Prasugrel: Difference between revisions
consistent citation formatting |
→Mechanism of action: The decreased responsiveness observed in prasugrel is likely due to its HPR which is estimated to be about 3-15%. Although low percentages, this characteristics has been shown to affect the effect of prasugrel in some patients. |
||
| Line 97: | Line 97: | ||
Clopidogrel, unlike prasugrel, was issued a [[black box warning]] from the FDA on March 12, 2010, as the estimated 2–14% of the US population who have low levels of the [[CYP2C19]] liver enzyme needed to activate clopidogrel may not get the full effect. Tests are available to predict if a patient would be susceptible to this problem or not.<ref>{{cite press release | title = FDA Announces New Boxed Warning on Plavix: Alerts patients, health care professionals to potential for reduced effectiveness | date = March 12, 2010 | url = https://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm204253.htm | publisher = [[Food and Drug Administration (United States)]] | access-date = March 13, 2010 }}</ref><ref>{{cite web | url = https://www.fda.gov/Drugs/DrugSafety/PostmarketDrugSafetyInformationforPatientsandProviders/ucm203888.htm | title = FDA Drug Safety Communication: Reduced effectiveness of Plavix (clopidogrel) in patients who are poor metabolizers of the drug | work = Drug Safety and Availability | publisher = [[Food and Drug Administration (United States)]] | date = March 12, 2010 | access-date = March 13, 2010 }}</ref> |
Clopidogrel, unlike prasugrel, was issued a [[black box warning]] from the FDA on March 12, 2010, as the estimated 2–14% of the US population who have low levels of the [[CYP2C19]] liver enzyme needed to activate clopidogrel may not get the full effect. Tests are available to predict if a patient would be susceptible to this problem or not.<ref>{{cite press release | title = FDA Announces New Boxed Warning on Plavix: Alerts patients, health care professionals to potential for reduced effectiveness | date = March 12, 2010 | url = https://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm204253.htm | publisher = [[Food and Drug Administration (United States)]] | access-date = March 13, 2010 }}</ref><ref>{{cite web | url = https://www.fda.gov/Drugs/DrugSafety/PostmarketDrugSafetyInformationforPatientsandProviders/ucm203888.htm | title = FDA Drug Safety Communication: Reduced effectiveness of Plavix (clopidogrel) in patients who are poor metabolizers of the drug | work = Drug Safety and Availability | publisher = [[Food and Drug Administration (United States)]] | date = March 12, 2010 | access-date = March 13, 2010 }}</ref> |
||
Unlike clopidogrel, prasugrel is effective in most |
Unlike clopidogrel, prasugrel is effective in most individual with the exception in patients over the age of 75, weight under 60 kg, and patients with a history of stroke or TIA due to increased risk of bleeding,<ref>{{Cite journal|last=Ruff|first=Christian T.|last2=Giugliano|first2=Robert P.|last3=Antman|first3=Elliott M.|last4=Murphy|first4=Sabina A.|last5=Lotan|first5=Chaim|last6=Heuer|first6=Herbertus|last7=Merkely|first7=Bela|last8=Baracioli|first8=Luciano|last9=Schersten|first9=Fredrik|last10=Seabro-Gomes|first10=Ricardo|last11=Braunwald|first11=Eugene|date=2012-03|title=Safety and efficacy of prasugrel compared with clopidogrel in different regions of the world|url=https://doi.org/10.1016/j.ijcard.2010.10.040|journal=International Journal of Cardiology|volume=155|issue=3|pages=424–429|doi=10.1016/j.ijcard.2010.10.040|issn=0167-5273}}</ref><ref>{{Cite journal|last=Wiviott|first=Stephen D.|last2=Braunwald|first2=Eugene|last3=McCabe|first3=Carolyn H.|last4=Montalescot|first4=Gilles|last5=Ruzyllo|first5=Witold|last6=Gottlieb|first6=Shmuel|last7=Neumann|first7=Franz-Joseph|last8=Ardissino|first8=Diego|last9=De Servi|first9=Stefano|last10=Murphy|first10=Sabina A.|last11=Riesmeyer|first11=Jeffrey|date=2007-11-15|title=Prasugrel versus Clopidogrel in Patients with Acute Coronary Syndromes|url=http://www.nejm.org/doi/abs/10.1056/NEJMoa0706482|journal=New England Journal of Medicine|language=en|volume=357|issue=20|pages=2001–2015|doi=10.1056/NEJMoa0706482|issn=0028-4793}}</ref>although several cases have been reported of decreased responsiveness to prasugrel.<ref>{{cite journal | vauthors = Silvano M, Zambon CF, De Rosa G, Plebani M, Pengo V, Napodano M, Padrini R | title = A case of resistance to clopidogrel and prasugrel after percutaneous coronary angioplasty | journal = Journal of Thrombosis and Thrombolysis | volume = 31 | issue = 2 | pages = 233–4 | date = February 2011 | pmid = 21088983 | doi = 10.1007/s11239-010-0533-x }}</ref>It has been suggested that the decreased responsiveness observed in prasugrel is likely due to its low but significant frequency of High Platelet Reactivity (HPR).<ref>{{Cite journal|last=Warlo|first=Ellen M. K.|last2=Arnesen|first2=Harald|last3=Seljeflot|first3=Ingebjørg|date=2019-12|title=A brief review on resistance to P2Y12 receptor antagonism in coronary artery disease|url=https://thrombosisjournal.biomedcentral.com/articles/10.1186/s12959-019-0197-5|journal=Thrombosis Journal|language=en|volume=17|issue=1|pages=11|doi=10.1186/s12959-019-0197-5|issn=1477-9560|pmc=PMC6558673|pmid=31198410}}</ref> |
||
===Pharmacodynamics=== |
===Pharmacodynamics=== |
||
Revision as of 09:06, 10 May 2020
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Effient, Efient |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a609027 |
| License data | |
| Pregnancy category |
|
| Routes of administration | Oral |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | ≥79% |
| Protein binding | Active metabolite: ~98% |
| Elimination half-life | ~7 h (range 2 h to 15 h) |
| Excretion | Urine (~68% inactive metabolites); feces (27% inactive metabolites) |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.228.719 |
| Chemical and physical data | |
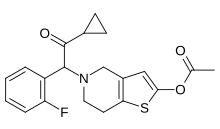
| Formula | C20H20FNO3S |
| Molar mass | 373.442 g/mol g·mol−1 |
| 3D model (JSmol) | |
| |
| |
| | |
Prasugrel (trade name Effient in the US, Australia and India, and Efient in the EU) is a drug used to prevent formation of blood clots. It is a platelet inhibitor and an irreversible antagonist of P2Y12 ADP receptors and is of the thienopyridine drug class. It was developed by Daiichi Sankyo Co. and produced by Ube and currently marketed in the United States in cooperation with Eli Lilly and Company.
Prasugrel was approved for use in Europe in February 2009,[1] and in the US in July 2009, for the reduction of thrombotic cardiovascular events (including stent thrombosis) in people with acute coronary syndrome (ACS) who are to be managed with percutaneous coronary intervention (PCI).[2]
Medical uses
Prasugrel is used in combination with low dose aspirin to prevent thrombosis in patients with ACS, including unstable angina pectoris, non-ST elevation myocardial infarction (NSTEMI), and ST elevation myocardial infarction (STEMI), who are planned for treatment with PCI. In studies, prasugrel was more effective than the related clopidogrel but also caused more bleeding. Overall mortality was the same.[1][3]
Prasugrel does not change the risk of death when given to people who have had a STEMI[citation needed] or NSTEMI. Prasugrel does however increase the risk of bleeding and may decrease the risk of further cardiovascular problems. Thus routine use in NSTEMI patients is of questionable value.[4]
Contraindications
Prasugrel should not be given to patients with active pathological bleeding, such as peptic ulcer or a history of transient ischemic attack or stroke, because of higher risk of stroke (thrombotic stroke and intracranial hemorrhage).[5]
Adverse effects
Adverse effects include:[6]
- Cardiovascular: Hypertension (8%), hypotension (4%), atrial fibrillation (3%), bradycardia (3%), noncardiac chest pain (3%), peripheral edema (3%), thrombotic thrombocytopenic purpura (TTP)
- Central nervous system: Headache (6%), dizziness (4%), fatigue (4%), fever (3%), extremity pain (3%)
- Dermatologic: Rash (3%)
- Endocrine and metabolic: Hypercholesterolemia/hyperlipidemia (7%)
- Gastrointestinal: Nausea (5%), diarrhea (2%), gastrointestinal hemorrhage (2%)
- Hematologic: Leukopenia (3%), anemia (2%)
- Neuromuscular and skeletal: Back pain (5%)
- Respiratory: Epistaxis (6%), dyspnea (5%), cough (4%)
- Hypersensitivity, including angioedema
Interactions
Prasugrel has a low potential for interactions. It may, for example, be used with proton pump inhibitors to reduce the risk of gastrointestinal bleeding without loss of its antiplatelet effect.[7][8][9][10]
Pharmacology
Mechanism of action
Prasugrel is a member of the thienopyridine class of ADP receptor inhibitors, like ticlopidine (trade name Ticlid) and clopidogrel (trade name Plavix). These agents reduce the aggregation ("clumping") of platelets by irreversibly binding to P2Y12 receptors. Prasugrel inhibits platelet aggregation more rapidly, more consistently, and to a greater extent than clopidogrel
[11][12] The TRITON-TIMI 38 study compared prasugrel with clopidogrel, and showed that prasugrel reduced rates of ischaemic events, but increased bleeding risk. Overall mortality rates were similar for each drug.[13]
Clopidogrel, unlike prasugrel, was issued a black box warning from the FDA on March 12, 2010, as the estimated 2–14% of the US population who have low levels of the CYP2C19 liver enzyme needed to activate clopidogrel may not get the full effect. Tests are available to predict if a patient would be susceptible to this problem or not.[14][15] Unlike clopidogrel, prasugrel is effective in most individual with the exception in patients over the age of 75, weight under 60 kg, and patients with a history of stroke or TIA due to increased risk of bleeding,[16][17]although several cases have been reported of decreased responsiveness to prasugrel.[18]It has been suggested that the decreased responsiveness observed in prasugrel is likely due to its low but significant frequency of High Platelet Reactivity (HPR).[19]
Pharmacodynamics
Prasugrel produces inhibition of platelet aggregation to 20 μM or 5 μM ADP, as measured by light transmission aggregometry.[20] Following a 60-mg loading dose of the drug, about 90% of patients had at least 50% inhibition of platelet aggregation by one hour. Maximum platelet inhibition was about 80%. Mean steady-state inhibition of platelet aggregation was about 70% following three to five days of dosing at 10 mg daily after a 60-mg loading dose. Platelet aggregation gradually returns to baseline values over five to 9 days after discontinuation of prasugrel, this time course being a reflection of new platelet production rather than pharmacokinetics of prasugrel. Discontinuing clopidogrel 75 mg and initiating prasugrel 10 mg with the next dose resulted in increased inhibition of platelet aggregation, but not greater than that typically produced by a 10-mg maintenance dose of prasugrel alone. Increasing platelet inhibition could increase bleeding risk. The relationship between inhibition of platelet aggregation and clinical activity has not been established.[6]
Pharmacokinetics

Prasugrel is a prodrug and is rapidly metabolized by carboxylesterase 2 in the intestine and carboxylesterase 1 in the liver to a likewise inactive thiolactone, which is then converted by CYP3A4 and CYP2B6, and to a minor extent by CYP2C9 and CYP2C19, to a pharmacologically active metabolite (R-138727).[21][22] R-138727 has an elimination half-life of about 7 hours (range 2 h to 15 h). Healthy subjects, patients with stable atherosclerosis, and patients undergoing PCI show similar pharmacokinetics.
Chemistry
Prasugrel has one chiral atom. It is used in racemic form as the hydrochloride salt, which is a white powder.
References
- ^ a b "European Public Assessment Report for Efient" (PDF). EMA. 2009.
- ^ Baker WL, White CM (2009). "Role of prasugrel, a novel P2Y(12) receptor antagonist, in the management of acute coronary syndromes". American Journal of Cardiovascular Drugs. 9 (4): 213–29. doi:10.2165/1131209-000000000-00000. PMID 19655817.
- ^ "Arzneimittelinformation der Arzneimittelkommission der deutschen Ärzteschaft (AkdÄ): Efient (Prasugrel)" (PDF) (in German). 16 April 2009. pp. 30–44.
- ^ Bellemain-Appaix A, Kerneis M, O'Connor SA, Silvain J, Cucherat M, Beygui F, et al. (October 2014). "Reappraisal of thienopyridine pretreatment in patients with non-ST elevation acute coronary syndrome: a systematic review and meta-analysis". Bmj. 349: g6269. doi:10.1136/bmj.g6269. PMC 4208629. PMID 25954988.
- ^ "Effient (prasugrel hydrochloride) Prescribing Information". FDA. September 2011.
- ^ a b Efient: Highlights of prescribing information
- ^ John J, Koshy SK (2012). "Current oral antiplatelets: focus update on prasugrel". Journal of the American Board of Family Medicine. 25 (3): 343–9. doi:10.3122/jabfm.2012.03.100270. PMID 22570398.
- ^ Demcsák A, Lantos T, Bálint ER, Hartmann P, Vincze Á, Bajor J, et al. (2018-11-19). "PPIs Are Not Responsible for Elevating Cardiovascular Risk in Patients on Clopidogrel-A Systematic Review and Meta-Analysis". Frontiers in Physiology. 9: 1550. doi:10.3389/fphys.2018.01550. PMC 6252380. PMID 30510515.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ O'Donoghue ML, Braunwald E, Antman EM, Murphy SA, Bates ER, Rozenman Y, et al. (September 2009). "Pharmacodynamic effect and clinical efficacy of clopidogrel and prasugrel with or without a proton-pump inhibitor: an analysis of two randomised trials". Lancet. 374 (9694): 989–997. doi:10.1016/S0140-6736(09)61525-7. PMID 19726078.
- ^ Vaduganathan M, Cannon CP, Cryer BL, Liu Y, Hsieh WH, Doros G, et al. (September 2016). "Efficacy and Safety of Proton-Pump Inhibitors in High-Risk Cardiovascular Subsets of the COGENT Trial". The American Journal of Medicine. 129 (9): 1002–5. doi:10.1016/j.amjmed.2016.03.042. PMID 27143321.
- ^ Brandt JT, Payne CD, Wiviott SD, Weerakkody G, Farid NA, Small DS, et al. (January 2007). "A comparison of prasugrel and clopidogrel loading doses on platelet function: magnitude of platelet inhibition is related to active metabolite formation". American Heart Journal. 153 (1): 66.e9-16. doi:10.1016/j.ahj.2006.10.010. PMID 17174640.
- ^ Wiviott SD, Trenk D, Frelinger AL, O'Donoghue M, Neumann FJ, Michelson AD, et al. (December 2007). "Prasugrel compared with high loading- and maintenance-dose clopidogrel in patients with planned percutaneous coronary intervention: the Prasugrel in Comparison to Clopidogrel for Inhibition of Platelet Activation and Aggregation-Thrombolysis in Myocardial Infarction 44 trial". Circulation. 116 (25): 2923–32. doi:10.1161/CIRCULATIONAHA.107.740324. PMID 18056526.
- ^ Wiviott SD, Braunwald E, McCabe CH, Montalescot G, Ruzyllo W, Gottlieb S, et al. (November 2007). "Prasugrel versus clopidogrel in patients with acute coronary syndromes". The New England Journal of Medicine. 357 (20): 2001–15. doi:10.1056/NEJMoa0706482. PMID 17982182.
- ^ "FDA Announces New Boxed Warning on Plavix: Alerts patients, health care professionals to potential for reduced effectiveness" (Press release). Food and Drug Administration (United States). March 12, 2010. Retrieved March 13, 2010.
- ^ "FDA Drug Safety Communication: Reduced effectiveness of Plavix (clopidogrel) in patients who are poor metabolizers of the drug". Drug Safety and Availability. Food and Drug Administration (United States). March 12, 2010. Retrieved March 13, 2010.
- ^ Ruff, Christian T.; Giugliano, Robert P.; Antman, Elliott M.; Murphy, Sabina A.; Lotan, Chaim; Heuer, Herbertus; Merkely, Bela; Baracioli, Luciano; Schersten, Fredrik; Seabro-Gomes, Ricardo; Braunwald, Eugene (2012-03). "Safety and efficacy of prasugrel compared with clopidogrel in different regions of the world". International Journal of Cardiology. 155 (3): 424–429. doi:10.1016/j.ijcard.2010.10.040. ISSN 0167-5273.
{{cite journal}}: Check date values in:|date=(help) - ^ Wiviott, Stephen D.; Braunwald, Eugene; McCabe, Carolyn H.; Montalescot, Gilles; Ruzyllo, Witold; Gottlieb, Shmuel; Neumann, Franz-Joseph; Ardissino, Diego; De Servi, Stefano; Murphy, Sabina A.; Riesmeyer, Jeffrey (2007-11-15). "Prasugrel versus Clopidogrel in Patients with Acute Coronary Syndromes". New England Journal of Medicine. 357 (20): 2001–2015. doi:10.1056/NEJMoa0706482. ISSN 0028-4793.
- ^ Silvano M, Zambon CF, De Rosa G, Plebani M, Pengo V, Napodano M, Padrini R (February 2011). "A case of resistance to clopidogrel and prasugrel after percutaneous coronary angioplasty". Journal of Thrombosis and Thrombolysis. 31 (2): 233–4. doi:10.1007/s11239-010-0533-x. PMID 21088983.
- ^ Warlo, Ellen M. K.; Arnesen, Harald; Seljeflot, Ingebjørg (2019-12). "A brief review on resistance to P2Y12 receptor antagonism in coronary artery disease". Thrombosis Journal. 17 (1): 11. doi:10.1186/s12959-019-0197-5. ISSN 1477-9560. PMC 6558673. PMID 31198410.
{{cite journal}}: Check date values in:|date=(help)CS1 maint: PMC format (link) CS1 maint: unflagged free DOI (link) - ^ O'Riordan, Michael. "Switching from clopidogrel to prasugrel further reduces platelet function". TheHeart.org. Retrieved 1 April 2011.
- ^ Rehmel JL, Eckstein JA, Farid NA, Heim JB, Kasper SC, Kurihara A, et al. (April 2006). "Interactions of two major metabolites of prasugrel, a thienopyridine antiplatelet agent, with the cytochromes P450". Drug Metabolism and Disposition. 34 (4): 600–7. doi:10.1124/dmd.105.007989. PMID 16415119.
- ^ Kurokawa T, Fukami T, Yoshida T, Nakajima M (March 2016). "Arylacetamide Deacetylase is Responsible for Activation of Prasugrel in Human and Dog". Drug Metabolism and Disposition. 44 (3): 409–16. doi:10.1124/dmd.115.068221. PMID 26718653.
Further reading
- Dean L (2017). "Prasugrel Therapy and CYP Genotype". In Pratt VM, McLeod HL, Rubinstein WS, et al. (eds.). Medical Genetics Summaries. National Center for Biotechnology Information (NCBI). PMID 28520385. Bookshelf ID: NBK425796.
External links
- "Prasugrel". Drug Information Portal. U.S. National Library of Medicine.
- US 5288726 claims prasugrel compound; expired on 14 Apr 2017
- US 6693115 claims hydrochloride salt of prasugrel; will expire on 3 Jul 2021
