Joseph Lister: Difference between revisions
Mikenorton (talk | contribs) →First reception of Antisepsis: add some missing apostrophes and fix one mispelling |
Scope creep (talk | contribs) cde |
||
| Line 605: | Line 605: | ||
===Monuments and legacy=== |
===Monuments and legacy=== |
||
In 1903, the British Institute of |
In 1903, the British Institute of Preventitive Medicine was renamed [[Lister Institute of Preventitive Medicine]] in honour of Lister.<ref name=listinst>{{cite web | title = Our Heritage | publisher = The Lister Institute | url = http://www.lister-institute.org.uk/about-us/our-heritage/ | access-date = 24 November 2015 | url-status = dead | archive-url = https://web.archive.org/web/20151125042654/http://www.lister-institute.org.uk/about-us/our-heritage/ | archive-date = 25 November 2015 | df = dmy-all }}</ref> The building, along with another adjacent building, forms what is now the [[Lister Hospital (Chelsea)|Lister Hospital in Chelsea]], which opened in 1985. The building at [[Glasgow Royal Infirmary]] which houses the [[cytopathology]], [[microbiology]], and [[pathology]] departments was named in Lister's honour to recognise his work at the hospital.<ref>{{cite web |title=NHSGGC : Glasgow Royal Campus – New Lister Building|url=https://www.nhsggc.org.uk/patients-and-visitors/main-hospital-sites/glasgow-royal-campus/new-lister-building/#|access-date=20 August 2021|website=www.nhsggc.org.uk}}</ref> The [[Lister Hospital, Stevenage|Lister Hospital]] in [[Stevenage]], [[Hertfordshire]] is named after him.{{sfn|Pitt|Aubin|2012}} |
||
Lister's name is one of 23 people featured on the [[frieze]] of the [[London School of Hygiene & Tropical Medicine]]<ref name=lhshtm>{{cite web|url=http://www.lshtm.ac.uk/library/archives/history/frieze/lister.html|title=Behind the Frieze – Baron Lister of Lyme Regis (1827–1912)|publisher=London School of Hygiene and Tropical Medicine|access-date=22 November 2016|url-status=dead|archive-url=https://web.archive.org/web/20161122224155/http://www.lshtm.ac.uk/library/archives/history/frieze/lister.html|archive-date=22 November 2016}}</ref> – although the committee which chose the names to include on the frieze did not provide documentation about why certain names were chosen and others were not.<ref>{{cite web|url=https://www.lshtm.ac.uk/aboutus/introducing/history/behind-frieze|title=Behind the Frieze|publisher=London School of Hygiene and Tropical Medicine|access-date=6 November 2022|archive-url=https://web.archive.org/web/20170202001531/http://www.lshtm.ac.uk/library/archives/history/frieze/|archive-date=2 February 2017}}</ref> |
Lister's name is one of 23 people featured on the [[frieze]] of the [[London School of Hygiene & Tropical Medicine]]<ref name=lhshtm>{{cite web|url=http://www.lshtm.ac.uk/library/archives/history/frieze/lister.html|title=Behind the Frieze – Baron Lister of Lyme Regis (1827–1912)|publisher=London School of Hygiene and Tropical Medicine|access-date=22 November 2016|url-status=dead|archive-url=https://web.archive.org/web/20161122224155/http://www.lshtm.ac.uk/library/archives/history/frieze/lister.html|archive-date=22 November 2016}}</ref> – although the committee which chose the names to include on the frieze did not provide documentation about why certain names were chosen and others were not.<ref>{{cite web|url=https://www.lshtm.ac.uk/aboutus/introducing/history/behind-frieze|title=Behind the Frieze|publisher=London School of Hygiene and Tropical Medicine|access-date=6 November 2022|archive-url=https://web.archive.org/web/20170202001531/http://www.lshtm.ac.uk/library/archives/history/frieze/|archive-date=2 February 2017}}</ref> |
||
Revision as of 23:50, 15 January 2024
The Lord Lister | |
|---|---|
 Lister in 1902 | |
| 37th President of the Royal Society | |
| In office 1895–1900 | |
| Preceded by | The Lord Kelvin |
| Succeeded by | Sir William Huggins |
| Personal details | |
| Born | 5 April 1827 Upton House, West Ham, England |
| Died | 10 February 1912 (aged 84) Walmer, Kent, England |
| Resting place | Hampstead Cemetery, London |
| Spouse | |
| Parents |
|
| Signature | |
| Education | University College London |
| Known for | Surgical sterile techniques |
| Awards |
|
| Scientific career | |
| Fields | Medicine |
| Institutions | |
Joseph Lister, 1st Baron Lister, OM, PC, FRS, FRCSE, FRCPGlas, FRCS (5 April 1827 – 10 February 1912[1]) was a British surgeon, medical scientist, experimental pathologist and a pioneer of antiseptic surgery[2] and preventive healthcare.[1] Joseph Lister revolutionised the craft of surgery in the same manner that John Hunter revolutionised the science of surgery.[3]
From a technical viewpoint, Lister was not an exceptional surgeon,[2] but his research into bacteriology and infection in wounds raised his operative technique to a new plane where his observations, deductions and practices revolutionised surgery throughout the world.[4]
Lister's contributions were four-fold. Firstly, as a surgeon at the Glasgow Royal Infirmary, he introduced carbolic acid (modern-day phenol) as a steriliser for surgical instruments, patients' skins, sutures, surgeons' hands, and wards, promoting the principle of antiseptics. Secondly, he researched the role of inflammation and tissue perfusion in the healing of wounds. Thirdly, he advanced diagnostic science by analyzing specimens using microscopes. Fourthly, he devised strategies to increase the chances of survival after surgery. His most important contribution, however, was recognising that putrefaction in wounds is caused by germs, in connection to Louis Pasteur's then-novel germ theory of fermentation.[a][6]
Lister's work led to a reduction in post-operative infections and made surgery safer for patients, leading to him being distinguished as the "father of modern surgery".[7]
Early life
Lister was born to a prosperous, educated Quaker family in the village of Upton, then near but now in London,[8] England. He was the fourth child and second son of four sons and three daughters[9] born to gentleman scientist and wine merchant Joseph Jackson Lister and school assistant Isabella Lister née Harris.[10][11] On 14 July 1818, the couple were married in a ceremony in Ackworth, West Yorkshire.[12]
Lister's paternal great-great-grandfather, Thomas Lister, was the last of several generations of farmers who lived in Bingley in West Yorkshire.[13] Lister joined the Society of Friends as a young man and passed his beliefs on to his son, Joseph Lister.[13] He moved to London in 1720 to open a tobacconist [13] in Aldersgate Street in the City of London.[14] His son, John Lister, was born there. Lister's grandfather was apprenticed to a watchmaker, Isaac Rogers,[15] in 1752 and followed that trade on his own account in Bell Alley, Lombard Street from 1759 to 1766. He then took over his father's tobacco business,[13] but gave it up in 1769 in favour of working at his father-in-law Stephen Jackson's business as a wine-merchant at No 28 Old Wine and Brandy Values on Lothbury Street, opposite Tokenhouse Yard.[16]
His father was a pioneer in the design of achromatic object lenses for use in compound microscopes[8] He spent 30 years perfecting the microscope, and in the process, discovered the Law of Aplanatic Foci,[17] building a microscope where the image point of one lens coincided with the focal point of another.[8] Up until that point, the best higher magnification lenses produced an excessive secondary aberration known as a coma, which interfered with normal use.[8] It was considered a major advance that elevated histology into an independent science.[18] By 1832, Lister's work had built a reputation sufficient to enable his being elected to the Royal Society.[19][20] His mother, Isabella, was the youngest daughter of master mariner Anthony Harris.[21] Isabella worked at the Ackworth School, a Quaker school for the poor, assisting her widowed mother who was the superintendent of the school.[21]
The eldest daughter of the couple was Mary Lister. On 21 August 1851, she married the barrister Rickman Godlee[22] of Lincoln's Inn and the Middle Temple, who belonged to the Friends meeting house in Plaistow.[23] The couple had six children. Their second child was Rickman Godlee, a neurosurgeon, who became Professor of Clinical Surgery at the University College Hospital[22] and surgeon to Queen Victoria. He became Lister's biographer in 1917.[22] The eldest son of Joseph and Isabella Lister was John Lister, who died of a painful brain tumour.[24] With John's death, Joseph became the heir of the family.[24] The couple's second daughter was Isabella Sophia Lister, who married the Irish Quaker Thomas Pim[25] in 1848. Lister's other brother was William Henry Lister, who died after a long illness.[9] The youngest son of the couple was Arthur Lister, a wine merchant, botanist and lifelong Quaker, who studied Mycetozoa. He worked alongside his daughter Gulielma Lister to produce the standard monograph on Mycetozoa. By 1898, Lister's work had built a reputation sufficient to enable his being elected to the Royal Society.[26] Gulielma Lister, a talented artist later updated the standard monograph with colour drawings. Her work built a reputation sufficient to enable her to be elected a fellow of the Linnean Society in 1904, becoming its vice-president in 1929.[27] The couple's last child was Jane Lister; she married Smith Harrison, a wholesale tea merchant, who was marrying for a second time.[28]
After their marriage, the Listers lived at 5 Tokenhouse Yard in Central London for three years until 1822, where they ran a port wine business in partnership with Thomas Barton Beck.[29] Beck was the grandfather of the professor of surgery and proponent of the germ theory of disease, Marcus Beck,[30] who would later promote Lister's discoveries in his fight to introduce antiseptics.[31] In 1822, Lister's family moved to Stoke Newington.[32] In 1826, the family moved to Upton House, a long low Queen Anne style mansion[32] that came with 69 acres of land.[33] It had been rebuilt in 1731, to suit the style of the period.[34]
Education
School
As a child, Lister had a stammer and this was possibly the reason was educated at home until he was eleven.[35] Lister then attended Isaac Brown and Benjamin Abbott's Academy, a private[36] Quaker school in Hitchin in Hertfordshire.[37] When Lister was thirteen,[35] he attended Grove House School in Tottenham, also a private Quaker School[37] to study mathematics, natural science, and languages. His father was insistent that Lister received a good grounding in French and German, in the knowledge he would learn Latin at school.[38] From an early age, Lister was strongly encouraged by his father.[8] and would talk about his father's great influence later in life, particularly in encouraging him in his study of natural history.[35] Lister interest in natural history led him to collect and dissect small animals, fish and osteology, that were examined using his father's microscope[19] and then be drawn using the camera lucida technique that his father had explained to him,[30] or sketched.[37] His father's interests in microscopical research, developed in Lister the determination to become a surgeon[19] and prepared him for a life of scientific research.[8] None of Lister's relatives were in the medical profession. According to Godlee, the decision to become a physician seemed to be an entirely spontaneous decision.[39]
In 1843 his father decided to send him to university. As Lister was unable to attend either University of Oxford or the University of Cambridge owing to the religious tests that effectively barred him, [8] he decided to apply to the non-sectarian University College London Medical School (UCL), one of only a few institutions in Great Britain that accepted Quakers at that time.[40] Lister took the public examination in the junior class of botany; a required course that would enable him to matriculate.[41] Lister left school in the spring of 1844, when he was seventeen.[37]
University
In 1844, just before Lister's seventeenth birthday, he moved to an apartment at 28 London Road that he shared with Edward Palmer, who was also a Quaker.[42] Between 1844 and 1845, Lister continued his pre-matriculation studies, on Greek, Latin and natural philosophy.[43] In the Latin and Greek classes, he won a "Certificate of Honour".[44] For the experimental natural philosophy class, Lister won first prize and was awarded a copy of Charles Hutton's "Recreations in Mathematics and Natural Philosophy".[43]
Although his father wanted him to continue his general education,[45] the university had demanded since 1837, that each student obtain a Bachelor of Arts (BA) degree before commencing medical training. [46] Lister matriculated in August 1845, initially studying for a BA in classics.[47] Between 1845 and 1846, Lister studied the mathematics of natural philosophy, mathematics and Greek earning a "Certificate of Honour" in each class.[44] Between 1846 and 1847, Lister studied both anatomy and atomic theory (chemistry) and won a prize for his essay.[44] On 21 December 1846, Lister and Palmer attended Robert Liston's famous operation where ether was applied by Lister's classmate, William Squire to anaesthetise a patient for the first time.[48][49] On 23 December 1847, Lister and Palmer moved to 2 Bedford place and were joined by John Hodgkin, the nephew of Thomas Hodgkin who discovered Hodgkin lymphoma.[50] Lister and Hodgkin had been school friends.[47]
In December 1847, Lister graduated with a degree of Bachelor of Arts 1st division, with a distinction in classics and botany.[8] While he was studying, Lister suffered from a mild bout of smallpox, a year after his elder brother died of the disease.[8] The bereavement combined with the stress of his classes led to a nervous breakdown in March 1848.[51] [52] Lister's nephew Godlee used the term to describe the situation and is perhaps indicative that adolescence was just as difficult in 1847, as it is now.[8] Lister decided to take a long holiday[36] to recuperate and this delayed the start of his studies.[36] In late April 1848, Lister visited the Isle of Man with Hodgkin and by 7 June 1848 he was visiting Ilfracombe.[53] At the end of June, Lister accepted an invitation to stay in home of Thoman Pim, a Dublin Quaker. Using it as his base, Lister travelled throughout Ireland.[54] On 1 July 1848, Lister received a letter full of warmth and love from his father where his last meeting was "...sunshine after a refreshing shower, following a time of cloud" and advised him to "cherish a pious cheerful spirit, open to see and to enjoy the bounties and the beauties spread around us :—not to give way to turning thy thoughts upon thyself nor even at present to dwell long on serious things".[36] From 22 July 1848, for almost a year, the record is blank.[55]
Medical student
Lister registered as a medical student in the winter of 1849.[47] During his studies, Lister was active in the University Debating Society and the Hospital Medical Society.[30] In the autumn of 1849, he returned to college, bearing a gift of a microscope from his father.[49] After completing courses in anatomy, physiology and surgery, he was awarded "Certificate of Honour's", winning the silver medal in anatomy and physiology and a gold medal in botany.[41]
His main lecturers were John Lindley professor of botany, Thomas Graham professor of chemistry, Robert Edmond Grant professor of comparative anatomy, George Viner Ellis professor of anatomy and William Benjamin Carpenter professor of medical jurisprudence.[36] Although Lister often spoke highly about Lindley and Graham in his writings, it was Wharton Jones professor of ophthalmic medicine and surgery and William Sharpey professor of physiology, who exercised the greatest influence on Lister.[36] As a student, Lister was greatly attracted by Dr. Sharpey's lectures, which inspired in him a love of experimental physiology and histology that never left him.[56]
Wharton Jones was praised by Thomas Henry Huxley for the method and quality of his physiology lectures.[36] As a clinical scientist working in physiological sciences, he was foremost in the number of discoveries he made.[36] He was also considered a brilliant ophthalmic surgeon, his main field.[36] He conducted research into the circulation of the blood and phenomena of inflammation that was carried out on the frog's web and the bat's wing, and no doubt suggested this method of research to Lister.[36] Sharpey was called the father of modern physiology as he was the first to give a series of lectures on the subject.[36] Prior to that the field has been considered part of anatomy. [36] Sharpey studied at Edinburgh university, then went to Paris to study clinical surgery under the French anatomist Guillaume Dupuytren and operative surgery under Jacques Lisfranc de St. Martin. It was in Paris that Sharpey met Syme and became life-long friends.[36] After moving to Edinburgh, he taught anatomy with Allen Thomson as his physiological colleague. He left Edinburgh in 1836, in order to become the first Professor of Physiology at University College, London[36]
Clinical instruction

Before he qualified for his degree, Lister had to complete two years of clinical instruction,[46] beginning his residency at University College Hospital in October 1850.[58] He began as an intern and then house physician to Walter Hayle Walshe.[30] professor of pathological anatomy and author of 1846 study, The Nature and Treatment of Cancer.[59] Lister continued his run of academic excellence in 1850 by being awarded "Certificates of Honours" and winning two gold medals in anatomy and silver medals in surgery and medicine.[41]
Then in his second year in 1851, Lister became first a dresser in January 1851[60] then a house surgeon to John Eric Erichsen in May 1851.[49] Erichsen was professor of surgery[7] and author of the 1853 Science and Art of Surgery[61] described as one of the most celebrated textbooks on surgery in English.[60] The book went through many editions, of which Marcus Beck edited the eighth and ninth editions, adding Lister's antiseptic techniques and Pasteur and Robert Koch's germ theory.[62] His first case notes were recorded on 5 February 1851. As a dresser, his immediate boss was Henry Thompson who recalled "..a shy Quaker...I remember that he had a better microscope than any man in the college".[58]
Lister had only just begun working in his role as dresser to Erichsen in January 1851, when there was an epidemic of erysipelas in the male ward.[63] An infected patient who came from an Islington workhouse was left in Erichsen's surgical ward for two hours.[63] The hospital had been free of infection but within days there were twelve cases of infection and four deaths.[63] In his notebook, Lister stated that the disease was a form of surgical fever, and particularly noted that recent surgical patients were infected the worst, but those with older operations with suppurating wounds, 'mostly escaped'.[63] It was while Lister worked for Erichsen, that his interest in the healing of wounds began.[7] Erichsen was a miasmist who thought the wounds were infected from miasmas that came from the wound itself and caused a noxious form of "bad air" that spread to other patients in the war.[7] Erichsen believed that 7 patients with an infected wound had led to saturation of the ward with "bad air" that spread to cause gangrene.[7] However, Lister took a more rational approach, seeing that some wounds when they were debrided and cleaned, would sometimes heal. He believed that something in the wound itself was at fault.[7]
When he became a house surgeon, Lister had patients put in his charge.[60] For the first time, he came into contact face-to-face with the various forms of blood-poisoning diseases like pyaemia[64] and hospital gangrene, the disease that rots living tissue with a remarkable rapidity.[60] While examining the excision of the elbow of a little boy during the autopsy, who had died of pyaemia, Lister noticed that a thick yellow-pus was present at the seat of the humerus bone, and that distended the brachial and axillary veins.[65] He also noticed the pus advanced in the reverse direction along the veins, bypassing the valves in the veins.[65] He also found suppuration in a knee-joint and multiple abscesses in the lungs.[65] Lister knew that Charles-Emmanuel Sédillot had discovered that multiple abscesses in the lungs were caused by introducing pus into the veins of an animal but at the time could not explain the facts but believed the pus in the organs had a metastatic origin.[65] On 2 October 1900, during The Huxley Lecture, Lister described how his interest in the germ theory of disease and how the theory applied to surgery, began with his investigation into the death of the little boy.[66]
There was an epidemic of gangrene during his surgeoncy. The method to effect a recovery was to chloroform the patient, scrape the soft slough off and burn the necrotic flesh away with mercury pernitrate [60] Occasionally the treatment would be success but if a grey film appeared at the edge of the wound, then it presaged death.[60] In one patient, the treatment was repeated several times due to it failing, resulting in Erichsen amputating the limb, which healed fine.[67] The evidence that Lister recognised was that disease was a "local poison" and probably parasitic in nature.[67] He examined the diseased tissues under his microscope. He saw peculiar objects that he could not identify, as he had no frame of reference to draw conclusions from the observations.[60] In his notebook he recorded:
I imagined they might be the materies morbi in the form of some kind of fungus.[b]
Lister wrote two papers on the epidemics; both were lost. The first paper was on Hospital gangrene [49] and the second was on the use of the Microscope. They were read to the Student Medical Society at UCL.[49]
Lister's first operation
On 26 June 2013, medical historian Ruth Richardson and orthopaedic surgeon Bryan Rhodes published a paper in which they described their discovery of Lister's first operation, made while both were researching his career.[49] At 1 pm on 27 June 1851, Lister, who was a second-year medical student and working at a casualty ward in Gower Street, conducted his first operation. The operation was on Julia Sullivan, a mother of eight grown children. She had been stabbed in the abdomen by her husband, a drunk and ne'er-do-well, who was taken into custody.[68] On 15 September 1851, Lister was called as a witness to his trial at the Old Bailey.[68] His testimony helped convict the husband, who was transported to Australia for 20 years.[68]
Lister found the woman with a coil of intestine about eight inches across, consisting about a yard of the small intestines, that were damaged in two places, protruding from her lower abdomen. The abdomen itself contained three open wounds.[49] After cleaning the intestines with blood-warm water, Lister was unable to place them back into the body, so he took the decision to extend the cut.[49] They were then placed back in the body, the wounds sewn shut and the abdomen sutured.[49] The patient was administered opium to induce constipation, to enable the intestines to recover. Sulivan recovered her health.[49] It was a full decade before his first public operation in the Glasgow Infirmary.[49]
This operation was missed by historians.[49] Liverpool consultant surgeon John Shepherd, in his essay on Lister, Joseph Lister and abdominal surgery, written in 1968,[69] failed to mention the operation, instead starting his dates from the 1860s onwards. He apparently was unaware of what Lister accomplished.[49]
Microscope experiments 1852
Observations on the Contractile Tissue of the Iris
Lister wrote his first paper[70] while he was still at university. It was considered good enough[71] to be published in the Quarterly Journal of Microscopical Science in 1853.[72]
On 11 August 1852, Lister was presented with piece of a fresh human iris by Wharton Jones, at the University College Hospital. Lister was present at the operation conducted by Jones[73] and took the rare opportunity to study the iris.[70] Lister reviewed the existing research, as well as studying tissue from a horse, a cat, a rabbit and a guinea-pig as well as taking six surgical specimens from patients who underwent a surgical operation on their eye.[74] Lister was unable to complete the research to his satisfaction, due to the need to pass his final examination. He offered an apology in the paper:
My engagements do not allow me to carry, the inquiry further at present; and my apology for offering the results of an incomplete investigation is that a contribution tending, in however small a degree, to extend our acquaintance with so important an organ as the eye, or to verify observations that may be thought doubtful, may probably be of interest to the physiologist.[71]
The paper advanced the work of Swiss physiologist Albert von Kölliker, demonstrating the existence of two distinct muscles, the dilator and sphincter in the iris,[19] that corrected the convictions of previous researchers that there was no dilator pupillae muscle.[74]
Observations on the Muscular Tissue of the Skin
His next paper was an investigation into goose bumps[75][76] that was published on 1 June 1853, in the same journal.[77] Lister was able to confirm Kölliker's experimental studies, that in humans the smooth muscle fibres are responsible for the making hair standout from the skin, in contrast to other mammals in which large tactile hairs are associated with striated muscle.[74] Lister demonstrated a new method of creating histological sections from the tissue of the scalp.[78]
Lister's microscopy skills were so advanced that he was able to correct the observations of German histologist, Friedrich Gustav Henle, who mistook small blood vessels for muscle fibres.[79] In each of the papers, he created camera lucida drawings that were so accurate, they could be used to scale and measure the observations.[77]
Both papers attracted significant attention both in Britain and abroad.[80] The naturalist Richard Owen, who was an old friend of Lister's father was particularly impressed by both papers.[80] Owen contemplated recruiting Lister for his own department and forwarded him a thank-you letter on 2 August 1853.[80] Kölliker was particularly pleased at the analysis that Lister had formulated. Kölliker who made many trips to Britain, would eventually meet Lister and became life-long friends.[80] Their close friendship was described in a letter by Kölliker on 17 November 1897, that Rickman Godlee choose to use to illustrate their relationship.[81] Kölliker sent a letter to Lister, when he was president of the Royal Society, congratulating Lister on receiving the Copley medal and fondly remembered his old friends who had died and celebrated his time in Scotland while with Syme and Lister. Kölliker was 80 years old at the time. [81]
Graduation
Lister graduated with Bachelor of Medicine with honours, in the autumn 1852.[72] During his final year, Lister won several prestigious awards, that were heavily contested among the student body of the London teaching hospitals.[82] He won the Longridge Prize
For the greatest proficiency evinced during the three years immediately preceding, on the Sessional Examinations for Honours in the classes of the Faculty of Medicine of the College; and for creditable performance of duties of offices at the Hospital
that included a £40 stipend.[82] He was also awarded a gold medals in Structural and Physiological Botany.[82][44] Lister obtained two of the four available gold medals in Anatomy and Physiology as well as surgery, that came with a medal scholarship of £50 a year, for two years, for his second examination in medicine.[82] In the same year, Lister passed the examination for the fellowship of the Royal College of Surgeons,[72] bringing to a close nine years of education.[72]
With his medical education completed, Sharpey advised Lister to spend a month at the medical practice of his lifelong friend James Syme in Edinburgh and then visit medical schools in Europe for a longer period for training.[83] Sharpey himself had been taught first in Edinburgh and later Paris. Sharpey had met Syme, a teacher of clinical surgery, who was widely considered the best surgeon in the United Kingdom[84] while he was in Paris.[85] Sharpey had gone north to Edinburgh in 1818,[86] along with many other surgeons since, due to the influence of John Hunter. [84] Hunter had taught Edward Jenner who is seen as the first surgeon to take a scientific approach to the study of medicine, that was known as the Hunterian method[87] Hunter was an early advocate for careful investigation and experimentation,[88] using the techniques of pathology and physiology to give himself a better understanding of healing than many of his colleagues.[84] For example, his 1794 paper, A treatise on the blood, inflammation and gun-shot wounds[88] was the first systematic study of swelling,[84] discovering that inflammation was common to all diseases.[89] Due to Hunter, surgery was raised from a job then practiced by hobbyists or amateurs into a true scientific profession.[84] As the Scottish universities taught medicine and surgery from a scientific viewpoint, surgeons who wished to emulate those techniques travelled north for training.[90] Scottish universities had several other features that distinguished them from the medical universities in the south.[91] They were inexpensive and did not require religious admissions tests, attracting the most scientifically progressive students in Britain.[91] The most important differentiator, was that medical schools in Scotland had evolved from a scholarly tradition, where English medical schools relied on hospitals and practice.[91] Experimental science had no practitioners at English medical schools and while Edinburgh University medical school was large and active at the time, southern medical schools were generally moribund, their laboratory space and teaching materials being inadequate.[91] English medical schools tended to view surgery as manual labour, not a respectable calling for a gentleman academic.[91]
Surgical profession 1854
Before Lister's studies of surgery, many people believed that chemical damage from exposure to "bad air", or miasma, was responsible for infections in wounds.[92] Hospital wards were occasionally aired out at midday as a precaution against the spread of infection via miasma, but facilities for washing hands or a patient's wounds were not available. A surgeon was not required to wash his hands before seeing a patient; in the absence of any theory of bacterial infection, such practices were not considered necessary. Despite the work of Ignaz Semmelweis and Oliver Wendell Holmes Sr., hospitals practised surgery under unsanitary conditions. Surgeons of the time referred to the "good old surgical stink" and took pride in the stains on their unwashed operating gowns as a display of their experience.[93]
Edinburgh 1853–1860
James Syme
Syme was a well-established clinical lecturer at Edinburgh University for more than two decades before he met Lister[94] and was considered the boldest and most original surgeon then living in Great Britain.[95] He became a surgical pioneer during his career, preferring simpler surgical procedures as he detested complexity,[94] in the era that immediately preceded the introduction of anesthesia.[96]
In September 1823, at the age of 24, Syme made a name for himself by first performing an amputation at the hip-joint,[96][97] the first time in Scotland. Considered the bloodiest operation in surgery, Syme completed it in less than a minute, [94][96] as speed was essential in a time before anesthesia. Syme became widely known and acclaimed for his development of a surgical operation that became known as Syme amputation, an amputation at the level of the ankle-joint, where the foot is removed and the heel pad is preserved.[98] Syme was considered a scientific surgeon, as evidenced by his paper On the Power of the Periosteum to form New Bone,[96] and became one of the first advocates of antiseptics.
Arrival in Edinburgh
In September 1853, Lister arrived in Edinburgh bearing letters of introduction from Sharpey to Syme.[99] Lister was anxious about his first appointment but decided to settle in Edinburgh after meeting Syme who embraced him with open arms, invited him to dinner and offered him an opportunity to assist in his private operations.[83]
Lister was invited to his Syme's house, Millbank, in Morningside (now part of Astley Ainslie Hospital),[100] where he met, amongst others, Agnes Syme, Syme's daughter by another marriage and granddaughter of the physician Robert Willis.[101][102] While Lister thought that Agnes was not conventionally pretty, he admired her quickness of mind, her familiarity with medical practice, and her warmth.[102] Lister became a frequent visitor to Millbank and met a much wider group of eminent people than he would have in London.[103]
In the same month, Lister began work as an assistant to Syme at the University of Edinburgh[83] In a letter to his father, Lister was surprised at the size of the Infirmary and spoke about his impressions of Syme, "..is larger than I expected to find it; there are 200 Surgical beds, and a large number in other departments. At University College Hospital there were only about 60 Surgical beds, so altogether a prospect appears to be opening of a very profitable stay here. ...Syme is, I suppose, the first of British surgeons, and to observe the practice and hear the conversation of such a man is of the greatest possible advantage".[104] By October 1853, Lister decided to spend the winter in Edinburgh. Syme was so impressed by Lister, that after a month Lister became Syme's supernumerary house surgeon at the Royal Infirmary of Edinburgh[105] and his assistant in his private hospital at Minto House in Chambers Street.[100] As house surgeon, he assisted Syme during every operation, taking notes.[105] It was a much coveted position[30] and gave Lister the option of choosing which of the ordinary cases he would attend.[19] During this period, Lister presented a paper at the Royal Edinburgh Medico-Chirurgical Society on the structure of cancellous exostoses that had been removed by Syme, demonstrating that the method of ossification of these growths was the same as that which occurs in epiphyseal cartilage.[106]
In September 1854, Lister's house surgeoncy appointment was finished.[107] With the prospect of being out of a job, he had spoken to his father about seeking a position at the Royal Free Hospital in London.[107] However, Sharpey had written to Syme, warning him that it was unlikely that Lister would be welcome at the Royal Free as he would have likely eclipsed Thomas H. Wakley, whose father held considerable sway at the hospital.[108] Lister then planned to tour Europe for a year.[109] However an opportunity presented itself, when the noted infirmary surgeon and surgical lecturer at the Edinburgh Extramural School of Medicine Richard James Mackenzie had died.[110] Mackenzie had been seen as a successor to Syme[110] but had contracted cholera in Balbec in Scutari, Istanbul, while on a four-month volunteer sabbatical as field surgeon to the 79th Highlanders during the Crimean War.[30] Lister took advantage of the situation and proposed to Syme that he take over Mackenzie's position to become assistant surgeon to Syme.[109] Syme initially rejected the idea as Lister was not licensed to operate in Scotland, but later warmed to the idea.[109] In October 1854, Lister was appointed a lecturer[111] Lister successfully transferred the lease held by Mackenzie at his lecture room at 4 High School Yards, to himself. On 21 April 1855, Lister was elected a Fellow of the Royal College of Surgeons of Edinburgh[112] and two days later, rented a house at 3 Rutland Square for living.[30] In June 1855, Lister made a hurried trip to Paris to take a course on operative surgery on the dead body and returned in June.[112]
Extramural lecturing

On 7 November 1855, Lister gave his first extramural lecture on the "Principles and Practice of Surgery", in a lecture theatre at 4 High School Yards[113] known as Old Jerusalem and directly located across from the Infirmary.[114] His first lecture was read from 21 pages of foolscap folio.[115] Lister's first lectures were based on notes, either read or spoken, but over time he used them less and less [114] becoming extempore in his speech, slowly and deliberately forming his argument as he went along.[116] By this deliberate way of speaking, he managed to overcome a slight, occasional stammer which, in his early days, had been more pronounced.[116]
His first student was John Batty Tuke,[114] in a class of nine or ten, mostly consisting of dressers.[115] Within a week, twenty-three people had joined.[115] In the next year, only eight folk turned up. In the summer of 1858, Lister had the ignominious experience of reading his lecture to a single student, who arrived ten minutes late. Seven more students arrived later.[117]
His first lecture focused on the concept of surgery, stating a definition of disease that linked it to the Hippocratic Oath.[118] He then explained that surgery could have more benefits than medicines, that could only comfort the patient at best. He then explained the attributes a good surgeon should exhibit, before finishing the lecture by recommending Syme's book "Principles of Surgery". Lister completed 114 lectures that followed a standard syllabus. Lecture VII described his earliest experiment on inflammation when he put mustard on his arm and watched the results. Lecture IV to IX dealt with the circulation of blood. Inflammation was discussed in lectures X to XIII. The second half of the course dealt with clinical surgery. For the last 4 days, he gave 2 lectures a day, in order to complete the event before his marriage, with the first course ending on 18 April 1856.[119] In the summer of 1858, Lister started a second, completely separate course, where he lectured on surgical pathology and operative surgery.[120]
Marriage
By mid-summer 1854, Lister realised that he was attracted to Agnes Syme[121] and he started to court her. Lister wrote to his father and mother about his love but both his parents were concerned about the union, particularly concerning the fact he was Quaker and Agnes have no indication that she was going to change her denomination.[122] During that time, when a Quaker married a person of another denomination, it would be considered as marrying out of the society.[111] Lister was determined to marry Agnes and sent a further letter to his father, asking his father if his financial support would continue should Lister and Agnes become married. Lister's father replied that Agnes not being in the Society of Friends would not affect his pecuniary arrangements.[123] Joseph Jackson offered his son extra money to buy furniture and suggested that Syme would offer a dowry and that he would negotiate with Syme directly on it [123] His father suggested that Lister should voluntarily resign from the Society of Friends.[123] Lister made up his mind and subsequently left the Quakers to become a protestant, later joining the congregation of the Saint Paul's Episcopal Church, in Jeffrey Street, Edinburgh.[124] In August 1855, Lister became engaged to Agnes Syme.[30] On 23 April 1856, Lister married Agnes Syme in the drawing room of Millbank, Syme's house in Morningside.[125] Agnes's sister stated that this was out of consideration of any Quaker relations. [123] Only the Syme family were present.[126] The Scottish physician and family friend John Brown toasted the couple after the reception.[123]
On their honeymoon, the couple spent a month at Upton and the Lake District,[125] followed by three months on a tour of the leading medical institutes in France, Germany, Switzerland, and Italy.[127] The couple returned in October 1856.[128] By this time, Agnes was enamoured of medical research and became Lister's partner in the laboratory for the rest of her life.[126] When they returned to Edinburgh, the couple moved into a rented house at 11 Rutland Street in Edinburgh.[128] The house was situated over three floors with a study on the first floor, that was converting into a consulting room for patients and a room with hot and cold taps on the second floor that became his laboratory.[123] The Scottish surgeon Watson Cheyne, who was almost a surrogate son to Lister, stated after his death that Agnes had entered into her work wholeheartedly, had been his only secretary, and that they discussed his work on an almost equal footing.[63]
Lister's books are full of Agnes' careful handwriting.[63] Agnes would take dictation from Lister, taken at hours at a stretch. Spaces would be left blank amongst the reams of Agnes' handwriting for small diagrams, that Lister would create using the camera lucida technique and Agnes would later paste in.[63]
Assistant surgeoncy
On 13 October 1856, he was unanimously elected to the position of Assistant Surgeoncy at Edinburgh Royal Infirmary.[128]
Contributions to physiology and pathology 1853–1859
While he was in Edinburgh, Lister conducted a series of physiological and pathological experiments between the years 1853 and 1859.[129] His approach was rigorous and meticulous in both measurement and description.[129] Lister was clearly aware of the latest advances of physiological research in France, Germany, and other European countries[8] and maintained an on-going discussion of his observations and results with other leading physicians in his peer group including Albert von Kölliker, Wilhelm von Wittich, Theodor Schwann, and Rudolf Virchow[129] and ensured he correctly cited their work.
Lister's primary instrument of research was his microscope and his primary research material were frogs. Before his honeymoon, the couple had visited his uncle's house in Kinross.[130] Lister had taken his microscope and captured several frogs, intending to use them in the study of inflammation, but they escaped.[130] When he returned from his honeymoon, he used frogs captured from Duddingston Loch in his experiments.[131] Lister carried out his experiments in his laboratory and in the veterinary college abattoir on animals that were either dead or when they were chloroformed. If Lister was using a frog they were pithed, to deprive them of sensation.[132] He also used bats, sheep, cats, rabbits, oxen and horses in his experiments.[132] Lister was tireless in his pursuit of knowledge and this is illustrated by Thomas Annandale, his assistant who stated:
I confess that on more than one occasion our patience was a little tried by the long hours were thus engaged, and more particularly when the dinner hour was many hours overdue, but no one could work with Mr. Lister without imbibing some of his enthusiasm[133]
These experiments resulted in the publication of eleven papers between 1857 and 1859.[129] They included the study of the nervous control of arteries, the earliest stages of inflammation, the early stages of coagulation, the structure of nerve fibres, and the study of the nervous control of the gut with reference to sympathetic nerves.[129] He continued the experiments for three years, until he was appointed to a position at the University of Glasgow.[134]
1855 Beginning of inflammation research
In a letter dated 16 September 1855, Lister recorded the beginnings of his research into inflammation, six weeks before his lectures were to begin.[135] Inflammation was the subject that would preoccupy him for the rest of his life.[136] Later in life, Lister stated that he considered his research into the nature of inflammation to be an "essential preliminary" to his conception of the antiseptic principle and insisted these early findings be included in any memorial volume of his work.[137] In 1905, when he was seventy eight years old, he wrote,
If my works are read when I am gone, these will be the ones most highly thought of[138]
Inflammation is defined by four symptoms, heat, redness, swelling and pain.[136] For surgeons prior to Lister, this meant the arrival of suppuration or putrefaction, meaning local or general infection.[139] As the germ theory of disease had not been discovered, infection as a concept did not exist.[139] However, Lister knew that the phenomena of the slowing of the blood through the capillaries seemed to precede inflammation.[139] Joseph Jackson Lister had written a paper with Thomas Hodgkin that described how blood cells behaved prior to a clot, i.e. specifically how the concave cells fitted themselves together into stacks.[139] Lister knew that to observe the next step, it was important that the tissue remain alive so the blood vessels could be observed through the microscope.[139]
In September 1855, Lister first experiment was on the artery of a frog viewed under his microscope, which was subjected to a water droplet of differing temperatures, to determine the early stage of inflammation.[140][141] He initially applied a water droplet at 80 °F (27 °C) which caused the artery to contract for a second and the flow ceased, then dilated and the area turned red and the flow of blood increased.[142] He progressively increased the temperature until it was 200 °F (93 °C). The blood slowed down then coagulated.[142] He continued the experiment on the wing of chloroformed bat to widen his research focus.[143] Lister concluded that the contraction of the vessels lead to the exclusion of blood cells from the capillaries, not their arrest and blood serum continued to flow. This was his first independent discovery.[118]
The experiments ceased between October 1855 and continued in September 1856 when the couple moved into Rutland Square.[144] Lister started with mustard as an irritant, then Croton oil, acetic acid, oil of Cantharidin and chloroform and many others.[144] They led to the production of three papers. His first paper grew out of need to prepare for this extramural lectures and had begun the year before, continuing in development for six weeks, after he moved into Rutland street.[145] The early paper titled: "On the early stages of inflammation as observed in the Foot of a Frog" was read to the Royal College of Surgeons of Edinburgh on 5 December 1856. The last third was read out extempore.[145]
1856 Beginning of coagulation research
Lister's research into the process of coagulation was the second major area of investigation that he conducted during this period.[146] He had observed during inflammation in certain cases of septicaemia, that it affected the blood vessels lining leading to intravascular blood clotting,[147] that led to putrefaction and secondary haemorrhage in wounds.[148] Beginning with a simple experiment in December 1856 that was described in a note by Agnes, where he pricked his own finger to observe the process of coagulation, [146] it led to five physiology papers on coagulation between 1858[120] and the last in 1863.[66]
There were several competing theories that explained the occurrence of a blood clot, and although the theories were largely abandoned, it was still thought that blood contained a liquifying agent,[149] i.e. fibrin held in a solution of ammonia[150] that became known as the "Ammonia theory".[148]
In 1824, Charles Scudamore had proposed carbonic acid as the solution.[151] The prevailing theory was from Benjamin Ward Richardson, who won the 1857 Astley Cooper triennial prize for his essay, where he postulated that blood remained liquid due the presence of ammonia. In the same year, Ernst Wilhelm von Brücke proposed that the vital actions of the vessels inhibited the bloods natural tendency to coagulate.[152]
1856 On the minute structure of involuntary muscle fibre
Lister's third paper[153][154] was published in 1858 in the same journal and was read before the Royal Society of Edinburgh on 1 December 1856.[153] It was research into the histology and function of the minute structures of involuntary muscle fibres.[74] The experiment was conducted in the autumn of 1856,[155] and was designed to confirm Kölliker's observations on the structure of individual muscle fibres.[74] Kölliker description had been criticised as he had used needles to separate the tissue, to observe the individual cells, so his critics stated that he had observed artefacts for the experiment rather than the real muscle cells.[145] Lister proved conclusively that the muscle fibres of blood vessels, described by Lister as slightly flattened elongated elements,[153] were similar to those found by Kölliker in pig intestine, but were wrapped spirally and individually, around the innermost membrane.[155] He stated that the different variations in shape, from long tubular bodies with pointed ends and elongated nuclei to short "spindles" with squat nuclei, were due to different phases of the contraction.[155] During "The Huxley Lecture" he stated he could not imagine a more efficient mechanism being used to constrict these vessels.[156]
1857 On the flow of the lacteal fluid in the mesentery of the mouse
His next paper, [157] was a short report, based on observations that he made in 1853.[158] This first experiment by Lister, as opposed to purely microscope work, was to prove two goals:[81] firstly to determine the nature of the flow of chyle in the lymphatics and secondly,[81] to determine if the lacteals in the gastrointestinal wall could absorb solid matter, in the form of granules, from the lumen.[81] For the first experiment, a mouse that was fed beforehand on bread and milk was chloroformed then had its abdomen opened and a length of intestine placed on glass under a microscope.[81] Lister repeated the experiment several times and each time saw mesenteric lymph flowing in a steady stream, without visible contractions of the lacteals. For the second experiment Lister dyed some bread with indigo dye and fed it to a mouse, with the result that no indigo particles were ever seen in the chyle.[159] Lister delivered the paper to the 27th meeting of the British Medical Association, that was held in Dublin between 26 August to 2 September 1857.[121] The paper was formally published in 1858 in the Quarterly Journal of Microscopical Science.[157]
Seven papers on the origin and mechanism of inflammation
In 1858, Lister published seven papers on physiological experiments he conducted on the origin and mechanism of inflammation.[160] Two of these papers were research into the neural control by the nervous system of blood vessels, "An Inquiry Regarding the Parts of the Nervous System Which Regulate the Contractions of the Arteries" and "On the Cutaneous Pigmentary System of the Frog", while the third and the principal paper in the series was titled: "On the Early Stages of Inflammation", which extended the research by Wharton Jones.[160] The three papers were read to the Royal Society of London on 18 June 1857.[161] They had originally been written as one paper and had been sent to Sharpey, John Goodsir and the English pathologist James Paget for review.[162] However, Paget and Goodsir both recommended that is should be published as three separate papers.[162][163]
1858 An Inquiry Regarding the Parts of the Nervous System Which Regulate the Contractions of the Arteries
The first of these series of experiments[164] was designed to satisfy a contemporary dispute between physiologists, concerning the origin of the influence exercised over blood vessel diameter (calibre) by the sympathetic nervous system.[147] The dispute began when Albrecht von Haller formulated a new theory known as Sensibility and Irritability in his 1752 thesis De partibus corporis humani sensibilibus et irritabilibus. The dispute had been debated since the middle of the 18th century. Haller put forward the view that contractability was a power inherent in the tissues which possessed it, and was fundamental fact of physiology.[165] It concerned the property of irratability, the supposed automatic response of muscular tissue, especially visceral tissue, to external stimulus, that caused them to contract when stimulated. [165] Even as late as 1853, highly respected textbooks, for example William Benjamin Carpenter Principles of Human Physiology stated the doctrine of 'irritability' was a fact beyond dispute.[166] and was still considered contentious when John Hughes Bennett created the Physiology article for the 8th edition of Encyclopædia Britannica in 1859.[165]
In his experiments that he started in the autumn of 1856, Lister used a microscope fitted with ocular micrometer to measure the diameter of blood vessels in a frogs web.[c] In a before and after experiment, he ablated parts of the central nervous system[167] and also before and after, with the splitting of the sciatic nerve.[168][160] Lister concluded that blood vessel tone[d] was controlled by the medulla oblongata and the spinal cord.[170] This refuted Wharton's conclusions, in his paper Observations on the State of the Blood and the Blood-Vessels in Inflammation.[171] who was not able to confirm that the control of blood vessels of the hind legs was dependent upon spinal centres.[172]
1858 On the Cutaneous Pigmentary System of the Frog
The second part of the original paper[173] that was an experiment into the nature and behaviour of pigment.[174] It had been known for some years that the skin of the frog is capable of varying in colour under different circumstances.[175] The first account of this mechanism and how it is affected had been first described by Ernst Wilhelm von Brücke of Vienna in 1832[175] and later investigated further by Wilhelm von Wittich in 1854[173] and Emile Harless in 1947.[176]
Lister had seen how the beginning of inflammation was always accompanied by a change of colour in the frogs web.[175] He determined that the pigments consisted of "very minute pigment-granules" that are contained in a network of stellate cells, the branches of which, subdividing minutely and anastomosing freely with one another and with those of neighbouring cells, constitute a delicate network in the substance of the true skin.[175] It had been supposed that the concentration and diffusion of the pigment depended upon the contraction and extension of the branches of the star-shaped cells in which it was contained; and that only these movements of the cells were under the influence of the nervous system. At the time, there was no cell theory of matter nor was they're any dyes or fixatives that could used to enhance experimental discovery.[174] Indeed, Lister wrote of this, stating "The extreme delicacy of the cell wall makes it very difficult to trace it among the surrounding tissue".[174] Lister observed that it was the pigment granules themselves and not the cells that moved, and that this movement is not merely brought about by the control of the nervous system, but that it may be caused by the direct action of irritants on the tissues themselves.[175] He believed that pigment reflected the activity of blood vessels, though it was the slowing of blood flow that initiates the process of inflammation.[174]
1858 On the early stages of inflammation
The focal study[177] was the longest paper of the three and the last to be published.[162] Like many of his colleagues, Lister was aware that inflammation was the first stage of many postoperative conditions[178] and that excessive inflammation often preceded the onset of a septic condition.[179] Once that happened, the patient would develop a fever.[179] Lister had come to the conclusion that accurate knowledge of the functioning of inflammation could not be obtained by researching the more advanced stages that were subject to secondary processes.[180] He therefore started, in quite a different way from that of almost all his predecessors by directing his enquiry to the very first deviations from health, hoping to find in them "the essential character of the morbid state most unequivocally stamped".[180] Essentially, Lister performed these experiments to discover the causes of erythrocyte adhesiveness. As well as experimenting on frogs web and bats wing,[180] Lister used blood that he had obtained from the end of his own finger that was inflamed and compared it against blood from one of his other fingers.[160] He discovered that after something irritating had been applied to living tissues which did not kill them outright firstly the blood-vessels contracted and their lumen became very small; the part became pale. Secondly, the vessels after an interval, dilated and the part became red. Thirdly, some of the blood in the most injured blood-vessels slowed down in its flow and coagulated. Redness occurred which, being solid, could not be pressed away. Lastly, the fluid of the blood passed through the vessel walls and formed a " blister " about the seat of injury.[132] He found that each tiny artery was surrounded by a muscle, which enables it to contract and dilate. He found further that this contraction and dilation was not an individual act on its part, but was an act dictated to it by the nervous cells in the spinal cord.[181]
The paper was divided into four sections:
- The aggregation of red blood cells when removed from the body, i.e., which occurs during coagulation.
- This section deals with the aggregation of the cells of the blood, which occurs during the process of clotting. It shows that when blood is removed from the body this aggregation depends on their possessing a certain degree of mutual adhesiveness, which is much greater in the white blood cells than in the red blood cells. This property, though apparently not depending upon vitality, is capable of remarkable variations, in consequence of very slight chemical changes in the blood plasma.[180]
- The structure and function of blood vessels.
- This section shows that the arteries regulate, by their contractility, the amount of blood transmitted in a given time through the capillaries, but that neither full dilatation, extreme contraction, nor any intermediate state of the arteries, is capable per se of producing accumulation of blood cells in the capillaries.[182]
- The effects of irritants on blood vessels, e.g., hot water.
- This section details how the effects are two-fold
- firstly, a dilatation of the arteries (commonly preceded by a brief period of contraction), which is developed through the nervous system and is not confined to the part brought into actual contact with the irritant, but implicates a surrounding area of greater or less extent; and
- secondly, an alteration in the tissues upon which the irritant directly acts, which makes them influence the blood in the same manner as does ordinary solid matter. This imparts adhesiveness to both the red and the white blood cells, making them prone to stick to one another and to the walls of the vessels, and so gives rise, if the damage to the tissues be severe, to stagnation of the blood flow and ultimately to obstruction.[182]
- This section details how the effects are two-fold
- The effects of irritants on tissue.[182]
- The fourth section describes the effects of irritants upon the tissues. It proves that those which destroy the tissues when they act powerfully, produce by their gentler action only a condition bordering on loss of vitality, i.e. a condition in which the tissues are incapacitated, but from which they may recover, provided the irritation has not been too severe or protracted.[182]
Lister's paper was able to show that capillary action is governed by the constriction and dilation of the arteries. The action is affected by trauma,[e] irritation or reflex action through the central nervous system.[160] He noticed that although the capillary walls lack muscle fibres, they are very elastic and are subject to significant capacity variations that are influenced by arterial blood flow into the circulatory system.[160] Drawings made with a camera lucida were used to depict the experimental reactions.[160] They displayed vascular stasis and congestion in the early stages of the body's reaction to damage. According to Lister, vascular alterations that were initially brought on by reflexes occurring within the nervous system were followed by changes that were brought on by local tissue damage. In the conclusions to the paper, Lister linked his experimental observations to physical clinical conditions, for example skin damage resulting from boiling water and trauma occurring after a surgical incision.[160]
After the paper was read to the Royal Society in June 1857, it was very well received and his name became known outside Edinburgh.[134]
On a Case of Spontaneous Gangrene from Arteritis, and on the Causes of Coagulation of the Blood in Diseases of the Blood-Vessels
Lister's first paper is an account of a case of spontaneous gangrene in a child.[183] The paper on coagulation[184] was read before the Medico-Chirugical Society of Edinburgh on 18 March 1858.[149] In an account written by Agnes, she states that there was no one at the medical school meeting who was capable of appreciating it, and the remarks made upon it were very poor. There was suggestions for improvement which Lister threw out. There was lots of cheering, proclaiming it a great success. The paper was written-up at 7pm, with Lister dictating and Agnes writing it during a 50-minute session, followed by the exposition to the society at George Street hall at 8pm.[185]
Lister first used the amputated legs from sheep and discovered that blood remained liquid in the blood vessels for up to six days and still underwent coagulation, albeit more slowly when the vessel was opened. He also noticed that if vessels remained fresh, the blood would remain fluid.[186] In later experiments he moved to cats.[149] He tried to emulate an inflamed blood vessel by exposing the jugular vein of the animal and applying irritants then constricting and opening the flow, to measure the effect. He noticed that in the damaged vessel the blood would coagulate[184][147] He eventually came to the conclusion that if there was ammonia in the blood, it was much less important than the condition of the vessel in stopping coagulation.[149] He tested his hypothesis on three cadavers by examining the condition of various veins and arteries and found he was correct.[187] He also concluded that the Ammonia theory did not apply to vessels in the body, but it could apply to blood outside the body. While that was incorrect, his other conclusions were accurate.[149] Specifically that inflammation in the blood vessel lining, results in coagulation occurring.[66] Lister realised that vascular occlusion increased the pressure through the network of small vessels, leading to the formation of "liquor sanguinis"[f] that lead to further localised damaged perfusion.[66] Certainly, Lister had no knowledge of the coagulation cascade but his experiments contributed to the current understanding of clotting,[147] the final product of coagulation.
Lister continued experimenting in April, examining vessels and blood from a horse. This resulted in another communication to the society on 7 April.[149] His work in coagulation continued until the end of year. Lister's second article on coagulation was published in August 1958, was one of two case histories he published in the Edinburgh Medical Journal in 1858.[188] Titled: "Case of Ligature of the Brachial Artery, Illustrating the Persistent Vitality of the Tissues".[189] The history described saving a patient's arm from being amputated which had been constricted by a tourniquet for thirty hours.[183] The second history was titled "Example of mixed Aortic Aneurysm" and published in December 1858.[190]
1858 Preliminary account of an inquiry into the functions of the visceral nerves
Lister continual interest in the nervous control of blood vessels led him to conduct a series of experiments during June and July 1858, where he researched the nervous control of the gut.[188] The research was published in the form of three letters sent to Sharpey. The first two letters were sent on 28 June and 7 July 1858 [191] The last letter was published as the "Preliminary Account of an Inquiry into the Functions of the Visceral Nerves, with special reference to the so-called Inhibitory System.".[192]
He had been studying the work of Claude Bernard, LJ Budge and Augustus Waller and had become interested in what was known as "sympathetic action", where inflammation appeared in a different area from the source of irritation.[193] This led him to study Pflüger's 1857 paper titled "About the inhibitory nervous system for the peristaltic movements of the intestines",[194] proposed that the splanchnic nerves instead of exciting the intestine muscle layer that they are connected to, inhibit their movement.[188] The German physiologist Eduard Weber made the same claim.[188] Pflüger had named these inhibitory nerves "Hemmungs-Nervensystem", a name that Syme, at Lister's request thought they should be translated as inhibitory nervous system.[195] Lister dismissed Pflüger's idea of inhibitory nerves as not only implausible but not supported by observation,[196] as a mild stimulus caused increased muscle activity which changed to a decreased muscle activity as the incoming stimulus became stronger.[196] Lister believed that it was questionable whether the motions of the heart or the intestines are ever checked by the spinal system, except for very brief periods.[196]
Lister conducted a series of experiments using mechanical irritation and galvanism to stimulate the nerves and spinal cord in rabbits and frogs.[196] and due to rabbits active gut movement, he considered them ideal for the experiment.[197] To ensure their gut reflexes were not impaired, the rabbits were not anaesthetised.[147] Lister conducted three experiments. In the first experiment, an incision was made in the rabbit's side and a section of intestine was pulled through the skin. Lister then connected a magnetic coil battery to the splanchnic nerves in the spinal cord. When the current was applied, the gut completely relaxed but when the current was applied locally, a small localised contraction occurred that did not spread to the bowel.[147] Lister stated that "this observation is of fundamental importance, since it proves that the inhibitory influence does not operate directly upon the muscular tissue, but upon the nervous apparatus by which its contractions are, under ordinary circumstances, elicited".[192] In the second experiment, Lister examined the reaction in a section of the bowel, when he restricted the blood supply by tying the vessels and found that there was increase in peristalsis. When he applied current the gut relaxed. He concluded that activity in the gut was under the control of bowel wall nerves and had been stimulated due to loss of blood.[192] In the third experiment he removed the nerves from a section of bowel while ensuring to maintain a good blood supply. This time, stimulation of the section had no effect except when the section would spontaneously contract. The experiment enabled Lister to conclude: "
During the histological study of the bowel wall, Lister discovered a plexus of neurons[197] the myenteric plexus, that confirmed the observations made by Georg Meissner in 1857.[198][199] Lister concluded, "...it appears that the intestines possess an intrinsic ganglionic apparatus which is in all cases essential to the peristaltic movements, and, while capable of independent action, is liable to be stimulated or checked by other parts of the nervous system".[196]
Although Lister did not believe in the inhibitory system, he did conclude that extrinsic nerves controlled the intestinal motor function indirectly through their effect on the plexus. It was not until 1964 that this was proven by Karl‐Axel Norberg.[200]
Notice of further researches on the coagulation of the blood
Lister's third paper on coagulation[201] was a short article in the form of a communication consisting of five pages that was read before the Medico-Chirugical Society of Edinburgh on 16 November 1859. In the paper, Lister found that the coagulation of blood was not solely dependent on the presence of ammonia, but may also be influenced by other factors. In a demonstration before the society, Lister had a sample of horse's blood that had been shed twenty-nine hours earlier and added acetic acid to it. The blood remained fluid despite being acidified, but it eventually coagulated after being left to stand for 15 minutes. Lister demonstrated that the Ammonia theory was incorrect as the coagulation of the blood was not dependent on the presence of ammonia. He concluded that the coagulation of blood may be influenced by other factors in addition to or instead of ammonia, and that the Ammonia theory was fallacious.[201]
Glasgow appointment
On 1 August 1859, Lister wrote to his father to inform him of the ill-health of James Adair Lawrie, Regius Professor of Surgery at the University of Glasgow, believing he was close to death.[202] The anatomist Allen Thomson had written to Syme to inform him of Lawrie's condition and that it was his opinion that Lister was the most suitable person for the position.[203] Lister stated that Syme believed he should become a candidate for the position.[202] He went on to discuss the merits of the post; a higher salary, being able to undertake more surgery and being able to create a bigger private practice.[202] Lawrie died on 23 November 1859.[204] In the following month, Lister received a private communication, although baseless, that confirmed he had received the appointment.[205] However, it was clear the matter was not settled when a letter appeared in the Glasgow Herald on 18 January 1860 that discussed a rumour that the decision had been handed over to the Lord Advocate and officials in Edinburgh.[206][205] The letter annoyed the members of the governing body of Glasgow University, the Senatus Academicus. The matter was referred to the Vice-Chancellor Thomas Barclay that tipped the decision in favour of Lister.[207] On 28 January 1860, Lister's appointment was confirmed.[30]
Glasgow 1860–1869

University life
To be formally induced into the academic staff, Lister had to deliver a Latin oration before the senatus academicus.[208] In a letter to his father, he described how surprised he was when a letter arrived from Allen Thomson informing him that the thesis had to be presented the next day on 9 March. Lister unable to start the paper until 2am the next night, had only prepared around two thirds of it, when he arrived in Glasgow. The rest was written at Thomson's house. In the letter, he described the dread he felt being admitted into the room prior to presenting the oration. After the thesis was read and Lister was inducted to the senate, he signed a statement not to act contrary to the wishes of the Church of Scotland.[209] While the contents of his thesis have been lost, the title is known, "De Arte Chirurgica Recte Erudienda" ("On the proper way of teaching the art of surgery").[210]
In early May 1860, the couple made the journey to Glasgow to move into their new house at 17 Woodside Place, at the time on the western edge of the city.[211] In 1860, university life in Glasgow was lived in the grimy quadrangles of the small college on Glasgow High Street, a mile east of the city centre next to Glasgow Royal Infirmary (GRI) and the Cathedral and surrounded by the most squalid part of the old medieval city.[212] The Scottish poet and novelist Andrew Lang wrote of his student days at the college, that while Coleridge could smell 75 different stenches during his student days in Cologne, Lang counted more.[212] The city was so polluted the grass did not grow.
The position of Professor of Surgery at Glasgow was peculiar, as it did not carry with it an appointment as surgeon to the Royal Infirmary, as the university was separate from the hospital. The allotment of surgical wards to the care of the Professor of Surgery depended upon the goodwill of the directors of the infirmary.[213] His predecessor Lawrie never held any hospital appointments at all.[214] Having no patients to care for, Lister immediately began a summer lecture course . He discovered that college classrooms were considered too small and had low ceilings for the number of students, which made them unpleasant to be in when filled to overcrowding.[212] Before his first lecture, the couple cleaned and painted the dingy lecture room assigned to them, at their own expense.[212] He inherited a large class of students from his predecessor that grew rapidly.[212]
After his first session, he wrote favourably of Glasgow:
The facilities I have here for prosecuting this course as compared to the difficulties I laboured under in Edinburgh are quite delightful – museums, abundant material and a good library all at my disposal and my colleague Allen Thompson co-operating in the kindest and most valuable manner[215]
In August 1860, Lister was visited by his parents, who took a "saloon" carriage on the Great Northern Railway. [216] In September 1860, Marcus Beck came to live with the Listers and their two servants, while he studied medicine at the university.[216] In the closing weeks of the summer, the Listers along with Beck, Lucy Syme and Ramsay went on a short holiday to Balloch, Loch Lomond. While the group was visiting Tarbet, Argyll, then men rowed across the loch and ascended Ben Lomond.[217]
Election to surgeoncy
In August 1860, Lister had been rejected for a post at the Royal Infirmary by David Smith, a shoemaker who was the chairman of the hospital board.[218] When Lister put his case to Smith explaining the need for anatomical demonstrations so the students could understand the practice of surgery, Smith stated his belief that "the infirmary was a curative institution, not an educational one".[217] The rejection both annoyed and surprised Lister as he had been promised by Thomson that the position was assured.[217] Indeed, he had informed his father of the fact that the post was guaranteed in his letter to his father.[218]
In November 1860, the winter lecture course began. In total 182 students registered for the lectures[219] and according to Godlee it was likely the "largest class of systematic surgery in Great Britain, if not in Europe".[219] The class consisting of mostly 4th year students with some 3rd and 2nd year students, was so enthused, that they decided to make Lister the Honorary President of their Medical Society.[217] When the time approached for the election to the surgeoncy in 1861, 161 students signed a petition on parchment supporting his claim for election.[219] Lister was not elected until 5 August 1861, in what was described by Beck as a "troublesome canvas".[220] Lister was put in charge of wards XXIV (24) and XXV (25) in October 1861.[221] It wasn't until November 1861 that he performed his first public operation.[222] Soon after Lister arrived at the GRI, a new surgical block was built and it was here that he conducted many of his trials of antisepsis.[223]
Holmes System of Surgery
During this period between the end of his winter lecture course and his appointment, Lister's correspondence contained little of scientific interest. Finally, a letter to his father dated 2 August 1861 explained the reason.[224] He has halted his experiments on coagulation to work on writing two chapters, "Amputation" and "On Æsthetics" (On anaesthetics) for a book by Timothy Holmes called System of Surgery that was published in four volumes in 1862.[225]
Chloroform was Lister's preferred anaesthetic.[226] He wrote three paper's for Holmes in 1861, 1870 and 1882 chapters.[227][228] The science of anaesthesia was in its infancy[229] when Lister had first recommended chloroform to Syme in 1855 and had continued to use it until the 1880s.[220] His sister Isabella Sophie had first described its use to him in 1848, when she had a tooth pulled. He had further clinical experience using it on three patients who had tumours of the jaw, without complications in 1854.[226] He had classed it along with alcohol and opium as a "specific irritant" in "On the early stages of imflammation".[226] Lister preferred it, as it was safer to use in artificial light than ether, it protected the heart and blood vessels and as Lister believed gave the patient "mental tranquility" as it was the safest. [220] In the 1871 edition, he reported there had been no deaths in Edinburgh or Glasgow infirmaries from chloroform, during the period between 1861 and 1870.[220] Lister described how his assistant applied the chloroform onto a simple handkerchief, as a mask while he watched the patients breathing. In 1870, he updated the chapter to state that he felt apprehension using chloroform on the "aged and infirm".[220] In the same edition he recommended nitrous oxide for tooth extraction and the use of ether to avoid vomiting after abdominal surgery. In the winter of 1873, the English medical journals reported that sulphuric ether should be used instead but Watson Cheyne stated there had been no deaths from chloroform during winter 1873. In 1880, the British Medical Association recommended the synthetic gas ethidene dichloride for clinical trials. On 14 November 1881, Paul Bert had published the dose-response curve of chloroform but Lister believed that smaller doses would be sufficient to anaesthetize the patient.[230] Starting in April 1882, Lister first conducted clinical research using ether and from July to November, lab experiments on chaffinches and then on himself and Agnes, to determine the correct dose.[231] The 1882 chapter continued to recommend chloroform.[231]
The chapter on amputation was much more technical than the anaesthesia chapter, for example describing the ways of cutting the skin to produce flaps to close over the wound.[g][231][232] In the first edition, Lister examined the history of amputation from Hippocrates to Thomas Pridgin Teale, William Hey, François Chopart, Nikolay Pirogov and Dominique Jean Larrey [233] and the discovery of the tourniquet by Etienne Morel.[121] In the first edition, Lister devoted 7 pages to dressings, but by the third edition only a single sentence to recommend a dry dressing[234] as opposed to the more common water dressing, where it was thought that water excluded the air.[235] By the third edition, Lister focused on describing three innovative surgical techniques. The first was a method for amputation through the thigh that he developed between 1858 and 1860 that was a modification of Henry Douglas Carden's technique for knee amputation. [231] The thigh amputation was through the femoral condyles, in a circular fashion with a small posterior flap that enabled a neat scar.[236]
The second technique was an aortic tourniquet for controlling blood flow in the abdominal aorta.[233] The vessels of the aorta were too tough to close properly and ligatures either damage the artery walls or caused premature death if left in too long.[231] The third technique was a method of bloodless operation that he created in 1863-1864 by elevating a limb and quickly applying an india rubber tourniquet to stop limb circulation[237] but it became unnecessary with the use of the Esmarch bandage.[121] In 1859, he advocated for the use of silver wire sutures that that been invented by J. Marion Sims, but their use fell out of favour with the introduction of antiseptics.[233]
Croonian Lecture
On 1 January 1863, Lister returned to the topic of coagulation when he presented the Croonian Lecture with the title "On the coagulation of the blood",[238] although there was little that was new.[239] The lecture was given at the invitation of the Royal Society and the Royal College of Physicians and was held in London.[183] Lister opened the lecture by reconfirming the fallacious nature of the Ammonia theory, instead proposing that shed blood coagulates when the solid and fluid elements of the blood meet. Through experiments he confirmed that blood plasma (liquor sanguinis) alone lacks the ability to coagulate, but gains it when in contact with the red blood cell.[66] Lister suggests that living tissues possess similar properties in relation to blood coagulation. He mentions the presence of coagulable fluid in the interstices of cellular tissue and describe instances of edema liquid coagulating after emission, possibly due to slight admixture of red blood cells.[238] Lister highlighted the tendency of inflamed tissues to induce coagulation in their vicinity, suggesting that inflamed tissues temporarily lose their vital properties and behave like ordinary solids, leading to coagulation. He provided examples of inflamed arteries and veins exhibiting coagulation on their interior, similar to artificially deprived vessels.[238] Lister then describes the difference between inflammatory exudations and oedema effusions, with inflamed tissues inducing coagulation while oedema effusions remain fluid. The increased pressure caused by accumulated red blood cells in inflamed capillaries is hypothesised to contribute to the loss of healthy condition in capillary walls, leading to coagulation.[238] In the closing sections of the lecture, Lister relates his previous microscopic investigation, published in the Philosophical Transactions, which supported the view that tissues can be temporarily deprived of vital power under the action of irritants. He proposes that inflammatory congestion arises from the adhesiveness of red blood cells caused by the interaction with irritated tissues, similar to their behaviour outside the body when encountering ordinary solids. In finishing the lecture, Lister was satisfied that his previous conclusions on the nature of inflammation was independently confirmed through his research into blood coagulation.[238]
On excision of the wrist for caries
Lister's most original work that he undertook during 1863 and the beginning of 1864 was the development of a surgical technique for the excision of caries from the wrist., i.e.the removal of diseased bone due to tuberculosis. [240] The procedure consisted of the removal of the ends of the bones entering into an articulation instead of amputating the whole limb and was considered a recent development in "conservative surgery".[241] Several surgeons had attempted the procedure. It was first performed by German surgeons Johann von Dietz in 1839 and Johann Ferdinand Heyfelder in 1849, followed by British surgeon William Fergusson in 1851.[242] While the development of techniques for excision of the elbow was largely successful, similar success for the excision of the wrist was elusive, so amputation was considered the most appropriate treatment even in 1860.[241] The complicated technique that Lister developed was the removal of the tissue where the disease was likely to occur but in the process preserving those structures that were used to move the fingers and wrist.[243] The technique was adopted by the profession and the only complaint from surgeons was the length of the operation at 90 minutes.[243] Lister waited almost a year before publishing the paper in March 1865 in The Lancet.[244] The paper presented 15 case histories.[245] In summary, ten people were cured, two had hopes of achieving a cure, two died of causes independent of the operation and Lister considered one operation unsatisfactory, which was a failure rate of 13%.[245]
Edinburgh position
In June 1864, the Professor of Systematic Surgery in Edinburgh James Miller, died.[246] The Edinburgh chair was considered the most prestigious within the Scottish medical community and came with annual stipend of between £700-£800 per year. Syme and his friends suggested that Lister should apply as his candidature was all but assured.[246] A number of reasons have been advanced on why Lister applied. In a letter to his father he said that he saw Glasgow as a stepping stone. There were a multitude of reasons either to stay or go. He was drawn to research, his friends were there and he found the routine nature in Glasgow, "working in a corner". There was also the fact that his tenure only lasted 10 years.[247] Testimonials from Christison, Paget, Buchanan and Syme followed the application. By the end of June, Lister was convinced the position was his.[248] However, the chair went with James Spence instead.[245] Lister was disappointed and in social settings tended to solipsism in conversation, but by October his father, in a letter said that it was, "very gratifying to learn thy complete reconcilement to remaining at Glasgow".[248]
Before he received the disappointing news, Lister had been called back to Upton as his mother Isabella was on her deathbed. She died on 3 September 1864.[249] His father was now living alone at Upton as the only daughter left at home had married in 1858.[249] Communication with his children became of paramount importance to Joseph Jackson and he started to send Lister a letter every week, stating in October "The thought that thou wilt look for letters from thee weekly, and the letters when they come, are alike gratifying to thy poor father.[248]
- Winter lecture course
On 1 November, Lister began the winter lecture course that was divided into two divisions: Those conditions common with tissue and organs and those conditions of physiology.[248] His first lectures were on blood, then nerves, then detailed special nerves which explained the process of inflammation.[250] In introducing the subject, he stated that any injury that didn't cause death would result in inflammation with the familiar symptons of redness, swelling and pain. These symptons were indicative of "inflammatory congestion"[251] that is the suspension of vital energy, which began with red corpuscles adhering together, that are caused by fibrin, which itself was caused by two substances in the blood, one in the blood cell and one in liquor sanguis (plasma). He described two types of inflammation, direct and indirect, direct by a noxious agent and indirect by "sympathy" which was an indication that Lister's frame of references was wholly inadequate.[250] He then provided various examples and then examined various types, for example acute, latent or chronic. The following lectures were devoted to explaining how to alleviate the symptom's of inflammation, for example raising a limb to enable blood to flow easier, or reducing tension for example, by draining an abscess.[252] The remarkable aspect of Lister's theory of inflammation was that while the details of the observations were correctly made, the theoretical structure used to explain the observations was completely wrong. Lister's error lay in his belief that inflammation was a "unitary disease", a single underlying disease when in effect it was a range of conditions.[252] The second division of the lecturers focused on the heart, blood vessels, lymphatic system, bones, joints and nerves.[253]
- Christmas
Lister and Agnes spent Christmas 1864 with Joseph Jackson at Upton.[253] In January, Lister attended a quite unusual operation by Syme in Edinburgh, whereby a patient's tongue was removed.[253] A month later, Lister received an interesting letter from Jackson on fees that indicated Lister's growing private practice that he began in 1861. His practice was unusual as it was solely dedicated to surgery, during a period when operations either took place at the doctor's surgey or at the patient's home.[253] In March 1865, Lister along with the colleagues became involved in the case of the murderer Edward William Pritchard who was employed as a doctor in Glasgow. Prichard had broken his oath. In a letter to his father, Lister expressed his sincere hope that he would be hung.[254]
Pasteur
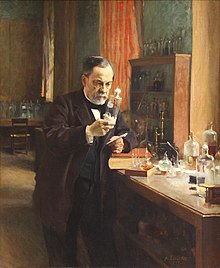
At the end of 1864[255][256] or during the spring of 1865[257] (sources vary) while walking home with Thomas Anderson,[258] the chemistry professor at Glasgow and discussing putrefaction, Anderson drew Lister's attention to the latest research of the French chemist Louis Pasteur,[259] who had discovered living things that caused fermentation and putrefaction.[260] At that time, Lister was not a wide reader of continental literature,[259] began reading the weekly journal Comptes rendus hebdomadaires of the French Academy of Sciences through the years 1860-1863 where Pasteur discussed fermentation and putrefaction.[261]
The two papers that Anderson recommended to Lister was Sur les corpuscules organisés qui existent dans l'atmosphère, examen de la doctrine des générations spontanées 1861 (On the organized particles that exist in the atmosphere, examination of the doctrine of spontaneous generations).[262] In this paper, Pasteur disproved the theory of spontaneous generation by proving the hypothesis that life in boiled infusions arose from spores.[263] He also proved that particles in the air could be cultivated; and if they were introduced from the air, into a sterile liquid, they would reappear and multiply in the liquid.[264] The second paper that Lister read that day was Pasteur's magnum opus, titled Examen du rôle attribué au gaz oxygène atmosphérique dans la destruction des matières animales et végétales après la mort 1863 (Examination of the role attributed to atmospheric oxygen gas in the destruction of animal and plant matter after death).[265] published on 29 June 1863.[255] The paper concluded that fermentation, putrefaction and slow combustion destroyed organic matter and these were necessary processes for life to exist.[263] Pasteur learned that slow combustion was related to the anaerobic conditions that were present if microorganisms were present.[263]
Several other papers would directly influence Lister's work on microorganisms.[264] The third paper was the Mémoire sur la fermentation appelée lactique (Extrait par l'auteur) (Memoir on the so-called lactic acid fermentation (Extracted by the author)) that was published in 1857[266] and describes the discovery of the microbe that is responsible for the process of fermentation in beer yeast.[263] The fourth paper was the Memoire sur la Fermentation Alcoolique (Memoir on Alcoholic Fermentation) that was published in Annales de chimie et de physique in 1860.[267] Pasteur described the living beings, microorganisms in yeast, Saccharomyces cerevisiae that were responsible for the effervescent change that lead to fermentation.[263] The last paper by Pasteur was the Animalcules infusoires vivant sans gaz oxygène libre et déterminant des fermentations, (Animal Infusoria Living in the Absence of Free Oxygen and their fermentations)[268] The paper that was presented in 1861, was seminal in enabling Lister to understand the nature of sepsis,[263] where the bodies response to infections leads to injury in the tissue and organs. Pasteur's research led him to believe the ferment that produced Butyric acid was a microbe that lived in the absence of oxygen.[263] The last paper that Lister found important was "Recherches sur la putréfaction" (Research on putrefaction)[269] that concluded stating "...that putrefecation is determined by living ferments".[270]
Lister was not the only surgeon who was interested in Pasteur's research.[271] Thomas Spencer Wells, who was surgeon to Queen Victoria, had emphasised the significance of Pasteur's work at a meeting of the British Medical Association in 1864,[272] stating "[By] applying the knowledge for which we are indebted to Pasteur of the presence in the atmosphere of organic germs ... it is easy to understand that some germs find their most appropriate nutriment in the secretions from wounds, or in pus, and that they so modify it as to convert it into a poison when absorbed". However, Wells did not have an experiment to demonstrate the germ theory and was unable to develop the techniques to put it into practice.[273]
Discovery
The discovery of Pasteur's work was serendipitous, as he read them during the time that he was struggling to control post-surgical infections.[274] Lister was one of the few surgeons who was able to accept Pasteur's conclusions without question. He accepted them as a simple explanation for a problem he had long experienced.[275][258] He was now convinced that infection and suppuration of wounds must be due to entry into the wound of minute living airborne creatures.[258] He recognised that contamination was the vector for infection, realising from the first that the surgeons hands, dressings and instruments would also be contaminated.[258] However, Pasteur's work could only confirm the view, which Lister had always expressed that contamination came from the air. Lister did not realise that it was not the air but the vast number of different microbial life that was responsible.[258] As Lister's work at that time was derived directly from Pasteur's work, Lister probably thought that infection of the wound was due to a single organism. He had no conception, nor indeed did anybody else of the vast number of types of germs that existed in nature.[276] The realisation that occurred after reading the papers, spurred him to determine how the hands, dressings and instruments he used could be rid of these ubiquitous organisms and how the wound could be cleared of them.[276]
Pasteur suggested three methods to eliminate microorganisms: filtration, exposure to heat, or exposure to chemical solutions. Lister was particularly interested in the efficacy of filtration and repeated many of Pasteur experiments in modified form for instruction in his class,[276] but eventually excluded the first two techniques as they were not applicable for the treatment of wounds.[271]
Lister confirmed Pasteur's conclusions with his own experiments and decided to use his findings to develop antiseptic techniques for wounds.[277]
Carbolic acid
In 1834, Friedlieb Ferdinand Runge discovered phenol, also known as carbolic acid, which he derived in an impure form from coal tar.[278] At that time, there was uncertainty between the substance of creosote – a chemical that had been used as a preservative on wood used for railway sleeper and ships since it protected the wood from rotting – and carbolic acid.[279] Upon hearing that creosote had been used for treating sewage[280] in Carlisle, Lister obtained a sample from Anderson.[281] Known as "German creosote", it was thick, smelly tarry substance.[282]
Lister's earliest experiments in antiseptic treatment were directed at treating compound fractures[283] as these were often the most fatal forms of injury.[282]
On 21 March 1865, Lister's began his first experiment with carbolic acid on a 22-year-old patient, Neil Kelly who had suffered a severe compound fracture of the leg.[284] His treatment consisted of cleaning the wound of all blood clots then apply the undiluted carbolic acid by the use of forceps across the whole wound. A piece of lint soaked in the acid was then laid on the leg, overlapping the wound and fixed by an adhesive plaster. A sheet of thin block tin or sheet lead was placed to cover the lint, to prevent the antiseptic evaporating. This was further fixed with adhesive plaster and packing was used between the limb and the splints for the purpose of soaking up any blood or discharges. A crust formed that was not removed except to apply new antiseptic.[285] While the treatment possessed many of the essential characteristics of the antiseptic dressings that Lister would subsequently introduce, it was a failure and suppuration began to occur,[285] leading to the death of the patient.
The disadvantages of the first primitive dressing consisting of lint soaked in carbolic acid, was soon apparent.[286] The German creosote was also far from ideal as it was irritating to the skin causing ulceration and then suppuration[287] that occasionally resulted in tissue necrosis. It was also almost insoluble in water.[286] Lister began to look for another source of phenol. Lister discovered[h] that Frederick Crace Calvert, an honorary chemistry professor from the Royal Manchester Institution was manufacturing small quantities of phenol at a much finer purity and managed to obtain some.[281] The phenol was in the form of small white crystals which liquified at 80 °F (27 °C)[281] and was readily soluble in a ratio of 1:20 parts of water and to any extent soluble in oil.[289] The watery solution could be used in a lotion of any strength[289] and be used for disinfection of wounds while the solution in oil that served as a reservoir of antiseptic seemed likely to provide a suitable dressing.[286] Lister began to experiment with the phenol and produced a new dressing made of a putty that consisted of carbonate of lime mixed with phenol and in boiled linseed oil in a ratio of 1:4 or 1:6.[290]
Antiseptic system



History
Hospitalism
The history of antiseptic surgery in the years before 1847, was preventing or treating infection in accidental wounds, often received in battle. [292]
1860's surgery and pathological theory
In the 1860s, Listers assumptions about surgery and theory of pathology were similar to those of his contemporaries.[293]
James Greenlees
On 12 August 1865, Lister achieved success for the first time when he used full-strength carbolic acid to disinfect a compound fracture.[281][294] He applied a piece of lint dipped in carbolic acid solution onto the wound of an 11-year-old boy, James Greenlees, who had sustained a compound fracture after a cart wheel had passed over his left leg.[295] After washing the wound with carbolic acid in linseed oil, a dressing of putty mixed with the acid was applied widely over the wound and a sheet of tin was then placed to cover the wound to protect it.[296] The putty was used to ensure the acid wasn't washed out of the wound by blood or lymph fluid.[296] The leg was then put in a splint and bandaged to hold the lot in place.[296] After four days, he renewed the pad and discovered that no infection had developed.[296] It was again dressed and left for 5 days. When the second dressing was removed, he found the skin around the wound was burnt. A dressing consisting of gauze soaked in a combination of 5% to 10% acid and olive oil was applied for a further four days. He then applied a water dressing to the wound until healing was complete.[296] After a total of six weeks, Lister was amazed to discover that the boy's bones had fused back together, without suppuration.[297]
On 19 May 1866, the first patient to use the improved method[297] was presented at Lister's accident ward with a compound fracture with extensive swelling and bruising.[298] The patient was John Hainy, a 21-year-old casting moulder in an iron foundry, who was supervising a crane when a chain broke and a metal box, containing a sand mould for an iron pipe and weighing 12 hundredweight, fell from a height of four feet and landed obliquely on his left leg.[299][300] Both of the leg bones were broken and a wound measuring 1.5 inches (38 mm) by 0.75 inches (19 mm) had bled profusely into the muscles and tissue of the leg. A secondary complication had occurred when air bubbles had mixed with the blood when the man was moved to the hospital.[299] In such a case, the normal treatment would be amputation, but Lister decided to treat the wound with phenol.[301] He squeezed the leg to remove as much air and blood as possible. Then he placed a piece of lint soaked in carbolic acid on the wound, covered by tin foil.[301] A bloody crust formed over the wound, consisting of a scab that was free of bacteria.[300] Lister saw for the first time how the scab was gradually converted into living tissue, even when new carbolic acid was being applied - something that was entirely new.[300] Unfortunately Hainy developed bed sores that became gangrenous and these were treated with nitric acid to remove the necrotic flesh and carbolic acid to sterlize the wound.[300] Hainy survived the injury. On 27 May, Lister wrote to his father expressing intense satisfaction, stating "I tried the application of carbolic acid to the wound, to prevent decomposition of the blood and to prevent the fearful mischief of supparation. It is now eight days since the accident and patient has been going exactly as though the fracture were a simple one." Two weeks later another letter followed, reporting "The great swelling has almost entirely subsided and the limb is becoming firm".[297] On 7 August 1866, Hainy was released from hospital.[300]
On a New Method of Treating Compound Fracture, Abscess
In the early months of 1867, Lister began writing up the compound fracture case histories of his experiments with carbolic acid into a new paper, in a first paper to describe his new technique of antiseptics.[302] The paper titled "On a New Method of treating Compound Fracture, Abscess, Etc., with Observations on the Conditions of Suppuration"[277] was published in The Lancet in 5 installments between March and July 1867[303] with the first installement appearing on the 10 March 1867.[302] The paper is divided into two sections, the main portion dealing with compound fractures and a short note on the treatment of abscesses.[303]
Lister's theory of inflammation was used to provide the conceptual structure in the article.[304] He stated that inflammation appeared immediately after a person was wounded and it was both necessary and dangerous. It was essentially a precursor to healing but at the same time, the fluids which flowed into the wound, were akin to dead tissue. Through the action of inflammation, putrefaction could occur.[304] Lister then described tissue healing by granulation which he believed was the likely outcome in wounds in compound fractures. Lister believed that cells in granulated tissue were remarkably active and since they were alive, were immune to putrefaction. They were also immune to secondary inflammation as they lacked the sensory nerves.[304] Lister then claimed that airborne putrefaction, "a danger that was underated", was proven by the scabs which appeared to protect small wounds from decomposition during wound healing.[305] Lister then explained how putrefaction affected tissue, that often it appeared in less than 24 hours and had an associated smell. He described the source of putrefaction and described how the "raw surface" of the wound could putrify before the granulations formed or the liquids on the surface of the granulations putrified. The liquids that was produced were extremely acrid and acted on the sensory nerves to initiate indirect inflammation and fever. This in turn led to an increase in cell turnover and resultant cellular death, increasing the quantity of putrescent material in the wound. When indirect putrefaction occurred, sloughs were produced that resulted in suppuration.[305] In the next section of the paper, Lister made his most famous declaration, namely that the decomposition of organic tissue was not caused by the gaseous components in the atmosphere but "minute particles suspended in [the air], which are the germs of various low forms of life, long since revealed by the microscope, and regarded as merely accidental concomitants of putrescence" and had been identified by Pasteur as the "essential cause" of putrefaction.[306] He described how the germs worked in the same manner as yeast that converts sugar to alcohol.[305] Lister's germs were scavengers who lived on dead tissue and he didn't see them as being parasitic on living tissue. In that respect, Lister's paper is open to many interpretations but in the context of wounds, he believed that living tissue could resist germs. He never made the distinction as to whether germs were living beings for example in erysipelas, that entered the body or were a chemical agent.[305]
In the rest of the paper, Lister describes using Carbolic Acid, along with a description of how the acid forms a dense crust that protects the wound from the ingress of germs. He then describes the outcome of his experiments on 11 patients.[307] Healing by granulation occurred in all cases except 7,10, 11 which didn't suppurate. Cases 1 and 9 did suppurate. Lister didn't regard pus as significant as it was not associated with inflammation or change in putrefaction. In essence, he had attained healing by granulation without inflammation in compound fracture cases. He believed that the elimination of suppuration wasn't a desirable therapuetic outcome, as a small amount of suppuration on a healthly granulation wasn't a cause for alarm.[307]
Antiseptic Principle of the Practice of Surgery
Within a few days of the publishing of the last part of the previous paper, Syme asked Lister to attend the British Medical Association meeting in Dublin in August 1867.[308] Lister had some difficulty preparing a new paper, the seminal "On the Antiseptic Principle in the Practice of Surgery-*" which was Listers second paper on antiseptic surgery.[308] It was later published in the British Medical Journal on 21 September 1867.[277]
Lister claimed that on basis of experiments on inflammation that the essential cause of suppuration in wounds was decomposition.[309] Several aspects of this claim needs to be examined. Firstly, it was specific to wounds only, as Lister had other views about suppuration in other sites on the body. Secondly, he stipulated that decomposition was the "essential" cause of suppuration, i.e. it wasn't the only cause. Thirdly that decomposition was the cause of pus appearing in wounds.[309] Lister's pronouncement is best described as that he had discovered the only important cause of suppuration in inflamed wounds is decomposition. Lister was specifically referring to the pathology of pus formation in inflamed tissue, the essential cause of harm in the practice of surgery.[309] His appeal to the reader, in essence to surgical consensus "To prevent the occurrence of suppuration, with all its attendant risks, was an object manifestly desirable" refers to the surgeons dread of pus appearing in an inflamed wound.[309] Lister then made a wholly inaccurate statement "...oxygen, which was universally regarded as the agent by which putrefaction was effected." when compared against other sources.[309] Lister introduced the work of Pasteur, claiming that decomposition may be avoided by a using a dressing that could destroy the minute organisms in the wound. [310] Lister decided to formulate his new surgical technique into a general principle.[309] He termed it the "antiseptic principle", thus linking its nomenclature with carbolic acid.[311] His principle was that all the local inflammatory mischief and general febrile disturbance which follow severe injuries are due to the irritating and poisoning influence of decomposing blood or sloughs.[i][310] He was stating a "great principle" – not that decomposition was the cause of disease in wounds,– it was the only cause.[310]
In the paper, Lister instructed surgeons to continue with the treatment even when suppuration appeared.[310] The reason for this was the carbolic acid induced suppuration but prevented decomposition, which was contrary to normal surgical treatment that saw suppuration as an indication that something was wrong, in Listers case essentially that the antiseptic treatment had failed.[310] He noted that he felt it necessary to affirm this position on "pathalogical principles" that granulation tissue had no inherent tendency to form pus but only did so when "subjected to a preternatural tendency". He explained that carbolic acid and decomposing substances were similar, i.e. they both caused suppuration by a chemical process but while carbolic acid only acted on the surface of the tissue to which it is applied, decomposition is a "self-propagating and self-aggravating poison". Decomposing tissue was a breeding ground for more decomposition that lead to putrefaction in the tissue surrounding it.[310]
Lister was arguing that the pus that formed by carbolic acid was acceptable as long as it wasn't accompanied with inflammation. In this respect, Listers approach to normal or abnormal healing by granulation were the same as the average surgeon of the period. Simply, that healthy healing didn't occur when inflammmation was present.[310]
Lister paid particular signifance to putrefaction, in the last part of the paper stating that decomposing wounds were the cause of disease in hospitals, which was not an uncommon belief amongst the surgical community.[312] He described how the two large wards where he offered treatement were the unhealthest in Glasgow and since the application of antiseptics, "wounds and abscesses no longer poison the atmosphere with putrid exhalations" leading to the wards completely changing their character.[312] Not a single instance of pyaemia, hospital gangrene, or erysipelas had occurred in them, since the new regime of antiseptics had began.[313] However, Lister never explained how the "putrid exhalations" led to fever.[312]
Illustrations of the Antiseptic System of Treatment in Surgery
On 21 September 1867, Lister published again in a new paper "Illustrations of the Antiseptic System of Treatment in Surgery" for The Lancet,[314] which was his third paper on antisepsis.
In the paper, Lister summarised his earlier claims and added a significant new observation on the agent of putrefaction.[312] He stated that the "character of the decomposition in a given fermentable substance is detetermined by the nature of the organism that develops in it".[312] He suggested that the cause of fermentation in food was caused by yeasts and the cause of putrefaction were possibly Vibrios.[312] At the end of the paper, he stated that on the basis of his new antiseptic theory "that a really trustworthy treatment for compound fractures and other severe contused wounds has been established for the first time, so far as I am aware, in the history of surgery".
- Sterility experiment
In October 1867, Lister decided to repeat Pasteur's experiment in a modified form, although the experiment was originally devised by the French chemist Chevreul. This was to support the germ theory and to disprove the theory that life arose from spontaneous generation.[315] Lister procured four glass flasks into which he poured his own urine. Lister then washed the necks to remove any urine and modified three of them, by extending and drawing their necks into a narrow tube that was bent at an acute angles.[276] The fourth had the neck cut short and left in a vertical position, but its diameter was reduced to a smaller size than the others. The flasks were then boiled and when the heat was withdrawn, air was allowed to rush into the flask to replace the condensed steam. The flasks were then left undisturbed in the same room, the ends of the necks, open to the air.[316] Within four days a vegetative mould appeared in the fourth flask while the other three flasks remained clear.[317] Lister would later use the flasks in demonnstrations. His dresser John Rudd Leeson described how Lister took the three flasks to London sitting on their knees, when they moved, in a specially reserved first class cabin to ensure they survived the journey.[315]
First reception of Antisepsis
Although Lister was so roundly honoured in later life, his ideas about the transmission of infection and the use of antiseptics were widely criticised in his early career.[318] On 24 August 1867 within a month of Lister's publishing his first paper on antiseptics, the editor of The Lancet and Listers nemesis James G. Wakley wrote an editorial crediting Pasteur for Lister's research and invited physicians to investigate Lister's claims and report their findings in journal.[319]
- Simpson's attack
On 21 September 1867, the Scottish obstetrician James Young Simpson, professor of medicine and midwifery at Edinburgh Uiveristy and discoverer of chloroform, published an editorial that attacked Lister in the Edinburgh Daily Review, written under the pen name "Chirurgicus", a common practice to signal a personal attack.[320] Simpson's motive for the attack was due to him trying to convince the medical community of the efficacy of his acupressure technique that used needles to halt arterial heamorrhage, which ran counter to Listers use of ligatures.[319] The editorial letter was the first of many and began a tit for tat argument that was conducted in the press over months and eventually led to acceptance of antisepsis.[citation needed]
Simpson claimed that Lister's last article was misleading[321] and accused him of plagiarising the work of the French doctor and pharmacist Jules Lemaire.[319] Lemaire had described carbolic acid as a constituent of coal tar in 1860 [322] in "Saponinated coal tar"[323] and after a long series of investigations[324] had followed up with a book in 1863 "De l'acide phénique, de son action sur les végétaux, les animaux, les ferments, les venins, les virus, les miasmes et de ses applications à l'industrie, à l'hygiène, aux sciences anatomiques et à la thérapeutique" (Carbolic acid, its action on plants, animals, ferments, venoms, viruses, miasmas and its applications to industry, hygiene, anatomical sciences and therapy) with the second edition in 1865, where he described the antiseptic power of carbolic acid.[325][326][320] While Lemaire was a believer in the germ theory and realised the causes of putrefaction, he had made no attempt to develop a process to exclude them from the wound.[322]
On 5 October 1867, Lister gave a robust reply to Simpson in a letter "On the Use of Carbolic Acid" in The Lancet, denying he had heard of Lemaire's work and argued that work had made little impact on the medical profession.[j][328] Lister went on to defend his work, stating
- "For my own part, I may say that, of all the gentlemen from Great Britain and both continents who have recently visited Glasgow, not one has ever expressed the slightest doubt that the system in question was entirely new; the novelty, I may remark, being, not the surgical use of carbolic acid (which I never claimed), but the methods of its employment with the view of protecting the reparatory processes from disturbance by external agency."
It was two weeks before Lister managed to read Lemaire's book.[329] He unsuccessfully searched Glasgow for a copy before finally discovering one in the library of Edinburgh University.[329] On the 19 October, Lister wrote a follow-up letter to The Lancet[329] and stated he didn't claim to be first physician to use carbolic acid and that he choose the acid due to its strength as an antiseptic. He also included a letter of support from a Carlisle medical student, Phillip Hair, who had studied in Paris. Hair stated he had seen no treatments there that were as effective as Lister's.[330] Lister's response angered Simpson and two weeks later on 2 November 1867, published a bitter reply, "Carbolic acid and its compounds in surgery" in the Lancet, under his own name.[331] Simpson reiterated his previous claims about Lemaire's and others' prior use of the acid, amongst them was James Spence who had used the acid to wash amputations but abandoned its use.[332] He cited a report by Sampson Gamgee who visited Paris and reported that surgeons were using a solution of 100:1 of water to acid, while Lister recommended 40:1.[330] In the last part of the letter, Simpson exposed his true motives when he compared his preferred technique of accupressure against Lister's use of ligatures. He used the work of William Pirrie, Professor of Surgery at Aberdeen University, who had used accupressure to stop pus formation during breast cancer operations, to illustrate his point, that there had been no deaths from pyaemia at the hospital, compared to the many death in Glasgow and Edinburgh.[330] Simpson was acutely embarrassed when Pirrie replied a week later in the Lancet in a small article: "On the Use of Carbolic Acid in Burns",[333] recommending its use for burn injuries and believing it proved effective in other treatments. Lister replied with a short note the 9 November[334] to ask the reader to: "to judge for themselves how far the present attack admits of justification, promising to publish additional articles on his antiseptic technique".[330]
The first experimentalist surgeon to question the validity of airborne microorganisms was the surgeon and professor of medicine at Edinburgh, John Hughes Bennett.[335] In January 1868, in a lecture for the Edinburgh Medical Journal, Bennett advanced an alternate theory in the article The Atmospheric Germ Theory[336] that was in agreement with the theories of Félix Archimède Pouchet professor of natural history at the University of Rouen, who believed in spontaneous generation of life.[337] Bennet described his own theory of molecular degeneration to explain how micro organisms transformed old tissue into new tissue by the action of molecules.[335] Bennet taught that molecules instead of cells, were the foundational building blocks of tissue and that microorganisms could be spontaneously created from different combinations of molecules. In his view, each molecule had a specific function, i.e. certain molecules were destructive to tissue, while others constructed tissue. Diseases resulted from the physical properties of the air, for example the chemical composition of air or changes in temperature.[335] Bennet believed that the germs that Pasteur's captured, couldn't be identified as organic organisms.[338] The component of the dust that Pasteur captured, were also found in minerals and they were either lint, debris from clothing or vegetable or pieces of seeds.[338] Bennet particularly disagreed about temperature. Pasteur stated that germs died when heated to 30 degrees above boiling and also from extreme cold. In the lecture, he referred to Pouchet's experiment that duplicated Pasteur's experiments, that refuted Pasteurs conclusions.[338] Bennet didn't realise that Pasteur's proved his theory by both isolating the germs and stopping them reappearing. In his experiments, Bennett reported that he "proved" that germs generate spontaneously, so one could never create a germ-free environment.[339]
It was likely that Hughes Bennett never adequately sterilized his experimental apparatus correctly.[339] On 8 November 1868, Lister gave a lecture on Germ theory, where he elaborated on the origin of germs, as a rebuttal of Bennett's theory. [340]
In 1869, at the meetings of the British Association at Leeds, Lister's ideas were mocked; and again, in 1873, the medical journal The Lancet warned the entire medical profession against his progressive ideas.[341] However, Lister did have some supporters including Marcus Beck, a consultant surgeon at University College Hospital, who not only practiced Lister's antiseptic technique, but included it in the next edition of one of the main surgical textbooks of the time.[31][342]
Lister's use of carbolic acid proved problematic, and he eventually repudiated it for superior methods. The spray irritated eyes and respiratory tracts, and the soaked bandages were suspected of damaging tissue, so his teachings and methods were not always adopted in their entirety.[343] Because his ideas were based on germ theory, which was in its infancy, their adoption was slow.[344] General criticism of his methods was exacerbated by the fact that he found it hard to express himself adequately in writing, so they seemed complicated, unorganised, and impractical.[345]
Lister left Glasgow University in October 1869[346] and was succeeded by George Husband Baird MacLeod.[347] Lister then returned to Edinburgh as successor to Syme as Professor of Surgery at the University of Edinburgh and continued to develop improved methods of antisepsis and asepsis. Amongst those he worked with there, who helped him and his work, was the senior apothecary and later MD, Alexander Gunn.[348] Lister's fame had spread by then, and audiences of 400 often came to hear him lecture. As the germ theory of disease became more understood, it was realised that infection could be better avoided by preventing bacteria from entering wounds in the first place. This led to the rise of aseptic surgery.
Edinburgh 1869–1877

When Lister attended Edinburgh, he had two primary objectives. The first was perfect the design of his dressings, the second was to improve the reliability of antiseptics by applying the technique to ever wider class of operations. The cases he selected for this were the repair of bone deformaties along with the rewiring of fractures where the union was malformed while healing.[349]
In 1870, Lister published "On the Effects of the Antiseptic System of Treatment upon the Salubrity of a Surgical Hospital".
Lister's meticulous nature became ever more apparent when he moved to work in Edinburgh and this is reflected in his casebooks for wards 4 and 5 at the infirmary.[350]
On 14 January 1871, Lister published his first details of Gauze and Spray in the British Medical Journal.[351]
In 1872 he was elected a member of the Aesculapian Club.[352]
Sprays

Therefore, Lister tested the results of spraying instruments, the surgical incisions, and dressings with a solution of carbolic acid. Lister found that the solution swabbed on wounds remarkably reduced the incidence of gangrene.[317]
London 1877–1900

On 10 February 1877, Scottish surgeon, Sir William Fergusson Chair of Systematic Surgery at King's College Hospital, died.[353] On 18 February, in reply to a tentative approach from a representative of Kings College, Lister stated that he would be willing to accept the Chair[354] on the proviso that he could radically reform the teaching there.[354] There was no doubt that Lister mission was both evangelical and apostolic and this was his true purpose in moving to London.[355]
British surgeon John Wood was originally next in line and was elected to the chair.[356] Wood was hostile to Lister obtaining the chair.[356] On 8 March 1877, in a private letter to an associate, Lister contrasted their differing teaching methods and stated in no uncertain terms his opinion of Fergusson, "The mere fact of Fergusson having held the clinical chair is surely a matter of no great moment".[357] In a comment to another colleague, Lister stated that his goal in taking the appointment was "the thorough working of the antiseptic system with a view to its diffusion in the Metropolis".[357] At a memorial held by his students to persuade him to remain, Lister criticised London teaching. His impromptu speech was heard by a reporter, that ensured it was published in the London and Edinburgh newspapers.[358] This jeopardised Lister's position, as word reached the governing council at King's College, who awarded the chair to John Wood, a few weeks later.[359]
However, negotiations were renewed in May and he was finally elected on 18 June 1877 to a newly created Chair of Clinical Surgery.[30] The second Clinical Surgery Chair was created specifically for Lister, as the hospital feared the negative publicity that would have resulted had Lister not been elected.[360]
Moving to Regents Park
On 11 September 1877, Joseph and Aggie moved to London[361] and the couple found a house at 12 Park Crescent, Regent's Park.[362] Lister began teaching on the first day of October.[361] The hospital made it mandatory that all students should attend Lister's lecturers.[361] Attendance was small compared to the four hundred who would regularly attend his classes in Edinburgh.[361] Lister's conditions of employment were met, but he was only provided with 24 beds, instead of the 60 beds that he was used to in Edinburgh.[363] Lister stipulated that he should be able to bring from Edinburgh four people who would constitute the core of his new staff at the hospital.[364] These were Watson Cheyne who became his assistant surgeon, John Stewart, an anatomical artist and senior assistant, along with W. H. Dobie and James Altham who were Lister's dressers (surgical assistants who dressed wounds).[364] There was considerable friction at Lister's first lecture, both from students who heckled him[363] and staff. Even the nurses were hostile.[364] This was clearly illustrated in October 1877[365] when a patient, Lizzie Thomas, who travelled from Edinburgh Royal Infirmary to be treated for a Psoas abscess, was not admitted due to not having the correct paperwork.[366] Lister could hardly believe that such a lack of sympathy from imperious nurses could exist.[367] More so, such a state of mind was a real danger to his patients, because his system depended on loyal staff to carry out the preparations for antiseptic surgery.[367]
Introductory address
On 1 October 1877, Lister held the customary introductory address, in essence his inaugural lecture in London, with the subject, "The nature of fermentation".[368] Lister described the fermentation of milk and explained how putrefaction was caused by fermentation of blood[369] and, in the process, tried to prove that all fermentation was due to microorganisms. For his demonstration he used a series of test tubes containing milk that were loosely covered with glass caps.[355] Although air had entered the test tubes and the milk had not decomposed demonstrated that air was responsible for fermentation.[355] The experiment had two conclusions, first that unboiled milk had no tendency to ferment and secondly that an organism that Lister had isolated,[370] Bacterium lactis was the cause of lactic acid fermentation.[355]
The address was badly received.[363] In defence, John Stewart described it as: "a brilliant and most hopeful beginning of what we regarded as a campaign in the enemy's country... There seemed to be a colossal apathy, an inconceivable indifference to the light which, to our minds, shone so brightly, a monstrous inertia to the force of new ideas."[371]
Wiring of fractured patellas
In October 1877, Lister performed an operation on a patient, Francis Smith, that was not considered life-threatening.[372][373] The open operation on a fractured patella, in front of 200 students, involved wiring the two fragments together[373] and was likely the first case in which a healthy knee-joint was ever opened.[374]
In 1881 Lister was elected President of the Clinical Society of London.[375]
In October 1883, St Clair Thomson gathered together Lister's first seven patients who had knee operations for examination at the Medical Society of London meeting.[374]
He also developed a method of repairing kneecaps with metal wire and improved the technique of mastectomy. He was also known for being the first surgeon to use catgut ligatures, sutures, and rubber drains, and developing an aortic tourniquet.[376][8] He also introduced a diluted spray of carbolic acid combined with its surgical use, however he abandoned the carbolic acid sprays in the late 1890s after he saw it provided no beneficial change in the outcomes of the surgeries performed with the carbolic acid spray. The only reported reactions were minor symptoms that did not affect the surgical outcome as a whole, like coughing, irritation of the eye, and minor tissue damage among his patients who were exposed to the carbolic acid sprays during the surgery.[377]
Reception abroad (1870–1876)
In 1869, Mathias Saxtorph from the University of Copenhagen visited Lister in Glasgow to adopt his methods.[378] In July 1870, Saxtorph recognised Lister's technique as being effective in a letter to Lister where he stated:
The Frederick Hospital, to which I am head surgeon is a very old building and I have 150 patients in the surgical wards. Foremerly, there used to be every year several cases of death from pyaemia, sometime, arising from the most trivial injuries. Now, I have had the satisfaction that not a single case of pyaemia has occurred since I came home last year, which result is certainly owing to the introduction of your antiseptic treatment.[379]
Germany
The first use of Lister's method in Germany was by Karl Thiersch in Leipzig in 1867.[380] Thiersch who practiced Lister's approach since its introduction, never published his results but taught Lister's methods to his students.[380] His house surgeon Hermann Georg Joseph, tested it on 16 patients who had abscesses, with favourable results.[378] Joseph wrote a thesis on his results proving the value of the Lister method, which was presented in Leipzig the following year.[381] In January 1870, Heinrich Adolf von Bardeleben presented a paper to the Berlin Medical Society that described the results but provided no statistical evaluation of those results.[381]
The adoption of Listerism on the European continent was halted during the Franco-Prussian War, but it became the greatest opportunity to advance Lister's ideas.[378] At the start of the war, Lister had written a pamphlet known as "A Method of Antiseptic Treatment Applicable To Wounded Soldiers in the Present War" that described a simplified technique of antiseptic that could be used on the battlefield and military hospital.[382] The pamphlet was immediately translated into German, however it never made a material difference.[381]
By far the most important advocate for Lister's antiseptic system in Germany was the surgeon and Osteotomy specialist,[383] Richard von Volkmann who taught at the University of Halle.[384][385] In August 1870, he became surgeon-general during the Franco-Prussian War and was responsible for 12 army hospitals and 1442 beds.[385] When he returned to his own hospital in the winter of 1871, he found large numbers of patients with infectious diseases throughout the ward.[385] He wrote of the experience:
The mortality after large amputations and complicated fractures grew year by year. In the summer of 1871, during my absence on the battlefield, the clinic was crowded by a large amount of injured. For eight months, in the winter 1871 to 1872, the numbers of blood poisoning and rose disease victims were so great, that I considered applying for a temporary closure of the facility. Without a morgue, the dead stayed in the cellar beneath the wards
In 1872, Volkmann sent his assistant Max Schede to visit Lister at his clinic, to learn his new techniques.[385] Once Schede returned in the autumn of 1872, Volkmann began to use Lister's new techniques.[385] On 16 February 1873, in a letter to Theodor Billroth, Volkmann wrote:
since autumn of last year (1872), I have been experimenting with Lister's method... Already, the first trials in the old 'contaminated' house, show wounds healing, uneventful, without fever and pus.[385]
In April 1874, Volkmann presented a lecture with the title: "About antiseptic occlusive bandages and their influence on the healing process of wounds" where he detailed the influence of Lister.[385] The lecture became famous in Germany, to such an extent that Lister's antiseptics were established in Germany, faster than in any other developed country. At the German Congress of Surgery, the members were so enthused with the results of Lister's work, that they invited him to visit Germany and see first hand the results of his work.[386] Lister decided to accept the invitation of a continental tour.[387]
In the spring of 1875, Lister along with Agnes, his sister-in-law and two nieces left Edinburgh.[387] The group spent several weeks in a tour that began in Cannes in France, visited the several cities in Italy and a finished with a four-day visit to Venice.[387] The first place in Germany that Lister visited was the "Allgemeines Krankenhaus" (general hospital) in Munich, which was run by Nussbaum.[388] A celebratory dinner was held in Munich for Lister, with seventy guests.[386] However, it was in Leipzig where Lister received his most glorious reception. A banquet was held with between three and four-hundred guests present, led by MC Karl Thiersch.[386] Lister then visited Volkmann in Halle before visiting Berlin, where the group was entertained by Heinrich Adolf von Bardeleben, who worked at the Charité hospital and was one of the earliest adopters of antiseptics.[381]
Later life

In December 1892, Lister attended the celebration in honour of the 70th birthday of Pasteur at the Sorbonne in Paris, [389] The theatre, designed to hold 2500 people was crowded and included the university governing staff, ministers of state, ambassadors, the President of France Sadi Carnot and representatives from the Institut de France.[390] At 10.30am, Pasteur entered beginning the ceremony. Lister, invited to give the address, received a great ovation when he stood up. In his speech he spoke about the debt that he and surgery owned to Pasteur.[390] In a scene that was captured later by Jean-André Rixens, Pasteur strode forward and kissed Lister on both cheeks.[390] In January 1896, Lister was present when Pasteur's body was laid in his tomb at the Pasteur Institute.[390]
In 1893, four days into their spring holiday in Rapallo, Italy, Agnes Lister died from acute pneumonia.[391] While still responsible for the wards at Kings College Hospital, Lister's private practice ceased along with an appetite for experimental work. Social gatherings were severely curtailed.[392] Studying and writing lost appeal for him and he sank into religious melancholy.[392] On 31 July 1895, Lister retired from Kings College Hospital.[393] Lister was presented with a portrait painted by Scottish artist John Henry Lorimer, in a small presentation, held in recognition of the affection and esteem that felt by his colleagues.[393]
Despite suffering a stroke, he still came into the public light from time to time. He had for several years been a Surgeon Extraordinary to Queen Victoria, and from March 1900 was appointed the Serjeant Surgeon to the Queen,[394] thus becoming the senior surgeon in the Medical Household of the Royal Household of the sovereign. After her death the following year, he was re-appointed as such to her successor, King Edward VII.[395]
On 24 June 1902, with a 10-day history of appendicitis with a distinct mass on the right lower quadrant, Edward was operated on by Sir Frederick Treves two days before his scheduled coronation.[396] Like all internal surgery at the time, the appendectomy needed by the King still posed an extremely high risk of death by post-operational infection, and surgeons did not dare operate without consulting Britain's leading surgical authority.[397] Lister obligingly advised them in the latest antiseptic surgical methods (which they followed to the letter), and the King survived, later telling Lister, "I know that if it had not been for you and your work, I wouldn't be sitting here today."[398]
In 1903, Lister left London to live in the coastal village of Walmer at Park House.[35]
Death
Lord Lister died on 10 February 1912 at his country home at the age of 84.[399] The first part of Lister's funeral was a large public service held at Westminster Abbey, which took place at 1.30pm on 16 February 1912.[400] His body was moved from his house and taken to The Chapel of St. Faith and a wreath of orchids and lilies was placed by the German ambassador Count Paul Wolff Metternich on behalf of the German Emperor Wilhelm II.[400] Before the start of the service, Frederick Bridge played the music of Henry Purcell, the funeral march by Chopin and Beethoven's Tres Aequili.[400] The body was then placed on a high catafalque, where his Order of Merit, Prussian Pour le Mérite and Grand Cross of the Order of the Dannebrog were placed.[400] It was then borne by several pallbearers including John William Strutt, Archibald Primrose, Rupert Guinness, Archibald Geikie, Donald MacAlister, Watson Cheyne, Godlee and Francis Mitchell Caird[400] where the catafalque was conveyed to Hampstead Cemetery in London,[399] reaching it at 4pm.[400] Lister's body was then buried in a plot in the south-east corner of central chapel, attended by a small group of his family and friends. Many tributes from learned societies all over the world were published in The Times on that day.[400] A memorial service was held in St Giles' Cathedral in Edinburgh on the same day.[400] Glasgow University held a memorial service in Bute Hall on 15 February 1912.[400]
A marble medallion of Lister was placed in the north transept of Westminster Abbey, that sits alongside four other noted men of science, Darwin, Stokes, Adams, and Watt.[399]
Lister Memorial Fund
Following his death, the Lord Lister Memorial Fund was established by the Royal Society as a public subscription to raise monies for the public good in honour of Lord Lister.[401] It led to the founding of the Lister Medal, considered the most prestigious prize that can be awarded to a surgeon.
Awards and honours
On 26 December 1883, Queen Victoria created Lister a baronet, of Park Crescent in the parish of St Marylebone in the county of Middlesex.[402]
In 1885, he was awarded the Pour le Mérite, the highest Prussian order of merit.[403] The order was restricted to 30 living Germans and as many foreigners.[403]
On 8 February 1897, he was further honoured when Her Majesty raised him to the peerage as Baron Lister, of Lyme Regis in the county of Dorset.[404][405]
In the 1902 Coronation Honours list published on 26 June 1902 (the original day of King Edward VII's coronation),[406] Lord Lister was appointed a privy counsellor and one of the original members of the new Order of Merit (OM). He received the order from the King on 8 August 1902,[407][408] and was sworn a member of the Privy Council at Buckingham Palace on 11 August 1902.[409]
In December 1902, the King of Denmark bestowed upon Lister the Knight of the Grand Cross of the Order of the Dannebrog,[410] an Order of chivalry that gave him more pleasure than any of his later honours.[410]
Medals
Throughout his life, Lister was awarded a number of medals for his achievements.
In May 1890, Lister was awarded the Cameron Prize for Therapeutics of the University of Edinburgh,[403] that included the delivery of a short oration or lecture, that was held at the Synod Hall in Edinburgh.[411]
Academic societies
Lister was a member of the Royal College of Surgeons of England between 1880 and 1888.
In 1877, Lister was awarded the Cothenius Medal of the German Society of Naturalists.[412] In 1886, he was elected vice president of the college, but declined the nomination for office of president, as he wished to devote his remaining time to further research.[413] In 1887, Lister presented the Bradshaw lecture with a lecture titled "On the Present Position of Antiseptic Treatment in Surgery".[30] In 1897, Lister was awarded the College Gold Medal, their highest honour.[30]
Lister was elected to the Royal Society in 1860.[30] He served as a trustee on the Royal Society council between 1881 and 1883.[30] Ten years later, in November 1893 Lister was elected for two years, to the position of foreign secretary of the society, succeeding the Scottish geologist Sir Archibald Geikie.[414] In 1895, he was elected president of the Royal Society[415] succeeding Lord Kelvin. He held the position until 1900.[30]
In March 1893, Lister received a telegram from Pasteur, Félix Guyon and Charles Bouchard that informed him he had been elected an associate of the Academie des Sciences.[416]
Monuments and legacy
In 1903, the British Institute of Preventitive Medicine was renamed Lister Institute of Preventitive Medicine in honour of Lister.[417] The building, along with another adjacent building, forms what is now the Lister Hospital in Chelsea, which opened in 1985. The building at Glasgow Royal Infirmary which houses the cytopathology, microbiology, and pathology departments was named in Lister's honour to recognise his work at the hospital.[418] The Lister Hospital in Stevenage, Hertfordshire is named after him.[7]
Lister's name is one of 23 people featured on the frieze of the London School of Hygiene & Tropical Medicine[419] – although the committee which chose the names to include on the frieze did not provide documentation about why certain names were chosen and others were not.[420]
Lister is one of only two surgeons in the United Kingdom who have the honour of having a public monument in London, Lister and John Hunter. The statue of Lister, created by Thomas Brock in bronze in 1924, stands at the north end of Portland Place.[421] There is a bronze statue of Lister, mounted on a granite base in Kelvingrove Park, Glasgow that was sculpted by George Henry Paulin in 1924. It sits next to the statue of Lord Kelvin.[422]
The Discovery Expedition of 1901–1904 named the highest point in the Royal Society Range, Antarctica, Mount Lister.[423]
In 1879, Listerine antiseptic (developed as a surgical antiseptic but nowadays best known as a mouthwash) was named by its American inventor, Joseph Lawrence, to honour Lister.[424]
Microorganisms named in his honour include the pathogenic bacterial genus Listeria named by J. H. H. Pirie, typified by the food-borne pathogen Listeria monocytogenes, as well as the slime mould genus Listerella, first described by Eduard Adolf Wilhelm Jahn in 1906.[425]
Lister is depicted in the Academy Award-winning 1936 film The Story of Louis Pasteur, by Halliwell Hobbes. In the film, Lister is one of the beleaguered microbiologist's most noted supporters in the otherwise largely hostile medical community, and is the key speaker in the ceremony in his honour.
Two postage stamps were issued in September 1965 to honour Lister on the centenary of his antiseptic surgery at the Glasgow Royal Infirmary of Greenlees, the first ever recorded instance of such treatment.[426]
Gallery
-
Lister Building, Glasgow Royal Infirmary
-
Lister Room, Royal College of Physicians and Surgeons of Glasgow
-
Lister Frieze, Polyclinic Umberto I hospital in Rome. The tympanum sculptures show Lister operating
-
Lister's name on the London School of Hygiene & Tropical Medicine, in Keppel Street
-
Coast House, Deal, with its blue plaque to Lister.
-
Lister's hearse prior to his funeral service at Westminster Abbey
-
Lord Lister Memorial in Portland Place by Sir Thomas Brock in bronze, 1924
-
Plaque commemorating Joseph Lister on the facade of the polyclinic in Vienna
-
Plaque at 12 Park Crescent, Regent's Park, London
-
Photogravure plaque, Wellcome Institute, London
Bibliography
Papers
- Lister BJ (1878). On the lactic fermentation and its bearings on pathology. London: J.E. Adlard. OCLC 30715167.
See also
- Discoveries of anti-bacterial effects of penicillium moulds before Fleming
- Joseph Sampson Gamgee
- Listerine, a mouthwash named after Lister
- Hector Charles Cameron
- Watson Cheyne
- Museum of Health Care
- List of presidents of the Royal Society
Notes
- ^ Fermentation was the word Lister used for the putrefactive process of sepsis that we might now describe as wound infection[5]
- ^ An obsolete medical term that describes a morbid material substance that acts as the immediate cause of a disease
- ^ The webbed feet of the hind leg of a chloroform frog.
- ^ Known as Vascular Tone, that is defined as the degree of constriction experienced by a blood vessel relative to its maximally dilated state[169]
- ^ Defined as traumatic injury, sudden physical injury caused by an external force, which does not rise to the level of major trauma
- ^ The Latin name for Blood plasma
- ^ The article as it appears in the Collected Papers is reprinted from the third edition published in 1883
- ^ Likely from Anderson[288]
- ^ Emphasis is present in the original
- ^ Contrary to Lister's appraisal, there was exited interest in Lemaire's work in France.[327]
References
Citations
- ^ a b Cartwright 2023.
- ^ a b Simmons 2002, pp. 94–99.
- ^ Moynihan 1927.
- ^ Ford 1928.
- ^ Richardson 2013a.
- ^ Gaw 1999, p. 144.
- ^ a b c d e f g Pitt & Aubin 2012.
- ^ a b c d e f g h i j k l Cope 1967.
- ^ a b Cameron 1949, pp. 21–22.
- ^ Godlee 1924, p. 5.
- ^ Fitzharris 2018, p. 20.
- ^ Cameron 1949, p. 20.
- ^ a b c d Cameron 1949, p. 18.
- ^ Godlee 1924, p. 1.
- ^ Goody 1973, p. 55.
- ^ Cameron 1949, p. 19.
- ^ Lister 1893, p. 347.
- ^ Davidson 2011.
- ^ a b c d e Clark 1920.
- ^ Chapman 2016, p. 376.
- ^ a b Godlee 1924, p. 4.
- ^ a b c Plarr's 2006.
- ^ The Court Magazine and Monthly Critic 1845, p. 11.
- ^ a b Dormandy 2004, p. 262.
- ^ Shaun 2009.
- ^ Nature 1908.
- ^ Ogilvie & Harvey 2003, p. 93.
- ^ Beck, Wells & Chalkley 1888, p. 331.
- ^ Gardner-Thorpe 2001, p. 9.
- ^ a b c d e f g h i j k l m n o Plarr's 2008.
- ^ a b Sakula 1985.
- ^ a b Godlee 1924, p. 7.
- ^ Wrench 1913, p. 23.
- ^ Powell 1973, pp. 50–57.
- ^ a b c d Lawrence 2004.
- ^ a b c d e f g h i j k l m n Godlee 1924, p. 16.
- ^ a b c d Godlee 1924, pp. 12–15.
- ^ Godlee 1924, p. 2.
- ^ Godlee 1924, p. 14.
- ^ Bankston 2005, p. 17.
- ^ a b c Lister 1859a, p. 26.
- ^ Fitzharris 2018, p. 29.
- ^ a b Fisher 1977, p. 34.
- ^ a b c d Lister 1859a.
- ^ Cameron 1949, p. 24.
- ^ a b Bonner 2000, p. 194.
- ^ a b c Fisher 1977, p. 38.
- ^ Squire 1888.
- ^ a b c d e f g h i j k l m Richardson & Rhodes 2013.
- ^ Fitzharris 2018, p. 40.
- ^ Fisher 1977, p. 43.
- ^ Fitzharris 2018, p. 55.
- ^ Fitzharris 2018, p. 44.
- ^ Fisher 1977, pp. 44–45.
- ^ Fisher 1977, p. 46.
- ^ Lister 1900, p. 6.
- ^ Wellcome Historical Medical Museum 1927, p. 134.
- ^ a b Fisher 1977, p. 49.
- ^ Walshe 1846.
- ^ a b c d e f g Wrench 1913, p. 32.
- ^ Erichsen 1853.
- ^ Plarr's 2012.
- ^ a b c d e f g Richardson 2013b.
- ^ Godlee 1924, p. 562.
- ^ a b c d Lister 1900, p. 7.
- ^ a b c d e Glass 2014.
- ^ a b Lister 1900, p. 9.
- ^ a b c Rose 2014.
- ^ Shepard 1968.
- ^ a b Lister 1853a.
- ^ a b Wrench 1913, p. 30.
- ^ a b c d Godlee 1924, p. 22.
- ^ Wrench 1913, p. 29.
- ^ a b c d e Howard 2013, p. 193.
- ^ Wrench 1913, p. 31.
- ^ Lister 1853b.
- ^ a b Godlee 1924, p. 23.
- ^ Godlee 1924, pp. 23–24.
- ^ Lister 1853b, pp. 6–7.
- ^ a b c d Godlee 1924, p. 24.
- ^ a b c d e f Godlee 1924, p. 25.
- ^ a b c d Fitzharris 2018, p. 74.
- ^ a b c Godlee 1924, pp. 28–29.
- ^ a b c d e Gaw 1999, p. 3.
- ^ Cameron 1949, p. 27.
- ^ Nature 1880.
- ^ Cohen 1956, pp. 645–650.
- ^ a b Moore & Hunter 2009.
- ^ Turk 1994.
- ^ Freeman 1989, pp. 320–321.
- ^ a b c d e Geison 1972.
- ^ Gaw 1999, p. 19.
- ^ Noble 1960, p. 24.
- ^ a b c Gaw 1999, p. 4.
- ^ Blore 1920, p. 350.
- ^ a b c d Plarr's 2013.
- ^ Syme 1824.
- ^ Harris 1956.
- ^ Cameron 1949, p. 33.
- ^ a b "Joseph Lister". The Royal College of Surgeons of Edinburgh Library and Archive. The Royal College of Surgeons of Edinburgh. Retrieved 26 January 2021.
- ^ LeFanu 1974, p. 1111.
- ^ a b Noble 1960, pp. 30–31.
- ^ Godlee 1924, p. 33.
- ^ Godlee 1924, p. 30.
- ^ a b Godlee 1924, p. 34.
- ^ Godlee 1924, p. 35.
- ^ a b Fitzharris 2018, p. 112.
- ^ Fitzharris 2018, p. 113.
- ^ a b c Fitzharris 2018, p. 114.
- ^ a b Godlee 1924, pp. 38–39.
- ^ a b Noble 1960, p. 38
- ^ a b Godlee 1924, p. 41.
- ^ Godlee 1924, p. 51.
- ^ a b c Godlee 1924, p. 53.
- ^ a b c Godlee 1924, p. 52.
- ^ a b Finlayson 1900, p. 10.
- ^ Cameron 1949, p. 40.
- ^ a b Fisher 1977, p. 72.
- ^ Fisher 1977, p. 73.
- ^ a b Godlee 1924, p. 67.
- ^ a b c d Bonnin & LeFanu 1967.
- ^ Fitzharris 2018, p. 117.
- ^ a b c d e f Fitzharris 2018, p. 119.
- ^ Godlee 1924, p. 42.
- ^ a b Godlee 1924, p. 54.
- ^ a b Noble 1960, p. 39
- ^ Godlee 1924, pp. 54–58.
- ^ a b c Godlee 1924, p. 58.
- ^ a b c d e Howard 2013, p. 192.
- ^ a b Fitzharris 2018, p. 123.
- ^ Fitzharris 2018, p. 124.
- ^ a b c Wrench 1913, p. 52.
- ^ Wrench 1913, p. 49.
- ^ a b Noble 1960, p. 42.
- ^ Godlee 1924, p. 43.
- ^ a b Fisher 1977, p. 70.
- ^ Cameron 1949, p. 41.
- ^ Fisher 1977, p. 89.
- ^ a b c d e Fisher 1977, p. 71.
- ^ Godlee 1924, pp. 43–45.
- ^ Lister 1900, p. 12.
- ^ a b Godlee 1924, p. 44.
- ^ Noble 1960, p. 41.
- ^ a b Fisher 1977, p. 86.
- ^ a b c Fisher 1977, p. 84.
- ^ a b Fisher 1977, p. 91.
- ^ a b c d e f Howard 2013, p. 195.
- ^ a b Bulloch 1927, p. 531.
- ^ a b c d e f Fisher 1977, p. 92.
- ^ "Part Fourth, Half-yearly report on physiology". The British and Foreign Medico-Chirurgical Review or Quarterly Journal of Practical Medicine and Surgery. XXVI. London: John Churchill: 234. July 1860.
- ^ Scudamore C (1824). An essay on the blood [electronic resource] : comprehending the chief circumstances which influence its coagulation; the nature of the buffy coat; with a concise medical view of the state of the blood in disease; and an account of the powers of a saturated solution of alum, as a styptic remedy in haemorrhage. London: Joseph Mallet. pp. exp 15- exp 26.
- ^ Brücke EW (January 1857). "An Essay on the Cause of the Coagulation of the Blood". The British and Foreign Medico-Chirurgical Review. 19 (37): 183–212. PMC 5183388. PMID 30163999.
- ^ a b c Godlee 1924, p. 45.
- ^ Lister 1858a.
- ^ a b c Best 1970, p. 11.
- ^ Lister 1900, p. 5.
- ^ a b Lister 1853c.
- ^ Godlee 1924, p. 64.
- ^ Godlee 1924, p. 26.
- ^ a b c d e f g h Howard 2013, p. 194.
- ^ Godlee 1924, p. 46.
- ^ a b c Fisher 1977, p. 87.
- ^ Rudolf 1933, p. 24.
- ^ Lister 1858b.
- ^ a b c Best 1970, p. 23.
- ^ Carpenter, William Benjamin (1853). Principles of Human Physiology (4th ed.). Philadelphia: Lea and Blanchard. p. 309.
- ^ Lister 1858b, pp. 610–611.
- ^ Lister 1858b, pp. 609–617.
- ^ Chatziprodromou I, Tricoli A, Poulikakos D, Ventikos Y (January 2007). "Haemodynamics and wall remodelling of a growing cerebral aneurysm: A computational model". Journal of Biomechanics. 40 (2): 412–426. doi:10.1016/j.jbiomech.2005.12.009. PMID 16527284.
- ^ Lister 1858b, p. 625.
- ^ Jones TW (January 1853). "Observations on the State of the Blood and the Blood-Vessels in Inflammation". Journal of the Royal Society of Medicine. MCT-36 (1): 391–402. doi:10.1177/095952875303600119. PMC 2104154. PMID 20896014.
- ^ Best 1970, p. 5.
- ^ a b Lister 1858c.
- ^ a b c d Fisher 1977, p. 88.
- ^ a b c d e Godlee 1924, p. 50.
- ^ Harless 1846.
- ^ Lister 1858d.
- ^ Bohrer D (2012). Sources of Contamination in Medicinal Products and Medical Devices. John Wiley & Sons. p. 4. ISBN 978-0470487501.
- ^ a b Fitzharris 2018, p. 120.
- ^ a b c d Godlee 1924, p. 47.
- ^ Wrench 1913, p. 53.
- ^ a b c d Godlee 1924, p. 48.
- ^ a b c Godlee 1924, p. 68.
- ^ a b Lister 1858f.
- ^ Godlee 1924, pp. 72–73.
- ^ Lister 1858f, p. 898.
- ^ Lister 1858f, p. 905.
- ^ a b c d Fisher 1977, p. 93.
- ^ Lister 1858g.
- ^ Lister J (December 1858). "Example of mixed Aortic Aneurysm". Edinburgh Medical Journal. 4: 546.
- ^ Rudolf 1933, pp. 12–19.
- ^ a b c Lister 1858e.
- ^ Smith 2020, p. 85.
- ^ Pflüger 1857.
- ^ Godlee 1924, p. 297.
- ^ a b c d e Smith 2020, p. 86.
- ^ a b Howard 2013, p. 196.
- ^ Meissner G (1857). "Zeitschrift für rationelle Medicin". Zeitschrift für rationelle Medicin (in German). 8: 364–366. ISSN 0259-7233.
- ^ Neckel PH (10 October 2022). "Annotated translation of Georg Meissner's first description of the submucosal plexus". Neurogastroenterology & Motility. 35 (3). University of Tübingen: e14480. doi:10.1111/nmo.14480. PMID 36210765. S2CID 252779274.
- ^ Norberg KA (September 1964). "Adrenergic innervation of the intestinal wall studied by fluorescence microscopy". International Journal of Neuropharmacology. 3 (4): 379–382. doi:10.1016/0028-3908(64)90067-x. PMID 14334869.
- ^ a b Lister 1859b.
- ^ a b c Godlee 1924, pp. 78–79.
- ^ Godlee 1924, pp. 77.
- ^ "James Lawrie". International Story. University of Glasgow. 26 February 2013. Retrieved 23 November 2021.
- ^ a b Godlee 1924, p. 80.
- ^ "Editors section". Glasgow Herald. Glasgow: George Outram & Co. 18 January 1860. p. 2.
- ^ Godlee 1924, p. 81.
- ^ Godlee 1924, p. 89.
- ^ Godlee 1924, p. 90.
- ^ Fisher 1977, p. 99.
- ^ Fisher 1977, pp. 98–100.
- ^ a b c d e Cameron 1949, p. 53.
- ^ Wrench 1913, pp. 61–62.
- ^ Cameron 1949, p. 52.
- ^ Cameron 1949, p. 54.
- ^ a b Fisher 1977, p. 101.
- ^ a b c d Fisher 1977, p. 102.
- ^ a b Fitzharris 2018, p. 135.
- ^ a b c Godlee 1924, p. 93.
- ^ a b c d e Fisher 1977, p. 109.
- ^ Summerly PA (2003). Visual pathology: a case study in late nineteenth century clinical photography in Glasgow, Scotland (PDF) (Phd Thesis). University of Glasgow. p. 153. Retrieved 15 September 2023.
- ^ Godlee 1924, p. 95.
- ^ Jenkinson J, Moss MS, Russell I (1994). The Royal : the history of Glasgow Royal Infirmary, 1794-1994. Glasgow: Bicentenary Committee on behalf of Glasgow Royal Infirmary NHS Trust. p. 107. ISBN 9780852614334.
- ^ Godlee 1924, p. 94.
- ^ Holmes T, ed. (1862). A System of Surgery, Theoretical and Practical, in treatises by various authors. London: Parker, Son and Bourn.
- ^ a b c Fisher 1977, p. 108.
- ^ Lister & Cameron 1909a, pp. 135–175.
- ^ Buxton 1924, p. 10.
- ^ Godlee 1924, p. 103.
- ^ Lister & Cameron 1909a, p. 162.
- ^ a b c d e Fisher 1977, p. 110.
- ^ Lister & Cameron 1909b, pp. 378–417.
- ^ a b c Godlee 1924, p. 97.
- ^ Godlee 1924, p. 96.
- ^ Fisher 1977, p. 130.
- ^ Louis 2010.
- ^ Godlee 1924, pp. 100–101.
- ^ a b c d e Lister 1863.
- ^ Fisher 1977, p. 112.
- ^ Fisher 1977, p. 113.
- ^ a b Godlee 1924, p. 118.
- ^ "On the excision of the wrist". The Retrospect of Medicine. LXIV: 180. 1872.
- ^ a b Godlee 1924, p. 119.
- ^ Lister 1865.
- ^ a b c Fisher 1977, p. 114.
- ^ a b Godlee 1924, p. 108.
- ^ Godlee 1924, pp. 109–110.
- ^ a b c d Fisher 1977, p. 115.
- ^ a b Godlee 1924, p. 111.
- ^ a b Fisher 1977, p. 116.
- ^ Wrench 1913, p. 57.
- ^ a b Fisher 1977, p. 117.
- ^ a b c d Fisher 1977, p. 118.
- ^ Fisher 1977, p. 119.
- ^ a b Fisher 1977, p. 121.
- ^ Cheyne 1925, p. 9.
- ^ Noble 1960, p. 457.
- ^ a b c d e Cameron 1949, p. 60.
- ^ a b Godlee 1924, p. 162.
- ^ Nuland 2011, p. 363.
- ^ Wrench 1913, p. 97.
- ^ Pasteur 1861a.
- ^ a b c d e f g DePaolo 2016, p. 14.
- ^ a b DePaolo 2016, p. 11.
- ^ Pasteur 1863a.
- ^ Pasteur 1857.
- ^ Pasteur 1860.
- ^ Pasteur 1861b.
- ^ Pasteur 1863b.
- ^ Wrench 1913, p. 98.
- ^ a b Fitzharris 2018, p. 159.
- ^ Simmons 2002, p. 96.
- ^ Worboys 2000, p. 79.
- ^ DePaolo 2016, p. 17.
- ^ Cartwright 1977, p. 144.
- ^ a b c d Cameron 1949, p. 61.
- ^ a b c Lister 1867a.
- ^ Tyman 1996, p. 1.
- ^ Schorlemmer C (30 March 1884). "The History of Creosote, Cedriret and Pittacal". Journal of the Society of Chemical Industry. 4: 152–157.
- ^ Pitt D, Aubain JM (October 2012). "Joseph Lister: father of modern surgery". Canadian Journal of Surgery. 55 (5): E8–9. doi:10.1503/cjs.007112. PMC 3468637. PMID 22992425.
- ^ a b c d Gaw 1999, p. 29.
- ^ a b Godlee 1924, p. 182.
- ^ Cameron 1927, p. 15.
- ^ Fisher 1977, p. 135.
- ^ a b Godlee 1924, pp. 182–183.
- ^ a b c Godlee 1924, p. 183.
- ^ Cameron 1949, p. 62.
- ^ Fitzharris 2018, p. 134.
- ^ a b Cameron 1949, p. 63.
- ^ Godlee 1924, p. 184.
- ^ "The Gross Clinic". medhum.med.nyu.edu. Retrieved 12 November 2020.
- ^ Cartwright 1968, p. 77.
- ^ Lawrence & Dixey 1992.
- ^ Lister 1867b, p. 4.
- ^ Gaw 1999, pp. 30.
- ^ a b c d e Fisher 1977, p. 136.
- ^ a b c Cameron 1949, p. 64.
- ^ Cameron 1949, p. 49.
- ^ a b Wrench 1913, p. 110.
- ^ a b c d e Fisher 1977, p. 138.
- ^ a b Wrench 1913, p. 111.
- ^ a b Fisher 1977, p. 144.
- ^ a b Godlee 1924, p. 188.
- ^ a b c Lawrence & Dixey 1992, p. 163.
- ^ a b c d Lawrence & Dixey 1992, p. 164.
- ^ Fitzharris 2018, p. 169.
- ^ a b Lawrence & Dixey 1992, p. 165.
- ^ a b Godlee 1924, p. 192.
- ^ a b c d e f Lawrence & Dixey 1992, p. 166.
- ^ a b c d e f g Lawrence & Dixey 1992, p. 167.
- ^ Fisher 1977, p. 149.
- ^ a b c d e f Lawrence & Dixey 1992, p. 168.
- ^ Lister 1867a, p. 45.
- ^ Lister J (21 September 1867). "Illustrations of the Antiseptic System of Treatment in Surgery". The Lancet: 354.
- ^ a b Louis 2010, pp. 30–38.
- ^ Godlee 1924, p. 223.
- ^ a b Lister 1868.
- ^ Barry 2018, p. 40-43.
- ^ a b c Gaw 1999, p. 31.
- ^ a b Fisher 1977, p. 151.
- ^ Fitzharris 2018, p. 201.
- ^ a b Gaw 1999, p. 32.
- ^ Lemaire 1860.
- ^ Godlee 1924, p. 160.
- ^ Lemaire 1865.
- ^ Lemay 1958.
- ^ Cheyne 1882, p. 355.
- ^ Gaw 1999, p. 33.
- ^ a b c Fisher 1977, p. 153.
- ^ a b c d Gaw 1999, p. 34.
- ^ Simpson SJ (2 November 1867). "Carbolic Acid and its Compunds in Surgery". The Lancet. 2. London: George Fall.
- ^ Fisher 1977, p. 154.
- ^ Pirrie W (9 November 1867). "On the Use of Carbolic Acid in Burns". The Lancet. 2. London: George Fall: 575.
- ^ Pirrie W (9 November 1867). "On the Use of Carbolic Acid in Burns". The Lancet. 2. London: George Fall: 595.
- ^ a b c Gaw 1999, p. 63.
- ^ Bennett JH (1868). "The Atmospheric Germ Theory: A Lecture Delivered to the Royal College of Surgeons in Edinburgh, January 17, 1868". Edinburgh Medical Journal. 13 (9): 810–834. PMC 5000128.
- ^ Bennett JH (17 January 1868). "The Atmospheric Germ Theory: A Lecture Delivered to the Royal College of Surgeons in Edinburgh, January 17, 1868". Edinburgh Medical Journal. 13 (9): 810–834. PMC 5000128.
- ^ a b c Gaw 1999, p. 64.
- ^ a b Ravichandran B (17 March 2007). "Celebrating the medical past, again". BMJ. 334 (7593): 587. doi:10.1136/bmj.39153.707465.59. PMC 1828304.
- ^ Gaw 1999, p. 65.
- ^ Boreham, F. W. Nuggets of Romance, p. 53.
- ^ Plarr's 2009.
- ^ Hurwitz B, Dupree M (March 2012). "Why celebrate Joseph Lister?". The Lancet. 379 (9820): e39–e40. doi:10.1016/s0140-6736(12)60245-1. ISSN 0140-6736. PMID 22385682. S2CID 13775300.
- ^ Connor JJ, Connor JT (1 June 2008). "Being Lister: ethos and Victorian medical discourse". Medical Humanities. 34 (1): 3–10. doi:10.1136/jmh.2008.000270. ISSN 1468-215X. PMID 23674533.
- ^ Nakayama D (2018). "Antisepsis and Asepsis and How They Shaped Modern Surgery". The American Surgeon. 84 (6). Atlanta, Georgia: Southeastern Surgical Congress: 766–771. doi:10.1177/000313481808400616. PMID 29981599. S2CID 51620954. ProQuest 2086806520.
- ^ Godlee 1924, p. 244.
- ^ "Biography of Sir George Husband Baird MacLeod". Universitystory.gla.ac.uk. 15 December 2016. Archived from the original on 1 December 2017. Retrieved 21 January 2018.
- ^ "Dr. Alexander Gunn". BMJ. 1 (2780). Obituary: 841. 11 April 1914. doi:10.1136/bmj.1.2780.841-a. S2CID 220034805.
- ^ Beatson GT (9 April 1927). "A Case Of Excision Of Knee And Elbow Joints By Lord Lister: Condition Forty Years After". British Medical Journal. 1 (3457): 662–663. doi:10.1136/bmj.1.3457.662. JSTOR 25323116. PMC 2454877. PMID 20773119.
- ^ Lister J (1870). Journal of Wards 4 and 4. The Royal College of Surgeons of Edinburgh Library and Archive, Edinburgh: Royal Infirmary of Edinburgh.
- ^ Beatson G (November 1880). "Practical Papers on the Materials of the Antiseptic Method of Treatment. 7. On Sponges and Antiseptic Drainage". Glasgow Medical Journal. 14 (11): 359–378. PMC 5895226. PMID 30433351.
- ^ Minute Books of the Aesculapian Club. Library of the Royal College of Physicians of Edinburgh.
- ^ Godlee 1924, p. 395.
- ^ a b Godlee 1924, p. 397.
- ^ a b c d Louis 2011.
- ^ a b Gaw 1999, p. 110.
- ^ a b Gaw 1999, p. 61.
- ^ Godlee 1924, p. 398.
- ^ Fitzharris 2018, p. 187.
- ^ Gaw 1999, p. 111.
- ^ a b c d Gaw 1999, p. 112.
- ^ Godlee 1924, p. 407.
- ^ a b c Gaw 1999, p. 113.
- ^ a b c Godlee 1924, p. 410.
- ^ Godlee 1924, p. 412.
- ^ Godlee 1924, pp. 412–413.
- ^ a b Godlee 1924, p. 413.
- ^ Godlee 1924, p. 414.
- ^ Godlee 1924, pp. 414–417.
- ^ Teuber M (1995). "The genus Lactococcus". In Wood BJ, Holzapfel WH (eds.). The Genera of Lactic Acid Bacteria. pp. 173–234. doi:10.1007/978-1-4615-5817-0_6. ISBN 978-1461376668.
- ^ Godlee 1924, p. 417.
- ^ Gaw 1999, pp. 113–114.
- ^ a b Godlee 1924, p. 421.
- ^ a b Thomson 1919, p. 102.
- ^ "Transactions of the Clinical Society of London Volume 18 1886". Clinical Society. 1885. Retrieved 23 October 2012. archive.org
- ^ Bailard EJ (1924). "Joseph Lister". The American Journal of Nursing. 24 (7): 576. JSTOR 3407651.
- ^ Hurwitz B, Dupree M (2012). "Why celebrate Joseph Lister?". The Lancet. 379 (9820): e39–e40. doi:10.1016/s0140-6736(12)60245-1. ISSN 0140-6736. PMID 22385682. S2CID 13775300.
- ^ a b c Linder & Forrest 2005.
- ^ Toledo-Pereyra & Toledo 1976, pp. 736–744.
- ^ a b Godlee 1924, p. 335.
- ^ a b c d Upmalis 1968.
- ^ Lister J (3 September 1870). "A Method of Antiseptic Treatment Applicable to Wounded Soldiers in the Present War". BMJ. 2 (505): 243–244. doi:10.1136/bmj.2.505.243. PMC 2261349. PMID 20745963.
- ^ Gaw 1999, p. 98.
- ^ Schlich 2013.
- ^ a b c d e f g Willy et al. 2008.
- ^ a b c Gaw 1999, p. 99.
- ^ a b c Godlee 1924, p. 366.
- ^ Lister 1875.
- ^ Cameron 1949, p. 120.
- ^ a b c d Cameron 1949, p. 121.
- ^ Godlee 1924, p. 525.
- ^ a b Godlee 1924, p. 526.
- ^ a b Hart E, Williams D, eds. (3 August 1895). "Testimonial to Sir Joseph Lister". British Medical Journal. 2 (July to December): 307. Retrieved 1 May 2021.
- ^ "No. 27175". The London Gazette. 20 March 1900. p. 1875.
- ^ "No. 27289". The London Gazette. 26 February 1901. p. 1414.
- ^ Schwartz S, Wilder J (1993). Surgical Reflections: Images in Paint and Prose. Taylor & Francis. p. 93. ISBN 978-0942219487. Retrieved 1 May 2021.
- ^ Bynum WF (1994). Science and the Practice of Medicine in the Nineteenth Century. Cambridge University Press. p. 137. ISBN 978-0521272056. Retrieved 1 May 2021.
- ^ Reminiscences of a Surgeon. Dorrance Publishing. p. 134.
- ^ a b c Godlee 1924, p. 596.
- ^ a b c d e f g h i Funeral 1912.
- ^ "Lister Memorial Fund". British Medical Journal. 2 (2743). Science Notes: 183. 26 July 1913. doi:10.1136/bmj.2.2743.183. PMC 2345484. PMID 20766738.
- ^ London Gazette, No. 25300 1883, p. 6687.
- ^ a b c Godlee 1924, p. 475.
- ^ London Gazette, No. 26821 1897, p. 758.
- ^ The Times, Friday, 1 January 1897; Issue 35089; p. 8; col A
- ^ "The Coronation Honours". The Times. No. 36804. London. 26 June 1902. p. 5.
- ^ The Times, No. 36842 1902, p. 6.
- ^ London Gazette, No. 27470 1902, p. 5679.
- ^ London Gazette, No. 27464 1902, p. 5173.
- ^ a b Godlee 1924, p. 581.
- ^ "Sir Joseph Lister in Edinburgh". Maryland Medical Journal. 25: 173. 1891. Retrieved 13 August 2020.
- ^ "Winners of the Cothenius Medal 1864 to 1953". German National Academy of Sciences Leopoldina. Nationale Akademie der Wissenschaften. Retrieved 30 August 2020.
- ^ Cameron 1949, p. 144.
- ^ Godlee 1924, p. 527.
- ^ "Fellow details". The Royal Society. 2020 The Royal Society. Retrieved 13 August 2020.
- ^ Godlee 1924, pp. 542–543.
- ^ "Our Heritage". The Lister Institute. Archived from the original on 25 November 2015. Retrieved 24 November 2015.
- ^ "NHSGGC : Glasgow Royal Campus – New Lister Building". www.nhsggc.org.uk. Retrieved 20 August 2021.
- ^ "Behind the Frieze – Baron Lister of Lyme Regis (1827–1912)". London School of Hygiene and Tropical Medicine. Archived from the original on 22 November 2016. Retrieved 22 November 2016.
- ^ "Behind the Frieze". London School of Hygiene and Tropical Medicine. Archived from the original on 2 February 2017. Retrieved 6 November 2022.
- ^ Godlee 1924, p. 535.
- ^ "Glasgow Memorial To Lord Lister". The British Medical Journal. 2 (3326): 594–595. 27 September 1924. doi:10.1136/bmj.2.3326.594. JSTOR 20437915. S2CID 34727479.
- ^ "Mount Lister". Geographic Names Information System. United States Geological Survey, United States Department of the Interior. Retrieved 9 February 2010.
- ^ Hicks J. "A Fresh Breath". Thanks to Chemistry. Chemical Heritage Foundation. Archived from the original on 12 July 2016. Retrieved 27 January 2015.
- ^ Ramaswamy V, Cresence VM, Rejitha JS, Lekshmi MU, Dharsana KS, Prasad SP, Vijila HM (February 2007). "Listeria – review of epidemiology and pathogenesis" (PDF). Journal of Microbiology, Immunology, and Infection = Wei Mian Yu Gan Ran Za Zhi. 40 (1): 4–13. PMID 17332901. Archived from the original (PDF) on 31 March 2020. Retrieved 17 May 2019.
- ^ Griffiths 1993.
Bibliography
Articles (journals and proceedings)
- Alberti S (1 March 2012). "Saints and Sinners: Joseph Lister". The Bulletin of the Royal College of Surgeons of England. 94 (3): 90–91. doi:10.1308/147363512X13189526440393.
- Barry RR (28 March 2018). "From Barbers and Butchers to Modern Surgeons". Distillations. 4 (1): 40–43.
- Best AE (January 1970). "Reflections on Joseph Lister's Edinburgh Experiments on Vaso-Motor Control". Medical History. 14 (1): 10–30. doi:10.1017/S0025727300015106. PMC 1034011. PMID 4904726.
- Bonnin JG, LeFanu WR (February 1967). "Joseph Lister 1827–1912. A bibliographical biography". The Journal of Bone and Joint Surgery. 49 (1): 4–23. doi:10.1302/0301-620X.49B1.4. PMID 5335466.
- Bulloch W (9 April 1927). "Some Aspects of Lister's Scientific Work" (PDF). Nature. 119 (2997): 531–533. Bibcode:1927Natur.119..531B. doi:10.1038/119531a0. S2CID 4114620.
- Buxton DW (July 1924). "Joseph, 1st Baron Lister, Paul Bert, and the Dosimetric Method of Administering Chloroform". British Journal of Anaesthesia. 2 (1): 1–12. doi:10.1093/bja/2.1.1.
- Cohen H (24 March 1956). "Reflections On The Hunterian Method". British Medical Journal. 1 (4968): 645–650. doi:10.1136/bmj.1.4968.645. JSTOR 20334843. PMC 1979293. PMID 20788514.
- Cope Z (1 April 1967). "Joseph Lister, 1827–1912". The British Medical Journal. 2 (5543): 7–8. doi:10.1136/bmj.2.5543.7. JSTOR 25411706. PMC 1841130. PMID 5336180. S2CID 31802186.
- Clark PF (December 1920). "Joseph Lister, his Life and Work". The Scientific Monthly. 11 (6). American Association for the Advancement of Science: 518–539. Bibcode:1920SciMo..11..518C.
- Davidson MW (28 April 2011). "Pioneers in Optics: Joseph Jackson Lister and Maksymilian Pluta". Microscopy Today. 19 (3). Cambridge: Microscopy Society of America 2011: 54–56. doi:10.1017/S1551929511000277. S2CID 137191223.
- Ford WW (January 1928). "The Bacteriological Work of Joseph Lister". The Scientific Monthly. 26 (1): 70–75. Bibcode:1928SciMo..26...70F. JSTOR 7951.
- Gaw JL (1999). ""A Time to Heal": The Diffusion of Listerism in Victorian Britain". Transactions of the American Philosophical Society. 89 (1). Philadelphia: American Philosophical Society: iii–173. doi:10.2307/3185883. JSTOR 3185883.
- Fox NJ (December 1988). "Scientific Theory Choice and Social Structure: The Case of Joseph Lister's Antisepsis, Humoral Theory and Asepsis". History of Science. 26 (4): 367–397. doi:10.1177/007327538802600402. PMID 11621887. S2CID 43861442.
- Geison Gl (January 1972). "Social and institutional factors in the stagnancy of English physiology, 1840–1870". Bulletin of the History of Medicine. 46 (1). The Johns Hopkins University Press: 43–45, 56–57. JSTOR 44447479. PMID 4552626.
- Glass GE (September 2014). "Beyond antisepsis: Examining the relevance of the works of Joseph Baron Lister to the contemporary surgeon-scientist". Indian Journal of Plastic Surgery. 47 (3): 407–411. doi:10.4103/0970-0358.146619. PMC 4292121. PMID 25593429.
- Harris RI (August 1956). "Syme's Amputation". The Journal of Bone and Joint Surgery. British Volume. 38-B (3): 614–632. doi:10.1302/0301-620X.38B3.614. PMID 13357587.
- Howard ER (20 September 2013). "Joseph Lister: his contributions to early experimental physiology". Notes and Records of the Royal Society. 67 (3): 191–198. doi:10.1098/rsnr.2013.0029. PMC 3744350. S2CID 2907106.
- Lemay P (1958). "Les débuts de l'acide phénique" [The beginnings of phenic acid]. Revue d'Histoire de la Pharmacie (in French). 46 (156): 241.
- Linder F, Forrest H (8 December 2005). "The propagation of Lister's ideas". British Journal of Surgery. 54 (13): 419–421. doi:10.1002/bjs.1800541305. PMID 5337656. S2CID 28896502.
- Louis FK (1 December 2010). "Great Names in the History of Orthopaedics XIV: Joseph Lister (1827–1912) Part 1". Journal of Orthopaedics, Trauma and Rehabilitation. 14 (2): 30–38. doi:10.1016/j.jotr.2010.08.004. S2CID 207943872.
- Louis FK (June 2011). "Great Names in the History of Orthopaedics XIV: Joseph Lister (1827–1912) Part 2". Journal of Orthopaedics, Trauma and Rehabilitation. 15 (1): 29–36. doi:10.1016/j.jotr.2010.11.002.
- Moynihan B (9 April 1927). "Lister As A Surgeon". The British Medical Journal. 1 (3457): 656–658. doi:10.1136/bmj.1.3457.656. JSTOR 25323114. PMC 2454878. PMID 20773117.
- Pitt D, Aubin JM (1 September 2012). "Joseph Lister: father of modern surgery". Canadian Journal of Surgery. 55 (5): e8–e9. doi:10.1503/cjs.007112. ISSN 0008-428X. PMC 3468637. PMID 22992425.
- Richardson R (20 September 2013a). "Inflammation, suppuration, putrefaction, fermentation: Joseph Lister's microbiology". Notes and Records of the Royal Society. 67 (3): 211–229. doi:10.1098/rsnr.2013.0034. PMC 3744354. S2CID 73323223.
- Richardson R (28 September 2013b). "Joseph Lister's domestic science". The Lancet. 382 (9898): e8–e9. doi:10.1016/S0140-6736(13)62023-1. PMID 24083310. S2CID 26888101.
- Richardson R, Rhodes B (20 December 2013). "Joseph Lister's first operation". Notes and Records of the Royal Society. 67 (4): 375–385. doi:10.1098/rsnr.2013.0033. PMC 3826195. S2CID 71289054.
- Rutkow I (June 2013). "Joseph Lister and His 1876 Tour of America". Annals of Surgery. 257 (6): 1181–1187. doi:10.1097/SLA.0b013e31826d9116. PMID 23059499. S2CID 389275.
- Sakula A (1985). "Marcus Beck Library: Who Was Marcus Beck?". Journal of the Royal Society of Medicine. 78 (12): 1047–1049. doi:10.1177/014107688507801214. PMC 1290062. PMID 3906125.
- Santer M (20 March 2010). "Joseph Lister: first use of a bacterium as a 'model organism' to illustrate the cause of infectious disease of humans". Notes and Records of the Royal Society. 64 (1): 59–65. doi:10.1098/rsnr.2009.0029. PMID 20503823. S2CID 1940342.
- Schlich T (20 September 2013). "Farmer to industrialist: Lister's antisepsis and the making of modern surgery in Germany". Notes and Records of the Royal Society. 67 (3). Royal Society: 245–260. doi:10.1098/rsnr.2013.0032. PMC 3744353. S2CID 168067.
- Squire W (December 1888). "On the Introduction of Ether Inhalation as an anæsthetic in London". The Lancet. 132 (3408): 1220–1221. doi:10.1016/S0140-6736(02)25293-9.
- Syme J (1 January 1824). "Successful Case of Amputation at the Hip-Joint". Edinburgh Medical and Surgical Journal. 21 (78): 19–27. PMC 5826417. PMID 30331868.
- Toledo-Pereyra LH, Toledo MM (June 1976). "A critical study of lister's work on antiseptic surgery". The American Journal of Surgery. 131 (6): 736–744. doi:10.1016/0002-9610(76)90192-6. PMID 779507.
- Thomson SC (June 1919). Pakard FR (ed.). "A House-Surgeon's Memories of Joseph Lister". Annals of Medical History. 2 (2). New York: Paul R. Hoeber: 93–108. PMC 7944781. PMID 33944058.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - Turk JL (December 1994). "Inflammation: John Hunter's "A treatise on the blood, inflammation and gun-shot wounds"". International Journal of Experimental Pathology. 75 (6): 385–395. PMC 2001919. PMID 7734328.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - Upmalis I (May 1968). "The introduction of Lister's treatment in Germany". Bulletin of the History of Medicine. 42 (3). The Johns Hopkins University Press: 221–240. PMID 4875745.
- Willy C, Schneider P, Engelhardt M, Hargens AR, Mubarak SJ (February 2008). "Richard von Volkmann: Surgeon and Renaissance Man". Clinical Orthopaedics & Related Research. 466 (2): 500–506. doi:10.1007/s11999-007-0007-4. PMC 2505124. PMID 18196438.
- "Funeral Of Lord Lister". The British Medical Journal. 1 (2669): 440–446. 24 February 1912. JSTOR 25296192.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - "Arthur Lister, F.R.S". Nature. 78 (2023): 325. 6 August 1908. Bibcode:1908Natur..78Q.325.. doi:10.1038/078325a0. ISSN 1476-4687. S2CID 4035846.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - "William Sharpey M.D., F.R.S." Nature. 21 (546): 567–568. April 1880. Bibcode:1880Natur..21..567.. doi:10.1038/021567a0. S2CID 4001006.
Joseph Lister
- Lister J (1 January 1853a). Lankester E, Busk G (eds.). "Observations on the Contractile Tissue of the Iris". Quarterly Journal of Microscopical Science. s1-1 (1). W. Clowes and Sons: 8–17.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - Lister J (1 October 1853b). Lankester E, Busk G (eds.). "Observations on the muscular tissue of the skin". Quarterly Journal of Microscopical Science. s1-1 (4). W. Clowes and Sons: 262–268.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- Lister J (January 1858a). "On the Minute Structure of Involuntary Muscular Fibre". Transactions of the Microscopical Society & Journal. 6 (1): 5–14. doi:10.1111/j.1365-2818.1858.tb04533.x. S2CID 73003542.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - Lister J (1 October 1853c). Lankester E, Busk G (eds.). "Proceedings of Societies: Observations on the Flow of the Lacteal Fluid in the Mesentery of the Mouse". Quarterly Journal of Microscopical Science. s1-6 (21). W. Clowes and Sons: 262–268.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - Lister J (1858b). "An Inquiry Regarding the Parts of the Nervous System Which Regulate the Contractions of the Arteries". Philosophical Transactions of the Royal Society of London. 148. Royal Society: 607–625. Bibcode:1858RSPT..148..607L. JSTOR 108676.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - Lister J (31 December 1858c). "On the cutaneous pigmentary system of the frog". Philosophical Transactions of the Royal Society of London. 148: 627–643. doi:10.1098/rstl.1858.0030. JSTOR 108677. S2CID 110331946.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - Lister J (31 December 1858d). "On the early stages of inflammation". Philosophical Transactions of the Royal Society of London. 148. Royal Society: 645–702. ISSN 0261-0523. JSTOR 108678.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - Lister J (13 August 1858e). "Preliminary Account of an Inquiry into the Functions of the Visceral Nerves, with Special Reference to the So-Called 'Inhibitory System'". Proceedings of the Royal Society of London. 9. Royal Society: 367–380. Bibcode:1857RSPS....9..367L. JSTOR 111523.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - Lister J (April 1858f). "On a Case of Spontaneous Gangrene from Arteritis, and on the Causes of Coagulation of the Blood in Diseases of the Blood-Vessels". Edinburgh Medical Journal. 3 (10): 893–907. PMC 5311802. PMID 29646397.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - Lister J (December 1859b). "Notice of Further Researches on the Coagulation of the Blood". Edinburgh Medical Journal. 5 (6): 536–540. PMC 5277241.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - Lister J (August 1858g). "Case of Ligature of the Brachial Artery, Illustrating the Persistent Vitality of the Tissues". Edinburgh Medical Journal. 4 (2): 119–120. PMC 5309046. PMID 29646615.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - Lister J (21 September 1867a). "On the Antiseptic Principle in the Practice of Surgery". BMJ. 2 (351): 246–248. doi:10.1136/bmj.2.351.246. JSTOR 25212827. PMC 2310614. PMID 20744875.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - Lister J (March 1867b). "On a New Method of Treating Compound Fracture, Abscess, etc., with Observations on the Conditions of Suppuration" (PDF). The Lancet. 89 (2272): 326–329. doi:10.1016/S0140-6736(02)51192-2.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - Lister J (25 December 1875). "An Address On The Effect Of The Antiseptic Treatment Upon The General Salubrity Of Surgical Hospitals". The British Medical Journal. 2 (782). BMJ: 769–771. doi:10.1136/bmj.2.782.769. JSTOR 25242441. PMC 2297857. PMID 20748054.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - Lister J (3 September 1870). "A Method of Antiseptic Treatment Applicable to Wounded Soldiers in the Present War". BMJ. 2 (505): 243–244. doi:10.1136/bmj.2.505.243. JSTOR 25219599. PMC 2261349. PMID 20745963.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- Lister J (March 1865). "On excision of the wrist for caries". The Lancet. 85 (2169): 308–312. doi:10.1016/S0140-6736(00)63737-6.
- Lister J (1868). "An Address On The Antiseptic System Of Treatment In Surgery". The British Medical Journal. 2 (411): 515–517. doi:10.1136/bmj.2.394.53. ISSN 0007-1447. JSTOR 25215501. PMC 2310876. PMID 20745202.
Louis Pasteur
- Pasteur L (1 January 1857). "Mémoire sur la fermentation appelée lactique (Extrait par l'auteur)". Comptes Rendus Chimie (in French). Paris: Comptes rendus de l'Académie des Sciences: 913–916.
- Pasteur L (1860). "Mémoire sur la fermentation alcoolique". Annales de chimie et de physique (in French). 58. Mallet-Bachelier: 323–426.
- Pasteur L (19 May 1861a). "Sur les corpuscules organisés qui existent dans l'atmosphère, examen de la doctrine des générations spontanées" (in French). Paris: Society of Chemists of Paris.
- Pasteur L (1 August 1861b). "Animalcules infusoires vivant sans gaz oxygène libre et déterminant des fermentations". Comptes rendus de l'Académie des Sciences (in French). Paris: 344–347.
- Pasteur L (29 June 1863a). "Examen du rôle attribué au gaz oxygène atmosphérique dans la destruction des matières animales et végétales après la mort". Comptes rendus de l'Académie des Sciences (in French). Paris: Académie des sciences: 734–740.
- Pasteur L (1863b). "Recherches sur la putréfaction". Comptes rendus de l'Académie des Sciences (in French). 56. French Academy of Sciences: 1189–1194.
Books and monographs
- Beck W, Wells W, Chalkley H (1888). "Smith Harrison". Biographical Catalogue: Being an Account of the Lives of Friends and Others Whose Portraits are in the London Friends' Institute. Also Descriptive Notices of Those of the Friends' Schools and Institutions of which the Gallery Contains Illustrations, &c., &c., &c. Friends' institute.
- Bankston J (2005). Joseph Lister and the Story of Antiseptics (Uncharted, Unexplored, and Unexplained). Bear, Del: Mitchell Lane Publishers. ISBN 978-1584152620.
- Blore GH (1920). Victorian Worthies: Sixteen Biographies. Library of Alexandria. p. 350. ISBN 978-1465508751.
- Bonner TN (2000). Becoming a Physician: Medical Education in Britain, France, Germany, and the United States, 1750–1945. Baltimore: Johns Hopkins University Press. p. 194. ISBN 978-0801864827.
- Cartwright FF (1977). A social history of medicine. London: Longman. ISBN 978-0582483934. OCLC 2464630.
- Cameron HC (1949). Joseph Lister, the friend of man, by Hector Charles Cameron. London: William Heinemann Medical Books. OCLC 459047072.
- Cameron HC (1927). "A Short Account of the Evolution of Lister's System of Antiseptic Surgery". In Wellcome Historical Medical Museum (ed.). Lister Centenary Exhibition. London: The Wellcome Foundation Ltd. pp. 15–61.
- Chapman A (2016). Physicians, Plagues and Progress: The History of Western Medicine from Antiquity to Antibiotics. Lion Books. ISBN 978-0745970400. Retrieved 5 June 2020.
- Cheyne WW (1882). Antiseptic surgery; its principles, practice, history, and results. London: Smith Elder & Co.
- DePaolo C (2016). William Watson Cheyne and the Advancement of Bacteriology. Jefferson: McFarland & company. ISBN 978-1476666518. OCLC 1122854566.
- Dormandy T (2004). Moments of Truth: Four Creators of Modern Medicine. John Wiley & Sons. ISBN 978-0470867242.
- Freeman A (1989). Elizabethan eccentrics: brief lives of English misfits, exploiters, rogues, & failures, 1580–1660. New York: Dorset Press. ISBN 978-0880294379. OCLC 317465273.
- Finlayson J, Royal College of Surgeons of England (1900). Lord Lister and the development of antiseptic surgery. Retrieved 26 September 2021.
- Fisher RB (1977). Joseph Lister, 1827–1912. New York: Stein and Day. ISBN 978-0812821567. OCLC 2595463.
- Fitzharris L (2018). The butchering art: Joseph Lister's quest to transform the grisly world of Victorian medicine. UK: Penguin Books. ISBN 978-0141983387. OCLC 1066085821.
- Gardner-Thorpe C (2001). "Henry Head (1861–1940)". In Rose FC (ed.). Twentieth Century Neurology: The British Contribution. World Scientific. p. 9. ISBN 978-1783261604. Retrieved 9 August 2021.
- Godlee SR (October 1924). Lord Lister (3rd, Rev. ed.). Oxford: Oxford University Press. ISBN 978-1333634315.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - Goody J (1973). The Character of kinship. Cambridge: Cambridge University Press. ISBN 978-0521202909. OCLC 1156434238.
- Lawrence C, Dixey R (1992). "Practising on principle: Joseph Lister and the germ theories of disease". In Lawrence C (ed.). Medical Theory, Surgical Practice. Routledge Library Editions: History of Medicie. London: Routledge. pp. 153–215. doi:10.4324/9780429020094. ISBN 978-0429020094. S2CID 70482526.
- Lemaire J (1860). Du Coaltar saponiné, désinfectant énergique, de ses applications à l'hygiène, à la thérapeutique, à l'histoire naturelle, par Jules Lemaire [Saponinated Coaltar, energetic disinfectant, its applications to hygiene, therapy, natural history] (in French). Paris: Libraire de Germer Baillière.
- Lemaire J (1865). De l'Acide phénique, de son action sur les végétaux, les animaux, les ferments, les venins, les virus, les miasmes, et de ses applications à l'industrie, à l'hygiène, aux sciences anatomiques et à la thérapeutique, par le Dr Jules Lemaire (in French). Paris: Germer-Baillière.
- LeFanu W (1974). "Robert Willis – physician, librarian, medical historian". Proceedings of the XXIII International Congress of the History of Medicine, London, 2-9 September 1972. Vol. 2. London: Wellcome Institute of the History of Medicine.
- Noble I (1960). The Courage of Dr. Lister. New York: Julian Messner, Inc.
- Ogilvie M, Harvey J (2003). The Biographical Dictionary of Women in Science: Pioneering Lives From Ancient Times to the Mid-20th Century. Routledge. ISBN 978-1135963439.
- Powell W, ed. (1973). "West Ham: Domestic buildings". A History of the County of Essex. Vol. 6. London: Victoria County History.
- Shepard FF (1968). "Lister and the development of abdominal surgery". In Poynter FN (ed.). Medicine and science in the 1860s: Proceedings of the Sixth British Congress on the History of Medicine University of Sussex 6–9 September 1967. Publications of the Wellcome Institute of the History of Medicine. Vol. XVI. London: Wellcome Institute of the History of Medicine, Cluneberry Press. OCLC 14498003.
- Cartwright FF (1968). "Antiseptic Surgery". In Poynter FN (ed.). Medicine and science in the 1860s: Proceedings of the Sixth British Congress on the History of Medicine University of Sussex 6–9 September 1967. Publications of the Wellcome Institute of the History of Medicine. Vol. XVI. London: Wellcome Institute of the History of Medicine, Cluneberry Press. OCLC 14498003.
- Pflüger EF (1857). Ueber das Hemmungs-Nervensystem für die peristaltischen Bewegungen der Gedärme (in German). Berlin: Verlag von August Hirschwald.
- Nuland SB (2011). Doctors: The Biography of Medicine. Knopf Doubleday Publishing Group. ISBN 978-0307807892.
- Simmons JG (2002). "Joseph Lister Antisepsis and Modern Surgery". Doctors and discoveries: lives that created today's medicine. Boston: Houghton Mifflin. pp. 94–99. ISBN 978-0618152766. OL 7603987M.
- Smith R (2020). Inhibition : History and Meaning in the Sciences of Mind and Brain Inhibition. Berkeley: University of California Press. doi:10.1525/9780520911703. ISBN 978-0520911703.
- Tyman JH (21 August 1996). Synthetic and Natural Phenols. Amsterdam: Elsevier. ISBN 978-0-08-054219-5.
- Walshe WH (1846). The nature and treatment of cancer. London: Taylor and Walton. OCLC 970800717.
- Worboys M (2000). Spreading Germs: Disease Theories and Medical Practice in Britain, 1865–1900. Cambridge: Cambridge University Press. ISBN 978-0-521-77302-7.
- Wrench GT (1913). Lord Lister; his life and work. London: Fisher Unwin, New York: Frederick A. Stokes Company – via Cornell University.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - Wellcome Historical Medical Museum (1927). Lister centenary exhibition at the Wellcome historical medical museum. London: The Wellcome Foundation Ltd. OCLC 4257520.
- Welcome HS (1910). The Evolution of Antiseptic Surgery, American Medical Association. St. Louis: Burrroughs Welcome and Co. pp. 63–84.
- "Miscellany and monthly Critic". The Court Magazine and Monthly Critic, and Lady's Magazine and Museum: A Family Journal of the Belles Lettres, Music, Fine Arts, Drama, Fashion, Etc. Vol. 27. Dobbs. July 1845.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
Joseph Lister
Two quarto volumes of Lister's collected papers, that were prepared by Sir Hector Charles Cameron, Sir W. Watson Cheyne, Rickman J. Godlee, C. J. Martin and Dawson Williams:
- Lister BJ, Cameron HC (1909a). The collected papers of Joseph Baron Lister. Vol. 1. Oxford University Press, Hodder and Stoughton. OCLC 838259550.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - Lister BJ, Cameron HC (1909b). The collected papers of Joseph Baron Lister. Vol. 2. Oxford University Press, Hodder and Stoughton. OCLC 841851608.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - Lister J (1859a). Testimonials in favour of Joseph Lister, Esq., F.R.C.S. Eng. and Edin., Assistant-Surgeon to the Royal Infirmary of Edinburgh : candidate for the Professorship of Surgery in the University of Glasgow. Edinburgh: T. Constable.
Chapters and contributions
- Lister J (1862). "Amputation". In Holmes T (ed.). System of Surgery. Vol. III. London: Parker, Son and Bourn, West Strand. pp. 51–69.
In four volumes. Operative surgery; diseases of the organs of Special sense, respiration, circulation, locomotion and innervation
Dictionaries and encyclopedias
- Cartwright FF (2023). "Joseph Lister". Encyclopædia Britannica. Retrieved 8 February 2018.
- Lawrence C (23 September 2004). "Lister, Joseph, Baron Lister (1827–1912), surgeon and founder of a system of antiseptic surgery". Oxford Dictionary of National Biography. Vol. 1 (online ed.). Oxford University Press. doi:10.1093/ref:odnb/34553. (Subscription or UK public library membership required.)
- Lister J (1893). "Lister, Joseph Jackson". In Stephen L, Lee S (eds.). Dictionary of National Biography. Vol. 33. London: Smith, Elder, and Co. p. 347.
- Shaun B (2009). Dictionary of Irish Biography. Dublin: Royal Irish Academy. Pim, John Harold.
Lectures and addresses
- Cheyne SW (14 May 1925). Lister and his achievement : being the first Lister memorial lecture delivered at the Royal college of surgeons of England on May 14, 1925. London: Longmans, Green and Co.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - Lister J (6 October 1877). "Introductory Address Delivered in the Medical Department of King's College". BMJ. 2 (875): 465–469. doi:10.1136/bmj.2.875.465. PMC 2221161. PMID 20748639.
Introductory Address Delivered in the Medical Department of King's College
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - Lister J (June 1863). "The Croonian Lecture: On the Coagulation of the Blood". Proceedings of the Royal Society of London. 12. Royal Society: 580–611. JSTOR 112320.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - Lister J (1869). "Introductory Lecture Delivered In The University Of Edinburgh, November 8th, 1869". The British Medical Journal. 2 (466): 601–604. ISSN 0007-1447. JSTOR 25217818.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - Lister J (6 October 1900). "The Huxley Lecture". BMJ. 2 (2075): 969–977. doi:10.1136/bmj.2.2075.969. PMC 2463910. PMID 20759189.
{{cite journal}}: CS1 maint: ref duplicates default (link) This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
Letters
- Rudolf CR (1933). "Eight Letters Of Joseph (Lord) Lister To William Sharpey". The British Journal of Surgery. XX (77, 79). J. Wright, Wellcome Library.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
Medical registers
- "Lister, Joseph (1827–1912)". Plarr's Lives of the Fellows. The Royal College of Surgeons of England. 24 April 2008.
- "Beck, Marcus (1843–1893)". Plarr's Lives of the Fellows. Royal College of Surgeons of England. 11 December 2009.
- "Erichsen, Sir John Eric". Plarr's Lives of the Fellows. London: Royal College of Surgeons of England. 22 March 2012.
- "Godlee, Sir Rickman John (1849–1925)". Plarr's Lives of the Fellows. London: The Royal College of Surgeons of England. 11 May 2006.
- "Syme, James (1799–1870)". Plarr's Lives of the Fellows. London: The Royal College of Surgeons of England. 11 April 2013.
Newspapers
- "No. 25300". The London Gazette. 28 December 1883. p. 6687.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - "No. 26821". The London Gazette. 9 February 1897. p. 758.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - "No. 27464". The London Gazette. 12 August 1902. p. 5173.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - "No. 27470". The London Gazette. 2 September 1902. p. 5679.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - "Court Circular". The Times. No. 36842. London. 9 August 1902. p. 6.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
Theses
- Harless E (1846). Inaugural-Abhandlung über den Einfluss der Gase auf die Form der Blutkörperchen von Rana temporaria : als erster Abschnitt der Untersuchung über die Wirkung der Gase auf die Blutkörperchen sämmtlicher Thierklassen / von Emil Harless [Inaugural treatise on the influence of gases on the form of the blood corpuscles of Rana temporaria : as the first section of the investigation into the effect of gases on the blood corpuscles of all classes of animals] (pdf) (in German). Erlagen: Verlag von Carl Heyder, Royal College of Surgeons of England.
- Erichsen J (1853). The Science and Art of Surgery. Being a treatise on surgical injuries, diseases, and operations. By John Erichsen, Professor of Surgery in University College, and Surgeon to University College Hospital. Illustrated by Two Hundred and Fifty Engravings on Wood. London: Walton and Maberly, Upper Gower Street, and Ivy Lane, Paternoster Row.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
Websites
- Dronsfield A, Ellis P (1 September 2009). "Solving an infectious problem". Education in chemistry. Royal Society of Chemistry. Retrieved 28 February 2022.
- Griffiths A (July 1993). "Joseph Lister, Antiseptic Surgery" (PDF). The Postal Museum. Retrieved 13 September 2020.
- Moore W, Hunter J (2009). "John Hunter (1728–1793). Commentaries on the history of treatment evaluation". JLL Bulletin. London: Royal College of Physicians of Edinburgh. Retrieved 18 November 2021.
- Rose B (29 January 2014). "Joseph Lister's unknown operation uncovered". BBC News. Retrieved 13 July 2021.
External links
- Works by Joseph Lister at Project Gutenberg
- Works by Lord Lister at Project Gutenberg
- Works by or about Joseph Lister at the Internet Archive
- Works by Joseph Lister at LibriVox (public domain audiobooks)

- The Lister Institute
- Collection of portraits of Lister at the National Portrait Gallery, London
- Statue of Sir Joseph Lister by Louis Linck at The International Museum of Surgical Science in Chicago
- 1827 births
- 1912 deaths
- 19th-century English medical doctors
- 19th-century surgeons
- Academics of King's College London
- Academics of the University of Edinburgh
- Academics of the University of Glasgow
- Alumni of the University of London
- Barons in the Peerage of the United Kingdom
- English Quakers
- English surgeons
- Fellows of the Royal College of Surgeons of England
- Fellows of the Royal Society
- Foreign associates of the National Academy of Sciences
- Knights Commander of the Royal Victorian Order
- Medical hygiene
- Members of the Order of Merit
- Members of the Privy Council of the United Kingdom
- Members of the Royal Society of Sciences in Uppsala
- Peers of the United Kingdom created by Queen Victoria
- People associated with Edinburgh
- People associated with Glasgow
- People from West Ham
- Presidents of the British Science Association
- Presidents of the Royal Society
- Recipients of the Copley Medal
- Recipients of the Pour le Mérite (civil class)
- Recipients of the Cothenius Medal
- Royal Medal winners