Alternative medicine: Difference between revisions
→Acupuncture: add body manipulation systematic reviews |
Reverted to revision 541037042 by Qexigator: removed co tract material added without consensus. (TW) |
||
| Line 1: | Line 1: | ||
{{Merge|Integrative medicine|date=February 2013}} |
{{Merge|Integrative medicine|date=February 2013}} |
||
{{NPOV|date=February 2013}} |
{{NPOV|date=February 2013}} |
||
{{primary|date=March 2013}} |
|||
{{pp-semi-sock|small=yes}} |
{{pp-semi-sock|small=yes}} |
||
{{Alternative medical systems |
{{Alternative medical systems |
||
| Line 18: | Line 17: | ||
| HCPCSlevel2 = |
| HCPCSlevel2 = |
||
}} |
}} |
||
'''Alternative medicine''' is any of a wide range of [[health care]] practices, products and therapies which, at least up to the end of the twentieth century, were typically not included in the degree courses of established [[medical schools]] teaching western medicine in the tradition of the [[Flexner Report]] or similar.<ref>[[Peking Union Medical College]] is an instance of the influence of the Flexner Report outside N. America: Mary Brown Bullock, ''An American Transplant: The Rockefeller Foundation and the Peking Union Medical College'', Berkeley: University of California Press, 1980. Top Chinese Universities in Medicine, 2012[http://www.cucas.edu.cn/HomePage/majorrankings/2011-11-11/1320997392d2449.shtml] [[Peking University Health Science Center]] (formerly Beijing Medical University) was the first of the kind in China to teach western medicine and train medical professionals. Top Chinese Universities in Medicine, 2012[http://www.cucas.edu.cn/HomePage/majorrankings/2011-11-11/1320997392d2449.shtml]. </ref> <ref>A [[Medical college in India]] is one awarding MBBS degrees ([[Bachelor of Medicine, Bachelor of Surgery]]), the course for which starts with subjects such as biochemistry, physiology, anatomy, microbiology, pathology and pharmacology, as in western medical schools.</ref> Examples |
'''Alternative medicine''' is any of a wide range of [[health care]] practices, products and therapies which, at least up to the end of the twentieth century, were typically not included in the degree courses of established [[medical schools]] teaching western medicine in the tradition of the [[Flexner Report]] or similar.<ref>[[Peking Union Medical College]] is an instance of the influence of the Flexner Report outside N. America: Mary Brown Bullock, ''An American Transplant: The Rockefeller Foundation and the Peking Union Medical College'', Berkeley: University of California Press, 1980. Top Chinese Universities in Medicine, 2012[http://www.cucas.edu.cn/HomePage/majorrankings/2011-11-11/1320997392d2449.shtml] [[Peking University Health Science Center]] (formerly Beijing Medical University) was the first of the kind in China to teach western medicine and train medical professionals. Top Chinese Universities in Medicine, 2012[http://www.cucas.edu.cn/HomePage/majorrankings/2011-11-11/1320997392d2449.shtml]. </ref> <ref>A [[Medical college in India]] is one awarding MBBS degrees ([[Bachelor of Medicine, Bachelor of Surgery]]), the course for which starts with subjects such as biochemistry, physiology, anatomy, microbiology, pathology and pharmacology, as in western medical schools.</ref> Examples include [[homeopathy]], [[Ayurveda]], [[chiropractic]] and [[acupuncture]]. |
||
'''Complementary medicine''' is alternative medicine used together with conventional medical treatment, in a [[belief]], not proven by using scientific methods, that it increases the [[efficacy|effectiveness]], or "complements", the treatment.<ref name="whccamp.hhs.gov">{{cite web |title=White House Commission on Complementary and Alternative Medicine Policy |url=http://whccamp.hhs.gov/fr2.html |date=March 2002| archiveurl = http://www.webcitation.org/61C8iiefX | archivedate = 2011-08-25| deadurl=no}}"The Commissioners believe and have repeatedly stated in this Report that our response should be to hold all systems of health and healing, including conventional and CAM, to the same rigorous standards of good science and health services research. Although the Commissioners support the provision of the most accurate information about the state of the science of all CAM modalities, they believe that it is premature to advocate the wide implementation and reimbursement of CAM modalities that are yet unproven."</ref><ref>{{cite journal|author=[[Edzard Ernst|Ernst E.]] |title=Complementary medicine: common misconceptions |journal=[[Journal of the Royal Society of Medicine]] |year=1995 |volume=88 |issue=5 |pages=244–247| pmid = 7636814|pmc=1295191 }}"Complementary medicine, defined as health care which lies for the most part outside the mainstream of conventional medicine"</ref><ref>{{cite journal |author=Joyce CR |title=Placebo and complementary medicine |journal=[[The Lancet]] |year=1994 |volume=344|issue=8932 |pages=1279–1281 |doi=10.1016/S0140-6736(94)90757-9}}</ref><ref |
'''Complementary medicine''' is alternative medicine used together with conventional medical treatment, in a [[belief]], not proven by using scientific methods, that it increases the [[efficacy|effectiveness]], or "complements", the treatment.<ref name="whccamp.hhs.gov">{{cite web |title=White House Commission on Complementary and Alternative Medicine Policy |url=http://whccamp.hhs.gov/fr2.html |date=March 2002| archiveurl = http://www.webcitation.org/61C8iiefX | archivedate = 2011-08-25| deadurl=no}}"The Commissioners believe and have repeatedly stated in this Report that our response should be to hold all systems of health and healing, including conventional and CAM, to the same rigorous standards of good science and health services research. Although the Commissioners support the provision of the most accurate information about the state of the science of all CAM modalities, they believe that it is premature to advocate the wide implementation and reimbursement of CAM modalities that are yet unproven."</ref><ref>{{cite journal|author=[[Edzard Ernst|Ernst E.]] |title=Complementary medicine: common misconceptions |journal=[[Journal of the Royal Society of Medicine]] |year=1995 |volume=88 |issue=5 |pages=244–247| pmid = 7636814|pmc=1295191 }}"Complementary medicine, defined as health care which lies for the most part outside the mainstream of conventional medicine"</ref><ref>{{cite journal |author=Joyce CR |title=Placebo and complementary medicine |journal=[[The Lancet]] |year=1994 |volume=344|issue=8932 |pages=1279–1281 |doi=10.1016/S0140-6736(94)90757-9}}</ref><ref>{{cite web | quote = alternative medicine refers to all treatments that have not been proven effective using scientific methods | title = Science and Technology: Public Attitudes and Public Understanding Science Fiction and Pseudoscience - Belief in Alternative Medicine | publisher = [[National Science Foundation]] | url = http://www.nsf.gov/statistics/seind02/c7/c7s5.htm }}</ref> '''CAM''' is the abbreviation for '''Complementary and alternative medicine'''.<ref name=ernstinterview>{{cite web |url=http://www.harcourt-international.com/ernst/interview.cfm |archiveurl=http://web.archive.org/web/20070311015608/http://www.harcourt-international.com/ernst/interview.cfm |publisher=Elsevier Science |title=Interview with [[Edzard Ernst]], editor of ''The Desktop Guide to Complementary and Alternative Medicine'' |year=2002 |archivedate=2007-03-11}}</ref><ref name=CassilethDeng2004>{{cite journal |author=Cassileth BR, Deng G |title=Complementary and alternative therapies for cancer |journal=[[The Oncologist]] |volume=9 |issue=1 |pages=80–9 |year=2004 |pmid=14755017 |doi=10.1634/theoncologist.9-1-80}}</ref> [[Integrative medicine]] (or integrative health) is the combination of the practices and methods of alternative medicine with [[evidence-based medicine]].<ref name=BMJ_May>{{cite journal | journal=British Medical Journal | volume=343 | doi=10.1136/bmj.d4372 | date=12 July 2011 | title=College of Medicine: What is integrative health? | author=James May | url=http://www.bmj.com/content/343/bmj.d4372.full | pages=d4372 | pmid=21750063}}</ref> |
||
The term ''alternative medicine'' is used in information issued by public bodies in the United States of America<ref>[http://www.fda.gov/Drugs/ResourcesForYou/Consumers/BuyingUsingMedicineSafely/MedicationHealthFraud/ucm207747.htm FDA, Drugs, information for consumers]</ref> and the United Kingdom.<ref name="NHS">[http://www.nhscareers.nhs.uk/explore-by-career/wider-healthcare-team/careers-in-the-wider-healthcare-team/clinical-support-staff/complementary-and-alternative-medicine-(cam)/ NHS complementary provision]</ref> Regulation and licensing of alternative medicine and [[health care provider]]s varies from country to country, and state to state. |
The term ''alternative medicine'' is used in information issued by public bodies in the United States of America<ref>[http://www.fda.gov/Drugs/ResourcesForYou/Consumers/BuyingUsingMedicineSafely/MedicationHealthFraud/ucm207747.htm FDA, Drugs, information for consumers]</ref> and the United Kingdom.<ref name="NHS">[http://www.nhscareers.nhs.uk/explore-by-career/wider-healthcare-team/careers-in-the-wider-healthcare-team/clinical-support-staff/complementary-and-alternative-medicine-(cam)/ NHS complementary provision]</ref> Regulation and licensing of alternative medicine and [[health care provider]]s varies from country to country, and state to state. |
||
==Introduction== |
== Introduction == |
||
=== |
===Public discussion: how alternative medicine got its name=== |
||
Dating from the 1970s, medical professionals, sociologists, anthropologists and other commentators noted the increasing visibility of a wide variety of health practices that had neither derived directly from nor been verified by mainstream biomedical science.<ref name="bivins 2011">{{cite book|last=Bivins|first=Roberta|editor=Jackson, Mark|title=The Oxford Handbook of the History of Medicine|url=http://books.google.com/books?id=cpjgoazGIC4C|date=25 August 2011|publisher=Oxford University Press|isbn=978-0-19-954649-7|pages=578–597|chapter=Histories of Hetodoxy}}</ref> Since that time, those who have analyzed this trend have deliberated over the most apt language with which to describe this emergent health field.<ref name="bivins 2011" /> A variety of terms have been used, including heterodox, irregular, fringe and alternative medicine while others, particularly medical commentators, have been satisfied to label them as instances of quackery.<ref name="bivins 2011" /> The most persistent term has been alternative medicine but its use is problematic as it assumes a value-laden dichotomy between a medical fringe, implicitly of borderline acceptability at best, and a privileged medical orthodoxy, associated with validated medico-scientific norms.<ref name="jutte 2001" /> As a relational concept, the category of alternative medicine can never become an object of analysis in its own right, but can only be understood in terms of the current medical orthodoxy.<ref>{{cite pmid|16562317|noedit}}</ref> It can also be misleading as the use of the term alternative may also erroneously imply that a real medical alternative exists.<ref name="jutte 1999">{{cite pmid|10885128}}</ref> As with near-synonymous expressions, such as unorthodox, complementary, marginal, or the nakedly polemical "quack", these linguistic devices have served, in the context of processes of professionalisation and market competition, to establish the authority of official medicine and police the boundary between it and its unconventional rivals.<ref name="jutte 2001">{{Cite book| publisher = European Association for the History of Medicine and Health| pages = 11–26| editors = Motzi Eklof and Marie C. Nelson (eds)| last = Jütte| first = Robert| title = Historical Aspects of Unconventional Medicine: Approaches, Concepts, Case Studies| chapter = Alternative Medicine and Medico-Historical Semantics| date = 2001|chapterurl=http://www.igm-bosch.de/content/language1/downloads/EAHMH_4_02jue.pdf|isbn=095365222X}} Robert Jütte is an adjunct professor of history at the University of Stuttgart and editor of the journal ''Medizin, Gesellschaft und Geschicht''.</ref> From a historical perspective, the emergence of alternative medicine, if not the term itself, is typically dated to the 19th century.<ref> {{cite book|last=Porter|first=Roy|chapter=Before the Fringe: 'Quackery' and the Eighteenth-Century Medical Market|editor=Cooter, Roger (ed.)|title=Studies in the History of Alternative Medicine|year=1988|publisher=MacMillan|location=London|isbn=9780333462133|url=http://books.google.ie/books?id=FFE2AQAAIAAJ&q}}; {{cite pmid|10885126}}; {{cite pmid|17139061}}</ref> This is despite the fact that there are variants of Western non-conventional medicine that arose in the late-eighteenth century or earlier and some non-Western medical traditions, currently considered alternative in the West and elsewhere, which boast extended historical pedigrees.<ref name="jutte 2001" /> Alternative medical systems, however, can only be said to exist when there is an identifiable, regularized and authoritative medical orthodoxy, such as arose in the West during the nineteenth-century, to which they can function as an alternative. <ref name="Bivins2007p171">{{cite book|last=Bivins|first=Roberta|title=Alternative Medicine? A History|publisher=Oxford University Press|location=Oxford|isbn=9780199218875|url=http://books.google.com/?id=_x1zg5GPgxgC|year=2007|page=171}}</ref> |
|||
The [[history of alternative medicine]] is such that not until the end of the nineteenth century does the concept of alternative medicine as a historical category become tenable.<ref>Ramsey, Matthew (1999), "Alternative Medicine in Modern France", Medical history 43 (3): 286–322, PMC 1044147, PMID 10885126, http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1044147 </ref> Alternative medical systems can only exist when there is an identifiable, regularized and authoritative medical orthodoxy, such as arose in the west during the nineteenth-century, to which they can function or act as an alternative. <ref name="Bivins2007p171">{{cite book|last=Bivins|first=Roberta|title=Alternative Medicine? A History|publisher=Oxford University Press|location=Oxford|isbn=9780199218875|url=http://books.google.ie/books/about/Alternative_Medicine_A_History.html?id=_x1zg5GPgxgC&redir_esc=y|year=2007|page=171}} Roberta Bivins is an associate professor and the director of the Centre for the History of Medicine at the University of Warwick, England.</ref> According to Robert Jütte, labels used to describe health belief systems other than modern, scientific, Western medicine, are either misleading or carry a semantic load, as for example "alternative", "marginal", "fringe", "unorthodox" or "irregular",<ref>{{Cite book| publisher = European Association for the History of Medicine and Health| pages = 11-26| editors = Motzi Eklof and Marie C. Nelson (eds)| last = Jütte| first = Robert| title = Historical Aspects of Unconventional Medicine: Approaches, Concepts, Case Studies| chapter = Alternative Medicine and Medico-Historical Semantics| date = 2001|chapterurl=http://www.igm-bosch.de/content/language1/downloads/EAHMH_4_02jue.pdf|isbn=095365222X}} Robert Jütte is an adjunct professor of history at the University of Stuttgart and editor of the journal ''Medizin, Gesellschaft und Geschicht''.</ref> and historians have had some difficulty simply to name and describe without connotative judgement. Jütte found that in the period from the mid-nineteenth century to the first two decades of the twentieth, the opposition of the developing medical establishment in Germany, based on modern scientific medicine, had resulted in the threat from homeopaths, naturopaths, mesmerists and others being stemmed by legal and organizational measures.<ref>''The Historiography of Nonconventional Medicine in Germany: A Concise Overview'', 1999[http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1044149/pdf/medhist00018-0066.pdf]</ref> |
|||
During the late eighteenth and nineteenth centuries regular and irregular medical practitioners became more clearly differentiated throughout much of Europe.<ref>{{cite book|last=Brunton|first=Deborah|chapter=The Emergence of a Modern Profession?|title=Medicine Transformed: Health, Disease and Society in Europe, 1800-1930|editor=Brunton, Deborah|location=Manchester|publisher=Open University|year=2004|isbn=9780719067358}}; {{cite book|last=Brown|first=Michael|chapter=Medicine, Quackery and the Free Market: The 'War' against Morison's Pills and the Construction of the Medical Profession, ''c''. 1830-''c''. 1850|editor=Mark S.R. Jenner & Patrick Wallis|title=Medicine and the Market in England and Its Colonies, c.1450-c.1850|location=New York|publisher=Palgrave and MacMillan|year=2007|pages=238–61|isbn=9780230506435}}</ref> |
|||
As the nineteenth century progressed, most Western states converged in the creation of legally delimited and semi-protected medical markets.<ref>{{cite book|last=Pickstone|first=John|chapter=Medicine, Society and the State|editor=Roy Porter|title=The Cambridge History of Medicine|publisher=Cambridge University Press|location=New York|year=2006|pages=260–97|isbn=9780521864268|ref=harv}}</ref> It is at this point that an "official" medicine, created in cooperation with the state and employing a scientific rhetoric of [[Legitimation|legitimacy]], emerges as a recognizable entity and that the concept of alternative medicine as a historical category becomes tenable.<ref name="ramsey 1999">{{cite pmid|10885126|noedit}}</ref> As part of this process, professional adherents of mainstream medicine in countries such as Germany, France, and Britain increasingly invoked the scientific basis of their discipline as a means of engendering internal professional unity and of external differentiation in the face of sustained market competition from homeopaths, naturopaths, mesmerists and other nonconventional medical practitioners, finally achieving a degree of imperfect dominance through alliance with the state and the passage of regulatory legislation.<ref name="jutte 1999" /><ref name="jutte 2001" /> In the United States the [[Johns Hopkins School of Medicine|Johns Hopkins University School of Medicine]], based in Baltimore, Maryland, opened in 1893 and was the first medical school devoted to teaching "German scientific medicine".<ref>Barry D. Silverman, ''William Henry Welch (1850–1934): the road to Johns Hopkins''. Proc (Bayl Univ Med Cent). 2011 July; 24(3): 236–242.[http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3124910/]</ref> Buttressed by the increased authority consequent to the significant advances in the medical sciences of the late 19th century onwards — including the development and application of the [[germ theory of disease]] by the chemist [[Louis Pasteur]] and the surgeon [[Joseph Lister, 1st Baron Lister]], and of the use of [[X-ray]]s ([[Röntgen ray]]s) — the 1910 [[Flexner Report]] called upon [[Medical school in the United States|American medical schools]] to follow the model set by the John Hopkins School of Medicine and adhere to mainstream science in their teaching and research. This was in a belief, mentioned in the Report's introduction, that the preliminary and professional training then prevailing in medical schools should be reformed in view of the new means for diagnosing and combating disease being made available to physicians and surgeons by the sciences on which medicine depended.<ref>Flexner Report, Introduction p.viii "The fundamental sciences upon which medicine depends have been greatly extended. The laboratory has come to furnish alike to the physician and to the surgeon a new means for diagnosing and combating disease. The education of the medical practitioner under these changed conditions makes entirely different demands in respect of both preliminary and professional training."[http://www.carnegiefoundation.org/sites/default/files/elibrary/Carnegie_Flexner_Report.pdf]</ref> Among putative medical practices available at the time which later became known as "alternative medicine" were homeopathy (founded in Germany in the early 19c.) and chiropractic (founded in North America in the late 19c.). These conflicted in principle with the developments in medical science upon which the Flexner reforms were based, and they have not become compatible with further advances of medical science such as listed in [[Timeline of medicine and medical technology]], 1900-1999 and 2000-present, nor have Ayurveda, acupuncture or other kinds of alternative medicine. |
|||
By 1893 [[Johns Hopkins University]] Baltimore, Maryland, had opened America's first medical school devoted to teaching "German scientific medicine",<ref>Barry D. Silverman, ''William Henry Welch (1850–1934): the road to Johns Hopkins''. Proc (Bayl Univ Med Cent). 2011 July; 24(3): 236–242.[http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3124910/]</ref> and such were the advances in medical science being made, including the development and application of the [[germ theory of disease]] by the chemist [[Louis Pasteur]] and the surgeon [[Joseph Lister, 1st Baron Lister]], and of the use of [[X-ray]]s ([[Röntgen ray]]s), that by 1910 the [[Flexner Report]] called upon [[Medical school in the United States|American medical schools]] to adhere to mainstream science in their teaching and research. This was in a belief, mentioned in the Report's introduction, that the preliminary and professional training then prevailing in medical schools should be reformed in view of the new means for diagnosing and combating disease being made available to physicians and surgeons by the sciences on which medicine depended.<ref>Flexner Report, Introduction p.viii "The fundamental sciences upon which medicine depends have been greatly extended. The laboratory has come to furnish alike to the physician and to the surgeon a new means for diagnosing and combating disease. The education of the medical practitioner under these changed conditions makes entirely different demands in respect of both preliminary and professional training."[http://www.carnegiefoundation.org/sites/default/files/elibrary/Carnegie_Flexner_Report.pdf]</ref> Among putative medical practices available at the time which later became known as "alternative medicine" were homeopathy (founded in Germany in the early 19c.) and chiropractic (founded in North America in the late 19c.). These conflicted in principle with the developments in medical science upon which the Flexner reforms were based, and they have not become compatible with further advances of medical science such as listed in [[Timeline of medicine and medical technology]], 1900-1999 and 2000-present, nor have Ayurveda, acupuncture or other kinds of alternative medicine. |
|||
At the same time "[[Tropical medicine]]" was being developed as a specialist branch of western medicine in research establishments such as [[Liverpool School of Tropical Medicine]] founded 1898, [[London School of Hygiene & Tropical Medicine]], founded 1899 and [[Tulane University School of Public Health and Tropical Medicine]], founded 1912. A distinction was being made between western scientific medicine and indigenous systems. An example is given by an official report about indigenous systems of medicine in India, including Ayurveda, submitted by [[Mohammad Usman of Madras]] and others in 1923. This stated that the first question the Committee considered was "to decide whether the indigenous systems of medicine were scientific or not".<ref>''The report of the Committee on the Indigenous systems of medicine, Madras'' (also known as the ''Usman Report'').Gram Vichar, ''What is the role of indigenous medical sciences in our health care system?'' December 1984, condensed in Perspective, Vol.10, no.3, 1985[http://www.vikalpa.com/pdf/articles/1985/1985_july_sep_271_277.pdf] [http://www.worldcat.org/title/report-of-the-committee-on-the-indigenous-systems-of-medicine-madras/oclc/229483035&referer=brief_results]</ref><ref>Bivins, Roberta, ''Alternative Medicine? A History'' pp.164-170, Oxford University Press, 2007</ref> |
|||
At the same time "[[Tropical medicine]]" was being developed as a specialist branch of western medicine in research establishments such as [[Liverpool School of Tropical Medicine]] founded 1898, [[London School of Hygiene & Tropical Medicine]], founded 1899 and [[Tulane University School of Public Health and Tropical Medicine]], founded 1912. A distinction was being made between western scientific medicine and indigenous systems. An example is given by an official report about indigenous systems of medicine in Madras, India, including Ayurveda, submitted by [[Mohammad Usman of Madras]] and others in 1923. This stated that the first question the Committee considered was "to decide whether the indigenous systems of medicine were scientific or not".<ref>''The report of the Committee on the Indigenous systems of medicine, Madras'' (also known as the ''Usman Report'').Gram Vichar, ''What is the role of indigenous medical sciences in our health care system?'' December 1984, condensed in Perspective, Vol.10, no.3, 1985[http://www.vikalpa.com/pdf/articles/1985/1985_july_sep_271_277.pdf] [http://www.worldcat.org/title/report-of-the-committee-on-the-indigenous-systems-of-medicine-madras/oclc/229483035&referer=brief_results]</ref> |
|||
By the later twentieth century the term 'alternative medicine' had come into use for the purposes of public discussion,<ref>According to the ''Oxford English Dictionary'', the earliest recorded English language usage in a print medium of the term "alternative medicine" is found in a 1974 text by Helen Kruger. {{cite book|chapter=alternative|title=Oxford English Dictionary|edition=OED Online|date=December 2012|publisher=Oxford University Press|url=http://www.oed.com/view/Entry/5803?redirectedFrom=Alternative+medicine|accessdate=20 February 2013}}; {{cite book|year=1974|first=Helen|last=Kruger|title=Other healers, other cures: a guide to alternative medicine|url=http://books.google.ie/books?id=S5_8AAAACAAJ&dq|publisher=Bobbs-Merrill|isbn=9780672517082}} See also: {{cite book|last=British Medical Association|title=Complementary Medicine, New Approach to Good Practice|publisher=Oxford University Press|year=1993|url=http://books.google.ie/books/about/Complementary_medicine.html?id=rTFrAAAAMAAJ|isbn=9780192861665}}; {{cite book|last1=Cant|first1=Sarah|last2=Sharma|first2=Ursula|chapter=Alternative health practices and systems|pages=433–|editor1-last=Albrecht|editor1-first=Gary L|editor2-last=Fitzpatrick|editor2-first=Ray|editor3-last=Scrimshaw|editor3-first=Susan C.|title=The Handbook of Social Studies in Health and Medicine|url=http://books.google.com/books?id=LyK1e6U7fU0C&pg=PA433|date=22 October 1999|publisher=SAGE|isbn=978-1-84787-096-4}}; {{cite book|last=Saks|first=Mike|title=Orthodox and Alternative Medicine: Politics, Professionalization and Health Care|url=http://books.google.com/books?id=zW2_iJsZFS0C&pg=PA117|year=2003|publisher=SAGE|isbn=978-1-4462-6536-9|page=117}}</ref> but it was not always being used with the same meaning by all parties. [[Arnold S. Relman]] remarked in 1998 that in the best kind of medical practice, all proposed treatments must be tested objectively, and that in the end there will only be treatments that pass and those that do not, those that are proven worthwhile and those that are not. He asked 'Can there be any reasonable "alternative"?'(NEJM, 1998)<ref>Arnold S. Relman, a former editor of ''[[The New England Journal of Medicine]]'' |
|||
By the later twentieth century the term 'alternative medicine' had come into use for the purposes of public discussion,<ref>According to the ''Oxford English Dictionary'', the earliest recorded English language usage in a print medium of the term "alternative medicine" is found in a 1974 text by Helen Kruger. {{cite book|chapter=alternative|title=Oxford English Dictionary|edition=OED Online|date=December 2012|publisher=Oxford University Press|url=http://www.oed.com/view/Entry/5803?redirectedFrom=Alternative+medicine|accessdate=20 February 2013}}; {{cite book|year=1974|first=Helen|last=Kruger|title=Other healers, other cures: a guide to alternative medicine|url=http://books.google.ie/books?id=S5_8AAAACAAJ&dq|publisher=Bobbs-Merrill|isbn=9780672517082}} See also: {{cite book|last=British Medical Association|title=Complementary Medicine, New Approach to Good Practice|publisher=Oxford University Press|year=1993|url=http://books.google.ie/books/about/Complementary_medicine.html?id=rTFrAAAAMAAJ|isbn=9780192861665}}; {{cite book|last1=Cant|first1=Sarah|last2=Sharma|first2=Ursula|chapter=Alternative health practices and systems|pages=426–439|editor1-last=Albrecht|editor1-first=Gary L|editor2-last=Fitzpatrick|editor2-first=Ray|editor3-last=Scrimshaw|editor3-first=Susan C.|title=The Handbook of Social Studies in Health and Medicine|url=http://books.google.com/books?id=LyK1e6U7fU0C&pg=PA433|date=22 October 1999|publisher=SAGE|isbn=978-1-84787-096-4|pages=433–}}; {{cite book|last=Saks|first=Mike|title=Orthodox and Alternative Medicine: Politics, Professionalization and Health Care|url=http://books.google.com/books?id=zW2_iJsZFS0C&pg=PA117|year=2003|publisher=SAGE|isbn=978-1-4462-6536-9|page=117}}</ref> but it was not always being used with the same meaning by all parties. [[Arnold S. Relman]] remarked in 1998 that in the best kind of medical practice, all proposed treatments must be tested objectively, and that in the end there will only be treatments that pass and those that do not, those that are proven worthwhile and those that are not. He asked 'Can there be any reasonable "alternative"?'(NEJM, 1998)<ref>Arnold S. Relman, a former editor of ''[[The New England Journal of Medicine]]'' |
|||
[http://www.quackwatch.org/11Ind/weil.html A trip to Stonesville.] ''[[The New Republic]]'', Dec 14, 1998.</ref> |
[http://www.quackwatch.org/11Ind/weil.html A trip to Stonesville.] ''[[The New Republic]]'', Dec 14, 1998.</ref> |
||
In respect of alternative medicine [[History of alternative medicine#altmed since the 1970s|since the 1970s]] in North America, Great Britain and elsewhere, there has been a tendency for the terms ‘alternative’ and ‘complementary’ to be used interchangeably to describe a wide diversity of therapies that attempt to use the self-healing powers of the body by amplifying natural recuperative processes to restore health. By 1990, approximately 60 million Americans had used one or more complementary or alternative therapies to address health issues, according to a nationwide survey in the United States published in 1993 by David Eisenberg. <ref>{{cite journal | author = Eisenberg DM |year=1993|title=Unconventional Medicine in the United States |
In respect of alternative medicine [[History of alternative medicine#altmed since the 1970s|since the 1970s]] in North America, Great Britain and elsewhere, there has been a tendency for the terms ‘alternative’ and ‘complementary’ to be used interchangeably to describe a wide diversity of therapies that attempt to use the self-healing powers of the body by amplifying natural recuperative processes to restore health. By 1990, approximately 60 million Americans had used one or more complementary or alternative therapies to address health issues, according to a nationwide survey in the United States published in 1993 by David Eisenberg. <ref>{{cite journal | author = Eisenberg DM |year=1993|title=Unconventional Medicine in the United States – Prevalence, Costs, and Patterns of Use|journal= N Engl J Med|volume= 328|pages=246–252|doi=10.1056/NEJM199301283280406 | pmid=8418405 | author-separator = , | display-authors = 1 | last2 = Kessler | first2 = Ronald C. | last3 = Foster | first3 = Cindy | last4 = Norlock | first4 = Frances E. | last5 = Calkins | first5 = David R. | last6 = Delbanco | first6 = Thomas L. | issue = 4 }}</ref> A study published in the November 11, 1998 issue of the [[Journal of the American Medical Association]] reported that 42% of Americans had used complementary and alternative therapies, up from 34% in 1990.<ref>{{cite journal | author = Eisenberg DM |year=1998|title= Trends in alternative medicine use in the United States, 1990–1997: results of a follow-up national survey |journal=JAMA|volume= 280 |issue=18|pages=1569–75|pmid=9820257 |doi=10.1001/jama.280.18.1569 | author-separator = , | author2 = Davis RB | author3 = Ettner SL | display-authors = 3 | last4 = Appel | first4 = S | last5 = Wilkey | first5 = S | last6 = Van Rompay | first6 = M | last7 = Kessler | first7 = RC}}</ref> However, despite the growth in patient demand for complementary medicine, most of the early alternative/complementary medical centers failed.<ref name=bestpractices>Best Practices in Integrative Medicine: A Report from the Bravewell Clinical Network. Published 2007. The Bravewell Collaborative. Page 4.</ref> |
||
Based on an analysis of trends in the coverage of complementary and alternative medicine (CAM) in five prestigious American medical journals during the period of reorganization within medicine (1965–1999), one writer proposed that the medical profession responded to the growth of CAM in three phases. In each phase, there were changes in the medical marketplace which influenced the type of response in the journals. The changes were such as relaxed medical licensing, the development of managed care, rising consumerism, and the establishment of the USA Office of Alternative Medicine (now [[National Center for Complementary and Alternative Medicine]]).<ref> ''In 1991 the Senate Appropriations Committee responsible for funding the National Institutes of Health (NIH) declared itself "not satisfied that the conventional medical community as symbolized at the NIH has fully explored the potential that exists in unconventional medical practices." '' James Harvey Young, The Development of the Office of Alternative Medicine in the National Institutes of Health, 1991-1996. From: Bulletin of the History of Medicine Volume 72, Number 2, Summer 1998 pp. 279-298 | 10.1353/bhm.1998.0110[http://muse.jhu.edu/login?auth=0&type=summary&url=/journals/bulletin_of_the_history_of_medicine/v072/72.2young.html]</ref> In the "condemnation" phase, from the late 1960s to the early 1970s, authors ridiculed, exaggerated the risks, and petitioned the state to contain CAM. In the "reassessment" phase (mid-1970s through early 1990s), when increased consumer utilization of CAM was prompting concern, authors pondered whether patient dissatisfaction and shortcomings in conventional care contributed to the trend. In the "integration" phase of the 1990s, struggles to outlaw CAM were abandoned, physicians began learning to work around or administer CAM, and the subjugation of CAM to scientific scrutiny became the primary means of control.<ref> |
|||
{{Cite journal| doi = 10.1525/sp.2005.52.1.38| issn = 0037-7791| volume = 52| issue = 1| pages = |
{{Cite journal| doi = 10.1525/sp.2005.52.1.38| issn = 0037-7791| volume = 52| issue = 1| pages = 38-61| last = Winnick| first = Terri A.| title = From Quackery to “Complementary” Medicine: The American Medical Profession Confronts Alternative Therapies| journal = Social Problems| accessdate = 2013-02-13| date = 2005-02-01|url=http://www.jstor.org/stable/10.1525/sp.2005.52.1.38|jstor=10.1525/sp.2005.52.1.38}}</ref> |
||
===Medical education (20c. to present)=== |
===Medical education (20c. to present)=== |
||
Mainly as a result of reforms following the [[Flexner Report]] of 1910<ref>{{ |
Mainly as a result of reforms following the [[Flexner Report]] of 1910<ref>{{Citation | author=Flexner, Abraham | year=1910 | title=Medical Education in the United States and Canada: A Report to the Carnegie Foundation for the Advancement of Teaching | series=Bulletin No. 4. | publisher=The Carnegie Foundation for the Advancement of Teaching | location=New York City | pages=346 | oclc=9795002 | url=http://www.carnegiefoundation.org/publications/medical-education-united-states-and-canada-bulletin-number-four-flexner-report-0 | accessdate=April 20, 2010 }}</ref> [[medical education]] in established [[medical schools]] in the United States of America has generally not included alternative medicine as a teaching topic. Typically, their teaching is based on current practice and scientific knowledge about: anatomy, physiology, histology, embryology, neuroanatomy, pathology, pharmacology, microbiology and immunology.<ref>'How Becoming a Doctor Works: Medical School Curriculum' |
||
[http://people.howstuffworks.com/becoming-a-doctor9.htm]</ref> Medical schools' teaching includes such topics as doctor-patient communication, ethics, the art of medicine,<ref>Stanford[http://med.stanford.edu/md/curriculum/]</ref> and engaging in complex clinical reasoning (medical decision-making).<ref>[http://medicine.yale.edu/education/curriculum/curriculum/overview/index.aspx Curriculum Overview > Medical Student Education Program | Medical Education | Yale School of Medicine<!-- Bot generated title -->]</ref> Writing in 2002, Snyderman and Weil remarked that by the early twentieth century the Flexner model had helped to create the 20th-century academic health center in which education, research and practice were inseparable. But, while this had much improved medical practice by defining with increasing certainty the [[pathophysiological]] basis of disease, a single-minded focus on the pathophysiological had diverted much of mainstream American medicine from clinical conditions which were not well understood in mechanistic terms and were not effectively treated by conventional therapies.<ref name=Snyderman>{{cite journal |author=Snyderman R, Weil AT |title=Integrative medicine: bringing medicine back to its roots |journal=Archives of Internal Medicine |volume=162 |issue=4 |pages=395–7 |year=2002 |month=February |pmid=11863470 |doi=10.1001/archinte.162.4.395}}</ref> |
[http://people.howstuffworks.com/becoming-a-doctor9.htm]</ref> Medical schools' teaching includes such topics as doctor-patient communication, ethics, the art of medicine,<ref>Stanford[http://med.stanford.edu/md/curriculum/]</ref> and engaging in complex clinical reasoning (medical decision-making).<ref>[http://medicine.yale.edu/education/curriculum/curriculum/overview/index.aspx Curriculum Overview > Medical Student Education Program | Medical Education | Yale School of Medicine<!-- Bot generated title -->]</ref> Writing in 2002, Snyderman and Weil remarked that by the early twentieth century the Flexner model had helped to create the 20th-century academic health center in which education, research and practice were inseparable. But, while this had much improved medical practice by defining with increasing certainty the [[pathophysiological]] basis of disease, a single-minded focus on the pathophysiological had diverted much of mainstream American medicine from clinical conditions which were not well understood in mechanistic terms and were not effectively treated by conventional therapies.<ref name=Snyderman>{{cite journal |author=Snyderman R, Weil AT |title=Integrative medicine: bringing medicine back to its roots |journal=Archives of Internal Medicine |volume=162 |issue=4 |pages=395–7 |year=2002 |month=February |pmid=11863470 |doi=10.1001/archinte.162.4.395}}</ref> |
||
By 2001 some form of CAM training was being offered by most medical schools in USA (at least 75 out of 125).<ref>Berman, B. M (2001-01-20). "Complementary medicine and medical education". BMJ 322 (7279): 121-122. doi:10.1136/bmj.322.7279.121. ISSN 09598138. [http://www.bmj.com.eproxy.ucd.ie/content/322/7279/121]</ref> and, exceptionally, the School of Medicine of the [[University of Maryland, Baltimore]] in the state of Maryland, includes a research institute for integrative medicine (a member entity of the Cochrane Collaboration).<ref>Center for Integrative Medicine of the University of Maryland School of Medicine[http://medschool.umaryland.edu/about.asp],[http://medschool.umaryland.edu/centers.asp], [http://www.compmed.umm.edu/cochrane_about.asp] |
By 2001 some form of CAM training was being offered by most medical schools in USA (at least 75 out of 125).<ref>Berman, B. M (2001-01-20). "Complementary medicine and medical education". BMJ 322 (7279): 121-122. doi:10.1136/bmj.322.7279.121. ISSN 09598138. [http://www.bmj.com.eproxy.ucd.ie/content/322/7279/121]</ref> and, exceptionally, the School of Medicine of the [[University of Maryland, Baltimore]] in the state of Maryland, includes a research institute for integrative medicine (a member entity of the Cochrane Collaboration).<ref>Center for Integrative Medicine of the University of Maryland School of Medicine[http://medschool.umaryland.edu/about.asp],[http://medschool.umaryland.edu/centers.asp], [http://www.compmed.umm.edu/cochrane_about.asp][http://www.compmed.umm.edu/default.asp]</ref> Medical schools are responsible for conferring medical degrees, but a physician typically may not legally practice medicine until licensed by the local government authority. Licensed [[physicians in the United States ]] who have attended one of the established medical schools there have usually graduated Doctor of Medicine (MD).<ref>{{cite web |url=http://www.nlm.nih.gov/medlineplus/ency/article/001936.htm |title=Doctor of medicine profession (MD) |author=Medline Plus |year=2012 |work= |publisher=U.S. National Library of Medicine of National Institutes of Health |accessdate=20 December 2012}}</ref> All states require that applicants for MD licensure be graduates of an approved medical school and complete the United States Medical Licensing Exam (USMLE).<ref> |
||
Doctor of medicine profession[(MDhttp://www.nlm.nih.gov/medlineplus/ency/article/001936.htm]</ref> |
Doctor of medicine profession[(MDhttp://www.nlm.nih.gov/medlineplus/ency/article/001936.htm]</ref> |
||
| Line 53: | Line 52: | ||
===Proponents and opponents=== |
===Proponents and opponents=== |
||
The [[Cochrane Collaboration]] Complementary Medicine Field explains its "Scope and Topics" by giving a broad and general defintion for complementary medicine as including practices and ideas which are outside the domain of conventional medicine in several countries and defined by its users as preventing or treating illness, or promoting health and well being, and which complement mainstream medicine in three ways: by contributing to a common whole, by satisfying a demand not met by conventional practices, and by diversifying the conceptual framework of medicine.<ref name=Cochranedefinition>{{cite web |url=http://www.mrw.interscience.wiley.com/cochrane/clabout/articles/CE000052/frame.html |title=Cochrane Complementary Medicine Field |work=Cochrane COllaboration |accessdate=}}</ref> |
The [[Cochrane Collaboration]] Complementary Medicine Field explains its "Scope and Topics" by giving a broad and general defintion for complementary medicine as including practices and ideas which are outside the domain of conventional medicine in several countries and defined by its users as preventing or treating illness, or promoting health and well being, and which complement mainstream medicine in three ways: by contributing to a common whole, by satisfying a demand not met by conventional practices, and by diversifying the conceptual framework of medicine.<ref name=Cochranedefinition>{{cite web |url=http://www.mrw.interscience.wiley.com/cochrane/clabout/articles/CE000052/frame.html |title=Cochrane Complementary Medicine Field |work=Cochrane COllaboration |accessdate=}}</ref> |
||
[[Edzard Ernst]], a former professor of complementary medicine, characterized the evidence for many alternative techniques as weak, nonexistent, or negative.<ref name=goodbadugly>{{cite web |url=http://www.healthwatch-uk.org/awardwinners/edzardernst.html |title=Complementary medicine: the good the bad and the ugly |work=Edzard Ernst |accessdate=}}</ref> Ernst has concluded that 95% of the alternative treatments he and his team studied, including acupuncture, herbal medicine, homeopathy, and reflexology, are "statistically indistinguishable from placebo treatments", but he also believes there is something that conventional doctors can usefully learn from the chiropractors and homeopath: this is the therapeutic value of the [[placebo effect]], one of the strangest phenomena in medicine.<ref>''[[The Economist]]'', "[http://www.economist.com/node/18710090 Alternative Medicine: Think yourself better]", 21 May 2011, pp. 83–84.[http://www.economist.com/node/18710090?zid=318&ah=ac379c09c1c3fb67e0e8fd1964d5247f].Edzard Ernst, ''Placebo and other Non-specific Effects'' 8th article in ''Healing, Hype, or Harm? |
[[Edzard Ernst]], a former professor of complementary medicine, characterized the evidence for many alternative techniques as weak, nonexistent, or negative.<ref name=goodbadugly>{{cite web |url=http://www.healthwatch-uk.org/awardwinners/edzardernst.html |title=Complementary medicine: the good the bad and the ugly |work=Edzard Ernst |accessdate=}}</ref> Ernst has concluded that 95% of the alternative treatments he and his team studied, including acupuncture, herbal medicine, homeopathy, and reflexology, are "statistically indistinguishable from placebo treatments", but he also believes there is something that conventional doctors can usefully learn from the chiropractors and homeopath: this is the therapeutic value of the [[placebo effect]], one of the strangest phenomena in medicine.<ref>''[[The Economist]]'', "[http://www.economist.com/node/18710090 Alternative Medicine: Think yourself better]", 21 May 2011, pp. 83–84.[http://www.economist.com/node/18710090?zid=318&ah=ac379c09c1c3fb67e0e8fd1964d5247f].Edzard Ernst, ''Placebo and other Non-specific Effects'' 8th article in ''Healing, Hype, or Harm? |
||
| Line 59: | Line 58: | ||
Proponents of an [[Evidence based medicine|evidence-base for medicine]]<ref>J.Belsey and T.Snell ''What is evidence-based medicine?'' 2nd edition, 'Supported by Sanofi-aventis', pubished by Hayward Medical Communications, Hayward Group Ltd, 2009. |
Proponents of an [[Evidence based medicine|evidence-base for medicine]]<ref>J.Belsey and T.Snell ''What is evidence-based medicine?'' 2nd edition, 'Supported by Sanofi-aventis', pubished by Hayward Medical Communications, Hayward Group Ltd, 2009. |
||
[http://www.medicine.ox.ac.uk/bandolier/painres/download/whatis/ebm.pdf]</ref> <ref>BMJ 'Evidence based medicine is the conscientious, explicit, and judicious use of current best evidence in making decisions about the care of individual patients'.[http://www.bmj.com/content/312/7023/71] 'Evidence-Based Medicine systematically searches a wide range of international medical journals applying strict criteria for the validity of research. Experts critically appraise the validity of the most clinically relevant articles and summarize them including commentary on their clinical applicability. EBM also publishes articles relevant to the study and practice of evidence-based medicine. EBM is about integrating individual clinical expertise and the best external evidence. Evidence based medicine, whose philosophical origins extend back to mid-19th century Paris and earlier, remains a hot topic for clinicians, public health practitioners, purchasers, planners, and the public. British centres for evidence based practice have been established or planned in adult medicine, child health, surgery, pathology, pharmacotherapy, nursing, general practice, and dentistry; the Cochrane Collaboration and Britain's Centre for Review and Dissemination in York are providing systematic reviews of the effects of health care'.[http://ebm.bmj.com/]</ref> <ref>Nuffield Trust: 'source of evidence-based research and policy analysis for improving health care in the UK.'[http://www.nuffieldtrust.org.uk/our-work?gclid=CKyP2rWM1LUCFUbKtAodbzEAQQ]</ref> <ref>Research methods & information tools[http://www.isnuffieldtrust.org.uk/our-work/research-methods-information-tools], 'Predictive risk and health care: an overview'[http://www.nuffieldtrust.org.uk/publications/predictive-risk-and-health-care-overview]</ref> such as the [[Cochrane Collaboration]] (founded in 1993 and from 2011 providing input for [[WHO]] resolutions) take a position that ''all'' systematic reviews of treatments, whether "mainstream" or "alternative", ought to be held to the current standards of scientific method.<ref name="UMM">{{cite web |url=http://www.compmed.umm.edu/cochrane.asp |title=Cochrane CAM Field: Integrative Medicine |work= |accessdate=}}</ref> In a study titled ''Development and classification of an operational definition of complementary and alternative medicine for the Cochrane Collaboration'' (2011) it was proposed that indicators that a therapy is accepted include government licensing of practitioners, coverage by [[health insurance]], statements of approval by government agencies, and recommendation as part of a practice guideline; and that if something is currently a standard, accepted therapy, then it is not likely to be widely considered as CAM.<ref>''Development and classification of an operational definition of complementary and alternative medicine for the Cochrane Collaboration'' L. Susan Wieland, Center for Integrative Medicine, University of Maryland School of Medicine, Eric Manheimer, research associate, and Brian M. Berman, founder and director. National Center for Biotechnology Information (NCBI), a division of [[US National Library of Medicine]], [[National Institutes of Health]] |
[http://www.medicine.ox.ac.uk/bandolier/painres/download/whatis/ebm.pdf]</ref> <ref>BMJ 'Evidence based medicine is the conscientious, explicit, and judicious use of current best evidence in making decisions about the care of individual patients'.[http://www.bmj.com/content/312/7023/71] 'Evidence-Based Medicine systematically searches a wide range of international medical journals applying strict criteria for the validity of research. Experts critically appraise the validity of the most clinically relevant articles and summarize them including commentary on their clinical applicability. EBM also publishes articles relevant to the study and practice of evidence-based medicine. EBM is about integrating individual clinical expertise and the best external evidence. Evidence based medicine, whose philosophical origins extend back to mid-19th century Paris and earlier, remains a hot topic for clinicians, public health practitioners, purchasers, planners, and the public. British centres for evidence based practice have been established or planned in adult medicine, child health, surgery, pathology, pharmacotherapy, nursing, general practice, and dentistry; the Cochrane Collaboration and Britain's Centre for Review and Dissemination in York are providing systematic reviews of the effects of health care'.[http://ebm.bmj.com/]</ref> <ref>Nuffield Trust: 'source of evidence-based research and policy analysis for improving health care in the UK.'[http://www.nuffieldtrust.org.uk/our-work?gclid=CKyP2rWM1LUCFUbKtAodbzEAQQ]</ref> <ref>Research methods & information tools[http://www.isnuffieldtrust.org.uk/our-work/research-methods-information-tools], 'Predictive risk and health care: an overview'[http://www.nuffieldtrust.org.uk/publications/predictive-risk-and-health-care-overview]</ref> such as the [[Cochrane Collaboration]] (founded in 1993 and from 2011 providing input for [[WHO]] resolutions) take a position that ''all'' systematic reviews of treatments, whether "mainstream" or "alternative", ought to be held to the current standards of scientific method.<ref name="UMM">{{cite web |url=http://www.compmed.umm.edu/cochrane.asp |title=Cochrane CAM Field: Integrative Medicine |work= |accessdate=}}</ref> In a study titled ''Development and classification of an operational definition of complementary and alternative medicine for the Cochrane Collaboration'' (2011) it was proposed that indicators that a therapy is accepted include government licensing of practitioners, coverage by [[health insurance]], statements of approval by government agencies, and recommendation as part of a practice guideline; and that if something is currently a standard, accepted therapy, then it is not likely to be widely considered as CAM.<ref>''Development and classification of an operational definition of complementary and alternative medicine for the Cochrane Collaboration'' L. Susan Wieland, Center for Integrative Medicine, University of Maryland School of Medicine, Eric Manheimer, research associate, and Brian M. Berman, founder and director. National Center for Biotechnology Information (NCBI), a division of [[US National Library of Medicine]], [[National Institutes of Health]][http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3196853/#BX1]</ref> |
||
In other studies or reports it has been proposed that "alternative medicine" refers to any practice (not included in the degree courses of established medical schools), that is put forward as having the healing effects of [[medicine]], but is not based on [[evidence]] gathered with the [[scientific method]],<ref name=NSF_altmed /> when used independently or in place of medicine based on science (NCCAM, 2005),<ref name=NCCAMwhatiscam/> (NCI at NHI, (2012)<ref name=NationalCancerInstitute>{{cite web| url=http://www.cancer.gov/cancertopics/pdq/cam/cam-cancer-treatment/patient/page2| title=Complementary and Alternative Medicine in Cancer Treatment |accessdate=2012-12-11 |publisher=National Vancer Institute| archiveurl = | archivedate = | deadurl=}}</ref> (Borkan, 2012)<ref name=Borkan>.{{cite journal|last=Borkan|first=Jeffrey|title=Complementary alternative health care in Israel and the western world |journal=Isr J Health Policy Res|year=2012|volume=1|issue=8|pages= |
In other studies or reports it has been proposed that "alternative medicine" refers to any practice (not included in the degree courses of established medical schools), that is put forward as having the healing effects of [[medicine]], but is not based on [[evidence]] gathered with the [[scientific method]],<ref name=NSF_altmed /> when used independently or in place of medicine based on science (NCCAM, 2005),<ref name=NCCAMwhatiscam/> (NCI at NHI, (2012)<ref name=NationalCancerInstitute>{{cite web| url=http://www.cancer.gov/cancertopics/pdq/cam/cam-cancer-treatment/patient/page2| title=Complementary and Alternative Medicine in Cancer Treatment |accessdate=2012-12-11 |publisher=National Vancer Institute| archiveurl = | archivedate = | deadurl=}}</ref> (Borkan, 2012)<ref name=Borkan>.{{cite journal|last=Borkan|first=Jeffrey|title=Complementary alternative health care in Israel and the western world |journal=Isr J Health Policy Res|year=2012|volume=1|issue=8|pages=|doi=10.1186/2045-4015-1-8|pmid=22913745}}</ref> (Kong and others, 2005) <ref name=Kong>{{cite journal |author=Kong SC, Hurlstone DP, Pocock CY, Walkington LA, Farquharson NR, Bramble MG, McAlindon ME, Sanders DS. |title=The Incidence of self-prescribed oral complementary and alternative medicine use by patients with gastrointestinal diseases |journal=J Clin Gastroenterol |volume=39 |issue=2 |pages=138–41 |year=2005 |month= |pmid=15681910 |doi=}}</ref> "'''Complementary medicine'''" refers to use of alternative medicine alongside conventional science based medicine, in the belief that it increases the effectiveness.<ref name=NCCAMwhatiscam/><ref name=NationalCancerInstitute/><ref name=Borkan/> In ''Science and Technology: Public Attitudes and Public Understanding'', chapter 7 of a report ''Science and Technology: Public Attitudes and Public Understanding'', 2002, issued by a United States government agency (The National Science Foundation), it was stated that the term "alternative medicine" was there being used to refer to all treatments that had not been proven effective using scientific methods (NSF of SRS, of NSB, 2002).<ref>{{cite web | quote = alternative medicine refers to all treatments that have not been proven effective using scientific methods | title = Science and Technology: Public Attitudes and Public Understanding Science Fiction and Pseudoscience - Belief in Alternative Medicine | publisher = [[National Science Foundation]] | url = http://www.nsf.gov/statistics/seind02/c7/c7s5.htm }}</ref><ref>Chapter 7, ''Science and Technology: Public Attitudes and Public Understanding''of ''Science and Engineering Indicators 2002'', National Science Board, Science and Engineering Indicators – 2002. Arlington, VA: National Science Foundation, 2002 (NSB-02-1[http://www.nsf.gov/statistics/seind02/c7/c7h.htm]</ref> Many of the claims regarding the safety and efficacy of alternative medicine are controversial. Some alternative treatments have been associated with unexpected side effects, which can be fatal. |
||
Some opponents, focused upon health fraud, misinformation, and quackery as public health problems in the United States, are highly critical of alternative medicine, notably [[Wallace Sampson]] and [[Paul Kurtz]] founders of [[Scientific Review of Alternative Medicine]] and [[Stephen Barrett]], co-founder of [[The National Council Against Health Fraud]] and webmaster of [[Quackwatch]].<ref>Stephen Barret, NCAHF[http://www.ncahf.org/about/mission.html]</ref> That alternative medicine has been on the rise "in countries where Western science and scientific method generally are accepted as the major foundations for healthcare, and 'evidence-based' practice is the dominant paradigm" was described as an "[[enigma]]" in the Medical Journal of Australia.<ref name=RRCAM>The Rise and Rise of Complementary and Alternative Medicine: a Sociological Perspective, Ian D Coulter and Evan M Willis, Medical Journal of Australia, 2004; 180 (11): 587-589</ref> |
Some opponents, focused upon health fraud, misinformation, and quackery as public health problems in the United States, are highly critical of alternative medicine, notably [[Wallace Sampson]] and [[Paul Kurtz]] founders of [[Scientific Review of Alternative Medicine]] and [[Stephen Barrett]], co-founder of [[The National Council Against Health Fraud]] and webmaster of [[Quackwatch]].<ref>Stephen Barret, NCAHF[http://www.ncahf.org/about/mission.html]</ref> That alternative medicine has been on the rise "in countries where Western science and scientific method generally are accepted as the major foundations for healthcare, and 'evidence-based' practice is the dominant paradigm" was described as an "[[enigma]]" in the Medical Journal of Australia.<ref name=RRCAM>The Rise and Rise of Complementary and Alternative Medicine: a Sociological Perspective, Ian D Coulter and Evan M Willis, Medical Journal of Australia, 2004; 180 (11): 587-589</ref> |
||
Grounds for opposing alternative medicine which have been stated are: |
Grounds for opposing alternative medicine which have been stated are: |
||
* |
*that it is usually based on [[religion]], tradition, [[superstition]], belief in [[supernatural]] energies, [[pseudoscience]], [[fallacy|errors in reasoning]], propaganda, or fraud.<ref name=NSF_altmed>[[National Science Foundation]] survey: [http://www.nsf.gov/statistics/seind02/c7/c7s5.htm Science and Technology: Public Attitudes and Public Understanding. Science Fiction and Pseudoscience.]</ref><ref name=ATRAMM>{{cite doi | 10.1111/j.1749-6632.1996.tb23138.x }}</ref><ref name=AMCER>{{cite pmid | 11242572}}</ref><ref name="psycnet.apa.org">Other sources: |
||
* |
*''Nature Medicine'', September 1996, Volume 2 Number 9, p1042 |
||
* |
*''Pseudoscience and the Paranormal'', Hines, Terence, ''American Psychological Association'', [http://psycnet.apa.org/psycinfo/2003-02869-000] |
||
* |
*''The Need for Educational Reform in Teaching about Alternative Therapies'', ''Journal of the Association of Medical Colleges'', March 2001 - Volume 76 - Issue 3 - p 248-250 |
||
* |
*''The Rise and Rise of Complementary and Alternative Medicine: a Sociological Perspective'', Ian D Coulter and Evan M Willis, ''Medical Journal of Australia'', 2004; 180 (11): 587-589 |
||
* |
*''Ignore Growing Patient Interest in Alternative Medicine at Your Peril - MDs Warned'', Heather Kent, ''Canadian Medical Association Journal'', November 15, 1997 vol. 157 no. 10 |
||
* |
*''The Demon-Haunted World: Science as a Candle in the Dark'', [[Carl Sagan]], Random House, ISBN 0-394-53512-X, 1996</ref> |
||
* that alternative therapies typically lack any [[scientific validation]], and their effectiveness is either [[Scientific method|unproved]] or [[Scientific evidence|disproved]].<ref name=ATRAMM /><ref name=IGPIAMAYP>''Ignore Growing Patient Interest in Alternative Medicine at Your Peril — MDs Warned'', Heather Kent, ''Canadian Medical Association Journal'', November 15, 1997 vol. 157 no. 10</ref><ref name=NP>Goldrosen MH, Straus SE. [http://www.nature.com/nri/journal/v4/n11/pdf/nri1486.pdf "Complementary and alternative medicine: assessing the evidence for immunological benefits."] ''Nature Perspectives'', November 2004 vol. 4, pp. 912-921.</ref> |
|||
*that alternative therapies typically lack any [[scientific validation]], and their effectiveness is either [[Scientific method|unproved]] or [[Scientific evidence|disproved]].<ref name=ATRAMM /><ref name=IGPIAMAYP>''Ignore Growing Patient Interest in Alternative Medicine at Your Peril - MDs Warned'', Heather Kent, ''Canadian Medical Association Journal'', November 15, 1997 vol. 157 no. 10</ref><ref name=NP>Goldrosen MH, Straus SE. [http://www.nature.com/nri/journal/v4/n11/pdf/nri1486.pdf "Complementary and alternative medicine: assessing the evidence for immunological benefits."] ''Nature Perspectives'', November 2004 vol. 4, pp. 912-921.</ref> {{dubious|date=January 2013}} |
|||
* that the treatments are those that are not part of the conventional healthcare system.<ref name=NCCAMwhatiscam>{{cite web| url=http://nccam.nih.gov/health/whatiscam/| title=What is Complementary and Alternative Medicine (CAM)? |accessdate=2006-07-11 |publisher=[[NCCAM|National Center for Complementary and Alternative Medicine]]| archiveurl = http://www.webcitation.org/5C1oRX8Qq | archivedate = 2005-12-08| deadurl=no}}</ref><ref name=Zollman>{{cite journal |author= Zollman C, Vickers A|title= ABC of complementary medicine What is complementary medicine? |journal=British Medical Journal |volume=319 |issue=693 |pages= 693|year=1999 |month= |pmid= |doi=10.1136/bmj.319.7211.693 |url=/}}</ref><ref name=IOM/><ref name=WHO>{{cite web |url=http://www.who.int/medicines/areas/traditional/definitions/en/index.html |title=Traditional Medicine: Definitions |publisher=[[World Health Organization]] |pages= |year=2000 |quote= |accessdate=2012-11-11}}</ref> |
|||
* that research on alternative medicine is frequently of low quality and methodologically flawed.<ref name=IOM2005/> |
|||
*that the treatments are those that are not part of the conventional, science-based healthcare system.<ref name=NCCAMwhatiscam>{{cite web| url=http://nccam.nih.gov/health/whatiscam/| title=What is Complementary and Alternative Medicine (CAM)? |accessdate=2006-07-11 |publisher=[[NCCAM|National Center for Complementary and Alternative Medicine]]| archiveurl = http://www.webcitation.org/5C1oRX8Qq | archivedate = 2005-12-08| deadurl=no}}</ref><ref name=Zollman>{{cite journal |author= Zollman C, Vickers A|title= ABC of complementary medicine What is complementary medicine? |journal=British Medical Journal |volume=319 |issue=693 |pages= 693|year=1999 |month= |pmid= |doi=10.1136/bmj.319.7211.693 |url=/}}</ref><ref name=IOM/><ref name=WHO>{{cite web |url=http://www.who.int/medicines/areas/traditional/definitions/en/index.html |title=Traditional Medicine: Definitions |publisher=[[World Health Organization]] |pages= |year=2000 |quote= |accessdate=2012-11-11}}</ref> |
|||
* that where alternative treatments are used in place of conventional science-based medicine, even with the very safest alternative medicines, failure to use or delay in using conventional science-based medicine has resulted in deaths.<ref name='Lilienfeld_2002'/><ref name=ineffecive/> |
|||
*that research on alternative medicine is frequently of low quality and methodologically flawed.<ref name=IOM2005/> |
|||
* that where alternative treatments are used in place of conventional science-based medicine, even with the very safest alternative medicines, failure to use or delay in using conventional science-based medicine has resulted in deaths.<ref name='Lilienfeld_2002'/><ref name=ineffecive/> |
|||
Critics say the expression is deceptive because it implies there is an effective alternative to science-based medicine, and that ''complementary'' is deceptive because the word implies that the treatment increases the effectiveness of (complements) science-based medicine, while alternative medicines which have been tested nearly always have no measurable positive effect compared to a [[placebo]].<ref name=ATRAMM/><ref>Carroll RT. [http://www.skepdic.com/compmed.html "complementary medicine"] at ''The Skeptic's Dictionary''</ref><ref name=APNEJM>Acupuncture Pseudoscience in the New England Journal of Medicine, Science Based Medicine, Steven Novella, [http://www.sciencebasedmedicine.org/?p=6391 Science-Based Medicine » Acupuncture Pseudoscience in the New England Journal of Medicine]</ref><ref name="Credulityabout">Credulity about acupuncture infiltrates the New England Journal of Medicine, Science Based Medicine, David Gorski, [http://www.sciencebasedmedicine.org/?p=6381 Science-Based Medicine » Credulity about acupuncture infiltrates the New England Journal of Medicine]</ref> Despite such objections, some fields of alternative practice are regulated in a manner similar to that governing evidence-based medicine, and others have no regulation. |
Critics say the expression is deceptive because it implies there is an effective alternative to science-based medicine, and that ''complementary'' is deceptive because the word implies that the treatment increases the effectiveness of (complements) science-based medicine, while alternative medicines which have been tested nearly always have no measurable positive effect compared to a [[placebo]].<ref name=ATRAMM/><ref>Carroll RT. [http://www.skepdic.com/compmed.html "complementary medicine"] at ''The Skeptic's Dictionary''</ref><ref name=APNEJM>Acupuncture Pseudoscience in the New England Journal of Medicine, Science Based Medicine, Steven Novella, [http://www.sciencebasedmedicine.org/?p=6391 Science-Based Medicine » Acupuncture Pseudoscience in the New England Journal of Medicine]</ref><ref name="Credulityabout">Credulity about acupuncture infiltrates the New England Journal of Medicine, Science Based Medicine, David Gorski, [http://www.sciencebasedmedicine.org/?p=6381 Science-Based Medicine » Credulity about acupuncture infiltrates the New England Journal of Medicine]</ref> Despite such objections, some fields of alternative practice are regulated in a manner similar to that governing evidence-based medicine, and others have no regulation. |
||
Alternative medicine practices and beliefs are diverse in their foundations and methodologies, and typically make use of preparations and dosages other than such as are included in the [[Pharmacopeia]] recognised by established medical schools. Methods may incorporate or base themselves on [[traditional medicine]], [[Home remedy|folk knowledge]], spiritual beliefs, ignorance or misunderstanding of scientific principles, errors in reasoning, or newly conceived approaches claiming to heal.<ref name=ATRAMM/><ref name=AMCER/><ref>{{cite book |author=Acharya, Deepak and Shrivastava Anshu |year=2008 |title=Indigenous Herbal Medicines: Tribal Formulations and Traditional Herbal Practices |publisher=Aavishkar Publishers Distributor |location=[[Jaipur]] |isbn=978-81-7910-252-7 |page=440}}</ref> African, Caribbean, Pacific Island, Native American, and other regional cultures have traditional medical systems as diverse as their diversity of cultures.<ref name=NCCAMwhatiscam/> |
Alternative medicine practices and beliefs are diverse in their foundations and methodologies, and typically make use of preparations and dosages other than such as are included in the [[Pharmacopeia]] recognised by established medical schools. Methods may incorporate or base themselves on [[traditional medicine]], [[Home remedy|folk knowledge]], spiritual beliefs, ignorance or misunderstanding of scientific principles, errors in reasoning, or newly conceived approaches claiming to heal.<ref name=ATRAMM/><ref name=AMCER/><ref>{{cite book |author=Acharya, Deepak and Shrivastava Anshu |year=2008 |title=Indigenous Herbal Medicines: Tribal Formulations and Traditional Herbal Practices |publisher=Aavishkar Publishers Distributor |location=[[Jaipur]] |isbn=978-81-7910-252-7 |page=440}}</ref> African, Caribbean, Pacific Island, Native American, and other regional cultures have traditional medical systems as diverse as their diversity of cultures.<ref name=NCCAMwhatiscam/> A short but not comprehensive list is: |
||
*[[Prayer]] to heal is the most common alternative medicine in many western countries, and [[faith healing]] is a part of many religions. |
|||
*Some believe that [[meditation]] affects health.{{citation needed|date=February 2013}} |
|||
*[[Yoga as exercise or alternative medicine|Yoga]] as a healing practice involves stretching, exercise and meditation related to the [[Hinduism|Hindu]] religion, and makes claims to healing in the spiritual realm.{{citation needed|date=February 2013}} |
|||
*[[Traditional Chinese medicine]] and the [[Ayurvedic medicine]] of India are complex systems developed over thousands of years, both based on regional supernatural belief systems and traditional use of herbs and other substances. {{citation needed|date=February 2013}} |
|||
*[[Acupuncture]] is a part of Traditional Chinese medicine in which needles are inserted in the body to alter the flow of supernatural energy believed to propel the blood and influence health.{{citation needed|date=February 2013}} |
|||
*[[Chiropractic]] manipulation of the spine was developed in the United States, and involves manipulating the spine to influence supernatural energies believed to cause disease. {{citation needed|date=February 2013}} |
|||
*[[Homeopathy]] was developed in Europe before the existence of science of chemistry, which has subsequently proven the premises of homeopathy to be false.{{citation needed|date=February 2013}} |
|||
*Magnets and light are used in therapies based on a misunderstanding of [[electricity]] and [[magnetism]]. {{citation needed|date=February 2013}} |
|||
*Dietary supplements that are unproven by science are considered alternative medicines.{{citation needed|date=February 2013}} |
|||
==Examples and classes of alternative medicines== |
==Examples and classes of alternative medicines == |
||
{{Further2|[[List of branches of alternative medicine]]}} |
{{Further2|[[List of branches of alternative medicine]]}} |
||
[[File:Botanica.jpg|thumb|right|150px|A [[Botanica]] of traditional Hispanic medicines.]] |
[[File:Botanica.jpg|thumb|right|150px|A [[Botanica]] of traditional Hispanic medicines.]] |
||
| Line 96: | Line 108: | ||
Alternative medical systems are complete health systems with their own approaches to diagnosis and treatment that differ from the conventional biomedical approach to health. Some are cultural systems such as [[Ayurveda]] and [[Traditional Chinese Medicine]], while others, such as [[Homeopathy]] and [[Naturopathy]] are relatively recent and were developed in the West.<ref name="NP"/> |
Alternative medical systems are complete health systems with their own approaches to diagnosis and treatment that differ from the conventional biomedical approach to health. Some are cultural systems such as [[Ayurveda]] and [[Traditional Chinese Medicine]], while others, such as [[Homeopathy]] and [[Naturopathy]] are relatively recent and were developed in the West.<ref name="NP"/> |
||
Writing as a historian Matthew Ramsey has asked whether some counter-hegemonic medicines are better understood as manifestations of more general developments in the larger society, or as the product of a coherent alternative world view.<ref |
Writing as a historian Matthew Ramsey has asked whether some counter-hegemonic medicines are better understood as manifestations of more general developments in the larger society, or as the product of a coherent alternative world view.<ref>Matthew Ramsey, Vanderbilt University, Nashville, TN ''Alternative medicine in modern France'' Cambridge Journals, Med Hist. 1999 July; 43(3): 286–322.[http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1044147/pdf/medhist00018-0010.pdf]</ref> |
||
====Ayurvedic medicine==== |
====Ayurvedic medicine==== |
||
[[Ayurvedic medicine]] is a traditional medicine of India and has strong links with [[Buddhism]] and [[Hinduism]]. It is based on the belief that health is controlled by 3 "humours" with disease caused by an imbalance of these "humours". The basis of treatment has some similarities with "Western medicine". Rememdies are mainly plant based with some use of animal materials. <ref>The Roots of Ayurveda: Selections from Sanskrit Medical Writings, D. Wujastyk, p xviii, 2003, ISBN 0-14-044824-1</ref> Safety concerns have been raised about Ayurveda, with two U.S. studies finding about 20 percent of Ayurvedic Indian-manufactured [[patent medicine]]s contained toxic levels of heavy metals such as [[lead]], [[Mercury (element)|mercury]] and [[arsenic]]. Other concerns include the use of herbs containing toxic compounds and the lack of quality control in Ayurvedic facilities.<ref name="Saper2008">{{cite journal |last=Saper|first=R. B. |title=Lead, Mercury, and Arsenic in US- and Indian-manufactured ayurvedic Medicines Sold via the Internet |journal=Journal of the American Medical Association |volume=300 |issue=8 |pages=915–923 |year=2008 |pmid=18728265 |doi=10.1001/jama.300.8.915 |pmc=2755247 |author2=Phillips, R. S. |last3=Sehgal |first3=A. |display-authors=2 |last4=Khouri |first4=N. |last5=Davis |first5=R. B. |last6=Paquin |first6=J. |last7=Thuppil |first7=V. |last8=Kales |first8=S. N.}}</ref><ref name="Valiathan06">{{cite journal|last=Valiathan|first=M. S.|title=Ayurveda: Putting the House in Order|journal=Current Science|volume=90|issue=1|pages=5–6|year=2006|publisher=[[Indian Academy of Sciences]]|url=http://www.ias.ac.in/currsci/jan102006/contents.htm}}</ref> |
[[Ayurvedic medicine]] is a traditional medicine of India and has strong links with [[Buddhism]] and [[Hinduism]]. It is based on the belief that health is controlled by 3 "humours" with disease caused by an imbalance of these "humours". The basis of treatment has some similarities with "Western medicine". Rememdies are mainly plant based with some use of animal materials. <ref>The Roots of Ayurveda: Selections from Sanskrit Medical Writings, D. Wujastyk, p xviii, 2003, ISBN 0-14-044824-1</ref> Safety concerns have been raised about Ayurveda, with two U.S. studies finding about 20 percent of Ayurvedic Indian-manufactured [[patent medicine]]s contained toxic levels of heavy metals such as [[lead]], [[Mercury (element)|mercury]] and [[arsenic]]. Other concerns include the use of herbs containing toxic compounds and the lack of quality control in Ayurvedic facilities.<ref name="Saper2008">{{cite journal |last=Saper|first=R. B. |title=Lead, Mercury, and Arsenic in US- and Indian-manufactured ayurvedic Medicines Sold via the Internet |journal=Journal of the American Medical Association |volume=300 |issue=8 |pages=915–923 |year=2008 |pmid=18728265 |doi=10.1001/jama.300.8.915 |pmc=2755247 |author2=Phillips, R. S. |last3=Sehgal |first3=A. |display-authors=2 |last4=Khouri |first4=N. |last5=Davis |first5=R. B. |last6=Paquin |first6=J. |last7=Thuppil |first7=V. |last8=Kales |first8=S. N.}}</ref><ref name="Valiathan06">{{cite journal|last=Valiathan|first=M. S.|title=Ayurveda: Putting the House in Order|journal=Current Science|volume=90|issue=1|pages=5–6|year=2006|publisher=[[Indian Academy of Sciences]]|url=http://www.ias.ac.in/currsci/jan102006/contents.htm}}</ref> |
||
====Traditional Chinese Medicine==== |
====Traditional Chinese Medicine==== |
||
[[Traditional Chinese Medicine]] is based on a concept of "spirit" called [[qi]],<ref>{{cite book|last= Ho |first= Peng Yoke| year=2000|month=Oct |title= Li, Qi, and Shu: An Introduction to Science and Civilization in China |publisher= Dover Publications |isbn=0-486-41445-0}}</ref> considerations of [[Chinese Astrology]] as in acupuncture,<ref name=CLHRAM>Celestial lancets: a history and rationale of acupuncture and moxa, Needham, J; Lu GD, 2002, Routledge, ISBN 0-7007-1458-8</ref> traditional use of herbs and other substances found in China, and a belief that a map of the body is contained on the tongue, which reflects changes in the body.<ref>Tongue Diagnosis in Chinese Medicine, G Cia, 1995, Eastland Press. ISBN 0-939616-19-X.</ref> |
[[Traditional Chinese Medicine]] is based on a concept of "spirit" called [[qi]],<ref>{{cite book|last= Ho |first= Peng Yoke| year=2000|month=Oct |title= Li, Qi, and Shu: An Introduction to Science and Civilization in China |publisher= Dover Publications |isbn=0-486-41445-0}}</ref> considerations of [[Chinese Astrology]] as in acupuncture,<ref name=CLHRAM>Celestial lancets: a history and rationale of acupuncture and moxa, Needham, J; Lu GD, 2002, Routledge, ISBN 0-7007-1458-8</ref> traditional use of herbs and other substances found in China, and a belief that a map of the body is contained on the tongue, which reflects changes in the body.<ref>Tongue Diagnosis in Chinese Medicine, G Cia, 1995, Eastland Press. ISBN 0-939616-19-X.</ref> |
||
====Homeopathy==== |
====Homeopathy==== |
||
[[Homeopathy]] is based on the belief that a disease can be cured by a very low dose of substance that creates similar symptoms in a healthy person. These ideas are known as 'like cures like' and the 'law of the minimum dose'<ref name="Hahnemann">{{cite book | title=The Homœopathic Medical Doctrine, or "Organon of the Healing Art" | publisher=W.F. Wakeman | author=Hahnemann, Samuel | authorlink=Samuel Hahnemann | year=1833 | location=Dublin | pages=[http://books.google.com/books?id=EnEFAAAAQAAJ&pg=PR3 iii], [http://books.google.com/books?id=EnEFAAAAQAAJ&pg=PA48 48–49] | quote=Observation, reflection, and experience have unfolded to me that the best and true method of cure is founded on the principle, ''[[similia similibus curentur]].'' To cure in a mild, prompt, safe, and durable manner, it is necessary to choose in each case a medicine that will excite an affection similar (''{{lang|el|ὅμοιος πάθος}}'') to that against which it is employed. | others=Charles H. Devrient, Esq.}}</ref> This conflicts with fundamental concepts of physics and chemistry and there is no good evidence from reviews of research to support its use.<ref name="pmid12492603">{{Cite journal |last1=Ernst |first1=E. |title=A systematic review of systematic reviews of homeopathy |journal=British Journal of Clinical Pharmacology |volume=54 |issue=6 |pages=577–82 |year=2002 |pmid=12492603 |pmc=1874503 |doi=10.1046/j.1365-2125.2002.01699.x |postscript=<!-- Bot inserted parameter. Either remove it; or change its value to "." for the cite to end in a ".", as necessary. -->{{inconsistent citations}}}}</ref><ref name=inquiry_cfm>UK Parliamentary Committee Science and Technology Committee - [http://www.parliament.uk/business/committees/committees-a-z/commons-select/science-and-technology-committee/inquiries/homeopathy-/ "Evidence Check 2: Homeopathy"]</ref><ref name="shang">{{Cite journal |last1=Shang |first1=Aijing |last2=Huwiler-Müntener |first2=Karin |last3=Nartey |first3=Linda |last4=Jüni |first4=Peter |last5=Dörig |first5=Stephan |last6=Sterne |first6=Jonathan AC |last7=Pewsner |first7=Daniel |last8=Egger |first8=Matthias |title=Are the clinical effects of homoeopathy placebo effects? Comparative study of placebo-controlled trials of homoeopathy and allopathy |journal=The Lancet |volume=366 |pages=726–732 |year=2005 |doi=10.1016/S0140-6736(05)67177-2 |pmid=16125589 |issue=9487 |postscript=<!-- Bot inserted parameter. Either remove it; or change its value to "." for the cite to end in a ".", as necessary. -->{{inconsistent citations}}}}</ref><ref name="nih overview">http://nccam.nih.gov/health/homeopathy "Homeopathy: An Introduction" a NCAAM webpage</ref> |
|||
Homeopathy is based on the belief that a disease can be cured by a very low dose of substance that creates similar symptoms in a healthy person. These ideas are known as 'like cures like' and the 'law of the minimum dose'<ref name="Hahnemann">{{cite book | title=The Homœopathic Medical Doctrine, or "Organon of the Healing Art" | publisher=W.F. Wakeman | author=Hahnemann, Samuel | authorlink=Samuel Hahnemann | year=1833 | location=Dublin | pages=[http://books.google.com/books?id=EnEFAAAAQAAJ&pg=PR3 iii], [http://books.google.com/books?id=EnEFAAAAQAAJ&pg=PA48 48–49] | quote=Observation, reflection, and experience have unfolded to me that the best and true method of cure is founded on the principle, ''[[similia similibus curentur]].'' To cure in a mild, prompt, safe, and durable manner, it is necessary to choose in each case a medicine that will excite an affection similar (''{{lang|el|ὅμοιος πάθος}}'') to that against which it is employed. | translator=Charles H. Devrient, Esq.}}</ref> This conflicts with fundamental concepts of physics and chemistry and there is no good evidence from reviews of research to support its use.<ref name="pmid12492603">{{Citation |last1=Ernst |first1=E. |title=A systematic review of systematic reviews of homeopathy |journal=British Journal of Clinical Pharmacology |volume=54 |issue=6 |pages=577–82 |year=2002 |pmid=12492603 |pmc=1874503 |doi=10.1046/j.1365-2125.2002.01699.x}}</ref><ref name=inquiry_cfm>UK Parliamentary Committee Science and Technology Committee - [http://www.parliament.uk/business/committees/committees-a-z/commons-select/science-and-technology-committee/inquiries/homeopathy-/ "Evidence Check 2: Homeopathy"]</ref><ref name="shang">{{Citation |last1=Shang |first1=Aijing |last2=Huwiler-Müntener |first2=Karin |last3=Nartey |first3=Linda |last4=Jüni |first4=Peter |last5=Dörig |first5=Stephan |last6=Sterne |first6=Jonathan AC |last7=Pewsner |first7=Daniel |last8=Egger |first8=Matthias |title=Are the clinical effects of homoeopathy placebo effects? Comparative study of placebo-controlled trials of homoeopathy and allopathy |journal=The Lancet |volume=366 |pages=726–732 |year=2005 |doi=10.1016/S0140-6736(05)67177-2 |pmid=16125589 |issue=9487}}</ref><ref name="nih overview">http://nccam.nih.gov/health/homeopathy "Homeopathy: An Introduction" a NCAAM webpage</ref> |
|||
The prevailing point of view among physicians practising conventional medicine is that homeopathy is considered to be [[quackery]].<ref name="pmid17719708">{{ |
The prevailing point of view among physicians practising conventional medicine is that homeopathy is considered to be [[quackery]].<ref name="pmid17719708">{{Citation |last1=Wahlberg |first1=A |title=A quackery with a difference—New medical pluralism and the problem of ‘dangerous practitioners’ in the United Kingdom |journal=Social Science & Medicine |volume=65 |pages=2307–16 |year=2007 |doi=10.1016/j.socscimed.2007.07.024 |pmid=17719708 |issue=11}}</ref> |
||
====Naturopathy==== |
====Naturopathy==== |
||
Naturopathy is based on a belief in [[vitalism]], which posits that a special energy called vital energy or vital force guides bodily processes such as [[metabolism]], reproduction, growth, and adaptation.<ref>Sarris, J., and Wardle, J. 2010. Clinical naturopathy: an evidence-based guide to practice. Elsevier Australia. Chatswood, NSW.</ref> Naturopathy favors a [[holistic health|holistic]] approach with non-invasive treatment and, similar to conventional medicine, encourages minimal use of [[surgery]] and [[Medication|drugs]]. |
|||
Naturopathy is based on a belief in [[vitalism]], which posits that a special energy called vital energy or vital force guides bodily processes such as [[metabolism]], reproduction, growth, and adaptation.<ref>Sarris, J., and Wardle, J. 2010. Clinical naturopathy: an evidence-based guide to practice. Elsevier Australia. Chatswood, NSW.</ref> Naturopathy favors a [[holistic health|holistic]] approach with non-invasive treatment and, similar to conventional medicine, encourages minimal use of [[surgery]] and [[Medication|drugs]]. |
|||
The term "naturopathy" is derived from Greek and Latin, and literally translates as "nature disease".<ref name=NCCAM> |
The term "naturopathy" is derived from Greek and Latin, and literally translates as "nature disease".<ref name=NCCAM> |
||
| Line 119: | Line 136: | ||
| format =PDF |
| format =PDF |
||
| accessdate =20 Nov 10 }} |
| accessdate =20 Nov 10 }} |
||
</ref> Modern naturopathy grew out of the Natural Cure movement of Europe.<ref name=pmid1139856>{{cite journal |pmc=1139856 |title=Nineteenth-century American health reformers and the early nature cure movement in Britain |author=Brown PS |journal=Medical History |volume=32 |pages=174–194 |pmid=3287059 |issue=2 |date= April 1, 1988 |
</ref> Modern naturopathy grew out of the Natural Cure movement of Europe.<ref name=pmid1139856>{{cite journal |pmc=1139856 |title=Nineteenth-century American health reformers and the early nature cure movement in Britain |author=Brown PS |journal=Medical History |volume=32 |pages=174–194 |pmid=3287059 |issue=2 |date= April 1, 1988 }}</ref><ref name=N-UK-hist>{{Cite book |author=Langley, Stephen |chapter=History of Naturopathy|title=Excerpt from The Naturopathy Workbook|publisher=College of Natural Medicine (CNM)|location=UK |url=http://www.naturopathy-uk.com/blog/2007/11/28/history-of-naturopathy/ |year=2007 |postscript=<!-- Bot inserted parameter. Either remove it; or change its value to "." for the cite to end in a ".", as necessary. -->{{inconsistent citations}}}}</ref> The term was coined in 1895 by John Scheel and popularized by [[Benedict Lust]],<ref name=ama_1997>{{cite web | url =http://www.ama-assn.org/ama/no-index/about-ama/13638.shtml | title = Report 12 of the Council on Scientific Affairs (A-97) | year = 1997 | publisher = [[American Medical Association]] |accessdate= |doi= |pmid= }}</ref> the "father of U.S. naturopathy".<ref name=Baer2001>{{Cite journal | last = Baer |first =H. A. | year = 2001 | title = The sociopolitical status of U.S. naturopathy at the dawn of the 21st century | journal = Medical Anthropology Quarterly | pmid = 11693035 | volume = 15 | issue = 3 | pages = 329–346| doi = 10.1525/maq.2001.15.3.329 }}</ref> Beginning in the 1970s, there was a revival of interest in the United States and Canada in conjunction with the [[holistic health]] movement.<ref name=Baer2001/><ref name=Gale_Frey> |
||
{{Cite web |
{{Cite web |
||
| last =Frey |
| last =Frey |
||
| Line 138: | Line 155: | ||
[[File:Chiropractic spinal adjustment.jpg|thumb|right|150px|[[Chiropractic]] was developed in the US in the belief that manipulation of the spine affects a supernatural [[vitalism|vital energy]] that influences health and disease.]] |
[[File:Chiropractic spinal adjustment.jpg|thumb|right|150px|[[Chiropractic]] was developed in the US in the belief that manipulation of the spine affects a supernatural [[vitalism|vital energy]] that influences health and disease.]] |
||
[[Energy (spirituality)#Biofields|Biofield]] therapies are intended to influence energy fields that, it is purported, surround and penetrate the body.<ref name=NCCAMwhatiscam/> Writers such as [[Carl Sagan]] (1934-1996), noted astrophysicist, advocate of skeptical thinking ([[Scientific skepticism]]) and author of ''[[The Demon-Haunted World]]: Science as a Candle in the Dark'' (1996), have described the lack of empirical evidence to support the existence of the putative energy fields on which these therapies are predicated.<ref>Demon Haunted World, Carl Sagan</ref> |
[[Energy (spirituality)#Biofields|Biofield]] therapies are intended to influence energy fields that, it is purported, surround and penetrate the body.<ref name=NCCAMwhatiscam/> Writers such as [[Carl Sagan]] (1934-1996), noted astrophysicist, advocate of skeptical thinking ([[Scientific skepticism]]) and author of ''[[The Demon-Haunted World]]: Science as a Candle in the Dark'' (1996), have described the lack of empirical evidence to support the existence of the putative energy fields on which these therapies are predicated.<ref>Demon Haunted World, Carl Sagan</ref> |
||
[[Acupuncture]] is a component of Traditional Chinese Medicine. In acupuncture, it is believed that a supernatural energy called [[qi]] flows through the universe and through the body, and helps propel the blood, blockage of which leads to disease.<ref name=CLHRAM/> It is believed that insertion of needles at various parts of the body determined by astrological calculations can restore balance to the blocked flows, and thereby cure disease.<ref name=CLHRAM/> |
[[Acupuncture]] is a component of Traditional Chinese Medicine. In acupuncture, it is believed that a supernatural energy called [[qi]] flows through the universe and through the body, and helps propel the blood, blockage of which leads to disease.<ref name=CLHRAM/> It is believed that insertion of needles at various parts of the body determined by astrological calculations can restore balance to the blocked flows, and thereby cure disease.<ref name=CLHRAM/> |
||
Chiropractic was developed in the belief that manipulating the spine affects the flow of a supernatural [[vital energy]] and thereby affects health and disease. |
Chiropractic was developed in the belief that manipulating the spine affects the flow of a supernatural [[vital energy]] and thereby affects health and disease. |
||
In the western version of Japanese [[Reiki]], the palms are placed on the patient near [[Chakras]], believed to be centers of supernatural energies, in a belief that the supernatural energies can transferred through the palms of the practitioner, to heal the patient. |
In the western version of Japanese [[Reiki]], the palms are placed on the patient near [[Chakras]], believed to be centers of supernatural energies, in a belief that the supernatural energies can transferred through the palms of the practitioner, to heal the patient. |
||
====Electromagnetic Fields==== |
====Electromagnetic Fields==== |
||
| Line 150: | Line 167: | ||
===Mind Body Therapies=== |
===Mind Body Therapies=== |
||
Mind–body therapies attempt to use the mind to affect bodily symptoms and functions; examples include yoga, spirituality and relaxation. |
Mind–body therapies attempt to use the mind to affect bodily symptoms and functions; examples include yoga, spirituality and relaxation. |
||
[[Mind-body medicine]] takes a holistic approach to health that explores the interconnection between the mind, body, and spirit. It works under the premise that the mind can affect "bodily functions and symptoms".<ref name=NCCAMwhatiscam/> Mind body medicines includes healing claims made in [[Yoga as exercise or alternative medicine|yoga]], [[meditation]], [[deep-breathing exercises]], [[guided imagery]], [[hypnotherapy]], [[progressive relaxation]], [[qi gong]], and [[tai chi]].<ref name=NCCAMwhatiscam/> |
[[Mind-body medicine]] takes a holistic approach to health that explores the interconnection between the mind, body, and spirit. It works under the premise that the mind can affect "bodily functions and symptoms".<ref name=NCCAMwhatiscam/> Mind body medicines includes healing claims made in [[Yoga as exercise or alternative medicine|yoga]], [[meditation]], [[deep-breathing exercises]], [[guided imagery]], [[hypnotherapy]], [[progressive relaxation]], [[qi gong]], and [[tai chi]].<ref name=NCCAMwhatiscam/> |
||
| Line 156: | Line 173: | ||
Yoga, a method of traditional stretches, excercises, and meditations in [[Hinduism]], may also be classified as an energy medicine insofar as its healing effects are believed by to be due to a healing "life energy" that is absorbed into the body through the breath, and is thereby believed to treat a wide variety of illnesses and complaints.<ref>Psychophysiologic Effects of Hatha Yoga on Musculoskeletal and Cardiopulmonary Function: A Literature Review, The Journal of Alternative and Complementary Medicine, J. A. Raub, (2002), 8(6): 797-812. doi:10.1089/10755530260511810.</ref> |
Yoga, a method of traditional stretches, excercises, and meditations in [[Hinduism]], may also be classified as an energy medicine insofar as its healing effects are believed by to be due to a healing "life energy" that is absorbed into the body through the breath, and is thereby believed to treat a wide variety of illnesses and complaints.<ref>Psychophysiologic Effects of Hatha Yoga on Musculoskeletal and Cardiopulmonary Function: A Literature Review, The Journal of Alternative and Complementary Medicine, J. A. Raub, (2002), 8(6): 797-812. doi:10.1089/10755530260511810.</ref> |
||
[[File:Fallerjfa.JPG|thumb|right|150px|Christian priest [[Faith healer]] laying hands on sick girl in belief in divine healing.]] |
[[File:Fallerjfa.JPG|thumb|right|150px|Christian priest [[Faith healer]] laying hands on sick girl in belief in divine healing.]] |
||
Religion based healing practices, such as use of [[prayer]] and the laying of hands in [[Christian]] [[faith healing]], rely on belief in divine intervention for healing. |
Religion based healing practices, such as use of [[prayer]] and the laying of hands in [[Christian]] [[faith healing]], rely on belief in divine intervention for healing. |
||
===Herbs, Diet and Vitamins=== |
|||
===Herbal and other nutritional supplementation=== |
|||
Biological approaches include the use of herbal medicines, special diets or very high doses of vitamins. |
Biological approaches include the use of herbal medicines, special diets or very high doses of vitamins. |
||
Substance based practices use substances found in nature such as herbs, foods, non-vitamin supplments and megavitmins, and minerals, and includes traditional herbal remedies with herbs specific to regions in which the cultural practices arose.<ref name=NCCAMwhatiscam/> "Herbal" remedies in this case, may include use of nonherbal toxic chemicals from a nonbiological sources, such as use of the poison [[lead]] in Traditional Chinese Medicine.<ref name=NIHNGS>According to a New Government Survey, 38 Percent of Adults and 12 Percent of Children Use Complementary and Alternative Medicine, NIH, [http://nccam.nih.gov/news/2008/121008.htm]</ref> Nonvitamin supplements include [[fish oil]], [[Omega-3 fatty acid]], [[glucosamine]], [[echinacea]], [[flaxseed oil]] or pills, and [[ginseng]], when used under a claim to have healing effects.<ref name=NIHNGS/> |
|||
===Body manipulation=== |
===Body manipulation=== |
||
Body-based therapies such as massage, chiropractic and [[osteopathy]] use movement and physical manipulation of joints and muscles. |
|||
Manipulative and body-based practices focus primarily on the structures and systems of the body, including the bones and joints, soft tissues, and circulatory and lymphatic systems. <ref>{{cite web|title=http://nccam.nih.gov/health/whatiscam|url=http://nccam.nih.gov/health/whatiscam|publisher=NCCAM/NIH|accessdate=2 March 2013}}</ref>Two commonly used therapies fall within this category: |
|||
*Spinal manipulative therapy is practiced by health care professionals such as chiropractors, osteopathic physicians, naturopathic physicians, physical therapists, and some medical doctors. Practitioners perform spinal manipulation by using their hands or a device to apply a controlled force to a joint of the spine. The amount of force applied depends on the form of manipulation used. The goal of the treatment is to relieve pain and improve physical functioning. |
|||
Manipulative and body-based practices feature manipulation or movement of body parts, such as is done in [[chiropractic]] manipulation. |
|||
*Massage therapy encompasses many different techniques. In general, therapists press, rub, and otherwise manipulate the muscles and other soft tissues of the body. People use massage for a variety of health-related purposes, including to relieve pain, rehabilitate sports injuries, reduce stress, increase relaxation, address anxiety and depression, and aid general well-being. <ref>{{cite web|title=http://nccam.nih.gov/health/whatiscam|url=http://nccam.nih.gov/health/whatiscam|publisher=NCCAM/NIH|accessdate=2 March 2013}}</ref> |
|||
==Criticism== |
==Criticism== |
||
CAM, and use of the term "alternative medicine", have been criticised, mainly in the USA, on various grounds and for various reasons in the name of consumers, physicians and research scientists, in medical journals or elsewhere. |
CAM, and use of the term "alternative medicine", have been criticised, mainly in the USA, on various grounds and for various reasons in the name of consumers, physicians and research scientists, in medical journals or elsewhere. Some of the criticism makes assertions about misleading terminology or makes adverse inferences about motivation, some is on scientific grounds or errors of reasoning, or about taking resources from real medical research, or abuse of medical authority, ethics, dangerous misinformation or fraud, and some of the criticism has been with support from independent research or evidence, such as research studies of effectivenes. For instance, a US government agency, the [[National Science Foundation]], reporting on ''Public Attitudes and Public Understanding'' in ''Science and Engineering Indicators 2002'' stated that the term "alternative medicine" as used in the report was referring to treatments that had not been proven effective using scientific methods.<ref>{{cite web | quote = alternative medicine refers to all treatments that have not been proven effective using scientific methods | title = Science and Technology: Public Attitudes and Public Understanding Science Fiction and Pseudoscience - Belief in Alternative Medicine | publisher = [[National Science Foundation]] | url = http://www.nsf.gov/statistics/seind02/c7/c7s5.htm }}</ref><ref>Chapter 7, ''Science and Technology: Public Attitudes and Public Understanding''of ''Science and Engineering Indicators 2002'', National Science Board, Science and Engineering Indicators – 2002. Arlington, VA: National Science Foundation, 2002 (NSB-02-1[http://www.nsf.gov/statistics/seind02/c7/c7h.htm]</ref> |
||
Instances of criticism by individuals include [[Wallace Sampson]], writing in an article in Annals of the New York Academy of Sciences, June 1995 (first published online Dec 2006).<ref |
Instances of criticism by individuals include [[Wallace Sampson]], writing in an article in Annals of the New York Academy of Sciences, June 1995 (first published online Dec 2006).<ref>{{cite journal|last=Sampson|first=Wallace|title=Antiscience trends in the rise of the "alternative medicine" movement|journal=Annals of the New York Academy of Sciences|date=1 June 1995|volume=775|issue=1|pages=188–197|doi=10.1111/j.1749-6632.1996.tb23138.x|pages=189–191}} [[Wallace Sampson]]</ref>. There, Sampson argued that proponents of alternative medicine often used terminology which was loose or ambiguous to create the appearance that a choice between "alternative" effective treatments existed when it did not, or that there was effectiveness or scientific validity when it did not exist, or to suggest that a dichotomy existed when it did not, or to suggest that consistency with science existed when it might not; that the term "'''alternative'''" was to suggest that a patient had a choice between effective treatments when there wsa not; that use of the word "'''conventional'''" or "'''mainstream'''" was to suggest that the difference between alternative medicine and science based medicine was the prevalence of use, rather than lack of a scientific basis of alternative medicine as compared to "conventional" or "mainstream" science based medicine; |
||
that use of the term "complementary" was to suggest that purported supernatural energies of alternative medicine could add to or complement science based medicine; that use of the term "integrative" was to suggest that supernatural beliefs can be consistently integrated with science and the result has scientific validity. |
that use of the term "'''complementary'''" was to suggest that purported supernatural energies of alternative medicine could add to or complement science based medicine; that use of the term "'''integrative'''" was to suggest that supernatural beliefs can be consistently integrated with science and the result has scientific validity. Sampson, [[Stanford University]] medical professor, former chairperson of the [[National Council Against Health Fraud]], advisor to the California Attorney General and numerous district attorneys on medical fraud, and editor of [[Scientific Review of Alternative Medicine]], has also written that CAM is the "propagation of the absurd", and argued that ''alternative'' and ''complementary'' have been substituted for ''quackery'', ''dubious'' and ''implausible''.<ref name=absurd/>. |
||
Other criticism has been that " |
Other criticism has been that "'''Integrative medicine'''" ("integrated medicine") is used either to refer to a belief that medicine based on science can be "integrated" with practices that are not, or that a combination of alternative medical treatments with conventional science based treatments that have some scientific proof of efficacy, in which case it is identical with CAM;<ref name=BMJ_May/> that there is only medicine that has been adequately tested and that which has not;<ref name=Angell>{{cite journal |author=Angell M, Kassirer JP |title=Alternative medicine--the risks of untested and unregulated remedies |journal=The New England Journal of Medicine |volume=339 |issue=12 |pages=839–41 |year=1998 |month=September |pmid=9738094 |doi=10.1056/NEJM199809173391210 |url=http://kitsrus.com/pdf/nejm_998.pdf |quote=It is time for the scientific community to stop giving alternative medicine a free ride. There cannot be two kinds of medicine – conventional and alternative. There is only medicine that has been adequately tested and medicine that has not, medicine that works and medicine that may or may not work. Once a treatment has been tested rigorously, it no longer matters whether it was considered alternative at the outset. If it is found to be reasonably safe and effective, it will be accepted. But assertions, speculation, and testimonials do not substitute for evidence. Alternative treatments should be subjected to scientific testing no less rigorous than that required for conventional treatments.}}</ref> that ''"There really is no such thing as alternative medicine--only medicine that has been proved to work and medicine that has not."'' - Arnold Relman, editor in chief emeritus of ''[[The New England Journal of Medicine]]'';<ref>The New England Journal of Medicine, July 1995.</ref>{{full|date=November 2012}} |
||
Another critic, with reference to government funding studies of integrating alternative medicine techniques into the mainstream, [[Steven Novella]], a neurologist at Yale School of Medicine, wrote that it "is used to lend an appearance of legitimacy to treatments that are not legitimate." Another, [[Marcia Angell]], former executive editor of ''The New England Journal of Medicine'' argued that it was a new name for snake oil."<ref name="HttpwwwwashingtonpostcomwpdyncontentarticleARhtml" /> Angell considered that critics felt that healthcare practices should be classified based solely on [[evidence-based medicine|scientific evidence]], and if a treatment had been rigorously tested and found safe and effective, science based medicine will adopt it regardless of whether it was considered "alternative" to begin with.<ref name=Angell/> It was thus possible for a method to change categories (proven vs. unproven), based on increased knowledge of its effectiveness or lack thereof. Prominent supporters of this position include [[George D. Lundberg]], former editor of the [[Journal of the American Medical Association]] (JAMA).<ref name=Fontanarosa>{{cite journal |author=Fontanarosa PB, Lundberg GD |title=Alternative medicine meets science |journal=JAMA |volume=280 |issue=18 |pages=1618–9 |year=1998 |month=November |pmid=9820267 |doi= 10.1001/jama.280.18.1618|url=}}</ref> |
Another critic, with reference to government funding studies of integrating alternative medicine techniques into the mainstream, [[Steven Novella]], a neurologist at Yale School of Medicine, wrote that it "is used to lend an appearance of legitimacy to treatments that are not legitimate." Another, [[Marcia Angell]], former executive editor of ''The New England Journal of Medicine'' argued that it was a new name for snake oil."<ref name="HttpwwwwashingtonpostcomwpdyncontentarticleARhtml" /> Angell considered that critics felt that healthcare practices should be classified based solely on [[evidence-based medicine|scientific evidence]], and if a treatment had been rigorously tested and found safe and effective, science based medicine will adopt it regardless of whether it was considered "alternative" to begin with.<ref name=Angell/> It was thus possible for a method to change categories (proven vs. unproven), based on increased knowledge of its effectiveness or lack thereof. Prominent supporters of this position include [[George D. Lundberg]], former editor of the [[Journal of the American Medical Association]] (JAMA).<ref name=Fontanarosa>{{cite journal |author=Fontanarosa PB, Lundberg GD |title=Alternative medicine meets science |journal=JAMA |volume=280 |issue=18 |pages=1618–9 |year=1998 |month=November |pmid=9820267 |doi= 10.1001/jama.280.18.1618|url=}}</ref> |
||
[[Richard Dawkins]], an evolutionary biologist, has defined alternative medicine as a "set of practices that cannot be tested, refuse to be tested, or consistently fail tests."<ref name=Dawkins>{{cite book | last = Dawkins | first = Richard | author = Richard Dawkins | year = 2003 | title = A Devil's Chaplain | publisher = Weidenfeld & Nicolson | isbn = 978-0-618-33540-4}}</ref> He has also stated that "there is no alternative medicine. There is only medicine that works and medicine that doesn't work."<ref name=Dawkins2>{{cite book |title=A Devil's Chaplain |last=Dawkins |first=Richard |year=2003 |publisher=Houghton Mifflin |location=United States |isbn=978-0-618-33540-4 |page=58}}</ref> He has argued that if a technique is demonstrated effective in properly performed trials, it ceases to be alternative and simply becomes medicine.<ref>{{cite news |url=http://www.guardian.co.uk/books/2003/feb/15/scienceandnature.highereducation1 |title=Review: A Devil's Chaplain by Richard Dawkins |work=The Guardian |accessdate= 2010-04-23| location=London | date=2003-02-15| archiveurl= http://web.archive.org/web/20100411001657/http://www.guardian.co.uk/books/2003/feb/15/scienceandnature.highereducation1| archivedate= 11 April 2010 <!--DASHBot-->| deadurl= no}}</ref> |
[[Richard Dawkins]], an evolutionary biologist who is not a medical practitioner of any kind nor has qualified as a physician or surgeon, has defined alternative medicine as a "set of practices that cannot be tested, refuse to be tested, or consistently fail tests."<ref name=Dawkins>{{cite book | last = Dawkins | first = Richard | author = Richard Dawkins | year = 2003 | title = A Devil's Chaplain | publisher = Weidenfeld & Nicolson | isbn = 978-0-618-33540-4}}</ref> He has also stated that "there is no alternative medicine. There is only medicine that works and medicine that doesn't work."<ref name=Dawkins2>{{cite book |title=A Devil's Chaplain |last=Dawkins |first=Richard |year=2003 |publisher=Houghton Mifflin |location=United States |isbn=978-0-618-33540-4 |page=58}}</ref> He has argued that if a technique is demonstrated effective in properly performed trials, it ceases to be alternative and simply becomes medicine.<ref>{{cite news |url=http://www.guardian.co.uk/books/2003/feb/15/scienceandnature.highereducation1 |title=Review: A Devil's Chaplain by Richard Dawkins |work=The Guardian |accessdate= 2010-04-23| location=London | date=2003-02-15| archiveurl= http://web.archive.org/web/20100411001657/http://www.guardian.co.uk/books/2003/feb/15/scienceandnature.highereducation1| archivedate= 11 April 2010 <!--DASHBot-->| deadurl= no}}</ref> |
||
In an article first published in ''CA: A Cancer Journal for Clinicians'', November/December 1999, ''Evaluating complementary and alternative therapies for cancer patients'', Barrie R. Cassileth mentioned that a 1997 letter to the US Senate Subcommittee on Public Health and Safety which had deplored the lack of critical thinking and scientific rigor in OAM-supported research had been signed by four Nobel Laureates and other prominent scientists. (This was supported by the [[National Institutes of Health]] (NIH).)<ref name=Cassileth_evaluating>{{cite journal |author=Cassileth BR |title=Evaluating complementary and alternative therapies for cancer patients |journal=CA Cancer J Clin |volume=49 |issue=6 |pages=362–75 |year=1999 |pmid=11198952 |doi= 10.3322/canjclin.49.6.362|url=http://onlinelibrary.wiley.com/doi/10.3322/canjclin.49.6.362/full}}</ref> |
In an article first published in ''CA: A Cancer Journal for Clinicians'', November/December 1999, ''Evaluating complementary and alternative therapies for cancer patients'', Barrie R. Cassileth mentioned that a 1997 letter to the US Senate Subcommittee on Public Health and Safety which had deplored the lack of critical thinking and scientific rigor in OAM-supported research had been signed by four Nobel Laureates and other prominent scientists. (This was supported by the [[National Institutes of Health]] (NIH).)<ref name=Cassileth_evaluating>{{cite journal |author=Cassileth BR |title=Evaluating complementary and alternative therapies for cancer patients |journal=CA Cancer J Clin |volume=49 |issue=6 |pages=362–75 |year=1999 |pmid=11198952 |doi= 10.3322/canjclin.49.6.362|url=http://onlinelibrary.wiley.com/doi/10.3322/canjclin.49.6.362/full}}</ref> |
||
In March, 2009 a ''Washington Post'' staff writer reported that the impending national discussion about broadening access to health care, improving medical practice and saving money was giving a group of scientists an opening to propose shutting down the [[National Center for Complementary and Alternative Medicine]], quoting one of them, Steven Salzberg, a genome researcher and computational biologist at the University of Maryland, saying "One of our concerns is that NIH is funding pseudoscience." They argued that the vast majority of studies were based on fundamental misunderstandings of [[physiology]] and [[disease]], and have shown little or no effect.<ref name=Brown>{{cite news |url=http://www.washingtonpost.com/wp-dyn/content/article/2009/03/16/AR2009031602139.html?hpid=sec-health |title=Scientists Speak Out Against Federal Funds for Research on Alternative Medicine|work=Washingtonpost |date=March 17, 2009 | first=David | last=Brown | accessdate=2010-04-23}}</ref> |
In March, 2009 a ''Washington Post'' staff writer reported that the impending national discussion about broadening access to health care, improving medical practice and saving money was giving a group of scientists an opening to propose shutting down the [[National Center for Complementary and Alternative Medicine]], quoting one of them, Steven Salzberg, a genome researcher and computational biologist at the University of Maryland, saying "One of our concerns is that NIH is funding pseudoscience." They argued that the vast majority of studies were based on fundamental misunderstandings of [[physiology]] and [[disease]], and have shown little or no effect.<ref name=Brown>{{cite news |url=http://www.washingtonpost.com/wp-dyn/content/article/2009/03/16/AR2009031602139.html?hpid=sec-health |title=Scientists Speak Out Against Federal Funds for Research on Alternative Medicine|work=Washingtonpost |date=March 17, 2009 | first=David | last=Brown | accessdate=2010-04-23}}</ref> |
||
[[Stephen Barrett]], founder and operator of [[Quackwatch]], has argued that practices labeled "alternative" should be reclassified as either genuine, experimental, or questionable. Here he defines genuine as being methods that have sound evidence for safety and effectiveness, experimental as being unproven but with a plausible rationale for effectiveness, and questionable as groundless without a scientifically plausible rationale.<ref name=Quackwatch/> |
[[Stephen Barrett]], founder and operator of [[Quackwatch]], has argued that practices labeled "alternative" should be reclassified as either genuine, experimental, or questionable. Here he defines genuine as being methods that have sound evidence for safety and effectiveness, experimental as being unproven but with a plausible rationale for effectiveness, and questionable as groundless without a scientifically plausible rationale.<ref name=Quackwatch/> |
||
Sampson has also pointed out that CAM tolerated [[falacy|contradiction]] without thorough reason and experiment.<ref name=absurd>{{cite journal |author=Sampson W, Atwood Iv K |title=Propagation of the absurd: demarcation of the absurd revisited |journal=Med. J. Aust. |volume=183 |issue=11–12 |pages=580–1 |year=2005 |pmid=16336135 |doi= |url=}}</ref> Barrett has pointed out that there is a policy at the NIH of never saying something doesn't work only that a different version or dose might give different results.<ref name="$2.5 billion"/> Barrett also expressed concern that, just because some "alternatives" have merit, there is the impression that the rest deserve equal consideration and respect even though most are worthless, since they are all classified under the one heading of alternative medicine.<ref name=Quackwatch>{{cite news|first=Stephen|last=Barrett|title=Be Wary of "Alternative" Health Methods|url=http://www.quackwatch.org/01QuackeryRelatedTopics/altwary.html|work=[[Stephen Barrett|Stephen Barrett, M.D.]]|publisher=[[Quackwatch]]|date=February 10, 2004 |accessdate = 2008-03-03}}</ref> |
|||
A group of prominent scientists argued before the federal government, USA, that plausibility of interventions such as diet, relaxation, yoga and botanical remedies, should not be used to support research on implausible interventions based on superstition and belief in the supernatural, and that the plausible methods can be studied just as well in other parts of NIH, where they should be made to compete on an equal footing with other research projects.<ref name=Brown/> The [[National Center for Complementary and Alternative Medicine|NCCAM]] budget has been criticized<ref name="HttpwwwwashingtonpostcomwpdyncontentarticleARhtml">[http://www.washingtonpost.com/wp-dyn/content/article/2009/03/16/AR2009031602139.html Scientists Speak Out Against Federal Funds for Research on Alternative Medicine – washingtonpost.com]</ref> because, despite the duration and intensity of studies to measure the efficacy of alternative medicine, there had been no effective [[Complementary and Alternative Medicine|CAM]] treatments supported by scientific evidence as of 2002 according to the QuackWatch website.<ref name="HttpwwwquackwatchorgQuackeryRelatedTopicsnccamhtml">[http://www.quackwatch.org/01QuackeryRelatedTopics/nccam.html Why the National Center for Complementary and Alternative Medicine (NCCAM) Should Be Defunded]</ref> Despite this, the [[National Center for Complementary and Alternative Medicine]] budget has been on a sharp sustained rise to support complementary medicine. In fact, the whole CAM field has been called by critics the SCAM.<ref name="HttpwwwquackwatchorgQuackeryRelatedTopicsnccamhtml" /> There have been negative results in almost all studies conducted over ten years at a cost of $2.5 billion by the NCCAM.<ref>[http://nccam.nih.gov/research/results/ Research Results of Complementary and Alternative Medicine [NCCAM Research]]</ref> |
|||
Sampson has also pointed out that CAM tolerated [[falacy|contradiction]] without thorough reason and experiment.<ref name=absurd>{{cite journal |author=Sampson W, Atwood Iv K |title=Propagation of the absurd: demarcation of the absurd revisited |journal=Med. J. Aust. |volume=183 |issue=11–12 |pages=580–1 |year=2005 |pmid=16336135 |doi= |url=}}</ref> Barrett has pointed out that there is a policy at the NIH of never saying something doesn't work only that a different version or dose might give different results.<ref name="$2.5 billion"/> Barrett also expressed concern that, just because some "alternatives" have merit, there is the impression that the rest deserve equal consideration and respect even though most are worthless, since they are all classified under the one heading of alternative medicine.<ref name=Quackwatch>{{cite news|first=Stephen|last=Barrett|title=Be Wary of "Alternative" Health Methods|url=http://www.quackwatch.org/01QuackeryRelatedTopics/altwary.html|work=[[Stephen Barrett|Stephen Barrett, M.D.]]|publisher=[[Quackwatch]]|date=February 10, 2004 |accessdate = 2008-03-03}}</ref> |
|||
A group of prominent scientists argued before the federal government, USA, that plausibility of interventions such as diet, relaxation, yoga and botanical remedies, should not be used to support research on implausible interventions based on superstition and belief in the supernatural, and that the plausible methods can be studied just as well in other parts of NIH, where they should be made to compete on an equal footing with other research projects.<ref name=Brown/> The [[National Center for Complementary and Alternative Medicine|NCCAM]] budget has been criticized<ref name="HttpwwwwashingtonpostcomwpdyncontentarticleARhtml">[http://www.washingtonpost.com/wp-dyn/content/article/2009/03/16/AR2009031602139.html Scientists Speak Out Against Federal Funds for Research on Alternative Medicine – washingtonpost.com]</ref> because, despite the duration and intensity of studies to measure the efficacy of alternative medicine, there had been no effective [[Complementary and Alternative Medicine|CAM]] treatments supported by scientific evidence as of 2002 according to the QuackWatch website.<ref name="HttpwwwquackwatchorgQuackeryRelatedTopicsnccamhtml">[http://www.quackwatch.org/01QuackeryRelatedTopics/nccam.html Why the National Center for Complementary and Alternative Medicine (NCCAM) Should Be Defunded]</ref> Despite this, the [[National Center for Complementary and Alternative Medicine]] budget has been on a sharp sustained rise to support complementary medicine. There have been negative results in almost all studies conducted over ten years at a cost of $2.5 billion by the NCCAM.<ref>[http://nccam.nih.gov/research/results/ Research Results of Complementary and Alternative Medicine [NCCAM Research]]</ref> |
|||
A research methods expert and author of "Snake Oil Science", R. Barker Bausell, has stated that "it's become politically correct to investigate nonsense."<ref name="$2.5 billion">{{cite web |url=http://www.msnbc.msn.com/id/31190909/ |title=$2.5 billion spent, no alternative cures found |
A research methods expert and author of "Snake Oil Science", R. Barker Bausell, has stated that "it's become politically correct to investigate nonsense."<ref name="$2.5 billion">{{cite web |url=http://www.msnbc.msn.com/id/31190909/ |title=$2.5 billion spent, no alternative cures found – Alternative medicine- msnbc.com |work=MSNBC |date=June 10, 2009}}</ref> There are concerns that just having NIH support is being used to give unfounded "legitimacy to treatments that are not legitimate."<ref name=Brown/> |
||
Use of placebos in order to achieve a [[placebo effect]] in integrative medicine has been criticized as “diverting research time, money, and other resources from more fruitful lines of investigation in order to pursue a theory that has no basis in biology”.<ref name="Credulityabout" /><ref>Acupuncture Pseudoscience in the New England Journal of Medicine, Science Based Medicine, Steven Novella [http://www.sciencebasedmedicine.org/?p=6391 Science-Based Medicine » Acupuncture Pseudoscience in the New England Journal of Medicine]</ref> |
Use of placebos in order to achieve a [[placebo effect]] in integrative medicine has been criticized as “diverting research time, money, and other resources from more fruitful lines of investigation in order to pursue a theory that has no basis in biology”.<ref name="Credulityabout" /><ref>Acupuncture Pseudoscience in the New England Journal of Medicine, Science Based Medicine, Steven Novella [http://www.sciencebasedmedicine.org/?p=6391 Science-Based Medicine » Acupuncture Pseudoscience in the New England Journal of Medicine]</ref> |
||
Speaking of [[ethics]], in November 2011 [[Edzard Ernst]] stated that the "level of misinformation about alternative medicine has now reached the point where it has become dangerous and unethical. So far, alternative medicine has remained an ethics-free zone. It is time to change this."<ref name=ernst-ethics>[[Edzard Ernst]]. [http://www.guardian.co.uk/science/blog/2011/nov/08/alternative-medicine-ethics-free-zone "Alternative medicine remains an ethics-free zone."] ''[[The Guardian]]'' 8 November 2011</ref> Ernst requested that [[Prince Charles]] recall two guides to alternative medicine published by the Foundation for Integrated Health, on the grounds that "[t]hey both contain numerous misleading and inaccurate claims concerning the supposed benefits of alternative medicine" and that "[t]he nation cannot be served by promoting ineffective and sometimes dangerous alternative treatments."<ref name=Henderson>Mark Henderson, Science Editor, "[http://www.timesonline.co.uk/tol/life_and_style/health/alternative_medicine/article3760857.ece Prince of Wales's guide to alternative medicine 'inaccurate']" ''Times Online'', April 17, 2008</ref> In general, he believes that CAM can and should be subjected to scientific testing.<ref name="UMM" /><ref name=goodbadugly /><ref name="brit_gen_prac">"Complementary medicine is diagnosis, treatment and/or prevention that complements mainstream medicine by contributing to a common whole, by satisfying a demand not met by orthodoxy or by diversifying the conceptual frameworks of medicine." Ernst et al. ''British General Practitioner'' 1995; 45:506.</ref> Ernst requested that [[Prince Charles]] recall two guides to alternative medicine published by the Foundation for Integrated Health, on the grounds that "[t]hey both contain numerous misleading and inaccurate claims concerning the supposed benefits of alternative medicine" and that "[t]he nation cannot be served by promoting ineffective and sometimes dangerous alternative treatments".<ref name="UMM" /><ref name=goodbadugly /><ref name="Henderson"/><ref name="brit_gen_prac"/> |
Speaking of [[ethics]], in November 2011 [[Edzard Ernst]] stated that the "level of misinformation about alternative medicine has now reached the point where it has become dangerous and unethical. So far, alternative medicine has remained an ethics-free zone. It is time to change this."<ref name=ernst-ethics>[[Edzard Ernst]]. [http://www.guardian.co.uk/science/blog/2011/nov/08/alternative-medicine-ethics-free-zone "Alternative medicine remains an ethics-free zone."] ''[[The Guardian]]'' 8 November 2011</ref> Ernst requested that [[Prince Charles]] recall two guides to alternative medicine published by the Foundation for Integrated Health, on the grounds that "[t]hey both contain numerous misleading and inaccurate claims concerning the supposed benefits of alternative medicine" and that "[t]he nation cannot be served by promoting ineffective and sometimes dangerous alternative treatments."<ref name=Henderson>Mark Henderson, Science Editor, "[http://www.timesonline.co.uk/tol/life_and_style/health/alternative_medicine/article3760857.ece Prince of Wales's guide to alternative medicine 'inaccurate']" ''Times Online'', April 17, 2008</ref> In general, he believes that CAM can and should be subjected to scientific testing.<ref name="UMM" /><ref name=goodbadugly /><ref name="brit_gen_prac">"Complementary medicine is diagnosis, treatment and/or prevention that complements mainstream medicine by contributing to a common whole, by satisfying a demand not met by orthodoxy or by diversifying the conceptual frameworks of medicine." Ernst et al. ''British General Practitioner'' 1995; 45:506.</ref> Ernst requested that [[Prince Charles]] recall two guides to alternative medicine published by the Foundation for Integrated Health, on the grounds that "[t]hey both contain numerous misleading and inaccurate claims concerning the supposed benefits of alternative medicine" and that "[t]he nation cannot be served by promoting ineffective and sometimes dangerous alternative treatments".<ref name="UMM" /><ref name=goodbadugly /><ref name="Henderson"/><ref name="brit_gen_prac"/> |
||
According to two writers, Wallace Sampson and K.Butler, [[Marketing]] is part of the medical training required in [[chiropractic]] educaion, and propoganda methods in alternative medicine have been traced back to those used by Hitler and Goebels in their promotion of pseudoscience in medicine.<ref name=ATRAMM /><ref name=CGAM>Butler K (1992). A Consumer's Guide to "ALTERNATIVE MEDICINE": A close look at Homeopathy, Acupuncture, Faith-healing and other Unconventional Treatments</ref> |
According to two writers, Wallace Sampson and K.Butler, [[Marketing]] is part of the medical training required in [[chiropractic]] educaion, and propoganda methods in alternative medicine have been traced back to those used by Hitler and Goebels in their promotion of pseudoscience in medicine.<ref name=ATRAMM /><ref name=CGAM>Butler K (1992). A Consumer's Guide to "ALTERNATIVE MEDICINE": A close look at Homeopathy, Acupuncture, Faith-healing and other Unconventional Treatments</ref> |
||
| Line 203: | Line 219: | ||
==Use and regulation== |
==Use and regulation== |
||
===Prevalence of use=== |
===Prevalence of use=== |
||
[[File:Bangladesh Prayer.jpg|200px|thumb|Studies show that prayer is a common "complementary" practice, in the belief it might increase the efficacy of science based medicine.]] |
[[File:Bangladesh Prayer.jpg|200px|thumb|Studies show that prayer is a common "complementary" practice, in the belief it might increase the efficacy of science based medicine.]] |
||
'''Complementary and alternative medicine''' (CAM) has been described as a broad domain of healing resources that encompasses all health systems, modalities, and practices and their accompanying theories and beliefs, other than those intrinsic to the politically dominant health system of a particular society or culture in a given historical period. CAM includes all such practices and ideas self-defined by their users as preventing or treating illness or promoting health and well-being. Boundaries within CAM and between the CAM domain and that of the dominant system are not always sharp or fixed<ref name="Cochrane definition of CAM">{{cite journal|coauthors=Wieland LS, Manheimer E, Berman BM.|title=Development and classification of an operational definition of complementary and alternative medicine for the Cochrane collaboration|journal=Altern Ther Health Med.|year=2011|month=Mar-April|volume=17|issue=2|pages= |
'''Complementary and alternative medicine''' (CAM) has been described as a broad domain of healing resources that encompasses all health systems, modalities, and practices and their accompanying theories and beliefs, other than those intrinsic to the politically dominant health system of a particular society or culture in a given historical period. CAM includes all such practices and ideas self-defined by their users as preventing or treating illness or promoting health and well-being. Boundaries within CAM and between the CAM domain and that of the dominant system are not always sharp or fixed<ref name="Cochrane definition of CAM">{{cite journal|coauthors=Wieland LS, Manheimer E, Berman BM.|title=Development and classification of an operational definition of complementary and alternative medicine for the Cochrane collaboration.|journal=Altern Ther Health Med.|year=2011|month=Mar-April|volume=17|issue=2|pages=50-59|pmid=21717826|accessdate=15 February 2013}}</ref>{{dubious|date=February 2013}} |
||
In respect of taxation in the U.S.A. the Internal Revenue Service has discriminated in favour of medical expenses for acupuncture and chiropractor (and others including [[Christian Science practitioner]]) but against homeopathy and the use of non-prescription required medicine.<ref>Internal Revenue Service Pubication 502 ''Medical and Dental Expenses'' (for 2012 rerurns), section 5 ''What Medical Expenses Are Includible?'': "Medical expenses are the costs of diagnosis, cure, mitigation, treatment, or prevention of disease, and the costs for treatments affecting any part or function of the body. These expenses include payments for legal medical services rendered by physicians, surgeons, dentists and other medical practitioners.... primarily to alleviate or prevent a physical or mental defect or illness.'' ''Medicines: You can include expenses amounts you pay for prescribed medicines and drugs. A prescribed drug is one that requires a prescription by a doctor for its use by an individual." |
In respect of taxation in the U.S.A. the Internal Revenue Service has discriminated in favour of medical expenses for acupuncture and chiropractor (and others including [[Christian Science practitioner]]) but against homeopathy and the use of non-prescription required medicine.<ref>Internal Revenue Service Pubication 502 ''Medical and Dental Expenses'' (for 2012 rerurns), section 5 ''What Medical Expenses Are Includible?'': "Medical expenses are the costs of diagnosis, cure, mitigation, treatment, or prevention of disease, and the costs for treatments affecting any part or function of the body. These expenses include payments for legal medical services rendered by physicians, surgeons, dentists and other medical practitioners.... primarily to alleviate or prevent a physical or mental defect or illness.'' ''Medicines: You can include expenses amounts you pay for prescribed medicines and drugs. A prescribed drug is one that requires a prescription by a doctor for its use by an individual." |
||
| Line 233: | Line 250: | ||
===Regulation=== |
===Regulation=== |
||
{{Further|Regulation of alternative medicine | Regulation and prevalence of homeopathy}} |
{{Further|Regulation of alternative medicine | Regulation and prevalence of homeopathy}} |
||
Some professions of complementary/traditional/alternative medicine, such as [[chiropractic|chiropractic medicine]], have achieved full regulation in North America and other parts of the world <ref name=WHO-guidelines>{{cite journal |author= World Health Organization|year=2005|title= WHO guidelines on basic training and safety in chiropractic|url=http://www.who.int/medicines/areas/traditional/Chiro-Guidelines.pdf|format=PDF|isbn= 92-4-159371-7|accessdate=2008-02-29}}</ref> and are are regulated in a manner similar to that governing science-based medicine. In contrast, other approaches may be partially recognized and others have no regulation at all. Regulation and licensing of alternative medicine ranges widely from country to country, and state to state.<ref name= |
Some professions of complementary/traditional/alternative medicine, such as [[chiropractic|chiropractic medicine]], have achieved full regulation in North America and other parts of the world <ref name=WHO-guidelines>{{cite journal |author= World Health Organization|year=2005|title= WHO guidelines on basic training and safety in chiropractic|url=http://www.who.int/medicines/areas/traditional/Chiro-Guidelines.pdf|format=PDF|isbn= 92-4-159371-7|accessdate=2008-02-29}}</ref> and are are regulated in a manner similar to that governing science-based medicine. In contrast, other approaches may be partially recognized and others have no regulation at all. Regulation and licensing of alternative medicine ranges widely from country to country, and state to state.<ref name=WHO-guidelines>{{cite journal |author= World Health Organization|year=2005|title= WHO guidelines on basic training and safety in chiropractic|url=http://www.who.int/medicines/areas/traditional/Chiro-Guidelines.pdf|format=PDF|isbn= 92-4-159371-7|accessdate=2008-02-29}}</ref> |
||
Government bodies in the USA and elsewhere have published information or guidance about alternative medicine. One of those is the [[U.S. Food and Drug Administration]] (FDA), which mentions specifically [[homeopathic]] products, [[traditional Chinese medicine]] and [[Ayurvedic]] products.<ref>http://www.fda.gov/Drugs/ResourcesForYou/Consumers/BuyingUsingMedicineSafely/MedicationHealthFraud/ucm207747.htm FDA, Drugs, information for consumers]</ref> A document which the FDA has issued for comment is headed ''Guidance for Industry: Complementary and Alternative Medicine Products and Their Regulation by the Food and Drug Administration'', last updated 04/06/2012.<ref>[vhttp://www.fda.gov/ICECI/ComplianceManuals/CompliancePolicyGuidanceManual/ucm074360.htm]</ref> The document opens with three preliminary paragraphs which explain that ''in the document'': |
Government bodies in the USA and elsewhere have published information or guidance about alternative medicine. One of those is the [[U.S. Food and Drug Administration]] (FDA), which mentions specifically [[homeopathic]] products, [[traditional Chinese medicine]] and [[Ayurvedic]] products.<ref>http://www.fda.gov/Drugs/ResourcesForYou/Consumers/BuyingUsingMedicineSafely/MedicationHealthFraud/ucm207747.htm FDA, Drugs, information for consumers]</ref> A document which the FDA has issued for comment is headed ''Guidance for Industry: Complementary and Alternative Medicine Products and Their Regulation by the Food and Drug Administration'', last updated 04/06/2012.<ref>[vhttp://www.fda.gov/ICECI/ComplianceManuals/CompliancePolicyGuidanceManual/ucm074360.htm]</ref> The document opens with three preliminary paragraphs which explain that ''in the document'': |
||
| Line 245: | Line 262: | ||
: - no mention (in the document) of a particular CAM therapy, practice or product should be taken as expressing FDA's support or endorsement of it or as an agency determination that a particular product is safe and effective. |
: - no mention (in the document) of a particular CAM therapy, practice or product should be taken as expressing FDA's support or endorsement of it or as an agency determination that a particular product is safe and effective. |
||
==Efficacy== |
== Efficacy == |
||
Criteria and principles about evidence and the validity of clinical tests or trials applicable to healthcare interventions, including alternative medicine, were considered by Steven Woolf and others in a paper published in 2012 titled ''Developing clinical practice guidelines: types of evidence and outcomes''.<ref>''Developing clinical practice guidelines: types of evidence and outcomes; values and economics, synthesis, grading, and presentation and deriving recommendations'', Steven Woolf and others, 2012.[http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3436711/] Implementation Science[http://www.implementationscience.com/content/7/1/61]</ref> This indicated the importance of skill, knowledge and objectivity in the design and conduct of trials and in recording and reporting the benefits, harms, and other outcomes that were considered. |
Criteria and principles about evidence and the validity of clinical tests or trials applicable to healthcare interventions, including alternative medicine, were considered by Steven Woolf and others in a paper published in 2012 titled ''Developing clinical practice guidelines: types of evidence and outcomes''.<ref>''Developing clinical practice guidelines: types of evidence and outcomes; values and economics, synthesis, grading, and presentation and deriving recommendations'', Steven Woolf and others, 2012.[http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3436711/] Implementation Science[http://www.implementationscience.com/content/7/1/61]</ref> This indicated the importance of skill, knowledge and objectivity in the design and conduct of trials and in recording and reporting the benefits, harms, and other outcomes that were considered. |
||
The position of [[Arnold S. Relman]], a physician who has also written on [[Health care reform]] in U.S.A., is that most varieties of "alternative" therapies that have not been proven effective in clinical trials should be among the exclusions from health care benefits prescribed by physicians.<ref>Relman, Arnold S., ''A Second Opinion: Rescuing America's Health Care'' (2007), |
The position of [[Arnold S. Relman]], a physician who has also written on [[Health care reform]] in U.S.A., is that most varieties of "alternative" therapies that have not been proven effective in clinical trials should be among the exclusions from health care benefits prescribed by physicians.<ref>Relman, Arnold S., ''A Second Opinion: Rescuing America's Health Care'' (2007), |
||
[http://www.publicaffairsbooks.com/publicaffairsbooks-cgi-bin/display?book=9781586484811&view=note] chapter 5 ''The reform we need''</ref> |
[http://www.publicaffairsbooks.com/publicaffairsbooks-cgi-bin/display?book=9781586484811&view=note] chapter 5 ''The reform we need''</ref> |
||
Alternative therapies lack the requisite [[scientific validation]], and their [[efficacy|effectiveness]] is either [[Scientific method|unproved]] or [[Scientific evidence|disproved]].<ref name=NSF_altmed/><ref name=ATRAMM/><ref name="IGPIAMAYP"/><ref name="NP"/> Many of the claims regarding the efficacy of alternative medicines are controversial, since research on them is frequently of low quality and methodologically flawed.<ref name=IOM2005/> [[Publication bias|Selective publication of results]] (misleading results from only publishing postive results, and not all results), marked differences in product quality and standardisation, and some companies making unsubstantiated claims, call into question the claims of efficacy of isolated examples where herbs may have some evidence of containing chemicals that may affect health.<ref name=Sarris>{{cite journal |author=Sarris Jerome |title=Current challenges in appraising complementary medicine evidence |journal=The Medical Journal of Australia |volume=196 |issue=5 |pages=310–311 |year=2012 |url=https://www.mja.com.au/journal/2012/196/5/current-challenges-appraising-complementary-medicine-evidence#3 |pmid=22432660 |doi=10.5694/mja11.10751}}</ref> ''The Scientific Review of Alternative Medicine'' points to confusions in the general population |
Alternative therapies lack the requisite [[scientific validation]], and their [[efficacy|effectiveness]] is either [[Scientific method|unproved]] or [[Scientific evidence|disproved]].<ref name=NSF_altmed/><ref name=ATRAMM/><ref name="IGPIAMAYP"/><ref name="NP"/> Many of the claims regarding the efficacy of alternative medicines are controversial, since research on them is frequently of low quality and methodologically flawed.<ref name=IOM2005/> [[Publication bias|Selective publication of results]] (misleading results from only publishing postive results, and not all results), marked differences in product quality and standardisation, and some companies making unsubstantiated claims, call into question the claims of efficacy of isolated examples where herbs may have some evidence of containing chemicals that may affect health.<ref name=Sarris>{{cite journal |author=Sarris Jerome |title=Current challenges in appraising complementary medicine evidence |journal=The Medical Journal of Australia |volume=196 |issue=5 |pages=310–311 |year=2012 |url=https://www.mja.com.au/journal/2012/196/5/current-challenges-appraising-complementary-medicine-evidence#3 |pmid=22432660 |doi=10.5694/mja11.10751}}</ref> ''The Scientific Review of Alternative Medicine'' points to confusions in the general population - a person may attribute symptomatic relief to an otherwise-ineffective therapy just because they are taking something (the [[placebo effect]]); the natural recovery from or the cyclical nature of an illness (the [[regression fallacy]]) gets misattributed to an alternative medicine being taken; a person not diagnosed with science based medicine may never originally have had a true illness diagnosed as an alternative disease category.<ref>James Alcock PhD, ''Alternative Medicine and the Psychology of Belief'', The Scientific Review of Alternative Medicine, Fall/Winter 1999 Volume 3 ~ Number 2. [http://www.quackwatch.org/01QuackeryRelatedTopics/altpsych.html available online]</ref> |
||
===Acupuncture=== |
|||
There is evidence of benefit for acupuncture combined with exercise is effective for shoulder pain after stroke. <ref>{{cite journal|coauthors=Lee JA, Park SW, Hwang PW, Lim SM, Kook S, Choi KI, Kang KS.|title=Acupuncture for shoulder pain after stroke: a systematic review|journal=J Altern Complement Med. 18(9):818-23.|year=2012|month=Sept|volume=18|issue=9|page=818–823|doi=10.1089/acm.2011.0457|pmid=2292441|last1=Lee|first1=Jung Ah|pages=213–8}}</ref> reducing nausea post surgery <ref>{{cite journal|coauthors=Holmér Pettersson P, Wengström Y.|title=Acupuncture prior to surgery to minimise postoperative nausea and vomiting: a systematic review|journal=J Clin Nurs. 2012|year=2012|month=July|volume=21|issue=13–14|pages=799–805.|pmid=22672450|last1=Holmér Pettersson|first1=P|doi=10.1111/j.1365-2702.2012.04114.x}}</ref> and is cost-effective for some chronic pain syndromes. <ref>{{cite journal|coauthors=Ambrósio EM, Bloor K, MacPherson H.|title=Costs and consequences of acupuncture as a treatment for chronic pain: a systematic review of economic evaluations conducted alongside randomised controlled trials|journal=Complement Ther Med.|year=2012|month=Oct|volume=20|issue=5|pages=364–74.|pmid=22863652|doi=10.1016/j.ctim.2012.05.002|last1=Ambrósio|first1=EM}}</ref> |
|||
====Body manipulation==== |
|||
Manual and manipulative therapies commonly are used primarily to help treat low back pain and other neuromusculoskeletal disorders. Spinal manipulation is effective for chronic non-specific [[low back pain]]<ref name=Cochrane-2011>{{cite journal|journal= [[Cochrane Database Syst Rev]]|year=2011|issue=2|pages=CD008112|title= Spinal manipulative therapy for chronic low-back pain|author= Rubinstein SM, van Middelkoop M, Assendelft WJ, de Boer MR, van Tulder MW|doi=10.1002/14651858.CD008112.pub2|pmid=21328304|volume=|editor1-last= Rubinstein|editor1-first= Sidney M}}</ref> For acute low back pain, spinal manipulative therapy does not appear better than commonly recommended therapies such as analgesics, acupuncture, back pain education or exercise therapy.<ref>{{cite journal|coauthors=Rubinstein SM, Terwee CB, Assendelft WJ, de Boer MR, van Tulder MW.|title=Spinal manipulative therapy for acute low-back pain.|journal=Cochrane Database Syst Rev|year=2012|month=Sept|volume=12|issue=9|pmid=22972127|accessdate=11 February 2013}}</ref> <ref name=Dagenais-2010>{{cite journal|journal= [[Spine J]]|year=2010|volume=10|issue=10|pages=918–940|title= NASS Contemporary Concepts in Spine Care: Spinal manipulation therapy for acute low back pain|author= Dagenais S, Gay RE, Tricco AC, Freeman MD, Mayer JM|doi=10.1016/j.spinee.2010.07.389|pmid=20869008}}</ref><ref name=Bronfort-Haas>{{cite journal|journal= Chiropractic & Osteopathy|year=2010|volume=18|issue=3|title= Effectiveness of manual therapies: the UK evidence report|author= Bronfort G, Haas M, Evans R, Leininger B, Triano J|doi=10.1186/1746-1340-18-3|pmid=20184717|url=http://chiromt.com/content/18/1/3|pmc=2841070|page= 3}}</ref> Spinal manipulation may be effective for [[Lumbar vertebrae|lumbar]] [[spinal disc herniation|disc herniation]] with [[radiculopathy]],<ref name="Leininger B, Bronfort G, Evans R, Reiter T 2011 105–25">{{cite journal|journal= Phys Med Rehabil Clin N Am|year=2011|volume=22|issue=1|pages=105–25|title= Spinal manipulation or mobilization for radiculopathy: a systematic review|author= Leininger B, Bronfort G, Evans R, Reiter T|pmid=21292148|doi=10.1016/j.pmr.2010.11.002}}</ref><ref name="Hahne AJ, Ford JJ, McMeeken JM 2010 E488–504">{{cite journal|journal= Spine|year=2010|volume=35|issue=11|pages=E488–504|title= Conservative management of lumbar disc herniation with associated radiculopathy: a systematic review|author= Hahne AJ, Ford JJ, McMeeken JM|pmid=20421859|doi=10.1097/BRS.0b013e3181cc3f56}}</ref> neck pain,<ref name="Gross A, Miller J, D'Sylva J, Burnie SJ, Goldsmith CH, Graham N, Haines T, Brønfort G, Hoving JL 2010 315–333">{{cite journal|journal= Manual Therapy|year= 2010|volume=15|issue=4|pages=315–333|title= Manipulation or mobilisation for neck pain: a Cochrane Review|author= Gross A, Miller J, D'Sylva J, Burnie SJ, Goldsmith CH, Graham N, Haines T, Brønfort G, Hoving JL|pmid=20510644|doi= 10.1016/j.math.2010.04.002 }}</ref> some forms of headache,<ref name="Chaibi A, Tuchin PJ, Russell MB 2011">{{cite journal|journal= J Headache Pain|year=2011|volume= 12|issue= 2|pages= 127–33|title= Manual therapies for migraine: a systematic review|author= Chaibi A, Tuchin PJ, Russell MB|pmid=21298314|doi=10.1007/s10194-011-0296-6|pmc=3072494}}</ref><ref name="Bronfort G, Nilsson N, Haas M et al. 2004 CD001878">{{cite journal|journal= Cochrane Database Syst Rev|year=2004|issue=3|pages=CD001878|title= Non-invasive physical treatments for chronic/recurrent headache|author= Bronfort G, Nilsson N, Haas M ''et al.''|doi=10.1002/14651858.CD001878.pub2|pmid=15266458|editor1-last= Brønfort|editor1-first= Gert}}</ref> and some extremity joint conditions.<ref name="Brantingham JW, Globe G, Pollard H, Hicks M, Korporaal C, Hoskins W 2009 53–71">{{cite journal|author= Brantingham JW, Globe G, Pollard H, Hicks M, Korporaal C, Hoskins W|title= Manipulative therapy for lower extremity conditions: expansion of literature review|journal= J Manipulative Physiol Ther|volume=32|issue=1|pages=53–71|year=2009|pmid=19121464|doi=10.1016/j.jmpt.2008.09.013}}</ref><ref name="pmid21109059">{{Cite pmid|21109059}}</ref> In general, manipulative interventions appears equivalent to standard medical care, exercise therapy or physical therapy for neuromusculoskeletal complaints.[http://www.ncbi.nlm.nih.gov/pubmed/21328304][http://www.ncbi.nlm.nih.gov/pubmed/22621391]. There is insufficient evidence regarding the effectiveness of spinal manipulation on non-musculoskeletal conditions.<ref name=Trick-or-Treatment>{{cite book|pages=145–90|chapter=The truth about chiropractic therapy|title=Trick or Treatment: The Undeniable Facts about Alternative Medicine|author=Singh S, Ernst E|year=2008|publisher=W.W. Norton|isbn=978-0-393-06661-6 }}</ref> Other manual therapies such as [[massage]] have also been found to be effective for mechanical neck pain.<ref name=Bronfort-Haas>{{cite journal|journal= Chiropractic & Osteopathy|year=2010|volume=18|issue=3|title= Effectiveness of manual therapies: the UK evidence report|author= Bronfort G, Haas M, Evans R, Leininger B, Triano J|doi=10.1186/1746-1340-18-3|pmid=20184717|url=http://chiromt.com/content/18/1/3|pmc=2841070|page= 3}}</ref><ref>{{cite journal|coauthors=Hurwitz EL, Carragee EJ, van der Velde G, Carroll LJ, Nordin M, Guzman J, Peloso PM, Holm LW, Côté P, Hogg-Johnson S, Cassidy JD, Haldeman S; Bone and Joint Decade 2000-2010 Task Force on Neck Pain and Its Associated Disorders.|title=Treatment of neck pain: noninvasive interventions: results of the Bone and Joint Decade 2000-2010 Task Force on Neck Pain and Its Associated Disorders.|journal=Spine| year=2008| month=|volume=33 |issue=4|pages=123-152| pmid=18204386|accessdate=}}</ref><ref name=Vernon>{{cite journal|journal= [[Eura Medicophys]]|year=2007|volume=43|issue=1|pages=91–118|title= Manual therapy for neck pain: an overview of randomized clinical trials and systematic reviews|author= Vernon H, Humphreys BK|pmid=17369783|url=http://www.minervamedica.it/en/getfreepdf.php?cod=R33Y2007N01A0091|format=PDF}}</ref><ref name=CCA-CFCREAB-CPG/> |
|||
===Homeopathy=== |
|||
There is insufficient good evidence to enable robust conclusions to be made about Oscillococcinum(®) in the prevention or treatment of influenza and influenza-like illness. <ref>{{cite journal|coauthors=Mathie RT, Frye J, Fisher P.|title=Homeopathic Oscillococcinum(®) for preventing and treating influenza and influenza-like illness|journal=Cochrane Database Syst Rev.|year=2012|volume=12|issue=12|pmid=23235586|last1=Mathie|first1=RT|pages=CD001957|doi=10.1002/14651858.CD001957.pub5|editor1-last=Mathie|editor1-first=Robert T}}</ref> The evidence from controlled clinical trials therefore fails to show that homeopathy is an efficacious treatment for eczema.<ref>{{cite journal|coauthors=Ernst, E.|title=Homeopathy for eczema: a systematic review of controlled clinical trials|journal=Br J Dermatol.|year=2012|month=June|volume=166|issue=6|pages=1170–2|pmid=22568455|doi=10.1111/j.1365-2133.2012.10994.x|last1=Ernst|first1=E}}</ref> Limited evidence does not demonstrate a statistically significant effect of homeopathic medicines for insomnia treatment. <ref>{{cite journal|coauthors=Cooper KL, Relton C.|title=Homeopathy for insomnia: a systematic review of research evidence|journal=Sleep Med Rev.|year=2010|month=Oct|volume=14|issue=5|pages=329–37|pmid=20223686|doi=10.1016/j.smrv.2009.11.005|last1=Cooper|first1=KL}}</ref> |
|||
===Mind/body medicine=== |
|||
The use of evidence-based mind-body therapies can alleviate depression severity. <ref>{{cite journal|coauthors=D'Silva S, Poscablo C, Habousha R, Kogan M, Kligler B.|title=Mind-body medicine therapies for a range of depression severity: a systematic review|journal=Psychosomatics.|year=2012|month=Sep-Oct;|volume=53|issue=5|pages=407–23|pmid=22902090|doi=10.1016/j.psym.2012.04.006|last1=d'Silva|first1=S}}</ref> Mindfulness and acceptance-based interventions are associated with robust and substantial reductions in symptoms of anxiety and comorbid depressive symptoms. <ref>{{cite journal|coauthors=Vøllestad J, Nielsen MB, Nielsen GH.|title=Mindfulness- and acceptance-based interventions for anxiety disorders: a systematic review and meta-analysis.|journal=Br J Clin Psychol.|year=2012|month=Sept|volume=51|issue=3|pages=239-60.|pmid=22803933|accessdate=2 March 2013}}</ref> There is some efficacy of meditative therapies in reducing anxiety symptoms, which has important clinical implications for applying meditative techniques in treating anxiety. <ref>{{cite journal|coauthors=Chen KW, Berger CC, Manheimer E, Forde D, Magidson J, Dachman L, Lejuez CW.|title=Meditative therapies for reducing anxiety: a systematic review and meta-analysis of randomized controlled trials.|journal=Depress Anxiety|year=2012|month=July|volume=29|issue=7|pages=545-62|pmid=22700446|accessdate=2 March 2013}}</ref> |
|||
===Yoga=== |
|||
Yoga may be superior to conventional physical-activity interventions in elderly people. <ref>{{cite journal|coauthors=Patel NK, Newstead AH, Ferrer RL.|title=The effects of yoga on physical functioning and health related quality of life in older adults: a systematic review and meta-analysis|journal=J Altern Complement Med. 902-17|year=2012|volume=18|issue=10|pages=902–17|pmid=22909385|doi=10.1089/acm.2011.0473|last1=Patel|first1=NK}}</ref> In addition, Yoga therapy has been found to reduce high blood pressure but it has also been demonstrated to effectively reduce blood glucose level, cholesterol level, and body weight.<ref>{{cite journal|coauthors=Okonta NR.|title=Does yoga therapy reduce blood pressure in patients with hypertension?: an integrative review|journal=Holist Nurs Pract.|year=2012|month=May-June|volume=26|issue=3|pages=137–141|pmid=22517349|last1=Okonta|first1=NR|doi=10.1097/HNP.0b013e31824ef647}}</ref> and may effective as an ancillary treatment of neurological and psychiatric disorders <ref>{{cite journal|coauthors=Meyer HB, Katsman A, Sones AC, Auerbach DE, Ames D, Rubin RT.|title=Yoga as an ancillary treatment for neurological and psychiatric disorders: a review|journal=J Neuropsychiatry Clin Neurosci.|year=2012|volume=24|issue=2|pages=152–164|pmid=22772663|last1=Meyer|first1=HB|doi=10.1176/appi.neuropsych.11040090}}</ref> |
|||
==Testing== |
==Testing== |
||
| Line 283: | Line 285: | ||
:Contrary to much popular and scientific writing, many alternative cancer treatments have been investigated in good-quality clinical trials, and they have been shown to be ineffective. In this article, clinical trial data on a number of alternative cancer cures including Livingston-Wheeler, Di Bella Multitherapy, antineoplastons, vitamin C, hydrazine sulfate, [[Laetrile]], and psychotherapy are reviewed. The label "unproven" is inappropriate for such therapies; it is time to assert that many alternative cancer therapies have been "disproven."<ref name=Vickers_disproven>{{cite journal | doi = 10.3322/canjclin.54.2.110 | author = Andrew Vickers PhD | year = 2004 | title = Alternative Cancer Cures: "Unproven" or "Disproven"? | url = http://onlinelibrary.wiley.com/doi/10.3322/canjclin.54.2.110/full | journal = [[CA Cancer J Clin]] | volume = 54 | issue = 2| pages = 110–118 | pmid=15061600}}</ref> |
:Contrary to much popular and scientific writing, many alternative cancer treatments have been investigated in good-quality clinical trials, and they have been shown to be ineffective. In this article, clinical trial data on a number of alternative cancer cures including Livingston-Wheeler, Di Bella Multitherapy, antineoplastons, vitamin C, hydrazine sulfate, [[Laetrile]], and psychotherapy are reviewed. The label "unproven" is inappropriate for such therapies; it is time to assert that many alternative cancer therapies have been "disproven."<ref name=Vickers_disproven>{{cite journal | doi = 10.3322/canjclin.54.2.110 | author = Andrew Vickers PhD | year = 2004 | title = Alternative Cancer Cures: "Unproven" or "Disproven"? | url = http://onlinelibrary.wiley.com/doi/10.3322/canjclin.54.2.110/full | journal = [[CA Cancer J Clin]] | volume = 54 | issue = 2| pages = 110–118 | pmid=15061600}}</ref> |
||
==Safety== |
== Safety == |
||
{{See also|List of herbs with known adverse effects}} |
{{See also|List of herbs with known adverse effects}} |
||
=== Adequacy of Regulation and CAM Safety === |
|||
There is general agreement that acupuncture is safe when administered by well-trained practitioners using sterile needles<ref name="NCCAM2006-Acupuncture">{{cite web |title=Acupuncture |url=http://nccam.nih.gov/health/acupuncture/ |publisher=US [[National Center for Complementary and Alternative Medicine]] |year=2006 |accessdate=2006-03-02| archiveurl= http://web.archive.org/web/20060208042446/http://nccam.nih.gov/health/acupuncture/| archivedate= 8 February 2006 <!--DASHBot-->| deadurl= no}}</ref><ref name="pmid12801494">{{cite journal |last1=Ernst |first1=G |last2=Strzyz |first2=H |last3=Hagmeister |first3=H |title=Incidence of adverse effects during acupuncture therapy—a multicentre survey |journal=Complementary Therapies in Medicine |volume=11 |issue=2 |pages=93–7 |year=2003 |pmid=12801494 |doi=10.1016/S0965-2299(03)00004-9}}</ref><ref name="pmid12564354"/><ref name = "pmid22106073">{{cite pmid | 22106073}}</ref> and carries a very low risk of serious [[adverse effects]].<ref name = "pmid15551936" /> There is considerable debate regarding the safety of spinal manipulation, particularly with the upper [[cervical spine]].<ref name=Ernst-adverse>{{cite journal|pmid=17606755|doi=10.1258/jrsm.100.7.330|laysummary=http://www.medicalnewstoday.com/articles/75754.php|laysource=Med News Today|laydate=2 July 2007|year=2007|month=Jul|last1=Ernst|first1=E|title=Adverse effects of spinal manipulation: a systematic review|volume=100|issue=7|pages=330–8|issn=0141-0768|journal=Journal of the Royal Society of Medicine|pmc=1905885}}</ref> Although serious injuries and fatal consequences can occur and may be under-reported,<ref name=Ernst-death/> these are generally considered to be rare as spinal manipulation is relatively safe<ref>{{cite journal|coauthors=Rubinstein SM, Terwee CB, Assendelft WJ, de Boer MR, van Tulder MW.|title=Spinal manipulative therapy for acute low-back pain.|journal=Cochrane Database Syst Rev|year=2012|month=Sept|volume=12|issue=9|pmid=22972127|accessdate=11 February 2013}}</ref> when employed skillfully and appropriately.<ref name=WHO-guidelines/> |
|||
One of the commonly voiced concerns about complementary alternative medicine (CAM) is the manner in which is regulated. There have been significant developments in how CAMs should be assessed prior to re-sale in the United Kingdom and the European Union (EU) in the last 2 years. Despite this, it has been suggested that current regulatory bodies have been ineffective in preventing deception of patients as many companies have re-labelled their drugs to avoid the new laws.<ref>{{cite journal|last=Colquhoun|first=Professor David|title=Regulation of Alternative Medicine ‐ why it doesn’t work.|journal=Scottish Universities Medical Journal|year=2012|month=October|volume=1 (EPub series)|issue=16|pages=1–9|url=http://sumj.dundee.ac.uk/data/uploads/epub-article/016-sumj.epub.pdf|accessdate=25 November}}</ref> There is no general consensus about how to balance consumer protection (from false claims, toxicity, and advertising) with freedom to choose remedies. |
|||
Advocates of CAM suggest that regulation of the industry will adversely affect patients looking for alternative ways to manage their symptoms, even if many of the benefits may represent the placebo affect.<ref>{{cite journal|last=Connelly|first=P|title=The Ethics of Acupuncture|journal=Scottish Universities Medical Journal|year=2012|month=August|volume=1|issue=2|pages=165–169|url=http://sumj.dundee.ac.uk/data/uploads/volume2/sumjv1i2p.165-169.pdf}}</ref> Some contend that alternative medicines should not require any more regulation than over-the-counter medicines that can also be toxic in overdose (such as paracetamol).<ref>{{cite journal|last=Malcolm|first=Dr R|title=Small but Intriguing - The Unfolding Story of Homeopathic Medicine|journal=Scottish Universities Medical Journal|year=2012|month=October|volume=1 (EPub series)|issue=15|pages=1–7|url=http://sumj.dundee.ac.uk/data/uploads/epub-article/015-sumj.epub.pdf|accessdate=2012-11-30}}</ref> |
|||
===Adequacy of regulation and CAM safety=== |
|||
One of the commonly voiced concerns about complementary alternative medicine (CAM) is the manner in which is regulated. There have been significant developments in how CAMs should be assessed prior to re-sale in the United Kingdom and the European Union (EU) in the last 2 years. Despite this, it has been suggested that current regulatory bodies have been ineffective in preventing deception of patients as many companies have re-labelled their drugs to avoid the new laws.<ref>{{cite journal|last=Colquhoun|first=Professor David|title=Regulation of Alternative Medicine ‐ why it doesn't work|journal=Scottish Universities Medical Journal|year=2012|month=October|volume=1 (EPub series)|issue=16|pages=1–9|url=http://sumj.dundee.ac.uk/data/uploads/epub-article/016-sumj.epub.pdf|accessdate=25 November}}</ref> There is no general consensus about how to balance consumer protection (from false claims, toxicity, and advertising) with freedom to choose remedies. |
|||
==== Interactions with conventional pharmaceuticals ==== |
|||
Advocates of CAM suggest that regulation of the industry will adversely affect patients looking for alternative ways to manage their symptoms, even if many of the benefits may represent the placebo affect.<ref>{{cite journal|last=Connelly|first=P|title=The Ethics of Acupuncture|journal=Scottish Universities Medical Journal|year=2012|month=August|volume=1|issue=2|pages=165–169|url=http://sumj.dundee.ac.uk/data/uploads/volume2/sumjv1i2p.165-169.pdf}}</ref> Some contend that alternative medicines should not require any more regulation than over-the-counter medicines that can also be toxic in overdose (such as paracetamol).<ref>{{cite journal|last=Malcolm|first=Dr R|title=Small but Intriguing — The Unfolding Story of Homeopathic Medicine|journal=Scottish Universities Medical Journal|year=2012|month=October|volume=1 (EPub series)|issue=15|pages=1–7|url=http://sumj.dundee.ac.uk/data/uploads/epub-article/015-sumj.epub.pdf|accessdate=2012-11-30}}</ref> |
|||
Forms of alternative medicine that are biologically active can be dangerous even when used in conjunction with conventional medicine. Examples include immuno-augmentation therapy, shark cartilage, bioresonance therapy, oxygen and ozone therapies, insulin potentiation therapy. Some herbal remedies can cause dangerous interactions with chemotherapy drugs, radiation therapy, or anesthetics during surgery, among other problems.<ref name=autogenerated2>{{cite journal |author=Cassileth BR, Deng G |title=Complementary and alternative therapies for cancer |journal=The Oncologist |volume=9 |issue=1 |pages=80–9 |year=2004 |pmid=14755017 |doi=10.1634/theoncologist.9-1-80}}</ref> An anecdotal example of these dangers was reported by Associate Professor Alastair MacLennan of Adelaide University, Australia regarding a patient who almost bled to death on the operating table after neglecting to mention that she had been taking "natural" potions to "build up her strength" before the operation, including a powerful anticoagulant that nearly caused her death.<ref name='BenHills'>{{cite web|url=http://benhills.com/articles/articles/MED06a.html |title=Fake healers. Why Australia's $1 billion-a-year alternative medicine industry is ineffective and out of control. |accessdate = 2008-03-06 |last=Hills |first=Ben |work=Medical Mayhem }}</ref> |
|||
====Interactions with conventional pharmaceuticals==== |
|||
Forms of alternative medicine that are biologically active can be dangerous even when used in conjunction with conventional medicine. Examples include immuno-augmentation therapy, shark cartilage, bioresonance therapy, oxygen and ozone therapies, insulin potentiation therapy. Some herbal remedies can cause dangerous interactions with chemotherapy drugs, radiation therapy, or anesthetics during surgery, among other problems.<ref name=autogenerated2>{{cite journal |author=Cassileth BR, Deng G |title=Complementary and alternative therapies for cancer |journal=The Oncologist |volume=9 |issue=1 |pages=80–9 |year=2004 |pmid=14755017 |doi=10.1634/theoncologist.9-1-80}}</ref> An anecdotal example of these dangers was reported by Associate Professor Alastair MacLennan of Adelaide University, Australia regarding a patient who almost bled to death on the operating table after neglecting to mention that she had been taking "natural" potions to "build up her strength" before the operation, including a powerful anticoagulant that nearly caused her death.<ref name='BenHills'>{{cite web|url=http://benhills.com/articles/articles/MED06a.html |title=Fake healers. Why Australia's $1 billion-a-year alternative medicine industry is ineffective and out of control |accessdate = 2008-03-06 |last=Hills |first=Ben |work=Medical Mayhem }}</ref> |
|||
To ''ABC Online'', MacLennan also gives another possible mechanism: |
To ''ABC Online'', MacLennan also gives another possible mechanism: |
||
:And lastly {{sic}} there's the cynicism and disappointment and depression that some patients get from going on from one alternative medicine to the next, and they find after three months the placebo effect wears off, and they're disappointed and they move on to the next one, and they're disappointed and disillusioned, and that can create depression and make the eventual treatment of the patient with anything effective difficult, because you may not get compliance, because they've seen the failure so often in the past.|<ref name='ABC_Maclennan'>{{cite news | first=Norman | last=Swan | coauthors= | title=Alternative Medicine |
:And lastly {{sic}} there's the cynicism and disappointment and depression that some patients get from going on from one alternative medicine to the next, and they find after three months the placebo effect wears off, and they're disappointed and they move on to the next one, and they're disappointed and disillusioned, and that can create depression and make the eventual treatment of the patient with anything effective difficult, because you may not get compliance, because they've seen the failure so often in the past.|<ref name='ABC_Maclennan'>{{cite news | first=Norman | last=Swan | coauthors= | title=Alternative Medicine – Part Three | date=2000-10-02 | publisher=ABC Radio National | url =http://www.abc.net.au/rn/talks/8.30/helthrpt/stories/s195441.htm | work =The Health Report | pages = | accessdate = 2008-03-06 | language = | archiveurl= http://web.archive.org/web/20080306230537/http://www.abc.net.au/rn/talks/8.30/helthrpt/stories/s195441.htm| archivedate= 6 March 2008 <!--DASHBot-->| deadurl= no}}</ref> |
||
==== Potential side-effects ==== |
|||
Conventional treatments are subjected to testing for undesired [[Adverse effect (medicine)|side-effects]], whereas alternative treatments, in general, are not subjected to such testing at all. Any treatment – whether conventional or alternative – that has a biological or psychological effect on a patient may also have potential to possess dangerous biological or psychological side-effects. Attempts to refute this fact with regard to alternative treatments sometimes use the ''[[appeal to nature]]'' fallacy, i.e., "that which is natural cannot be harmful". |
|||
An exception to the normal thinking regarding side-effects is [[Homeopathy]]. Since 1938, the [[U.S. Food and Drug Administration]] (FDA) has regulated homeopathic products in "several significantly different ways from other drugs."<ref name=Stehlin>Isadora Stehlin. "[http://web.archive.org/web/20071012070120/http://www.fda.gov/fdac/features/096_home.html Homeopathy: Real Medicine or Empty Promises?]" – FDA Consumer magazine (December 1996)</ref> Homeopathic preparations, termed "remedies," are extremely dilute, often far beyond the point where a single molecule of the original active (and possibly toxic) ingredient is likely to remain. They are, thus, considered safe on that count, but "their products are exempt from good manufacturing practice requirements related to expiration dating and from finished product testing for identity and strength," and their alcohol concentration may be much higher than allowed in conventional drugs.<ref name=Stehlin/> |
|||
====Potential side-effects==== |
|||
Conventional treatments are subjected to testing for undesired [[Adverse effect (medicine)|side-effects]], whereas alternative treatments, in general, are not subjected to such testing at all. Any treatment – whether conventional or alternative – that has a biological or psychological effect on a patient may also have potential to possess dangerous biological or psychological side-effects. Attempts to refute this fact with regard to alternative treatments sometimes use the ''[[appeal to nature]]'' fallacy, i.e., "that which is natural cannot be harmful". |
|||
==== Treatment delay ==== |
|||
An exception to the normal thinking regarding side-effects is [[Homeopathy]]. Since 1938, the [[U.S. Food and Drug Administration]] (FDA) has regulated homeopathic products in "several significantly different ways from other drugs."<ref name=Stehlin>Isadora Stehlin. "[http://web.archive.org/web/20071012070120/http://www.fda.gov/fdac/features/096_home.html Homeopathy: Real Medicine or Empty Promises?]" – FDA Consumer magazine (December 1996)</ref> Homeopathic preparations, termed "remedies," are extremely dilute, often far beyond the point where a single molecule of the original active (and possibly toxic) ingredient is likely to remain. They are, thus, considered safe on that count, but "their products are exempt from good manufacturing practice requirements related to expiration dating and from finished product testing for identity and strength," and their alcohol concentration may be much higher than allowed in conventional drugs.<ref name=Stehlin/> |
|||
Those having experienced or perceived success with one alternative therapy for a minor ailment may be convinced of its efficacy and persuaded to extrapolate that success to some other alternative therapy for a more serious, possibly life-threatening illness.<ref>{{cite journal|url=http://content.nejm.org/cgi/content/extract/354/7/731 |title=NEJM – Drug-Related Hepatotoxicity |doi=10.1056/NEJMra052270 |publisher=Content.nejm.org |date=2006-05-18 |accessdate=2009-12-16|last1=Navarro|first1=Victor J.|last2=Senior|first2=John R.|journal=New England Journal of Medicine|volume=354|issue=7|pages=731–9|pmid=16481640}}</ref> For this reason, critics argue that therapies that rely on the placebo effect to define success are very dangerous. According to mental health journalist Scott Lilienfeld in 2002, "unvalidated or scientifically unsupported mental health practices can lead individuals to forgo effective treatments" and refers to this as "[[opportunity cost]]". Individuals who spend large amounts of time and money on ineffective treatments may be left with precious little of either, and may forfeit the opportunity to obtain treatments that could be more helpful. In short, even innocuous treatments can indirectly produce negative outcomes.<ref name='Lilienfeld_2002'>{{cite journal|title=Our Raison d'Être|journal=The Scientific Review of Mental Health Practice|year=2002|first=Scott O.|last=Lilienfeld|coauthors=|volume=1|issue=1|pages=|url=http://www.srmhp.org/0101/raison-detre.html|accessdate = 2008-01-28 | archiveurl = http://www.webcitation.org/5QcyAPtwV | archivedate = 2007-07-26| deadurl=no}}</ref> |
|||
====Treatment delay==== |
|||
Those having experienced or perceived success with one alternative therapy for a minor ailment may be convinced of its efficacy and persuaded to extrapolate that success to some other alternative therapy for a more serious, possibly life-threatening illness.<ref>{{cite journal|url=http://content.nejm.org/cgi/content/extract/354/7/731 |title=NEJM – Drug-Related Hepatotoxicity |doi=10.1056/NEJMra052270 |publisher=Content.nejm.org |date=2006-05-18 |accessdate=2009-12-16|last1=Navarro|first1=Victor J.|last2=Senior|first2=John R.|journal=New England Journal of Medicine|volume=354|issue=7|pages=731–9|pmid=16481640}}</ref> For this reason, critics argue that therapies that rely on the placebo effect to define success are very dangerous. According to mental health journalist Scott Lilienfeld in 2002, "unvalidated or scientifically unsupported mental health practices can lead individuals to forgo effective treatments" and refers to this as "[[opportunity cost]]". Individuals who spend large amounts of time and money on ineffective treatments may be left with precious little of either, and may forfeit the opportunity to obtain treatments that could be more helpful. In short, even innocuous treatments can indirectly produce negative outcomes.<ref name='Lilienfeld_2002'>{{cite journal|title=Our Raison d'Être|journal=The Scientific Review of Mental Health Practice|year=2002|first=Scott O.|last=Lilienfeld|coauthors=|volume=1|issue=1|pages=|url=http://www.srmhp.org/0101/raison-detre.html|accessdate = 2008-01-28 | archiveurl = http://www.webcitation.org/5QcyAPtwV | archivedate = 2007-07-26| deadurl=no}}</ref> |
|||
Between 2001 and 2003, four children died in Australia because their parents chose ineffective naturopathic, homeopathic, or other alternative medicines and diets rather than conventional therapies.<ref name=ineffecive>{{cite news |
Between 2001 and 2003, four children died in Australia because their parents chose ineffective naturopathic, homeopathic, or other alternative medicines and diets rather than conventional therapies.<ref name=ineffecive>{{cite news |
||
| Line 322: | Line 325: | ||
--> |
--> |
||
====Unconventional cancer "cures"==== |
==== Unconventional cancer "cures" ==== |
||
Perhaps because many forms of [[cancer]] are difficult or impossible to cure, there have always been many therapies offered outside of conventional cancer treatment centers and based on theories not found in [[biomedicine]]. These alternative cancer cures have often been described as "unproven," suggesting that appropriate clinical trials have not been conducted and that the therapeutic value of the treatment is unknown. However, many alternative cancer treatments have been investigated in good-quality clinical trials, and they have been shown to be ineffective. |
Perhaps because many forms of [[cancer]] are difficult or impossible to cure, there have always been many therapies offered outside of conventional cancer treatment centers and based on theories not found in [[biomedicine]]. These alternative cancer cures have often been described as "unproven," suggesting that appropriate clinical trials have not been conducted and that the therapeutic value of the treatment is unknown. However, many alternative cancer treatments have been investigated in good-quality clinical trials, and they have been shown to be ineffective. |
||
<ref name=Vickers>{{cite journal |last1=Vickers |first1=A. |title=Alternative Cancer Cures: 'Unproven' or 'Disproven'? |journal=CA |volume=54 |issue=2 |pages=110–8 |year=2004 |pmid=15061600 |doi=10.3322/canjclin.54.2.110 | url=http://onlinelibrary.wiley.com/doi/10.3322/canjclin.54.2.110/full }}</ref> |
<ref name=Vickers>{{cite journal |last1=Vickers |first1=A. |title=Alternative Cancer Cures: 'Unproven' or 'Disproven'? |journal=CA |volume=54 |issue=2 |pages=110–8 |year=2004 |pmid=15061600 |doi=10.3322/canjclin.54.2.110 | url=http://onlinelibrary.wiley.com/doi/10.3322/canjclin.54.2.110/full }}</ref> |
||
===Research funding=== |
=== Research funding === |
||
Although the Dutch government funded CAM research between 1986 and 2003, it formally ended funding in 2006.<ref>{{cite journal |author=Renckens CN |title=A Dutch view of the ''science'' of CAM 1986--2003 |journal=Eval Health Prof |volume=32 |issue=4 |pages=431–50 |year=2009 |month=December |pmid=19926606 |doi=10.1177/0163278709346815 |url=}}</ref> |
Although the Dutch government funded CAM research between 1986 and 2003, it formally ended funding in 2006.<ref>{{cite journal |author=Renckens CN |title=A Dutch view of the ''science'' of CAM 1986--2003 |journal=Eval Health Prof |volume=32 |issue=4 |pages=431–50 |year=2009 |month=December |pmid=19926606 |doi=10.1177/0163278709346815 |url=}}</ref> |
||
==Appeal== |
==Appeal== |
||
A study published in 1998<ref name="Astin">{{cite journal |author=Astin JA |title=Why patients use alternative medicine: results of a national study |journal=JAMA |volume=279 |issue=19 |pages=1548–53 |year=1998 |month=May |pmid=9605899 |doi=10.1001/jama.279.19.1548}}</ref> indicates that a majority of alternative medicine use was in conjunction with standard medical treatments. Approximately 4.4 percent of those studied used alternative medicine as a replacement for conventional medicine. The research found that those having used alternative medicine tended to have higher education or report poorer health status. Dissatisfaction with conventional medicine was not a meaningful factor in the choice, but rather the majority of alternative medicine users appear to be doing so largely because "they find these healthcare alternatives to be more congruent with their own values, beliefs, and philosophical orientations toward health and life." In particular, subjects reported a holistic orientation to health, a transformational experience that changed their worldview, identification with a number of groups committed to environmentalism, feminism, psychology, and/or spirituality and personal growth, or that they were suffering from a variety of common and minor ailments – notable ones being anxiety, back problems, and chronic pain. |
|||
A study published in 1998<ref name="Astin">{{cite journal |author=Astin JA |title=Why patients use alternative medicine: results of a national study |journal=JAMA |volume=279 |issue=19 |pages=1548–53 |year=1998 |month=May |pmid=9605899 |doi=10.1001/jama.279.19.1548}}</ref> indicates that a majority of alternative medicine use was in conjunction with standard medical treatments. Approximately 4.4 percent of those studied used alternative medicine as a replacement for conventional medicine. The research found that those having used alternative medicine tended to have higher education or report poorer health status. Dissatisfaction with conventional medicine was not a meaningful factor in the choice, but rather the majority of alternative medicine users appear to be doing so largely because "they find these healthcare alternatives to be more congruent with their own values, beliefs, and philosophical orientations toward health and life." In particular, subjects reported a holistic orientation to health, a transformational experience that changed their worldview, identification with a number of groups committed to environmentalism, feminism, psychology, and/or spirituality and personal growth, or that they were suffering from a variety of common and minor ailments – notable ones being anxiety, back problems, and chronic pain. |
|||
Authors have speculated on the socio-cultural and psychological reasons for the appeal of alternative medicines among that minority using them ''in lieu'' of conventional medicine. There are several socio-cultural reasons for the interest in these treatments centered on the low level of [[scientific literacy]] among the public at large and a concomitant increase in [[antiscience|antiscientific]] attitudes and [[new age]] [[mysticism]].<ref name=Beyerstein /> Related to this are vigorous [[advertising|marketing]]<ref name=Weber>{{cite journal |author=Weber DO |title=Complementary and alternative medicine. Considering the alternatives |journal=Physician Executive |volume=24 |issue=6 |pages=6–14 |year=1998 |pmid=10351720}}</ref> of extravagant claims by the alternative medical community combined with inadequate media scrutiny and attacks on critics.<ref name=Beyerstein2>{{cite journal |author=Beyerstein BL |title=Alternative medicine and common errors of reasoning |journal=Academic Medicine |volume=76 |issue=3 |pages=230–7 |year=2001 |month=March |pmid=11242572 |doi=10.1097/00001888-200103000-00009}}</ref><ref name=Beyerstein>{{cite journal|author=Beyerstein BL|url=http://www.sram.org/0302/bias.html|title=Psychology and 'Alternative Medicine' Social and Judgmental Biases That Make Inert Treatments Seem to Work|journal=The Scientific Review of Alternative Medicine|year=1999|volume=3|issue=2|accessdate=2008-07-07}}</ref> |
Authors have speculated on the socio-cultural and psychological reasons for the appeal of alternative medicines among that minority using them ''in lieu'' of conventional medicine. There are several socio-cultural reasons for the interest in these treatments centered on the low level of [[scientific literacy]] among the public at large and a concomitant increase in [[antiscience|antiscientific]] attitudes and [[new age]] [[mysticism]].<ref name=Beyerstein /> Related to this are vigorous [[advertising|marketing]]<ref name=Weber>{{cite journal |author=Weber DO |title=Complementary and alternative medicine. Considering the alternatives |journal=Physician Executive |volume=24 |issue=6 |pages=6–14 |year=1998 |pmid=10351720}}</ref> of extravagant claims by the alternative medical community combined with inadequate media scrutiny and attacks on critics.<ref name=Beyerstein2>{{cite journal |author=Beyerstein BL |title=Alternative medicine and common errors of reasoning |journal=Academic Medicine |volume=76 |issue=3 |pages=230–7 |year=2001 |month=March |pmid=11242572 |doi=10.1097/00001888-200103000-00009}}</ref><ref name=Beyerstein>{{cite journal|author=Beyerstein BL|url=http://www.sram.org/0302/bias.html|title=Psychology and 'Alternative Medicine' Social and Judgmental Biases That Make Inert Treatments Seem to Work|journal=The Scientific Review of Alternative Medicine|year=1999|volume=3|issue=2|accessdate=2008-07-07}}</ref> |
||
| Line 344: | Line 350: | ||
CAM's popularity may be related to other factors which [[Edzard Ernst]] mentions in an interview in ''[[The Independent]]'': |
CAM's popularity may be related to other factors which [[Edzard Ernst]] mentions in an interview in ''[[The Independent]]'': |
||
: Why is it so popular, then? Ernst blames the providers, customers and the doctors whose neglect, he says, has created the opening into which alternative therapists have stepped. "People are told lies. There are 40 million websites and 39.9 million tell lies, sometimes outrageous lies. They mislead cancer patients, who are encouraged not only to pay their last penny but to be treated with something that shortens their lives. "At the same time, people are gullible. It needs gullibility for the industry to succeed. It doesn't make me popular with the public, but it's the truth.<ref name="Con?">{{cite news |url=http://www.independent.co.uk/life-style/health-and-wellbeing/features/complementary-therapies-the-big-con-813248.html |title=Complementary therapies: The big con? |
: Why is it so popular, then? Ernst blames the providers, customers and the doctors whose neglect, he says, has created the opening into which alternative therapists have stepped. "People are told lies. There are 40 million websites and 39.9 million tell lies, sometimes outrageous lies. They mislead cancer patients, who are encouraged not only to pay their last penny but to be treated with something that shortens their lives. "At the same time, people are gullible. It needs gullibility for the industry to succeed. It doesn't make me popular with the public, but it's the truth.<ref name="Con?">{{cite news |url=http://www.independent.co.uk/life-style/health-and-wellbeing/features/complementary-therapies-the-big-con-813248.html |title=Complementary therapies: The big con? – The Independent |work= |accessdate= 2010-04-23| location=London | date=2008-04-22 |deadurl=yes| archiveurl= http://web.archive.org/web/20100417080412/http://www.independent.co.uk/life-style/health-and-wellbeing/features/complementary-therapies-the-big-con-813248.html| archivedate= 17 April 2010}}</ref> |
||
In a paper published in October 2010 entitled ''The public's enthusiasm for complementary and alternative medicine amounts to a critique of mainstream medicine'', Ernst describes these views in greater detail and concludes: |
In a paper published in October 2010 entitled ''The public's enthusiasm for complementary and alternative medicine amounts to a critique of mainstream medicine'', Ernst describes these views in greater detail and concludes: |
||
| Line 350: | Line 356: | ||
: [CAM] is popular. An analysis of the reasons why this is so points towards the therapeutic relationship as a key factor. Providers of CAM tend to build better therapeutic relationships than mainstream healthcare professionals. In turn, this implies that much of the popularity of CAM is a poignant criticism of the failure of mainstream healthcare. We should consider it seriously with a view of improving our service to patients.<ref>{{cite pmid| 20846193}}</ref> |
: [CAM] is popular. An analysis of the reasons why this is so points towards the therapeutic relationship as a key factor. Providers of CAM tend to build better therapeutic relationships than mainstream healthcare professionals. In turn, this implies that much of the popularity of CAM is a poignant criticism of the failure of mainstream healthcare. We should consider it seriously with a view of improving our service to patients.<ref>{{cite pmid| 20846193}}</ref> |
||
Physicians who practice complementary medicine usually discuss and advise patients as to available complementary therapies. Patients often express interest in mind-body complementary therapies because they offer a non-drug approach to treating some health conditions.<ref>{{cite journal |author=Sobel DS |title=The cost-effectiveness of mind-body medicine interventions |journal=Progress in Brain Research |volume=122 |issue= |pages=393–412 |year=2000 |pmid=10737073 |doi=10.1016/S0079-6123(08)62153-6 |series=Progress in Brain Research |isbn=978-0-444-50049-6}}</ref> Some mind-body techniques, such as cognitive-behavioral therapy, were once considered complementary medicine, but are now a part of conventional medicine in the United States.<ref>[http://www.webmd.com/balance/tc/complementary-medicine-mind-body-interventions Complementary Medicine |
Physicians who practice complementary medicine usually discuss and advise patients as to available complementary therapies. Patients often express interest in mind-body complementary therapies because they offer a non-drug approach to treating some health conditions.<ref>{{cite journal |author=Sobel DS |title=The cost-effectiveness of mind-body medicine interventions |journal=Progress in Brain Research |volume=122 |issue= |pages=393–412 |year=2000 |pmid=10737073 |doi=10.1016/S0079-6123(08)62153-6 |series=Progress in Brain Research |isbn=978-0-444-50049-6}}</ref> Some mind-body techniques, such as cognitive-behavioral therapy, were once considered complementary medicine, but are now a part of conventional medicine in the United States.<ref>[http://www.webmd.com/balance/tc/complementary-medicine-mind-body-interventions Complementary Medicine – Mind-Body Interventions], WebMD, Inc., 2007</ref> |
||
==Efforts at abstract characterizations== |
==Efforts at abstract characterizations== |
||
| Line 366: | Line 372: | ||
[http://whqlibdoc.who.int/hq/2000/WHO_EDM_TRM_2000.1.pdf]</ref> |
[http://whqlibdoc.who.int/hq/2000/WHO_EDM_TRM_2000.1.pdf]</ref> |
||
In a consensus report released in 2005, entitled ''Complementary and Alternative Medicine in the United States'', the [[Institute of Medicine]] (IOM) described complementary and alternative medicine (CAM) as health systems, modalities, and practices and their accompanying theories and beliefs, other than those intrinsic to the dominant health system of a particular society or culture in a given historical period.<ref name=IOM>{{cite web |url=http://iom.edu/Reports/2005/Complementary-and-Alternative-Medicine-in-the-United-States.aspx |title=Complementary and Alternative Medicine in the United States |publisher=United States [[Institute of Medicine]] |pages=16–20 |date=12 January 2005 |quote=Complementary and alternative medicine (CAM) is a broad domain of resources that encompasses health systems, modalities, and practices and their accompanying theories and beliefs, other than those intrinsic to the dominant health system of a particular society or culture in a given historical period. CAM includes such resources perceived by their users as associated with positive health outcomes. Boundaries within CAM and between the CAM domain and the domain of the dominant system are not always sharp or fixed. |accessdate=2011-01-18 }}</ref> Similar wording has been adopted by the Cochrane Collaboration,<ref name=Zollman/><ref name=Cochranedefinition /> and official government bodies such as the UK Department of Health.<ref>{{cite web |url=http://www.dh.gov.uk/en/Publichealth/Healthimprovement/Complementaryandalternativemedicine/index.htm |title=Complementary and alternative medicine : Department of Health |
In a consensus report released in 2005, entitled ''Complementary and Alternative Medicine in the United States'', the [[Institute of Medicine]] (IOM) described complementary and alternative medicine (CAM) as health systems, modalities, and practices and their accompanying theories and beliefs, other than those intrinsic to the dominant health system of a particular society or culture in a given historical period.<ref name=IOM>{{cite web |url=http://iom.edu/Reports/2005/Complementary-and-Alternative-Medicine-in-the-United-States.aspx |title=Complementary and Alternative Medicine in the United States |publisher=United States [[Institute of Medicine]] |pages=16–20 |date=12 January 2005 |quote=Complementary and alternative medicine (CAM) is a broad domain of resources that encompasses health systems, modalities, and practices and their accompanying theories and beliefs, other than those intrinsic to the dominant health system of a particular society or culture in a given historical period. CAM includes such resources perceived by their users as associated with positive health outcomes. Boundaries within CAM and between the CAM domain and the domain of the dominant system are not always sharp or fixed. |accessdate=2011-01-18 }}</ref> Similar wording has been adopted by the Cochrane Collaboration,<ref name=Zollman/><ref name=Cochranedefinition /> and official government bodies such as the UK Department of Health.<ref>{{cite web |url=http://www.dh.gov.uk/en/Publichealth/Healthimprovement/Complementaryandalternativemedicine/index.htm |title=Complementary and alternative medicine : Department of Health – Public health |work=Department of Health |accessdate=}}</ref> |
||
While some herbal therapies are mainstream in Europe, but are alternative in the United States.<ref name=CompAltMentalHealth>{{cite book |author=Walter R., PhD. Frontera; DeLisa, Joel A.; Gans, Bruce M.; NICHOLAS E. WALSH |title=Physical medicine and rehabilitation: principles and practice |publisher=Lippincott Williams & Wilkins |location=Hagerstwon, MD |year=2005 |pages=Chapter 19 |isbn=978-0-7817-4130-9 |oclc= |url=http://books.google.com/?id=1sWk1GYCvKoC&printsec=frontcover |accessdate=}}</ref> |
While some herbal therapies are mainstream in Europe, but are alternative in the United States.<ref name=CompAltMentalHealth>{{cite book |author=Walter R., PhD. Frontera; DeLisa, Joel A.; Gans, Bruce M.; NICHOLAS E. WALSH |title=Physical medicine and rehabilitation: principles and practice |publisher=Lippincott Williams & Wilkins |location=Hagerstwon, MD |year=2005 |pages=Chapter 19 |isbn=978-0-7817-4130-9 |oclc= |url=http://books.google.com/?id=1sWk1GYCvKoC&printsec=frontcover |accessdate=}}</ref> |
||
===Special terminology used by selected individuals=== |
===Special terminology used by selected individuals=== |
||
Two advocates of integrative medicine claim that it also addresses alleged problems with medicine based on science, which are not addressed by CAM; [[Ralph Snyderman]] and [[Andrew Weil]] state that "integrative medicine is not synonymous with complementary and alternative medicine. It has a far larger meaning and mission in that it calls for restoration of the focus of medicine on health and healing and emphasizes the centrality of the patient-physician relationship."<ref name= |
Two advocates of integrative medicine claim that it also addresses alleged problems with medicine based on science, which are not addressed by CAM; [[Ralph Snyderman]] and [[Andrew Weil]] state that "integrative medicine is not synonymous with complementary and alternative medicine. It has a far larger meaning and mission in that it calls for restoration of the focus of medicine on health and healing and emphasizes the centrality of the patient-physician relationship."<ref name=Snyderman>{{cite journal |author=Snyderman R, Weil AT |title=Integrative medicine: bringing medicine back to its roots |journal=Archives of Internal Medicine |volume=162 |issue=4 |pages=395–7 |year=2002 |month=February |pmid=11863470 |doi=10.1001/archinte.162.4.395}}</ref> <!-- WE CAN'T USE PROJECTIONS SEVERAL YEARS AFTER THE FACT; ALSO, THE ESTIMATE IS UNCITED In 2002, the growth estimate during the years 1995 to 2005 in the USA and other developed countries for the number of chiropractors, acupuncturists, naturopaths, and other nonphysician clinicians was double that of physicians.<ref name=Cassileth>{{cite journal | author = Cassileth, Barrie R. | title = The Role of Complementary & Alternative Medicine: Accommodating Pluralism | journal = NEJM | volume = 347 | pages = 860–861 | year = 2002 | doi = 10.1056/NEJM200209123471123 | issue = 11}}</ref>--> |
||
==Academic resources== |
== Academic resources == |
||
* [http://www.vifab.dk/uk/cochrane+and+alternative+medicine Cochrane and alternative medicine] (full lists of updated reviews found on [http://www.vifab.dk/uk Knowledge and Research Center for Alternative Medicine]) |
* [http://www.vifab.dk/uk/cochrane+and+alternative+medicine Cochrane and alternative medicine] (full lists of updated reviews found on [http://www.vifab.dk/uk Knowledge and Research Center for Alternative Medicine]) |
||
==See also== |
== See also == |
||
* [[Alternative cancer treatments]] |
* [[Alternative cancer treatments]] |
||
* [[Energy medicine]] |
* [[Energy medicine]] |
||
| Line 387: | Line 393: | ||
* [[Traditional medicine]] |
* [[Traditional medicine]] |
||
==References== |
== References == |
||
{{Reflist|2}} |
{{Reflist|2}} |
||
==Further reading== |
== Further reading == |
||
* {{cite book |
* {{cite book |
||
| last = Bausell | first = R. Barker |
| last = Bausell | first = R. Barker |
||
| Line 410: | Line 416: | ||
* {{cite book |author=Planer, Felix E. |year=1988 |title=Superstition |edition=Revised |location=Buffalo, New York |publisher=Prometheus Books |isbn=978-0-87975-494-5 |oclc=18616238}} |
* {{cite book |author=Planer, Felix E. |year=1988 |title=Superstition |edition=Revised |location=Buffalo, New York |publisher=Prometheus Books |isbn=978-0-87975-494-5 |oclc=18616238}} |
||
* {{cite web |url=http://www.cwru.edu/med/epidbio/mphp439/Sources_of_Healthcare.htm |author=Rosenfeld, Anna |title=Where Do Americans Go for Healthcare? |publisher=[[Case Western Reserve University]] |location=[[Cleveland, Ohio]] |year=circa 2000 |accessdate=23 September 2010}} |
* {{cite web |url=http://www.cwru.edu/med/epidbio/mphp439/Sources_of_Healthcare.htm |author=Rosenfeld, Anna |title=Where Do Americans Go for Healthcare? |publisher=[[Case Western Reserve University]] |location=[[Cleveland, Ohio]] |year=circa 2000 |accessdate=23 September 2010}} |
||
* {{cite book | last=Singh | first=S | authorlink =Simon Singh | coauthors=[[Edzard Ernst|Ernst E]] | year = 2008 | title = [[Trick or Treatment|Trick or treatment: The undeniable facts about alternative medicine]] | isbn =978-0-393-06661-6 <!-- isbn-status = May be invalid |
* {{cite book | last=Singh | first=S | authorlink =Simon Singh | coauthors=[[Edzard Ernst|Ernst E]] | year = 2008 | title = [[Trick or Treatment|Trick or treatment: The undeniable facts about alternative medicine]] | isbn =978-0-393-06661-6 <!-- isbn-status = May be invalid – please double check -->|oclc=181139440 | publisher = [[W. W. Norton & Company|Norton]] }}; [http://books.google.com/books?id=bZjlC2LELlIC preview at [[Google Book Search|Google Books]] ] |
||
* {{cite journal |author=Tonelli MR |title=The limits of evidence-based medicine |journal=Respiratory Care |volume=46 |issue=12 |pages=1435–40; discussion 1440–1 |year=2001 |month=December |pmid=11728302}} |
* {{cite journal |author=Tonelli MR |title=The limits of evidence-based medicine |journal=Respiratory Care |volume=46 |issue=12 |pages=1435–40; discussion 1440–1 |year=2001 |month=December |pmid=11728302}} |
||
* {{cite book |editor=Trivieri Larry, Jr. |editor2=Anderson, John W. |title=Alternative Medicine: The Definitive Guide |location=Berkeley |publisher=[[Ten Speed Press]] |year=2002 |isbn=978-1-58761-141-4}} |
* {{cite book |editor=Trivieri Larry, Jr. |editor2=Anderson, John W. |title=Alternative Medicine: The Definitive Guide |location=Berkeley |publisher=[[Ten Speed Press]] |year=2002 |isbn=978-1-58761-141-4}} |
||
| Line 416: | Line 422: | ||
* {{cite journal|author=Zalewski Z |title=Importance of philosophy of science to the history of medical thinking |journal=[[CMJ]] |year=1999 |volume=40 |issue=1 |pages=8–13 |url=http://www.bsb.mefst.hr/cmj/1999/4001/400102.htm |archiveurl = http://web.archive.org/web/20040206092548/http://www.bsb.mefst.hr/cmj/1999/4001/400102.htm |archivedate = 2004-02-06}} |
* {{cite journal|author=Zalewski Z |title=Importance of philosophy of science to the history of medical thinking |journal=[[CMJ]] |year=1999 |volume=40 |issue=1 |pages=8–13 |url=http://www.bsb.mefst.hr/cmj/1999/4001/400102.htm |archiveurl = http://web.archive.org/web/20040206092548/http://www.bsb.mefst.hr/cmj/1999/4001/400102.htm |archivedate = 2004-02-06}} |
||
===World Health Organization publication=== |
=== World Health Organization publication === |
||
* [http://apps.who.int/bookorders/anglais/detart1.jsp?sesslan=1&codlan=1&codcol=15&codcch=614 WHO Global Atlas of Traditional, Complementary and Alternative Medicine] |
* [http://apps.who.int/bookorders/anglais/detart1.jsp?sesslan=1&codlan=1&codcol=15&codcch=614 WHO Global Atlas of Traditional, Complementary and Alternative Medicine] |
||
===Journals dedicated to alternative medicine research=== |
=== Journals dedicated to alternative medicine research === |
||
* Alternative therapies in health and medicine. Aliso Viejo, CA : InnoVision Communications, c1995- NLM ID: [http://locatorplus.gov/cgi-bin/Pwebrecon.cgi?DB=local&v2=1&ti=1,1&Search_Arg=9502013&Search_Code=0359&CNT=20&SID=1 9502013] |
* Alternative therapies in health and medicine. Aliso Viejo, CA : InnoVision Communications, c1995- NLM ID: [http://locatorplus.gov/cgi-bin/Pwebrecon.cgi?DB=local&v2=1&ti=1,1&Search_Arg=9502013&Search_Code=0359&CNT=20&SID=1 9502013] |
||
* Alternative medicine review : a journal of clinical therapeutic. Sandpoint, Idaho : Thorne Research, Inc., c1996- NLM ID: [http://locatorplus.gov/cgi-bin/Pwebrecon.cgi?DB=local&v2=1&ti=1,1&Search_Arg=9705340&Search_Code=0359&CNT=20&SID=1 9705340] |
* Alternative medicine review : a journal of clinical therapeutic. Sandpoint, Idaho : Thorne Research, Inc., c1996- NLM ID: [http://locatorplus.gov/cgi-bin/Pwebrecon.cgi?DB=local&v2=1&ti=1,1&Search_Arg=9705340&Search_Code=0359&CNT=20&SID=1 9705340] |
||
| Line 435: | Line 441: | ||
* [http://www.cancer.gov/cam/ The Office of Cancer Complementary and Alternative Medicine]: U.S. [[National Cancer Institute]], National Institutes of Health |
* [http://www.cancer.gov/cam/ The Office of Cancer Complementary and Alternative Medicine]: U.S. [[National Cancer Institute]], National Institutes of Health |
||
* [http://www.vifab.dk/uk Knowledge and Research Center for Alternative Medicine]: Denmark, the Ministry of the Interior and Health |
* [http://www.vifab.dk/uk Knowledge and Research Center for Alternative Medicine]: Denmark, the Ministry of the Interior and Health |
||
* |
*[http://www.cancer.org/docroot/eto/content/eto_5_3x_guidelines_for_using_complementary_and_alternative_methods.asp Guidelines For Using Complementary and Alternative Methods]: from the [[American Cancer Society]] |
||
* [http://www.umm.edu/altmed/ Complementary and Alternative Medicine Index]: from the [[University of Maryland, Baltimore|University of Maryland Medical Center]] |
* [http://www.umm.edu/altmed/ Complementary and Alternative Medicine Index]: from the [[University of Maryland, Baltimore|University of Maryland Medical Center]] |
||
* [http://www.fammed.wisc.edu/integrative/modules Integrative Medicine Podcasts and Handouts]: Teaching modules from the [[University of Wisconsin]] Integrative Medicine Program |
* [http://www.fammed.wisc.edu/integrative/modules Integrative Medicine Podcasts and Handouts]: Teaching modules from the [[University of Wisconsin]] Integrative Medicine Program |
||
| Line 446: | Line 452: | ||
===Criticism=== |
===Criticism=== |
||
* [http://www.theness.com/what-is-complementary-and-alternative-medicine/ What is Complementary and Alternative Medicine?] – [[Steven Novella]], MD |
|||
* [http://www.theness.com/what-is-complementary-and-alternative-medicine/ What is Complementary and Alternative Medicine?] – [[Steven Novella]], MD |
|||
* [http://www.skepdic.com/althelth.html "Alternative" health practice] – [[Skeptic's Dictionary]] |
|||
* [http://www.skepdic.com/althelth.html "Alternative" health practice] – [[Skeptic's Dictionary]] |
|||
* [http://www.quackwatch.org Quackwatch.org] – [[Stephen Barrett]] (See also: [[Quackwatch]])<!--- DO NOT REMOVE! DOCUMENTATION FOR QUACKWATCH AS A RELIABLE SOURCE ABOUT CAM: Among many other sources listed on the Quackwatch article, the [[American Cancer Society]] lists Quackwatch as one of ten reputable sources of information about Alternative and Complementary Therapies in their book "Cancer Medicine",<ref name=ACS>[http://www.ncbi.nlm.nih.gov/books/bv.fcgi?indexed=google&rid=cmed6.table.18497 Reputable Sources of Information about Alternative and Complementary Therapies] – [[American Cancer Society]] {{Wayback|url=http://www.ncbi.nlm.nih.gov/books/bv.fcgi?indexed=google&rid=cmed6.table.18497|date =20090306160714}}</ref> and lists it as one of four sources for information about Alternative & Complementary Therapies in an article about on-line cancer information and support.<ref name=ACS_info>[http://www.cancer.org/docroot/ESN/content/ESN_2_4X_Cancer_information_and_support_available_online.asp Cancer Information & Support Available Online] – [[American Cancer Society]] {{Wayback|url=http://www.cancer.org/docroot/ESN/content/ESN_2_4X_Cancer_information_and_support_available_online.asp|date =20110605180613}}</ref> It also uses Quackwatch as a reference in a long series of articles on many forms of alternative medicine.<ref name=ACS_altmed_series>[http://www.google.com/search?hl=en&rlz=1T4GWYE_enUS238US238&q=quackwatch+site%3Acancer.org&btnG=Search A Google search lists a long series of articles] on many forms of alternative medicine on the [[American Cancer Society]] website that use Quackwatch as a source.</ref> --> |
|||
* [http://www.quackwatch.org Quackwatch.org] – [[Stephen Barrett]] (See also: [[Quackwatch]])<!--- DO NOT REMOVE! DOCUMENTATION FOR QUACKWATCH AS A RELIABLE SOURCE ABOUT CAM: Among many other sources listed on the Quackwatch article, the [[American Cancer Society]] lists Quackwatch as one of ten reputable sources of information about Alternative and Complementary Therapies in their book "Cancer Medicine",<ref name=ACS>[http://www.ncbi.nlm.nih.gov/books/bv.fcgi?indexed=google&rid=cmed6.table.18497 Reputable Sources of Information about Alternative and Complementary Therapies] – [[American Cancer Society]] {{Wayback|url=http://www.ncbi.nlm.nih.gov/books/bv.fcgi?indexed=google&rid=cmed6.table.18497|date =20090306160714}}</ref> and lists it as one of four sources for information about Alternative & Complementary Therapies in an article about on-line cancer information and support.<ref name=ACS_info>[http://www.cancer.org/docroot/ESN/content/ESN_2_4X_Cancer_information_and_support_available_online.asp Cancer Information & Support Available Online] – [[American Cancer Society]] {{Wayback|url=http://www.cancer.org/docroot/ESN/content/ESN_2_4X_Cancer_information_and_support_available_online.asp|date =20110605180613}}</ref> It also uses Quackwatch as a reference in a long series of articles on many forms of alternative medicine.<ref name=ACS_altmed_series>[http://www.google.com/search?hl=en&rlz=1T4GWYE_enUS238US238&q=quackwatch+site%3Acancer.org&btnG=Search A Google search lists a long series of articles] on many forms of alternative medicine on the [[American Cancer Society]] website that use Quackwatch as a source.</ref> --> |
|||
* [http://metapsychology.mentalhelp.net/poc/view_doc.php?type=book&id=4690&cn=452 ''Healing, Hype, or Harm? A Critical Analysis of Complementary or Alternative Medicine'', by Edzard Ernst (Editor) (2008), reviewed in ''Metapsychology''.] |
* [http://metapsychology.mentalhelp.net/poc/view_doc.php?type=book&id=4690&cn=452 ''Healing, Hype, or Harm? A Critical Analysis of Complementary or Alternative Medicine'', by Edzard Ernst (Editor) (2008), reviewed in ''Metapsychology''.] |
||
* [http://whatstheharm.net/ What's the harm?] Website created by Tim Farley listing cases of people harmed by various alternative treatments. |
* [http://whatstheharm.net/ What's the harm?] Website created by Tim Farley listing cases of people harmed by various alternative treatments. |
||
Revision as of 21:39, 2 March 2013
It has been suggested that this article be merged with Integrative medicine. (Discuss) Proposed since February 2013. |
| This article is part of a series on |
| Alternative medicine |
|---|
| Alternative medicine | |
|---|---|
| MeSH | D000529 |
Alternative medicine is any of a wide range of health care practices, products and therapies which, at least up to the end of the twentieth century, were typically not included in the degree courses of established medical schools teaching western medicine in the tradition of the Flexner Report or similar.[1] [2] Examples include homeopathy, Ayurveda, chiropractic and acupuncture.
Complementary medicine is alternative medicine used together with conventional medical treatment, in a belief, not proven by using scientific methods, that it increases the effectiveness, or "complements", the treatment.[3][4][5][6] CAM is the abbreviation for Complementary and alternative medicine.[7][8] Integrative medicine (or integrative health) is the combination of the practices and methods of alternative medicine with evidence-based medicine.[9]
The term alternative medicine is used in information issued by public bodies in the United States of America[10] and the United Kingdom.[11] Regulation and licensing of alternative medicine and health care providers varies from country to country, and state to state.
Introduction
Public discussion: how alternative medicine got its name
The history of alternative medicine is such that not until the end of the nineteenth century does the concept of alternative medicine as a historical category become tenable.[12] Alternative medical systems can only exist when there is an identifiable, regularized and authoritative medical orthodoxy, such as arose in the west during the nineteenth-century, to which they can function or act as an alternative. [13] According to Robert Jütte, labels used to describe health belief systems other than modern, scientific, Western medicine, are either misleading or carry a semantic load, as for example "alternative", "marginal", "fringe", "unorthodox" or "irregular",[14] and historians have had some difficulty simply to name and describe without connotative judgement. Jütte found that in the period from the mid-nineteenth century to the first two decades of the twentieth, the opposition of the developing medical establishment in Germany, based on modern scientific medicine, had resulted in the threat from homeopaths, naturopaths, mesmerists and others being stemmed by legal and organizational measures.[15]
By 1893 Johns Hopkins University Baltimore, Maryland, had opened America's first medical school devoted to teaching "German scientific medicine",[16] and such were the advances in medical science being made, including the development and application of the germ theory of disease by the chemist Louis Pasteur and the surgeon Joseph Lister, 1st Baron Lister, and of the use of X-rays (Röntgen rays), that by 1910 the Flexner Report called upon American medical schools to adhere to mainstream science in their teaching and research. This was in a belief, mentioned in the Report's introduction, that the preliminary and professional training then prevailing in medical schools should be reformed in view of the new means for diagnosing and combating disease being made available to physicians and surgeons by the sciences on which medicine depended.[17] Among putative medical practices available at the time which later became known as "alternative medicine" were homeopathy (founded in Germany in the early 19c.) and chiropractic (founded in North America in the late 19c.). These conflicted in principle with the developments in medical science upon which the Flexner reforms were based, and they have not become compatible with further advances of medical science such as listed in Timeline of medicine and medical technology, 1900-1999 and 2000-present, nor have Ayurveda, acupuncture or other kinds of alternative medicine.
At the same time "Tropical medicine" was being developed as a specialist branch of western medicine in research establishments such as Liverpool School of Tropical Medicine founded 1898, London School of Hygiene & Tropical Medicine, founded 1899 and Tulane University School of Public Health and Tropical Medicine, founded 1912. A distinction was being made between western scientific medicine and indigenous systems. An example is given by an official report about indigenous systems of medicine in Madras, India, including Ayurveda, submitted by Mohammad Usman of Madras and others in 1923. This stated that the first question the Committee considered was "to decide whether the indigenous systems of medicine were scientific or not".[18]
By the later twentieth century the term 'alternative medicine' had come into use for the purposes of public discussion,[19] but it was not always being used with the same meaning by all parties. Arnold S. Relman remarked in 1998 that in the best kind of medical practice, all proposed treatments must be tested objectively, and that in the end there will only be treatments that pass and those that do not, those that are proven worthwhile and those that are not. He asked 'Can there be any reasonable "alternative"?'(NEJM, 1998)[20]
In respect of alternative medicine since the 1970s in North America, Great Britain and elsewhere, there has been a tendency for the terms ‘alternative’ and ‘complementary’ to be used interchangeably to describe a wide diversity of therapies that attempt to use the self-healing powers of the body by amplifying natural recuperative processes to restore health. By 1990, approximately 60 million Americans had used one or more complementary or alternative therapies to address health issues, according to a nationwide survey in the United States published in 1993 by David Eisenberg. [21] A study published in the November 11, 1998 issue of the Journal of the American Medical Association reported that 42% of Americans had used complementary and alternative therapies, up from 34% in 1990.[22] However, despite the growth in patient demand for complementary medicine, most of the early alternative/complementary medical centers failed.[23]
Based on an analysis of trends in the coverage of complementary and alternative medicine (CAM) in five prestigious American medical journals during the period of reorganization within medicine (1965–1999), one writer proposed that the medical profession responded to the growth of CAM in three phases. In each phase, there were changes in the medical marketplace which influenced the type of response in the journals. The changes were such as relaxed medical licensing, the development of managed care, rising consumerism, and the establishment of the USA Office of Alternative Medicine (now National Center for Complementary and Alternative Medicine).[24] In the "condemnation" phase, from the late 1960s to the early 1970s, authors ridiculed, exaggerated the risks, and petitioned the state to contain CAM. In the "reassessment" phase (mid-1970s through early 1990s), when increased consumer utilization of CAM was prompting concern, authors pondered whether patient dissatisfaction and shortcomings in conventional care contributed to the trend. In the "integration" phase of the 1990s, struggles to outlaw CAM were abandoned, physicians began learning to work around or administer CAM, and the subjugation of CAM to scientific scrutiny became the primary means of control.[25]
Medical education (20c. to present)
Mainly as a result of reforms following the Flexner Report of 1910[26] medical education in established medical schools in the United States of America has generally not included alternative medicine as a teaching topic. Typically, their teaching is based on current practice and scientific knowledge about: anatomy, physiology, histology, embryology, neuroanatomy, pathology, pharmacology, microbiology and immunology.[27] Medical schools' teaching includes such topics as doctor-patient communication, ethics, the art of medicine,[28] and engaging in complex clinical reasoning (medical decision-making).[29] Writing in 2002, Snyderman and Weil remarked that by the early twentieth century the Flexner model had helped to create the 20th-century academic health center in which education, research and practice were inseparable. But, while this had much improved medical practice by defining with increasing certainty the pathophysiological basis of disease, a single-minded focus on the pathophysiological had diverted much of mainstream American medicine from clinical conditions which were not well understood in mechanistic terms and were not effectively treated by conventional therapies.[30]
By 2001 some form of CAM training was being offered by most medical schools in USA (at least 75 out of 125).[31] and, exceptionally, the School of Medicine of the University of Maryland, Baltimore in the state of Maryland, includes a research institute for integrative medicine (a member entity of the Cochrane Collaboration).[32] Medical schools are responsible for conferring medical degrees, but a physician typically may not legally practice medicine until licensed by the local government authority. Licensed physicians in the United States who have attended one of the established medical schools there have usually graduated Doctor of Medicine (MD).[33] All states require that applicants for MD licensure be graduates of an approved medical school and complete the United States Medical Licensing Exam (USMLE).[34]
The British Medical Association, in its publication Complementary Medicine, New Approach to Good Practice (1993), gave as a working definition of non-conventional therapies (including acupuncture, chiropractic and homeopathy): "those forms of treatment which are not widely used by the orthodox health-care professions, and the skills of which are not part of the undergraduate curriculum of orthodox medical and paramedical health-care courses".[35] By 2000 some medical schools in the United Kingdom were offering CAM familiarisation courses to undergraduate medical students while some were also offering modules specifically on CAM. [36]
Proponents and opponents
The Cochrane Collaboration Complementary Medicine Field explains its "Scope and Topics" by giving a broad and general defintion for complementary medicine as including practices and ideas which are outside the domain of conventional medicine in several countries and defined by its users as preventing or treating illness, or promoting health and well being, and which complement mainstream medicine in three ways: by contributing to a common whole, by satisfying a demand not met by conventional practices, and by diversifying the conceptual framework of medicine.[37]
Edzard Ernst, a former professor of complementary medicine, characterized the evidence for many alternative techniques as weak, nonexistent, or negative.[38] Ernst has concluded that 95% of the alternative treatments he and his team studied, including acupuncture, herbal medicine, homeopathy, and reflexology, are "statistically indistinguishable from placebo treatments", but he also believes there is something that conventional doctors can usefully learn from the chiropractors and homeopath: this is the therapeutic value of the placebo effect, one of the strangest phenomena in medicine.[39]
Proponents of an evidence-base for medicine[40] [41] [42] [43] such as the Cochrane Collaboration (founded in 1993 and from 2011 providing input for WHO resolutions) take a position that all systematic reviews of treatments, whether "mainstream" or "alternative", ought to be held to the current standards of scientific method.[44] In a study titled Development and classification of an operational definition of complementary and alternative medicine for the Cochrane Collaboration (2011) it was proposed that indicators that a therapy is accepted include government licensing of practitioners, coverage by health insurance, statements of approval by government agencies, and recommendation as part of a practice guideline; and that if something is currently a standard, accepted therapy, then it is not likely to be widely considered as CAM.[45]
In other studies or reports it has been proposed that "alternative medicine" refers to any practice (not included in the degree courses of established medical schools), that is put forward as having the healing effects of medicine, but is not based on evidence gathered with the scientific method,[46] when used independently or in place of medicine based on science (NCCAM, 2005),[47] (NCI at NHI, (2012)[48] (Borkan, 2012)[49] (Kong and others, 2005) [50] "Complementary medicine" refers to use of alternative medicine alongside conventional science based medicine, in the belief that it increases the effectiveness.[47][48][49] In Science and Technology: Public Attitudes and Public Understanding, chapter 7 of a report Science and Technology: Public Attitudes and Public Understanding, 2002, issued by a United States government agency (The National Science Foundation), it was stated that the term "alternative medicine" was there being used to refer to all treatments that had not been proven effective using scientific methods (NSF of SRS, of NSB, 2002).[51][52] Many of the claims regarding the safety and efficacy of alternative medicine are controversial. Some alternative treatments have been associated with unexpected side effects, which can be fatal.
Some opponents, focused upon health fraud, misinformation, and quackery as public health problems in the United States, are highly critical of alternative medicine, notably Wallace Sampson and Paul Kurtz founders of Scientific Review of Alternative Medicine and Stephen Barrett, co-founder of The National Council Against Health Fraud and webmaster of Quackwatch.[53] That alternative medicine has been on the rise "in countries where Western science and scientific method generally are accepted as the major foundations for healthcare, and 'evidence-based' practice is the dominant paradigm" was described as an "enigma" in the Medical Journal of Australia.[54]
Grounds for opposing alternative medicine which have been stated are:
- that it is usually based on religion, tradition, superstition, belief in supernatural energies, pseudoscience, errors in reasoning, propaganda, or fraud.[46][55][56][57]
- that alternative therapies typically lack any scientific validation, and their effectiveness is either unproved or disproved.[55][58][59] [dubious – discuss]
- that the treatments are those that are not part of the conventional, science-based healthcare system.[47][60][61][62]
- that research on alternative medicine is frequently of low quality and methodologically flawed.[63]
- that where alternative treatments are used in place of conventional science-based medicine, even with the very safest alternative medicines, failure to use or delay in using conventional science-based medicine has resulted in deaths.[64][65]
Critics say the expression is deceptive because it implies there is an effective alternative to science-based medicine, and that complementary is deceptive because the word implies that the treatment increases the effectiveness of (complements) science-based medicine, while alternative medicines which have been tested nearly always have no measurable positive effect compared to a placebo.[55][66][67][68] Despite such objections, some fields of alternative practice are regulated in a manner similar to that governing evidence-based medicine, and others have no regulation.
Alternative medicine practices and beliefs are diverse in their foundations and methodologies, and typically make use of preparations and dosages other than such as are included in the Pharmacopeia recognised by established medical schools. Methods may incorporate or base themselves on traditional medicine, folk knowledge, spiritual beliefs, ignorance or misunderstanding of scientific principles, errors in reasoning, or newly conceived approaches claiming to heal.[55][56][69] African, Caribbean, Pacific Island, Native American, and other regional cultures have traditional medical systems as diverse as their diversity of cultures.[47] A short but not comprehensive list is:
- Prayer to heal is the most common alternative medicine in many western countries, and faith healing is a part of many religions.
- Some believe that meditation affects health.[citation needed]
- Yoga as a healing practice involves stretching, exercise and meditation related to the Hindu religion, and makes claims to healing in the spiritual realm.[citation needed]
- Traditional Chinese medicine and the Ayurvedic medicine of India are complex systems developed over thousands of years, both based on regional supernatural belief systems and traditional use of herbs and other substances. [citation needed]
- Acupuncture is a part of Traditional Chinese medicine in which needles are inserted in the body to alter the flow of supernatural energy believed to propel the blood and influence health.[citation needed]
- Chiropractic manipulation of the spine was developed in the United States, and involves manipulating the spine to influence supernatural energies believed to cause disease. [citation needed]
- Homeopathy was developed in Europe before the existence of science of chemistry, which has subsequently proven the premises of homeopathy to be false.[citation needed]
- Magnets and light are used in therapies based on a misunderstanding of electricity and magnetism. [citation needed]
- Dietary supplements that are unproven by science are considered alternative medicines.[citation needed]
Examples and classes of alternative medicines

Complementary and alternative medicines include a wide range of treatments and practices. Some stem from nineteenth century North America, such as Chiropractic and Naturopathy, some, mentioned by Jütte, originated in eighteenth- and nineteenth-century Germany, such as homeopathy and hydropathy,[70] some have originated in China or India.
The following examples include some of the more common methods in use. Most therapies can be considered as part of five broad classes; biological based approaches, energy therapies, alternative medical systems, muscle and joint manipulation and mind body therapies.
Alternative Medical Systems

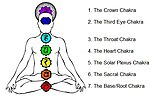
Alternative medical systems are complete health systems with their own approaches to diagnosis and treatment that differ from the conventional biomedical approach to health. Some are cultural systems such as Ayurveda and Traditional Chinese Medicine, while others, such as Homeopathy and Naturopathy are relatively recent and were developed in the West.[59]
Writing as a historian Matthew Ramsey has asked whether some counter-hegemonic medicines are better understood as manifestations of more general developments in the larger society, or as the product of a coherent alternative world view.[72]
Ayurvedic medicine
Ayurvedic medicine is a traditional medicine of India and has strong links with Buddhism and Hinduism. It is based on the belief that health is controlled by 3 "humours" with disease caused by an imbalance of these "humours". The basis of treatment has some similarities with "Western medicine". Rememdies are mainly plant based with some use of animal materials. [73] Safety concerns have been raised about Ayurveda, with two U.S. studies finding about 20 percent of Ayurvedic Indian-manufactured patent medicines contained toxic levels of heavy metals such as lead, mercury and arsenic. Other concerns include the use of herbs containing toxic compounds and the lack of quality control in Ayurvedic facilities.[74][75]
Traditional Chinese Medicine
Traditional Chinese Medicine is based on a concept of "spirit" called qi,[76] considerations of Chinese Astrology as in acupuncture,[77] traditional use of herbs and other substances found in China, and a belief that a map of the body is contained on the tongue, which reflects changes in the body.[78]
Homeopathy
Homeopathy is based on the belief that a disease can be cured by a very low dose of substance that creates similar symptoms in a healthy person. These ideas are known as 'like cures like' and the 'law of the minimum dose'[79] This conflicts with fundamental concepts of physics and chemistry and there is no good evidence from reviews of research to support its use.[80][81][82][83]
The prevailing point of view among physicians practising conventional medicine is that homeopathy is considered to be quackery.[84]
Naturopathy
Naturopathy is based on a belief in vitalism, which posits that a special energy called vital energy or vital force guides bodily processes such as metabolism, reproduction, growth, and adaptation.[85] Naturopathy favors a holistic approach with non-invasive treatment and, similar to conventional medicine, encourages minimal use of surgery and drugs.
The term "naturopathy" is derived from Greek and Latin, and literally translates as "nature disease".[86] Modern naturopathy grew out of the Natural Cure movement of Europe.[87][88] The term was coined in 1895 by John Scheel and popularized by Benedict Lust,[89] the "father of U.S. naturopathy".[90] Beginning in the 1970s, there was a revival of interest in the United States and Canada in conjunction with the holistic health movement.[90][91] Today, naturopathy is primarily practiced in the United States and Canada.[92] The scope of practice varies widely between jurisdictions, and naturopaths in unregulated jurisdictions may use the Naturopathic Doctor designation or other titles regardless of level of education.[93]
Energy Therapies
Energy therapies are designed to influence energy fields (biofields) that practitioners believe surround and enter the body. Some energy therapies involve the use of crystals, while others use magnets and electric fields. NCCAM (the US-based National Center for Complementary and Alternative Medicine) has distinguished two types of energy medicine: one, "Veritable" involving scientifically observable energy, including magnet therapy, colorpuncture and light therapy; the other "Putative" which invoke physically undetectable or unverifiable energy.[94]
Biofields


Biofield therapies are intended to influence energy fields that, it is purported, surround and penetrate the body.[47] Writers such as Carl Sagan (1934-1996), noted astrophysicist, advocate of skeptical thinking (Scientific skepticism) and author of The Demon-Haunted World: Science as a Candle in the Dark (1996), have described the lack of empirical evidence to support the existence of the putative energy fields on which these therapies are predicated.[95]
Acupuncture is a component of Traditional Chinese Medicine. In acupuncture, it is believed that a supernatural energy called qi flows through the universe and through the body, and helps propel the blood, blockage of which leads to disease.[77] It is believed that insertion of needles at various parts of the body determined by astrological calculations can restore balance to the blocked flows, and thereby cure disease.[77]
Chiropractic was developed in the belief that manipulating the spine affects the flow of a supernatural vital energy and thereby affects health and disease.
In the western version of Japanese Reiki, the palms are placed on the patient near Chakras, believed to be centers of supernatural energies, in a belief that the supernatural energies can transferred through the palms of the practitioner, to heal the patient.
Electromagnetic Fields
Bioelectromagnetic-based therapies use verifiable electromagnetic fields, such as pulsed fields, alternating-current, or direct-current fields in an unconventional manner.[47] Magnetic healing does not claim existence of supernatural energies, but asserts that magnets can be used to defy the laws of physics to influence health and disease.
Mind Body Therapies
Mind–body therapies attempt to use the mind to affect bodily symptoms and functions; examples include yoga, spirituality and relaxation.
Mind-body medicine takes a holistic approach to health that explores the interconnection between the mind, body, and spirit. It works under the premise that the mind can affect "bodily functions and symptoms".[47] Mind body medicines includes healing claims made in yoga, meditation, deep-breathing exercises, guided imagery, hypnotherapy, progressive relaxation, qi gong, and tai chi.[47]
Yoga, a method of traditional stretches, excercises, and meditations in Hinduism, may also be classified as an energy medicine insofar as its healing effects are believed by to be due to a healing "life energy" that is absorbed into the body through the breath, and is thereby believed to treat a wide variety of illnesses and complaints.[96]

Religion based healing practices, such as use of prayer and the laying of hands in Christian faith healing, rely on belief in divine intervention for healing.
Herbs, Diet and Vitamins
Biological approaches include the use of herbal medicines, special diets or very high doses of vitamins.
Substance based practices use substances found in nature such as herbs, foods, non-vitamin supplments and megavitmins, and minerals, and includes traditional herbal remedies with herbs specific to regions in which the cultural practices arose.[47] "Herbal" remedies in this case, may include use of nonherbal toxic chemicals from a nonbiological sources, such as use of the poison lead in Traditional Chinese Medicine.[97] Nonvitamin supplements include fish oil, Omega-3 fatty acid, glucosamine, echinacea, flaxseed oil or pills, and ginseng, when used under a claim to have healing effects.[97]
Body manipulation
Body-based therapies such as massage, chiropractic and osteopathy use movement and physical manipulation of joints and muscles.
Manipulative and body-based practices feature manipulation or movement of body parts, such as is done in chiropractic manipulation.
Criticism
CAM, and use of the term "alternative medicine", have been criticised, mainly in the USA, on various grounds and for various reasons in the name of consumers, physicians and research scientists, in medical journals or elsewhere. Some of the criticism makes assertions about misleading terminology or makes adverse inferences about motivation, some is on scientific grounds or errors of reasoning, or about taking resources from real medical research, or abuse of medical authority, ethics, dangerous misinformation or fraud, and some of the criticism has been with support from independent research or evidence, such as research studies of effectivenes. For instance, a US government agency, the National Science Foundation, reporting on Public Attitudes and Public Understanding in Science and Engineering Indicators 2002 stated that the term "alternative medicine" as used in the report was referring to treatments that had not been proven effective using scientific methods.[98][99]
Instances of criticism by individuals include Wallace Sampson, writing in an article in Annals of the New York Academy of Sciences, June 1995 (first published online Dec 2006).[100]. There, Sampson argued that proponents of alternative medicine often used terminology which was loose or ambiguous to create the appearance that a choice between "alternative" effective treatments existed when it did not, or that there was effectiveness or scientific validity when it did not exist, or to suggest that a dichotomy existed when it did not, or to suggest that consistency with science existed when it might not; that the term "alternative" was to suggest that a patient had a choice between effective treatments when there wsa not; that use of the word "conventional" or "mainstream" was to suggest that the difference between alternative medicine and science based medicine was the prevalence of use, rather than lack of a scientific basis of alternative medicine as compared to "conventional" or "mainstream" science based medicine; that use of the term "complementary" was to suggest that purported supernatural energies of alternative medicine could add to or complement science based medicine; that use of the term "integrative" was to suggest that supernatural beliefs can be consistently integrated with science and the result has scientific validity. Sampson, Stanford University medical professor, former chairperson of the National Council Against Health Fraud, advisor to the California Attorney General and numerous district attorneys on medical fraud, and editor of Scientific Review of Alternative Medicine, has also written that CAM is the "propagation of the absurd", and argued that alternative and complementary have been substituted for quackery, dubious and implausible.[101].
Other criticism has been that "Integrative medicine" ("integrated medicine") is used either to refer to a belief that medicine based on science can be "integrated" with practices that are not, or that a combination of alternative medical treatments with conventional science based treatments that have some scientific proof of efficacy, in which case it is identical with CAM;[9] that there is only medicine that has been adequately tested and that which has not;[102] that "There really is no such thing as alternative medicine--only medicine that has been proved to work and medicine that has not." - Arnold Relman, editor in chief emeritus of The New England Journal of Medicine;[103][full citation needed]
Another critic, with reference to government funding studies of integrating alternative medicine techniques into the mainstream, Steven Novella, a neurologist at Yale School of Medicine, wrote that it "is used to lend an appearance of legitimacy to treatments that are not legitimate." Another, Marcia Angell, former executive editor of The New England Journal of Medicine argued that it was a new name for snake oil."[104] Angell considered that critics felt that healthcare practices should be classified based solely on scientific evidence, and if a treatment had been rigorously tested and found safe and effective, science based medicine will adopt it regardless of whether it was considered "alternative" to begin with.[102] It was thus possible for a method to change categories (proven vs. unproven), based on increased knowledge of its effectiveness or lack thereof. Prominent supporters of this position include George D. Lundberg, former editor of the Journal of the American Medical Association (JAMA).[105]
Richard Dawkins, an evolutionary biologist who is not a medical practitioner of any kind nor has qualified as a physician or surgeon, has defined alternative medicine as a "set of practices that cannot be tested, refuse to be tested, or consistently fail tests."[106] He has also stated that "there is no alternative medicine. There is only medicine that works and medicine that doesn't work."[107] He has argued that if a technique is demonstrated effective in properly performed trials, it ceases to be alternative and simply becomes medicine.[108]
In an article first published in CA: A Cancer Journal for Clinicians, November/December 1999, Evaluating complementary and alternative therapies for cancer patients, Barrie R. Cassileth mentioned that a 1997 letter to the US Senate Subcommittee on Public Health and Safety which had deplored the lack of critical thinking and scientific rigor in OAM-supported research had been signed by four Nobel Laureates and other prominent scientists. (This was supported by the National Institutes of Health (NIH).)[109] In March, 2009 a Washington Post staff writer reported that the impending national discussion about broadening access to health care, improving medical practice and saving money was giving a group of scientists an opening to propose shutting down the National Center for Complementary and Alternative Medicine, quoting one of them, Steven Salzberg, a genome researcher and computational biologist at the University of Maryland, saying "One of our concerns is that NIH is funding pseudoscience." They argued that the vast majority of studies were based on fundamental misunderstandings of physiology and disease, and have shown little or no effect.[110] Stephen Barrett, founder and operator of Quackwatch, has argued that practices labeled "alternative" should be reclassified as either genuine, experimental, or questionable. Here he defines genuine as being methods that have sound evidence for safety and effectiveness, experimental as being unproven but with a plausible rationale for effectiveness, and questionable as groundless without a scientifically plausible rationale.[111] Sampson has also pointed out that CAM tolerated contradiction without thorough reason and experiment.[101] Barrett has pointed out that there is a policy at the NIH of never saying something doesn't work only that a different version or dose might give different results.[112] Barrett also expressed concern that, just because some "alternatives" have merit, there is the impression that the rest deserve equal consideration and respect even though most are worthless, since they are all classified under the one heading of alternative medicine.[111]
A group of prominent scientists argued before the federal government, USA, that plausibility of interventions such as diet, relaxation, yoga and botanical remedies, should not be used to support research on implausible interventions based on superstition and belief in the supernatural, and that the plausible methods can be studied just as well in other parts of NIH, where they should be made to compete on an equal footing with other research projects.[110] The NCCAM budget has been criticized[104] because, despite the duration and intensity of studies to measure the efficacy of alternative medicine, there had been no effective CAM treatments supported by scientific evidence as of 2002 according to the QuackWatch website.[113] Despite this, the National Center for Complementary and Alternative Medicine budget has been on a sharp sustained rise to support complementary medicine. In fact, the whole CAM field has been called by critics the SCAM.[113] There have been negative results in almost all studies conducted over ten years at a cost of $2.5 billion by the NCCAM.[114]
A research methods expert and author of "Snake Oil Science", R. Barker Bausell, has stated that "it's become politically correct to investigate nonsense."[112] There are concerns that just having NIH support is being used to give unfounded "legitimacy to treatments that are not legitimate."[110]
Use of placebos in order to achieve a placebo effect in integrative medicine has been criticized as “diverting research time, money, and other resources from more fruitful lines of investigation in order to pursue a theory that has no basis in biology”.[68][115]
Speaking of ethics, in November 2011 Edzard Ernst stated that the "level of misinformation about alternative medicine has now reached the point where it has become dangerous and unethical. So far, alternative medicine has remained an ethics-free zone. It is time to change this."[116] Ernst requested that Prince Charles recall two guides to alternative medicine published by the Foundation for Integrated Health, on the grounds that "[t]hey both contain numerous misleading and inaccurate claims concerning the supposed benefits of alternative medicine" and that "[t]he nation cannot be served by promoting ineffective and sometimes dangerous alternative treatments."[117] In general, he believes that CAM can and should be subjected to scientific testing.[44][38][118] Ernst requested that Prince Charles recall two guides to alternative medicine published by the Foundation for Integrated Health, on the grounds that "[t]hey both contain numerous misleading and inaccurate claims concerning the supposed benefits of alternative medicine" and that "[t]he nation cannot be served by promoting ineffective and sometimes dangerous alternative treatments".[44][38][117][118]
According to two writers, Wallace Sampson and K.Butler, Marketing is part of the medical training required in chiropractic educaion, and propoganda methods in alternative medicine have been traced back to those used by Hitler and Goebels in their promotion of pseudoscience in medicine.[55][119]
Another critic has argued that academic proponents of integrative medicine sometimes recommend misleading patients by using known placebo treatments in order to achieve a placebo effect.[120] However, a 2010 survey of family physicians found that 56% of respondents said they had used a placebo in clinical practice as well. Eighty-five percent of respondents believed placebos can have both psychological and physical benefits.[121][122]
Integrative medicine has been criticized in that its practitioners, trained in science based medicine, deliberately mislead patients by pretending placebos are not. "Quackademic medicine" is a pejorative term used for “integrative medicine”, which is considered to be an infiltration of quackery into academic science-based medicine.[68]
Use and regulation
Prevalence of use

Complementary and alternative medicine (CAM) has been described as a broad domain of healing resources that encompasses all health systems, modalities, and practices and their accompanying theories and beliefs, other than those intrinsic to the politically dominant health system of a particular society or culture in a given historical period. CAM includes all such practices and ideas self-defined by their users as preventing or treating illness or promoting health and well-being. Boundaries within CAM and between the CAM domain and that of the dominant system are not always sharp or fixed[123][dubious – discuss]
In respect of taxation in the U.S.A. the Internal Revenue Service has discriminated in favour of medical expenses for acupuncture and chiropractor (and others including Christian Science practitioner) but against homeopathy and the use of non-prescription required medicine.[124]
About 50% of people in developed countries use some kind of complementary and alternative medicine other than prayer for health.[125][126][127][128] About 40% of cancer patients use some form of CAM.[129] The use of alternative medicine in developed countries is increasing,[46][130][131] with a 50 percent increase in expenditures and a 25 percent increase in the use of alternative therapies between 1990 and 1997 in America.[132] Americans spend many billions on the therapies annually.[132] Most Americans used CAM to treat and/or prevent musculoskeletal conditions or other conditions associated with chronic or recurring pain.[126] In America, women were more likely than men to use CAM., with the biggest difference in use of mind-body therapies including prayer specifically for health reasons".[126] In 2008, more than 37% of American hospitals offered alternative therapies, up from 26.5 percent in 2005, and 25% in 2004.[133][134] More than 70% of the hospitals offering CAM were in urban areas.[134]
A survey of Americans found that 88 percent agreed that "there are some good ways of treating sickness that medical science does not recognize".[46] Use of magnets was the most common tool in energy medicine in America, and among users of it, 58 percent described it as at least “sort of scientific”, when it is not at all scientific.[46] In 2002, at least 60 percent of US medical schools have at least some class time spent teaching alternative therapies.[46] "Therapeutic touch," was taught at more than 100 colleges and universities in 75 countries before the practice was debunked by a nine-year-old child for a school science project.[46][46][135] In Austria and Germany complementary and alternative medicine is mainly in the hands of doctors with MDs,[7] and half or more of the American alternative practitioners are licensed MDs.[136] In Germany herbs are tightly regulated: half are prescribed by doctors and covered by health insurance.[137]
In developing nations, access to essential medicines is severely restricted by lack of resources and poverty. Traditional remedies, often closely resembling or forming the basis for alternative remedies, may comprise primary healthcare or be integrated into the healthcare system. In Africa, traditional medicine is used for 80% of primary healthcare, and in developing nations as a whole over one-third of the population lack access to essential medicines.[138]
A 1997 survey found that 13.7% of respondents in the United States had sought the services of both a medical doctor and an alternative medicine practitioner. The same survey found that 96% of respondents who sought the services of an alternative medicine practitioner also sought the services of a medical doctor in the past 12 months. Medical doctors are often unaware of their patient's use of alternative medical treatments as only 38.5% of the patients alternative therapies were discussed with their medical doctor.[130] A British telephone survey by the BBC of 1209 adults in 1998 shows that around 20% of adults in Britain had used alternative medicine in the past 12 months.[139]
Prevalence of use of specific therapies
The most common CAM therapies used in the US in 2002 were prayer (45.2%), herbalism (18.9%), breathing meditation (11.6%), meditation (7.6%), chiropractic medicine (7.5%), yoga (5.1%-6.1%), body work (5.0%), diet-based therapy (3.5%), progressive relaxation (3.0%), mega-vitamin therapy (2.8%) and Visualization (2.1%)[126][140]
In Britain, the most often used alternative therapies were Alexander technique, Aromatherapy, Bach and other flower remedies, Body work therapies including massage, Counselling stress therapies, hypnotherapy, Meditation, Reflexology, Shiatsu, Ayurvedic medicine, Nutritional medicine, and Yoga.[141]
According to the National Health Service (England), the most commonly used complementary and alternative medicines (CAM) supported by the NHS in the UK are: acupuncture, aromatherapy, chiropractic, homeopathy, massage, osteopathy and clinical hypnotherapy.[11]
"Complementary medicine treatments used for pain include: acupuncture, low-level laser therapy, meditation, aroma therapy, Chinese medicine, dance therapy, music therapy, massage, herbalism, therapeutic touch, yoga, osteopathy, chiropractic, naturopathy, and homeopathy."[142]
Palliative care
Complementary therapies are often used in palliative care or by practitioners attempting to manage chronic pain in patients. Complementary medicine is considered more acceptable in the interdisciplinary approach used in palliative care than in other areas of medicine. "From its early experiences of care for the dying, palliative care took for granted the necessity of placing patient values and lifestyle habits at the core of any design and delivery of quality care at the end of life. If the patient desired complementary therapies, and as long as such treatments provided additional support and did not endanger the patient, they were considered acceptable."[143] The non-pharmacologic interventions of complementary medicine can employ mind-body interventions designed to "reduce pain and concomitant mood disturbance and increase quality of life."[144]
Regulation
Some professions of complementary/traditional/alternative medicine, such as chiropractic medicine, have achieved full regulation in North America and other parts of the world [145] and are are regulated in a manner similar to that governing science-based medicine. In contrast, other approaches may be partially recognized and others have no regulation at all. Regulation and licensing of alternative medicine ranges widely from country to country, and state to state.[145]
Government bodies in the USA and elsewhere have published information or guidance about alternative medicine. One of those is the U.S. Food and Drug Administration (FDA), which mentions specifically homeopathic products, traditional Chinese medicine and Ayurvedic products.[146] A document which the FDA has issued for comment is headed Guidance for Industry: Complementary and Alternative Medicine Products and Their Regulation by the Food and Drug Administration, last updated 04/06/2012.[147] The document opens with three preliminary paragraphs which explain that in the document:
- - "complementary and alternative medicine" (CAM) are being used to encompass a wide array of health care practices, products, and therapies which are distinct from those used in "conventional" or "allopathic" medicine.
- - some forms of CAM, such as traditional Chinese medicine and Ayurvedic medicine, have been practiced for centuries, and others, such as electrotherapy, are of more recent origin.
- - in a publication of The Institute of Medicine it has been stated that more than one-third of American adults reported using some form of CAM and that visits to CAM providers each year exceed those to primary care physicians (Institute of Medicine, Complementary and Alternative Medicine in the United States, pages 34-35, 2005).
- - no mention (in the document) of a particular CAM therapy, practice or product should be taken as expressing FDA's support or endorsement of it or as an agency determination that a particular product is safe and effective.
Efficacy
Criteria and principles about evidence and the validity of clinical tests or trials applicable to healthcare interventions, including alternative medicine, were considered by Steven Woolf and others in a paper published in 2012 titled Developing clinical practice guidelines: types of evidence and outcomes.[148] This indicated the importance of skill, knowledge and objectivity in the design and conduct of trials and in recording and reporting the benefits, harms, and other outcomes that were considered.
The position of Arnold S. Relman, a physician who has also written on Health care reform in U.S.A., is that most varieties of "alternative" therapies that have not been proven effective in clinical trials should be among the exclusions from health care benefits prescribed by physicians.[149]
Alternative therapies lack the requisite scientific validation, and their effectiveness is either unproved or disproved.[46][55][58][59] Many of the claims regarding the efficacy of alternative medicines are controversial, since research on them is frequently of low quality and methodologically flawed.[63] Selective publication of results (misleading results from only publishing postive results, and not all results), marked differences in product quality and standardisation, and some companies making unsubstantiated claims, call into question the claims of efficacy of isolated examples where herbs may have some evidence of containing chemicals that may affect health.[150] The Scientific Review of Alternative Medicine points to confusions in the general population - a person may attribute symptomatic relief to an otherwise-ineffective therapy just because they are taking something (the placebo effect); the natural recovery from or the cyclical nature of an illness (the regression fallacy) gets misattributed to an alternative medicine being taken; a person not diagnosed with science based medicine may never originally have had a true illness diagnosed as an alternative disease category.[151]
Testing
In 2003, a project funded by the CDC identified 208 condition-treatment pairs, of which 58% had been studied by at least one randomized controlled trial (RCT), and 23% had been assessed with a meta-analysis.[152] According to a 2005 book by a US Institute of Medicine panel, the number of RCTs focused on CAM has risen dramatically. The book cites Vickers (1998), who found that many of the CAM-related RCTs are in the Cochrane register, but 19% of these trials were not in MEDLINE, and 84% were in conventional medical journals.[63]: 133
As of 2005, the Cochrane Library had 145 CAM-related Cochrane systematic reviews and 340 non-Cochrane systematic reviews. An analysis of the conclusions of only the 145 Cochrane reviews was done by two readers. In 83% of the cases, the readers agreed. In the 17% in which they disagreed, a third reader agreed with one of the initial readers to set a rating. These studies found that, for CAM, 38.4% concluded positive effect or possibly positive (12.4%) effect, 4.8% concluded no effect, 0.69% concluded harmful effect, and 56.6% concluded insufficient evidence. An assessment of conventional treatments found that 41.3% concluded positive or possibly positive effect, 20% concluded no effect, 8.1% concluded net harmful effects, and 21.3% concluded insufficient evidence. However, the CAM review used the 2004 Cochrane database, while the conventional review used the 1998 Cochrane database.[63]: 135–136
Lists of the Cochrane Reviews on alternative medicine including summaries of the results sorted by type of therapy (updated monthly) are made available at ViFABs (Knowledge and Research Center for Alternative Medicines) home page, see the lists here: http://www.vifab.dk/uk/cochrane+and+alternative+medicine
Most alternative medical treatments are not patentable, which may lead to less research funding from the private sector. In addition, in most countries, alternative treatments (in contrast to pharmaceuticals) can be marketed without any proof of efficacy—also a disincentive for manufacturers to fund scientific research.[153] Some have proposed adopting a prize system to reward medical research.[154] However, public funding for research exists. Increasing the funding for research on alternative medicine techniques is the purpose of the US National Center for Complementary and Alternative Medicine. NCCAM and its predecessor, the Office of Alternative Medicine, have spent more than $2.5 billion on such research since 1992; this research has largely not demonstrated the efficacy of alternative treatments.[112][155][156]
In the same way as for conventional therapies, drugs, and interventions, it can be difficult to test the efficacy of alternative medicine in clinical trials. In instances where an established, effective, treatment for a condition is already available, the Helsinki Declaration states that withholding such treatment is unethical in most circumstances. Use of standard-of-care treatment in addition to an alternative technique being tested may produce confounded or difficult-to-interpret results.[157]
Cancer researcher Andrew J. Vickers has stated:
- Contrary to much popular and scientific writing, many alternative cancer treatments have been investigated in good-quality clinical trials, and they have been shown to be ineffective. In this article, clinical trial data on a number of alternative cancer cures including Livingston-Wheeler, Di Bella Multitherapy, antineoplastons, vitamin C, hydrazine sulfate, Laetrile, and psychotherapy are reviewed. The label "unproven" is inappropriate for such therapies; it is time to assert that many alternative cancer therapies have been "disproven."[158]
Safety
Adequacy of Regulation and CAM Safety
One of the commonly voiced concerns about complementary alternative medicine (CAM) is the manner in which is regulated. There have been significant developments in how CAMs should be assessed prior to re-sale in the United Kingdom and the European Union (EU) in the last 2 years. Despite this, it has been suggested that current regulatory bodies have been ineffective in preventing deception of patients as many companies have re-labelled their drugs to avoid the new laws.[159] There is no general consensus about how to balance consumer protection (from false claims, toxicity, and advertising) with freedom to choose remedies.
Advocates of CAM suggest that regulation of the industry will adversely affect patients looking for alternative ways to manage their symptoms, even if many of the benefits may represent the placebo affect.[160] Some contend that alternative medicines should not require any more regulation than over-the-counter medicines that can also be toxic in overdose (such as paracetamol).[161]
Interactions with conventional pharmaceuticals
Forms of alternative medicine that are biologically active can be dangerous even when used in conjunction with conventional medicine. Examples include immuno-augmentation therapy, shark cartilage, bioresonance therapy, oxygen and ozone therapies, insulin potentiation therapy. Some herbal remedies can cause dangerous interactions with chemotherapy drugs, radiation therapy, or anesthetics during surgery, among other problems.[162] An anecdotal example of these dangers was reported by Associate Professor Alastair MacLennan of Adelaide University, Australia regarding a patient who almost bled to death on the operating table after neglecting to mention that she had been taking "natural" potions to "build up her strength" before the operation, including a powerful anticoagulant that nearly caused her death.[163]
To ABC Online, MacLennan also gives another possible mechanism:
- And lastly [sic] there's the cynicism and disappointment and depression that some patients get from going on from one alternative medicine to the next, and they find after three months the placebo effect wears off, and they're disappointed and they move on to the next one, and they're disappointed and disillusioned, and that can create depression and make the eventual treatment of the patient with anything effective difficult, because you may not get compliance, because they've seen the failure so often in the past.|[164]
Potential side-effects
Conventional treatments are subjected to testing for undesired side-effects, whereas alternative treatments, in general, are not subjected to such testing at all. Any treatment – whether conventional or alternative – that has a biological or psychological effect on a patient may also have potential to possess dangerous biological or psychological side-effects. Attempts to refute this fact with regard to alternative treatments sometimes use the appeal to nature fallacy, i.e., "that which is natural cannot be harmful".
An exception to the normal thinking regarding side-effects is Homeopathy. Since 1938, the U.S. Food and Drug Administration (FDA) has regulated homeopathic products in "several significantly different ways from other drugs."[165] Homeopathic preparations, termed "remedies," are extremely dilute, often far beyond the point where a single molecule of the original active (and possibly toxic) ingredient is likely to remain. They are, thus, considered safe on that count, but "their products are exempt from good manufacturing practice requirements related to expiration dating and from finished product testing for identity and strength," and their alcohol concentration may be much higher than allowed in conventional drugs.[165]
Treatment delay
Those having experienced or perceived success with one alternative therapy for a minor ailment may be convinced of its efficacy and persuaded to extrapolate that success to some other alternative therapy for a more serious, possibly life-threatening illness.[166] For this reason, critics argue that therapies that rely on the placebo effect to define success are very dangerous. According to mental health journalist Scott Lilienfeld in 2002, "unvalidated or scientifically unsupported mental health practices can lead individuals to forgo effective treatments" and refers to this as "opportunity cost". Individuals who spend large amounts of time and money on ineffective treatments may be left with precious little of either, and may forfeit the opportunity to obtain treatments that could be more helpful. In short, even innocuous treatments can indirectly produce negative outcomes.[64]
Between 2001 and 2003, four children died in Australia because their parents chose ineffective naturopathic, homeopathic, or other alternative medicines and diets rather than conventional therapies.[65] In all, they found 17 instances in which children were significantly harmed by a failure to use conventional medicine.
Unconventional cancer "cures"
Perhaps because many forms of cancer are difficult or impossible to cure, there have always been many therapies offered outside of conventional cancer treatment centers and based on theories not found in biomedicine. These alternative cancer cures have often been described as "unproven," suggesting that appropriate clinical trials have not been conducted and that the therapeutic value of the treatment is unknown. However, many alternative cancer treatments have been investigated in good-quality clinical trials, and they have been shown to be ineffective. [167]
Research funding
Although the Dutch government funded CAM research between 1986 and 2003, it formally ended funding in 2006.[168]
Appeal
A study published in 1998[128] indicates that a majority of alternative medicine use was in conjunction with standard medical treatments. Approximately 4.4 percent of those studied used alternative medicine as a replacement for conventional medicine. The research found that those having used alternative medicine tended to have higher education or report poorer health status. Dissatisfaction with conventional medicine was not a meaningful factor in the choice, but rather the majority of alternative medicine users appear to be doing so largely because "they find these healthcare alternatives to be more congruent with their own values, beliefs, and philosophical orientations toward health and life." In particular, subjects reported a holistic orientation to health, a transformational experience that changed their worldview, identification with a number of groups committed to environmentalism, feminism, psychology, and/or spirituality and personal growth, or that they were suffering from a variety of common and minor ailments – notable ones being anxiety, back problems, and chronic pain.
Authors have speculated on the socio-cultural and psychological reasons for the appeal of alternative medicines among that minority using them in lieu of conventional medicine. There are several socio-cultural reasons for the interest in these treatments centered on the low level of scientific literacy among the public at large and a concomitant increase in antiscientific attitudes and new age mysticism.[169] Related to this are vigorous marketing[170] of extravagant claims by the alternative medical community combined with inadequate media scrutiny and attacks on critics.[171][169]
There is also an increase in conspiracy theories toward conventional medicine and pharmaceutical companies, mistrust of traditional authority figures, such as the physician, and a dislike of the current delivery methods of scientific biomedicine, all of which have led patients to seek out alternative medicine to treat a variety of ailments.[171] Many patients lack access to contemporary medicine, due to a lack of private or public health insurance, which leads them to seek out lower-cost alternative medicine.[126] Medical doctors are also aggressively marketing alternative medicine to profit from this market.[170]
In addition to the social-cultural underpinnings of the popularity of alternative medicine, there are several psychological issues that are critical to its growth. One of the most critical is the placebo effect, which is a well-established observation in medicine.[172] Related to it are similar psychological effects such as the will to believe,[169] cognitive biases that help maintain self-esteem and promote harmonious social functioning,[169] and the post hoc, ergo propter hoc fallacy.[169]
Patients can also be averse to the painful, unpleasant, and sometimes-dangerous side effects of biomedical treatments. Treatments for severe diseases such as cancer and HIV infection have well-known, significant side-effects. Even low-risk medications such as antibiotics can have potential to cause life-threatening anaphylactic reactions in a very few individuals. Also, many medications may cause minor but bothersome symptoms such as cough or upset stomach. In all of these cases, patients may be seeking out alternative treatments to avoid the adverse effects of conventional treatments.[171][169]
Schofield et al., in a systematic review published in 2011, make ten recommendations which they think may increase the effectiveness of consultations in a conventional (here: oncology) setting, such as "Ask questions about CAM use at critical points in the illness trajectory"; "Respond to the person's emotional state"; and "Provide balanced, evidence-based advice". They suggest that this approach may address "... concerns surrounding CAM use [and] encourage informed decision-making about CAM and ultimately, improve outcomes for patients".[173]
CAM's popularity may be related to other factors which Edzard Ernst mentions in an interview in The Independent:
- Why is it so popular, then? Ernst blames the providers, customers and the doctors whose neglect, he says, has created the opening into which alternative therapists have stepped. "People are told lies. There are 40 million websites and 39.9 million tell lies, sometimes outrageous lies. They mislead cancer patients, who are encouraged not only to pay their last penny but to be treated with something that shortens their lives. "At the same time, people are gullible. It needs gullibility for the industry to succeed. It doesn't make me popular with the public, but it's the truth.[174]
In a paper published in October 2010 entitled The public's enthusiasm for complementary and alternative medicine amounts to a critique of mainstream medicine, Ernst describes these views in greater detail and concludes:
- [CAM] is popular. An analysis of the reasons why this is so points towards the therapeutic relationship as a key factor. Providers of CAM tend to build better therapeutic relationships than mainstream healthcare professionals. In turn, this implies that much of the popularity of CAM is a poignant criticism of the failure of mainstream healthcare. We should consider it seriously with a view of improving our service to patients.[175]
Physicians who practice complementary medicine usually discuss and advise patients as to available complementary therapies. Patients often express interest in mind-body complementary therapies because they offer a non-drug approach to treating some health conditions.[176] Some mind-body techniques, such as cognitive-behavioral therapy, were once considered complementary medicine, but are now a part of conventional medicine in the United States.[177]
Efforts at abstract characterizations
There is no clear and consistent definition for either alternative or complementary medicine.[63]: 17
Self-characterization
The US National Center for Complementary and Alternative Medicine (NCCAM) defines CAM as "a group of diverse medical and healthcare systems, practices, and products, that are not currently part of conventional medicine”, in a context where conventional medicine is that which is scientifically proven.[47] This definition of CAM is widely known and used and is inclusive of many different types of therapies and products.[178][179]
The Danish Knowledge and Research Center for Alternative Medicine an independent institution under the Danish Ministry of the Interior and Health (Danish abbreviation: ViFAB) uses the term “alternative medicine” for:
- Treatments performed by therapists that are not authorized healthcare professionals, where authorized healthcare professionals are those practicing what is proven by science.
- Treatments performed by authorized healthcare professionals, but those based on methods otherwise used mainly outside the healthcare system, which is based on science in Denmark. People without a healthcare authorisation must be able to perform the treatments.
Institutions
In General Guidelines for Methodologies on Research and Evaluation of Traditional Medicine, published in 2000 by the World Health Organization, complementary and alternative medicine were there defined as a broad set of health care practices that are not part of that country's own tradition and are not integrated into the dominant health care system.[62][180]
In a consensus report released in 2005, entitled Complementary and Alternative Medicine in the United States, the Institute of Medicine (IOM) described complementary and alternative medicine (CAM) as health systems, modalities, and practices and their accompanying theories and beliefs, other than those intrinsic to the dominant health system of a particular society or culture in a given historical period.[61] Similar wording has been adopted by the Cochrane Collaboration,[60][37] and official government bodies such as the UK Department of Health.[181]
While some herbal therapies are mainstream in Europe, but are alternative in the United States.[182]
Special terminology used by selected individuals
Two advocates of integrative medicine claim that it also addresses alleged problems with medicine based on science, which are not addressed by CAM; Ralph Snyderman and Andrew Weil state that "integrative medicine is not synonymous with complementary and alternative medicine. It has a far larger meaning and mission in that it calls for restoration of the focus of medicine on health and healing and emphasizes the centrality of the patient-physician relationship."[30]
Academic resources
- Cochrane and alternative medicine (full lists of updated reviews found on Knowledge and Research Center for Alternative Medicine)
See also
- Alternative cancer treatments
- Energy medicine
- Folk medicine
- Health freedom movement
- History of alternative medicine
- List of branches of alternative medicine
- Program for Evaluating Complementary Medicine
- Shakoor v Situ
- Traditional medicine
References
- ^ Peking Union Medical College is an instance of the influence of the Flexner Report outside N. America: Mary Brown Bullock, An American Transplant: The Rockefeller Foundation and the Peking Union Medical College, Berkeley: University of California Press, 1980. Top Chinese Universities in Medicine, 2012[1] Peking University Health Science Center (formerly Beijing Medical University) was the first of the kind in China to teach western medicine and train medical professionals. Top Chinese Universities in Medicine, 2012[2].
- ^ A Medical college in India is one awarding MBBS degrees (Bachelor of Medicine, Bachelor of Surgery), the course for which starts with subjects such as biochemistry, physiology, anatomy, microbiology, pathology and pharmacology, as in western medical schools.
- ^ "White House Commission on Complementary and Alternative Medicine Policy". March 2002. Archived from the original on 2011-08-25.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help)"The Commissioners believe and have repeatedly stated in this Report that our response should be to hold all systems of health and healing, including conventional and CAM, to the same rigorous standards of good science and health services research. Although the Commissioners support the provision of the most accurate information about the state of the science of all CAM modalities, they believe that it is premature to advocate the wide implementation and reimbursement of CAM modalities that are yet unproven." - ^ Ernst E. (1995). "Complementary medicine: common misconceptions". Journal of the Royal Society of Medicine. 88 (5): 244–247. PMC 1295191. PMID 7636814."Complementary medicine, defined as health care which lies for the most part outside the mainstream of conventional medicine"
- ^ Joyce CR (1994). "Placebo and complementary medicine". The Lancet. 344 (8932): 1279–1281. doi:10.1016/S0140-6736(94)90757-9.
- ^ "Science and Technology: Public Attitudes and Public Understanding Science Fiction and Pseudoscience - Belief in Alternative Medicine". National Science Foundation.
alternative medicine refers to all treatments that have not been proven effective using scientific methods
- ^ a b "Interview with [[Edzard Ernst]], editor of The Desktop Guide to Complementary and Alternative Medicine". Elsevier Science. 2002. Archived from the original on 2007-03-11.
{{cite web}}: URL–wikilink conflict (help) - ^ Cassileth BR, Deng G (2004). "Complementary and alternative therapies for cancer". The Oncologist. 9 (1): 80–9. doi:10.1634/theoncologist.9-1-80. PMID 14755017.
- ^ a b James May (12 July 2011). "College of Medicine: What is integrative health?". British Medical Journal. 343: d4372. doi:10.1136/bmj.d4372. PMID 21750063.
- ^ FDA, Drugs, information for consumers
- ^ a b NHS complementary provision
- ^ Ramsey, Matthew (1999), "Alternative Medicine in Modern France", Medical history 43 (3): 286–322, PMC 1044147, PMID 10885126, http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1044147
- ^ Bivins, Roberta (2007). Alternative Medicine? A History. Oxford: Oxford University Press. p. 171. ISBN 9780199218875. Roberta Bivins is an associate professor and the director of the Centre for the History of Medicine at the University of Warwick, England.
- ^ Jütte, Robert (2001). "Alternative Medicine and Medico-Historical Semantics". Historical Aspects of Unconventional Medicine: Approaches, Concepts, Case Studies. European Association for the History of Medicine and Health. pp. 11–26. ISBN 095365222X.
{{cite book}}: External link in|chapterurl=|chapterurl=ignored (|chapter-url=suggested) (help); Unknown parameter|editors=ignored (|editor=suggested) (help) Robert Jütte is an adjunct professor of history at the University of Stuttgart and editor of the journal Medizin, Gesellschaft und Geschicht. - ^ The Historiography of Nonconventional Medicine in Germany: A Concise Overview, 1999[3]
- ^ Barry D. Silverman, William Henry Welch (1850–1934): the road to Johns Hopkins. Proc (Bayl Univ Med Cent). 2011 July; 24(3): 236–242.[4]
- ^ Flexner Report, Introduction p.viii "The fundamental sciences upon which medicine depends have been greatly extended. The laboratory has come to furnish alike to the physician and to the surgeon a new means for diagnosing and combating disease. The education of the medical practitioner under these changed conditions makes entirely different demands in respect of both preliminary and professional training."[5]
- ^ The report of the Committee on the Indigenous systems of medicine, Madras (also known as the Usman Report).Gram Vichar, What is the role of indigenous medical sciences in our health care system? December 1984, condensed in Perspective, Vol.10, no.3, 1985[6] [7]
- ^ According to the Oxford English Dictionary, the earliest recorded English language usage in a print medium of the term "alternative medicine" is found in a 1974 text by Helen Kruger. "alternative". Oxford English Dictionary (OED Online ed.). Oxford University Press. December 2012. Retrieved 20 February 2013.; Kruger, Helen (1974). Other healers, other cures: a guide to alternative medicine. Bobbs-Merrill. ISBN 9780672517082. See also: British Medical Association (1993). Complementary Medicine, New Approach to Good Practice. Oxford University Press. ISBN 9780192861665.; Cant, Sarah; Sharma, Ursula (22 October 1999). "Alternative health practices and systems". In Albrecht, Gary L; Fitzpatrick, Ray; Scrimshaw, Susan C. (eds.). The Handbook of Social Studies in Health and Medicine. SAGE. pp. 433–. ISBN 978-1-84787-096-4.; Saks, Mike (2003). Orthodox and Alternative Medicine: Politics, Professionalization and Health Care. SAGE. p. 117. ISBN 978-1-4462-6536-9.
- ^ Arnold S. Relman, a former editor of The New England Journal of Medicine A trip to Stonesville. The New Republic, Dec 14, 1998.
- ^ Eisenberg DM; et al. (1993). "Unconventional Medicine in the United States – Prevalence, Costs, and Patterns of Use". N Engl J Med. 328 (4): 246–252. doi:10.1056/NEJM199301283280406. PMID 8418405.
{{cite journal}}: Unknown parameter|author-separator=ignored (help) - ^ Eisenberg DM; Davis RB; Ettner SL; et al. (1998). "Trends in alternative medicine use in the United States, 1990–1997: results of a follow-up national survey". JAMA. 280 (18): 1569–75. doi:10.1001/jama.280.18.1569. PMID 9820257.
{{cite journal}}: Unknown parameter|author-separator=ignored (help) - ^ Best Practices in Integrative Medicine: A Report from the Bravewell Clinical Network. Published 2007. The Bravewell Collaborative. Page 4.
- ^ In 1991 the Senate Appropriations Committee responsible for funding the National Institutes of Health (NIH) declared itself "not satisfied that the conventional medical community as symbolized at the NIH has fully explored the potential that exists in unconventional medical practices." James Harvey Young, The Development of the Office of Alternative Medicine in the National Institutes of Health, 1991-1996. From: Bulletin of the History of Medicine Volume 72, Number 2, Summer 1998 pp. 279-298 | 10.1353/bhm.1998.0110[8]
- ^ Winnick, Terri A. (2005-02-01). "From Quackery to "Complementary" Medicine: The American Medical Profession Confronts Alternative Therapies". Social Problems. 52 (1): 38–61. doi:10.1525/sp.2005.52.1.38. ISSN 0037-7791. JSTOR 10.1525/sp.2005.52.1.38. Retrieved 2013-02-13.
- ^ Flexner, Abraham (1910), Medical Education in the United States and Canada: A Report to the Carnegie Foundation for the Advancement of Teaching, Bulletin No. 4., New York City: The Carnegie Foundation for the Advancement of Teaching, p. 346, OCLC 9795002, retrieved April 20, 2010
- ^ 'How Becoming a Doctor Works: Medical School Curriculum' [9]
- ^ Stanford[10]
- ^ Curriculum Overview > Medical Student Education Program | Medical Education | Yale School of Medicine
- ^ a b Snyderman R, Weil AT (2002). "Integrative medicine: bringing medicine back to its roots". Archives of Internal Medicine. 162 (4): 395–7. doi:10.1001/archinte.162.4.395. PMID 11863470.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Berman, B. M (2001-01-20). "Complementary medicine and medical education". BMJ 322 (7279): 121-122. doi:10.1136/bmj.322.7279.121. ISSN 09598138. [11]
- ^ Center for Integrative Medicine of the University of Maryland School of Medicine[12],[13], [14][15]
- ^ Medline Plus (2012). "Doctor of medicine profession (MD)". U.S. National Library of Medicine of National Institutes of Health. Retrieved 20 December 2012.
- ^ Doctor of medicine profession[(MDhttp://www.nlm.nih.gov/medlineplus/ency/article/001936.htm]
- ^ British Medical Association Complementary Medicine, New Approach to Good Practice, Oxford University Press, 1993
- ^ House of Lords, United Kingdom, Select Committee on Science and Technology (2000) [16]
- ^ a b "Cochrane Complementary Medicine Field". Cochrane COllaboration.
- ^ a b c "Complementary medicine: the good the bad and the ugly". Edzard Ernst.
- ^ The Economist, "Alternative Medicine: Think yourself better", 21 May 2011, pp. 83–84.[17].Edzard Ernst, Placebo and other Non-specific Effects 8th article in Healing, Hype, or Harm? A Critical Analysis of Complementary or Alternative Medicine (2008), reviewed[18]
- ^ J.Belsey and T.Snell What is evidence-based medicine? 2nd edition, 'Supported by Sanofi-aventis', pubished by Hayward Medical Communications, Hayward Group Ltd, 2009. [19]
- ^ BMJ 'Evidence based medicine is the conscientious, explicit, and judicious use of current best evidence in making decisions about the care of individual patients'.[20] 'Evidence-Based Medicine systematically searches a wide range of international medical journals applying strict criteria for the validity of research. Experts critically appraise the validity of the most clinically relevant articles and summarize them including commentary on their clinical applicability. EBM also publishes articles relevant to the study and practice of evidence-based medicine. EBM is about integrating individual clinical expertise and the best external evidence. Evidence based medicine, whose philosophical origins extend back to mid-19th century Paris and earlier, remains a hot topic for clinicians, public health practitioners, purchasers, planners, and the public. British centres for evidence based practice have been established or planned in adult medicine, child health, surgery, pathology, pharmacotherapy, nursing, general practice, and dentistry; the Cochrane Collaboration and Britain's Centre for Review and Dissemination in York are providing systematic reviews of the effects of health care'.[21]
- ^ Nuffield Trust: 'source of evidence-based research and policy analysis for improving health care in the UK.'[22]
- ^ Research methods & information tools[23], 'Predictive risk and health care: an overview'[24]
- ^ a b c "Cochrane CAM Field: Integrative Medicine".
- ^ Development and classification of an operational definition of complementary and alternative medicine for the Cochrane Collaboration L. Susan Wieland, Center for Integrative Medicine, University of Maryland School of Medicine, Eric Manheimer, research associate, and Brian M. Berman, founder and director. National Center for Biotechnology Information (NCBI), a division of US National Library of Medicine, National Institutes of Health[25]
- ^ a b c d e f g h i National Science Foundation survey: Science and Technology: Public Attitudes and Public Understanding. Science Fiction and Pseudoscience.
- ^ a b c d e f g h i j "What is Complementary and Alternative Medicine (CAM)?". National Center for Complementary and Alternative Medicine. Archived from the original on 2005-12-08. Retrieved 2006-07-11.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ a b "Complementary and Alternative Medicine in Cancer Treatment". National Vancer Institute. Retrieved 2012-12-11.
{{cite web}}: Cite has empty unknown parameter:|deadurl=(help) - ^ a b .Borkan, Jeffrey (2012). "Complementary alternative health care in Israel and the western world". Isr J Health Policy Res. 1 (8). doi:10.1186/2045-4015-1-8. PMID 22913745.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Kong SC, Hurlstone DP, Pocock CY, Walkington LA, Farquharson NR, Bramble MG, McAlindon ME, Sanders DS. (2005). "The Incidence of self-prescribed oral complementary and alternative medicine use by patients with gastrointestinal diseases". J Clin Gastroenterol. 39 (2): 138–41. PMID 15681910.
{{cite journal}}: Cite has empty unknown parameter:|month=(help)CS1 maint: multiple names: authors list (link) - ^ "Science and Technology: Public Attitudes and Public Understanding Science Fiction and Pseudoscience - Belief in Alternative Medicine". National Science Foundation.
alternative medicine refers to all treatments that have not been proven effective using scientific methods
- ^ Chapter 7, Science and Technology: Public Attitudes and Public Understandingof Science and Engineering Indicators 2002, National Science Board, Science and Engineering Indicators – 2002. Arlington, VA: National Science Foundation, 2002 (NSB-02-1[26]
- ^ Stephen Barret, NCAHF[27]
- ^ The Rise and Rise of Complementary and Alternative Medicine: a Sociological Perspective, Ian D Coulter and Evan M Willis, Medical Journal of Australia, 2004; 180 (11): 587-589
- ^ a b c d e f Attention: This template ({{cite doi}}) is deprecated. To cite the publication identified by doi: 10.1111/j.1749-6632.1996.tb23138.x , please use {{cite journal}} (if it was published in a bona fide academic journal, otherwise {{cite report}} with
|doi= 10.1111/j.1749-6632.1996.tb23138.xinstead. - ^ a b Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 11242572, please use {{cite journal}} with
|pmid= 11242572instead. - ^ Other sources:
- Nature Medicine, September 1996, Volume 2 Number 9, p1042
- Pseudoscience and the Paranormal, Hines, Terence, American Psychological Association, [28]
- The Need for Educational Reform in Teaching about Alternative Therapies, Journal of the Association of Medical Colleges, March 2001 - Volume 76 - Issue 3 - p 248-250
- The Rise and Rise of Complementary and Alternative Medicine: a Sociological Perspective, Ian D Coulter and Evan M Willis, Medical Journal of Australia, 2004; 180 (11): 587-589
- Ignore Growing Patient Interest in Alternative Medicine at Your Peril - MDs Warned, Heather Kent, Canadian Medical Association Journal, November 15, 1997 vol. 157 no. 10
- The Demon-Haunted World: Science as a Candle in the Dark, Carl Sagan, Random House, ISBN 0-394-53512-X, 1996
- ^ a b Ignore Growing Patient Interest in Alternative Medicine at Your Peril - MDs Warned, Heather Kent, Canadian Medical Association Journal, November 15, 1997 vol. 157 no. 10
- ^ a b c Goldrosen MH, Straus SE. "Complementary and alternative medicine: assessing the evidence for immunological benefits." Nature Perspectives, November 2004 vol. 4, pp. 912-921.
- ^ a b Zollman C, Vickers A (1999). [/ "ABC of complementary medicine What is complementary medicine?"]. British Medical Journal. 319 (693): 693. doi:10.1136/bmj.319.7211.693.
{{cite journal}}: Check|url=value (help); Cite has empty unknown parameter:|month=(help) - ^ a b "Complementary and Alternative Medicine in the United States". United States Institute of Medicine. 12 January 2005. pp. 16–20. Retrieved 2011-01-18.
Complementary and alternative medicine (CAM) is a broad domain of resources that encompasses health systems, modalities, and practices and their accompanying theories and beliefs, other than those intrinsic to the dominant health system of a particular society or culture in a given historical period. CAM includes such resources perceived by their users as associated with positive health outcomes. Boundaries within CAM and between the CAM domain and the domain of the dominant system are not always sharp or fixed.
- ^ a b "Traditional Medicine: Definitions". World Health Organization. 2000. Retrieved 2012-11-11.
- ^ a b c d e Institute of Med (2005). Complementary and Alternative Medicine in the United States. National Academy Press. ISBN 978-0-309-09270-8.
- ^ a b Lilienfeld, Scott O. (2002). "Our Raison d'Être". The Scientific Review of Mental Health Practice. 1 (1). Archived from the original on 2007-07-26. Retrieved 2008-01-28.
{{cite journal}}: Cite has empty unknown parameter:|coauthors=(help); Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ a b Dominic Hughes (23 December 2010). "Alternative remedies 'dangerous' for kids says report". BBC News.
- ^ Carroll RT. "complementary medicine" at The Skeptic's Dictionary
- ^ Acupuncture Pseudoscience in the New England Journal of Medicine, Science Based Medicine, Steven Novella, Science-Based Medicine » Acupuncture Pseudoscience in the New England Journal of Medicine
- ^ a b c Credulity about acupuncture infiltrates the New England Journal of Medicine, Science Based Medicine, David Gorski, Science-Based Medicine » Credulity about acupuncture infiltrates the New England Journal of Medicine
- ^ Acharya, Deepak and Shrivastava Anshu (2008). Indigenous Herbal Medicines: Tribal Formulations and Traditional Herbal Practices. Jaipur: Aavishkar Publishers Distributor. p. 440. ISBN 978-81-7910-252-7.
- ^ Robert Jütte, "Historiography of Nonconventional Medicine in Germany" [29]
- ^ Srimad Bhagavatam 1.3.17. Reference: http://vedabase.com/en/sb/1/3/17
- ^ Matthew Ramsey, Vanderbilt University, Nashville, TN Alternative medicine in modern France Cambridge Journals, Med Hist. 1999 July; 43(3): 286–322.[30]
- ^ The Roots of Ayurveda: Selections from Sanskrit Medical Writings, D. Wujastyk, p xviii, 2003, ISBN 0-14-044824-1
- ^ Saper, R. B.; Phillips, R. S.; et al. (2008). "Lead, Mercury, and Arsenic in US- and Indian-manufactured ayurvedic Medicines Sold via the Internet". Journal of the American Medical Association. 300 (8): 915–923. doi:10.1001/jama.300.8.915. PMC 2755247. PMID 18728265.
- ^ Valiathan, M. S. (2006). "Ayurveda: Putting the House in Order". Current Science. 90 (1). Indian Academy of Sciences: 5–6.
- ^ Ho, Peng Yoke (2000). Li, Qi, and Shu: An Introduction to Science and Civilization in China. Dover Publications. ISBN 0-486-41445-0.
{{cite book}}: Unknown parameter|month=ignored (help) - ^ a b c Celestial lancets: a history and rationale of acupuncture and moxa, Needham, J; Lu GD, 2002, Routledge, ISBN 0-7007-1458-8
- ^ Tongue Diagnosis in Chinese Medicine, G Cia, 1995, Eastland Press. ISBN 0-939616-19-X.
- ^ Hahnemann, Samuel (1833). The Homœopathic Medical Doctrine, or "Organon of the Healing Art". Translated by Charles H. Devrient, Esq. Dublin: W.F. Wakeman. pp. iii, 48–49.
Observation, reflection, and experience have unfolded to me that the best and true method of cure is founded on the principle, similia similibus curentur. To cure in a mild, prompt, safe, and durable manner, it is necessary to choose in each case a medicine that will excite an affection similar (ὅμοιος πάθος) to that against which it is employed.
- ^ Ernst, E. (2002), "A systematic review of systematic reviews of homeopathy", British Journal of Clinical Pharmacology, 54 (6): 577–82, doi:10.1046/j.1365-2125.2002.01699.x, PMC 1874503, PMID 12492603
- ^ UK Parliamentary Committee Science and Technology Committee - "Evidence Check 2: Homeopathy"
- ^ Shang, Aijing; Huwiler-Müntener, Karin; Nartey, Linda; Jüni, Peter; Dörig, Stephan; Sterne, Jonathan AC; Pewsner, Daniel; Egger, Matthias (2005), "Are the clinical effects of homoeopathy placebo effects? Comparative study of placebo-controlled trials of homoeopathy and allopathy", The Lancet, 366 (9487): 726–732, doi:10.1016/S0140-6736(05)67177-2, PMID 16125589
- ^ http://nccam.nih.gov/health/homeopathy "Homeopathy: An Introduction" a NCAAM webpage
- ^ Wahlberg, A (2007), "A quackery with a difference—New medical pluralism and the problem of 'dangerous practitioners' in the United Kingdom", Social Science & Medicine, 65 (11): 2307–16, doi:10.1016/j.socscimed.2007.07.024, PMID 17719708
- ^ Sarris, J., and Wardle, J. 2010. Clinical naturopathy: an evidence-based guide to practice. Elsevier Australia. Chatswood, NSW.
- ^
"Naturopathy: An Introduction" (PDF). National Center for Complementary and Alternative Medicine. 2007. Retrieved 20 Nov 10.
{{cite web}}: Check date values in:|accessdate=(help) - ^ Brown PS (April 1, 1988). "Nineteenth-century American health reformers and the early nature cure movement in Britain". Medical History. 32 (2): 174–194. PMC 1139856. PMID 3287059.
- ^ Langley, Stephen (2007). "History of Naturopathy". Excerpt from The Naturopathy Workbook. UK: College of Natural Medicine (CNM)Template:Inconsistent citations
{{cite book}}: CS1 maint: postscript (link) - ^ "Report 12 of the Council on Scientific Affairs (A-97)". American Medical Association. 1997.
- ^ a b Baer, H. A. (2001). "The sociopolitical status of U.S. naturopathy at the dawn of the 21st century". Medical Anthropology Quarterly. 15 (3): 329–346. doi:10.1525/maq.2001.15.3.329. PMID 11693035.
- ^
Frey, Rebecca (April 1). "Naturopathic medicine". Encyclopedia of Medicine. Gale (Cengage). Retrieved 20 Nov 10.
{{cite web}}: Check date values in:|accessdate=and|date=(help) - ^ "A study of costs and length of stay of inpatient naturopathy--evidence from Germany". Complement Ther Clin Pract. 2011. Retrieved 2012-09-28>.
{{cite web}}: Check date values in:|accessdate=(help) - ^ Iowa Board of Medicine policy statement on naturopathy
- ^ Energy Medicine: An Overview, National Center for Complementary and Alternative Medicine[31]
- ^ Demon Haunted World, Carl Sagan
- ^ Psychophysiologic Effects of Hatha Yoga on Musculoskeletal and Cardiopulmonary Function: A Literature Review, The Journal of Alternative and Complementary Medicine, J. A. Raub, (2002), 8(6): 797-812. doi:10.1089/10755530260511810.
- ^ a b According to a New Government Survey, 38 Percent of Adults and 12 Percent of Children Use Complementary and Alternative Medicine, NIH, [32]
- ^ "Science and Technology: Public Attitudes and Public Understanding Science Fiction and Pseudoscience - Belief in Alternative Medicine". National Science Foundation.
alternative medicine refers to all treatments that have not been proven effective using scientific methods
- ^ Chapter 7, Science and Technology: Public Attitudes and Public Understandingof Science and Engineering Indicators 2002, National Science Board, Science and Engineering Indicators – 2002. Arlington, VA: National Science Foundation, 2002 (NSB-02-1[33]
- ^ Sampson, Wallace (1 June 1995). "Antiscience trends in the rise of the "alternative medicine" movement". Annals of the New York Academy of Sciences. 775 (1): 189–191. doi:10.1111/j.1749-6632.1996.tb23138.x. Wallace Sampson
- ^ a b Sampson W, Atwood Iv K (2005). "Propagation of the absurd: demarcation of the absurd revisited". Med. J. Aust. 183 (11–12): 580–1. PMID 16336135.
- ^ a b Angell M, Kassirer JP (1998). "Alternative medicine--the risks of untested and unregulated remedies" (PDF). The New England Journal of Medicine. 339 (12): 839–41. doi:10.1056/NEJM199809173391210. PMID 9738094.
It is time for the scientific community to stop giving alternative medicine a free ride. There cannot be two kinds of medicine – conventional and alternative. There is only medicine that has been adequately tested and medicine that has not, medicine that works and medicine that may or may not work. Once a treatment has been tested rigorously, it no longer matters whether it was considered alternative at the outset. If it is found to be reasonably safe and effective, it will be accepted. But assertions, speculation, and testimonials do not substitute for evidence. Alternative treatments should be subjected to scientific testing no less rigorous than that required for conventional treatments.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ The New England Journal of Medicine, July 1995.
- ^ a b Scientists Speak Out Against Federal Funds for Research on Alternative Medicine – washingtonpost.com
- ^ Fontanarosa PB, Lundberg GD (1998). "Alternative medicine meets science". JAMA. 280 (18): 1618–9. doi:10.1001/jama.280.18.1618. PMID 9820267.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Dawkins, Richard (2003). A Devil's Chaplain. Weidenfeld & Nicolson. ISBN 978-0-618-33540-4.
{{cite book}}: More than one of|author=and|last=specified (help) - ^ Dawkins, Richard (2003). A Devil's Chaplain. United States: Houghton Mifflin. p. 58. ISBN 978-0-618-33540-4.
- ^ "Review: A Devil's Chaplain by Richard Dawkins". The Guardian. London. 2003-02-15. Archived from the original on 11 April 2010. Retrieved 2010-04-23.
{{cite news}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ Cassileth BR (1999). "Evaluating complementary and alternative therapies for cancer patients". CA Cancer J Clin. 49 (6): 362–75. doi:10.3322/canjclin.49.6.362. PMID 11198952.
- ^ a b c Brown, David (March 17, 2009). "Scientists Speak Out Against Federal Funds for Research on Alternative Medicine". Washingtonpost. Retrieved 2010-04-23.
- ^ a b Barrett, Stephen (February 10, 2004). "Be Wary of "Alternative" Health Methods". Stephen Barrett, M.D. Quackwatch. Retrieved 2008-03-03.
- ^ a b c "$2.5 billion spent, no alternative cures found – Alternative medicine- msnbc.com". MSNBC. June 10, 2009.
- ^ a b Why the National Center for Complementary and Alternative Medicine (NCCAM) Should Be Defunded
- ^ Research Results of Complementary and Alternative Medicine [NCCAM Research]
- ^ Acupuncture Pseudoscience in the New England Journal of Medicine, Science Based Medicine, Steven Novella Science-Based Medicine » Acupuncture Pseudoscience in the New England Journal of Medicine
- ^ Edzard Ernst. "Alternative medicine remains an ethics-free zone." The Guardian 8 November 2011
- ^ a b Mark Henderson, Science Editor, "Prince of Wales's guide to alternative medicine 'inaccurate'" Times Online, April 17, 2008
- ^ a b "Complementary medicine is diagnosis, treatment and/or prevention that complements mainstream medicine by contributing to a common whole, by satisfying a demand not met by orthodoxy or by diversifying the conceptual frameworks of medicine." Ernst et al. British General Practitioner 1995; 45:506.
- ^ Butler K (1992). A Consumer's Guide to "ALTERNATIVE MEDICINE": A close look at Homeopathy, Acupuncture, Faith-healing and other Unconventional Treatments
- ^ "real acupuncture treatments were no more effective than sham acupuncture treatments. There was, nevertheless, evidence that both real acupuncture and sham acupuncture were more effective than no treatment, and that acupuncture can be a useful supplement to other forms of conventional therapy for low back pain", Acupuncture for Chronic Low Back Pain, New England Journal of Medicine, 2010; 363:454-461, Brian M. Berman, M.D., Brian M. Berman, founder of the Center for Integrative Medicine, University of Maryland School of Medicine, and Helene M. Langevin, M.D., Claudia M. Witt, M.D., M.B.A., and Ronald Dubner, D.D.S., Ph.D., MMS: Error Template:WebCite
- ^ Kermen R, Hickner J, Brody H, Hasham I (2010). "Family physicians believe the placebo effect is therapeutic but often use real drugs as placebos". Fam Med. 42 (9): 636–42. PMID 20927672.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ http://www.stfm.org/fmhub/fm2010/October/Rachel636.pdf
- ^ "Development and classification of an operational definition of complementary and alternative medicine for the Cochrane collaboration". Altern Ther Health Med. 17 (2): 50–59. 2011. PMID 21717826.
{{cite journal}}:|access-date=requires|url=(help); Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|month=ignored (help) - ^ Internal Revenue Service Pubication 502 Medical and Dental Expenses (for 2012 rerurns), section 5 What Medical Expenses Are Includible?: "Medical expenses are the costs of diagnosis, cure, mitigation, treatment, or prevention of disease, and the costs for treatments affecting any part or function of the body. These expenses include payments for legal medical services rendered by physicians, surgeons, dentists and other medical practitioners.... primarily to alleviate or prevent a physical or mental defect or illness. Medicines: You can include expenses amounts you pay for prescribed medicines and drugs. A prescribed drug is one that requires a prescription by a doctor for its use by an individual." [34]
- ^ Ernst E (2003). "Obstacles to research in complementary and alternative medicine". The Medical Journal of Australia. 179 (6): 279–80. PMID 12964907.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ a b c d e Barnes PM, Powell-Griner E, McFann K, Nahin RL (2004). "Complementary and alternative medicine use among adults: United States, 2002" (PDF). Advance Data (343): 1–19. PMID 15188733.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Reasons people use CAM. NCCAM
- ^ a b Astin JA (1998). "Why patients use alternative medicine: results of a national study". JAMA. 279 (19): 1548–53. doi:10.1001/jama.279.19.1548. PMID 9605899.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Horneber M, Bueschel G, Dennert G, Less D, Ritter E, Zwahlen M. (2011). "How many cancer patients use complementary and alternative medicine: a systematic review and metaanalysis". Integr Cancer Ther. 11 (3): 187–203. doi:10.1177/1534735411423920. PMID 22019489.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ a b Eisenberg DM; Davis RB; Ettner SL; et al. (1998). "Trends in alternative medicine use in the United States, 1990–1997: results of a follow-up national survey". JAMA. 280 (18): 1569–75. doi:10.1001/jama.280.18.1569. PMID 9820257.
{{cite journal}}: Unknown parameter|author-separator=ignored (help); Unknown parameter|month=ignored (help) - ^ House of Lords report on CAM Template:WebCite
- ^ a b "Trends in Alternative Medicine Use in the United States, 1990–1997: Results of a Follow-up National Survey." Journal of the American Medical Association, Eisenberg, D.M., R.B. Davis, S.I. Ettner, et al, 280: 1569–75, 1998
- ^ Alternative Medicine Goes Mainstream CBS News. Published July 20, 2006. Retrieved June 13, 2009.
- ^ a b "Press Release : Latest Survey Shows More Hospitals Offering Complementary and Alternative Medicine Services". American Hospital Association. 2008-09-15. Retrieved 2009-11-18.
- ^ "A Close Look at Therapeutic Touch." Journal of the American Medical Association, Rosa, L., Rosa, E., Sarner, L., and Barrett, S. 279(13): 1005–10, 1998
- ^ Cassileth, Barrie R. (June 1996). "Alternative and Complementary Cancer Treatments". The Oncologist. 1 (3): 173–9. PMID 10387984.
- ^ Marty (1999). "The Complete German Commission E Monographs: Therapeutic Guide to Herbal Medicines". J Amer Med Assoc. 281 (19): 1852–3. doi:10.1001/jama.281.19.1852.
- ^ "Traditional medicine". Fact sheet 134. World Health Organization. 2003-05. Archived from the original on 2008-07-28. Retrieved 2008-03-06.
{{cite web}}: Check date values in:|date=(help); Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ Thomas KJ, Nicholl JP, Coleman P (2001). "Use and expenditure on complementary medicine in England: a population based survey". Complementary Therapies in Medicine. 9 (1): 2–11. doi:10.1054/ctim.2000.0407. PMID 11264963.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ http://nccam.nih.gov/sites/nccam.nih.gov/files/news/nhsr12.pdf/
- ^ House of Lords Select Committee on Science and Technology. 2000. Complementary and Alternative Medicine. London: The Stationery Office.
- ^ Glossary, Continuum Health Partners, 2005.
- ^ Allan Kellehear, Complementary medicine: is it more acceptable in palliative care practice? MJA 2003; 179 (6 Suppl): S46-S48 online
- ^ Menefee LA, Monti DA (2005). "Nonpharmacologic and complementary approaches to cancer pain management". J Am Osteopath Assoc. 105 (suppl 5): S15–20. PMID 16368903.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ a b World Health Organization (2005). "WHO guidelines on basic training and safety in chiropractic" (PDF). ISBN 92-4-159371-7. Retrieved 2008-02-29.
{{cite journal}}: Cite journal requires|journal=(help) - ^ http://www.fda.gov/Drugs/ResourcesForYou/Consumers/BuyingUsingMedicineSafely/MedicationHealthFraud/ucm207747.htm FDA, Drugs, information for consumers]
- ^ [vhttp://www.fda.gov/ICECI/ComplianceManuals/CompliancePolicyGuidanceManual/ucm074360.htm]
- ^ Developing clinical practice guidelines: types of evidence and outcomes; values and economics, synthesis, grading, and presentation and deriving recommendations, Steven Woolf and others, 2012.[35] Implementation Science[36]
- ^ Relman, Arnold S., A Second Opinion: Rescuing America's Health Care (2007), [37] chapter 5 The reform we need
- ^ Sarris Jerome (2012). "Current challenges in appraising complementary medicine evidence". The Medical Journal of Australia. 196 (5): 310–311. doi:10.5694/mja11.10751. PMID 22432660.
- ^ James Alcock PhD, Alternative Medicine and the Psychology of Belief, The Scientific Review of Alternative Medicine, Fall/Winter 1999 Volume 3 ~ Number 2. available online
- ^ Katz DL; Williams AL; Girard C; et al. (2003). "The evidence base for complementary and alternative medicine: methods of Evidence Mapping with application to CAM". Alternative Therapies in Health and Medicine. 9 (4): 22–30. PMID 12868249.
{{cite journal}}: Unknown parameter|author-separator=ignored (help) - ^ Ernst E (2005). "The efficacy of herbal medicine--an overview". Fundamental & Clinical Pharmacology. 19 (4): 405–9. doi:10.1111/j.1472-8206.2005.00335.x. PMID 16011726.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Horrobin DF (1986). "Glittering prizes for research support". Nature. 324 (6094): 221. Bibcode:1986Natur.324..221H. doi:10.1038/324221a0.
- ^ "NCCAM Funding: Appropriations History". NCCAM. 2008-01-09. Archived from the original on 2009-06-11. Retrieved 2008-04-02.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ Atwood, Kimball C. (2003-09). "The Ongoing Problem with the National Center for Complementary and Alternative Medicine". Skeptical Inquirer. Archived from the original on 16 November 2009. Retrieved 2009-11-18.
{{cite news}}: Check date values in:|date=(help); Cite has empty unknown parameter:|coauthors=(help); Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 12356597, please use {{cite journal}} with
|pmid=12356597instead. - ^ Andrew Vickers PhD (2004). "Alternative Cancer Cures: "Unproven" or "Disproven"?". CA Cancer J Clin. 54 (2): 110–118. doi:10.3322/canjclin.54.2.110. PMID 15061600.
- ^ Colquhoun, Professor David (2012). "Regulation of Alternative Medicine ‐ why it doesn't work" (PDF). Scottish Universities Medical Journal. 1 (EPub series) (16): 1–9. Retrieved 25 November.
{{cite journal}}: Check date values in:|accessdate=(help); Unknown parameter|month=ignored (help) - ^ Connelly, P (2012). "The Ethics of Acupuncture" (PDF). Scottish Universities Medical Journal. 1 (2): 165–169.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Malcolm, Dr R (2012). "Small but Intriguing - The Unfolding Story of Homeopathic Medicine" (PDF). Scottish Universities Medical Journal. 1 (EPub series) (15): 1–7. Retrieved 2012-11-30.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Cassileth BR, Deng G (2004). "Complementary and alternative therapies for cancer". The Oncologist. 9 (1): 80–9. doi:10.1634/theoncologist.9-1-80. PMID 14755017.
- ^ Hills, Ben. "Fake healers. Why Australia's $1 billion-a-year alternative medicine industry is ineffective and out of control". Medical Mayhem. Retrieved 2008-03-06.
- ^ Swan, Norman (2000-10-02). "Alternative Medicine – Part Three". The Health Report. ABC Radio National. Archived from the original on 6 March 2008. Retrieved 2008-03-06.
{{cite news}}: Cite has empty unknown parameter:|coauthors=(help); Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ a b Isadora Stehlin. "Homeopathy: Real Medicine or Empty Promises?" – FDA Consumer magazine (December 1996)
- ^ Navarro, Victor J.; Senior, John R. (2006-05-18). "NEJM – Drug-Related Hepatotoxicity". New England Journal of Medicine. 354 (7). Content.nejm.org: 731–9. doi:10.1056/NEJMra052270. PMID 16481640. Retrieved 2009-12-16.
- ^ Vickers, A. (2004). "Alternative Cancer Cures: 'Unproven' or 'Disproven'?". CA. 54 (2): 110–8. doi:10.3322/canjclin.54.2.110. PMID 15061600.
- ^ Renckens CN (2009). "A Dutch view of the science of CAM 1986--2003". Eval Health Prof. 32 (4): 431–50. doi:10.1177/0163278709346815. PMID 19926606.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ a b c d e f Beyerstein BL (1999). "Psychology and 'Alternative Medicine' Social and Judgmental Biases That Make Inert Treatments Seem to Work". The Scientific Review of Alternative Medicine. 3 (2). Retrieved 2008-07-07.
- ^ a b Weber DO (1998). "Complementary and alternative medicine. Considering the alternatives". Physician Executive. 24 (6): 6–14. PMID 10351720.
- ^ a b c Beyerstein BL (2001). "Alternative medicine and common errors of reasoning". Academic Medicine. 76 (3): 230–7. doi:10.1097/00001888-200103000-00009. PMID 11242572.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ van Deventer MO (2008). "Meta-placebo: do doctors have to lie about giving a fake treatment?". Medical Hypotheses. 71 (3): 335–9. doi:10.1016/j.mehy.2008.03.040. PMID 18485613.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 19783116, please use {{cite journal}} with
|pmid= 19783116instead. - ^ "Complementary therapies: The big con? – The Independent". London. 2008-04-22. Archived from the original on 17 April 2010. Retrieved 2010-04-23.
{{cite news}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 20846193, please use {{cite journal}} with
|pmid= 20846193instead. - ^ Sobel DS (2000). "The cost-effectiveness of mind-body medicine interventions". Progress in Brain Research. Progress in Brain Research. 122: 393–412. doi:10.1016/S0079-6123(08)62153-6. ISBN 978-0-444-50049-6. PMID 10737073.
- ^ Complementary Medicine – Mind-Body Interventions, WebMD, Inc., 2007
- ^ Toupin April K, Moher D, Stinson J, Byrne A, White M, Boon H, Duffy CM, Rader T, Vohra S, Tugwell P. (2012). Phillips, Robert S (ed.). "Measurement properties of questionnaires assessing complementary and alternative medicine use in pediatrics: a systematic review". PLoS One. 7 (6): e39611. doi:10.1371/journal.pone.0039611. PMC 3387262. PMID 22768098.
{{cite journal}}: Cite has empty unknown parameter:|month=(help)CS1 maint: multiple names: authors list (link) CS1 maint: unflagged free DOI (link) - ^ "Complementary and Alternative Medicine in the United States: Definition of CAM". United States Institute of Medicine. 12 January 2005. p. 19. Retrieved 2012-12-15.
- ^ General Guidelines for Methodologies on Research and Evaluation of Traditional Medicine [38]
- ^ "Complementary and alternative medicine : Department of Health – Public health". Department of Health.
- ^ Walter R., PhD. Frontera; DeLisa, Joel A.; Gans, Bruce M.; NICHOLAS E. WALSH (2005). Physical medicine and rehabilitation: principles and practice. Hagerstwon, MD: Lippincott Williams & Wilkins. pp. Chapter 19. ISBN 978-0-7817-4130-9.
{{cite book}}: CS1 maint: multiple names: authors list (link)
Further reading
- Bausell, R. Barker (2007). Snake Oil Science: The Truth About Complementary and Alternative Medicine. Oxford University Press. ISBN 978-0-19-531368-0.
- Benedetti F, Maggi G, Lopiano L. "Open Versus Hidden Medical Treatments: The Patient's Knowledge About a Therapy Affects the Therapy Outcome." Prevention & Treatment, 2003; 6(1), APA online
- Bivins, Roberta "Alternative Medicine?: A History" Oxford University Press 2008
- Diamond, J. Snake Oil and Other Preoccupations, 2001, ISBN 978-0-09-942833-6 , foreword by Richard Dawkins reprinted in Dawkins, R., A Devil's Chaplain, 2003, ISBN 978-0-7538-1750-6 .
- Downing AM, Hunter DG (2003). "Validating clinical reasoning: a question of perspective, but whose perspective?". Manual Therapy. 8 (2): 117–9. doi:10.1016/S1356-689X(02)00077-2. PMID 12890440.
{{cite journal}}: Unknown parameter|month=ignored (help) - Eisenberg DM (1997). "Advising patients who seek alternative medical therapies". Annals of Internal Medicine. 127 (1): 61–9. doi:10.1059/0003-4819-127-1-199707010-00010. PMID 9214254.
{{cite journal}}: Unknown parameter|month=ignored (help) - Gunn IP (1998). "A critique of Michael L. Millenson's book, Demanding medical excellence: doctors and accountability in the information age, and its relevance to CRNAs and nursing". AANA Journal. 66 (6): 575–82. PMID 10488264.
{{cite journal}}: Unknown parameter|month=ignored (help) - Hand, Wayland Debs (1980). "Folk Magical Medicine and Symbolism in the West". Magical Medicine. Berkeley: University of California Press. pp. 305–19. ISBN 978-0-520-04129-5. OCLC 6420468.
- Illich, Ivan (1976). Limits to medicine : medical nemesis : the expropriation of health. Penguin. ISBN 978-0-14-022009-4. OCLC 4134656.
- Mayo Clinic (2007). Mayo Clinic Book of Alternative Medicine: The New Approach to Using the Best of Natural Therapies and Conventional Medicine. Parsippany, New Jersey: Time Inc Home Entertainment. ISBN 978-1-933405-92-6.
- Phillips Stevens Jr. (2001). "Magical Thinking in Complementary and Alternative Medicine". Skeptical Inquirer Magazine.
{{cite journal}}: Unknown parameter|month=ignored (help) - Planer, Felix E. (1988). Superstition (Revised ed.). Buffalo, New York: Prometheus Books. ISBN 978-0-87975-494-5. OCLC 18616238.
- Rosenfeld, Anna (circa 2000). "Where Do Americans Go for Healthcare?". Cleveland, Ohio: Case Western Reserve University. Retrieved 23 September 2010.
{{cite web}}: Check date values in:|year=(help)CS1 maint: year (link) - Singh, S (2008). Trick or treatment: The undeniable facts about alternative medicine. Norton. ISBN 978-0-393-06661-6. OCLC 181139440.
{{cite book}}: Unknown parameter|coauthors=ignored (|author=suggested) (help); preview at Google Books - Tonelli MR (2001). "The limits of evidence-based medicine". Respiratory Care. 46 (12): 1435–40, discussion 1440–1. PMID 11728302.
{{cite journal}}: Unknown parameter|month=ignored (help) - Trivieri Larry, Jr.; Anderson, John W., eds. (2002). Alternative Medicine: The Definitive Guide. Berkeley: Ten Speed Press. ISBN 978-1-58761-141-4.
- Wisneski LA, Anderson L (2005). The Scientific Basis of Integrative Medicine. CRC Press. ISBN 978-0-8493-2081-1.
- Zalewski Z (1999). "Importance of philosophy of science to the history of medical thinking". CMJ. 40 (1): 8–13. Archived from the original on 2004-02-06.
World Health Organization publication
Journals dedicated to alternative medicine research
- Alternative therapies in health and medicine. Aliso Viejo, CA : InnoVision Communications, c1995- NLM ID: 9502013
- Alternative medicine review : a journal of clinical therapeutic. Sandpoint, Idaho : Thorne Research, Inc., c1996- NLM ID: 9705340
- BMC complementary and alternative medicine. London : BioMed Central, 2001- NLM ID: 101088661
- Complementary therapies in medicine. Edinburgh ; New York : Churchill Livingstone, c1993- NLM ID: 9308777
- Evidence based complementary and alternative medicine
- Evidence Based journal of Integrative medicine
- Forschende Komplementärmedizin / Research in Complementary Medicine
- Journal of Integrative medicine.
- Journal for Alternative and Complementary Medicine New York, NY : Mary Ann Liebert, Inc., c1995
- Scientific Review of Alternative Medicine (SRAM)
External links
- The National Center for Complementary and Alternative Medicine: U.S. National Institutes of Health
- The Office of Cancer Complementary and Alternative Medicine: U.S. National Cancer Institute, National Institutes of Health
- Knowledge and Research Center for Alternative Medicine: Denmark, the Ministry of the Interior and Health
- Guidelines For Using Complementary and Alternative Methods: from the American Cancer Society
- Complementary and Alternative Medicine Index: from the University of Maryland Medical Center
- Integrative Medicine Podcasts and Handouts: Teaching modules from the University of Wisconsin Integrative Medicine Program
- "Alternative Medicine": A BBC/Open University television series that examines the evidence scientifically
- "Complementary and alternative medicine: What is it?": from the Mayo Clinic
- Natural Standard Research Collaboration
- Alternative Medicine Health Directory
- A Different Way to Heal? and Videos: from PBS and Scientific American Frontiers
- Who Gets to Validate Alternative Medicine?: from PBS
Criticism
- What is Complementary and Alternative Medicine? – Steven Novella, MD
- "Alternative" health practice – Skeptic's Dictionary
- Quackwatch.org – Stephen Barrett (See also: Quackwatch)
- Healing, Hype, or Harm? A Critical Analysis of Complementary or Alternative Medicine, by Edzard Ernst (Editor) (2008), reviewed in Metapsychology.
- What's the harm? Website created by Tim Farley listing cases of people harmed by various alternative treatments.

