Cholera: Difference between revisions
| Line 198: | Line 198: | ||
=== Research === |
=== Research === |
||
no research has been done on this topic |
|||
The Russian-born bacteriologist [[Waldemar Haffkine]] developed the first cholera vaccine around 1900. The bacterium had been originally isolated thirty years earlier (1855) by Italian anatomist [[Filippo Pacini]], but its exact nature and his results were not widely known around the world. |
|||
One of the major contributions to fighting cholera was made by the physician and pioneer medical scientist [[John Snow (physician)|John Snow]] (1813–1858), who found a link between cholera and contaminated drinking water in 1854.<ref name="Rosenberg" /> Dr Snow proposed a microbial origin for epidemic cholera in 1849. In his major "state of the art" review of 1855, he proposed a substantially complete and correct model for the [[aetiology]] of the disease. In two pioneering epidemiological field-studies, he was able to demonstrate that human [[sewage]] contamination was the most probable disease vector in two major epidemics in London in 1854.<ref>Dr John Snow, ''The mode of communication of cholera'', London 1855</ref> His model was not immediately accepted, but it was seen to be the more plausible as medical microbiology developed over the next thirty years or so. |
|||
Cities in developed nations made massive investment in clean water supply and well-separated sewage treatment infractures was made between the mid-1850s and the 1900s. This eliminated the threat of cholera epidemics from the major developed cities in the world. [[Robert Koch]], 30 years later, identified ''V. cholerae'' with a microscope as the bacillus causing the disease in 1885. |
|||
Cholera has been a laboratory for the study of evolution of virulence. The province of Bengal in [[British Raj|British India]] was partitioned into [[West Bengal]] and [[East Pakistan]] in 1947. Prior to partition, both regions had cholera pathogens with similar characteristics. After 1947, India made more progress on public health than East Pakistan (now [[Bangladesh]]). As a consequence,{{Clarify|date=April 2010}} the strains of the pathogen that succeeded in India had a greater incentive in the longevity of the host. They have become less virulent than the strains prevailing in Bangladesh. These uninhibitedly draw upon the resources of the host population, thus rapidly killing many victims. |
|||
More recently, in 2002, Alam et al. studied stool samples from patients at the [[International Centre for Diarrhoeal Disease Research, Bangladesh|International Centre for Diarrhoeal Disease]] (ICDDR) in [[Dhaka, Bangladesh]]. From the various experiments they conducted, the researchers found a correlation between the passage of ''V. cholerae'' through the human digestive system and an increased infectivity state. Furthermore, the researchers found that the bacterium creates a hyper-infected state where [[gene]]s that control biosynthesis of [[amino acid]]s, [[iron]] uptake systems, and formation of periplasmic nitrate reductase complexes were induced just before defecation. These induced characteristics allow the cholera vibrios to survive in the "rice water" stools, an environment of limited oxygen and iron, of patients with a cholera infection.<ref name="Merrell2002" /> |
|||
=== Notable cases === |
=== Notable cases === |
||
Revision as of 14:14, 6 September 2010
The article's lead section may need to be rewritten. (April 2010) |
| Cholera | |
|---|---|
| Specialty | Infectious diseases, emergency medicine |
Cholera[1] is a severe infection caused by the bacterium Vibrio cholerae, which primarily affects the small intestine. The main symptoms include profuse watery diarrhea and vomiting. Transmission is primarily by the acquisition of the pathogen through contaminated drinking water or infected food. The severity of the diarrhea and associated vomiting can lead to rapid dehydration and electrolyte loss, which can lead to death. Cholera is a major cause of death in the world.
The study of cholera has been used as an example of early epidemiology. Study of the V. cholerae bacterium has also shed light on many of the mechanisms used by bacteria to infect and survive in their hosts.
Signs and symptoms
The primary symptoms of cholera are profuse diarrhea, severe dehydration and abdominal pain. Cholera may also cause vomiting. These symptoms start suddenly, usually one to five days after infection, and are the result of a toxin produced by the vibrio cholerae bacterium that compels profuse amounts of fluid from the blood supply into the small and large intestines. [2] An untreated cholera patient may produce around 10 litres of diarrhoeal fluid a day.
Cause

Most of the V. cholerae bacteria in the contaminated water consumed by the host do not survive the highly acidic conditions of the human stomach.[3] The few bacteria that do survive conserve their energy and stored nutrients during the passage through the stomach by shutting down much protein production. When the surviving bacteria exit the stomach and reach the small intestine, they need to propel themselves through the thick mucus that lines the small intestine to get to the intestinal wall where they can thrive. V. cholerae bacteria start up production of the hollow cylindrical protein flagellin to make flagella, the curly whip-like tails that they rotate to propel themselves through the mucus of the small intestine.
Once the cholera bacteria reach the intestinal wall, they do not need the flagella propellers to move any longer. The bacteria stop producing the protein flagellin, thus again conserving energy and nutrients by changing the mix of proteins which they manufacture in response to the changed chemical surroundings. On reaching the intestinal wall, V. cholerae start producing the toxic proteins that give the infected person a watery diarrhea. This carries the multiplying new generations of V. cholerae bacteria out into the drinking water of the next host if proper sanitation measures are not in place.
The cholera toxin (CTX or CT) is an oligomeric complex made up of six protein subunits: a single copy of the A subunit (part A), and five copies of the B subunit (part B), connected by a disulfide bond. The five B subunits form a five-membered ring that binds to GM1 gangliosides on the surface of the intestinal epithelium cells. The A1 portion of the A subunit is an enzyme that ADP-ribosylates G proteins, while the A2 chain fits into the central pore of the B subunit ring. Upon binding, the complex is taken into the cell via receptor-mediated endocytosis. Once inside the cell, the disulfide bond is reduced and the A1 subunit is freed to bind with a human partner protein called ADP-ribosylation factor 6 (Arf6).[4] Binding exposes its active site, allowing it to permanently ribosylate the Gs alpha subunit of the heterotrimeric G protein. This results in constitutive cAMP production, which in turn leads to secretion of H2O, Na+, K+, Cl−, and HCO3− into the lumen of the small intestine and rapid dehydration. The gene encoding the cholera toxin is introduced into V. cholerae by horizontal gene transfer. Virulent strains of V. cholerae carry a variant of lysogenic bacteriophage called CTXf or CTXφ.
Microbiologists have studied the genetic mechanisms by which the V. cholerae bacteria turn off the production of some proteins and turn on the production of other proteins as they respond to the series of chemical environments they encounter, passing through the stomach, through the mucous layer of the small intestine, and on to the intestinal wall.[5] Of particular interest have been the genetic mechanisms by which cholera bacteria turn on the protein production of the toxins that interact with host cell mechanisms to pump chloride ions into the small intestine, creating an ionic pressure which prevents sodium ions from entering the cell. The chloride and sodium ions create a salt-water environment in the small intestines, which through osmosis can pull up to six liters of water per day through the intestinal cells, creating the massive amounts of diarrhea. The host can become rapidly dehydrated if an appropriate mixture of dilute salt water and sugar is not taken to replace the blood's water and salts lost in the diarrhea.
By inserting separate, successive sections of V. cholerae DNA into the DNA of other bacteria such as E. coli that would not naturally produce the protein toxins, researchers have investigated the mechanisms by which V. cholerae responds to the changing chemical environments of the stomach, mucous layers, and intestinal wall. Researchers have discovered that there is a complex cascade of regulatory proteins that control expression of V. cholerae virulence determinants. In responding to the chemical environment at the intestinal wall, the V. cholerae bacteria produce the TcpP/TcpH proteins, which, together with the ToxR/ToxS proteins, activate the expression of the ToxT regulatory protein. ToxT then directly activates expression of virulence genes that produce the toxins that cause diarrhea in the infected person and that permit the bacteria to colonize the intestine.[5] Current research aims at discovering "the signal that makes the cholera bacteria stop swimming and start to colonize (that is, adhere to the cells of) the small intestine."[5]
Pathophysiology
Susceptibility
Recent epidemiologic research suggests that an individual's susceptibility to cholera (and other diarrheal infections) is affected by their blood type: those with type O blood are the most susceptible,[6][7] while those with type AB are the most resistant. Between these two extremes are the A and B blood types, with type A being more resistant than type B.[citation needed]
About one million V. cholerae bacteria must typically be ingested to cause cholera in normally healthy adults, although increased susceptibility may be observed in those with a weakened immune system, individuals with decreased gastric acidity (as from the use of antacids), or those who are malnourished.
It has also been hypothesized that the cystic fibrosis genetic mutation has been maintained in humans due to a selective advantage: heterozygous carriers of the mutation (who are thus not affected by cystic fibrosis) are more resistant to V. cholerae infections.[8] In this model, the genetic deficiency in the cystic fibrosis transmembrane conductance regulator channel proteins interferes with bacteria binding to the gastrointestinal epithelium, thus reducing the effects of an infection.
Transmission
People infected with cholera suffer acute diarrhea. This highly liquid diarrhea, colloquially referred to as "rice-water stool," is loaded with bacteria that can infect water used by other people.[9] Cholera is transmitted through ingestion of water contaminated with the cholera bacterium, usually from feces or other effluent. The source of the contamination is typically other cholera patients when their untreated diarrhea discharge is allowed to get into waterways or into groundwater or drinking water supplies. Any infected water and any foods washed in the water, as well as shellfish living in the affected waterway, can cause an infection. Cholera is rarely spread directly from person to person. V. cholerae harbors naturally in the zooplankton of fresh, brackish, and salt water, attached primarily to their chitinous exoskeleton.[10] Both toxic and non-toxic strains exist. Non-toxic strains can acquire toxicity through a lysogenic bacteriophage.[11] Coastal cholera outbreaks typically follow zooplankton blooms, thus making cholera a zoonotic disease.
Potential human contribution to transmissibility
Cholera bacteria grown in vitro encounter difficulty subsequently growing in humans without additional stomach acid buffering. In a 2002 study at Tufts University School of Medicine, it was found that stomach acidity is a principal agent that advances epidemic spread.[12] In their findings, the researchers found that human colonization creates a hyperinfectious bacterial state that is maintained after dissemination and that may contribute to epidemic spread of the disease. When these hyperinfectious bacteria underwent transcription profiles, they were found to possess a unique physiological and behavioral state, characterized by high expression levels of genes required for nutrient acquisition and motility, and low expression levels of genes required for bacterial chemotaxis. Thus, the spread of cholera can be expedited by host physiology.
Diagnosis
In epidemic situations, a clinical diagnosis is made by taking a history of symptoms from the patient and by a brief examination only. Treatment is usually started without or before confirmation by laboratory analysis of specimens.
Stool and swab samples collected in the acute stage of the disease, before antibiotics have been administered, are the most useful specimens for laboratory diagnosis. If an epidemic of cholera is suspected, the most common causative agent is Vibrio cholerae O1. If V. cholerae serogroup O1 is not isolated, the laboratory should test for V. cholerae O139. However, if neither of these organisms is isolated, it is necessary to send stool specimens to a reference laboratory. Infection with V. cholerae O139 should be reported and handled in the same manner as that caused by V. cholerae O1. The associated diarrheal illness should be referred to as cholera and must be reported.[13]
A number of special media have been employed for the cultivation for cholera vibrios. They are classified as follows:
Enrichment media
- Alkaline peptone water at pH 8.6
- Monsur's taurocholate tellurite peptone water at pH 9.2
Plating media
- Alkaline bile salt agar (BSA): The colonies are very similar to those on nutrient agar.
- Monsur's gelatin Tauro cholate trypticase tellurite agar (GTTA) medium: Cholera vibrios produce small translucent colonies with a greyish black centre.
- TCBS medium: This the mostly widely used medium. This medium contains thiosulphate, citrate, bile salts and sucrose. Cholera vibrios produce flat 2–3 mm in diameter, yellow nucleated colonies.
Direct microscopy of stool is not recommended as it is unreliable. Microscopy is preferred only after enrichment, as this process reveals the characteristic motility of Vibrios and its inhibition by appropriate antiserum. Diagnosis can be confirmed as well as serotyping done by agglutination with specific sera.
Prevention
Although cholera may be life-threatening, prevention of the disease is normally straightforward if proper sanitation practices are followed. In developed countries, due to nearly universal advanced water treatment and sanitation practices, cholera is no longer a major health threat. The last major outbreak of cholera in the United States occurred in 1910-1911.[14][15] Travelers should be aware of how the disease is transmitted and what can be done to prevent it. Effective sanitation practices, if instituted and adhered to in time, are usually sufficient to stop an epidemic. There are several points along the cholera transmission path at which its spread may be (and should be) halted:

- Sterilization: Proper disposal and treatment of infected fecal waste water produced by cholera victims and all contaminated materials (e.g. clothing, bedding, etc.) is essential. All materials that come in contact with cholera patients should be sterilized by washing in hot water using chlorine bleach if possible. Hands that touch cholera patients or their clothing, bedding, etc., should be thoroughly cleaned and disinfected with chlorinated water or other effective anti-microbial agents.
- Sewage: anti-bacterial treatment of general sewage by chlorine, ozone, ultra-violet light or other effective treatment before it enters the waterways or underground water supplies helps prevent undiagnosed patients from inadvertently spreading the disease.
- Sources: Warnings about possible cholera contamination should be posted around contaminated water sources with directions on how to decontaminate the water (boiling, chlorination etc.) for possible use.
- Water purification: All water used for drinking, washing, or cooking should be sterilized by either boiling, chlorination, ozone water treatment, ultra-violet light sterilization, or anti-microbal filtration in any area where cholera may be present. Chlorination and boiling are often the least expensive and most effective means of halting transmission. Cloth filters, though very basic, have significantly reduced the occurrence of cholera when used in poor villages in Bangladesh that rely on untreated surface water. Better anti-microbial filters like those present in advanced individual water treatment hiking kits are most effective. Public health education and adherence to appropriate sanitation practices are of primary importance to help prevent and control transmission of cholera and other diseases.
A vaccine for cholera is available in some countries, but prophylactic usage is not currently recommended for routine use by the Centers for Disease Control and Prevention (CDC).[16] During recent years, substantial progress has been made in developing new oral vaccines against cholera. Two oral cholera vaccines, which have been evaluated with volunteers from industrialized countries and in regions with endemic cholera, are commercially available in several countries: a killed whole-cell V. cholerae O1 in combination with purified recombinant B subunit of cholera toxin and a live-attenuated live oral cholera vaccine, containing the genetically manipulated V. cholerae O1 strain CVD 103-HgR. The appearance of V. cholerae O139 has influenced efforts in order to develop an effective and practical cholera vaccine since none of the currently available vaccines is effective against this strain.[13] The newer vaccine (brand name: Dukoral), an orally administered inactivated whole cell vaccine, appears to provide somewhat better immunity and have fewer adverse effects than the previously available vaccine.[16] This safe and effective vaccine is available for use by individuals and health personnel. Work is under way to investigate the role of mass vaccination.[17]
Sensitive surveillance and prompt reporting allow for containing cholera epidemics rapidly. Cholera exists as a seasonal disease in many endemic countries, occurring annually mostly during rainy seasons. Surveillance systems can provide early alerts to outbreaks, therefore leading to coordinated response and assist in preparation of preparedness plans. Efficient surveillance systems can also improve the risk assessment for potential cholera outbreaks. Understanding the seasonality and location of outbreaks provide guidance for improving cholera control activities for the most vulnerable. This will also aid in the developing indicators for appropriate use of oral cholera vaccine.[18]
Treatment
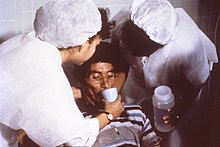
In most cases cholera can be successfully treated with oral rehydration therapy (ORT). ORT is highly effective, safe, and simple to administer: prompt replacement of water and electrolytes is the principal treatment for cholera, as dehydration and electrolyte depletion occur rapidly. In situations where commercially produced ORT sachets are too expensive or difficult to obtain, alternative homemade solutions using various formulas of water, sugar, table salt, baking soda, and fruit offer less expensive methods of electrolyte repletion. In severe cholera cases with significant dehydration, the administration of intravenous rehydration solutions may be necessary.
Antibiotics shorten the course of the disease and reduce the severity of the symptoms; however, oral rehydration therapy remains the principal treatment. Tetracycline is typically used as the primary antibiotic, although some strains of V. cholerae have shown resistance. Other antibiotics that have been proven effective against V. cholerae include cotrimoxazole, erythromycin, doxycycline, chloramphenicol, and furazolidone.[19] Fluoroquinolones such as norfloxacin also may be used, but resistance has been reported.[20]
Rapid diagnostic assay methods are available for the identification of multi-drug resistant V. cholerae.[21] New generation antimicrobials have been discovered which are effective against V. cholerae in in vitro studies.[22]
The success of treatment is significantly affected by the speed and method of treatment. If cholera patients are treated quickly and properly, the mortality rate is less than 1%; however, with untreated cholera, the mortality rate rises to 50–60%.[23][24]
Epidemiology

- In 2000, some 140,000 cholera cases were officially notified to WHO. Africa accounted for 87% of these cases.[25]
- July - December 2007 - A lack of clean drinking water in Iraq has led to an outbreak of cholera.[26] As of 2 December 2007, the UN has reported 22 deaths and 4,569 laboratory-confirmed cases.[27]
- August 2007 - The cholera epidemic started in Orissa, India. The outbreak has affected Rayagada, Koraput and Kalahandi districts where more than 2,000 people have been admitted to hospitals.[28]
- August - October 2008 - As of 29 October 2008, a total of 644 laboratory-confirmed cholera cases, including eight deaths, had been verified in Iraq.[29]
- March - April 2008 - 2,490 people from 20 provinces throughout Vietnam have been hospitalized with acute diarrhea. Of those hospitalized, 377 patients tested positive for cholera.[30]
- November 2008 - Doctors Without Borders reported an outbreak in a refugee camp in the Democratic Republic of the Congo's eastern provincial capital of Goma. Some 45 cases were reportedly treated between November 7 through 9th.
- August 2008 - April 2009: In the 2008 Zimbabwean cholera outbreak, which is still continuing, an estimated 96,591 people in the country have been infected with cholera and, by 16 April 2009, 4,201 deaths had been reported.[31] According to the World Health Organization, during the week of 22–28 March 2009, the "Crude Case Fatality Ratio (CFR)" had dropped from 4.2% to 3.7%.[31] The daily updates for the period 29 March 2009 to 7 April 2009, list 1748 cases and 64 fatalities, giving a weekly CFR of 3.66% (see table above);[32] however, those for the period 8 April to 16 April list 1375 new cases and 62 deaths (and a resulting CFR of 4.5%).[32] The CFR had remained above 4.7% for most of January and early February 2009.[33]
- January 2009 - The Mpumalanga province of South Africa has confirmed over 381 new cases of Cholera, bringing the total number of cases treated since November 2008 to 2276. 19 people have died in the province since the outbreak.[34]
- August 2010 - Nigeria is reaching epidemic proportions after wide spread confirmation of the Cholera outbreaks in 12 of its 36 states. 6400 cases have been reported with 352 reported deaths. The health ministry blamed the outbreak on heavy seasonal rainfall and poor sanitation. [35]
Pandemic genetic diversity
Amplified fragment length polymorphism (AFLP) fingerprinting of the pandemic isolates of Vibrio cholerae has revealed variation in the genetic structure. Two clusters have been identified: Cluster I and Cluster II. For the most part Cluster I consists of strains from the 1960s and 1970s, while Cluster II largely contains strains from the 1980s and 1990s, based on the change in the clone structure. This grouping of strains is best seen in the strains from the African Continent.[36]
History

Origin and spread
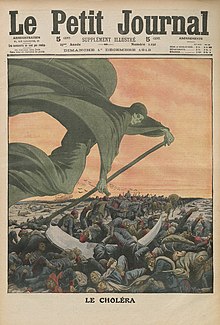
Cholera likely has its origins in and is endemic to the Indian subcontinent. The disease spread by trade routes (land and sea) to Russia, then to Western Europe, and from Europe to North America. Cholera is now no longer considered a pressing health threat in Europe and North America due to filtering and chlorination of water supplies, but still heavily affects populations in developing countries.
- 1816-1826 - First cholera pandemic: Previously restricted, the pandemic began in Bengal, and then spread across India by 1820. 10,000 British troops and countless Indians died during this pandemic.[37] The cholera outbreak extended as far as China, Indonesia (where more than 100,000 people succumbed on the island of Java alone) and the Caspian Sea before receding. Deaths in India between 1817 and 1860 are estimated to have exceeded 15 million persons. Another 23 million died between 1865 and 1917.[38]
- 1829-1851 - Second cholera pandemic reached Russia (see Cholera Riots), Hungary (about 100,000 deaths) and Germany in 1831, London (more than 55,000 people died in the United Kingdom)[39] and Paris in 1832. In London, the disease claimed 6,536 victims and came to be known as "King Cholera"; in Paris, 20,000 succumbed (out of a population of 650,000) with about 100,000 deaths in all of France.[40] The epidemic reached Quebec, Ontario and New York in the same year and the Pacific coast of North America by 1834.[41] The 1831 cholera epidemic killed 150,000 people in Egypt.[42] In 1846, cholera struck Mecca, killing over 15,000 people.[43] A two-year outbreak began in England and Wales in 1848 and claimed 52,000 lives.[44] Cholera was found in Dundee in 1832. One influential UK pamphlet explaining how to nurse cholera patients and prevent the disease was Hints on the Cholera morbus (1832) by the home economics writer Esther Copley.
- 1849 - Second major outbreak in Paris. In London, it was the worst outbreak in the city's history, claiming 14,137 lives, over twice as many as the 1832 outbreak. Cholera hit Ireland in 1849 and killed many of the Irish Famine survivors already weakened by starvation and fever.[45] In 1849 cholera claimed 5,308 lives in the port city of Liverpool, England, and 1,834 in Hull, England.[40] An outbreak in North America took the life of former U.S. President James K. Polk. Cholera, believed spread from ship(s) from England, spread throughout the Mississippi river system killing over 4,500 in St. Louis[40] and over 3,000 in New Orleans[40] as well as thousands in New York.[40] Mexico was similarly attacked.[43] In 1849 cholera was spread along the California, Mormon and Oregon Trails as 6,000 to 12,000[46] are believed to have died on their way to the California Gold Rush, Utah and Oregon in the cholera years of 1849-1855.[40] It is believed that over 150,000 Americans died during the two pandemics between 1832 and 1849.[47][48]
- 1852-1860 - Third cholera pandemic mainly affected Russia, with over a million deaths. In 1852, cholera spread east to Indonesia and later invaded China and Japan in 1854. The Philippines were infected in 1858 and Korea in 1859. In 1859, an outbreak in Bengal once again led to the transmission of the disease to Iran, Iraq, Arabia and Russia.[43] There were at least seven major outbreaks of cholera in Japan between 1858 and 1902. The Ansei outbreak of 1858-60, for example, is believed to have killed between 100,000 and 200,000 people in Tokyo alone.[49]
- 1854 - Outbreak of cholera in Chicago took the lives of 5.5% of the population (about 3,500 people).[40][50] In 1853-4, London's epidemic claimed 10,738 lives. The Soho outbreak in London ended after removal of the handle of the Broad Street pump by a committee instigated to action by John Snow.[51] This proved that contaminated water (although it didn't identify the contaminant) was the main agent spreading cholera. It would take almost 50 years for this message to be believed and acted upon. Building and maintaining a safe water system was and is not cheap—but is absolutely essential.
- 1863-1875 - Fourth cholera pandemic spread mostly in Europe and Africa. At least 30,000 of the 90,000 Mecca pilgrims fell victim to the disease. Cholera claimed 90,000 lives in Russia in 1866.[52] The epidemic of cholera that spread with the Austro-Prussian War (1866) is estimated to have claimed 165,000 lives in the Austrian Empire.[53] Hungary and Belgium both lost 30,000 people and in the Netherlands 20,000 perished. In 1867, Italy lost 113,000 lives.[54]


- 1866 - 1873 - Outbreaks in North America. It killed some 50,000 Americans.[47] In London, a localized epidemic in the East End claimed 5,596 lives just as London was completing its major sewage and water treatment systems—the East End was not quite complete. William Farr, using the work of John Snow et al. as to contaminated drinking water being the likely source of the disease, was able to relatively quickly identify the East London Water Company as the source of the contaminated water. Quick action prevented further deaths.[40] Also a minor outbreak at Ystalyfera in South Wales. Caused by the local water works using contaminated canal water, it was mainly its workers and their families who suffered, 119 died. In the same year more than 21,000 people died in Amsterdam, The Netherlands. In the 1870s, cholera spread in the US as epidemic from New Orleans along the Mississippi River and related ports of tributaries, with thousands dying.
- 1881-1896 - Fifth cholera pandemic ; According to Dr A. J. Wall, the 1883-1887 epidemic cost 250,000 lives in Europe and at least 50,000 in Americas. Cholera claimed 267,890 lives in Russia (1892);[55] 120,000 in Spain;[56] 90,000 in Japan and over 60,000 in Persia.[55] In Egypt cholera claimed more that 58,000 lives. The 1892 outbreak in Hamburg killed 8,600 people. Although generally held responsible for the virulence of the epidemic, the city government went largely unchanged. This was the last serious European cholera outbreak.
- 1899-1923 - Sixth cholera pandemic had little effect in Europe because of advances in public health, but major Russian cities (more than 500,000 people dying of cholera during the first quarter of the 20th century)[57] and the Ottoman Empire were particularly hard hit by cholera deaths. The 1902-1904 cholera epidemic claimed 200,000 lives in the Philippines.[58] 27 epidemics were recorded during pilgrimages to Mecca from the 19th century to 1930, and more than 20,000 pilgrims died of cholera during the 1907–08 hajj.[57] The sixth pandemic killed more than 800,000 in India. The last outbreak in the United States was in 1910-1911 when the steamship Moltke brought infected people to New York City. Vigilant health authorities isolated the infected on Swinburne Island. Eleven people died, including a health care worker on Swinburne Island.[14][15][59]
- 1961-1970s - Seventh cholera pandemic began in Indonesia, called El Tor after the strain, and reached East Pakistan (now Bangladesh) in 1963, India in 1964, and the USSR in 1966. From North Africa it spread into Italy by 1973. In the late 1970s, there were small outbreaks in Japan and in the South Pacific. There were also many reports of a cholera outbreak near Baku in 1972, but information about it was suppressed in the USSR.
- January 1991 to September 1994 - Outbreak in South America, apparently initiated when a ship discharged ballast water. Beginning in Peru there were 1.04 million identified cases and almost 10,000 deaths. The causative agent was an O1, El Tor strain, with small differences from the seventh pandemic strain. In 1992 a new strain appeared in Asia, a non-O1, nonagglutinable vibrio (NAG) named O139 Bengal. It was first identified in Tamil Nadu, India and for a while displaced El Tor in southern Asia before decreasing in prevalence from 1995 to around 10% of all cases. It is considered to be an intermediate between El Tor and the classic strain and occurs in a new serogroup. There is evidence of the emergence of wide-spectrum resistance to drugs such as trimethoprim, sulfamethoxazole and streptomycin.
False historical report
A persistent myth states that 90,000 people died in Chicago of cholera and typhoid fever in 1885, but this story has no factual basis.[60] In 1885, there was a torrential rainstorm that flushed the Chicago River and its attendant pollutants into Lake Michigan far enough that the city's water supply was contaminated. However, because cholera was not present in the city, there were no cholera-related deaths, though the incident caused the city to become more serious about its sewage treatment.
Cholera morbus
The term cholera morbus was used in the 19th and early 20th centuries to describe both non-epidemic cholera and other gastrointestinal diseases (sometimes epidemic) that resembled cholera. The term is not in current use, but is found in many older references.[61] The other diseases are now known collectively as gastroenteritis.
Other historical information
In the past, people traveling in ships would hang a yellow quarantine flag if one or more of the crew members suffered from cholera. Boats with a yellow flag hung would not be allowed to disembark at any harbor for an extended period, typically 30 to 40 days.[62] In modern international maritime signal flags the quarantine flag is yellow and black.
Research
no research has been done on this topic
Notable cases
The pathos in the last movement of Tchaikovsky's (c. 1840-1893) last symphony made people think that Tchaikovsky had a premonition of death. One observer noted that a week after the premiere of his Sixth Symphony, "Tchaikovsky was dead--6 November 1893. The cause of this indisposition and stomach ache was suspected to be his intentionally infecting himself with cholera by drinking contaminated water. The day before, while having lunch with Modest (his brother and biographer), he is said to have poured tap water from a pitcher into his glass and drunk a few swallows. Since the water was not boiled and cholera was once again rampaging St. Petersburg, such a connection was quite plausible ...."[63]
Other famous people believed to have died of cholera include:
- Elliott Frost, son of American poet Robert Frost[64]
See also
- The Ghost Map: The Story of London's Most Terrifying Epidemic - and How it Changed Science, Cities and the Modern World - which tells the story of how John Snow found the cause of a cholera epidemic, which was the start of modern epidemiology.
- The Painted Veil, starring Naomi Watts and Edward Norton, in which cholera is a prominent subject, based on the novel of the same name by W. Somerset Maugham.
- The Horseman on the Roof (1995 film), starring Juliette Binoche and Olivier Martinez, in which the 1832 cholera outbreak in southern France is a major influence to the story line.
- The Dress Lodger by Sheri Holman - A historical novel set in Sunderland, England during the cholera epidemic of 1831.
- In the novel Death in Venice by Thomas Mann (also a 1971 film by Lucino Visconti starring Dirk Bogard), the main character dies of cholera in Venice; the epidemic is a recurring sub-plot of the story.
- Love in the Time of Cholera, a novel by Nobel Prize winning Colombian author Gabriel García Márquez, and its English-language film adaptation.
Notes
- ^ From Template:Lang-el kholera from χολή kholē "bile".
- ^ D.Kindersley (editor) (1989). AMA Encyclopedia of Medicine. Random House. ISBN 0-394-56528-2.
{{cite book}}:|author=has generic name (help) - ^ Hartwell LH, Hood L, Goldberg ML, Reynolds AE, Silver LM, and Veres RC (2004). Genetics: From genes to genomes. Boston: Mc-Graw Hill. pp. 551–552, 572–574.
{{cite book}}: CS1 maint: multiple names: authors list (link) (using the turning off and turning on of gene expression to make toxin proteins in cholera bacteria as a "comprehensive example" of what is known about the mechanisms by which bacteria change the mix of proteins they manufacture to respond to the changing opportunities for surviving and thriving in different chemical environments). - ^ O'Neal C, Jobling M, Holmes R, Hol W (2005). "Structural basis for the activation of cholera toxin by human ARF6-GTP". Science. 309 (5737): 1093–6. doi:10.1126/science.1113398. PMID 16099990.
{{cite journal}}: Invalid|ref=harv(help)CS1 maint: multiple names: authors list (link) - ^ a b c DiRita VJ, Parsot C, Jander G, Mekalanos JJ (1991). "Regulatory cascade controls virulence in Vibrio cholerae". Proc. Natl. Acad. Sci. U.S.A. 88 (12): 5403–7. doi:10.1073/pnas.88.12.5403. PMC 51881. PMID 2052618.
{{cite journal}}: Invalid|ref=harv(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Swerdlow DL, Mintz ED, Rodriguez M; et al. (1994). "Severe life-threatening cholera associated with blood group O in Peru: implications for the Latin American epidemic". J. Infect. Dis. 170 (2): 468–72. PMID 8035040.
{{cite journal}}: Explicit use of et al. in:|author=(help); Invalid|ref=harv(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Harris JB, Khan AI, LaRocque RC; et al. (2005). "Blood group, immunity, and risk of infection with Vibrio cholerae in an area of endemicity". Infect. Immun. 73 (11): 7422–7. doi:10.1128/IAI.73.11.7422-7427.2005. PMC 1273892. PMID 16239542.
{{cite journal}}: Explicit use of et al. in:|author=(help); Invalid|ref=harv(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Bertranpetit J, Calafell F (1996). "Genetic and geographical variability in cystic fibrosis: evolutionary considerations". Ciba Found. Symp. 197: 97–114, discussion 114–8. PMID 8827370.
{{cite journal}}: Invalid|ref=harv(help) - ^ Ryan KJ, Ray CG (editors) (2004). Sherris Medical Microbiology (4th ed.). McGraw Hill. pp. 376–7. ISBN 0838585299.
{{cite book}}:|author=has generic name (help) - ^ Kirn TJ, Jude BA, Taylor RK (2005). "A colonization factor links Vibrio cholerae environmental survival and human infection". Nature. 438 (7069): 863–6. doi:10.1038/nature04249. PMID 16341015.
{{cite journal}}: Invalid|ref=harv(help); Unknown parameter|DUPLICATE DATA: doi=ignored (help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Archivist (1997). "Cholera phage discovery". Arch Dis Child. 76: 274. doi:10.1136/adc.76.3.274.
{{cite journal}}: Invalid|ref=harv(help) - ^ Merrell DS, Butler SM, Qadri F; et al. (2002). "Host-induced epidemic spread of the cholera bacterium". Nature. 417 (6889): 642–5. doi:10.1038/nature00778. PMC 2776822. PMID 12050664.
{{cite journal}}: Explicit use of et al. in:|author=(help); Invalid|ref=harv(help); Unknown parameter|DUPLICATE DATA: doi=ignored (help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ a b "Laboratory Methods for the Diagnosis of Epidemic Dysentery and Cholera" (pdf). Atlanta, GA: CDC. 1999. Retrieved 2010-02-01.
- ^ a b "Cholera Kills Boy. All Other Suspected Cases Now in Quarantine and Show No Alarming Symptoms" (PDF). New York Times. July 18, 1911. Retrieved 2008-07-28.
The sixth death from cholera since the arrival in this port from Naples of the steamship Moltke, thirteen days ago, occurred yesterday at Swineburne Island. The victim was Francesco Farando, 14 years old.
{{cite news}}: Cite has empty unknown parameter:|coauthors=(help) - ^ a b "More Cholera in Port". Washington Post. October 10, 1910. Retrieved 2008-12-11.
A case of cholera developed today in the steerage of the Hamburg-American liner Moltke, which has been detained at quarantine as a possible cholera carrier since Monday last. Dr. A.H. Doty, health officer of the port, reported the case tonight with the additional information that another cholera patient from the Moltke is under treatment at Swinburne Island.
{{cite news}}: Cite has empty unknown parameter:|coauthors=(help) - ^ a b "Is a vaccine available to prevent cholera?". CDC disease info: Cholera. 2008-03-27. Retrieved 2010-02-01.
- ^ "Cholera vaccines". Health topics. WHO. 2008. Retrieved 2010-02-01.
- ^ "Cholera: prevention and control". Health topics. WHO. 2008. Retrieved 2008-12-08.
- ^ "Cholera treatment". Molson Medical Informatics. 2007. Retrieved 2008-01-03.
- ^ Krishna BV, Patil AB, Chandrasekhar MR (2006). "Fluoroquinolone-resistant Vibrio cholerae isolated during a cholera outbreak in India". Trans. R. Soc. Trop. Med. Hyg. 100 (3): 224–6. doi:10.1016/j.trstmh.2005.07.007. PMID 16246383.
{{cite journal}}: Invalid|ref=harv(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^
Mackay IM (editor) (2007). Real-Time PCR in microbiology: From diagnosis to characterization. Caister Academic Press. ISBN 978-1-904455-18-9.
{{cite book}}:|author=has generic name (help) - ^ Ramamurthy T (2008). "Antibiotic resistance in Vibrio cholerae". Vibrio cholerae: Genomics and molecular biology. Caister Academic Press. ISBN 978-1-904455-33-2.
- ^ http://www.netdoctor.co.uk/travel/diseases/cholera.htm
- ^ http://www.textbookofbacteriology.net/cholera.html
- ^ Disease fact sheet: Cholera. IRC International Water and Sanitation Centre.
- ^ "U.N. reports cholera outbreak in northern Iraq". CNN. 2007-08-30. Retrieved 2010-02-01.
- ^ Smith D (2007-12-02). "Cholera crisis hits Baghdad". The Observer. Retrieved 2010-02-01.
- ^ Jena S (2007-08-29). "Cholera death toll in India rises". BBC News. Retrieved 2010-02-01.
- ^ "Situation report on diarrhoea and cholera in Iraq". ReliefWeb. 2008-10-29. Retrieved 2010-02-01.
- ^ Cholera Country Profile: Vietnam. WHO.
- ^ a b World Health Organization. Cholera in Zimbabwe: Epidemiological Bulletin Number 16 Week 13 (22-28 March 2009). March 31, 2009.; WHO Zimbabwe Daily Cholera Update, 16 April 2009.
- ^ a b World Health Organization: Zimbabwe Daily Cholera Updates. Cite error: The named reference "zimbabwe" was defined multiple times with different content (see the help page).
- ^ Mintz & Guerrant 2009
- ^ 381 new cholera cases in Mpumalanga, News24, 24 January 2009.
- ^ http://www.msnbc.msn.com/id/38852637/ns/health/ Cholera epidemic death toll rises to 352], MSNBC, 25 August 2010.
- ^ Lan R, Reeves PR (2002). "Pandemic Spread of Cholera: Genetic Diversity and Relationships within the Seventh Pandemic Clone of Vibrio cholerae Determined by Amplified Fragment Length Polymorphism" (Free full text). Journal of Clinical Microbiology. 40 (1): 172–181. doi:10.1128/JCM.40.1.172-181.2002. ISSN 0095-1137. PMC 120103. PMID 11773113.
{{cite journal}}: Invalid|ref=harv(help); Unknown parameter|month=ignored (help) - ^ Pike J (2007-10-23). "Cholera- Biological Weapons". Weapons of Mass Destruction (WMD). GlobalSecurity.com. Retrieved 2010-02-01.
- ^ Beardsley GW (2000). "The 1832 Cholera Epidemic in New York State: 19th Century Responses to Cholerae Vibrio (part 1)". The Early America Review. 3 (2). Retrieved 2010-02-01.
{{cite journal}}: Invalid|ref=harv(help) - ^ Asiatic Cholera Pandemic of 1826-37
- ^ a b c d e f g h Rosenberg, Charles E. (1987). The cholera years: the United States in 1832, 1849 and 1866. Chicago: University of Chicago Press. ISBN 0-226-72677-0.
- ^ Wilford JN (2008-04-15). "How Epidemics Helped Shape the Modern Metropolis". New York Times. Retrieved 2010-02-01.
On a Sunday in July 1832, a fearful and somber crowd of New Yorkers gathered in City Hall Park for more bad news. The epidemic of cholera, cause unknown and prognosis dire, had reached its peak.
- ^ Cholera Epidemic in Egypt (1947).
- ^ a b c Asiatic Cholera Pandemic of 1846-63. UCLA School of Public Health.
- ^ Cholera's seven pandemics, cbc.ca, December 2, 2008.
- ^ The Irish Famine.
- ^ Unruh, John David (1993). The plains across: the overland emigrants and the trans-Mississippi West, 1840-60. Urbana, IL: University of Illinois Press. pp. 408–10. ISBN 0-252-06360-0.
- ^ a b Beardsley GW (2000). "The 1832 Cholera Epidemic in New York State: 19th Century Responses to Cholerae Vibrio (part 2)". The Early America Review. 3 (2). Retrieved 2010-02-01.
{{cite journal}}: Invalid|ref=harv(help) - ^ Vibrio cholerae in recreational beach waters and tributaries of Southern California.
- ^ "Local agrarian societies in colonial India: Japanese perspectives.". Kaoru Sugihara, Peter Robb, Haruka Yanagisawa (1996). p 313.
- ^ Chicago Daily Tribune, July 12th, 1854
- ^ Snow, John (1855). "On the Mode of Communication of Cholera".
- ^ Eastern European Plagues and Epidemics 1300-1918.
- ^ Impact of infectious diseases on war. Matthew R. Smallman-Raynor PhD and Andrew D. Cliff DSc [1].
- ^ Vibrio Cholerae and Cholera - The History and Global Impact.
- ^ a b Cholera (11th ed.). 1911. p. 265. Retrieved 2010-01-31.
{{cite book}}:|work=ignored (help) - ^ "The cholera in Spain". New York Times. 1890-06-20. Retrieved 2008-12-08.
- ^ a b "Cholera (pathology): Seven pandemics". Britannica Online Encyclopedia. Retrieved 2010-01-31.
- ^ 1900s: The Epidemic years, Society of Philippine Health History.
- ^ The Boston Medical and Surgical journal. Massachusetts Medical Society. 1911.
In New York, up to July 22, there were eleven deaths from cholera, one of the victims being an employee at the hospital on Swinburne Island, who had been discharged. The tenth was a lad, seventeen years of age, who had been a steerage passenger on the steamship, Moltke. The plan has been adopted of taking cultures from the intestinal tracts of all persons held under observation at Quarantine, and in this way it was discovered that five of the 500 passengers of the Moltke and Perugia, although in excellent health at the time, were harboring cholera microbes.
{{cite book}}: Cite has empty unknown parameter:|coauthors=(help) - ^ "Did 90,000 people die of typhoid fever and cholera in Chicago in 1885?". The Straight Dope. 2004-11-12. Retrieved 2010-02-01.
- ^ "Archaic medical terms". Antiquus Morbus. 2007. Retrieved 2010-02-01.
- ^ Sehdev PS (2002). "The origin of quarantine". Clin. Infect. Dis. 35 (9): 1071–2. doi:10.1086/344062. PMID 12398064.
{{cite journal}}: Invalid|ref=harv(help); Unknown parameter|month=ignored (help) - ^ Meumayr A (1997). Music and medicine: Chopin, Smetana, Tchaikovsky, Mahler: Notes on their lives, works, and medical histories. Med-Ed Press. pp. 282–3. (summarizing various theories on what killed the composer Tchaikovsky, including his brother Modest's idea that Tchaikovksy drank cholera infested water the day before he became ill).
- ^ Burnshaw S (2000). "Robert Frost". American National Biography Online. Archived from the original on 2001-03-18.
References
- Colwell RR (1996). "Global climate and infectious disease: the cholera paradigm". Science. 274 (5295): 2025–31. doi:10.1126/science.274.5295.2025. PMID 8953025.
{{cite journal}}: Invalid|ref=harv(help); Unknown parameter|month=ignored (help) - Drasar, B. S.; Forrest, Bruce D., eds. (1996). Cholera and the ecology of Vibrio cholerae. Springer. p. 355. ISBN 0412612208.
{{cite book}}: Invalid|ref=harv(help) - Furuque, Shah M.; Nair, G. Balakrish, eds. (2008). Vibrio Cholerae: Genomics and Molecular Biology. Horizon Scientific Press. p. 218. ISBN 1904455336.
{{cite book}}: Invalid|ref=harv(help) - Gilbert, Pamela K. (2008). "Cholera and Nation: Doctoring the Social Body in Victorian England" (Document). SUNY Press. p. 231.
{{cite document}}: Invalid|ref=harv(help); Unknown parameter|isbn=ignored (help); Unknown parameter|url=ignored (help) - Jermyn, William S.; O'Shea, Yvonne A.; Quirke, Anne Marie; Boyd, E. Fidelma (2006). "Genomics and the Evolution of Pathogenic Vibrio Cholerae". In Chan, Voon L.; Sherman, Philip M.; Bourke, Billy (eds.). Bacterial genomes and infectious diseases. Humana Press. p. 270. ISBN 158829496X.
{{cite book}}: Invalid|ref=harv(help) - Mintz ED, Guerrant RL (2009). "A lion in our village--the unconscionable tragedy of cholera in Africa". N. Engl. J. Med. 360 (11): 1060–3. doi:10.1056/NEJMp0810559. PMID 19279337.
{{cite journal}}: Invalid|ref=harv(help); Unknown parameter|month=ignored (help) - Pardio Sedas, Violeta T. (2008). "Impact of Climate and Environmental Factors on the Epidemiology of Vibrio choerae in Aquatic Ecosystems". In Hofer, Tobias N. (ed.). Marine Pollution: New Research. Nova Science publishers. p. 448. pp. 221–254. ISBN 1604562420.
{{cite book}}: Invalid|ref=harv(help) - Ryan, Kenneth J.; Ray, C. George, eds. (2003). Sherris medical microbiology: an introduction to infectious diseases (4th ed.). ISBN 0838585299.
{{cite book}}: Invalid|ref=harv(help); Unknown parameter|unused_data=ignored (help) - Wachsmuth, Kaye; Blake, Paul A.; Olsvik, Ørjan, eds. (1994). Vibrio cholerae and cholera: molecular to global perspectives. ASM Press. p. 465. ISBN 1555810675.
{{cite book}}: Invalid|ref=harv(help)
Further reading
- Crump JA, Bopp CA, Greene KD; et al. (2003). "Toxigenic Vibrio cholerae serogroup O141-associated cholera-like diarrhea and bloodstream infection in the United States". J. Infect. Dis. 187 (5): 866–8. doi:10.1086/368330. PMID 12599062.
{{cite journal}}: Explicit use of et al. in:|author=(help); Invalid|ref=harv(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Steinberg EB, Greene KD, Bopp CA, Cameron DN, Wells JG, Mintz ED (2001). "Cholera in the United States, 1995-2000: trends at the end of the twentieth century". J. Infect. Dis. 184 (6): 799–802. doi:10.1086/322989. PMID 11517445.
{{cite journal}}: Invalid|ref=harv(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link)
External links
- Cholera - World Health Organization
- Map of recent international outbreaks
- What is Cholera? - Centers for Disease Control and Prevention
- Cholera information for travelers - Centers for Disease Control and Prevention
- Steven Shapin, "Sick City: Maps and mortality in the time of cholera", The New Yorker May 2006. A review of Steven Johnson, “The Ghost Map: The story of London’s most terrifying epidemic — and how it changed science, cities, and the modern world”
- Cholera Epidemic in NYC in 1832 New York Times 15 April 2008
