Bortezomib
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Valcade, Chemobort by CYTOGEN Pharma |
| Other names | PS-341 |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a607007 |
| License data |
|
| Pregnancy category |
|
| Routes of administration | Subcutaneous, IV |
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Protein binding | 83% |
| Metabolism | Hepatic, CYP extensively involved |
| Elimination half-life | 9 to 15 hours |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| ChEMBL | |
| PDB ligand | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.125.601 |
| Chemical and physical data | |
| Formula | C19H25BN4O4 |
| Molar mass | 384.237 g/mol g·mol−1 |
| 3D model (JSmol) | |
| |
| |
| (verify) | |
Bortezomib (BAN, INN and USAN; marketed as Velcade by Takeda Oncology; Chemobort by Cytogen and Bortecad by Cadila Healthcare) is an anti-cancer drug and the first therapeutic proteasome inhibitor to be used in humans. Proteasomes are cellular complexes that break down proteins. In some cancers, the proteins that normally kill cancer cells are broken down too quickly. Bortezomib interrupts this process and lets those proteins kill the cancer cells. It is approved in the U.S. and Europe for treating relapsed multiple myeloma and mantle cell lymphoma.[1][2][3] In multiple myeloma, complete clinical responses have been obtained in patients with otherwise refractory or rapidly advancing disease.
Origin and development
Bortezomib was originally synthesized in 1995 at Myogenics. The drug (PS-341) was tested in a small Phase I clinical trial on patients with multiple myeloma. It was brought to further clinical trials by Millennium Pharmaceuticals in October 1999.
In May 2003, seven years after the initial synthesis, bortezomib (marketed as Velcade by Millennium Pharmaceuticals Inc.) was approved in the United States by the Food and Drug Administration (FDA) for use in multiple myeloma, based on the results from the SUMMIT Phase II trial.[4] Bortezomib is approved for initial treatment of patients with multiple myeloma by the U.S. FDA in 2008.[5]
Later in August 2014, this Administration approved Velcade for the retreatment of adult patients with multiple myeloma[6] who had previously responded to Velcade therapy and relapsed at least six months following completion of prior treatment.
Pharmacology

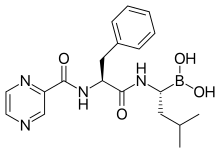
Structure
The drug is an N-protected dipeptide and can be written as Pyz-Phe-boroLeu, which stands for pyrazinoic acid, phenylalanine and Leucine with a boronic acid instead of a carboxylic acid. Peptides are written N-terminus to C-terminus, and this convention is used here even though the "C-terminus" is a boronic acid instead of a carboxylic acid.
Mechanism
The boron atom in bortezomib binds the catalytic site of the 26S proteasome[7] with high affinity and specificity. In normal cells, the proteasome regulates protein expression and function by degradation of ubiquitylated proteins, and also cleanses the cell of abnormal or misfolded proteins. Clinical and preclinical data support a role in maintaining the immortal phenotype of myeloma cells, and cell-culture and xenograft data support a similar function in solid tumor cancers. While multiple mechanisms are likely to be involved, proteasome inhibition may prevent degradation of pro-apoptotic factors, thereby triggering programmed cell death in neoplastic cells. Recently, it was found that bortezomib caused a rapid and dramatic change in the levels of intracellular peptides that are produced by the proteasome.[8] Some intracellular peptides have been shown to be biologically active, and so the effect of bortezomib on the levels of intracellular peptides may contribute to the biological and/or side effects of the drug.
Pharmacokinetics and pharmacodynamics
After subcutaneous administration, peak plasma levels are ~25-50 nM and this peak is sustained for 1-2 hrs. After intravenous injection, peak plasma levels are ~500 nM but only for ~5 minutes, after which the levels rapidly drop as the drug distributes to tissues (volume of distribution is ~500 L).[9][10] Both routes provide equal drug exposures and generally comparable therapeutic efficacy. Elimination half life is 9–15 hours and the drug is primarily cleared by hepatic metabolism.[11]
Pharmacodynamics are measured by measuring proteasome inhibition in peripheral blood mononuclear cells. The much greater sensitivity of myeloma cell lines and mantle cell lines to proteasome inhibition compared with normal peripheral blood mononuclear cells and most other cancer cell lines is poorly understood.
Costs
In the UK, NICE initially recommended against Velcade in October 2006 due to its cost of about £18,000 per patient, and because studies reviewed by NICE reported that it could only extend the life expectancy by an average of six months over standard treatment.[12] However, the company later proposed a performance-linked cost reduction for multiple myeloma,[13] and this was accepted.[14]
Adverse effects
Bortezomib is associated with peripheral neuropathy in 30% of patients; occasionally, it can be painful. This can be worse in patients with pre-existing neuropathy. In addition, myelosuppression causing neutropenia and thrombocytopenia can also occur and be dose-limiting. However, these side effects are usually mild relative to bone marrow transplantation and other treatment options for patients with advanced disease. Bortezomib is associated with a high rate of shingles,[15] although prophylactic acyclovir can reduce the risk of this.[16] Acute interstitial nephritis has also been reported.[17]
Gastro-intestinal (GI) effects and asthenia are the most common adverse events.[18]
Drug interactions
Green tea extract epigallocatechin gallate (EGCG), which had been expected to have a synergistic effect, was found to reduce the effectiveness of bortezomib in the test tube.[19]
Therapeutic efficacy
Two open-label, phase II trials (SUMMIT and CREST) established the efficacy of bortezomib 1.3 mg/m2 (with or without dexamethasone) administered by intravenous bolus on days 1,4,8, and 11 of a 21-day cycle for a maximum of eight cycles in heavily pretreated patients with relapsed/refractory multiple myeloma.[20] The phase III APEX trial demonstrated the superiority of bortezomib 1.3 mg/m2 over a high-dose dexamethasone regimen (e.g. median TTP 6.2 vs 3.5 months, and 1-year survival 80% vs 66%).[20]
Experimental use
Bortezomib has been trialled for systemic lupus erythematosus (SLE) and appeared to reduce disease activity and plasma cell numbers, however 7 of 12 patients dropped out due to side effects, some of which were severe.[21] Bortezomib has been studied for the treatment of antibody-mediated rejection of transplanted kidneys. One study found that the use of high-dose intravenous immunoglobulins in combination with a bortezomib-based treatment regimen seems to be useful, especially when compared to a historical group of patients treated with low-dose intravenous immunoglobulins, plasmapheresis, and rituximab. [22]
See also
- Ixazomib, a proteasome inhibitor that is given by mouth
References
- ^ Takimoto CH, Calvo E. "Principles of Oncologic Pharmacotherapy" in Pazdur R, Wagman LD, Camphausen KA, Hoskins WJ (Eds) Cancer Management: A Multidisciplinary Approach. 11 ed. 2008.
- ^ House, Douglas W. (2014-10-09). "FDA clears Velcade label expansion". Seeking Alpha.
- ^ Haberfeld, H, ed. (2016). Austria-Codex (in German). Vienna: Österreichischer Apothekerverlag.
- ^ Adams J, Kauffman M (2004). "Development of the Proteasome Inhibitor Velcade (Bortezomib)". Cancer Invest. 22 (2): 304–11. doi:10.1081/CNV-120030218. PMID 15199612.
- ^ "U.S. Department of Health and Human Services". fda.gov. June 23, 2008.
- ^ "Millenium: The Takeda Oncology Company". .millennium.com. 2014-08-08.[permanent dead link]
- ^ Bonvini P, Zorzi E, Basso G, Rosolen A (2007). "Bortezomib-mediated 26S proteasome inhibition causes cell-cycle arrest and induces apoptosis in CD-30+ anaplastic large cell lymphoma". Leukemia. 21 (4): 838–42. doi:10.1038/sj.leu.2404528. PMID 17268529.
- ^ Gelman JS, Sironi J, Berezniuk I, Dasgupta S, Castro LM, Gozzo FC, Ferro ES, Fricker LD (2013). "Alterations of the intracellular peptidome in response to the proteasome inhibitor bortezomib". PLOS ONE. 8 (1): e53263. doi:10.1371/journal.pone.0053263. PMC 3538785. PMID 23308178.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Reece DE, Sullivan D, Lonial S, Mohrbacher AF, Chatta G, Shustik C, Burris H 3rd, Venkatakrishnan K, Neuwirth R, Riordan WJ, Karol M, von Moltke LL, Acharya M, Zannikos P, Keith Stewart A (2011). "Pharmacokinetic and pharmacodynamic study of two doses of bortezomib in patients with relapsed multiple myeloma". Cancer Chemother Pharmacol. 67: 57–67. doi:10.1007/s00280-010-1283-3. PMC 3951913.
- ^ Voorhees PM, Dees EC, O'Neil B, Orlowski RZ (2003). "The proteasome as a target for cancer therapy". Clin Cancer Res. 9 (17): 6316–25. PMID 14695130.
- ^ Moreau P, Pylypenko H, Grosicki S, Karamanesht I, Leleu X, Grishunina M, Rekhtman G, Masliak Z, Robak T, Shubina A, Arnulf B, Kropff M, Cavet J, Esseltine DL, Feng H, Girgis S, van de Velde H, Deraedt W, Harousseau JL (2011). "Subcutaneous versus intravenous administration of bortezomib in patients with relapsed multiple myeloma: a randomised, phase 3, non-inferiority study". The Lancet Oncology. 12: 431–40. doi:10.1016/s1470-2045(11)70081-x.
- ^ "NHS watchdog rejects cancer drug". BBC News UK. 2006-10-20. Retrieved 2009-08-14.
- ^ "Summary of VELCADE Response Scheme" (PDF). Archived from the original (PDF) on 2009-04-19. Retrieved 2009-08-14.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ "More Velcade-Style Risk-Sharing In The UK?". Euro Pharma Today. 2009-01-21. Archived from the original on 2011-07-10. Retrieved 2009-08-14.
{{cite web}}: Unknown parameter|dead-url=ignored (|url-status=suggested) (help) - ^ Oakervee HE, Popat R, Curry N, et al. (2005). "PAD combination therapy (PS-341/bortezomib, doxorubicin and dexamethasone) for previously untreated patients with multiple myeloma". Br J Haematol. 129 (6): 755–62. doi:10.1111/j.1365-2141.2005.05519.x. PMID 15953001.
- ^ Pour L.; Adam Z.; Buresova L.; et al. (2009). "Varicella-zoster virus prophylaxis with low-dose acyclovir in patients with multiple myeloma treated with bortezomib". Clinical Lymphoma & Myeloma. 9 (2): 151–3. doi:10.3816/CLM.2009.n.036. PMID 19406726.
- ^ "Bortezomib-induced acute interstitial nephritis". Nephrol. Dial. Transplant. 30 (7): 1225–1229. 2015. doi:10.1093/ndt/gfv222.
- ^ Highlights Of Prescribing Information Archived February 19, 2009, at the Wayback Machine
- ^ Golden, EB; Lam, PY; Kardosh, A; Gaffney, KJ; Cadenas, E; Louie, SG; Petasis, NA; Chen, TC; Schönthal, AH (4 June 2009). "Green tea polyphenols block the anticancer effects of bortezomib and other boronic acid-based proteasome inhibitors". Blood. 113 (23): 5927–37. doi:10.1182/blood-2008-07-171389. PMID 19190249.
- ^ a b Curran M, McKeage K (2009). "Bortezomib: A Review of its Use in Patients with Multiple Myeloma". Drugs. 69 (7): 859–888. doi:10.2165/00003495-200969070-00006. PMID 19441872. Archived from the original on 2011-10-08. Retrieved 2010-03-26.
{{cite journal}}: Unknown parameter|dead-url=ignored (|url-status=suggested) (help) - ^ Alexanter T; et al. (2015). "The proteasome inhibitior bortezomib depletes plasma cells and ameliorates clinical manifestations of refractory systemic lupus erythematosus". Ann Rheum Dis. 74: 1474–8. doi:10.1136/annrheumdis-2014-206016. PMC 4484251. PMID 25710470.
- ^ Nils Lachmann, Michael Duerr, Constanze Schönemann, Axel Pruß, Klemens Budde, and Johannes Waiser, “Treatment of Antibody-Mediated Renal Allograft Rejection: Improving Step by Step,” Journal of Immunology Research, vol. 2017, Article ID 6872046, 9 pages, 2017. https://doi.org/10.1155/2017/6872046.
External links
- [1]
- Myeloma patients campaigning for access to a life prolonging cancer drug
- Millennium Pharmaceuticals website on Velcade
- Multiple Myeloma Research Foundation article on Velcade
- International Myeloma Foundation article on Velcade
- U.S. Food and Drugs Administration on Velcade
- Dedicated website for European audience
