Intersex
| Intersex topics |
|---|
 |
| Part of a series on |
| LGBTQ topics |
|---|
|
|

Intersex people are individuals born with any of several sex characteristics, including chromosome patterns, gonads, or genitals that, according to the Office of the United Nations High Commissioner for Human Rights, "do not fit typical binary notions of male or female bodies".[1][2]
Sex assignment at birth usually aligns with a child's external genitalia. The number of births with ambiguous genitals is in the range of 1:4,500–1:2,000 (0.02%–0.05%).[3] Other conditions involve the development of atypical chromosomes, gonads, or hormones.[4][2] Some persons may be assigned and raised as a girl or boy but then identify with another gender later in life, while most continue to identify with their assigned sex.[5][6][7] The number of births where the baby is intersex has been reported differently depending on who reports and which definition of intersex is used. Anne Fausto-Sterling and her book co-authors claim the prevalence of "nondimorphic sexual development" in humans might be as high as 1.7%.[8][9] However, a response published by Leonard Sax reports this figure includes conditions such as late onset congenital adrenal hyperplasia and Klinefelter syndrome, which most clinicians do not recognize as intersex; Sax states, "if the term intersex is to retain any meaning, the term should be restricted to those conditions in which chromosomal sex is inconsistent with phenotypic sex, or in which the phenotype is not classifiable as either male or female", stating the prevalence of intersex is about 0.018% (one in 5,500 births), about 100 times less than Fausto-Sterling's estimate.[4][10][11]
Terms used to describe intersex people are contested, and change over time and place. Intersex people were previously referred to as "hermaphrodites" or "congenital eunuchs".[12][13] In the 19th and 20th centuries, some medical experts devised new nomenclature in an attempt to classify the characteristics that they had observed, the first attempt to create a taxonomic classification system of intersex conditions. Intersex people were categorized as either having "true hermaphroditism", "female pseudohermaphroditism", or "male pseudohermaphroditism".[14] These terms are no longer used, and terms including the word "hermaphrodite" are considered to be misleading, stigmatizing, and scientifically specious in reference to humans.[15] In biology, the term "hermaphrodite" is used to describe an organism that can produce both male and female gametes.[16][17] Some people with intersex traits use the term "intersex", and some prefer other language.[18][19][page range too broad] In clinical settings, the term "disorders of sex development" (DSD) has been used since 2006,[20] a shift in language considered controversial since its introduction.[21][22][23]
Intersex people face stigmatization and discrimination from birth, or following the discovery of intersex traits at stages of development such as puberty.[24] Intersex people may face infanticide, abandonment, and stigmatization from their families.[25][26][27] Globally, some intersex infants and children, such as those with ambiguous outer genitalia, are surgically or hormonally altered to create more socially acceptable sex characteristics. This is considered controversial, with no firm evidence of favorable outcomes.[28] Such treatments may involve sterilization. Adults, including elite female athletes, have also been subjects of such treatment.[29][30] Increasingly, these issues are considered human rights abuses, with statements from international[31][32] and national human rights and ethics institutions.[33][34] Intersex organizations have also issued statements about human rights violations, including the 2013 Malta declaration of the third International Intersex Forum.[35] In 2011, Christiane Völling became the first intersex person known to have successfully sued for damages in a case brought for non-consensual surgical intervention.[36] In April 2015, Malta became the first country to outlaw non-consensual medical interventions to modify sex anatomy, including that of intersex people.[37][38]
Terminology
There is no clear consensus definition of intersex and no clear delineation of which specific conditions qualify an individual as intersex.[39] The World Health Organization's International Classification of Diseases (ICD), the American Psychiatric Association's Diagnostic and Statistical Manual of Mental Disorders (DSM), and many medical journals classify intersex traits or conditions among disorders of sex development (DSD).[40]
A common adjective for people with disorders of sex development (DSD) is "intersex".[citation needed]
Etymology and definitions

In 1917, Richard Goldschmidt created the term "intersexuality" to refer to a variety of physical sex ambiguities.[14] However, according to The SAGE Encyclopedia of LGBTQ Studies, it was not until Anne Fausto Sterling published her article "The Five Sexes: Why Male and Female Are Not Enough" in 1993 that the term reached popularity.[41]
According to the UN Office of the High Commissioner for Human Rights:
Intersex people are born with sex characteristics (including genitals, gonads and chromosome patterns) that do not fit typical binary notions of male or female bodies. Intersex is an umbrella term used to describe a wide range of natural bodily variations.[2]
Attitudes towards the term
Some intersex organizations reference "intersex people" and "intersex variations or traits"[42] while others use more medicalized language such as "people with intersex conditions",[43] or people "with intersex conditions or DSDs (differences of sex development)" and "children born with variations of sex anatomy".[44] In May 2016, interACT published a statement recognizing "increasing general understanding and acceptance of the term 'intersex'".[45]
Australian sociological research on 272 "people born with atypical sex characteristics", published in 2016, found that 60% of respondents used the term "intersex" to self-describe their sex characteristics, including people identifying themselves as intersex, describing themselves as having an intersex variation or, in smaller numbers, having an intersex condition. Respondents also commonly used diagnostic labels and referred to their sex chromosomes, with word choices depending on audience.[6][46]
Research on 202 respondents by the Lurie Children's Hospital, Chicago, and the AIS-DSD Support Group (now known as InterConnect Support Group)[47] published in 2017 found that 80% of Support Group respondents "strongly liked, liked or felt neutral about intersex" as a term, while caregivers were less supportive.[48] The hospital reported that the use of the term "disorders of sex development" may negatively affect care.[49]
Another study by a group of children's hospitals in the United States found that 53% of 133 parent and adolescent participants recruited at five clinics did not like the term "intersex".[50] Participants who were members of support groups were more likely to dislike the term.[50] A "dsd-LIFE" study in 2020 found that around 43% of 179 participants thought the term "intersex" was bad, 20% felt neutral about the term, while 37% thought the term was good.[51]
The term "hermaphrodite"
Historically, the term "hermaphrodite" was used in law to refer to people whose sex was in doubt. The 12th century Decretum Gratiani states that "Whether an hermaphrodite may witness a testament, depends on which sex prevails" ("Hermafroditus an ad testamentum adhiberi possit, qualitas sexus incalescentis ostendit").[52][53] Similarly, the 17th century English jurist and judge Edward Coke (Lord Coke), wrote in his Institutes of the Lawes of England on laws of succession stating, "Every heire is either a male, a female, or an hermaphrodite, that is both male and female. And an hermaphrodite (which is also called Androgynus) shall be heire, either as male or female, according to that type of sexe which doth prevaile."[54][55]
During the Victorian era, medical authors attempted to ascertain whether or not humans could be hermaphrodites, adopting a precise biological definition for the term,[56] and making distinctions between "male pseudohermaphrodite", "female pseudohermaphrodite" and especially "true hermaphrodite".[57] These terms, which reflected histology (microscopic appearance) of the gonads, are no longer used.[58][59][60] Until the mid-20th century, "hermaphrodite" was used synonymously with "intersex".[61] Medical terminology shifted in the early 21st century, not only due to concerns about language, but also a shift to understandings based on genetics.[citation needed] The term "hermaphrodite" is also controversial as it implies the existence of someone fully male and fully female. This is a fantasy by certain people who seek "hermaphrodite" sex partners; in the Intersex movement, such people are called "wannafucks".[62] As such the term "hermaphrodite" is often seen as degrading and offensive, although many intersex activists use it as a direct form of self empowerment and critique such as in the ISNA's first newsletter Hermaphrodites with Attitude.[62]
The Intersex Society of North America has stated that hermaphrodites should not be confused with intersex people and that using "hermaphrodite" to refer to intersex individuals is considered to be stigmatizing and misleading.[63]
Prevalence
This section needs additional citations for verification. (June 2024) |

Estimates of the number of people who are intersex vary, depending on which conditions are counted as intersex.[4] The now-defunct Intersex Society of North America stated that:
If you ask experts at medical centers how often a child is born so noticeably atypical in terms of genitalia that a specialist in sex differentiation is called in, the number comes out to about 1 in 1,500 to 1 in 2,000 births [0.07–0.05%]. But a lot more people than that are born with subtler forms of sex anatomy variations, some of which won't show up until later in life.[64]
Anne Fausto-Sterling and her co-authors stated in 2000 that "[a]dding the estimates of all known causes of nondimorphic sexual development suggests that approximately 1.7% of all live births do not conform to a Platonic ideal of absolute sex chromosome, gonadal, genital, and hormonal dimorphism";[9][8] these publications have been widely quoted by intersex activists.[65][66][67] Of the 1.7%, 1.5% points (88% of those considered "nondimorphic sexual development" in this figure) consist of individuals with late onset congenital adrenal hyperplasia (LOCAH) which may be asymptomatic but can present after puberty and cause infertility.[68]
Leonard Sax, in response to Fausto-Sterling, estimated that the prevalence of intersex was about 0.018% of the world's population,[4] discounting several conditions included in Fausto-Sterling's estimate that included LOCAH, Klinefelter syndrome (47,XXY), Turner syndrome (45,X), the chromosomal variants of 47,XYY and 47,XXX, and vaginal agenesis. Sax reasons that in these conditions chromosomal sex is consistent with phenotypic sex and phenotype is classifiable as either male or female.[4]
In a 2003 letter to the editor, political scientist Carrie Hull analyzed the data used by Fausto-Sterling and said the estimated intersex rate should instead have been 0.37%, due to many errors.[69] In a response letter published simultaneously, Fausto-Sterling welcomed the additional analysis and said "I am not invested in a particular final estimate, only that there BE an estimate."[69] A 2018 review reported that the number of births with ambiguous genitals is in the range of 0.02% to 0.05%.[3]
Intersex Human Rights Australia says it maintains 1.7% as its preferred upper limit "despite its flaws", stating both that the estimate "encapsulates the entire population of people who are stigmatized—or risk stigmatization—due to innate sex characteristics", and that Sax's definitions exclude individuals who experience such stigma and who have helped to establish the intersex movement.[70] According to InterACT, a major organization for intersex rights in the US, states that 1.7% of people have some variation of sexual development, 0.5% have atypical genitalia, and 0.05% have mixed/ambiguous genitalia.[71][72][73][74][a] A study relying on a nationally representative survey conducted in Mexico between 2021 and 2022 obtained similar estimates: around 1.6% of individuals aged 15 to 64 reported being born with sex variations.[24]
The following summarizes prevalences of traits that medical experts consider to be intersex (where sex chromosome anomalies are involved, the karyotype is often summarized by the total number of chromosomes followed by the sex chromosomes present in each cell):
| Intersex condition | Sex specificity | Approximate prevalence |
|---|---|---|
| Late onset congenital adrenal hyperplasia (nonclassical forms)[i] | Female (males are generally asymptomatic)[78] | One in 50–1,000 births (0.1–0.2% up to 1–2% depending on population)[79] |
| Hypospadias | Male | One in 200–10,000 male births (0.01%–0.5%), prevalence estimates vary considerably[80] |
| Klinefelter syndrome (47, XXY) | Male | One in 500–1,000 male births (0.1–0.2%)[81] |
| Trisomy X or triple X syndrome (47, XXX) | Female | One in 1,000 female births (0.10%)[82] |
| Turner syndrome (45, X) | Female | One in 2,500 female births (0.04%)[83] |
| Müllerian agenesis (of vagina, i.e., MRKH Syndrome) | Female | One in 4,500 female births (0.022%)[84] |
| Vaginal atresia | Female | One in 5,000 female births (0.02%)[85] |
| 45,X/46,XY mosaicism | None (usually male) | One in 6,666 births (0.015%)[86] |
| 47, XYY syndrome | Male | One in 7,000 male births (0.0142%)[87] |
| Congenital adrenal hyperplasia (classical forms) | None (but virilization of female infants)[79][68] | One in 10,000–20,000 births (0.01–0.02%)[68] |
| 48, XXXY syndrome | Male | One in 50,000 male births (0.002%) |
| 49, XXXXY syndrome | Male | One in 85,000-100,000 male births (0.001%) |
| 48, XXYY syndrome | Male | One in 18,000–40,000 male births (0.0025%–0.0055%)[88] |
| 49, XXXYY syndrome | Male | Less than one in 1000000 births[89][90] |
| XX male or de la Chapelle syndrome | Male[91] | One in 20,000 male births (0.005%)[92] |
| Ovotesticular syndrome | None | One in 20,000 births (0.005%)[93] |
| XY gonadal dysgenesis | Phenotypic female[94] | One in 80,000 births (0.0013%)[95] |
| Androgen insensitivity syndrome (complete and partial phenotypes) | Genetic male[96] | One in 22,000-64,000 male births (0.0045-0.001%)[97] |
| Androgen deficiency | None | No estimate |
| Idiopathic (no discernable medical cause) | None | One in 110,000 births (0.0009%)[98] |
| Iatrogenic (caused by medical treatment, e.g., progestogen administered to pregnant mother) | None | No estimate |
| 5-alpha-reductase deficiency | Male | No estimate[ii] |
| Aromatase excess syndrome | None | No estimate |
| Aromatase deficiency syndrome | None | No estimate |
| Anorchia | Male | One in 20,000 male births (0.005%) |
| Persistent Müllerian duct syndrome | Male | No estimate |
| 46,XX/46,XY | None | No estimate |
| Leydig cell hypoplasia | Male | One in 1,000,000 male births (0.0.0001%) |
| Gonadotropin-releasing hormone insensitivity | None | No estimate |
| Familial male-limited precocious puberty | Male | No estimate |
| Cytochrome P450 oxidoreductase deficiency | None | No estimate |
| Isolated 17,20-lyase deficiency | None | No estimate |
| Testicular dysgenesis syndrome | Male | No estimate |
| Penoscrotal transposition | Male | No estimate |
| Kallmann syndrome | None | One in 30,000 male births, 1 in 125,000 female births (0.003–0.0008%) |
| Hyperandrogenism | None | No estimate |
| Hyperestrogenism | None | No estimate |
| Polyorchidism | Male | No estimate |
| Aphallia | Male | No estimate |
| Cryptorchidism | Male | One in 33–100 male births (3–1%) |
| Cloacal exstrophy (born with XY chromosomes) | Male | One in 400,000 live births (0.0025%) |
Notes:
- ^ Categorization of late onset congenital adrenal hyperplasia as an intersex condition is disputed by some experts[4][77] as explained in the Prevalence section.
- ^ In the Dominican Republic, 5-alpha-reductase deficiency is not uncommon in the town of Las Salinas, resulting in social acceptance of the intersex trait.[99] Men with the trait are called "güevedoces" (Spanish for "eggs at twelve"). 12 out of 13 families had one or more male family members that carried the gene. The overall incidence for the town was 1 in every 90 males were carriers, with other males either non-carriers or non-affected carriers.[100]
History

From early history, societies have been aware of intersex people. Some of the earliest evidence is found in mythology: the Greek historian Diodorus Siculus wrote of the mythological Hermaphroditus in the first century BC, who was "born with a physical body which is a combination of that of a man and that of a woman", and reputedly possessed supernatural properties.[101] He also recounted the lives of Diophantus of Abae and Callon of Epidaurus.[102] Ardhanarishvara, an androgynous composite form of male deity Shiva and female deity Parvati, originated in Kushan culture as far back as the first century AD.[103] A statue depicting Ardhanarishvara is included in India's Meenakshi Temple; this statue clearly shows both male and female bodily elements.[104]
Hippocrates (c. 460 – c. 370 BC, Greek physician) and Galen (129 – c. 200/216 AD, Roman physician, surgeon, and philosopher) both viewed sex as a spectrum between men and women, with "many shades in between, including hermaphrodites, a perfect balance of male and female".[105] Pliny the Elder (AD 23/24–79), a Roman naturalist, described "those who are born of both sexes, whom we call hermaphrodites, at one time androgyni" (from the Greek andr-, "man", and gyn-, "woman").[106] Augustine (354 – 430 AD), the influential Catholic theologian, wrote in The Literal Meaning of Genesis that humans were created in two sexes, despite "as happens in some births, in the case of what we call androgynes".[105]
In medieval and early modern European societies, Roman law, post-classical canon law, and later common law, referred to a person's sex as male, female or hermaphrodite, with legal rights as male or female depending on the characteristics that appeared most dominant.[107] The 12th century Decretum Gratiani states, "Whether an hermaphrodite may witness a testament, depends on which sex prevails."[108][109][110] The foundation of common law, the 17th century Institutes of the Lawes of England described how a hermaphrodite could inherit "either as male or female, according to that kind of sexe which doth prevaile".[111][55] Legal cases have been described in canon law and elsewhere over the centuries.
Some non-European societies have sex or gender systems that recognize more than the two categories of male/man and female/woman. Some of these cultures, for instance the South-Asian Hijra communities, may include intersex people in a third gender category.[112][113] Although—according to Morgan Holmes—early Western anthropologists categorized such cultures as "primitive", Holmes has argued that analyses of these cultures have been simplistic or romanticized and fail to take account of the ways that subjects of all categories are treated.[114]
During the Victorian era, medical authors introduced the terms "true hermaphrodite" for an individual who has both ovarian and testicular tissue, "male pseudo-hermaphrodite" for a person with testicular tissue, but either female or ambiguous sexual anatomy, and "female pseudo-hermaphrodite" for a person with ovarian tissue, but either male or ambiguous sexual anatomy. Some later shifts in terminology have reflected advances in genetics, while other shifts are suggested to be due to pejorative associations.[115]
The term "intersexuality" was coined by Richard Goldschmidt in 1917.[116] The first suggestion to replace the term "hermaphrodite" with "intersex" was made by Cawadias in the 1940s.[61]
Since the rise of modern medical science, some intersex people with ambiguous external genitalia have had their genitalia surgically modified to resemble either female or male genitals. Surgeons pinpointed intersex babies as a "social emergency" when born.[117] An 'optimal gender policy', initially developed by John Money, stated that early intervention helped avoid gender identity confusion, but this lacks evidence.[118] Early interventions have adverse consequences for psychological and physical health.[34] Since advances in surgery have made it possible for intersex conditions to be concealed, many people are not aware of how frequently intersex conditions arise in human beings or that they occur at all.[119]
Dialogue between what were once antagonistic groups of activists and clinicians has led to only slight changes in medical policies and how intersex patients and their families are treated in some locations.[120] In 2011, Christiane Völling became the first intersex person known to have successfully sued for damages in a case brought for non-consensual surgical intervention.[36] In April 2015, Malta became the first country to outlaw non-consensual medical interventions to modify sex anatomy, including that of intersex people.[37] Many civil society organizations and human rights institutions now call for an end to unnecessary "normalizing" interventions, including in the Malta declaration.[121][citation needed]
Human rights and legal issues

Human rights institutions are placing increasing scrutiny on harmful practices and issues of discrimination against intersex people. These issues have been addressed by a rapidly increasing number of international institutions including, in 2015, the Council of Europe, the United Nations Office of the United Nations High Commissioner for Human Rights and the World Health Organization (WHO). In 2024, the United Nations Human Rights Council adopted its first resolution to protect the rights of intersex people.[122] These developments have been accompanied by International Intersex Forums and increased cooperation among civil society organizations. However, the implementation, codification, and enforcement of intersex human rights in national legal systems remains slow.
Physical integrity and bodily autonomy
Parts of this article (those related to map) need to be updated. (May 2021) |

Stigmatization and discrimination from birth may include infanticide, abandonment, and the stigmatization of families. The birth of an intersex child was often viewed as a curse or a sign of a witch mother, especially in parts of Africa.[25][26] Abandonments and infanticides have been reported in Uganda,[25] Kenya,[123] South Asia,[124] and China.[27]
Infants, children and adolescents also experience "normalising" interventions on intersex persons that are medically unnecessary and the pathologisation of variations in sex characteristics. In countries where the human rights of intersex people have been studied, medical interventions to modify the sex characteristics of intersex people have still taken place without the consent of the intersex person.[125][126] Interventions have been described by human rights defenders as a violation of many rights, including (but not limited to) bodily integrity, non-discrimination, privacy, and experimentation.[127] These interventions have frequently been performed with the consent of the intersex person's parents, when the person is legally too young to consent. Such interventions have been criticized by the WHO, other UN bodies such as the Office of the High Commissioner for Human Rights, and an increasing number of regional and national institutions due to their adverse consequences, including trauma, impact on sexual function and sensation, and violation of rights to physical and mental integrity.[citation needed] The UN organizations decided that infant intervention should not be allowed, in favor of waiting for the child to mature enough to be a part of the decision-making—this allows for a decision to be made with total consent.[128] In April 2015, Malta became the first country to outlaw surgical intervention without consent.[37][38] In the same year, the Council of Europe became the first institution to state that intersex people have the right not to undergo sex affirmation interventions.[65]
Anti-discrimination and equal treatment

People born with intersex bodies are seen as different. Intersex infants, children, adolescents and adults "are often stigmatized and subjected to multiple human rights violations", including discrimination in education, healthcare, employment, sport, and public services.[2] Researchers have documented significant disparities in mental, physical, and sexual health when comparing intersex individuals to the general population, including higher rates of bullying, stigmatization, harassment, violence, and suicidal intention, as well as substantial barriers in the workplace.[24]
Several countries have so far explicitly protected intersex people from discrimination, with landmarks including South Africa,[129] Australia,[130][131] and, most comprehensively, Malta.[132][133][134]
Remedies and claims for compensation
Claims for compensation and remedies for human rights abuses include the 2011 case of Christiane Völling in Germany.[36][135] A second case was adjudicated in Chile in 2012, involving a child and his parents.[136][137] A further successful case in Germany, taken by Michaela Raab, was reported in 2015.[138] In the United States, the Minor Child (M.C. v Aaronson) lawsuit was "a medical malpractice case related to the informed consent for a surgery performed on the Crawford's adopted child (known as M.C.) at [Medical University of South Carolina] in April 2006".[139] The case was one of the first lawsuit of its type to challenge "legal, ethical, and medical issues regarding genital-normalizing surgery" in minors, and was eventually settled out of court by the Medical University of South Carolina for $440,000 in 2017.[140]
Information and support
Access to information, medical records, peer and other counselling and support. With the rise of modern medical science in Western societies, a secrecy-based model was also adopted, in the belief that this was necessary to ensure normal physical and psychosocial development.[141][142][143]
Legal recognition
The Asia Pacific Forum of National Human Rights Institutions states that legal recognition is firstly "about intersex people who have been issued a male or a female birth certificate being able to enjoy the same legal rights as other men and women".[35] In some regions, obtaining any form of birth certification may be an issue. A Kenyan court case in 2014 established the right of an intersex boy, "Baby A", to a birth certificate.[144]
Like all individuals, some intersex individuals may be raised as a certain sex (male or female) but then identify with another later in life, while most do not.[145][5][146][147] Recognition of third sex or gender classifications occurs in several countries,[148][149][150][151] however, it is controversial when it becomes assumed or coercive, as is the case with some German infants.[152][153] Sociological research in Australia, a country with a third 'X' sex classification, shows that 19% of people born with atypical sex characteristics selected an "X" or "other" option, while 75% of survey respondents self-described as male or female (52% as women, 23% as men), and 6% as unsure.[6][46]
LGBT and LGBTI


Intersex conditions can be contrasted with transgender gender identities and the attached gender dysphoria a transgender person may feel, wherein their gender identity does not match their assigned sex.[154][155][156] However, some people are both intersex and transgender; although intersex people by definition have variable sex characteristics that do not align with either typically male or female, this may be considered separate to an individual's assigned gender, the way they are raised and perceived, and their internal gender identity.[157] A 2012 clinical review paper found that between 8.5% and 20% of people with intersex variations experienced gender dysphoria.[146] In an analysis of the use of preimplantation genetic diagnosis to eliminate intersex traits, Behrmann and Ravitsky state: "Parental choice against intersex may ... conceal biases against same-sex attractedness and gender nonconformity."[158]
The relationship of intersex people and communities to LGBTQ communities is complex,[159] but intersex people are often added to the LGBT acronym, resulting in the acronym LGBTI (or when also including asexual people, LGBTQIA+[160]). Emi Koyama describes how inclusion of intersex in LGBTI can fail to address intersex-specific human rights issues, including creating false impressions "that intersex people's rights are protected" by laws protecting LGBT people, and failing to acknowledge that many intersex people are not LGBT.[161] Organisation Intersex International Australia states that some intersex individuals are homosexual, and some are heterosexual, but "LGBTI activism has fought for the rights of people who fall outside of expected binary sex and gender norms."[162][163] Julius Kaggwa of SIPD Uganda has written that, while the gay community "offers us a place of relative safety, it is also oblivious to our specific needs".[164] Mauro Cabral has written that transgender people and organizations "need to stop approaching intersex issues as if they were trans issues", including use of intersex conditions and people as a means of explaining being transgender; "we can collaborate a lot with the intersex movement by making it clear how wrong that approach is."[165]
In society
Fiction, literature and media

An intersex character is the narrator in Jeffrey Eugenides' Pulitzer Prize-winning novel Middlesex.
The memoir, Born Both: An Intersex Life (Hachette Books, 2017), by intersex author and activist Hida Viloria, received strong praise from The New York Times Book Review, The Washington Post, Rolling Stone, People Magazine, and Psychology Today, was one of School Library Journal's 2017 Top Ten Adult Books for Teens, and was a 2018 Lambda Literary Award nominee.
Television works about intersex and films about intersex are scarce. The Spanish-language film XXY won the Critics' Week grand prize at the 2007 Cannes Film Festival and the ACID/CCAS Support Award.[166] Faking It is notable for providing both the first intersex main character in a television show,[167] and television's first intersex character played by an intersex actor.[168]
Civil society institutions
Intersex peer support and advocacy organizations have existed since at least 1985, with the establishment of the Androgen Insensitivity Syndrome Support Group Australia in 1985.[169] The Androgen Insensitivity Syndrome Support Group (UK) was established in 1988.[170] The Intersex Society of North America (ISNA) may have been one of the first intersex civil society organizations to have been open to people regardless of diagnosis; it was active from 1993 to 2008.[171]
Events
Intersex Awareness Day is an internationally observed civil awareness day designed to highlight the challenges faced by intersex people, occurring annually on 26 October. It marks the first public demonstration by intersex people, which took place in Boston on 26 October 1996, outside a venue where the American Academy of Pediatrics was holding its annual conference.[172]
Intersex Day of Remembrance, also known as Intersex Solidarity Day, is an internationally observed civil awareness day designed to highlight issues faced by intersex people, occurring annually on 8 November. It marks the birthday of Herculine Barbin, a French intersex person whose memoirs were later published by Michel Foucault in Herculine Barbin: Being the Recently Discovered Memoirs of a Nineteenth-century French Hermaphrodite.
Flags
-
Intersex flag
-
Autistic intersex flag (2022)
-
Transgender intersex flag (2017)
-
The Progress Pride flag with the intersex flag (2021)
The intersex flag was created in July 2013 by Morgan Carpenter of Intersex Human Rights Australia to create a flag "that is not derivative, but is yet firmly grounded in meaning". The circle is described as "unbroken and unornamented, symbolising wholeness and completeness, and our potentialities. We are still fighting for bodily autonomy and genital integrity, and this symbolises the right to be who and how we want to be."[173]
The intersex flag has been remixed and adapted in numerous ways. One way has been to replace the middle ring with the symbol of another group, to indicate the intersection of these groups. For example, the autistic intersex flag replaces the ring with an infinity symbol to represent autism.[174] Another technique is to inset another flag inside the ring: e.g. the pride flag for transgender intersex people puts the transgender flag in the centre. In 2021, Valentino Vecchietti of Intersex Equality Rights UK redesigned the Progress Pride Flag to incorporate the intersex flag.[175] This design added a yellow triangle with a purple circle in it to the chevron of the Progress Pride flag. It also changed the color of green to a lighter shade without adding new symbolism. Intersex Equality Rights UK posted the new flag on Instagram and Twitter.[176][177]
Religion
In Judaism, the Talmud contains extensive discussion concerning the status of two types of intersex people in Jewish law; namely, the androgynous, who exhibit both male and female external sexual organs, and the tumtum, who exhibit neither. In the 1970s and 1980s, the treatment of intersex babies started to be discussed in Orthodox Jewish medical halacha by prominent rabbinic leaders, such as Eliezer Waldenberg and Moshe Feinstein.[178]
Sport

Erik Schinegger, Foekje Dillema, Maria José Martínez-Patiño and Santhi Soundarajan were subject to adverse sex verification testing resulting in ineligibility to compete in organised competitive competition. Stanisława Walasiewicz, an athlete diagnosed posthumously with Turner syndrome was posthumously ruled ineligible to have competed.[179]
The South African middle-distance runner Caster Semenya won 3 World Championships gold medals and 2 Olympic gold medals in the women's 800 metres. When Semenya won gold at the 2009 World Championships, the International Association of Athletics Federations (IAAF) requested sex verification tests on the very same day. The results were not released, and Semenya was ruled eligible to compete.[180] In 2019, new IAAF rules came into force for athletes like Semenya with certain disorders of sex development (DSDs) requiring medication to suppress testosterone levels in order to participate in 400m, 800m, and 1500m women's events. Semenya objected to undergoing the treatment which is now mandatory. She has filed a series of legal cases to restore her ability to compete in these events without testosterone suppression, arguing that the World Athletics rules are discriminatory.[181]
Katrina Karkazis, Rebecca Jordan-Young, Georgiann Davis and Silvia Camporesi have claimed that IAAF policies on "hyperandrogenism" in female athletes are "significantly flawed", arguing that the policy does not protect against breaches of privacy, requires athletes to undergo unnecessary treatment in order to compete, and intensifies "gender policing", and recommended that athletes be able to compete in accordance with their legally-recognised gender.[182]
In April 2014, the BMJ reported that four elite women athletes with XY chromosomes and 5α-reductase 2 deficiency were subjected to sterilization and "partial clitoridectomies" in order to compete in sport. The authors noted that partial clitoridectomy was "not medically indicated" and "does not relate to real or perceived athletic 'advantage'".[29] Intersex advocates[who?] regarded this intervention as "a clearly coercive process".[183] In 2016, the United Nations Special Rapporteur on health, Dainius Pūras, criticized "current and historic" sex verification policies, describing how "a number of athletes have undergone gonadectomy (removal of reproductive organs) and partial clitoridectomy (a form of female genital mutilation) in the absence of symptoms or health issues warranting those procedures."[184]
Biology
The notion of intersex individuals can be understood in the context of sexual system biology that varies across different types of organisms. Most animal species (~95%, including humans) are gonochoric, in which individuals are of either a female or male sex.[185] Hermaphroditic species (some animals and most flowering plants[186]) are represented by individuals that can express both sexes simultaneously or sequentially during their lifetimes.[187] Intersex individuals in a number of gonochoric species, who express both female and male phenotypic characters to some degree,[188] are known to exist at very low prevalences.
Although "hermaphrodite" and "intersex" have been used synonymously in humans,[189][pages needed] a hermaphrodite is specifically an individual capable of producing female and male gametes.[190] While there are reports of individuals that seemed to have the potential to produce both types of gamete,[191] in more recent years the term hermaphrodite as applied to humans has fallen out of favor, since female and male reproductive functions have not been observed together in the same individual.[192]
Medical
Research in the late 20th century led to a growing medical consensus that diverse intersex bodies are normal, but relatively rare, forms of human biology.[5][193][194][195] Clinician and researcher Milton Diamond stresses the importance of care in the selection of language related to intersex people:
Foremost, we advocate use of the terms "typical", "usual", or "most frequent" where it is more common to use the term "normal". When possible avoid expressions such as maldeveloped or undeveloped, errors of development, defective genitals, abnormal, or mistakes of nature. Emphasize that all of these conditions are biologically understandable while they are statistically uncommon.[196]
Medical classifications
Sexual differentiation
The common pathway of sexual differentiation, where a productive human female has an XX chromosome pair, and a productive male has an XY pair, is relevant to the development of intersex conditions.
During fertilization, the sperm adds either an X (female) or a Y (male) chromosome to the X in the ovum. This determines the genetic sex of the embryo. During the first weeks of development, genetic male and female fetuses are "anatomically indistinguishable", with primitive gonads beginning to develop during approximately the sixth week of gestation. The gonads, in a bipotential state, may develop into either testes (the male gonads) or ovaries (the female gonads), depending on the consequent events.[197] Up until and including the seventh week, genetically female and genetically male fetuses appear identical.
At around eight weeks of gestation, the gonads of an XY embryo differentiate into functional testes, secreting testosterone. Ovarian differentiation, for XX embryos, does not occur until approximately week 12 of gestation. In typical female differentiation, the Müllerian duct system develops into the uterus, fallopian tubes, and inner third of the vagina. In males, the Müllerian duct-inhibiting hormone AMH causes this duct system to regress. Next, androgens cause the development of the Wolffian duct system, which develops into the vas deferens, seminal vesicles, and ejaculatory ducts.[197] By birth, the typical fetus has been completely sexed male or female, meaning that the genetic sex (XY-male or XX-female) corresponds with the phenotypical sex; that is to say, genetic sex corresponds with internal and external gonads, and external appearance of the genitals.
Signs
There are a variety of symptoms that can occur. Ambiguous genitalia is the most common sign. There can be micropenis, clitoromegaly, partial labial fusion, electrolyte abnormalities, delayed or absent puberty, unexpected changes at puberty, hypospadias, labial or inguinal (groin) masses (which may turn out to be testes) in girls and undescended testes (which may turn out to be ovaries) in boys.[198]
Ambiguous genitalia
Ambiguous genitalia may appear as a large clitoris or as a small penis.
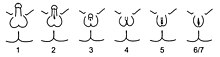
Because there is variation in all of the processes of the development of the sex organs, a child can be born with a sexual anatomy that is typically female or feminine in appearance with a larger-than-average clitoris (clitoral hypertrophy) or typically male or masculine in appearance with a smaller-than-average penis that is open along the underside. The appearance may be quite ambiguous, describable as female genitals (a vulva) with a very large clitoris and partially fused labia, or as male genitals with a very small penis, completely open along the midline ("hypospadic"), and empty scrotum. Fertility is variable.[citation needed]
Measurement systems for ambiguous genitalia
The orchidometer is a medical instrument to measure the volume of the testicles. It was developed by Swiss pediatric endocrinologist Andrea Prader. The Prader scale[199] and Quigley scale are visual rating systems that measure genital appearance. These measurement systems were satirized in the Phall-O-Meter, created by the (now defunct) Intersex Society of North America.[200][201][202]
Other signs
In order to help in classification, methods other than a genitalia inspection can be performed. For instance, a karyotype display of a tissue sample may determine which of the causes of intersex is prevalent in the case. Additionally, electrolyte tests, endoscopic exam, ultrasound and hormone stimulation tests can be done.[203]
Causes
Intersex can be divided into four categories which are: 46, XX intersex; 46, XY intersex; true gonadal intersex; and complex or undetermined intersex.[198]
46, XX intersex
This condition used to be called "female pseudohermaphroditism". Persons with this condition have female internal genitalia and karyotype (XX) and various degree of external genitalia virilization.[204] External genitalia is masculinized congenitally when female fetus is exposed to excess androgenic environment.[198] Hence, the chromosome of the person is of a female, the ovaries of a female, but external genitals that appear like a male. The labia fuse, and the clitoris enlarges to appear like a penis. The causes of this can be male hormones taken during pregnancy, congenital adrenal hyperplasia, male-hormone-producing tumors in the mother and aromatase deficiency.[198]
46, XY intersex
This condition used to be called "male pseudohermaphroditism". This is defined as incomplete masculinization of the external genitalia.[205] Thus, the person has male chromosomes, but the external genitals are incompletely formed, ambiguous, or clearly female.[198][206] This condition is also called 46, XY with undervirilization.[198] 46, XY intersex has many possible causes, which can be problems with the testes and testosterone formation.[198] Also, there can be problems with using testosterone. Some people lack the enzyme needed to convert testosterone to dihydrotestosterone, which is a cause of 5-alpha-reductase deficiency.[198] Androgen insensitivity syndrome is the most common cause of 46, XY intersex.[198]
True gonadal intersex
This condition used to be called "true hermaphroditism". This is defined as having asymmetrical gonads with ovarian and testicular differentiation on either sides separately or combined as ovotestis.[207] In most cases, the cause of this condition is unknown.
Complex or undetermined intersex
This is the condition of having any chromosome configurations rather than 46, XX or 46, XY intersex. This condition does not result in an imbalance between internal and external genitalia. However, there may be problems with sex hormone levels, overall sexual development, and altered numbers of sex chromosomes.[198]
Conditions
There are a variety of opinions on what conditions or traits are and are not intersex, dependent on the definition of intersex that is used. Current human rights based definitions stress a broad diversity of sex characteristics that differ from expectations for male or female bodies.[2] During 2015, the Council of Europe,[65] the European Union Agency for Fundamental Rights[208] and Inter-American Commission on Human Rights[209] have called for a review of medical classifications on the basis that they presently impede enjoyment of the right to health; the Council of Europe expressed concern that "the gap between the expectations of human rights organisations of intersex people and the development of medical classifications has possibly widened over the past decade."[65][208][209]
Medical interventions
Rationales

Medical interventions take place to address physical health concerns and psychosocial risks. Both types of rationale are the subject of debate, particularly as the consequences of surgical (and many hormonal) interventions are lifelong and irreversible. Questions regarding physical health include accurately assessing risk levels, necessity, and timing. Psychosocial rationales are particularly susceptible to questions of necessity as they reflect social and cultural concerns.[citation needed]
There remains no clinical consensus about an evidence base, surgical timing, necessity, type of surgical intervention, and degree of difference warranting intervention.[210][211][212] Such surgeries are the subject of significant contention due to consequences that include trauma, impact on sexual function and sensation, and violation of rights to physical and mental integrity.[citation needed] This includes community activism,[115] and multiple reports by international human rights[31][65][35][213] and health[143] institutions and national ethics bodies.[34][214]
In the cases where gonads may pose a cancer risk, as in some cases of androgen insensitivity syndrome,[215] concern has been expressed that treatment rationales and decision-making regarding cancer risk may encapsulate decisions around a desire for surgical "normalization".[33]
Types
- Feminizing and masculinizing surgeries: Surgical procedures depend on the diagnosis, and there is often a concern as to whether surgery should be performed at all. Typically, surgery is performed shortly after birth. Defenders of the practice argue that individuals must be clearly identified as male or female for them to function socially and develop "normally". Psychosocial reasons are often stated.[20] This is criticised by many human rights institutions, and authors. Unlike other aesthetic surgical procedures performed on infants, such as corrective surgery for a cleft lip, genital surgery may lead to negative consequences for sexual functioning in later life, or feelings of freakishness and unacceptability.[216]
- Hormone treatment: There is widespread evidence of prenatal testing and hormone treatment to prevent or eliminate intersex traits,[217] associated also with the problematization of sexual orientation and gender non-conformity.[217][218]
- Psychosocial support: All stakeholders support psychosocial support. A joint international statement by participants at the Third International Intersex Forum in 2013 sought, among other demands: "Recognition that medicalization and stigmatisation of intersex people result in significant trauma and mental health concerns. In view of ensuring the bodily integrity and well-being of intersex people, autonomous non-pathologising psycho-social and peer support be available to intersex people throughout their life (as self-required), as well as to parents and/or care providers."[This quote needs a citation]
- Genetic selection and terminations: The ethics of preimplantation genetic diagnosis to select against intersex traits was the subject of 11 papers in the October 2013 issue of the American Journal of Bioethics.[219] There is widespread evidence of pregnancy terminations arising from prenatal testing, as well as prenatal hormone treatment to prevent intersex traits. Behrmann and Ravitsky find social concepts of sex, gender and sexual orientation to be "intertwined on many levels. Parental choice against intersex may thus conceal biases against same-sex attractedness and gender nonconformity."[158]
- Medical display. Photographs of intersex children's genitalia are circulated in medical communities for documentary purposes, and individuals with intersex traits may be subjected to repeated genital examinations and display to medical teams. Problems associated with experiences of medical photography of intersex children have been discussed[220] along with their ethics, control and usage.[221][222] "The experience of being photographed has exemplified for many people with intersex conditions the powerlessness and humiliation felt during medical investigations and interventions."[221]
- Gender dysphoria: The DSM-5 included a change from using gender identity disorder to gender dysphoria. This revised code now specifically includes intersex people who do not identify with their sex assigned at birth and experience clinically significant distress or impairment, using the language of disorders of sex development.[223]
See also
- Intersex Awareness Day
- Intersex people and military service
- Sexual differentiation in humans
- Intersex healthcare
- Gynandromorphism
- Endosex
- True hermaphroditism
- Androgyny
- 46,XX/46,XY
Notes
- ^ Sex within this context refers to the gonads, many individuals with intersex variations have an assigned sex and gender identity that differs from gonadal sex. Individuals with complete androgen insensitivity syndrome are phenotypically female, are assigned female at birth, and usually have a female gender identity but have testis. The definition of biological sex within intersex topics are often arbitrary.[75][76]
References
- ^ "Intersex people". OHCHR. Archived from the original on 8 July 2023. Retrieved 11 June 2023.
- ^ a b c d e "Free & Equal Campaign Fact Sheet: Intersex" (PDF). United Nations Office of the High Commissioner for Human Rights. 2015. Archived (PDF) from the original on 4 March 2016. Retrieved 28 March 2016.
- ^ a b Selma Feldman Witchel (2018). "Disorders of Sex Development". Best Practice & Research. Clinical Obstetrics & Gynaecology. 48: 90–102. doi:10.1016/j.bpobgyn.2017.11.005. PMC 5866176. PMID 29503125.
The estimated frequency of genital ambiguity is reported to be in the range of 1:2000–1:4500
- ^ a b c d e f Sax L (August 2002). "How common is intersex? a response to Anne Fausto-Sterling". Journal of Sex Research. 39 (3): 174–178. doi:10.1080/00224490209552139. PMID 12476264. S2CID 33795209. Alt URL Archived 28 February 2021 at the Wayback Machine
- ^ a b c Alice Domurat Dreger (2001). Hermaphrodites and the Medical Invention of Sex. US: Harvard University Press. ISBN 978-0-674-00189-3.
- ^ a b c "New publication "Intersex: Stories and Statistics from Australia"". Organisation Intersex International Australia. 3 February 2016. Archived from the original on 29 August 2016. Retrieved 18 August 2016.
- ^ "Intersex population figures". Intersex Human Rights Australia. 28 September 2013. Archived from the original on 17 July 2018. Retrieved 1 January 2021.
- ^ a b Fausto-Sterling A (2000). Sexing the Body: Gender Politics and the Construction of Sexuality. Basic Books. p. 53. ISBN 978-0-465-07714-4.
- ^ a b Blackless M, Charuvastra A, Derryck A, Fausto-Sterling A, Lauzanne K, Lee E (March 2000). "How sexually dimorphic are we? Review and synthesis". American Journal of Human Biology. 12 (2): 151–166. doi:10.1002/(SICI)1520-6300(200003/04)12:2<151::AID-AJHB1>3.0.CO;2-F. PMID 11534012. S2CID 453278.
- ^ "How Common is Intersex? An Explanation of the Stats". Intersex Campaign for Equality. 1 April 2015. Archived from the original on 11 February 2021. Retrieved 1 January 2021.
- ^ Ripley A (27 February 2005). "Who Says A Woman Can't Be Einstein?". Time. Time. Archived from the original on 1 August 2008. Retrieved 29 December 2008.
- ^ Mason H.J. (1978). "Favorinus' Disorder: Reifenstein's Syndrome in Antiquity?". Janus. 66 (1–2–3): 1–13. PMID 11610651.
- ^ Nguyễn Khắc Thuần (1998), Việt sử giai thoại (History of Vietnam's tales), vol. 8, Vietnam Education Publishing House, p. 55
- ^ a b Zucker KJ, Bradley SJ, Sullivan CB (March 1992). "Gender Identity Disorder in Children". Annual Review of Sex Research. 3 (1): 73–120. doi:10.1080/10532528.1992.10559876.
- ^ Dreger AD, Chase C, Sousa A, Gruppuso PA, Frader J (18 August 2005). "Changing the Nomenclature/Taxonomy for Intersex: A Scientific and Clinical Rationale". Journal of Pediatric Endocrinology and Metabolism. 18 (8): 729–33. doi:10.1515/JPEM.2005.18.8.729. PMID 16200837. S2CID 39459050.
- ^ Kilman R (14 April 2016). Encyclopedia of Evolutionary Biology. Elsevier Science. ISBN 978-0-12-800426-5.
- ^ Avise J, Nicholson T (15 March 2011). Hermaphroditism. Columbia University Press. pp. 1–7. ISBN 978-0-231-52715-6.
- ^ Preves SE (2003). Intersex and identity: the contested self. New Brunswick, N.J.: Rutgers University Press. ISBN 0-8135-3228-0. OCLC 50334056.
- ^ Harper C (2007). Intersex (English ed.). Oxford: Berg. ISBN 978-1-84788-339-1. OCLC 608598019.
- ^ a b Houk CP, Hughes IA, Ahmed SF, Lee PA, Writing Committee for the International Intersex Consensus Conference Participants (August 2006). "Summary of Consensus Statement on Intersex Disorders and Their Management". Pediatrics. 118 (2): 753–757. doi:10.1542/peds.2006-0737. PMID 16882833. S2CID 46508895.
- ^ Davis G (11 September 2015). Contesting Intersex: The Dubious Diagnosis. New York University Press. pp. 87–89. ISBN 978-1-4798-8704-0.
- ^ Holmes M (September 2011). "The Intersex Enchiridion: Naming and Knowledge". Somatechnics. 1 (2): 388–411. doi:10.3366/soma.2011.0026.
- ^ Beh H, Diamond M (27 July 2006). "Variations of Sex Development Instead of Disorders of Sex Development". Archives of Disease in Childhood. 91 (7): 554–563. doi:10.1136/adc.2006.098319. PMC 2082839. PMID 16624884.
- ^ a b c Muñoz E, Saavedra M, Sansone D (6 June 2024), The Lives of Intersex People: Socio-Economic and Health Disparities in Mexico, doi:10.18235/0013001, hdl:10419/300963.
- ^ a b c Civil Society Coalition on Human Rights and Constitutional Law, Human Rights Awareness and Promotion Forum, Rainbow Health Foundation, Sexual Minorities Uganda, Support Initiative for Persons with Congenital Disorders (2014). "Uganda Report of Violations based on Sex Determination, Gender Identity, and Sexual Orientation". Archived from the original on 3 May 2015. Retrieved 15 May 2017.
- ^ a b Grady H, Soy A (4 May 2017). "The midwife who saved intersex babies". BBC World Service, Kenya. Archived from the original on 15 May 2017.
- ^ a b Beyond the Boundary – Knowing and Concerns Intersex (October 2015). "Intersex report from Hong Kong China, and for the UN Committee Against Torture: the Convention against Torture and Other Cruel Inhuman or Degrading Treatment or Punishment". Archived from the original on 26 March 2017.
- ^ Submission 88 to the Australian Senate inquiry on the involuntary or coerced sterilisation of people with disabilities in Australia Archived 23 September 2015 at the Wayback Machine, Australasian Paediatric Endocrine Group (APEG), 27 June 2013
- ^ a b Jordan-Young RM, Sonksen PH, Karkazis K (April 2014). "Sex, health, and athletes". BMJ. 348 (apr28 9): –2926–g2926. doi:10.1136/bmj.g2926. PMID 24776640. S2CID 2198650.
- ^ Macur J (6 October 2014). "Fighting for the Body She Was Born With". The New York Times. Archived from the original on 12 January 2015. Retrieved 9 February 2015.
- ^ a b Report of the UN Special Rapporteur on Torture Archived 29 April 2019 at the Wayback Machine, Office of the UN High Commissioner for Human Rights, February 2013.
- ^ Eliminating forced, coercive and otherwise involuntary sterilization, An interagency statement Archived 11 July 2015 at the Wayback Machine, World Health Organization, May 2014.
- ^ a b Involuntary or coerced sterilisation of intersex people in Australia. Canberra: Senate of Australia Community Affairs References Committee. 2013. ISBN 978-1-74229-917-4. Archived from the original on 23 September 2015.
- ^ a b c On the management of differences of sex development. Ethical issues relating to "intersexuality". Opinion No. 20/2012 (PDF). Berne: Swiss National Advisory Commission on Biomedical Ethics NEK-CNE. November 2012. Archived from the original (PDF) on 23 April 2015. Retrieved 24 July 2018.
- ^ a b c Asia Pacific Forum of National Human Rights Institutions (June 2016). Promoting and Protecting Human Rights in relation to Sexual Orientation, Gender Identity and Sex Characteristics. ISBN 978-0-9942513-7-4. Archived from the original on 15 January 2017.
- ^ a b c International Commission of Jurists. "In re Völling, Regional Court Cologne, Germany (6 February 2008)". Archived from the original on 5 January 2016. Retrieved 27 December 2015.
- ^ a b c "Surgery and Sterilization Scrapped in Malta's Benchmark LGBTI Law". The New York Times. Reuters. 1 April 2015. Archived from the original on 4 April 2015. Retrieved 29 August 2020.
- ^ a b "Malta passes law outlawing forced surgical intervention on intersex minors". Star Observer. 2 April 2015. Archived from the original on 14 August 2015.
- ^ Dreger AD, Herndon AM (1 January 2009). "Progress and Politics in the Intersex Rights Movement: Feminist Theory in Action". GLQ: A Journal of Lesbian and Gay Studies. 15 (2): 199–224. doi:10.1215/10642684-2008-134. S2CID 145754009.
In our experience some clinicians have played a sort of moving target game whereby their definition of intersex changes from venue to venue, or moment to moment. We end up spending a remarkable amount of time just trying to agree on which diagnoses (and thus which people) count in the conversation we're trying to have. This does not usually seem to be a purposeful attempt to stall or derail conversation (although that does sometimes result); rather it seems to stem from a lack of systematic consideration of what the term might mean. For example, some want to call intersex only those born with visibly ambiguous genitalia, or only those who have had a particularly unusual mix of prenatal sex hormones.
- ^ Jordan-Young RM, Sönksen PH, Karkazis K (April 2014). "Sex, health, and athletes". BMJ. 348: g2926. doi:10.1136/bmj.g2926. PMID 24776640. S2CID 2198650. Archived from the original on 11 September 2014. Retrieved 19 July 2021.
- ^ Goldberg AE (10 May 2016). The SAGE Encyclopedia of LGBTQ Studies. SAGE Publications. p. 614. ISBN 978-1-4833-7129-0.
- ^ Welcome to OII Australia – we promote human rights and bodily autonomy for intersex people, and provide information, education and peer support Archived 31 October 2014 at the Wayback Machine, Intersex Human Rights Australia, 4 April 2004
- ^ Answers to Your Questions About Individuals With Intersex Conditions Archived 31 October 2014 at the Wayback Machine, American Psychological Association, 2006.
- ^ Advocates for Informed Choice Archived 11 August 2011 at the Wayback Machine, Advocates for Informed Choice, undated, retrieved 19 September 2014
- ^ interACT (May 2016). "interACT Statement on Intersex Terminology". Interact Advocates for Intersex Youth. Archived from the original on 8 June 2016. Retrieved 30 May 2016.
- ^ a b Jones T, Hart B, Carpenter M, Ansara G, Leonard W, Lucke J (2016). Intersex: Stories and Statistics from Australia (PDF). Cambridge, UK: Open Book Publishers. ISBN 978-1-78374-208-0. Archived from the original (PDF) on 14 September 2016. Retrieved 2 February 2016.
- ^ "InterConnect Support - Support Embrace Educate Network". Archived from the original on 19 April 2021. Retrieved 9 April 2021.
- ^ Johnson EK, Rosoklija I, Finlayson C, Chen D, Yerkes EB, Madonna MB, Holl JL, Baratz AB, Davis G, Cheng EY (December 2017). "Attitudes towards 'disorders of sex development' nomenclature among affected individuals". Journal of Pediatric Urology. 13 (6): 608.e1–608.e8. doi:10.1016/j.jpurol.2017.03.035. PMID 28545802.
- ^ Newswise (11 May 2017). "Term "Disorders of Sex Development" May Have Negative Impact". Newswise. Archived from the original on 15 May 2017. Retrieved 11 May 2017.
- ^ a b D'Oro A, Rosoklija I, Jacobson DL, Finlayson C, Chen D, Tu DD, Austin PF, Karaviti LP, Gunn SK, Nahata L, Kapa HM, Kokorowski PJ, Kim MS, Messina AC, Kolon TF, Yerkes EB, Cheng EY, Johnson EK (October 2020). "Patient and Caregiver Attitudes toward Disorders of Sex Development Nomenclature". Journal of Urology. 204 (4): 835–842. doi:10.1097/JU.0000000000001076. PMID 32302259.
- ^ Bennecke E, Köhler B, Röhle R, Thyen U, Gehrmann K, Lee P, Nordenström A, Cohen-Kettenis P, Bouvattier C, Wiesemann C (4 May 2021). "Disorders or Differences of Sex Development? Views of Affected Individuals on DSD Terminology". The Journal of Sex Research. 58 (4): 522–531. doi:10.1080/00224499.2019.1703130. PMID 31985272.
- ^ Decretum Gratiani, C. 4, q. 2 et 3, c. 3
- ^ "Decretum Gratiani (Kirchenrechtssammlung)". Bayerische StaatsBibliothek (Bavarian State Library). 5 February 2009. Archived from the original on 20 December 2016.
- ^ E Coke, The First Part of the Institutes of the Laws of England, Institutes 8.a. (1st Am. Ed. 1812).
- ^ a b Greenberg J (1999). "Defining Male and Female: Intersexuality and the Collision Between Law and Biology". Arizona Law Review. 41: 277–278. SSRN 896307.
- ^ Reis E (2009). Bodies in Doubt: An American History of Intersex. Baltimore: Johns Hopkins University Press. pp. 55–81. ISBN 978-0-8018-9155-7.
- ^ Molina B Dayal, MD, MPH, Assistant Professor, Fertility and IVF Center, Division of Reproductive Endocrinology and Infertility, Medical Faculty Associates, George Washington University distinguishes what 'true hermaphroditism' encompasses in their study of Ovotestis. Found here: "Ovotesticular Disorder of Sexual Development". Archived from the original on 31 December 2007. Retrieved 2 January 2008.
- ^ W. S. Alexander M.D., O. D. Beresford M.D., M.R.C.P. (1953) wrote extensively about 'female pseudohermaphrodite' origins in utera, in his paper "Masculinization of Ovarian Origin, published An International Journal of Obstetrics and Gynaecology Volume 60 Issue 2 pp. 252–258, April 1953.
- ^ Am J Psychiatry 164:1499–1505, October 2007: Noted Mayo Clinic researchers J.M. Bostwick, MD, and Kari A Martin MD in A Man's Brain in an Ambiguous Body: A Case of Mistaken Gender wrote of the distinctions in male pseudohermaphrodite condition.
- ^ Langman, Jan, Thomas Sadler (2006). Langman's medical embryology. Hagerstown, MD: Lippincott Williams & Wilkins. p. 252. ISBN 978-0-7817-9485-5.
- ^ a b Cawadias, A. P. (1943) Hermaphoditus the Human Intersex, London, Heinemann Medical Books Ltd.
- ^ a b Alice D. Dreger, April M. Herndon. "Progress and Politics in the intersex rights movement, Feminist theory in action" (PDF). Archived (PDF) from the original on 21 June 2023. Retrieved 25 April 2023.
- ^ "Is a person who is intersex a hermaphrodite? | Intersex Society of North America". Isna.org. Archived from the original on 1 July 2013. Retrieved 5 July 2013.
- ^ "How common is intersex? | Intersex Society of North America". Isna.org. Archived from the original on 22 August 2009. Retrieved 21 August 2009.
- ^ a b c d e Human rights and intersex people, Issue Paper (Report). Council of Europe Commissioner for Human Rights. April 2015. Archived from the original on 6 January 2016. Retrieved 29 August 2020.
- ^ "On the number of intersex people". Organisation Intersex International Australia. 28 September 2013. Archived from the original on 4 July 2015. Retrieved 4 July 2015.
- ^ Chaleyer R (10 March 2015). "Intersex: the 'I' in 'LGBTI'". Special Broadcasting Service. Archived from the original on 5 July 2015. Retrieved 4 July 2015.
- ^ a b c Merke DP, Auchus RJ (September 2020). "Congenital Adrenal Hyperplasia Due to 21-Hydroxylase Deficiency". The New England Journal of Medicine. 383 (13): 1248–1261. doi:10.1056/NEJMra1909786. PMID 32966723. S2CID 221884108.
- ^ a b Hull CL, Fausto-Sterling A (January 2003). "Letter to the Editor". American Journal of Human Biology. 15 (1): 112–116. doi:10.1002/ajhb.10122. PMID 12552585.
- ^ "Intersex population figures". 28 September 2013. Archived from the original on 17 July 2018. Retrieved 17 April 2021.
- ^ "Variation in Sex Characteristics". www.healthit.gov. Archived from the original on 14 May 2023. Retrieved 28 July 2023.
- ^ Clune-Taylor C (14 May 2010). "From Intersex to DSD: the Disciplining of Sex Development". PhaenEx. 5 (2): 152–178. doi:10.22329/p.v5i2.3087. Archived from the original on 14 May 2023. Retrieved 27 July 2023 – via ojs.uwindsor.ca.
- ^ "What is intersex?" (PDF). 2015. Archived (PDF) from the original on 27 July 2023. Retrieved 27 July 2023.
- ^ "Key Issues Facing People With Intersex Traits". InterACT. 26 October 2021. Archived from the original on 30 June 2023. Retrieved 27 July 2023.
- ^ "Androgen insensitivity syndrome: MedlinePlus Genetics". medlineplus.gov. Archived from the original on 21 October 2023. Retrieved 15 October 2023.
- ^ Zucker KJ (February 2002). "Intersexuality and Gender Identity Differentiation". Journal of Pediatric and Adolescent Gynecology. 15 (1): 3–13. doi:10.1016/s1083-3188(01)00133-4. PMID 11888804.
- ^ Best J (14 September 2013). Stat-spotting: a field guide to identifying dubious data (1st, Updated and expand ed.). Berkeley: University of California Press. pp. 12–13. ISBN 978-0-520-27998-8.
- ^ Witchel SF, Azziz R (2010). "Nonclassic Congenital Adrenal Hyperplasia". International Journal of Pediatric Endocrinology. 2010: 625105. doi:10.1155/2010/625105. PMC 2910408. PMID 20671993.
- ^ a b Speiser PW, Arlt W, Auchus RJ, Baskin LS, Conway GS, Merke DP, Meyer-Bahlburg HF, Miller WL, Murad MH, Oberfield SE, White PC (November 2018). "Congenital Adrenal Hyperplasia Due to Steroid 21-Hydroxylase Deficiency: An Endocrine Society Clinical Practice Guideline". The Journal of Clinical Endocrinology and Metabolism. 103 (11): 4043–4088. doi:10.1210/jc.2018-01865. PMC 6456929. PMID 30272171.
- ^ Springer A, van den Heijkant M, Baumann S (June 2016). "Worldwide prevalence of hypospadias". Journal of Pediatric Urology. 12 (3): 152.e1–152.e7. doi:10.1016/j.jpurol.2015.12.002. PMID 26810252.
- ^ "Klinefelter syndrome Genetic and Rare Diseases Information Center (GARD) – an NCATS Program". rarediseases.info.nih.gov. Archived from the original on 29 August 2020. Retrieved 19 December 2019.
- ^ Wigby K, D'Epagnier C, Howell S, Reicks A, Wilson R, Cordeiro L, Tartaglia N (November 2016). "Expanding the phenotype of Triple X syndrome: A comparison of prenatal versus postnatal diagnosis". American Journal of Medical Genetics Part A. 170 (11): 2870–2881. doi:10.1002/ajmg.a.37688. PMC 6501572. PMID 27644018.
- ^ Reference GH. "Turner syndrome". Genetics Home Reference. Archived from the original on 29 August 2020. Retrieved 19 December 2019.
- ^ Morcel K, Camborieux L, Guerrier D (2007). "Mayer-Rokitansky-Küster-Hauser (MRKH) syndrome". Orphanet Journal of Rare Diseases. 2 (1): 13. doi:10.1186/1750-1172-2-13. PMC 1832178. PMID 17359527.
- ^ "Urology Care Foundation – What is Vaginal Agenesis?". www.urologyhealth.org. Archived from the original on 4 January 2019. Retrieved 21 January 2018.
- ^ Mohammadpour Lashkari F, Sadighi Gilani MA, Ghaheri A, Zamanian MR, Borjian Boroujeni P, Mohseni Meybodi A, Sabbaghian M (June 2018). "Clinical aspects of 49 infertile males with 45,X/46,XY mosaicism karyotype: A case series". Andrologia. 50 (5): e13009. doi:10.1111/and.13009. PMID 29527714. S2CID 3833188.
Chromosomal analysis plays an important role in the DSD determination. 45,X/46,XY mosaicism is a rare karyotype, and its prevalence is about 1.5 in 10,000 newborns.
- ^ Stochholm K, Juul S, Gravholt CH (2010). "Diagnosis and mortality in 47,XYY persons: a registry study". Orphanet Journal of Rare Diseases. 5 (1): 15. doi:10.1186/1750-1172-5-15. PMC 2889887. PMID 20509956.
- ^ Tartaglia N, Ayari N, Howell S, D'Epagnier C, Zeitler P (June 2011). "48,XXYY, 48,XXXY and 49,XXXXY syndromes: not just variants of Klinefelter syndrome". Acta Paediatrica. 100 (6): 851–860. doi:10.1111/j.1651-2227.2011.02235.x. PMC 3314712. PMID 21342258.
- ^ Alekri A, Busehail M, Rhayel N, Almosawi SM (2023). "XXXYY variant of Klinefelter syndrome: A case report". Int J Health Sci (Qassim). 17 (3): 39–45. PMC 10155245. PMID 37151746.
- ^ Verhoeven WM, Egger JI, Mergler S, Meijer TA, Pfundt R, Willemsen MH (2022). "A Patient with Moderate Intellectual Disability and 49, XXXYY Karyotype". Int J Gen Med. 15: 2799–2806. doi:10.2147/IJGM.S348844. PMC 8921824. PMID 35300132.
- ^ Kusz K, Kotecki M, Wojda A, Szarras-Czapnik M, Latos-Bielenska A, Warenik-Szymankiewicz A, Ruszczynska-Wolska A, Jaruzelska J (1 June 1999). "Incomplete masculinisation of XX subjects carrying the SRY gene on an inactive X chromosome". Journal of Medical Genetics. 36 (6): 452–456. doi:10.1136/jmg.36.6.452. PMC 1734388. PMID 10874632. Archived from the original on 30 March 2019. Retrieved 19 July 2023 – via jmg.bmj.com.
- ^ "46,XX testicular disorder of sex development". Genetics Home Reference. Archived from the original on 17 May 2019. Retrieved 24 December 2019.
- ^ "Ovotesticular Disorder of Sex Development". NORD (National Organization for Rare Disorders). Archived from the original on 29 August 2020. Retrieved 21 December 2019.
- ^ Yen and Jaffe's reproductive endocrinology: physiology, pathophysiology, and clinical management (7th ed.). Elsevier/Saunders. 13 September 2013. ISBN 978-1-4557-2758-2.
phenotypically, pure XY GD individuals are unambiguously phenotypic females (previously known as Swyer syndrome) but usually internally possess hypoplastic müllerian structures.
- ^ Reference GH. "Swyer syndrome". Genetics Home Reference. Archived from the original on 16 December 2019. Retrieved 21 December 2019.
- ^ Sinnecker GH, Hiort O, Nitsche EM, Holterhus PM, Kruse K (29 June 1996). "Functional assessment and clinical classification of androgen sensitivity in patients with mutations of the androgen receptor gene". European Journal of Pediatrics. 156 (1): 7–14. doi:10.1007/s004310050542. PMID 9007482. S2CID 34427651.
In the genetic male, mutations of the androgen receptor (AR) gene cause phenotypes ranging from female to subfertile male.
- ^ Boehmer AL, Brüggenwirth H, van Assendelft C, Otten BJ, Verleun-Mooijman MC, Niermeijer MF, Brunner HG, Rouwé CW, Waelkens JJ, Oostdijk W, Kleijer WJ, van der Kwast TH, de Vroede MA, Drop SL (September 2001). "Genotype Phenotype in Families with Androgen Insensitivity Syndrome". The Journal of Clinical Endocrinology & Metabolism. 86 (9): 4151–4160. doi:10.1210/jcem.86.9.7825. PMID 11549642.
- ^ Anne Fausto-Sterling (2000). Sexing the Body: Gender Politics and the Construction of Sexuality. New York: Basic Books.
- ^ Mosley M (20 September 2015). "The extraordinary case of the Guevedoces". BBC News. Archived from the original on 23 September 2015. Retrieved 23 September 2015.
- ^ Imperato-McGinley J, Guerrero L, Gautier T, Peterson RE (December 1974). "Steroid 5alpha-reductase deficiency in man: an inherited form of male pseudohermaphroditism". Science. 186 (4170): 1213–1215. Bibcode:1974Sci...186.1213I. doi:10.1126/science.186.4170.1213. PMID 4432067. S2CID 36427689.
- ^ Diodorus Siculus (1935). Library of History (Book IV). Loeb Classical Library Volumes 303 and 340. C H Oldfather (trans.). Cambridge, MA: Harvard University Press. Archived from the original on 27 September 2008.
- ^ Markantes G, Deligeoroglou E, Armeni A, Vasileiou V, Damoulari C, Mandrapilia A, Kosmopoulou F, Keramisanou V, Georgakopoulou D, Creatsas G, Georgopoulos N (10 July 2015). "Callo: The first known case of ambiguous genitalia to be surgically repaired in the history of Medicine, described by Diodorus Siculus". Hormones. 14 (3): 459–461. doi:10.14310/horm.2002.1608. PMID 26188239. Archived from the original on 25 June 2021. Retrieved 25 June 2021.
- ^ Swami P (2004). Encyclopaedia of the Śaivism (1st ed.). New Delhi: Sarup & Sons. ISBN 978-81-7625-427-4. OCLC 54930404.
- ^ Shankar G (March–April 2015). "The Many Genders of Old India". The Gay & Lesbian Review Worldwide. 22: 24–26 – via ProQuest.
- ^ a b DeVun L (June 2018). "Heavenly hermaphrodites: sexual difference at the beginning and end of time". Postmedieval. 9 (2): 132–146. doi:10.1057/s41280-018-0080-8. S2CID 165449144.
- ^ Pliny, Natural History 7.34: gignuntur et utriusque sexus quos hermaphroditos vocamus, olim androgynos vocatos; Veronique Dasen, "Multiple Births in Graeco-Roman Antiquity", Oxford Journal of Archaeology 16.1 (1997), p. 61.
- ^ Lynn E. Roller, "The Ideology of the Eunuch Priest", Gender & History 9.3 (1997), p. 558.
- ^ Decretum Gratiani, C. 4, q. 2 et 3, c. 3
- ^ "Decretum Gratiani (Kirchenrechtssammlung)". Bayerische StaatsBibliothek (Bavarian State Library). 5 February 2009. Archived from the original on 20 December 2016.
- ^ Raming I, Macy G, Bernard J C (2004). A History of Women and Ordination. Scarecrow Press. p. 113.
- ^ E Coke, The First Part of the Institutes of the Laws of England, Institutes 8.a. (1st Am. Ed. 1812) (16th European ed. 1812).
- ^ "India's Third Gender Rises Again". Sapiens. Wenner-Gren Foundation for Anthropological Research. 26 September 2019. Archived from the original on 29 August 2020. Retrieved 26 April 2020.
- ^ "Hijra: India's third gender claims its place in law". The Guardian. 16 April 2014. Archived from the original on 15 April 2017. Retrieved 26 April 2020.
- ^ Holmes M (July 2004). "Locating Third Sexes" (PDF). Transformations Journal (8). Archived (PDF) from the original on 16 April 2017. Retrieved 28 December 2014.
- ^ a b Cabral M, Carpenter M, eds. (2014). Intersex Issues in the International Classification of Diseases: a revision (PDF). Intersex Day. Archived (PDF) from the original on 11 August 2016.
- ^ Goldschmidt R (1917). "Intersexuality and the endocrine aspect of sex". Endocrinology. 1 (4): 433–456. doi:10.1210/endo-1-4-433. Archived from the original on 29 August 2020. Retrieved 4 July 2019.
- ^ Coran AG, Polley TZ (July 1991). "Surgical management of ambiguous genitalia in the infant and child". Journal of Pediatric Surgery. 26 (7): 812–820. CiteSeerX 10.1.1.628.4867. doi:10.1016/0022-3468(91)90146-K. PMID 1895191.
- ^ Hughes IA, Houk C, Ahmed SF, Lee PA, LWPES1/ESPE2 Consensus Group (June 2005). "Consensus statement on management of intersex disorders". Archives of Disease in Childhood. 91 (7): 554–563. doi:10.1136/adc.2006.098319. PMC 2082839. PMID 16624884.
- ^ Alice Domurat Dreger (May 1998). ""Ambiguous Sex"—or Ambivalent Medicine?". The Hastings Center Report. 28 (3): 24–35. doi:10.2307/3528648. JSTOR 3528648. PMID 9669179.
- ^ Dreger A (3 April 2015). "Malta Bans Surgery on Intersex Children". The Stranger SLOG. Archived from the original on 18 July 2015.
- ^ Public statement by the third international intersex forum. Malta. 2 December 2013. Archived from the original on 24 November 2016.
- ^ https://www.reuters.com/world/un-rights-body-adopts-first-resolution-protect-rights-intersex-people-2024-04-04/
- ^ Odero J (23 December 2015). "Intersex in Kenya: Held captive, beaten, hacked. Dead". 76 CRIMES. Archived from the original on 25 April 2016. Retrieved 1 October 2016.
- ^ Warne GL, Raza J (September 2008). "Disorders of sex development (DSDs), their presentation and management in different cultures". Reviews in Endocrine and Metabolic Disorders. 9 (3): 227–236. CiteSeerX 10.1.1.469.9016. doi:10.1007/s11154-008-9084-2. PMID 18633712. S2CID 8897416.
- ^ Ghattas DC, Heinrich-Böll-Stiftung (2013). Human Rights between the Sexes A preliminary study on the life situations of inter*individuals (PDF). Berlin: Heinrich-Böll-Stiftung. ISBN 978-3-86928-107-0. Archived (PDF) from the original on 23 September 2015.
- ^ ""Intersex", Radio Netherlands Archives, April 21, 2004". 21 April 2004. Archived from the original on 29 August 2020. Retrieved 16 April 2019.
- ^ Carpenter M (December 2018). "Intersex Variations, Human Rights, and the International Classification of Diseases". Health and Human Rights. 20 (2): 205–214. PMC 6293350. PMID 30568414.
- ^ Greenberg JA (June 2017). "Legal, ethical, and human rights considerations for physicians treating children with atypical or ambiguous genitalia". Seminars in Perinatology. 41 (4): 252–255. doi:10.1053/j.semperi.2017.03.012. PMID 28478089.
- ^ Government Gazette Archived 9 June 2011 at the Wayback Machine, Republic of South Africa, Vol. 487, Cape Town, 11 January 2006.
- ^ Sex Discrimination Amendment (Sexual Orientation, Gender Identity and Intersex Status) Act 2013, No. 98, 2013 Archived 6 October 2014 at the Wayback Machine, ComLaw, C2013A00098, 2013.
- ^ On the historic passing of the Sex Discrimination Amendment (Sexual Orientation, Gender Identity and Intersex Status) Act 2013 Archived 6 October 2014 at the Wayback Machine, Organisation Intersex International Australia, 25 June 2013.
- ^ Malta (April 2015). "Gender Identity, Gender Expression and Sex Characteristics Act: Final version". Archived from the original on 5 July 2015. Retrieved 4 July 2015.
- ^ OII Europe (1 April 2015). "OII-Europe applauds Malta's Gender Identity, Gender Expression and Sex Characteristics Act. This is a landmark case for intersex rights within European law reform". Archived from the original on 22 May 2015. Retrieved 3 July 2015.
- ^ Transgender Europe (1 April 2015). Malta Adopts Ground-breaking Trans and Intersex Law – TGEU Press Release. Archived from the original on 3 November 2016. Retrieved 4 July 2015.
- ^ Zwischengeschlecht (12 August 2009). "Christiane Völling: Hermaphrodite wins damage claim over removal of reproductive organs". Archived from the original on 5 July 2015. Retrieved 20 July 2015.
- ^ "Condenan al H. de Talca por error al determinar sexo de bebé". diario.latercera.com (in Spanish). Archived from the original on 15 February 2017. Retrieved 15 February 2017.
- ^ García G (20 June 2013). "Identidad forzada". www.paula.cl (in Spanish). Archived from the original on 15 February 2017.
- ^ Zwischengeschlecht (17 December 2015). "Nuremberg Hermaphrodite Lawsuit: Michaela "Micha" Raab Wins Damages and Compensation for Intersex Genital Mutilations!". Archived from the original on 11 May 2016. Retrieved 21 December 2015.
- ^ "M.C. V. AARONSON". Archived from the original on 29 August 2020. Retrieved 1 August 2019.
- ^ Dutta A, Pintens W (12 September 2018). "Private International Law Aspects of Intersex". In Jens M. Scherpe, Anatol Dutta, Tobias Helms (eds.). The Legal Status of Intersex Persons. Intersentia. pp. 415–426. doi:10.1017/9781780687704.026. ISBN 978-1-78068-770-4. S2CID 158683664.
- ^ Holmes M. "Is Growing up in Silence Better Than Growing up Different?". Intersex Society of North America. Archived from the original on 5 March 2016.
- ^ Intersex Society of North America. "What's wrong with the way intersex has traditionally been treated?". Archived from the original on 26 June 2014.
- ^ a b World Health Organization (2015). Sexual health, human rights and the law. Geneva: World Health Organization. ISBN 978-92-4-156498-4.
- ^ "Kenya takes step toward recognizing intersex people in landmark ruling". Reuters. 5 December 2014. Archived from the original on 24 September 2015.
- ^ Money J, Ehrhardt, Anke A. (1972). Man & Woman Boy & Girl. Differentiation and dimorphism of gender identity from conception to maturity. US: The Johns Hopkins University Press. ISBN 978-0-8018-1405-1.
- ^ a b Furtado P. S., et al. (2012). "Gender dysphoria associated with disorders of sex development". Nat. Rev. Urol. 9 (11): 620–627. doi:10.1038/nrurol.2012.182. PMID 23045263. S2CID 22294512.
- ^ Marañón G (1929). Los estados intersexuales en la especie humana. Madrid: Morata.
- ^ "Australian Government Guidelines on the Recognition of Sex and Gender, 30 May 2013". Archived from the original on 1 July 2015. Retrieved 6 October 2014.
- ^ Holme I (2008). "Hearing People's Own Stories". Science as Culture. 17 (3): 341–344. doi:10.1080/09505430802280784. S2CID 143528047.
- ^ "New Zealand Passports - Information about Changing Sex / Gender Identity". Archived from the original on 23 September 2014. Retrieved 6 October 2014.
- ^ Third sex option on birth certificates Archived 10 October 2014 at the Wayback Machine, Deutsche Welle, 1 November 2013.
- ^ ""Intersex: Third Gender in Germany" (Spiegel, Huff Post, Guardian, …): Silly Season Fantasies vs. Reality of Genital Mutilations". Stop IGM. 1 November 2013. Archived from the original on 11 March 2021. Retrieved 15 March 2021.
- ^ Sham package for Intersex: Leaving sex entry open is not an option Archived 29 August 2014 at the Wayback Machine, OII Europe, 15 February 2013
- ^ Rupprecht M (6 September 2013). "Children's right to physical integrity". Parliamentary Assembly of the Council of Europe. Archived from the original on 26 December 2013. Retrieved 1 January 2021.
- ^ "Trans? Intersex? Explained!". interACT. Archived from the original on 18 October 2014. Retrieved 1 January 2021.
{{cite web}}: CS1 maint: unfit URL (link) - ^ "Basic differences between intersex and trans". Organisation Intersex International Australia. 3 June 2011. Archived from the original on 4 September 2014. Retrieved 10 July 2013.
- ^ "The marks on our bodies". Intersex Day. 25 October 2015. Archived from the original on 5 April 2016. Retrieved 1 January 2021.
- ^ a b Behrmann J, Ravitsky V (October 2013). "Queer Liberation, Not Elimination: Why Selecting Against Intersex is Not "Straight" Forward". The American Journal of Bioethics. 13 (10): 39–41. doi:10.1080/15265161.2013.828131. PMID 24024805. S2CID 27065247.
- ^ Dreger A (4 May 2015). "Reasons to Add and Reasons NOT to Add "I" (Intersex) to LGBT in Healthcare" (PDF). Association of American Medical Colleges. Archived (PDF) from the original on 9 June 2016. Retrieved 18 May 2016.
- ^ Gold M (21 June 2018). "The ABCs of L.G.B.T.Q.I.A.+". The New York Times. Archived from the original on 18 April 2021. Retrieved 27 July 2023.
- ^ Koyama E. "Adding the "I": Does Intersex Belong in the LGBT Movement?". Intersex Initiative. Archived from the original on 17 May 2016. Retrieved 18 May 2016.
- ^ "Intersex for allies". 21 November 2012. Archived from the original on 7 June 2016. Retrieved 18 May 2016.
- ^ Busby C (1 June 2014). "OII Releases New Resource on Intersex Issues". Intersex Human Rights Australia. Archived from the original on 6 June 2014. Retrieved 1 January 2021.
- ^ Kaggwa J (19 September 2016). "I'm an intersex Ugandan – life has never felt more dangerous". The Guardian. Archived from the original on 6 October 2016. Retrieved 3 October 2016.
- ^ "IAD2016: A Message from Mauro Cabral". Global Action for Trans Equality. 26 October 2016. Archived from the original on 3 November 2016. Retrieved 1 January 2021.
- ^ Leffler R (26 May 2007). "Critics Week grand prize to 'XXY'". The Hollywood Reporter. Archived from the original on 30 September 2007. Retrieved 12 February 2017.
- ^ Peitzman L (23 September 2014). "Meet television's groundbreaking intersex character". BuzzFeed News. Archived from the original on 29 May 2016. Retrieved 1 January 2021.
- ^ Avery D (1 April 2016). ""Faking It" Breaks New Ground With First Intersex Actor To Play Intersex Character On TV". NewNowNext. Logo TV. Archived from the original on 5 April 2016. Retrieved 1 January 2021.
- ^ Androgen Insensitivity Syndrome Support Group Australia, Briffa A (22 January 2003). "Discrimination against People affected by Intersex Conditions: Submission to NSW Government" (PDF). Archived (PDF) from the original on 11 March 2016. Retrieved 16 May 2016.
- ^ "Androgen Insensitivity Syndrome Support Group (AISSG)". Archived from the original on 21 January 2016. Retrieved 16 May 2016.
- ^ "Dear ISNA Friends and Supporters". 2008. Archived from the original on 19 May 2016. Retrieved 16 May 2016.
- ^ "When Max Beck and Morgan Holmes went to Boston". Intersex Day. 17 October 2015. Archived from the original on 20 October 2015. Retrieved 1 January 2021.
- ^ An intersex flag Archived 9 July 2018 at the Wayback Machine, Intersex Human Rights Australia, 5 July 2013
- ^ intersex q (5 April 2022). "I made a few more intersex + disabled icons/flags for anybody who wants them". Retrieved 27 June 2024.
- ^ Parsons V (7 June 2021). "Progress Pride flag gets 2021 redesign to better represent intersex people". PinkNews. Retrieved 10 June 2021.
- ^ "The Progress Pride Flag Is Getting an Intersex-Inclusive Makeover". them.us. 8 June 2021. Archived from the original on 10 July 2021. Retrieved 3 August 2021.
- ^ Intersex Equality Rights UK [@intersex_equality_rights_uk] (5 June 2021). "Slide 1. Happy Pride 2021! For our Intersex Inclusion Campaign we'd like to share with you our new intersex inclusive Pride Progress…" – via Instagram.
- ^ Schifrin D (19 September 2014). "Stanford prof: Talmudic rabbis were into analyzing sexuality". J. Archived from the original on 10 October 2014. Retrieved 1 January 2021.
- ^ Klaudia Snochowska-Gonzales. "Walasiewicz była kobietą (Walasiewicz Was a Woman)". Gazeta Wyborcza (in Polish). 190 (14 August 2004): 8. Archived from the original on 14 May 2020. Retrieved 31 May 2006.
- ^ Cooky C, Shari L. Dworkin (February 2013). "Policing the Boundaries of Sex: A Critical Examination of Gender Verification and the Caster Semenya Controversy". Journal of Sex Research. 50 (2): 103–111. doi:10.1080/00224499.2012.725488. PMID 23320629. S2CID 1353785.
- ^ "Caster Semenya Opens Up About Discrimination Battle Against World Athletics". 2 November 2023. Retrieved 5 August 2024.
- ^ Karkazis K, Jordan-Young R, Davis G, Camporesi S (July 2012). "Out of Bounds? A Critique of the New Policies on Hyperandrogenism in Elite Female Athletes". The American Journal of Bioethics. 12 (7): 3–16. doi:10.1080/15265161.2012.680533. PMC 5152729. PMID 22694023.
- ^ "UN Human Rights Council: resolution, statement and side event, "The time has come"". Organisation Intersex International Australia. 11 September 2014. Archived from the original on 30 September 2014. Retrieved 28 September 2014.
- ^ Pūras D, Special Rapporteur on the right of everyone to the enjoyment of the highest attainable standard of physical and mental health (4 April 2016). Sport and healthy lifestyles and the right to health. Report A/HRC/32/33 (Report). United Nations. Archived from the original on 15 December 2016.
- ^ Muyle A, Marais G (2016). "Mating Systems in Plants, Genome Evolution and". Encyclopedia of Evolutionary Biology. pp. 480–492. doi:10.1016/B978-0-12-800049-6.00320-6. ISBN 978-0-12-800426-5.
- ^ Christopher DA, Mitchell RJ, Trapnell DW, Smallwood PA, Semski WR, Karron JD (August 2019). "Hermaphroditism promotes mate diversity in flowering plants". American Journal of Botany. 106 (8): 1131–1136. doi:10.1002/ajb2.1336. PMC 6852098. PMID 31403705.
- ^ Auld J, Jarne P (2016). "Sex and Recombination in Snails". Encyclopedia of Evolutionary Biology. pp. 49–60. doi:10.1016/B978-0-12-800049-6.00149-9. ISBN 978-0-12-800426-5.
- ^ Fusco G, Minelli A (10 October 2019). The Biology of Reproduction. Cambridge University Press. p. 116. ISBN 978-1-108-49985-9.
- ^ Dreger AD (1998). Hermaphrodites and the medical invention of sex. Cambridge, Mass.: Harvard University Press. ISBN 978-0-674-00189-3.
- ^ Ross L, Blackmon H (2016). "Sex Determination". Encyclopedia of Evolutionary Biology. pp. 81–88. doi:10.1016/B978-0-12-800049-6.00146-3. ISBN 978-0-12-800426-5.
- ^ Krob G, Braun A, Kuhnle U (January 1994). "True hermaphroditism: Geographical distribution, clinical findings, chromosomes and gonadal histology". European Journal of Pediatrics. 153 (1): 2–10. doi:10.1007/BF02000779. PMID 8313919. S2CID 1931001.
- ^ Rosenfield KA (2018). "Hermaphrodite". In Vonk J, Shackelford T (eds.). Hermaphrodite. Encyclopedia of Animal Cognition and Behavior. Cham: Springer International. pp. 1–2. doi:10.1007/978-3-319-47829-6_329-1. ISBN 978-3-319-47829-6.
The term "hermaphrodite" has sometimes been used to refer to humans whose biological sex is ambiguous. This usage has fallen out of favor and in any case was technically incorrect. The essential characteristic of hermaphrodites is the ability to reproduce as both male and female. No such case has been identified in any human
- ^ Zderic S (2002). Pediatric gender assignment: a critical reappraisal; [proceedings from a conference ... in Dallas in the spring of 1999 which was entitled "pediatric gender assignment – a critical reappraisal"]. New York, NY [u.a.]: Kluwer Acad. / Plenum Publ. ISBN 978-0-306-46759-2.
- ^ Frader J, Alderson P, Asch A, Aspinall C, Davis D, Dreger A, Edwards J, Feder EK, Frank A, Hedley LA, Kittay E, Marsh J, Miller PS, Mouradian W, Nelson H, Parens E (May 2004). "Health care professionals and intersex conditions". Arch. Pediatr. Adolesc. Med. 158 (5): 426–8. CiteSeerX 10.1.1.572.1572. doi:10.1001/archpedi.158.5.426. PMID 15123472.
- ^ Wiesemann C, Ude-Koeller S, Sinnecker GH, Thyen U (June 2010). "Ethical principles and recommendations for the medical management of differences of sex development (DSD)/intersex in children and adolescents". European Journal of Pediatrics. 169 (6): 671–679. doi:10.1007/s00431-009-1086-x. PMC 2859219. PMID 19841941.
- ^ Diamond M, H. Keith Sigmundson (1997). "Management of intersexuality: Guidelines for dealing with individuals with ambiguous genitalia". Archives of Pediatrics and Adolescent Medicine. June. Archived from the original on 8 February 2007. Retrieved 8 April 2007.
- ^ a b Kolodny RC, Masters WH, Johnson VE (1979). Textbook of Sexual Medicine (1st ed.). Boston: Little, Brown and Company. ISBN 978-0-316-50154-5.
- ^ a b c d e f g h i j "Intersex: MedlinePlus Medical Encyclopedia". medlineplus.gov. Archived from the original on 29 August 2020. Retrieved 25 March 2019.
- ^ Diamond M, Linda W (2004). "Androgen insensitivity syndrome and Klinefelter's syndrome: sex and gender considerations". Child Adolesc Psychiatric Clin N Am. No. 13. pp. 623–640. Archived from the original on 1 July 2013.
- ^ Forrester J (2009). "The psychology of the sexual–reproductive–gender system" (PDF). Wellcome History (42): 13–15. Archived (PDF) from the original on 29 August 2020. Retrieved 26 June 2018.
- ^ Marchal J (3 July 2010). "Bodies Bound for Circumcision and Baptism: An Intersex Critique and the Interpretation of Galatians". Theology & Sexuality. 16 (2): 163–182. doi:10.1558/tse.v16i2.163. S2CID 143514837.
- ^ López DJ (25 February 2015). "La intersexualidad en el discurso médico-jurídico". Eunomía (in Spanish) (8): 54–70.
- ^ Baylis F, Borgerson K, Hoffmaster B, Sherwin S (6 October 2011). Health Care Ethics in Canada. Cengage Learning. ISBN 978-0-17-650464-9. Archived from the original on 29 August 2020. Retrieved 28 May 2020.
- ^ Kamijo H, Narita O (November 1997). "[Female pseudohermaphroditism]". Nihon Rinsho. Japanese Journal of Clinical Medicine. 55 (11): 2925–2929. PMID 9396289.
- ^ Migeon CJ (July 1980). "Male pseudohermaphroditism". Annales d'Endocrinologie. 41 (4): 311–343. PMID 7011168.
- ^ Fernández-Cancio M, Camats N, Flück CE, Zalewski A, Dick B, Frey BM, Monné R, Torán N, Audí L (29 April 2018). "Mechanism of the Dual Activities of Human CYP17A1 and Binding to Anti-Prostate Cancer Drug Abiraterone Revealed by a Novel V366M Mutation Causing 17,20 Lyase Deficiency". Pharmaceuticals. 11 (2): 37. doi:10.3390/ph11020037. PMC 6027421. PMID 29710837.
- ^ Iqbal MZ, Jam MR, Saleem M, Ahmad M (30 July 2011). "True Hermaphrodite: A Case Report". APSP Journal of Case Reports. 2 (2): 16. PMC 3418019. PMID 22953283.
- ^ a b European Union Agency for Fundamental Rights (April 2015). "The fundamental rights situation of intersex people" (PDF). Archived from the original (PDF) on 5 March 2016. Retrieved 3 January 2016.
- ^ a b Comisión Interamericana de Derechos Humanos (12 November 2015). "Violencia contra Personas Lesbianas, Gays, Bisexuales, Trans e Intersex en América" (PDF) (in Spanish). Comisión Interamericana de Derechos Humanos. Archived (PDF) from the original on 7 January 2016.
- ^ Lee PA, Nordenström A, Houk CP, Ahmed SF, Auchus R, Baratz A, Baratz Dalke K, Liao LM, Lin-Su K, Looijenga LH, Mazur T, Meyer-Bahlburg HF, Mouriquand P, Quigley CA, Sandberg DE, Vilain E, Witchel S, and the Global DSD Update Consortium (28 January 2016). "Global Disorders of Sex Development Update since 2006: Perceptions, Approach and Care". Hormone Research in Paediatrics. 85 (3): 158–180. doi:10.1159/000442975. PMID 26820577.
- ^ Mouriquand PD, Gorduza DB, Gay CL, Meyer-Bahlburg HF, Baker L, Baskin LS, Bouvattier C, Braga LH, Caldamone AC, Duranteau L, El Ghoneimi A, Hensle TW, Hoebeke P, Kaefer M, Kalfa N, Kolon TF, Manzoni G, Mure PY, Nordenskjöld A, Pippi Salle JL, Poppas DP, Ransley PG, Rink RC, Rodrigo R, Sann L, Schober J, Sibai H, Wisniewski A, Wolffenbuttel KP, Lee P (2016). "Surgery in disorders of sex development (DSD) with a gender issue: If (why), when, and how?". Journal of Pediatric Urology. 12 (3): 139–149. doi:10.1016/j.jpurol.2016.04.001. PMID 27132944.
- ^ Creighton SM, Michala L, Mushtaq I, Yaron M (2 January 2014). "Childhood surgery for ambiguous genitalia: glimpses of practice changes or more of the same?" (PDF). Psychology and Sexuality. 5 (1): 34–43. doi:10.1080/19419899.2013.831214. S2CID 89605693. Archived (PDF) from the original on 19 July 2018. Retrieved 13 January 2019.
- ^ Comisión Interamericana de Derechos Humanos (12 November 2015). "Violencia contra Personas Lesbianas, Gays, Bisexuales, Trans e Intersex en América" (PDF). Comisión Interamericana de Derechos Humanos. Archived (PDF) from the original on 7 January 2016.
- ^ German Ethics Council (February 2012). Intersexuality, Opinion. ISBN 978-3-941957-50-3. Archived from the original on 21 April 2017. Retrieved 25 January 2020.
- ^ Cools M, Koen van Aerde, Anne-Marie Kersemaekers, Marjan Boter, Stenvert L. S Drop, Katja P. Wolffenbuttel, Ewout W. Steyerberg, J. Wolter Oosterhuis, Leendert H. J. Looijenga (September 2005). "Morphological and Immunohistochemical Differences between Gonadal Maturation Delay and Early Germ Cell Neoplasia in Patients with Undervirilization Syndromes". J. Clin. Endocrinol. Metab. 90 (9): 5295–5303. doi:10.1210/jc.2005-0139. hdl:1854/LU-848324. PMID 15998778.
- ^ Intersex Society of North America (24 May 2006). What evidence is there that you can grow up psychologically healthy with intersex genitals (without "normalizing" surgeries)? Archived 8 December 2006 at the Wayback Machine. Retrieved 25 November 2006.
- ^ a b Bioethics Forum blog – Preventing Homosexuality (and Uppity Women) in the Womb? Archived 2 April 2016 at the Wayback Machine, Alice Dreger, Ellen K. Feder, Anne Tamar-Mattis (2010), at Hastings Center Bioethics Blog, retrieved 18 May 2012.
- ^ Meyer-Bahlburg H (1990). "Will prenatal hormone treatment prevent homosexuality?". Journal of Child and Adolescent Psychopharmacology. 1 (4): 279–283. doi:10.1089/cap.1990.1.279.
- ^ "American Journal of Bioethics, 13:10, 51–53. Retrieved 11 September 2013". October 2013. Archived from the original on 11 October 2014. Retrieved 6 October 2014.
- ^ Preves S (2003). Intersex and Identity, the Contested Self. Rutgers. ISBN 0-8135-3229-9. p. 72.
- ^ a b Creighton S, Alderson J, Brown S, Minto C (2002). "Medical photography: ethics, consent and the intersex patient". BJU International. 89 (1): 67–71. doi:10.1046/j.1464-410X.2002.02558.x. PMID 11849163. S2CID 26513690. p. 70.
- ^ Dreger AD (2000). "Jarring Bodies: Thoughts on the Display of Unusual Anatomies". Perspectives in Biology and Medicine. 43 (2): 161–172. doi:10.1353/pbm.2000.0002. PMID 10804583. S2CID 34463546.
- ^ Kraus C (May 2015). "Classifying Intersex in DSM-5: Critical Reflections on Gender Dysphoria". Archives of Sexual Behavior. 44 (5): 1147–1163. doi:10.1007/s10508-015-0550-0. PMID 25944182. S2CID 24390697.
Bibliography
- Asia Pacific Forum of National Human Rights Institutions (June 2016). Promoting and Protecting Human Rights in relation to Sexual Orientation, Gender Identity and Sex Characteristics. ISBN 978-0-9942513-7-4. Archived from the original on 15 January 2017. Retrieved 29 August 2016.
- Blackless M, Charuvastra A, Derryck A, Fausto-Sterling A, Lauzanne K, Lee E (2000). "How sexually dimorphic are we? Review and synthesis". Am J Hum Biol. 12 (2): 151–166. doi:10.1002/(SICI)1520-6300(200003/04)12:2<151::AID-AJHB1>3.0.CO;2-F. PMID 11534012. S2CID 453278.
- Council of Europe, Commissioner for Human Rights (April 2015). "Human rights and intersex people, Issue Paper".
- Davis G (2015). Contesting Intersex, The Dubious Diagnosis. New York: NYU Press. ISBN 978-1-4798-3786-1.
- Elders MJ, Satcher D, Carmona R (June 2017). "Re-Thinking Genital Surgeries on Intersex Infants" (PDF). Palm Center.
- Fausto-Sterling A (2000). Sexing the Body: Gender Politics and the Construction of Sexuality. Basic Books. ISBN 978-0-465-07714-4.
- Ghattas DC, Heinrich-Böll-Stiftung (2013). Human Rights between the Sexes: A preliminary study on the life situations of inter*individuals. Berlin: Heinrich-Böll-Stiftung. ISBN 978-3-86928-107-0.
- Holmes M, ed. (2009). Critical intersex. Queer interventions. Burlington, VT: Ashgate Publishing. ISBN 978-0-7546-7311-8.
- Hughes IA, Houk C, Ahmed SF, Lee PA, LWPES1/ESPE2 Consensus Group (June 2005). "Consensus statement on management of intersex disorders". Archives of Disease in Childhood. 91 (7): 554–563. doi:10.1136/adc.2006.098319. PMC 2082839. PMID 16624884.
- Marcus de María Arana, de María Arana M (2005). A Human Rights Investigation Into The Medical "Normalization" Of Intersex People. Human Rights Commission of the City and County of San Francisco.
- Human Rights Watch, interACT (July 2017). I Want to Be Like Nature Made Me. Human Rights Watch. ISBN 978-1-62313-502-7.
- Jones T, Hart B, Carpenter M, Ansara G, Leonard W, Lucke J (2016). Intersex: Stories and Statistics from Australia (PDF). Cambridge, UK: Open Book Publishers. ISBN 978-1-78374-208-0. Archived from the original (PDF) on 27 May 2018. Retrieved 2 February 2016.
- Jones T (2018). "Intersex Studies: A Systematic Review of International Health Literature". SAGE Open. 2018 (1): 1–22. doi:10.1177/2158244017745577.
- Karkazis K (2008). Fixing Sex: Intersex, Medical Authority, and Lived Experience. Duke University Press. ISBN 978-0-8223-4318-9.
- Lee PA, Nordenström A, Houk CP, Ahmed SF, Auchus R, Baratz A, Baratz Dalke K, Liao LM, Lin-Su K, Looijenga LH, Mazur T, Meyer-Bahlburg HF, Mouriquand P, Quigley CA, Sandberg DE, Vilain E, Witchel S, and the Global DSD Update Consortium (28 January 2016). "Global Disorders of Sex Development Update since 2006: Perceptions, Approach and Care". Hormone Research in Paediatrics. 85 (3): 158–180. doi:10.1159/000442975. PMID 26820577.
- Organisation Intersex International Australia, Carpenter M (April 2014). "Submission on the Review of Part B of the Ethical Guidelines for the Use of Assisted Reproductive Technology in Clinical Practice and Research, 2007". Sydney. Archived from the original on 6 October 2014. Retrieved 6 May 2014.
- Regmi E (2016). "Stories of Intersex People from Nepal" (PDF). Archived from the original (PDF) on 3 May 2016.
- Tamar-Mattis A (2014). "Medical Treatment of People with Intersex Conditions as Torture and Cruel, Inhuman, or Degrading Treatment or Punishment". Torture in Healthcare Settings: Reflections on the Special Rapporteur on Torture's 2013 Thematic Report (PDF). Washington, DC: Washington College of Law Center for Human Rights & Humanitarian Law. pp. 91–104. Archived from the original (PDF) on 27 March 2014.
- United Nations Office of the High Commissioner for Human Rights (2015). "Free & Equal Campaign Fact Sheet: Intersex" (PDF).
- UN Committee against Torture, UN Committee on the Rights of the Child, UN Committee on the Rights of People with Disabilities, UN Subcommittee on Prevention of Torture and other Cruel, Inhuman or Degrading Treatment or Punishment, Juan Méndez, Dainius Pūras, Dubravka Šimonoviæ, Marta Santos Pais, African Commission on Human and Peoples' Rights, Council of Europe Commissioner for Human Rights, Inter-American Commission on Human Rights (24 October 2016). "Intersex Awareness Day – Wednesday 26 October. End violence and harmful medical practices on intersex children and adults, UN and regional experts urge". Office of the High Commissioner for Human Rights.
- World Health Organization, OHCHR, UN Women, UNAIDS, UNDP, UNFPA, UNICEF (2014). Eliminating forced, coercive and otherwise involuntary sterilization, An interagency statement (PDF). ISBN 978-92-4-150732-5.
- Zwischengeschlecht (March 2014). "IGM – Historical Overview. Hermaphrodites in the 'Developed World': From Legal Self-Determination to IGM, Supplement 1" (PDF). NGO Report to the 2nd, 3rd and 4th Periodic Report of Switzerland on the Convention on the Rights of the Child (CRC) (2 ed.). pp. 49–62.
External links
 Media related to Intersex at Wikimedia Commons
Media related to Intersex at Wikimedia Commons
| External videos | |
|---|---|