Vitamin B12: Difference between revisions
Tag: references removed |
Rescuing orphaned refs ("BPE" from rev 850904754) |
||
| Line 93: | Line 93: | ||
B<sub>12</sub> is only produced in nature by certain [[bacteria]], and [[archaea]].<ref name="Fang">{{cite journal | vauthors = Fang H, Kang J, Zhang D | title = 12: a review and future perspectives | journal = Microbial Cell Factories | volume = 16 | issue = 1 | pages = 15 | date = January 2017 | pmid = 28137297 | doi = 10.1186/s12934-017-0631-y }}</ref><ref>{{cite journal | vauthors = Moore SJ, Warren MJ | title = The anaerobic biosynthesis of vitamin B12 | journal = Biochemical Society Transactions | volume = 40 | issue = 3 | pages = 581–6 | date = June 2012 | pmid = 22616870 | doi = 10.1042/BST20120066 }}</ref><ref>{{cite book|last1=Graham|first1=Ross M.|last2=Deery|first2=Evelyne|last3=Warren|first3=Martin J.|editor1-last=Warren|editor1-first=Martin J.|editor2-last=Smith|editor2-first=Alison G.|editorlink2=Alison Gail Smith | name-list-format = vanc |title=Tetrapyrroles Birth, Life and Death|date=2009|publisher=Springer-Verlag|location=New York, NY|isbn=978-0-387-78518-9|page=286|chapter=18: Vitamin B<sub>12</sub>: Biosynthesis of the Corrin Ring|doi=10.1007/978-0-387-78518-9_18}}</ref> It is synthesized by some bacteria in the [[gut flora]] in humans and other animals, but humans cannot absorb this as it is made in the [[Large intestine|colon]], downstream from the [[small intestine]], where the absorption of most nutrients occurs.<ref name=Gille2015rev>{{cite journal | vauthors = Gille D, Schmid A | title = Vitamin B12 in meat and dairy products | journal = Nutrition Reviews | volume = 73 | issue = 2 | pages = 106–15 | date = February 2015 | pmid = 26024497 | doi = 10.1093/nutrit/nuu011 }}</ref> Ruminants, such as cows and sheep, absorb B<sub>12</sub> produced by bacteria in their guts.<ref name=Gille2015rev/> For gut bacteria of ruminants to produce B<sub>12</sub> the animal must consume sufficient amounts of [[Cobalt#Biological role|cobalt]].<ref name=McDowell>{{cite book|last1=McDowell|first1=Lee Russell| name-list-format = vanc |title=Vitamins in Animal and Human Nutrition|date=2008|publisher=John Wiley & Sons|location=Hoboken|isbn=9780470376683|pages=525, 539|edition=2nd|url=https://books.google.com/books?id=UR9MnQ806LsC&pg=PA525}}</ref> These grazing animals acquire the bacteria that produce vitamin B<sub>12</sub>, and the vitamin itself. |
B<sub>12</sub> is only produced in nature by certain [[bacteria]], and [[archaea]].<ref name="Fang">{{cite journal | vauthors = Fang H, Kang J, Zhang D | title = 12: a review and future perspectives | journal = Microbial Cell Factories | volume = 16 | issue = 1 | pages = 15 | date = January 2017 | pmid = 28137297 | doi = 10.1186/s12934-017-0631-y }}</ref><ref>{{cite journal | vauthors = Moore SJ, Warren MJ | title = The anaerobic biosynthesis of vitamin B12 | journal = Biochemical Society Transactions | volume = 40 | issue = 3 | pages = 581–6 | date = June 2012 | pmid = 22616870 | doi = 10.1042/BST20120066 }}</ref><ref>{{cite book|last1=Graham|first1=Ross M.|last2=Deery|first2=Evelyne|last3=Warren|first3=Martin J.|editor1-last=Warren|editor1-first=Martin J.|editor2-last=Smith|editor2-first=Alison G.|editorlink2=Alison Gail Smith | name-list-format = vanc |title=Tetrapyrroles Birth, Life and Death|date=2009|publisher=Springer-Verlag|location=New York, NY|isbn=978-0-387-78518-9|page=286|chapter=18: Vitamin B<sub>12</sub>: Biosynthesis of the Corrin Ring|doi=10.1007/978-0-387-78518-9_18}}</ref> It is synthesized by some bacteria in the [[gut flora]] in humans and other animals, but humans cannot absorb this as it is made in the [[Large intestine|colon]], downstream from the [[small intestine]], where the absorption of most nutrients occurs.<ref name=Gille2015rev>{{cite journal | vauthors = Gille D, Schmid A | title = Vitamin B12 in meat and dairy products | journal = Nutrition Reviews | volume = 73 | issue = 2 | pages = 106–15 | date = February 2015 | pmid = 26024497 | doi = 10.1093/nutrit/nuu011 }}</ref> Ruminants, such as cows and sheep, absorb B<sub>12</sub> produced by bacteria in their guts.<ref name=Gille2015rev/> For gut bacteria of ruminants to produce B<sub>12</sub> the animal must consume sufficient amounts of [[Cobalt#Biological role|cobalt]].<ref name=McDowell>{{cite book|last1=McDowell|first1=Lee Russell| name-list-format = vanc |title=Vitamins in Animal and Human Nutrition|date=2008|publisher=John Wiley & Sons|location=Hoboken|isbn=9780470376683|pages=525, 539|edition=2nd|url=https://books.google.com/books?id=UR9MnQ806LsC&pg=PA525}}</ref> These grazing animals acquire the bacteria that produce vitamin B<sub>12</sub>, and the vitamin itself. |
||
[[Feces]] are a rich source of vitamin B<sub>12</sub>, and are eaten by many animals, including dogs and cats.<ref name=BPE/><ref>{{cite web|title=Vitamin B<sub>12</sub>|url=http://www.dsm.com/markets/anh/en_US/Compendium/companion_animals/vitamin_B12.html|publisher=DSM|access-date=January 17, 2017}}</ref> [[Lagomorpha]] species, including [[rabbit]]s and [[hare]]s, form fecal pellets in their [[cecum]] called [[cecotropes]], which consist of chewed plant material that has been metabolized by cecal bacteria; cecotropes contain digestible carbohydrates and B vitamins synthesized by the resident bacteria. These animals ingest cecotropes which have been expelled in their feces. |
[[Feces]] are a rich source of vitamin B<sub>12</sub>, and are eaten by many animals, including dogs and cats.<ref name=BPE>{{cite news|last1=Rooke|first1=Jennifer| name-list-format = vanc |title=Do carnivores need Vitamin B<sub>12</sub> supplements?|url=http://baltimorepostexaminer.com/carnivores-need-vitamin-b12-supplements/2013/10/30|work=Baltimore Post Examiner|date=October 30, 2013}}</ref><ref>{{cite web|title=Vitamin B<sub>12</sub>|url=http://www.dsm.com/markets/anh/en_US/Compendium/companion_animals/vitamin_B12.html|publisher=DSM|access-date=January 17, 2017}}</ref> [[Lagomorpha]] species, including [[rabbit]]s and [[hare]]s, form fecal pellets in their [[cecum]] called [[cecotropes]], which consist of chewed plant material that has been metabolized by cecal bacteria; cecotropes contain digestible carbohydrates and B vitamins synthesized by the resident bacteria. These animals ingest cecotropes which have been expelled in their feces. |
||
=== Animals === |
=== Animals === |
||
Revision as of 10:11, 22 July 2018
 | |
 | |
| Clinical data | |
|---|---|
| Other names | vitamin B12, vitamin B-12 |
| AHFS/Drugs.com | Monograph |
| Routes of administration | by mouth, sublingual, IV, IM, intranasal |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | Readily absorbed in distal half of the ileum |
| Protein binding | Very high to specific transcobalamins plasma proteins Binding of hydroxocobalamin is slightly higher than cyanocobalamin. |
| Metabolism | liver |
| Elimination half-life | Approximately 6 days (400 days in the liver) |
| Excretion | kidney |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| DrugBank | |
| ChemSpider | |
| KEGG | |
| ChEMBL | |
| Chemical and physical data | |
| Formula | C63H88CoN14O14P |
| Molar mass | 1355.37 g/mol g·mol−1 |
| 3D model (JSmol) | |
| |
| |
| | |
Vitamin B12, also called cobalamin, is a water-soluble vitamin that is involved in the metabolism of every cell of the human body: it is a cofactor in DNA synthesis, and in both fatty acid and amino acid metabolism.[1] It is particularly important in the normal functioning of the nervous system via its role in the synthesis of myelin,[2][3] and in the maturation of developing red blood cells in the bone marrow.[4]
Vitamin B12 is one of eight B vitamins; it is the largest and most structurally complicated vitamin. It consists of a class of chemically related compounds (vitamers), all of which show physiological activity. It contains the biochemically rare element cobalt (chemical symbol Co) positioned in the center of a corrin ring. The only organisms to produce vitamin B12 are certain bacteria, and archaea. Some of these bacteria are found in the soil around the grasses that ruminants eat; they are taken into the animal, proliferate, form part of their gut flora, and continue to produce vitamin B12.
Most people in developed countries obtain enough vitamin B12 from consuming animal products including meat, milk, eggs, and fish.[5] Other staple foods are fortified by having the vitamin added to them. Vitamin B12 supplements are available in single agent or multivitamin tablets; and pharmaceutical preparations may be given by intramuscular injection.[6][7]
The most common cause of vitamin B12 deficiency in developed countries is impaired absorption due to a loss of gastric intrinsic factor, which must be bound to food-source B12 in order for absorption to occur. This condition, called pernicious anemia, is more likely after age 60, and increases in incidence with advancing age.[6] Dietary deficiency is very rare in developed countries due to access to dietary meat and fortified foods, but children in some regions of developing countries are at particular risk due to increased requirements during growth coupled with lack of access to dietary B12; adults in these regions are also at risk. Other causes of vitamin B12 deficiency are much less frequent.[8]
Vitamin B12 is produced industrially via bacterial fermentation. Vitamin B12 total synthesis has been achieved, but has no practical value. Vitamin B12 was discovered as a result of its relationship to pernicious anemia.[9]
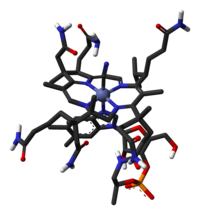
Chemistry

B12 is the most chemically complex of all the vitamins. The structure of B12 is based on a corrin ring, which is similar to the porphyrin ring found in heme. The central metal ion is cobalt. Four of the six coordination sites are provided by the corrin ring, and a fifth by a dimethylbenzimidazole group. The sixth coordination site, the reactive center, is variable, being a cyano group (–CN), a hydroxyl group (–OH), a methyl group (–CH3) or a 5′-deoxyadenosyl group (here the C5′ atom of the deoxyribose forms the covalent bond with cobalt respectively, to yield the four vitamers (forms) of B12. Historically, the covalent C-Co bond is one of the first examples of carbon-metal bonds to be discovered in biology. The hydrogenases and, by necessity, enzymes associated with cobalt utilization, involve metal-carbon bonds.[10]
Vitamin B12 is a generic descriptor name referring to a collection of cobalt and corrin ring molecules which are defined by their particular vitamin function in the body. All of the substrate cobalt-corrin molecules from which B12 is made must be synthesized by bacteria. After this synthesis is complete, the human body has the ability (except in rare cases) to convert any form of B12 to an active form, by means of enzymatically removing certain prosthetic chemical groups from the cobalt atom and replacing them with others.
Vitamers
The four vitamers of B12 are all deeply red colored crystals and water solutions, due to the color of the cobalt-corrin complex.
- Cyanocobalamin is one form of B12 because it can be metabolized in the body to an active coenzyme form. The cyanocobalamin form of B12 does not occur in nature normally, but is a byproduct of the fact that other forms of B12 are avid binders of cyanide (–CN) which they pick up in the process of activated charcoal purification of the vitamin after it is made by bacteria in the commercial process. Since the cyanocobalamin form of B12 is easy to crystallize and is not sensitive to air-oxidation, it is typically used as a form of B12 for food additives and in many common multivitamins. Pure cyanocobalamin possesses the deep pink color associated with most octahedral cobalt(II) complexes and the crystals are well formed and easily grown up to millimeter size.
- Hydroxocobalamin is another vitamer of B12 commonly encountered in pharmacology, but is not normally present in the human body. Hydroxocobalamin is sometimes denoted B12a. This is the form of B12 produced by bacteria, and which is converted to cyanocobalmin in the commercial charcoal filtration step of production. Hydroxocobalamin has an avid affinity for cyanide ions and has been used as an antidote to cyanide poisoning. It is supplied typically in water solution for injection. Hydroxocobalamin is thought to be converted to the active enzymic forms of B12 more easily than cyanocobalamin, and since it is little more expensive than cyanocobalamin, and has longer retention times in the body, has been used for vitamin replacement in situations where added reassurance of activity is desired. Intramuscular administration of hydroxocobalamin is also the preferred treatment for pediatric patients with intrinsic cobalamin metabolic diseases, for vitamin B12 deficient patients with tobacco amblyopia (which is thought to perhaps have a component of cyanide poisoning from cyanide in cigarette smoke); and for treatment of patients with pernicious anemia who have optic neuropathy.
- Adenosylcobalamin (adoB12) and methylcobalamin (MeB12) are the two enzymatically active cofactor forms of B12 that naturally occur in the body. Most of the body's reserves are stored as adoB12 in the liver. These are converted to the other methylcobalamin form as needed.
Dietary recommendations
The U.S. Institute of Medicine (IOM) updated Estimated Average Requirements (EARs) and Recommended Dietary Allowances (RDAs) for vitamin B12 in 1998. The current EAR for vitamin B12 for women and men ages 14 and up is 2.0 μg/day; the RDA is 2.4 μg/day. RDAs are higher than EARs so as to identify amounts that will cover people with higher than average requirements. RDA for pregnancy equals 2.6 μg/day. RDA for lactation equals 2.8 μg/day. For infants up to 12 months the Adequate Intake (AI) is 0.4–0.5 μg/day. (AIs are established when there is insufficient information to determine EARs and RDAs.) For children ages 1–13 years the RDA increases with age from 0.9 to 1.8 μg/day. Because 10 to 30 percent of older people may be unable to effectively absorb vitamin B12 naturally occurring in foods, it is advisable for those older than 50 years to meet their RDA mainly by consuming foods fortified with vitamin B12 or a supplement containing vitamin B12. As for safety, the IOM sets Tolerable Upper Intake Levels (known as ULs) for vitamins and minerals when evidence is sufficient. In the case of vitamin B12 there is no UL, as there is no human data for adverse effects from high doses. Collectively the EARs, RDAs, AIs and ULs are referred to as Dietary Reference Intakes (DRIs).[11]
The European Food Safety Authority (EFSA) refers to the collective set of information as Dietary Reference Values, with Population Reference Intake (PRI) instead of RDA, and Average Requirement instead of EAR. AI and UL defined the same as in United States. For women and men over age 18 the Adequate Intake (AI) is set at 4.0 μg/day. AI for pregnancy is 4.5 μg/day, for lactation 5.0 μg/day. For children aged 1–17 years the AIs increase with age from 1.5 to 3.5 μg/day. These AIs are higher than the U.S. RDAs.[12] The EFSA also reviewed the safety question and reached the same conclusion as in United States - that there was not sufficient evidence to set a UL for vitamin B12.[13]
For U.S. food and dietary supplement labeling purposes the amount in a serving is expressed as a percent of Daily Value (%DV). For vitamin B12 labeling purposes 100% of the Daily Value was 6.0 μg, but as of May 27, 2016 was revised downward to 2.4 μg.[14] A table of the old and new adult Daily Values is provided at Reference Daily Intake. The original deadline to be in compliance was July 28, 2018, but on September 29, 2017 the FDA released a proposed rule that extended the deadline to January 1, 2020 for large companies and January 1, 2021 for small companies.[15]
Sources
Most people in developed countries obtain enough vitamin B12 from consuming animal products including, meat, fish, eggs, and milk.[5]
Bacteria and archaea
B12 is only produced in nature by certain bacteria, and archaea.[16][17][18] It is synthesized by some bacteria in the gut flora in humans and other animals, but humans cannot absorb this as it is made in the colon, downstream from the small intestine, where the absorption of most nutrients occurs.[19] Ruminants, such as cows and sheep, absorb B12 produced by bacteria in their guts.[19] For gut bacteria of ruminants to produce B12 the animal must consume sufficient amounts of cobalt.[20] These grazing animals acquire the bacteria that produce vitamin B12, and the vitamin itself.
Feces are a rich source of vitamin B12, and are eaten by many animals, including dogs and cats.[21][22] Lagomorpha species, including rabbits and hares, form fecal pellets in their cecum called cecotropes, which consist of chewed plant material that has been metabolized by cecal bacteria; cecotropes contain digestible carbohydrates and B vitamins synthesized by the resident bacteria. These animals ingest cecotropes which have been expelled in their feces.
Animals
Animals store vitamin B12 in liver and muscle and some pass the vitamin into their eggs and milk; meat, liver, eggs and milk are therefore sources of the vitamin for other animals as well as humans.[7][8][21] For humans, the bioavailability from eggs is less than 9%, compared to 40% to 60% from fish, fowl and meat.[23] Insects are a source of B12 for animals (including other insects and humans).[21][24]
Food sources with a high concentration of vitamin B12—50 to 99 µg B12 per 100 grams of food[25]—include clams; liver and other organ meats from lamb, veal, beef, and turkey; mackerel; and crab meat.[6][7]
Plants and algae
Natural sources of B12 include dried and fermented plant foods, such as tempeh, and laver, a seaweed.[26][27][28] Many other types of algae are rich in vitamin B12, with some species, such as Porphyra yezoensis,[26] containing as much cobalamin as liver.[29]
Fortified foods
The UK Vegan Society, the Vegetarian Resource Group, and the Physicians Committee for Responsible Medicine, among others, recommend that every vegan who is not consuming adequate B12 from fortified foods take supplements.[30][31][32][33]
Foods for which B12-fortified versions are widely available include breakfast cereals, soy products, energy bars, and nutritional yeast.[25]
Supplements

Vitamin B12 is included in multivitamin pills; and in some countries grain-based foods such as bread and pasta are fortified with B12. In the U.S. non-prescription products can be purchased providing up to 5,000 µg per serving, and it is a common ingredient in energy drinks and energy shots, usually at many times the recommended dietary allowance of B12. The vitamin can also be a prescription product via injection or other means. Tablets have sufficiently large quantities of the vitamin such that 1% to 5% of the free crystalline B12 is absorbed along the entire intestine by passive diffusion.
Sublingual methylcobalamin, which contains no cyanide, is available in 5-mg tablets. The metabolic fate and biological distribution of methylcobalamin are expected to be similar to that of other sources of vitamin B12 in the diet.[34], but the amount of cyanide in cyanocobalamin even in the largest available dose—20 µg of cyanide in a 1,000-µg cyanocobalamin tablet—is less than the daily consumption of cyanide from food, and so cyanocobalamin is not considered a health risk.[34]
Parenteral administration
Injection and patches are sometimes used if digestive absorption is impaired, but this course of action may not be necessary with high-potency oral supplements (such as 0.5–1 mg or more). Even pernicious anemia can be treated entirely by the oral route.[35][36][37]
If the person has inborn errors in the methyltransfer pathway (cobalamin C disease, combined methylmalonic aciduria and homocystinuria), treatment with intravenous, intramuscular hydroxocobalamin or transdermal B12 is needed.[38][39][40][41][42]
Pseudovitamin-B12
Pseudovitamin-B12 refers to B12-like analogues that are biologically inactive in humans and yet found to be present alongside B12 in humans,[43] many food sources (including animals[44]), and possibly supplements and fortified foods.[45] Most cyanobacteria, including Spirulina, and some algae, such as dried Asakusa-nori (Porphyra tenera), have been found to contain mostly pseudovitamin-B12 instead of biologically active B12.[46][47] In one common form of pseudo-B12 available to Salmonella enterica serovar Typhimurium, the α-axial ligand is changed from dimethylbenzimidazole to adenine.[48]
Biochemistry
Coenzyme function
Vitamin B12 functions as a coenzyme, meaning that its presence is required for enzyme-catalyzed reactions.[49][50] Three types of enzymes:
- Isomerases
- Rearrangements in which a hydrogen atom is directly transferred between two adjacent atoms with concomitant exchange of the second substituent, X, which may be a carbon atom with substituents, an oxygen atom of an alcohol, or an amine. These use the adoB12 (adenosylcobalamin) form of the vitamin.
- Methyltransferases
- Methyl (–CH3) group transfers between two molecules. These use MeB12 (methylcobalamin) form of the vitamin.
- Dehalogenases
- Reactions in which a halogen atom is removed from an organic molecule. Enzymes in this class have not been identified in humans.
In humans, two major coenzyme B12-dependent enzyme families corresponding to the first two reaction types, are known. These are typified by the following two enzymes:
- MUT is an isomerase which uses the AdoB12 form and reaction type 1 to catalyze a carbon skeleton rearrangement (the X group is -COSCoA). MUT's reaction converts MMl-CoA to Su-CoA, an important step in the extraction of energy from proteins and fats. This functionality is lost in vitamin B12 deficiency, and can be measured clinically as an increased methylmalonic acid (MMA) level. Unfortunately, an elevated MMA, though sensitive to B12 deficiency, is probably overly sensitive, and not all who have it actually have B12 deficiency. For example, MMA is elevated in 90–98% of patients with B12 deficiency; 20–25% of patients over the age of 70 have elevated levels of MMA, yet 25–33% of them do not have B12 deficiency. For this reason, assessment of MMA levels is not routinely recommended in the elderly. There is no "gold standard" test for B12 deficiency because as a B12 deficiency occurs, serum values may be maintained while tissue B12 stores become depleted. Therefore, serum B12 values above the cut-off point of deficiency do not necessarily indicate adequate B12 status. The MUT function is necessary for proper myelin synthesis and is not affected by folate supplementation.
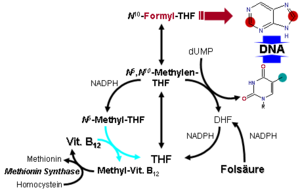
- MTR, also known as methionine synthase, is a methyltransferase enzyme, which uses the MeB12 and reaction type 2 to transfer a methyl group from 5-methyltetrahydrofolate to homocysteine, thereby generating tetrahydrofolate (THF) and methionine.[51] This functionality is lost in vitamin B12 deficiency, resulting in an increased homocysteine level and the trapping of folate as 5-methyl-tetrahydrofolate, from which THF (the active form of folate) cannot be recovered. THF plays an important role in DNA synthesis so reduced availability of THF results in ineffective production of cells with rapid turnover, in particular red blood cells, and also intestinal wall cells which are responsible for absorption. THF may be regenerated via MTR or may be obtained from fresh folate in the diet. Thus all of the DNA synthetic effects of B12 deficiency, including the megaloblastic anemia of pernicious anemia, resolve if sufficient dietary folate is present. Thus the best-known "function" of B12 (that which is involved with DNA synthesis, cell-division, and anemia) is actually a facultative function which is mediated by B12-conservation of an active form of folate which is needed for efficient DNA production.[52] Other cobalamin-requiring methyltransferase enzymes are also known in bacteria, such as Me-H4-MPT, coenzyme M methyltransferase.
Enzyme function
If folate is present in quantity, then of the two absolutely vitamin B12-dependent enzyme-family reactions in humans, the MUT-family reactions show the most direct and characteristic secondary effects, focusing on the nervous system (see below). This is because the MTR (methyltransferase-type) reactions are involved in regenerating folate, and thus are less evident when folate is in good supply.
Since the late 1990s, folic acid has begun to be added to fortify flour in many countries, so folate deficiency is now more rare. At the same time, since DNA synthetic-sensitive tests for anemia and erythrocyte size are routinely done in even simple medical test clinics (so that these folate-mediated biochemical effects are more often directly detected), the MTR-dependent effects of B12 deficiency are becoming apparent not as anemia due to DNA-synthetic problems (as they were classically), but now mainly as a simple and less obvious elevation of homocysteine in the blood and urine (homocysteinuria). This condition may result in long-term damage to arteries and in clotting (stroke and heart attack), but this effect is difficult to separate from other common processes associated with atherosclerosis and aging.
The specific myelin damage resulting from B12 deficiency, even in the presence of adequate folate and methionine, is more specifically and clearly a vitamin deficiency problem. It has been connected to B12 most directly by reactions related to MUT, which is absolutely required to convert methylmalonyl coenzyme A into succinyl coenzyme A. Failure of this second reaction to occur results in elevated levels of MMA, a myelin destabilizer. Excessive MMA will prevent normal fatty acid synthesis, or it will be incorporated into fatty acids itself rather than normal malonic acid. If this abnormal fatty acid subsequently is incorporated into myelin, the resulting myelin will be too fragile, and demyelination will occur. Although the precise mechanism or mechanisms are not known with certainty, the result is subacute combined degeneration of spinal cord.[53] Whatever the cause, it is known that B12 deficiency causes neuropathies, even if folic acid is present in good supply, and therefore anemia is not present.
Vitamin B12-dependent MTR reactions may also have neurological effects, through an indirect mechanism. Adequate methionine (which, like folate, must otherwise be obtained in the diet, if it is not regenerated from homocysteine by a B12 dependent reaction) is needed to make S-adenosyl methionine (SAMe), which is in turn necessary for methylation of myelin sheath phospholipids. Although production of SAMe is not B12 dependent, help in recycling for provision of one adequate substrate for it (the essential amino acid methionine) is assisted by B12. In addition, SAMe is involved in the manufacture of certain neurotransmitters, catecholamines and in brain metabolism. These neurotransmitters are important for maintaining mood, possibly explaining why depression is associated with B12 deficiency. Methylation of the myelin sheath phospholipids may also depend on adequate folate, which in turn is dependent on MTR recycling, unless ingested in relatively high amounts.
Physiology
Absorption
Methyl-B12 is absorbed by two processes. The first is an intestinal mechanism using intrinsic factor through which 1–2 micrograms can be absorbed every few hours. The second is a diffusion process by which approximately 1% of the remainder is absorbed.[54] The human physiology of vitamin B12 is complex, and therefore is prone to mishaps leading to vitamin B12 deficiency. Protein-bound vitamin B12 must be released from the proteins by the action of digestive proteases in both the stomach and small intestine.[55] Gastric acid releases the vitamin from food particles; therefore antacid and acid-blocking medications (especially proton-pump inhibitors) may inhibit absorption of B12.
B12 taken in a low-solubility, non-chewable supplement pill form may bypass the mouth and stomach and not mix with gastric acids, but acids are not necessary for the absorption of free B12 not bound to protein; acid is necessary only to recover naturally-occurring vitamin B12 from foods.
R-protein (also known as haptocorrin and cobalophilin) is a B12 binding protein that is produced in the salivary glands. It must wait to bind food-B12 until B12 has been freed from proteins in food by pepsin in the stomach. B12 then binds to the R-protein to avoid degradation of it in the acidic environment of the stomach.[56]
This pattern of B12 transfer to a special binding protein secreted in a previous digestive step, is repeated once more before absorption. The next binding protein for B12 is intrinsic factor (IF), a protein synthesized by gastric parietal cells that is secreted in response to histamine, gastrin and pentagastrin, as well as the presence of food. In the duodenum, proteases digest R-proteins and release their bound B12, which then binds to IF, to form a complex (IF/B12). B12 must be attached to IF for it to be efficiently absorbed, as receptors on the enterocytes in the terminal ileum of the small bowel only recognize the B12-IF complex; in addition, intrinsic factor protects the vitamin from catabolism by intestinal bacteria.
Absorption of food vitamin B12 thus requires an intact and functioning stomach, exocrine pancreas, intrinsic factor, and small bowel. Problems with any one of these organs makes a vitamin B12 deficiency possible. Individuals who lack intrinsic factor have a decreased ability to absorb B12. In pernicious anemia, there is a lack of IF due to autoimmune atrophic gastritis, in which antibodies form against parietal cells. Antibodies may alternately form against and bind to IF, inhibiting it from carrying out its B12 protective function. Due to the complexity of B12 absorption, geriatric patients, many of whom are hypoacidic due to reduced parietal cell function, have an increased risk of B12 deficiency.[57] This results in 80–100% excretion of oral doses in the feces versus 30–60% excretion in feces as seen in individuals with adequate IF.[57]
Once the IF/B12 complex is recognized by specialized ileal receptors, it is transported into the portal circulation. The vitamin is then transferred to transcobalamin II (TC-II/B12), which serves as the plasma transporter. Hereditary defects in production of the transcobalamins and their receptors may produce functional deficiencies in B12 and infantile megaloblastic anemia, and abnormal B12 related biochemistry, even in some cases with normal blood B12 levels. For the vitamin to serve inside cells, the TC-II/B12 complex must bind to a cell receptor, and be endocytosed. The transcobalamin-II is degraded within a lysosome, and free B12 is finally released into the cytoplasm, where it may be transformed into the proper coenzyme, by certain cellular enzymes (see above).
Investigations into the intestinal absorption of B12 point out that the upper limit of absorption per single oral dose, under normal conditions, is about 1.5 µg: "Studies in normal persons indicated that about 1.5 µg is assimilated when a single dose varying from 5 to 50 µg is administered by mouth. In a similar study Swendseid et al. stated that the average maximum absorption was 1.6 µg [...]"[58] The bulk diffusion process of B12 absorption noted in the first paragraph above, may overwhelm the complex R-factor and IGF-factor dependent absorption, when oral doses of B12 are very large (a thousand or more µg per dose) as commonly happens in dedicated-pill oral B12 supplementation. It is this last fact which allows pernicious anemia and certain other defects in B12 absorption to be treated with oral megadoses of B12, even without any correction of the underlying absorption defects.[59] See the section on supplements above.
Storage and excretion
The total amount of vitamin B12 stored in body is about 2–5 mg in adults. Around 50% of this is stored in the liver. Approximately 0.1% of this is lost per day by secretions into the gut, as not all these secretions are reabsorbed. Bile is the main form of B12 excretion; most of the B12 secreted in the bile is recycled via enterohepatic circulation. Excess B12 beyond the blood's binding capacity is typically excreted in urine. Owing to the extremely efficient enterohepatic circulation of B12, the liver can store 3 to 5 years’ worth of vitamin B12;[60] therefore, nutritional deficiency of this vitamin is rare. How fast B12 levels change depends on the balance between how much B12 is obtained from the diet, how much is secreted and how much is absorbed. B12 deficiency may arise in a year if initial stores are low and genetic factors unfavourable, or may not appear for decades. In infants, B12 deficiency can appear much more quickly.[61]
Deficiency
Vitamin B12 deficiency can potentially cause severe and irreversible damage, especially to the brain and nervous system.[62] At levels only slightly lower than normal, a range of symptoms such as fatigue, lethargy, depression, poor memory, breathlessness, headaches, and pale skin, among others, may be experienced, especially in elderly people (over age 60)[6][63] who produce less stomach acid as they age, thereby increasing their probability of B12 deficiencies.[8] Vitamin B12 deficiency can also cause symptoms of mania and psychosis.[64]
Vitamin B12 deficiency is most commonly caused by low intakes, but can also result from malabsorption, certain intestinal disorders, low presence of binding proteins, and use of certain medications. Vitamin B12 is rare from plant sources, so vegetarians are more likely to suffer from vitamin B12 deficiency. Infants are at a higher risk of vitamin B12 deficiency if they were born to vegetarian mothers. The elderly who have diets with limited meat or animal products are vulnerable populations as well. Vitamin B12 deficiency may occur in between 40% to 80% of the vegetarian population who are not also consuming a vitamin B12 supplement.[65] In Hong Kong and India, vitamin B12 deficiency has been found in roughly 80% of the vegan population as well. Vegans can avoid this by eating B12 fortified foods like cereals, plant-based milks, and nutritional yeast as a regular part of their diet. [66] Despite worries concerning those following a vegetarian or vegan diet, there have also been studies which found that approximately 39 percent of the general population may have possible B12 deficiencies or difficulty with the absorption of this nutrient. Taking a B12 supplement could be beneficial to most people.[67]
B12 is a co-substrate of various cell reactions involved in methylation synthesis of nucleic acid and neurotransmitters. Synthesis of the trimonoamine neurotransmitters can enhance the effects of a traditional antidepressant.[68] The intracellular concentrations of vitamin B12 can be inferred through the total plasma concentration of homocysteine, which can be converted to methionine through an enzymatic reaction that uses 5-methyltetrahydrofolate as the methyl donor group. Consequently, the plasma concentration of homocysteine falls as the intracellular concentration of vitamin B12 rises. The active metabolite of vitamin B12 is required for the methylation of homocysteine in the production of methionine, which is involved in a number of biochemical processes including the monoamine neurotransmitters metabolism. Thus, a deficiency in vitamin B12 may impact the production and function of those neurotransmitters.[69]
Medical uses

Repletion of deficiency
Severe vitamin B12 deficiency is corrected with frequent intramuscular injections of large doses of the vitamin, followed by maintenance doses at longer intervals. Tablets are sometimes used for repletion in mild deficiency; and for maintenance regardless of severity.
Cyanide poisoning
For cyanide poisoning, a large amount of hydroxocobalamin may be given intravenously and sometimes in combination with sodium thiosulfate.[70] The mechanism of action is straightforward: the hydroxycobalamin hydroxide ligand is displaced by the toxic cyanide ion, and the resulting harmless B12 complex is excreted in urine. In the United States, the Food and Drug Administration approved the use of hydroxocobalamin for acute treatment of cyanide poisoning.[71]
Drug interactions
H2-receptor antagonists and proton-pump inhibitors
Gastric acid is needed to release vitamin B12 from protein for absorption. Reduced secretion of gastric acid and pepsin produced by H2 blocker or proton-pump inhibitor (PPI) drugs can reduce absorption of protein-bound (dietary) vitamin B12, although not of supplemental vitamin B12. H2-receptor antagonist examples include cimetidine, famotidine, nizatidine, and ranitidine. PPIs examples include omeprazole, lansoprazole, rabeprazole, pantoprazole, and esomeprazole. Clinically significant vitamin B12 deficiency and megaloblastic anemia are unlikely, unless these drug therapies are prolonged for two or more years, or if in addition the person's diet is below recommended intakes. Symptomatic vitamin deficiency is more likely if the person is rendered achlorhydric (complete absence of gastric acid secretion), which occurs more frequently with proton pump inhibitors than H2 blockers.[72]
Metformin
Reduced serum levels of vitamin B12 occur in up to 30% of people taking long-term anti-diabetic metformin.[73][74][75] Deficiency does not develop if dietary intake of vitamin B12 is adequate or prophylactic B12 supplementation is given. If the deficiency is detected, metformin can be continued while the deficiency is corrected with B12 supplements.[76]
Industrial production
Industrial production of B12 is achieved through fermentation of selected microorganisms.[77] Streptomyces griseus, a bacterium once thought to be a yeast, was the commercial source of vitamin B12 for many years.[78][79] The species Pseudomonas denitrificans and Propionibacterium freudenreichii subsp. shermanii are more commonly used today.[80] These are frequently grown under special conditions to enhance yield, and at least one company uses genetically engineered versions of one or both of these species.[citation needed] Since a number of species of Propionibacterium produce no exotoxins or endotoxins and are generally recognized as safe (have been granted GRAS status) by the Food and Drug Administration of the United States, they are presently the FDA-preferred bacterial fermentation organisms for vitamin B12 production.[81]
The total world production of vitamin B12, by four companies (the French Sanofi-Aventis and three Chinese companies) in 2008 was 35 tonnes.[82]
Laboratory synthesis
No eukaryotic organisms (including plants, animals, and fungi) are independently capable of constructing vitamin B12.[83] Only bacteria and archaea[84] have the enzymes required for its biosynthesis. Like all tetrapyrroles, it is derived from uroporphyrinogen III. This porphyrinogen is methylated at two pyrrole rings to give dihydrosirohydrochlorin, which is oxidized to sirohydrochlorin, which undergoes further reactions, notably a ring contraction, to give the corrin ring.
The complete laboratory synthesis of B12 was achieved by Robert Burns Woodward[85] and Albert Eschenmoser in 1972,[86][87] and remains one of the classic feats of organic synthesis, requiring the effort of 91 postdoctoral fellows (mostly at Harvard) and 12 PhD students (at ETH) from 19 nations. The synthesis constitutes a formal total synthesis, since the research groups only prepared the known intermediate cobyric acid, whose chemical conversion to vitamin B12 was previously reported. Though it constitutes an intellectual achievement of the highest caliber, the Eschenmoser–Woodward synthesis of vitamin B12 is of no practical consequence due to its length, taking 72 chemical steps and giving an overall chemical yield well under 0.01%.[88] And although there have been sporadic synthetic efforts since 1972,[89] the Eschenmoser–Woodward synthesis remains the only completed (formal) total synthesis. Bacterial (or, perhaps archaeal) fermentation remains the only industrially viable source of the vitamin for food production and medicine.
Species from the following genera and species are known to synthesize B12: Propionibacterium shermanii, Pseudomonas denitrificans, Streptomyces griseus,[90] Acetobacterium, Aerobacter, Agrobacterium, Alcaligenes, Azotobacter, Bacillus, Clostridium, Corynebacterium, Flavobacterium, Lactobacillus, Micromonospora, Mycobacterium, Nocardia, Protaminobacter, Proteus, Rhizobium, Salmonella, Serratia, Streptococcus and Xanthomonas [91] [92].
History
- 1849 - Thomas Addison first described a case of pernicious anemia.[4] Chapter 36: Megaloblastic anemias: disorders of impaired DNA synthesis by Ralph Carmel, page 927</ref>
- 1877 - William Osler and William Gardner first described a case of neuropathy in this condition.[4]
- 1878 - Hayem first described large red cells in the peripheral blood in this condition, which he called "giant blood corpuscles", now called macrocytes.[4]
- 1880 - Paul Ehrlich first identified megaloblasts in the bone marrow in this condition.[4]
- 1887 - Ludwig Lichtheim first described a case of myopathy in this condition.[4]
- 1920 -George Whipple discovered that ingesting large amounts of liver seemed to most rapidly cure the anemia of blood loss in dogs, and hypothesized that eating liver might treat pernicious anemia.[citation needed]
- 1926 - George Minot shared the 1934 Nobel Prize with William Murphy and George Whipple, for discovery of an effective treatment for pernicious anemia using liver concentrate, later found to contain a large amount of vitamin B12.[4]
- 1928 -Edwin Cohn prepared a liver extract that was 50 to 100 times more potent in treating pernicious anema than the natural liver products. Whipple, Minot, and Murphy shared the 1934 Nobel Prize in Physiology or Medicine.[93]
- 1929 - William Castle demonstrated that gastric juice contained an "intrinsic factor" which when combined with meat ingestion resulted in absorption of the vitamin in this condition.[4]
- 1947 - Mary Shaw Shorb, in a collaborative project with Karl Folkers, was provided with a US$400 grant to develop the so-called "LLD assay" for B12. LLD stood for Lactobacillus lactis Dorner,[94] a strain of bacterium which required "LLD factor" for growth, which was eventually identified as B12.
- 1948 - Shorb and colleagues Karl A. Folkers and Alexander R. Todd used the LLD assay to rapidly extract the anti-pernicious anemia factor from liver extracts, and pure B12 was isolated.[95]
- 1949 - Shorb and Folkers received the Mead Johnson Award from the American Society of Nutritional Sciences for their discovery.[95]
- 1956 - The chemical structure of the molecule was determined by Dorothy Hodgkin, based on crystallographic data.[96] She was awarded the 1964 Nobel Prize in Chemistry for determining the structure of vitamin B12 and other complex molecules.
- 1959 - methods of producing the vitamin in large quantities from bacteria cultures were developed.
- 1981 - Observations of stereospecificity encountered by R. B. Woodward during the synthesis of vitamin B12 led to the formulation of the principle of the conservation of orbital symmetry, which would result in a Nobel Prize in Chemistry by R. Hoffmann and K. Fukui.
Six Nobel Prizes have been awarded in direct and indirect efforts to study vitamin B12.[97]
References
- ^ Yamada, Kazuhiro (2013). "Chapter 9. Cobalt: Its Role in Health and Disease". In Sigel, Astrid; Sigel, Helmut; Sigel, Roland K. O. (eds.). Interrelations between Essential Metal Ions and Human Diseases. Metal Ions in Life Sciences. Vol. 13. Springer. pp. 295–320. doi:10.1007/978-94-007-7500-8_9.
{{cite book}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ Miller A, Korem M, Almog R, Galboiz Y (June 2005). "Vitamin B12, demyelination, remyelination and repair in multiple sclerosis". Journal of the Neurological Sciences. 233 (1–2): 93–7. doi:10.1016/j.jns.2005.03.009. PMID 15896807.
- ^ "Vitamin B12". April 22, 2014.
- ^ a b c d e f g h Greer, John P. (2014). Wintrobe's Clinical Hematology Thirteenth Edition. Philadelphia, PA: Wolters Kluwer/Lippincott Williams & Wilkins. ISBN 978-1-4511-7268-3.
{{cite book}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) Chapter 36: Megaloblastic anemias: disorders of impaired DNA synthesis by Ralph Carmel - ^ a b "Office of Dietary Supplements - Vitamin B12".
- ^ a b c d "Vitamin B12". Micronutrient Information Center, Linus Pauling Institute, Oregon State University. 2014. Retrieved February 16, 2017.
- ^ a b c "Foods highest in Vitamin B12 (based on levels per 100-gram serving)". Nutrition Data. Condé Nast, USDA National Nutrient Database, release SR-21. 2014. Retrieved February 16, 2017.
- ^ a b c "Dietary Supplement Fact Sheet: Vitamin B12". Office of Dietary Supplements, National Institutes of Health. Retrieved September 28, 2011.
- ^ Scott JM, Molloy AM (November 2012). "The discovery of vitamin B(12)". Annals of Nutrition & Metabolism. 61 (3): 239–45. doi:10.1159/000343114. PMID 23183296.
- ^ Jaouen G, ed. (2006). Bioorganometallics: Biomolecules, Labeling, Medicine. Weinheim: Wiley-VCH. ISBN 3-527-30990-X.[page needed]
- ^ Institute of Medicine (1998). "Vitamin B12". Dietary Reference Intakes for Thiamin, Riboflavin, Niacin, Vitamin B6, Folate, Vitamin B12, Pantothenic Acid, Biotin, and Choline. Washington, DC: The National Academies Press. pp. 340–342. ISBN 0-309-06554-2. Retrieved February 7, 2012.
- ^ "Overview on Dietary Reference Values for the EU population as derived by the EFSA Panel on Dietetic Products, Nutrition and Allergies" (PDF). 2017.
- ^ "Tolerable Upper Intake Levels For Vitamins And Minerals" (PDF). European Food Safety Authority. 2006.
- ^ "Food Labeling: Revision of the Nutrition and Supplement Facts Labels" (PDF). Federal Register. May 27, 2016. p. 33982.
- ^ "Changes to the Nutrition Facts Panel - Compliance Date"
- ^ Fang H, Kang J, Zhang D (January 2017). "12: a review and future perspectives". Microbial Cell Factories. 16 (1): 15. doi:10.1186/s12934-017-0631-y. PMID 28137297.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Moore SJ, Warren MJ (June 2012). "The anaerobic biosynthesis of vitamin B12". Biochemical Society Transactions. 40 (3): 581–6. doi:10.1042/BST20120066. PMID 22616870.
- ^ Graham, Ross M.; Deery, Evelyne; Warren, Martin J. (2009). "18: Vitamin B12: Biosynthesis of the Corrin Ring". In Warren, Martin J.; Smith, Alison G. (eds.). Tetrapyrroles Birth, Life and Death. New York, NY: Springer-Verlag. p. 286. doi:10.1007/978-0-387-78518-9_18. ISBN 978-0-387-78518-9.
{{cite book}}: Unknown parameter|editorlink2=ignored (|editor-link2=suggested) (help); Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ a b Gille D, Schmid A (February 2015). "Vitamin B12 in meat and dairy products". Nutrition Reviews. 73 (2): 106–15. doi:10.1093/nutrit/nuu011. PMID 26024497.
- ^ McDowell, Lee Russell (2008). Vitamins in Animal and Human Nutrition (2nd ed.). Hoboken: John Wiley & Sons. pp. 525, 539. ISBN 9780470376683.
{{cite book}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ a b c Rooke, Jennifer (October 30, 2013). "Do carnivores need Vitamin B12 supplements?". Baltimore Post Examiner.
{{cite news}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ "Vitamin B12". DSM. Retrieved January 17, 2017.
- ^ Watanabe F (November 2007). "Vitamin B12 sources and bioavailability". Experimental Biology and Medicine. 232 (10): 1266–74. doi:10.3181/0703-MR-67. PMID 17959839.
- ^ Dossey, Aaron T. (February 1, 2013). "Why Insects Should Be in Your Diet". The Scientist.
{{cite news}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ a b "Vitamin B12 content, all foods ordered by content in µg per 100 g". United States Department of Agriculture, Agricultural Research Service, National Nutrient Database for Standard Reference, Release 28. May 2016. Retrieved April 6, 2017.
- ^ a b Watanabe F, Yabuta Y, Bito T, Teng F (May 2014). "Vitamin B₁₂-containing plant food sources for vegetarians". Nutrients. 6 (5): 1861–73. doi:10.3390/nu6051861. PMC 4042564. PMID 24803097.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Kwak CS, Lee MS, Lee HJ, Whang JY, Park SC (June 2010). "Dietary source of vitamin B(12) intake and vitamin B(12) status in female elderly Koreans aged 85 and older living in rural area". Nutrition Research and Practice. 4 (3): 229–34. doi:10.4162/nrp.2010.4.3.229. PMC 2895704. PMID 20607069.
- ^ Kwak CS, Lee MS, Oh SI, Park SC (2010). "Discovery of novel sources of vitamin b(12) in traditional korean foods from nutritional surveys of centenarians". Current Gerontology and Geriatrics Research. 2010: 374897. doi:10.1155/2010/374897. PMC 3062981. PMID 21436999.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Croft MT, Lawrence AD, Raux-Deery E, Warren MJ, Smith AG (November 2005). "Algae acquire vitamin B12 through a symbiotic relationship with bacteria". Nature. 438 (7064): 90–3. doi:10.1038/nature04056. PMID 16267554.
- ^ Watanabe F (November 2007). "Vitamin B12 sources and bioavailability". Experimental Biology and Medicine. 232 (10): 1266–74. doi:10.3181/0703-MR-67. PMID 17959839.
- ^ Walsh, Stephen. "Vegan Society B12 factsheet". Vegan Society. Archived from the original on May 26, 2008. Retrieved January 17, 2008.
{{cite web}}: Unknown parameter|dead-url=ignored (|url-status=suggested) (help); Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ Mangels, Reed. "Vitamin B12 in the Vegan Diet". Vegetarian Resource Group. Retrieved January 17, 2008.
{{cite web}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ "Don't Vegetarians Have Trouble Getting Enough Vitamin B12?". Physicians Committee for Responsible Medicine. Retrieved January 17, 2008.
- ^ a b European Food Safety Authority (September 25, 2008). "5′-deoxyadenosylcobalamin and methylcobalamin as sources for Vitamin B12 added as a nutritional substance in food supplements: Scientific opinion of the Scientific Panel on Food Additives and Nutrient Sources added to food". EFSA Journal. 815 (10): 1–21. doi:10.2903/j.efsa.2008.815. "the metabolic fate and biological distribution of methylcobalamin and 5′-deoxyadenosylcobalamin are expected to be similar to that of other sources of vitamin B12 in the diet."
- ^ Bolaman Z, Kadikoylu G, Yukselen V, Yavasoglu I, Barutca S, Senturk T (December 2003). "Oral versus intramuscular cobalamin treatment in megaloblastic anemia: a single-center, prospective, randomized, open-label study". Clinical Therapeutics. 25 (12): 3124–34. doi:10.1016/S0149-2918(03)90096-8. PMID 14749150.
- ^ Lane LA, Rojas-Fernandez C (2002). "Treatment of vitamin b(12)-deficiency anemia: oral versus parenteral therapy". The Annals of Pharmacotherapy. 36 (7–8): 1268–72. doi:10.1345/aph.1A122. PMID 12086562.
- ^ Butler CC, Vidal-Alaball J, Cannings-John R, McCaddon A, Hood K, Papaioannou A, Mcdowell I, Goringe A (June 2006). "Oral vitamin B12 versus intramuscular vitamin B12 for vitamin B12 deficiency: a systematic review of randomized controlled trials". Family Practice. 23 (3): 279–85. doi:10.1093/fampra/cml008. PMID 16585128.
- ^ Andersson HC, Shapira E (January 1998). "Biochemical and clinical response to hydroxocobalamin versus cyanocobalamin treatment in patients with methylmalonic acidemia and homocystinuria (cblC)". The Journal of Pediatrics. 132 (1): 121–4. doi:10.1016/S0022-3476(98)70496-2. PMID 9470012.
- ^ Roze E, Gervais D, Demeret S, Ogier de Baulny H, Zittoun J, Benoist JF, Said G, Pierrot-Deseilligny C, Bolgert F (October 2003). "Neuropsychiatric disturbances in presumed late-onset cobalamin C disease". Archives of Neurology. 60 (10): 1457–62. doi:10.1001/archneur.60.10.1457. PMID 14568819.
- ^ Thauvin-Robinet C, Roze E, Couvreur G, Horellou MH, Sedel F, Grabli D, Bruneteau G, Tonneti C, Masurel-Paulet A, Perennou D, Moreau T, Giroud M, de Baulny HO, Giraudier S, Faivre L (June 2008). "The adolescent and adult form of cobalamin C disease: clinical and molecular spectrum". Journal of Neurology, Neurosurgery, and Psychiatry. 79 (6): 725–8. doi:10.1136/jnnp.2007.133025. PMID 18245139.
- ^ Heil SG, Hogeveen M, Kluijtmans LA, van Dijken PJ, van de Berg GB, Blom HJ, Morava E (October 2007). "Marfanoid features in a child with combined methylmalonic aciduria and homocystinuria (CblC type)". Journal of Inherited Metabolic Disease. 30 (5): 811. doi:10.1007/s10545-007-0546-6. PMID 17768669.
- ^ Tsai AC, Morel CF, Scharer G, Yang M, Lerner-Ellis JP, Rosenblatt DS, Thomas JA (October 2007). "Late-onset combined homocystinuria and methylmalonic aciduria (cblC) and neuropsychiatric disturbance". American Journal of Medical Genetics. Part A. 143A (20): 2430–4. doi:10.1002/ajmg.a.31932. PMID 17853453.
- ^ Albert MJ, Mathan VI, Baker SJ (February 1980). "Vitamin B12 synthesis by human small intestinal bacteria". Nature. 283 (5749): 781–2. doi:10.1038/283781a0. PMID 7354869.
- ^ Kelly RJ, Gruner TM, Furlong JM, Sykes AR (August 2006). "Analysis of corrinoids in ovine tissues". Biomedical Chromatography. 20 (8): 806–14. doi:10.1002/bmc.604. PMID 16345011.
- ^ Yamada K, Shimodaira M, Chida S, Yamada N, Matsushima N, Fukuda M, Yamada S (2008). "Degradation of vitamin B12 in dietary supplements". International Journal for Vitamin and Nutrition Research. Internationale Zeitschrift Fur Vitamin- Und Ernahrungsforschung. Journal International De Vitaminologie et De Nutrition. 78 (4–5): 195–203. doi:10.1024/0300-9831.78.45.195. PMID 19326342.
- ^ Watanabe F, Katsura H, Takenaka S, Fujita T, Abe K, Tamura Y, Nakatsuka T, Nakano Y (November 1999). "Pseudovitamin B(12) is the predominant cobamide of an algal health food, spirulina tablets". Journal of Agricultural and Food Chemistry. 47 (11): 4736–41. doi:10.1021/jf990541b. PMID 10552882.
- ^ Yamada K, Yamada Y, Fukuda M, Yamada S (November 1999). "Bioavailability of dried asakusanori (porphyra tenera) as a source of Cobalamin (Vitamin B12)". International Journal for Vitamin and Nutrition Research. Internationale Zeitschrift Fur Vitamin- Und Ernahrungsforschung. Journal International De Vitaminologie et De Nutrition. 69 (6): 412–8. doi:10.1024/0300-9831.69.6.412. PMID 10642899.
- ^ Taga ME, Walker GC (February 2008). "Pseudo-B12 joins the cofactor family". Journal of Bacteriology. 190 (4): 1157–9. doi:10.1128/JB.01892-07. PMC 2238202. PMID 18083805.
- ^ Voet, Judith G.; Voet, Donald (1995). Biochemistry. New York: J. Wiley & Sons. p. 675. ISBN 0-471-58651-X. OCLC 31819701.
{{cite book}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ Banerjee R, Ragsdale SW (2003). "The many faces of vitamin B12: catalysis by cobalamin-dependent enzymes". Annual Review of Biochemistry. 72: 209–47. doi:10.1146/annurev.biochem.72.121801.161828. PMID 14527323.
- ^ Banerjee RV, Matthews RG (March 1990). "Cobalamin-dependent methionine synthase". FASEB Journal. 4 (5): 1450–9. doi:10.1096/fasebj.4.5.2407589. PMID 2407589.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Wickramasinghe SN (September 1995). "Morphology, biology and biochemistry of cobalamin- and folate-deficient bone marrow cells". Bailliere's Clinical Haematology. 8 (3): 441–59. doi:10.1016/S0950-3536(05)80215-X. PMID 8534956.
- ^ Naidich MJ, Ho SU (October 2005). "Case 87: Subacute combined degeneration". Radiology. 237 (1): 101–5. doi:10.1148/radiol.2371031757. PMID 16183926.
- ^ "CerefolinNAC® Caplets" (PDF). intetlab.com.
- ^ Marks, Allan D. (2009). Basic Medical Biochemistry: A Clinical Approach (3rd ed.). Lippincott, Williams & Wilkins. p. 757. ISBN 078177022X.
{{cite book}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ Allen RH, Seetharam B, Podell E, Alpers DH (January 1978). "Effect of proteolytic enzymes on the binding of cobalamin to R protein and intrinsic factor. In vitro evidence that a failure to partially degrade R protein is responsible for cobalamin malabsorption in pancreatic insufficiency". The Journal of Clinical Investigation. 61 (1): 47–54. doi:10.1172/JCI108924. PMC 372512. PMID 22556.
- ^ a b Combs, Gerald F. (2008). The vitamins: fundamental aspects in nutrition and health (3rd ed.). Amsterdam: Elsevier Academic Press. ISBN 0-12-183492-1. OCLC 150255807.
{{cite book}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help)[page needed] - ^ Abels J, Vegter JJ, Woldring MG, Jans JH, Nieweg HO (October 1959). "The physiologic mechanism of vitamin B12 absorption". Acta Medica Scandinavica. 165 (2): 105–13. doi:10.1111/j.0954-6820.1959.tb14477.x. PMID 13791463.
- ^ Kuzminski AM, Del Giacco EJ, Allen RH, Stabler SP, Lindenbaum J (August 1998). "Effective treatment of cobalamin deficiency with oral cobalamin". Blood. 92 (4): 1191–8. PMID 9694707.
- ^ "If a person stops consuming the vitamin, the body's stores of this vitamin usually take about 3 to 5 years to exhaust".
- ^ "B12: An essential part of a healthy plant-based diet". International Vegetarian Union.
- ^ van der Put NM, van Straaten HW, Trijbels FJ, Blom HJ (April 2001). "Folate, homocysteine and neural tube defects: an overview". Experimental Biology and Medicine. 226 (4): 243–70. doi:10.1177/153537020122600402. PMID 11368417.
- ^ "Vitamin B12 or folate deficiency anaemia - Symptoms". National Health Service, England. May 16, 2016. Retrieved February 16, 2017.
- ^ Masalha R, Chudakov B, Muhamad M, Rudoy I, Volkov I, Wirguin I (September 2001). "Cobalamin-responsive psychosis as the sole manifestation of vitamin B12 deficiency". The Israel Medical Association Journal. 3 (9): 701–3. PMID 11574992.
- ^ Pawlak R, Parrott SJ, Raj S, Cullum-Dugan D, Lucus D (February 2013). "How prevalent is vitamin B(12) deficiency among vegetarians?". Nutrition Reviews. 71 (2): 110–7. doi:10.1111/nure.12001. PMID 23356638.
- ^ Woo KS, Kwok TC, Celermajer DS (August 2014). "Vegan diet, subnormal vitamin B-12 status and cardiovascular health". Nutrients. 6 (8): 3259–73. doi:10.3390/nu6083259. PMC 4145307. PMID 25195560.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ https://academic.oup.com/ajcn/article/71/2/514/4729184
- ^ Biemans E, Hart HE, Rutten GE, Cuellar Renteria VG, Kooijman-Buiting AM, Beulens JW (April 2015). "Cobalamin status and its relation with depression, cognition and neuropathy in patients with type 2 diabetes mellitus using metformin". Acta Diabetologica. 52 (2): 383–93. doi:10.1007/s00592-014-0661-4. PMID 25315630.
- ^ Bottiglieri T, Laundy M, Crellin R, Toone BK, Carney MW, Reynolds EH (August 2000). "Homocysteine, folate, methylation, and monoamine metabolism in depression". Journal of Neurology, Neurosurgery, and Psychiatry. 69 (2): 228–32. doi:10.1136/jnnp.69.2.228. PMC 1737050. PMID 10896698.
- ^ Hall AH, Rumack BH (1987). "Hydroxycobalamin/sodium thiosulfate as a cyanide antidote". The Journal of Emergency Medicine. 5 (2): 115–121. doi:10.1016/0736-4679(87)90074-6. PMID 3295013.
- ^ Dart RC (2006). "Hydroxocobalamin for acute cyanide poisoning: new data from preclinical and clinical studies; new results from the prehospital emergency setting". Clinical Toxicology. 44 Suppl 1 (Suppl. 1): 1–3. doi:10.1080/15563650600811607. PMID 16990188.
- ^ DeVault KR, Talley NJ (September 2009). "Insights into the future of gastric acid suppression". Nat Rev Gastroenterol Hepatol. 6 (9): 524–532. doi:10.1038/nrgastro.2009.125. PMID 19713987.
- ^ Ahmed, MA (2016). "Metformin and Vitamin B12 Deficiency: Where Do We Stand?". Journal of pharmacy & pharmaceutical sciences : a publication of the Canadian Society for Pharmaceutical Sciences, Societe canadienne des sciences pharmaceutiques. 19 (3): 382–398. PMID 27806244.
- ^ Andrès E, Noel E, Goichot B (October 2002). "Metformin-associated vitamin B12 deficiency". Archives of Internal Medicine. 162 (19): 2251–2252. doi:10.1001/archinte.162.19.2251-a. PMID 12390080.
- ^ Gilligan MA (February 2002). "Metformin and vitamin B12 deficiency". Archives of Internal Medicine. 162 (4): 484–485. doi:10.1001/archinte.162.4.484. PMID 11863489.
- ^ Copp, Samantha (December 1, 2007). "What effect does metformin have on vitamin B12 levels?". UK Medicines Information, NHS. Archived from the original on September 27, 2007.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help); Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ Martens JH, Barg H, Warren MJ, Jahn D (March 2002). "Microbial production of vitamin B12". Applied Microbiology and Biotechnology. 58 (3): 275–285. doi:10.1007/s00253-001-0902-7. PMID 11935176.
- ^ Linnell JC, Matthews DM (February 1984). "Cobalamin metabolism and its clinical aspects". Clinical Science. 66 (2): 113–121. doi:10.1042/cs0660113. PMID 6420106.
- ^ 21 CFR 184.1945
- ^ De Baets S, Vandedrinck S, Vandamme EJ (2000). "Vitamins and Related Biofactors, Microbial Production". In Lederberg J (ed.). Encyclopedia of Microbiology. Vol. 4 (2nd ed.). New York: Academic Press. pp. 837–853. ISBN 0-12-226800-8.
- ^ Riaz, Muhammad; Iqbal, Fouzia; Akram, Muhammad (2007). "Microbial production of vitamin B12 by methanol utilizing strain of Pseudomonas species". Pakistan Journal of Biochemistry & Molecular Biology. 1. 40: 5–10.
{{cite journal}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ Zhang, Yemei (January 26, 2009). "New round of price slashing in vitamin B12 sector (Fine and Specialty)". China Chemical Reporter.
{{cite news}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ Loeffler G (2005). Basiswissen Biochemie. Heidelberg: Springer. p. 606. ISBN 3-540-23885-9.
- ^ Bertrand EM, Saito MA, Jeon YJ, Neilan BA (May 2011). "Vitamin B₁₂ biosynthesis gene diversity in the Ross Sea: the identification of a new group of putative polar B₁₂ biosynthesizers". Environmental Microbiology. 13 (5): 1285–98. doi:10.1111/j.1462-2920.2011.02428.x. PMID 21410623.
- ^ Khan, Adil Ghani; Eswaran, S. V. (2003). "Woodward's synthesis of vitamin B12". Resonance. 8 (6): 8–16. doi:10.1007/BF02837864.
{{cite journal}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ Eschenmoser A, Wintner CE (June 1977). "Natural product synthesis and vitamin B12". Science. 196 (4297): 1410–20. doi:10.1126/science.867037. PMID 867037.
- ^ Riether, Doris; Mulzer, Johann (2003). "Total Synthesis of Cobyric Acid: Historical Development and Recent Synthetic Innovations". European Journal of Organic Chemistry. 2003: 30–45. doi:10.1002/1099-0690(200301)2003:1<30::AID-EJOC30>3.0.CO;2-I.
{{cite journal}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ "Synthesis of Cyanocobalamin by Robert B. Woodward (1973)". www.synarchive.com. Retrieved February 15, 2018.
- ^ Riether, Doris; Mulzer, Johann (January 1, 2003). "Total Synthesis of Cobyric Acid: Historical Development and Recent Synthetic Innovations". European Journal of Organic Chemistry. 2003 (1): 30–45. doi:10.1002/1099-0690(200301)2003:13.0.CO;2-I (inactive April 29, 2018). ISSN 1099-0690.
{{cite journal}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help)CS1 maint: DOI inactive as of April 2018 (link) - ^ "Vegan Sources". VeganHealth.org. Archived from the original on October 21, 2017. Retrieved December 21, 2017.
{{cite web}}: Unknown parameter|dead-url=ignored (|url-status=suggested) (help) - ^ Perlman D (1959). "Microbial synthesis of cobamides". Advances in Applied Microbiology. 1: 87–122. PMID 13854292.
- ^ Martens JH, Barg H, Warren MJ, Jahn D (March 2002). "Microbial production of vitamin B12". Applied Microbiology and Biotechnology. 58 (3): 275–85. doi:10.1007/s00253-001-0902-7. PMID 11935176.
- ^ The Nobel Prize in Physiology or Medicine 1934, Nobelprize.org, Nobel Media AB 2014. Retrieved December 2, 2015.
- ^ "Mary Shorb Lecture in Nutrition". Retrieved March 3, 2016.
- ^ a b Shorb, Mary Shaw (May 10, 2012). "Annual Lecture". Department of Animal & Avian Sciences, University of Maryland. Archived from the original on December 12, 2012. Retrieved August 2, 2014.
{{cite web}}: Unknown parameter|dead-url=ignored (|url-status=suggested) (help); Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ Kirkland, Kyle (2010). Biological Sciences: Notable Research and Discoveries. Facts on File. p. 87. ISBN 0816074399.
{{cite book}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ "The Nobel Prize and the Discovery of Vitamins". www.nobelprize.org. Retrieved February 15, 2018.
External links
- Cyanocobalamin at the U.S. National Library of Medicine Medical Subject Headings (MeSH)
