Influenza vaccine
| Influenza (flu) |
|---|
 |
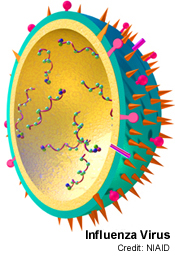
The influenza vaccine is an annual vaccine to protect against the highly variable influenza virus[1]. Each injected seasonal influenza vaccine contains three influenza viruses: one A (H3N2) virus, one regular seasonal A (H1N1) virus (not the 2009 pandemic H1N1 virus), and one B virus.[2]
Purpose and benefits of annual flu vaccination
"Influenza vaccination is the most effective method for preventing influenza virus infection and its potentially severe complications."[3][4][5]
An influenza epidemic emerges during each winter's flu season. Each year there are two flu seasons due to the occurrence of influenza at different times in the Northern and Southern Hemispheres. It is frequently estimated that 36,000 people die each year from influenza and accompanying opportunistic infections and complications in the United States alone.[6] Worldwide, seasonal influenza kills an estimated 250,000 to 500,000 people each year. The majority of deaths in the industrialized world occur in adults age of 65 and over.[7] A review at the NIAID division of the NIH in 2008 concluded that "Seasonal influenza causes more than 200,000 hospitalizations and 41,000 deaths in the U.S. every year, and is the seventh leading cause of death in the U.S."[8] The economic costsin the U.S. have been estimated at over $80 billion.
The number of annual influenza-related hospitalizations is many times the number of deaths.[9] "The high costs of hospitalizing young children for influenza creates a significant economic burden in the United States, underscoring the importance of preventive flu shots for children and the people with whom they have regular contact..."[10]
In Canada, the National Advisory Committee on Immunization, the group that advises the Public Health Agency of Canada, currently recommends that everyone aged 2 to 64 years be encouraged to receive annual influenza vaccination, and that children between the age of six and 24 months, and their household contacts, should be considered a high priority for the flu vaccine.[11]
In the United States, the CDC recommends to clinicians that
- In general, anyone who wants to reduce their chances of getting influenza can get vaccinated. Vaccination is especially important for people at higher risk of serious influenza complications or people who live with or care for people at higher risk for serious complications.[12]
Vaccination against influenza is recommended for most members of high-risk groups who would be likely to suffer complications from influenza. Specific recommendations include all children and teenagers, from six months to 18 years of age;[11] [13]
- In expanding the new upper age limit to 18 years, the aim is to reduce both the time children and parents lose from visits to pediatricians and missing school and the need for antibiotics for complications ...
- An added expected benefit would be indirect — to reduce the number of influenza cases among parents and other household members, and possibly spread to the general community.[14]
In the event of exposure to a pandemic influenza virus, seasonal flu vaccine may also offer some protection against both the H5N1-type (avian influenza)H5N1 infection[15][16][17] and the 2009 flu pandemic (the H1N1 "swine flu.")[18][19][20][21][22]
History of the flu vaccine
Vaccines are used in both humans and nonhumans. Human vaccine is meant unless specifically identified as a veterinary, poultry or livestock vaccine.
Influenza
The first influenza pandemic was recorded in 1580; since this time, various methods have been employed to eradicate its cause.[23] The etiological cause of influenza, the orthomyxoviridae was finally discovered by the Medical Research Council (MRC) of the United Kingdom in 1933.[24]
Known flu pandemics:[25]
- 1889–90 — Asiatic (Russian) Flu, mortality rate said to be 0.75–1 death per 1000 possibly H2N2
- 1900 — Possibly H3N8
- 1918–20 – Spanish Flu, 500 million ill, at least 20–40 million died of H1N1
- 1957–58 – Asian Flu, 1 to 1.5 million died of H2N2
- 1968–69 – Hong Kong Flu, 3/4 to 1 million died of H3N2
- 2009 - Swine Flu, caused by H1N1
Flu vaccine origins and development
In the world wide Spanish flu pandemic of 1918, "Physicians tried everything they knew, everything they had ever heard of, from the ancient art of bleeding patients, to administering oxygen, to developing new vaccines and sera (chiefly against what we now call Hemophilus influenzae—a name derived from the fact that it was originally considered the etiological agent—and several types of pneumococci). Only one therapeutic measure, transfusing blood from recovered patients to new victims, showed any hint of success."[26]
In 1931, viral growth in embryonated hens' eggs was discovered, and in the 1940s, the US military developed the first approved inactivated vaccines for influenza, which were used in the Second World War. Greater advances were made in vaccinology and immunology, and vaccines became safer and mass-produced. Today, thanks to the advances of molecular technology, we are on the verge of making influenza vaccines through the genetic manipulation of influenza genes.[27]
Flu vaccine acceptance
According to the CDC: "Influenza vaccination is the primary method for preventing influenza and its severe complications. [...] Vaccination is associated with reductions in influenza-related respiratory illness and physician visits among all age groups, hospitalization and death among persons at high risk, otitis media among children, and work absenteeism among adults. Although influenza vaccination levels increased substantially during the 1990s, further improvements in vaccine coverage levels are needed".[28]
The current egg-based technology for producing influenza vaccine was created in the 1950s.[29] In the U.S. swine flu scare of 1976, President Gerald Ford was confronted with a potential swine flu pandemic. The vaccination program was rushed, yet plagued by delays and public relations problems. Meanwhile, maximum military containment efforts succeeded unexpectedly in confining the new strain to the single army base where it had originated. On that base a number of soldiers fell severely ill, but only one died. The program was canceled, after about 24% of the population had received vaccinations. An excess in deaths of twenty-five over normal annual levels as well as 400 excess hospitalizations, both from Guillain-Barré syndrome, were estimated to have occurred from the vaccination program itself, illustrating that vaccine itself is not free of risks. The result has been cited to stoke lingering doubts about vaccination[30].
Current status
Influenza research includes molecular virology, molecular evolution, pathogenesis, host immune responses, genomics, and epidemiology. These help in developing influenza countermeasures such as vaccines, therapies and diagnostic tools. Improved influenza countermeasures require basic research on how viruses enter cells, replicate, mutate, evolve into new strains and induce an immune response. The Influenza Genome Sequencing Project is creating a library of influenza sequences[citation needed] that will help us understand what makes one strain more lethal than another, what genetic determinants most affect immunogenicity, and how the virus evolves over time. Solutions to limitations in current vaccine methods are being researched.
The rapid development, production, and distribution of pandemic influenza vaccines could potentially save millions of lives during an influenza pandemic. Due to the short time frame between identification of a pandemic strain and need for vaccination, researchers are looking at novel technologies for vaccine production that could provide better "real-time" access and be produced more affordably, thereby increasing access for people living in low- and moderate-income countries, where an influenza pandemic may likely originate, such as live attenuated (egg-based or cell-based) technology and recombinant technologies (proteins and virus-like particles).[31] As of July 2009, more than 70 known clinical trials have been completed or are ongoing for pandemic influenza vaccines.[32] In September 2009, the US Food and Drug Administration approved four vaccines against the 2009 H1N1 influenza virus (the current pandemic strain), and expected the initial vaccine lots to be available within the following month.[33]
Clinical trials of vaccines
A vaccine is assessed by the reduction of the risk of disease that is produced by vaccination, the vaccine's efficacy. In contrast, in the field, the effectiveness of a vaccine is the practical reduction in risk for an individual when they are vaccinated under real-world conditions.[34] Measuring efficacy of influenza vaccines is relatively simple, as the immune response produced by the vaccine can be assessed in animal models, or the amount of antibody produced in vaccinated people can be measured,[35] or most rigorously, by immunising adult volunteers and then challenging with virulent influenza virus.[36] In studies such as these, influenza vaccines showed high efficacy and produced a protective immune response. For ethical reasons, such challenge studies cannot be performed in the population most at risk from influenza – the elderly and young children. However, studies on the effectiveness of flu vaccines in the real world are uniquely difficult. The vaccine may not be matched to the viruses in circulation that year; virus prevalence varies widely between years, and influenza is often confused with other influenza-like illnesses.[37]
Nevertheless, multiple clinical trials of both live and inactivated influenza vaccines against seasonal influenza have been performed and their results pooled and analyzed in several recent meta-analyses. Studies on live vaccines have very limited data, but these preparations may be more effective than inactivated vaccines.[36] The meta-analyses examined the efficacy and effectiveness of inactivated vaccines against seasonal influenza in adults,[38] children,[39] and the elderly.[40][41] In adults, vaccines show high efficacy against the targeted strains, but low effectiveness overall, so the benefits of vaccination are small, with a one-quarter reduction in risk of contracting influenza but no significant effect on the rate of hospitalization.[38] However, the risk of serious complications from influenza is small in adults, so unless the effect from vaccination is large it might not have been detected. In children, vaccines again showed high efficacy, but low effectiveness in preventing "flu-like illness", in children under two the data are extremely limited, but vaccination appeared to confer no measurable benefit.[39] In the elderly, vaccination does not reduce the frequency of influenza, but seems to reduce pneumonia, hospital admission and deaths from influenza or pneumonia.[40][41] However, the current data on the effectiveness of influenza vaccines in the elderly may be unreliable, due to high levels of selection bias.[42]
Overall, the benefit of influenza vaccination is clear in the elderly and vaccination of children may be beneficial. Routine vaccination of adults is not predicted to produce significant improvements in public health. The apparent contradiction between vaccines with high efficacy, but low effectiveness, may reflect the difficulty in diagnosing influenza under clinical conditions and the large number of strains circulating in the population.[37] In contrast, during an influenza pandemic, where a single strain of virus is responsible for illnesses, an effective vaccine could produce a large decrease in the number of cases and be highly effective in controlling an epidemic.[43] However, such a vaccine would have to be produced and distributed rapidly to have maximum effect.[44]
Effectiveness of vaccine
The CDC reports that studies demonstrate that vaccination can be a cost-effective counter-measure to seasonal outbreaks of influenza;[45] but not perfect. A study led by Dr. David K. Shay in February, 2008 reported that
- "full immunization against flu provided about a 75 percent effectiveness rate in preventing hospitalizations from influenza complications in the 2005-6 and 2006-7 influenza seasons."[46]
Modern influenza vaccines have been criticized for a lack of effectiveness demonstrated in controlled studies. A 2006 Cochrane review of influenza vaccination in the elderly stated "The apparent high effectiveness of the vaccines in preventing death from all causes may reflect a baseline imbalance in health status and other systematic differences in the two groups of participants[47]. A study on selection bias for influenza vaccine in the elderly found that it could account for the entirety of the protective effect.[48] A 2008 Cochrane review of healthy children found "Influenza vaccines are efficacious in children older than two but little evidence is available for children under two." [49]. The CDC recommends every child over 6 months be given the influenza vaccine.[50] A 2007 Cochrane review on influenza vaccines in healthy adults found that while vaccines were effective against the influenza strains they are designed to vaccinate against, this ended up translating to only a modest impact on working days lost due to influenza-like infections.[51]
The group most vulnerable to flu, the elderly, is also the least affected by the vaccine, with an average efficacy rate ranging from 40-50% at age 65, and 15-30% past age 70.[52][53][54] There are multiple reasons behind this steep decline in vaccine efficacy, the most common of which are the declining immunological function and frailty associated with advanced age.[55]
In the United States a person aged 50–64 is nearly ten times more likely to die an influenza-associated death than a younger person, and a person over age 65 is over ten times more likely to die an influenza-associated death than the 50–64 age group.[56] Vaccination of those over age 65 reduces influenza-associated death by about 50%.[57][58] However, it is unlikely that the vaccine completely explains the results since elderly people who get vaccinated are probably more healthy and health-conscious than those who do not.[59][60][61] Elderly participants randomized to a high-dose group (60 micrograms) had antibody levels 44 to 79 percent higher than did those who received the normal dose of vaccine. Elderly volunteers receiving the higher dose were more likely to achieve protective levels of antibody.[62]
As mortality is also high among infants who contract influenza, the household contacts and caregivers of infants should be vaccinated to reduce the risk of passing an influenza infection to the infant.[63] Data from the years when Japan required annual flu vaccinations for school-aged children indicate that vaccinating children—the group most likely to catch and spread the disease—has a strikingly positive effect on reducing mortality among older people: one life saved for every 420 children who received the flu vaccine.[64] This may be due to herd immunity or to direct causes, such as individual older people not being exposed to influenza. For example, retired grandparents often risk infection by caring for their sick grandchildren in households where the parents can't take time off work or are sick themselves.
In most years (16 of the 19 years before 2007), the flu vaccine strains have been a good match for the circulating strains.[65] In other flu seasons like that of 2007/2008, the match was less useful. But even a mis-matched vaccine can often provide some protection:
- ...[A]ntibodies made in response to vaccination with one strain of influenza viruses can provide protection against different, but related strains. A less than ideal match may result in reduced vaccine effectiveness against the variant viruses, but it still can provide enough protection to prevent or lessen illness severity and prevent flu-related complications. In addition, it’s important to remember that the influenza vaccine contains three virus strains so the vaccine can also protect against the other two viruses. For these reasons, even during seasons when there is a less than ideal match, CDC continues to recommend influenza vaccination. This is particularly important for people at high risk for serious flu complications and their close contacts.[66]
Comparing flu shot to nasal spray
Flu vaccines are available either as
- TIV (flu shot (injection) of trivalent (three strains; usually A/H1N1, A/H3N2, and B) inactivated (killed) vaccine) or
- LAIV (nasal spray (mist) of live attenuated influenza vaccine.)
TIV works by putting into the bloodstream those parts of three strains of flu virus that the body uses to create antibodies; while LAIV works by inoculating against those same three strains that have been genetically modified to minimize symptoms of illness.
LAIV is not recommended for individuals under age 2 or over age 50,[67] but might be comparatively more effective among children over age 2.[68]
A military study on military personnel showed that flu shots yielded less illness than nasal spray. Based on one of the largest head-to-head studies comparing LAIV and TIV (which was conducted by the U.S. Armed Forces Surveillance Center on military personnel who were stationed in the United States during three flu seasons from 2004 through 2007), investigators concluded that: "It may be prudent to use TIV in patients who were vaccinated at least once in the past 2 years [...] but LAIV against pandemic strains may be be more protective than inactivated vaccines, because the population will probably lack preexisting immunity."[69]
Vaccination recommendations

Various public health organizations, including the World Health Organization, have recommended that yearly influenza vaccination be routinely offered to patients at risk of complications of influenza and those individuals who live with or care for high-risk individuals, including:
- the elderly (UK recommendation is those aged 65 or above)
- patients with chronic lung diseases (asthma, COPD, etc.)
- patients with chronic heart diseases (congenital heart disease, chronic heart failure, ischaemic heart disease)
- patients with chronic liver diseases (including cirrhosis)
- patients with chronic renal diseases (such as the nephrotic syndrome)
- patients who are immunosuppressed (those with HIV or who are receiving drugs to suppress the immune system such as chemotherapy and long-term steroids) and their household contacts
- people who live together in large numbers in an environment where influenza can spread rapidly, such as prisons, nursing homes, schools, and dormitories
- healthcare workers (both to prevent sickness and to prevent spread to patients)[70]
- pregnant women[71][72]
- children from ages six months to two years
- individuals with no health insurance or on Medicaid
Both types of flu vaccines are contraindicated for those with severe allergies to egg proteins and people with a history of Guillain-Barré syndrome.[73]
Side effects
Side effects of the inactivated/dead flu vaccine injection include:
- mild soreness, redness, and swelling where the shot was given
- fever
- aches
These problems usually begin soon after the injection, and last 1–2 days.[74]
Side effects of the activated/live/LAIV flu nasal spray vaccine:
Some children and adolescents 2–17 years of age have reported:[75]
- runny nose, nasal congestion or cough
- fever
- headache and muscle aches
- wheezing
- abdominal pain or occasional vomiting or diarrhea
Some adults 18–49 years of age have reported:[75]
- runny nose or nasal congestion
- sore throat
- cough, chills, tiredness/weakness
- headache
More severe, but very rare side effects include:[75]
- life-threatening allergic reaction
A review has concluded that the 2009 H1N1 ("swine flu") vaccine has a safety profile similar to that of seasonal vaccine.[76]
Some injection-based flu vaccines intended for adults in the United States contain thiomersal. Despite some controversy in the media,[77] the World Health Organization has concluded that there is no evidence of toxicity from thiomersal in vaccines and no reason on grounds of safety to change to more-expensive single-dose administration.[78]
Flu vaccine manufacturing
Flu vaccine is usually grown in fertilized chicken eggs.
As of November 2007, both the conventional injection and the nasal spray are manufactured using chicken eggs. The European Union has also approved Optaflu, a vaccine produced by Novartis using vats of animal cells. This technique is expected to be more scalable and avoid problems with eggs, such as allergic reactions and incompatibility with strains that affect avians like chickens. A DNA-based vaccination, which is hoped to be even faster to manufacture, is currently in clinical trials, but has not yet been proven safe and effective. Research continues into the idea of a "universal" influenza vaccine (but no vaccine candidates have been announced) which would not need to be tailored to work on particular strains, but would be effective against a broad variety of influenza viruses.[79]
In a 2007 report, the current global capacity of approximately 826 million seasonal influenza vaccine doses (inactivated and live) was double the current production of 413 million doses. In an aggressive scenario of producing pandemic influenza vaccines by 2013, only 2.8 billion courses could be produced in a six-month time frame. If all high- and upper-middle-income countries sought vaccines for their entire populations in a pandemic, nearly 2 billion courses would be required. If China pursued this goal as well, more than 3 billion courses would be required to serve these populations.[80] Vaccine research and development is ongoing to identify novel vaccine approaches that could produce much greater quantities of vaccine at a price that is affordable to the global population.
An effective method of vaccine generation that bypasses the need for eggs is the construction of "influenza virus-like particle (VLP)". VLP is a non-egg, non-mammalian cell culture-based vaccine, purified from the supernatants of Spodoptera frugiperda Sf9 insect cells following infection of baculovirus vectors encoding an expression cassette comprised of only three influenza virus structural proteins, hemagglutinin (HA), neuraminidase (NA), and matrix (M1)[81] VLPs elicit antibodies that recognize a broader panel of antigenically distinct viral isolates compared to other vaccines in the hemagglutination-inhibition (HAI) assay.
H5N1
 |
Vaccines have been formulated against several of the avian H5N1 influenza varieties. Vaccination of poultry against the ongoing H5N1 epizootic is widespread in certain countries. Some vaccines also exist for use in humans, and others are in testing, but none have been made available to civilian populations, nor produced in quantities sufficient to protect more than a tiny fraction of the Earth's population in the event of an H5N1 pandemic.
Three H5N1 vaccines for humans have been licensed as of June 2008:[82]
- Sanofi Pasteur's vaccine approved by the United States in April 2007,
- GlaxoSmithKline's vaccine Pandemrix approved by the European Union in May 2008, and
- CSL Limited's vaccine approved by Australia in June 2008.
All are produced in eggs and would require many months to be altered to a pandemic version.
H5N1 continually mutates, meaning vaccines based on current samples of avian H5N1 cannot be depended upon to work in the case of a future pandemic of H5N1. While there can be some cross-protection against related flu strains, the best protection would be from a vaccine specifically produced for any future pandemic flu virus strain. Dr. Daniel Lucey, co-director of the Biohazardous Threats and Emerging Diseases graduate program at Georgetown University, has made this point, "There is no H5N1 pandemic so there can be no pandemic vaccine." However, "pre-pandemic vaccines" have been created; are being refined and tested; and do have some promise both in furthering research and preparedness for the next pandemic. Vaccine manufacturing companies are being encouraged to increase capacity so that if a pandemic vaccine is needed, facilities will be available for rapid production of large amounts of a vaccine specific to a new pandemic strain.
Problems with H5N1 vaccine production include:
- lack of overall production capacity
- lack of surge production capacity (it is impractical to develop a system that depends on hundreds of millions of 11-day old specialized eggs on a standby basis)
- the pandemic H5N1 might be lethal to chickens
Cell culture (cell-based) manufacturing technology can be applied to influenza vaccines as they are with most viral vaccines and thereby solve the problems associated with creating flu vaccines using chicken eggs as is currently done.[83] :
- Currently, influenza vaccine for the annual, seasonal influenza program comes from four manufacturers. However, only a single manufacturer produces the annual vaccine entirely within the U.S. Thus, if a pandemic occurred and existing U.S.-based influenza vaccine manufacturing capacity was completely diverted to producing a pandemic vaccine, supply would be severely limited. Moreover, because the annual influenza manufacturing process takes place during most of the year, the time and capacity to produce vaccine against potential pandemic viruses for a stockpile, while continuing annual influenza vaccine production, is limited. Since supply will be limited, it is critical for HHS to be able to direct vaccine distribution in accordance with predefined groups (see Appendix D); HHS will ensure the building of capacity and will engage states in a discussion about the purchase and distribution of pandemic influenza vaccine.
- Vaccine production capacity: The protective immune response generated by current influenza vaccines is largely based on viral hemagglutinin (HA) and neuraminidase (NA) antigens in the vaccine. As a consequence, the basis of influenza vaccine manufacturing is growing massive quantities of virus in order to have sufficient amounts of these protein antigens to stimulate immune responses. Influenza vaccines used in the United States and around world are manufactured by growing virus in fertilized hens’ eggs, a commercial process that has been in place for decades. To achieve current vaccine production targets millions of 11-day old fertilized eggs must be available every day of production.
- In the near term, further expansion of these systems will provide additional capacity for the U.S.-based production of both seasonal and pandemic vaccines, however, the surge capacity that will be needed for a pandemic response cannot be met by egg-based vaccine production alone, as it is impractical to develop a system that depends on hundreds of millions of 11-day old specialized eggs on a standby basis. In addition, because a pandemic could result from an avian influenza strain that is lethal to chickens, it is impossible to ensure that eggs will be available to produce vaccine when needed.
- In contrast, cell culture manufacturing technology can be applied to influenza vaccines as they are with most viral vaccines (e.g., polio vaccine, measles-mumps-rubella vaccine, chickenpox vaccine). In this system, viruses are grown in closed systems such as bioreactors containing large numbers of cells in growth media rather than eggs. The surge capacity afforded by cell-based technology is insensitive to seasons and can be adjusted to vaccine demand, as capacity can be increased or decreased by the number of bioreactors or the volume used within a bioreactor. In addition to supporting basic research on cell-based influenza vaccine development, HHS is currently supporting a number of vaccine manufacturers in the advanced development of cell-based influenza vaccines with the goal of developing U.S.-licensed cell-based influenza vaccines produced in the United States.</ref>[84] The US government has purchased from Sanofi Pasteur and Chiron Corporation several million doses of vaccine meant to be used in case of an influenza pandemic of H5N1 avian influenza and is conducting clinical trials with these vaccines.[85] Researchers at the University of Pittsburgh have had success with a genetically engineered vaccine that took only a month to make and completely protected chickens from the highly pathogenic H5N1 virus.[86]
According to the United States Department of Health & Human Services:
- In addition to supporting basic research on cell-based influenza vaccine development, HHS is currently supporting a number of vaccine manufacturers in the advanced development of cell-based influenza vaccines with the goal of developing U.S.-licensed cell-based influenza vaccines produced in the United States. Dose-sparing technologies. Current U.S.-licensed vaccines stimulate an immune response based on the quantity of HA (hemagglutinin) antigen included in the dose. Methods to stimulate a strong immune response using less HA antigen are being studied in H5N1 and H9N2 vaccine trials. These include changing the mode of delivery from intramuscular to intradermal and the addition of immune-enhancing adjuvant to the vaccine formulation. Additionally, HHS is soliciting contract proposals from manufacturers of vaccines, adjuvants, and medical devices for the development and licensure of influenza vaccines that will provide dose-sparing alternative strategies.[87]
Chiron Corporation is now recertified and under contract with the National Institutes of Health to produce 8,000–10,000 investigational doses of Avian Flu (H5N1) vaccine. MedImmune and Aventis Pasteur are under similar contracts.[88] The United States government hopes to obtain enough vaccine in 2006 to treat 4 million people. However, it is unclear whether this vaccine would be effective against a hypothetical mutated strain that would be easily transmitted through human populations, and the shelflife of stockpiled doses has yet to be determined.[89]
The New England Journal of Medicine reported on March 30, 2006 on one of dozens of vaccine studies currently being conducted. The Treanor et al. study was on vaccine produced from the human isolate (A/Vietnam/1203/2004 H5N1) of a virulent clade 1 influenza A (H5N1) virus with the use of a plasmid rescue system, with only the hemagglutinin and neuraminidase genes expressed and administered without adjuvant. "The rest of the genes were derived from an avirulent egg-adapted influenza A/PR/8/34 strain. The hemagglutinin gene was further modified to replace six basic amino acids associated with high pathogenicity in birds at the cleavage site between hemagglutinin 1 and hemagglutinin 2. Immunogenicity was assessed by microneutralization and hemagglutination-inhibition assays with the use of the vaccine virus, although a subgroup of samples were tested with the use of the wild-type influenza A/Vietnam/1203/2004 (H5N1) virus." The results of this study combined with others scheduled to be completed by spring 2007 is hoped will provide a highly immunogenic vaccine that is cross-protective against heterologous influenza strains.[90]
On August 18, 2006. the World Health Organization changed the H5N1 strains recommended for candidate vaccines for the first time since 2004. "The WHO's new prototype strains, prepared by reverse genetics, include three new H5N1 subclades. The hemagglutinin sequences of most of the H5N1 avian influenza viruses circulating in the past few years fall into two genetic groups, or clades. Clade 1 includes human and bird isolates from Vietnam, Thailand, and Cambodia and bird isolates from Laos and Malaysia. Clade 2 viruses were first identified in bird isolates from China, Indonesia, Japan, and South Korea before spreading westward to the Middle East, Europe, and Africa. The clade 2 viruses have been primarily responsible for human H5N1 infections that have occurred during late 2005 and 2006, according to WHO. Genetic analysis has identified six subclades of clade 2, three of which have a distinct geographic distribution and have been implicated in human infections:
- Subclade 1, Indonesia
- Subclade 2, Middle East, Europe, and Africa
- Subclade 3, China
On the basis of the three subclades, the WHO is offering companies and other groups that are interested in pandemic vaccine development these three new prototype strains:
- An A/Indonesia/2/2005-like virus
- An A/Bar headed goose/Quinghai/1A/2005-like virus
- An A/Anhui/1/2005-like virus
[...] Until now, researchers have been working on prepandemic vaccines for H5N1 viruses in clade 1. In March, the first clinical trial of a U.S. vaccine for H5N1 showed modest results. In May, French researchers showed somewhat better results in a clinical trial of an H5N1 vaccine that included an adjuvant. Vaccine experts aren't sure if a vaccine effective against known H5N1 viral strains would be effective against future strains. Although the new viruses will now be available for vaccine research, WHO said clinical trials using the clade 1 viruses should continue as an essential step in pandemic preparedness, because the trials yield useful information on priming, cross-reactivity, and cross-protection by vaccine viruses from different clades and subclades."[91][92]
As of November 2006, the United States Department of Health and Human Services still had enough H5N1 pre-pandemic vaccine to treat about 3 million people (5.9 million full-potency doses) in spite of 0.2 million doses used for research and 1.4 million doses that have begun to lose potency (from the original 7.5 million full-potency doses purchased from Sanofi Pasteur and Chiron Corp.). The expected shelf life of seasonal flu vaccine is about a year so the fact that most of the H5N1 pre-pandemic stockpile is still good after about 2 years is considered encouraging.[93]
Annual reformulation of flu vaccine
Each year, three strains are chosen for selection in that year's flu vaccination by the WHO Global Influenza Surveillance Network. The chosen strains are the H1N1, H3N2, and Type-B strains thought most likely to cause significant human suffering in the coming season. Due to the high mutation rate of the virus a particular vaccine formulation is effective for at most about a year. The World Health Organization coordinates the contents of the vaccine each year to contain the most likely strains of the virus to attack the next year.
- "The WHO Global Influenza Surveillance Network was established in 1952. The network comprises 4 WHO Collaborating Centres (WHO CCs) and 112 institutions in 83 countries, which are recognized by WHO as WHO National Influenza Centres (NICs). These NICs collect specimens in their country, perform primary virus isolation and preliminary antigenic characterization. They ship newly isolated strains to WHO CCs for high level antigenic and genetic analysis, the result of which forms the basis for WHO recommendations on the composition of influenza vaccine for the Northern and Southern Hemisphere each year."[94]
The Global Influenza Surveillance Network's selection of viruses for the vaccine manufacturing process is based on its best estimate of which strains will be predominant the next year, amounting in the end to well-informed but fallible guesswork.[95]
2002–2003 season (Northern Hemisphere)
The vaccines produced for the 2002–2003 season use[96]:
- an A/New Caledonia/20/1999-like(H1N1);
- an A/Moscow/10/1999-like(H3N2);
- a B/Hong Kong/330/2001-like viruses.
2003 season (Southern Hemisphere)
The composition of influenza virus vaccines for use in the 2003 Southern Hemisphere influenza season recommended by the World Health Organization was [97] :
- an A/New Caledonia/20/99(H1N1)-like virus
- an A/Moscow/10/99(H3N2)-like virus (The widely used vaccine strain is A/Panama/2007/99)
- a B/Hong Kong/330/2001-like virus (Some vaccine strains used were B/Shandong/7/97, B/Hong Kong/330/2001, B/Hong Kong/1434/2002)
2003–2004 season (Northern Hemisphere)
The production of flu vaccine requires a lead time of about six months before the season. It is possible that by flu season a strain becomes common for which the vaccine does not provide protection. In the 2003–2004 season the vaccine was produced to protect against A/Panama, A/New Caledonia, and B/Hong Kong. A new strain, A/Fujian, was discovered after production of the vaccine started and vaccination gave only partial protection against this strain.
Nature magazine reported that the Influenza Genome Sequencing Project, using phylogenetic analysis of 156 H3N2 genomes, "explains the appearance, during the 2003–2004 season, of the 'Fujian/411/2002'-like strain, for which the existing vaccine had limited effectiveness" as due to an epidemiologically significant reassortment. "Through a reassortment event, a minor clade provided the haemagglutinin gene that later became part of the dominant strain after the 2002–2003 season. Two of our samples, A/New York/269/2003 (H3N2) and A/New York/32/2003 (H3N2), show that this minor clade continued to circulate in the 2003–2004 season, when most other isolates were reassortants."[98]
According to the CDC:
- During the 2003–2004 influenza season, influenza A (H1), A (H3N2), and B viruses co-circulated worldwide, and influenza A (H3N2) viruses predominated. Several Asian countries reported widespread outbreaks of avian influenza A (H5N1) among poultry. In Vietnam and Thailand, these outbreaks were associated with severe illnesses and deaths among humans. In the United States, the 2003–2004 influenza season began earlier than most seasons, peaked in December, was moderately severe in terms of its impact on mortality, and was associated predominantly with influenza A (H3N2) viruses.[99]
During September 28, 2003 – May 22, 2004, WHO and NREVSS collaborating laboratories in the United States tested 130,577 respiratory specimens for influenza viruses; 24,649 (18.9%) were positive. Of these, 24,393 (99.0%) were influenza A viruses, and 249 (1.0%) were influenza B viruses. Among the influenza A viruses, 7,191 (29.5%) were subtyped; 7,189 (99.9%) were influenza A (H3N2) viruses, and two (0.1%) were influenza A (H1) viruses. The proportion of specimens testing positive for influenza first increased to >10% during the week ending October 25, 2003 (week 43), peaked at 35.2% during the week ending November 29 (week 48), and declined to <10% during the week ending January 17, 2004 (week 2). The peak percentage of specimens testing positive for influenza during the previous four seasons had ranged from 23% to 31% and peaked during late December to late February.[99]
As of June 15, 2004, CDC had antigenically characterized 1,024 influenza viruses collected by U.S. laboratories since October 1, 2003: 949 influenza A (H3N2) viruses, three influenza A (H1) viruses, one influenza A (H7N2) virus, and 71 influenza B viruses. Of the 949 influenza A (H3N2) isolates characterized, 106 (11.2%) were similar antigenically to the vaccine strain A/Panama/2007/99 (H3N2), and 843 (88.8%) were similar to the drift variant, A/Fujian/411/2002 (H3N2). Of the three A (H1) isolates that were characterized, two were H1N1 viruses, and one was an H1N2 virus. The hemagglutinin proteins of the influenza A (H1) viruses were similar antigenically to the hemagglutinin of the vaccine strain A/New Caledonia/20/99. Of the 71 influenza B isolates that were characterized, 66 (93%) belonged to the B/Yamagata/16/88 lineage and were similar antigenically to B/Sichuan/379/99, and five (7%) belonged to the B/Victoria/2/87 lineage and were similar antigenically to the corresponding vaccine strain B/Hong Kong/330/2001.[99]
- H9N2
In December 2003, one confirmed case of avian influenza A (H9N2) virus infection was reported in a child aged five years in Hong Kong. The child had fever, cough, and nasal discharge in late November, was hospitalized for two days, and fully recovered. The source of this child's H9N2 infection is unknown.[99]
- H5N1
During January–March 2004, a total of 34 confirmed human cases of avian influenza A (H5N1) virus infection were reported in Vietnam and Thailand. The cases were associated with severe respiratory illness requiring hospitalization and a case-fatality proportion of 68% (Vietnam: 22 cases, 15 deaths; Thailand: 12 cases, eight deaths). A substantial proportion of the cases were among children and young adults (i.e., persons aged 5–24 years). These cases were associated with widespread outbreaks of highly pathogenic H5N1 influenza among domestic poultry.[99]
- H7N3
During March 2004, health authorities in Canada reported two confirmed cases of avian influenza A (H7N3) virus infection in poultry workers who were involved in culling of poultry during outbreaks of highly pathogenic H7N3 on farms in the Fraser River Valley, British Columbia. One patient had unilateral conjunctivitis and nasal discharge, and the other had unilateral conjunctivitis and headache. Both illnesses resolved without hospitalization.[99]
- H7N2
During the 2003–2004 influenza season, a case of avian influenza A (H7N2) virus infection was detected in an adult male from New York, who was hospitalized for upper and lower respiratory tract illness in November 2003. Influenza A (H7N2) virus was isolated from a respiratory specimen from the patient, whose acute symptoms resolved. The source of this person's infection is unknown.[99]
2004 season (Southern Hemisphere)
The composition of influenza virus vaccines for use in the 2004 Southern Hemisphere influenza season recommended by the World Health Organization was:
- an A/New Caledonia/20/99(H1N1)-like virus
- an A/Fujian/411/2002(H3N2)-like virus (A/Kumamoto/102/2002 and A/Wyoming/3/2003 were egg-grown A/Fujian/411/2002-like viruses)
- a B/Hong Kong/330/2001-like virus (B/Shandong/7/97, B/Hong Kong/330/2001 and B/Hong Kong/1434/2002 were among those used at the time. B/Brisbane/32/2002 was also available.)[100][101]
2004–2005 season (Northern Hemisphere)
According to the CDC:
- On the basis of antigenic analyses of recently isolated influenza viruses, epidemiologic data, and postvaccination serologic studies in humans, the Food and Drug Administration's Vaccines and Related Biological Products Advisory Committee (VRBPAC) recommended that the 2004–05 trivalent influenza vaccine for the United States contain A/New Caledonia/20/99-like (H1N1), A/Fujian/411/2002-like (H3N2), and B/Shanghai/361/2002-like viruses. Because of the growth properties of the A/Wyoming/3/2003 and B/Jiangsu/10/2003 viruses, U.S. vaccine manufacturers are using these antigenically equivalent strains in the vaccine as the H3N2 and B components, respectively. The A/New Caledonia/20/99 virus will be retained as the H1N1 component of the vaccine.[99]
2005 season (Southern Hemisphere)
The composition of influenza virus vaccines for use in the 2005 Southern Hemisphere influenza season recommended by the World Health Organization was:
- an A/New Caledonia/20/99(H1N1)-like virus;
- an A/Wellington/1/2004(H3N2)-like virus;
- a B/Shanghai/361/2002-like virus (B/Shanghai/361/2002, B/Jilin/20/2003 and B/Jiangsu/10/2003 were used at the time)[102][103]
2005–2006 season (Northern Hemisphere)
The vaccines produced for the 2005–2006 season use:
- an A/New Caledonia/20/1999-like(H1N1);
- an A/California/7/2004-like(H3N2) (or the antigenically equivalent strain A/New York/55/2004);
- a B/Jiangsu/10/2003-like viruses.
In people in the United States, overall flu and pneumonia deaths were below those of a typical flu season with 84% Influenzavirus A and the rest Influenzavirus B. Of the patients who had Type A viruses, 80% had viruses identical or similar to the A bugs in the vaccine. 70% of the people testing positive for a B virus had Type B Victoria, a version not found in the vaccine.[104]
"During the 2005–06 season, influenza A (H3N2) viruses predominated overall, but late in the season influenza B viruses were more frequently isolated than influenza A viruses. Influenza A (H1N1) viruses circulated at low levels throughout the season. Nationally, activity was low from October through early January, increased during February, and peaked in early March. Peak activity was less intense, but activity remained elevated for a longer period of time this season compared to the previous three seasons. The longer period of elevated activity may be due in part to regional differences in the timing of peak activity and intensity of influenza B activity later in the season."[105]
2006 season (Southern Hemisphere)
The composition of influenza virus vaccines for use in the 2006 Southern Hemisphere influenza season recommended by the World Health Organization was:
- an A/New Caledonia/20/99(H1N1)-like virus;
- an A/California/7/2004(H3N2)-like virus (A/New York/55/2004 was used at the time);
- a B/Malaysia/2506/2004-like virus[106][107]
2006–2007 season (Northern Hemisphere)
The 2006–2007 influenza vaccine composition recommended by the World Health Organization on February 15, 2006 and the U.S. FDA's Vaccines and Related Biological Products Advisory Committee (VRBPAC) on February 17, 2006 use:
- an A/New Caledonia/20/99 (H1N1)-like virus;
- an A/Wisconsin/67/2005 (H3N2)-like virus (A/Wisconsin/67/2005 and A/Hiroshima/52/2005 strains);
- a B/Malaysia/2506/2004-like virus from B/Malaysia/2506/2004 and B/Ohio/1/2005 strains which are of B/Victoria/2/87 lineage.[108]
2007 season (Southern Hemisphere)
The composition of influenza virus vaccines for use in the 2007 Southern Hemisphere influenza season recommended by the World Health Organization on September 20, 2006[109] was:
- an A/New Caledonia/20/99(H1N1)-like virus,
- an A/Wisconsin/67/2005(H3N2)-like virus (A/Wisconsin/67/2005 and A/Hiroshima/52/2005 were used at the time),
- a B/Malaysia/2506/2004-like virus[110][111]
2007–2008 season (Northern Hemisphere)
The composition of influenza virus vaccines for use in the 2007–2008 Northern Hemisphere influenza season recommended by the World Health Organization on February 14, 2007[112] was:
- an A/Solomon Islands/3/2006 (H1N1)-like virus;
- an A/Wisconsin/67/2005 (H3N2)-like virus (A/Wisconsin/67/2005 (H3N2) and A/Hiroshima/52/2005 were used at the time);
- a B/Malaysia/2506/2004-like virus[113][114]
In the US, the CDC reported in Feb 2008 that the H1N1 component was a good match (96%) to the infections occurring. But 87% of the H3N2 are A/Brisbane/10/2007-like viruses, which are a recent antigenic variant of the vaccine strain, A/Wisconsin. And 93% of the B viruses are in a B/Yamagata lineage that is relatively distinct from the vaccine strain B/Victoria lineage. Only one of the three components was a good match; A/Wisconsin is moderately protective against the drifted A/Brisbane strain. 4.5% of those viruses tested are resistant to Oseltamivir, or Tamiflu—a significant increase over previous years.[115]
This vaccine has been described as 40% effective compared to other years that have been 85–95% effective.[115][116]
2008 season (Southern Hemisphere)
The composition of virus vaccines for use in the 2008 Southern Hemisphere influenza season recommended by the World Health Organization on September 17-19, 2007 was:
- an A/Solomon Islands/3/2006 (H1N1)-like virus;
- an A/Brisbane/10/2007 (H3N2)-like virus;
- a B/Florida/4/2006-like virus[117][118]
2008-2009 season (Northern Hemisphere)
The composition of virus vaccines for use in the 2008-2009 Northern Hemisphere influenza season recommended by the World Health Organization on February 14, 2008[119] was:
- an A/Brisbane/59/2007 (H1N1)-like virus;
- an A/Brisbane/10/2007 (H3N2)-like virus;
- a B/Florida/4/2006-like virus (B/Florida/4/2006 and B/Brisbane/3/2007 (a B/Florida/4/2006-like virus) were used at the time).[120][121]
As of May 30, 2009: "CDC has antigenically characterized 1,567 seasonal human influenza viruses [947 influenza A (H1), 162 influenza A (H3) and 458 influenza B viruses] collected by U.S. laboratories since October 1, 2008, and 84 novel influenza A (H1N1) viruses. All 947 influenza seasonal A (H1) viruses are related to the influenza A (H1N1) component of the 2008-09 influenza vaccine (A/Brisbane/59/2007). All 162 influenza A (H3N2) viruses are related to the A (H3N2) vaccine component (A/Brisbane/10/2007). All 84 novel influenza A (H1N1) viruses are related to the A/California/07/2009 (H1N1) reference virus selected by WHO as a potential candidate for novel influenza A (H1N1) vaccine. Influenza B viruses currently circulating can be divided into two distinct lineages represented by the B/Yamagata/16/88 and B/Victoria/02/87 viruses. Sixty-one influenza B viruses tested belong to the B/Yamagata lineage and are related to the vaccine strain (B/Florida/04/2006). The remaining 397 viruses belong to the B/Victoria lineage and are not related to the vaccine strain."[122]
2009 season (Southern Hemisphere)
The composition of virus vaccines for use in the 2009 Southern Hemisphere influenza season recommended by the World Health Organization on September 17-19, 2008[123] was:
- an A/Brisbane/59/2007 (H1N1)-like virus;
- an A/Brisbane/10/2007 (H3N2)-like virus;
- a B/Florida/4/2006-like virus[124]
2009-2010 season (Northern Hemisphere)
The composition of virus vaccines for use in the 2009-2010 Northern Hemisphere influenza season recommended by the World Health Organization on February 12, 2009[125] was:
- an A/Brisbane/59/2007 (H1N1)-like virus;
- an A/Brisbane/10/2007 (H3N2)-like virus;
- a B/Brisbane/60/2008-like virus.[126][127]
Since the A/Brisbane/59/2007 (H1N1)-like virus used in the vaccine is an unrelated seasonal strain of influenza, it probably cannot create immunity to the new, non-seasonal strain of influenza A virus subtype H1N1 responsible for the 2009 swine flu outbreak.[122]
Flu vaccine for nonhumans
"Vaccination in the veterinary world pursues four goals: (i) protection from clinical disease, (ii) protection from infection with virulent virus, (iii) protection from virus excretion, and (iv) serological differentiation of infected from vaccinated animals (so-called DIVA principle). In the field of influenza vaccination, neither commercially available nor experimentally tested vaccines have been shown so far to fulfil all of these requirements."[128]
Horses
Horses with horse flu can run a fever, have a dry hacking cough, have a runny nose, and become depressed and reluctant to eat or drink for several days but usually recover in two to three weeks. "Vaccination schedules generally require a primary course of 2 doses, 3–6 weeks apart, followed by boosters at 6–12 month intervals. It is generally recognised that in many cases such schedules may not maintain protective levels of antibody and more frequent administration is advised in high-risk situations."[129]
It is a common requirement at shows in the United Kingdom that horses be vaccinated against equine flu and a vaccination card must be produced; the FEI requires vaccination every six months.[130] [131]
Poultry
Poultry vaccines for bird flu are made on the cheap and are not filtered and purified like human vaccines to remove bits of bacteria or other viruses. They usually contain whole virus, not just hemagglutinin as in most human flu vaccines. Purification to standards needed for humans is far more expensive than the original creation of the unpurified vaccine from eggs. There is no market for veterinary vaccines that are that expensive. Another difference between human and poultry vaccines is that poultry vaccines are adjuvated with mineral oil, which induces a strong immune reaction but can cause inflammation and abscesses. "Chicken vaccinators who have accidentally jabbed themselves have developed painful swollen fingers or even lost thumbs, doctors said. Effectiveness may also be limited. Chicken vaccines are often only vaguely similar to circulating flu strains — some contain an H5N2 strain isolated in Mexico years ago. 'With a chicken, if you use a vaccine that's only 85 percent related, you'll get protection,' Dr. Cardona said. 'In humans, you can get a single point mutation, and a vaccine that's 99.99 percent related won't protect you.' And they are weaker [than human vaccines]. 'Chickens are smaller and you only need to protect them for six weeks, because that's how long they live till you eat them,' said Dr. John J. Treanor, a vaccine expert at the University of Rochester. Human seasonal flu vaccines contain about 45 micrograms of antigen, while an experimental A(H5N1) vaccine contains 180. Chicken vaccines may contain less than 1 microgram. 'You have to be careful about extrapolating data from poultry to humans,' warned Dr. David E. Swayne, director of the agriculture department's Southeast Poultry Research Laboratory. 'Birds are more closely related to dinosaurs.'"[132]
Researchers, led by Nicholas Savill of the University of Edinburgh in Scotland, used mathematical models to simulate the spread of H5N1 and concluded that "at least 95 per cent of birds need to be protected to prevent the virus spreading silently. In practice, it is difficult to protect more than 90 per cent of a flock; protection levels achieved by a vaccine are usually much lower than this."[133] The Food and Agriculture Organization of the United Nations has issued recommendations on the prevention and control of avian influenza in poultry, including the use of vaccination.[134]
Pigs
Swine origin Influenza Virus (SoIV) vaccines are extensively used in the swine industry in Europe and North America. Most swine flu vaccine manufacturers include an H1N1 and an H3N2 SoIV strains.
Swine influenza has become a greater problem in recent decades. Evolution of the virus has resulted in inconsistent responses to traditional vaccines. Standard commercial swine origin flu vaccines are effective in controlling the problem when the virus strains match enough to have significant cross-protection and custom (autogenous) vaccines made from the specific viruses isolated are created and used in the more difficult cases.[135] SoIV vaccine manufacture Novartis paints this picture: "A strain of swine origin influenza virus (SoIV) called H3N2, first identified in the US in 1998, has brought exasperating production losses to swine producers. Abortion storms are a common sign. Sows go off feed for two or three days and run a fever up to 106°F. Mortality in a naïve herd can run as high as 15%."[136]
Dogs
In 2004, Influenza A virus subtype H3N8 was discovered to cause canine influenza. Because of the lack of previous exposure to this virus, dogs have no natural immunity to this virus. However a vaccine is now available.[137]
Computer-assisted vaccine design
A new parameter has been defined to quantify the antigenic distance between two H3N2 influenza strains. This parameter was used to measure antigenic distance between circulating H3N2 strains and the closest vaccine component of the influenza vaccine. For the data between 1971 and 2004, the measure of antigenic distance correlated better with efficacy in humans of the H3N2 influenza A annual vaccine than did current measures of antigenic distance such as phylogenetic sequence analysis or ferret antisera inhibition assays. This measure of antigenic distance could be used to guide the design of the annual flu vaccine. The antigenic distance combined with a multiple-strain avian influenza transmission model was used to study the threat of simultaneous introduction of multiple avian influenza strains. Population at Risk (PaR) can be used to quantify the risk of a flu pandemic and to calculate the improvement that a multiple vaccine offers.[138]
See also
- Influenza
- 2009 flu pandemic vaccine
- H5N1
- Influenza research
- Influenza pandemic
- Vaccine shortage of 2004
References
- ^ Couch R. B. Seasonal inactivated influenza virus vaccines. Vaccine. 2008 Sep 12;26 Suppl 4:D5-9. Review. PMID 18602728
- ^ http://www.cdc.gov/FLU/protect/keyfacts.htm
- ^ Influenza Vaccination: A Summary for Clinicians http://www.cdc.gov/flu/professionals/vaccination/vax-summary.htm
- ^ Flu Shots Halve Risk of Death, Cut Illness in Elderly (Update1)
- Influenza vaccines ... cut the risk that elderly people will die of the virus in half and reduced the chance of hospitalization by more than a quarter, according to a study released today by the New England Journal of Medicine. http://www.bloomberg.com/apps/news?pid=20601081&sid=aoDQn_PvtPGw&refer=Australia
- ^ A Multitude of Vaccine Benefits, Yet Controversy Persists
- Public health experts generally agree that after clean water and flush toilets, the most important health advances in history have been vaccinations.
- ^ Flu shots leave heart failure patients at risk
Reuters
Sat Mar 29, 2008
- Influenza causes 36,000 deaths and more than 200,000 hospitalizations in the United States each year, according to the U.S. Centers for Disease Control and Prevention.
- ^ World Health Organization. Seasonal Influenza. http://www.who.int/mediacentre/factsheets/fs211/en/index.html.
- ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 18679129, please use {{cite journal}} with
|pmid=18679129instead. - ^ Huge flu vaccine trial to be held
March 31, 2008
- "Professor Robert Booy, of the National Centre for Immunisation Research and Surveillance at Westmead in Sydney, said influenza put 15,000 Australians in hospital each year."
- ...
- "About 1500 deaths annually are attributed to the virus and it costs our country millions of dollars annually in lost productivity, Professor Robert Booy said.
- ^ Young Children Hospitalized for Flu Associated With Higher Costs and Higher Risk Illness.
Study results presented May 4 at the Pediatric Academic Society annual meeting in Honolulu, Hawaii http://www.prnewswire.com/cgi-bin/stories.pl?ACCT=109&STORY=/www/story/05-01-2008/0004804012&EDATE=After analyzing data in three U.S. cities over the course of three flu
seasons (2003-2006), the researchers found that 90 percent of the
highest-cost hospitalizations for children were linked to influenza, or flu with a co-infection of the respiratory tract.
- ^ a b U.S. panel recommends all kids get the flu shot Updated Wed. Feb. 27 2008 1:56 PM ET CTV.ca News Staff http://www.ctv.ca/servlet/ArticleNews/story/CTVNews/20080227/flu_shot_080226/20080227?hub=TopStories
- ^ CDC - Influenza (Flu) | Vaccination: Summary for Clinicians
- ^ CDC Primary Changes and Updates in the Recommendations The 2009 recommendations include three principal changes or updates: * Annual vaccination of all children aged 6 months--18 years should begin as soon as the 2009--10 influenza vaccine is available. Annual vaccination of all children aged 6 months--4 years (59 months) and older children with conditions that place them at increased risk for complications from influenza should continue to be a primary focus of vaccination efforts as providers and programs transition to routinely vaccinating all children. http://www.cdc.gov/mmwr/preview/mmwrhtml/rr58e0724a1.htm
- ^ Panel Advises Flu Shots for Children Up to Age 18 The New York Times By LAWRENCE K. ALTMAN Published: February 28, 2008 Quoting Dr. Anne Schuchat, who directs the CDC’s program on immunization and respiratory diseases. http://www.nytimes.com/2008/02/28/health/28flu.html
- ^ Seasonal Flu Vaccination May Offer Partial Immunity to H5N1 http://www.upmc-cbn.org/report_archive/2007/02_February_2007/cbnreport_02212007.html
- ^ Cross-Reactive Neuraminidase Antibodies Afford Partial Protection against H5N1 in Mice and Are Present in Unexposed Humans
Matthew R. Sandbulte, Gretchen S. Jimenez, Adrianus C. M. Boon, Larry R. Smith, John J. Treanor, Richard J. Webby*
- "These data reveal that humoral immunity elicited by huN1 can partially protect against H5N1 infection in a mammalian host. Our results suggest that a portion of the human population could have some degree of resistance to H5N1 influenza, with the possibility that this could be induced or enhanced through immunization with seasonal influenza vaccines."
- ^ 1918 Spanish flu records could hold the key to solving future pandemics November 2008. Australian study suggesting city dwellers, who were more likely to have been exposed to common flu may have benefitted from some protection from the 1918 pandemic influenza (the "Spanish Flu"). http://www.physorg.com/news145530214.html
- ^ Ponce-de-León-Rosales, Alpuche-Aranda, Rodriguez-López, Perez-Padilla, Hernandez-Avila Partial protection against novel pandemic influenza A/H1N1 2009 from seasonal flu vaccine: case-control study http://www.bmj.com/cgi/content/full/339/oct06_2/b3928 Reference: BMJ 2009; 339: b3928 (study), b4014 (editorial) Published 6 October 2009, doi:10.1136/bmj.b3928 Date published: 09/10/2009 17:15 British NHS summary: http://www.nelm.nhs.uk/en/NeLM-Area/News/2009---October/09/Partial-protection-against-novel-pandemic-influenza-AH1N1-2009-from-seasonal-flu-vaccine-case-control-study-/
- ^ Chen H, Wang Y, Liu W, Zhang J, Dong B, Fan X, et al. Serologic survey of pandemic (H1N1) 2009 virus, Guangxi Province, China [letter]. Emerg Infect Dis. 2009 Nov; [Epub ahead of print] Serologic Survey of Pandemic (H1N1) 2009 DOI: 10.3201/eid1511.090868
- ^ Xing Z, Cardona CJ. Preexisting immunity to pandemic (H1N1) 2009 [letter]. Emerg Infect Dis. 2009 Nov; [Epub ahead of print] Preexisting Immunity to Pandemic (H1N1) 2009 Virus, Guangxi Province, China DOI: 10.3201/eid1511.090685
- ^ Z. Xing and C.J. Cardona. Preexisting Immunity to Pandemic (H1N1) 2009. Emerging Infectious Diseases, 2009; DOI: 10.3201/eid1511.090685
- ^ Seasonal flu vaccine protects against H1N1: Study Article by Neka Sehgal - November 21, 2009 http://www.themoneytimes.com/featured/20091121/seasonal-flu-vaccine-protects-against-h1n1-study-id-1091674.html
- ^
Webster, R. G. and Walker, E. J. (2003). "The world is teetering on the edge of a pandemic that could kill a large fraction of the human population". American Scientist. 91 (2): 122. doi:10.1511/2003.2.122.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Blakemore, C. (2006-04-09). "Battle of time, luck and science". The Sunday Times - Britain. Retrieved 2006-06-22.
- ^ Influenza PDF.
- ^ The Threat of Pandemic Influenza: Are We Ready? Workshop Summary (2005) (free online book) page 62
- ^ Influenza Report article Vaccines by Stephen Korsman
- ^ CDC report Prevention and Control of Influenza published April 12, 2002
- ^ NEJM Volume 352:1839-1842 May 5, 2005 Number 18 article Preparing for the Next Pandemic by Michael T. Osterholm
- ^ The Sky is Falling: An Analysis of the Swine Flu Affair of 1976
- ^ World Health Organization. Acyte Respiratory Infections: Influenza. 2009. http://www.who.int/vaccine_research/diseases/ari/en/index1.html
- ^ World Health Organization. Tables on the Clinical trials of pandemic influenza prototype vaccines. July 2009. http://www.who.int/vaccine_research/immunogenicity/immunogenicity_table.xls
- ^ US Food & Drug Administration. FDA Approves Vaccines for 2009 H1N1 Influenza Virus Approval Provides Important Tool to Fight Pandemic. September 15, 2009. http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm182399.htm
- ^ Fedson D (1998). "Measuring protection: efficacy versus effectiveness". Dev Biol Stand. 95: 195–201. PMID 9855432.
- ^ Stephenson I, Zambon M, Rudin A, Colegate A, Podda A, Bugarini R, Del Giudice G, Minutello A, Bonnington S, Holmgren J, Mills K, Nicholson K (2006). "Phase I evaluation of intranasal trivalent inactivated influenza vaccine with nontoxigenic Escherichia coli enterotoxin and novel biovector as mucosal adjuvants, using adult volunteers". J Virol. 80 (10): 4962–70. doi:10.1128/JVI.80.10.4962-4970.2006. PMC 1472052. PMID 16641287.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ a b Treanor J, Kotloff K, Betts R, Belshe R, Newman F, Iacuzio D, Wittes J, Bryant M (1999). "Evaluation of trivalent, live, cold-adapted (CAIV-T) and inactivated (TIV) influenza vaccines in prevention of virus infection and illness following challenge of adults with wild-type influenza A (H1N1), A (H3N2), and B viruses". Vaccine. 18 (9–10): 899–906. doi:10.1016/S0264-410X(99)00334-5. PMID 10580204.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ a b Jefferson T (2006). "Influenza vaccination: policy versus evidence". BMJ. 333 (7574): 912–5. doi:10.1136/bmj.38995.531701.80. PMC 1626345. PMID 17068038.
- ^ a b Demicheli V, Rivetti D, Deeks J, Jefferson T (2004). "Vaccines for preventing influenza in healthy adults". Cochrane Database Syst Rev (3): CD001269. doi:10.1002/14651858.CD001269.pub2. PMID 15266445.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ a b Smith S, Demicheli V, Di Pietrantonj C, Harnden A, Jefferson T, Matheson N, Rivetti A (2006). "Vaccines for preventing influenza in healthy children". Cochrane Database Syst Rev (1): CD004879. doi:10.1002/14651858.CD004879.pub2. PMID 16437500.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ a b Rivetti D, Jefferson T, Thomas R, Rudin M, Rivetti A, Di Pietrantonj C, Demicheli V (2006). "Vaccines for preventing influenza in the elderly". Cochrane Database Syst Rev. 3: CD004876. doi:10.1002/14651858.CD004876.pub2. PMID 16856068.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ a b Jefferson T, Rivetti D, Rivetti A, Rudin M, Di Pietrantonj C, Demicheli V (2005). "Efficacy and effectiveness of influenza vaccines in elderly people: a systematic review". Lancet. 366 (9492): 1165–74. doi:10.1016/S0140-6736(05)67339-4. PMID 16198765.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Simonsen L, Viboud C, Taylor RJ, Miller MA, Jackson L (2009). "Influenza vaccination and mortality benefits: new insights, new opportunities". Vaccine. 27 (45): 6300–4. doi:10.1016/j.vaccine.2009.07.008. PMID 19840664.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Nuño, M (2007). "Assessing the role of basic control measures, antivirals and vaccine in curtailing pandemic influenza: scenarios for the US, UK and the Netherlands". Journal of the Royal Society, Interface / the Royal Society. 4 (14): 505–521. doi:10.1098/rsif.2006.0186. PMC 2373400. PMID 17251132. Retrieved 2009-09-24.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Ferguson, Neil M. (2006). "Strategies for mitigating an influenza pandemic". Nature. 442 (7101): 448–452. doi:10.1038/nature04795. PMID 16642006.
{{cite journal}}:|access-date=requires|url=(help); Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ CDC article Influenza (Flu) | Comparisons of LAIV and TAIV Efficacy
- ^ New York Times article Panel Advises Flu Shots for Children Up to Age 18 Published: February 28, 2008
- ^ Attention: This template ({{cite doi}}) is deprecated. To cite the publication identified by doi:10.1002/14651858.CD004876.pub2, please use {{cite journal}} (if it was published in a bona fide academic journal, otherwise {{cite report}} with
|doi=10.1002/14651858.CD004876.pub2instead. - ^ Attention: This template ({{cite doi}}) is deprecated. To cite the publication identified by doi:10.1093/ije/dyi274, please use {{cite journal}} (if it was published in a bona fide academic journal, otherwise {{cite report}} with
|doi=10.1093/ije/dyi274instead. - ^ Jefferson T, Rivetti A, Harnden A, Di Pietrantonj C, Demicheli V (2008). "Vaccines for preventing influenza in healthy children". Cochrane Database Syst Rev (2): CD004879. doi:10.1002/14651858.CD004879.pub3. PMID 18425905.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Children, the Flu, and the Flu Vaccine http://www.cdc.gov/flu/protect/children.htm
- ^ Attention: This template ({{cite doi}}) is deprecated. To cite the publication identified by doi:10.1002/14651858.CD001269.pub3, please use {{cite journal}} (if it was published in a bona fide academic journal, otherwise {{cite report}} with
|doi=10.1002/14651858.CD001269.pub3instead. - ^ Nichol, K.L., Nordin, J.D., Nelson, D.B., Mullooly, J.D., & Hak, E. (2007). Effectiveness of Influenza Vaccine in the community-dwelling elderly. The New England Journal of Medicine, 357(14), 1373-1381.
- ^ Vu, T., Farish, S., Jenkins, M., & Kelly, H. (2002). A meta-analysis of effectiveness of influenza vaccine in persons aged 65 years and over living in the community. Vaccine, 20, 1831-1836.
- ^ Nordin, J., Mullooly, J., Poblete, S., Strikas, R., Petrucci, R., Wei, F., et al. (2001). Influenza vaccine effectiveness in preventing hospitalizations and deaths in persons 65 years or older in Minnesota, New York, and Oregon: Data from 3 health plans. The Journal of Infectious Diseases, 184(6), 665-670.
- ^ Simonsen, L., Taylor, R.J., Viboud, C., Miller, M.A., & Jackson, L.A. (2007). Mortality benefits of influenza vaccination in elderly people: An ongoing controversy. The Lancet Infectious Diseases, 7, 658-666.
- ^ Thompson WW, Shay DK, Weintraub E, Brammer L, Cox N, Anderson LJ, Fukuda K (2003). "Mortality associated with influenza and respiratory syncytial virus in the United States". The Journal of the American Medical Association. 289 (2): 179–186. doi:10.1001/jama.289.2.179. PMID 12517228.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Hak E, Buskens E, van Essen GA, de Bakker DH, Grobbee DE, Tacken MA, van Hout BA, Verheij TJ (2005). "Clinical effectiveness of vaccination in persons younger than 65 years with high-risk medical conditions: the PRISMA study". Archives of Internal Medicine. 165 (3): 274–280. doi:10.1001/archinte.165.3.274. PMID 15710789.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Nichol KL, Nordin J, Mullooly J, Lask R, Fillbrandt K, Iwane M (2003). "Influenza vaccination and reduction in hospitalizations for cardiac disease and stroke among the elderly". The New England Journal of Medicine. 348 (14): 1322–1332. doi:10.1056/NEJMoa025028. PMID 12672859.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Woloshin S, Schwartz LM, Welch HG (2005-10-25). "A shot of fear". The Washington Post. Retrieved 2006-11-09.
{{cite news}}: CS1 maint: multiple names: authors list (link) - ^ Jackson LA, Jackson ML, Nelson JC, Neuzil KM, Weiss NS (2006). "Evidence of bias in estimates of influenza vaccine effectiveness in seniors". Int J Epidemiol. 35 (2): 337–44. doi:10.1093/ije/dyi274. PMID 16368725.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Attention: This template ({{cite doi}}) is deprecated. To cite the publication identified by doi:10.1093/ije/dyi275, please use {{cite journal}} (if it was published in a bona fide academic journal, otherwise {{cite report}} with
|doi=10.1093/ije/dyi275instead. - ^ W Keitel "et al.". Safety of high doses of influenza vaccine and effect on antibody responses in elderly persons "Archives of Internal Medicine" DOI: 10.1001/archinternmed.166.10.1121 (2006). c.f., NIAID Study Finds Higher Dose Of Flu Vaccine Improves Immune Response In The Elderly http://www.epa.gov/aging/press/othernews/2006/2006_0522_ons_1.htm http://www.nih.gov/news/pr/may2006/niaid-22.htm
- ^ World Health Organization Seasonal Influenza fact sheet. http://www.who.int/mediacentre/factsheets/fs211/en/index.html
- ^ NEJM - The Japanese Experience with Vaccinating Schoolchildren against Influenza
- ^ http://www.cdc.gov/flu/about/qa/season.htm
- ^ CDC - seasonal flu
- ^ immunize.org article Summary of Recommendations for Adult Immunization which is linked from CDC website CDC
- ^ CDC
- ^ Wang Z, Tobler S, Roayaei J, et al article "Live Attenuated or Inactivated Influenza Vaccines and Medical Encounters for Respiratory Illnesses Among US Military Personnel"
- ^ Thomas RE, Jefferson TO, Demicheli V, Rivetti D (2006). "Influenza vaccination for health-care workers who work with elderly people in institutions: a systematic review". Lancet Infect Dis. 6 (5): 273–279. doi:10.1016/S1473-3099(06)70462-5. PMID 16631547.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ "Should pregnant women get the flu shot?", Dr. Judith Reichman, MSNBC, 2007 Oct. 1.
- ^ Mother’s Flu Shot Protects Newborns Newswise, Retrieved on September 17, 2008.
- ^ CDC
- ^ CDC - Inactivated Influenza Vaccine 2007-2008 - What You Need To Know
- ^ a b c Flu - LAIV
- ^ Review Shows Safety of H1N1 Vaccine, Officials Say "No substantial differences between H1N1 and seasonal influenza vaccines were noted in the proportion or types of serious adverse events reported." http://www.nytimes.com/2009/12/05/health/05flu.html?ref=health
- ^ Offit PA (2007). "Thimerosal and vaccines—a cautionary tale". N Engl J Med. 357 (13): 1278–9. doi:10.1056/NEJMp078187. PMID 17898096.
- ^ Global Advisory Committee on Vaccine Safety (2006-07-14). "Thiomersal and vaccines". World Health Organization. Retrieved 2007-11-20.
- ^ New and Old Ways to Make Flu Vaccines, 8 November 2007, National Public Radio.
- ^ PATH, Oliver Wyman. Influenza Vaccine Strategies for Broad Global Access. 2007. http://www.path.org/files/VAC_infl_publ_rpt_10-07.pdf
- ^ Bright RA, Carter DM, Daniluk S, Toapanta FR, Ahmad A, Gavrilov V, Massare M, Pushko P, Mytle N, Rowe T, Smith G, Ross TM. Influenza virus-like particles elicit broader immune responses than whole virion inactivated influenza virus or recombinant hemagglutinin. Vaccine. 2007 May 10;25(19):3871-8.
- ^ CIDRAP article Australia approves CSL's H5N1 vaccine published June 17, 2008
- ^ According to the U.S. HHS (United States Department of Health & Human Services) Pandemic Influenza Plan Appendix F: Current HHS Activities last revised on November 8, 2005 at http://www.hhs.gov/pandemicflu/plan/appendixf.html
- ^ Bardiya N, Bae J (2005). "Influenza vaccines: recent advances in production technologies". Appl Microbiol Biotechnol. 67 (3): 299–305. doi:10.1007/s00253-004-1874-1. PMID 15660212.
- ^ New York Times article ""Doubt Cast on Stockpile of a Vaccine for Bird Flu"" by Denise Grady. Published: March 30, 2006. Accessed 19 Oct 06
- ^ Wired News JVI
- ^ Department of Health & Human Services
- ^ NAID - 2004 News NAID - 2005 News
- ^ NPR
- ^ New England Journal of MedicineVolume 354:1411-1413 - March 30, 2006 - Number 13 - Vaccines against Avian Influenza — A Race against Time
- ^ CIDRAP News article WHO changes H5N1 strains for pandemic vaccines, raising concern over virus evolution published August 18, 2006
- ^ WHO (PDF) article Antigenic and genetic characteristics of H5N1 viruses and candidate H5N1 vaccine viruses developed for potential use as pre-pandemic vaccines published August 18, 2006
- ^ CIDRAP article HHS: Most H5N1 vaccine on hand is still potent published November 17, 2006
- ^ WHO article Global influenza surveillance
- ^ Keeping ahead of flu comes down to guessing game : Health and Fitness : Knoxville News Sentinel
- ^ Update: Influenza Activity -- United States and Worldwide, 2001-02 Season, and Composition of the 2002-03 Influenza Vaccine
- ^ WHO - Recommendations for Influenza Vaccine Composition: Southern hemisphere: 2003
- ^ Nature
- ^ a b c d e f g h CDC article Update: Influenza Activity — United States and Worldwide, 2003–04 Season, and Composition of the 2004–05 Influenza Vaccine published July 2, 2004
- ^ WHO website recommendation for the 2004 season
- ^ WHO — Recommended composition of influenza virus vaccines for use in the 2004 influenza season
- ^ WHO website recommendation for the 2005 season
- ^ WHO — Weekly epidemiological record — 8 October 2004, No. 41, 2004, 79, 369–376 (PDF)
- ^ Yahoo News Associated Press article CDC: Milder Than Normal Flu Season Ending published April 27, 2006
- ^ CDC - 2005-06 U.S. INFLUENZA SEASON SUMMARY
- ^ WHO website recommendation for the 2006 season
- ^ WHO — Weekly epidemiological record — 7 October 2005, No. 40, 2005, 80, 341–352 (PDF)
- ^ CDC fluwatch B/Victoria/2/87 lineage
- ^ 20 September 2006: WHO information meeting (Morning)
- ^ WHO website recommendation for 2007 season
- ^ WHO — Recommended composition of influenza virus vaccines for use in the 2007 influenza season — September 2006 (PDF)
- ^ 14 February 2007: WHO information meeting (Morning)
- ^ WHO website recommendation for 2007–2008 season.
- ^ WHO — Recommended composition of influenza virus vaccines for use in the 2007-2008 influenza season (PDF)
- ^ a b CDC News Conference on Influenza on February 8, 2008.
- ^ Flu Outbreak Widespread.
- ^ WHO website recommendation for 2008 season
- ^ WHO — Recommended composition of influenza virus vaccines for use in the 2008 influenza season (PDF)
- ^ 14 February 2008: Information meeting (Morning)
- ^ WHO website recommendation for 2008-2009 season
- ^ WHO — Recommended composition of influenza virus vaccines for use in the 2008–2009 influenza season (PDF)
- ^ a b CDC article "2008-2009 Influenza Season Week 21 ending May 30, 2009" published May 30, 2009
- ^ 20 September 2008: Information meeting (Morning)
- ^ WHO website recommendation for 2009 season
- ^ 12 February 2009: Information meeting (Morning)
- ^ WHO website recommendation for 2009-2010 season
- ^ WHO — Recommended composition of influenza virus vaccines for use in the 2009–2010 influenza season (PDF)
- ^ Influenza Report (online book) chapter Avian Influenza by Timm C. Harder and Ortrud Werner
- ^ equiflunet_vaccines
- ^ UAE Equestrian & Racing Federation
- ^ FEI guidelines
- ^ New York Times article Turning to Chickens in Fight With Bird Flu published May 2, 2006
- ^ SciDev.Net article Bird flu warning over partial protection of flocks published August 16, 2006
- ^ FAO Recommendations on the Prevention, Control and Eradication of Highly Pathogenic Avian Influenza (HPAI) in Asia http://www.fao.org/docs/eims/upload/246982/aj126e00.pdf
- ^ National Hog Farmer article Swine Flu Virus Turns Endemic published September 15, 2007
- ^ livestock.novartis.com Custom Vaccines: Swine
- ^ Karaca K, Dubovi E, Siger L, Robles A, Audonnet J, Jiansheng Y, Nordgren R, Minke J (2007). "Evaluation of the ability of canarypox-vectored equine influenza virus vaccines to induce humoral immune responses against canine influenza viruses in dogs". Am. J. Vet. Res. 68 (2): 208–12. doi:10.2460/ajvr.68.2.208. PMID 17269888.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Zhou; et al. (2010). "Computer-assisted Vaccine Design". Influenza: Molecular Virology. Caister Academic Press. ISBN 978-1-904455-57-8.
{{cite book}}: Explicit use of et al. in:|author=(help); Unknown parameter|ISBN-status=ignored (help)
External links
- Vaccine Research Center Information regarding preventative vaccine research studies
- About the flu jab (NHS Direct)
- World Health Organization's Initiative for Vaccine Research Influenza web page
- PandemicFlu.gov
- Influenza Strategies for Broad Global Access
- PATH's Vaccine Resource Library influenza resources
- Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 8985189, please use {{cite journal}} with
|pmid=8985189instead. - Influenza vaccination for health care workers: A duty of care
- CDC 2009 H1N1 Influenza Vaccine Supply Status
- CDC Vaccine Information Statement Inactivated Influenza Vaccine
- 2009-10 Swine Flu Vaccination Clinic Locations in Canada
- Read Congressional Research Service (CRS) Reports regarding Influenza and vaccines
- Influenza Research Database – Database of influenza genomic sequences and related information.
- Health-EU portal EU response to influenza
- European Commission - Public Health EU coordination on Pandemic (H1N1) 2009
