Vaccine hesitancy


Evidence surrounding vaccination shows that prevented suffering and death from infectious diseases outweigh any adverse effects.[1] Despite this, vaccine controversies have raged since almost 80 years before the terms vaccine and vaccination were introduced, and continue to this day. Opponents question the effectiveness, safety, and necessity of recommended vaccines. They also argue that mandatory vaccination violate individual rights to medical decisions and religious principles.[2] These arguments have reduced vaccination rates in certain communities, resulting in outbreaks and deaths from preventable childhood diseases.[3][4][5]
Immunization programs depend on public confidence to be effective. Safety concerns often follow a pattern: a potential adverse effect is hypothesized; a premature announcement is made; the initial study is not reproduced; and finally, it takes several years to regain public confidence in the vaccine.[1] A recent and notable example involved Andrew Wakefield's discredited claims of MMR vaccines causing autism.
Public reaction has contributed to a significant increase in preventable diseases, notably measles.[6] In 2011 the vaccine-autism connection was described as "the most damaging medical hoax of the last 100 years".[7]
Variolation
Early attempts to prevent smallpox involved deliberate inoculation of the disease in hopes that a mild result would confer immunity. Originally called inoculation, this technique was later called variolation to avoid confusion with cowpox inoculation (vaccination) when that was introduced by Edward Jenner. Although variolation had a long history in China and India, it was first used in North America and England in 1721. Reverend Cotton Mather introduced variolation to Boston, Massachusetts, during the 1721 smallpox epidemic.[8] Many[citation needed] had religious objections, but Mather convinced Dr. Zabdiel Boylston to try it. Boylston first experimented on his 6-year-old son, his slave, and his slave's son; each subject contracted the disease and was sick for several days, until the sickness vanished and they were "no longer gravely ill".[8] Boylston went on to variolate thousands of Massachusetts residents, and many places were named for him in gratitude as a result. Lady Mary Wortley Montagu introduced variolation to England. She had seen it used in Turkey and, in 1718, had her son successfully variolated in Constantinople under the supervision of Dr. Charles Maitland. When she returned to England in 1721, she had her daughter variolated by Maitland. This aroused considerable interest, and Sir Hans Sloane organized the variolation of some inmates in Newgate Prison. These were successful, and after a further short trial in 1722, two daughters of Caroline of Ansbach Princess of Wales were variolated without mishap. With this royal approval, the procedure became common when smallpox epidemics threatened.[9]
Religious arguments against inoculation were soon advanced. For example, in a 1772 sermon entitled "The Dangerous and Sinful Practice of Inoculation", the English theologian Reverend Edmund Massey argued that diseases are sent by God to punish sin and that any attempt to prevent smallpox via inoculation is a "diabolical operation".[10] It was customary at the time for popular preachers to publish sermons, which reached a wide audience. This was the case with Massey, whose sermon reached North America, where there was early religious opposition, particularly by John Williams. A greater source of opposition there was Dr. William Douglass, a medical graduate of Edinburgh University and a Fellow of the Royal Society, who had settled in Boston.[9]: 114–22
Smallpox vaccination
After Edward Jenner introduced the smallpox vaccine in 1798, variolation declined and was banned in some countries.[11][12]

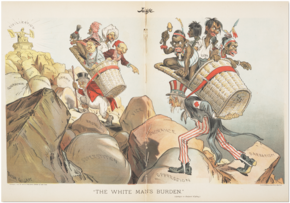
As with variolation, there was some religious opposition to vaccination, although this was balanced to some extent by support from clergymen who not only preached in its favour but also performed vaccination themselves. These included Reverend Robert Ferryman, a friend of Jenner's, and Rowland Hill.[9]: 221 There was also opposition from some variolators who saw the loss of a lucrative monopoly. William Rowley published illustrations of deformities allegedly produced by vaccination, lampooned in James Gillray's famous caricature depicted on this page, and Benjamin Moseley likened cowpox to syphilis, starting a controversy that would last into the 20th century.[9]: 203–5
There was legitimate concern from supporters of vaccination about its safety and efficacy, but this was overshadowed by general condemnation, particularly when legislation started to introduce compulsory vaccination. The reason for this was that vaccination was introduced before laboratory methods were developed to control its production and account for its failures.[13] Vaccine was maintained initially through arm-to-arm transfer and later through production on the skin of animals, and bacteriological sterility was impossible. Further, identification methods for potential pathogens were not available until the late 19th to early 20th century. Diseases later shown to be caused by contaminated vaccine included erysipelas, tuberculosis, tetanus, and syphilis. This last, though rare—estimated at 750 cases in 100 million vaccinations[14]—attracted particular attention. Much later, Dr. Charles Creighton, a leading medical opponent of vaccination, claimed that the vaccine itself was a cause of syphilis and devoted a whole book to the subject.[15] As cases of smallpox started to occur in those who had been vaccinated earlier, supporters of vaccination pointed out that these were usually very mild and occurred years after the vaccination. In turn, opponents of vaccination pointed out that this contradicted Jenner's belief that vaccination conferred complete protection.[13]: 17–21 The views of opponents of vaccination that it was both dangerous and ineffective led to the development of determined anti-vaccination movements in England when legislation was introduced to make vaccination compulsory.[16]
- Opposition to legislation in England
Because of its greater risks, variolation was banned in England by the 1840 Vaccination Act, which also introduced free voluntary vaccination for infants. Thereafter Parliament passed successive acts that imposed and enforced compulsory vaccination.[17] The 1853 act introduced compulsory vaccination, with fines for non-compliance and imprisonment for non-payment. The 1867 act extended the age requirement to 14 years and introduced repeated fines for repeated refusal for the same child. Initially, vaccination regulations were organised by the local Poor Law Guardians, and in towns where there was strong opposition to vaccination, sympathetic Guardians were elected who did not pursue prosecutions. This was changed by the 1871 act, which required Guardians to act. This significantly changed the relationship between the government and the public, and organized protests increased.[17] In Keighley, Yorkshire, in 1876 the Guardians were arrested and briefly imprisoned in York Castle, prompting large demonstrations in support of the "Keighley Seven".[16]: 108–9 The protest movements crossed social boundaries. The financial burden of fines fell hardest on the working class, who would provide the largest numbers at public demonstrations.[18] Societies and publications were organized by the middle classes, and support came from celebrities such as George Bernard Shaw and Alfred Russel Wallace, doctors such as Charles Creighton and Edgar Crookshank, and parliamentarians such as Jacob Bright and James Allanson Picton.[17] By 1885, with over 3,000 prosecutions pending in Leicester, a mass rally there was attended by over 20,000 protesters.[19]
Under increasing pressure, the government appointed a Royal Commission on Vaccination in 1889, which issued six reports between 1892 and 1896, with a detailed summary in 1898.[20] Its recommendations were incorporated into the 1898 Vaccination Act, which still required compulsory vaccination but allowed exemption on the grounds of conscientious objection on presentation of a certificate signed by two magistrates.[2][17] These were not easy to obtain in towns where magistrates supported compulsory vaccination, and after continued protests, a further act in 1907 allowed exemption on a simple signed declaration.[19] Although this solved the immediate problem, the compulsory vaccination acts remained legally enforceable, and determined opponents lobbied for their repeal. No Compulsory Vaccination was one of the demands of the 1900 Labour Party General Election Manifesto.[21] This was done as a matter of routine when the National Health Service was introduced in 1948, with "almost negligible" opposition from supporters of compulsory vaccination.[22]
Vaccination in Wales was covered by English legislation, but the Scottish legal system was separate. Vaccination was not made compulsory there until 1863, and conscientious objection was allowed after vigorous protest only in 1907.[13]: 10–11
In the late 19th century, the city of Leicester in the UK received much attention because of the way smallpox was managed there. There was particularly strong opposition to compulsory vaccination, and medical authorities had to work within this framework. They developed a system that did not use vaccination but was based on strict isolation of cases and contacts and the provision of isolation hospitals. This proved successful but required acceptance of compulsory isolation rather than vaccination. C. Killick Millard, initially a supporter of compulsory vaccination, was appointed Medical Officer of Health in 1901. He moderated his views on compulsion but encouraged contacts and his staff to accept vaccination. This approach, developed initially due to overwhelming opposition to government policy, became known as the Leicester Method.[22][23] In time it became generally accepted as the most appropriate way to deal with smallpox outbreaks and was listed as one of the "important events in the history of smallpox control" by those most involved in the World Health Organization's successful Smallpox Eradication Campaign. The final stages of the campaign, generally referred to as "surveillance containment", owed much to the Leicester method.[24][25]
- Opposition to vaccination in the United States and Brazil
In the US, President Thomas Jefferson took a close interest in vaccination, alongside Dr. Waterhouse, chief physician at Boston. Jefferson encouraged the development of ways to transport vaccine material through the Southern states, which included measures to avoid damage by heat, a leading cause of ineffective batches. Smallpox outbreaks were contained by the latter half of the 19th century, a development widely attributed to the vaccination of a large portion of the population. Vaccination rates fell after this decline in smallpox cases, and the disease again became epidemic in the late 19th century (see Smallpox).[26]
After an 1879 visit to New York by prominent British anti-vaccinationist William Tebb, The Anti-Vaccination Society of America was founded.[27][28] The New England Anti-Compulsory Vaccination League formed in 1882, and the Anti-Vaccination League of New York City in 1885.[28] Tactics in the US largely followed those used in England.[29] Vaccination in the US was regulated by individual states, in which there followed the progression of compulsion, opposition, and repeal similar to that in England.[30] Although generally organized on a state-by-state basis, the vaccination controversy reached the US Supreme Court in 1905. There, in the case of Jacobson v. Massachusetts, the court issued a landmark ruling that the public good overrode personal freedom.
John Pitcairn, the wealthy founder of the Pittsburgh Plate Glass Company (now PPG Industries), emerged as a major financier and leader of the American anti-vaccination movement. On March 5, 1907, in Harrisburg, Pennsylvania, he delivered an address to the Committee on Public Health and Sanitation of the Pennsylvania General Assembly criticizing vaccination.[31] He later sponsored the National Anti-Vaccination Conference, which, held in Philadelphia in October 1908, led to the creation of The Anti-Vaccination League of America. When the league organized later that month, members chose Pitcairn as their first president.[32]
On December 1, 1911, Pitcairn was appointed by Pennsylvania Governor John K. Tener to the Pennsylvania State Vaccination Commission, and subsequently authored a detailed report strongly opposing the commission's conclusions.[32] He remained a staunch opponent of vaccination until his death in 1916.
In November 1904, in response to years of inadequate sanitation and disease, followed by a poorly explained public health campaign led by the renowned Brazilian public health official Oswaldo Cruz, citizens and military cadets in Rio de Janeiro arose in a Revolta da Vacina, or Vaccine Revolt. Riots broke out on the day a vaccination law took effect; vaccination symbolized the most feared and most tangible aspect of a public health plan that included other features, such as urban renewal, that many had opposed for years.[33]
Since the early 19th century, the anti-vaccination movement has drawn members from a wide range of society.
Later vaccines and antitoxins
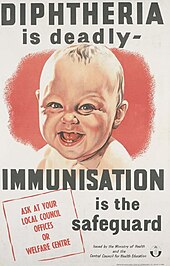
Opposition to smallpox vaccination continued into the 20th century and was joined by controversy over new vaccines and the introduction of antitoxin treatment for diphtheria. Injection of horse serum into humans as used in antitoxin can cause hypersensitivity, commonly referred to as serum sickness. Moreover, the continued production of smallpox vaccine in animals and the production of antitoxins in horses prompted anti-vivisectionists to oppose vaccination.
Diphtheria antitoxin was serum from horses that had been immunized against diphtheria, and was used to treat human cases by providing passive immunity. In 1901, antitoxin from a horse named Jim was contaminated with tetanus and killed 13 children in St Louis, Missouri. This incident, together with nine deaths from tetanus from contaminated smallpox vaccine in Camden, New Jersey, led directly and quickly to the passing of the Biologics Control Act in 1902.[34]
Robert Koch developed tuberculin in 1890. Inoculated into individuals who have had tuberculosis, it produces a hypersensitivity reaction, and is still used to detect those who have been infected. However, Koch used tuberculin as a vaccine. This caused serious reactions and deaths in individuals whose latent tuberculosis was reactivated by the tuberculin.[35] This was a major setback for supporters of new vaccines.[13]: 30–31 Such incidents and others ensured that any untoward results concerning vaccination and related procedures received continued publicity, which grew as the number of new procedures increased.
In 1955, in a tragedy known as the Cutter incident, Cutter Laboratories produced 120,000 doses of the Salk polio vaccine that inadvertently contained some live polio virus along with inactivated virus. This vaccine caused 40,000 cases of polio, 53 cases of paralysis, and five deaths. The disease spread through the recipients' families, creating a polio epidemic that led to a further 113 cases of paralytic polio and another five deaths. It was one of the worst pharmaceutical disasters in US history.[36]
Later 20th-century events include the 1982 broadcast of DPT: Vaccine Roulette, which sparked debate over the DPT vaccine,[37] and the 1998 publication of a fraudulent academic article by Andrew Wakefield[38] which sparked the MMR vaccine controversy. Also recently, the HPV vaccine has become controversial due to concerns that it may encourage promiscuity when given to 11- and 12-year-old girls.[39][40]
Arguments against vaccines in the 21st century are often similar to those of 19th-century anti-vaccinationists.[2]
Effectiveness

Scientific evidence for the effectiveness of large-scale vaccination campaigns is well established. Vaccination campaigns helped eradicate smallpox, which once killed as many as one in seven children in Europe,[41] and have nearly eradicated polio.[42] As a more modest example, infections caused by Haemophilus influenzae, a major cause of bacterial meningitis and other serious diseases in children, have decreased by over 99% in the US since the introduction of a vaccine in 1988.[43] Full vaccination, from birth to adolescence, of all US children born in a given year saves an estimated 33,000 lives and prevents an estimated 14 million infections.[44]
Some opponents of vaccination argue that these reductions in infectious disease are a result of improved sanitation and hygiene (rather than vaccination), or that these diseases were already in decline before the introduction of specific vaccines. These claims are not supported by scientific data; the incidence of vaccine-preventable diseases tended to fluctuate over time until the introduction of specific vaccines, at which point the incidence dropped to near zero. A Centers for Disease Control website aimed at countering common misconceptions about vaccines argued, "Are we expected to believe that better sanitation caused incidence of each disease to drop, just at the time a vaccine for that disease was introduced?"[45]
Other critics argue that the immunity granted by vaccines is only temporary and requires boosters, whereas those who survive the disease become permanently immune.[2] As discussed below, the philosophies of some alternative medicine practitioners are incompatible with the idea that vaccines are effective.[46]
Population health

Incomplete vaccine coverage increases the risk of disease for the entire population, including those who have been vaccinated, because it reduces herd immunity. For example, the measles vaccine targets children between the ages of 9 and 12 months, and the short window between the disappearance of maternal antibody (before which the vaccine often fails to seroconvert) and natural infection means that vaccinated children are frequently still vulnerable. Herd immunity lessens this vulnerability if all the children are vaccinated. Increasing herd immunity during an outbreak or threatened outbreak is perhaps the most widely accepted justification for mass vaccination. Mass vaccination also helps to increase coverage rapidly, thus obtaining herd immunity, when a new vaccine is introduced.[48]
By increasing the herd immunity, it also help the people who have a compromised immune system. Some children who have a compromised immune system cannot get some vaccines and thus have to rely on others to be vaccinated for certain diseases. If the immunocompromised child is surrounded by children who have not been vaccinated and have the disease, the immunocompromised child will likely contract the disease. The outcomes for the child with a compromised immune system who get infected is worse than usually. Increasing the herd immunity and requiring vaccines in children would help decrease this risk.[49]
Cost-effectiveness
Commonly used vaccines are a cost-effective and preventive way of promoting health, compared to the treatment of acute or chronic disease. In the US during the year 2001, routine childhood immunizations against seven diseases were estimated to save over $40 billion per birth-year cohort in overall social costs, including $10 billion in direct health costs, and the societal benefit-cost ratio for these vaccinations was estimated to be 16.5.[50]
Events following reductions in vaccination
In several countries, reductions in the use of some vaccines were followed by increases in the diseases' morbidity and mortality.[51][52] According to the Centers for Disease Control and Prevention, continued high levels of vaccine coverage are necessary to prevent resurgence of diseases that have been nearly eliminated.[53] Pertussis remains a major health problem in developing countries, where mass vaccination is not practiced; the World Health Organization estimates it caused 294,000 deaths in 2002.[54]
Stockholm, smallpox (1873–74)
An anti-vaccination campaign motivated by religious objections, concerns about effectiveness, and concerns about individual rights led to the vaccination rate in Stockholm dropping to just over 40%, compared to about 90% elsewhere in Sweden. A major smallpox epidemic then started in 1873. It led to a rise in vaccine uptake and an end of the epidemic.[55]
Vietnam
During the Vietnam War,vaccination was necessary for soldiers in order for them to fight overseas. Because disease follows soldiers, they had to receive vaccines preventing cholera, influenza, measles, meningococcal, plague, poliovirus, smallpox,tetanus-diphtheria, typhoid, typhus, and yellow fever. However, the diseases mainly prevalent in Vietnam at this time were measles and polio. After arriving in Vietnam, the United States Military conducted the "Military Public Health Assistance Project." [56] This public health program was a joint United States Military and the Government of Vietnam concept to create or expand public medical facilities throughout South Vietnam.[57] Local villages in Vietnam were inoculated. The United States military screened patients, dispensed medication, distributed clothing and food, and even passed out propaganda such as comic books.
UK, pertussis (1970s–80s)
In a 1974 report ascribing 36 reactions to whooping cough (pertussis) vaccine, a prominent public-health academic claimed that the vaccine was only marginally effective and questioned whether its benefits outweigh its risks, and extended television and press coverage caused a scare. Vaccine uptake in the UK decreased from 81% to 31%, and pertussis epidemics followed, leading to the deaths of some children. Mainstream medical opinion continued to support the effectiveness and safety of the vaccine; public confidence was restored after the publication of a national reassessment of vaccine efficacy. Vaccine uptake then increased to levels above 90%, and disease incidence declined dramatically.[51]
Sweden, pertussis (1979–96)
In the vaccination moratorium period that occurred when Sweden suspended vaccination against whooping cough (pertussis) from 1979 to 1996, 60% of the country's children contracted the potentially fatal disease before the age of 10; close medical monitoring kept the death rate from whooping cough at about one per year.[52]
Netherlands, measles (1999–2000)
An outbreak at a religious community and school in the Netherlands illustrates the effect of measles in an unvaccinated population.[58] The population in the several provinces affected had a high level of immunization, with the exception of one of the religious denominations, which traditionally does not accept vaccination. The three measles-related deaths and 68 hospitalizations that occurred among 2,961 cases in the Netherlands demonstrate that measles can be severe and may result in death, even in industrialized countries.
UK and Ireland, measles (2000)
As a result of the MMR vaccine controversy, vaccination compliance dropped sharply in the United Kingdom after 1996.[59] From late 1999 until the summer of 2000, there was a measles outbreak in North Dublin, Ireland. At the time, the national immunization level had fallen below 80%, and in part of North Dublin the level was around 60%. There were more than 100 hospital admissions from over 300 cases. Three children died and several more were gravely ill, some requiring mechanical ventilation to recover.[60]
Nigeria, polio, measles, diphtheria (2001–)
In the early first decade of the 21st century, conservative religious leaders in northern Nigeria, suspicious of Western medicine, advised their followers not to have their children vaccinated with oral polio vaccine. The boycott was endorsed by the governor of Kano State, and immunization was suspended for several months. Subsequently, polio reappeared in a dozen formerly polio-free neighbors of Nigeria, and genetic tests showed the virus was the same one that originated in northern Nigeria. Nigeria had become a net exporter of the polio virus to its African neighbors. People in the northern states were also reported to be wary of other vaccinations, and Nigeria reported over 20,000 measles cases and nearly 600 deaths from measles from January through March 2005.[61] In 2006, Nigeria accounted for over half of all new polio cases worldwide.[62] Outbreaks continued thereafter; for example, at least 200 children died in a late-2007 measles outbreak in Borno State.[63]
Indiana, United States, measles (2005)
A 2005 measles outbreak in the US state of Indiana was attributed to parents who had refused to have their children vaccinated.[64] Most cases of pediatric tetanus in the US occur in children whose parents objected to their vaccination.[65]
Multiple states, United States, measles (2013–)
In 2000, measles was declared eliminated from the United States because internal transmission had been interrupted for one year; remaining reported cases were due to importation.[66]
Centers for Disease Control and Prevention (CDC) reported that the three biggest outbreaks of measles in 2013 were attributed to clusters of people who were unvaccinated due to their philosophical or religious beliefs. As of August 2013, three pockets of outbreak—New York City, North Carolina, and Texas—contributed to 64% of the 159 cases of measles reported in 16 states.[67][68]
The number of cases in 2014 quadrupled to 644,[69] including transmission by unvaccinated visitors to Disneyland in California.[70][71] Some 97% of cases in the first half of the year were confirmed to be due directly or indirectly to importation (the remainder were unknown), and 49% from the Philippines. 165 of the 288 victims (57%) during that time were confirmed to be unvaccinated by choice; 30 (10%) were confirmed to have been vaccinated.[72] The final count of measles outbreaks in 2014 is 668 cases in 27 states.[73]
From January 1 to June 26, 2015, 178 people from 24 states and the District of Columbia were reported to have measles. Most of these cases (117 cases [66%]) were part of a large multi-state outbreak linked to Disneyland in California, continued from 2014. Analysis by the CDC scientists showed that the measles virus type in this outbreak (B3) was identical to the virus type that caused the large measles outbreak in the Philippines in 2014.[73] On July 2, 2015, the first confirmed death from measles in 12 years was recorded. An immunocompromised woman in Washington State was infected and later died of pneumonia due to measles.[74]
Swansea, measles (2013)
In 2013, an outbreak of measles occurred in the Welsh city of Swansea. One death was reported.[75] Some estimates indicate that while in 1995, MMR uptake for two-year-olds was at 94% in Wales, it fell to as low as 67.5% in Swansea in 2003, meaning the region had a "vulnerable" age group.[76] This has been linked to the MMR vaccine controversy, which caused a significant number of parents to fear allowing their children to receive the MMR vaccine.[75]
Safety
Few deny the vast improvements vaccination has made to public health; a more common concern is their safety.[77] As with any medical treatment, there is a potential for vaccines to cause serious complications, such as severe allergic reactions,[78] but unlike most other medical interventions, vaccines are given to healthy people and so a higher standard of safety is expected.[79] While serious complications from vaccinations are possible, they are extremely rare and much less common than similar risks from the diseases they prevent.[45] As the success of immunization programs increases and the incidence of disease decreases, public attention shifts away from the risks of disease to the risk of vaccination,[1] and it becomes challenging for health authorities to preserve public support for vaccination programs.[80]
Concerns about immunization safety often follow a pattern. First, some investigators suggest that a medical condition of increasing prevalence or unknown cause is an adverse effect of vaccination. The initial study and subsequent studies by the same group have inadequate methodology—typically a poorly controlled or uncontrolled case series. A premature announcement is made about the alleged adverse effect, resonating with individuals suffering from the condition, and underestimating the potential harm of foregoing vaccination to those whom the vaccine could protect. Other groups attempt to replicate the initial study but fail to get the same results. Finally, it takes several years to regain public confidence in the vaccine.[1] Adverse effects ascribed to vaccines typically have an unknown origin, an increasing incidence, some biological plausibility, occurrences close to the time of vaccination, and dreaded outcomes.[81] In almost all cases, the public health effect is limited by cultural boundaries: English speakers worry about one vaccine causing autism, while French speakers worry about another vaccine causing multiple sclerosis, and Nigerians worry that a third vaccine causes infertility.[82]
Autism controversies
There is no evidence that vaccines cause autism despite popular press and media linking the two.[1][83][84]
Thiomersal
Thiomersal (spelled "thimerosal" in the US) is an antifungal preservative used in small amounts in some multi-dose vaccines (where the same vial is opened and used for multiple patients) to prevent contamination of the vaccine.[85] Despite thiomersal's efficacy, the use of thiomersal is controversial because it contains mercury. As a result, in 1999, the Centers for Disease Control (CDC) and the American Academy of Pediatrics (AAP) asked vaccine makers to remove thiomersal from vaccines as quickly as possible on the precautionary principle. Thiomersal is now absent from all common US and European vaccines, except for some preparations of influenza vaccine.[86] (Trace amounts remain in some vaccines due to production processes, at an approximate maximum of 1 microgramme, around 15% of the average daily mercury intake in the USA for adults and 2.5% of the daily level considered tolerable by the WHO.[87][88]) The action sparked concern that thiomersal could have been responsible for autism.[86] The idea is now considered disproven, as incidence rates for autism increased steadily even after thiomersal was removed from childhood vaccines.[89] Currently there is no accepted scientific evidence that exposure to thiomersal is a factor in causing autism.[90] Since 2000, parents in the United States have pursued legal compensation from a federal fund arguing that thiomersal caused autism in their children.[91] A 2004 Institute of Medicine (IOM) committee favored rejecting any causal relationship between thiomersal-containing vaccines and autism.[92]
MMR vaccine
In the UK, the MMR vaccine was the subject of controversy after the publication in The Lancet of a 1998 paper by Andrew Wakefield and others reporting case histories of 12 children mostly with autism spectrum disorders with onset soon after administration of the vaccine.[93] At a 1998 press conference, Wakefield suggested that giving children the vaccines in three separate doses would be safer than a single vaccination. This suggestion was not supported by the paper, and several subsequent peer-reviewed studies have failed to show any association between the vaccine and autism.[94] It later emerged that Wakefield had received funding from litigants against vaccine manufacturers and that he had not informed colleagues or medical authorities of his conflict of interest;[95] had this been known, publication in The Lancet would not have taken place in the way that it did.[96] Wakefield has been heavily criticized on scientific grounds and for triggering a decline in vaccination rates[97] (vaccination rates in the UK dropped to 80% in the years following the study),[70] as well as on ethical grounds for the way the research was conducted.[98] In 2004, the MMR-and-autism interpretation of the paper was formally retracted by 10 of Wakefield's 12 coauthors,[99] and in 2010 The Lancet's editors fully retracted the paper.[100] Wakefield was struck off the UK medical register, with a statement identifying deliberate falsification in the research published in The Lancet,[101] and is barred from practising medicine in the UK.[102]
The CDC,[103] the IOM of the National Academy of Sciences,[92] and the UK National Health Service[104] have all concluded that there is no evidence of a link between the MMR vaccine and autism. A systematic review by the Cochrane Library concluded that there is no credible link between the MMR vaccine and autism, that MMR has prevented diseases that still carry a heavy burden of death and complications, that the lack of confidence in MMR has damaged public health, and that the design and reporting of safety outcomes in MMR vaccine studies are largely inadequate.[105]
In 2009, The Sunday Times reported that Wakefield had manipulated patient data and misreported results in his 1998 paper, creating the appearance of a link with autism.[106] A 2011 article in the British Medical Journal described how the data in the study had been falsified by Wakefield so that it would arrive at a predetermined conclusion.[107] An accompanying editorial in the same journal described Wakefield's work as an "elaborate fraud" that led to lower vaccination rates, putting hundreds of thousands of children at risk and diverting energy and money away from research into the true cause of autism.[108]
A special court convened in the United States to review claims under the National Vaccine Injury Compensation Program ruled on February 12, 2009 that parents of autistic children are not entitled to compensation in their contention that certain vaccines caused autism in their children.[109]
Vaccine overload
Vaccine overload is the notion that giving many vaccines at once may overwhelm or weaken a child's immature immune system and lead to adverse effects.[110] Despite scientific evidence that strongly contradicts this idea,[89] some parents of autistic children believe that vaccine overload causes autism.[111] The resulting controversy has caused many parents to delay or avoid immunizing their children.[110] Such parental misperceptions are major obstacles towards immunization of children.[112]
The concept of vaccine overload is flawed on several levels.[89] Despite the increase in the number of vaccines over recent decades, improvements in vaccine design have reduced the immunologic load from vaccines; the total number of immunological components in the 14 vaccines administered to US children in 2009 is less than 10% of what it was in the 7 vaccines given in 1980.[89] A study published in 2013 found no correlation between autism and the antigen number in the vaccines the children were administered up to the age of two. Of the 1,008 children in the study, one quarter of those diagnosed with autism were born between 1994 and 1999, when the routine vaccine schedule could contain more than 3,000 antigens (in a single shot of DTP vaccine). The vaccine schedule in 2012 contains several more vaccines, but the number of antigens the child is exposed to by the age of two is 315.[113][114] Vaccines pose a minuscule immunologic load compared to the pathogens naturally encountered by a child in a typical year;[89] common childhood conditions such as fevers and middle-ear infections pose a much greater challenge to the immune system than vaccines,[115] and studies have shown that vaccinations, even multiple concurrent vaccinations, do not weaken the immune system[89] or compromise overall immunity.[116] The lack of evidence supporting the vaccine overload hypothesis, combined with these findings directly contradicting it, has led to the conclusion that currently recommended vaccine programs do not "overload" or weaken the immune system.[1][117][118]
Any experiment based on withholding vaccines from children has been considered unethical,[119] and observational studies would likely be confounded by differences in the health care-seeking behaviours of under-vaccinated children. Thus, no study directly comparing rates of autism in vaccinated and unvaccinated children has been done. However, the concept of vaccine overload is biologically implausible, vaccinated and unvaccinated children have the same immune response to non-vaccine-related infections, and autism is not an immune-mediated disease, so claims that vaccines could cause it by overloading the immune system go against current knowledge of the pathogenesis of autism. As such, the idea that vaccines cause autism has been effectively dismissed by the weight of current evidence.[89]
Prenatal infection
There is evidence that schizophrenia is associated with prenatal exposure to rubella, influenza, and toxoplasmosis infection. For example, one study found a sevenfold increased risk of schizophrenia when mothers were exposed to influenza in the first trimester of gestation. This may have public health implications, as strategies for preventing infection include vaccination, antibiotics, and simple hygiene.[120] Based on studies in animal models, theoretical concerns have been raised about a possible link between schizophrenia and maternal immune response activated by virus antigens; a 2009 review concluded that there was insufficient evidence to recommend routine use of trivalent influenza vaccine during the first trimester of pregnancy, but that the vaccine was still recommended outside the first trimester and in special circumstances such as pandemics or in women with certain other conditions.[121] The CDC's Advisory Committee on Immunization Practices, the American College of Obstetricians and Gynecologists, and the American Academy of Family Physicians all recommend routine flu shots for pregnant women, for several reasons:[122]
- their risk for serious influenza-related medical complications during the last two trimesters;
- their greater rates for flu-related hospitalizations compared to non-pregnant women;
- the possible transfer of maternal anti-influenza antibodies to children, protecting the children from the flu; and
- several studies that found no harm to pregnant women or their children from the vaccinations.
Despite this recommendation, only 16% of healthy pregnant US women surveyed in 2005 had been vaccinated against the flu.[122]
Aluminium
Aluminium compounds are used as immunologic adjuvants to increase the effectiveness of many vaccines. The aluminium apparently simulates or causes small amounts of tissue damage, driving the body to respond more powerfully to what it sees as a serious infection and promoting the development of a lasting immune response.[123][124] In some cases these compounds have been associated with redness, itching, and low-grade fever,[123] but the use of aluminium in vaccines has not been associated with serious adverse events.[125] In some cases, aluminium-containing vaccines are associated with macrophagic myofasciitis (MMF), localized microscopic lesions containing aluminium salts that persist for up to 8 years. However, recent case-controlled studies have found no specific clinical symptoms in individuals with biopsies showing MMF, and there is no evidence that aluminium-containing vaccines are a serious health risk or justify changes to immunization practice.[125] Over the first six months of its life, an infant ingests more aluminium from dietary sources such as breast milk and infant formula than it does from vaccinations.[126][127]
Other safety concerns
Other safety concerns about vaccines have been published on the Internet, in informal meetings, in books, and at symposia. These include hypotheses that vaccination can cause sudden infant death syndrome, epileptic seizures, allergies, multiple sclerosis, and autoimmune diseases such as type 1 diabetes, as well as hypotheses that vaccinations can transmit bovine spongiform encephalopathy, hepatitis C virus, and HIV. These hypotheses have been investigated, with the conclusion that currently used vaccines meet high safety standards and that criticism of vaccine safety in the popular press is not justified.[118]
Individual liberty
Compulsory vaccination policies have provoked opposition at various times from people who say that governments should not infringe on an individual's freedom to choose medications, even if that choice increases the risk of disease to themselves and others.[2][128] If a vaccination program successfully reduces the disease threat, it may reduce the perceived risk of disease as cultural memories of the effects of that disease fade. At this point, parents may consider that they have nothing to lose by refusing vaccinations.[129] If enough people hope to become free-riders, gaining the benefits of herd immunity without vaccination, vaccination levels may drop to a level where herd immunity ceases to be as effective.[130]
In the United States, mandatory vaccination laws sometimes provoke reactions from members of anti-government or libertarian factions, who profess concern for what they view as the convergence or merger of the public and private sectors. They point to possible conflicts of interest due to vaccine research funding and misinformation that fuel debate on both sides (Wolfe, Sharpe). Others argue that, for compulsory vaccination to work to broadly prevent disease, there must be not only available vaccines and a population willing to immunize, but also sufficient ability to decline vaccination on grounds of personal belief.[131]
Vaccination offers ethical issues beyond the normal issues of a parent deciding on medical care for their children, as unvaccinated but asymptomatic or weakly infected individuals may spread disease to people (especially children and the elderly) with weaker immune systems, and to individuals in whom the vaccine has not been effective. For this reason, even where not required by law some schools and doctors' surgeries have prohibited parents with unvaccinated children from enrolling.[132][133]
Religion
Vaccination has been opposed on religious grounds ever since it was introduced, even when vaccination is not compulsory. Some Christian opponents argued, when vaccination was first becoming widespread, that if God had decreed that someone should die of smallpox, it would be a sin to thwart God's will via vaccination.[10] Religious opposition continues to the present day, on various grounds, raising ethical difficulties when the number of unvaccinated children threatens harm to the entire population.[134] Many governments allow parents to opt out of their children's otherwise mandatory vaccinations for religious reasons; some parents falsely claim religious beliefs to get vaccination exemptions.[135]
The Haredi burqa sect in Israel took a moral stand against vaccinations or medical treatments, which led to the death of at least one baby from untreated influenza.[136]
In the United States, there are currently only three states (Mississippi, West Virginia, and California) that do not provide exemptions based on religious beliefs.
The cell culture media of some viral vaccines, and the virus of the rubella vaccine, are derived from tissues taken from therapeutic abortions performed in the 1960s, leading to moral questions. For example, the principle of double effect, originated by Thomas Aquinas, holds that actions with both good and bad consequences are morally acceptable in specific circumstances, and the question is how this principle applies to vaccination.[137] The Vatican Curia has expressed concern about the rubella vaccine's embryonic cell origin, saying that Catholics have "a grave responsibility to use alternative vaccines and to make a conscientious objection with regard to those which have moral problems."[138] The Vatican concluded that until an alternative becomes available, it is acceptable for Catholics to use the existing vaccine, writing, "This is an unjust alternative choice, which must be eliminated as soon as possible."[138]
Alternative medicine
Many forms of alternative medicine are based on philosophies that oppose vaccination and have practitioners who voice their opposition. These include some elements of the chiropractic community, some homeopaths, and naturopaths.[46] The reasons for this negative vaccination view are complicated and rest at least in part on the early philosophies that shape the foundation of these groups.[46]
Chiropractic
Historically, chiropractic strongly opposed vaccination based on its belief that all diseases were traceable to causes in the spine and therefore could not be affected by vaccines. Daniel D. Palmer, the founder of chiropractic, wrote, "It is the very height of absurdity to strive to 'protect' any person from smallpox or any other malady by inoculating them with a filthy animal poison."[139] Vaccination remains controversial within the profession.[140] Although most chiropractic writings on vaccination focus on its negative aspects,[139] The American Chiropractic Association and the International Chiropractic Association support individual exemptions to compulsory vaccination laws; a 1995 survey of US chiropractors found that about one third believed there was no scientific proof that immunization prevents disease.[140] While the Canadian Chiropractic Association supports vaccination,[139] a survey in Alberta in 2002 found that 25% of chiropractors advised patients for, and 27% advised against, vaccinations for patients or their children.[141]
Although most chiropractic colleges try to teach about vaccination responsibly, several have faculty who seem to stress negative views.[140] A survey of a 1999–2000 cross-section of students of Canadian Memorial Chiropractic College (CMCC), which does not formally teach anti-vaccination views, reported that fourth-year students opposed vaccination more strongly than did first-year students, with 29.4% of fourth-year students opposing vaccination.[142] In a follow-up study on 2011–12 CMCC students, it was found that pro-vaccination attitudes heavily predominated. Students reported support rates ranging from 83.9% to 90%. This difference in attitude was proposed to be due to the lack of the previous influence of a "subgroup of some charismatic students who were enrolled at CMCC at the time, students who championed the Palmer postulates that advocated against the use of vaccination".[143]
Some chiropractic groups still oppose attempts to limit or eliminate nonmedical exemptions to vaccination. In March 2015, the Oregon Chiropractic Association invited Andrew Wakefield, chief author of a fraudulent research paper, to testify against Senate Bill 442,[144] "a bill that would eliminate nonmedical exemptions from Oregon's school immunization law."[145] The California Chiropractic Association lobbied against a 2015 bill ending belief exemptions for vaccines. They had also opposed a 2012 bill related to vaccination exemptions.[146]
Homeopathy
Several surveys have shown that some practitioners of homeopathy, particularly homeopaths without any medical training, advise patients against vaccination.[147] For example, a survey of registered homeopaths in Austria found that only 28% considered immunization an important preventive measure, and 83% of homeopaths surveyed in Sydney, Australia, did not recommend vaccination.[46] Many practitioners of naturopathy also oppose vaccination.[46]
Homeopathic "vaccines" (nosodes) are ineffective because they do not contain any active ingredients and thus do not stimulate the immune system. They can be dangerous if they take the place of effective treatments.[148] Some medical organizations have taken action against nosodes. In Canada, the labeling of homeopathic nosodes require the statement: "This product is neither a vaccine nor an alternative to vaccination."[149]
Financial motives
Alternative medicine proponents gain from promoting vaccine conspiracy theories through the sale of ineffective and expensive medications, supplements, and procedures such as chelation therapy and hyperbaric oxygen therapy, sold as able to cure the 'damage' caused by vaccines.[150] Homeopaths in particular gain through the promotion of water injections or 'nosodes' which are alleged to have a 'natural' vaccine-like effect.[151] Additional bodies with a vested interest in promoting the unsafeness of vaccines may include lawyers and legal groups organizing court cases and class action lawsuits against vaccine providers. Conversely, alternative medicine providers have accused the vaccine industry of misrepresenting the safety and effectiveness of vaccines, covering up and suppressing information, and influencing health policy decisions for financial gain.[2]
In the late 20th century, vaccines were a product with low profit margins,[152] and the number of companies involved in vaccine manufacture declined. In addition to low profits and liability risks, manufacturers complained about low prices paid for vaccines by the CDC and other US government agencies.[153] In the early 21st century, the vaccine market greatly improved with the approval of the vaccine Prevnar, along with a small number of other high-priced blockbuster vaccines, such as Gardasil and Pediarix, which each had sales revenues of over $1 billion in 2008.[152]
War
The United States has a very complex history with compulsory vaccination, particularly in enforcing compulsory vaccinations both domestically and abroad to protect American soldiers during times of war. There are hundreds of thousands of examples of soldier deaths that were not the result of combat wounds, but were instead from disease.[154] Among wars with high death tolls from disease is the Civil War where an estimated 620,000 soldiers died from disease. War ultimately becomes as much of a battle against disease as it is a battle against the enemy. American soldiers actively spread diseases in other countries that ultimately disrupted entire societies with inflicted famine, poverty, and disrupted entire healthcare systems.[154]
Spanish–American War
The Spanish–American War began in April 1898 and ended in August 1898. During this time the United States gained control of Cuba, Puerto Rico, and the Philippines from Spain. As a military police power and as colonizers the United States took a very hands-on approach in administering healthcare particularly vaccinations to natives during the invasion and conquest of these countries.[154] Although the Spanish–American War occurred during the era of "bacteriological revolution" where knowledge of disease was bolstered by germ theory more than half of the soldier casualties in this war were from disease.[154] Unknowingly American soldiers acted as agents of disease fostering bacteria in their haphazardly made camps. These soldiers invaded Cuba, Puerto Rico, and the Philippines and connected parts of these countries that had never before been connected due to the countries disperse nature thereby beginning epidemics.[154] The mobility of American soldiers around these countries encouraged a newfound mobility of disease that quickly infected natives.
Military personnel used Rudyard's Kipling's poem "The White Man's Burden" to explain their imperialistic actions in Cuba, the Philippines, and Puerto Rico and the need for the United States to help the "dark-skinned Barbarians"[154] reach modern sanitary standards. American actions abroad before, during, and after the war emphasized a need for proper sanitation habits especially on behalf of the natives. Natives who refuse to oblige with American health standards and procedures risked fines or imprisonment.[154] One penalty in Puerto Rico included a $10 fine for a failure to vaccinate and an additional $5 fine for any day you continue to be unvaccinated, refusal to pay resulted in ten or more days of imprisonment. If entire villages refused the army's current sanitation policy at any given time they risked being burnt to the ground in order to preserve the health and safety of soldiers from endemic smallpox and yellow fever.[154] Vaccines were forcibly administered in order to combat the barbaric health and nature of the uncivilized, dark skinned Puerto Ricans, Cubans, and Filipinos. Military personnel in Puerto Rico provided Public Health services which culminated in military orders that mandated vaccinations for children before they were six months as well as another order that issued a general vaccination order.[154] By the end of 1899 in Puerto Rico alone the U.S. military and other hired native vaccinators called practicantes, vaccinated an estimated 860,000 natives in a five-month period. This period began the United State's movement toward an expansion of medical practices that included "tropical medicine" in an attempt to protect the lives to soldiers abroad.[154]
See also
References
- ^ a b c d e f Bonhoeffer J, Heininger U (2007). "Adverse events following immunization: perception and evidence" (PDF). Current Opinion in Infectious Diseases. 20 (3): 237–46. doi:10.1097/QCO.0b013e32811ebfb0. PMID 17471032.
- ^ a b c d e f Wolfe R, Sharp L (2002). "Anti-vaccinationists past and present". BMJ. 325 (7361): 430–2. doi:10.1136/bmj.325.7361.430. PMC 1123944. PMID 12193361.
- ^ Poland GA, Jacobson RM (January 13, 2011). "The Age-Old Struggle against the Antivaccinationists". N Engl J Med. 364 (2): 97–9. doi:10.1056/NEJMp1010594. PMID 21226573.
- ^ Wallace A (October 19, 2009). "An epidemic of fear: how panicked parents skipping shots endangers us all". Wired. Retrieved October 21, 2009.
- ^ Poland G, Jacobson R (2001). "Understanding those who do not understand: a brief review of the anti-vaccine movement". Vaccine. 19 (17–19): 2440–5. doi:10.1016/S0264-410X(00)00469-2. PMID 11257375.
- ^ "Frequently Asked Questions (FAQ)". Boston Children's Hospital. Archived from the original on October 17, 2013. Retrieved February 11, 2014.
- ^ Flaherty DK (October 2011). "The vaccine-autism connection: a public health crisis caused by unethical medical practices and fraudulent science". Annals of Pharmacotherapy. 45 (10): 1302–4. doi:10.1345/aph.1Q318. PMID 21917556.
- ^ a b Allen, Arthur (2007). Vaccine: The Controversial Story of Medicine's Greatest Lifesaver. New York, NY: W. W. Norton & Company, Inc. pp. 25–36. ISBN 978-0-393-05911-3.
- ^ a b c d Williams, Gareth (2010). Angel Of Death; the story of smallpox. Basingstoke, UK: Palgrave Macmillan. pp. 87–94. ISBN 978 0 230 27471 6.
- ^ a b
Early religious opposition:
- White AD (1896). "Theological opposition to inoculation, vaccination, and the use of anæsthetics". A History of the Warfare of Science with Theology in Christendom. New York: Appleton.
{{cite book}}: External link in|chapterurl=|chapterurl=ignored (|chapter-url=suggested) (help) - Bazin H (2001). "The ethics of vaccine usage in society: lessons from the past". Endeavour. 25 (3): 104–8. doi:10.1016/S0160-9327(00)01376-4. PMID 11725304.
- Noble M (2005). "Ethics in the trenches: a multifaceted analysis of the stem cell debate". Stem Cell Rev. 1 (4): 345–76. doi:10.1385/SCR:1:4:345. PMID 17142878.
- White AD (1896). "Theological opposition to inoculation, vaccination, and the use of anæsthetics". A History of the Warfare of Science with Theology in Christendom. New York: Appleton.
- ^ Bazin, Hervé (October 1, 2003). "A brief history of the prevention of infectious diseases by immunisations". Comparative Immunology, Microbiology and Infectious Diseases. 26 (5–6): 293–308. doi:10.1016/S0147-9571(03)00016-X. PMID 12818618.
- ^ Ellner P (1998). "Smallpox: gone but not forgotten". Infection. 26 (5): 263–9. doi:10.1007/BF02962244. PMID 9795781.
- ^ a b c d Baxby, Derrick (2001). Smallpox Vaccine, Ahead of its Time. Berkeley, UK: the Jenner Museum. pp. 12–21. ISBN 0 9528695 1 9.
- ^ Bazin, Hervé (2000). The Eradication of Smallpox. London: Academic Press. p. 122. ISBN 0 12 083475 8.
- ^ Creighton, Charles (1887). The Natural History of Cowpox and Vaccinal Syphilis. London: Cassell.
- ^ a b Williamson, Stanley (2007). The Vaccination Controversy; the rise, reign and decline of compulsory vaccination. Liverpool: Liverpool University Press. ISBN 9781846310867.
- ^ a b c d Porter, Dorothy; Porter, Roy (1988). "The Politics of Prevention; anti-vaccinationism and public health in nineteenth-century England". Med. Hist. 32: 231–52. doi:10.1017/s0025727300048225. PMC 1139881. PMID 3063903.
- ^ Durbach, Nadjya (2000). "They might as well brand us; working-class resistance to compulsory vaccination in Victorian England". Soc. Hist. Med. 13 (1): 45–63. doi:10.1093/shm/13.1.45. PMID 11624425.
- ^ a b Baxby, Derrick (1999). "The End of Smallpox". History Today. 49: 14–16.
- ^ (Royal Commission) (1898). Vaccination and its Results; a Report based on the Evidence taken by the Royal Commission. London: New Sydenham Society.
- ^ "Labour Party Manifesto 1900". Voice of Anti-Capitalism in Guildford. Retrieved July 2, 2015.
- ^ a b Millard, C. Killick (1948). "The End of Compulsory Vaccination". Brit. Med. J. 2: 1073–5. doi:10.1136/bmj.2.4589.1073. PMC 2092290. PMID 18121624.
- ^ Fraser, Stuart M.F. (1980). "Leicester and Smallpox: the Leicester Method". Med. Hist. 24: 315–32. doi:10.1017/s0025727300040345. PMC 1082657. PMID 6997656.
- ^ Fenner, Frank; Henderson, D.A.; Arita, I.; Jezek, Z.; Ladnyi, I.D. (1988). Smallpox and its Eradication. Geneva: World Health Organization. pp. 247, 275. ISBN 92 4 156110 6.
- ^ Henderson, Donald, A. (2009). Smallpox; the death of a disease. Amherst, N.Y.: Prometheus Books. pp. 90–92. ISBN 978 1 59102 722 5.
{{cite book}}: CS1 maint: multiple names: authors list (link) - ^ Henderson DA, Moss B. Public health. In: Plotkin SA, Orenstein WA. Vaccines. 3rd ed. Philadelphia: 1999. ISBN 0-7216-7443-7.
- ^ Robert M. Wolfe and Lisa K Sharp (August 24, 2002). "Anti-vaccinationists past and present". BMJ. 325: 430–2. doi:10.1136/bmj.325.7361.430. PMC 1123944. PMID 12193361.
In 1879, after a visit to New York by William Tebb, the leading British anti-vaccinationist, the Anti-Vaccination Society of America was founded. Subsequently, the New England Anti-Compulsory Vaccination League was formed in 1882 and the Anti-Vaccination League of New York City in 1885.
- ^ a b "History of Anti-vaccination Movements". College of Physicians of Philadelphia. March 8, 2012. Retrieved February 11, 2015.
The Anti Vaccination Society of America was founded in 1879, following a visit to America by leading British anti-vaccinationist William Tebb. Two other leagues, the New England Anti Compulsory Vaccination League (1882) and the Anti-Vaccination League of New York City (1885) followed. ...
- ^ Kaufman, M. (1967). "The American Anti-vaccinionationists and their Arguments". Bull. Hist. Med. 41: 463–78. PMID 4865041.
- ^ Hopkins, Donald R. (2002). The Greatest Killer; smallpox in history. Chicago: University of Chicago Press. pp. 83–4. ISBN 0226351661.
- ^ Pitcairn J (1907). Vaccination. Anti-Vaccination League of Pennsylvania. OCLC 454411147.
- ^ a b Higgins CM (1920). "Life sketch of John Pitcairn by a Philadelphia friend". Horrors of Vaccination Exposed and Illustrated. Brooklyn, NY: C. M. Higgins. pp. 73–5. OCLC 447437840.
- ^ Meade T (1989). "'Living worse and costing more': resistance and riot in Rio de Janeiro, 1890–1917". J Lat Am Stud. 21 (2): 241–66. doi:10.1017/S0022216X00014784.
- ^ Lilienfield, D.E. (2008). "The First Pharmacoepidemiologic Investigations: national drug safety policy in the United States, 1901–1902". Perspect. Biol. Med. 51 (2): 188–98. doi:10.1353/pbm.0.0010. PMID 18453724.
- ^ Gradman, Christopher (2009). Laboratory Disease; Robert Koch's medical bacteriology. Baltimore: Johns Hopkins University Press. pp. 133–6. ISBN 978 0 8018 9313 1.
- ^ Offit, Paul A (April 7, 2005). "The Cutter Incident, 50 Years Later". New England Journal of Medicine. 352 (14): 1411–2. doi:10.1056/NEJMp048180. PMID 15814877.
- ^ "Scientist: autism paper had catastrophic effects". NPR. February 7, 2010.
- ^ Goldacre B (August 30, 2008). "The MMR hoax". The Guardian. London. Archived from the original on August 30, 2008. Retrieved August 30, 2008.
- ^ Knox, Richard (September 19, 2011). "HPV Vaccine: The Science Behind The Controversy". NPR. Retrieved September 30, 2015.
- ^ Chatterjee, Archana; O’Keefe, Catherine (May 2010). "Current controversies in the USA regarding vaccine safety". Expert Review of Vaccines. 9 (5): 497–502. doi:10.1586/erv.10.36.
- ^ Fenner F, Henderson DA, Arita I, Ježek Z, Ladnyi, ID (1988). Smallpox and its Eradication (PDF). Geneva: World Health Organization. ISBN 92-4-156110-6. Retrieved September 4, 2007.
{{cite book}}: CS1 maint: multiple names: authors list (link) - ^ Sutter RW, Maher C (2006). "Mass vaccination campaigns for polio eradication: an essential strategy for success". Curr Top Microbiol Immunol. Current Topics in Microbiology and Immunology. 304: 195–220. doi:10.1007/3-540-36583-4_11. ISBN 978-3-540-29382-8. PMID 16989271.
- ^ Centers for Disease Control and Prevention (CDC) (2002). "Progress toward elimination of Haemophilus influenzae type b invasive disease among infants and children—United States, 1998–2000". MMWR Morb Mortal Wkly Rep. 51 (11): 234–7. PMID 11925021.
- ^ Park A (May 21, 2008). "How safe are vaccines?". Time.
- ^ a b "Some common misconceptions about vaccination and how to respond to them". National Center for Immunization and Respiratory Diseases, Centers for Disease Control and Prevention. Retrieved September 28, 2012.
- ^ a b c d e Ernst E (2001). "Rise in popularity of complementary and alternative medicine: reasons and consequences for vaccination". Vaccine. 20 (Suppl 1): S89–93. doi:10.1016/S0264-410X(01)00290-0. PMID 11587822.
- ^ Wane, Joanna. "The case for vaccination" (PDF). North & South. Retrieved July 3, 2015.
- ^ Heymann DL, Aylward RB (2006). "Mass vaccination: when and why". Curr Top Microbiol Immunol. Current Topics in Microbiology and Immunology. 304: 1–16. doi:10.1007/3-540-36583-4_1. ISBN 978-3-540-29382-8. PMID 16989261.
- ^ http://www.cdc.gov/features/ReasonsToVaccinate
- ^ Zhou F, Santoli J, Messonnier ML, et al. (2005). "Economic evaluation of the 7-vaccine routine childhood immunization schedule in the United States, 2001". Arch Pediatr Adolesc Med. 159 (12): 1136–44. doi:10.1001/archpedi.159.12.1136. PMID 16330737.
- ^ a b Gangarosa EJ, Galazka AM, Wolfe CR, et al. (1998). "Impact of anti-vaccine movements on pertussis control: the untold story". Lancet. 351 (9099): 356–61. doi:10.1016/S0140-6736(97)04334-1. PMID 9652634.
- ^ a b Allen A (2002). "Bucking the herd". The Atlantic. 290 (2): 40–2. Retrieved November 7, 2007.
- ^ "What would happen if we stopped vaccinations?". Centers for Disease Control and Prevention. June 12, 2007. Retrieved April 25, 2008.
- ^ Centers for Disease Control and Prevention (2007). "Pertussis". In Atkinson W, Hamborsky J, McIntyre L, Wolfe S (ed.). Epidemiology and Prevention of Vaccine-Preventable Diseases. Washington, DC: Public Health Foundation. ISBN 0-01-706605-0.
{{cite book}}: External link in|chapterurl=|chapterurl=ignored (|chapter-url=suggested) (help)CS1 maint: multiple names: editors list (link) - ^ Nelson MC, Rogers J (1992). "The right to die? Anti-vaccination activity and the 1874 smallpox epidemic in Stockholm". Soc Hist Med. 5 (3): 369–88. doi:10.1093/shm/5.3.369. PMID 11645870.
- ^ Grabenstein, John D.; Pittman, Phillip R.; Greenwood, John T.; Engler, Renata J. M. (August 1, 2006). "Immunization to Protect the US Armed Forces: Heritage, Current Practice, and Prospects". Epidemiologic Reviews. 28 (1): 3–26. doi:10.1093/epirev/mxj003. ISSN 0193-936X. PMID 16763072.
- ^ "The Night the Viet Cong Stopped the War". History Net: Where History Comes Alive - World & US History Online. Retrieved November 18, 2015.
- ^ Centers for Disease Control and Prevention (2000). "Measles outbreak—Netherlands, April 1999 – January 2000". MMWR Morb Mortal Wkly Rep. 49 (14): 299–303. PMID 10825086.
- ^ Pepys MB (2007). "Science and serendipity". Clin Med. 7 (6): 562–78. doi:10.7861/clinmedicine.7-6-562. PMID 18193704.
- ^ Ireland measles outbreak:
- "Measles outbreak feared". BBC News. May 30, 2000.
- McBrien J, Murphy J, Gill D, Cronin M, O'Donovan C, Cafferkey M (2003). "Measles outbreak in Dublin, 2000". Pediatr Infect Dis J. 22 (7): 580–4. doi:10.1097/00006454-200307000-00002. PMID 12867830.
{{cite journal}}: CS1 maint: multiple names: authors list (link)
- ^ Clements CJ, Greenough P, Shull D (2006). "How vaccine safety can become political – the example of polio in Nigeria" (PDF). Curr Drug Saf. 1 (1): 117–9. doi:10.2174/157488606775252575. PMID 18690921.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ "Wild poliovirus 2000–2008" (PDF). Global Polio Eradication Initiative. February 5, 2008. Archived from the original (PDF) on September 27, 2007. Retrieved February 11, 2008.
- ^ "'Hundreds' dead in measles outbreak". IRIN. December 14, 2007. Retrieved February 10, 2008.
- ^ Parker A, Staggs W, Dayan G, et al. (2006). "Implications of a 2005 measles outbreak in Indiana for sustained elimination of measles in the United States". N Engl J Med. 355 (5): 447–55. doi:10.1056/NEJMoa060775. PMID 16885548.
- ^ Fair E, Murphy TV, Golaz A, Wharton M (2002). "Philosophic objection to vaccination as a risk for tetanus among children younger than 15 years". Pediatrics. 109 (1): e2. doi:10.1542/peds.109.1.e2. PMID 11773570.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ "Frequently Asked Questions about Measles in U.S." Centers for Disease Control and Prevention.
- ^ Jaslow, Ryan (September 12, 2013). "CDC: Vaccine "philosophical differences" driving up U.S. measles rates". CBS News. Retrieved September 19, 2013.
- ^ Centers for Disease Control and Prevention (September 13, 2013). "National, State, and Local Area Vaccination Coverage Among Children Aged 19–35 Months – United States, 2012". Morbidity and Mortality Weekly Report. 62 (36): 741–3. PMID 24025754.
- ^ Rañoa R, Zarracina J (January 15, 2015). "The spread of Disneyland measles outbreak". Los Angeles Times.
- ^ a b Alazraki M (January 12, 2011). "The Autism Vaccine Fraud: Dr. Wakefield's Costly Lie to Society". DailyFinance, AOL Money & Finance.
- ^ "Measles outbreak worsens in US after unvaccinated woman visits Disneyland". January 19, 2015. Retrieved June 1, 2015.
- ^ "Measles — United States, January 1–May 23, 2014". MMWR Morb. Mortal. Wkly. Rep. 63 (22): 496–9. 2014. PMID 24898167.
{{cite journal}}: Unknown parameter|authors=ignored (help) - ^ a b CDC (June 30, 2015). "Measles Cases and Outbreaks". CDC. Retrieved July 2, 2015.
- ^ Press Release (July 2, 2015). "Measles led to death of Clallam Co. woman; first in US in a dozen years". Washington Department of Health.
- ^ a b "Swansea measles epidemic officially over". BBC News. July 3, 2013. Retrieved October 8, 2014.
Large numbers of children in the 10–18 age group were not given the MMR vaccine as babies, the result of a scare that caused panic among parents. It followed research by Dr Andrew Wakefield in the late 1990s which linked the vaccine with autism and bowel disease. His report, which was published in The Lancet medical journal, was later discredited, with health officials insisting the vaccine was completely safe.
- ^ "Swansea measles epidemic: Worries over MMR uptake after outbreak". BBC News. July 10, 2013. Retrieved October 8, 2014.
- ^ "Tackling negative perceptions towards vaccination". Lancet Infect Dis. 7 (4): 235. 2007. doi:10.1016/S1473-3099(07)70057-9. PMID 17376373.
- ^ "Possible Side-effects from Vaccines". Centers for Disease Control and Prevention. August 26, 2013. Retrieved January 3, 2014.
- ^ Chen, Robert T.; Hibbs, Beth (July 1998). "Vaccine Safety: Current and Future Challenges". Pediatric Annals. 27 (7). Retrieved January 3, 2014.
- ^ Mooney C (June 2009). "Why does the vaccine/autism controversy live on?". Discover.
- ^ Leask J, Chapman S, Cooper Robbins SC. "All manner of ills": The features of serious diseases attributed to vaccination. Vaccine. 2009. doi:10.1016/j.vaccine.2009.10.042. PMID 19879997.
- ^ Goldacre, Ben (2009). Bad Science. London: Fourth Estate. pp. 292–294. ISBN 9780007284870.
- ^ Boseley, Sarah (February 2, 2010). "Lancet retracts 'utterly false' MMR paper". The Guardian. Retrieved February 2, 2010.
- ^ Taylor, Luke E.; Swerdfeger, Amy L.; Eslick, Guy D. (June 2014). "Vaccines are not associated with autism: An evidence-based meta-analysis of case-control and cohort studies". Vaccine. 32 (29): 3623–9. doi:10.1016/j.vaccine.2014.04.085. PMID 24814559.
- ^ Baker JP (2008). "Mercury, Vaccines, and Autism: One Controversy, Three Histories". Am J Public Health. 98 (2): 244–53. doi:10.2105/AJPH.2007.113159. PMC 2376879. PMID 18172138.
- ^ a b Offit PA (2007). "Thimerosal and vaccines—a cautionary tale". N Engl J Med. 357 (13): 1278–9. doi:10.1056/NEJMp078187. PMID 17898096.
- ^ http://www.fda.gov/BiologicsBloodVaccines/SafetyAvailability/VaccineSafety/UCM096228
- ^ Bose-O'Reilly S, McCarty KM, Steckling N, Lettmeier B. "Mercury Exposure and Children's Health". Curr Probl Pediatr Adolesc Health Care. Retrieved July 4, 2015.
- ^ a b c d e f g Gerber JS, Offit PA (2009). "Vaccines and Autism: A Tale of Shifting Hypotheses". Clin Infect Dis. 48 (4): 456–61. doi:10.1086/596476. PMC 2908388. PMID 19128068.
{{cite journal}}: Unknown parameter|laydate=ignored (help); Unknown parameter|laysource=ignored (help); Unknown parameter|laysummary=ignored (help) - ^ Doja A, Roberts W (2006). "Immunizations and autism: a review of the literature". Can J Neurol Sci. 33 (4): 341–6. doi:10.1017/s031716710000528x. PMID 17168158.
- ^ Sugarman SD (2007). "Cases in vaccine court—legal battles over vaccines and autism". N Engl J Med. 357 (13): 1275–7. doi:10.1056/NEJMp078168. PMID 17898095.
- ^ a b Immunization Safety Review Committee (2004). Immunization Safety Review: Vaccines and Autism. The National Academies Press. ISBN 0-309-09237-X.
- ^ Wakefield A, Murch S, Anthony A, et al. (1998). "Ileal-lymphoid-nodular hyperplasia, non-specific colitis, and pervasive developmental disorder in children". Lancet. 351 (9103): 637–41. doi:10.1016/S0140-6736(97)11096-0. PMID 9500320. Retrieved September 5, 2007. (Retracted)
- ^ National Health Service (2004). "MMR: myths and truths". Retrieved September 3, 2007.
- ^ Deer B (February 22, 2004). "Revealed: MMR research scandal". The Sunday Times. Retrieved September 23, 2007.
- ^ Horton R (2004). "The lessons of MMR". Lancet. 363 (9411): 747–9. doi:10.1016/S0140-6736(04)15714-0. PMID 15016482.
- ^ "Doctors issue plea over MMR jab". BBC News. June 26, 2006. Retrieved November 23, 2007.
- ^ "MMR scare doctor 'paid children'". BBC News. July 16, 2007.
- ^ Murch SH, Anthony A, Casson DH, et al. (2004). "Retraction of an interpretation". Lancet. 363 (9411): 750. doi:10.1016/S0140-6736(04)15715-2. PMID 15016483.
- ^ The Editors Of The Lancet (February 2010). "Retraction—Ileal-lymphoid-nodular hyperplasia, non-specific colitis, and pervasive developmental disorder in children". Lancet. 375 (9713): 445. doi:10.1016/S0140-6736(10)60175-4. PMID 20137807.
{{cite journal}}:|last1=has generic name (help); Unknown parameter|laydate=ignored (help); Unknown parameter|laysource=ignored (help); Unknown parameter|laysummary=ignored (help) - ^ "General Medical Council, Fitness to Practise Panel Hearing, 24 May 2010, Andrew Wakefield, Determination of Serious Professional Misconduct" (PDF). General Medical Council. Retrieved September 18, 2011.
- ^ Meikle, James; Boseley, Sarah (May 24, 2010). "MMR row doctor Andrew Wakefield struck off register". The Guardian. London. Archived from the original on May 27, 2010. Retrieved May 24, 2010.
{{cite news}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ "Concerns about autism". Centers for Disease Control and Prevention. January 15, 2010.
- ^ MMR Fact Sheet, from the United Kingdom National Health Service. Retrieved June 13, 2007.
- ^ Demicheli V, Rivetti A, Debalini MG, Di Pietrantonj C (2012). Demicheli, Vittorio (ed.). "Vaccines for measles, mumps and rubella in children". Cochrane Database Syst Rev. 2: CD004407. doi:10.1002/14651858.CD004407.pub3. PMID 22336803.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Deer B (February 8, 2009). "MMR doctor Andrew Wakefield fixed data on autism". Sunday Times. Retrieved February 9, 2009.
- ^ Deer B (2011). "How the case against the MMR vaccine was fixed". BMJ. 342: c5347. doi:10.1136/bmj.c5347. PMID 21209059.
- ^ Godlee F, Smith J, Marcovitch H (2011). "Wakefield's article linking MMR vaccine and autism was fraudulent". BMJ. 342:c7452: c7452. doi:10.1136/bmj.c7452. PMID 21209060.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Vaccine court and autism:
- "Vaccine didn't cause autism, court rules". CNN. February 12, 2009. Retrieved February 12, 2009.
- Theresa Cedillo and Michael Cedillo, as parents and natural guardians of Michelle Cedillo vs. Secretary of Health and Human Services, 98-916V (United States Court of Federal Claims 2009-02-12).
- ^ a b Hilton S, Petticrew M, Hunt K (2006). "'Combined vaccines are like a sudden onslaught to the body's immune system': parental concerns about vaccine 'overload' and 'immune-vulnerability'". Vaccine. 24 (20): 4321–7. doi:10.1016/j.vaccine.2006.03.003. PMID 16581162.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Hurst L (October 30, 2009). "Vaccine phobia runs deep". Toronto Star. Retrieved November 4, 2009.
- ^ Heininger U (2006). "An internet-based survey on parental attitudes towards immunization". Vaccine. 24 (37–39): 6351–5. doi:10.1016/j.vaccine.2006.05.029. PMID 16784799.
- ^ Willingham, Emily (March 29, 2013). "Vaccines Not Linked To Autism. Again". Forbes. Retrieved April 4, 2013.
- ^ DeStefano, Frank; Price, Cristofer; Weintraub, Eric (April 1, 2013). "Increasing Exposure to Antibody-Stimulating Proteins and Polysaccharides in Vaccines Is Not Associated with Risk of Autism" (PDF). Journal of Pediatrics. 163 (2): 561–7. doi:10.1016/j.jpeds.2013.02.001. PMID 23545349. Retrieved April 4, 2013.
- ^ Immune challenges:
- Murphy TF (1996). "Branhamella catarrhalis: epidemiology, surface antigenic structure, and immune response" (PDF). Microbiol Rev. 60 (2): 267–79. PMC 239443. PMID 8801433.
- Sloyer JL, Howie VM, Ploussard JH, Ammann AJ, Austrian R, Johnston RB (1974). "Immune Response to Acute Otitis Media in Children I. Serotypes Isolated and Serum and Middle Ear Fluid Antibody in Pneumococcal Otitis Media" (PDF). Infect Immun. 9 (6): 1028–32. PMC 414928. PMID 4151506.
{{cite journal}}: CS1 maint: multiple names: authors list (link)
- ^ Vaccine burden:
- Miller E, Andrews N, Waight P, Taylor B (2003). "Bacterial infections, immune overload, and MMR vaccine". Arch Dis Child. 88 (3): 222–3. doi:10.1136/adc.88.3.222. PMC 1719482. PMID 12598383.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Hviid A, Wohlfahrt J, Stellfeld M, Melbye M (2005). "Childhood vaccination and nontargeted infectious disease hospitalization". JAMA. 294 (6): 699–705. doi:10.1001/jama.294.6.699. PMID 16091572.
{{cite journal}}: CS1 maint: multiple names: authors list (link)
- Miller E, Andrews N, Waight P, Taylor B (2003). "Bacterial infections, immune overload, and MMR vaccine". Arch Dis Child. 88 (3): 222–3. doi:10.1136/adc.88.3.222. PMC 1719482. PMID 12598383.
- ^ Vaccine schedules and "overload":
- Gregson AL, Edelman R (2003). "Does antigenic overload exist? The role of multiple immunizations in infants". Immunol Allergy Clin North Am. 23 (4): 649–64. doi:10.1016/S0889-8561(03)00097-3. PMID 14753385.
- Offit PA, Quarles J, Gerber MA, et al. (2002). "Addressing parents' concerns: do multiple vaccines overwhelm or weaken the infant's immune system?". Pediatrics. 109 (1): 124–9. doi:10.1542/peds.109.1.124. PMID 11773551.
- ^ a b Schneeweiss B, Pfleiderer M, Keller-Stanislawski B (2008). "Vaccination Safety Update". Dtsch Arztebl Int. 105 (34–5): 590–5. doi:10.3238/arztebl.2008.0590. PMC 2680557. PMID 19471677.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Deen, J. L.; Clemens, J. D. (2006). "Issues in the design and implementation of vaccine trials in less developed countries". Nature Reviews Drug Discovery. 5 (11): 932–940. doi:10.1038/nrd2159. PMID 17080029.
- ^ Fineberg AM, Ellman LM (May 2013). "Inflammatory cytokines and neurological and neurocognitive alterations in the course of schizophrenia". Biol. Psychiatry. 73 (10): 951–66. doi:10.1016/j.biopsych.2013.01.001. PMC 3641168. PMID 23414821.
- ^ Skowronski DM, De Serres G (2009). "Is routine influenza immunization warranted in early pregnancy?". Vaccine. 27 (35): 4754–70. doi:10.1016/j.vaccine.2009.03.079. PMID 19515466.
- ^ a b Fiore AE, Shay DK, Haber P, Iskander JK, Uyeki TM, Mootrey G, Bresee JS, Cox NJ, Advisory Committee on Immunization Practices (ACIP), Centers for Disease Control and Prevention (CDC) (2007). "Prevention and control of influenza: recommendations of the Advisory Committee on Immunization Practices (ACIP), 2007". MMWR Recomm Rep. 56 (RR–6): 1–54. PMID 17625497.
- ^ a b Baylor, N.; Egan, W.; Richman, P. (2002). "Aluminum salts in vaccines?US perspective*1". Vaccine. 20: S18–x20. doi:10.1016/S0264-410X(02)00166-4. PMID 12184360.
- ^ Leslie M (2013). "Solution to Vaccine Mystery Starts to Crystallize". Science. 341: 26–27. doi:10.1126/science.341.6141.26.
- ^ a b François, G.; Duclos, P.; Margolis, H.; Lavanchy, D.; Siegrist, C. A.; Meheus, A. ?; Lambert, P. H.; Emiroğlu, N.; Badur, S.; Van Damme, P. (2005). "Vaccine Safety Controversies and the Future of Vaccination Programs". The Pediatric Infectious Disease Journal. 24 (11): 953–961. doi:10.1097/01.inf.0000183853.16113.a6. PMID 16282928.
{{cite journal}}: Unknown parameter|displayauthors=ignored (|display-authors=suggested) (help) - ^ Offit, P.; Moser, C. (2009). "The problem with Dr Bob's alternative vaccine schedule". Pediatrics. 123 (1): e164–e169. doi:10.1542/peds.2008-2189. PMID 19117838. lay summary
- ^ "Vaccine Education Center: Vaccines and Aluminum". Children's Hospital of Philadelphia. April 2013. Retrieved October 29, 2013.
- ^ Colgrove J, Bayer R (2005). "Manifold Restraints: Liberty, Public Health, and the Legacy of Jacobson v Massachusetts". Am J Public Health. 95 (4): 571–6. doi:10.2105/AJPH.2004.055145. PMC 1449222. PMID 15798111.
- ^ Fine PE, Clarkson JA (1986). "Individual versus public priorities in the determination of optimal vaccination policies". Am J Epidemiol. 124 (6): 1012–20. PMID 3096132.
- ^ Buttenheim, AM; Asch, DA (December 2013). "Making vaccine refusal less of a free ride". Human vaccines & immunotherapeutics. 9 (12): 2674–5. doi:10.4161/hv.26676. PMC 4162060. PMID 24088616.
- ^ Salmon Daniel A; et al. "Compulsory vaccination and conscientious or philosophical exemptions: past, present, and future". The Lancet. 367 (9508): 436–442. doi:10.1016/s0140-6736(06)68144-0.
- ^ "Should Pediatricians Refuse Unvaccinated Kids?". The Huffington Post. Retrieved July 4, 2015.
- ^ Bachai, Sabrina. "NYC Schools Are Now Allowed To Ban Unvaccinated Kids, Rules Federal Judge". Medical Daily. Retrieved July 4, 2015.
- ^ May T, Silverman RD (2005). "Free-riding, fairness and the rights of minority groups in exemption from mandatory childhood vaccination" (PDF). Hum Vaccin. 1 (1): 12–5. doi:10.4161/hv.1.1.1425. PMID 17038833.
- ^ LeBlanc S (October 17, 2007). "Parents use religion to avoid vaccines". USA Today. Retrieved November 24, 2007.
- ^ "Haredi Burka Cult Family Flees After Baby Dies From Alleged Neglect".
- ^ Grabenstein JD (1999). "Moral considerations with certain viral vaccines" (PDF). Christ Pharm. 2 (2): 3–6. ISSN 1094-9534. Retrieved May 11, 2009.
- ^ a b Pontifical Academy for Life (2005). "Moral reflections on vaccines prepared from cells derived from aborted human foetuses". Medicina e Morale. Center for Bioethics, Catholic University of the Sacred Heart. Archived from the original on May 7, 2006. Retrieved December 3, 2008.
- ^ a b c Busse JW, Morgan L, Campbell JB (2005). "Chiropractic antivaccination arguments". J Manipulative Physiol Ther. 28 (5): 367–73. doi:10.1016/j.jmpt.2005.04.011. PMID 15965414.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ a b c Campbell JB, Busse JW, Injeyan HS (2000). "Chiropractors and vaccination: a historical perspective". Pediatrics. 105 (4): e43. doi:10.1542/peds.105.4.e43. PMID 10742364.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Russell ML, Injeyan HS, Verhoef MJ, Eliasziw M (2004). "Beliefs and behaviours: understanding chiropractors and immunization". Vaccine. 23 (3): 372–9. doi:10.1016/j.vaccine.2004.05.027. PMID 15530683.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Busse JW, Wilson K, Campbell JB (2008). "Attitudes towards vaccination among chiropractic and naturopathic students". Vaccine. 26 (49): 6237–42. doi:10.1016/j.vaccine.2008.07.020. PMID 18674581.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Lameris M, Schmidt C, Gleberzon B, Ogrady J; Schmidt; Gleberzon; Ogrady (2013). "Attitudes toward vaccination: A cross-sectional survey of students at the Canadian Memorial Chiropractic College". J Can Chiropr Assoc. 57 (3): 214–220. PMC 3743647. PMID 23997247.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Yoo, Saerom (February 24, 2015), "Vaccine researcher Wakefield to testify in Oregon", Statesman Journal, retrieved March 3, 2015
- ^ Yoo, Saerom (February 26, 2015), "Meeting on vaccine mandate bill canceled", Statesman Journal, retrieved March 3, 2015
- ^ Mason, Melanie (March 5, 2015), "Chiropractors lobby against bill ending belief exemptions for vaccines", Los Angeles Times, retrieved March 6, 2015
- ^ Schmidt K, Ernst E (2003). "MMR vaccination advice over the Internet". Vaccine. 21 (11–12): 1044–7. doi:10.1016/S0264-410X(02)00628-X. PMID 12559777.
- ^ Crislip, Mark (November 5, 2010). "Homeopathic Vaccines".
- ^ Stop Nosodes/Bad Science Watch (August 2015). "Nosode Use in Canada".
- ^ Kerr MA (2009). "Movement impact". The Autism Spectrum Disorders / vaccine link debate: a health social movement (PDF). University of Pittsburgh. pp. 194–203. Archived from the original (PDF) on July 18, 2011. Retrieved February 25, 2010.
- ^ Weeks, Carly. "Health experts question lack of crackdown on 'homeopathic vaccines'". The Globe and Mail. Retrieved July 4, 2015.
- ^ a b Sheridan C (2009). "Vaccine market boosters". Nat Biotechnol. 27 (6): 499–501. doi:10.1038/nbt0609-499. PMID 19513043.
- ^ Allen A (2007). "Epilogue: our best shots". Vaccine: the Controversial Story of Medicine's Greatest Lifesafer. W. W. Norton. pp. 421–42. ISBN 0-393-05911-1.
- ^ a b c d e f g h i j Willrich, Michael (2010). Pox: An American History. New York, New York: Penguin Group. pp. 117–165. ISBN 9781101476222.
Further reading
- Largent, Mark A. (2012). Vaccine: The Debate in Modern America. Johns Hopkins University Press. ISBN 978-1421406077.
- Bedford H, Elliman D (2000). "Concerns about immunisation". BMJ. 320 (7229): 240–3. doi:10.1136/bmj.320.7229.240. PMC 1117437. PMID 10642238.
- Davies P, Chapman S, Leask J (2002). "Antivaccination activists on the world wide web". Arch Dis Child. 87 (1): 22–5. doi:10.1136/adc.87.1.22. PMC 1751143. PMID 12089115.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Elliman D, Bedford H (2004). "MMR: Science and Fiction. Exploring the Vaccine Crisis; MMR and Autism: What Parents Need to Know". BMJ. 329 (7473): 1049. doi:10.1136/bmj.329.7473.1049.
- Friedlander E (2007). "The anti-immunization activists: a pattern of deception". Retrieved November 13, 2007.
- Hanratty B, Holt T, Duffell E, Patterson W, Ramsay M, White J, Jin L, Litton P (2000). "UK measles outbreak in non-immune anthroposophic communities: the implications for the elimination of measles from Europe". Epidemiol Infect. 125 (2): 377–83. doi:10.1017/S0950268899004525. PMC 2869610. PMID 11117961.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Herlihy, Stacy Mintzer; Hagood, E. Allison; Offit, Paul A. (2012). Your Baby's Best Shot: Why Vaccines Are Safe and Save Lives. Rowman & Littlefield Publishers. ISBN 978-1442215788.
- Miller, C. L. (1985). "Deaths from measles in England and Wales, 1970–83". Br Med J (Clin Res Ed). 290 (6466): 443–4. doi:10.1136/bmj.290.6466.443. PMC 1417782. PMID 3918622.
- Myers MG, Pineda D (2008). Do Vaccines Cause That?! A Guide for Evaluating Vaccine Safety Concerns. Galveston, TX: Immunizations for Public Health (i4ph). ISBN 0-9769027-1-0.
- Naono, Atsuko, (2006). "Vaccination Propaganda: The Politics of Communicating Colonial Medicine in Nineteenth-Century Burma" (PDF). SOAS Bulletin of Burma Research. 4 (1): 30–44.
{{cite journal}}: CS1 maint: extra punctuation (link) CS1 maint: multiple names: authors list (link) - Offit, Paul A. (2008). Autism's False Prophets: Bad Science, Risky Medicine, and the Search for a Cure. Columbia University Press. ISBN 978-0-231-14636-4.
- Offit, Paul A. (2012). Deadly Choices: How the Anti-Vaccine Movement Threatens Us All. Basic Books. ISBN 978-0465029624.
- Orenstein W, Hinman A (1999). "The immunization system in the United States – the role of school immunization laws". Vaccine. 17 Suppl 3: S19–24. doi:10.1016/S0264-410X(99)00290-X. PMID 10559531.
- Spier R (1998). "Ethical aspects of vaccines and vaccination". Vaccine. 16 (19): 1788–94. doi:10.1016/S0264-410X(98)00169-8. PMID 9795382.
- Vermeersch E (1999). "Individual rights versus societal duties". Vaccine. 17 (Suppl 3): S14–7. doi:10.1016/s0264-410x(99)00289-3. PMID 10627239.
- Wolfe RM, Sharp LK, Lipsky MS (2002). "Content and design attributes of antivaccination web sites". JAMA. 287 (24): 3245–8. doi:10.1001/jama.287.24.3245. PMID 12076221.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - "Six common misconceptions about immunization". World Health Organization. February 16, 2006. Retrieved November 2, 2006.
- Lewandowsky et al. Anti-Vax Psychology Study Report. - Mooney, Chris (October 2, 2013). "If You Distrust Vaccines, You're More Likely to Think NASA Faked the Moon Landings". Mother Jones. Retrieved February 2, 2016.
{{cite news}}: Italic or bold markup not allowed in:|publisher=(help)
