NMDA receptor antagonist

NMDA receptor antagonists are a class of anesthetics that work to antagonize, or inhibit the action of, the N-Methyl-D-aspartate receptor (NMDAR). They are used as anesthetics for animals and for humans; the state of anesthesia they induce is referred to as dissociative anesthesia. There is evidence that NMDA receptor antagonists can cause a certain type of neurotoxicity or brain damage referred to as Olney's Lesions in rodents, although such damage has never been conclusively observed in adult primates like humans. Recent research conducted on primates suggests that, while very consistent and long-term ketamine use may be neurotoxic, acute use is not.[1][2]
Several synthetic opioids function additionally as NMDAR-antagonists, such as pethidine, methadone, dextropropoxyphene, tramadol and ketobemidone.
Some NMDA receptor antagonists, such as ketamine, dextromethorphan (DXM), phencyclidine (PCP), methoxetamine (MXE), and nitrous oxide (N2O), are popular recreational drugs used for their dissociative, hallucinogenic, and euphoriant properties. When used recreationally, they are classified as dissociative drugs.
Uses and effects
NMDA receptor antagonists induce a state called dissociative anesthesia, marked by catalepsy, amnesia, and analgesia.[3] Ketamine is a favored anesthetic for emergency patients with unknown medical history and in the treatment of burn victims because it depresses breathing and circulation less than other anesthetics.[4][5] Dextrorphan, a metabolite of dextromethorphan (one of the most commonly used cough suppressants in the world[6]), is known to be an NMDA receptor antagonist.
Depressed NMDA receptor function is associated with an array of negative symptoms. For example, NMDA receptor hypofunction that occurs as the brain ages may be partially responsible for memory deficits associated with aging.[7] Schizophrenia may also have to do with irregular NMDA receptor function (the glutamate hypothesis of schizophrenia).[8] Increased levels of another NMDA antagonist, kynurenic acid, may aggravate the symptoms of schizophrenia, according to the "kynurenic hypothesis".[9] NMDA receptor antagonists can mimic these problems; they sometimes induce "psychotomimetic" side effects, symptoms resembling psychosis. Such side effects caused by NMDA receptor inhibitors include hallucinations, paranoid delusions, confusion, difficulty concentrating, agitation, alterations in mood, nightmares,[10] catatonia,[11] ataxia,[12] anaesthesia,[13] and learning and memory deficits.[14]
Because of these psychotomimetic effects, NMDA receptor antagonists, especially phencyclidine, ketamine, and dextromethorphan, are used as recreational drugs. At subanesthetic doses, these drugs have mild stimulant effects and, at higher doses, begin inducing dissociation and hallucinations, though these effects and the strength thereof vary from drug to drug.[15]
Most NMDA receptor antagonists are metabolized in the liver.[16][17] Frequent administration of most NMDA receptor antagonists can lead to tolerance, whereby the liver will more quickly eliminate NMDA receptor antagonists from the bloodstream.[18]
Neurotoxicity
Although NMDA antagonists were once thought to reliably cause neurotoxicity in humans in the form of Olney's lesions, recent research suggests otherwise. Olney's lesions involve mass vacuolization of neurons observed in rodents.[19][20] However, many suggest that this is not a valid model of human use, and studies conducted on primates have shown that use must be heavy and chronic to cause neurotoxicity.[1][2] Indeed, a 2009 review found no evidence of ketamine-induced neuron death in humans.[21] Temporary cognitive impairment seems to occur, though. A large-scale, longitudinal study found that current frequent ketamine users have modest cognitive deficits, while infrequent or former heavy users do not.[22] Many drugs have been found that lessen the risk of neurotoxicity from NMDA receptor antagonists. Centrally acting alpha 2 agonists such as clonidine and guanfacine are thought to most directly target the etiology of NMDA neurotoxicity. Other drugs acting on various neurotransmitter systems known to inhibit NMDA antagonist neurotoxicity include: anticholinergics, diazepam, barbiturates,[23] ethanol,[24] 5-HT2A serotonin receptor agonists,[25] and muscimol.[26]
Potential for treatment of excitotoxicity
Since NMDA receptor overactivation is implicated in excitotoxicity, NMDA receptor antagonists have held much promise for the treatment of conditions that involve excitotoxicity, including benzodiazepine withdrawal, traumatic brain injury, stroke, and neurodegenerative diseases such as Alzheimer's, Parkinson's, and Huntington's. This is counterbalanced by the risk of developing Olney's lesions,[27] which have only ever been observed in rodents, and studies have started to find agents that prevent this neurotoxicity.[24][26] Most clinical trials involving NMDA receptor antagonists have failed due to unwanted side effects of the drugs; since the receptors also play an important role in normal glutamatergic neurotransmission, blocking them causes side-effects. These results have not yet been reproduced in humans, however.[28] Mild NMDA receptor antagonists like amitriptyline have been found to be helpful in benzodiazepine withdrawal.[29]
Mechanism of action
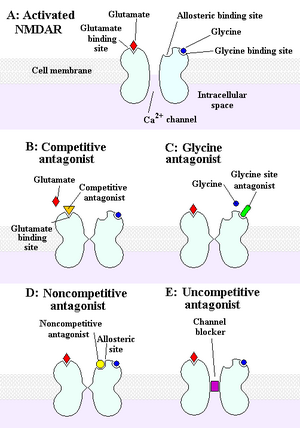
The NMDA receptor is an ionotropic receptor that allows for the transfer of electrical signals between neurons in the brain and in the spinal column. For electrical signals to pass, the NMDA receptor must be open. To remain open, glutamate and glycine must bind to the NMDA receptor. An NMDA receptor that has glycine and glutamate bound to it and has an open ion channel is called "activated."
Chemicals that deactivate the NMDA receptor are called antagonists. NMDAR antagonists fall into four categories: Competitive antagonists, which bind to and block the binding site of the neurotransmitter glutamate; glycine antagonists, which bind to and block the glycine site; noncompetitive antagonists, which inhibit NMDARs by binding to allosteric sites; and uncompetitive antagonists, which block the ion channel by binding to a site within it.[12]
Examples
Competitive antagonists
- AP5 (APV, R-2-amino-5-phosphonopentanoate)[30]
- AP7 (2-amino-7-phosphonoheptanoic acid)[31]
- CPPene (3-[(R)-2-carboxypiperazin-4-yl]-prop-2-enyl-1-phosphonic acid)[32]
- Selfotel: an anxiolytic, anticonvulsant but with possible neurotoxic effects.
Uncompetitive channel blockers
- Amantadine: used for treating Parkinson's disease and influenza and Alzheimer's.[33][34]
- Atomoxetine: a norepinephrine reuptake inhibitor used in the treatment of ADHD.[35]
- AZD6765
- Agmatine: Blocks NMDA receptors and other cation ligand-gated channels. Can also potentiate opioid analgesia.
- Chloroform: an early anesthetic.
- Dextrallorphan: a more potent analogue of dextromethorphan.
- Dextromethorphan: a common antitussive found in cough medicines.[36]
- Dextrorphan: active metabolite of dextromethorphan.
- Diphenidine: a novel designer drug sold on the internet.[37]
- Dizocilpine (MK-801): an experimental drug used in scientific research.[38]
- Ethanol: also known as alcohol, a widely used legal intoxicant.
- Eticyclidine: a Schedule I controlled substance in the United States.
- Gacyclidine: an experimental drug developed for neuroprotection.
- Ibogaine: a Schedule I controlled substance in the United States.[39][40]
- Magnesium
- Memantine: treatment for Alzheimer's disease.[41]
- Methoxetamine: a novel designer drug sold on the internet.[citation needed]
- Nitromemantine: a novel memantine derivative.[42]
- Nitrous oxide: used for anesthesia, particularly in dentistry.[43]
- Phencyclidine: a Schedule II controlled substance in the United States.[39]
- Rolicyclidine: a Schedule I controlled substance in the United States.
- Tenocyclidine: a Schedule I controlled substance in the United States.
- Methoxydine: 4-meo-pcp
- Tiletamine: an animal anesthetic.[44]
- Neramexane: a memantine analogue with nootropic, antidepressant properties. Also a nicotinic acetylcholine antagonist.
- Eliprodil: an anticonvulsant drug with neuroprotective properties.
- Etoxadrol: a potent dissociative similar to PCP.
- Dexoxadrol: similar to etoxadrol.
- WMS-2539: potent fluorinated derivative of dexoxadrol.[45]
- NEFA: a moderate affinity antagonist.
- Remacemide: a low affinity antagonist also a sodium-channel blocker.
- Delucemine: also a SSRI with neuroprotective properties.
- 8A-PDHQ: a high affinity PCP structural analogue.
Non-competitive antagonists
- Aptiganel (Cerestat, CNS-1102): binds the Mg2+ binding site within the channel of the NMDA receptor.
- HU-211: an enantiomer of the potent cannabinoid HU-210 which lacks cannabinoid effects and instead acts as a potent non-competitive NMDA antagonist.[46]
- Remacemide: principle metabolite is an uncompetitive antagonist with a low affinity for the binding site.[47]
- Rhynchophylline an alkaloid.
- Ketamine: a dissociative psychedelic with antidepressant properties used as an anesthesia in humans and animals, a possible treatment in bipolar disorder patients with Treatment-resistant depression, and used recreationally for its effects on the CNS[48]
Glycine antagonists
These drugs act at the glycine binding site:
- Rapastinel (GLYX-13) (weak partial agonist; IA = ~20%)
- NRX-1074 (weak partial agonist)
- 7-Chlorokynurenic acid[49]
- 4-Chlorokynurenine (AV-101) (prodrug for 7-chlorokynurenic acid)
- 5,7-Dichlorokynurenic acid[50]
- Kynurenic acid (a naturally-occurring antagonist)[51]
- TK-40 (competitive antagonist at the GluN1 glycine binding site)[52]
- 1-Aminocyclopropanecarboxylic acid (ACPC)
- L-Phenylalanine,[53] a naturally occurring amino acid (equilibrium dissociation constant (KB) from Schild regression is 573 µM[54]).
- Xenon: an anesthetic.[55]
See also
References
- ^ a b Sun, Lin; Qi Li, Qing Li, Yuzhe Zhang, Dexiang Liu, Hong Jiang, Fang Pan, David T. Yew (12 November 2012). "Chronic ketamine exposure induces permanent impairment of brain functions in adolescent cynomolgus monkeys". Addiction Biology. 19: 185–194. doi:10.1111/adb.12004. PMID 23145560.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ a b Slikker, W.; Zou, X.; Hotchkiss, C. E.; Divine, R. L.; Sadovova, N.; Twaddle, N. C.; Doerge, D. R.; Scallet, A. C.; Patterson, T. A.; Hanig, J. P.; Paule, M. G.; Wang, C. (2007). "Ketamine-Induced Neuronal Cell Death in the Perinatal Rhesus Monkey". Toxicological Sciences. 98 (1): 145–158. doi:10.1093/toxsci/kfm084. PMID 17426105.
- ^ Pender J (1971). "Dissociative anesthesia". JAMA. 215 (7): 1126–30. doi:10.1001/jama.1971.03180200050011. PMID 5107596.
- ^ Ceber M, Salihoglu T (2006). "Ketamine may be the first choice for anesthesia in burn patients". J Burn Care Res. 27 (5): 760–2. doi:10.1097/01.BCR.0000238091.41737.7C. PMID 16998413.
- ^ Heshmati F, Zeinali M, Noroozinia H, Abbacivash R, Mahoori A (2003). "Use of ketamine in severe status asthmaticus in intensive care unit". Iran J Allergy Asthma Immunol. 2 (4): 175–80. PMID 17301376.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Equinozzi R, Robuschi M (2006). "Comparative Efficacy and Tolerability of Pholcodine and Dextromethorphan in the Management of Patients with Acute, Non-Productive Cough: A Randomized, Double-Blind, Multicenter Study". Treat Respir Med. 5 (6): 509–513. doi:10.2165/00151829-200605060-00014. PMID 17154678.
- ^ Newcomer, JW; Krystal JH (2001). "NMDA receptor regulation of memory and behavior in humans". Hippocampus. 11 (5): 529–542. doi:10.1002/hipo.1069. PMID 11732706.
- ^ Lipina, T; Labrie V, Weiner I, Roder J (2005). "Modulators of the glycine site on NMDA receptors, D-serine and ALX 5407, display similar beneficial effects to clozapine in mouse models of schizophrenia". Psychopharmacology. 179 (1): 54–67. doi:10.1007/s00213-005-2210-x. PMID 15759151.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Erhardt S, Schwieler L, Nilsson L, Linderholm K, Engberg G (September 2007). "The kynurenic acid hypothesis of schizophrenia". Physiol. Behav. 92 (1–2): 203–9. doi:10.1016/j.physbeh.2007.05.025. PMID 17573079.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Muir, KW; Lees KR (1995). "Clinical Experience With Excitatory Amino Acid Antagonist Drugs". Stroke. 26 (3): 503–513. doi:10.1161/01.STR.26.3.503. PMID 7886734.
- ^ Aarts, MM; Tymianski M (2003). "Novel Treatment of Excitotoxicity: Targeted Disruption of Intracellular Signalling From Glutamate Receptors". Biochemical Pharmacology. 66 (6): 877–886. doi:10.1016/S0006-2952(03)00297-1. PMID 12963474.
- ^ a b c Kim AH, Kerchner GA, Choi DW (2002). "Blocking Excitotoxicity". In Marcoux FW, Choi DW (ed.). CNS Neuroprotection. New York: Springer. pp. 3–36.
{{cite book}}: CS1 maint: multiple names: authors list (link) - ^ Kristensen, JD; Svensson B, and Gordh T Jr (1992). "The NMDA-Receptor Antagonist CPP Abolishes Neurogenic Wind-Up Pain After Intrathecal Administration in Humans". Pain. 51 (2): 249–253. doi:10.1016/0304-3959(92)90266-E. PMID 1484720.
- ^ Rockstroh, S; Emre M, Tarral A, and Pokorny R (1996). "Effects of the Novel NMDA-Receptor Antagonist SDZ EAA 494 on Memory and Attention in Humans". Psychopharmacology. 124 (3): 261–266. doi:10.1007/BF02246666. PMID 8740048.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Lim D (2003). "Ketamine Associated Psychedelic Effects and Dependence". Singapore Med J. 44 (1): 31–34. PMID 12762561.
- ^ Chia YY, Liu K, Chow LH, Lee TY (1999). "The preoperative administration of intravenous dextromethorphan reduces postoperative morphine consumption". Anesth. Analg. 89 (3): 748–52. doi:10.1097/00000539-199909000-00041. PMID 10475318.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Kharasch ED, Labroo R (1992). "Metabolism of ketamine stereoisomers by human liver microsomes". Anesthesiology. 77 (6): 1201–7. doi:10.1097/00000542-199212000-00022. PMID 1466470.
- ^ Livingston A, Waterman AE (1978). "The development of tolerance to ketamine in rats and the significance of hepatic metabolism". Br. J. Pharmacol. 64 (1): 63–9. doi:10.1111/j.1476-5381.1978.tb08641.x. PMC 1668251. PMID 698482.
- ^ Olney J, Labruyere J, Price M (1989). "Pathological changes induced in cerebrocortical neurons by phencyclidine and related drugs". Science. 244 (4910): 1360–2. doi:10.1126/science.2660263. PMID 2660263.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Hargreaves R, Hill R, Iversen L (1994). "Neuroprotective NMDA antagonists: the controversy over their potential for adverse effects on cortical neuronal morphology". Acta Neurochir Suppl (Wien). 60: 15–9. doi:10.1007/978-3-7091-9334-1_4. PMID 7976530.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Green SM, Coté CJ (August 2009). "Ketamine and neurotoxicity: clinical perspectives and implications for emergency medicine". Ann Emerg Med. 54 (2): 181–90. doi:10.1016/j.annemergmed.2008.10.003. PMID 18990467.
- ^ Morgan, Celia J. A.; Muetzelfeldt, Leslie; Curran, H. Valerie (2009). "Consequences of chronic ketamine self-administration upon neurocognitive function and psychological wellbeing: a 1-year longitudinal study". Addiction. 105 (1): 121–33. doi:10.1111/j.1360-0443.2009.02761.x. PMID 19919593.
- ^ Olney J, Labruyere J, Wang G, Wozniak D, Price M, Sesma M (1991). "NMDA antagonist neurotoxicity: mechanism and prevention". Science. 254 (5037): 1515–8. doi:10.1126/science.1835799. PMID 1835799.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ a b Farber, NB; Heinkel, C; Dribben, WH; Nemmers, B; Jiang, X (2004). "In the adult CNS, ethanol prevents rather than produces NMDA antagonist-induced neurotoxicity". Brain Research. 1028 (1): 66–74. doi:10.1016/j.brainres.2004.08.065. PMID 15518643.
- ^ Farber N, Hanslick J, Kirby C, McWilliams L, Olney J (1998). "Serotonergic agents that activate 5HT2A receptors prevent NMDA antagonist neurotoxicity". Neuropsychopharmacology. 18 (1): 57–62. doi:10.1016/S0893-133X(97)00127-9. PMID 9408919.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ a b Farber, NB; Jiang, X; Dikranian, K; Nemmers, B (2003). "Muscimol prevents NMDA antagonist neurotoxicity by activating GABAA receptors in several brain regions". Brain Research. 993 (1–2): 90–100. doi:10.1016/j.brainres.2003.09.002. PMID 14642834.
- ^ Maas, AI (2001). "Neuroprotective agents in traumatic brain injury". Expert Opinion on Investigational Drugs. 10 (4): 753–767. doi:10.1517/13543784.10.4.753. PMID 11281824.
- ^ Chen, HS; Lipton SA (2006). "The chemical biology of clinically tolerated NMDA receptor antagonists". Journal of Neurochemistry. 97 (6): 1611–26. doi:10.1111/j.1471-4159.2006.03991.x. PMID 16805772.
- ^ Gardoni, F; Di Luca M (2006). "New targets for pharmacological intervention in the glutamatergic synapse". European Journal of Pharmacology. 545 (1): 2–10. doi:10.1016/j.ejphar.2006.06.022. PMID 16831414.
- ^ Abizaid A, Liu Z, Andrews Z, Shanabrough M, Borok E, Elsworth J, Roth R, Sleeman M, Picciotto M, Tschöp M, Gao X, Horvath T (2006). "Ghrelin modulates the activity and synaptic input organization of midbrain dopamine neurons while promoting appetite". J Clin Invest. 116 (12): 3229–39. doi:10.1172/JCI29867. PMC 1618869. PMID 17060947.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ van den Bos R, Charria Ortiz G, Cools A (1992). "Injections of the NMDA-antagonist D-2-amino-7-phosphonoheptanoic acid (AP-7) into the nucleus accumbens of rats enhance switching between cue-directed behaviours in a swimming test procedure". Behav Brain Res. 48 (2): 165–70. doi:10.1016/S0166-4328(05)80153-6. PMID 1535501.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Eblen F, Löschmann P, Wüllner U, Turski L, Klockgether T (1996). "Effects of 7-nitroindazole, NG-nitro-L-arginine, and D-CPPene on harmaline-induced postural tremor, N-methyl-D-aspartate-induced seizures, and lisuride-induced rotations in rats with nigral 6-hydroxydopamine lesions". Eur J Pharmacol. 299 (1–3): 9–16. doi:10.1016/0014-2999(95)00795-4. PMID 8901001.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ "Effects of N-Methyl-D-Aspartate (NMDA)-Receptor Antagonism on Hyperalgesia, Opioid Use, and Pain After Radical Prostatectomy", University Health Network, Toronto, September 2005
- ^ "MedlinePlus Drug Information: Amantadine." MedlinePlus website Accessed May 29, 2007
- ^ Ludolph, Andrea G; Udvardi, Patrick T; Schaz, Ulrike; Henes, Carolin; Adolph, Oliver; Weigt, Henry U; Fegert, Joerg M; Boeckers, Tobias M; Föhr, Karl J (1 May 2010). "Atomoxetine acts as an NMDA receptor blocker in clinically relevant concentrations". British Journal of Pharmacology. pp. 283–291. doi:10.1111/j.1476-5381.2010.00707.x. Retrieved 1 January 2014.
{{cite web}}: CS1 maint: multiple names: authors list (link) - ^ Wong BY, Coulter DA, Choi DW, Prince DA (1988). "Dextrorphan and dextromethorphan, common antitussives, are antiepileptic and antagonize N-methyl-D-aspartate in brain slices". Neurosci. Lett. 85 (2): 261–6. doi:10.1016/0304-3940(88)90362-X. PMID 2897648.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ European Patent 0346791 1,2-Diarylethylamines for Treatment of Neurotoxic Injury
- ^ Fix AS, Horn JW, Wightman KA, et al. (1993). "Neuronal vacuolization and necrosis induced by the noncompetitive N-methyl-D-aspartate (NMDA) antagonist MK(+)801 (dizocilpine maleate): a light and electron microscopic evaluation of the rat retrosplenial cortex". Exp. Neurol. 123 (2): 204–15. doi:10.1006/exnr.1993.1153. PMID 8405286.
- ^ a b Controlled Substances Act. Accessed from the US Drug Enforcement Administration website on May 29, 2007.
- ^ Popik, P; Layer, RT; Skolnick, P (1994). "The putative anti-addictive drug ibogaine is a competitive inhibitor of [3H]MK-801 binding to the NMDA receptor complex". Psychopharmacology (Berl). 114 (4): 672–4. doi:10.1007/BF02245000. PMID 7531855.
{{cite journal}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ Chawla, PS; Kochar MS (2006). "What's new in clinical pharmacology and therapeutics". WMJ. 105 (3): 24–29. PMID 16749321.
- ^ Talantova, M.; Sanz-Blasco, S.; Zhang, X.; Xia, P.; Akhtar, M. W.; Okamoto, S. -I.; Dziewczapolski, G.; Nakamura, T.; Cao, G.; Pratt, A. E.; Kang, Y. -J.; Tu, S.; Molokanova, E.; McKercher, S. R.; Hires, S. A.; Sason, H.; Stouffer, D. G.; Buczynski, M. W.; Solomon, J. P.; Michael, S.; Powers, E. T.; Kelly, J. W.; Roberts, A.; Tong, G.; Fang-Newmeyer, T.; Parker, J.; Holland, E. A.; Zhang, D.; Nakanishi, N.; Chen, H. -S. V. (2013). "Aβ induces astrocytic glutamate release, extrasynaptic NMDA receptor activation, and synaptic loss". Proceedings of the National Academy of Sciences. 110 (27): E2518. doi:10.1073/pnas.1306832110. PMC 3704025. PMID 23776240.
- ^ Grasshoff C, Drexler B, Rudolph U, Antkowiak B (2006). "Anaesthetic drugs: linking molecular actions to clinical effects". Curr. Pharm. Des. 12 (28): 3665–79. doi:10.2174/138161206778522038. PMID 17073666.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Ko JC, Smith TA, Kuo WC, Nicklin CF (1998). "Comparison of anesthetic and cardiorespiratory effects of diazepam-butorphanol-ketamine, acepromazine-butorphanol-ketamine, and xylazine-butorphanol-ketamine in ferrets". Journal of the American Animal Hospital Association. 34 (5): 407–16. doi:10.5326/15473317-34-5-407. PMID 9728472.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Banerjee A, Schepmann D, Köhler J, Würthwein EU, Wünsch B (November 2010). "Synthesis and SAR studies of chiral non-racemic dexoxadrol analogues as uncompetitive NMDA receptor antagonists". Bioorg. Med. Chem. 18 (22): 7855–67. doi:10.1016/j.bmc.2010.09.047. PMID 20965735.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Nadler V, Mechoulam R, Sokolovsky M (November 1993). "The non-psychotropic cannabinoid (+)-(3S,4S)-7-hydroxy-delta 6- tetrahydrocannabinol 1,1-dimethylheptyl (HU-211) attenuates N-methyl-D-aspartate receptor-mediated neurotoxicity in primary cultures of rat forebrain". Neurosci. Lett. 162 (1–2): 43–5. doi:10.1016/0304-3940(93)90555-Y. PMID 8121633.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Muir, KW (2005). "Glutamate-based therapeutic approaches: clinical trials with NMDA antagonists". Current Opinion in Pharmacology. 6 (1): 53–60. doi:10.1016/j.coph.2005.12.002. PMID 16359918.
- ^ Harrison N, Simmonds M (1985). "Quantitative studies on some antagonists of N-methyl D-aspartate in slices of rat cerebral cortex". Br J Pharmacol. 84 (2): 381–91. doi:10.1111/j.1476-5381.1985.tb12922.x. PMC 1987274. PMID 2858237.
- ^ Hartley DM, Monyer H, Colamarino SA, Choi DW (1990). "7-Chlorokynurenate Blocks NMDA Receptor-Mediated Neurotoxicity in Murine Cortical Culture". Eur J Neurosci. 2 (4): 291–5. doi:10.1111/j.1460-9568.1990.tb00420.x. PMID 12106035.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Frankiewicz T, Pilc A, Parsons C (2000). "Differential effects of NMDA-receptor antagonists on long-term potentiation and hypoxic/hypoglycaemic excitotoxicity in hippocampal slices". Neuropharmacology. 39 (4): 631–42. doi:10.1016/S0028-3908(99)00168-9. PMID 10728884.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Khan MJ, Seidman MD, Quirk WS, Shivapuja BG (2000). "Effects of kynurenic acid as a glutamate receptor antagonist in the guinea pig". Eur Arch Otorhinolaryngol. 257 (4): 177–81. doi:10.1007/s004050050218. PMID 10867830.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Kvist, T; et al. (November 2013). "Crystal structure and pharmacological characterization of a novel N-methyl-D-aspartate (NMDA) receptor antagonist at the GluN1 glycine binding site". J Biol Chem. 288 (46): 33124–35. doi:10.1074/jbc.M113.480210. PMID 24072709.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Glushakov, AV; Dennis, DM; Morey, TE; Sumners, C; Cucchiara, RF; Seubert, CN; Martynyuk, AE (2002). "Specific inhibition of N-methyl-D-aspartate receptor function in rat hippocampal neurons by L-phenylalanine at concentrations observed during phenylketonuria". Molecular Psychiatry. 7 (4): 359–67. doi:10.1038/sj.mp.4000976. PMID 11986979.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Glushakov, AV; Glushakova, O; Varshney, M; Bajpai, LK; Sumners, C; Laipis, PJ; Embury, JE; Baker, SP; Otero, DH; Dennis, DM; Seubert, CN; Martynyuk, AE (February 2005). "Long-term changes in glutamatergic synaptic transmission in phenylketonuria". Brain. 128 (Pt 2): 300–7. doi:10.1093/brain/awh354. PMID 15634735.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Bank P, Franks NP, Dickinson R, (2010). "Competitive inhibition at the glycine site of the N-methyl-D-aspartate receptor mediates xenon neuroprotection against hypoxia-ischemia". Anesthesiology. 112 (3): 614–22. doi:10.1097/ALN.0b013e3181cea398. PMID 20124979.
{{cite journal}}: CS1 maint: extra punctuation (link) CS1 maint: multiple names: authors list (link)
