}}</ref> Sometimes dental materials or certain medications can cause a lichenoid reaction.<ref name=Greenberg2008 /> They can also occur in association with [[graft versus host disease]].<ref name=Greenberg2008 /><ref name=Barnes2009>{{cite book|last=Barnes L (editor)|title=Surgical pathology of the head and neck|year=2009|publisher=Informa healthcare|location=New York|isbn=9781420091632|edition=3rd}}</ref>{{rp|258}} |
|||
The cause of lichen planus is not known, however there are cases of lichen planus-type rashes (known as lichenoid reactions) occurring as [[allergic reaction]]s to [[medications]] for [[high blood pressure]], [[heart disease]] and [[arthritis]]. These lichenoid reactions are referred to as lichenoid mucositis (of the mucosa) or dermatitis (of the skin). Lichen planus has been reported as a complication of chronic hepatitis C virus infection. It has been suggested that true lichen planus may respond to stress, where lesions may present on the mucosa or skin during times of stress in those with the disease. Lichen planus affects women more than men 3:2, and occurs most often in middle-aged adults. Lichen planus in children is rare. |
|||
==Classification== |
|||
== Clinical features == |
|||
Lichen planus has been described as an autoimmune disease,<ref name="Thongprasom 2011" /> a [[dermatosis]],<ref name="Asch 2011" /> a [[papulosquamous disorder]],<!-- <ref name="Sharma 2012" /> --> a [[mucocutaneous disease]],<ref name="Sharma 2012">{{cite journal|last=Sharma|first=A|author2=Białynicki-Birula, R |author3=Schwartz, RA |author4= Janniger, CK |title=Lichen planus: an update and review.|journal=Cutis; cutaneous medicine for the practitioner|date=July 2012|volume=90|issue=1|pages=17–23|pmid=22908728}}</ref> and an [[inflammatory disease]].<ref name="Cheng 2012" /> |
|||
Lichen planus lesions are so called because of their "lichen-like" appearance<ref name=TG2009>{{cite book|last=Limited|first=Therapeutic Guidelines|title=Therapeutic guidelines.|year=2009|publisher=Therapeutic Guidelines|location=North Melbourne, Vic.|isbn=978-0-9804764-3-9|pages=254–255, 302|edition=Version 3.}}</ref> and can be classified by the site they involve, or by their morphology. |
|||
The typical rash of lichen planus is well-described by the "5 P's": well-defined pruritic, planar, purple, polygonal papules. The commonly affected sites are near the wrist and the ankle. The rash tends to heal with prominent blue-black or brownish discoloration that persists for a long time. Besides the typical lesions, many morphological varieties of the rash may occur. |
|||
===Site=== |
|||
Lichen planus may be categorized as affecting [[mucous membrane|mucosal]] or [[skin|cutaneous]] surfaces. |
|||
* ''Cutaneous'' forms are those affecting the skin, scalp, and nails.<ref name="Asch 2011">{{cite journal|last=Asch|first=S|author2=Goldenberg, G |title=Systemic treatment of cutaneous lichen planus: an update.|journal=Cutis; cutaneous medicine for the practitioner|date=March 2011|volume=87|issue=3|pages=129–34|pmid=21488570}}</ref><ref name="Sharma 2012"/><ref name="Usatine 2011" /> |
|||
* ''Mucosal'' forms are those affecting the lining of the [[gastrointestinal tract]] (mouth, pharynx, esophagus, stomach, anus), [[larynx]], and other mucosal surfaces including the genitals, [[peritoneum]], ears, nose, bladder and [[conjunctiva]] of the eyes.<ref name="Cheng 2012">{{cite journal|last=Cheng|first=S|author2=Kirtschig, G |author3=Cooper, S |author4=Thornhill, M |author5=Leonardi-Bee, J |author6= Murphy, R |title=Interventions for erosive lichen planus affecting mucosal sites.|journal=The Cochrane database of systematic reviews|date=Feb 15, 2012|volume=2|pages=CD008092|doi=10.1002/14651858.CD008092.pub2|pmid=22336835}}</ref><ref name=YAMADA2009 /><ref name="Bruch 2010">{{cite book|last=Treister NS, Bruch JM|title=Clinical oral medicine and pathology|year=2010|publisher=Humana Press|location=New York|isbn=978-1-60327-519-4|pages=59–62}}</ref> |
|||
===Pattern=== |
|||
The presence of lesions is not constant and may wax and wane over time. |
|||
Lichen planus lesions can occur in many different forms: |
|||
{| class="wikitable" |
|||
|- |
|||
! Lesion morphology!! Description<ref name=FITZPATRICK2003pp465-8>{{cite book |editor1-first=Irwin M. |editor1-last=Freedberg |title=Fitzpatrick's dermatology in general medicine |year=2003 |publisher=McGraw-Hill |location=New York, NY |isbn=0-07-138076-0 |pages=465–8 |edition=6th}}</ref><ref name=ANDREWS2006pp219-24>{{cite book |first1=William D. |last1=James |first2=Dirk M. |last2=Elston |first3=Timothy G. |last3=Berger |title=Andrews' Diseases of the skin : clinical dermatology |publisher=Saunders/ Elsevier |location=London |isbn=1-4377-0314-3 |edition=11th |pages=219–24}}</ref> |
|||
|- |
|||
| Annular || 'Ring-shaped' lesions that develop gradually from single small pigmented spots into circular groups of papules with clear, unaffected skin in the center. Annular lesions occur in approximately ten percent of lichen planus cases. The ring-like lesions may very slowly enlarge, co-join and morph into larger irregular (serpentine) bands, sometimes accompanied by lines (See Linear, below). |
|||
|- |
|||
| Linear || Papules are arranged in a line (the "Blaschko line").<ref name="GOROUHI2009">{{cite journal|last=Gorouhi|first=F|author2=Firooz A |author3=Khatami A |author4=Ladoyanni E |author5=Bouzari N |author6=Kamangar F |author7=Gill JK |title=Interventions for cutaneous lichen planus |journal=Cochrane Database of Systematic Reviews|year=2009|issue=4|doi=10.1002/14651858.CD008038|url=http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD008038/full}}</ref> This pattern may develop secondary to trauma ([[Koebner phenomenon|koebnerization]]) or, uncommonly, as a spontaneous, isolated eruption, usually on the extremities, and rarely on the face.<ref name=BOLOGNIA2008>{{cite book |editor1-last=Bolognia |editor1-first=Jean L. |title=Dermatology |year=2008 |publisher=Mosby/Elsevier |location=St. Louis |isbn=1-4160-2999-0 |edition=2nd |editor2-first=Joseph L. |editor2-last=Jorizzo |editor3-first=Ronald P. |editor3-last=Rapini}}</ref> |
|||
|- |
|||
| Hypertrophic || This pattern usually occurs on the extremities, especially the shins and the interphalangeal joints, and tends to be the most [[pruritic]] variant of lichen planus. Also known as "Lichen planus verrucosus". |
|||
|- |
|||
| Atrophic || This morphology is characterized by the presence of a few well-demarcated, white-bluish [[papule]]s or plaques with central superficial atrophy. This is a rare variant of lichen planus. |
|||
|- |
|||
| Bullous || This morphology is characterized by the development of vesicles and bullae with the skin lesions. This is a rare variant of lichen planus, and also known as "Vesiculobullous lichen planus". |
|||
|- |
|||
| Ulcerative || This morphology is characterized by chronic, painful bullae and ulceration of the feet, often with [[cicatricial alopecia|cicatricial]] sequelae evident. This is a rare variant of lichen planus. |
|||
|- |
|||
| Pigmented || This morphology is characterized by hyperpigmented, dark-brown [[macule]]s in sun-exposed areas and flexural folds. This is a rare variant of lichen planus. |
|||
|} |
|||
===Overlap syndromes=== |
|||
Inside the mouth, the disease may present in the (1) reticular form or in the (2) erosive form. |
|||
Occasionally, lichen planus is known to occur with other conditions. For example: |
|||
(1) The reticular form is the more common presentation and manifests as white lacy streaks on the mucosa (known as [[Wickham striae]]) or as smaller papules (small raised area). The lesions tend to be bilateral and are asymptomatic. The lacy streaks may also be seen on other parts of the mouth, including the gingiva (gums), the tongue, palate and lips. |
|||
* [[Lupus erythematosus]] overlap syndrome. Lesions of this syndrome share features of both lupus erythematosus and lichen planus. Lesions are usually large and hypopigmented, atrophic, and with a red-to-blue colour and minimal scaling. [[Telangectasia]] may be present.<ref name=ANDREWS2006pp219-24/><ref name=FITZPATRICK2003pp366_470-1>{{cite book |editor1-first=Irwin M. |editor1-last=Freedberg |title=Fitzpatrick's dermatology in general medicine |year=2003 |publisher=McGraw-Hill |location=New York, NY |isbn=0-07-138076-0 |pages=366, 470–1 |edition=6th}}</ref> |
|||
(2) The erosive form presents with erythematous (red) areas that are ulcerated and uncomfortable. The erosion of the thin covering of cells (the epithelium) may occur in multiple areas of the mouth, or in one area, such as the gums. Wickham's striae may also be seen near these ulcerated areas. |
|||
* [[Lichen sclerosus]] overlap syndrome, sharing features of lichen planus and lichen sclerosus.<ref name=ANDREWS2006p220>{{cite book |first1=William D. |last1=James |first2=Dirk M. |last2=Elston |first3=Timothy G. |last3=Berger |title=Andrews' Diseases of the skin : clinical dermatology |publisher=Saunders/ Elsevier |location=London |isbn=1-4377-0314-3 |edition=11th |page=220}}</ref> |
|||
==Signs and symptoms== |
|||
Oral lesions tend to last far longer than skin LP lesions. |
|||
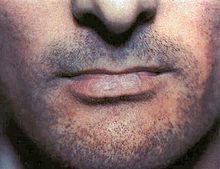
[[File:Lichen planus lip.jpg|thumb|right |Lichen planus affecting the lower lip.]] |
|||
Although lichen planus can present with a variety of lesions, the most common presentation is as a well-defined area of purple-coloured, itchy, flat-topped papules with interspersed lacy white lines (Wickham's striae). This description is known as the characteristic "6 Ps" of lichen planus: planar (flat-topped), purple, polygonal, pruritic, papules, and plaques.<ref name="Usatine 2011" /> This rash, after regressing, is likely to leave an area of hyperpigmentation that slowly fades. That said, a variety of other lesions can also occur.<ref name=TG2009 /> |
|||
Lichen planus may also affect the genital mucosa - vulvovaginal-gingival lichen planus. It can resemble other skin conditions such as [[atopic dermatitis]] and [[psoriasis]]. |
|||
===Cutaneous lichen planus=== |
|||
== Differential Diagnosis == |
|||
[[File:Lichen planus on leg.JPG|thumbnail|right|Cutaneous lichen planus on the shin.]] |
|||
[[File:Lehman, 2009 Fig11.tiff|thumbnail|right|Lichen planus involving the nails.]] |
|||
Variants of cutaneous lichen planus are distinguished based upon the appearance of the lesions and/or their distribution.<ref name=FITZPATRICK2003p466>{{cite book |editor1-first=Irwin M. |editor1-last=Freedberg |title=Fitzpatrick's dermatology in general medicine |year=2003 |publisher=McGraw-Hill |location=New York, NY |isbn=0-07-138076-0 |page=466 |edition=6th}}</ref> Lesions can affect the: |
|||
* Extremities (face, dorsal hands, arms, and nape of neck).{{efn|Cutaneous lichen planus affecting the extremities is also known as "Lichen planus actinicus", "Actinic lichen niditus," "Lichen planus atrophicus annularis," "Lichen planus subtropicus," "Lichen planus tropicus," "Lichenoid melanodermatitis," and "Summertime actinic lichenoid eruption"}} This is more common in Middle Eastern countries in spring and summer, where sunlight appears to have a precipitating effect.<ref name=BOLOGNIA2008 /><ref name=FITZPATRICK2003p468>{{cite book |editor1-first=Irwin M. |editor1-last=Freedberg |title=Fitzpatrick's dermatology in general medicine |year=2003 |publisher=McGraw-Hill |location=New York, NY |isbn=0-07-138076-0 |page=468 |edition=6th}}</ref><ref name=ANDREWS2006p223>{{cite book |first1=William D. |last1=James |first2=Dirk M. |last2=Elston |first3=Timothy G. |last3=Berger |title=Andrews' Diseases of the skin : clinical dermatology |publisher=Saunders/ Elsevier |location=London |isbn=1-4377-0314-3 |edition=11th |page=223}}</ref> |
|||
* Palms and soles |
|||
* [[Intertriginous]] areas of the skin. This is also known as "Inverse lichen planus".<ref name=BOLOGNIA2008 /> |
|||
* Nails<ref name="Gordon 2011">{{cite journal|last=Gordon|first=KA|author2=Vega, JM |author3=Tosti, A |title=Trachyonychia: a comprehensive review |journal=Indian journal of dermatology, venereology and leprology|date=Nov–Dec 2011|volume=77|issue=6|pages=640–5|doi=10.4103/0378-6323.86470|pmid=22016269}}</ref> characterized by irregular longitudinal grooving and ridging of the nail plate, thinning of the nail plate, pterygium formation, shedding of the nail plate with atrophy of the nail bed, subungual keratosis, longitudinal erthronychia (red streaks), and subungual hyperpigmentation.<ref name=ANDREWS2006p781>{{cite book |first1=William D. |last1=James |first2=Dirk M. |last2=Elston |first3=Timothy G. |last3=Berger |title=Andrews' Diseases of the skin : clinical dermatology |publisher=Saunders/ Elsevier |location=London |isbn=1-4377-0314-3 |edition=11th |page=781}}</ref> A [[Trachyonychia|sand-papered appearance]] is present in around 10% of individuals with nail lichen planus.<ref name="Gordon 2011" /> |
|||
* Scalp. This is also known as lichen planopilaris, acuminatus, follicular lichen planus, and peripilaris,<ref name=FITZPATRICK2003p467>{{cite book |editor1-first=Irwin M. |editor1-last=Freedberg |title=Fitzpatrick's dermatology in general medicine |year=2003 |publisher=McGraw-Hill |location=New York, NY |isbn=0-07-138076-0 |page=467 |edition=6th}}</ref> characterised by violaceous, scaly, pruritic papules. Scalp lichen planus can cause [[scarring alopecia]] if it is untreated.<ref name="Usatine 2011">{{cite journal|last=Usatine|first=RP|author2=Tinitigan, M |title=Diagnosis and treatment of lichen planus |journal=American family physician|date=Jul 1, 2011|volume=84|issue=1|pages=53–60|pmid=21766756|url=http://www.aafp.org/afp/2011/0701/p53.html#afp20110701p53-b6}}</ref><ref name=ANDREWS2006p223/><ref name="pmid17467854">{{cite journal |author=Cevasco NC, Bergfeld WF, Remzi BK, de Knott HR |title=A case-series of 29 patients with lichen planopilaris: the Cleveland Clinic Foundation experience on evaluation, diagnosis, and treatment |journal=J. Am. Acad. Dermatol. |volume=57 |issue=1 |pages=47–53 |year=2007 |pmid=17467854 |doi=10.1016/j.jaad.2007.01.011}}</ref> |
|||
* Hair. This variant causes [[cicatricial alopecia|inflammation of hair follicles]] and gradual replacement with scarring. About 10% of people with lichen planus have the scalp or nail variants of the condition.<ref name="Usatine 2011" /> |
|||
Other variants may include: |
|||
* ''Lichen planus pemphigoides'' characterized by the development of tense blisters atop lesions of lichen planus or the development vesicles de novo on uninvolved skin.<ref name=FITZPATRICK2003p471>{{cite book |editor1-first=Irwin M. |editor1-last=Freedberg |title=Fitzpatrick's dermatology in general medicine |year=2003 |publisher=McGraw-Hill |location=New York, NY |isbn=0-07-138076-0 |page=471 |edition=6th}}</ref> |
|||
* ''Keratosis lichenoides chronica'' (also known as "Nekam's disease") is a rare dermatosis characterized by violaceous papular and nodular lesions, often arranged in a linear or reticulate pattern on the dorsal hands and feet, extremities, and buttock, and some cases manifests by sorrheic dermatitis like eruption on the scalp and face, also palmo plantar keratosis has been reported.<ref name=BOLOGNIA2008 /><ref name=FITZPATRICK2003p472>{{cite book |editor1-first=Irwin M. |editor1-last=Freedberg |title=Fitzpatrick's dermatology in general medicine |year=2003 |publisher=McGraw-Hill |location=New York, NY |isbn=0-07-138076-0 |page=472 |edition=6th}}</ref><ref name=ANDREWS2006p224>{{cite book |first1=William D. |last1=James |first2=Dirk M. |last2=Elston |first3=Timothy G. |last3=Berger |title=Andrews' Diseases of the skin : clinical dermatology |publisher=Saunders/ Elsevier |location=London |isbn=1-4377-0314-3 |edition=11th |page=224}}</ref> |
|||
* ''Lichenoid keratoses'' (also known as "Benign lichenoid keratosis," and "Solitary lichen planus"<ref name=BOLOGNIA2008 />) is a cutaneous condition characterized by brown to red scaling maculopapules, found on sun-exposed skin of extremities.<ref name=BOLOGNIA2008 /><ref name=FITZPATRICK2003p473>{{cite book |editor1-first=Irwin M. |editor1-last=Freedberg |title=Fitzpatrick's dermatology in general medicine |year=2003 |publisher=McGraw-Hill |location=New York, NY |isbn=0-07-138076-0 |page=473 |edition=6th}}</ref> Restated, this is a cutaneous condition usually characterized by a solitary dusky-red to violaceous papular skin lesion.<ref name=ANDREWS2006p639>{{cite book |first1=William D. |last1=James |first2=Dirk M. |last2=Elston |first3=Timothy G. |last3=Berger |title=Andrews' Diseases of the skin : clinical dermatology |publisher=Saunders/ Elsevier |location=London |isbn=1-4377-0314-3 |edition=11th |page=639}}</ref> |
|||
* ''Lichenoid dermatitis'' represents a wide range of cutaneous disorders characterized by lichen planus-like skin lesions.<ref name=BOLOGNIA2008 /><ref name=FITZPATRICK2003p473/> |
|||
===Mucosal lichen planus=== |
|||
The clinical presentation of lichen planus may also resemble other conditions, including: |
|||
[[File:Lichen Planus Fig7.tiff|thumbnail|right|Lichen planus on the lips and the lateral border of the tongue]] |
|||
Lichen planus affecting mucosal surfaces may have one lesion or be multifocal.<ref name="Ebrahimi 2012">{{cite journal|last=Ebrahimi|first=M|author2=Lundqvist, L |author3=Wahlin, YB |author4= Nylander, E |title=Mucosal lichen planus, a systemic disease requiring multidisciplinary care: a cross-sectional clinical review from a multidisciplinary perspective |journal=Journal of lower genital tract disease|date=October 2012|volume=16|issue=4|pages=377–80|pmid=22622344|doi=10.1097/LGT.0b013e318247a907}}</ref> Examples of lichen planus affecting mucosal surfaces include:<ref name="Ebrahimi 2012"/> |
|||
* ''[[Esophagus|Esophageal]] lichen planus'', affecting the esophageal mucosa. This can present with [[dysphagia|difficulty or pain when swallowing]] due to [[esophagitis|oesophageal inflammation]], or as the development of an [[esophageal stricture]]. It has also been hypothesized that it is a precursor to squamous cell carcinoma of the esophagus.<ref name=YAMADA2009>{{cite book|last=Yamada T, Alpers DH|title=Textbook of gastroenterology|year=2009|publisher=Blackwell Pub.|location=Chichester, West Sussex|isbn=978-1-4051-6911-0|edition=5th|page=3304|display-authors=etal}}</ref><ref>{{cite journal|last=Chandan|first=VS|author2=Murray, JA |author3=Abraham, SC |title=Esophageal lichen planus |journal=Archives of pathology & laboratory medicine|date=June 2008|volume=132|issue=6|pages=1026–9|pmid=18517264|doi=10.1043/1543-2165(2008)132[1026:ELP]2.0.CO;2}}</ref> |
|||
* ''Genital lichen planus,'' which may cause lesions on the [[glans penis]] or skin of the scrotom in males, and the vulva or vagina in females.<ref name="Usatine 2011" /> Symptoms may include [[lower urinary tract symptom]]s associated with [[stenosis]] of the [[urethra]], [[dyspareunia|painful sexual intercourse]], and itching.<ref name="Usatine 2011" /> In females, ''Vulvovaginal-gingival syndrome,'' is severe and distinct variant affecting the [[vulva]], [[vagina]], and gums, with complications including scarring, vaginal stricture formation,<ref>{{cite journal|last=Panagiotopoulou|first=N|author2=Wong, CS |author3=Winter-Roach, B |title=Vulvovaginal-gingival syndrome.|journal=Journal of obstetrics and gynaecology : the journal of the Institute of Obstetrics and Gynaecology|date=April 2010|volume=30|issue=3|pages=226–30|pmid=20373919|doi=10.3109/01443610903477572}}</ref> or vulva destruction.<ref name="Schlosser 2010">{{cite journal|last=Schlosser|first=BJ|title=Lichen planus and lichenoid reactions of the oral mucosa.|journal=Dermatologic therapy|date=May–Jun 2010|volume=23|issue=3|pages=251–67|doi=10.1111/j.1529-8019.2010.01322.x|pmid=20597944}}</ref> The corresponding syndrome in males, affecting the glans penis and gums, is the ''peno-gingival syndrome''.<ref name=BOLOGNIA2008 /> It is associated with [[HLA-DQB1]].<ref name=BOLOGNIA2008 /><ref name="Nico 2011">{{cite journal|last=Nico|first=MM|author2=Fernandes, JD |author3=Lourenço, SV |title=Oral lichen planus.|journal=Anais brasileiros de dermatologia|date=Jul–Aug 2011|volume=86|issue=4|pages=633–41; quiz 642–3|pmid=21987126|url=http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0365-05962011000400002&lng=en&nrm=iso&tlng=en}}</ref> |
|||
====Oral lichen planus==== |
|||
* Lichenoid drug reaction |
|||
Oral lichen planus (also termed ''oral mucosal lichen planus''),<ref>{{cite journal|last=Alam|first=F|author2=Hamburger, J |title=Oral mucosal lichen planus in children.|journal=International journal of paediatric dentistry / the British Paedodontic Society [and] the International Association of Dentistry for Children|date=May 2001|volume=11|issue=3|pages=209–14|pmid=11484471}}</ref> is a form of mucosal lichen planus, where lichen planus involves the [[oral mucosa]], the lining of the mouth. This may occur in combination with other variants of lichen planus.<ref name="Scully 2013" /> Six clinical forms of oral lichen planus are recognized:<ref name="Scully 2013">{{cite book|last=Scully C|title=Oral and maxillofacial medicine : the basis of diagnosis and treatment|year=2008|publisher=Churchill Livingstone|location=Edinburgh|isbn=9780702049484|edition=3rd|pages=192–199}}</ref> |
|||
* Discoid Lupus Erythematosus |
|||
* ''Reticular'', the most common presentation of oral lichen planus,<ref name="Thongprasom 2011" /> is characterised by the net-like or spider web-like appearance of lacy white lines, oral variants of Wickham's straiae.<ref name="Scully 2013" /> This is usually asymptomatic.<ref name="Thongprasom 2011" /> |
|||
* Chronic Ulcerative Stomatitis |
|||
* ''Erosive/ulcerative'', the second most common form of oral lichen planus,<ref name="Thongprasom 2011" /> is characterised by [[mouth ulcer|oral ulcers]] presenting with persistent, irregular areas of [[erythema|redness]], ulcerations and erosions covered with a yellow slough.<!-- <ref name="Scully 2013" /> --> This can occur in one or more areas of the mouth. In 25% of people with erosive oral lichen planus, the gums are involved, described as [[desquamative gingivitis]] (a condition not unique to lichen planus). <!-- <ref name="Scully 2013" /> --> This may be the initial or only sign of the condition.<ref name="Scully 2013" /> |
|||
* Pemphigus Vulgaris |
|||
* ''Papular,'' with white papules. |
|||
* Benign Mucous Membrane Pemphigoid |
|||
* ''Plaque-like'' appearing as a white patch which may resemble [[leukoplakia]].<ref name="Scully 2013" /> |
|||
* Oral leukoplakia |
|||
* ''Atrophic,'' appearing as areas. Atrophic oral lichen planus may also manifest as desquamative gingivitis.<ref name="Scully 2013" /> |
|||
* Fricional keratosis |
|||
* ''Bullous,'' appearing as fluid-filled vesicles which project from the surface. |
|||
These types often coexist in the same individual. Oral lichen planus tends to present bilaterally as mostly white lesions on the [[buccal mucosa|inner cheek]],<ref name="Thongprasom 2011" /> although any mucosal site in the mouth may be involved. Other sites, in decreasing order of frequency, may include the tongue, lips, gingivae, floor of the mouth, and very rarely, the palate.<ref name="Thongprasom 2011" /> |
|||
A biopsy is useful in identifying histological features that help differentiate lichen planus from these conditions. |
|||
Generally, oral lichen planus tends not to cause any discomfort or pain, although some people may experience soreness when eating or drinking acidic or spicy foodstuffs or beverages.<ref name="Scully 2013" /> When symptoms arise, they are most commonly associated with the atrophic and ulcerative subtypes. These symptoms can include a burning sensation to severe pain.<ref name="Thongprasom 2011" /> |
|||
== Cure == |
|||
==Causes== |
|||
Currently there is no cure for lichen planus but there are certain types of medicines used to reduce the effects of the inflammation. Lichen planus may go into a dormant state after treatment. There are also reports that lichen planus can flare up years after it is considered cured. |
|||
The cause of lichen planus is unknown,<ref name=TG2009 /><ref name="Nico 2011" /><ref name="Roopashree 2010">{{cite journal|last=Roopashree|first=MR|author2=Gondhalekar, RV |author3=Shashikanth, MC |author4=George, J |author5=Thippeswamy, SH |author6= Shukla, A |title=Pathogenesis of oral lichen planus--a review.|journal=Journal of oral pathology & medicine : official publication of the International Association of Oral Pathologists and the American Academy of Oral Pathology|date=November 2010|volume=39|issue=10|pages=729–34|pmid=20923445|doi=10.1111/j.1600-0714.2010.00946.x}}</ref> but it is not contagious and does not involve any known [[pathogen]].<ref name=DAVIDSONS2009 /> It is thought to be a [[T cell]] mediated [[autoimmunity|autoimmune]] reaction (where the body's immune system targets its own tissues).<ref name="Thongprasom 2011" /> This autoimmune process triggers [[apoptosis]] of the [[epithelium|epithelial cells]].<ref name="Thongprasom 2011" /> Several [[cytokine]]s are involved in lichen planus, including [[tumor necrosis factor alpha]], [[interferon gamma]], [[IL1A|interleukin-1 alpha]], [[interleukin 6]], and [[interleukin 8]].<ref name="Thongprasom 2011" /> This autoimmune, T cell mediated, process is thought to be in response to some [[antigen]]ic change in the oral mucosa, but a specific antigen has not been identified.<ref name="Thongprasom 2011" /> |
|||
Where a causal or triggering agent is identified, this is termed a '''lichenoid reaction''' rather than lichen planus. These may include:<ref name="Bruch 2010" /> |
|||
Medicines used to treat lichen planus include: |
|||
* Drug reactions, with the most common inducers including gold salts, [[beta blocker]]s, traditional [[malaria|antimalarials]] (e.g. [[quinine]]), [[thiazide diuretics]], [[furosemide]], [[spironolactone]], [[Metformin]] and [[penicillamine]].<ref name=DAVIDSONS2009>{{cite book|first=the editors Nicki R. Colledge, Brian R. Walker, Stuart H. Ralston ; illustrated by Robert Britton|title=Davidson's principles and practice of medicine.|year=2010|publisher=Churchill Livingstone/Elsevier|location=Edinburgh|isbn=978-0-7020-3085-7|pages=1265–1266|edition=21st}}</ref> |
|||
* [[Oral]] and [[topical]] [[steroids]]. |
|||
* Reactions to amalgam (metal alloys) fillings (or when they are removed/replaced),<ref name=ISSA2004>{{cite journal|last=Issa|first=Y|author2=Brunton, PA |author3=Glenny, AM |author4= Duxbury, AJ |title=Healing of oral lichenoid lesions after replacing amalgam restorations: a systematic review.|journal=Oral surgery, oral medicine, oral pathology, oral radiology, and endodontics|date=November 2004|volume=98|issue=5|pages=553–65|pmid=15529127|doi=10.1016/j.tripleo.2003.12.027}}</ref> |
|||
* Oral [[retinoids]] |
|||
* [[Graft-versus-host disease]] lesions, which chronic lichenoid lesions seen on the palms, soles, face and upper trunk after several months.<ref name=DAVIDSONS2009 /> |
|||
* immunosuppressant medications |
|||
* Hepatitis, specifically [[hepatitis B]] and [[hepatitis C]] infection, and [[primary biliary cirrhosis]].<ref name=ANDREWS2006p220/><ref name=DAVIDSONS2009 /> |
|||
* [[hydroxychloroquine]] |
|||
* [[tacrolimus]] |
|||
* [[dapsone]] |
|||
It has been suggested that lichen planus may respond to [[Stress (medicine)|stress]], where lesions may present during times of stress. Lichen planus can be part of [[Grinspan's syndrome]].{{Citation needed|date=August 2013}} |
|||
== Lichen planopilaris == |
|||
It has also been suggested that mercury exposure may contribute to lichen planus.<ref>{{cite journal |vauthors=Dunsche A, Frank MP, Lüttges J, etal |title=Lichenoid reactions of murine mucosa associated with amalgam |journal=The British Journal of Dermatology |volume=148 |issue=4 |pages=741–8 | date=April 2003 |pmid=12752133 |doi=10.1046/j.1365-2133.2003.05229.x}}</ref> |
|||
Lichen Planopilaris is the specific name given to lichen planus on the [[scalp]] that may cause permanent, scarring [[alopecia]]. If left untreated the scarring will cause permanent hair loss. The Cicatricial Alopecia Research Foundation is a non-profit organization that provides support and resources for people with lichen planopilaris. |
|||
==Diagnosis== |
|||
== External links == |
|||
Lichen planus lesions are diagnosed clinically by their "lichen-like" appearance.<ref name=TG2009 /> A [[biopsy]] can be used to rule out conditions that may resemble lichen planus, and can pick up any secondary malignancies.<ref name="Kerawala 2010" /> |
|||
* [http://www.carfintl.org/faq.html Links to photo of Lichen planopilaris (Cicatricial Alopecia Research Foundation)] |
|||
* [http://www.lib.uiowa.edu/hardin/md/lichenplanus.html Links to pictures of Lichen planus (Hardin MD/Univ of Iowa)] |
|||
*[http://www.histopathology-india.net/LichenPlanus.htm Lichen planus-like cutaneous lesions] |
|||
*[http://www.dermnet.org.nz/scaly/lichen-planus.html Lichen planus] at DermNet NZ. |
|||
* Lichen Planus information, symptoms, variants, causes, diagnosis, and various treatment options. http://www.lichenplanus.com |
|||
[[Category:Dermatology]] |
|||
===Histopathology=== |
|||
[[fr:Lichen plan]] |
|||
[[File:lichen planus intermed mag.jpg|thumb|[[Micrograph]] of lichen planus. [[H&E stain]].]] |
|||
[[he:ילפת שטוחה]] |
|||
Lichen planus has a [[pathognomonic|unique]] microscopic appearance that is similar between cutaneous, mucosal and oral. A [[Periodic acid-Schiff stain]] of the biopsy may be used to visualise the specimen. [[Histology|Histological]] features seen include:<ref name=SCULLY1985 /> |
|||
[[ja:扁平苔癬]] |
|||
* thickening of the [[stratum corneum]] both with nuclei present ([[parakeratosis]]) and without ([[orthokeratosis]]). Parakeratosis is more common in oral variants of lichen planus. |
|||
[[nl:Lichen planus]] |
|||
* thickening of the [[stratum granulosum]] |
|||
[[pl:Liszaj płaski]] |
|||
* thickening of the [[stratum spinosum]] ([[acanthosis]]) with formation of colloid bodies (also known as Civatte bodies, Sabouraud bodies) that may stretch down to the lamina propria. |
|||
* liquefactive degeneration of the [[stratum basale]], with separation from the underlying [[lamina propria]], as a result of desmosome loss, creating small spaces (Max Joseph spaces). |
|||
* Infiltration of [[T cell]]s in a band-like pattern into the [[dermis]]<ref name="Thongprasom 2011" /> "hugging" the basal layer. |
|||
* Development of a "saw-tooth" appearance of the [[rete pegs]], which is much more common in non-oral forms of lichen planus. |
|||
===Differential diagnosis=== |
|||
The [[differential diagnosis]] for OLP includes: |
|||
* Other oral vesiculo-ulcerative conditions such as [[Pemphigus vulgaris]] and [[Benign mucous membrane pemphigoid]] |
|||
* [[Lupus erythematosus]], with lesions more commonly occur on the palate and appear as centrally ulcerated or erythematous with radiating white striae. In contrast, OLP and lichenoid reactions rarely occur on the palate, and the striae are randomly arranged rather than radial.<ref name="Odell 2010">{{cite book|last=Odell EW (Editor)|title=Clinical problem solving in dentistry|year=2010|publisher=Churchill Livingstone|location=Edinburgh|isbn=9780443067846|pages=159–162, 192|edition=3rd}}</ref> |
|||
* [[Chronic ulcerative stomatitis]] |
|||
* Frictional [[keratosis]] and [[Morsicatio buccarum]] (chronic [[cheek]] biting) |
|||
* Oral [[leukoplakia]] |
|||
* [[Oral candidiasis]] |
|||
==Treatment== |
|||
<!-- ONLY SOURCES WHICH MEET THE SOURCING POLICY FOR MEDICAL CONTENT ON WIKIPEDIA TO BE INCLUDED (SEE: http://en.wikipedia.org/wiki/MEDRS ), CONTENT BASED ON UNSUITABLE SOURCES WILL BE REMOVED --> |
|||
There is no cure for lichen planus,<ref name="Thongprasom 2011" /> and so treatment of cutaneous and oral lichen planus is for symptomatic relief or due to cosmetic concerns.<ref name="Thongprasom 2011" /><ref name=TG2009 /><ref name="Kerawala 2010" /> When medical treatment is pursued, first-line treatment typically involves [[corticosteroid]]s,<ref name=TG2009 /> and removal of any triggers.<ref name=ISSA2004 /> Without treatment, most lesions will spontaneously resolve within 6–9 months for cutaneous lesions,<ref name=TG2009 /> and longer for mucosal lesions <ref name=SCULLY1985>{{cite journal|last=Scully|first=C.|author2=El-Kom, M. |title=Lichen planus: review and update on pathogenesis|journal=Journal of Oral Pathology and Medicine|date=1 July 1985|volume=14|issue=6|pages=431–458|doi=10.1111/j.1600-0714.1985.tb00516.x}}</ref> |
|||
===Cutaneous lichen planus=== |
|||
Many different treatments have been reported for cutaneous lichen planus, however there is a general lack of evidence of efficacy for any treatment.<ref name=GOROUHI2009 /><ref name=CRIBIER1998 /> Treatments tend to be prolonged, partially effective and disappointing.<ref name=GOROUHI2009 /> First-line treatments may include [[retinoid]]s such as [[Acitretin]], or [[corticosteroids]] <ref name=TG2009 /><ref name=GOROUHI2009 /><ref name=CRIBIER1998>{{cite journal|last=Cribier|first=B|author2=Frances, C |author3=Chosidow, O |title=Treatment of lichen planus. An evidence-based medicine analysis of efficacy.|journal=Archives of dermatology|date=December 1998|volume=134|issue=12|pages=1521–30|pmid=9875189|doi=10.1001/archderm.134.12.1521}}</ref> |
|||
A variety of other therapies are also used if these are unsuccessful. These include oral corticosteroids, [[vitamin D3]] analogues, [[antibiotic]]s such as [[Dapsone]], [[hydroxychloroquine]] and [[Cyclosporin]], some [[anti-coagulant]]s,{{which|date=August 2013}} and [[psoralen]] plus ultraviolet-A.<ref name = TG2009 /><ref name=GOROUHI2009 /><ref name=CRIBIER1998 /> |
|||
Cosmetic treatments may include [[laser surgery]], [[cryotherapy]], and [[phototherapy]].<ref name=GOROUHI2009 /><ref name=CRIBIER1998 /> |
|||
===Oral lichen planus=== |
|||
Reassurance that the condition is benign, elimination of precipitating factors and improving [[oral hygiene]] are considered initial management for symptomatic OLP, and these measures are reported to be useful.<ref name="Thongprasom 2011" /> Treatment usually involves [[topical medication|topical]] [[corticosteroids]] (such as [[betamethasone]],<!-- <ref name="Thongprasom 2011" /> --> [[clobetasol]],<!-- <ref name="Thongprasom 2011" /> --> [[dexamethasone]],<!-- <ref name="Thongprasom 2011" /> --> and [[triamcinolone]]<!-- <ref name="Thongprasom 2011" /> -->) and [[analgesic]]s, or if these are ineffective and the condition is severe, the systemic corticosteroids may be used. [[Calcineurin inhibitor]]s (such as [[pimecrolimus]],<!-- <ref name="Thongprasom 2011" /> --> [[tacrolimus]]<!-- <ref name="Thongprasom 2011" /> -->) or [[cyclosporin]]<!-- <ref name="Thongprasom 2011" /> and [[retinoid]]s (such as [[tretinoin]]--><!-- <ref name="Thongprasom 2011" /> -->) are sometimes used.<ref name="Thongprasom 2011" /> |
|||
==Prognosis== |
|||
In contrast to cutaneous lichen planus, lichen planus lesions in the mouth may persist for many years,<ref name="Kerawala 2010" /> and tend to be difficult to treat, with relapses being common.<ref name="Nico 2011" /> Atrophic/erosive lichen planus is associated with a small risk of malignant transformation,<ref name="Kerawala 2010" /> and so people with OLP tend to be kept on long term review to detect any potential change early. Sometimes OLP can become secondarily infected with Candida organisms.{{citation needed|date=August 2013}} |
|||
==Epidemiology== |
|||
The overall [[prevalence]] of lichen planus in the general population is about 0.1 - 4%.<ref name="Usatine 2011" /> It generally occurs more commonly in females, in a ratio of 3:2, and most cases are diagnosed between the ages of 30 and 60, but it can occur at any age.<ref name="Usatine 2011" /><ref>{{cite journal |author=Yu TC, Kelly SC, Weinberg JM, Scheinfeld NS |title=Isolated lichen planus of the lower lip |journal=Cutis |volume=71 |issue=3 |pages=210–2 | date=March 2003 |pmid=12661749}}</ref> |
|||
Oral lichen planus is relatively common,<ref name="Nico 2011" /> It is one of the most common mucosal diseases. The prevalence in the general population is about 1.27-2.0%,<ref name="Thongprasom 2011" /><ref name="Kerawala 2010">{{cite book|editor=Kerawala C, Newlands C |title=Oral and maxillofacial surgery|year=2010|publisher=Oxford University Press|location=Oxford|isbn=978-0-19-920483-0|pages=412–413}}</ref> and it occurs more commonly middle aged people.<ref name="Thongprasom 2011">{{cite journal|last=Thongprasom|first=K|author2=Carrozzo, M |author3=Furness, S |author4= Lodi, G |title=Interventions for treating oral lichen planus.|journal=The Cochrane database of systematic reviews|date=Jul 6, 2011|issue=7|pages=CD001168|doi=10.1002/14651858.CD001168.pub2|pmid=21735381}}</ref> OLP in children is rare. About 50% of females with oral lichen planus were reported to have undiagnosed vulvar lichen planus.<ref name="Usatine 2011" /> |
|||
==History== |
|||
Lichen planus was first reported in 1869 by [[Erasmus Wilson]].<ref name=SCULLY1985 /> |
|||
==Notes== |
|||
{{notelist}} |
|||
==References== |
|||
{{Reflist|2}} |
|||
==External links== |
|||
{{commons category}} |
|||
* {{DMOZ|Health/Conditions_and_Diseases/Skin_Disorders/Lichen_Planus/}} |
|||
{{Diseases of the skin and appendages by morphology}} |
|||
{{Papulosquamous disorders}} |
|||
{{oral pathology}} |
|||
{{DEFAULTSORT:Lichen Planus}} |
|||
[[Category:Lichenoid eruptions]] |
|||
[[Category:Conditions of the mucous membranes]] |
|||
[[Category:Hepatitis C virus-associated diseases]] |
|||
[[Category:Autoimmune diseases]] |
|||
[[Category:Oral mucosal pathology]] |
|||
Revision as of 16:02, 1 September 2015
| Lichen planus | |
|---|---|
| Specialty | Dermatology |
Lichen planus (LP) is a disease of the skin and/or mucous membranes that resembles lichen. The cause is unknown, but it is thought to be the result of an autoimmune process with an unknown initial trigger. There is no cure, but many different medications and procedures have been used to control the symptoms.
The term lichenoid reaction (or lichenoid lesion) refers to a lesion of similar or identical histopathologic and clinical appearance to lichen planus (i.e. an area which looks the same as lichen planus, both to the naked eye and under a microscope).[1][2] Sometimes dental materials or certain medications can cause a lichenoid reaction.[1] They can also occur in association with graft versus host disease.[1][3]: 258
Classification
Lichen planus has been described as an autoimmune disease,[4] a dermatosis,[5] a papulosquamous disorder, a mucocutaneous disease,[6] and an inflammatory disease.[7]
Lichen planus lesions are so called because of their "lichen-like" appearance[8] and can be classified by the site they involve, or by their morphology.
Site
Lichen planus may be categorized as affecting mucosal or cutaneous surfaces.
- Cutaneous forms are those affecting the skin, scalp, and nails.[5][6][9]
- Mucosal forms are those affecting the lining of the gastrointestinal tract (mouth, pharynx, esophagus, stomach, anus), larynx, and other mucosal surfaces including the genitals, peritoneum, ears, nose, bladder and conjunctiva of the eyes.[7][10][11]
Pattern
Lichen planus lesions can occur in many different forms:
| Lesion morphology | Description[12][13] |
|---|---|
| Annular | 'Ring-shaped' lesions that develop gradually from single small pigmented spots into circular groups of papules with clear, unaffected skin in the center. Annular lesions occur in approximately ten percent of lichen planus cases. The ring-like lesions may very slowly enlarge, co-join and morph into larger irregular (serpentine) bands, sometimes accompanied by lines (See Linear, below). |
| Linear | Papules are arranged in a line (the "Blaschko line").[14] This pattern may develop secondary to trauma (koebnerization) or, uncommonly, as a spontaneous, isolated eruption, usually on the extremities, and rarely on the face.[15] |
| Hypertrophic | This pattern usually occurs on the extremities, especially the shins and the interphalangeal joints, and tends to be the most pruritic variant of lichen planus. Also known as "Lichen planus verrucosus". |
| Atrophic | This morphology is characterized by the presence of a few well-demarcated, white-bluish papules or plaques with central superficial atrophy. This is a rare variant of lichen planus. |
| Bullous | This morphology is characterized by the development of vesicles and bullae with the skin lesions. This is a rare variant of lichen planus, and also known as "Vesiculobullous lichen planus". |
| Ulcerative | This morphology is characterized by chronic, painful bullae and ulceration of the feet, often with cicatricial sequelae evident. This is a rare variant of lichen planus. |
| Pigmented | This morphology is characterized by hyperpigmented, dark-brown macules in sun-exposed areas and flexural folds. This is a rare variant of lichen planus. |
Overlap syndromes
Occasionally, lichen planus is known to occur with other conditions. For example:
- Lupus erythematosus overlap syndrome. Lesions of this syndrome share features of both lupus erythematosus and lichen planus. Lesions are usually large and hypopigmented, atrophic, and with a red-to-blue colour and minimal scaling. Telangectasia may be present.[13][16]
- Lichen sclerosus overlap syndrome, sharing features of lichen planus and lichen sclerosus.[17]
Signs and symptoms
Although lichen planus can present with a variety of lesions, the most common presentation is as a well-defined area of purple-coloured, itchy, flat-topped papules with interspersed lacy white lines (Wickham's striae). This description is known as the characteristic "6 Ps" of lichen planus: planar (flat-topped), purple, polygonal, pruritic, papules, and plaques.[9] This rash, after regressing, is likely to leave an area of hyperpigmentation that slowly fades. That said, a variety of other lesions can also occur.[8]
Cutaneous lichen planus


Variants of cutaneous lichen planus are distinguished based upon the appearance of the lesions and/or their distribution.[18] Lesions can affect the:
- Extremities (face, dorsal hands, arms, and nape of neck).[a] This is more common in Middle Eastern countries in spring and summer, where sunlight appears to have a precipitating effect.[15][19][20]
- Palms and soles
- Intertriginous areas of the skin. This is also known as "Inverse lichen planus".[15]
- Nails[21] characterized by irregular longitudinal grooving and ridging of the nail plate, thinning of the nail plate, pterygium formation, shedding of the nail plate with atrophy of the nail bed, subungual keratosis, longitudinal erthronychia (red streaks), and subungual hyperpigmentation.[22] A sand-papered appearance is present in around 10% of individuals with nail lichen planus.[21]
- Scalp. This is also known as lichen planopilaris, acuminatus, follicular lichen planus, and peripilaris,[23] characterised by violaceous, scaly, pruritic papules. Scalp lichen planus can cause scarring alopecia if it is untreated.[9][20][24]
- Hair. This variant causes inflammation of hair follicles and gradual replacement with scarring. About 10% of people with lichen planus have the scalp or nail variants of the condition.[9]
Other variants may include:
- Lichen planus pemphigoides characterized by the development of tense blisters atop lesions of lichen planus or the development vesicles de novo on uninvolved skin.[25]
- Keratosis lichenoides chronica (also known as "Nekam's disease") is a rare dermatosis characterized by violaceous papular and nodular lesions, often arranged in a linear or reticulate pattern on the dorsal hands and feet, extremities, and buttock, and some cases manifests by sorrheic dermatitis like eruption on the scalp and face, also palmo plantar keratosis has been reported.[15][26][27]
- Lichenoid keratoses (also known as "Benign lichenoid keratosis," and "Solitary lichen planus"[15]) is a cutaneous condition characterized by brown to red scaling maculopapules, found on sun-exposed skin of extremities.[15][28] Restated, this is a cutaneous condition usually characterized by a solitary dusky-red to violaceous papular skin lesion.[29]
- Lichenoid dermatitis represents a wide range of cutaneous disorders characterized by lichen planus-like skin lesions.[15][28]
Mucosal lichen planus

Lichen planus affecting mucosal surfaces may have one lesion or be multifocal.[30] Examples of lichen planus affecting mucosal surfaces include:[30]
- Esophageal lichen planus, affecting the esophageal mucosa. This can present with difficulty or pain when swallowing due to oesophageal inflammation, or as the development of an esophageal stricture. It has also been hypothesized that it is a precursor to squamous cell carcinoma of the esophagus.[10][31]
- Genital lichen planus, which may cause lesions on the glans penis or skin of the scrotom in males, and the vulva or vagina in females.[9] Symptoms may include lower urinary tract symptoms associated with stenosis of the urethra, painful sexual intercourse, and itching.[9] In females, Vulvovaginal-gingival syndrome, is severe and distinct variant affecting the vulva, vagina, and gums, with complications including scarring, vaginal stricture formation,[32] or vulva destruction.[33] The corresponding syndrome in males, affecting the glans penis and gums, is the peno-gingival syndrome.[15] It is associated with HLA-DQB1.[15][34]
Oral lichen planus
Oral lichen planus (also termed oral mucosal lichen planus),[35] is a form of mucosal lichen planus, where lichen planus involves the oral mucosa, the lining of the mouth. This may occur in combination with other variants of lichen planus.[36] Six clinical forms of oral lichen planus are recognized:[36]
- Reticular, the most common presentation of oral lichen planus,[4] is characterised by the net-like or spider web-like appearance of lacy white lines, oral variants of Wickham's straiae.[36] This is usually asymptomatic.[4]
- Erosive/ulcerative, the second most common form of oral lichen planus,[4] is characterised by oral ulcers presenting with persistent, irregular areas of redness, ulcerations and erosions covered with a yellow slough. This can occur in one or more areas of the mouth. In 25% of people with erosive oral lichen planus, the gums are involved, described as desquamative gingivitis (a condition not unique to lichen planus). This may be the initial or only sign of the condition.[36]
- Papular, with white papules.
- Plaque-like appearing as a white patch which may resemble leukoplakia.[36]
- Atrophic, appearing as areas. Atrophic oral lichen planus may also manifest as desquamative gingivitis.[36]
- Bullous, appearing as fluid-filled vesicles which project from the surface.
These types often coexist in the same individual. Oral lichen planus tends to present bilaterally as mostly white lesions on the inner cheek,[4] although any mucosal site in the mouth may be involved. Other sites, in decreasing order of frequency, may include the tongue, lips, gingivae, floor of the mouth, and very rarely, the palate.[4]
Generally, oral lichen planus tends not to cause any discomfort or pain, although some people may experience soreness when eating or drinking acidic or spicy foodstuffs or beverages.[36] When symptoms arise, they are most commonly associated with the atrophic and ulcerative subtypes. These symptoms can include a burning sensation to severe pain.[4]
Causes
The cause of lichen planus is unknown,[8][34][37] but it is not contagious and does not involve any known pathogen.[38] It is thought to be a T cell mediated autoimmune reaction (where the body's immune system targets its own tissues).[4] This autoimmune process triggers apoptosis of the epithelial cells.[4] Several cytokines are involved in lichen planus, including tumor necrosis factor alpha, interferon gamma, interleukin-1 alpha, interleukin 6, and interleukin 8.[4] This autoimmune, T cell mediated, process is thought to be in response to some antigenic change in the oral mucosa, but a specific antigen has not been identified.[4]
Where a causal or triggering agent is identified, this is termed a lichenoid reaction rather than lichen planus. These may include:[11]
- Drug reactions, with the most common inducers including gold salts, beta blockers, traditional antimalarials (e.g. quinine), thiazide diuretics, furosemide, spironolactone, Metformin and penicillamine.[38]
- Reactions to amalgam (metal alloys) fillings (or when they are removed/replaced),[39]
- Graft-versus-host disease lesions, which chronic lichenoid lesions seen on the palms, soles, face and upper trunk after several months.[38]
- Hepatitis, specifically hepatitis B and hepatitis C infection, and primary biliary cirrhosis.[17][38]
It has been suggested that lichen planus may respond to stress, where lesions may present during times of stress. Lichen planus can be part of Grinspan's syndrome.[citation needed]
It has also been suggested that mercury exposure may contribute to lichen planus.[40]
Diagnosis
Lichen planus lesions are diagnosed clinically by their "lichen-like" appearance.[8] A biopsy can be used to rule out conditions that may resemble lichen planus, and can pick up any secondary malignancies.[41]
Histopathology

Lichen planus has a unique microscopic appearance that is similar between cutaneous, mucosal and oral. A Periodic acid-Schiff stain of the biopsy may be used to visualise the specimen. Histological features seen include:[42]
- thickening of the stratum corneum both with nuclei present (parakeratosis) and without (orthokeratosis). Parakeratosis is more common in oral variants of lichen planus.
- thickening of the stratum granulosum
- thickening of the stratum spinosum (acanthosis) with formation of colloid bodies (also known as Civatte bodies, Sabouraud bodies) that may stretch down to the lamina propria.
- liquefactive degeneration of the stratum basale, with separation from the underlying lamina propria, as a result of desmosome loss, creating small spaces (Max Joseph spaces).
- Infiltration of T cells in a band-like pattern into the dermis[4] "hugging" the basal layer.
- Development of a "saw-tooth" appearance of the rete pegs, which is much more common in non-oral forms of lichen planus.
Differential diagnosis
The differential diagnosis for OLP includes:
- Other oral vesiculo-ulcerative conditions such as Pemphigus vulgaris and Benign mucous membrane pemphigoid
- Lupus erythematosus, with lesions more commonly occur on the palate and appear as centrally ulcerated or erythematous with radiating white striae. In contrast, OLP and lichenoid reactions rarely occur on the palate, and the striae are randomly arranged rather than radial.[43]
- Chronic ulcerative stomatitis
- Frictional keratosis and Morsicatio buccarum (chronic cheek biting)
- Oral leukoplakia
- Oral candidiasis
Treatment
There is no cure for lichen planus,[4] and so treatment of cutaneous and oral lichen planus is for symptomatic relief or due to cosmetic concerns.[4][8][41] When medical treatment is pursued, first-line treatment typically involves corticosteroids,[8] and removal of any triggers.[39] Without treatment, most lesions will spontaneously resolve within 6–9 months for cutaneous lesions,[8] and longer for mucosal lesions [42]
Cutaneous lichen planus
Many different treatments have been reported for cutaneous lichen planus, however there is a general lack of evidence of efficacy for any treatment.[14][44] Treatments tend to be prolonged, partially effective and disappointing.[14] First-line treatments may include retinoids such as Acitretin, or corticosteroids [8][14][44]
A variety of other therapies are also used if these are unsuccessful. These include oral corticosteroids, vitamin D3 analogues, antibiotics such as Dapsone, hydroxychloroquine and Cyclosporin, some anti-coagulants,[which?] and psoralen plus ultraviolet-A.[8][14][44]
Cosmetic treatments may include laser surgery, cryotherapy, and phototherapy.[14][44]
Oral lichen planus
Reassurance that the condition is benign, elimination of precipitating factors and improving oral hygiene are considered initial management for symptomatic OLP, and these measures are reported to be useful.[4] Treatment usually involves topical corticosteroids (such as betamethasone, clobetasol, dexamethasone, and triamcinolone) and analgesics, or if these are ineffective and the condition is severe, the systemic corticosteroids may be used. Calcineurin inhibitors (such as pimecrolimus, tacrolimus) or cyclosporin) are sometimes used.[4]
Prognosis
In contrast to cutaneous lichen planus, lichen planus lesions in the mouth may persist for many years,[41] and tend to be difficult to treat, with relapses being common.[34] Atrophic/erosive lichen planus is associated with a small risk of malignant transformation,[41] and so people with OLP tend to be kept on long term review to detect any potential change early. Sometimes OLP can become secondarily infected with Candida organisms.[citation needed]
Epidemiology
The overall prevalence of lichen planus in the general population is about 0.1 - 4%.[9] It generally occurs more commonly in females, in a ratio of 3:2, and most cases are diagnosed between the ages of 30 and 60, but it can occur at any age.[9][45]
Oral lichen planus is relatively common,[34] It is one of the most common mucosal diseases. The prevalence in the general population is about 1.27-2.0%,[4][41] and it occurs more commonly middle aged people.[4] OLP in children is rare. About 50% of females with oral lichen planus were reported to have undiagnosed vulvar lichen planus.[9]
History
Lichen planus was first reported in 1869 by Erasmus Wilson.[42]
Notes
- ^ Cutaneous lichen planus affecting the extremities is also known as "Lichen planus actinicus", "Actinic lichen niditus," "Lichen planus atrophicus annularis," "Lichen planus subtropicus," "Lichen planus tropicus," "Lichenoid melanodermatitis," and "Summertime actinic lichenoid eruption"
References
- ^ a b c Greenberg MS, Glick M, Ship JA (2008). Burket's oral medicine (11th ed.). Hamilton, Ont.: BC Decker. pp. 89–97. ISBN 9781550093452.
{{cite book}}: CS1 maint: multiple names: authors list (link) - ^ Lewis MAO, Jordan RCK (2012). Oral medicine (2nd ed.). London: Manson Publishing. pp. 66–72. ISBN 9781840761818.
- ^ Barnes L (editor) (2009). Surgical pathology of the head and neck (3rd ed.). New York: Informa healthcare. ISBN 9781420091632.
{{cite book}}:|last=has generic name (help) - ^ a b c d e f g h i j k l m n o p q r Thongprasom, K; Carrozzo, M; Furness, S; Lodi, G (Jul 6, 2011). "Interventions for treating oral lichen planus". The Cochrane database of systematic reviews (7): CD001168. doi:10.1002/14651858.CD001168.pub2. PMID 21735381.
- ^ a b Asch, S; Goldenberg, G (March 2011). "Systemic treatment of cutaneous lichen planus: an update". Cutis; cutaneous medicine for the practitioner. 87 (3): 129–34. PMID 21488570.
- ^ a b Sharma, A; Białynicki-Birula, R; Schwartz, RA; Janniger, CK (July 2012). "Lichen planus: an update and review". Cutis; cutaneous medicine for the practitioner. 90 (1): 17–23. PMID 22908728.
- ^ a b Cheng, S; Kirtschig, G; Cooper, S; Thornhill, M; Leonardi-Bee, J; Murphy, R (Feb 15, 2012). "Interventions for erosive lichen planus affecting mucosal sites". The Cochrane database of systematic reviews. 2: CD008092. doi:10.1002/14651858.CD008092.pub2. PMID 22336835.
- ^ a b c d e f g h i Limited, Therapeutic Guidelines (2009). Therapeutic guidelines (Version 3. ed.). North Melbourne, Vic.: Therapeutic Guidelines. pp. 254–255, 302. ISBN 978-0-9804764-3-9.
- ^ a b c d e f g h i Usatine, RP; Tinitigan, M (Jul 1, 2011). "Diagnosis and treatment of lichen planus". American family physician. 84 (1): 53–60. PMID 21766756.
- ^ a b Yamada T, Alpers DH; et al. (2009). Textbook of gastroenterology (5th ed.). Chichester, West Sussex: Blackwell Pub. p. 3304. ISBN 978-1-4051-6911-0.
- ^ a b Treister NS, Bruch JM (2010). Clinical oral medicine and pathology. New York: Humana Press. pp. 59–62. ISBN 978-1-60327-519-4.
- ^ Freedberg, Irwin M., ed. (2003). Fitzpatrick's dermatology in general medicine (6th ed.). New York, NY: McGraw-Hill. pp. 465–8. ISBN 0-07-138076-0.
- ^ a b James, William D.; Elston, Dirk M.; Berger, Timothy G. Andrews' Diseases of the skin : clinical dermatology (11th ed.). London: Saunders/ Elsevier. pp. 219–24. ISBN 1-4377-0314-3.
- ^ a b c d e f Gorouhi, F; Firooz A; Khatami A; Ladoyanni E; Bouzari N; Kamangar F; Gill JK (2009). "Interventions for cutaneous lichen planus". Cochrane Database of Systematic Reviews (4). doi:10.1002/14651858.CD008038.
- ^ a b c d e f g h i Bolognia, Jean L.; Jorizzo, Joseph L.; Rapini, Ronald P., eds. (2008). Dermatology (2nd ed.). St. Louis: Mosby/Elsevier. ISBN 1-4160-2999-0.
- ^ Freedberg, Irwin M., ed. (2003). Fitzpatrick's dermatology in general medicine (6th ed.). New York, NY: McGraw-Hill. pp. 366, 470–1. ISBN 0-07-138076-0.
- ^ a b James, William D.; Elston, Dirk M.; Berger, Timothy G. Andrews' Diseases of the skin : clinical dermatology (11th ed.). London: Saunders/ Elsevier. p. 220. ISBN 1-4377-0314-3.
- ^ Freedberg, Irwin M., ed. (2003). Fitzpatrick's dermatology in general medicine (6th ed.). New York, NY: McGraw-Hill. p. 466. ISBN 0-07-138076-0.
- ^ Freedberg, Irwin M., ed. (2003). Fitzpatrick's dermatology in general medicine (6th ed.). New York, NY: McGraw-Hill. p. 468. ISBN 0-07-138076-0.
- ^ a b James, William D.; Elston, Dirk M.; Berger, Timothy G. Andrews' Diseases of the skin : clinical dermatology (11th ed.). London: Saunders/ Elsevier. p. 223. ISBN 1-4377-0314-3.
- ^ a b Gordon, KA; Vega, JM; Tosti, A (Nov–Dec 2011). "Trachyonychia: a comprehensive review". Indian journal of dermatology, venereology and leprology. 77 (6): 640–5. doi:10.4103/0378-6323.86470. PMID 22016269.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ James, William D.; Elston, Dirk M.; Berger, Timothy G. Andrews' Diseases of the skin : clinical dermatology (11th ed.). London: Saunders/ Elsevier. p. 781. ISBN 1-4377-0314-3.
- ^ Freedberg, Irwin M., ed. (2003). Fitzpatrick's dermatology in general medicine (6th ed.). New York, NY: McGraw-Hill. p. 467. ISBN 0-07-138076-0.
- ^ Cevasco NC, Bergfeld WF, Remzi BK, de Knott HR (2007). "A case-series of 29 patients with lichen planopilaris: the Cleveland Clinic Foundation experience on evaluation, diagnosis, and treatment". J. Am. Acad. Dermatol. 57 (1): 47–53. doi:10.1016/j.jaad.2007.01.011. PMID 17467854.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Freedberg, Irwin M., ed. (2003). Fitzpatrick's dermatology in general medicine (6th ed.). New York, NY: McGraw-Hill. p. 471. ISBN 0-07-138076-0.
- ^ Freedberg, Irwin M., ed. (2003). Fitzpatrick's dermatology in general medicine (6th ed.). New York, NY: McGraw-Hill. p. 472. ISBN 0-07-138076-0.
- ^ James, William D.; Elston, Dirk M.; Berger, Timothy G. Andrews' Diseases of the skin : clinical dermatology (11th ed.). London: Saunders/ Elsevier. p. 224. ISBN 1-4377-0314-3.
- ^ a b Freedberg, Irwin M., ed. (2003). Fitzpatrick's dermatology in general medicine (6th ed.). New York, NY: McGraw-Hill. p. 473. ISBN 0-07-138076-0.
- ^ James, William D.; Elston, Dirk M.; Berger, Timothy G. Andrews' Diseases of the skin : clinical dermatology (11th ed.). London: Saunders/ Elsevier. p. 639. ISBN 1-4377-0314-3.
- ^ a b Ebrahimi, M; Lundqvist, L; Wahlin, YB; Nylander, E (October 2012). "Mucosal lichen planus, a systemic disease requiring multidisciplinary care: a cross-sectional clinical review from a multidisciplinary perspective". Journal of lower genital tract disease. 16 (4): 377–80. doi:10.1097/LGT.0b013e318247a907. PMID 22622344.
- ^ Chandan, VS; Murray, JA; Abraham, SC (June 2008). "Esophageal lichen planus". Archives of pathology & laboratory medicine. 132 (6): 1026–9. doi:10.1043/1543-2165(2008)132[1026:ELP]2.0.CO;2. PMID 18517264.
- ^ Panagiotopoulou, N; Wong, CS; Winter-Roach, B (April 2010). "Vulvovaginal-gingival syndrome". Journal of obstetrics and gynaecology : the journal of the Institute of Obstetrics and Gynaecology. 30 (3): 226–30. doi:10.3109/01443610903477572. PMID 20373919.
- ^ Schlosser, BJ (May–Jun 2010). "Lichen planus and lichenoid reactions of the oral mucosa". Dermatologic therapy. 23 (3): 251–67. doi:10.1111/j.1529-8019.2010.01322.x. PMID 20597944.
- ^ a b c d Nico, MM; Fernandes, JD; Lourenço, SV (Jul–Aug 2011). "Oral lichen planus". Anais brasileiros de dermatologia. 86 (4): 633–41, quiz 642–3. PMID 21987126.
- ^ Alam, F; Hamburger, J (May 2001). "Oral mucosal lichen planus in children". International journal of paediatric dentistry / the British Paedodontic Society [and] the International Association of Dentistry for Children. 11 (3): 209–14. PMID 11484471.
- ^ a b c d e f g Scully C (2008). Oral and maxillofacial medicine : the basis of diagnosis and treatment (3rd ed.). Edinburgh: Churchill Livingstone. pp. 192–199. ISBN 9780702049484.
- ^ Roopashree, MR; Gondhalekar, RV; Shashikanth, MC; George, J; Thippeswamy, SH; Shukla, A (November 2010). "Pathogenesis of oral lichen planus--a review". Journal of oral pathology & medicine : official publication of the International Association of Oral Pathologists and the American Academy of Oral Pathology. 39 (10): 729–34. doi:10.1111/j.1600-0714.2010.00946.x. PMID 20923445.
- ^ a b c d Davidson's principles and practice of medicine (21st ed.). Edinburgh: Churchill Livingstone/Elsevier. 2010. pp. 1265–1266. ISBN 978-0-7020-3085-7.
{{cite book}}:|first=has generic name (help);|first=missing|last=(help)CS1 maint: multiple names: authors list (link) - ^ a b Issa, Y; Brunton, PA; Glenny, AM; Duxbury, AJ (November 2004). "Healing of oral lichenoid lesions after replacing amalgam restorations: a systematic review". Oral surgery, oral medicine, oral pathology, oral radiology, and endodontics. 98 (5): 553–65. doi:10.1016/j.tripleo.2003.12.027. PMID 15529127.
- ^ Dunsche A, Frank MP, Lüttges J, et al. (April 2003). "Lichenoid reactions of murine mucosa associated with amalgam". The British Journal of Dermatology. 148 (4): 741–8. doi:10.1046/j.1365-2133.2003.05229.x. PMID 12752133.
- ^ a b c d e Kerawala C, Newlands C, ed. (2010). Oral and maxillofacial surgery. Oxford: Oxford University Press. pp. 412–413. ISBN 978-0-19-920483-0.
- ^ a b c Scully, C.; El-Kom, M. (1 July 1985). "Lichen planus: review and update on pathogenesis". Journal of Oral Pathology and Medicine. 14 (6): 431–458. doi:10.1111/j.1600-0714.1985.tb00516.x.
- ^ Odell EW (Editor) (2010). Clinical problem solving in dentistry (3rd ed.). Edinburgh: Churchill Livingstone. pp. 159–162, 192. ISBN 9780443067846.
{{cite book}}:|last=has generic name (help) - ^ a b c d Cribier, B; Frances, C; Chosidow, O (December 1998). "Treatment of lichen planus. An evidence-based medicine analysis of efficacy". Archives of dermatology. 134 (12): 1521–30. doi:10.1001/archderm.134.12.1521. PMID 9875189.
- ^ Yu TC, Kelly SC, Weinberg JM, Scheinfeld NS (March 2003). "Isolated lichen planus of the lower lip". Cutis. 71 (3): 210–2. PMID 12661749.
{{cite journal}}: CS1 maint: multiple names: authors list (link)
