Asthma
| Asthma | |
|---|---|
| Specialty | Pulmonology, immunology |
Asthma is a common chronic inflammatory disease of the airways characterized by variable and recurring symptoms, airflow obstruction, and bronchospasm.[1] Symptoms include wheezing, cough, chest tightness, and shortness of breath.[2]
Medicines such as inhaled short-acting beta-2 agonists may be used to treat acute attacks.[3] Attacks can also be prevented by avoiding triggering factors such as allergens[4] or rapid temperature changes[5] and through drug treatment such as inhaled corticosteroids.[6] Leukotriene antagonists are less effective than corticosteroids, but have fewer side effects.[7] The monoclonal antibody omalizumab is sometimes effective.[8]
It affects 7% of the population of the United States,[9] 5% of British people,[10] and a total of 300 million worldwide.[11] [citation needed] Asthma causes 4,000 deaths per year in the United States[12] and 250,000 deaths per year worldwide.[13] Prognosis is good with treatment.
Although asthma is a chronic obstructive condition, it is not considered as a part of chronic obstructive pulmonary disease as this term refers specifically to combinations of bronchiectasis, chronic bronchitis, and emphysema. Unlike these diseases, the airway obstruction in asthma is usually reversible; however, if left untreated, asthma can result in chronic inflammation of the lungs and irreversible obstruction.[14] In contrast to emphysema, asthma affects the bronchi, not the alveoli.[15] Public attention in the developed world has increased recently because of its rapidly increasing prevalence, affecting up to one quarter of urban children.[16]
Classification
| Severity | Symptom frequency |
Nighttime symptoms |
%FEV1 of predicted |
FEV1 Variability |
|---|---|---|---|---|
| Intermittent | <1 per week | ≤2 per month | ≥80% | <20% |
| Mild persistent | >1 per week but <1 per day |
>2 per month | ≥80% | 20–30% |
| Moderate persistent | Daily | >1 per week | 60–80% | >30% |
| Severe persistent | Daily | Frequent | <60% | >30% |
Asthma is clinically classified according to the frequency of symptoms, forced expiratory volume in 1 second (FEV1), and peak expiratory flow rate.[17] Asthma may also be classified as atopic (extrinsic) or non-atopic (intrinsic), based on whether symptoms are precipitated by allergens (atopic) or not (non-atopic).[18]
Brittle asthma
Brittle asthma is a term used to describe two types of asthma, distinguishable by recurrent, severe attacks.[19] Type 1 brittle asthma refers to disease with wide peak flow variability, despite intense medication. Type 2 brittle asthma describes background well-controlled asthma, with sudden severe exacerbations.[19]
Signs and symptoms
Because of the spectrum of severity among asthma patients, some people with asthma only rarely experience symptoms, usually in response to triggers, where as other more severe cases may have marked airflow obstruction at all times.[20] Common symptoms of asthma include wheezing, shortness of breath, chest tightness and coughing. Symptoms are often worse at night or in the early morning, or in response to exercise or cold air.[21]
Asthma attack
| Near-fatal asthma | High PaCO2 and/or requiring mechanical ventilation | |
|---|---|---|
| Life threatening asthma | Any one of the following in a person with severe asthma:- | |
| Clinical signs | Measurements | |
| Altered conscious level | Peak flow < 33% | |
| Exhaustion | Oxygen saturation < 92% | |
| Arrhythmia | PaO2 < 8 kPa | |
| Low blood pressure | "Normal" PaCO2 | |
| Cyanosis | ||
| Silent chest | ||
| Poor respiratory effort | ||
| Acute severe asthma | Any one of:- | |
| Peak flow 33-50% | ||
| Respiratory rate ≥ 25 breaths per minute | ||
| Heart rate ≥ 110 beats per minute | ||
| Unable to complete sentences in one breath | ||
| Moderate asthma exacerbation | Worsening symptoms | |
| Peak flow > 50% best or predicted | ||
| No features of acute severe asthma | ||
An acute exacerbation of asthma is commonly referred to as an asthma attack. The cardinal symptoms of an attack are shortness of breath (dyspnea), wheezing, and chest tightness.[22] Although the former is often regarded as the primary symptom of asthma,[23] some people present primarily with coughing, and in the late stages of an attack, air motion may be so impaired that no wheezing is heard.[19] When present the cough may sometimes produce clear sputum. The onset may be sudden, with a sense of constriction in the chest, as breathing becomes difficult and wheezing occurs (primarily upon expiration, but sometimes in both respiratory phases). It is important to note inspiratory stridor without expiratory wheeze however, as an upper airway obstruction may manifest with symptoms similar to an acute exacerbation of asthma, with stridor instead of wheezing, and will remain unresponsive to bronchodilators.[23]
Signs of an asthmatic episode include wheezing, prolonged expiration, a rapid heart rate (tachycardia), and rhonchous lung sounds (audible through a stethoscope). The affected patient may also appear pale. During a serious asthma attack, the accessory muscles of respiration (sternocleidomastoid and scalene muscles of the neck) may be used, shown as in-drawing of tissues between the ribs and above the sternum and clavicles, and there may be the presence of a paradoxical pulse (a pulse that is weaker during inhalation and stronger during exhalation), and over-inflation of the chest.[citation needed]
During very severe attacks, an asthma sufferer's face and fingernails can turn blue from lack of oxygen, and can experience chest pain or even loss of consciousness. A patient's fingernails may also turn purple due to a lack, or low amount of oxygen circulating through the bloodstream. Just before loss of consciousness, there is a chance that the patient will feel numbness in the limbs and palms may start to sweat. The person's feet may become cold. Severe asthma attacks which are not responsive to standard treatments, called status asthmaticus, are life-threatening and may lead to respiratory arrest and death.[24]
Though symptoms may be very severe during an acute exacerbation, between attacks a patient may show few or even no signs of the disease.[25]
Cause
Asthma is caused by environmental and genetic factors.[26] These factors influence how severe asthma is and how well it responds to medication.[27] The interaction is complex and not fully understood.[28]
Environmental
Many environmental risk factors have been associated with asthma development and morbidity in children.
Environmental tobacco smoke, especially maternal cigarette smoking, is associated with high risk of asthma prevalence and asthma morbidity, wheeze, and respiratory infections.[29] Low air quality, from traffic pollution or high ozone levels,[30] has been repeatedly associated with increased asthma morbidity and has a suggested association with asthma development that needs further research.[31][32]
Recent studies show a relationship between exposure to air pollutants (e.g. from traffic) and childhood asthma.[33] This research finds that both the occurrence of the disease and exacerbation of childhood asthma are affected by outdoor air pollutants.
Viral respiratory infections are not only one of the leading triggers of an exacerbation but may increase one's risk of developing asthma.[34]
Psychological stress has long been suspected of being an asthma trigger, but only in recent decades has convincing scientific evidence substantiated this hypothesis. Rather than stress directly causing the asthma symptoms, it is thought that stress modulates the immune system to increase the magnitude of the airway inflammatory response to allergens and irritants.[31][35]
Antibiotic use early in life has been linked to development of asthma in several examples; it is thought that antibiotics make one susceptible to development of asthma because they modify gut flora, and thus the immune system (as described by the hygiene hypothesis).[36] The hygiene hypothesis (see below) is a hypothesis about the cause of asthma and other allergic disease, and is supported by epidemiologic data for asthma.[37] All of these things may negatively affect exposure to beneficial bacteria and other immune system modulators that are important during development, and thus may cause an increased risk for asthma and allergy.
Caesarean sections have been associated with asthma, possibly because of modifications to the immune system (as described by the hygiene hypothesis).[38]
Respiratory infections such as rhinovirus, Chlamydia pneumoniae and Bordetella pertussis are correlated with asthma exacerbations.[39][40]
Genetic
Over 100 genes have been associated with asthma in at least one genetic association study.[41] However, such studies must be repeated to ensure the findings are not due to chance. Through the end of 2005, 25 genes had been associated with asthma in six or more separate populations:[41]
Template:Multicol-break
Template:Multicol-break
Template:Multicol-break
Template:Multicol-break
Template:Multicol-end
Many of these genes are related to the immune system or to modulating inflammation. However, even among this list of highly replicated genes associated with asthma, the results have not been consistent among all of the populations that have been tested.[41] This indicates that these genes are not associated with asthma under every condition, and that researchers need to do further investigation to figure out the complex interactions that cause asthma. One theory is that asthma is a collection of several diseases, and that genes might have a role in only subsets of asthma.[citation needed] For example, one group of genetic differences (single nucleotide polymorphisms in 17q21) was associated with asthma that develops in childhood.[42]
Gene–environment interactions
| Endotoxin levels | CC genotype | TT genotype |
|---|---|---|
| High exposure | Low risk | High risk |
| Low exposure | High risk | Low risk |
Research suggests that some genetic variants may only cause asthma when they are combined with specific environmental exposures, and otherwise may not be risk factors for asthma.[26]
The genetic trait, CD14 single nucleotide polymorphism (SNP) C-159T and exposure to endotoxin (a bacterial product) are a well-replicated example of a gene-environment interaction that is associated with asthma. Endotoxin exposure varies from person to person and can come from several environmental sources, including environmental tobacco smoke, dogs, and farms. Researchers have found that risk for asthma changes based on a person’s genotype at CD14 C-159T and level of endotoxin exposure.[43][better source needed]
Exacerbation
Some individuals will have stable asthma for weeks or months and then suddenly develop an episode of acute asthma. Different asthmatic individuals react differently to various factors.[citation needed] However, most individuals can develop severe exacerbation of asthma from several triggering agents.[44]
Home factors that can lead to exacerbation include dust, house mites, animal dander (especially cat and dog hair), cockroach allergens and molds at any given home. Perfumes are a common cause of acute attacks in females and children. Both virus and bacterial infections of the upper respiratory tract infection can worsen asthma.[citation needed]
Risk factors
Studying the prevalence of asthma and related diseases such as eczema and hay fever have yielded important clues about some key risk factors. The strongest risk factor for developing asthma is a history of atopic disease;[34] this increases one's risk of hay fever by up to 5x and the risk of asthma by 3-4x.[45][failed verification] In children between the ages of 3-14, a positive skin test for allergies and an increase in immunoglobulin E increases the chance of having asthma.[46] In adults, the more allergens one reacts positively to in a skin test, the higher the odds of having asthma.[47]
Because much allergic asthma is associated with sensitivity to indoor allergens and because Western styles of housing favor greater exposure to indoor allergens, much attention has focused on increased exposure to these allergens in infancy and early childhood as a primary cause of the rise in asthma.[48][49][full citation needed] Primary prevention studies aimed at the aggressive reduction of airborne allergens in a home with infants have shown mixed findings. Strict reduction of dust mite allergens, for example, reduces the risk of allergic sensitization to dust mites, and modestly reduces the risk of developing asthma up until the age of 8 years old.[50][51][52][53] However, studies also showed that the effects of exposure to cat and dog allergens worked in the converse fashion; exposure during the first year of life was found to reduce the risk of allergic sensitization and of developing asthma later in life.[54][55][56][failed verification]
The inconsistency of this data has inspired research into other facets of Western society and their impact upon the prevalence of asthma. One subject that appears to show a strong correlation is the development of asthma and obesity. In the United Kingdom and United States, the rise in asthma prevalence has echoed an almost epidemic rise in the prevalence of obesity.[57][58][failed verification] In Taiwan, symptoms of allergies and airway hyper-reactivity increased in correlation with each 20% increase in body-mass index.[59][failed verification]
Hygiene hypothesis
One theory for the cause of the increase in asthma prevalence worldwide is the so-called "hygiene hypothesis"—that the rise in the prevalence of allergies and asthma is a direct and unintended result of the success of modern hygienic practices in preventing childhood infections.[60] Children living in less hygienic environments (East Germany vs. West Germany,[61] families with many children,[62][63][64] day care environments[65]) tend to have lower incidences of asthma and allergic diseases. This seems to run counter to the logic that viruses are often causative agents in exacerbation of asthma.[66][67][68] Additionally, other studies have shown that viral infections of the lower airway may in some cases induce asthma, as a history of bronchiolitis or croup in early childhood is a predictor of asthma risk in later life.[69] Studies which show that upper respiratory tract infections are protective against asthma risk also tend to show that lower respiratory tract infections conversely tend to increase the risk of asthma.[70]
Population disparities
Asthma prevalence in the US is higher than in most other countries in the world, but varies drastically between diverse US populations.[31] In the US, asthma prevalence is highest in Puerto Ricans, African Americans, Filipinos, Irish Americans, and Native Hawaiians, and lowest in Mexicans and Koreans.[71][72][73] Mortality rates follow similar trends, and response to Salbutamol is lower in Puerto Ricans than in African Americans or Mexicans.[74][75] As with worldwide asthma disparities, differences in asthma prevalence, mortality, and drug response in the US may be explained by differences in genetic, social and environmental risk factors.
Asthma prevalence also differs between populations of the same ethnicity who are born and live in different places.[76] US-born Mexican populations, for example, have higher asthma rates than non-US born Mexican populations that are living in the US.[77]
Asthma prevalence and asthma deaths also differ by gender. Males are more likely to be diagnosed with asthma as children, but asthma is more likely to persist into adulthood in females.[78][better source needed] Women account for nearly 65% of all asthma related deaths.[79] This difference may be attributable to hormonal differences, among other things. In support of this, girls who reach puberty before age 12 were found to have a later diagnosis of asthma more than twice as much as girls who reach puberty after age 12.[citation needed] Asthma is also the number one cause of missed days from school.[citation needed]
Socioeconomic factors
The incidence of asthma is highest among low-income populations both nationally and worldwide.[citation needed] Asthma deaths are most common in low and middle income countries[80]), and in the Western world, it is found in those low-income neighborhoods whose populations consist of large percentages of ethnic minorities[81].[failed verification] Additionally, asthma has been strongly associated with the presence of cockroaches in living quarters; these insects are more likely to be found in those same neighborhoods.[82]
Most likely due to income and geography, the incidence of and treatment quality for asthma varies among different racial groups.[citation needed] For example, African Americans are less likely to receive outpatient treatment for asthma despite their higher prevalence of the disease. They are much more likely to require an emergency room visit or hospitalization for their asthma symptoms which is probably a contributing factor to their higher likelihood as a race of dying from an asthma attack compared to whites. The prevalence of "severe persistent" asthma is also greater in low-income communities than those with better access to treatment.[83][failed verification][84][dead link] It is important that parents, particularly those of relatively low socioeconomic status, educate themselves as much as possible about asthma since their families are more vulnerable to persistent asthma, especially their children. For this reason, more health organizations are helping to inform and educate low-income families in their fight against asthma.[citation needed]
Socioeconomic factors and poor living situations exacerbate the likelihood of developing asthma, but an over-arching factor worth mentioning is environmental racism. Asthma has been shown to be disproportionally distributed among population groups. It has been reported that there is a direct relationship between asthma levels and both income and ethnicity. [85][failed verification] The, “asthma epidemic,” as termed by Robert D. Bullard, has never been as bad and widespread as it is now. “The number of asthma sufferers doubled from 6.7 million in 1980 to 17.3 million in 1998.” This spike in the frequency of asthmatic individuals is likely to be directly correlated with the population growth over the years and the resulting increase in air pollution.[citation needed] Environmental injustice can be seen when polluting factories or industries are purposefully sited closer to communities with higher-than-average minority and/or low-income populations. The proximity of toxic facilities, often ones that are poorly designed or regulated, has severe effects on the health of the nearby population. “African Americans and Latino are almost three times more likely than whites to die from asthma” as a result of often being the targets of the siting of dumps, factories, etc.[86][failed verification]
Athletics
Asthma appears to be more prevalent in athletes than in the general population. One survey of participants in the 1996 Summer Olympic Games, in Atlanta, Georgia, U.S., showed that 15% had been diagnosed with asthma, and that 10% were on asthma medication.[87]
There appears to be a relatively high incidence of asthma in sports such as cycling, mountain biking, and long-distance running, and a relatively lower incidence in weightlifting and diving. It is unclear how much of these disparities are from the effects of training in the sport.[87][88]
Occupation
Asthma as a result of (or worsened by) workplace exposures is the world's most commonly reported occupational respiratory disease.[citation needed] Still most cases of occupational asthma are not reported or are not recognized as such. Estimates by the American Thoracic Society (2004) suggest that 15–23% of new-onset asthma cases in adults are work related.[89] In one study monitoring workplace asthma by occupation, the highest percentage of cases occurred among operators, fabricators, and laborers (32.9%), followed by managerial and professional specialists (20.2%), and in technical, sales, and administrative support jobs (19.2%). Most cases were associated with the manufacturing (41.4%) and services (34.2%) industries.[89] Animal proteins, enzymes, flour, natural rubber latex, and certain reactive chemicals are commonly associated with work-related asthma. When recognized, these hazards can be mitigated, dropping the risk of disease.[90]
Pathophysiology
This section needs additional citations for verification. (May 2010) |

Asthma is an airway disease that can be classified physiologically as a variable and partially reversible obstruction to air flow, and pathologically with overdeveloped mucus glands, airway thickening due to scarring and inflammation, and bronchoconstriction, the narrowing of the airways in the lungs due to the tightening of surrounding smooth muscle. Bronchial inflammation also causes narrowing due to edema and swelling caused by an immune response to allergens.
Diagnosis
Asthma is defined simply as reversible airway obstruction. Reversibility occurs either spontaneously or with treatment. The basic measurement is peak flow rates and the following diagnostic criteria are used by the British Thoracic Society:[91][failed verification]
- ≥20% difference on at least three days in a week for at least two weeks;
- ≥20% improvement of peak flow following treatment, for example:
- 10 minutes of inhaled β-agonist (e.g., salbutamol);
- six weeks of inhaled corticosteroid (e.g., beclometasone);
- 14 days of 30 mg prednisolone.
- ≥20% decrease in peak flow following exposure to a trigger (e.g., exercise).
In many cases, asthma is diagnosed via typical symptoms and signs. Asthma is strongly suspected if a person suffers from eczema or other allergic conditions—suggesting a general atopic constitution—or has a family history of asthma. While measurement of airway function is possible for adults, most new cases are diagnosed in children who are unable to perform such tests.[citation needed]
In children, the key to asthma diagnosis is the sound of wheezing or a high-pitched sound upon exhalation. Other clues are recurrent wheezing, breathing difficulty, or chest tightness, or a history of coughing that is worse at night. The doctor should also know if the child's symptoms are worse with exercise, colds,or exposure to certain irritants such as smoke, emotional stress, or changes in the weather.[92]
Other information important to diagnosis is the age at which symptoms began and how they progressed, the timing and pattern of wheezing, when and how often a child had to visit a clinic or hospital emergency department because of symptoms, whether the child ever took bronchodilator medication for the symptoms and the nature of the response to medication.[92]
Although pediatricians may tend to ask parents for information about their children's symptoms, studies suggest that children themselves are reliable sources as early as age 7 and perhaps even as early as age 6.[93]
In adults and older children, diagnosis can be made with spirometry or a peak flow meter (which tests airway restriction), looking at both the diurnal variation and any reversibility following inhaled bronchodilator medication. The latest guidelines from the U.S. National Asthma Education and Prevention Program (NAEPP) recommend spirometry at the time of initial diagnosis, after treatment is initiated and symptoms are stabilized, whenever control of symptoms deteriorates, and every 1 or 2 years on a regular basis.[94]
The NAEPP guidelines do not recommend testing peak expiratory flow as a regular screening method because it is more variable than spirometry. However, testing peak flow at rest (or baseline) and after exercise can be helpful, especially in young patients who may experience only exercise-induced asthma. It may also be useful for daily self-monitoring and for checking the effects of new medications.[94] Peak flow readings can be charted on graph paper charts together with a record of symptoms or use peak flow charting software. This allows patients to track their peak flow readings and pass information back to their doctor or nurse.[95]
In the Emergency Department, doctors may use a capnography which measures the amount of exhaled carbon dioxide,[96][failed verification] along with pulse oximetry which shows the percentage of hemoglobin that is carrying oxygen, to determine the severity of an asthma attack as well as the response to treatment.
More recently, exhaled nitric oxide has been studied as a breath test indicative of airway inflammation in asthma.[citation needed]
Differential diagnosis
Before diagnosing asthma, alternative possibilities should be considered such as the use of known bronchoconstrictors (substances that cause narrowing of the airways, e.g. certain anti-inflammatory agents or beta-blockers). Among elderly people, the presenting symptom may be fatigue, cough, or difficulty breathing, all of which may be erroneously attributed to Chronic obstructive pulmonary disease(COPD), congestive heart failure, or simple aging.[97]
Chronic obstructive pulmonary disease closely resembles asthma, is correlated with more exposure to cigarette smoke, an older age, less symptom reversibility after bronchodilator administration (as measured by spirometry), and decreased likelihood of family history of atopy.[98][citation needed]
Pulmonary aspiration, whether direct due to dysphagia (swallowing disorder) or indirect (due to acid reflux), can show similar symptoms to asthma. However, with aspiration, fevers might also indicate aspiration pneumonia. Direct aspiration (dysphagia) can be diagnosed by performing a modified barium swallow test. If the aspiration is indirect (from acid reflux), then treatment is directed at this is indicated.[citation needed]
Prevention
This section needs additional citations for verification. (April 2010) |

Prevention of the development of asthma is different from prevention of asthma episodes. Aggressive treatment of mild allergy with immunotherapy has been shown to reduce the likelihood of asthma development. In controlling symptoms, the first step is establishing a plan of action to prevent episodes of asthma by avoiding triggers and allergens, regularly testing for lung function, and using preventive medications. http://www.nhlbi.nih.gov/guidelines/asthma/asthgdln.htm
Current treatment protocols recommend controller medications such as an inhaled corticosteroid, which helps to suppress inflammation and reduces the swelling of the lining of the airways, in anyone who has frequent (greater than twice a week) need of relievers or who has severe symptoms. If symptoms persist, additional controller drugs are added until almost all asthma symptoms are prevented. With the proper use of control drugs, patients with asthma can avoid the complications that result from overuse of rescue medications.
Patients with asthma sometimes stop taking their controller medication when they feel fine and have no problems breathing. This often results in further attacks after a time, and no long-term improvement.
The only preventive agent known is allergen immunotherapy. Controller medications include the following:
- Inhaled glucocorticoids such as beclomethasone are the most widely used prevention medications and normally come as inhalers. Side effects, while they may occur are generally not seen with the inhaled steroids when used in conventional doses for control of asthma due to the smaller dose which is targeted to the lungs, unlike the higher doses of oral or injected preparations. Deposition of steroids in the mouth may result in oral thrush. Deposition near the vocal cords can cause hoarse voice. These may be minimised by rinsing the mouth with water after inhaler use, as well as by using a spacer. Spacers also generally increase the amount of drug that reaches the lungs.
- Leukotriene modifiers such as montelukast provide both anti-spasm and anti-inflammatory effects. They are less effective than inhaled corticosteroids, but do not have any steroid related side-effects and the benefit is additive with inhaled steroid.
- Mast cell stabilizers such as (cromoglicate (cromolyn), and nedocromil). These medications are believed to prevent the initiation of the allergy reaction, by stabilizing the mast cell. They are not effective once the reaction has already begun, and typically must be used 4 times a day for maximal effect. But they do truly prevent asthma symptoms and are nearly free of side-effects.
- Antimuscarinics/anticholinergics (ipratropium, oxitropium, and tiotropium). These agents both relieve spasm and reduce formation of mucous. They are more effective in patients with empysema or 'smokers lung.' They are rarely effective in asthma and are not true asthma controller medications.
- Methylxanthines (theophylline and aminophylline). These agents are bronchodilators with minimal anti-inflammatory effect. At one time they were the only effective asthma medications available. They are sometimes considered if sufficient control cannot be achieved with inhaled glucocorticoid, leukotriene modifier, and long-acting β-agonist combinations.
- Antihistamines are often used to treat the nasal allergies which can accompany asthma. Older agents are too drying and can result in thick mucous so should be avoided. Newer antihistamines which do not have this effect can safely be used by patients with asthma.[verification needed]
- Allergy Desensitization, also known as allergy immunotherapy, may be recommended in some cases where allergy is the suspected cause or trigger of asthma. Allergy shots are dangerous in severe asthma and in uncontrolled asthma. However if allergy immunotherapy is started early in the disease there is a good chance that a remission of asthma can be induced (aka "asthma cure"). Typically the need for medication is reduced by about half with injection allergy immunotherapy, when done correctly. If a patient is only allergic to one or two items, oral allergy immunotherapy can be used. This is safe, much easier in young children, and is about half as effective. Unfortunately if a patient is allergic to more than 2 or 3 items then oral therapy cannot be given in a dose which is proven safe and effective.
Trigger avoidance
As is common with respiratory disease, smoking is believed to adversely affect patients in several ways, including increasing the severity of symptoms (likely due to increased inflammation[99][better source needed]), a more rapid decline of lung function, and decreased response to preventive medications.[100] Automobile emissions are considered an even more significant cause and aggravating factor.[citation needed] Patients with asthma who smoke or who live near traffic[citation needed] typically require additional medications to help control their disease. Furthermore, exposure of both non-smokers and smokers to second-hand smoke is detrimental, resulting in more severe asthma, more emergency room visits, and more asthma-related hospital admissions, but the effect of woodstove and gas stove fumes is uncertain.[101][citation needed] Smoking cessation and avoidance of second-hand smoke is strongly encouraged in people who have asthma.[102] Air filters and room air cleaners may help prevent some asthma symptoms.[103] Ozone is also considered as a major factor in increasing asthma.[104] The report by the National Heart, Lung and Blood Institute [105] supports the idea of an asthma management plan that includes the avoidance of as many allergens as possible to which the individual is sensitive. This report, and others [106][107] also agree that no one single approach is sufficient to reduce allergens; a multifactorial approach is required. The Asthma and Allergy Friendly Certification Program that is operated in the USA by the Asthma and Allergy Foundation of America and in Canada by the Asthma Society of Canada [2] is based on this multifactorial approach to trigger control.[citation needed]
For those in whom exercise can trigger an asthma attack (exercise-induced asthma), higher levels of ventilation and cold, dry air tend to exacerbate attacks.[citation needed] For this reason, activities in which a patient breathes large amounts of cold air, such as skiing and running, tend to be worse for people with asthma, whereas swimming in an indoor, heated pool with warm, humid air is less likely to provoke a response.[23]
Alternative medicine
Evidence is insufficient to support the usage of Vitamin C in people with asthma.[108]
Guaifenesin is an effective and common chest decongestant that works by thinning mucus and lubricating the airway.
Magnesium may relax respiratory muscles in asthmatics. Avoidance of known food triggers may help curb attacks by preventing hyper-secretion of mucus in the airway.
Management
A specific, customized plan for proactively monitoring and managing symptoms should be created. Someone who has asthma should understand the importance of reducing exposure to allergens, testing to assess the severity of symptoms, and the usage of medications. The treatment plan should be written down and adjusted according to changes in symptoms.[109]
The most effective treatment for asthma is identifying triggers, such as cigarette smoke, pets, or aspirin, and eliminating exposure to them.[citation needed] If trigger avoidance is insufficient, medical treatment is recommended. Medical treatments used depends on the severity of illness and the frequency of symptoms. Specific medications for asthma are broadly classified in to fast acting and long acting.[110][111]
Bronchodilators are recommended for short-term relief of symptoms. For occasional attacks, no other medication is needed. If mild persistent disease is present (more than two attacks a week), low-dose inhaled glucocorticoids or alternatively, an oral leukotriene modifier or a mast-cell stabilizer. For those who suffer daily attacks, a higher dose of glucocorticoid is used. In a severe asthma exacerbation, oral glucocorticoids are added to these treatments.[citation needed]
Medications

Medications used to treat asthma are divided into two general classes: quick-relief medications used to treat acute symptoms and long-term control medications used to prevent further exacerbation.[112]
- Fast acting
- Short-acting, selective beta2-adrenoceptor agonists, such as salbutamol (albuterol USAN), levalbuterol, terbutaline and bitolterol.[citation needed]
Tremors, the major side effect, have been greatly reduced by inhaled delivery, which allows the drug to target the lungs specifically; oral and injected medications are delivered throughout the body. There may also be cardiac side effects at higher doses (due to Beta-1 agonist activity), such as elevated heart rate or blood pressure. However, levalbuterol has been shown to have fewer cardiac side effects and significantly more anti-inflammatory effects on bronchial smooth muscle than its racemic counterpart albuterol. The question becomes does this justify its 5-10 fold higher cost. Some hospitals start a patient on levalbuterol until symptoms wane and then switch to albuterol. Patients must be cautioned against using these medicines too frequently, as with such use their efficacy may decline, producing desensitization resulting in an exacerbation of symptoms which may lead to refractory asthma and death.[citation needed] - Older, less selective adrenergic agonists, such as inhaled epinephrine and ephedrine tablets, have also been used; the brand Primatene Mist, for example. Cardiac side effects occur with these agents at either similar or lesser rates to albuterol.[113] [114] When used solely as a relief medication, inhaled epinephrine has been shown to be an effective agent to terminate an acute asthmatic exacerbation.[113][better source needed] In emergencies, these drugs were sometimes administered by injection. Their use via injection has declined due to related adverse effects.[citation needed]
- Anticholinergic medications, such as ipratropium bromide may be used instead.[citation needed] They have no cardiac side effects and thus can be used in patients with heart disease; however, they take up to an hour to achieve their full effect and are not as powerful as the β2-adrenoreceptor agonists.[citation needed]
- Long term control
- Inhaled glucocorticoids are mainly considered as preventive medications while oral glucocorticoids are often used to supplement treatment of emergent moderate to severe attacks.[115] They should be used twice daily in children with mild to moderate persistent asthma.[116][better source needed] A randomized controlled trial has demonstrated the benefit of 250 microg beclomethasone when taken as an as-needed combination inhaler with 100 microg of albuterol.[117][better source needed]
- Long-acting β2-agonists (LABD) are similar in structure to short-acting selective beta2-adrenoceptor agonists, but have much longer side chains resulting in a 12-hour effect.[citation needed] While people report improved symptom control, these drugs do not replace the need for routine preventers, and their slow onset means the short-acting dilators are still be required. In November 2005, the American FDA released a health advisory alerting the public to findings that show the use of long-acting β2-agonists could lead to a worsening of symptoms, and in some cases death.[118][dead link] In December 2008, members of the FDA's drug-safety office recommended withdrawing approval for these medications in children. Discussion is ongoing about their use in adults.[119] A recent meta-analysis of long-acting beta-agonists indicate a danger in asthma with an 2—4 fold increased risk for asthma hospitalizations and asthma deaths compared with placebo.[120]
Medications are typically provided as metered-dose inhalers (MDIs) in combination with an asthma spacer or as a dry powder inhaler. The spacer is a plastic cylinder that mixes the medication with air, making it easier to receive a full dose of the drug. A nebulizer may also be used. There is no clear evidence, however, that they are more effective than inhalers used with a spacer.
Acute exacerbation
Acute exacerbation of asthma is generally referred to as an acute asthmatic attack. When an acute asthma attack is present, symptoms are quite dramatic and this is an emergent condition. In an instant, the individual can have breathing difficulties and even lose consciousness.[121][citation needed]
When an asthma attack is unresponsive to a patient's usual medication, other treatment options available for emergency management include:[122]
- Oxygen to alleviate the hypoxia that results from extreme asthma attacks (but not the asthma attack itself).
- Nebulized salbutamol or terbutaline (short-acting beta-2-agonists), often combined with ipratropium (an anticholinergic).
- Systemic steroids, oral or intravenous (prednisone, prednisolone, methylprednisolone, dexamethasone, or hydrocortisone). Some research has looked into an alternative inhaled route.[123][better source needed] A non tapered 5 - 10 day course seems to be sufficient.[124]
- Other bronchodilators that are occasionally effective when the usual drugs fail:[citation needed]
- Intravenous salbutamol
- Nonspecific beta-agonists, injected or inhaled (epinephrine, isoetharine, isoproterenol, metaproterenol)
- Anticholinergics, IV or nebulized, with systemic effects (glycopyrrolate, atropine, ipratropium)
- Methylxanthines (theophylline, aminophylline)
- Inhalation anesthetics that have a bronchodilatory effect (isoflurane, halothane, enflurane)
- The dissociative anaesthetic ketamine, often used in endotracheal tube induction
- Magnesium sulfate intravenous treatment has been shown to provide a bronchodilating effect when used in addition to other treatment in severe acute asthma attacks.[125][126]
- Intubation and mechanical ventilation, for patients in or approaching respiratory arrest.
- Heliox, a mixture of helium and oxygen, may be used in a hospital setting. It has a more laminar flow than ambient air and moves more easily through constricted airways.
Complementary medicine
Many asthma patients, like those who suffer from other chronic disorders, use alternative treatments; surveys show that roughly 50% of asthma patients use some form of unconventional therapy.[127][needs update][128] There is little data to support the effectiveness of most of these therapies. The Buteyko breathing technique for controlling hyperventilation may result in a reduction in medications used however does not have any effect on lung function.[129]
A Cochrane review of acupuncture for asthma found no evidence of efficacy.[130] A similar review of air ionisers found no evidence that they improve asthma symptoms or benefit lung function; this applied equally to positive and negative ion generators.[131] Another study reviewed a range of dust mite control measures, including air filtration, chemicals to kill mites, vacuuming, mattress covers and others. Overall these methods had no effect on asthma symptoms.[132] However, a review of 30 studies found that "bedding encasement might be an effective asthma treatment under some conditions" (when the patient is highly allergic to dust mite and the intervention reduces the dust mite exposure level from high levels to low levels). [133]
A study of "manual therapies" for asthma, including osteopathic, chiropractic, physiotherapeutic and respiratory therapeutic manoeuvres, found there is insufficient evidence to support or refute their use in treating asthma;[134] these manoeuvers include various osteopathic and chiropractic techniques to "increase movement in the rib cage and the spine to try and improve the working of the lungs and circulation"; chest tapping, shaking, vibration, and the use of "postures to help shift and cough up phlegm." One meta-analysis found that homeopathy may have a potentially mild benefit in reducing the intensity of symptoms.[135] However, the number of patients involved in the analysis was small, and subsequent studies have not supported this finding.[136]
Prognosis
The prognosis for asthma is good, especially for children with mild disease.[92][failed verification] Of asthma diagnosed during childhood, 54% of cases will no longer carry the diagnosis after a decade.[citation needed] The extent of permanent lung damage in people with asthma is unclear. Airway remodeling is observed, but it is unknown whether these represent harmful or beneficial changes.[137] Although conclusions from studies are mixed, most studies show that early treatment with glucocorticoids prevents or ameliorates decline in lung function as measured by several parameters.[138] For those who continue to suffer from mild symptoms, corticosteroids can help most to live their lives with few disabilities. It is more likely to consider immediate medication of inhaled corticosteroids as soon as asthma attacks occur. According to studies conducted, patients with relatively mild asthma who have received inhaled corticosteroids within 12 months of their first asthma symptoms achieved good functional control of asthma after 10 years of individualized therapy as compared to patients who received this medication after 2 years (or more) from their first attacks.[citation needed] Though they (delayed) also had good functional control of asthma,they were observed to exhibited slightly less optimal disease control and more signs of airway inflammation.[citation needed]
Asthma mortality has decreased over the last few decades due to better recognition and improvement in care.[139]
Epidemiology

Rates of asthma have increased significantly between the 1960s and 2008.[141][142] Some 9% of US children had asthma in 2001, compared with just 3.6% in 1980. The World Health Organization (WHO) reports that some 10% of the Swiss population suffers from asthma today,[143] compared with just 2% some 25–30 years ago.
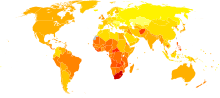
A 1998 study of asthma prevalence worldwide found great disparities (as high as a 20 to 60-fold difference) in asthma across the world, with a trend toward more developed and westernized countries having higher rates of asthma.[144] Westernization however does not explain the entire difference in asthma prevalence between countries, and the disparities may also be affected by differences in genetic, social and environmental risk factors.[31] Mortality however is most common in low to middle income countries,[145] well symptoms were most prevalent (as much as 20%) in the United Kingdom, Australia, New Zealand, and Republic of Ireland; they were lowest (as low as 2–3%) in Eastern Europe, Indonesia, Greece, Uzbekistan, India, and Ethiopia.[144][needs update]
While asthma is more common in affluent countries, it is by no means a restricted problem; the WHO estimate that there are between 15 and 20 million people with asthma in India.[citation needed] In the U.S., urban residents, Hispanics, and African Americans are affected more than the population as a whole.[citation needed] Striking increases in asthma prevalence have been observed in populations migrating from a rural environment to an urban one,[146][needs update] or from a third-world country to Westernized one.[147][needs update]
In 2005 in the United States asthma affected more than 22 million people including 6 million children.[148] It accounted for nearly 1/2 million hospitalizations,[148] and 14 million missed days of school annually.[citation needed] More boys have asthma than girls, but more women have it than men.[149] Of all children, African Americans and Latinos who live in cities are more at risk for developing asthma.[citation needed] African American children in the U.S. are four times more likely to die of asthma and three times more likely to be hospitalized, compared to their white counterparts.[citation needed] In some Latino neighborhoods, as many as one in three children has been found to have asthma.[150]
In England, an estimated 261,400 people were newly diagnosed with asthma in 2005; 5.7 million people had an asthma diagnosis and were prescribed 32.6 million asthma-related prescriptions.[151]
History
Asthma was first recognized and named by Hippocrates circa 450 BC. During the 1930s–50s, asthma was considered as being one of the 'holy seven' psychosomatic illnesses. Its aetiology was considered to be psychological, with treatment often based on psychoanalysis and other 'talking cures'.[152]
As these psychoanalysts interpreted the asthmatic wheeze as the suppressed cry of the child for its mother, so they considered that the treatment of depression was especially important for individuals with asthma.[152]
Research
Desensitization has been suggested as a potential treatment.[153]
References
- ^ NHLBI 2007 p.11—12
- ^ BTS 2009 p.3
- ^ NHLBI 2007 p.214
- ^ NHLBI 2007 p.169–172
- ^ Koskela HO (2007). "Cold air-provoked respiratory symptoms: the mechanisms and management". International Journal of Circumpolar Health. 66 (2): 91–100. PMID 17515249.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ GINA 2009 p.69
- ^ NHLBI p.228
- ^ BTS 2009 p.42
- ^ "Asthma: Lung and Airway Disorders: Merck Manual Home Edition".
- ^ Anderson, HR (2007). "50 years of asthma: UK trends from 1955 to 2004" (PDF). Thorax. 62 (1): 85–90. PMID 17189533.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|month=ignored (help) - ^ Fanta CH (2009). "Asthma". N. Engl. J. Med. 360 (10): 1002–14. doi:10.1056/NEJMra0804579. PMID 19264689.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Getahun D, Demissie K, Rhoads GG (2005). "Recent trends in asthma hospitalization and mortality in the United States". J Asthma. 42 (5): 373–8.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ GINA 2009 p.2
- ^ Delacourt, C (2004). "Bronchial changes in untreated asthma". Archives de Pédiatrie. 11 (Suppl. 2): 71s–73s. PMID 15301800.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ George Schiffman, MD, FCCP (2009-12-18). "Chronic Obstructive Pulmonary Disease / COPD". MedicineNet/WebMD. Retrieved 27 January 2010.
{{cite web}}: CS1 maint: multiple names: authors list (link) - ^ Lilly CM (2005). "Diversity of asthma: evolving concepts of pathophysiology and lessons from genetics". J. Allergy Clin. Immunol. 115 (4 Suppl): S526–31. doi:10.1016/j.jaci.2005.01.028. PMID 15806035.
- ^ a b Yawn, BP (2008). "Factors accounting for asthma variability: achieving optimal symptom control for individual patients" (PDF). Primary Care Respiratory Journal. 17 (3): 138–147. doi:10.3132/pcrj.2008.00004. PMID 18264646.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Kumar, Vinay (2010). Robbins and Cotran Pathologic Basis of Disease (8th ed.). Saunders. p. 688. ISBN 9781416031215.
{{cite book}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ a b c d BTS 2009 p.54
- ^ GINA 2009 p.8–9
- ^ BTS 2009 p.12
- ^ Saunders (2005). "Asthma". Mason: Murray & Nadel's Textbook of Respiratory Medicine (Homer A. Boushey Jr. M.D. David B. Corry M.D. John V. Fahy M.D. Esteban G. Burchard M.D. Prescott G. Woodruff M.D. et al. (eds)) (4th ed.). Elsevier.
- ^ a b c Barnes PJ (2008). "Asthma". Harrison's Principles of Internal Medicine (Fauci AS, Braunwald E, Kasper DL, et al. (eds)) (17th ed.). New York: McGraw-Hill. pp. 1596–1607.
- ^ Werner, HA (2001). "Status asthmaticus in children: a review". Chest. 119 (6): 1596–1607. PMID 11399724.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Longmore, Murray; et al. (2007). Oxford Handbook of Clinical Medicine (7 ed.). Oxford University Press. ISBN 978-0198568377.
{{cite book}}: Explicit use of et al. in:|first=(help) - ^ a b Martinez FD (2007). "Genes, environments, development and asthma: a reappraisal". Eur Respir J. 29 (1): 179–84. doi:10.1183/09031936.00087906. PMID 17197483.
- ^ Choudhry S, Seibold MA, Borrell LN; et al. (2007). "Dissecting complex diseases in complex populations: asthma in latino americans". Proc Am Thorac Soc. 4 (3): 226–33. doi:10.1513/pats.200701-029AW. PMC 2647623. PMID 17607004.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Miller, RL (2008). "Environmental epigenetics and asthma: current concepts and call for studies". American Journal of Respiratory and Critical Care Medicine. 177 (6): 567–573. PMID 18187692.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|month=ignored (help) - ^ GINA 2009. p.6
- ^ GINA 2009. p.56
- ^ a b c d Gold DR,Wright R; Wright, R (2005). "Population disparities in asthma". Annu Rev Public Health. 26: 89–113. doi:10.1146/annurev.publhealth.26.021304.144528. PMID 15760282.
- ^ "California Children's Health Study".
- ^ M Salam et al., "Recent evidence for adverse effects of residential proximity to traffic sources on asthma", Current Opinion Pulmonary Medicine, 2008, Vol. 14, Issue 1
- ^ a b NHLBI 2007. p.11
- ^ Chen E, Miller GE (2007). "Stress and inflammation in exacerbations of asthma". Brain Behav Immun. 21 (8): 993–9. doi:10.1016/j.bbi.2007.03.009. PMC 2077080. PMID 17493786.
- ^ Droste, JH (2000). "Does the use of antibiotics in early childhood increase the risk of asthma and allergic disease?". Clinical and Experimental Allergy. 30 (11): 1547–1553. PMID 11069562.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|month=ignored (help) - ^ Bufford, JD (2005). "The hygiene hypothesis revisited". Immunology and Allergy Clinics of North America. 25 (2): 247–262. PMID 15878454.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|month=ignored (help) - ^ BTS 2009 p.72
- ^ Harju TH, Leinonen M, Nokso-Koivisto J; et al. (2006). "Pathogenic bacteria and viruses in induced sputum or pharyngeal secretions of adults with stable asthma". Thorax. 61 (7): 579–84. doi:10.1136/thx.2005.056291. PMC 2104650. PMID 16517571.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Richeldi L, Ferrara G, Fabbri LM, Lasserson TJ, Gibson PG (2005). "Macrolides for chronic asthma". Cochrane Database Syst Rev (4): CD002997. doi:10.1002/14651858.CD002997.pub3. PMID 16235309.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ a b c Ober C,Hoffjan S; Hoffjan, S (2006). "Asthma genetics 2006: the long and winding road to gene discovery". Genes Immun. 7 (2): 95–100. doi:10.1038/sj.gene.6364284. PMID 16395390.
- ^ Bouzigon E, Corda E, Aschard H; et al. (2008). "Effect of 17q21 Variants and Smoking Exposure in Early-Onset Asthma". The New England journal of medicine. 359 (19): 1985. doi:10.1056/NEJMoa0806604. PMID 18923164.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ a b Martinez FD (2007). "CD14, endotoxin, and asthma risk: actions and interactions". Proc Am Thorac Soc. 4 (3): 221–5. doi:10.1513/pats.200702-035AW. PMC 2647622. PMID 17607003.
- ^ Asthma definition Mayo Clinic. Retrieved on 2010-02-08
- ^ Ronmark E, Lundback B, Jonsson EA, et al.: "Incidence of asthma in adults: Report from the obstructive lung disease in northern Sweden study." Allergy 1997; 52:1071-1081.
- ^ Burrows B, Martinez FD, Holonen M, et al.: "Association of asthma with serum IgE levels and skin-test reactivity to allergens." N Engl J Med 1989; 320:271-277.
- ^ Simpson BM, Custovic A, Simpson A, et al.: NAC Manchester Asthma and Allergy Study (NACMAAS): "Risk factors for asthma and allergic disorders in adults." Clin Exp Allergy 2001; 31:391-399.
- ^ Peat JK, Tovey E, Toelle BG, et al.: "House dust mite allergens: A major risk factor for childhood asthma in Australia." Am J Respir Crit Care Med 1996; 153:141-146.
- ^ Custovic A, Smith AC, Woodcock A: "Indoor allergens are a primary cause of asthma: Asthma and the environment." Eur Respir Rev 1998; 53:155-158.
- ^ Chan-Yeung M, Manfreda J, Dimich-Ward H, et al.: "A randomized controlled study on the effectiveness of a multifaceted intervention program in the primary prevention of asthma in high-risk infants." Arch Pediatr Adolesc Med 2000; 154:657-663.
- ^ Custovic A, Simpson BM, Simpson A, et al.: "Effect of environmental manipulation in pregnancy and early life on respiratory symptoms and atopy during first year of life: A randomised trial." Lancet 2001; 358:188-193.
- ^ Arshad SH, Bojarskas J, Tsitoura S, et al.: "Prevention of sensitization to house dust mite by allergen avoidance in school age children: A randomized controlled study." Clin Exp Allergy 2002; 32:843-849.
- ^ Arshad SH, Bateman B, Matthews SM: "Primary prevention of asthma and atopy during childhood by allergen avoidance in infancy: A randomised controlled study." Thorax 2003; 58:489-493.
- ^ Celedon JC, Litonjua AA, Ryan L, et al.: "Exposure to cat allergen, maternal history of asthma, and wheezing in first 5 years of life." Lancet 2002; 360:781-782.
- ^ Ownby DR, Johnson CC, Peterson EL: "Exposure to dogs and cats in the first year of life and risk of allergic sensitization at 6 to 7 years of age." JAMA 2002; 288:963-972.
- ^ Perzanowski MS, Ronmark E, Platts-Mills TA, Lundback B: "Effect of cat and dog ownership on sensitization and development of asthma among preteenage children." Am J Respir Crit Care Med 2002; 166:696-702.
- ^ Kuczmarski RJ, Flegal KM, Campbell SM, Johnson CL: "Increasing prevalence of overweight among US adults: The National Health and Nutrition Examination Surveys, 1960–1991." JAMA 1994; 272:205-211.
- ^ Troiano RP, Flegal KM, Kuczmarski RJ, et al.: "Overweight prevalence and trends for children and adolescents: The National Health and Nutrition Examination Surveys, 1963–1991." Arch Pediatr Adolesc Med 1995; 149:1085-1091.
- ^ Huang S-L, Shiao GM, Chou P: "Association between body mass index and allergy in teenage girls in Taiwan." Clin Exp Allergy 1998; 29:323-329.
- ^ Ramsey, CD (2005). "The hygiene hypothesis and asthma". Current Opinion in Pulmonary Medicine. 11 (1): 14–20. PMID 15591883.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|month=ignored (help) - ^ de Lara, C (2007). "Dishing the dirt on asthma: What we can learn from poor hygiene". Biologics. 1 (2): 139–150. PMID 19707324.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|month=ignored (help) - ^ Strachan DP: "Hay fever, hygiene, and household size." BMJ 1989; 299:1259-1260.
- ^ Von Mutius E, Martinez FD, Fritzsch C, et al.: "Skin test reactivity and number of siblings." BMJ 1994; 308:692-695.
- ^ Jarvis D, Chinn S, Luczynska C, Burney P: "The association of family size with atopy and atopic disease." Clin Exp Allergy 1997; 27:240-245.
- ^ Ball TM, Castro-Rodriguez JA, Griffith KA, et al.: "Siblings, day-care attendance, and the risk of asthma and wheezing during childhood. N Engl J Med 2000; 343:538-543. etc)
- ^ Pattemore PK, Johnston SL, Bardin PG: "Viruses as precipitants of asthma symptoms. I Epidemiology." Clin Exp Allergy 1992; 22:325-336.
- ^ Nicholson KG, Kent J,chloes loves kurt Ireland DC: "Respiratory viruses and exacerbations of asthma in adults." BMJ 1993; 307:982-996.
- ^ Tan WC, Xiang X, Qiu D, et al.: "Epidemiology of respiratory viruses in patients hospitalized with near-fatal asthma, acute exacerbations of asthma, or chronic obstructive pulmonary disease." Am J Med 2003; 115:272-277.
- ^ Weiss ST, Tager IB, Munoz A, Speizer FE: "The relationship of respiratory infections in early childhood to the occurrence of increased levels of bronchial responsiveness and atopy." Am Rev Respir Dis 1985; 131:573-578.
- ^ Illi S, von Mutius E, Lau S, et al.: "Early childhood infectious diseases and the development of asthma up to school age: A birth cohort study." BMJ 2001; 322:390-395.
- ^ Lara M, Akinbami L, Flores G,Morgenstern H (2006). "Heterogeneity of childhood asthma among Hispanic children: Puerto Rican children bear a disproportionate burden". Pediatrics. 117 (1): 43–53. doi:10.1542/peds.2004-1714. PMID 16396859.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Davis AM, Kreutzer R, Lipsett M, King G,Shaikh N (2006). "Asthma prevalence in Hispanic and Asian American ethnic subgroups: results from the California Healthy Kids Survey". Pediatrics. 118 (2): e363–70. doi:10.1542/peds.2005-2687. PMID 16882779.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Johnson DB, Oyama N, LeMarchand L,Wilkens L (2004). "Native Hawaiians mortality, morbidity, and lifestyle: comparing data from 1982, 1990, and 2000". Pac Health Dialog. 11 (2): 120–30. PMID 16281689.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Naqvi M, Thyne S, Choudhry S; et al. (2007). "Ethnic-specific differences in bronchodilator responsiveness among african americans, puerto ricans, and mexicans with asthma". J Asthma. 44 (8): 639–48. doi:10.1080/02770900701554441. PMID 17943575.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Burchard EG, Avila PC, Nazario S; et al. (2004). "Lower bronchodilator responsiveness in Puerto Rican than in Mexican subjects with asthma". Am J Respir Crit Care Med. 169 (3): 386–92. doi:10.1164/rccm.200309-1293OC. PMID 14617512.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Gold DR,Acevedo-Garcia D; Acevedo-Garcia, D (2005). "Immigration to the United States and acculturation as risk factors for asthma and allergy". J Allergy Clin Immunol. 116 (1): 38–41. doi:10.1016/j.jaci.2005.04.033. PMID 15990770.
- ^ Eldeirawi KM,Persky VW; Persky, VW (2006). "Associations of acculturation and country of birth with asthma and wheezing in Mexican American youths". J Asthma. 43 (4): 279–86. doi:10.1080/0277090060022869. PMID 16809241.
- ^ Osman M,Hansell A, Simpson CR, Hollowell J, Helms PJ (2007). "Gender specific presentations for asthma, allergic rhinitis and eczema to Primary Care". Prim Care Resp J. 16 (1): 28–35. doi:10.3132/pcrj.2007.00006. PMID 17297524.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ "Asthma and Allergy Foundation of America - Information About Asthma, Allergies, Food Allergies and More!". Aafa.org. Retrieved 2010-04-16.
- ^ "WHO | Asthma". Who.int. 2008-06-03. Retrieved 2010-04-16.
- ^ "Patient/Public Education: Fast Facts — Asthma Demographics/Statistics". American Academy of Allergy Asthma & Immunology. Retrieved 2006-05-02.
- ^ Environmental Protection Agency. "Cockroaches and Pests — Indoor Environmental Asthma Triggers". Environmental Protection Agency. Retrieved 23 November 2009.
- ^ National Heart, Lung, and Blood Institute (2004). "Morbidity & Mortality: 2004 Chart Book On Cardiovascular, Lung, and Blood Diseases". National Institutes of Health.
{{cite journal}}: Cite journal requires|journal=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ National Center for Health Statistics (7 April 2006). "Asthma Prevalence, Health Care Use and Mortality, 2002". Centers for Disease Control and Prevention.
- ^ *[ Rauh VA, Ginger L, Chew GL, Garfinkel RS. Deteriorated housing contributes to high cockroach allergen levels in inner-city households. Environ Health Perspect 110(suppl 2):323–327 (2002).]
- ^ *[1]
- ^ a b Weiler JM, Layton T, Hunt M (1998). "Asthma in United States Olympic athletes who participated in the 1996 Summer Games". J. Allergy Clin. Immunol. 102 (5): 722–6. doi:10.1016/S0091-6749(98)70010-7. PMID 9819287.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Helenius I, Haahtela T (2000). "Allergy and asthma in elite summer sport athletes". J. Allergy Clin. Immunol. 106 (3): 444–52. doi:10.1067/mai.2000.107749. PMID 10984362.
- ^ a b "Fatal and Nonfatal Injuries, and Selected Illnesses and Conditions: Respiratory Diseases". Worker Health Chartbook 2004. National Institute for Occupational Safety and Health. September 2004. Retrieved December 17, 2008.
- ^ "Asthma and Allergies". National Institute for Occupational Safety and Health. September 22, 2008. Retrieved March 23, 2009.
- ^ Pinnock H, Shah R (2007). "Asthma". BMJ. 334 (7598): 847–50. doi:10.1136/bmj.39140.634896.BE. PMC 1853223. PMID 17446617.
- ^ a b c Tippets B, Guilbert TW (2009). "Managing Asthma in Children: Part 1: Making the Diagnosis, Assessing Severity". Consultant for Pediatricians. 8 (5).
- ^ Hirsch L and Pohl CA (February 1, 2007). "How Old Is Old Enough to Report on Asthma Symptoms?". Consultant for Pediatricians. 6 (2).
- ^ a b Sapp J and Niven AS (April 7, 2008). "Making the most of pulmonary function testing in the diagnosis of asthma". Journal of Respiratory Diseases.
- ^ "'Be in control' pack" (PDF). Asthma UK. Retrieved 2007-11-19.
- ^ Corbo J, Bijur P, Lahn M, Gallagher EJ (2005). "Concordance between capnography and arterial blood gas measurements of carbon dioxide in acute asthma". Annals of emergency medicine. 46 (4): 323–7. doi:10.1016/j.annemergmed.2004.12.005. PMID 16187465.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ deShazo RD and Stupko JE (October 1, 2008). "Diagnosing asthma in seniors: An algorithmic approach". Journal of Respiratory Diseases.
- ^ Hargreave, FE (2006). "Asthma, COPD and bronchitis are just components of airway disease". European Respiratory Journal. 28 (2): 264–267. doi:10.1183/09031936.06.00056106. PMID 16880365.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|month=ignored (help) - ^ Sarir H, Mortaz E, Karimi K, Kraneveld AD, Rahman I, Caldenhoven E, Nijkamp FP, Folkerts G. Cigarette smoke regulates the expression of TLR4 and IL-8 production by human macrophages. J Inflamm (Lond). 2009 May 1;6:12.PMID: 19409098
- ^ Thomson NC, Spears M (2005). "The influence of smoking on the treatment response in patients with asthma". Curr Opin Allergy Clin Immunol. 5 (1): 57–63. PMID 15643345.
- ^ Eisner MD, Yelin EH, Katz PP, Earnest G, Blanc PD (2002). "Exposure to indoor combustion and adult asthma outcomes: environmental tobacco smoke, gas stoves, and woodsmoke". Thorax. 57 (11): 973–8. doi:10.1136/thorax.57.11.973. PMC 1746223. PMID 12403881.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ National Asthma Education and Prevention Program. Expert Panel Report: Guidelines for the Diagnosis and Management of Asthma. National Institutes of Health pub no 97–4051. Bethesda, MD, 1997.PDF
- ^ Carol Sorgen, PhD (2007). "Asthma and Air Filters" (HTTP). WebMD, LLC. Retrieved 2009-01-05.
- ^ Reitze, Arnold W. (2001). Air Pollution Control Law. Environmental Law Institute. p. 35. ISBN 9781585760275.
- ^ "NHLBI Guidelines for the Diagnosis and Treatment of Asthma". Nhlbi.nih.gov. Retrieved 2010-04-16.
- ^ O'Connor, J Allergy Clin Immunol, 2005
- ^ Platts-Mills, J Allergy Clin Immunol, 2008
- ^ Kaur, B (2009). "Vitamin C supplementation for asthma". Cochrane Database Syst Rev (1): CD000993. doi:10.1002/14651858.CD000993.pub3. PMID 19160185.
{{cite journal}}: Text "coauthorsRowe BH, Arnold E" ignored (help) - ^ Tippets B Guilbert TW (2009). "Managing Asthma in Children, Part 2: Achieving and Maintaining Control". Consultant for Pediatricians. 8 (6).
- ^ NHBLI 2007, p.213
- ^ "British Guideline on the Management of Asthma" (PDF). Scottish Intercollegiate Guidelines Network. 2008. Retrieved 2008-08-04.
- ^ NHLBI 2007,p.213
- ^ a b Hendeles L, Marshik PL, Ahrens R, Kifle Y, Shuster J (2005). "Response to nonprescription epinephrine inhaler during nocturnal asthma". Ann. Allergy Asthma Immunol. 95 (6): 530–4. PMID 16400891.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Rodrigo GJ, Nannini LJ (2006). "Comparison between nebulized adrenaline and beta2 agonists for the treatment of acute asthma. A meta-analysis of randomized trials". Am J Emerg Med. 24 (2): 217–22. doi:10.1016/j.ajem.2005.10.008. PMID 16490653.
- ^ Alangari, A (2010). "Genomic and non-genomic actions of glucocorticoids in asthma" (PDF). Ann Thorac Med (5): 133–139.
- ^ "BestBets: Inhaled steroids in the treatment of mild to moderate persistent asthma in children: once or twice daily administration?". Retrieved December 16, 2008.
- ^ Papi A, Canonica GW, Maestrelli P; et al. (2007). "Rescue use of beclomethasone and albuterol in a single inhaler for mild asthma". N. Engl. J. Med. 356 (20): 2040–52. doi:10.1056/NEJMoa063861. PMID 17507703.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ "Serevent Diskus, Advair Diskus, and Foradil Information (Long Acting Beta Agonists) - Drug information". FDA. 2006-03-03.
- ^ "FDA sees asthma drug risks — Yahoo! News". Retrieved December 5, 2008.
- ^ Salpeter S, Buckley N, Ormiston T, Salpeter E (2006). "Meta-analysis: effect of long-acting beta-agonists on severe asthma exacerbations and asthma-related deaths". Ann Intern Med. 144 (12): 904–12. PMID 16754916.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Acute asthma symptoms and treatment Retrieved on 2010-02-08
- ^ Rodrigo GJ, Rodrigo C, Hall JB (2004). "Acute asthma in adults: a review". Chest. 125 (3): 1081–102. doi:10.1378/chest.125.3.1081. PMID 15006973.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Rodrigo G (2005). "Comparison of inhaled fluticasone with intravenous hydrocortisone in the treatment of adult acute asthma". Am J Respir Crit Care Med. 171 (11): 1231–6. doi:10.1164/rccm.200410-1415OC. PMID 15764724.
- ^ Krishnan JA, Davis SQ, Naureckas ET, Gibson P, Rowe BH (2009). "An umbrella review: corticosteroid therapy for adults with acute asthma". Am. J. Med. 122 (11): 977–91. doi:10.1016/j.amjmed.2009.02.013. PMID 19854321.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ 10.1378/chest.122.2.396 CHEST August 2002 vol. 122 no. 2 396-398
- ^ Allam MF, Lucena RA. Selenium supplementation for asthma. Cochrane Database of Systematic Reviews 2004, Issue 2. Art. No.: CD003538. DOI: 10.1002/14651858.CD003538.pub2.
- ^ Blanc PD, Trupin L, Earnest G, Katz PP, Yelin EH, Eisner MD (2001). "Alternative therapies among adults with a reported diagnosis of asthma or rhinosinusitis : data from a population-based survey". Chest. 120 (5): 1461–7. doi:10.1378/chest.120.5.1461. PMID 11713120.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Shenfield G, Lim E, Allen H (2002). "Survey of the use of complementary medicines and therapies in children with asthma". J Paediatr Child Health. 38 (3): 252–7. doi:10.1046/j.1440-1754.2002.00770.x. PMID 12047692.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ "www.sign.ac.uk" (PDF). May 2008. p. 37.
- ^ McCarney RW, Brinkhaus B, Lasserson TJ, Linde K (2004). "Acupuncture for chronic asthma". Cochrane Database Syst Rev (1): CD000008. doi:10.1002/14651858.CD000008.pub2. PMID 14973944.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Blackhall K, Appleton S, Cates CJ (2003). "Ionisers for chronic asthma". Cochrane Database Syst Rev (3): CD002986. doi:10.1002/14651858.CD002986. PMID 12917939.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ PC Gøtzsche, HK Johansen (2008). "House dust mite control measures for asthma". Cochrane Database Syst Rev (2): CD001187. doi:10.1002/14651858.CD001187.pub3.
- ^ Author=Recer GM; title=A review of the effects of impermeable bedding encasements on dust-mite allergen exposure and bronchial hyper-responsiveness in dust-mite-sensitized patients; journal= Clin Exp Allergy; 2004 Feb;34(2):268-75.
- ^ Hondras MA, Linde K, Jones AP (2005). "Manual therapy for asthma". Cochrane Database Syst Rev (2): CD001002. doi:10.1002/14651858.CD001002.pub2. PMID 15846609.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Reilly D, Taylor MA, Beattie NG; et al. (1994). "Is evidence for homoeopathy reproducible?". Lancet. 344 (8937): 1601–6. doi:10.1016/S0140-6736(94)90407-3. PMID 7983994.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ White A, Slade P, Hunt C, Hart A, Ernst E (2003). "Individualised homeopathy as an adjunct in the treatment of childhood asthma: a randomised placebo controlled trial". Thorax. 58 (4): 317–21. doi:10.1136/thorax.58.4.317. PMC 1746635. PMID 12668794.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Maddox L, Schwartz DA (2002). "The pathophysiology of asthma". Annu. Rev. Med. 53: 477–98. doi:10.1146/annurev.med.53.082901.103921. PMID 11818486.
- ^ Beckett PA, Howarth PH (2003). "Pharmacotherapy and airway remodelling in asthma?". Thorax. 58 (2): 163–74. doi:10.1136/thorax.58.2.163. PMC 1746582. PMID 12554904.
- ^ NHBLI 2007, p.1
- ^ "WHO Disease and injury country estimates". World Health Organization. 2009. Retrieved November 11, 2009.
- ^ Grant EN, Wagner R, Weiss KB (1999). "Observations on emerging patterns of asthma in our society". J Allergy Clin Immunol. 104: S1–S9. PMID 10452783.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Anandan C, Nurmatov U, van Schayck OC, Sheikh A (2010). "Is the prevalence of asthma declining? Systematic review of epidemiological studies". Allergy. 65 (2): 152–67. doi:10.1111/j.1398-9995.2009.02244.x. PMID 19912154.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ World Health Organization (2007). "Global surveillance, prevention and control of chronic respiratory diseases: a comprehensive approach" (PDF). pp. 15–20, 49. ISBN 9789241563468. Retrieved 2010-05-14.
- ^ a b "Worldwide variation in prevalence of symptoms of asthma, allergic rhinoconjunctivitis, and atopic eczema: ISAAC. The International Study of Asthma and Allergies in Childhood (ISAAC) Steering Committee". Lancet. 351 (9111): 1225–32. 1998. PMID 9643741.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ World Health Organization. "WHO: Asthma". Retrieved 2007-12-29.
- ^ Ng'ang'a LW, Odhiambo JA, Mungai MW; et al. (1998). "Prevalence of exercise induced bronchospasm in Kenyan school children: An urban-rural comparison". Thorax. 53 (11): 919–26. PMC 1745121. PMID 10193388.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Waite DA, Eyles EF, Tonkin SL, O'Donnell TV (1980). "Asthma prevalence in Tokelauan children in two environments". Clin Allergy. 10 (1): 71–5. PMID 7363447.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ a b NHLBI 2007, p.1
- ^ Hayden, Merrill (19 September 2009). "Asthma Guide".
- ^ Corbett, Sara (March/April 2005). "The Asthma Trap". Mother Jones.
{{cite news}}: Check date values in:|date=(help) - ^ Simpson CR, Sheikh A (2010). "Trends in the epidemiology of asthma in England: a national study of 333,294 patients". J R Soc Med. 103: 98–106. doi:10.1258/jrsm.2009.090348. PMID 20200181.
- ^ a b Opolski M, Wilson I (2005). "Asthma and depression: a pragmatic review of the literature and recommendations for future research". Clin Pract Epidemol Ment Health. 1: 18. doi:10.1186/1745-0179-1-18. PMC 1253523. PMID 16185365.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: unflagged free DOI (link) - ^ Abramson MJ, Puy RM, Weiner JM (1995). "Is allergen immunotherapy effective in asthma? A meta-analysis of randomized controlled trials". Am. J. Respir. Crit. Care Med. 151 (4): 969–74. PMID 7697274.
{{cite journal}}: CS1 maint: multiple names: authors list (link)
- Bibliography
External links
- World Health Organization site on asthma
- National Heart, Lung, and Blood Institute — Asthma – U.S. NHLBI Information for Patients and the Public page.
- MedLinePlus: Asthma – a U.S. National Library of Medicine page
- Asthma Management Handbook 2006 National Asthma Council Australia
- Neurogenic mechanisms of asthma
- the Global Initiative for Asthma (GINA)
- NHS Guidance for the management of Asthma
- Types of Asthma by NHS
