Pregnancy: Difference between revisions
ClueBot NG (talk | contribs) m Reverting possible vandalism by 122.106.129.193 to version by XLinkBot. False positive? Report it. Thanks, ClueBot NG. (867010) (Bot) |
|||
| Line 422: | Line 422: | ||
* [http://www.merckmanuals.com/home/womens_health_issues/pregnancy_complicated_by_disease/overview_of_disease_during_pregnancy.html Merck Manual Home Health Handbook] – further details on the diseases, disorders, etc., which may complicate pregnancy. |
* [http://www.merckmanuals.com/home/womens_health_issues/pregnancy_complicated_by_disease/overview_of_disease_during_pregnancy.html Merck Manual Home Health Handbook] – further details on the diseases, disorders, etc., which may complicate pregnancy. |
||
* [http://www.nhs.uk/Planners/pregnancycareplanner/Pages/PregnancyHome.aspx Pregnancy care planner] – NHS guide to having baby including preconception, pregnancy, labor, and birth. |
* [http://www.nhs.uk/Planners/pregnancycareplanner/Pages/PregnancyHome.aspx Pregnancy care planner] – NHS guide to having baby including preconception, pregnancy, labor, and birth. |
||
* [67-helpful-smart-topics.com/pregnancy/gender_choice/tips_about_conceiveing]- new information. |
|||
{{Pregnancy}} |
{{Pregnancy}} |
||
{{Pathology of pregnancy, childbirth and the puerperium}} |
{{Pathology of pregnancy, childbirth and the puerperium}} |
||
Revision as of 08:35, 7 February 2012
| Pregnancy | |
|---|---|
| Specialty | Gynaecology |
Pregnancy is the fertilization and development of one or more offspring, known as an embryo or fetus, in a woman's uterus. In a pregnancy, there can be multiple gestations, as in the case of twins or triplets. Childbirth usually occurs about 38 weeks after conception; in women who have a menstrual cycle length of four weeks, this is approximately 40 weeks from the start of the last normal menstrual period (LNMP). Human pregnancy is the most studied of all mammalian pregnancies.
The term embryo is used to describe the developing offspring during the first 8 weeks following conception, and subsequently the term fetus is used henceforth until birth.[1][2] 40% of pregnancies in the United States and United Kingdom are unplanned.[3][4]
In many societies’ medical or legal definitions, human pregnancy is somewhat arbitrarily divided into three trimester periods, as a means to simplify reference to the different stages of prenatal development. The first trimester carries the highest risk of miscarriage (natural death of embryo or fetus). During the second trimester, the development of the fetus can be more easily monitored and diagnosed. The beginning of the third trimester often approximates the point of viability, or the ability of the fetus to survive, with or without medical help, outside of the uterus.[5]
Etymology
One scientific term for the state of pregnancy is gravidity (adjective "gravid"), latin for “heavy” and a pregnant female is sometimes referred to as a gravida.[6] Similarly, the term parity (abbreviated as “para”) is used for the number of previous successful live births. Medically, a woman who has never been pregnant is referred to as a “nulligravida”, a woman who is (or has been only) pregnant for the first time as a “primigravida”,[7] and a woman in subsequent pregnancies as a multigravida or “multiparous.”[6][8][9] Hence, during a second pregnancy a woman would be described as “gravida 2, para 1” and upon live delivery as “gravida 2, para 2.” An in-progress pregnancy, as well as abortions, miscarriages, or stillbirths account for parity values being less than the gravida number. In the case of twins, triplets etc., gravida number and parity value are increased by one only. Women who have never carried a pregnancy achieving more than 20 weeks of gestation age are referred to as “nulliparous.”[10]
Progression

Initiation
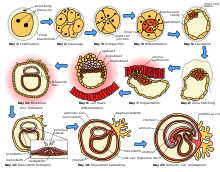
Although pregnancy begins with implantation, the process leading to pregnancy occurs earlier as the result of the female gamete, or oocyte, merging with the male gamete, spermatozoon. In medicine this process is referred to as fertilization; in lay terms, it is more commonly known as “conception.” After the point of fertilization, the fused product of the female and male gamete is referred to as a zygote or fertilized egg. The fusion of male and female gametes usually occurs following the act of sexual intercourse, resulting in spontaneous pregnancy. However, the advent of artificial insemination and in vitro fertilisation have made achieving pregnancy possible without engaging in sexual intercourse. This approach may be undertaken as a voluntary choice or due to infertility.
The process of fertilization occurs in several steps, and the interruption of any of them can lead to failure. Through fertilization, the egg is activated to begin its developmental process, and the haploid nuclei of the two gametes come together to form the genome of a new diploid organism[11]
At the beginning of the process, the sperm undergoes a series of changes, as freshly ejaculated sperm is unable or poorly able to fertilize,[12] The sperm must undergo capacitation in the female's reproductive tract over several hours, which increases its motility and destabilizes its membrane, preparing it for the acrosome reaction, the enzymatic penetration of the egg's tough membrane, the zona pellucida, which surrounds the oocyte. The sperm and the egg cell, which has been released from one of the female's two ovaries, unite in one of the two fallopian tubes. The fertilized egg, known as a zygote, then moves toward the uterus, a journey that can take up to a week to complete. Cell division begins approximately 24 to 36 hours after the male and female cells unite. Cell division continues at a rapid rate and the cells then develop into what is known as a blastocyst. The blastocyst is made up of three layers: the ectoderm (which will become the skin and nervous system), the endoderm (which will become the digestive and respiratory systems), and the mesoderm (which will become the muscle and skeletal systems). Finally, the blastocyst arrives at the uterus and attaches to the uterine wall, a process known as implantation.
The mass of cells, now known as an embryo, begins the embryonic stage which continues until cell differentiation is almost complete at eight weeks. Structures important to the support of the embryo develop, including the placenta and umbilical cord. During this time, cells begin to differentiate into the various body systems. The basic outlines of the organ, body, and nervous systems are established. By the end of the embryonic stage, the beginnings of features such as fingers, eyes, mouth, and ears become visible.
Once cell differentiation is mostly complete, the embryo enters the final stage and becomes known as a fetus. The early body systems and structures that were established in the embryonic stage continue to develop. Sex organs begin to appear during the third month of gestation. The fetus continues to grow in both weight and length, although the majority of the physical growth occurs in the last weeks of pregnancy.
Duration
Healthcare professionals name three different dates as the start of pregnancy:
- the first day of the woman's last normal menstrual period,
- the date of conception (about two weeks before her next expected menstrual period), and
- the date of implantation (about one week after conception).
Since these are spread over a significant period of time, the duration of pregnancy necessarily depends on the date selected as the starting point chosen.
The most common system used among healthcare professionals is Naegele's rule, which was developed in the early 19th century. This calculates the expected due date from the first day of the last normal menstrual period (LMP or LNMP) regardless of factors known to make this inaccurate, such as a shorter or longer menstrual cycle length. Pregnancy most commonly lasts for 40 weeks according to this LNMP-based method, assuming that the woman has a predictable menstrual cycle length of close to 28 days and conceives on the 14th day of that cycle, and a birth between 37 and 42 weeks LNMP is considered full-term.[13] Other, more accurate algorithms take into account a variety of other variables, such as whether this is the first or subsequent child (i.e., pregnant woman is a primipara or a multipara, respectively), ethnicity, parental age, length of menstrual cycle, and menstrual regularity), but these are rarely used by healthcare professionals.
There is a standard deviation of 8–9 days surrounding due dates calculated with even the most accurate methods. This means that fewer than 5 percent of births occur at exactly 40 weeks; 50 percent of births are within a week of this duration, and about 80 percent are within 2 weeks.[14] It is much more useful and accurate, therefore, to consider a range of due dates, rather than one specific day, with some online due date calculators providing this information.[15]
Pregnancy is considered "at term" when gestation attains 37 complete weeks but is less than 42 (between 259 and 294 days since LMP). Events before completion of 37 weeks (259 days) are considered preterm; from week 42 (294 days) events are considered postterm.[16] When a pregnancy exceeds 42 weeks (294 days), the risk of complications for both the woman and the fetus increases significantly.[13][17] Therefore, in an otherwise uncomplicated pregnancy, obstetricians usually prefer to induce labour at some stage between 41 and 42 weeks.[18][19]
Birth before 39 weeks, even if considered "at term", increases the risk of complications and premature death, from factors including under-developed lungs, infection due to under-developed immune system, problems feeding due to under-developed brain, and jaundice from under-developed liver. Some hospitals in the United States have noted a significant increase in neonatal intensive care unit patients when women schedule deliveries for convenience and are taking steps to reduce induction for non-medical reasons.[20] Complications from Caesarean section are more common than for live births.
Recent medical literature prefers the terminology preterm and postterm to premature and postmature. Preterm and postterm are unambiguously defined as above, whereas premature and postmature have historical meaning and relate more to the infant's size and state of development rather than to the stage of pregnancy.[21][22]
Accurate dating of pregnancy is important, because it is used in calculating the results of various prenatal tests, (for example, in the triple test). A decision may be made to induce labour if a fetus is perceived to be overdue. Furthermore, if LMP and ultrasound dating predict different respective due dates, with the latter being later, this might signify slowed fetal growth and therefore require closer review.
The age of fetal viability has been receding because of continued medical progress. Whereas it used to be 28 weeks, it has been brought back to as early as 23, or even 22 weeks in some countries.[citation needed]
Childbirth
Childbirth is the process whereby an infant is born. It is considered to be the beginning of the infant's life, and age is defined relative to this event in most cultures.
A woman is considered to be in labour when she begins experiencing regular uterine contractions, accompanied by changes of her cervix – primarily effacement and dilation. While childbirth is widely experienced as painful, some women do report painless labours, while others find that concentrating on the birth helps to quicken labour and lessen the sensations. Most births are successful vaginal births, but sometimes complications arise and a woman may undergo a cesarean section.
During the time immediately after birth, both the mother and the baby are hormonally cued to bond, the mother through the release of oxytocin, a hormone also released during breastfeeding. Studies show that skin-to-skin contact between a mother and her newborn immediately after birth is beneficial for both mother and baby. A review done by the World Health Organization found that skin-to-skin contact between mothers and babies after birth reduces crying, improves mother-infant interaction, and helps mothers to breastfeed successfully. They recommend that neonates be allowed to bond with the mother during their first two hours after birth, the period that they tend to be more alert than in the following hours of early life.[23]
Postnatal period
The postnatal period begins immediately after the birth of a child and then extends for about six weeks. During this period, the mother's body begins the return to prepregnancy conditions that includes changes in hormone levels and uterus size.
Diagnosis

The beginning of pregnancy may be detected in a number of different ways, either by a pregnant woman without medical testing, or by using medical tests with or without the assistance of a medical professional.
Most pregnant women experience a number of symptoms,[24] which can signify pregnancy. The symptoms can include nausea and vomiting, excessive tiredness and fatigue, cravings for certain foods that are not normally sought out, and frequent urination particularly during the night.
A number of early medical signs are associated with pregnancy.[25][26] These signs typically appear, if at all, within the first few weeks after conception. Although not all of these signs are universally present, nor are all of them diagnostic by themselves, taken together they make a presumptive diagnosis of pregnancy. These signs include the presence of human chorionic gonadotropin (hCG) in the blood and urine, missed menstrual period, implantation bleeding that occurs at implantation of the embryo in the uterus during the third or fourth week after last menstrual period, increased basal body temperature sustained for over 2 weeks after ovulation, Chadwick's sign (darkening of the cervix, vagina, and vulva), Goodell's sign (softening of the vaginal portion of the cervix), Hegar's sign (softening of the uterus isthmus), and pigmentation of linea alba – Linea nigra, (darkening of the skin in a midline of the abdomen, caused by hyperpigmentation resulting from hormonal changes, usually appearing around the middle of pregnancy).[25][26] Breast tenderness is common during the first trimester, and is more common in women who are pregnant at a young age.[27]
Pregnancy detection can be accomplished using one or more various pregnancy tests,[28] which detect hormones generated by the newly formed placenta. Clinical blood and urine tests can detect pregnancy 12 days after implantation.[29] Blood pregnancy tests are more accurate than urine tests.[30] Home pregnancy tests are urine tests, and normally cannot detect a pregnancy until at least 12 to 15 days after fertilization. A quantitative blood test can determine approximately the date the embryo was conceived.
In the post-implantation phase, the blastocyst secretes a hormone named human chorionic gonadotropin, which in turn stimulates the corpus luteum in the woman's ovary to continue producing progesterone. This acts to maintain the lining of the uterus so that the embryo will continue to be nourished. The glands in the lining of the uterus will swell in response to the blastocyst, and capillaries will be stimulated to grow in that region. This allows the blastocyst to receive vital nutrients from the woman.
Despite all the signs, some women may not realize they are pregnant until they are quite far along in their pregnancy. In some cases, a few women have not been aware of their pregnancy until they begin labour. This can be caused by many factors, including irregular periods (quite common in teenagers), certain medications (not related to conceiving children), and obese women who disregard their weight gain. Others may be in denial of their situation.
An early obstetric ultrasonography can determine the age of the pregnancy fairly accurately. In practice, medical professionals typically express the age of a pregnancy (i.e., an "age" for an embryo) in terms of "menstrual date" based on the first day of a woman's last menstrual period, as the woman reports it. Unless a woman's recent sexual activity has been limited, she has been charting her cycles, or the conception is the result of some types of fertility treatment (such as IUI or IVF), the exact date of fertilization is unknown. Without symptoms such as morning sickness, often the only visible sign of a pregnancy is an interruption of the woman's normal monthly menstruation cycle, (i.e., a "late period"). Hence, the "menstrual date" is simply a common educated estimate for the age of a fetus, which is an average of 2 weeks later than the first day of the woman's last menstrual period. The term "conception date" may sometimes be used when that date is more certain, though even medical professionals can be imprecise with their use of the two distinct terms. The due date can be calculated by using Naegele's rule. The expected date of delivery may also be calculated from sonogram measurement of the fetus. This method is slightly more accurate than methods based on LMP.[31] Additional obstetric diagnostic techniques can estimate the health and presence or absence of congenital diseases at an early stage.
Physiology

Pregnancy is typically broken into three periods, or trimesters, each of about three months.[32] While there are no hard and fast rules, these distinctions are useful in describing the changes that take place over time.
First trimester
Traditionally, medical professionals have measured pregnancy from a number of convenient points, including the day of last menstruation, ovulation, fertilization, implantation and chemical detection. In medicine, pregnancy is often defined as beginning when the developing embryo becomes implanted in the endometrial lining of a woman's uterus. Most pregnant women do not have any specific signs or symptoms of implantation, although it is not uncommon to experience minimal bleeding. After implantation, the uterine endometrium is called the decidua. The placenta, which is formed partly from the decidua and partly from outer layers of the embryo, connects the developing embryo to the uterine wall to allow nutrient uptake, waste elimination, and gas exchange via the mother's blood supply. The umbilical cord is the connecting cord from the embryo or fetus to the placenta. The developing embryo undergoes tremendous growth and changes during the process of fetal development.
Morning sickness occurs in about seventy percent of all pregnant women, and typically improves after the first trimester.[33] Although described as "morning sickness", women can experience this nausea during afternoon, evening, and throughout the entire day.
Shortly after conception, the nipples and areolas begin to darken due to a temporary increase in hormones.[34] This process continues throughout the pregnancy.
The first 12 weeks of pregnancy are considered to make up the first trimester. The first two weeks from the first trimester are calculated as the first two weeks of pregnancy even though the pregnancy does not actually exist. These two weeks are the two weeks before conception and include the woman's last period.
The third week is the week in which fertilization occurs and the 4th week is the period when implantation takes place. In the 4th week, the fecundated egg reaches the uterus and burrows into its wall which provides it with the nutrients it needs. At this point, the zygote becomes a blastocyst and the placenta starts to form. Moreover, most of the pregnancy tests may detect a pregnancy beginning with this week.
The 5th week marks the start of the embryonic period. This is when the embryo's brain, spinal cord, heart and other organs begin to form.[35] At this point the embryo is made up of three layers, of which the top one (called the ectoderm) will give rise to the embryo's outermost layer of skin, central and peripheral nervous systems, eyes, inner ear, and many connective tissues.[35] The heart and the beginning of the circulatory system as well as the bones, muscles and kidneys are made up from the mesoderm (the middle layer). The inner layer of the embryo will serve as the starting point for the development of the lungs, intestine and bladder. This layer is referred to as the endoderm. An embryo at 5 weeks is normally between 1⁄16 and 1⁄8 inch (1.6 and 3.2 mm) in length.
In the 6th week, the embryo will be developing basic facial features and its arms and legs start to grow. At this point, the embryo is usually no longer than 1⁄6 to 1⁄4 inch (4.2 to 6.4 mm). In the following week, the brain, face and arms and legs quickly develop. In the 8th week, the embryo starts moving and in the next 3 weeks, the embryo's toes, neck and genitals develop as well. According to the American Pregnancy Association, by the end of the first trimester, the fetus will be about 3 inches (76 mm) long and will weigh approximately 1 ounce (28 g).[36] Once pregnancy moves into the second trimester, all the risks of miscarriage and birth defects occurring drop drastically.
Second trimester

Weeks 13 to 28 of the pregnancy are called the second trimester. Most women feel more energized in this period, and begin to put on weight as the symptoms of morning sickness subside and eventually fade away.
The uterus, the muscular organ that holds the developing fetus, can expand up to 20 times its normal size during pregnancy.
Although the fetus begins to move and takes a recognizable human shape during the first trimester, it is not until the second trimester that movement of the fetus, often referred to as "quickening", can be felt. This typically happens in the fourth month, more specifically in the 20th to 21st week, or by the 19th week if the woman has been pregnant before. However, it is not uncommon for some women not to feel the fetus move until much later. The placenta fully functions at this time and the fetus makes insulin and urinates. The reproductive organs distinguish the fetus as male or female.
During the second trimester, most women begin to wear maternity clothes.
Third trimester

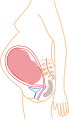
Final weight gain takes place, which is the most weight gain throughout the pregnancy. The fetus will be growing the most rapidly during this stage, gaining up to 28 g per day. The woman's belly will transform in shape as the belly drops due to the fetus turning in a downward position ready for birth. During the second trimester, the woman's belly would have been very upright, whereas in the third trimester it will drop down quite low, and the woman will be able to lift her belly up and down. The fetus begins to move regularly, and is felt by the woman. Fetal movement can become quite strong and be disruptive to the woman. The woman's navel will sometimes become convex, "popping" out, due to her expanding abdomen. This period of her pregnancy can be uncomfortable, causing symptoms like weak bladder control and backache. Movement of the fetus becomes stronger and more frequent and via improved brain, eye, and muscle function the fetus is prepared for ex utero viability. The woman can feel the fetus "rolling" and it may cause pain or discomfort when it is near the woman's ribs and spine.
There is head engagement in the third trimester, that is, the fetal head descends into the pelvic cavity so that only a small part (or none) of it can be felt abdominally. The perenium and cervix are further flattened and the head may be felt vaginally.[37] Head engagement is known colloquially as the baby drop, and in natural medicine as the lightening because of the release of pressure on the upper abdomen and renewed ease in breathing. However, it severely reduces bladder capacity, increases pressure on the pelvic floor and the rectum, and the mother may experience the perpetual sensation that the fetus will "fall out" at any moment.[38]
It is during this time that a baby born prematurely may survive. The use of modern medical intensive care technology has greatly increased the probability of premature babies surviving, and has pushed back the boundary of viability to much earlier dates than would be possible without assistance.[39] In spite of these developments, premature birth remains a major threat to the fetus, and may result in ill health in later life, even if the baby survives.
Embryonic and fetal development and ultrasound imaging
Prenatal development is divided into two primary biological stages. The first is the embryonic stage, which lasts for about two months. At this point, the fetal stage begins. At the beginning of the fetal stage, the risk of miscarriage decreases sharply,[40] and all major structures including the head, brain, hands, feet, and other organs are present, and they continue to grow and develop. When the fetal stage commences, a fetus is typically about 30 mm (1.2 inches) in length, and the heart can be seen beating via ultrasound; the fetus can be seen making various involuntary motions at this stage.[41]
Electrical brain activity is first detected between the 5th and 6th week of gestation, though this is still considered primitive neural activity rather than the beginning of conscious thought, something that develops much later in fetation. Synapses begin forming at 17 weeks, and at about week 28 begin to multiply at a rapid pace which continues until 3 to 4 months after birth.[42]
-
Relative size in 1st month (simplified illustration)
-
Relative size in 3rd month (simplified illustration)
-
Relative size in 5th month (simplified illustration)
-
Relative size in 9th month (simplified illustration)
One way to observe prenatal development is via ultrasound images. Modern 3D ultrasound images provide greater detail for prenatal diagnosis than the older 2D ultrasound technology.[47] While 3D is popular with parents desiring a prenatal photograph as a keepsake,[48] both 2D and 3D are discouraged by the FDA for non-medical use,[49][dead link] but there are no definitive studies linking ultrasound to any adverse medical effects.[50] The following 3D ultrasound images were taken at different stages of pregnancy:
-
75-mm fetus (about 14 weeks gestational age)
-
Fetus at 17 weeks
-
Fetus at 20 weeks
Physiological changes

During pregnancy, the woman undergoes many physiological changes, which are entirely normal, including cardiovascular, hematologic, metabolic, renal and respiratory changes that become very important in the event of complications. The body must change its physiological and homeostatic mechanisms in pregnancy to ensure the fetus is provided for. Increases in blood sugar, breathing and cardiac output are all required. Levels of progesterone and oestrogens rise continually throughout pregnancy, suppressing the hypothalamic axis and subsequently the menstrual cycle.
Management
Prenatal medical care is the medical and nursing care recommended for women before and during pregnancy. The aim of good prenatal care is to detect any potential problems early, to prevent them if possible (through recommendations on adequate nutrition, exercise, vitamin intake etc.), and to direct the woman to appropriate specialists, hospitals, etc. if necessary.
Nutrition
A balanced, nutritious diet is an important aspect of a healthy pregnancy. Eating a healthy diet, balancing carbohydrates, fat, and proteins, and eating a variety of fruits and vegetables, usually ensures good nutrition. Those whose diets are affected by health issues, religious requirements, or ethical beliefs may choose to consult a health professional for specific advice.
Adequate periconceptional folic acid (also called folate or Vitamin B9) intake has been proven to limit fetal neural tube defects, preventing spina bifida, a very serious birth defect. The neural tube develops during the first 28 days of pregnancy, explaining the necessity to guarantee adequate periconceptional folate intake.[51][52] Folates (from folia, leaf) are abundant in spinach (fresh, frozen, or canned), and are found in green leafy vegetables e.g. salads, beets, broccoli, asparagus, citrus fruits and melons, chickpeas (i.e. in the form of hummus or falafel), and eggs. In the United States and Canada, most wheat products (flour, noodles) are fortified with folic acid.[53]
DHA omega-3 is a major structural fatty acid in the brain and retina, and is naturally found in breast milk. It is important for the woman to consume adequate amounts of DHA during pregnancy and while nursing to support her well-being and the health of her infant. Developing infants cannot produce DHA efficiently, and must receive this vital nutrient from the woman through the placenta during pregnancy and in breast milk after birth.[54]
Several micronutrients are important for the health of the developing fetus, especially in areas of the world where insufficient nutrition is prevalent.[55] In developed areas, such as Western Europe and the United States, certain nutrients such as Vitamin D and calcium, required for bone development, may require supplementation.[56][57][58] A 2011 study examined cord blood of healthy neonates and found that low levels of vitamin D are associated with increased risk of lower respiratory tract infection the first year of life.[59]
Dangerous bacteria or parasites may contaminate foods, particularly Listeria and toxoplasma, toxoplasmosis agent. Careful washing of fruits and raw vegetables may remove these pathogens, as may thoroughly cooking leftovers, meat, or processed meat. Soft cheeses may contain Listeria; if milk is raw, the risk may increase. Cat feces pose a particular risk of toxoplasmosis. Pregnant women are also more prone to Salmonella infections from eggs and poultry, which should be thoroughly cooked. Practicing good hygiene in the kitchen can reduce these risks.[60]
Weight gain
Caloric intake must be increased to ensure proper development of the fetus. The amount of weight gained during a single pregnancy varies among women. The Institute of Medicine recommends an overall pregnancy weight gain for women starting pregnancy at a normal weight, with a body mass index of 18.5–24.9, of 25–35 pounds (11.4–15.9 kg).[61] Women who are underweight, with a BMI of less than 18.5, may need to gain between 28–40 lbs. Overweight women are advised to gain between 15–25 lbs, whereas an obese woman may expect to gain between 11–20 lbs. Doctors and dietitians may make different, or more individualized, recommendations for specific patients, based on factors including low maternal age, nutritional status, fetal development, and morbid obesity.
During pregnancy, insufficient or excessive weight gain can compromise the health of the mother and fetus. All women are encouraged to choose a healthy diet regardless of pre-pregnancy weight. Exercise during pregnancy, such as walking and swimming, is recommended for healthy pregnancies. Exercise has notable health benefits for both mother and baby, including preventing excessive weight gain.[62]
Immune tolerance
The fetus inside a pregnant woman may be viewed as an unusually successful allograft, since it genetically differs from the woman.[63] In the same way, many cases of spontaneous abortion may be described in the same way as maternal transplant rejection.[63]
Medication use
Drugs used during pregnancy can have temporary or permanent effects on the fetus. Therefore many physicians would prefer not to prescribe for pregnant women, the major concern being over teratogenicity of the drugs.
Drugs have been classified into categories A,B,C,D and X based on the Food and Drug Administration (FDA) rating system to provide therapeutic guidance based on potential benefits and fetal risks. Drugs, including some multivitamins, that have demonstrated no fetal risks after controlled studies in humans are classified as Category A. On the other hand drugs like thalidomide with proven fetal risks that outweigh all benefits are classified as Category X.[64]
Exposure to toxins
Various toxins pose a significant hazard to fetuses during development. A 2011 study found that virtually all U.S. pregnant women carry multiple chemicals, including some banned since the 1970s, in their bodies. Researchers detected polychlorinated biphenyls, organochlorine pesticides, perfluorinated compounds, phenols, polybrominated diphenyl ethers, phthalates, polycyclic aromatic hydrocarbons, perchlorate PBDEs, compounds used as flame retardants, and dichlorodiphenyltrichloroethane (DDT), a pesticide banned in the United States in 1972, in the bodies of 99 to 100 percent of the pregnant women they tested. Bisphenol A (BPA) was identified in 96 percent of the women surveyed. Several of the chemicals were at the same concentrations that have been associated with negative effects in children from other studies and it is thought that exposure to multiple chemicals can have a greater impact than exposure to only one substance.[65]
- Alcohol ingestion during pregnancy may cause fetal alcohol syndrome, a permanent and often devastating birth-defect syndrome. A number of studies have shown that light to moderate drinking during pregnancy might not pose a risk to the fetus, although no amount of alcohol during pregnancy can be guaranteed to be absolutely safe.[66][67][68]
- Numerous studies show that children exposed to prenatal cigarette smoke may experience a wide range of behavioral, neurological, and physical difficulties.[69]
- Elemental mercury and methylmercury are two forms of mercury that may pose risks in pregnancy. Methylmercury, a worldwide contaminant of seafood and freshwater fish, is known to produce adverse nervous system effects, especially during brain development.[70] Eating fish is the main source of mercury exposure in humans and some fish may contain enough mercury to harm the developing nervous system of an embryo or fetus, sometimes leading to learning disabilities. Mercury is present in many types of fish, but it is mostly found in certain large fish. The United States Food and Drug Administration and the Environmental Protection Agency advise pregnant women not to eat swordfish, shark, king mackerel and tilefish and limit consumption of albacore tuna to 6 ounces or less a week.[71]
- The Center for Children's Environmental Health reports studies that demonstrate that exposure to air pollution during pregnancy is related to adverse birth outcomes including low birth weight, premature delivery, and heart malformations. Cord blood of exposed babies shows DNA damage that has been linked to cancer. Follow-up studies show a higher level of developmental delays at age three, lower scores on IQ tests and increased behavioral problems at ages six and eight.[72][73]
- According to the U.S. Centers for Disease Control, the developing nervous system of the fetus is particularly vulnerable to lead toxicity. Neurological toxicity is observed in children of exposed women as a result of the ability of lead to cross the placental barrier and to cause neurological impairment in the fetus. A special concern for pregnant women is that some of the bone lead accumulation is released into the blood during pregnancy. Several studies have provided evidence that even low maternal exposures to lead produce intellectual and behavioral deficits in children1.[74]
- A 2006 study found that children who were exposed prenatally to the insecticide chlorpyrifos had significantly poorer mental and motor development by three years of age and increased risk for behavior problems.[75] A 2007 study using a mouse model suggested that exposure to polycyclic aromatic hydrocarbons prior to conceiving and when lactating reduces the number of eggs in the ovaries of female offspring by two-thirds.[76] A 2009 study of pregnant women exposed to tetrachloroethylene in drinking water found an increased risk of oral clefts and neural tube defects in their children.[77] A 2009 study found that prenatal exposure to phthalates, the chemical compounds used as plasticizers in a wide variety of personal care products, children's toys, and medical devices, may be an environmental risk factor for low birth weight in infants."[78] A 2010 study found that prenatal exposure to flame retardant compounds called polybrominated diphenyl ethers is associated with adverse neurodevelopmental effects in young children.[79]
Sexual activity during pregnancy
Most women can continue to engage in sexual activity throughout pregnancy.[80] Most research suggests that during pregnancy both sexual desire and frequency of sexual relations decrease.[81][82] In context of this overall decrease in desire, some studies indicate a second-trimester increase, preceding a decrease during the third trimester.[83][84] Some individuals are sexually attracted to pregnant women (pregnancy fetishism, also known as maiesiophilia).
Sex during pregnancy is a low-risk behavior except when the healthcare provider advises that sexual intercourse be avoided for particular medical reasons. Otherwise, for a healthy pregnant woman who is not ill or weak, there is no safe or right way to have sex during pregnancy: it is enough to apply the common sense rule that both partners avoid putting pressure on the uterus, or a partner’s full weight on a pregnant belly.[85]
Exercise
The Clinical Practice Obstetrics Committee of Canada recommends that "All women without contraindications should be encouraged to participate in aerobic and strength-conditioning exercises as part of a healthy lifestyle during their pregnancy". Although an upper level of safe exercise intensity has not been established, women who were regular exercisers before pregnancy and who have uncomplicated, healthy pregnancies should be able to engage in high intensity exercise programs, such as jogging and aerobics for less than 45 minutes, with no adverse effects if they are mindful of the possibility that they may need to increase their energy intake and are careful to not become overheated. In the absence of either medical or obstetric complications,they advise an accumulation of 30 minutes a day of exercise on most if not all days of the week. In general, participation in a wide range of recreational activities appears to be safe, with the avoidance of those with a high risk of falling such as horseback riding or sking or those that carry a risk of abdominal trauma, such as soccer or hockey.[86]
The American College of Obstetricians and Gynecologists reports that in the past, the main concerns of exercise in pregnancy were focused on the fetus and any potential maternal benefit was thought to be offset by potential risks to the fetus. However, they write that more recent information suggests that in the uncomplicated pregnancy, fetal injuries are highly unlikely. They do, however, list several circumstances when a woman should contact her health care provider before continuing with an exercise program. Contraindications include: Vaginal bleeding, dyspnea before exertion, dizziness, headache, chest pain, muscle weakness, preterm labor, decreased fetal movement, amniotic fluid leakage, and calf pain or swelling (to rule out thrombophlebitis. [87]
The Journal for Nurse Practitioners (2007) reports that many pregnant women do not exercise and they recommend that moderate exercise should be advised for pregnant women as part of prenatal care. They advise that exercise has benefits for both mother and fetus as well. [88]
A 2006 Cochrane review of prenatal exercise-related studies assessed the effects of regular aerobic exercise (at least two to three times per week) on physical fitness, the course of labor and delivery, and the outcome of pregnancy in healthy women. They concluded that regular aerobic exercise during pregnancy appears to improve (or maintain) physical fitness, however the authors noted that the trials were small and not of high methodologic quality and the data was insufficient to infer important risks or benefits for the mother or infant. The authors suggested that larger and better trials are needed before confident recommendations can be made about the benefits and risk of aerobic exercise in pregnancy.[89]
Complications
Each year, according to the WHO, ill-health as a result of pregnancy is experienced (sometimes permanently) by more than 20 million women around the world. Furthermore, the "lives of eight million women are threatened, and more than 500,000 women are estimated to have died in 1995 as a result of causes related to pregnancy and childbirth."[90]
Pregnancy poses varying levels of health risk for women, depending on their medical profile before pregnancy.
The following are some of the complaints that may occur during and/or after pregnancy due to the many changes which pregnancy causes in a woman's body:
- Pregnancy induced hypertension
- Anemia[91]
- Back pain. A particularly common complaint in the third trimester when the patient's center of gravity has shifted.
- Carpal tunnel syndrome in between an estimated 21% to 62% of cases, possibly due to edema.[92]
- Constipation. A complaint that is caused by decreased bowel mobility secondary to elevated progesterone (normal in pregnancy), which can lead to greater absorption of water.
- Braxton Hicks contractions. Occasional, irregular, and often painless contractions that occur several times per day.
- Edema (swelling). Common complaint in advancing pregnancy. Caused by compression of the inferior vena cava (IVC) and pelvic veins by the uterus leads to increased hydrostatic pressure in lower extremities.
- Regurgitation, heartburn, and nausea. Common complaints that may be caused by Gastroesophageal Reflux Disease (GERD); this is determined by relaxation of the lower esophageal sphincter (LES) and increased transit time in the stomach (normal in pregnancy), as well as by increased intraabdominal pressure, caused by the enlarging uterus.
- Haemorrhoids. Complaint that is often noted in advancing pregnancy. Caused by increased venous stasis and IVC compression leading to congestion in venous system, along with increased abdominal pressure secondary to the pregnant space-occupying uterus and constipation.
- Pelvic girdle pain. PGP disorder is complex and multi-factorial and likely to be represented by a series of sub-groups with different underlying pain drivers from peripheral or central nervous system,[93] altered laxity/stiffness of muscles,[94] laxity to injury of tendinous/ligamentous structures[95] to ‘mal-adaptive’ body mechanics.[96] Musculo-Skeletal Mechanics involved in gait and weightbearing activities can be mild to grossly impaired. PGP can begin peri or postpartum. There is pain, instability or dysfunction in the symphysis pubis and/or sacroiliac joints.
- Postpartum depression
- Postpartum psychosis
- Round Ligament Pain. Pain experienced when the ligaments positioned under the uterus stretch and expand to support the woman's growing uterus
- Thromboembolic disorders. The leading cause of death in pregnant women in the USA.[97]
- Increased urinary frequency. A common complaint referred by the gravida, caused by increased intravascular volume, elevated GFR (glomerular filtration rate), and compression of the bladder by the expanding uterus.
- Urinary tract infection[98]
- Varicose veins. Common complaint caused by relaxation of the venous smooth muscle and increased intravascular pressure.
- PUPPP skin disease that develop around the 32nd week. (Pruritic Urticarial Papules and Plaques of Pregnancy), red plaques, papules, itchiness around the belly button that spread all over the body except for the inside of hands and face.
Ectopic pregnancy
An ectopic pregnancy is a complication of pregnancy in which the embryo implants outside the uterine cavity.[99] With rare exceptions, ectopic pregnancies are not viable. Most ectopic pregnancies occur in the Fallopian tube (so-called tubal pregnancies), but implantation can also occur in the cervix, ovaries, and abdomen. It should be considered in any woman with abdominal pain or vaginal bleeding who has a positive pregnancy test. An ultrasound showing a gestational sac with fetal heart in a location other than the uterine cavity is clear evidence of an ectopic pregnancy. Tubal ectopic pregnancy is the most common cause of maternal death in the first trimester of pregnancy.[100]
About 1% of pregnancies are in an ectopic location with implantation not occurring inside of the womb, and of these 98% occur in the Fallopian tubes.[100] In a typical ectopic pregnancy, the embryo adheres to the lining of the fallopian tube and burrows into the tubal lining. Most commonly this invades blood vessels which causes bleeding resulting in the expulsion of the implantation from the tube. Termed "tubal abortions", about half of ectopic pregnancies will resolve without treatment. The use of methotrexate treatment for ectopic pregnancy has reduced the need for surgery, but surgical intervention is still required in cases where the Fallopian tube has ruptured or is in danger of doing so. The surgical intervention may be laparoscopic or through a larger incision, known as a laparotomy.[101]
A woman who has had a previous ectopic pregnancy is more likely to have another. The majority of women with ectopic pregnancies have had pelvic inflammatory disease or salpingitis, an inflammation of the fallopian tube. A history of gonorrhea or chlamydia can also cause tubal problems that increase the risk. Endometriosis, a condition that causes the tissue that normally lines the uterus to develop outside the uterus may slightly increase the incidence of an ectopic. The risk is increased in women who have unusually shaped fallopian tubes or tubes which has been damaged, possibly during surgery. Taking medication to stimulate ovulation increases the risk of ectopic pregnancy. When used properly, pregnancy is rare when using birth control pills or an intrauterine device (IUD) however, if it does occur, it's more likely to be ectopic. Although pregnancy is rare after tubal ligation, if it does occur, it's more likely to be ectopic.[102] A recent meta-analysis of clinical outcomes has shown that cigarette smoking significantly increases the risk of tubal ectopic pregnancy.[100]
Concomitant diseases
In addition to complications of pregnancy that can arise, a woman may have other diseases or conditions (not directly caused by the pregnancy) that may become worse or be a potential risk to the pregnancy.
- Diabetes mellitus and pregnancy deals with the interactions of diabetes mellitus (not restricted to gestational diabetes) and pregnancy. Risks for the child include miscarriage, growth restriction, growth acceleration, fetal obesity (macrosomia), polyhydramnios and birth defects.
- In the case of concomitant systemic lupus erythematosis and pregnancy, there is an increased rate of fetal death in utero and spontaneous abortion (miscarriage), as well as of neonatal lupus.
Stem cell collection
Two different types of stem cells can be collected before childbirth: amniotic stem cells and umbilical cord blood stem cells. The collection of amniotic stem cells is part of the process of amniocentesis. Umbilical cord blood stem cells can be stored in both public and private banks, such as the Biocell Center in Boston.[103][104][105]
Society and culture

In most cultures, pregnant women have a special status in society and receive particularly gentle care.[citation needed] At the same time, they are subject to expectations that may exert great psychological pressure, such as having to produce a son and heir. In many traditional societies, pregnancy must be preceded by marriage, on pain of ostracism of mother and (illegitimate) child.
Depictions of pregnant women can serve as mystically connotated symbols of fertility. The so-called Venus of Willendorf with its exaggerated female sexual characteristics (huge breasts and belly, prominent mons pubis) has been interpreted as indicative of a fertility fertility cult in paleolithic Europe.
Overall, pregnancy is accompanied by numerous customs that are often subject to ethnological research, often rooted in traditional medicine or religion. The baby shower is an example of a modern custom.
Pregnancy is an important topic in sociology of the family. The prospective child is preliminarily placed into numerous social roles such as prospective heir or welfare recipient. (This may accelerate weddings.) The parents' relationship and the relation between parents and their surroundings are also affected.

Visitation, circa 1305
Arts
Due to the important role of the Mother of God in Christianity, the Western visual arts have a long tradition of depictions of pregnancy.[citation needed]
Pregnancy, and especially pregnancy of unmarried women, is also an important motif in literature. Notable examples include Hardy's Tess of the d'Urbervilles and Goethe's Faust.
Demography
In Europe, the average childbearing age has been rising continuously for some time. In Western, Northern, and Southern Europe, first-time mothers are on average 26 to 29 years old, up from 23 to 25 years at the start of the 1970s. In a number of European countries (Spain), the mean age of women at first childbirth has now even crossed the 30 year threshold.
This process is not restricted to Europe. Asia, Japan and the United States are all seeing average age at first birth on the rise, and increasingly the process is spreading to countries in the developing world like China, Turkey and Iran. In the U.S., the age of first childbirth was 25 in 2006.[106]
Desired and undesired pregnancies
Reproductive medicine
Modern reproductive medicine offers a choice of measures for couples who stay childless against their will: fertility treatment, artificial insemination and surrogacy.
Abortion
An abortion is the termination of an embryo or fetus, either naturally or via medical methods. When done electively, it is more often done within the first trimester than the second, and rarely in the third.[40] Contraceptive failure, insufficient contraception, poor family planning or rape can lead to undesired pregnancies. Legality of socially indicated abortions varies widely both internationally and through time. In most countries of Western Europe, abortions during the first trimester were a criminal offense a few decades ago but have since been legalized, sometimes subject to mandatory consultations. In Germany, for example, as of 2009 less than 3% of abortions had a medical indication.
Legal protection for pregnant women
Many countries have various legal regulations in place to protect pregnant women and their children. Maternity protection ensures that pregnant women are exempt from activities such as night shifts or carrying heavy stocks. Maternity leave typically provides paid leave from work during roughly the last trimester of pregnancy and for some time after birth. Notable extreme cases include Norway (8 months with full pay) and the United States (no paid leave at all except in some states). Moreover, many countries have laws against pregnancy discrimination.
Post-menopausal pregnancies
With technology developments cases of post-menopausal pregnancies have occurred, and there are several known cases of older women carrying a pregnancy to term, usually with in vitro fertilization of a donor egg. A 61-year-old Brazilian woman with implantation of a donor egg, expected her first child September 2011.[107]
See also
- Anticoagulation in pregnancy
- Beginning of pregnancy controversy
- Denial of pregnancy
- False pregnancy
- Male pregnancy
- Pregnancy fetishism
- Pregnancy over age 50
- Pregnancy rate
- Simulated pregnancy
- Thyroid in pregnancy
References
- ^ "Embryo Definition". MedicineNet.com. MedicineNet, Inc. Retrieved 17 January 2008.
- ^ "Fetus Definition". MedicineNet.com. MedicineNet, Inc. Retrieved 17 January 2008.
- ^ 40% of pregnancies 'unplanned' retrieved 2 February 2012
- ^ Unplanned pregnancies in US at 40% retrieved 2 February 2012
- ^ "Trimester Definition". MedicineNet.com. MedicineNet, Inc. Retrieved 17 January 2008.
- ^ a b "Definition of gravida". The Free Dictionary/Medical Dictionary. Farlex, Inc. Retrieved 17 January 2008.
- ^ Robinson, Victor, ed. (1939). "Primipara". The Modern Home Physician, A New Encyclopedia of Medical Knowledge. WM. H. Wise & Company (New York)., page 596.
- ^ The American Heritage Medical Dictionary Copyright (definition of nulligravida).
- ^ Merriam-Webster's Medical Dictionary Definition of nulligravida Merriam-Webster's Medical Dictionary.
- ^ "Nulliparous Definition". MedicineNet.com. MedicineNet, Inc. Retrieved 17 January 2008.
- ^ "Fertilization". Retrieved 28 July 2010. [dead link]
- ^ "Fertilization". Retrieved 28 July 2010.
- ^ a b Norwitz, MD, PhD, Errol R (2007). "Patient information: Postterm pregnancy". UpToDate. UpToDate, inc. Retrieved 16 January 2008.
{{cite web}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Dr H. Kieler, O. Axelsson, S. Nilsson, U. Waldenströ (1995). "The length of human pregnancy as calculated by ultrasonographic measurement of the fetal biparietal diameter". Ultrasound in Obstetrics & Gynecology. 6 (5): 353–357. doi:10.1046/j.1469-0705.1995.06050353.x. PMID 8590208.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ "Pregnancy Due Date Ranges". Spacefem.com. Retrieved 25 November 2011.
- ^ "Definitions". Saskatchewan Prevention Institute. Retrieved 16 January 2008.
- ^ The American College of Obstetricians and Gynecologists (2006). "What To Expect After Your Due Date". Medem. Medem, Inc. Retrieved 16 January 2008.
{{cite web}}: Unknown parameter|month=ignored (help) - ^ Royal College of Obstetricians and Gynaecologists (2001). "Royal College of Obstetricians and Gynaecologists Induction of labour Evidence based Guideline" (PDF). Royal College of Obstetricians and Gynaecologists. Royal College of Obstetricians and Gynaecologists. Archived from the original (PDF) on 30 December 2006. Retrieved 18 January 2008.
- ^ Stovall, M.D., Thomas G. (23 March 2004). "Postdate Pregnancy". Durham Obstetrics and Gynecology. Durham Obstetrics and Gynecology. Retrieved 18 January 2008. [dead link]
- ^ "Doctors To Pregnant Women: Wait At Least 39 Weeks". 18 July 2011. Retrieved 20 August 2011.
- ^ "Definition of Premature birth". Medicine.net. Retrieved 16 January 2008.
- ^ Lama Rimawi, MD (22 September 2006). "Premature Infant". Disease & Conditions Encyclopedia. Discovery Communications, LLC. Retrieved 16 January 2008.
- ^ http://apps.who.int/rhl/newborn/gpcom/en/index.html
- ^ "Pregnancy Symptoms". National Health Service (NHS). 11 March 2010. Retrieved 11 March 2010.
- ^ a b "Early symptoms of pregnancy: What happens right away". Mayo Clinic. 22 February 2007. Retrieved 22 August 2007.
- ^ a b "Pregnancy Symptoms – Early Signs of Pregnancy : American Pregnancy Association". Retrieved 16 January 2008.
- ^ MedlinePlus > Breast pain Update Date: 12/31/2008. Updated by: David C. Dugdale, Susan Storck. Also reviewed by David Zieve.
- ^ "NHS Pregnancy Planner". National Health Service (NHS). 19 March 2010. Retrieved 19 March 2010.
- ^ Qasim SM, Callan C, Choe JK (1996). "The predictive value of an initial serum beta human chorionic gonadotropin level for pregnancy outcome following in vitro fertilization". Journal of Assisted Reproduction and Genetics. 13 (9): 705–8. doi:10.1007/BF02066422. PMID 8947817.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ "BestBets: Serum or Urine beta-hCG?".
- ^ Nguyen, T.H. (1999). "Evaluation of ultrasound-estimated date of delivery in 17 450 spontaneous singleton births: do we need to modify Naegele's rule?" (abstract). Ultrasound in Obstetrics and Gynecology. 14 (1): 23–28. doi:10.1046/j.1469-0705.1999.14010023.x. PMID 10461334. Retrieved 18 August 2007.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ thefreedictionary.com > trimester Citing:
- The American Heritage® Dictionary of the English Language, Fourth Edition, copyright 2000
- Collins English Dictionary – Complete and Unabridged, copyright 2003
- ^ "Early pregnancy symptoms: Morning sickness, fatigue and other common symptoms". Retrieved 2011.
{{cite web}}: Check date values in:|accessdate=(help) - ^ "Pregnancy video". Channel 4. 2008. Retrieved 22 January 2009.
- ^ a b "Pregnancy week by week". Retrieved 28 July 2010.
- ^ "Pregnancy Week by week Symptoms". Retrieved 28 July 2010.
- ^ "Starting labour". pregnancy-bliss.co.uk. Retrieved 14 January 2009.
- ^ "Lightening During Pregnancy as an Early Sign of Labor". Giving Birth Naturally. Retrieved 22 August 2010.
- ^ Iams JD (12 January 2008). "Primary, secondary, and tertiary interventions to reduce the morbidity and mortality of preterm birth". Lancet. 371 (9607): 164–75. doi:10.1016/S0140-6736(08)60108-7. PMID 18191687.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ a b • Q&A: Miscarriage. (6 August 2002). BBC News. Retrieved 2007-04-22: “The risk of miscarriage lessens as the pregnancy progresses. It decreases dramatically after the 8th week.”
• Lennart Nilsson, A Child is Born 91 (1990): at eight weeks, "the danger of a miscarriage … diminishes sharply."
• “Women’s Health Information”, Hearthstone Communications Limited: “The risk of miscarriage decreases dramatically after the 8th week as the weeks go by.” Retrieved 2007-04-22. - ^ Prechtl, Heinz. "Prenatal and Early Postnatal Development of Human Motor Behavior" in Handbook of brain and behaviour in human development, Kalverboer and Gramsbergen eds., pp. 415–418 (2001 Kluwer Academic Publishers). Retrieved 2007-03-04.
- ^ Illes, Judy. Neuroethics: Defining the Issues in Theory, Practice, and Policy (Oxford University Press 2006): "The first sign of electrical brain activity occurs at the end of week 5 and the beginning of week 6 (Brody 1975). This is far from the beginning of conscious brain activity; it is primitive neural activity. [...] synapses start forming during week 17 and multiply rapidly around week 28, continuing at a rapid pace up until 3–4 months after birth. However, despite all this amazing and rapid growth and development, it is not until week 23 that the fetus can survive, with major medical support, outside of the womb. Before this, the fetus is simply laying the foundations for a brain—a very different thing from having a sustainable human brain." Retrieved 2008-12-11.
- ^ 3D Pregnancy (Image from gestational age of 6 weeks). Retrieved 2007-08-28. A rotatable 3D version of this photo is available here, and a sketch is available here.
- ^ 3D Pregnancy (Image from gestational age of 10 weeks). Retrieved 2007-08-28. A rotatable 3D version of this photo is available here, and a sketch is available here.
- ^ 3D Pregnancy (Image from gestational age of 20 weeks). Retrieved 2007-08-28. A rotatable 3D version of this photo is available here, and a sketch is available here.
- ^ 3D Pregnancy (Image from gestational age of 40 weeks). Retrieved 2007-08-28. A rotatable 3D version of this photo is available here, and a sketch is available here.
- ^ Dimitrova V, Markov D, Dimitrov R (2007). "[3D and 4D ultrasonography in obstetrics]". Akush Ginekol (Sofiia) (in Bulgarian). 46 (2): 31–40. PMID 17469450.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Sheiner E, Hackmon R, Shoham-Vardi I; et al. (2007). "A comparison between acoustic output indices in 2D and 3D/4D ultrasound in obstetrics". Ultrasound Obstet Gynecol. 29 (3): 326–8. doi:10.1002/uog.3933. PMID 17265534.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Rados C (January–February 2004). "FDA Cautions Against Ultrasound 'Keepsake' Images". FDA Consumer Magazine.
- ^ Kempley R (9 August 2003). "The Grin Before They Bear It; Peek-a-Boo: Prenatal Portraits for the Ultrasound Set". Washington Post.
- ^ Klusmann A, Heinrich B, Stöpler H, Gärtner J, Mayatepek E, Von Kries R (2005). "A decreasing rate of neural tube defects following the recommendations for periconceptional folic acid supplementation". Acta Paediatr. 94 (11): 1538–42. doi:10.1080/08035250500340396. PMID 16303691. Retrieved 20 January 2008.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Stevenson RE, Allen WP, Pai GS, Best R, Seaver LH, Dean J, Thompson S (2000). "Decline in prevalence of neural tube defects in a high-risk region of the United States". Pediatrics. 106 (4): 677–83. doi:10.1542/peds.106.4.677. PMID 11015508.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Centers for Disease Control and Prevention (CDC) (2008). "Use of supplements containing folic acid among women of childbearing age—United States, 2007". MMWR Morb. Mortal. Wkly. Rep. 57 (1): 5–8. PMID 18185493.
- ^ Salem, Jr. N, et al. Mechanisms of action of docosahexaenoic acid in the nervous system. Lipids, 2001. 36:945-59.
- ^ Haider BA, Bhutta ZA (2006). Bhutta, Zulfiqar A (ed.). "Multiple-micronutrient supplementation for women during pregnancy". Cochrane Database Syst Rev (4): CD004905. doi:10.1002/14651858.CD004905.pub2. PMID 17054223.
- ^ Theobald HE (2007). "Eating for pregnancy and breast-feeding". J Fam Health Care. 17 (2): 45–9. PMID 17476978.
- ^ Basile LA, Taylor SN, Wagner CL, Quinones L, Hollis BW (2007). "Neonatal vitamin D status at birth at latitude 32 degrees 72': evidence of deficiency". J Perinatol. 27 (9): 568–71. doi:10.1038/sj.jp.7211796. PMID 17625571.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Kuoppala T, Tuimala R, Parviainen M, Koskinen T, Ala-Houhala M (1986). "Serum levels of vitamin D metabolites, calcium, phosphorus, magnesium and alkaline phosphatase in Finnish women throughout pregnancy and in cord serum at delivery". Hum Nutr Clin Nutr. 40 (4): 287–93. PMID 3488981.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ "Cord Blood Vitamin D Deficiency is Associated With Respiratory Syncytial Virus Bronchiolitis". Pediatrics.aappublications.org. 9 May 2011. Retrieved 25 November 2011.
- ^ Tarlow MJ; Alpar, H. O.; Brown, M. R. W. (1994). "Epidemiology of neonatal infections". J Antimicrob Chemother. 34 (Suppl A): 43–52. doi:10.1093/jac/34.1.43. PMID 7844073.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ "Weight Gain During Pregnancy: Reexaminging the Guidelines, Report Brief". Institute of Medicine. Retrieved 29 July 2010.
- ^ "Pregnancy and Exercise: Baby Let's Move!". Mayo Clinic. Retrieved 29 July 2010.
- ^ a b Clark DA, Chaput A, Tutton D (1986). "Active suppression of host-vs-graft reaction in pregnant mice. VII. Spontaneous abortion of allogeneic CBA/J x DBA/2 fetuses in the uterus of CBA/J mice correlates with deficient non-T suppressor cell activity". J. Immunol. 136 (5): 1668–75. PMID 2936806.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ [1], Reena Shaji,MD.Obstetrics & Gynecology
- ^ "99% of pregnant women in US test positive for multiple chemicals including banned ones, study suggests". Sciencedaily.com. 14 January 2011. doi:10.1289/ehp.1002727. Retrieved 25 November 2011.
- ^ * Day NL (1992). "The effects of prenatal exposure to alcohol." Alcohol Health and Research World, 16(2), 328–244.
- ^ Goodlett CR, Peterson SD (1995). "Sex differences in vulnerability to developmental spatial learning deficits induced by limited binge alcohol exposure in neonatal rats." Neurobiological Learning and Memory, 64(3), 265–275. PMID 8564380>
- ^ Streissguth AP, et al. (1994). "Prenatal alcohol and offspring development: the first fourteen years." Drug and Alcohol Dependence, 36(2), 89–99. PMID 7851285
- ^ "Cigarette Smoking Causes Child Learning Disabilities – Attention Deficit and Behavior Disorders". Chem-tox.com. 4 September 1992. Retrieved 25 November 2011.
- ^ "Prenatal Exposure to Mercury From a Maternal Diet High in Seafood Can Irreversibly Impair Certain Brain Functions in Children – February 06, 2004 -2004 Releases – Press Release Archives – Press Releases – Harvard School of Public Health". Hsph.harvard.edu. 6 February 2004. Retrieved 25 November 2011.
- ^ "March of Dimes". March of Dimes. Retrieved 25 November 2011.
- ^ http://www.ccceh.org/pdf-press/Time10-4-10.pdf
- ^ "Exposure to Common Pollutant in Womb Might Lower IQ". Health.usnews.com. 20 July 2009. Retrieved 25 November 2011.
- ^ "Chapter 1, Lead-based Paint Hazards, 98–112". Cdc.gov. Retrieved 25 November 2011.
- ^ "Exposures To Insecticide Chlorpyrifos In Pregnancy Adversely Affect Child Development, Study Finds". Sciencedaily.com. 6 December 2006. Retrieved 25 November 2011.
- ^ "Environmental Toxins May Limit Fertility In Offspring". Sciencedaily.com. 21 November 2007. Retrieved 25 November 2011.
- ^ phthalate exposure might be an environmental risk factor for low birth weight in infants." Although these associations are not 195108.htm[dead link]
- ^ "News & Articles in Science, Health, Environment & Technology". Science Daily. 7 November 2008. Retrieved 25 November 2011.
- ^ "Prenatal exposure to flame-retardant compounds affects neurodevelopment of young children". Sciencedaily.com. 19 January 2010. Retrieved 25 November 2011.
- ^ http://www.mayoclinic.com/health/sex-during-pregnancy/HO00140
- ^ M.P. Bermudez (2001). "Influence of the Gestation Period on Sexual Desire". Psychology in Spain. 5 (1): 14–16.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Wing Yee Fok (2005). "Sexual behavior and activity in Chinese pregnant women". Acta Obstetricia et Gynecologica Scandinavica. 84 (10): 934–938. doi:10.1111/j.0001-6349.2005.00743.x. PMID 16167907.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|month=ignored (help) - ^ Reamy K (1982). "Sexuality and pregnancy. A prospective study". J Reprod Med. 27 (6): 321–7. PMID 7120209.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|month=ignored (help) - ^ Malarewicz A, Szymkiewicz J, Rogala J (2006). "[Sexuality of pregnant women]". Ginekol. Pol. (in Polish). 77 (9): 733–9. PMID 17219804.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Cory Silverberg (19 September 2011). "Pregnancy Sex Positions: ideas for comfortable sex positions during pregnancy". About.com Guide.
- ^ http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1724598
- ^ http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1724598/pdf/v037p00006.pdf
- ^ WADSWORTH, P (1 May 2007). "The Benefits of Exercise in Pregnancy". The Journal for Nurse Practitioners. 3 (5): 333–339. doi:10.1016/j.nurpra.2007.03.002.
- ^ http://www.ncbi.nlm.nih.gov/pubmed/16855953
- ^ "Reproductive Health and Research Publications: Making Pregnancy Safer". World Health Organization Regional Office for South-East Asia. 2009. Retrieved 7 December 2009.
- ^ Merck. "Pregnancy complicated by disease". Merck Manual, Home Health Handbook. Merck Sharp & Dohme.
- ^ Mondelli,M.; Rossi,S.; Monti,E.; Aprile,I.; Caliandro,P.; Pazzaglia,C.; Romano,C.; Padua,L. (2007) Long term follow-up of carpal tunnel syndrome during pregnancy: a cohort study and review of the literature. Electromyogr Clin Neurophysiol. 2007 Sep;47(6):259–71.
- ^ Diagnosis and classification of pelvic girdle pain disorders—Part 1: A mechanism based approach within a biopsychosocial framework Manual Therapy, Volume 12, Issue 2, May 2007, Peter B. O’Sullivan and Darren J. Beales.
- ^ European guidelines for the diagnosis and treatment of pelvic girdle pain.Eur Spine J. 2008 Feb 8 Vleeming A, Albert HB, Ostgaard HC, Sturesson B, Stuge B.
- ^ Possible role of the long dorsal sacroiliac ligament in women with peripartum pelvic pain. Acta Obstetricia et Gynecologica Scandinavica Volume 81 Issue 5 Page 430-436, May 2002, Andry Vleeming, Haitze J. de Vries, Jan M. A Mens, Jan-Paul van Wingerden
- ^ Diagnosis and classification of pelvic girdle pain disorders—Part 1: A mechanism based approach within a biopsychosocial framework.Manual Therapy, Volume 12, Issue 2, May 2007, Pages 86–97 Peter B. O’Sullivan, and Darren J. Bealesa.
- ^ Merck. "Thromboembolic disorders during pregnancy". Merck Manual, Home Health Handbook. Merck Sharp & Dohme.
- ^ Merck. "Urinary tract infections during pregnancy". Merck Manual Home Health Handbook.
- ^ Page EW, Villee CA, Villee DB. Human Reproduction, 2nd Edition. W. B. Saunders, Philadelphia, 1976. p. 211. ISBN 0-7216-7042-3.
{{cite book}}: CS1 maint: multiple names: authors list (link) - ^ a b c http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2880914/?tool=pmcentrez
- ^ https://www.laparoscopyhospital.com/helpdesk/support/index.php?/Knowledgebase/Article/View/10/0/laparoscopic-ectopic-pregnancy-surgery
- ^ http://www.mayoclinic.com/health/ectopic-pregnancy/DS00622/DSECTION=risk-factors
- ^ "European Biotech Company Biocell Center Opens First U.S. Facility for Preservation of Amniotic Stem Cells in Medford, Massachusetts | Reuters". 22 October 2009. Retrieved 11 January 2010.
- ^ "Europe's Biocell Center opens Medford office – Daily Business Update – The Boston Globe". 22 October 2009. Retrieved 11 January 2010.
- ^ "The Ticker". Retrieved 11 January 2010.
- ^ Infertility by the numbers Colleen Mastony. 21 June 2009
- ^ "Woman, 61, pregnant". 27 September 2011.
External links
- Template:Dmoz
- Merck Manual Home Health Handbook – further details on the diseases, disorders, etc., which may complicate pregnancy.
- Pregnancy care planner – NHS guide to having baby including preconception, pregnancy, labor, and birth.
- [67-helpful-smart-topics.com/pregnancy/gender_choice/tips_about_conceiveing]- new information.

![Embryo at 4 weeks after fertilization[43]](http://upload.wikimedia.org/wikipedia/commons/a/aa/6_weeks_pregnant.png)
![Fetus at 8 weeks after fertilization[44]](http://upload.wikimedia.org/wikipedia/commons/c/c4/10_weeks_pregnant.png)
![Fetus at 18 weeks after fertilization[45]](http://upload.wikimedia.org/wikipedia/commons/3/3f/20_weeks_pregnant.png)
![Fetus at 38 weeks after fertilization[46]](http://upload.wikimedia.org/wikipedia/commons/e/ea/40_weeks_pregnant.png)