Vagina: Difference between revisions
→Other animals: WL |
→Other animals: rm ref to shell gland - goes to mollusc feature |
||
| Line 222: | Line 222: | ||
The female [[spotted hyena]] does not have an external vagina. Instead, the vagina [[Female genitalia of spotted hyenas|exits through the clitoris]], allowing the females to urinate, copulate and give birth through the clitoris.<ref name="courtship">{{cite journal |vauthors=Szykman M, Van Horn RC, Engh AL, Boydston EE, Holekamp KE |year=2007 |title=Courtship and mating in free-living spotted hyenas |url=http://tuvalu.santafe.edu/~bowles/Dominance/Papers/SzykmanetalHyenaMatingBehaviour2007.pdf |journal=Behaviour |volume=144 |issue=7 |pages=815–846 |doi=10.1163/156853907781476418}}</ref> The female vagina of the [[coyote]] contracts during copulation, forming a [[Canine reproduction#Copulation|copulatory tie]].<ref name = "Bekoff">{{Cite journal |vauthors=Bekoff M, Diamond J |title=Precopulatory and Copulatory Behavior in Coyotes |journal=[[Journal of Mammalogy]] |volume=57 |issue=2 |pages=372–375 |publisher=[[American Society of Mammalogists]] |date=May 1976 |jstor=1379696 |doi=10.2307/1379696}}</ref> |
The female [[spotted hyena]] does not have an external vagina. Instead, the vagina [[Female genitalia of spotted hyenas|exits through the clitoris]], allowing the females to urinate, copulate and give birth through the clitoris.<ref name="courtship">{{cite journal |vauthors=Szykman M, Van Horn RC, Engh AL, Boydston EE, Holekamp KE |year=2007 |title=Courtship and mating in free-living spotted hyenas |url=http://tuvalu.santafe.edu/~bowles/Dominance/Papers/SzykmanetalHyenaMatingBehaviour2007.pdf |journal=Behaviour |volume=144 |issue=7 |pages=815–846 |doi=10.1163/156853907781476418}}</ref> The female vagina of the [[coyote]] contracts during copulation, forming a [[Canine reproduction#Copulation|copulatory tie]].<ref name = "Bekoff">{{Cite journal |vauthors=Bekoff M, Diamond J |title=Precopulatory and Copulatory Behavior in Coyotes |journal=[[Journal of Mammalogy]] |volume=57 |issue=2 |pages=372–375 |publisher=[[American Society of Mammalogists]] |date=May 1976 |jstor=1379696 |doi=10.2307/1379696}}</ref> |
||
In the case of other animals, birds, monotremes, and some reptiles have a part of the [[oviduct]] that leads |
In the case of other animals, birds, monotremes, and some reptiles have a part of the [[oviduct]] that leads to the [[cloaca]].<ref name="Iannaccone">{{cite book |vauthors=Iannaccone P |title=Biological Aspects of Disease |publisher=[[CRC Press]] |isbn=3718606135|year=1997|pages=315–316|url=https://books.google.com/books?id=CNt2tOsBnc8C&pg=PA315}}</ref><ref name="Fishbeck">{{cite book |vauthors=Fishbeck DW, Sebastiani A |title=Comparative Anatomy: Manual of Vertebrate Dissection|publisher=Morton Publishing Company|isbn=1617310042|year=2012|pages=66–68 |url=https://books.google.com/books?id=JijAAgAAQBAJ&pg=PA66}}</ref> Chickens have a vaginal aperture that opens from the vertical apex of the cloaca. The vagina extends upward from the aperture and becomes the egg gland.<ref name="Fishbeck" /> In some [[jawless fish]], there is neither oviduct nor vagina and instead the egg travels directly through the body cavity (and is fertilised externally as in most [[fish]] and [[amphibian]]s). In insects and other [[invertebrate]]s, the vagina can be a part of the oviduct (see [[insect reproductive system]]).<ref name="Chapman">{{cite book |vauthors=Chapman RF, Simpson SJ, Douglas AE |title=The Insects: Structure and Function|publisher=[[Cambridge University Press]]|isbn=052111389X|year=2013|pages=314–316 |url=https://books.google.com/books?id=NXJEi8fo7CkC&pg=PA314}}</ref> Females of some waterfowl species have developed vaginal structures called dead end sacs and clockwise coils to protect themselves from [[sexual coercion]].<ref name="twenty six">Brennan, P. L. R., Clark, C. J. & Prum, R. O. Explosive eversion and functional morphology of the duck penis supports sexual conflict in waterfowl genitalia. Proceedings: Biological Sciences 277, 1309–14 (2010).</ref> |
||
In 2014, the scientific journal ''[[Current Biology]]'' reported that four species of Brazilian insects in the genus ''[[Neotrogla]]'' were found to have sex-reversed genitalia. The male insects of those species have vagina-like openings, while the females have penis-like organs.<ref>Arielle Duhaime-Ross (April 17, 2014). [https://www.theverge.com/2014/4/17/5617766/scientists-discover-insect-with-female-penis "Scientists discover the animal kingdom's first 'female penis’"]. ''The Verge''. Retrieved March 29, 2015.</ref><ref>{{cite journal |vauthors=Yoshizawae K, Ferreira RL, Kamimura Y, Lienhard C |title=Female Penis, Male Vagina, and Their Correlated Evolution in a Cave Insect|journal=Current Biology|date=April 17, 2014|url=http://www.cell.com/current-biology/abstract/S0960-9822(14)00314-5 |doi=10.1016/j.cub.2014.03.022 |volume=24 |issue=9 |pages=1006–1010 |pmid=24746797}}</ref><ref>{{cite news|title=In sex-reversed cave insects, females have the penises |url=http://www.sciencedaily.com/releases/2014/04/140417101146.htm |access-date=April 27, 2014 |newspaper=Science Daily |date=April 17, 2014}}</ref> |
In 2014, the scientific journal ''[[Current Biology]]'' reported that four species of Brazilian insects in the genus ''[[Neotrogla]]'' were found to have sex-reversed genitalia. The male insects of those species have vagina-like openings, while the females have penis-like organs.<ref>Arielle Duhaime-Ross (April 17, 2014). [https://www.theverge.com/2014/4/17/5617766/scientists-discover-insect-with-female-penis "Scientists discover the animal kingdom's first 'female penis’"]. ''The Verge''. Retrieved March 29, 2015.</ref><ref>{{cite journal |vauthors=Yoshizawae K, Ferreira RL, Kamimura Y, Lienhard C |title=Female Penis, Male Vagina, and Their Correlated Evolution in a Cave Insect|journal=Current Biology|date=April 17, 2014|url=http://www.cell.com/current-biology/abstract/S0960-9822(14)00314-5 |doi=10.1016/j.cub.2014.03.022 |volume=24 |issue=9 |pages=1006–1010 |pmid=24746797}}</ref><ref>{{cite news|title=In sex-reversed cave insects, females have the penises |url=http://www.sciencedaily.com/releases/2014/04/140417101146.htm |access-date=April 27, 2014 |newspaper=Science Daily |date=April 17, 2014}}</ref> |
||
Revision as of 17:16, 1 January 2018
| Vagina | |
|---|---|
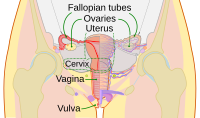 Diagram of the female human reproductive tract and ovaries | |
 Vulva with pubic hair removed and labia separated to show the opening of the vagina
1: Clitoral hood 2: Clitoris 3: Labia minora 4: Urethral opening 5: Vaginal opening 6: Perineum 7: Anus | |
| Details | |
| Precursor | urogenital sinus and paramesonephric ducts |
| Artery | superior part to uterine artery, middle and inferior parts to vaginal artery |
| Vein | uterovaginal venous plexus, vaginal vein |
| Nerve | Sympathetic: lumbar splanchnic plexus Parasympathetic: pelvic splanchnic plexus |
| Lymph | upper part to internal iliac lymph nodes, lower part to superficial inguinal lymph nodes |
| Identifiers | |
| Latin | Vagina |
| MeSH | D014621 |
| TA98 | A09.1.04.001 |
| TA2 | 3523 |
| FMA | 19949 |
| Anatomical terminology | |
In mammals, the vagina is a muscular and tubular part of the female genital tract, which, in humans, extends from the vulva to the cervix. The outer vaginal opening may be partly covered by a membrane called the hymen. At the deep end, the cervix (neck of the uterus) bulges into the vagina. The vagina allows for sexual intercourse and childbirth, and channels menstrual flow, which occurs periodically as part of the menstrual cycle.
The vagina has been studied in humans more than it has been in other animals. Its location and structure varies among species, and may vary in size within the same species. Female mammals usually have two external openings, the urethral opening for the urinary tract and the vaginal opening for the genital tract. This is different from male mammals, who usually have a single opening, the external urethral opening for both urination and reproduction. The vaginal opening is much larger than the nearby urethral opening, and both are protected by the labia in humans. In amphibians, birds, reptiles and monotremes, the cloaca is the single external opening for the gastrointestinal tract and the urinary and reproductive tracts.
To accommodate smoother penetration of the vagina during sexual intercourse or other sexual activity, vaginal moisture increases during sexual arousal in human females and also in other female mammals. This increase in moisture is vaginal lubrication, which reduces friction. The texture of the vaginal walls creates friction for the penis during sexual intercourse and stimulates it toward ejaculation, enabling fertilization. Along with pleasure and bonding, women's sexual behavior with others (which can include heterosexual or lesbian sexual activity) can result in sexually transmitted infections (STIs), the risk of which can be reduced by recommended safe sex practices. Other disorders may also affect the human vagina.
The vagina and vulva have evoked strong reactions in societies throughout history, including negative perceptions and language, cultural taboos, and their use as symbols for female sexuality, spirituality, or regeneration of life. In common speech, the word vagina is often used to refer to the vulva or to the female genitals in general. By its dictionary and anatomical definitions, however, vagina refers exclusively to the specific internal structure, and understanding the distinction can improve knowledge of the female genitalia and aid in health care communication.
Etymology and definition
The term vagina is from Latin vāgīnae, literally "sheath" or "scabbard"; the Latinate plural of vagina is vaginae.[1] The vagina may also be referred to as "the birth canal" in the context of pregnancy and childbirth.[2][3] Although by its dictionary and anatomical definitions, the term vagina refers exclusively to the specific internal structure, it is colloquially used to refer to the vulva or to both the vagina and vulva.[4][5]
Using the term vagina to mean "vulva" can pose medical or legal confusion; for example, a person's interpretation of its location might not match another person's interpretation of the location.[4][6] Medically, the vagina is the muscular canal between the hymen (or remnants of the hymen) and the cervix, while, legally, it begins at the vulva (between the labia).[4] Scholars such as Craig A. Hill[7] argue that incorrect use of the term vagina is likely because not as much thought goes into the anatomy of the female genitalia. This has contributed to an absence of correct vocabulary for the external female genitals, even among health professionals, which can pose sexual and psychological harm with regard to female development. Because of this, researchers endorse correct terminology for the vulva.[6][7][8]
Structure
Overview
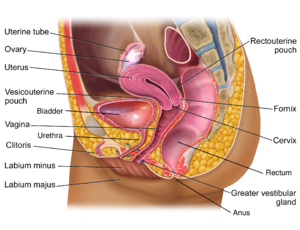
The human vagina is an elastic muscular canal that extends from the vulva to the cervix.[9][10] It is pink in color, and it connects the outer vulva to the cervix of the uterus. The part of the vagina surrounding the cervix is called the fornix.[11] The opening of the vagina lies in the urogenital triangle in the perineum, between the opening of the urethra and the anus. The vaginal canal then travels upwards and backwards, between the urethra at the front, and the rectum at the back. Near the upper vagina, the cervix protrudes into the vagina on its front surface at approximately a 90 degree angle.[12] The vaginal and urethral openings are protected by the labia.[13]
In its unexcited state, the vagina is a collapsed tube, with the anterior and posterior walls placed together. The lateral walls, especially their middle area, are relatively more rigid. Because of this, the collapsed vagina has an H-shaped cross section.[10][14] Behind, the inner vagina is separated from the rectum by the recto-uterine pouch, the middle vagina by loose connective tissue, and the lower vagina by the perineal body.[11] Where the vaginal lumen surrounds the cervix of the uterus, it is divided into four continuous regions or vaginal fornices; these are the anterior, posterior, right lateral, and left lateral fornices.[9][10] The posterior fornix is deeper than the anterior fornix.[10]
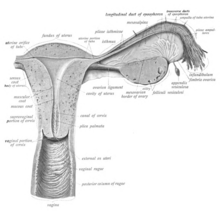
Different muscles and ligaments support the vagina at its upper, middle, and lower portions. At the upper part, three sets of ligaments attached to the upper surface of the levator ani, give support to the cervix and vagina. These are the cardinal ligaments (transverse cervical ligaments), pubocervical ligaments, and the uterosacral ligaments the sacrocervical ligaments. The middle third of the vagina involves the urogenital diaphragm and the pelvic floor. The lower third is supported by the perineal body that is also attached to the levator ani.[9][15][16]
Vaginal opening and hymen
The vaginal opening is at the outer end of the vulva, posterior to the opening of the urethra, at the posterior end of the vestibule. The opening is closed by the labia minora in virgins and in females who have never given birth (nulliparous), but may be exposed in females who have given birth (parous).[10][17]
The hymen is a membrane of tissue that surrounds or partially covers the vaginal opening.[10] The effects of intercourse and childbirth on the hymen are variable. Where it is broken, it may completely disappear or remnants known as carunculae myrtiformes may persist. Otherwise being very elastic it may return to its normal position.[18] Additionally, the hymen may be lacerated by disease, injury, medical examination, masturbation or physical exercise. For these reasons, it is not possible to definitively determine whether or not a female is a virgin by examining her hymen.[18][19]
Variations and size
The length of the vagina varies between women of child-bearing age. Because of the presence of the cervix in the front wall of the vagina, there is a difference in length between the front (anterior) wall, approximately 7.5 cm (2.5 to 3 in) long, and the back (posterior) wall, approximately 9 cm (3.5 in) long.[10][20] During sexual arousal, the vagina expands in both length and width. If a woman stands upright, the vaginal lumen, from the vulva upward, forms an angle of approximately 45 degrees where it meets the uterus and about 60 degrees to the horizontal.[10][15] Because of the involutions of the rugae, the total surface area of the vagina is 360cm2 (one square foot).[17] The vaginal opening and hymen also vary in size; in children, although a common appearance of the hymen is crescent-shaped, many shapes are possible.[10][21]
Development
The vaginal plate is the precursor to the vagina.[22] During development, the vaginal plate begins to grow where the solid ends of the paramesonephric ducts (Müllerian ducts) enter the back wall of the urogenital sinus. As the plate grows, it separates the sinus into the urethra and the vagina and extends the vagina by pushing the cervix deeper. Originally full of cells, as the central cells of the plate break down, the lumen of the vagina is formed.[22] This usually occurs by the twenty to twenty-fourth week of development. If the lumen does not form, or is incomplete, membranes across or around the tract called septae can form, which may cause obstruction of the outflow tract later in life.[22]
During sexual differentiation, without testosterone, the urogenital sinus persists as the vestibule of the vagina. The two urogenital folds (elongated spindle-shaped structures that contribute to the formation of the urethral groove on the belly aspect of the genital tubercle) form the labia minora, and the labioscrotal swellings enlarge to form the labia majora.[23][24]
Sources differ on which portion of the vagina is formed from the Müllerian ducts and which from the urogenital sinus by the growth of the sinovaginal bulb.[22][25] Dewhurst's Textbook of Obstetrics and Gynaecology states, "Some believe that the upper four-fifths of the vagina is formed by the Müllerian duct and the lower fifth by the urogenital sinus, while others believe that sinus upgrowth extends to the cervix displacing the Müllerian component completely and the vagina is thus derived wholly from the endoderm of the urogenital sinus." It adds, "It seems certain that some of the vagina is derived from the urogenital sinus, but it has not been determined whether or not the Müllerian component is involved."[22]
Microanatomy
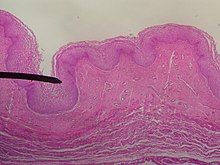

The wall of the vagina from the lumen outwards consists firstly of a mucosa of non-keratinized stratified squamous epithelium with an underlying lamina propria of connective tissue. Secondly, there is a layer of smooth muscle with bundles of circular fibers internal to longitudinal fibers. Lastly is an outer layer of connective tissue called the adventitia. Some texts list four layers by counting the two sublayers of the mucosa (epithelium and lamina propria) separately.[26][27]
The lamina propria is rich in blood vessels and lymphatic channels. The muscular layer is composed of smooth muscle fibers, with an outer layer of longitudinal muscle, an inner layer of circular muscle, and oblique muscle fibers between. The outer layer, the adventitia, is a thin dense layer of connective tissue, and it blends with loose connective tissue containing blood vessels, lymphatic vessels and nerve fibers that is present between the pelvic organs.[12][27][20] The vaginal mucosa is absent of glands. It forms folds or rugae, which are more prominent in the outer third of the vagina; they appear as transverse ridges and their function is to provide the vagina with increased surface area for extension and stretching.[9][10]


The epithelial covering of the cervix is contiguous with the epithelial lining of the vagina.[10] The vaginal epithelium is divided into layers of cells, including the basal cells, the parabasal cells, the superficial squamous flat cells, and the intermediate cells.[28] The basal layer of the epithelium is the most mitotically active and reproduces new cells.[29] The superficial cells exfoliate continuously and basal cells replace them.[10][30][31] Estrogen induces the intermediate and superficial cells to fill with glycogen.[31][32] Cells from the lower basal layer transition from active metabolic activity to death (apoptosis). In these mid-layers of the epithelia, the cells begin to lose their mitochondria and other organelles.[29][33] The cells retain an usually high level of glycogen compared to other epithelial tissue in the body.[29]
The permeability of the epithelium allows for an effective response from the immune system since antibodies and other immune components can easily reach the surface.[17] The vaginal epithelium differs from the similar tissue of the skin. The epidermis of the skin is relatively resistant to water because it contains high levels of lipids. The vaginal epithelium contains lower levels of lipids. This allows the passage of water and water-soluble substances through the tissue.[17]
Under the influence of maternal estrogen, newborn females have a thick stratified squamous epithelium for two to four weeks after birth. After that, the epithelium remains thin with only a few layers of cells without glycogen.[31] The epithelium also has few rugae and is red in color before puberty.[4] When puberty begins, the epithelium thickens and glycogen containing cells are formed again, under the influence of the girl's rising estrogen levels.[31] Finally, the epithelium thins out during menopause onward and eventually ceases to contain glycogen, because of the lack of estrogen.[10][30][34]
Keratinization happens when the epithelium is exposed to the dry external atmosphere.[10] In abnormal circumstances, such as in pelvic organ prolapse, the mucosa may be exposed to air, becoming dry and keratinized.[35]
Blood and nerve supply
Blood is mainly supplied to the vagina via the vaginal artery, which emerges from a branch of the internal iliac artery or the uterine artery.[9][36] With anastomosis, the vaginal arteries are joined along the side of the vagina with the cervical branch of the uterine artery; this forms the azygos artery,[36] which lies on the midline of the anterior and posterior vagina.[11] Other arteries which supply the vagina include the middle rectal artery and the internal pudendal artery,[10] all branches of the internal iliac artery.[11] Three groups of lymphatic vessels accompany these arteries; the upper group accompanies the vaginal branches of the uterine artery; a middle group accompanies the vaginal arteries; and the lower group, draining lymph from the area outside the hymen, drain to the inguinal lymph nodes.[11][37] Ninety-five percent of the lymphatic channels of the vagina are in the first 3 mm from the surface of the vagina.[38]
Two main veins drain blood from the vagina, one on the left and one on the right. These form a network of smaller veins (an anastomosis) on the sides of the vagina, connecting with similar networks of the uterine, vesical and rectal networks. These ultimately drain into the internal iliac veins.[11]
The nerve supply of the upper vagina is provided by the sympathetic and parasympathetic areas of the pelvic plexus. The lower vagina is supplied by the pudendal nerve supplying the lower area.[10][11]
Function
Secretions
The vaginal mucosa and epithelium vary in thickness and composition during the menstrual cycle.[39] The vagina provides a path for menstrual blood and tissue to leave the body. In industrial societies, tampons, menstrual cups and sanitary napkins may be used to absorb or capture these fluids. Vaginal secretions are primarily from the uterus, cervix, and vaginal epithelium in addition to minuscule vaginal lubrication from the Bartholin's glands upon sexual arousal. It takes little vaginal secretion to make the vagina moist; secretions may increase during sexual arousal, the middle of menstruation, a little prior to menstruation, or during pregnancy.[10]
The Bartholin's glands, located near the vaginal opening, were originally considered the primary source for vaginal lubrication, but further examination showed that they provide only a few drops of mucus.[40] The significant majority of vaginal lubrication is now believed to be provided by plasma seepage from the vaginal walls, which is called vaginal transudation. Vaginal transudation, which initially forms as sweat-like droplets, is caused by vascular engorgement of the vagina (vasocongestion), resulting in the pressure inside the capillaries increasing the transudation of plasma through the vaginal epithelium.[40][41][42]
Before and during ovulation, the mucus glands within the cervix secrete different variations of mucus, which provides an alkaline, fertile environment in the vaginal canal that is favorable to the survival of sperm.[43] Following menopause, vaginal lubrication naturally decreases.[44]
Sexual activity
Nerve endings in the vagina can provide pleasurable sensations when the vagina is stimulated during sexual activity. Women may derive pleasure from one part of the vagina, or from a feeling of closeness and fullness during vaginal penetration.[45] The vagina is not rich in nerve endings, and this often contributes to a woman's inability to receive sufficient sexual stimulation, including orgasm, solely from penetration of the vagina.[45][46][47] While the literature cites the existence of a greater concentration of nerve endings near the entrance of the vagina (at the outer one-third or lower third), making it more sensitive to touch than the inner (or upper) two-thirds of the vagina,[46][47][48] some scientific examinations of vaginal wall innervation indicate no single area with a greater density of nerve endings.[49][50] Other research indicates that only some women have a greater density of nerve endings in the anterior vaginal wall.[49][51] By having a higher concentration of nerve endings in the outer part rather than along the whole length,[52] childbirth pain is significantly more tolerable.[47][53][54]
Vaginal pleasure can come from a variety of different sexual activities. In addition to penile penetration, pleasure may be by masturbation, fingering, oral sex (cunnilingus), or specific sex positions (such as the missionary position or the spoons sex position).[55] Heterosexual couples may engage in cunnilingus or fingering as forms of foreplay to incite sexual arousal, with penile-vaginal penetration as the primary sexual activity, or they may engage in them in addition to penile-vaginal penetration; in other cases, heterosexual couples use the latter acts as a way to preserve virginity or as a type of birth control.[56][57] By contrast, lesbians and other women who have sex with women commonly engage in cunnilingus or fingering as main forms of sexual activity.[58][59] Some women and couples use sex toys, such as a vibrator or dildo, for vaginal pleasure.[60] Other women may adopt Kegel exercises,[61] with the aim of tightening the vagina to increase sexual pleasure.[62] The Kama Sutra, an ancient Hindu text written by Vātsyāyana, which includes a number of sexual positions, may also be used to increase sexual pleasure,[62] with special emphasis on female sexual satisfaction.[63]
The clitoris additionally plays a part in vaginal stimulation, as it is a sex organ of multiplanar structure containing an abundance of nerve endings, with a broad attachment to the pubic arch and extensive supporting tissue to the mons pubis and labia; it is centrally attached to the urethra, and research indicates that it forms a tissue cluster with the vagina. This tissue is perhaps more extensive in some women than in others, which may contribute to orgasms experienced vaginally.[46][64][65]
During sexual arousal, and particularly the stimulation of the clitoris, the walls of the vagina lubricate. This begins after ten to thirty seconds of sexual arousal, and increases in amount the longer the woman is aroused.[66] It reduces friction or injury that can be caused by insertion of the penis into the vagina or other penetration of the vagina during sexual activity. The vagina lengthens during the arousal, and can continue to lengthen in response to pressure; as the woman becomes fully aroused, the vagina expands in length and width, while the cervix retracts.[66][67] With the upper two-thirds of the vagina expanding and lengthening, the uterus rises into the greater pelvis, and the cervix is elevated above the vaginal floor, resulting in tenting of the mid-vaginal plane.[66] This is known as the tenting or ballooning effect.[68] As the elastic walls of the vagina stretch or contract, with support from the pelvic muscles, to wrap around the inserted penis (or other object),[48] this stimulates the penis and helps to cause a man to experience orgasm and ejaculation, which in turn enables fertilization.[69]
An area in the vagina that may be an erogenous zone is the G-spot; it is typically defined as being located at the anterior wall of the vagina, a couple or few inches in from the entrance, and some women experience intense pleasure, and sometimes an orgasm, if this area is stimulated during sexual activity.[49][51] A G-spot orgasm may be responsible for female ejaculation, leading some doctors and researchers to believe that G-spot pleasure comes from the Skene's glands, a female homologue of the prostate, rather than any particular spot on the vaginal wall; other researchers consider the connection between the Skene's glands and the G-spot area to be weak.[49][50][51] The G-spot's existence, and existence as a distinct structure, is still under dispute, as its reported location can vary from woman to woman, appears to be nonexistent in some women, and it is hypothesized to be an extension of the clitoris and therefore the reason for orgasms experienced vaginally.[49][53][65]
Childbirth

The vagina provides a channel to deliver a newborn to its independent life outside the body of the mother. When childbirth (or labor) nears, several symptoms may occur, including vaginal discharge, and the rupture of membranes and resulting gush of amniotic fluid through the vagina (also known as water breaking).[70] When the water breaks, there can be an irregular or small stream of fluid from the vagina, or a gush of fluid.[71][72]
When the body prepares for childbirth, the cervix softens, thins, moves forward to face the front, and may begin to open. This allows the fetus to settle or "drop" into the pelvis.[70] When the fetus settles into the pelvis, this may result in pain in the sciatic nerves, increased vaginal discharge, and increased urinary frequency. While these symptoms are likelier to happen after labor has already begun for women who have given birth before, they may happen approximately ten to fourteen days before labor in women experiencing the effects of nearing labor for the first time.[70]
The fetus begins to lose the support of the cervix when uterine contractions begin. With cervical dilation reaching a diameter of more than 10 cm (4 in) to accommodate the head of the fetus, the head moves from the uterus to the vagina.[70] The elasticity of the vagina allows it to stretch to many times its normal diameter in order to deliver the child.[20]
Injections for pain control during childbirth is often administered through the vaginal wall and near the pudendal nerve. This nerve carries sensations to the lower part of the vagina and vulva. This is only used late in labor, usually right before the baby's head comes out. With a pudendal nerve block, there is some relief from the pain and the laboring woman remains awake, alert, and able to push the baby out. The baby is not affected by this medicine and it has very few disadvantages.[73]
Vaginal births are more common, but there are sometimes complications and a woman might undergo a caesarean section (commonly known as a C-section) instead of a vaginal delivery. The vaginal mucosa has an abnormal accumulation of fluid (edematous) and is thin, with few rugae, a little after birth. The mucosa thickens and rugae return in approximately three weeks once the ovaries regain usual function and estrogen flow is restored. The vaginal opening gapes and is relaxed, until it returns to its approximate pre-pregnant state by six to eight weeks in the period beginning immediately after the birth (the postpartum period); however, it will maintain a larger shape than it previously had.[74]
Vaginal microbiota
The vagina is a complex ecosystem that undergoes long-term changes throughout the life of a woman, from birth to menopause. The vaginal microbiota resides in and on the outermost layer of the vaginal epithelium.[17] This microbiome consists of species and genera which typically do not cause symptoms or infections in women with normal immunity. The vaginal microbiome is dominated by Lactobacillus species.[75] These species metabolize glycogen, breaking it down into sugar. Lactobacilli metabolize the sugar into glucose and lactic acid. Under the influence of hormones, such as estrogen, progesterone and follicle-stimulating hormone (FSH), the vaginal ecosystem undergoes cyclic or periodic changes.[76] When the normal Lactobacillus-based microbiota changes to a microbiome populated by bacteria characteristic of Bacterial Vaginosis the risk of adverse pregnancy outcome is greater.[77]
Clinical significance
General
The vagina is self-cleansing and therefore usually does not need special hygiene.[78] Clinicians generally discourage the practice of douching for maintaining vulvovaginal health.[78] Since a healthy vagina is colonized by a mutually symbiotic flora of microorganisms that protect its host from disease-causing microbes, any attempt to upset this balance may cause many undesirable outcomes, including abnormal discharge and yeast infection.[78]
The healthy vagina of a woman of child-bearing age is acidic, with a pH normally ranging between 3.8 and 4.5.; this is due to the degradation of glycogen to lactic acid by enzymes secreted by the Döderlein's bacillus, which is a normal commensal of the vagina.[76] The acidity delays or slows the growth of many strains of pathogenic microbes.[76] An increased pH of the vagina (with a commonly used cut-off of pH 4.5 or higher) can be caused by bacterial overgrowth, as occurs in bacterial vaginosis and trichomoniasis, or rupture of membranes in pregnancy.[76][79] There are different types of bacterial vaginosis.[76]
The acidic balance of the vagina may also be affected by pregnancy, menstruation, diabetes, oral contraceptive pills (birth control), certain antibiotics, illness, poor diet, and stress (such as from a lack of sleep).[80][81] Any of these changes to the acidic balance of the vagina may contribute to yeast infection.[80]
The multiple layers of the vagina provide protection from pathogens, such as Chlamydia trachomatis and Neisseria gonorrhoeae.[17] The vaginal lymph nodes can trap cancerous cells that originate from the vagina so that they can be assessed for the presence of disease. Selective assessment (rather total and more invasive removal) of vaginal lymph nodes reduces the risk of complications that can accompany more radical surgeries. These selective nodes act as sentinel lymph nodes.[38] Instead of surgery, the lymph nodes of concern are sometimes treated with radiation therapy administered to the patient's pelvic or inguinal lymph nodes, or both.[82]
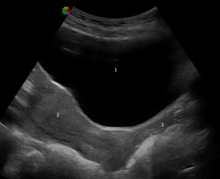
The vagina and cervix are examined during gynecological examinations of the pelvis, often using a speculum, which holds the vagina open for visual inspection or taking samples (see pap smear).[83] This and other medical procedures involving the vagina, including digital internal examinations and administration of medicine,[83][84] are referred to as being per vaginam, the Latin for "via the vagina",[85] often abbreviated to "p.v.".[84] Examination of the vagina may also be done during a cavity search.[86]

Intravaginal administration is a route of administration where the medication is applied to vaginal wall. Pharmacologically, it has the potential advantage to result in effects primarily in the vagina or nearby structures (such as the vaginal portion of cervix) with limited systemic adverse effects compared to other routes of administration.[87][88]
Injuries to the vagina can occur during sexual assault. These can be tears, bruises, inflammation and abrasions. Sexual assault with objects can damage the vagina and X-ray examination may reveal the presence of foreign objects.[4]
Effects of aging and childbirth
Average vaginal pH varies significantly during a woman's lifespan, from 7.0 in premenarchal girls, to 3.8-4.4 in women of reproductive age to 6.5-7.0 during menopause without hormone therapy and 4.5-5.0 with hormone replacement therapy (HRT).[89] Estrogen, glycogen and lactobacilli are important factors in this variation.[76]
After menopause, the body produces less estrogen, which causes the vaginal walls to thin out significantly.[10][30][90] The effects of menopause can lead to vaginal dryness (due to a decrease in vaginal lubrication), which causes vaginal discomfort on its own or discomfort or pain during sexual intercourse.[91] This can be alleviated with hormone replacement therapy,[92] estrogen-containing vaginal creams,[5] or non-prescription, non-hormonal products,[91] but there are risks and adverse effects associated with hormone replacement therapy.[93]
Vaginal support structures also change in composition after menopause. Specific collagens become altered in composition and ratios. It is thought that the weakening of the support structures of the vagina is due to the physiological changes in this connective tissue.[94]
Stress can impact every system of the body,[81] trigger hot flashes,[95] and make hot flashes worse during menopause,[81] although the exact origin of hot flashes are not well understood.[95] Some women have an increase in sexual desire following menopause.[91] Masters and Johnson's research indicates that menopausal women who continue to engage in sexual activity regularly experience vaginal lubrication similar to levels in women who have not entered menopause, and can enjoy sexual intercourse fully.[91]
Vaginal changes that happen with aging and childbirth include mucosal redundancy, rounding of the posterior aspect of the vagina with shortening of the distance from the distal end of the anal canal to the vaginal opening, diastasis or disruption of the pubococcygeus muscles caused by poor repair of an episiotomy, and blebs that may protrude beyond the area of the vaginal opening.[96] Other vaginal changes related to aging and childbirth are stress urinary incontinence, rectocele, and cystocele.[96] Similar vaginal and labial changes may be due to significant weight gain and subsequent loss.[96]
During the third stage of labor, while the infant is being born, the vagina undergoes significant changes. A gush of blood from the vagina may be seen right before the baby is born. Lacerations to the vagina that can occur during birth vary in depth, severity and the amount of adjacent tissue involvement.[4][97] The laceration can be so extensive as to involve the rectum and anus. This event can be especially distressing to a new mother.[97][98] When this occurs, fecal incontinence develops and stool can leave through the vagina.[97] Lacerations can occur unrelated to childbirth.[4]
Sometimes the attending physician performs an episiotomy. This is a surgical incision that widens the opening of the vagina to reduce the tissue resistance. It is performed right before the baby is born.[17][99] The incision is made through the skin, vaginal epithelium, subcutaneous fat, perineal body and superficial transverse perineal muscle and extends from the vagina to the anus.[100][101] The two types of episiotomies performed are the medial incision and the medio-lateral incision. The median incision is a perpendicular cut between the vagina and the anus and is the most common.[17][102] The medio-lateral incision is made between the vagina at an angle and is not as likely to tear through to the anus. The medio-lateral cut takes more time to heal than the median cut.[17] Lacerations and episiotomies can be painful after delivery. Some surgical techniques result in less pain than others. Close to 85% of spontaneous vaginal births develop some form of tearing. Out of these, 60-70% require suturing. Women often report pain during sexual intercourse up to three months after laceration repair or an episiotomy.[103][104] Lacerations from labor do not always happen, and not having an episiotomy is found to have better results than episiotomy.[17]
Infections, safe sex, and disorders
There are infections, diseases and disorders that can affect the vagina, including candidal vulvovaginitis, vaginitis, vaginismus, sexually transmitted infections (STIs) and cancer. Vaginitis is an inflammation of the vagina, and is attributed to several vaginal diseases, while vaginismus is an involuntary tightening of the vagina muscles caused by a conditioned reflex, or disease, during vaginal penetration.[105] HIV/AIDS, human papillomavirus (HPV), genital herpes and trichomoniasis are some of the STIs that may affect the vagina, and health sources recommend safe sex (or barrier method) practices to prevent the transmission of these and other STIs.[106][107]
Safe sex commonly involves the use of condoms (also known as male condoms), but female condoms, which give women more control during the safe sex practice, may also be used; both condoms keep semen from coming in contact with the vagina, which can help prevent unwanted pregnancy.[108][109] There is, however, little research on whether female condoms are as effective as male condoms at preventing STIs,[109] and they are slightly less effective than male condoms at preventing pregnancy, which may be due to the female condom not fitting as tightly as the male condom or because it can slip into the vagina and spill semen.[110]
Cervical cancer may be prevented by pap smear screening and HPV vaccines, but HPV vaccines only cover HPV types 16 and 18, the cause of 70% of cervical cancers.[111][112] Vaginal cancer and vulvar cancer are very rare, and are primarily matters for elderly women.[113][114] Because vaginal cancer often occurs at the same time or develops consequently in relation to cervical cancer, it may be that their causes are the same.[113][115] Some symptoms of cervical and vaginal cancer are dyspareunia, and abnormal vaginal bleeding or vaginal discharge, especially after sexual intercourse or menopause.[116][117] However, most cervical cancers are asymptomatic (present no symptoms).[116] Vaginal intracavity brachytherapy (VBT) is used to treat endometrial, vaginal and cervical cancer. An applicator is inserted into the vagina to allow the administration of radiation as close to the site of cancer as possible.[99][118] Survival rates increase with VBT when compared to external beam radiation therapy.[99] By using the vagina to place the emitter as close to the cancerous growth as possible, the systemic effects of radiation therapy are less and cure rates for vaginal cancer are higher.[119]
There can be a vaginal obstruction, such as one caused by agenesis, an imperforate hymen or, less commonly, a transverse vaginal septum; these cases require differentiation because surgery for them significantly varies.[120] When there is a lump obstructing the vaginal opening, it is likely a Bartholin's cyst.[121]
Vaginal prolapse is characterized by a portion of the vaginal canal protruding (prolapsing) from the opening of the vagina. It may result in the case of weakened pelvic muscles, which is a common result of childbirth; in the case of this prolapse, the rectum, uterus, or bladder pushes on the vagina, and severe cases result in the vagina protruding out of the body. Kegel exercises have been used to strengthen the pelvic floor, and may help prevent or remedy vaginal prolapse.[61]
Modification
The vagina, including the vaginal opening, may be altered as a result of genital modification during vaginectomy, vaginoplasty or labiaplasty.[96][122] Those who undergo vaginoplasty are usually older and have given birth to one or more children.[96] A thorough examination of the vagina before a vaginoplasty is standard, as well as being referred to a urogynecologist for possible vaginal disorders.[96] With regard to labiaplasty, reduction of the labia minora is quick without hindrance, and any complications are rare and can be corrected. The complications are minor enough that those with them may still be satisfied with the procedure. Any scarring from the procedure is minimal, and long-term chronic problems have not been identified.[96]
Vaginectomy is surgery to remove all or part of the vagina, and is usually used as a treatment for vaginal cancer.[122] The vulva or vagina may be altered in the case of gynecologic cancers (such as cervical cancer, vaginal cancer or vulvar cancer). Removal of some or all of the reproductive organs and genitalia can result in damage to the nerves and leave behind scarring or adhesions.[123] Sexual function may also be impaired as a result, as in the case of some cervical cancer surgeries, which impact vaginal lubrication, elasticity, pain, and sexual arousal. This mostly resolves after one year of recovery, but remedying vaginal dryness and decreased sexual satisfaction may take longer.[123]
Female genital mutilation (FGM), another aspect of female genital modification, may additionally be known as female circumcision or female genital cutting (FGC).[124][125] FGM has no known health benefits. The most severe form of FGM is infibulation, in which there is removal of all or part of the inner and outer labia (labia minora and labia majora) and the closure of the vagina; this is called Type III FGM, and it involves a small hole being left for the passage of urine and menstrual blood, with the vagina being opened up for sexual intercourse and childbirth.[125]
Society and culture
Perceptions, symbolism and vulgarity
Various perceptions of the vagina have existed throughout history, including the belief it is the center of sexual desire, a metaphor for life via birth, inferior to the penis, unappealing to sight or smell, or vulgar.[126][127][128] These views can largely be attributed to sex differences, and how they are interpreted. David Buss, an evolutionary psychologist, stated that because a penis is significantly larger than a clitoris and it is readily visible while the vagina is not, and males urinate through the penis, boys are taught from childhood to touch their penises while girls are often taught that they should not touch their vulva or vagina, which implies that there is harm in doing so. Buss attributed this to the reason why many women are not as familiar with their genitalia as men are familiar with their own, and that researchers assume these sex differences explain why boys learn to masturbate before girls, and masturbate more often than girls.[129]
The word vagina is commonly avoided in conversation,[130] and many people are confused about the vagina's anatomy, including that it is not used for urination.[131][132][133] This is exacerbated by phrases such as "boys have a penis, girls have a vagina", which causes children to think that girls have one orifice in the pelvic area.[132] Author Hilda Hutcherson stated, "Because many [women] have been conditioned since childhood through verbal and nonverbal cues to think of [their] genitals as ugly, smelly and unclean, [they] aren't able to fully enjoy intimate encounters" because of fear that their partner will dislike the sight, smell, or taste of their genitals. She argued that women, unlike men, did not have locker room experiences in school where they compared each other's genitals, which is one reason so many women wonder if their genitals are normal.[127] Scholar Catherine Blackledge stated that having a vagina meant she would typically be treated less well than her vagina-less counterparts and subject to inequalities (such as job inequality), which she categorized as being treated like a second-class citizen.[130]

Negative views of the vagina are simultaneously contrasted by views that it is a powerful symbol of female sexuality, spirituality, or life. Author Denise Linn stated that the vagina "is a powerful symbol of womanliness, openness, acceptance, and receptivity. It is the inner valley spirit."[134] Sigmund Freud placed significant value on the vagina,[135] postulating the concept of vaginal orgasm, that it is separate from clitoral orgasm, and that, upon reaching puberty, the proper response of mature women is a change-over to vaginal orgasms (meaning orgasms without any clitoral stimulation). This theory made many women feel inadequate, as the majority of women cannot achieve orgasm via vaginal intercourse alone.[136][137][138] Regarding religion, the vagina represents a powerful symbol as the yoni in Hinduism, and this may indicate the value that Hindu society has given female sexuality and the vagina's ability to birth life.[139]
While, in ancient times, the vagina was often considered equivalent (homologous) to the penis, with anatomists Galen (129 AD – 200 AD) and Vesalius (1514–1564) regarding the organs as structurally the same except for the vagina being inverted, anatomical studies over latter centuries showed the clitoris to be the penile equivalent.[64][140] Another perception of the vagina was that the release of vaginal fluids would cure or remedy a number of ailments; various methods were used over the centuries to release "female seed" (via vaginal lubrication or female ejaculation) as a treatment for suffocation ex semine retento (suffocation of the womb), green sickness, and possibly for female hysteria. Reported methods for treatment included a midwife rubbing the walls of the vagina or insertion of the penis or penis-shaped objects into the vagina. Symptoms of the female hysteria diagnosis – a concept that is no longer recognized by medical authorities as a medical disorder – included faintness, nervousness, insomnia, fluid retention, heaviness in abdomen, muscle spasm, shortness of breath, irritability, loss of appetite for food or sex, and a propensity for causing trouble.[141] It may be that women who were considered suffering from female hysteria condition would sometimes undergo "pelvic massage" – stimulation of the genitals by the doctor until the woman experienced "hysterical paroxysm" (i.e., orgasm). In this case, paroxysm was regarded as a medical treatment, and not a sexual release.[141]
The vagina and vulva have additionally been termed many vulgar names, three of which are cunt, twat, and pussy. Cunt is also used as a derogatory epithet referring to people of either sex. This usage is relatively recent, dating from the late nineteenth century.[142] Reflecting different national usages, cunt is described as "an unpleasant or stupid person" in the Compact Oxford English Dictionary,[143] whereas Merriam-Webster has a usage of the term as "usually disparaging and obscene: woman,"[144] noting that it is used in the U.S. as "an offensive way to refer to a woman."[145] Random House defines it as "a despicable, contemptible or foolish man."[142] Some feminists of the 1970s sought to eliminate disparaging terms such as cunt.[146] Twat is widely used as a derogatory epithet, especially in British English, referring to a person considered obnoxious or stupid.[147][148] Pussy can indicate "cowardice or weakness", and "the human vulva or vagina" or by extension "sexual intercourse with a woman".[149] In contemporary English, use of the word pussy to refer to women is considered derogatory or demeaning, treating people as sexual objects.[150]
In contemporary literature and art

The vagina loquens, or "talking vagina", is a significant tradition in literature and art, dating back to the ancient folklore motifs of the "talking cunt".[151][152] These tales usually involve vaginas talking due to the effect of magic or charms, and often admitting to their unchastity.[151] Another folk tale regarding the vagina is "vagina dentata" (Latin for "toothed vagina"). In these folk tales, a woman's vagina is said to contain teeth, with the associated implication that sexual intercourse might result in injury, emasculation, or castration for the man involved. These stories were frequently told as cautionary tales warning of the dangers of unknown women and to discourage rape.[153]
In 1966, the French artist Niki de Saint Phalle collaborated with Dadaist artist Jean Tinguely and Per Olof Ultvedt on a large sculpture installation entitled "hon-en katedral" (also spelled "Hon-en-Katedrall", which means "she-a cathedral") for Moderna Museet, in Stockholm, Sweden. The outer form is a giant, reclining sculpture of a woman with her legs spread. Museum patrons can go inside her body by entering a door-sized vaginal opening.[154] Sainte Phalle stated that the sculpture represented a fertility goddess who was able to receive visitors into her body and then "give birth" to them again.[155]
From 1974 to 1979, Judy Chicago, a feminist artist, created the vagina-themed installation artwork "The Dinner Party". It consists of 39 elaborate place settings arranged along a triangular table for 39 mythical and historical famous women. Virginia Woolf, Susan B. Anthony, Sojourner Truth, Eleanor of Aquitaine, and Theodora of Byzantium are among those honored. Each plate, except the one corresponding to Sojourner Truth (a Black woman), depicts a brightly-colored, elaborately styled vagina-esque form. After it was produced, despite resistance from the art world, it toured to 16 venues in six countries to a viewing audience of 15 million.[156]
The Vagina Monologues, a 1996 episodic play by Eve Ensler, has contributed to making female sexuality a topic of public discourse. It is made up of a varying number of monologues read by a number of women. Initially, Ensler performed every monologue herself, with subsequent performances featuring three actresses; latter versions feature a different actress for every role. Each of the monologues deals with an aspect of the feminine experience, touching on matters such as sexual activity, love, rape, menstruation, female genital mutilation, masturbation, birth, orgasm, the various common names for the vagina, or simply as a physical aspect of the body. A recurring theme throughout the pieces is the vagina as a tool of female empowerment, and the ultimate embodiment of individuality.[157][158]
In 2012, an image of an 1866 Gustave Courbet painting of the female genitals, entitled "The Origin of the World", being posted on Facebook led to a legal dispute. After a French teacher posted an image of the painting, Facebook considered the image to be pornographic and suspended his account for violating its terms of use.[159] G. Roger Denson of Huff Post called the painting "a frank image of a vagina."[160] Mark Stern of Slate, who called the painting a stunning, brilliant "....cornerstone of the French Realistic movement", stated that the teacher sued the website for allegedly violating his freedom of speech.[159] In October 2013, artist Peter Reynosa created a "... red and white acrylic painting [that] depicts [pop singer] Madonna painted in the shape of a defiant yonic symbol that looks like a vagina or vulva."[161]
Cosmetic or traditional reasons for vaginal modification
Cosmetic reasons for modification of the female genitalia may be due to FGM, voluntary cosmetic operations, or surgery for intersex conditions.[162] There are two main categories of women seeking cosmetic genital surgery: those with congenital conditions (such as an intersex condition), and those with no underlying condition who experience physical discomfort or wish to alter the appearance of their genitals because they believe they do not fall within a normal range.[162]
Significant controversy surrounds FGM,[124][125] with the World Health Organization (WHO) being one of many health organizations that have campaigned against the procedures on behalf of human rights, stating that it is "a violation of the human rights of girls and women" and "reflects deep-rooted inequality between the sexes".[125] FGM has existed at one point or another in almost all human civilizations,[163] most commonly to exert control over the sexual behavior, including masturbation, of girls and women.[125][163] It is carried out in several countries, especially in Africa, and to a lesser extent in other parts of the Middle East and Southeast Asia, on girls from a few days old to mid-adolescent, often to reduce sexual desire in an effort to preserve vaginal virginity.[124][125][163] Comfort Momoh stated it may be that FGM was "practiced in ancient Egypt as a sign of distinction among the aristocracy"; there are reports that traces of infibulation are on Egyptian mummies.[163]
Custom and tradition are the most frequently cited reasons for FGM, with some cultures believing that not performing it has the possibility of disrupting the cohesiveness of their social and political systems, such as FGM also being a part of a girl's initiation into adulthood.[125][163] Often, a girl is not considered an adult in a FGM-practicing society unless she has undergone FGM.[125]
Other animals
The vagina is a feature of animals in which the female is internally fertilized, rather than by traumatic insemination used by some invertebrates. The shape of the vagina varies among different animals. In placental mammals and marsupials, the vagina leads from the uterus to the exterior of the female body. Female marsupials have two lateral vaginas, which lead to separate uteri, but both open externally through the same orifice.[164] The female spotted hyena does not have an external vagina. Instead, the vagina exits through the clitoris, allowing the females to urinate, copulate and give birth through the clitoris.[165] The female vagina of the coyote contracts during copulation, forming a copulatory tie.[166]
In the case of other animals, birds, monotremes, and some reptiles have a part of the oviduct that leads to the cloaca.[167][168] Chickens have a vaginal aperture that opens from the vertical apex of the cloaca. The vagina extends upward from the aperture and becomes the egg gland.[168] In some jawless fish, there is neither oviduct nor vagina and instead the egg travels directly through the body cavity (and is fertilised externally as in most fish and amphibians). In insects and other invertebrates, the vagina can be a part of the oviduct (see insect reproductive system).[169] Females of some waterfowl species have developed vaginal structures called dead end sacs and clockwise coils to protect themselves from sexual coercion.[170]
In 2014, the scientific journal Current Biology reported that four species of Brazilian insects in the genus Neotrogla were found to have sex-reversed genitalia. The male insects of those species have vagina-like openings, while the females have penis-like organs.[171][172][173]
See also
References
- ^ Stevenson A (2010). Oxford Dictionary of English. Oxford University Press. p. 1962. ISBN 0199571120.
- ^ Nevid J, Rathus S, Rubenstein H (1998). Health in the New Millennium: The Smart Electronic Edition (S.E.E.). Macmillan. p. 297. ISBN 1572591714.
- ^ Lipsky MS (2006). American Medical Association Concise Medical Encyclopedia. Random House Reference. p. 96. ISBN 0375721800.
- ^ a b c d e f g Dalton M (2014). Forensic Gynaecology. Cambridge University Press. p. 65. ISBN 1107064295.
- ^ a b Jones T, Wear D, Friedman LD (2014). Health Humanities Reader. Rutgers University Press. pp. 231–232. ISBN 081357367X.
- ^ a b Kirkpatrick M (2012). Human Sexuality: Personality and Social Psychological Perspectives. Springer Science & Business Media. p. 175. ISBN 1468436562.
- ^ a b Hill CA (2007). Human Sexuality: Personality and Social Psychological Perspectives. Sage Publications. pp. 265–266. ISBN 1506320120.
Little thought apparently has been devoted to the nature of female genitals in general, likely accounting for the reason that most people use incorrect terms when referring to female external genitals. The term typically used to talk about female genitals is vagina, which is actually an internal sexual structure, the muscular passageway leading outside from the uterus. The correct term for the female external genitals is vulva, as discussed in chapter 6, which includes the clitoris, labia majora, and labia minora.
- ^ Sáenz-Herrero M (2014). Psychopathology in Women: Incorporating Gender Perspective into Descriptive Psychopathology. Springer. p. 250. ISBN 3319058703.
In addition, there is a current lack of appropriate vocabulary to refer to the external female genitals, using, for example, 'vagina' and 'vulva' as if they were synonyms, as if using these terms incorrectly were harmless to the sexual and psychological development of women.'
- ^ a b c d e Snell RS (2004). Clinical Anatomy: An Illustrated Review with Questions and Explanations. Lippincott Williams & Wilkins. p. 98. ISBN 978-0-7817-4316-7.
- ^ a b c d e f g h i j k l m n o p q r Dutta DC (2014). DC Dutta's Textbook of Gynecology. JP Medical Ltd. pp. 2–7. ISBN 9351520684.
- ^ a b c d e f g Standring S, Borley NR, eds. (2008). Gray's anatomy : the anatomical basis of clinical practice (40th ed.). London: Churchill Livingstone. p. 1281–4. ISBN 978-0-8089-2371-8.
- ^ a b Mulhall JP (2011). Mulhall JP, Incrocci L, Goldstein I, Rosen R (eds.). Cancer and Sexual Health. Springer. pp. 13, 20–21. ISBN 1-60761-915-6.
- ^ Ransons A (May 15, 2009). "Reproductive Choices". Health and Wellness for Life. Human Kinetics 10%. p. 221. ISBN 978-0-7360-6850-5. Retrieved July 30, 2013.
- ^ Beckmann CR (2010). Obstetrics and Gynecology. Lippincott Williams & Wilkins. p. 37. ISBN 0781788072.
Because the vagina is collapsed, it appears H-shaped in cross section.
- ^ a b Manual of Obstetrics (3rd ed.). Elsevier. 2011. pp. 1–16. ISBN 9788131225561.
- ^ Snell RS (2012). Clinical anatomy by regions (9th ed.). Baltimore: Lippincott Williams & Wilkins. p. 288. ISBN 978-1609134464.
- ^ a b c d e f g h i j Anderson DJ, Marathe J, Pudney J (June 2014). "The Structure of the Human Vaginal Stratum Corneum and its Role in Immune Defense". American Journal of Reproductive Immunology. 71 (6): 618–623. doi:10.1111/aji.12230. ISSN 1600-0897.
- ^ a b Knight B (1997). Simpson's Forensic Medicine (11th ed.). London: Arnold. p. 114. ISBN 0-7131-4452-1.
- ^ Perlman SE, Nakajyma ST, Hertweck SP (2004). Clinical protocols in pediatric and adolescent gynecology. Parthenon. p. 131. ISBN 1-84214-199-6.
- ^ a b c Wylie L (2005). Essential Anatomy and Physiology in Maternity Care. Elsevier Health Sciences. pp. 157–158. ISBN 0-443-10041-1.
- ^ Emans SJ (2000). "Physical Examination of the Child and Adolescent". Evaluation of the Sexually Abused Child: A Medical Textbook and Photographic Atlas (2nd ed.). Oxford University Press. pp. 61–65. ISBN 0199747822.
- ^ a b c d e Edmonds K (2012). Dewhurst's Textbook of Obstetrics and Gynaecology. John Wiley & Sons. p. 423. ISBN 0470654570.
- ^ Merz E, Bahlmann F (2004). Ultrasound in Obstetrics and Gynecology. Vol. 1. Thieme Medical Publishers. p. 129. ISBN 978-1-58890-147-7.
- ^ Schuenke M, Schulte E, Schumacher U (2010). General Anatomy and Musculoskeletal System. Thieme Medical Publishers. p. 192. ISBN 978-1-60406-287-8.
- ^ Cai Y (2009). "Revisiting old vaginal topics: conversion of the Müllerian vagina and origin of the "sinus" vagina". Int J Dev Biol. 53 (7): 925–34. doi:10.1387/ijdb.082846yc. PMID 19598112.
- ^ Brown L (2012). Pathology of the Vulva and Vagina. Springer Science+Business Media. pp. 6–7. ISBN 0857297570.
- ^ a b Arulkumaran S, Regan L, Papageorghiou A, Monga A, Farquharson D (2011). Oxford Desk Reference: Obstetrics and Gynaecology. Oxford University Press. p. 471. ISBN 0191620874.
- ^ Mayeaux EJ, Cox JT (2011). Modern Colposcopy Textbook and Atlas. Lippincott Williams & Wilkins. ISBN 145115383X.
- ^ a b c Kurman RJ, ed. (2002). Blaustein's Pathology of the Female Genital Tract (5th ed.). Spinger. p. 154.
- ^ a b c Beckmann CR (2010). Obstetrics and Gynecology. Lippincott Williams & Wilkins. pp. 241–245. ISBN 0781788072.
- ^ a b c d Robboy SJ (2009). Robboy's Pathology of the Female Reproductive Tract. Elsevier Health Sciences. p. 111. ISBN 0443074771.
- ^ Nunn KL, Forney LJ (September 2016). "Unraveling the Dynamics of the Human Vaginal Microbiome". The Yale Journal of Biology and Medicine. 89 (3): 331–337. ISSN 0044-0086. PMC 5045142. PMID 27698617.
- ^ Gupta R (2011). Reproductive and developmental toxicology. London: Academic Press. p. 1005. ISBN 978-0-12-382032-7.
{{cite book}}: Cite has empty unknown parameter:|1=(help) - ^ Gad SC (2008). Pharmaceutical Manufacturing Handbook: Production and Processes. John Wiley & Sons. p. 817. ISBN 0470259809.
- ^ Dutta DC (2014). DC Dutta's Textbook of Gynecology. JP Medical Ltd. p. 206. ISBN 9351520684.
- ^ a b Zimmern PE, Haab F, Chapple CR (2007). Vaginal Surgery for Incontinence and Prolapse. Springer Science & Business Media. p. 6. ISBN 1846283469.
- ^ O'Rahilly R (2008). "Blood vessels, nerves and lymphatic drainage of the pelvis". In O'Rahilly R, Müller F, Carpenter S, Swenson R (eds.). Basic Human Anatomy: A Regional Study of Human Structure. Dartmouth Medical School. Retrieved December 13, 2017.
- ^ a b Sabater S, Andres I, Lopez-Honrubia V, Berenguer R, Sevillano M, Jimenez-Jimenez E, Rovirosa A, Arenas M (August 9, 2017). "Vaginal cuff brachytherapy in endometrial cancer – a technically easy treatment?". Cancer Management and Research. 9: 351–362. doi:10.2147/CMAR.S119125. ISSN 1179-1322. PMC 5557121. PMID 28848362.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Wangikar P, Ahmed T, Vangala S (2011). "Toxicologic pathology of the reproductive system". In Gupta RC (ed.). Reproductive and developmental toxicology. London: Academic Press. p. 1005. ISBN 9780123820327. OCLC 717387050.
- ^ a b Sloane E (2002). Biology of Women. Cengage Learning. pp. 32, 41–42. ISBN 0-7668-1142-5.
- ^ Bourcier A, McGuire EJ, Abrams P (2004). Pelvic Floor Disorders. Elsevier Health Sciences. p. 20. ISBN 0-7216-9194-3.
- ^ Wiederman MW, Whitley BE Jr (2012). Handbook for Conducting Research on Human Sexuality. Psychology Press. ISBN 978-1-135-66340-7.
- ^ Cummings M (2006). Human Heredity: Principles and Issues (Updated ed.). Cengage Learning. pp. 153–154. ISBN 0495113085.
- ^ Sirven JI, Malamut BL (2008). Clinical Neurology of the Older Adult. Lippincott Williams & Wilkins. pp. 230–232. ISBN 0781769477.
- ^ a b Lee MT (2013). Love, Sex and Everything in Between. Marshall Cavendish International Asia Pte Ltd. p. 76. ISBN 9814516783.
- ^ a b c Sex and Society. Vol. 2. Marshall Cavendish Corporation. 2009. p. 590. ISBN 9780761479079.
- ^ a b c Weiten W, Dunn D, Hammer E (2011). Psychology Applied to Modern Life: Adjustment in the 21st Century. Cengage Learning. p. 386. ISBN 1-111-18663-4.
- ^ a b Greenberg JS, Bruess CE, Conklin SC (2010). Exploring the Dimensions of Human Sexuality. Jones & Bartlett Publishers. p. 126. ISBN 9814516783.
- ^ a b c d e Greenberg JS, Bruess CE, Oswalt SB (2014). Exploring the Dimensions of Human Sexuality. Jones & Bartlett Publishers. pp. 102–104. ISBN 1449648517.
- ^ a b Hines T (August 2001). "The G-Spot: A modern gynecologic myth". Am J Obstet Gynecol. 185 (2): 359–62. doi:10.1067/mob.2001.115995. PMID 11518892.
- ^ a b c Bullough VL, Bullough B (2014). Human Sexuality: An Encyclopedia. Routledge. pp. 229–231. ISBN 1135825092.
- ^ Asthana NC, Nirmal A (2010). Myth Buster: 150 Great Misconceptions Clarified. Sterling Publishers Pvt. Ltd. p. 96. ISBN 8120742109.
- ^ a b Balon R, Segraves RT (2009). Clinical Manual of Sexual Disorders. American Psychiatric Pub. p. 258. ISBN 1585629057.
- ^ Rosenthal M (2012). Human Sexuality: From Cells to Society. Cengage Learning. p. 76. ISBN 0-618-75571-3.
- ^ Carroll J (2012). Discovery Series: Human Sexuality. Cengage Learning. pp. 282–289. ISBN 1111841896.
- ^ Strong B, DeVault C, Cohen TF (2010). The Marriage and Family Experience: Intimate Relationship in a Changing Society. Cengage Learning. p. 186. ISBN 0-534-62425-1.
Most people agree that we maintain virginity as long as we refrain from sexual (vaginal) intercourse. But occasionally we hear people speak of 'technical virginity' [...] Data indicate that 'a very significant proportion of teens ha[ve] had experience with oral sex, even if they haven't had sexual intercourse, and may think of themselves as virgins' [...] Other research, especially research looking into virginity loss, reports that 35% of virgins, defined as people who have never engaged in vaginal intercourse, have nonetheless engaged in one or more other forms of heterosexual sexual activity (e.g., oral sex, anal sex, or mutual masturbation).
- ^ See 272 and page 301 for two different definitions of outercourse (first of the pages for no-penetration definition; second of the pages for no-penile-penetration definition). Rosenthal M (2012). Human Sexuality: From Cells to Society (1st ed.). Cengage Learning. ISBN 0618755713.
- ^ Carroll JL (2009). Sexuality Now: Embracing Diversity. Cengage Learning. p. 272. ISBN 0-495-60274-4.
- ^ Zenilman J, Shahmanesh M (2011). Sexually Transmitted Infections: Diagnosis, Management, and Treatment. Jones & Bartlett Publishers. pp. 329–330. ISBN 0495812943.
- ^ Taormino T (2009). The Big Book of Sex Toys. Quiver. p. 52. ISBN 978-1-59233-355-4.
- ^ a b Hagen S, Stark D (2011). "Conservative prevention and management of pelvic organ prolapse in women". Cochrane Database Syst Rev. 12 (12): CD003882. doi:10.1002/14651858.CD003882.pub4. PMID 22161382.
- ^ a b Pitts-Taylor V (2008). Cultural Encyclopedia of the Body. Greenwood Publishing Group. p. 525. ISBN 0313341451.
- ^ Kramarae C, Spender D (2004). Routledge International Encyclopedia of Women: Global Women's Issues and Knowledge. Routledge. p. 1840. ISBN 1135963150.
- ^ a b O'Connell HE, Sanjeevan KV, Hutson JM (October 2005). "Anatomy of the clitoris". The Journal of Urology. 174 (4 Pt 1): 1189–95. doi:10.1097/01.ju.0000173639.38898.cd. PMID 16145367.
{{cite journal}}: Unknown parameter|laydate=ignored (help); Unknown parameter|laysource=ignored (help); Unknown parameter|laysummary=ignored (help) - ^ a b Kilchevsky A, Vardi Y, Lowenstein L, Gruenwald I (January 2012). "Is the Female G-Spot Truly a Distinct Anatomic Entity?". The Journal of Sexual Medicine. 9 (3): 719–26. doi:10.1111/j.1743-6109.2011.02623.x. PMID 22240236.
{{cite journal}}: Unknown parameter|laydate=ignored (help); Unknown parameter|laysource=ignored (help); Unknown parameter|laysummary=ignored (help) - ^ a b c Heffner LJ, Schust DJ (2014). The Reproductive System at a Glance. John Wiley & Sons. p. 39. ISBN 1118607015.
- ^ Silbernagl S, Despopoulos A (2011). Color Atlas of Physiology. Thieme. p. 310. ISBN 1449648517.
- ^ Carroll JL (2015). Sexuality Now: Embracing Diversity. Cengage Learning. p. 271. ISBN 1305446038.
- ^ Brewster S, Bhattacharya S, Davies J, Meredith S, Preston P (2011). The Pregnant Body Book. Penguin. pp. 66–67. ISBN 0756687128.
- ^ a b c d Orshan SA (2008). Maternity, Newborn, and Women's Health Nursing: Comprehensive Care Across the Lifespan. Lippincott Williams & Wilkins. pp. 585–586. ISBN 0781742544.
- ^ Evans JM, Aronson R (2005). The Whole Pregnancy Handbook: An Obstetrician's Guide to Integrating Conventional and Alternative Medicine Before, During, and After Pregnancy. Penguin. pp. 435–436. ISBN 1592401112.
- ^ Boston Women's Health Book Collective (2008). Our Bodies, Ourselves: Pregnancy and Birth. Simon & Schuster. pp. 172–174. ISBN 1416565914.
- ^ Maclean A, Reid W (2011). "40". In Shaw R (ed.). Gynaecology. Edinburgh New York: Churchill Livingstone/Elsevier. pp. 599–612. ISBN 978-0-7020-3120-5.
- ^ Ricci SS, Kyle T (2009). Maternity and Pediatric Nursing. Lippincott Williams & Wilkins. pp. 431–432. ISBN 0781780551.
- ^ Petrova MI, Lievens E, Malik S, Imholz N, Lebeer S (2015). "Lactobacillus species as biomarkers and agents that can promote various aspects of vaginal health". Frontiers in Physiology. 6. doi:10.3389/fphys.2015.00081. ISSN 1664-042X.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ a b c d e f King TL, Brucker MC (2010). Pharmacology for Women's Health. Jones & Bartlett Publishers. pp. 951–953. ISBN 1449610730.
- ^ Lamont RF, Sobel JD, Akins RA, Hassan SS, Chaiworapongsa T, Kusanovic JP, Romero R (April 2011). "The vaginal microbiome: new information about genital tract flora using molecular based techniques". BJOG: An International Journal of Obstetrics & Gynaecology. 118 (5): 533–549. doi:10.1111/j.1471-0528.2010.02840.x. ISSN 1471-0528. PMC 3055920. PMID 21251190.
- ^ a b c Grimes JA, Smith LA, Fagerberg K (2013). Sexually Transmitted Disease: An Encyclopedia of Diseases, Prevention, Treatment, and Issues: An Encyclopedia of Diseases, Prevention, Treatment, and Issues. ABC-CLIO. pp. 144, 590–592. ISBN 1440801355.
- ^ Alldredge BK, Corelli RL, Ernst ME (2012). Koda-Kimble and Young's Applied Therapeutics: The Clinical Use of Drugs. Lippincott Williams & Wilkins. pp. 1636–1641. ISBN 1609137132.
- ^ a b AAOS (2011). AEMT: Advanced Emergency Care and Transportation of the Sick and Injured. Jones & Bartlett Publishers. p. 766. ISBN 1449684289.
- ^ a b c Leifer G (2014). Introduction to Maternity and Pediatric Nursing - E-Book. Elsevier Health Sciences. p. 276. ISBN 0323293581.
- ^ "Stage I Vaginal Cancer". National Cancer Institute. National Institutes of Health. February 9, 2017. Retrieved December 14, 2017.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ^ a b Vickery DM, Fries JF (2013). Take Care of Yourself: The Complete Illustrated Guide to Medical Self-Care. Da Capo Press. pp. 427–428. ISBN 0786752181.
- ^ a b Hinrichsen C, Lisowski P (2007). Anatomy Workbook. World Scientific Publishing Company. p. 101. ISBN 9812569065.
Digital examination per vaginam are made by placing one or two fingers in the vagina.
- ^ Anderson DM, ed. (2002). Mosby's Medical, Nursing & Allied Health Dictionary (6th UK ed.). St. Louis, Missouri: Mosby. p. 1324. ISBN 0-7234-3225-2.
- ^ Stering R (2004). Police Officer's Handbook: An Introductory Guide. Jones & Bartlett Learning. p. 80. ISBN 0763747890.
- ^ Ranade VV, Cannon JB (2011). Drug Delivery Systems (3rd ed.). CRC Press. p. 337. ISBN 1439806187.
- ^ Lehne RA, Rosenthal L (2014). Pharmacology for Nursing Care. Elsevier Health Sciences. p. 1146. ISBN 0323293549.
- ^ Danielsson D, Teigen PK, Moi H (August 2011). "The genital econiche: focus on microbiota and bacterial vaginosis". Annals of the New York Academy of Sciences. 1230: 48–58. doi:10.1111/j.1749-6632.2011.06041.x. PMID 21824165.
- ^ Di Saia PH (2012). Clinical Gynecologic Oncology. Elsevier Health Sciences. p. 140. ISBN 0323074197.
- ^ a b c d Ward S, Hisley S (2015). Maternal-Child Nursing Care Optimizing Outcomes for Mothers, Children, & Families. F. A. Davis Company. pp. 147–150. ISBN 0803644906.
- ^ Jones RE, Davis KH (2013). Human Reproductive Biology. Academic Press. p. 127. ISBN 0123821851.
- ^ Greenstein B, Greenstein A (2007). Concise Clinical Pharmacology. Pharmaceutical Press. p. 186. ISBN 0853695768.
- ^ Walters MD, Karram MM (2015). Urogynecology and reconstructive pelvic surgery (4th ed.). Philadelphia: Elsevier Saunders. pp. 60–82. ISBN 9780323113779. OCLC 894111717.
- ^ a b Winterton ME, Mayhew MS (2013). Pharmacology for the Primary Care Provider - E-Book. Elsevier Health Sciences. p. 631. ISBN 0323087914.
- ^ a b c d e f g Siemionow MZ, Eisenmann-Klein M (2010). Plastic and Reconstructive Surgery. Springer Science & Business Media. pp. 688–690. ISBN 1848825137.
- ^ a b c Durham R, Chapman L (2014). Maternal-newborn nursing : the critical components of nursing care (2nd ed.). Philadelphia. pp. 212–213. ISBN 9780803637047. OCLC 829937238.
{{cite book}}: CS1 maint: location missing publisher (link) - ^ Kettle C (August 2010). "Absorbable suture materials for primary repair of episiotomy and second degree tears". Journal of Evidence-Based Medicine. 3 (3): 185–185. doi:10.1111/j.1756-5391.2010.01093.x. ISSN 1756-5391.
- ^ a b c "Cervical, Endometrial, Vaginal and Vulvar Cancers - Gynecologic Brachytherapy". radonc.ucla.edu. Retrieved December 13, 2017.
- ^ "Episiotomy: MedlinePlus Medical Encyclopedia". Medlineplus.gov. Retrieved December 13, 2017.
- ^ Ellis H, Mahadevan V (2013). Clinical anatomy : applied anatomy for students and junior doctors (13th ed.). Chichester, West Sussex, UK: Wiley-Blackwell. p. 148. ISBN 9781118373774. OCLC 856017698.
- ^ Verghese TS, Champaneria R, Kapoor DS, Latthe PM (October 2016). "Obstetric anal sphincter injuries after episiotomy: systematic review and meta-analysis". International Urogynecology Journal. 27 (10): 1459–1467. doi:10.1007/s00192-016-2956-1. ISSN 0937-3462.
- ^ Kettle C, Dowswell T, Ismail KM (2017). Comparative analysis of continuous and interrupted suturing techniques for repair of episiotomy or second degree perineal tear. International Journal of Reproduction, Contraception, Obstetrics and Gynecology. doi:10.1002/14651858.cd000947.pub3.
- ^ Fernando R (January 2011). "Episiotomy or perineal tears: compared with catgut, synthetic sutures reduce risk of short-term pain and need for resuturing; rapidly absorbing sutures comparable to synthetic but reduce the need for suture removal". BMJ, Evidence-Based Nursing. 14 (1): 17–18. doi:10.1136/ebn1110. ISSN 1367-6539. PMID 21163794.
- ^ Ferri FF (2012). Ferri's Clinical Advisor 2013. Elsevier Health Sciences. pp. 1134–1140. ISBN 0323083730.
- ^ Hales D (2008). An Invitation to Health Brief 2010-2011. Cengage Learning. pp. 269–271. ISBN 0495391921.
- ^ Alexander W, Bader H, LaRosa JH (2011). New Dimensions in Women's Health. Jones & Bartlett Publishers. p. 211. ISBN 1449683754.
- ^ Knox D, Schacht C (2007). Choices in Relationships: Introduction to Marriage and the Family. Cengage Learning. pp. 296–297. ISBN 0495091855.
- ^ a b Kumar B, Gupta S (2014). Sexually Transmitted Infections. Elsevier Health Sciences. pp. 126–127. ISBN 8131229785.
- ^ Hornstein T, Schwerin JL (2012). Biology of Women. Cengage Learning. pp. 126–127. ISBN 143540033X.
- ^ Berek JS, Hacker NF (2010). Berek and Hacker's Gynecologic Oncology. Lippincott Williams & Wilkins. p. 225. ISBN 0781795125.
- ^ Bibbo M, Wilbur D (2014). Comprehensive Cytopathology E-Book. Elsevier Health Sciences. p. 49. ISBN 0323265766.
- ^ a b Salhan S (2011). Textbook of Gynecology. JP Medical Ltd. p. 270. ISBN 9350253690.
- ^ Paludi MA (2014). The Praeger Handbook on Women's Cancers: Personal and Psychosocial Insights. ABC-CLIO. p. 111. ISBN 1440828148.
- ^ Chi D, Berchuck A, Dizon DS, Yashar CM (2017). Principles and Practice of Gynecologic Oncology. Lippincott Williams & Wilkins. p. 87. ISBN 1496355105.
- ^ a b Daniels R, Nicoll LH (2011). Contemporary Medical-Surgical Nursing. Cengage Learning. p. 1776. ISBN 1133418759.
- ^ Washington CM, Leaver DT (2015). Principles and Practice of Radiation Therapy. Elsevier Health Sciences. p. 749. ISBN 0323287816.
- ^ Sabater S, Andres I, Lopez-Honrubia V, Berenguer R, Sevillano M, Jimenez-Jimenez E, Rovirosa A, Arenas M (August 9, 2017). "Vaginal cuff brachytherapy in endometrial cancer – a technically easy treatment?". Cancer Management and Research. 9: 351–362. doi:10.2147/CMAR.S119125. ISSN 1179-1322. PMC 5557121. PMID 28848362.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Harkenrider MM, Block AM, Alektiar KM, Gaffney DK, Jones E, Klopp A, Viswanathan AN, Small W (January–February 2017). "American Brachytherapy Task Group Report: Adjuvant vaginal brachytherapy for early-stage endometrial cancer: A comprehensive review". Brachytherapy. 16 (1): 95–108. doi:10.1016/j.brachy.2016.04.005.
- ^ Coran AG, Caldamone A, Adzick NS, Krummel TM, Laberge JM, Shamberger R (2012). Pediatric Surgery. Elsevier Health Sciences. p. 1599. ISBN 032309161X.
- ^ Marx J, Walls R, Hockberger R (2013). Rosen's Emergency Medicine - Concepts and Clinical Practice. Elsevier Health Sciences. p. 1314. ISBN 1455749877.
- ^ a b Venes D (2009). Taber’s Cyclopedic Medical Dictionary. F.A. Davis. p. 2433. ISBN 9780803629776.
- ^ a b Holland JC, Breitbart WD, Jacobsen PB (2015). Psycho-oncology. Oxford University Press. p. 220. ISBN 0199363315.
- ^ a b c Crooks R, Baur K (2010). Our Sexuality. Cengage Learning. pp. 55–56. ISBN 978-0-495-81294-4.
- ^ a b c d e f g h "Female genital mutilation". Media centre. World Health Organization. Retrieved August 22, 2012.
- ^ Stone L (2002). New Directions in Anthropological Kinship. Rowman & Littlefield. p. 164. ISBN 058538424X.
- ^ a b Hutcherson H (2003). What Your Mother Never Told You about Sex. Penguin. p. 8. ISBN 0399528539.
- ^ LaFont S (2003). Constructing Sexualities: Readings in Sexuality, Gender, and Culture. Prentice Hall. p. 145. ISBN 013009661X.
- ^ Buss DM, Meston CM (2009). Why Women Have Sex: Understanding Sexual Motivations from Adventure to Revenge (and Everything in Between). Macmillan. p. 33. ISBN 1429955228.
- ^ a b Blackledge C (2003). The Story of V: A Natural History of Female Sexuality. Rutgers University Press. pp. 4–5. ISBN 0813534550.
- ^ Rosenthal MS (2003). Gynecological Health : a Comprehensive Sourcebook for Canadian Women. Viking Canada. p. 10. ISBN 0670043583.
The urine flows from the bladder through the urethra to the outside. Little girls often make the common mistake of thinking that they're urinating out of their vaginas. A woman's urethra is two inches long, while a man's is ten inches long.
- ^ a b Hickling M (2005). The New Speaking of Sex: What Your Children Need to Know and When They Need to Know It. Wood Lake Publishing. p. 149. ISBN 1896836704.
- ^ Rankin L (2011). Sex, Orgasm, and Coochies: A Gynecologist Answers Your Most Embarrassing Questions. Macmillan. p. 22. ISBN 1429955228.
- ^ Linn D (2009). Secret Language of Signs. Random House Publishing Group. p. 276. ISBN 0307559556.
- ^ Laqueur TW (1992). Making Sex: Body and Gender from the Greeks to Freud. Harvard University Press. p. 236. ISBN 0674543556.
- ^ Zastrow C (2007). Introduction to Social Work and Social Welfare: Empowering People. Cengage Learning. p. 228. ISBN 0495095109.
- ^ Irvine JM (2005). Disorders of Desire: Sexuality and Gender in Modern American Sexology. Temple University Press. pp. 37–38. ISBN 978-1592131518.
- ^ Gould SJ (2002). The Structure of Evolutionary Theory. Harvard University Press. pp. 1262–1263. ISBN 0674006135.
- ^ Wignaraja P, Hussain A (1989). The Challenge in South Asia: Development, Democracy and Regional Cooperation. United Nations University Press. p. 309. ISBN 0803996039.
- ^ Angier N (1999). Woman: An Intimate Geography. Houghton Mifflin Harcourt. p. 92. ISBN 978-0-395-69130-4.
- ^ a b Maines RP (1998). The Technology of Orgasm: "Hysteria", the Vibrator, and Women's Sexual Satisfaction. Baltimore: The Johns Hopkins University Press. p. 188. ISBN 0-8018-6646-4.
- ^ a b Hughes G (2015). An Encyclopedia of Swearing: The Social History of Oaths, Profanity, Foul Language, and Ethnic Slurs in the English-speaking World. Routledge. p. 112. ISBN 1317476786.
- ^ "cunt". Compact Oxford English Dictionary of Current English (3rd (revised) ed.). Oxford: Oxford University Press. 2008.
- ^ "Definition of CUNT". Dictionary – Merriam-Webster online. Merriam-Webster. Retrieved June 9, 2014.
- ^ "cunt". Merriam-Webster's Learner's Dictionary. Merriam-Webster. Retrieved September 13, 2013.
- ^ Johnston H, Klandermans B (1995). Social Movements and Culture. Routledge. p. 174. ISBN 1-85728-500-X.
- ^ "Twat". Dictionary.com. 2015. Retrieved June 16, 2015. This source aggregates material from paper dictionaries, including Random House Dictionary, Collins English Dictionary, and Harper's Online Etymology Dictionary.
- ^ "Definition of twat in English". Oxford Dictionaries. Oxford University Press. British and World English lexicon. Retrieved June 16, 2015.
- ^ "pussy, n. and adj.2". Oxford English Dictionary (3rd ed.). Oxford: Oxford University Press. 2007.
- ^ James D (Winter 1998). "Gender-linked derogatory terms and their use by women and men". American Speech. 73 (4): 399–420. doi:10.2307/455584. JSTOR 455584.
- ^ a b Randolph V, Legman G (1992). Unprintable Ozark Folksongs and Folklore: Blow the candle out. University of Arkansas Press. pp. 819–820. ISBN 1557282374.
- ^ Zizek S (2004). Organs without bodies: Deleuze and consequences. Routledge. p. 173. ISBN 0415969212.
- ^ Rankin L (2010). What's Up Down There?: Questions You'd Only Ask Your Gynecologist If She Was Your Best Friend. St. Martin's Press. p. 59. ISBN 978-0-312-64436-9.
- ^ "Life & Work". nikidesaintphalle.org. 2017. Retrieved November 8, 2014.
- ^ Tripp A. "In sorrow, she created delight: An Appeal for a Greater Appraisal of the Life and Art of Niki de Saint Phalle". Academia.edu. p. 10. Retrieved October 22, 2015.
- ^ Reilly M. "Tour and Home". Elizabeth A. Sackler Center for Feminist Art. Brooklyn Museum. Retrieved October 22, 2015.
- ^ Ensler E (2001). The Vagina Monologues: The V-Day Edition. Random House LLC. ISBN 0375506586.
- ^ Coleman C (2006). Coming to Read "The Vagina Monologues": A Biomythographical Unravelling of the Narrative. University of New Brunswick. ISBN 0494466553.
- ^ a b Stern MJ (July 3, 2012). "France Wants To Punish Facebook For Censoring A Painting of A Vagina. Terrible Idea". Slate. Retrieved October 2, 2015.
- ^ Denson GR (November 11, 2011). "150-Year-Old Painting STILL Too Graphic For Facebook". Huff Post. Retrieved October 2, 2015.
- ^ McCroy W (October 10, 2013). "Controversial Madonna Painting Opens Magnet HIV Clinic Art Show". Edge Media Network. Archived from the original on November 25, 2015. Retrieved October 19, 2015.
- ^ a b Lloyd J, Crouch NS, Minto CL, Liao LM, Creighton SM (May 2005). "Female genital appearance: 'normality' unfolds". British Journal of Obstetrics and Gynaecology. 112 (5): 643–646. doi:10.1111/j.1471-0528.2004.00517.x. PMID 15842291.
- ^ a b c d e Momoh C (2005). "Female Genital Mutation". In Momoh C (ed.). Female Genital Mutilation. Radcliffe Publishing. pp. 5–12. ISBN 978-1-85775-693-7.
- ^ Hecht M (2013). Major Patterns in Vertebrate Evolution. Springer Science & Business Media. pp. 439–516. ISBN 1468488511.
- ^ Szykman M, Van Horn RC, Engh AL, Boydston EE, Holekamp KE (2007). "Courtship and mating in free-living spotted hyenas" (PDF). Behaviour. 144 (7): 815–846. doi:10.1163/156853907781476418.
- ^ Bekoff M, Diamond J (May 1976). "Precopulatory and Copulatory Behavior in Coyotes". Journal of Mammalogy. 57 (2). American Society of Mammalogists: 372–375. doi:10.2307/1379696. JSTOR 1379696.
- ^ Iannaccone P (1997). Biological Aspects of Disease. CRC Press. pp. 315–316. ISBN 3718606135.
- ^ a b Fishbeck DW, Sebastiani A (2012). Comparative Anatomy: Manual of Vertebrate Dissection. Morton Publishing Company. pp. 66–68. ISBN 1617310042.
- ^ Chapman RF, Simpson SJ, Douglas AE (2013). The Insects: Structure and Function. Cambridge University Press. pp. 314–316. ISBN 052111389X.
- ^ Brennan, P. L. R., Clark, C. J. & Prum, R. O. Explosive eversion and functional morphology of the duck penis supports sexual conflict in waterfowl genitalia. Proceedings: Biological Sciences 277, 1309–14 (2010).
- ^ Arielle Duhaime-Ross (April 17, 2014). "Scientists discover the animal kingdom's first 'female penis’". The Verge. Retrieved March 29, 2015.
- ^ Yoshizawae K, Ferreira RL, Kamimura Y, Lienhard C (April 17, 2014). "Female Penis, Male Vagina, and Their Correlated Evolution in a Cave Insect". Current Biology. 24 (9): 1006–1010. doi:10.1016/j.cub.2014.03.022. PMID 24746797.
- ^ "In sex-reversed cave insects, females have the penises". Science Daily. April 17, 2014. Retrieved April 27, 2014.
