Antipsychotic: Difference between revisions
trimmed lead section of excess details |
→Comparison of medications: Adding pharmacokinetic data table. |
||
| Line 504: | Line 504: | ||
N-DEBN - N-deethylblonanserin |
N-DEBN - N-deethylblonanserin |
||
===Pharmacokinetic=== |
|||
{| class = "wikitable" |
|||
! Drug<ref>{{cite web|title=Article title|publisher=WebMD|accessdate=29 November 2013|url=http://reference.medscape.com/medscapetoday|work=Medscape Reference}}</ref><ref>{{cite web|title=article title|work=TGA eBusiness Services|publisher=[Drug sponsor]|date=[date page was last modified]|accessdate=29 November 2013|url=https://www.ebs.tga.gov.au/|format=PDF}}</ref><ref name = DM>{{cite web|title=DailyMed|work=DailyMed|publisher=[Drug sponsor]|date=[Date page was last modified]|accessdate=29 November 2013|url=http://dailymed.nlm.nih.gov/dailymed/about.cfm?}}</ref><ref>{{cite web|title=Article title|work=electronic Medicines Compendium|publisher=Drug Sponsor|date=date last modified|accessdate=29 November 2013|url=http://www.medicines.org.uk/emc/default.aspx}}</ref> !! [[Bioavailability]] !! [[Biological_half-life|t<sub>1/2</sub>]] parent drug <br>(active metabolite) !! Protein binding !! [[Pharmacokinetics#Metrics|t<sub>max</sub>]] !![[Pharmacokinetics#Metrics|C<sub>max</sub>]] !! [[Volume of distribution|V<sub>d</sub>]] !! Excretion !! Routes of administration !! Metabolising enzymes<ref name = GG/> !! Active metabolites |
|||
|- |
|||
| [[Amisulpride]] || 48% || 12 hr || 16% || 3-4 hr || 54±4 ng/mL || 5.8 L/kg || Faeces (20%), urine (50%, when given IV) || Oral || ? ||None |
|||
|- |
|||
| [[Aripiprazole]] || 87% (Oral), 100% (IM) || 75 hr (94 hr) || 99% || 3-5 hr || ? || 4.9 L/kg || Faeces (55%), urine (25%) || Oral,[[Intramuscular|IM]] (including depot) || [[CYP2D6]], [[CYP3A4]] || Dehydroaripiprazole |
|||
|- |
|||
| [[Asenapine]] || 35% (sublingual) || 24 hr || 95% || 0.5-1.5 hr || 4 ng/mL || 20-25 L/kg || Urine (50%), faeces (40%) || Sublingual ||[[CYP1A2]], [[UGT1A4]], [[CYP2D6]] || None |
|||
|- |
|||
| [[Blonanserin]]<ref>{{cite journal|title=Blonanserin A Review of its Use in the Management of Schizophrenia|journal=CNS Drugs|date=January 2010|author=Deeks, ED; Keating, GM|volume=24|issue=1|pages=65-84|pmid=20030420|doi=10.2165/11202620-000000000-00000}}</ref><ref>{{cite journal|title=Profile of blonanserin for the treatment of schizophrenia|journal=Neuropsychiatric Disease and Treatment|date=2013|volume=9|pages=587-594|doi=10.2147/NDT.S34433|pmid=23766647|author=Tenjin, T; Miyamoto, S; Ninomiya, Y; Kitajima, R; Ogino, S; Miyake, N; Yamaguchi, N}}</ref><ref>{{cite journal|title=Population pharmacokinetics of blonanserin in Chinese healthy volunteers and the effect of the food intake|journal=Human Psychopharmacology|date=March 2013|volume=28|issue=2|pages=134-141|doi=10.1002/hup.2290|pmid=23417765|author=Wen, YG; Shang, DW; Xie, HZ; Wang, XP; Ni, XJ; Zhang, M; Lu, W; Qiu, C; Liu, X; Li, FF; Li, X; Luo, FT}}</ref> || 55% || 10.7-16.2 hr (single dosing), 67.9 hr (repeated dosing) || ≥99.7% || 1.5-2 hr || 0.14-0.76 ng/mL (0.57 ng/mL for repeated dosing) || 8560-9500 L || Urine (59%), faeces (30%) || Oral || [[CYP3A4]] || N-deethylblonanserin |
|||
|- |
|||
| [[Chlorpromazine]] || 20% || 30 hr || 92-97% || ? || ? || 20 L/kg || Urine || Oral, [[Intramuscular|IM]], [[Intravenous|IV]] ||[[CYP2D6]] || Several active metabolites |
|||
|- |
|||
| [[Clozapine]] || 50-60% || 12 hr || 97% || 1.5-2.5 hr || 102-771 ng/mL || 4.67 L/kg || Urine (50%), faeces (30%) || Oral || [[CYP1A2]],[[CYP2D6]], [[CYP3A4]] || [[Norclozapine]] |
|||
|- |
|||
| [[Droperidol]] || ? || 2 hr (8-12 hr) || Extensive || 60 min (IM) || ? || 2 L/kg (adults), 0.58 L/kg (children) || Urine (75%), faeces (22%) || [[Intramuscular|IM]], [[Intravenous|IV]] || ? || None |
|||
|- |
|||
| [[Flupentixol]] || 40-55% (Oral) || 35 hr || ? || 7 days (depot) || ? || 12-14 L/kg || Urine || Oral, IM (including depot) || ? || None |
|||
|- |
|||
| [[Fluphenazine]] || 2.7% (Oral) || 14-16 hrs, 14 days (depot) || ? || 2 hr (Oral), 8-10 hr (depot) || ? || ? || Urine, faeces || Oral, IM (including depot) || ? || None |
|||
|- |
|||
| [[Haloperidol]] || 60-70% (Oral) || 10-20 hrs (short-acting IM), 3 weeks (depot) || 92% || 2-6 hr (Oral), 10-20 mins (short-acting IM), 6-7 days (depot) || ? || 8-18 L/kg || Urine (30%), faeces (15%) || Oral, IM, IV || [[CYP3A4]] || None |
|||
|- |
|||
| [[Iloperidone]] || 96% || ? || 95% || 2-4 hr || ? || 1340-2800 L || Urine (45-58%), faeces (20-22%) || Oral || [[CYP3A4]], [[CYP2D6]]|| None notable. |
|||
|- |
|||
| [[Levomepromazine]] || ? || 30 hr || ? || 2-3 hr || ? || ? || Urine, faeces || IM, IV || ? || Methotrimeprazine sulfoxide |
|||
|- |
|||
| [[Loxapine]] || High || 6-8 hr (Inhaled), 4-12 hr (Oral) || 96.6% || 2 mins (inhaled), 2 hr (oral), 5 hr (IM) || 257 ng/mL (inhaled), 6-13 ng/mL (Oral) || ? || Urine (56-70%), faeces [Only oral data available] || Oral, IM, Inhalation || [[CYP1A2]], [[CYP3A4]], [[CYP2D6]]|| [[Amoxapine]] (a tricyclic antidepressant), 7-OH loxapine, 8-OH loxapine |
|||
|- |
|||
| [[Lurasidone]] || 9-19% || 18 hr || 99% || 1-3 hr || ? || 6173 L || Urine (9%), faeces (80%) || Oral || [[CYP3A4]] || 2 active |
|||
|- |
|||
| [[Melperone]]<ref>{{cite journal|last=Borgström|first=L|coauthors=Larsson, H; Molander, L|title=Pharmacokinetics of parenteral and oral melperone in man|journal=European Journal of Clinical Pharmacology|year=1982|volume=23|issue=2|pages=173–176|pmid=7140807|url=http://link.springer.com/article/10.1007/BF00545974|doi=10.1007/BF00545974}}</ref> || 54% (Oral via syrup), 65% (Oral via tablets), 87% (IM) || 2.1-6.4 hrs (Oral), 6.6±3.7 hrs (IM) || 50% || 1.6-2.4 hr (Oral, tablets), 1 hr (Oral, syrup) || 1132±814 ng/mL (25 mg, orally), 2228-3416 ng/mL (50 mg, orally), 89539±37001 ng/mL (100 mg, orally) ||9.9±3.7 L/kg (10 mg), 7±1.61 L/kg (20 mg) || Urine (70% as metabolites, 5.5-10.4% as parent drug) || Oral, IM || ? || None |
|||
|- |
|||
| [[Olanzapine]] || 87% (Oral) || 30 hr || 93% || 6 hr (Oral), 15-45 min (short-acting IM), 7 days (depot) || 4-20.4 mg/mL<ref>{{cite journal|title=Olanzapine. Pharmacokinetic and pharmacodynamic profile|journal=Clinical Pharmacokinetics|date=September 1999|volume=37|issue=3|pages=177-193|doi=10.2165/00003088-199937030-00001|author=Callaghan, JT; Bergstrom, RF; Ptak, LR; Beasley, CM|pmid=10511917}}</ref> || 1000 L || Urine (57%), faeces (30%) || Oral, IM (including depot) || [[CYP1A2]] || None |
|||
|- |
|||
| [[Paliperidone]] || 28% (Oral) || 23 hr (Oral), 25-49 days (IM) || 74% || 24 hr (Oral), 13 days (IM) || 8.85-11.7 ng/mL<ref>{{cite journal|title=Absorption, Metabolism, and Excretion of Paliperidone, a New Monoaminergic Antagonist, in Humans|date=April 2008|volume=36|issue=4|journal=Drug Metabolism and Disposition|pages=769-779|doi=10.1124/dmd.107.018275|pmid=18227146|author=Vermeir, M; Naessens, I; Remmerie, B; Mannens, G; Hendrickx, J; Sterkens, P; Talluri, K; Boom, S; Eerdekens, M; van Osselaer, N; Cleton, A|url=http://dmd.aspetjournals.org/content/36/4/769.full.pdf|format=PDF}}</ref><ref>{{cite journal|title=The Pharmacological Role and Clinical Applications of Antipsychotics’ Active Metabolites: Paliperidone versus Risperidone|journal=Clinical and Experimental Pharmacology|date=January 2013|url=http://www.omicsonline.org/the-pharmacological-role-and-clinical-applications-of-antipsychotics-active-metabolites-paliperidone-versus-risperidone-2161-1459.1000117.pdf|format=PDF|author=Álamo, C; López-Muñoz, F|volume=3|issue=1|pages=117|doi=10.4172/2161-1459.1000117}}</ref> || 390-487 L || Urine (80%), faeces (11%) || Oral, IM (depot) ||[[CYP3A4]], [[CYP2D6]] || None |
|||
|- |
|||
| [[Periciazine]] || ? || 12 hr || ? || 2 hr || 150 ng/mL || ? || Urine || Oral || ? || ? |
|||
|- |
|||
| [[Perospirone]]<ref>{{cite journal |author = Onrust, SV; McClellan, K | title = Perospirone | journal = CNS Drugs | volume = 15 | issue = 4 | pages = 329–37; discussion 338| year = 2001 | pmid = 11463136 | doi = 10.2165/00023210-200115040-00006 | url =http://link.springer.com/article/10.2165%2F00023210-200115040-00006}}</ref> || ? || 1.9-2.5 hr || 92% || 1.5 hr || 5.7 ng/mL || ? ||Urine (0.4% as unchanged drug) || Oral || ? || None |
|||
|- |
|||
| [[Perphenazine]] || ? || 9-12 hr (10-19 hr) || ? || 1-3 hr; 2-4 hr (metabolite) || 0.984 ng/mL; 0.509 ng/mL || ? || Urine, faeces ||Oral || [[CYP2D6]] || 7-OH perphenazine |
|||
|- |
|||
| [[Pimozide]] || 40-50% || 55 hr || ? || 6-8 hr || 4-19 ng/mL (dose-dependent) || ? || Urine || Oral || [[CYP3A4]], [[CYP2D6]] || None |
|||
|- |
|||
| [[Prochlorperazine]] || 12.5% || 6.8-9 hr || High || ? || ? || 12.9-17.7 L/hr || Urine, bile || Oral, IM, IV || ? || N-desmethylprochlorperazine |
|||
|- |
|||
| [[Quetiapine]] || 100% || 6 hr (IR), 7 hr (XR); active metabolite: 12 hr || 83% || 1.5 hr (IR), 6 hr (XR) || @ 250 mg q8hr 778 ng/mL (male), 879 ng/mL (female)<ref>{{cite journal|title=Clinical Pharmacokinetics of Quetiapine An Atypical Antipsychotic|journal=Clinical Pharmacokinetics|date=2001|volume=40|issue=7|pages=509-522|doi=10.2165/00003088-200140070-00003|pmid=11510628|author=DeVane, CL; Nemeroff, CB}}</ref> || 6-14 L/kg || Urine (73%), faeces (20%) || Oral || [[CYP3A4]] || Norquetiapine (a [[norepinephrine reuptake inhibitor]] and [[5-HT1A receptor|5-HT<sub>1A</sub> receptor]] partial agonist) |
|||
|- |
|||
| [[Risperidone]] || 70% || 3-17 hr (24 hr) || 90% (active metabolite: 77%) || 3-17 hr || ? || 1-2 L/kg || Urine (70%), faeces (14%) ||Oral, IM (including depot) || [[CYP2D6]] || [[Paliperidone]] |
|||
|- |
|||
| [[Sertindole]] || ? || 3 days || 99.5% || 10 hr || ? || 20 L/kg || Urine (4%), faeces (46-56%) || Oral || [[CYP2D6]] || None |
|||
|- |
|||
| [[Sulpiride]]<ref>{{cite journal|title=The pharmacokinetics of intravenous and oral sulpiride in healthy human subjects|journal=European Journal of Clinical Pharmacology|date=May 1980|volume=17|issue=5|pages=385-391|pmid=7418717|author=Wiesel, FA; Alfredsson, G; Ehrnebo, M; Sedvall, G|doi=10.1007/BF00558453|url=http://link.springer.com/content/pdf/10.1007/BF00558453.pdf|format=PDF}}</ref> || 27±9% || 8 hr || 40% || 3-6 hr || ? || 2.72±0.66 L/kg || Urine, faeces || Oral || ? || None |
|||
|- |
|||
| [[Thioridazine]] || ? || 24 hr || 95% || ? || ? || ? || ? || Oral || [[CYP2D6]] || None |
|||
|- |
|||
| [[Thiothixene|Tiotixene]] || ? || 24 hr || 90% || ? || ? || ? || ? || Oral || [[CYP1A2]] || None |
|||
|- |
|||
| [[Trifluoperazine]] || ? || 24 hr || ? || ? || ? || ? || ? || Oral || ? || None |
|||
|- |
|||
| [[Ziprasidone]] || 60% (Oral), 100% (IM) || 7 hr (Oral), 2-5 hr (IM) || 99% || 6-8 hr (Oral), ≤60 mins (IM) || ? || 1.5 L/kg || Faeces (66%), urine (20%) || Oral, IM || [[CYP3A4]], [[CYP1A2]] || None |
|||
|- |
|||
| [[Zotepine]]<ref>{{cite journal|title=Zotepine: A Review of its Pharmacodynamic and Pharmacokinetic Properties and Therapeutic Efficacy in the Management of Schizophrenia|journal=CNS Drugs|volume=9|issue=2|pages=153-175|doi=10.2165/00023210-199809020-00006|date=January 1998|author=Prakash, A; Lamb, HM}}</ref><ref>Product Information: Nipolept(R), zotepine. Klinge Pharma GmbH, Munich, 1996.</ref> || 7-13%|| 13.7-15.9 hr (12 hr) || 97% || 1-4 hr || 31-240 || 10 L/kg || Urine (17%) || Oral || [[CYP1A2]], [[CYP3A4]] || Norzotepine (a norepinephrine reuptake inhibitor) |
|||
|- |
|||
| [[Zuclopenthixol]] || 49% || 20 hr || 98% || 2-12 hr (mean: 4 hr) || ? || 20 L/kg || Faeces, urine (10%) || Oral, IM (including depot)|| [[CYP2D6]] || None |
|||
|} |
|||
==Society and culture== |
==Society and culture== |
||
Revision as of 06:32, 29 November 2013

Antipsychotics (also known as neuroleptics or major tranquilizers)[1] are a class of psychiatric medication primarily used to manage psychosis (including delusions, hallucinations, or disordered thought), particularly in schizophrenia and bipolar disorder, and is increasingly being used in the management of non-psychotic disorders (ATC code N05A). The word neuroleptic originates from the Greek word lepsis ("seizure" or "fit").[2]
A first generation of antipsychotics, known as typical antipsychotics, was discovered in the 1950s. Most of the drugs in the second generation, known as atypical antipsychotics, have been developed more recently, although the first atypical antipsychotic, clozapine, was discovered in the 1950s and introduced clinically in the 1970s. Both generations of medication tend to block receptors in the brain's dopamine pathways, but atypicals tend to act on serotonin receptors as well.
Notable and relatively common adverse effects of antipsychotics include extrapyramidal symptoms (which involve motor control) and hyperprolactinaemia primarily in typicals and weight gain and metabolic abnormalities mostly in atypicals.[3] Temporary withdrawal symptoms including insomnia, agitation, psychosis, and motor disorders may occur during dosage reduction of antipsychotics, and can be mistaken for the return of the underlying condition.[4][5]
History
The original antipsychotic drugs were happened upon largely by chance and then tested for their effectiveness. The first, chlorpromazine, was developed as a surgical anesthetic. It was first used on psychiatric patients because of its powerful calming effect; at the time it was regarded as a non-permanent "pharmacological lobotomy".[7] Lobotomy at the time was used to treat many behavioral disorders, including psychosis, although its effect was to markedly reduce behavior and mental functioning of all types. However, chlorpromazine proved to reduce the effects of psychosis in a more effective and specific manner than lobotomy, even though it was known to be capable of causing severe sedation. The underlying neurochemistry involved has since been studied in detail, and subsequent antipsychotic drugs have been discovered by an approach that incorporates this sort of information.
The discovery of chlorpromazine's psychoactive effects in 1952 led to greatly reduced use of restraint, seclusion, and sedation in the management of agitated patients,[7] and also led to further research that resulted in the development of antidepressants, anxiolytics, and the majority of other drugs now used in the management of psychiatric conditions. In 1952, Henri Laborit described chlorpromazine only as inducing indifference towards what was happening around them in nonpsychotic, nonmanic patients, and Jean Delay and Pierre Deniker described it as controlling manic or psychotic agitation. The former claimed to have discovered a treatment for agitation in anyone, and the latter team claimed to have discovered a treatment for psychotic illness.[8]
Until the 1970s there was considerable debate within psychiatry on the most appropriate term to use to describe the new drugs.[9] In the late 1950s the most widely used term was "neuroleptic", followed by "major tranquilizer" and then "ataraxic".[9] The first recorded use of the term tranquilizer dates from the early nineteenth century.[10] In 1953 Frederik F. Yonkman, a chemist at the Swiss based Ciba pharmaceutical company, first used the term tranquilizer to differentiate reserpine from the older sedatives.[11] The word neuroleptic was derived from the Greek: "νεῦρον"(neuron, originally meaning "sinew" but today referring to the nerves) and "λαμβάνω" (lambanō, meaning "take hold of"). Thus, the word means taking hold of one's nerves. This may refer to common side effects such as reduced activity in general, as well as lethargy and impaired motor control. Although these effects are unpleasant and in some cases harmful, they were at one time, along with akathisia, considered a reliable sign that the drug was working.[7] The term "ataraxy" was coined by the neurologist Howard Fabing and the classicist Alister Cameron to describe the observed effect of psychic indifference and detachment in patients treated with chlorpromazine.[12] This term derived from the Greek adjective "ἀτάρακτος" (ataraktos) which means "not disturbed, not excited, without confusion, steady, calm".[9] In the use of the terms "tranquilizer" and "ataractic", medical practitioners distinguished between the "major tranquilizers" or "major ataractics", which referred to drugs used to treat psychoses, and the "minor tranquilizers" or "minor ataractics", which referred to drugs used to treat neuroses.[9] While popular during the 1950s, these terms are infrequently used today. They are being abandoned in favor of "antipsychotic", which refers to the drug's desired effects.[9] Today, "minor tranquilizer" can refer to anxiolytic and/or hypnotic drugs such as the benzodiazepines and nonbenzodiazepines which have some antipsychotic properties and are recommended for concurrent use with antipsychotics, and are useful for insomnia or drug-induced psychosis.[13] They are powerful (and potentially addictive) sedatives.
Antipsychotics are broadly divided into two groups, the typical or first-generation antipsychotics and the atypical or second-generation antipsychotics. The typical antipsychotics are classified according to their chemical structure while the atypical antipsychotics are classified according to their pharmacological properties. These include serotonin-dopamine antagonists (see dopamine antagonist and serotonin antagonist), multi-acting receptor-targeted antipsychotics (MARTA, those targeting several systems), and dopamine partial agonists, which are often categorized as atypicals.[14]
Antipsychotic drugs are now the top-selling class of pharmaceuticals in America, generating annual revenue of about $14.6 billion.[15]
Medical uses
Antipsychotics are most frequently used for the following conditions:
- Schizophrenia
- Schizoaffective disorder most commonly in conjunction with either an antidepressant (in the case of the depressive subtype) or a mood stabiliser (in the case of the bipolar subtype).
- Bipolar disorder (acute mania and mixed episodes may be treated with either typical or atypical antipsychotics, although atypical antipsychotics are usually preferred seeing how they tend to have more favourable adverse effect profiles[16] and, according to a recent meta-analysis, they tend to have a lower liability for causing conversion from mania to depression.[17] Bipolar depression can be treated with quetiapine,[18][19][20][21] olanzapine[22] or lurasidone.[23][24] As for bipolar maintenance several atypical antipsychotics have demonstrated efficacy in preventing manic/mixed relapse[25] but few (with the exception of quetiapine[25][26][27] and olanzapine[28]) have demonstrated efficacy in preventing manic, mixed and depressive relapse as a monotherapy)
- Psychotic depression. In this indication it is a common practice for the attending psychiatrist to prescribe a combination of an atypical antipsychotic and an antidepressant as this practice is best supported by the evidence.[29]
- Treatment-resistant (and not necessarily psychotic) major depression as an adjunct to standard antidepressant therapy.[29]
They are not recommended for dementia or insomnia unless other treatments have not worked.[30] They are not recommended in children unless other treatments are not effective or unless the child has psychosis.[30] Two different antipsychotics should not typically be used in the same person.[30]
List of agents



Clinically used antipsychotic medications are listed below by drug group. Trade names appear in parentheses.
Notes:
† indicates drugs that are no longer marketed in English-speaking countries.
‡ denotes drugs that are no longer (or were never to begin with) marketed in the US. Some antipsychotics are not firmly placed in either first-generation or second-generation classes.
# denotes drugs that have been withdrawn worldwide.
First-generation
Butyrophenones
- Benperidol (Anguil, Benguil, Frenactil, Glianimon)‡
- Bromperidol (Bromodol, Impromen)†
- Droperidol (Droleptan, Inapsine)‡
- Haloperidol (Haldol, Serenace)
- Moperone (Luvatren (discontinued))†
- Pipamperone (Dipiperon, Piperonil (discontinued))†
- Timiperone (Celmanil, Tolopelon)†
Diphenylbutylpiperidine
- Fluspirilene (Imap)
- Penfluridol (Semap)
- Pimozide (Orap)
Phenothiazines
- Acepromazine (Plegicil)† — although it is mostly used in veterinary medicine.
- Chlorpromazine (Largactil, Thorazine (discontinued))
- Cyamemazine (Tercian)†
- Dixyrazine (Esucos)†
- Fluphenazine (Modecate, Permitil (discontinued), Prolixin (discontinued)) – Available in decanoate (long-acting) form
- Levomepromazine (Levinan, Levoprome (discontinued), Nozinan)‡
- Mesoridazine (Lidanil, Serentil (discontinued))†
- Perazine (Peragal, Perazin, Pernazinum, Taxilan)
- Pericyazine (Neulactil, Neuleptil)‡
- Perphenazine (Trilafon)
- Pipotiazine (Lonseren, Piportil)‡
- Prochlorperazine (Compazine)
- Promazine (Prozine, Sparine (discontinued))
- Promethazine (Avomine, Phenergan)
- Prothipendyl (Dominal)†
- Thioproperazine (Majeptil)‡ (only English-speaking country it is available in is Canada)
- Thioridazine (Aldazine (discontinued), Mellaril (discontinued), Melleril (discontinued))
- Trifluoperazine (Stelazine)
- Triflupromazine (Vesprin (discontinued))†
Thioxanthenes
- Chlorprothixene (Cloxan, Taractan, Truxal)†
- Clopenthixol (Sordinol)
- Flupentixol (Depixol, Fluanxol)‡
- Tiotixene (Navane, Thixit)
- Zuclopenthixol (Acuphase, Cisordinol, Clopixol)‡
Others
- Loxapine (Adasuve, Loxitane)
- Prothipendyl (Dominal)†
Disputed/Unknown
This category is for drugs which have been called both first and second-generation, depending on the literature being used.
- Carpipramine (Defekton, Prazinil)†
- Clocapramine (Clofekton, Padrasen)†
- Molindone (Moban)#
- Mosapramine (Cremin)†
- Sulpiride (Meresa)‡
- Sultopride (Barnetil, Topral)†
- Veralipride (Agreal)†
Second-generation
- Amisulpride (Solian)‡– Selective dopamine antagonist. Higher doses (greater than 400 mg) act upon post-synaptic dopamine receptors resulting in a reduction in the positive symptoms of schizophrenia, such as psychosis. Lower doses, however, act upon dopamine autoreceptors, resulting in increased dopamine transmission, improving the negative symptoms of schizophrenia. Lower doses of amisulpride have also been shown to have antidepressant and anxiolytic effects in non-schizophrenic patients, leading to its use indysthymia and social phobias.‡
- Amoxapine (Asendin), active metabolite of loxapine, that's most frequently used as a tricyclic antidepressant and has, in a few clinical trials, been found to possess atypical antipsychotic effects.[31][32][33]
- Aripiprazole (Abilify) – Partial agonist at the D2 receptor unlike all other clinically-utilised antipsychotics.[34]
- Asenapine (Saphris, Sycrest) is a 5-HT2A- and D2-receptor antagonist developed for the treatment of schizophrenia and acute mania associated with bipolar disorder.
- Clozapine (Clozaril) – Requires complete blood counts every one to four weeks due to the risk of agranulocytosis. It has unparalleled efficacy in the treatment of treatment-resistant schizophrenia.
- Blonanserin (Lonasen)† — an antipsychotic that is used in Japan and Korea. May have a beneficial effect on cognition via its antagonism of the 5-HT6 receptor.
- Iloperidone (Fanapt, Fanapta, and previously known as Zomaril) – Approved by the FDA in 2009, it is fairly well tolerated, although hypotension, dizziness, and somnolence were very common side effects. Has not received regulatory approval in other countries, however.
- Lurasidone (Latuda), recently approved by the FDA for schizophrenia and bipolar depression. Given once daily, it has shown mixed Phase III efficacy results but has a relatively well-tolerated side effect profile. It is also licensed for use as schizophrenia treatment in Canada. Not yet licensed elsewhere, however. Has procognitive effects via its antagonism of the 5-HT7 receptor.
- Melperone (Buronil, Buronon, Eunerpan, Melpax, Neuril)†, an atypical antipsychotic that is only used in a few European countries. No English-speaking country has licensed it to date.
- Nemonapride (Emilace)†
- Olanzapine (Zyprexa) – Used to treat psychotic disorders including schizophrenia, acute manic episodes, and maintenance of bipolar disorder. Used as an adjunct to antidepressant therapy, especially to fluoxetine treatment in the form of Symbyax.
- Paliperidone (Invega)– Primary Metabolite of risperidone that was approved in 2006, it offers a controlled releaseonce-daily dose, or a once-monthly depot injection.
- Perospirone (Lullan)† — has a higher incidence of extrapyramidal side effects than other atypical antipsychotics.[35]
- Quetiapine (Seroquel) – Used primarily to treat bipolar disorder and schizophrenia. Also used and licensed in a few countries (including Australia, UK and US) as an adjunct to antidepressant therapy in patients with major depressive disorder. It's the only antipsychotic that's demonstrated efficacy as a monotherapy for the treatment ofmajor depressive disorder. It indirectly serves as a norepinephrine reuptake inhibitor by means of its active metabolite, norquetiapine.
- Remoxipride (Roxiam)# has a risk of causing aplastic anaemia.
- Risperidone (Risperdal) – Divided dosing is recommended until initial titration is completed, at which time the drug can be administered once daily. Used off-label to treat Tourette syndrome and anxiety disorder.
- Sertindole (Serdolect, Serlect)‡. Sertindole was developed by the Danish pharmaceutical company H. Lundbeck. Like the other atypical antipsychotics, it is believed to have antagonist activity at dopamine and serotonin receptors in the brain.
- Trimipramine (Surmontil)
- Ziprasidone (Geodon, Zeldox) – Approved in 2004[36] to treat bipolar disorder. Side-effects include a prolonged QT interval in the heart, which can be dangerous for patients with heart disease or those taking other drugs that prolong the QT interval.
- Zotepine (Lodopin, Losizopilon, Nipolept, Setous) – An atypical antipsychotic indicated for acute and chronic schizophrenia. It is still used in Japan and was once used in Germany but it was recently discontinued.†
Investigational agents
- Bitopertin a GlyT1 inhibitor. Being investigated as a treatment for mostly negative and cognitive symptoms.
- Brexpiprazole a D2/5-HT1A partial agonist.
- Cannabidiol (CBD), one of the active constituents of cannabis that has antipsychotic effects, unlike the chief active constituent of cannabis, namely, tetrahydrocannabinol which has psychotomimetic effects.[37]
- Cariprazine a D3-selective D2/D3 partial agonist.
- Pimavanserin a 5-HT2A inverse agonist. Being investigated as an adjunct to antipsychotics in schizophrenia and as a monotherapy for Parkinson's disease psychosis.
- Pomaglumetad methionil‡‡ a mGluR2/3-selective agonist; development has been ceased due to negative phase III trial results both as a monotherapy and as an adjunct to antipsychotics.[38]
- Vabicaserin‡‡ a 5-HT2C full agonist.
- Xanomeline‡‡ a M1 & M4 agonist.
* where ‡‡ indicates drugs for which development has ceased
Mechanism of action
All antipsychotic drugs tend to block D2 receptors in the dopamine pathways of the brain. This means that dopamine released in these pathways has less effect. Excess release of dopamine in the mesolimbic pathway has been linked to psychotic experiences. It has also been proven[citation needed] less dopamine released in the prefrontal cortex in the brain, and excess dopamine released from all other pathways, has also been linked to psychotic experiences, caused by abnormal dopaminergic function as a result of patients suffering from schizophrenia or bipolar disorder. Various neuroleptics such as haloperidol and chlorpromazine suppress dopamine chemicals throughout its pathways, in order for dopamine receptors to function normally.
In addition of the antagonistic effects of dopamine, antipsychotics (particular atypical narcoleptic) also block serotonin receptors. The over-activation of the serotonin receptor subtype, 5-HT2A has been linked to psychotic experiences such as visual and auditory hallucinations, various delusion disorders, and manic episodes.
Typical antipsychotics are not particularly selective and also block dopamine receptors in the mesocortical pathway, tuberoinfundibular pathway, and the nigrostriatal pathway. Blocking D2 receptors in these other pathways is thought to produce some of the unwanted side effects that the typical antipsychotics can produce (see above). They were commonly classified on a spectrum of low potency to high potency, where potency referred to the ability of the drug to bind to dopamine receptors, and not to the effectiveness of the drug. High-potency antipsychotics such as haloperidol, in general, have doses of a few milligrams and cause less sleepiness and calming effects than low-potency antipsychotics such as chlorpromazine and thioridazine, which have dosages of several hundred milligrams. The latter have a greater degree of anticholinergic and antihistaminergic activity, which can counteract dopamine-related side effects.
Atypical antipsychotic drugs have a similar blocking effect on D2 receptors, however, most also act on serotonin receptors, especially 5-HT2A and 5-HT2C receptors. Both clozapine and quetiapine appear to bind just long enough to elicit antipsychotic effects but not long enough to induce extrapyramidal side effects and prolactin hypersecretion.[39] 5-HT2A antagonism increases dopaminergic activity in the nigrostriatal pathway, leading to a lowered extrapyramidal side effect liability among the atypical antipsychotics.[39][40]
Efficacy
Schizophrenia
In people with schizophrenia less than half (41%) showed any therapeutic response to an atypical antipsychotic, compared to 24% on placebo, there is a decline in treatment response over time, and potentially a biases in the literature in favor of these medication.[41] Risperidone (an atypical antipsychotic), shows only slight benefit compared with placebo and that, despite its widespread use, evidence remains limited, poorly reported and probably biased in favor of risperidone due to pharmaceutical company funding of trials.[42]
Some doubts have been raised about the long-term effectiveness of antipsychotics for schizophrenia, in part because two World Health Organization studies found individuals diagnosed with schizophrenia tend to have better long-term outcomes in developing countries (where there is lower availability and use of antipsychotics and mental health problems are treated with more informal, community-led methods only) than in developed countries.[43][44]
Some argue that the evidence for antipsychotics from discontinuation-relapse studies may be flawed, because they do not take into account that antipsychotics may sensitize the brain and provoke psychosis if discontinued, which may then be wrongly interpreted as a relapse of the original condition.[5] Evidence from comparison studies indicates that at least some individuals with schizophrenia recover from psychosis without taking antipsychotics, and may do better in the long term than those that do take antipsychotics.[45] Some argue that, overall, the evidence suggests that antipsychotics only help if they are used selectively and are gradually withdrawn as soon as possible[46] and have referred to the "Myth of the antipsychotic".[47]
The methods used in trials of antipsychotics, despite stating that the overall quality is "rather good," reported issues with the selection of participants (including that in schizophrenia trials up to 90% of people who are generally suitable do not meet the elaborate inclusion and exclusion criteria, and that negative symptoms have not been properly assessed despite companies marketing the newer antipsychotics for these); issues with the design of trials (including pharmaceutical company funding of most of them, and inadequate experimental "blinding" so that trial participants could sometimes tell whether they were on placebo or not); and issues with the assessment of outcomes (including the use of a minimal reduction in scores to show "response," lack of assessment of quality of life or recovery, a high rate of discontinuation, selective highlighting of favorable results in the abstracts of publications, and poor reporting of side-effects).[48]
While flupenthixol an injectable form of antipsychotic which is given every few weeks is extensively used there is little evidence to support this use.[49] There is little long term data on the benefits of antipsychotics (beyond two to three years).[50] It is recommended that if a person is without symptoms for a year stopping the use of antipsychotics be considered.[50]
Bipolar disorder
Antipsychotics are routinely used, often in conjunction with mood stabilisers such as lithium/valproate, as a first-line treatment for manic and mixed episodes associated with bipolar disorder.[29][51] The reason for this combination is the therapeutic delay of the aforementioned mood stabilisers (for valproate therapeutic effects are usually seen around five days after treatment is commenced whereas lithium usually takes at least a week[51] before the full therapeutic effects are seen) and the comparatively rapid antimanic effects of antipsychotic drugs.[52] The antipsychotics that have documented efficacy as monotherapies in acute mania/mixed episodes include:[16]
- Aripiprazole
- Asenapine (which appears to have efficacy in improving depressive symptoms in acute mania/mixed episodes[53])
- Haloperidol (although this treatment is not recommended because of its relatively high propensity for inducing a depressive switch when compared to the atypical antipsychotics[17])
- Olanzapine
- Paliperidone[54]
- Quetiapine
- Risperidone
- Ziprasidone
Three atypical antipsychotics (lurasidone,[23] olanzapine[22] and quetiapine[19]) have also been found to possess efficacy in the treatment of bipolar depression as a monotherapy. Whereas only olanzapine[28] and quetiapine[26][27] have been proven to be effective broad-spectrum (i.e. against all three types of relapse — manic, mixed and depressive) prophylactic (or maintenance) treatments in patients with bipolar disorder. A recent Cochrane review also found that olanzapine had a less favourable risk/benefit ratio than lithium as a maintenance treatment for bipolar disorder.[55]
The American Psychiatric Association and the UK National Institute for Health and Clinical Excellence recommend antipsychotics for managing acute psychotic episodes in schizophrenia or bipolar disorder, and as a longer-term maintenance treatment for reducing the likelihood of further episodes.[56][57] They state that response to any given antipsychotic can be variable so that trials may be necessary, and that lower doses are to be preferred where possible. A number of studies have looked at levels of "compliance" or "adherence" with antipsychotic regimes and found that discontinuation (stopping taking them) by patients is associated with higher rates of relapse, including hospitalization.
Dementia
Antipsychotics in old age dementia showed a modest benefit compared to placebo in managing aggression or psychosis, but that this was combined with a significant increase in serious adverse events. Thus antipsychotics should not be used routinely to treat dementia patients with aggression or psychosis, but may be an option in a few cases where there is severe distress or risk of physical harm to others.[58]
Unipolar Depression
A number of second-generation (or atypical) antipsychotics have proven to be effective adjuncts in the treatment of major depressive disorder[59][60] of which aripiprazole, quetiapine and olanzapine (when used in conjunction with fluoxetine) have received FDA labelling for this indication.[20] Quetiapine has also proven effective as a monotherapy in major depressive disorder.[61]
Other
Besides the above uses antipsychotics may be used for Obsessive-compulsive disorder, Posttraumatic stress disorder, personality disorders, Tourette syndrome, autism (for which both aripiprazole and risperidone are FDA-labelled) and agitation in those with dementia.[62] Evidence however does not support the use of atypical antipsychotics in eating disorders or personality disorder.[63] Risperidone may be useful for obsessive compulsive disorder.[62] The use of low doses of antipsychotics for insomnia, while common, is not recommended as there is little evidence of benefit and concerns regarding adverse effects.[63][64] Low dose antipsychotics may also be used in treatment of impulse-behavioural and cognitive-perceptual symptoms of borderline personality disorder.[65]
In children they may be used in those with disruptive behavior disorders, mood disorders and pervasive developmental disorders or mental retardation.[66] Antipsychotics are only weakly recommended for Tourette syndrome as well they are effective side effects are common.[67] The situation is similar in autism spectrum disorder.[68] Much of the evidence for the off-label use of antipsychotics (for example, for dementia, OCD, PTSD, Personality Disorders, Tourette's) was of insufficient scientific quality to support such use, especially as there was strong evidence of increased risks of stroke, tremors, significant weight gain, sedation, and gastrointestinal problems.[69] A UK review of unlicensed usage in children and adolescents reported a similar mixture of findings and concerns.[70] A survey of children with pervasive developmental disorder found that 16.5% were taking an antipsychotic drug, most commonly for irritability, aggression, and agitation. Recently, risperidone was approved by the US FDA for the treatment of irritability in children and adolescents with autism.[71]
Aggressive challenging behavior in adults with intellectual disability is often treated with antipsychotic drugs despite lack of an evidence base. A recent randomized controlled trial, however, found no benefit over placebo and recommended that the use of antipsychotics in this way should no longer be regarded as an acceptable routine treatment.[72]
Typicals versus atypicals
While the atypical (second-generation) antipsychotics were marketed as offering greater efficacy and reduced side effects than typical medications this may not be true.[73][74] One review concluded there were no differences[14] while another[75] found that atypicals were "only moderately more efficacious".[14] These conclusions were, however, questioned by another review, which found that clozapine, amisulpride, and olanzapine and risperidone were more effective[14][76] Clozapine has appeared to be more effective than other atypical antipsychotics,[14][77] although it has previously been banned due to its potentially lethal side effects. While controlled clinical trials of atypicals reported that extrapyramidal symptoms occurred in 5–15% of patients, a study of bipolar disorder in a real world clinical setting found a rate of 63%, questioning the generalizability of the trials.[78] Due to bias in the research the accuracy of comparisons of atypical antipsychotics is a concern.[79]
In 2005 the US government body National Institute of Mental Health published the results of a major independent (not funded by the pharmaceutical companies) multi-site, double-blind study (the CATIE project).[80] This study compared several atypical antipsychotics to an older typical antipsychotic, perphenazine, among 1493 persons with schizophrenia. The study found that only olanzapine outperformed perphenazine in discontinuation rate (the rate at which people stopped taking it due to its effects). The authors noted an apparent superior efficacy of olanzapine to the other drugs in terms of reduction in psychopathology and rate of hospitalizations, but olanzapine was associated with relatively severe metabolic effects such as a major weight gain problem (averaging 44 pounds (20 kg) over 18 months) and increases in glucose, cholesterol, and triglycerides. The mean and maximal doses used for olanzapine were considerably higher than standard practice, and this has been postulated as a biasing factor that may explain olanzapine's superior efficacy over the other atypical antipsychotics studied, where doses were more in line with clinically relevant practices.[81] No other atypical studied (risperidone, quetiapine, and ziprasidone) did better than the typical perphenazine on the measures used, nor did they produce fewer adverse effects than the typical antipsychotic perphenazine, although more patients discontinued perphenazine owing to extrapyramidal effects compared to the atypical agents (8% vs. 2% to 4%).[82]
Compliance has not been shown to be different between the two types.[83]
Many researchers question the first-line prescribing of atypicals over typicals, and some even question the distinction between the two classes.[84][85][86] In contrast, other researchers point to the significantly higher risk of tardive dyskinesia and EPS[expand acronym] with the typicals and for this reason alone recommend first-line treatment with the atypicals, notwithstanding a greater propensity for metabolic adverse effects in the latter.[81][87] The UK government organization NICE recently revised its recommendation favoring atypicals, to advise that the choice should be an individual one based on the particular profiles of the individual drug and on the patient's preferences.
The re-evaluation of the evidence has not necessarily slowed the bias towards prescribing the atypicals.[88]
Adverse effects
Antipsychotics are associated with a range of side effects. It is well-recognized that many people stop taking them (around two-thirds even in controlled drug trials) due in part to adverse effects.[89]
- Common (≥1% and up to 50% incidence for most antipsychotic drugs) adverse effects of antipsychotics include
- Sedation (particularly common in patients on clozapine, olanzapine, quetiapine, chlorpromazine and zotepine[90])
- Headaches
- Dizziness
- Diarrhoea
- Anxiety
- Extrapyramidal side effects (particularly common in patients on first-generation antipsychotics) which includes:
- - Akathisia — an often distressing sense of inner restlessness.
- - Dystonia
- - Parkinsonism
- - Tremor
- Hyperprolactinaemia (rare for those on clozapine, quetiapine and aripiprazole[29][90]) which can cause:
- - Galactorrhoea — unusual secretion of breast milk.
- - Gynaecomastia
- - Sexual dysfunction (in both sexes)
- - Osteoporosis
- Orthostatic hypotension
- Weight gain (particularly prominent in patients on clozapine, olanzapine, quetiapine and zotepine[90])
- Anticholinergic side effects such as:
- - Amnesia (although this is not a common adverse effect in patients on antipsychotics)
- - Angle-closure glaucoma (also rare in patients on antipsychotics)
- - Blurred vision
- - Constipation
- - Dry mouth (although hypersalivation may also occur)
- - Reduced perspiration
- Tardive dyskinesia appears to be more frequent in those on high-potency first-generation antipsychotics such as haloperidol and tends to appear after chronic and not acute treatment.[91] It is characterised by slow (hence the tardive) repetitive, involuntary and purposeless movements, most often of the face, lips, legs or torso which tend to resist treatment and are frequently irreversible. The rate of appearance of TD is about 5% per year of use of antipsychotic drug (whatever the drug used).
- Rare/Uncommon (<1% incidence for most antipsychotic drugs) adverse effects of antipsychotics include
- Blood dyscarias (e.g. agranulocytosis, leukopaenia and neutropaenia) which is more common in patients on clozapine.
- Metabolic syndrome and other metabolic problems such as Type II diabetes mellitus — particularly common with clozapine, olanzapine and zotepine. In American studies African Americans appeared to be at a heightened risk for developing type II diabetes mellitus.[92] Evidence suggests that females are more sensitive to the metabolic side effects of first-generation antipsychotic drugs than males.[93] Metabolic adverse effects appears to be mediated by the following mechanisms:
- - Blocking the M3 muscarinic acetylcholine receptor which is responsible for regulating the release of insulin.[94]
- - Inappropriately changing the body's energy source from carbohydrates to lipids.[95]
- - Causing weight gain by antagonising the histamine H1 and serotonin 5-HT2C receptors[96] and perhaps by interacting with other neurochemical pathways in the central nervous system.[97]
- Neuroleptic malignant syndrome a potentially fatal condition characterised by:
- - Autonomic instability which can manifest itself with tachycardia, nausea, vomiting, diaphoresis, etc.
- - Hyperthermia — elevated body temperature.
- - Mental status change (confusion, hallucinations, coma, etc.)
- - Muscle rigidity
- - Laboratory abnormalities (e.g. elevated creatinine kinase, reduced iron plasma levels, electrolyte abnormalities, etc.)
- Pancreatitis[98]
- Pharyngitis[99]
- QT interval prolongation — more prominent in patients on amisulpride, pimozide, sertindole, thioridazine and ziprasidone.[29][90]
- Seizures which is particularly common in patients on chlorpromazine and clozapine.
- Thromboembolism
- Myocardial infarction
- Stroke
- Torsades de Pointes
Some studies have found decreased life expectancy associated with the use of antipsychotics, and argued that more studies are needed.[100][101] Antipsychotics may also increase the risk of early death in individuals with dementia.[102] In individuals without psychosis, doses of antipsychotics can produce the "negative symptoms" of schizophrenia such as amotivation.[103] Antipsychotics typically worsen symptoms in people who suffer from depersonalisation disorder.[104] Antipsychotic polypharmacy (prescribing two or more antipsychotics at the same time for an individual) is said to be a common practice but not necessarily evidence-based or recommended, and there have been initiatives to curtail it.[105] Similarly, the use of excessively high doses (often the result of polypharmacy) continues despite clinical guidelines and evidence indicating that it is usually no more effective but is usually more harmful.[106]
Postulated Adverse Effects
Note: This section is for adverse effects for which the relevance to clinical practice is unknown at the current time.
Chronic treatment with antipsychotics may reduce amounts of brain tissue and potentially cause some of the symptoms believed to be due to schizophrenia[107] According to studies in macaque monkeys cell loss only affects the number of glial cells and not the numbers of neuronal cells.[108] Continuous use of neuroleptics has been shown to decrease the total brain volume by 10% in macaque monkeys.[109][110] The effects may differ for typical versus atypical antipsychotics and may interact with different stages of disorders.[111] Such effects were not clearly tested for by pharmaceutical companies prior to obtaining approval for placing the drugs on the market.[112][113]
A minor loss of brain tissue has been reported in schizophrenics treated with antipsychotics.[114] Brain volume was negatively correlated with both duration of illness and antipsychotic dosage. No association was found with severity of illness or abuse of other substances. An accompanying editorial said: "The findings should not be construed as an indication for discontinuing the use of antipsychotic medications as a treatment for schizophrenia. But they do highlight the need to closely monitor the benefits and adverse effects of these medications in individual patients, to prescribe the minimal amount needed to achieve the therapeutic goal [and] to consider the addition of nonpharmacological approaches that may improve outcomes."[114][115]
Withdrawal
Withdrawal symptoms from antipsychotics may emerge during dosage reduction and discontinuation. Withdrawal symptoms can include nausea, emesis, anorexia, diarrhea, rhinorrhea, diaphoresis, myalgia, paresthesia, anxiety, agitation, restlessness, and insomnia. The psychological withdrawal symptoms can include psychosis, and can be mistaken for a relapse of the underlying disorder. Conversely, the withdrawal syndrome may also be a trigger for relapse. Better management of the withdrawal syndrome may improve the ability of individuals to discontinue antipsychotics.[4][5]
Tardive dyskinesia may abate during withdrawal from the antispsychotic agent, or it may persist.[116] Withdrawal-related psychosis from antipsychotics is called "supersensitivity psychosis", and is attributed to increased number and sensitivity of brain dopamine receptors, due to blockade of dopaminergic receptors by the antipsychotics,[117] which often leads to exacerbated symptoms in the absence of neuroleptic medication.[118] Efficacy of antipsychotics may likewise be reduced over time, due to this development of drug tolerance.[5]
Withdrawal effects may also occur when switching a person from one antipsychotic to another, (presumably due to variations of potency and receptor activity). Such withdrawal effects can include cholinergic rebound, an activation syndrome, and motor syndromes including dyskinesias. These adverse effects are more likely during rapid changes between antipsychotic agents, so making a gradual change between antipsychotics minimises these withdrawal effects.[119] The British National Formulary recommends a gradual withdrawal when discontinuing antipsychotic treatment to avoid acute withdrawal syndrome or rapid relapse.[120] The process of cross-titration involves gradually increasing the dose of the new medication while gradually decreasing the dose of the old medication.[91]
Comparison of medications
Tolerability
| Generic name [16][29][90][121][122][123] |
Discontinuation rate[90]
(OR with 95% CI in brackets) |
Anticholinergic effects | Sedation | EPSE | Weight Gain | Metabolic AEs | QTc prolongation
(ORs & 95% CIs) |
PE | Hypotension | Notes (e.g. notable AEs*) |
|---|---|---|---|---|---|---|---|---|---|---|
| Amisulpride | 0.43 (0.32-0.57) | - | - | + | + | +/- | +++ (0.66 [0.39-0.91]) | +++/++ | - | Torsades de Pointes common on overdose.[124] Has a comparatively low penetrability of the blood-brain barrier. |
| Aripiprazole | 0.61 (0.51-0.72) | - | + | +/- (Akathisia mostly) | + | +/- | - (0.01 [–0.13-0·15]) | - (can reduce prolactin levels) | - | Only clinically-utilised antipsychotic that does not act by antagonising the D2 receptor and rather partially agonises this receptor. |
| Asenapine | 0.69 (0.54-0.86) | - | ++ | + | + | +/- | ++/+ (0.30 [–0.04-0.65]) | ++ | + | Oral hypoesthesia. Has a complex pharmacologic profile. |
| Blonanserin[125][126] | ~0.7 | + | + | ++/+ | +/- | +/- | - | ++/+ | +/- | Only used in a few East Asian countries. |
| Chlorpromazine | 0.65 (0.5-0.84) | +++ | +++ | ++ | ++ | ++ | ++ | +++ | +++ | First marketed antipsychotic, sort of the prototypical low-potency first-generation (typical) antipsychotic. |
| Clozapine | 0.46 (0.32-0.65) | +++ | +++ | - | +++ | +++ | + | - | +++ | Notable AEs: Agranulocytosis, neutropaenia, leukopaenia and myocarditis. Dose-dependent seizure risk.[127] Overall the most effective antipsychotic, on average. Usually reserved for treatment-resistant cases or highly suicidal patients. |
| Droperidol | ? | +/- | +/- | +++ | +/- | +/- | ? | +++ | ? | Mostly used for postoperative nausea and vomiting. |
| Flupenthixol | ? | ++ | + | ++ | ++ | ++ | + | +++ | + | Also used in lower doses for depression. |
| Fluphenazine | 0.69 (0.24-1.97)[128] | ++ | + | +++ | + | + | + | +++ | + | High-potency first-generation (typical) antipsychotic. |
| Haloperidol | 0.8 (0.71-0.90) | + | + | +++ | + | +/- | + (0.11 [0.03-0.19]) | +++ | + | Prototypical high-potency first-generation (typical) antipsychotic. |
| Iloperidone | 0.69 (0.56-0.84) | - | +/- | + | ++ | ++ | ++ (0.34 [0.22-0.46]) | ++/+ | + | ? |
| Levomepromazine | ? | +++ | +++ | ++/+ | ++ | ++ | ? | +++ | +++ | Also used as an analgesic, agitation, anxiety and emesis. |
| Loxapine | 0.52 (0.28-0.98)[129] | + | ++ | +++ | + | +/- | ? | +++ | ++ | ? |
| Lurasidone | 0.77 (0.61-0.96) | - | - | ++/+ | - | - | - (–0.10 [–0.21-0.01]) | ++/+ | - | May be particularly helpful in ameloriating the cognitive symptoms of schizophrenia, likely due to its 5-HT7 receptor.[130] |
| Melperone | ? | - | +/- | +/- | +/- | +/- | +++/++ | +/- | ++/+ | Several smaller low-quality clinical studies have reported its efficacy in the treatment of treatment-resistant schizophrenia. Only approved for use in a few European countries. It is known that off-licence prescribing of melperone is occurring in the United Kingdom.[131] Is a butyrophenone, low-potency atypical antipsychotic that has been tried as a treatment for Parkinson's disease psychosis, although with negative results. |
| Molindone[132] | ? | - | ++/+ | + | - | - | ? | +++ | +/- | Withdrawn from the market. Seems to promote weight loss (which is rather unique for an antipsychotic seeing how they tend to promote weight gain).[132] |
| Olanzapine | 0.46 (0.41-0.52) | + | ++ | + | +++ | +++ | + (0.22 [0.11-0.31]) | + | + | ? |
| Paliperidone | 0.48 (0.39-0.58) | - | - | ++/+ (dose-dependent) | ++ | + | - (0.05 [–0.18-0.26]) | +++ | ++ | Active metabolite of risperidone. |
| Perazine | 0.62 (0.35-1.10)[133] | ? | ? | ? | ? | ? | ? | ? | ? | Limited data available on adverse effects. |
| Pericyazine | ? | +++ | +++ | + | ++ | + | ? | +++ | ++ | Also used to treat severe anxiety. Not licensed for use in the US. |
| Perospirone[134] | ? | +/- | + | ++/+[135] | +/- | ? | - | ++/+ | - | Usually grouped with the atypical antipsychotics despite its relatively high propensity for causing extrapyramidal side effects.[135] |
| Perphenazine | 0.40 (0.08-1.90)[136] | + | + | +++ | + | + | + | +++ | + | Has additional antiemetic effects. |
| Pimozide | 0.66 (0.45-0.98)[137] | + | + | + | + | + | +++ | +++ | + | High potency first-generation (typical) antipsychotic. |
| Prochlorperazine | ? | ? | ? | +++ | ? | ? | + | +++ | ? | Primarily used in medicine as an antiemetic. |
| Quetiapine | 0.61 (0.52-0.71) | ++/+ | ++ | - | ++ | ++/+ | + (0.17 [0.06-0.29]) | - | ++ | Binds to the D2 receptor in a hit and run fashion. That is it rapidly dissociates from said receptor and hence produces antipsychotic effects but does not bind to the receptor long enough to produce extrapyramidal side effects and hyperprolactinaemia. |
| Risperidone | 0.53 (0.46-0.60) | - | ++/+ (dose-dependent) | ++ | ++ | ++/+ | ++ (0.25 [0.15-0.36]) | +++ | ++ | ? |
| Sertindole | 0.78 (0.61-0.98) | - | - | - | ++ | ++/+ | +++ (0.90 [0.76-1.02]) | - | +++ | Not licensed for use in the US. |
| Sulpiride | 1.00 (0.25-4.00)[138] | - | - | + | + | +/- | + | +++/++ | - | Not licensed for use in the US. |
| Thioridazine | 0.67 (0.32-1.40)[139] | +++ | +++ | + | ++ | ++ | +++ | +++ | +++ | Dose-dependent risk for degenerative retinopathies.[140] Found utility in reducing the resistance of multidrug and even extensively resistant strains of tuberculosis to antibiotics. |
| Tiotixene | ? | - | + | +++ | ++ | ++/+ | + | +++ | + | ? |
| Trifluoperazine | 0.94 (0.59-1.48)[141] | +/- | + | +++ | + | +/- | ? | +++ | + | ? |
| Ziprasidone | 0.72 (0.59 to 0.86) | - | ++ | + | - | - | ++ (0.41 [0.31 to 0.51]) | ++/+ | + | ? |
| Zotepine | 0.69 (0.41 to 1.07) | + | +++ | ++ | +++ | +++ | ++ | ++/+ | ++ | Dose-dependent risk of seizures.[142] Not licensed for use in the US. |
| Zuclopenthixol | ? | ++ | ++ | +++ | ++ | ++ | ? | +++ | + | Not licensed for use in the US. |
Note: "Notable" is to mean side effects that are particularly unique to the antipsychotic drug in question. e.g. clozapine is notorious for its ability to cause agranulocytosis. If data on the propensity of a particular drug to cause a particular AE is unavailable an estimation is substituted based on the pharmacologic profile of the drug.
Acronyms used:
AE - Adverse effect
OR - Odds ratio
CI - Confidence Interval
EPSE - Extrapyramidal Side Effect
QTc - Corrected QT interval
PE - Prolactin elevation
'
Legend:
- very low propensity for this AE
+ low propensity/severity for this AE
++ moderate propensity/severity for this AE
+++ high propensity/severity for this AE
Efficacy
| Generic drug name | Schizophrenia[16][90] | Mania[143][144] | Bipolar depression[145] | Bipolar maintenance[146][147] | Adjunct in major depression[148] |
|---|---|---|---|---|---|
| Amisulpride | +++ | ? | ? | ? | ? (+++ in dysthymia) |
| Aripiprazole | ++ | ++ | - | ++ (prevents manic and mixed but not depressive episodes) | +++ |
| Asenapine | ++/+ | ++ | ? | ++ | ? |
| Chlorpromazine | ++ | ? | ? | ? | ? |
| Clozapine | +++ | ? | ? | ? | ? |
| Haloperidol | ++ | +++ | ? | ? | ? |
| Iloperidone | + | ? | ? | ? | ? |
| Loxapine | +++/++ | +++ (only in the treatment of agitation) | ? | ? | ? |
| Lurasidone | + | ? | +++ | ? | ? |
| Melperone | +++ | ? | ? | ? | ? |
| Olanzapine | +++ | +++/++ | ++ | ++ (most effective at preventing manic/mixed relapse) | ++ |
| Paliperidone | ++ | +++/++ | ? | ? | ? |
| Perospirone[149] | + | ? | ? | ? | ? |
| Quetiapine | ++ | ++ | +++ | +++ | ++ |
| Risperidone | +++ | +++ | - | ++ | +++ |
| Sertindole | ++ | ? | ? | ? | ? |
| Ziprasidone | ++/+ | + | ? | + | ? |
| Zotepine | ++ | ? | ? | ? | ? |
Binding affinity
| Generic drug name[96][150] | SERT | 5-HT1A | 5-HT2A | 5-HT2C | 5-HT6 | 5-HT7 | α1A | α2A | α2C | NET | D1 | D2 | D3 | D4 | 5-HT2A/D2 | H1 | M1 | M3 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Amisulpride | >10,000 | >10,000 | 8,304 | >10,000 | 4,154 | 73.5 | >10,000 | 1,114 | 1,540 | >10,000 | >10,000 | 2.2 | 2.4 | 2,370 | 3774.5 | >10,000 | >10,000 | >10,000 |
| Aripiprazole | 1,081 | 5.6 | 8.7 | 22.4 | 642.4 | 9.97 | 25.85 | 74.1 | 37.63 | 2091.5 | 1,173.5 | 1.64 | 5.35 | 514 | 5.3 | 27.93 | 6,778 | 4,678 |
| Asenapine[151] | ND | 2.5 | 0.06 | 0.03 | 0.25 | 0.13 | 1.2 | 1.2 | 1.2 | ND | 1.4 | 1.3 | 0.42 | 1.1 | 0.0462 | 1.0 | 8,128 | 8,128 |
| Blonanserin[152] | ND | 804 | 0.812 | 26.4 | 41.9 | 183 | 26.7 (RB) | 530 (RC) | ND | ND | 1,070 | 0.142 | 0.494 | 150 | 5.72 | 765 | 100 | ND |
| N-DEBN[153] | ND | ND | 1.28 | 4.50 | 5.03 | 206 (RC) | ND | ND | ND | ND | 1,020 | 1.38 | 0.23 | ND | 0.93 | ND | ND | ND |
| Chlorpromazine | 1,296 | 2,115.5 | 4.5 | 15.6 | 17.0 | 28.4 | 0.28 | 184 | 46 | 2,443 | 76.3 | 1.40 | 4.65 | 5.33 | 3.21 | 3.09 | 32.3 | 57.0 |
| Clozapine | 1,624 | 123.7 | 5.35 | 9.44 | 13.5 | 17.95 | 1.62 | 37 | 6.0 | 3,168 | 266.3 | 157 | 269.1 | 26.4 | 0.0341 | 1.13 | 6.17 | 19.25 |
| Norclozapine | 316.6 | 13.9 | 10.9 | 11.9 (RC) | 11.6 | 60.1 | 104.8 | 137.6 | 117.7 | 493.9 | 14.3 | 94.5 | 153 | 63.94 | 0.115 | 3.4 | 67.6 | 95.7 |
| cis-Flupenthixol | ND | 8,028 | 87.5 (HFC) | 102.2 (RC) | ND | ND | ND | ND | ND | ND | 3.5 | 0.35 | 1.75 | 66.3 | 250 | 0.86 | ND | ND |
| Fluphenazine | 5,950 | 1,039.9 | 37.93 | 982.5 | 34.67 | 8.00 | 6.45 | 314.1 | 28.9 | 3,076 | 17.33 | 0.30 | 1.75 | 40.0 | 126.4 | 14.15 | 1,095 | 1,441 |
| Haloperidol | 3,256 | 2,066.83 | 56.81 | 4,801 | 5,133 | 377.6 | 12.0 | 801.5 | 403 | 2,112 | 121.8 | 0.7 | 3.96 | 2.71 | 81.2 | 1698 | >10,000 | >10,000 |
| Iloperidone | ND | 93.21 | 1.94 | 147 | 63.09 | 112 | 0.3 | 160 | 16.2 | 1479 | 129.32 | 10.86 | 10.55 | 13.75 | 0.179 | 12 | 4,898 | >10,000 |
| Loxapine | >10,000 | 2,456 | 6.63 | 13.25 | 31.0 | 87.6 | 31.0 | 150.9 | 80.0 | 5,698 | 54 | 28.1 | 19.33 | 7.80 | 0.236 | 4.90 | 119.45 | 211.33 |
| Amoxapine | 58 | ND | 0.5 | 2.0 (RC) | 50 | 40.21 | 50 | ND | ND | 16 | ND | 20.8 | 21.0 | 21.0 | 0.0240 | 25 | 1,000 | 1,000 |
| Lurasidone[154][155] | ND | 6.8 | 2.0 | 415 | ND | 0.5 | 48 | 1.6 | 10.8 | ND | 262 | 1.7 | ND | ND | 1.18 | >10,000 | >10,000 | >10,000 |
| Melperone | ND | 2,200 (HB) | 230 | 2,100 (HB) | 1,254 (RC) | 578 (HB) | 180 (HB) | 150 (HB) | ND | ND | ND | 194 | 8.95 | 555 | 1.186 | 580 | >10,000 | >10,000 |
| Molindone | ND | 3,797 | 3773 | >10,000 | 1,008 | 3,053 | 2,612 | 1,097 | 172.6 | ND | ND | 6.0 | 72.5 | 2,950 | 628.83 | 2,130 | ND | >10,000 |
| Olanzapine | 3,676 | 2282 | 3.73 | 10.2 | 8.07 | 105.2 | 112 | 314 | 28.9 | >10,000 | 70.33 | 34.23 | 47.0 | 14.33 | 0.109 | 2.19 | 2.5 | 56.33 |
| Paliperidone | 3,717 | 616.6 | 0.71 | 48 | 2,414 | 2.7 | 2.5 | 17.35 | 7.35 | >10,000 | 41.04 | 0.7 | 0.5 | 54.3 | 1.104 | 18.8 | >10,000 | >10,000 |
| Perphenazine | ND | 421 | 5.6 | 132 | 17 | 23 | 10 | 810.5 | 85.2 | ND | ND | 0.14 | 0.13 | 17 | 40 | 8 | 1,500 | 1,848 |
| Pimozide | ND | 650 | 48.35 | 2,112 | 71 | 0.5 | 197.7 | 1,593 | 376.5 | ND | >10,000 | 1.45 | 0.25 | 1.8 | 33.34 | 692.2 | 800 (HB) | 1,955 |
| Prochlorperazine | ND | 5,900 (HC) | 15 (HC) | 122 | 148 (RC) | 196 (RC) | 23.8 (HB) | 1,694.91 (HB) | ND | ND | ND | 0.65 | 2.90 | 5.40 | 23.1 | 18.86 (HB) | 555.55 (HB) | ND |
| Quetiapine | >10,000 | 394.2 | 912 | 1,843 | 948.75 | 307.6 | 22 | 3,630 | 28.85 | >10,000 | 994.5 | 379 | 340 | 2,019 | 2.41 | 6.90 | 489 | 1631.5 |
| Norquetiapine[156] | ND | 45 | 48 | 107 | ND | 76 | 144 | 237 | ND | 12 | 99.8 (RC) | 196 | ND | ND | 0.245 | 3.5 | 38.3 (RC) | ND |
| Risperidone | >10,000 | 422.88 | 0.17 | 12 | 2057.17 | 6.6 | 5 | 16.5 | 1.3 | >10,000 | 243.53 | 3.57 | 2.0 | 4.66 | 0.0476 | 20.05 | >10,000 | >10,000 |
| Sertindole | ND | 280 | 0.39 | 0.9 | 5.4 | 28 | 1.8 | 640 | 450 | ND | ND | 2.35 | 2.30 | 4.92 | 0.166 | 130 | >5,000 | 2,692 |
| Sulpiride | ND | >10,000 | >10,000 (RC) | >10,000 (RC) | 5,000 (RC) | 4,000 (RC) | >10,000 (RB) | 4,893 (RB) | ND | ND | >10,000 | 9.80 | 8.05 | 54 | >1,000 | >10,000 (RB) | >10,000 (RB) | >10,000 (RB) |
| Thioridazine | 1,259 | 144.35 | 27.67 | 53 | 57.05 | 99 | 3.15 | 134.15 | 74.9 | 842 | 94.5 | 2.20 | 1.50 | 6.00 | 12.58 | 16.5 | 12.8 | 29 |
| Thiothixene | 3,878 | 410.2 | 50 | 1355.5 | 245.47 | 15.25 | 11.5 | 79.95 | 51.95 | >10,000 | 51 | 0.12 | 0.40 | 203 | 416.7 | 8 | >10,000 | >10,000 |
| Trifluoperazine | ND | 950 | 74 | 378 | 144 | 290.8 | 24 | 653.7 | 391.5 | ND | ND | 1.12 | ND | 38.1 | 66.07 | 63 | ND | 1,001 |
| Ziprasidone | 112 | 54.67 | 0.73 | 13 | 60.95 | 6.31 | 18 | 160 | 68 | 44 | 30 | 4.35 | 7.85 | 52.9 | 0.1678 | 62.67 | >10,000 | >10,000 |
| Zotepine | 151 | 470.5 | 2.7 | 3.2 | 6 | 12 | 7 | 208 | 106 | 530 | 71 | 25 | 6.4 | 18 | 0.108 | 3.21 | 18 | 73 |
Acronyms used:
HFC - Human frontal cortex receptor
RB - Rat brain receptor
RC - Cloned rat receptor
ND - No data
HB - Human brain receptor
HC - Human cortex receptor
N-DEBN - N-deethylblonanserin
Pharmacokinetic
| Drug[157][158][159][160] | Bioavailability | t1/2 parent drug (active metabolite) |
Protein binding | tmax | Cmax | Vd | Excretion | Routes of administration | Metabolising enzymes[96] | Active metabolites |
|---|---|---|---|---|---|---|---|---|---|---|
| Amisulpride | 48% | 12 hr | 16% | 3-4 hr | 54±4 ng/mL | 5.8 L/kg | Faeces (20%), urine (50%, when given IV) | Oral | ? | None |
| Aripiprazole | 87% (Oral), 100% (IM) | 75 hr (94 hr) | 99% | 3-5 hr | ? | 4.9 L/kg | Faeces (55%), urine (25%) | Oral,IM (including depot) | CYP2D6, CYP3A4 | Dehydroaripiprazole |
| Asenapine | 35% (sublingual) | 24 hr | 95% | 0.5-1.5 hr | 4 ng/mL | 20-25 L/kg | Urine (50%), faeces (40%) | Sublingual | CYP1A2, UGT1A4, CYP2D6 | None |
| Blonanserin[161][162][163] | 55% | 10.7-16.2 hr (single dosing), 67.9 hr (repeated dosing) | ≥99.7% | 1.5-2 hr | 0.14-0.76 ng/mL (0.57 ng/mL for repeated dosing) | 8560-9500 L | Urine (59%), faeces (30%) | Oral | CYP3A4 | N-deethylblonanserin |
| Chlorpromazine | 20% | 30 hr | 92-97% | ? | ? | 20 L/kg | Urine | Oral, IM, IV | CYP2D6 | Several active metabolites |
| Clozapine | 50-60% | 12 hr | 97% | 1.5-2.5 hr | 102-771 ng/mL | 4.67 L/kg | Urine (50%), faeces (30%) | Oral | CYP1A2,CYP2D6, CYP3A4 | Norclozapine |
| Droperidol | ? | 2 hr (8-12 hr) | Extensive | 60 min (IM) | ? | 2 L/kg (adults), 0.58 L/kg (children) | Urine (75%), faeces (22%) | IM, IV | ? | None |
| Flupentixol | 40-55% (Oral) | 35 hr | ? | 7 days (depot) | ? | 12-14 L/kg | Urine | Oral, IM (including depot) | ? | None |
| Fluphenazine | 2.7% (Oral) | 14-16 hrs, 14 days (depot) | ? | 2 hr (Oral), 8-10 hr (depot) | ? | ? | Urine, faeces | Oral, IM (including depot) | ? | None |
| Haloperidol | 60-70% (Oral) | 10-20 hrs (short-acting IM), 3 weeks (depot) | 92% | 2-6 hr (Oral), 10-20 mins (short-acting IM), 6-7 days (depot) | ? | 8-18 L/kg | Urine (30%), faeces (15%) | Oral, IM, IV | CYP3A4 | None |
| Iloperidone | 96% | ? | 95% | 2-4 hr | ? | 1340-2800 L | Urine (45-58%), faeces (20-22%) | Oral | CYP3A4, CYP2D6 | None notable. |
| Levomepromazine | ? | 30 hr | ? | 2-3 hr | ? | ? | Urine, faeces | IM, IV | ? | Methotrimeprazine sulfoxide |
| Loxapine | High | 6-8 hr (Inhaled), 4-12 hr (Oral) | 96.6% | 2 mins (inhaled), 2 hr (oral), 5 hr (IM) | 257 ng/mL (inhaled), 6-13 ng/mL (Oral) | ? | Urine (56-70%), faeces [Only oral data available] | Oral, IM, Inhalation | CYP1A2, CYP3A4, CYP2D6 | Amoxapine (a tricyclic antidepressant), 7-OH loxapine, 8-OH loxapine |
| Lurasidone | 9-19% | 18 hr | 99% | 1-3 hr | ? | 6173 L | Urine (9%), faeces (80%) | Oral | CYP3A4 | 2 active |
| Melperone[164] | 54% (Oral via syrup), 65% (Oral via tablets), 87% (IM) | 2.1-6.4 hrs (Oral), 6.6±3.7 hrs (IM) | 50% | 1.6-2.4 hr (Oral, tablets), 1 hr (Oral, syrup) | 1132±814 ng/mL (25 mg, orally), 2228-3416 ng/mL (50 mg, orally), 89539±37001 ng/mL (100 mg, orally) | 9.9±3.7 L/kg (10 mg), 7±1.61 L/kg (20 mg) | Urine (70% as metabolites, 5.5-10.4% as parent drug) | Oral, IM | ? | None |
| Olanzapine | 87% (Oral) | 30 hr | 93% | 6 hr (Oral), 15-45 min (short-acting IM), 7 days (depot) | 4-20.4 mg/mL[165] | 1000 L | Urine (57%), faeces (30%) | Oral, IM (including depot) | CYP1A2 | None |
| Paliperidone | 28% (Oral) | 23 hr (Oral), 25-49 days (IM) | 74% | 24 hr (Oral), 13 days (IM) | 8.85-11.7 ng/mL[166][167] | 390-487 L | Urine (80%), faeces (11%) | Oral, IM (depot) | CYP3A4, CYP2D6 | None |
| Periciazine | ? | 12 hr | ? | 2 hr | 150 ng/mL | ? | Urine | Oral | ? | ? |
| Perospirone[168] | ? | 1.9-2.5 hr | 92% | 1.5 hr | 5.7 ng/mL | ? | Urine (0.4% as unchanged drug) | Oral | ? | None |
| Perphenazine | ? | 9-12 hr (10-19 hr) | ? | 1-3 hr; 2-4 hr (metabolite) | 0.984 ng/mL; 0.509 ng/mL | ? | Urine, faeces | Oral | CYP2D6 | 7-OH perphenazine |
| Pimozide | 40-50% | 55 hr | ? | 6-8 hr | 4-19 ng/mL (dose-dependent) | ? | Urine | Oral | CYP3A4, CYP2D6 | None |
| Prochlorperazine | 12.5% | 6.8-9 hr | High | ? | ? | 12.9-17.7 L/hr | Urine, bile | Oral, IM, IV | ? | N-desmethylprochlorperazine |
| Quetiapine | 100% | 6 hr (IR), 7 hr (XR); active metabolite: 12 hr | 83% | 1.5 hr (IR), 6 hr (XR) | @ 250 mg q8hr 778 ng/mL (male), 879 ng/mL (female)[169] | 6-14 L/kg | Urine (73%), faeces (20%) | Oral | CYP3A4 | Norquetiapine (a norepinephrine reuptake inhibitor and 5-HT1A receptor partial agonist) |
| Risperidone | 70% | 3-17 hr (24 hr) | 90% (active metabolite: 77%) | 3-17 hr | ? | 1-2 L/kg | Urine (70%), faeces (14%) | Oral, IM (including depot) | CYP2D6 | Paliperidone |
| Sertindole | ? | 3 days | 99.5% | 10 hr | ? | 20 L/kg | Urine (4%), faeces (46-56%) | Oral | CYP2D6 | None |
| Sulpiride[170] | 27±9% | 8 hr | 40% | 3-6 hr | ? | 2.72±0.66 L/kg | Urine, faeces | Oral | ? | None |
| Thioridazine | ? | 24 hr | 95% | ? | ? | ? | ? | Oral | CYP2D6 | None |
| Tiotixene | ? | 24 hr | 90% | ? | ? | ? | ? | Oral | CYP1A2 | None |
| Trifluoperazine | ? | 24 hr | ? | ? | ? | ? | ? | Oral | ? | None |
| Ziprasidone | 60% (Oral), 100% (IM) | 7 hr (Oral), 2-5 hr (IM) | 99% | 6-8 hr (Oral), ≤60 mins (IM) | ? | 1.5 L/kg | Faeces (66%), urine (20%) | Oral, IM | CYP3A4, CYP1A2 | None |
| Zotepine[171][172] | 7-13% | 13.7-15.9 hr (12 hr) | 97% | 1-4 hr | 31-240 | 10 L/kg | Urine (17%) | Oral | CYP1A2, CYP3A4 | Norzotepine (a norepinephrine reuptake inhibitor) |
| Zuclopenthixol | 49% | 20 hr | 98% | 2-12 hr (mean: 4 hr) | ? | 20 L/kg | Faeces, urine (10%) | Oral, IM (including depot) | CYP2D6 | None |
Society and culture
Sales
Antipsychotics are among the biggest selling and most profitable of all drugs, generating $22 billion in global sales in 2008.[173] By 2003 in the US, an estimated 3.21 million patients received antipsychotics, worth an estimated $2.82 billion. Over 2/3 of prescriptions were for the newer more expensive atypicals, each costing on average $164 compared to $40 for the older types.[174] By 2008, sales in the US reached $14.6 billion, the biggest selling drugs in the US by therapeutic class.[175] The number of prescriptions for children and adolescents doubled to 4.4 million between 2003 and 2006, in part because of increases in diagnoses of bipolar disorder.[citation needed]
Formulations
Antipsychotics are sometimes administered as part of compulsory psychiatric treatment via inpatient (hospital) commitment or outpatient commitment. They may be administered orally or, in some cases, through long-acting (depot) injections administered in the dorsgluteal, ventrogluteal or deltoid muscle.
Controversy
According to The Guardian newspaper: "At the heart of years of dissent against psychiatry through the ages has been its use of drugs, particularly antipsychotics, to treat distress. Do such drugs actually target any "psychiatric condition"? Or are they chemical control—a socially-useful reduction of the paranoid, deluded, distressed, bizarre and odd into semi-vegetative zombies?"[47]
Use of this class of drugs has a history of criticism in residential care. As the drugs used can make patients calmer and more compliant, critics claim that the drugs can be overused. Outside doctors can feel under pressure from care home staff.[176] In an official review commissioned by UK government ministers it was reported that the needless use of anti-psychotic medication in dementia care was widespread and was linked to 1800 deaths per year.[177][178] In the US, the government has initiated legal action against the pharmaceutical company Johnson & Johnson for allegedly paying kickbacks to Omnicare to promote its antipsychotic Risperidone (Risperdal) in nursing homes.[179]
There is some controversy over maintenance therapy for schizophrenia.[5][180] A review of studies about maintenance therapy concluded that long-term antipsychotic treatment was superior to placebo in reducing relapse in individuals with schizophrenia, although some of the studies were small.[181] A review of major longitudinal studies in North America found that a moderate number of patients with schizophrenia were seen to recover over time from their symptoms, raising the possibility that some patients may not require maintenance medication.[180] It has also been argued that much of the research into long-term antipsychotic maintenance may be flawed due to failure to take into account the role of antipsychotic withdrawal effects on relapse rates.[5]
There has also been controversy about the role of pharmaceutical companies in marketing and promoting antipsychotics, including allegations of downplaying or covering up adverse effects, expanding the number of conditions or illegally promoting off-label usage; influencing drug trials (or their publication) to try to show that the expensive and profitable newer atypicals were superior to the older cheaper typicals that were out of patent. Following charges of illegal marketing, settlements by two large pharmaceutical companies in the US set records for the largest criminal fines ever imposed on corporations.[15] One case involved Eli Lilly and Company's antipsychotic Zyprexa, and the other involved Bextra. In the Bextra case, the government also charged Pfizer with illegally marketing another antipsychotic, Geodon.[15] In addition, Astrazeneca faces numerous personal-injury lawsuits from former users of Seroquel (quetiapine), amidst federal investigations of its marketing practices.[182] By expanding the conditions for which they were indicated, Astrazeneca's Seroquel and Eli Lilly's Zyprexa had become the biggest selling antipsychotics in 2008 with global sales of $5.5 billion and $5.4 billion respectively.[173]
Harvard medical professor Joseph Biederman conducted research on bipolar disorder in children that led to an increase in such diagnoses. A 2008 Senate investigation found that Biederman also received $1.6 million in speaking and consulting fees between 2000 and 2007 — some of them undisclosed to Harvard — from companies including makers of antipsychotic drugs prescribed for children with bipolar disorder. Johnson & Johnson gave more than $700,000 to a research center that was headed by Biederman from 2002 to 2005, where research was conducted, in part, on Risperdal, the company's antipsychotic drug. Biederman has responded saying that the money did not influence him and that he did not promote a specific diagnosis or treatment.[15]
Pharmaceutical companies have also been accused of attempting to set the mental heath agenda through activities such as funding consumer advocacy groups.[183]
References
- ^ Cubeddu, Richard Finkel, Michelle A. Clark, Luigi X. (2009). Pharmacology (4th ed. ed.). Philadelphia: Lippincott Williams & Wilkins. p. 151. ISBN 9780781771559.
{{cite book}}:|edition=has extra text (help)CS1 maint: multiple names: authors list (link) - ^ Moby's Medical Dictionary. Elsevier.
- ^ Frankenburg FR, Dunayevich E, Albucher RC, Talavera F. Schizophrenia. 2013 Aug 22 [cited 2013 Oct 2]; Available from: http://emedicine.medscape.com/article/288259-overview
- ^ a b Dilsaver SC, Alessi NE (1988). "Antipsychotic withdrawal symptoms: phenomenology and pathophysiology". Acta Psychiatr Scand. 77 (3): 241–6. doi:10.1111/j.1600-0447.1988.tb05116.x. PMID 2899377.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ a b c d e f Moncrieff J (2006). "Why is it so difficult to stop psychiatric drug treatment? It may be nothing to do with the original problem". Med. Hypotheses. 67 (3): 517–23. doi:10.1016/j.mehy.2006.03.009. PMID 16632226. Cite error: The named reference "Moncrieff-2006" was defined multiple times with different content (see the help page).
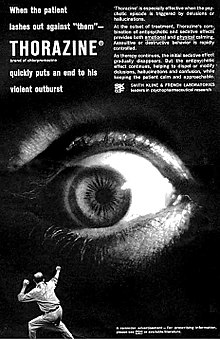
- ^ The text reads: When the patient lashes out against "them" - THORAZINE (brand of chlorpromazine) quickly puts an end to his violent outburst. 'Thorazine' is especially effective when the psychotic episode is triggered by delusions or hallucinations. At the outset of treatment, Thorazine's combination of antipsychotic and sedative effects provides both emotional and physical calming. Assaultive or destructive behavior is rapidly controlled. As therapy continues, the initial sedative effect gradually disappears. But the antipsychotic effect continues, helping to dispel or modify delusions, hallucinations and confusion, while keeping the patient calm and approachable. SMITH KLINE AND FRENCH LABORATORIES leaders in psychopharmaceutical research.
- ^ a b c Pieters, Toine (1 December 2011). "The introduction of chlorpromazine in Belgium and the Netherlands (1951–1968); tango between old and new treatment features". Studies in History and Philosophy of Science Part C: Studies in History and Philosophy of Biological and Biomedical Sciences. 42 (4): 443–452. doi:10.1016/j.shpsc.2011.05.003.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Healy, D. 2005. Psychiatric Drugs Explained. 4th Ed. Britain:Elsevier Limited. P. 8, 17.
- ^ a b c d e King, Caroline (2002-05). "What's in a name? The evolution of the nomenclature of antipsychotic drugs". Journal of Psychiatry and Neuroscience. 27 (3): 168–75. ISSN 1180-4882. PMC 161646. PMID 12066446.
{{cite journal}}: Check date values in:|date=(help); Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ "tranquillizer, n". Oxford English Dictionary. 1989. Retrieved 9 August 2011.
- ^ Healy, David (2008). "The intersection of psychopharmacology and psychiatry in the second half of the twentieth century". In Wallace, Edwin R.; Gach, John (ed.). History of Psychiatry and Medical Psychology. Boston, MA: Springer US. p. 421. ISBN 978-0-387-34707-3. Retrieved 9 August 2011.
{{cite book}}: CS1 maint: multiple names: editors list (link) - ^ Owens, David Griffith Cunningham (13 April 1999). A guide to the extrapyramidal side-effects of antipsychotic drugs. Cambridge University Press. p. 12. ISBN 978-0-521-63353-6.
- ^ Tasman, Allan. Psychiatry Volume 2. Saunders. p. 956. ISBN 0-7216-5257-3.
- ^ a b c d e Horacek J; Bubenikova-Valesova V; Kopecek M; et al. (2006). "Mechanism of action of atypical antipsychotic drugs and the neurobiology of schizophrenia". CNS Drugs. 20 (5): 389–409. doi:10.2165/00023210-200620050-00004. PMID 16696579.
{{cite journal}}: Unknown parameter|author-separator=ignored (help) - ^ a b c d Wilson, Duff (2 October 2010). "Side Effects May Include Lawsuits". New York Times.
- ^ a b c d Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 19058842, please use {{cite journal}} with
|pmid=19058842instead. - ^ a b Goikolea JM, Colom F, Torres I, Capapey J, Valentí M, Undurraga J, et al. Lower rate of depressive switch following antimanic treatment with second-generation antipsychotics versus haloperidol. Journal of Affective Disorders [Internet]. 2013 Jan 25 [cited 2013 Oct 2];144(3):191–8. Available from: http://www.sciencedirect.com/science/article/pii/S0165032712005691
- ^ Young AH, McElroy SL, Bauer M, Philips N, Chang W, Olausson B, et al. A double-blind, placebo-controlled study of quetiapine and lithium monotherapy in adults in the acute phase of bipolar depression (EMBOLDEN I). J Clin Psychiatry. 2010 Feb;71(2):150–62.
- ^ a b Thase ME. Quetiapine monotherapy for bipolar depression. Neuropsychiatr Dis Treat [Internet]. 2008 Feb [cited 2013 Oct 2];4(1):21–31. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2515925/
- ^ a b Truven Health Analytics, Inc. DrugPoint® System (Internet) [cited 2013 Oct 2]. Greenwood Village, CO: Thomsen Healthcare; 2013.
- ^ Suppes T, Datto C, Minkwitz M, Nordenhem A, Walker C, Darko D. Effectiveness of the extended release formulation of quetiapine as monotherapy for the treatment of acute bipolar depression. Journal of Affective Disorders [Internet]. 2010 Feb [cited 2013 Oct 2];121(1–2):106–15. Available from: http://www.sciencedirect.com/science/article/pii/S0165032709004674
- ^ a b Tohen M, Katagiri H, Fujikoshi S, Kanba S. Efficacy of olanzapine monotherapy in acute bipolar depression: A pooled analysis of controlled studies. Journal of Affective Disorders [Internet]. 2013 Jul [cited 2013 Oct 2];149(1–3):196–201. Available from: http://www.sciencedirect.com/science/article/pii/S0165032713000773
- ^ a b Lowes R. Lurasidone Approved for Bipolar Depression [Internet]. Medscape. 2013 [cited 2013 Oct 2]. Available from: http://www.medscape.com/viewarticle/807204
- ^ Fruyt JD, Deschepper E, Audenaert K, Constant E, Floris M, Pitchot W, et al. Second generation antipsychotics in the treatment of bipolar depression: a systematic review and meta-analysis. J Psychopharmacol [Internet]. 2012 May 1 [cited 2013 Oct 2];26(5):603–17. Available from: http://jop.sagepub.com/content/26/5/603
- ^ a b Popovic D, Reinares M, Goikolea JM, Bonnin CM, Gonzalez-Pinto A, Vieta E. Polarity index of pharmacological agents used for maintenance treatment of bipolar disorder. European Neuropsychopharmacology [Internet]. 2012 May [cited 2013 Oct 2];22(5):339–46. Available from: http://www.sciencedirect.com/science/article/pii/S0924977X11002616
- ^ a b Duffy A, Milin R, Grof P. Maintenance treatment of adolescent bipolar disorder: open study of the effectiveness and tolerability of quetiapine. BMC Psychiatry [Internet]. 2009 [cited 2013 Oct 1];9(1):4. Available from: http://www.biomedcentral.com/1471-244X/9/4
- ^ a b Weisler RH, Nolen WA, Neijber A, Hellqvist A, Paulsson B, Trial 144 Study Investigators. Continuation of quetiapine versus switching to placebo or lithium for maintenance treatment of bipolar I disorder (Trial 144: a randomized controlled study). J Clin Psychiatry. 2011 Nov;72(11):1452–64.
- ^ a b Tohen M, Greil W, Calabrese JR, Sachs GS, Yatham LN, Oerlinghausen BM, et al. Olanzapine Versus Lithium in the Maintenance Treatment of Bipolar Disorder: A 12-Month, Randomized, Double-Blind, Controlled Clinical Trial. Am J Psychiatry [Internet]. 2005 Jul 1 [cited 2013 Oct 1];162(7):1281–90. Available from: http://dx.doi.org/10.1176/appi.ajp.162.7.1281
- ^ a b c d e f Taylor D, Paton C, Kapur S, Taylor D, South London and Maudsley NHS Trust. The Maudsley prescribing guidelines in psychiatry. Chichester, West Sussex: John Wiley & Sons; 2012. pp. 233-234 Cite error: The named reference "Maudsley" was defined multiple times with different content (see the help page).
- ^ a b c "American Psychiatric Association Five Things Physicians and Patients Should Question". Choosing Wisely. Retrieved 23 September 2013.
- ^ Chaudhry IB, Husain N, Khan S, Badshah S, Deakin B, Kapur S. Amoxapine as an Antipsychotic: Comparative Study Versus Haloperidol. Journal of Clinical Psychopharmacology [Internet]. 2007 Dec [cited 2013 Oct 2];27(6):575–81. Available from: http://journals.lww.com/psychopharmacology/pages/articleviewer.aspx?year=2007&issue=12000&article=00004&type=abstract
- ^ Apiquian R, Fresan A, Ulloa R-E, de la Fuente-Sandoval C, Herrera-Estrella M, Vazquez A, et al. Amoxapine as an Atypical Antipsychotic: A Comparative Study Vs Risperidone. Neuropsychopharmacology [Internet]. 2005 Jun 8 [cited 2013 Oct 2];30(12):2236–44. Available from: http://www.nature.com/npp/journal/v30/n12/full/1300796a.html
- ^ Apiquian R, Ulloa E, Fresan A, Loyzaga C, Nicolini H, Kapur S. Amoxapine shows atypical antipsychotic effects in patients with schizophrenia: results from a prospective open-label study. Schizophrenia Research [Internet]. 2003 Jan 1 [cited 2013 Oct 2];59(1):35–9. Available from:http://www.sciencedirect.com/science/article/pii/S0920996401003425
- ^ Swainston Harrison T, Perry CM (2004). "Aripiprazole: a review of its use in schizophrenia and schizoaffective disorder". Drugs. 64 (15): 1715–36. doi:10.2165/00003495-200464150-00010. PMID 15257633.
- ^ Onrust, SV; McClellan, K (2001). "Perospirone". CNS Drugs. 15 (4): 329–37, discussion 338. doi:10.2165/00023210-200115040-00006. PMID 11463136.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Nemeroff CB, Lieberman JA, Weiden PJ, Harvey PD, Newcomer JW, Schatzberg AF, Kilts CD, Daniel DG. (2005). "From clinical research to clinical practice: a 4-year review of ziprasidone". CNS Spectr. 10 (11 Suppl 17): 1–20. PMID 16381088.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Zuardi AW, Crippa JA, Hallak JE; et al. (2012). "A critical review of the antipsychotic effects of cannabidiol: 30 years of a translational investigation". Curr. Pharm. Des. 18 (32): 5131–40. doi:10.2174/138161212802884681. PMID 22716160.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Patil ST; Zhang L; Martenyi F; et al. (2007). "Activation of mGlu2/3 receptors as a new approach to treat schizophrenia: a randomized Phase 2 clinical trial". Nature Medicine. 13 (9): 1102–7. doi:10.1038/nm1632. PMID 17767166.
{{cite journal}}:|first10=missing|last10=(help);|first11=missing|last11=(help); Unknown parameter|author-separator=ignored (help); Unknown parameter|laydate=ignored (help); Unknown parameter|laysource=ignored (help); Unknown parameter|laysummary=ignored (help); Unknown parameter|month=ignored (help) - ^ a b Stahl, SM (2003). "Describing an Atypical Antipsychotic: Receptor Binding and Its Role in Pathophysiology" (PDF). Prim Care Companion J Clin Psychiatry. 5 (Suppl. 3): 9–13.
- ^ Gross, Gerhard; Geyer, Mark A. (2012). Current Antipsychotics. Springer. pp. 88–89. doi:10.1007/978-3-642-25761-2. ISBN 978-3-642-25761-2.
- ^ Leucht S, Arbter D, Engel RR, Kissling W, Davis JM (2009). "How effective are second-generation antipsychotic drugs? A meta-analysis of placebo-controlled trials". Mol. Psychiatry. 14 (4): 429–47. doi:10.1038/sj.mp.4002136. PMID 18180760.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Rattehalli RD, Jayaram MB, Smith M (2010). Rattehalli, Ranganath (ed.). "Risperidone versus placebo for schizophrenia". Cochrane Database of Systematic Reviews (1): CD006918. doi:10.1002/14651858.CD006918. PMID 20091611.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Jablensky A, Sartorius N, Ernberg G; et al. (1992). "Schizophrenia: manifestations, incidence and course in different cultures. A World Health Organization ten-country study". Psychol Med Monogr Suppl. 20: 1–97. doi:10.1017/S0264180100000904. PMID 1565705.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Hopper K, Wanderling J (2000). "Revisiting the developed versus developing country distinction in course and outcome in schizophrenia: results from ISoS, the WHO collaborative followup project. International Study of Schizophrenia". Schizophr Bull. 26 (4): 835–46. doi:10.1093/oxfordjournals.schbul.a033498. PMID 11087016.
- ^ Harrow M, Jobe TH (2007). "Factors involved in outcome and recovery in schizophrenia patients not on antipsychotic medications: a 15-year multifollow-up study". J. Nerv. Ment. Dis. 195 (5): 406–14. doi:10.1097/01.nmd.0000253783.32338.6e. PMID 17502806.
{{cite journal}}: Unknown parameter|doi_brokendate=ignored (|doi-broken-date=suggested) (help); Unknown parameter|month=ignored (help) - ^ Whitaker R (2004). "The case against antipsychotic drugs: a 50-year record of doing more harm than good". Med. Hypotheses. 62 (1): 5–13. doi:10.1016/S0306-9877(03)00293-7. PMID 14728997.
- ^ a b James, Adam (2 March 2008). "Myth of the antipsychotic". The Guardian. Guardian News and Media Limited. Retrieved 27 July 2012.
- ^ Leucht S, Heres S, Hamann J, Kane JM (2008). "Methodological issues in current antipsychotic drug trials". Schizophr Bull. 34 (2): 275–85. doi:10.1093/schbul/sbm159. PMC 2632403. PMID 18234700.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Shen X, Xia J, Adams CE (2012). Shen, Xiaohong (ed.). "Flupenthixol versus placebo for schizophrenia". Cochrane Database of Systematic Reviews. 11: CD009777. doi:10.1002/14651858.CD009777.pub2. PMID 23152280.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ a b Harrow M, Jobe TH (2013). "Does Long-Term Treatment of Schizophrenia With Antipsychotic Medications Facilitate Recovery?". Schizophr Bull. 39 (5): 962–5. doi:10.1093/schbul/sbt034. PMC 3756791. PMID 23512950.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ a b Young LL, Kradjan WA, Guglielmo BJ, Corelli RL, Williams BR, Koda-Kimble MA, et al. Applied Therapeutics: The Clinical Use of Drugs. 9th ed. Lippincott Williams & Wilkins; 2009.
- ^ Correll CU, Sheridan EM, DelBello MP. Antipsychotic and mood stabilizer efficacy and tolerability in pediatric and adult patients with bipolar I mania: a comparative analysis of acute, randomized, placebo-controlled trials. Bipolar Disorders [Internet]. 2010 [cited 2013 Oct 2];12(2):116–41. Available from: http://onlinelibrary.wiley.com/doi/10.1111/j.1399-5618.2010.00798.x/abstract
- ^ Azorin JM, Sapin C, Weiller E. Effect of asenapine on manic and depressive symptoms in bipolar I patients with mixed episodes: Results from post hoc analyses. Journal of Affective Disorders [Internet]. 2013 Feb 15 [cited 2013 Oct 2];145(1):62–9. Available from: http://www.jad-journal.com/article/S0165-0327(12)00532-0/abstract
- ^ Berwaerts J, Xu H, Nuamah I, Lim P, Hough D. Evaluation of the efficacy and safety of paliperidone extended-release in the treatment of acute mania: A randomized, double-blind, dose-response study. Journal of Affective Disorders [Internet]. 2012 Jan [cited 2013 Oct 2];136(1–2):e51–e60. Available from: http://www.sciencedirect.com/science/article/pii/S0165032710004581
- ^ Cipriani A, Rendell JM, Geddes J (2009). Cipriani, Andrea (ed.). "Olanzapine in long-term treatment for bipolar disorder". Cochrane Database of Systematic Reviews (1): CD004367. doi:10.1002/14651858.CD004367.pub2. PMID 19160237.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Lehman AF, Lieberman JA, Dixon LB; et al. (2004). "Practice guideline for the treatment of patients with schizophrenia, second edition". Am J Psychiatry. 161 (2 Suppl): 1–56. PMID 15000267.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ The Royal College of Psychiatrists & The British Psychological Society (2003). Schizophrenia. Full national clinical guideline on core interventions in primary and secondary care (PDF). London: Gaskell and the British Psychological Society.[dead link][page needed]
- ^ Ballard C, Waite J (2006). Ballard, Clive G (ed.). "The effectiveness of atypical antipsychotics for the treatment of aggression and psychosis in Alzheimer's disease". Cochrane Database of Systematic Reviews (1): CD003476. doi:10.1002/14651858.CD003476.pub2. PMID 16437455.
- ^ Komossa K, Depping AM, Gaudchau A, Kissling W, Leucht S. Second-generation antipsychotics for major depressive disorder and dysthymia. Cochrane Database of Systematic Reviews [Internet]. John Wiley & Sons, Ltd; 2010 [cited 2013 Oct 2]. Available from: http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD008121.pub2/abstract
- ^ Spielmans GI, Berman MI, Linardatos E, Rosenlicht NZ, Perry A, Tsai AC. Adjunctive Atypical Antipsychotic Treatment for Major Depressive Disorder: A Meta-Analysis of Depression, Quality of Life, and Safety Outcomes. PLoS Med [Internet]. 2013 Mar 12 [cited 2013 Oct 2];10(3):e1001403. Available from: http://dx.doi.org/10.1371/journal.pmed.1001403
- ^ Maneeton N, Maneeton B, Srisurapanont M, Martin SD. Quetiapine monotherapy in acute phase for major depressive disorder: a meta-analysis of randomized, placebo-controlled trials. BMC Psychiatry [Internet]. 2012 Sep 27 [cited 2013 Oct 2];12:160. Available from: http://go.galegroup.com/ps/i.do?id=GALE%7CA315508130&v=2.1&u=james_cook&it=r&p=HRCA&sw=w
- ^ a b Maher AR, Theodore G (2012). "Summary of the comparative effectiveness review on off-label use of atypical antipsychotics". J Manag Care Pharm. 18 (5 Suppl B): S1–20. PMID 22784311.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ a b Maglione, Margaret; Maher, Alicia Ruelaz; Hu, Jianhui; Wang, Zhen; Shanman, Roberta; Shekelle, Paul G; Roth, Beth; Hilton, Lara; Suttorp, Marika J (2011). Off-Label Use of Atypical Antipsychotics: An Update. Comparative Effectiveness Reviews, No. 43. Rockville: Agency for Healthcare Research and Quality. PMID 22132426.[page needed]
- ^ Coe HV, Hong IS (2012). "Safety of low doses of quetiapine when used for insomnia". Annals of Pharmacotherapy. 46 (5): 718–22. doi:10.1345/aph.1Q697. PMID 22510671.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ American Psychiatric Association and American Psychiatric Association. Work Group on Borderline Personality Disorder (2001). Practice Guideline for the Treatment of Patients With Borderline Personality Disorder. American Psychiatric Pub. p. 4. ISBN 0890423199. Retrieved 5 June 2013.
- ^ Zuddas, A (2011 Aug). "Second generation antipsychotics (SGAs) for non-psychotic disorders in children and adolescents: a review of the randomized controlled studies". European neuropsychopharmacology : the journal of the European College of Neuropsychopharmacology. 21 (8): 600–20. doi:10.1016/j.euroneuro.2011.04.001. PMID 21550212.
{{cite journal}}: Check date values in:|date=(help); Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Pringsheim T, Doja A, Gorman D; et al. (2012). "Canadian guidelines for the evidence-based treatment of tic disorders: pharmacotherapy". Can J Psychiatry. 57 (3): 133–43. PMID 22397999.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ McPheeters ML, Warren Z, Sathe N; et al. (2011). "A systematic review of medical treatments for children with autism spectrum disorders". Pediatrics. 127 (5): e1312–21. doi:10.1542/peds.2011-0427. PMID 21464191.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ "Evidence Lacking to Support Many Off-label Uses of Atypical Antipsychotics" (Press release). Agency for Healthcare Research and Quality. 17 January 2007. Retrieved 29 July 2013.
- ^ James, Anthony C. (2010). "Prescribing antipsychotics for children and adolescents". Advances in Psychiatric Treatment. 16 (1): 63–75. doi:10.1192/apt.bp.108.005652.
- ^ Posey DJ, Stigler KA, Erickson CA, McDougle CJ (2008). "Antipsychotics in the treatment of autism". J. Clin. Invest. 118 (1): 6–14. doi:10.1172/JCI32483. PMC 2171144. PMID 18172517.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Romeo R, Knapp M, Tyrer P, Crawford M, Oliver-Africano P (2009). "The treatment of challenging behaviour in intellectual disabilities: cost-effectiveness analysis". J Intellect Disabil Res. 53 (7): 633–43. doi:10.1111/j.1365-2788.2009.01180.x. PMID 19460067.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Alexander GC, Gallagher SA, Mascola A, Moloney RM, Stafford RS (2011). "Increasing off-label use of antipsychotic medications in the United States, 1995-2008". Pharmacoepidemiol Drug Saf. 20 (2): 177–84. doi:10.1002/pds.2082. PMC 3069498. PMID 21254289.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Geddes J, Freemantle N, Harrison P, Bebbington P (2000). "Atypical antipsychotics in the treatment of schizophrenia: systematic overview and meta-regression analysis". BMJ. 321 (7273): 1371–6. doi:10.1136/bmj.321.7273.1371. PMC 27538. PMID 11099280.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Leucht S, Wahlbeck K, Hamann J, Kissling W (2003). "New generation antipsychotics versus low-potency conventional antipsychotics: a systematic review and meta-analysis". Lancet. 361 (9369): 1581–9. doi:10.1016/S0140-6736(03)13306-5. PMID 12747876.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Davis JM, Chen N, Glick ID (2003). "A meta-analysis of the efficacy of second-generation antipsychotics". Archives of General Psychiatry. 60 (6): 553–64. doi:10.1001/archpsyc.60.6.553. PMID 12796218.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Tuunainen A, Wahlbeck K, Gilbody SM (2000). Tuunainen, Arja (ed.). "Newer atypical antipsychotic medication versus clozapine for schizophrenia". Cochrane Database of Systematic Reviews (2): CD000966. doi:10.1002/14651858.CD000966. PMID 10796559.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Ghaemi SN, Hsu DJ, Rosenquist KJ, Pardo TB, Goodwin FK (2006). "Extrapyramidal side effects with atypical neuroleptics in bipolar disorder". Prog. Neuropsychopharmacol. Biol. Psychiatry. 30 (2): 209–13. doi:10.1016/j.pnpbp.2005.10.014. PMID 16412546.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Heres, S (2006 Feb). "Why olanzapine beats risperidone, risperidone beats quetiapine, and quetiapine beats olanzapine: an exploratory analysis of head-to-head comparison studies of second-generation antipsychotics". The American Journal of Psychiatry. 163 (2): 185–94. doi:10.1176/appi.ajp.163.2.185. PMID 16449469.
{{cite journal}}: Check date values in:|date=(help); Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Lieberman JA, Stroup TS, McEvoy JP; et al. (2005). "Effectiveness of antipsychotic drugs in patients with chronic schizophrenia". N. Engl. J. Med. 353 (12): 1209–23. doi:10.1056/NEJMoa051688. PMID 16172203.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ a b Meltzer HY, Bobo WV (2006). "Interpreting the efficacy findings in the CATIE study: what clinicians should know". CNS Spectr. 11 (7 Suppl 7): 14–24. PMID 16816796.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Leucht S, Corves C, Arbter D, Engel RR, Li C, Davis JM (2009). "Second-generation versus first-generation antipsychotic drugs for schizophrenia: a meta-analysis". Lancet. 373 (9657): 31–41. doi:10.1016/S0140-6736(08)61764-X. PMID 19058842.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Voruganti LP, Baker LK, Awad AG (2008). "New generation antipsychotic drugs and compliance behaviour". Current Opinion in Psychiatry. 21 (2): 133–9. doi:10.1097/YCO.0b013e3282f52851. PMID 18332660.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Paczynski RP, Alexander GC, Chinchilli VM, Kruszewski SP (2012). "Quality of evidence in drug compendia supporting off-label use of typical and atypical antipsychotic medications". Int J Risk Saf Med. 24 (3): 137–46. doi:10.3233/JRS-2012-0567. PMID 22936056.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Owens, D. C. (2008). "How CATIE brought us back to Kansas: a critical re-evaluation of the concept of atypical antipsychotics and their place in the treatment of schizophrenia". Advances in Psychiatric Treatment. 14 (1): 17–28. doi:10.1192/apt.bp.107.003970.
- ^ Fischer-Barnicol D, Lanquillon S, Haen E; et al. (2008). "Typical and atypical antipsychotics--the misleading dichotomy. Results from the Working Group 'Drugs in Psychiatry' (AGATE)". Neuropsychobiology. 57 (1–2): 80–7. doi:10.1159/000135641. PMID 18515977.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Casey DE (1999). "Tardive dyskinesia and atypical antipsychotic drugs". Schizophr. Res. 35 (Suppl 1): S61–6. doi:10.1016/S0920-9964(98)00160-1. PMID 10190226.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Makhinson M (2010). "Biases in medication prescribing: the case of second-generation antipsychotics". J Psychiatr Pract. 16 (1): 15–21. doi:10.1097/01.pra.0000367774.11260.e4. PMID 20098227.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Bellack AS (2006). "Scientific and Consumer Models of Recovery in Schizophrenia: Concordance, Contrasts, and Implications". Schizophrenia Bulletin. 32 (3): 432–42. doi:10.1093/schbul/sbj044. PMC 2632241. PMID 16461575.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ a b c d e f g Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 23810019, please use {{cite journal}} with
|pmid=23810019instead. - ^ a b Stahl, S. M. (2008). Stahl's Essential Psychopharmacology: Neuroscientific basis and practical applications. Cambridge University Press.[page needed]
- ^ Koller EA, Doraiswamy PM (2002). "Olanzapine-associated diabetes mellitus". Pharmacotherapy. 22 (7): 841–52. doi:10.1592/phco.22.11.841.33629. PMID 12126218.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Weston-Green K, Huang XF, Deng C (2010). "Sensitivity of the female rat to olanzapine-induced weight gain--far from the clinic?". Schizophr. Res. 116 (2–3): 299–300. doi:10.1016/j.schres.2009.09.034. PMID 19840894.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Weston-Green K, Huang XF, Lian J, Deng C (2012). "Effects of olanzapine on muscarinic M3 receptor binding density in the brain relates to weight gain, plasma insulin and metabolic hormone levels". Eur Neuropsychopharmacol. 22 (5): 364–73. doi:10.1016/j.euroneuro.2011.09.003. PMID 21982116.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Albaugh VL, Vary TC, Ilkayeva O, Wenner BR, Maresca KP, Joyal JL, et al. Atypical Antipsychotics Rapidly and Inappropriately Switch Peripheral Fuel Utilization to Lipids, Impairing Metabolic Flexibility in Rodents. Schizophr Bull [Internet]. 2012 Jan [cited 2013 Oct 2];38(1):153–66. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3245588/
- ^ a b c Brunton L, Chabner B, Knollman B. Goodman and Gilman’s The Pharmacological Basis of Therapeutics, Twelfth Edition. McGraw Hill Professional; 2010.
- ^ Weston-Green K, Huang XF, Deng C (2012). Chang, Alice Y. W (ed.). "Alterations to melanocortinergic, GABAergic and cannabinoid neurotransmission associated with olanzapine-induced weight gain". PLoS ONE. 7 (3): e33548. doi:10.1371/journal.pone.0033548. PMC 3306411. PMID 22438946.
{{cite journal}}: CS1 maint: multiple names: authors list (link) CS1 maint: unflagged free DOI (link) - ^ Koller EA, Cross JT, Doraiswamy PM, Malozowski SN (2003). "Pancreatitis associated with atypical antipsychotics: from the Food and Drug Administration's MedWatch surveillance system and published reports". Pharmacotherapy. 23 (9): 1123–30. doi:10.1592/phco.23.10.1123.32759. PMID 14524644.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ "Mosby's Medical Dictionary, 8th edition". Elsevier. 2009. Retrieved 30 June 2010.
- ^ Weinmann S, Read J, Aderhold V (2009). "Influence of antipsychotics on mortality in schizophrenia: systematic review". Schizophr. Res. 113 (1): 1–11. doi:10.1016/j.schres.2009.05.018. PMID 19524406.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Joukamaa M, Heliövaara M, Knekt P, Aromaa A, Raitasalo R, Lehtinen V (2006). "Schizophrenia, neuroleptic medication and mortality". Br J Psychiatry. 188 (2): 122–7. doi:10.1192/bjp.188.2.122. PMID 16449697.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ American Geriatrics Society 2012 Beers Criteria Update Expert Panel (2012). "American Geriatrics Society updated Beers Criteria for potentially inappropriate medication use in older adults". J Am Geriatr Soc. 60 (4): 616–31. doi:10.1111/j.1532-5415.2012.03923.x. PMC 3571677. PMID 22376048.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: numeric names: authors list (link) - ^ Artaloytia JF, Arango C, Lahti A; et al. (2006). "Negative signs and symptoms secondary to antipsychotics: a double-blind, randomized trial of a single dose of placebo, haloperidol, and risperidone in healthy volunteers". Am J Psychiatry. 163 (3): 488–93. doi:10.1176/appi.ajp.163.3.488. PMID 16513871.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Medford N, Sierra M, Baker D, David A. (2005). "Understanding and treating depersonalisation disorder". Advances in Psychiatric Treatment. 11 (2). Royal College of Psychiatrists: 92–100. doi:10.1192/apt.11.2.92.
{{cite journal}}: Cite has empty unknown parameter:|month=(help)CS1 maint: multiple names: authors list (link) - ^ Patrick V, Levin E, Schleifer S (2005). "Antipsychotic polypharmacy: is there evidence for its use?". J Psychiatr Pract. 11 (4): 248–57. doi:10.1097/00131746-200507000-00005. PMID 16041235.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Ito H, Koyama A, Higuchi T (2005). "Polypharmacy and excessive dosing: psychiatrists' perceptions of antipsychotic drug prescription". Br J Psychiatry. 187 (3): 243–7. doi:10.1192/bjp.187.3.243. PMID 16135861.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Moncrieff, J (2010 Sep). "A systematic review of the effects of antipsychotic drugs on brain volume". Psychological Medicine. 40 (9): 1409–22. doi:10.1017/S0033291709992297. PMID 20085668.
{{cite journal}}: Check date values in:|date=(help); Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Konopaske GT, Dorph-Petersen K-A, Pierri JN, Wu Q, Sampson AR, Lewis DA. Effect of Chronic Exposure to Antipsychotic Medication on Cell Numbers in the Parietal Cortex of Macaque Monkeys. Neuropsychopharmacology [Internet]. 2006 Oct 25 [cited 2013 Oct 2];32(6) 1216–23. Available from: http://www.nature.com/npp/journal/v32/n6/abs/1301233a.html
- ^ Dorph-Petersen KA, Pierri JN, Perel JM, Sun Z, Sampson AR, Lewis DA (2005). "The influence of chronic exposure to antipsychotic medications on brain size before and after tissue fixation: a comparison of haloperidol and olanzapine in macaque monkeys". Neuropsychopharmacology. 30 (9): 1649–61. doi:10.1038/sj.npp.1300710. PMID 15756305.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Breggin, P (2007). Brain disabling treatments in psychiatry. Springer Publishing Compan. p. 320. ISBN 082612934X.
{{cite book}}: Cite has empty unknown parameter:|coauthors=(help) - ^ Vita A, De Peri L (2007). "The effects of antipsychotic treatment on cerebral structure and function in schizophrenia". International Review of Psychiatry. 19 (4): 429–36. doi:10.1080/09540260701486332. PMID 17671875.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ DeLisi LE (2008). "The Concept of Progressive Brain Change in Schizophrenia: Implications for Understanding Schizophrenia". Schizophrenia Bulletin. 34 (2): 312–21. doi:10.1093/schbul/sbm164. PMC 2632405. PMID 18263882.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Konopaske GT, Dorph-Petersen KA, Sweet RA; et al. (2008). "Effect of chronic antipsychotic exposure on astrocyte and oligodendrocyte numbers in macaque monkeys". Biol. Psychiatry. 63 (8): 759–65. doi:10.1016/j.biopsych.2007.08.018. PMC 2386415. PMID 17945195.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ a b Ho BC, Andreasen NC, Ziebell S, Pierson R, Magnotta V (2011). "Long-term antipsychotic treatment and brain volumes: a longitudinal study of first-episode schizophrenia". Arch. Gen. Psychiatry. 68 (2): 128–37. doi:10.1001/archgenpsychiatry.2010.199. PMC 3476840. PMID 21300943.
{{cite journal}}: Unknown parameter|laydate=ignored (help); Unknown parameter|laysource=ignored (help); Unknown parameter|laysummary=ignored (help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Lewis DA (2011). "Antipsychotic medications and brain volume: do we have cause for concern?". Arch. Gen. Psychiatry. 68 (2): 126–7. doi:10.1001/archgenpsychiatry.2010.187. PMID 21300942.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Glazer WM (2000). "Expected incidence of tardive dyskinesia associated with atypical antipsychotics". J Clin Psychiatry. 61 Suppl 4: 21–6. PMID 10739327.
- ^ Samaha AN, Seeman P, Stewart J, Rajabi H, Kapur S (2007). ""Breakthrough" dopamine supersensitivity during ongoing antipsychotic treatment leads to treatment failure over time". J. Neurosci. 27 (11): 2979–86. doi:10.1523/JNEUROSCI.5416-06.2007. PMID 17360921.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Gitlin M, Nuechterlein K, Subotnik KL; et al. (2001). "Clinical outcome following neuroleptic discontinuation in patients with remitted recent-onset schizophrenia". Am J Psychiatry. 158 (11): 1835–42. doi:10.1176/appi.ajp.158.11.1835. PMID 11691689.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Lambert TJ (2007). "Switching antipsychotic therapy: what to expect and clinical strategies for improving therapeutic outcomes". J Clin Psychiatry. 68 Suppl 6: 10–3. PMID 17650054.
- ^ Group, BMJ, ed. (2009). "4.2.1". British National Formulary (57 ed.). United Kingdom: Royal Pharmaceutical Society of Great Britain. p. 192.
Withdrawal of antipsychotic drugs after long-term therapy should always be gradual and closely monitored to avoid the risk of acute withdrawal syndromes or rapid relapse.
{{cite book}}: Unknown parameter|month=ignored (help) - ^ Template:Cite isbn
- ^ Template:Cite isbn
- ^ "Approximate relative frequency (not intensity) of common adverse effects of antipsychotics (Table 8.21) [NB1]". eTherapeutic Guidelines complete. Therapeutic Guidelines Limited. February 2013. Retrieved 2 November 2013.
- ^ Isbister, GK; Balit, CR; Macleod, D; Duffull, SB (August 2010). "Amisulpride overdose is frequently associated with QT prolongation and torsades de pointes". Journal of Clinical Psychopharmacology. 30 (4): 391–395. doi:10.1097/JCP.0b013e3181e5c14c. PMID 20531221.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Deeks, ED; Keating, GM (January 2010). "Blonanserin A Review of its Use in the Management of Schizophrenia". CNS Drugs. 24 (1): 65–84. doi:10.2165/11202620-000000000-00000. PMID 20030420.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Tenjin, T; Miyamoto, S; Ninomiya, Y; Kitajima, R; Ogino, S; Miyake, N; Yamaguchi, N (2013). "Profile of blonanserin for the treatment of schizophrenia". Neuropsychiatric Disease and Treatment. 9: 587–594. doi:10.2147/NDT.S34433. PMID 23766647.
{{cite journal}}: CS1 maint: multiple names: authors list (link) CS1 maint: unflagged free DOI (link) - ^ "Clozapine". Martindale: The Complete Drug Reference. Royal Pharmaceutical Society of Great Britain. 30 January 2013. Retrieved 2 November 2013.
- ^ Matar, HE; Almerie, MQ; Sampson, S (July 2013). "Fluphenazine (oral) versus placebo for schizophrenia (Review)" (PDF). Cochrane Database of Systematic Reviews. 7: CD006352. doi:10.1002/14651858.CD006352.pub2. PMID 23861067.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Chakrabarti, A; Bagnall, A; Chue, P; Fenton, M; Palaniswamy, V; Wong, W; Xia, J (October 2007). "Loxapine for schizophrenia (Review)" (PDF). Cochrane Database of Systematic Reviews (4): CD001943. doi:10.1002/14651858.CD001943.pub2. PMID 17943763.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Harvey, PD; Ogasa, M; Cucchiaro, J; Loebel, A; Keefe, RS (April 2011). "Performance and interview-based assessments of cognitive change in a randomized, double-blind comparison of lurasidone vs. ziprasidone". Schizophrenia Research. 127 (1–3): 188–194. doi:10.1016/j.schres.2011.01.004. PMID 21277745.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Röhricht, F (2012). "Auditing Clinical Outcomes after Introducing Off-Licence Prescribing of Atypical Antipsychotic Melperone for Patients with Treatment Refractory Schizophrenia". Scientific World Journal. doi:10.1100/2012/512047. PMC 3330679. PMID 22566771.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help)CS1 maint: unflagged free DOI (link) - ^ a b Molindone Hydrochloride. The Royal Pharmaceutical Society of Great Britain. 30 January 2013. Retrieved 5 November 2013.
{{cite book}}:|work=ignored (help) - ^ Leucht, S; Hartung, B (April 2006). "Perazine for schizophrenia" (PDF). Cochrane Database of Systematic Reviews (2): CD002832. doi:10.1002/14651858.CD002832.pub2. PMID 16625562.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Onrust, SV; McClellan, K (April 2001). "Perospirone" (PDF). CNS Drugs. 15 (4): 329–337. doi:10.2165/00023210-200115040-00006. PMID 11463136.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ a b Brayfield, A, ed. (23 September 2011). Perospirone. London, UK: Pharmaceutical Press. Retrieved 3 November 2013.
{{cite book}}:|work=ignored (help) - ^ Hartung, B; Wada, M; Laux, G; Leucht, S (January 2005). "Perphenazine for schizophrenia" (PDF). The Cochrane Database of Systematic Review (1): CD003443. doi:10.1002/14651858.CD003443.pub2. PMID 15674907.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Rathbone, J; McMonagle, T (July 2007). "Pimozide for schizophrenia or related psychoses" (PDF). The Cochrane Database of Systematic Review (3): CD001949. doi:10.1002/14651858.CD001949.pub2. PMID 17636692.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Omori, IM; Wang, J (April 2009). "Sulpiride versus placebo for schizophrenia" (PDF). Cochrane Database of Systematic Reviews (2): CD007811. doi:10.1002/14651858.CD007811. PMID 19370694.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Fenton, M; Rathbone, J; Reilly, J; Sultana, A (July 2007). "Thioridazine for schizophrenia" (PDF). Cochrane Database of Systematic Reviews (3): CD001944. doi:10.1002/14651858.CD001944.pub2. PMID 17636691.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Fornaro, P; Calabria, G; Corallo, G; Picotti, GB (July 2002). "Pathogenesis of degenerative retinopathies induced by thioridazine and other antipsychotics: a dopamine hypothesis". Documenta Ophthalmologica. 105 (1): 41–49. doi:10.1023/A:1015768114192. PMID 12152801.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Marques, LO; Lima, MS; Soares, BG (2004). "Trifluoperazine for schizophrenia" (PDF). Cochrane Database of Systematic Reviews (1): CD003545. doi:10.1002/14651858.CD003545.pub2. PMID 14974020.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ "Zotepine". Martindale: The Complete Drug Reference. Royal Pharmaceutical Society of Great Britain. 16 August 2013. Retrieved 2 November 2013.
- ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 21851976, please use {{cite journal}} with
|pmid=21851976instead. - ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 23723707, please use {{cite journal}} with
|pmid=23723707instead. - ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 19638254, please use {{cite journal}} with
|pmid=19638254instead. - ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 22000157, please use {{cite journal}} with
|pmid=22000157instead. - ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 21733231, please use {{cite journal}} with
|pmid=21733231instead. - ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 21154393, please use {{cite journal}} with
|pmid=21154393instead. - ^ Kishi, T; Iwata, N (September 2013). "Efficacy and Tolerability of Perospirone in Schizophrenia: A Systematic Review and Meta-Analysis of Randomized Controlled Trials" (PDF). CNS Drugs. 27 (9): 731–741. doi:10.1007/s40263-013-0085-7. PMID 23812802.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Roth, BL; Driscol, J (12 January 2011). "PDSP Ki Database". Psychoactive Drug Screening Program (PDSP). University of North Carolina at Chapel Hill and the United States National Institute of Mental Health. Retrieved 11 November 2013.
{{cite web}}: CS1 maint: multiple names: authors list (link) - ^ Shahid M, Walker GB, Zorn SH, Wong E. Asenapine: a novel psychopharmacologic agent with a unique human receptor signature. J Psychopharmacol [Internet]. 2009 Jan 1 [cited 2013 Sep 22];23(1):65–73. Available from: http://jop.sagepub.com/content/23/1/65
- ^ Tenjin T, Miyamoto S, Ninomiya Y, Kitajima R, Ogino S, Miyake N, et al. Profile of blonanserin for the treatment of schizophrenia. Neuropsychiatr Dis Treat [Internet]. 2013 [cited 2013 Aug 6];9:587–94. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3677929/
- ^ Deeks ED, Keating GM. Blonanserin. CNS Drugs [Internet]. 2010 Jan 1 [cited 2013 Aug 6];24(1):65–84. Available from: http://link.springer.com/content/pdf/10.2165%2F11202620-000000000-00000.pdf
- ^ Ishibashi T, Horisawa T, Tokuda K, Ishiyama T, Ogasa M, Tagashira R, et al. Pharmacological Profile of Lurasidone, a Novel Antipsychotic Agent with Potent 5-Hydroxytryptamine 7 (5-HT7) and 5-HT1A Receptor Activity. J Pharmacol Exp Ther [Internet]. 2010 Jul 1 [cited 2013 Jul 26];334(1):171–81. Available from: http://jpet.aspetjournals.org/content/334/1/171
- ^ Ishiyama T, Tokuda K, Ishibashi T, Ito A, Toma S, Ohno Y. Lurasidone (SM-13496), a novel atypical antipsychotic drug, reverses MK-801-induced impairment of learning and memory in the rat passive-avoidance test. European Journal of Pharmacology [Internet]. 2007 Oct 31 [cited 2013 Sep 22];572(2–3):160–70. Available from: http://www.sciencedirect.com/science/article/pii/S0014299907007376
- ^ López-Muñoz F, Álamo C. Active metabolites as antidepressant drugs: the role of norquetiapine in the mechanism of action of quetiapine in the treatment of mood disorders. Front Psychiatry [Internet]. 2013 [cited 2013 Sep 22];4:102. Available from: http://www.frontiersin.org/Neuropharmacology/10.3389/fpsyt.2013.00102/abstract
- ^ "Article title". Medscape Reference. WebMD. Retrieved 29 November 2013.
- ^ "article title" (PDF). TGA eBusiness Services. [Drug sponsor]. [date page was last modified]. Retrieved 29 November 2013.
{{cite web}}: Check date values in:|date=(help) - ^ "DailyMed". DailyMed. [Drug sponsor]. [Date page was last modified]. Retrieved 29 November 2013.
{{cite web}}: Check date values in:|date=(help) - ^ "Article title". electronic Medicines Compendium. Drug Sponsor. date last modified. Retrieved 29 November 2013.
{{cite web}}: Check date values in:|date=(help) - ^ Deeks, ED; Keating, GM (January 2010). "Blonanserin A Review of its Use in the Management of Schizophrenia". CNS Drugs. 24 (1): 65–84. doi:10.2165/11202620-000000000-00000. PMID 20030420.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Tenjin, T; Miyamoto, S; Ninomiya, Y; Kitajima, R; Ogino, S; Miyake, N; Yamaguchi, N (2013). "Profile of blonanserin for the treatment of schizophrenia". Neuropsychiatric Disease and Treatment. 9: 587–594. doi:10.2147/NDT.S34433. PMID 23766647.
{{cite journal}}: CS1 maint: multiple names: authors list (link) CS1 maint: unflagged free DOI (link) - ^ Wen, YG; Shang, DW; Xie, HZ; Wang, XP; Ni, XJ; Zhang, M; Lu, W; Qiu, C; Liu, X; Li, FF; Li, X; Luo, FT (March 2013). "Population pharmacokinetics of blonanserin in Chinese healthy volunteers and the effect of the food intake". Human Psychopharmacology. 28 (2): 134–141. doi:10.1002/hup.2290. PMID 23417765.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Borgström, L (1982). "Pharmacokinetics of parenteral and oral melperone in man". European Journal of Clinical Pharmacology. 23 (2): 173–176. doi:10.1007/BF00545974. PMID 7140807.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Callaghan, JT; Bergstrom, RF; Ptak, LR; Beasley, CM (September 1999). "Olanzapine. Pharmacokinetic and pharmacodynamic profile". Clinical Pharmacokinetics. 37 (3): 177–193. doi:10.2165/00003088-199937030-00001. PMID 10511917.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Vermeir, M; Naessens, I; Remmerie, B; Mannens, G; Hendrickx, J; Sterkens, P; Talluri, K; Boom, S; Eerdekens, M; van Osselaer, N; Cleton, A (April 2008). "Absorption, Metabolism, and Excretion of Paliperidone, a New Monoaminergic Antagonist, in Humans" (PDF). Drug Metabolism and Disposition. 36 (4): 769–779. doi:10.1124/dmd.107.018275. PMID 18227146.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Álamo, C; López-Muñoz, F (January 2013). "The Pharmacological Role and Clinical Applications of Antipsychotics' Active Metabolites: Paliperidone versus Risperidone" (PDF). Clinical and Experimental Pharmacology. 3 (1): 117. doi:10.4172/2161-1459.1000117.
{{cite journal}}: CS1 maint: multiple names: authors list (link) CS1 maint: unflagged free DOI (link) - ^ Onrust, SV; McClellan, K (2001). "Perospirone". CNS Drugs. 15 (4): 329–37, discussion 338. doi:10.2165/00023210-200115040-00006. PMID 11463136.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ DeVane, CL; Nemeroff, CB (2001). "Clinical Pharmacokinetics of Quetiapine An Atypical Antipsychotic". Clinical Pharmacokinetics. 40 (7): 509–522. doi:10.2165/00003088-200140070-00003. PMID 11510628.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Wiesel, FA; Alfredsson, G; Ehrnebo, M; Sedvall, G (May 1980). "The pharmacokinetics of intravenous and oral sulpiride in healthy human subjects" (PDF). European Journal of Clinical Pharmacology. 17 (5): 385–391. doi:10.1007/BF00558453. PMID 7418717.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Prakash, A; Lamb, HM (January 1998). "Zotepine: A Review of its Pharmacodynamic and Pharmacokinetic Properties and Therapeutic Efficacy in the Management of Schizophrenia". CNS Drugs. 9 (2): 153–175. doi:10.2165/00023210-199809020-00006.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Product Information: Nipolept(R), zotepine. Klinge Pharma GmbH, Munich, 1996.
- ^ a b drugs to drive next market evolution (2009)[dead link]. Healthcarefinancenews.com (7 August 2009).
- ^ Aparasu, R. R.; Bhatara, V. (2006). "Antipsychotic Use and Expenditure in the United States". Psychiatric Services. 57 (12): 1693–1693. doi:10.1176/appi.ps.57.12.1693. PMID 17158480.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ 2008 U.S. Sales and Prescription Information: Top Therapeutic Classes by U.S. Sales (PDF). Imshealth.com.
- ^ GPs under 'pressure' to issue neuroleptics, claims professor, Chemist + Druggist, 15 January 2009
- ^ Nick Triggle (12 November 2009). "Dementia drug use 'killing many'". BBC. Retrieved 7 May 2013.
- ^ "UK study warns against anti-psychotics for dementia". reuters. 12 November 2009. Retrieved 7 May 2013.
- ^ Hilzenrath, David S. (16 January 2010). "Justice suit accuses Johnson & Johnson of paying kickbacks". The Washington Post. Retrieved 17 January 2010.
- ^ a b Jobe TH, Harrow M (2005). "Long-term outcome of patients with schizophrenia: a review" (PDF). Canadian Journal of Psychiatry. 50 (14): 892–900. PMID 16494258. Retrieved 5 July 2008.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Kane, JM.; Leucht, S. (2008). "Unanswered Questions in Schizophrenia Clinical Trials". Schizophr Bull. 34 (2): 302–9. doi:10.1093/schbul/sbm143. PMC 2632396. PMID 18199633.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ DUFF WILSON (27). "Drug Maker's E-Mail Released in Seroquel Lawsuit". The New York Times. The New York Times Company. Retrieved 27 July 2012.
{{cite news}}: Check date values in:|date=and|year=/|date=mismatch (help); Unknown parameter|month=ignored (help) - ^ Gosden R, Beder S (2001). "Pharmaceutical industry agenda setting in mental health policies". Ethical Human Sciences and Services : an International Journal of Critical Inquiry. 3 (3): 147–59. PMID 15278977.
External links
- Are atypical antipsychotics advantageous? - the case for, Australian Prescriber 2005 (note: pharmaceutical company conflict of interest statement at the end)
- Are atypical antipsychotics advantageous? - the case against, Australian Prescriber 2005
- First Generation Antipsychotics: An Introduction, Psychopharmacology Institute, 2012
- Bipolar Meds - The Antipsychotics, mcmanweb.com
- FDA Public Health Advisory[dead link] - Public Health Advisory for Antipsychotic Drugs used for Treatment of Behavioral Disorders in Elderly Patients, fda.gov
- FROTA LH. Partial Agonists in the Schizophrenia Armamentarium. Tardive Dysphrenia: The newest challenge to the last generation atypical antipsychotics drugs? J Bras Psiquiatr 2003; Vol 52 Supl 1;14-24. Free full-text in Portuguese with Abstracts in English, medicina.ufrj.br
- Antipsychotic Medication - information from mental health charity The Royal College of Psychiatrists
- Template:Pt icon FROTA LH. Fifty Years of Antipsychotic Drugs in Psychiatry. "Cinqüenta Anos de Medicamentos Antipsicóticos em Psiquiatria." 1st ed; Ebook: CD-Rom/On-Line Portuguese, ISBN 85-903827-1-0, File .pdf (Adobe Acrobat) 6Mb, Informática, Rio de Janeiro, August 2003, 486pp., medicina.ufrj.br
