Tacrolimus
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Prograf, Advagraf, Protopic |
| Pregnancy category |
|
| Routes of administration | Topical, oral, iv |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | 24% (5–67%), less after eating food rich in fat |
| Protein binding | ≥98.8% |
| Metabolism | Hepatic CYP3A4, CYP3A5 |
| Elimination half-life | 11.3 h for transplant patients (range 3.5–40.6 h) |
| Excretion | Mostly faecal |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.155.367 |
| Chemical and physical data | |
| Formula | C44H69NO12 |
| Molar mass | 804.018 g/mol g·mol−1 |
| 3D model (JSmol) | |
| |
| |
| | |
Tacrolimus (also FK-506 or fujimycin, trade names Prograf, Advagraf, Protopic) is an immunosuppressive drug used mainly after allogeneic organ transplant to lower the risk of organ rejection. It achieves this by inhibiting the production of interleukin-2, a molecule that promotes the development and proliferation of T cells, which are vital to the body's learned (or adaptive) immune response. Tacrolimus is also used in the treatment of other T cell-mediated diseases such as eczema (for which it is applied to the skin in a medicated ointment), severe refractory uveitis after bone marrow transplants, exacerbations of minimal change disease, Kimura's disease, and the skin condition vitiligo.
Chemically it is a 23-membered macrolide lactone that was first discovered in 1987 from the fermentation broth of a Japanese soil sample that contained the bacterium Streptomyces tsukubaensis.
Medical uses
Immunosuppression following transplantation
It has similar immunosuppressive properties to ciclosporin, but is much more potent. Immunosuppression with tacrolimus was associated with a significantly lower rate of acute rejection compared with ciclosporin-based immunosuppression (30.7% vs 46.4%) in one study.[2] Clinical outcome is better with tacrolimus than with ciclosporin during the first year of liver transplantation.[3][4] Long-term outcome has not been improved to the same extent. Tacrolimus is normally prescribed as part of a post-transplant cocktail including steroids, mycophenolate, and IL-2 receptor inhibitors such as basiliximab. Dosages are titrated to target blood levels.
Ulcerative colitis
In recent years, tacrolimus has been used to suppress the inflammation associated with ulcerative colitis (UC), a form of inflammatory bowel disease. Although almost exclusively used in trial cases only, tacrolimus has shown to be significantly effective in the suppression of outbreaks of UC.[5][6]
Dermatological use

As an ointment, tacrolimus is used in the treatment of eczema, in particular atopic dermatitis. It suppresses inflammation in a similar way to steroids, and is equally as effective as a mid-potency steroid. An important advantage of tacrolimus is that, unlike steroids, it does not cause skin thinning (atrophy), or other steroid related side effects.[7]
It is applied on the active lesions until they heal off, but may also be used continuously in low doses (twice a week), and applied to the thinner skin over the face and eyelids.[citation needed] Clinical trials of up to one year have been conducted. Recently it has also been used to treat segmental vitiligo in children, especially in areas on the face.[8]
Available forms
The branded version of the drug is owned by Astellas Pharma, and is sold under the trade name Prograf, given twice daily. A number of other manufacturers hold marketing authorisation for alternative brands of the twice-daily formulation.[9]
Once-daily formulations with marketing authorisation include Advagraf (Astellas Pharma) and Envarsus (marketed as Envarsus XR in US by Veloxis Pharmaceuticals and marketed in Europe by Chiesi).[9] These formulations are intended to reduce pharmacokinetic variation in blood levels and facilitate compliance with dosing.
The topical formulation is also marketed by Astellas Pharma under the name Protopic.[9]
Contraindications and precautions
Contraindications and precautions include:[10]
- Breast-feeding
- Hepatic disease
- Immunosuppression
- Infants
- Infection
- Neoplastic disease, such as:
- Oliguria
- Pregnancy
- QT interval prolongation
- Sunlight (UV) exposure
- Grapefruit juice[11]
For topical use
- Occlusive dressing
- Known or suspected malignant lesions
- Netherton's syndrome or similar skin diseases
- Certain skin infections[7]
Side effects
From oral and intravenous administration
Side effects can be severe and include infection, cardiac damage, hypertension, blurred vision, liver and kidney problems (tacrolimus nephrotoxicity),[12] hyperkalemia, hypomagnesemia, hyperglycemia, diabetes mellitus, itching, lung damage (sirolimus also causes lung damage),[13] and various neuropsychiatric problems such as loss of appetite, insomnia, posterior reversible encephalopathy syndrome, confusion, weakness, depression, vivid nightmares, cramps, neuropathy, seizures, tremors, and catatonia.[14]
In addition, it may potentially increase the severity of existing fungal or infectious conditions such as herpes zoster or polyoma viral infections.[10]
Carcinogenesis and mutagenesis
In people receiving immunosuppressants to reduce transplant graft rejection, an increase risk of malignancy (cancer) is a recognised complication.[10] The most common cancers are non-Hodgkin's lymphoma[citation needed] and skin cancers. The risk appears to be related to the intensity and duration of treatment.
From topical use
The most common adverse events associated with the use of topical tacrolimus ointments, especially if used over a wide area, include a burning or itching sensation on the initial applications, with increased sensitivity to sunlight and heat on the affected areas. Less common are flu-like symptoms, headache, cough, and burning eyes.[15]
Cancer risks
Tacrolimus and a related drug for eczema (pimecrolimus) were suspected of carrying a cancer risk, though the matter is still a subject of controversy. The FDA issued a health warning in March 2005 for the drug, based on animal models and a small number of patients. Until further human studies yield more conclusive results, the FDA recommends that users be advised of the potential risks. However, current practice by UK dermatologists is not to consider this a significant real concern and they are increasingly recommending the use of these new drugs.[16]
Interactions
Also like ciclosporin, it has a wide range of interactions. Tacrolimus is primarily metabolised by the cytochrome P450 system of liver enzymes, and there are many substances that interact with this system and induce or inhibit the system's metabolic activity.[10]
Interactions include that with grapefruit which increases tacrolimus plasma concentrations. As infections are a major cause of morbidity and mortality in the post-transplant patient, the most commonly[citation needed] reported interactions include interactions with anti-microbial drugs. Macrolide antibiotics including erythromycin and clarithromycin, as well as several of the newer classes of antifungals, especially of the azole class (fluconazole, voriconazole), increase tacrolimus levels by competing for cytochrome enzymes.[10]
Pharmacology
Mechanism of action
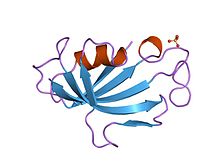
Tacrolimus is a macrolide calcineurin inhibitor. In T-cells, activation of the T-cell receptor normally increases intracellular calcium, which acts via calmodulin to activate calcineurin. Calcineurin then dephosphorylates the transcription factor nuclear factor of activated T-cells (NF-AT), which moves to the nucleus of the T-cell and increases the activity of genes coding for IL-2 and related cytokines. Tacrolimus prevents the dephosphorylation of NF-AT.[17]
In detail, tacrolimus reduces peptidylprolyl isomerase activity by binding to the immunophilin FKBP12 (FK506 binding protein), creating a new complex. This FKBP12–FK506 complex interacts with and inhibits calcineurin, thus inhibiting both T-lymphocyte signal transduction and IL-2 transcription.[18] Although this activity is similar to that of ciclosporin, the incidence of acute rejection is reduced by tacrolimus use over ciclosporin use.[2] Although short-term immunosuppression concerning patient and graft survival is found to be similar between the two drugs, tacrolimus results in a more favorable lipid profile, and this may have important long-term implications given the prognostic influence of rejection on graft survival.[19]
Pharmacokinetics
Oral tacrolimus is slowly absorbed in the gastrointestinal tract, with a total bioavailability of 20 to 25% (but with variations from 5 to 67%) and highest blood plasma concentrations (Cmax) reached after one to three hours. Taking the drug together with a meal, especially one rich in fat, slows down resorption and reduces bioavailability. In the blood, tacrolimus is mainly bound to erythrocytes; only 5% are found in the plasma, of which more than 98.8% are bound to plasma proteins.[10][20]
The substance is metabolized in the liver, mainly via CYP3A, and in the intestinal wall. All metabolites found in the circulation are inactive. Biological half-life varies widely and seems to be higher for healthy persons (43 hours on average) than for patients with liver transplants (12 hours) or kidney transplants (16 hours), due to differences in clearance. Tacrolimus is predominantly eliminated via the faeces in form of its metabolites.[10][20]
When applied locally on eczema, tacrolimus has little to no bioavailability.[10]
Pharmacogenetics
The predominant enzyme responsible for metabolism of tacrolimus is CYP3A5. Genetic variations within CYP3A5 that result in changes to the activity of the CYP3A5 protein can affect concentrations of tacrolimus within the body. In particular, individuals who are homozygous for the G allele at the single nucleotide polymorphism (SNP) rs776746 (also known as CYP3A5 *3/*3) have a non-functional CYP3A5 protein. The frequency of the G allele varies worldwide, from 4% in some African populations to 80–90% in Caucasian populations.[21] Across a large number of studies, individuals homozygous for the G allele have been shown to have higher concentrations of tacrolimus and require lower doses of the drug, as compared to individuals who are not homozygous for the G allele. Achieving target concentrations of tacrolimus is important – if levels are too low, then there is a risk of transplant rejection, if levels are too high, there is a risk of drug toxicities. There is evidence to suggest that dosing patients based on rs776746 genotype can result in faster and more frequent achievement of target tacrolimus levels. However, there is a lack of consistent evidence as to whether dosing based on rs776746 genotype results in improved clinical outcomes (such as a decreased risk for transplant rejection or drug toxicities), likely because patients taking tacrolimus are subject to therapeutic drug monitoring.[22][23][24][25]
History
Tacrolimus was discovered in 1987;[26] it was among the first macrolide immunosuppressants discovered, preceded by the discovery of rapamycin (sirolimus) on Rapa Nui (Easter Island) in 1975.[27] It is produced by a soil bacterium, Streptomyces tsukubaensis.[28] The name tacrolimus is derived from "Tsukuba macrolide immunosuppressant".[29]
Tacrolimus was first approved by the Food and Drug Administration in 1994 for use in liver transplantation; this has been extended to include kidney, heart, small bowel, pancreas, lung, trachea, skin, cornea, bone marrow, and limb transplants.
See also
- Tohru Kino
- Stuart Schreiber
- Thomas Starzl
- FK1012, a derivative
References
- ^ "FDA-sourced list of all drugs with black box warnings (Use Download Full Results and View Query links.)". nctr-crs.fda.gov. FDA. Retrieved 22 Oct 2023.
- ^ a b McCauley, Jerry (2004-05-19). "Long-Term Graft Survival In Kidney Transplant Recipients". Slide Set Series on Analyses of Immunosuppressive Therapies. Medscape. Retrieved 2006-06-06.
- ^ Haddad EM, McAlister VC, Renouf E, Malthaner R, Kjaer MS, Gluud LL (2006). McAlister V (ed.). "Cyclosporin versus Tacrolimus for Liver Transplanted Patients". Cochrane Database of Systematic Reviews. 4 (CD005161): CD005161. doi:10.1002/14651858.CD005161.pub2. PMID 17054241.
- ^ O'Grady JG, Burroughs A, Hardy P, Elbourne D, Truesdale A, The UK and Ireland Liver Transplant Study Group (2002). "Tacrolimus versus emulsified cyclosporin in liver transplantation: the TMC randomised controlled trial". Lancet. 360 (9340): 1119–1125. doi:10.1016/S0140-6736(02)11196-2. PMID 12387959.
- ^ Baumgart DC, Pintoffl JP, Sturm A, Wiedenmann B, Dignass AU (2006). "Tacrolimus is safe and effective in patients with severe steroid-refractory or steroid-dependent inflammatory bowel disease--a long-term follow-up". Am J Gastroenterol. 101 (5): 1048–1056. doi:10.1111/j.1572-0241.2006.00524.x. PMID 16573777.
- ^ Baumgart DC, Macdonald JK, Feagan B (2008). Baumgart DC (ed.). "Tacrolimus (FK506) for induction of remission in refractory ulcerative colitis". Cochrane Database Syst Rev. 16 (3): CD007216. doi:10.1002/14651858.CD007216. PMID 18646177.
- ^ a b Haberfeld, H, ed. (2015). Austria-Codex (in German). Vienna: Österreichischer Apothekerverlag. Protopic.
- ^ Silverberg, NB; Lin, P; Travis, L; Farley-Li, J; Mancini, AJ; Wagner, AM; Chamlin, SL; Paller, AS (2004). "Tacrolimus ointment promotes repigmentation of vitiligo in children: a review of 57 cases". Journal of the American Academy of Dermatology. 51 (5): 760–6. doi:10.1016/j.jaad.2004.05.036. PMID 15523355.
- ^ a b c Joint Formulary Committee. "British National Formulary (online)". London: BMJ Group and Pharmaceutical Press. Retrieved 24 September 2015.
- ^ a b c d e f g h Haberfeld, H, ed. (2015). Austria-Codex (in German). Vienna: Österreichischer Apothekerverlag. Prograf.
- ^ Fukatsu S, Fukudo M, Masuda S, Yano I, Katsura T, Ogura Y, Oike F, Takada Y, Inui K (2006). "Delayed effect of grapefruit juice on pharmacokinetics and pharmacodynamics of tacrolimus in a living-donor liver transplant recipient". Drug Metab Pharmacokinet. 21 (2): 122–5. doi:10.2133/dmpk.21.122. PMID 16702731.
- ^ Naesens M, Kuypers DR, Sarwal M (2009). "Calcineurin inhibitor nephrotoxicity". Clin. J. Am. Soc. Nephrol. 4 (2): 481–509. doi:10.2215/CJN.04800908. PMID 19218475.
- ^ Miwa Y, Isozaki T, Wakabayashi K, et al. (2008). "Tacrolimus-induced lung injury in a rheumatoid arthritis patient with interstitial pneumonitis". Mod Rheumatol. 18 (2): 208–11. doi:10.1007/s10165-008-0034-3. PMID 18306979.
- ^ O'Donnell MM, Williams JP, Weinrieb R, Denysenko L (2007). "Catatonic mutism after liver transplant rapidly reversed with lorazepam". Gen Hosp Psychiatry. 29 (3): 280–1. doi:10.1016/j.genhosppsych.2007.01.004. PMID 17484951.
- ^ Hanifin JM, Paller AS, Eichenfield L, Clark RA, Korman N, Weinstein G, Caro I, Jaracz E, Rico MJ, US Tacrolimus Ointment Study Group (2005). "Efficacy and safety of tacrolimus ointment treatment for up to 4 years in patients with atopic dermatitis". J Am Acad Derm. 53 (2 suppl 2): S186–94. doi:10.1016/j.jaad.2005.04.062. PMID 16021174.
{{cite journal}}: Cite has empty unknown parameter:|1=(help) - ^ N H Cox; Catherine H Smith (December 2002). "Advice to dermatologists re topical tacrolimus" (PDF). Therapy Guidelines Committee. British Association of Dermatologists.
{{cite web}}: Unknown parameter|lastauthoramp=ignored (|name-list-style=suggested) (help) - ^ William F. Ganong. Review of medical physiology (22nd ed.). Lange medical books. p. 530. ISBN 0-07-144040-2.
- ^ Liu J, Farmer J, Lane W, Friedman J, Weissman I, Schreiber S (1991). "Calcineurin is a common target of cyclophilin-cyclosporin A and FKBP-FK506 complexes". Cell. 66 (4): 807–15. doi:10.1016/0092-8674(91)90124-H. PMID 1715244.
- ^ M.M. Abou-Jaoude; R. Naim; J. Shaheen; N. Naufal; S. Abboud; M. AlHabash; M. Darwish; A. Mulhem; A. Ojjeh; W.Y. Almawi (2005). "Tacrolimus (FK506) versus cyclosporin microemulsion (Neoral) as maintenance immunosuppresion therapy in kidney transplant recipients". Transplantation Proceedings. 37 (7): 3025–3028. doi:10.1016/j.transproceed.2005.08.040. PMID 16213293.
{{cite journal}}: Unknown parameter|last-author-amp=ignored (|name-list-style=suggested) (help) - ^ a b Dinnendahl, V; Fricke, U, eds. (2003). Arzneistoff-Profile (in German). Vol. 9 (18 ed.). Eschborn, Germany: Govi Pharmazeutischer Verlag. ISBN 978-3-7741-9846-3.
- ^ Bains, Ripudaman Kaur. "Molecular diversity and population structure at the CYP3A5 gene in Africa" (PDF). University College London. Retrieved 13 June 2016.
- ^ Staatz, CE; Tett, SE (2004). "Clinical pharmacokinetics and pharmacodynamics of tacrolimus in solid organ transplantation". Clinical pharmacokinetics. 43 (10): 623–53. doi:10.2165/00003088-200443100-00001. PMID 15244495.
- ^ Staatz, CE; Goodman, LK; Tett, SE (March 2010). "Effect of CYP3A and ABCB1 single nucleotide polymorphisms on the pharmacokinetics and pharmacodynamics of calcineurin inhibitors: Part I.". Clinical pharmacokinetics. 49 (3): 141–75. doi:10.2165/11317350-000000000-00000. PMID 20170205.
- ^ Staatz, CE; Goodman, LK; Tett, SE (April 2010). "Effect of CYP3A and ABCB1 single nucleotide polymorphisms on the pharmacokinetics and pharmacodynamics of calcineurin inhibitors: Part II". Clinical pharmacokinetics. 49 (4): 207–21. doi:10.2165/11317550-000000000-00000. PMID 20214406.
- ^ Barbarino, JM; Staatz, CE; Venkataramanan, R; Klein, TE; Altman, RB (October 2013). "PharmGKB summary: cyclosporine and tacrolimus pathways". Pharmacogenetics and genomics. 23 (10): 563–85. doi:10.1097/fpc.0b013e328364db84. PMID 23922006.
- ^ Kino, T.et al.FK-506, a novel immunosuppressant isolated from aStreptomyces.1. Fermentation, isolation, and physico-chemical and biological characteristics. J. Antibiot.40,1249–1255 (1987).
- ^ Kino T, Hatanaka H, Hashimoto M, Nishiyama M, Goto T, Okuhara M, Kohsaka M, Aoki H, Imanaka H (1987). "FK-506, a novel immunosuppressant isolated from a Streptomyces. I. Fermentation, isolation, and physico-chemical and biological characteristics". J Antibiot (Tokyo). 40 (9): 1249–55. doi:10.7164/antibiotics.40.1249. PMID 2445721.
- ^ Pritchard D (2005). "Sourcing a chemical succession for cyclosporin from parasites and human pathogens". Drug Discov Today. 10 (10): 688–91. doi:10.1016/S1359-6446(05)03395-7. PMID 15896681. Supports source organism, but not team information
- ^ Ponner, B, Cvach, B (Fujisawa Pharmaceutical Co.): Protopic Update 2005
External links
- Tacrolimus levels in Liver Transplants-Indian Study by Dr.Pradeep Naik,Dr.Dharmesh Kapoor, Dr.DCS Reddy
- Prograf prescribing information at Fujisawa
- Pimecrolimus (Elidel Cream) FDA adivisory page (for eczema treatment)
- Tacrolimus (FK506) product page from Fermentek
- U.S. National Library of Medicine: Drug Information Portal - Tacrolimus
