Urinary tract infection: Difference between revisions
No edit summary |
added |
||
| Line 121: | Line 121: | ||
In what concerns the symptoms of the condition, bacteriuria appears to increase in prevalence with age in women, still being 50 times greater than the one in males. It is estimated that bacteriuria will be experienced by 20 to 50% of older women and 5 to 20% of older men. |
In what concerns the symptoms of the condition, bacteriuria appears to increase in prevalence with age in women, still being 50 times greater than the one in males. It is estimated that bacteriuria will be experienced by 20 to 50% of older women and 5 to 20% of older men. |
||
==Indwelling catheters== |
|||
[[Indwelling catheters]] are a risk factor for urinary tract infections. The risk of an associated infection can be decreased by only catheterizing when necessary, using [[aseptic technique]] for insertion, and maintaining unobstructed closed drainage of the catheter.<ref>{{cite journal |author=Nicolle LE |title=The chronic indwelling catheter and urinary infection in long-term-care facility residents |journal=Infect Control Hosp Epidemiol |volume=22 |issue=5 |pages=316–21 |year=2001 |month=May |pmid=11428445 |doi=10.1086/501908 |url=}}</ref><ref>{{cite journal |author=Phipps S, Lim YN, McClinton S, Barry C, Rane A, N'Dow J |title=Short term urinary catheter policies following urogenital surgery in adults |journal=Cochrane Database Syst Rev |volume= |issue=2 |pages=CD004374 |year=2006 |pmid=16625600 |doi=10.1002/14651858.CD004374.pub2 |url=}}</ref><ref>{{cite journal |author=Gould CV, Umscheid CA, Agarwal RK, Kuntz G, Pegues DA |title=Guideline for prevention of catheter-associated urinary tract infections 2009 |journal=Infect Control Hosp Epidemiol |volume=31 |issue=4 |pages=319–26 |year=2010 |month=April |pmid=20156062 |doi=10.1086/651091 |url=}}</ref> |
|||
==References== |
==References== |
||
Revision as of 22:37, 15 July 2010
| Urinary tract infection | |
|---|---|
| Specialty | Urology |
A urinary tract infection (UTI) is a bacterial infection that affects any part of the urinary tract. The main etiologic agent is Escherichia coli. Although urine contains a variety of fluids, salts, and waste products, it does not usually have bacteria in it.[1] When bacteria gets into the bladder or kidney and multiply in the urine, they may cause an UTI.
The most common type of UTI is acute cystitis often referred to as a bladder infection. An infection of the upper urinary tract or kidney is known as pyelonephritis, and is potentially more serious. Although they cause discomfort, urinary tract infections can usually be easily treated with a short course of antibiotics.[2] Symptoms include frequent feeling and/or need to urinate, pain during urination, and cloudy urine.[3]
Signs and symptoms
The most common symptoms of a bladder infection are burning with urination (dysuria), frequency of urination, an urge to urinate, without vaginal discharge or significant pain.[4] An upper urinary tract infection or pyelonephritis may additionally present with flank pain and a fever. Healthy women have an average of 5 days of symptoms.[4]
The symptoms of urinary tract infections may vary with age and the part of the urinary system that was affected. In young children, urinary tract infection symptoms may include diarrhea, loss of appetite, nausea and vomiting, fever and excessive crying that cannot be resolved by typical measures. [5] Older children on the other hand may experience abdominal pain, or incontinence. Lower urinary tract infections in adults may manifest with symptoms including hematuria (blood in the urine), inability to urinate despite the urge and malaise. [6]
Other signs of urinary tract infections include foul smelling urine and urine that appears cloudy. [7]
Depending on the site of infection, urinary tract infections may cause different symptoms. Urethritis, meaning only the urethra has been affected, does not usually cause any other symptoms besides dysuria. If the bladder is however affected (cystitis), the patient is likely to experience more symptoms including lower abdomen discomfort, low-grade fever, pelvic pressure and frequent urination all together with dysuria. [8] Infection of the kidneys (acute pyelonephritis) typically causes more serious symptoms such as chills, nausea, vomiting and high fever.
Whereas in newborns the condition may cause jaundice and hypothermia, in the elderly, symptoms of urinary tract infections may even include lethargy and a change in the mental status, signs that are otherwise nonspecific.
Risk factors
Sexual activity
In young sexually active women, sex is the cause of 75—90 % of bladder infections, with the risk of infection related to the frequency of sex.[4] The term "honeymoon cystitis" has been applied to this phenomenon of frequent UTIs during early marriage. In post menopausal women sexual activity does not affect the risk of developing a UTI.[4] Spermicide use independent of sexual frequency increase the risk of UTIs.[4]
Gender
Women are more prone to UTIs than men because in females, the urethra is much shorter and closer to the anus than in males,[9] and they lack the bacteriostatic properties of prostatic secretions. Among the elderly, UTI frequency is roughly equal proportions in women and men. This is due, in part, to an enlarged prostate in older men. An enlarged prostate means the gland has grown bigger. Prostate enlargement happens to almost all men as they get older. As the gland grows, it can press on the urethra and cause urination and bladder problems. As the gland grows, it obstructs the urethra, leading to increased difficulty in micturition. Because there is less urine flushing the urethra, there is a higher incidence of e. coli colonization.
Urinary catheters
Indwelling urinary catheters increase the risk of UTIs. Staphylococcus epidermidis is most common organism. Scrupulous aseptic techniques or the use of intermitent catherterization rather than an indwelling catherter may decrease these associated risks.
Genetics
A predisposition for bladder infections may run in families.[4]
Others
Other risk factors include diabetics[4] sickle-cell disease or anatomical malformations of the urinary tract such as prostate enlargement.
While ascending infections are generally the rule for lower urinary tract infections and cystitis, the same is not necessarily true for upper urinary tract infections like pyelonephritis which may originate from a blood born infection.
Pathogenesis
The most common organism implicated in UTIs (80—85 %) is E. Coli,[4] while Staphylococcus saprophyticus is the cause in 5—10 %.[4]
The bladder wall is coated with various mannosylated proteins, such as Tamm-Horsfall proteins (THP), which interfere with the binding of bacteria to the uroepithelium. As binding is an important factor in establishing pathogenicity for these organisms, its disruption results in reduced capacity for invasion of the tissues.[clarification needed] Moreover, the unbound bacteria are more easily removed when voiding. The use of urinary catheters (or other physical trauma) may physically disturb this protective lining, thereby allowing bacteria to invade the exposed epithelium.
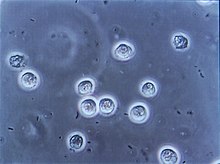
During cystitis, uropathogenic Escherichia coli (UPEC) subvert innate defenses by invading superficial umbrella cells and rapidly increasing in numbers to form intracellular bacterial communities (IBCs).[10] By working together, bacteria in biofilms build themselves into structures that are more firmly anchored in infected cells and are more resistant to immune system assaults and antibiotic treatments [11] This is often the cause of chronic urinary tract infections.
Prevention
The following are measures that studies suggest may reduce the incidence of urinary tract infections.
- A prolonged course ( 6 months to a year ) of low-dose antibiotics (usually nitrofurantoin or TMP/SMX) is effective in reducing the frequency of UTIs in those with recurrent UTIs.[4]
- Cranberry (juice or capsules) may decrease the incidence of UTI in those with frequent infections. Long term tolerance however is an issue.[12]
- For post-menopausal women intravaginal application of topical estrogen cream can prevent recurrent cystitis.[13] This however is not as useful as low dose antibiotics.[4]
- Studies have shown that breastfeeding can reduce the risk of UTIs in infants.[14]
Different prevention measures are indicated by medical health providers, particularly in individuals in whom the condition has recurred. Although the prevention measures do not ensure protection against the bacteria that might cause urinary tract infections, they may help reducing the risks of developing this condition. Firstly, patients are most likely to be advised to increase the daily consumption of liquids, particularly water. This will result in urinating more frequently, flushing away the bacteria that may have built up within the urinary tract, as well as hydrating the patient. It is also important not to resist the urge to urinate ("hold it in"), as this leads to the accumulation of bacteria. Although some specialists recommend cranberry juice as prevention measure it is not to be taken at the same time with medications that contain warfarin.
Changes in the personal hygiene might be suggested as well. Wiping from front to back after urinating may actually help in removing the possibility of the bacteria next to the anus spreading to the vagina and urethra, and therefore this could be an effective preventive measure although limited. [15]
As urinary tract infections are likely to occur after sexual intercourse because of the increased risks that the bacteria gets into the urinary tract, patients are usually advised to urinate after intercourse, immediately if possible, to flush away the bacteria from the system. Drinking water may also help. Some specialists recommend also cleansing the genital area before intercourse. [16]
Some cases of urinary tract infections are attributed to the use of feminine products that may irritate the urethra. Commonly, women are advised to avoid using such products which include douches and powders.
To avoid urinary tract infections in newborns, mothers are advised to change soiled diapers as soon as possible.
Ineffective measures
A number of measures that have not been found to affect UTI frequency include: the use of birth control pills or condoms, personal hygiene methods used after urinating or defecating, whether one takes a bath or shower.[4]
Diagnosis
In straight forward cases a diagnosis may be made and treatment given based on symptoms alone without further laboratory confirmation.[4] In complicated or questionable cases confirmation via urinalysis looking for the presence of nitrites, leukocytes or leukocyte esterase or via urine microscopy looking for the presence of red blood cells, white blood cells, and bacteria maybe useful.[4]
Urine culture showing a quantitative count of greater than or equal to colony forming units (CFU) per mL of a typical urinary tract organism along with antibiotic sensitives is useful to guide antibiotic choice.[4] However women with negative cultures may still improve with antibiotic treatment.[4]
Most cases of lower urinary tract infections in females are benign and do not need exhaustive laboratory work-ups. However, UTI in young infants may receive some imaging study, typically a retrograde urethrogram, to ascertain the presence/absence of congenital urinary tract anomalies. All males with a confirmed UTI should be investigated further. Specific methods of investigation include x-ray, nuclear medicine, MRI and CAT scans.
Differential
If the urine culture is negative:
- symptoms of urethritis may point at Chlamydia trachomatis or Neisseria gonorrheae infection.
- symptoms of cystitis may point at interstitial cystitis.
- in men, prostatitis may present with dysuria.
The presence of bacteria in the urinary tract of older adults, without symptoms or signs of infection, is a well recognized phenomenon which may not require antibiotics. This is usually referred to as asymptomatic bacteriuria. The overuse of antibiotics in the context of bacteriuria among the elderly is a concerning issue.
Treatment
Uncomplicated
Uncomplicated UTIs can be diagnosed and treated based on symptoms alone.[4] Oral antibiotics such as trimethoprim, cephalosporins, nitrofurantoin, or a fluoroquinolone such as ciprofloxacin substantially shorten the time to recovery. About 50% of people will recover without treatment within a few days or weeks.[4] The Infectious Diseases Society of America recommends a combination of trimethoprim and sulfamethoxazole as a first line agent in uncomplicated UTIs rather than fluoroquinolones.[17] Resistance has developed in the community to all of these medications due to their widespread use.[4]
A three-days treatment with trimethoprim, TMP/SMX, or a fluoroquinolone is usually sufficient while nitrofurantoin requires 7 days.[4] Trimethoprim is often recommended to be taken at night to ensure maximal urinary concentrations to increase its effectiveness. While trimethoprim / sulfamethoxazole was previously internationally used (and continues to be used in the U.S. and Canada); the addition of the sulfonamide gives little additional benefit compared to the trimethoprim component alone. It is responsible however for a high incidence of mild allergic reactions and rare but potentially serious complications. For simple UTIs children often respond well to a three-day course of antibiotics.[18]
Phenazopyridine can help with painful urination.[citation needed]
Pyelonephritis
Pyelonephritis is treated more aggressively than a simple bladder infection using either a longer course of oral antibiotics or intravenous antibiotics. Regimens vary, and include SMX/TMP and fluorquinolones. In the past, they have included aminoglycosides (such as gentamicin) used in combination with a beta-lactam, such as ampicillin or ceftriaxone. These are continued for 48 hours after fever subsides.
If there is a poor response to IV antibiotics (marked by persistent fever, worsening renal function), then imaging is indicated to rule out formation of an abscess either within or around the kidney, or the presence of an obstructing lesion such as a stone or tumor.[19]
Recurrent
Women with recurrent simple UTIs may benefit from self-treatment upon occurrence of symptoms with medical follow up only if the initial treatment fails.[4] Effective treatment can also be delivered over the phone.[4]
Epidemiology
Bladder infections are most common in young women with 10% of women getting an infection yearly and 60% having an infection at some point in their life.[4] Pyelonephritis occurs between 18—29 times less frequently.[4]
According to the 1997 National Ambulatory Medical Care Survey and National Hospital Ambulatory Medical Care Survey, urinary tract infection accounted for nearly 7 million office visits and 1 million emergency department visits, resulting in 100,000 hospitalizations. [20]
Nearly 1 in 3 women will have had at least 1 episode of urinary tract infections requiring antimicrobial therapy by the age of 24 years. The risk of urinary tract infection increases with increasing duration of catheterization. In non-institutionalized elderly populations, urinary tract infections are the second most common form of infection, accounting for nearly 25% of all infections. [21]
The condition rarely occurs in men who are younger than 50 years old and who did not undergo any genitourinary procedure. However, the incidence of urinary tract infections in men tends to rise after the age of 50.
According to statistics from 1990, the prevalence of urinary tract infections in pre-school and school girls was 1% to 3%, nearly 30-fold higher than that in boys. [22] Also, the statistics from the same year show that approximately 5% of girls will develop at least one urinary tract infection in their school years.
In what concerns the symptoms of the condition, bacteriuria appears to increase in prevalence with age in women, still being 50 times greater than the one in males. It is estimated that bacteriuria will be experienced by 20 to 50% of older women and 5 to 20% of older men.
Indwelling catheters
Indwelling catheters are a risk factor for urinary tract infections. The risk of an associated infection can be decreased by only catheterizing when necessary, using aseptic technique for insertion, and maintaining unobstructed closed drainage of the catheter.[23][24][25]
References
- ^ "Adult Health Advisor 2005.4: Bacteria in Urine, No Symptoms (Asymptomatic Bacteriuria)". Retrieved 2007-08-25.
- ^ "Urinary Tract Infections". Retrieved 2007-08-25.
- ^ "Bladder Infections". Retrieved 2010-02-04. "Urinary Tract Infections". Retrieved 2010-02-04.
- ^ a b c d e f g h i j k l m n o p q r s t u v w x Nicolle LE (2008). "Uncomplicated urinary tract infection in adults including uncomplicated pyelonephritis". Urol. Clin. North Am. 35 (1): 1–12, v. doi:10.1016/j.ucl.2007.09.004. PMID 18061019.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ "Signs and Symptoms". Retrieved 2010-06-25.
- ^ "Signs and Symptoms". Retrieved 2010-06-25.
- ^ "Bladder Infection and Cancer Treatment". Retrieved 2010-06-25.
- ^ "Symptoms". Retrieved 2010-06-25.
- ^ Urethra length is approximately 25–50 mm (1–2 in) long in females, versus about 20 cm (8 in) in males.[citation needed]
- ^ Justice S, Hunstad D, Seed P, Hultgren S (2006). "Filamentation by Escherichia coli subverts innate defenses during urinary tract infection". Proc Natl Acad Sci USA. 103 (52): 19884–9. doi:10.1073/pnas.0606329104. PMC 1750882. PMID 17172451.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ http://www.biofilmsonline.com/cgi-bin/biofilmsonline/00448.html
- ^ Jepson RG, Craig JC (2008). "Cranberries for preventing urinary tract infections". Cochrane Database Syst Rev (1): CD001321. doi:10.1002/14651858.CD001321.pub4. PMID 18253990.
- ^ Raz R, Stamm W (1993). "A controlled trial of intravaginal estriol in postmenopausal women with recurrent urinary tract infections". N Engl J Med. 329 (11): 753–6. doi:10.1056/NEJM199309093291102. PMID 8350884.
- ^ Hanson, LÅ (2004). "Protective effects of breastfeeding against urinary tract infection". Acta Pædiatr (93): 154–6.
- ^ "Prevention". Retrieved 2010-06-25.
- ^ "UTI Prevention". Retrieved 2010-06-25.
- ^ "Fluroquinolone Drug Class Review". Oregon State University College of Pharmacy. 2002. Retrieved 4 September 2009.
- ^ "BestBets: Is a short course of antibiotics better than a long course in the treatment of UTI in children".
- ^ Toxic Shock Syndrome: Bacterial Infections at Merck Manual of Diagnosis and Therapy Home Edition
- ^ "Epidemiology of urinary tract infections: incidence, morbidity, and economic costs". Retrieved 2010-06-25.
- ^ "pidemiology of urinary tract infections: incidence, morbidity, and economic costs". Retrieved 2010-06-25.
- ^ "The epidemiology of urinary tract infection and the concept of significant bacteriuria". Retrieved 2010-06-25.
- ^ Nicolle LE (2001). "The chronic indwelling catheter and urinary infection in long-term-care facility residents". Infect Control Hosp Epidemiol. 22 (5): 316–21. doi:10.1086/501908. PMID 11428445.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Phipps S, Lim YN, McClinton S, Barry C, Rane A, N'Dow J (2006). "Short term urinary catheter policies following urogenital surgery in adults". Cochrane Database Syst Rev (2): CD004374. doi:10.1002/14651858.CD004374.pub2. PMID 16625600.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Gould CV, Umscheid CA, Agarwal RK, Kuntz G, Pegues DA (2010). "Guideline for prevention of catheter-associated urinary tract infections 2009". Infect Control Hosp Epidemiol. 31 (4): 319–26. doi:10.1086/651091. PMID 20156062.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link)
External links
- NIH articles on Urinary Tract Infections in Adults and in Children.
- MedlinePlus Overview urinarytractinfections
- "Urinary tract infection". GPnotebook.
- Urinary tract infection at Curlie
- Urinary Tract Infection Video

