User:Zlavin/sandbox/neostigmine
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Bloxiverz, Prostigmin, Vagostigmin, others |
| AHFS/Drugs.com | Monograph |
| License data |
|
| Pregnancy category |
|
| Routes of administration | Intramuscular, intravenous, subcutaneous, by mouth |
| Drug class | Cholinesterase inhibitor |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | Unclear, probably less than 5% |
| Metabolism | Slow hydrolysis by acetylcholinesterase and also by plasma esterases |
| Onset of action | Within 10-20 min (injection),[3] with 4 hrs (by mouth) [citation needed] |
| Elimination half-life | 50–90 minutes |
| Duration of action | up to 4 hrs[3] |
| Excretion | Unchanged drug (up to 70%) and alcoholic metabolite (30%) are excreted in the urine |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| DrugBank |
|
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| Chemical and physical data | |
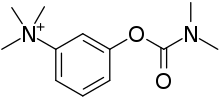
| Formula | C12H19N2O2+ |
| Molar mass | 223.296 g·mol−1 |
| 3D model (JSmol) | |
| |
| |
| | |
Neostigmine, sold under the brand name Bloxiverz, among others, is a medication used to treat myasthenia gravis, Ogilvie syndrome, and urinary retention without the presence of a blockage.[3][4] It is also used in anaesthesia to end the effects of non-depolarising neuromuscular blocking medication.[3] It is given by injection either into a vein, muscle, or under the skin.[3] After injection effects are generally greatest within 30 minutes and last up to 4 hours.[3][5]
Common side effects include nausea, increased saliva, crampy abdominal pain, and slow heart rate.[3] More severe side effects include low blood pressure, weakness, and allergic reactions.[3] It is unclear if use in pregnancy is safe for the baby.[3] Neostigmine is in the cholinergic family of medications.[3] It works by blocking the action of acetylcholinesterase and therefore increases the levels of acetylcholine.[3]
Neostigmine was patented in 1933.[6] It is on the World Health Organization's List of Essential Medicines.[7] The term is from Greek neos, meaning "new", and "-stigmine", in reference to its parent molecule, physostigmine, on which it is based.[8]
Medical uses[edit]
It is used to improve muscle tone in people with myasthenia gravis, and also to reverse the effects of non-depolarizing muscle relaxants such as rocuronium and vecuronium at the end of an operation.[9][10]
Another indication for use is the conservative management of acute colonic pseudo-obstruction, or Ogilvie's syndrome, in which patients get massive colonic dilatation in the absence of a true mechanical obstruction.[11]
Neostigmine is often prescribed for underactive urinary bladder.[12]
Hospitals sometimes administer a solution containing neostigmine intravenously to delay the effects of envenomation through snakebite.[13] Some promising research results have also been reported for administering the drug nasally as a snakebite treatment.[14]
Side effects[edit]
Neostigmine has a wide variety of side-effects due to its action that increases acetylcholine (ACh) binding muscarinic receptors on exocrine glandular cells throughout the body, cardiac muscle cells, and smooth muscle cells. These effects include: salivation, lacrimation, diarrhea, bradycardia, and bronchoconstriction.[15] Gastrointestinal symptoms occur earliest.[16]: 109
For this reason, it is usually given along with an anti-cholinergic drug such as atropine or glycopyrrolate which act only on muscarinic receptors while permitting neostigmine action at nicotinic receptors.[17]
Neostigmine can also induce generic ocular side effects including: headache, brow pain, blurred vision, phacodonesis, pericorneal injection, congestive iritis, various allergic reactions, and rarely, retinal detachment.[16]: 114
Mechanism of Action[edit]
Neostigmine affects the body by interfering with acetylcholinesterase, the enzyme responsible for breaking down acetylcholine. Acetylcholine is formed by certain neurons in order to activate postsynaptic membrane receptors, opening ion channels and sending signals to activate muscles. In normal body function, acetylcholinesterase quickly breaks down acetylcholine. At this point acetylcholine can no longer activate the receptors to send signals. When neostigmine is present, it binds to the acetylcholinesterase, preventing it from breaking down acetylcholine. This causes a buildup of acetylcholine, which continually activates the receptors. This unintended influx of signals can be very harmful to the body. As a medicine, neostigmine is used whenever extra signals are needed.[18]

Neostigmine acts as a reversible inhibitor of acetylcholinesterase. It is considered reversible because once attached it takes a matter of minutes to be removed from acetylcholinesterase via hydrolysis. For reference, the hydrolysis of acetylcholine is on the order of microseconds, and the hydrolysis of irreversible inhibitors (such as organophosphates) can take hours or days. First, neostigmine is oriented by having its positively charged nitrogen attracted to the anionic site in acetylcholinesterase. Then, an oxygen in the enzyme’s esteratic site attacks the carbon oxygen double bond in neostigmine. The now negatively charged oxygen tautomerizes, reforming the double bond and cleaving off the phenol group. Eventually, a water molecule is able to attack the same double bond, but this time the acetylcholinesterase’s oxygen is cleaved off, freeing the enzyme.[18]
Pharmacology[edit]
One benefit of neostigmine over physostigmine is the fact that neostigmine does not readily cross the blood-brain barrier. This is because of the positive charge on neostigmine’s quaternary nitrogen, as the positive charge makes the molecule polar and therefore more hydrophilic. Physostigmine is much more lipophilic and will cross the blood-brain barrier. Not crossing the blood-brain barrier can be beneficial by preventing the spread of neostigmine into the central nervous system, circumventing potential negative side effects.[19]
There are two types of postsynaptic membrane receptors that acetylcholine can activate, nicotinic and muscarinic. Neostigmine inhibits acetylcholinesterase which causes a buildup of acetylcholine, indirectly activating both receptors. Over activating the muscarinic receptors can cause undesirable side effects. To deal with this, muscarinic antagonists (drugs that can bind to the specifically muscarinic receptors without activating them) are often given with neostigmine. This blocks the acetylcholine from over activating the muscarinic receptors but does not interfere with activating the nicotinic receptors.[20]
Neostigmine is administered intravenously. The drug should be administered when a peripheral nerve stimulator shows a second twitch is present or when the first twitch response is considerably above 10% of baseline. Peak effect is at 7 to 10 minutes.[9] Neostigmine has moderate duration of action – usually two to four hours.[21] It is metabolized by enzymes in the liver and excreted in the urine.[9]
Chemistry[edit]
Neostigmine, which can be viewed as a simplified analog of physostigmine, is made by reacting 3-dimethylaminophenol with N-dimethylcarbamoyl chloride, which forms the dimethylcarbamate, and its subsequent alkylation using dimethyl sulfate forming the desired compound.[16]
Spectral data[edit]
Neostigmine shows notable UV/VIS absorption at 261 nm, 267 nm, and 225 nm.[22]
Neostigmine's 1H NMR Spectroscopy reveals shifts at: 7.8, 7.7, 7.4, 7.4, 3.8, and 3.1 parts per million. The higher shifts are due to the aromatic hydrogens. The lower shifts at 3.8 ppm and 3.1 ppm are due to the electronic withdrawing nature of the tertiary and quaternary nitrogen, respectively.[23]
History[edit]
Neostigmine was first synthesized as an analog of physostigmine, the active ingredient in calabar beans. The effects of the calabar bean were first studied in 1855. The first medicinal use of physostigmine was published in 1863 as the first drug able to constrict the pupil.[24]
The original synthesis of neostigmine was conducted by John A. Aeschlimann and Marc Reinert in 1931 while investigating the pharmacological properties of various physostigmine analogs. The experiment was based on the work of Edgar Stedman (and later Ellen Stedman and A. C. White). In a series of articles from 1926 to 1931, Stedman discovered some of the core structures allowing molecules to exhibit the same miotic activity as physostigmine. Aeschlimann and Reinert used this information to devise a method of generating physostigmine analogs. These analogs can be broken down into two main parts, a carbamic acid ester and a phenol with some basic substituent. The variations were generated by changing the substituents of these two main parts. One such variation would eventually become known as neostigmine. The experiment was done in hopes of finding a drug that had the medicinal properties of physostigmine but lacked some or all of its disadvantages, with emphasis on its instability in solution.[25]
Neostigmine was patented by Aeschlimann in 1933, under a patent describing two broad methods of synthesizing some physostigmine analogs. The main difference between the two methods is in the substituents of the starting materials. In the patent, Aeschlimann claims that all products are salts that easily dissolve in water, are stable when heated, and possess physostigmine-like properties.[26]
In 1934, Mary Walker discovered that neostigmine was an exceptional treatment for myasthenia gravis. She reached this conclusion by comparing the symptoms of myasthenia gravis to curare poisoning. The cure for curare poisoning is physostigmine, which led her to consider it and its analogs.[27] Soon, neostigmine became the preferred cure for myasthenia gravis.[28]
The term “neostigmine” was first used in 1941.[29] Before this, it was referred to as prostigmin.
Neostigmine was first approved by the FDA in May of 2013 under the name Bloxiverz, a neostigmine methylsulfate injection (the methylsulfate acts as a counter ion). This is because the Food, Drug, and Cosmetic Act wasn’t passed until 1938, well after neostigmine had been introduced to the market.[30]
References[edit]
- ^ "Neostigmine Use During Pregnancy". Drugs.com. 3 January 2020. Retrieved 21 January 2020.
- ^ "Bloxiverz- neostigmine methylsulfate injection". DailyMed. 3 March 2021. Retrieved 15 July 2022.
- ^ a b c d e f g h i j k "Neostigmine Bromide". The American Society of Health-System Pharmacists. Archived from the original on 21 December 2016. Retrieved 8 December 2016.
- ^ World Health Organization (2009). Stuart MC, Kouimtzi M, Hill SR (eds.). WHO Model Formulary 2008. World Health Organization. p. 428. hdl:10665/44053. ISBN 9789241547659.
- ^ "Neostigmine Methylsulfate Monograph for Professionals". Drugs.com. The American Society of Health-System Pharmacists. 19 September 2019. Retrieved 20 January 2020.
- ^ Fischer J, Ganellin CR (2006). Analogue-based Drug Discovery. John Wiley & Sons. p. 540. ISBN 9783527607495. Archived from the original on 20 December 2016.
- ^ World Health Organization (2019). World Health Organization model list of essential medicines: 21st list 2019. Geneva: World Health Organization. hdl:10665/325771. WHO/MVP/EMP/IAU/2019.06. License: CC BY-NC-SA 3.0 IGO.
- ^ "neostigmine: definition of neostigmine in Oxford dictionary (American English) (US)". www.oxforddictionaries.com. Archived from the original on 22 December 2015. Retrieved 17 December 2015.
- ^ a b c Neely GA, Sabir S, Kohli A (2022). "Neostigmine". StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. PMID 29261883.
- ^ "Neostigmine Injection: Indications, Side Effects, Warnings". Drugs.com.
- ^ Maloney N, Vargas HD (May 2005). "Acute intestinal pseudo-obstruction (Ogilvie's syndrome)". Clinics in Colon and Rectal Surgery. 18 (2): 96–101. doi:10.1055/s-2005-870890. PMC 2780141. PMID 20011348.
- ^ Moro C, Phelps C, Veer V, Clark J, Glasziou P, Tikkinen KA, Scott AM (January 2022). "The effectiveness of parasympathomimetics for treating underactive bladder: A systematic review and meta-analysis" (PDF). Neurourology and Urodynamics. 41 (1): 127–139. doi:10.1002/nau.24839. PMID 34816481. S2CID 244530010.
- ^ Franklin D (31 July 2013). "Potential Treatment For Snakebites Leads To A Paralyzing Test". NPR. Archived from the original on 9 August 2014.
- ^ Bulfone TC, Samuel SP, Bickler PE, Lewin MR (2018). "Developing Small Molecule Therapeutics for the Initial and Adjunctive Treatment of Snakebite". Journal of Tropical Medicine. 2018: 4320175. doi:10.1155/2018/4320175. PMC 6091453. PMID 30154870.
- ^ Naji A, Gatling JW (2022). "Muscarinic Antagonists". StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. PMID 32491473.
- ^ a b c Gilman AG, Goodman LS, Gilman Sr A (1980). Goodman & Gilman's The Pharmacological Basis of Therapeutics (6th ed.). New York: Macmillan Publishing Co., Inc.
- ^ Howard J, Wigley J, Rosen G, D'mello J (February 2017). "Glycopyrrolate: It's time to review". Journal of Clinical Anesthesia. 36: 51–53. doi:10.1016/j.jclinane.2016.09.013. PMID 28183573.
- ^ a b "Colinergic Drugs II - Anticholinesterase Agents & Acetylcholine Antagonists". Chemistry LibreTexts. 14 August 2017.
- ^ Kyung-soo Hong, Jason; Rauck, Richard (2018). "Exploring Nonopioid Analgesic Agents for Intrathecal Use". Neuromodulation: 847–860. doi:10.1016/B978-0-12-805353-9.00068-1.
- ^ Liu, J. (2017). "Neostigmine ☆". Reference Module in Biomedical Sciences: B9780128012383973148. doi:10.1016/B978-0-12-801238-3.97314-8.
- ^ Howland RD, Mycek MJ, Harvey RA, Champe PC, Mycek MJ (2008). Pharmacology (3rd ed.). Lippincott's Illustrated Reviews. p. 51.
- ^ Porst H, Kny L (May 1985). "[The structure of degradation products of neostigmine bromide]". Die Pharmazie (in German). 40 (5): 325–328. PMID 4034636.
- ^ Ferdous AJ, Waigh RD (June 1993). "Application of the WATR technique for water suppression in 1H NMR spectroscopy in determination of the kinetics of hydrolysis of neostigmine bromide in aqueous solution". The Journal of Pharmacy and Pharmacology. 45 (6): 559–562. doi:10.1111/j.2042-7158.1993.tb05598.x. PMID 8103105. S2CID 38613106.
- ^ Proudfoot, Alex (2006). "The Early Toxicology of Physostigmine: A Tale of Beans, Great Men and Egos". Toxicological Reviews. 25 (2): 99–138. doi:10.2165/00139709-200625020-00004.
- ^ Aeschlimann, John A.; Reinert, Marc (1 November 1931). "The Pharmacological Action of Some Analogues of Physostigmine" (PDF). Journal of Pharmacology and Experimental Therapeutics. 43 (3): 413–444. ISSN 0022-3565.
- ^ US 1905990, Aeschliman JA, issued 1933
- ^ Keeney, Arthur H.; Keeney, Virginia T. (March 1997). "Mary B. Walker, M.D. and the pioneering use of prostigmin to treat myasthenia gravis". Documenta Ophthalmologica. 93 (1–2): 125–134. doi:10.1007/BF02569052.
- ^ Viets, Henry R. (28 April 1945). "MYASTHENIA GRAVIS". Journal of the American Medical Association. 127 (17): 1089. doi:10.1001/jama.1945.02860170001001.
- ^ "Definition of NEOSTIGMINE". www.merriam-webster.com.
- ^ Lewis, Ashley N.; Sandra, Hanna (15 November 2013). "Neostigmine Methylsulfate Injection (Bloxiverz)".
External links[edit]
- "Neostigmine". Drug Information Portal. U.S. National Library of Medicine.
- "Neostigmine methylsulfate". Drug Information Portal. U.S. National Library of Medicine.
- "Neostigmine bromide". Drug Information Portal. U.S. National Library of Medicine.
