Platelet: Difference between revisions
→Dynamics: replace reference, which had nothing to do at all with platelets and clotting |
→Dynamics: ref |
||
| Line 80: | Line 80: | ||
The separation of platelet dynamics into three stages is useful, but artificial. In fact, each stage is initiated in rapid succession, and each continues until the trigger for that stage is no longer present, so there is overlap. |
The separation of platelet dynamics into three stages is useful, but artificial. In fact, each stage is initiated in rapid succession, and each continues until the trigger for that stage is no longer present, so there is overlap. |
||
Thrombus formation on an intact endothelium is prevented by [[nitric oxide]],<ref>{{cite journal |author=Palmer RM, Ferrige AG, Moncada S |title=Nitric oxide release accounts for the biological activity of endothelium-derived relaxing factor |journal=Nature |volume=327 |issue=6122 |pages=524–6 |year=1987 |pmid=3495737 |doi=10.1038/327524a0 }}</ref> [[prostacyclin]],<ref>{{ |
Thrombus formation on an intact endothelium is prevented by [[nitric oxide]],<ref>{{cite journal |author=Palmer RM, Ferrige AG, Moncada S |title=Nitric oxide release accounts for the biological activity of endothelium-derived relaxing factor |journal=Nature |volume=327 |issue=6122 |pages=524–6 |year=1987 |pmid=3495737 |doi=10.1038/327524a0 }}</ref> [[prostacyclin]],<ref name="Jones-2012">{{Cite journal | last1 = Jones | first1 = CI. | last2 = Barrett | first2 = NE. | last3 = Moraes | first3 = LA. | last4 = Gibbins | first4 = JM. | last5 = Jackson | first5 = DE. | title = Endogenous inhibitory mechanisms and the regulation of platelet function. | journal = Methods Molecular Biology | volume = 788 | issue = | pages = 341-66 | month = | year = 2012 | doi = 10.1007/978-1-61779-307-3_23 | PMID = 22130718 }}</ref> and [[CD39]].<ref>{{cite pmid|15852226}}</ref> |
||
===Adhesion=== |
===Adhesion=== |
||
Revision as of 19:53, 23 April 2014
| Platelets | |
|---|---|
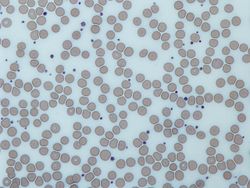 Image from a light microscope (500 ×) from a Giemsa-stained peripheral blood smear showing platelets (blue) surrounded by red blood cells | |
| Identifiers | |
| MeSH | D001792 |
| FMA | 62851 |
| Anatomical terminology | |
Platelets (also called "thrombocytes") are biconvex discs, fragments of cytoplasm 2–3 µm in diameter,[1] found only in the blood of mammals. Platelets form by budding off from megakaryocytes[2] in the bone marrow, and then entering the circulation. They help stop bleeding.
On a stained blood smear, platelets appear as dark purple spots, about 20% the diameter of red blood cells. The smear is used to examine platelets for size, shape, qualitative number, and clumping.
The main function of platelets is to contribute to hemostasis: the process of stopping bleeding at the site of interrupted endothelium. Hemostasis is a two-step process; primary hemostasis involves platelets coming together to form a platelet plug, while in secondary hemostasis the coagulation factors form a fibrin meshwork. During primary hemostasis, platelets go through three stages: first, they stick to substances outside the interrupted endothelium (adhesion); second, they change shape, turn on receptors and secrete chemical messengers (activation); and third, they stick to each other (aggregation). Addition of coagulation factors to this platelet plug via the coagulation cascade results in fibrin deposition, which both cross-links and links to platelets to complete formation of the clot.
Any abnormality of platelets is a thrombocytopathy.[3] Low platelet concentration is thrombocytopenia and is due to either decreased production or increased destruction. Elevated platelet concentration is thrombocytosis and is either congenital, reactive (to cytokines), or due to unregulated production: one of the myeloprolerative neoplasms.
Normal platelets can respond to an abnormality on the vessel wall rather than to hemorrhage, resulting in inappropriate platelet adhesion/activation and thrombosis. Examples are: extending the fibrin clot of venous thrombosis; extending an unstable or ruptured arterial plaque, causing arterial thrombosis; and responding to arteritis with thrombi. An arterial thrombus may partially obstruct blood flow, causing downstream ischemia; or completely obstruct it, causing downstream infarction.
Discovery and naming
The German anatomist Max Schultze (1825–1874) was the first to describe what he called "spherules", which he noted were much smaller than red blood cells, occasionally clumped, and were sometimes found in collections of fibrin material.[4][5]
Osler observed them and called them blood plaques.
Giulio Bizzozero (1846–1901), building on Schultze's findings, in 1882 used "living circulation" to study the blood of amphibians microscopically in vivo. He named Schultz's spherules (It.) piastrine: little plates, which later became platelets. He observed that platelets clump at the site of blood vessel injury, a process that precedes the formation of a clot. This observation confirmed the role of platelets in coagulation.[6]
The term thrombocyte (clot cell) arose in the early 1900's and is sometimes used as a synonym for platelet; but not generally in the scientific literature, especially since the discovery in non-mammalian vertebrates of nucleated cells that have a hemostatic function and were given the name thrombocyte.
A thrombus arises from physiologic hemostasis, thrombosis arises from a pathologic and excessive quantity of thrombin.[7]
Measurement
Platelet concentration is measured either manually using a hemacytometer or by placing blood in an automated analyzer, which uses light scattering or electrical impedance to count the platelets. The normal range (95% of population) for platelets is 150,000 to 400,000 per cubic millimeter, (the same as per microliter).[8] or 150–400 × 109/L. This normal range varies slightly in different laboratories.
The platelet concentration is often referred to informally as the platelet count without stating the units.
Symptoms of platelet disorders
Spontaneous bleeding can be caused by deficient numbers of platelets, dysfunctional platelets, or very excessive numbers of platelets: over 1.5 million/microliter. The bleeding from a skin cut such as a razor nick is prompt and excessive, but can be controlled by pressure. Spontaneous bleeding into the skin causes a purplish stain named by its size: petechiae, purpura, ecchymoses; bleeding into mucous membranes causes bleeding gums, nose bleed, and gastrointestinal bleeding. Intraretinal bleeding and intracranial bleeding can also occur.
Excessive numbers of platelets, and normal platelets responding to abnormal vessel walls, can result in venous thrombosis and arterial thrombosis. The symptoms depend on the site of thrombosis.
Kinetics

- Megakaryocyte and platelet production is regulated by thrombopoietin, a hormone produced in the liver and kidneys.
- Each megakaryocyte produces between 5,000 and 10,000 platelets during its lifetime.
- An average of 1011 platelets are produced daily in a healthy adult.
- Reserve platelets are stored in the spleen, and are released when needed by splenic contraction induced by the sympathetic nervous system.
- The life span of circulating platelets is 8 to 9 days.[9]
- Old platelets are destroyed by phagocytosis in the spleen and liver.
Dynamics

The separation of platelet dynamics into three stages is useful, but artificial. In fact, each stage is initiated in rapid succession, and each continues until the trigger for that stage is no longer present, so there is overlap.
Thrombus formation on an intact endothelium is prevented by nitric oxide,[10] prostacyclin,[11] and CD39.[12]
Adhesion
Endothelial cells are attached to the subendothelial collagen by von Willebrand factor (vWF) which these cells produce. vWF is also stored in endothelial cells and secreted constitutively into the blood. Platelets store vWF in their granules.
When the endothelial layer is disrupted, collagen and vWF anchor platelets to the subendothelium. Platelet GP-V-IX receptor binds with vWF; and GPVI receptor binds with collagen.[13] (In vitro, platelets can adhere to any negatively charged surface, such as glass.)
Activation

Inhibition
The intact endothelial lining inhibits platelet activation by producing nitric oxide, endothelial-ADPase, and PGI2. Endothelial-ADPase degrades the platelet activator, ADP.
Trigger
Platelet activation begins seconds after adhesion occurs. It is triggered when collagen from the subendothilium, and/or tissue factor from the media and adventitia[13] bind with their respective receptors on the platelet. These are G protein coupled receptors and they turn on cAMP mediated signaling pathways within the platelet. Families of three G proteins (Gi, Gq, G12) operate together for full activation.
Elements
One of the signaling pathways turns on scramblase, which moves negatively charged phospholipids from the inner to the outer platelet membrane surface. These phospholipids then bind the tenase and prothrombinase complexes, two of the sites of interplay between platelets and the coagulation cascade. Calcium ions are essential for the binding of these coagulation factors. Intraplatelet calcium concentration increases, stimulating actin and myosin filaments, resulting in platelets becoming more spherical and with pseudopods on their surface. Thus they assume a stellate shape: morphological evidence of the activated platelet.
Granule secretion

Platelets contain dense granules, lambda granules and alpha granules. Activated platelets secrete the contents of these granules through their canalicular systems to the exterior. Granule characteristics:
- dense (or delta) granules (containing ADP or ATP, calcium, and serotonin)
- lambda granules – similar to lysosomes and contain several hydrolytic enzymes.
- Alpha granules (containing P-selectin, platelet factor 4, transforming growth factor-β1, platelet-derived growth factor, fibronectin, B-thromboglobulin, vWF, fibrinogen, and coagulation factors V and XIII).
TXA2 synthesis increases during activation: it is secreted and acts on both its own thromboxane receptors (the so-called "out-in" mechanism), and those of other platelets. These receptors trigger intraplatelet signaling, which converts GPIIb/IIIa receptors to their active form to initiate aggregation.
Aggregation

Aggregation begins minutes after activation, and occurs as a result of turning on the GPIIb/IIIa receptor, which allows these receptors to bind with vWF or fibrinogen.[14] There are 50–100 of these receptors per platelet.[15] When any one of at least nine different platelet surface receptors are turned on, intraplatelet signaling pathways are activated which cause existing GpIIb/IIIa receptors to change shape — curled to straight — and thus become capable of binding.
Classically it was thought that this was the only mechanism involved in aggregation, but three new mechanisms have been identified which can initiate aggregation, depending on the velocity of blood flow (i.e. shear range).[16]
Platelet-coagulation factor interactions
In addition to interacting with vWF and fibrin, platelets interact with thrombin, Factors X, Va, VIIa, XI, IX, and prothrombin to complete clot formation via the coagulation cascade.[17][18]
Six studies suggested platelets express tissue factor: the definitive study shows they do not.[17]
Wound repair
The blood clot is only a temporary solution to stop bleeding; vessel repair is needed. The aggregated platelets secrete substances that promote the invasion of fibroblasts from surrounding connective tissue into the wound to resorb the clot and form a scar. The fibrin is slowly dissolved by the fibrinolytic enzyme, plasmin, and the platelets are cleared by phagocytosis.[19]
Clot formation in non-mammalian vertebrates
Non-mammalian vertebrates instead of having platelets have thrombocytes which have a nucleus and resemble B lymphocytes in morphology. They aggregate in response to thrombin (but not to ADP, serotonin, nor adrenaline, as platelets do).[20][21]
Role in inflammation
In addition to being the cellular effector of hemostasis, platelets are rapidly deployed to sites of injury or infection, and potentially modulate inflammatory processes by interacting with leukocytes and by secreting cytokines, chemokines, and other inflammatory mediators.[22][23][24][25]
[26] Platelets also secrete platelet-derived growth factor (PDGF).
Disorders of platelets
Disorders associated with a reduced platelet count:
- Thrombocytopenia
- Immune thrombocytopenic purpura(ITP) – formerly known as idiopathic thrombocytopenic purpura
- Thrombotic thrombocytopenic purpura
- Drug-induced thrombocytopenic purpura (for example heparin-induced thrombocytopenia (HIT))
- Gaucher's disease
- Aplastic anemia
- Onyalai
Alloimmune disorders
- Neonatal alloimmune thrombocytopenia
- Some transfusion reactions
Disorders associated with platelet dysfunction or reduced count:
Disorders associated with an elevated platelet count:
- Thrombocytosis, either reactive, or as an expression of some myeloproliferative neoplasms: essential thrombocytosis and polycythemia vera; may feature dysfunctional platelets
Disorders of platelet adhesion or aggregation:
Disorders of platelet activation:
- ADP Receptor defect
Disorders of platelet granule amount or release
Disorders of platelet metabolism
- Decreased cyclooxygenase activity, induced or congenital
- Storage pool defects, acquired or congenital
Disorders associated with compromised platelet signaling:
Platelet rich plasma in wound healing
Platelets release platelet-derived growth factor (PDGF), a potent chemotactic agent; and TGF beta, which stimulates the deposition of extracellular matrix; fibroblast growth factor, insulin-like growth factor 1, platelet-derived epidermal growth factor, and vascular endothelial growth factor. Local application of these factors in increased concentrations through Platelet-rich plasma (PRP) is used as an adjunct to wound healing.[31]
Drugs affecting platelets
Some drugs used to treat inflammation have the unwanted side effect of suppressing normal platelet function. These are the non-steroidal anti-inflammatory agents (NSAIDS). Aspirin irreversibly disrupts platelet function by inhibiting cyclooxygenase-1 (COX1), and hence normal hemostasis. The resulting platelets are unable to produce new cyclooxygenase because they have no DNA. Normal platelet function will not return until the use of aspirin has ceased and enough of the affected platelets have been replaced by new ones, which can take over a week. Ibuprofen, another NSAID, does not have such a long duration effect, with platelet function usually returning within 24 hours,[32] and taking ibuprofen before aspirin prevents the irreversible effects of aspirin.[33]
Uremia, a consequence of renal failure, leads to platelet dysfunction that may be ameliorated by the administration of desmopressin.
Drugs which suppress platelet function are used to prevent thrombus formation. The oral agents are aspirin, clopidogrel, cilostazol, ticlopidine, ticagrelor and prasugrel. The intravenous agents are abciximab, eptifibatide, and tirofiban.
Drugs which stimulate production of platelets and thus increase platelet count are Oprelvekin, Romiplostim, Eltrombopag.
Platelet transfusion
Platelet transfusion is most frequently used to correct unusually low platelet counts, either to prevent spontaneous bleeding (typically at counts below (10–15)×109/L) or in anticipation of medical procedures that will necessarily involve some bleeding. For example, in patients undergoing surgery, a level below 50×109/L is associated with abnormal surgical bleeding, and regional anaesthetic procedures such as epidurals are avoided for levels below 80×109/L.[34] Platelets may also be transfused when the platelet count is normal but the platelets are dysfunctional, such as when an individual is taking aspirin or clopidogrel.[35] Finally, platelets may be transfused as part of a massive transfusion protocol, in which the three major blood components (red blood cells, plasma, and platelets) are transfused to address severe hemorrhage. Platelet transfusion is contraindicated in thrombotic thrombocytopenic purpura (TTP), as it fuels the coagulopathy.

Platelets are either isolated from collected units of whole blood and pooled to make a therapeutic dose or collected by apheresis, sometimes concurrently with plasma or red blood cells. The industry standard is for platelets to be tested for bacteria before transfusion to avoid septic reactions, which can be fatal. Recently the AABB Industry Standards for Blood Banks and Transfusion Services (5.1.5.1) has allowed for use of pathogen reduction technology as an alternative to bacterial screenings in platelets.[36]
Pooled whole-blood platelets, sometimes called “random” platelets, are made primarily by two methods.[37] In the US, a unit of whole blood is placed into a large centrifuge in what is referred to as a “soft spin.” At these settings, the platelets remain suspended in the plasma. The platelet-rich plasma (PRP) is removed from the red cells, then centrifuged at a faster setting to harvest the platelets from the plasma. In other regions of the world, the unit of whole blood is centrifuged using settings that cause the platelets to become suspended in the “buffy coat” layer, which includes the platelets and the white blood cells. The “buffy coat” is isolated in a sterile bag, suspended in a small amount of red blood cells and plasma, then centrifuged again to separate the platelets and plasma from the red and white blood cells. Regardless of the initial method of preparation, multiple donations may be combined into one container using a sterile connection device to manufacture a single product with the desired therapeutic dose.
Apheresis platelets are collected using a mechanical device that draws blood from the donor and centrifuges the collected blood to separate out the platelets and other components to be collected. The remaining blood is returned to the donor. The advantage to this method is that a single donation provides at least one therapeutic dose, as opposed to the multiple donations for whole-blood platelets. This means that a recipient is not exposed to as many different donors and has less risk of transfusion-transmitted disease and other complications. Sometimes a person such as a cancer patient who requires routine transfusions of platelets will receive repeated donations from a specific donor to further minimize the risk. Pathogen reduction of platelets using for example, riboflavin and UV light treatments can also be carried out to reduce the infectious load of pathogens contained in donated blood products, thereby reducing the risk of transmission of transfusion transmitted diseases.[38][39]
Platelets do not need to be cross-matched to ensure immune compatibility between donor and recipient unless they contain a significant amount of red blood cells (RBCs). The presence of RBCs results in a reddish-orange color to the product, and is usually associated with whole-blood platelets. Apheresis methods are more efficient than “soft spin” centrifugation at isolating the specific components of blood needed. An effort is usually made to issue type specific platelets, but this is not as critical as it is with RBCs.
Platelets collected by either method have a very short shelf life, typically five days. This results in frequent problems with short supply, as testing the donations often requires up to a full day. Since there are no effective preservative solutions for platelets, they lose potency quickly and are best when fresh.
Platelets are stored under constant agitation at 20–24 °C (68–75.2 °F). Storage at room temperature provides an environment where any bacteria that are introduced to the blood component during the collection process may proliferate and subsequently cause bacteremia in the patient. Regulations are in place in the United States that require products to be tested for the presence of bacterial contamination before transfusion.[40]
Platelets, either apheresis-derived or random-donor, can be processed through a volume reduction process. In this process, the platelets are spun in a centrifuge and the excess plasma is removed, leaving 10 to 100 mL of platelet concentrate. Such volume-reduced platelets are normally transfused only to neonatal and pediatric patients, when a large volume of plasma could overload the child's small circulatory system. The lower volume of plasma also reduces the chances of an adverse transfusion reaction to plasma proteins.[41] Volume reduced platelets have a shelf life of only four hours.[42]
References
- ^ Campbell, Neil A. (2008). Biology (8th ed.). London: Pearson Education. p. 912. ISBN 978-0-321-53616-7.
Platelets are 2–3µm diameter.
- ^ Stenberg PE, Levin J (1989). "Mechanisms of platelet production". Blood Cells. 15 (1): 23–47. PMID 2649182.
- ^ Maton, Anthea (1993). Human Biology and Health. Englewood Cliffs NJ: Prentice Hall. ISBN 0-13-981176-1.
{{cite book}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Brewer DB (2006). "Max Schultze (1865), G. Bizzozero (1882) and the discovery of the platelet". Br. J. Haematol. 133 (3): 251–8. doi:10.1111/j.1365-2141.2006.06036.x. PMID 16643426.
- ^ Schultze M (1865). "Ein heizbarer Objecttisch und seine Verwendung bei Untersuchungen des Blutes". Arch Mikrosc Anat. 1 (1): 1–42. doi:10.1007/BF02961404.
- ^ Bizzozero, J. (1882). "Über einen neuen Forrnbestandteil des Blutes und dessen Rolle bei der Thrombose und Blutgerinnung". Arch Pathol Anat Phys Klin Med. 90 (2): 261–332. doi:10.1007/BF01931360.
- ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 18753650, please use {{cite journal}} with
|pmid=18753650instead. - ^ Parveen June Kumar, Michael L. Clark (2005). "8". Clinical Medicine (6th ed.). Elsevier Saunders. p. 469. ISBN 0-7020-2763-4.
- ^ Harker LA, Roskos LK, Marzec UM; et al. (April 2000). "Effects of megakaryocyte growth and development factor on platelet production, platelet life span, and platelet function in healthy human volunteers". Blood. 95 (8): 2514–22. PMID 10753829.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Palmer RM, Ferrige AG, Moncada S (1987). "Nitric oxide release accounts for the biological activity of endothelium-derived relaxing factor". Nature. 327 (6122): 524–6. doi:10.1038/327524a0. PMID 3495737.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Jones, CI.; Barrett, NE.; Moraes, LA.; Gibbins, JM.; Jackson, DE. (2012). "Endogenous inhibitory mechanisms and the regulation of platelet function". Methods Molecular Biology. 788: 341–66. doi:10.1007/978-1-61779-307-3_23. PMID 22130718.
{{cite journal}}: Cite has empty unknown parameter:|month=(help) - ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 15852226, please use {{cite journal}} with
|pmid=15852226instead. - ^ a b Dubois C, Panicot-Dubois L, Merrill-Skoloff G, Furie B, Furie BC (May 2006). "Glycoprotein VI-dependent and -independent pathways of thrombus formation in vivo". Blood. 107 (10): 3902–6. doi:10.1182/blood-2005-09-3687. PMC 1895285. PMID 16455953.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Yip J, Shen Y, Berndt MC, Andrews RK (2005). "Primary platelet adhesion receptors". IUBMB Life. 57 (2): 103–8. doi:10.1080/15216540500078962. PMID 16036569.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Phillips DR, Charo IF, Scarborough RM (May 1991). "GPIIb-IIIa: the responsive integrin". Cell. 65 (3): 359–62. PMID 2018971.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 1702031, please use {{cite journal}} with
|pmid=1702031instead. - ^ a b Bouchard BA, Mann KG, Butenas S (August 2010). "No evidence for tissue factor on platelets". Blood. 116 (5): 854–5. doi:10.1182/blood-2010-05-285627. PMC 2918337. PMID 20688968.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Ahmad SS, Rawala-Sheikh R, Walsh PN (1992). "Components and assembly of the factor X activating complex". Semin. Thromb. Hemost. 18 (3): 311–23. doi:10.1055/s-2007-1002570. PMID 1455249.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Movat HZ, Weiser WJ, Glynn MF, Mustard JF (1965). "Platelet phagocytosis and aggregation". J. Cell Biol. 27 (3): 531–43. doi:10.1083/jcb.27.3.531. PMC 2106759. PMID 4957257.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Schmaier AA, Stalker TJ, Runge JJ; et al. (September 2011). "Occlusive thrombi arise in mammals but not birds in response to arterial injury: evolutionary insight into human cardiovascular disease". Blood. 118 (13): 3661–9. doi:10.1182/blood-2011-02-338244. PMC 3186337. PMID 21816834.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Belamarich FA, Shepro D, Kien M (November 1968). "ADP is not involved in thrombin-induced aggregation of thrombocytes of a non-mammalian vertebrate". Nature. 220 (5166): 509–10. doi:10.1038/220509a0. PMID 5686175.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Weyrich AS, Zimmerman GA (2004). "Platelets: signaling cells in the immune continuum". Trends Immunol. 25 (9): 489–95. doi:10.1016/j.it.2004.07.003. PMID 15324742.
- ^ Wagner DD, Burger PC (2003). "Platelets in inflammation and thrombosis". Arterioscler. Thromb. Vasc. Biol. 23 (12): 2131–7. doi:10.1161/01.ATV.0000095974.95122.EC. PMID 14500287.
- ^ Diacovo TG, Puri KD, Warnock RA, Springer TA, von Andrian UH (1996). "Platelet-mediated lymphocyte delivery to high endothelial venules". Science. 273 (5272): 252–5. doi:10.1126/science.273.5272.252. PMID 8662511.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Iannacone M, Sitia G, Isogawa M, Marchese P, Castro MG, Lowenstein PR, Chisari FV, Ruggeri ZM, Guidotti LG (2005). "Platelets mediate cytotoxic T lymphocyte-induced liver damage". Nat. Med. 11 (11): 1167–9. doi:10.1038/nm1317. PMC 2908083. PMID 16258538.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Iannacone M.; et al. (2005). "Platelets mediate cytotoxic T lymphocyte-induced liver damage". Nat Med. 11 (11): 1167–9. doi:10.1038/nm1317. PMC 2908083. PMID 16258538.
{{cite journal}}: Explicit use of et al. in:|author=(help) - ^ Erpenbeck L, Schön MP (2010). "Deadly allies: the fatal interplay between platelets and metastasizing cancer cells". Blood. 115 (17): 3427–36. doi:10.1182/blood-2009-10-247296. PMC 2867258. PMID 20194899.
- ^ Pleass RJ (2009). "Platelet power: sticky problems for sticky parasites?". Trends Parasitol. 25 (7): 296–9. doi:10.1016/j.pt.2009.04.002. PMC 3116138. PMID 19539528.
- ^ Kornerup KN, Page CP (2007). "The role of platelets in the pathophysiology of asthma". Platelets. 18 (5): 319–28. doi:10.1080/09537100701230436. PMID 17654302.
- ^ Laidlaw TM, Kidder MS, Bhattacharyya N, Xing W, Shen S, Milne GL, Castells MC, Chhay H, Boyce JA (2012). "Cysteinyl leukotriene overproduction in aspirin-exacerbated respiratory disease is driven by platelet-adherent leukocytes". Blood. 119 (16): 3790–8. doi:10.1182/blood-2011-10-384826. PMC 3335383. PMID 22262771.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Gawaz M, Vogel S (October 2013). "Platelets in tissue repair: control of apoptosis and interactions with regenerative cells". Blood. 122 (15): 2550–4. doi:10.1182/blood-2013-05-468694. PMID 23963043.
- ^ "Platelet Function after Taking Ibuprofen for 1 Week". Annals of internal medicine. 142 (7): I54. 2005. PMID 15809457.
{{cite journal}}:|access-date=requires|url=(help) - ^ Rao GH, Johnson GG, Reddy KR, White JG (1983). "Ibuprofen protects platelet cyclooxygenase from irreversible inhibition by aspirin". Arteriosclerosis. 3 (4): 383–8. doi:10.1161/01.ATV.3.4.383. PMID 6411052.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ van Veen JJ, Nokes TJ, Makris M (2010). "The risk of spinal haematoma following neuraxial anaesthesia or lumbar puncture in thrombocytopenic individuals". Br. J. Haematol. 148 (1): 15–25. doi:10.1111/j.1365-2141.2009.07899.x. PMID 19775301.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Roback, J.; Grossman, B.; Harris, T.; Hillyer, C., eds. (2011). Technical Manual (17th ed.). Bethesda MD: AABB. p. 580. ISBN 978-1-56395-315-6.
- ^ American Association of Blood Banks (2003). "5.1.5.1". Standards for Blood Banks and Transfusion Services (22nd ed.). Bethesda MD: AABB.
- ^ Högman CF (1992). "New trends in the preparation and storage of platelets". Transfusion. 32 (1): 3–6. doi:10.1046/j.1537-2995.1992.32192116428.x. PMID 1731433.
- ^ Ruane PH, Edrich R, Gampp D, Keil SD, Leonard RL, Goodrich RP (2004). "Photochemical inactivation of selected viruses and bacteria in platelet concentrates using riboflavin and light". Transfusion. 44 (6): 877–85. doi:10.1111/j.1537-2995.2004.03355.x. PMID 15157255.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Perez-Pujol S, Tonda R, Lozano M, Fuste B, Lopez-Vilchez I, Galan AM, Li J, Goodrich R, Escolar G (2005). "Effects of a new pathogen-reduction technology (Mirasol PRT) on functional aspects of platelet concentrates". Transfusion. 45 (6): 911–9. doi:10.1111/j.1537-2995.2005.04350.x. PMID 15934989.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ AABB (2009). Standards for Blood Banks and Transfusion Services (26th ed.). Bethesda MD: AABB.
- ^ Schoenfeld H, Spies C, Jakob C (2006). "Volume-reduced platelet concentrates". Curr. Hematol. Rep. 5 (1): 82–8. PMID 16537051.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ CBBS: Washed and volume-reduced Plateletpheresis units. Cbbsweb.org (2001-10-25). Retrieved on 2011-11-14.
External reading
Michelson, Alan D. (2013). Platelets (3rd ed.). Academic. ISBN 0-12-387837-3.
