Vagina: Difference between revisions
Major expansion/Tweaks. Also added a bit taken from other Wikipedia articles, such cunt and labiaplasty. |
m Fixed my typo. Of course...focusing on the article body before the article lead can be more important, since it can tell an editor how to format the lead, but this article expansion has given me a decent or OK-ish outline for the lead. |
||
| Line 29: | Line 29: | ||
The vagina plays significant role in [[Human female|human female sexuality]] and [[sexual pleasure]]. During [[sexual arousal]] for humans and others animals, vaginal moisture increases by way of [[vaginal lubrication]], to reduce friction and allow for smoother penetration of the vagina during sexual activity. In the absence or presence of sufficient vaginal lubrication, the texture of the vaginal walls can create friction for the [[penis]] during sexual intercourse and stimulate it toward [[ejaculation]], enabling [[fertilization]].<ref name="Jacoby">{{cite book|authors=David B. Jacoby, R. M. Youngson|title=Encyclopedia of Family Health|accessdate=April 25, 2014|year=2004|publisher=[[Marshall Cavendish]]|isbn=0761474862|page=964|url=http://books.google.com/books?id=aDDBfZMVL04C&printsec=frontcover&dq=&hl=en&sa=X&ei=dBNbU-mSHZGqyASDq4HoBA&ved=0CD4Q6AEwAA#v=onepage&q=&f=false}}</ref> In addition, a variety of [[Sexually transmitted disease|sexually transmitted infections]] (STIs/STDs) and other disorders can affect the vagina.<ref name="Hales">{{Cite book|author=Dianne Hales|title=An Invitation to Health Brief 2010-2011| publisher = [[Cengage Learning]]|year = 2008|accessdate=August 29, 2013|pages =269–271| isbn = 0495391921|url=http://books.google.com/books?id=oP91HVIMPRIC&pg=PA269}}</ref><ref name="Alexander">{{cite book|authors=William Alexander, Helaine Bader, Judith H. LaRosa|title=New Dimensions in Women's Health|isbn =1449683754|publisher=[[Jones & Bartlett Learning|Jones & Bartlett Publishers]]|year=2011|page=211|accessdate=August 29, 2013|url=http://books.google.com/books?id=GVPHhIM3IZ0C&pg=PA211}}</ref> Because of the risk of STIs/STDs, health authorities, such as the [[World Health Organization]] (WHO), or other health outlets, recommend [[safe sex]] practices.<ref name="Hales"/><ref name="WHO">{{cite web| title = Global strategy for the prevention and control of sexually transmitted infections: 2006–2015. Breaking the chain of transmission| publisher = [[World Health Organization]]|year = 2007| accessdate=November 26, 2011|url=http://whqlibdoc.who.int/publications/2007/9789241563475_eng.pdf}}</ref> |
The vagina plays significant role in [[Human female|human female sexuality]] and [[sexual pleasure]]. During [[sexual arousal]] for humans and others animals, vaginal moisture increases by way of [[vaginal lubrication]], to reduce friction and allow for smoother penetration of the vagina during sexual activity. In the absence or presence of sufficient vaginal lubrication, the texture of the vaginal walls can create friction for the [[penis]] during sexual intercourse and stimulate it toward [[ejaculation]], enabling [[fertilization]].<ref name="Jacoby">{{cite book|authors=David B. Jacoby, R. M. Youngson|title=Encyclopedia of Family Health|accessdate=April 25, 2014|year=2004|publisher=[[Marshall Cavendish]]|isbn=0761474862|page=964|url=http://books.google.com/books?id=aDDBfZMVL04C&printsec=frontcover&dq=&hl=en&sa=X&ei=dBNbU-mSHZGqyASDq4HoBA&ved=0CD4Q6AEwAA#v=onepage&q=&f=false}}</ref> In addition, a variety of [[Sexually transmitted disease|sexually transmitted infections]] (STIs/STDs) and other disorders can affect the vagina.<ref name="Hales">{{Cite book|author=Dianne Hales|title=An Invitation to Health Brief 2010-2011| publisher = [[Cengage Learning]]|year = 2008|accessdate=August 29, 2013|pages =269–271| isbn = 0495391921|url=http://books.google.com/books?id=oP91HVIMPRIC&pg=PA269}}</ref><ref name="Alexander">{{cite book|authors=William Alexander, Helaine Bader, Judith H. LaRosa|title=New Dimensions in Women's Health|isbn =1449683754|publisher=[[Jones & Bartlett Learning|Jones & Bartlett Publishers]]|year=2011|page=211|accessdate=August 29, 2013|url=http://books.google.com/books?id=GVPHhIM3IZ0C&pg=PA211}}</ref> Because of the risk of STIs/STDs, health authorities, such as the [[World Health Organization]] (WHO), or other health outlets, recommend [[safe sex]] practices.<ref name="Hales"/><ref name="WHO">{{cite web| title = Global strategy for the prevention and control of sexually transmitted infections: 2006–2015. Breaking the chain of transmission| publisher = [[World Health Organization]]|year = 2007| accessdate=November 26, 2011|url=http://whqlibdoc.who.int/publications/2007/9789241563475_eng.pdf}}</ref> |
||
Cultural perceptions of the vagina have persisted throughout history; these perceptions range from viewing the vagina as the focus [[sexual desire]], a metaphor for life via birth, as an organ inferior to the penis, or as visually unappealing or otherwise [[Vulgarism|vulgar]]. |
Cultural perceptions of the vagina have persisted throughout history; these perceptions range from viewing the vagina as the focus of [[sexual desire]], a metaphor for life via birth, as an organ inferior to the penis, or as visually unappealing or otherwise [[Vulgarism|vulgar]]. |
||
==Etymology and definition== |
==Etymology and definition== |
||
Revision as of 09:05, 10 June 2014
| Vagina | |
|---|---|
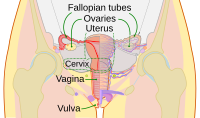 Vagina in the female human reproductive system. | |
 Vulva with vaginal opening | |
| Details | |
| Precursor | urogenital sinus and paramesonephric ducts |
| Artery | superior part to uterine artery, middle and inferior parts to vaginal artery |
| Vein | uterovaginal venous plexus, vaginal vein |
| Nerve | Sympathetic: lumbar splanchnic plexus Parasympathetic: pelvic splanchnic plexus |
| Lymph | upper part to internal iliac lymph nodes, lower part to superficial inguinal lymph nodes |
| Identifiers | |
| Latin | Vagina |
| MeSH | D014621 |
| TA98 | A09.1.04.001 |
| TA2 | 3523 |
| FMA | 19949 |
| Anatomical terminology | |
The vagina is a fibromuscular elastic tubular tract (passage) which is a sex organ and mainly functions for the facilitation of sexual intercourse and childbirth. In mammals (especially primates), menstruation, which is the periodic discharge of blood and mucosal tissue from the inner lining of the uterus through the vagina, is another primary function of the vagina and usually signals fertility. The location and size of the vagina varies among species, and may vary in size within the same species. In humans, the vagina leads from the opening of the vulva to the uterus (womb), but the vaginal tract ends at the cervix.
Unlike mammalian males, who usually have only one genital orifice, mammalian females usually have two, the urethra and the vagina. The vaginal opening is much larger than the urethral opening, and both openings are protected by the labia.[1][2] Regarding amphibians, birds, reptiles and monotremes, the female reproductive tract is generally known among zoologists as a cloaca; in these species, it may additionally serve as intestinal and urinary tracts.
The vagina plays significant role in human female sexuality and sexual pleasure. During sexual arousal for humans and others animals, vaginal moisture increases by way of vaginal lubrication, to reduce friction and allow for smoother penetration of the vagina during sexual activity. In the absence or presence of sufficient vaginal lubrication, the texture of the vaginal walls can create friction for the penis during sexual intercourse and stimulate it toward ejaculation, enabling fertilization.[3] In addition, a variety of sexually transmitted infections (STIs/STDs) and other disorders can affect the vagina.[4][5] Because of the risk of STIs/STDs, health authorities, such as the World Health Organization (WHO), or other health outlets, recommend safe sex practices.[4][6]
Cultural perceptions of the vagina have persisted throughout history; these perceptions range from viewing the vagina as the focus of sexual desire, a metaphor for life via birth, as an organ inferior to the penis, or as visually unappealing or otherwise vulgar.
Etymology and definition
The term vagina is from Latin vāgīna, literally "sheath" or "scabbard." It is often referred to as the birth canal in the context of pregnancy and childbirth, though the term is, by definition, the area between the outside of the vagina and the fully dilated uterus.[7]
The Latinate plural "vaginae" is rarely used in English. Colloquially, the word vagina is often used to refer to the vulva or to the female genitals in general.[8] However, by its dictionary and anatomical definitions, vagina refers exclusively to the specific internal structure.
Structure
Embryonic development
The vagina is derived from the embryonic Müllerian duct.[9] During sexual differentiation (sex development of the differences between males and females), if exposed to testosterone, fusion of the urogenital folds (elongated spindle-shaped structures that contribute to the formation of the urethral groove on the belly aspect of the genital tubercle) allows the urogenital sinus to close completely and form the spongy urethra, while the labioscrotal swellings unite to form the scrotum. In the absence of testosterone, the urogenital sinus persists as the vestibule of the vagina, the two urogenital folds form the labia minora, and the labioscrotal swellings enlarge to form the labia majora.[10][11]
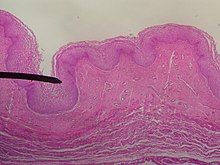
General structure and histology
The human vagina is an elastic muscular canal that extends from the cervix (or uterine cavity) to the vulva.[12][13] It, along with the inside of the vulva, is reddish pink in color, and it connects the superficial vulva to the cervix of the deep uterus. The vagina, posterior to the urethra and bladder, reaches across the perineum superiorly and posteriorly toward the cervix; at approximately a 90 degree angle, the cervix protrudes into the vagina.[14]
The vagina's internal lining consists of stratified squamous epithelium.[13][15] Beneath this lining is a layer of smooth muscle, which may contract during vaginal intercourse and when giving birth. Beneath the muscle is a layer of connective tissue called adventitia.[16]
Maternal estrogen, from birth to 10-14 days, is the reason newborn females have a stratified squamous epithelium. After this age range, to the prepubertal age and in the post-menopause age, the epithelium thins out and is composed of a few layers. The epithelium is absent of glands, beginning with puberty up until menopause.[13] Consisting of three different layers of cells – superficial cornified cells, intermediate cells and basal cells – estrogen supplies the intermediate and superficial cells with glycogen. The cells layering the vaginal area of the cervix become constant with the intermediate and superficial cells; the intermediate and superficial cells reach to the squamocolumnar junction at the external orifice of the uterus (external os). The superficial cells exfoliate continuously, especially while in an inflammatory or neoplastic state. The basal cells replace the superficial cells. Keratinization results when the epithelium is exposed to the dry external atmosphere.[13]
Regarding blood and nerve supply, relevant arteries are the cervicovaginal branch of the uterine artery, the vaginal artery, middle rectal artery, and the internal pudendal artery. The veins are connected by anastomosis (the connection of separate parts of a branching system to form a network), resulting in the formation of the anterior and posterior azygos (unpaired) arteries. The nerve supply of the vagina is provided by the sympathetic and parasympathetic areas of the pelvic plexus, with the pudendal nerve supplying the lower area.[13]
Regions and layers
Where the vaginal lumen surrounds the cervix of the uterus, it is divided into four regions of fornices (the vaginal fornix); these are the anterior, posterior, and the right lateral and left lateral (the lateral fornix).[12][13] The posterior is deeper and the anterior is shallow.[13] While the anterior and posterior walls are placed together, the lateral walls, especially their middle area, are relatively more rigid; because of this, they have an H-shape across the section.[13]
Supporting the vagina are its upper third, middle third and lower third. The upper third concerns the levator ani muscles (transcervical, pubocervical) and the sacrocervical ligaments; these areas are also described as the cardinal ligaments laterally and uterosacral ligaments posterolaterally. The middle third of the vagina concerns the urogenital diaphragm (also described as the paracolpos and pelvic diaphragm). The lower third concerns the perineal body; it is sometimes described as containing the perineal body, pelvic diaphragm and urogenital diaphragm.[12][17]
Three layers, sometimes categorized as four layers, compose the vaginal walls.[14][15][16][18] With regard to three layers, the walls may be described as:[14][16]
- the first layer is made up of a stratified squamous non-keratinized epithelium and is an underlying lamina propria of connective tissue (a layer of connective tissue that is highly vascular under the base area lining the epithelium)
- the second layer is the muscular layer, which is composed of smooth muscle fibers and situated longitudinally and circularly
- the third layer is the adventitia, which is a dense connective tissue that blends with the fascia surrounding the area
When categorized as four layers, the vaginal walls may be described in significantly more detail:[15][19]
- the first layer is an inner layer of non-keratinized squamous epithelium, which forms the folds or rugae and facilitate the vagina's ability to expand large enough for child birth. The rugae are a series of ridges produced by folding of the wall of the outer third of the vagina; they are transverse epithelial ridges and their function is to provide the vagina with increased surface area for extension and stretching
- the second layer of the vagina is connective tissue, which contains blood vessels
- the third layer is the muscle layer; it is an outer layer of longitudinal muscle, as well as the inner layer of circular muscle
- the fourth layer is an outer layer of connective tissue; it is continuous with the other pelvic organs and is made up of blood and lymphatic vessels and fibers
The upper one-fourth of the vagina is separated from the rectum by the recto-uterine pouch. Above the vagina is a cushion of fat called the mons pubis which surrounds the pubic bone and provides protective support during vaginal intercourse.
Vaginal opening and hymen
The vaginal opening (or orifice) is at the caudal end of the vulva, behind the opening of the urethra, resting at the posterior end of the vestibule. It is closed by the labia minora in female virgins and in females who have never given birth (nulliparae), but may be exposed in females who have given birth (parous females).[13]
The hymen is a membrane of tissue that surrounds or partially covers the vaginal opening.[13] The effects of vaginal intercourse and childbirth on the hymen are variable. If the hymen is sufficiently elastic, it may return to nearly its original condition. In other cases, there may be remnants (carunculae myrtiformes), or it may appear completely absent after repeated penetration.[3][20] Additionally, the hymen may be lacerated by disease, injury, medical examination, masturbation or physical exercise. For these reasons, it is not possible to definitively determine whether or not a girl or woman is a virgin by examining her hymen.[3][20][21][22]
Lubrication
The Bartholin's glands, located near the vaginal opening and cervix, were originally thought to be the primary source for vaginal lubrication, but they provide only a few drops of mucus for vaginal lubrication;[23] the significant majority of vaginal lubrication is generally believed to be provided by plasma seepage from the vaginal walls, which is called vaginal transudation. Vaginal transudation, which initially forms as sweat-like droplets, is caused by vascular engorgement of the vagina (vasocongestion); this results in the pressure inside the capillaries increasing the transudation of plasma through the vaginal epithelium.[23][24][25]
Before and during ovulation, the cervix's mucus glands secrete different variations of mucus, which provides an alkaline environment in the vaginal canal that is favorable to the survival of sperm. "Vaginal lubrication typically decreases as women age, but this is a natural physical change that does not normally mean there is any physical or psychological problem. After menopause, the body produces less estrogen, which, unless compensated for with estrogen replacement therapy, causes the vaginal walls to thin out significantly."[26]
Variations and size
In its normal state, there is anatomical variation in the length of the vagina of a woman of child-bearing age. The length is approximately 7.5 cm (2.5 to 3 in) across the anterior wall (front), and 9 cm (3.5 in) long across the posterior wall (rear), making the posterior fornix deeper than the anterior.[15][13] During sexual arousal, the vagina expands in both length and width.
If a woman stands upright, the vaginal tube points in an upward-backward direction and forms an angle of approximately 45 degrees with the uterus and of about 60 degrees to horizon.[13][17]

The vaginal opening and hymen can vary in size; in children, although a common appearance of the hymen is crescent-shaped, many shapes are possible.[13][27]
Function
Secretions
The vagina provides a path for menstrual blood and tissue to leave the body. In industrial societies, tampons, menstrual cups and sanitary napkins may be used to absorb or capture these fluids. Vaginal secretions are primarily from the uterus, cervix, and, during sexual arousal, transudation of the vaginal epithelium and miniscule lubrication from the Bartholin's glands. It takes little vaginal secretion to make the vagina moist. The secretions may be minor in excess during sexual arousal, the middle of the menstrual cycle, a little prior to menstruation, or during pregnancy.[13]
Sexual activity
The concentration of the nerve endings that lie close to the entrance of a woman's vagina (the lower third) can provide pleasurable vaginal sensations during sexual activity when stimulated, and many women additionally derive pleasure from a feeling of closeness and fullness during penetration of the vagina.[28][29] The vagina as a whole, however, lacks nerve endings, which commonly hinders a woman's ability to receive sufficient sexual stimulation, including orgasm, solely from vaginal sexual activity.[28][29][30][31] The outer one-third of the vagina, especially near the opening, contains the majority of the vaginal nerve endings, making it more sensitive to touch than the inner two-thirds of the vaginal barrel.[28][29][31] This factor is considered to make the process of child birth significantly less painful, because an increased number of nerve endings means that there is an increased possibility for pain as well as pleasure.[28][32][33]
There are a variety of ways that pleasure can be received from vaginal stimulation, including by masturbation, fingering (with or without a sexual partner, whether as foreplay or as a central activity), oral sex (cunnilingus), or by specific sex positions (such as the missionary position or the spoons sex position).[34] Some women use sex toys, such as a vibrator or dildo, for vaginal pleasure.[35] The clitoris additionally plays a part in vaginal stimulation, as it is a sex organ containing an abundance of nerve endings and is of multiplanar structure with a broad attachment to the pubic arch and extensive supporting tissue to the mons pubis and labia, centrally attached to the urethra and vagina. Clitoral tissue forms a tissue cluster with the vagina. The tissue is more extensive in some women than in others, which may contribute to orgasms experienced vaginally.[30][31][36]
During sexual arousal, and particularly the stimulation of the clitoris, the walls of the vagina lubricate. This reduces friction or injury that can be caused by insertion of the penis into the vagina or other penetration of the vagina during sexual activity.[3][26] With sexual arousal, the human vagina lengthens rapidly,[26] to an average of about 4 in.(10 cm), but can continue to lengthen in response to pressure. As the woman becomes fully aroused, the vagina tents (last ²⁄₃) expands in length and width, while the cervix retracts. The elastic walls of the vagina stretch or contract, with support from the pelvic muscles, to the size of the inserted penis or other object,[3][26] stimulating the penis and helping to cause the male to experience orgasm and ejaculation; this in turn enables fertilization.[3]
An area in the vagina that may be an erogenous zone is the G-spot (also known as the Gräfenberg spot); it is typically defined as being located at the anterior wall of the vagina, about five centimeters in from the entrance. Some women experience intense pleasure, and sometimes an orgasm, if this area is stimulated during sexual activity. A G-spot orgasm may be responsible for female ejaculation, leading some doctors and researchers to believe that G-spot pleasure comes from the Skene's glands, a female homologue of the prostate, rather than any particular spot on the vaginal wall.[37][38] Other researchers consider the connection between the Skene's glands and the G-spot to be weak.[39][40] They contend that the Skene's glands do not appear to have receptors for touch stimulation, and that there is no direct evidence for their involvement. The G-spot's existence, and existence as a distinct structure, is still under dispute, as its location can vary from woman to woman, appears to be nonexistent in some women,[32][36][39] and it is hypothesized to be an extension of the clitoris and therefore the reason for orgasms experienced vaginally.[30][36]
Childbirth
During childbirth, the vagina provides the channel to deliver the newborn from the uterus to its independent life outside the body of the mother. During birth, the elasticity of the vagina allows it to stretch to many times its normal diameter.
Vaginal ecosystem and acidity
The vagina is a nutrient rich environment that harbors a unique and complex microflora. It is a dynamic ecosystem that undergoes long term changes, from neonate to puberty and from the reproductive period (menarche) to menopause. Moreover, under the influence of hormones, such as estrogen (estradiol), progesterone and follicle stimulating hormone (FSH), the vaginal ecosystem undergoes cyclic or periodic changes, i.e. during menses and pregnancy.[41] One significant variable parameter is the vaginal pH, which varies significantly during a woman‘s lifespan, from 7.0 in premenarchal girls, to 3.8-4.4 in women of reproductive age to 6.5-7.0 during menopause without hormone therapy and 4.5-5.0 with hormone replacement therapy.[41] Estrogen, glycogen and lactobacilli are important factors in this variation.[41]
The vagina of a newborn is affected by the residual maternal estrogen still present. At birth, the vaginal mucosa is rich in glycogen and the vagina becomes colonized by lactic-acid producing bacteria, such as Lactobacillus spp., within the first day after birth. These estrogen effects will slowly disappear by the fourth week after birth and the glycogen content will diminish. The vaginal pH becomes neutral or alkaline, likely due to the almost absence of lactic-acid producing microorganisms.[42] In premenarchal girls, the vaginal microflora is composed of anaerobic and aerobic cocci and rods with low loads of lactobacilli, Gardnerella vaginalis and Mobiluncus spp.[41][42] During puberty, the estrogen levels rise until they reach the concentrations found in adult women. The estrogen causes the vaginal epithelium to thicken and the intracellular glycogen production to rise, which consequently causes a shift in the composition of the vaginal microflora.[42] At this moment, lactobacilli, probably from the rectum,[43][44] become the most important inhabitants colonizing the vaginal econiche, utilizing the available glycogen, which is converted to lactic acid, resulting in the acidification (pH < 4.4) of the vagina.[41][43][44][45] In addition, besides lactic acid, the principal vaginal acidifier, other organic acids, i.e. acetic and linoleic acid, are also normally found in vaginal fluid.[46]
The source of the lactic acid has been subject to debate. Some studies suggest that the presence of estrogen and not Lactobacillus is primarily related to acidification of the vagina, and even that lactobacilli cannot produce lactic acid from glycogen. The overall vaginal pH can be attributed to the total of estrogen mediated lactic acid production by the epithelial cells (producing only the L-isomer of lactate) and the lactic acid contribution by the endogenous vaginal bacteria (producing both D- and L-isomers of lactate).[46][47] Boskey et al.,[48] studying vaginal lactate production in 11 women, found that D-lactate (bacterial origin) in vaginal secretions ranged from 6% to 75%, with a mean of 55%. They concluded that these findings supported the role of Lactobacillus as the primary source for vaginal acidification, although the wide range found was not indicative for a dominant bacterial source of lactate in all women. Moreover, the midportion of the vagina has a higher pH than the vaginal fornix, although the lactobacilli concentration is uniform throughout the vaginal canal.[46] This is indicative for the fact that the vaginal mucosal metabolism may be more dominant in determining the final pH.[46]
However, in a pyrosequencing study by Ravel et al.[49] of the vaginal microflora of 396 asymptomatic North American women, representing four ethnic groups (white, black, Hispanic, and Asian), the higher median pH values in Hispanic (pH 5.0 ± 0.59) and black (pH 4.7 ± 1.04) women reflected a higher prevalence of communities not dominated by Lactobacillus spp. in these two ethnic groups, when compared with Asian (pH 4.4 ± 0.59) and white (pH 4.2 ± 0.3) women. Ravel et al.[49] found that the lowest pH values were associated with vaginal ecosystems dominated by L. iners and L. crispatus, and the highest pH values were associated with vaginal ecosystems not dominated by species of Lactobacillus.[49][50] The results of Ravel may be controversial for L.iners, which was strongly associated with Bacterial vaginosis-like vaginal microflora, which is characterized by alkaline pH.[51][52] Hummelen et al.[50] stated in their pyrosequencing study that L. crispatus is associated with a low pH, but when L. crispatus is not present, a large fraction of L. iners is required to predict a low pH.[50] Nevertheless, these results indicate that bacteria play an important role in the acidification of the vagina and more research, e.g. regarding the resource of glycogen, used to produce lactic acid and regarding the bacterial species that can metabolize glycogen, is needed to understand the various factors that govern vaginal pH.
Next to the protective effects of pH and the endogenous vaginal microflora, pathogen colonization is also prevented by the local components of the innate and acquired immune systems.[53] The innate immune system recognizes pathogen-associated molecular patterns (PAMPs) on microbial pathogens and includes soluble factors (e.g. mannose-binding lectin, complement components, defensins, secretory leukocyte protease inhibitor (SLPI) and nitric oxide), membrane-associated components (e.g. Toll-like receptors) and tissue-associated phagocytes (macrophages and neutrophils).[46][53] The vaginal adaptive (acquired) immunity produces locally IgG and IgA, which will recognize and bind to specific antigens on microorganisms in the vagina.[54] For instance, an IgA response against G. vaginalis vaginolysin has been reported and a correlation between this response and BV has been shown.[55]
Finally, after the reproductive years, women enter the menopause, which is characterized by the cessation of menstruation because of the loss of follicular activity. The circulating estrogen levels are low and the glycogen content is low to absent, resulting in a rise of the vaginal pH, and consequently the vagina is colonized by bacteria associated with intermediate/disturbed vaginal microflora.[56][57] It has been shown that estrogen therapy can augment the loads of lactobacilli, which in turn can diminish the increased risk for BV and urinary tract infections.[56] However, the absence of lactobacilli by itself is not related to an elevated prevalence of BV,[58] and estrogen replacement may merely potentiate the effect of lactobacilli present on the vaginal pH.[59]
The vaginal ecosystem is under the influence of many factors, endogenous (hormonal, innate immunity, ethnicity), as well as exogenous (behavioral factors, such as sexual activity, cigarette smoking, douching and antibiotic treatment in general),[60][61][62] that are determinative for the vaginal health. The endogenous susceptibility for disturbance of the vaginal microflora and for infections is determined by the genetic characteristics of each individual woman,[49][53] the specific composition of her vaginal microflora at a certain point in time and the genotypic differences between the vaginal lactobacilli present (at species and strain level).[63][64]
Clinical significance
General
The vagina is self-cleansing and therefore usually needs no special treatment. Doctors generally discourage the practice of douching.[65] Since a healthy vagina is colonized by a mutually symbiotic flora of microorganisms that protect its host from disease-causing microbes, any attempt to upset this balance may cause many undesirable outcomes, including but not limited to abnormal discharge and yeast infection.
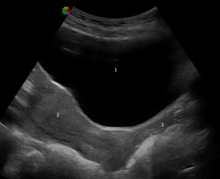
The vagina is examined during gynecological exams, often using a speculum, which holds the vagina open for visual inspection of the cervix or taking of samples (see pap smear).[66] Medical activities involving the vagina, including examinations, administration of medicine, and inspection of discharges, are also referred to as being per vaginam (or p.v.).[67]
The healthy vagina of a woman of child-bearing age is acidic, with a pH normally ranging between 3.8 and 4.5.[68] This is due to the degradation of glycogen to the lactic acid by enzymes secreted by the Döderlein's bacillus. This is a normal commensal of the vagina. The acidity retards the growth of many strains of pathogenic microbes.[69]
Intravaginal administration is a route of administration where the substance is applied to the inside of the vagina. Pharmacologically, it has the potential advantage to result in effects primarily in the vagina or nearby structures (such as the vaginal portion of cervix) with limited systemic adverse effects compared to other routes of administration.
Sexually transmitted infections and other disorders
The herpes simplex virus (HSV), which can be transmitted sexually, can infect the vulva, vagina, and cervix, and this may result in small, painful, recurring blisters and ulcers.[66] It is also common for there to be an absence of any noticeable symptoms.[66] Other sexually transmitted infections (STIs/STDs) that may infect the vagina include gonorrhea, chlamydia, trichomoniasis and human papillomavirus (HPV), which may cause genital warts.[66] HIV/AIDS can be contracted through the vagina during vaginal intercourse, but it is not associated with any local vaginal or vulval disease.[70] Health authorities and other health outlets recommend safe sex practices when engaging in sexual activity.[4][5][6]
Vaginismus, which is not the same thing as vaginitis (an inflammation of the vagina), is an involuntary tightening of the vagina due to a conditioned reflex of the muscles in the area during vaginal penetration.[66] It can affect any form of vaginal penetration, including sexual intercourse, insertion of tampons and menstrual cups, and the penetration involved in gynecological examinations. Various psychological and physical treatments are possible to help alleviate it.
With regard to other vaginal health issues, an increased pH of the vagina (with a commonly used cut-off of pH 4.5 or higher) can be caused by bacterial overgrowth, as occurs in bacterial vaginosis and trichomoniasis, or rupture of membranes in pregnancy.[68] Vaginal cancer is very rare, but its symptoms include abnormal vaginal bleeding or vaginal discharge.[66] Vaginal prolapse may result in the case of weakened pelvic muscles, which is a common result of childbirth; in the case of this prolapse, the rectum, uterus, or bladder pushes on the vagina, and severe cases result in the vagina protruding out of the body.[66] Kegel exercises have been used to strengthen the pelvic floor, and may help prevent or remedy vaginal prolapse.[66][71]
In the case of oral sex, a fatal condition known as an air embolism, in which an air bubble travels throughout the bloodstream and can obstruct the vessel, can result if air is blown into a pregnant woman's vagina during cunnilingus; this is because pregnant women have an increased vascularity of the vagina and uterus, and an air embolism can force air into the uterine veins.[34]
Another vaginal disorder is persistent genital arousal disorder (PGAD), which results in a spontaneous, persistent, and uncontrollable genital arousal, with or without orgasm, unrelated to any feelings of sexual desire.[72][73][74] Because PGAD is relatively rare and, as its own concept apart from clitoral priapism (a rare, potentially painful medical condition in which, for an unusually extended period of time, the erect clitoris does not return to its relaxed state), has only been researched since 2001, there is little research into what may cure or remedy the disorder.[74] In some recorded cases, PGAD was caused by, or caused, a pelvic arterial-venous malformation with arterial branches to the clitoris; surgical treatment was effective in these cases.[75]
Lumps
The presence of unusual lumps in the wall or base of the vagina is always abnormal. The most common of these is Bartholin's cyst.[76] The cyst, which can feel like a pea, is formed by a blockage in glands which normally supply the opening of the vagina. This condition is easily treated with minor surgery or silver nitrate. Other less common causes of small lumps or vesicles are herpes simplex. They are usually multiple and very painful with a clear fluid leaving a crust. They may be associated with generalized swelling and are very tender. Lumps associated with cancer of the vaginal wall are very rare and the average age of onset is seventy years.[77] The most common form is squamous cell carcinoma, then cancer of the glands or adenocarcinoma and finally, and even more rarely, melanoma.
Discharge
Most vaginal discharges occur due to normal bodily functions such as menstruation or sexual arousal (vaginal lubrication). Abnormal discharges, however, can indicate disease.
Normal vaginal discharges include blood or menses (from the uterus), the most common, and clear fluid either as a result of sexual arousal or secretions from the cervix. Other non-infective causes include dermatitis. Non-sexually transmitted discharges occur from bacterial vaginosis and thrush or candidiasis. The final group of discharges include the sexually transmitted diseases gonorrhea, chlamydia, and trichomoniasis. The discharge from thrush is slightly pungent and white, that from trichomoniasis more foul and greenish, and that from foreign bodies resembling the discharge of gonorrhea, greyish or yellow and purulent (pus-like).[78]
Sores
All sores involve a breakdown in the walls of the fine membrane of the vaginal wall. The most common of these are abrasions and small ulcers caused by trauma. While these can be inflicted during rape most are actually caused by excessive rubbing from clothing or improper insertion of a sanitary tampon. The typical ulcer or sore caused by syphilis is painless with raised edges. These are often undetected because they occur mostly inside the vagina. The sores of herpes which occur with vesicles are extremely tender and may cause such swelling that passing urine is difficult. In the developing world, a group of parasitic diseases also cause vaginal ulceration, such as leishmaniasis, but these are rarely encountered in the west. All of the aforementioned local vulvovaginal diseases are easily treated. Often, only shame prevents patients from presenting for treatment.[79]
Modification
The vagina may be an aspect of genital modification during female genital mutilation (FGM), which may additionally be known as female circumcision or female genital cutting (FGC).[80][81] The most severe form of FGM is infibulation, in which there is removal of all or part of the inner and outer labia (labia majora) and the closure of the vagina; this is called Type III FGM, and it involves a small hole being left for the passage of urine and menstrual blood, with the vagina being opened up for sexual intercourse and childbirth.[81]
Alteration to the vaginal lips (labia minora) may also be a factor, which is an aspect of labiaplasty. There are two main categories of women seeking cosmetic genital surgery: those with congenital conditions such as an intersex condition, and those with no underlying condition who experience physical discomfort or wish to alter the appearance of their genitals because they believe they do not fall within a normal range.[82]
Society and culture
Biological perceptions and vulgarity
There have been various perceptions of the vagina throughout history, ranging from it being the center of sexual desire, a symbol of sexual power, a metaphor for life via birth, inferior to the penis, visually unappealing or inherently "smelly," or otherwise vulgar.[83][84][85] In Ancient times, it was often considered equivalent (homologous) to the penis; anatomists Galen (129 AD – 200 AD) and Vesalius (1514–1564), regarded the organs as structurally the same, except for the vagina being inverted. Anatomical studies over latter centuries, however, showed the clitoris to be the penile equivalent.[30][86]
The vagina has been termed many vulgar names,[87] two being cunt and pussy. Cunt is used as a derogatory epithet referring to people of either sex. This usage is relatively recent, dating from the late nineteenth century.[88] Reflecting different national usages, cunt is described as "an unpleasant or stupid person" in the Compact Oxford English Dictionary, whereas Merriam-Webster has a usage of the term as "usually disparaging and obscene: woman",[89] noting that it is used in the U.S. as "an offensive way to refer to a woman";[90] and the Macquarie Dictionary of Australian English states that it is "a despicable man". When used with a positive qualifier (good, funny, clever, etc.) in Britain, New Zealand and Australia, it can convey a positive sense of the object or person referred to.[91] Pussy, on the other hand, can indicate "cowardice or weakness", and "the human vulva or vagina" or by extension "sexual intercourse with a woman".[92]
The release of vaginal fluids were considered by medical practitioners to cure or remedy a number of ailments; various methods were used over the centuries to release "female seed" (via vaginal lubrication or female ejaculation) as a treatment for suffocation ex semine retento (suffocation of the womb), female hysteria or green sickness. Methods included a midwife rubbing the inside of the vagina or insertion of the penis or penis-shaped objects into the vagina. Supposed symptoms of female hysteria included faintness, nervousness, insomnia, fluid retention, heaviness in abdomen, muscle spasm, shortness of breath, irritability, loss of appetite for food or sex, and "a tendency to cause trouble".[93] Women considered suffering from the condition would sometimes undergo "pelvic massage" — stimulation of the genitals by the doctor until the woman experienced "hysterical paroxysm" (i.e., orgasm). Paroxysm was regarded as a medical treatment, and not a sexual release.[93] The disorder has ceased to be recognized as a medical condition since the 1920s.
The Vagina Monologues
Today, the vagina is celebrated through modern conventions such as The Vagina Monologues, which is made up of a varying number of monologues read by a number of women. Initially, Eve Ensler performed every monologue herself, with subsequent performances featuring three actresses; latter versions feature a different actress for every role. Each of the monologues deals with an aspect of the feminine experience, touching on matters such as sexual activity, love, rape, menstruation, female genital mutilation (FGM), masturbation, birth, orgasm, the various common names for the vagina, or simply as a physical aspect of the body. A recurring theme throughout the pieces is the vagina as a tool of female empowerment, and the ultimate embodiment of individuality.[87][94]
Reasons for vaginal modification
With the exception of voluntary labiaplasty,[82] modification of the vagina is generally a matter of FGM. Significant controversy surrounds FGM,[81][80] with the World Health Organization (WHO) being one of many health organizations that have campaigned against the procedures on behalf of human rights, stating that "FGM has no health benefits" and that it is "a violation of the human rights of girls and women" and "reflects deep-rooted inequality between the sexes".[81] The practice has existed at one point or another in almost all human civilizations,[95] most commonly to exert control over the sexual behavior, including masturbation, of girls and women.[81][95] Custom and tradition are the most frequently cited reasons for FGM, with some cultures believing that not performing it has the possibility of disrupting the cohesiveness of their social and political systems, such as FGM also being a part of a girl's initiation into adulthood.[81][95] Often, a girl is not considered an adult in a FGM-practicing society unless she has undergone FGM.[81]
Female genital mutilation is carried out in several countries, especially in Africa, and to a lesser extent in other parts of the Middle East and Southeast Asia, on girls from a few days old to mid-adolescent, often to reduce sexual desire in an effort to preserve vaginal virginity.[81][80][95] It may also be that FGM was "practiced in ancient Egypt as a sign of distinction among the aristocracy"; there are reports that traces of infibulation are on Egyptian mummies.[95]
Other animals
The vagina (along with the penis) is a general feature of animals in which the female is internally fertilised (other than by traumatic insemination). The shape of the vagina varies among different animals.
In placental mammals and marsupials, the vagina leads from the uterus to the exterior of the female body. Female marsupials have two lateral vaginas, which lead to separate uteri, but both open externally through the same orifice.[96] The urethra and vagina of the female spotted hyena exits through the clitoris, allowing the females to urinate, copulate and give birth through the clitoris.[97]
In birds, monotremes, and some reptiles, a homologous part of the oviduct leads from the shell gland to the cloaca.[98][99] In some jawless fish, there is neither oviduct nor vagina and instead the egg travels directly through the body cavity (and is fertilised externally as in most fish and amphibians). In insects and other invertebrates, the vagina can be a part of the oviduct (see insect reproductive system).[100]
In 2014, the scientific journal Current Biology reported that four species of Brazilian insects in the genus Neotrogla were found to have sex-reversed genitalia. The male insects of those species have vagina-like openings, while the females have penis-like organs.[101][102][103]
See also
References
- ^ Clinical pediatric urology: A. Barry Belman, Lowell R. King, Stephen Alan Kramer (2002)
- ^ Kinetics, Human (15 May 2009). Health and Wellness for Life. Human Kinetics 10%. p. 221. ISBN 978-0-7360-6850-5. Retrieved 30 July 2013.
- ^ a b c d e f Encyclopedia of Family Health. Marshall Cavendish. 2004. p. 964. ISBN 0761474862. Retrieved 25 April 2014.
{{cite book}}: Unknown parameter|authors=ignored (help) Cite error: The named reference "Jacoby" was defined multiple times with different content (see the help page). - ^ a b c Dianne Hales (2008). An Invitation to Health Brief 2010-2011. Cengage Learning. pp. 269–271. ISBN 0495391921. Retrieved 29 August 2013.
- ^ a b New Dimensions in Women's Health. Jones & Bartlett Publishers. 2011. p. 211. ISBN 1449683754. Retrieved 29 August 2013.
{{cite book}}: Unknown parameter|authors=ignored (help) - ^ a b "Global strategy for the prevention and control of sexually transmitted infections: 2006–2015. Breaking the chain of transmission" (PDF). World Health Organization. 2007. Retrieved 26 November 2011.
- ^ "Princeton University's Wordnet search results for Birth Canal". Princeton. Retrieved 24 May 2010.
- ^ Words meaning vulva ('vagina'), female genitalia Online Slang Dictionary
- ^ Cai Y (2009). "Revisiting old vaginal topics: conversion of the Müllerian vagina and origin of the "sinus" vagina". Int J Dev Biol 2009; 53:925-34. 53 (7): 925–34. doi:10.1387/ijdb.082846yc. PMID 19598112.
- ^ Merz, Eberhard; Bahlmann, F. (2004). Ultrasound in Obstetrics and Gynecology. Vol. 1. Thieme Medical Publishers. p. 129. ISBN 978-1-58890-147-7.
{{cite book}}:|access-date=requires|url=(help) - ^ Schuenke, Michael; Schulte, Erik; Schumacher, Udo (2010). General Anatomy and Musculoskeletal System. Thieme Medical Publishers. p. 192. ISBN 978-1-60406-287-8. Retrieved 9 June 2014.
- ^ a b c Snell, Richard S. (2004). Clinical Anatomy: An Illustrated Review with Questions and Explanations. Lippincott Williams & Wilkins. p. 98. ISBN 978-0-7817-4316-7. Retrieved 19 February 2014.
- ^ a b c d e f g h i j k l m n Hiralal Konar (2014). DC Dutta's Textbook of Gynecology. JP Medical Ltd. pp. 2–7. ISBN 9351520684. Retrieved 9 June 2014.
- ^ a b c Mulhall, John P. (2011). Cancer and Sexual Health. Springer. pp. 13–22. ISBN 1-60761-915-6. Retrieved 21 February 2014.
{{cite book}}: Unknown parameter|editors=ignored (|editor=suggested) (help) - ^ a b c d Wylie, Linda (2005). Essential Anatomy and Physiology in Maternity Care. Elsevier Health Sciences. pp. 157–158. ISBN 0-443-10041-1. Retrieved 19 February 2014.
- ^ a b c Young, B, ed. (2006). Wheater's Functional Histology: A Text and Colour Atlas (5th ed.). Elsevier. p. 377. ISBN 978-0443068508. Cite error: The named reference "Wheater" was defined multiple times with different content (see the help page).
- ^ a b Manual of Obstetrics. (3rd ed.). Elsevier. 2011. pp. 1–16. ISBN 9788131225561.
- ^ Brown, Laurence (2012). Pathology of the Vulva and Vagina. Springer. pp. 6–7. ISBN 0857297570. Retrieved 21 February 2014.
- ^ Oxford Desk Reference: Obstetrics and Gynaecology. Oxford University Press. 2011. p. 471. ISBN 0191620874. Retrieved 21 February 2014.
{{cite book}}: Unknown parameter|authors=ignored (help) - ^ a b Knight, Bernard (1997). Simpson's Forensic Medicine (11th ed.). London: Arnold. p. 114. ISBN 0-7131-4452-1.
- ^ Rogers DJ, Stark M (August 1998). "The hymen is not necessarily torn after sexual intercourse". BMJ. 317 (7155): 414. doi:10.1136/bmj.317.7155.414. PMC 1113684. PMID 9694770.
- ^ Perlman, Sally E. (2004). Clinical protocols in pediatric and adolescent gynecology. Parthenon. p. 131. ISBN 1-84214-199-6.
{{cite book}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ a b Sloane, Ethel (2002). Biology of Women. Cengage Learning. pp. 32, 41–42. ISBN 0-7668-1142-5. Retrieved 19 February 2014.
- ^ Bourcier, A.; McGuire, Edward J.; Abrams, Paul (2004). Pelvic Floor Disorders. Elsevier Health Sciences. p. 20. ISBN 0-7216-9194-3. Retrieved 19 February 2014.
- ^ Wiederman, Michael W.; Whitley, Jr., Bernard E. (1 August 2001). Handbook for Conducting Research on Human Sexuality. Psychology Press. p. 143. ISBN 978-1-135-66340-7. Retrieved 19 February 2014.
- ^ a b c d "Vagina". health.discovery.com. Retrieved 11 February 2012.
- ^ Emans, S. Jean. "Physical Examination of the Child and Adolescent" (2000) in Evaluation of the Sexually Abused Child: A Medical Textbook and Photographic Atlas, Second edition, Oxford University Press. 61-65
- ^ a b c d Weiten, Wayne; Dunn, Dana; Hammer, Elizabeth (1 January 2011). Psychology Applied to Modern Life: Adjustment in the 21st Century. Cengage Learning. p. 386. ISBN 1-111-18663-4. Retrieved 19 February 2014.
- ^ a b c "I'm a woman who cannot feel pleasurable sensations during intercourse". Go Ask Alice!. 8 October 2004 (Last Updated/Reviewed on 17 October 2008). Archived from the original on January 7, 2011. Retrieved September 13, 2012.
{{cite web}}: Check date values in:|date=(help) - ^ a b c d O'Connell HE, Sanjeevan KV, Hutson JM (October 2005). "Anatomy of the clitoris". The Journal of Urology. 174 (4 Pt 1): 1189–95. doi:10.1097/01.ju.0000173639.38898.cd. PMID 16145367.
{{cite journal}}: Unknown parameter|laydate=ignored (help); Unknown parameter|laysource=ignored (help); Unknown parameter|laysummary=ignored (help)CS1 maint: multiple names: authors list (link) - ^ a b c Sex and Society, Volume 2. Marshall Cavendish Corporation. 2009. p. 590. ISBN 9780761479079. Retrieved 17 August 2012.
- ^ a b Clinical Manual of Sexual Disorders. American Psychiatric Pub. 2009. p. 258. ISBN 1585629057. Retrieved 21 February 2014.
{{cite book}}: Unknown parameter|authors=ignored (help) - ^ Rosenthal, Martha (6 January 2012). Human Sexuality: From Cells to Society. Cengage Learning. p. 76. ISBN 0-618-75571-3. Retrieved 19 February 2014.
- ^ a b Carroll, Janell (2012). Discovery Series: Human Sexuality. Cengage Learning. pp. 282–289. ISBN 1111841896. Retrieved 9 June 2014.
- ^ Taormino, Tristan (2009). The Big Book of Sex Toys. Quiver. p. 52. ISBN 978-1-59233-355-4. Retrieved 9 June 2014.
- ^ a b c Kilchevsky A, Vardi Y, Lowenstein L, Gruenwald I. (January 2012). "Is the Female G-Spot Truly a Distinct Anatomic Entity?". The Journal of Sexual Medicine. 2011 (3): 719–26. doi:10.1111/j.1743-6109.2011.02623.x. PMID 22240236.
{{cite journal}}: Unknown parameter|laydate=ignored (help); Unknown parameter|laysource=ignored (help); Unknown parameter|laysummary=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Jannini E, Simonelli C, Lenzi A (2002). "Sexological approach to ejaculatory dysfunction". Int J Androl. 25 (6): 317–23. doi:10.1046/j.1365-2605.2002.00371.x. PMID 12406363.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Jannini E, Simonelli C, Lenzi A (2002). "Disorders of ejaculation". J Endocrinol Invest. 25 (11): 1006–19. doi:10.1007/bf03344077. PMID 12553564.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ a b Hines T (August 2001). "The G-Spot: A modern gynecologic myth". Am J Obstet Gynecol. 185 (2): 359–62. doi:10.1067/mob.2001.115995. PMID 11518892.
- ^ Santos, F Taboga, S. (2003). "Female prostate: a review about biological repercussions of this gland in humans and rodents" (PDF). Animal Reproduction. 3 (1): 3–18. Retrieved 11 March 2012.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ a b c d e Danielsson, D., P. K. Teigen, and H. Moi. 2011. The genital econiche: Focus on microbiota and bacterial vaginosis" Ann. N. Y. Acad. Sci 1230:48-58
- ^ a b c Thoma, M. E., R. H. Gray, N. Kiwanuka, S. Aluma, M.-C. Wang, N. Sewankambo, and M. J. Wawer. 2011. Longitudinal changes in vaginal microbiota composition assessed by Gram stain among never sexually active pre- and postmenarcheal adolescents in Rakai, Uganda. J. Pediatr. Adolesc. Gynecol. 24:42-47.
- ^ a b El Aila, N. A., I. Tency, G. Claeys, H. Verstraelen, B. Saerens, G. Lopes dos Santos Santiago, E. De Backer, P. Cools, M. Temmerman, R. Verhelst, and M. Vaneechoutte. 2009. Identification and genotyping of bacteria from paired vaginal and rectal samples from pregnant women indicates similarity between vaginal and rectal microflora. BMC Infect. Dis.9:167.
- ^ a b El Aila, N. A., I. Tency, B. Saerens, E. De Backer, P. Cools, G. Lopes dos Santos Santiago, H. Verstraelen, R. Verhelst, M. Temmerman, and M. Vaneechoutte. 2011. Strong correspondence in bacterial loads between the vagina and rectum of pregnant women. Res. Microbiol. 162:506-513.
- ^ Antonio, M. A., L. K. Rabe, and S. L. Hillier. 2005. Colonization of the rectum by Lactobacillus species and decreased risk of bacterial vaginosis" J. Infect. Dis 192:394-398.
- ^ a b c d e Linhares, I. M., P. R. Summers, B. Larsen, P. C. Giraldo, and S. S. Witkin. 2011. Contemporary perspectives on vaginal pH and lactobacilli" Am. J. Obstet. Gynecol 204:120.e1-120.e5.
- ^ Gorodeski, G. I., U. Hopfer, C. C. Liu, and E. Margles. 2005. Estrogen acidifies vaginal pH by up-regulation of proton secretion via the apical membrane of vaginal-ectocervical epithelial cells. Endocrinol. 146:816-824.
- ^ Boskey, E. R., R. A. Cone, K. J. Whaley, and T. R. Moench. 2001. Origins of vaginal acidity:High D/L lactate ratio is consistent with bacteria being the primary source" Hum. Reprod 16:1809-1813.
- ^ a b c d Ravel, J., P. Gajer, Z. Abdo, G. M. Schneider, S. S. Koenig, S. L. McCulle, S. Karlebach, R. Gorle, J. Russell, C. O. Tacket, R. M. Brotman, C. C. Davis, K. Ault, L. Peralta, and L. J. Forney. 2011. Vaginal microbiome of reproductive-age women. Proc. Natl. Acad. Sci. U S A.108:4680-4687.
- ^ a b c Hummelen, R., A. D. Fernandes, J. M. Macklaim, R. J. Dickson, J. Changalucha, G. B. Gloor, and G. Reid. 2010. Deep sequencing of the vaginal microbiota of women with HIV. PloS One 5:e12078.
- ^ De Backer, E., R. Verhelst, H. Verstraelen, M. A. Alqumber, J. P. Burton, J. R. Tagg, M. Temmerman, and M. Vaneechoutte. 2007. Quantitative determination by real-time PCR of four vaginal Lactobacillus species, Gardnerella vaginalis and Atopobium vaginae indicates an inverse relationship between L. gasseri and L. iners. BMC Microbiol. 7:115.
- ^ Verhelst, R., H. Verstraelen, G. Claeys, G. Verschraegen, L. Van Simaey, C. De Ganck, E. De Backer, M. Temmerman, and M. Vaneechoutte. 2005. Comparison between Gram stain and culture for the characterization of vaginal microflora: Definition of a distinct grade that resembles grade I microflora and revised categorization of grade I microflora. BMC Microbiol. 5:61.
- ^ a b c Witkin, S. S., I. M. Linhares, and P. Giraldo. 2007. Bacterial flora of the female genital tract:function and immune regulation. Best Pract. Res. Clin. Obstet. Gynaecol. 21:347-354.
- ^ Mestecky, J., and M. W. Russell. 2000. Induction of mucosal immune responses in the human genital tract. FEMS Immunol. Med. Microbiol. 27:351-355.
- ^ Cauci, S., S. Driussi, R. Monte, P. Lanzafame, E. Pitzus, and F. Quadrifoglio. 1998. Immunoglobulin A response against Gardnerella vaginalis hemolysin and sialidase activity in bacterial vaginosis" Am. J. Obstet. Gynecol 178:511-515.
- ^ a b Burton, J. P., and G. Reid. 2002. Evaluation of the bacterial vaginal flora of 20 postmenopausal women by direct (Nugent score) and molecular (polymerase chain reaction and denaturing gradient gel electrophoresis) techniques" J. Infect. Dis 186:1770-1780.
- ^ Hillier, S. L., and R. J. Lau. 1997. Vaginal microflora in postmenopausal women who have not received estrogen replacement therapy" Clin. Infect. Dis 25:S123-S126.
- ^ Cauci, S., S. Driussi, D. De Santo, P. Penacchioni, T. Iannicelli, P. Lanzafame, F. De Seta, F. Quadrifoglio, D. de Aloysio, and S. Guaschino. 2002. Prevalence of bacterial vaginosis and vaginal flora changes in peri- and postmenopausal women" J. Clin. Microbiol 40:2147-2152.
- ^ Ginkel, P. D., D. E. Soper, R. C. Bump, and H. P. Dalton. 1993. Vaginal flora in postmenopausal women: The effect of estrogen replacement. Infect. Dis. Obstet. Gynecol. 1:94-97.
- ^ Cherpes, T. L., S. L. Hillier, L. A. Meyn, J. L. Busch, and M. A. Krohn. 2008. A delicate balance: Risk factors for acquisition of bacterial vaginosis include sexual activity, absence of hydrogen peroxide-producing lactobacilli, black race, and positive herpes simplex virus type 2 serology. Sex. Transm. Dis. 35:78-83.
- ^ Verstraelen, H. 2008. Bacterial vaginosis: A sexually enhanced disease. Int. J. STD AIDS 19:575-576.
- ^ Verstraelen, H., R. Verhelst, M. Vaneechoutte, and M. Temmerman. 2010. The epidemiology of bacterial vaginosis in relation to sexual behaviour. BMC Infect. Dis. 10:81.
- ^ Martin, R., and J. E. Suarez. 2010. Biosynthesis and degradation of H2O2 by vaginal lactobacilli" Appl. Environ. Microbiol 76:400-405.
- ^ McLean, N. W., and I. J. Rosenstein. 2000. Characterisation and selection of a Lactobacillus species to re-colonise the vagina of women with recurrent bacterial vaginosis. J. Med. Microbiol. 49:543-552.
- ^ "Vaginal Problems — Home Treatment". Women's Health. WebMD, LLC. Retrieved 28 August 2009.
- ^ a b c d e f g h "The Vagina (Human Anatomy)". WebMD. Retrieved 27 April 2014.
- ^ See, e.g., Colin Hinrichsen, Peter Lisowski, Anatomy Workbook (2007), p. 101: "Digital examination per vaginam are made by placing one or two fingers in the vagina".
- ^ a b Vaginal pH Test from Point of Care Testing, July 2009, at: University of California, San Francisco – Department of Laboratory Medicine. Prepared by: Patricia Nassos, PhD, MT and Clayton Hooper, RN.
- ^ Todar, Kenneth (2008). "The Nature of Bacterial Host-Parasite Relationships in Humans". Online Textbook of Bacteriology. Retrieved 28 August 2009.
- ^ "Hiv/Aids". MayoClinic.com. 11 August 2010. Retrieved 18 August 2011.
- ^ Hagen S, Stark D (2011). "Conservative prevention and management of pelvic organ prolapse in women". Cochrane Database Syst Rev. 12: CD003882. doi:10.1002/14651858.CD003882.pub4. PMID 22161382.
- ^ Andriole Jr., Gerald L. (2013). Year Book of Urology 2013. Elsevier Health Sciences. pp. 160–161. ISBN 1455773166. Retrieved 3 June 2014.
- ^ Porst, Hartmut; Buvat, Jacques (2008). Standard Practice in Sexual Medicine. John Wiley & Sons. pp. 293–297. ISBN 1405178728. Retrieved 3 June 2014.
- ^ a b Lehmiller, Justin J. (2013). The Psychology of Human Sexuality. John Wiley & Sons. p. 319. ISBN 1118351290. Retrieved 3 June 2014.
- ^ Goldstein, Irwin (1 March 2004). "Persistent Sexual Arousal Syndrome". Boston University Medical Campus Institute for Sexual Medicine. Retrieved 7 February 2013.
{{cite news}}: Cite has empty unknown parameter:|coauthors=(help) - ^ "Bartholin cyst". Mayo Clinic.com. 19 January 2010. Retrieved 18 August 2011.
- ^ Manetta A, Pinto JL, Larson JE, Stevens CW, Pinto JS, Podczaski ES (July 1988). "Primary invasive carcinoma of the vagina". Obstet Gynecol. 72 (1): 77–81. PMID 3380510.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Spence D, Melville C (December 2007). "Vaginal discharge". BMJ. 335 (7630): 1147–51. doi:10.1136/bmj.39378.633287.80. PMC 2099568. PMID 18048541.
- ^ Butcher J (January 1999). "Female sexual problems II: sexual pain and sexual fears". BMJ. 318 (7176): 110–2. doi:10.1136/bmj.318.7176.110. PMC 1114576. PMID 9880287.
- ^ a b c Crooks, Robert; Baur, Karla (2010). Our Sexuality. Cengage Learning. pp. 55–56. ISBN 978-0-495-81294-4. Retrieved 9 June 2014.
- ^ a b c d e f g h "Female genital mutilation". World Health Organization. Retrieved 22 August 2012.
- ^ a b Lloyd, Jillian et al. "Female genital appearance: 'normality' unfolds", British Journal of Obstetrics and Gynaecology, May 2005, 112(5), pp. 643–646. PMID 15842291
- ^ Stone, Linda (2002). New Directions in Anthropological Kinship. Rowman & Littlefield Publishers. p. 164. ISBN 058538424X. Retrieved 9 June 2014.
- ^ Hutcherson, Hilda (2003). What Your Mother Never Told You about Sex. Penguin. p. 8. ISBN 0399528539. Retrieved 9 June 2014.
- ^ LaFont, Suzanne (2003). Constructing Sexualities: Readings in Sexuality, Gender, and Culture. Prentice Hall. p. 145. ISBN 013009661X. Retrieved 9 June 2014.
- ^ Angier, Natalie (1999). Woman: An Intimate Geography. Houghton Mifflin Harcourt. p. 92. ISBN 978-0-395-69130-4. Retrieved 9 June 2014.
- ^ a b Ensler, Eve (2001). The Vagina Monologues: The V-Day Edition. Random House LLC. ISBN 0375506586. Retrieved 9 June 2014.
- ^ Morton, Mark (2004). The Lover's Tongue: A Merry Romp Through the Language of Love and Sex. Toronto, Canada: Insomniac Press. ISBN 978-1-894663-51-9.
- ^ "Definition of CUNT". Dictionary – Merriam-Webster online. Merriam-Webster. Retrieved 9 June 2014.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ "cunt". Merriam-Webster's Learner's Dictionary. Merriam-Webster. Retrieved 13 September 2013.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ For example, Glue by Irvine Welsh, p.266, "Billy can be a funny cunt, a great guy..."
- ^ "pussy, n. and adj.2". Oxford English Dictionary (third ed.). Oxford: Oxford University Press. 2007.
- ^ a b Maines, Rachel P. (1998). The Technology of Orgasm: "Hysteria", the Vibrator, and Women's Sexual Satisfaction. Baltimore: The Johns Hopkins University Press. ISBN 0-8018-6646-4.
- ^ Coleman, Christine (2006). Coming to Read "The Vagina Monologues": A Biomythographical Unravelling of the Narrative. University of New Brunswick . ISBN 0494466553. Retrieved 9 June 2014.
- ^ a b c d e Momoh, Comfort (2005). "Female Genital Mutation". In Momoh, Comfort (ed.). Female Genital Mutilation. Radcliffe Publishing. pp. 5–12. ISBN 978-1-85775-693-7.
{{cite book}}: Invalid|ref=harv(help) - ^ Luckett, W.P. 1977. Ontogeny of amniote fetal membranes and their application to phylogeny. Major patterns in Vertebrate Evolution. New York, London: Plenum Publishing Corporation. p 439-516
- ^ Szykman. M., Van Horn, R. C., Engh, A.L. Boydston, E. E. & Holekamp, K. E. (2007) Courtship and mating in free-living spotted hyenas. Behaviour. 144: 815–846.
- ^ Iannaccone, Philip (1997). Biological Aspects of Disease. CRC Press. pp. 35–36. ISBN 3718606135. Retrieved 9 June 2014.
- ^ Comparative Anatomy: Manual of Vertebrate Dissection. Morton Publishing Company. 2012. pp. 66–68. ISBN 1617310042. Retrieved 9 June 2014.
{{cite book}}: Unknown parameter|authors=ignored (help) - ^ The Insects: Structure and Function. Cambridge University Press. 2013. pp. 314–316. ISBN 052111389X. Retrieved 9 June 2014.
{{cite book}}: Unknown parameter|authors=ignored (help) - ^ http://www.theverge.com/2014/4/17/5617766/scientists-discover-insect-with-female-penis
- ^ Kazunori Yoshizawae (17 April 2014). "Female Penis, Male Vagina, and Their Correlated Evolution in a Cave Insect". Current Biology. Retrieved 27 April 2014.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Cell Press (17 April 2014). "In sex-reversed cave insects, females have the penises". Science Daily. Retrieved 27 April 2014.
