User:Aparnaji/sandbox: Difference between revisions
←Replaced content with '{{User sandbox}} <!-- EDIT BELOW THIS LINE -->' |
|||
| Line 1: | Line 1: | ||
{{User sandbox}} |
{{User sandbox}} |
||
<!-- EDIT BELOW THIS LINE --> |
<!-- EDIT BELOW THIS LINE --> |
||
{{about|pregnancy in humans|pregnancy in other animals|pregnancy (mammals)}} |
|||
<noinclude>{{pp-semi-vandalism|small=yes}} |
|||
{{pp-move-indef}}</noinclude> |
|||
{{Use dmy dates|date=December 2012}} |
|||
{{Infobox disease |
|||
| Name = Pregnancy |
|||
| Image = PregnantWoman.jpg| Caption = A pregnant woman. |
|||
| DiseasesDB = 10545 |
|||
| ICD10 = {{ICD10|Z|33||z|30}} |
|||
| ICD9 = {{ICD9|650}} |
|||
| MedlinePlus =002398 |
|||
| eMedicineSubj =article |
|||
| eMedicineTopic =259724 |
|||
| MeshID =D011247 |
|||
}} |
|||
'''Pregnancy''' is the [[Human fertilization|fertilization]] and development of one or more offspring, known as an [[embryo]] or [[fetus]], in a woman's [[uterus]]. It is the common name for [[gestation]] in [[human]]s. A [[multiple birth|multiple pregnancy]] involves more than one embryo or fetus a single pregnancy, such as with [[twin]]s. [[Childbirth]] usually occurs about 38 weeks after conception; in women who have a menstrual cycle length of four weeks, this is approximately 40 weeks from the start of the last normal menstrual period (LNMP). Human pregnancy is the most studied of all [[Pregnancy (mammals)|mammalian pregnancies]]. Conception can be achieved through [[sexual intercourse]] or [[assisted reproductive technology]]. |
|||
An ''[[embryo]]'' is the developing offspring during the first 8 weeks following conception, and subsequently the term ''fetus'' is used until birth.<ref>{{cite web |url=http://www.medterms.com/script/main/art.asp?articlekey=3225 |title=Embryo definition |date=27 April 2011 |publisher=MedicineNet, Inc}}</ref><ref>{{cite web |url=http://www.medterms.com/script/main/art.asp?articlekey=3424 |title=Fetus definition |date=27 April 2011|publisher=MedicineNet, Inc}}</ref> In many societies' medical or legal definitions, human pregnancy is somewhat arbitrarily divided into three trimester periods, as a means to simplify reference to the different stages of [[prenatal development]]. The first trimester carries the highest risk of [[miscarriage]] (natural death of embryo or fetus). During the second trimester, the development of the fetus can be more easily monitored and diagnosed. The beginning of the third trimester often approximates the point of [[Point of fetal viability|viability]], or the ability of the fetus to survive, with or without medical help, outside of the [[uterus]].<ref>{{cite web |url=http://www.medterms.com/script/main/art.asp?articlekey=11446 |title=Trimester definition |date=27 April 2011 |publisher=MedicineNet, Inc}}</ref> |
|||
In the United States and United Kingdom, 40% of pregnancies are [[Unintended pregnancy|unplanned]], and between a quarter and half of those unplanned pregnancies were [[unwanted pregnancies]].<ref>{{cite news|title=40% of pregnancies 'unplanned'|url=http://news.bbc.co.uk/2/hi/health/3515400.stm|newspaper=[[BBC News]]|date=16 March 2004}}</ref><ref>{{cite news|last=Jayson|first=Sharon|title=Unplanned pregnancies in U.S. at 40 percent|url=http://www.physorg.com/news/2011-05-unplanned-pregnancies-percent.html|newspaper=[[PhysOrg.com]]|date=20 May 2011}}</ref> Of those unintended pregnancies that occurred in the US, 60% of the women used [[birth control]] to some extent during the month pregnancy occurred.<ref>{{cite book |authors=K. Joseph Hurt, Matthew W. Guile, Jessica L. Bienstock, Harold E. Fox, Edward E. Wallach (eds.) |title=The Johns Hopkins manual of gynecology and obstetrics |publisher=Wolters Kluwer Health / Lippincott Williams & Wilkins |location=Philadelphia |isbn=9781605474335 |pages=232 |url=http://books.google.ca/books?id=4Sg5sXyiBvkC&pg=PR232 |edition=4th}}</ref> |
|||
{{TOC limit|3}} |
|||
==Terminology== |
|||
One scientific term for the state of pregnancy is ''gravidity'' (adjective ''"gravid"''), [[Latin]] for "heavy" and a pregnant female is sometimes referred to as a ''[[Gravidity|gravida]]''.<ref name = 'MFD'>{{cite web |url=http://medical-dictionary.thefreedictionary.com/gravida |title=definition of gravida |accessdate=17 January 2008 |publisher=[[TheFreeDictionary.com|The Free Dictionary]]}}</ref> Similarly, the term ''[[Parity (medicine)|parity]]'' (abbreviated as "para") is used for the number of times a female has given birth, counting twins and other multiple births as one pregnancy, and usually including [[stillbirth]]s. Medically, a woman who has never been pregnant is referred to as a ''nulligravida'', a woman who is (or has been only) pregnant for the first time as a ''primigravida'',<ref name=TMHP>{{cite-TMHP|Primipara}}, page 596.</ref> and a woman in subsequent pregnancies as a ''[[multigravida]]'' or ''multiparous.''<ref name = 'MFD' /><ref>{{cite web|title=Definition of nulligravida|url=http://medical.merriam-webster.com/medical/nulligravida|publisher=[[Merriam-Webster, Incorporated]]|accessdate=9 March 2012}}</ref> Hence, during a second pregnancy a woman would be described as ''gravida 2, para 1'' and upon live delivery as ''gravida 2, para 2.'' An in-progress pregnancy, as well as [[abortion]]s, [[miscarriage]]s, or [[stillbirth]]s account for parity values being less than the gravida number. In the case of twins, triplets etc., gravida number and parity value are increased by one only. Women who have never carried a pregnancy achieving more than 20 weeks of gestation age are referred to as ''nulliparous.''<ref>{{cite web |url=http://www.medterms.com/script/main/art.asp?articlekey=15259 |title=Nulliparous definition |date=18 November 2000 |publisher=MedicineNet, Inc}}</ref> |
|||
==Physiology== |
|||
[[File:Pregnancy timeline.png|center|thumb|700px|Timeline of pregnancy by [[gestational age]].]] |
|||
===Initiation=== |
|||
{{See also|Human fertilization}} |
|||
[[File:Human Fertilization.png|thumb|Fertilization and implantation in humans.]] |
|||
The most commonly used event to mark the initiation of pregnancy is the first day of the woman's last normal [[menstrual period]], and the resulting fetal age is called the [[gestational age]]. This choice is a result of a lack of a convenient way to discern the point in time when the actual creation of the baby naturally happens. In case of [[in vitro fertilisation]], gestational age is calculated by days from [[oocyte retrieval]] + 14 days.<ref>{{cite pmid|10776011}}</ref> |
|||
Still, already at the initiation of the preceding menstrual period the female body goes through changes to prepare for an upcoming conception, including a rise in [[follicle stimulating hormone]] that stimulates [[folliculogenesis]] and subsequently [[oogenesis]] in order to give rise to a mature [[egg cell]], which is the female [[gamete]]. [[Human fertilization|Fertilization]] is the event where the egg cell fuses with the male gamete, [[spermatozoon]]. In lay terms, it is more commonly known as "conception." After the point of [[fertilization]], the fused product of the female and male gamete is referred to as a [[zygote]] or fertilized egg. The fusion of male and female gametes usually occurs following the act of [[sexual intercourse]], resulting in ''spontaneous pregnancy''. It can also occur by [[assisted reproductive technology]] such as [[artificial insemination]] and [[in vitro fertilisation]], and may be undertaken as a voluntary choice or due to [[infertility]]. |
|||
The event of fertilization is sometimes used as a mark of the initiation of pregnancy, with the derived age being termed [[fertilization age]], and is an alternative to [[gestational age]]. Fertilization usually occurs about two weeks before her ''next'' expected menstrual period, and if either date is unknown in an individual case it is a frequent practice to add 14 days to the fertilization age to get the gestational age and [[vice versa]]. |
|||
===Development of embryo and fetus=== |
|||
{{Main|Prenatal development|Human embryogenesis|Fetus}} |
|||
[[File:HumanEmbryogenesis.svg|thumb|The initial stages of [[human embryogenesis]].]] |
|||
The sperm and the egg cell, which has been released from one of the female's two [[ovaries]], unite in one of the two [[fallopian tubes]]. The fertilized egg, known as a [[zygote]], then moves toward the uterus, a journey that can take up to a week to complete. Cell division begins approximately 24 to 36 hours after the male and female cells unite. Cell division continues at a rapid rate and the cells then develop into what is known as a [[blastocyst]]. The blastocyst arrives at the uterus and attaches to the uterine wall, a process known as [[implantation (human embryo)|implantation]]. |
|||
The development of the mass of cells that will become the baby is called [[Human embryogenesis|embryogenesis]] during the first approximately 10 weeks of gestation. During this time, cells begin to differentiate into the various body systems. The basic outlines of the organ, body, and nervous systems are established. By the end of the embryonic stage, the beginnings of features such as fingers, eyes, mouth, and ears become visible. Also during this time, there is development of structures important to the support of the embryo, including the [[placenta]] and [[umbilical cord]]. The [[placenta]] connects the developing embryo to the uterine wall to allow nutrient uptake, waste elimination, and gas exchange via the mother's blood supply. The [[umbilical cord]] is the connecting cord from the embryo or fetus to the placenta. |
|||
After about 10 weeks of gestational age, the embryo becomes known as a [[fetus]] instead. At the beginning of the fetal stage, the risk of miscarriage decreases sharply,<ref name=sharply> |
|||
*[[Lennart Nilsson]], [[A Child Is Born (book)|A Child is Born]] 91 (1990): at eight weeks, "the danger of a miscarriage … diminishes sharply." |
|||
*"[http://www.womens-health.co.uk/miscarr.asp Women's Health Information]", Hearthstone Communications Limited: "The risk of miscarriage decreases dramatically after the 8th week as the weeks go by." Retrieved 2007-04-22.</ref> When the fetal stage commences, a fetus is typically about 30 mm (1.2 inches) in length, and the heart can be seen beating via ultrasound; the fetus can be seen making various involuntary motions at this stage.<ref name="Prechtl">{{cite book|last1=Kalverboer|first1=Alex Fedde|last2=Gramsbergen|first2=Albertus Arend|title=Handbook of Brain and Behaviour in Human Development|url=http://books.google.com/books?id=FzyPozUyKPkC&pg=RA1-PA416|date=1 January 2001|publisher=Springer|isbn=978-0-7923-6943-1|pages=1–}}</ref> During continued fetal development, the early body systems and structures that were established in the embryonic stage continue to develop. Sex organs begin to appear during the third month of gestation. The fetus continues to grow in both weight and length, although the majority of the physical growth occurs in the last weeks of pregnancy. |
|||
Electrical [[brain activity]] is first detected between the 5th and 6th week of gestation, though this is still considered primitive neural activity rather than the beginning of conscious thought, something that develops much later in fetation. Synapses begin forming at 17 weeks, and at about week 28 begin to multiply at a rapid pace which continues until 3 to 4 months after birth.<ref>{{cite book|last=Illes|first=ed. by Judy|title=Neuroethics : defining the issues in theory, practice, and policy|year=2008|publisher=Oxford University Press|location=Oxford|isbn=9780198567219|pages=142|url=http://books.google.ca/books?id=m7USFu5Z0lQC&pg=PA142|edition=Repr.}}</ref> |
|||
<center><gallery> |
|||
Image:6 weeks pregnant.png|Embryo at 4 weeks after fertilization<ref><!--"6 weeks pregnant" is synonymous with "4 weeks after fertilization." See [[gestational age]]-->[http://www.3dpregnancy.com/static/pregnancy-week-6.html 3D Pregnancy] (Image from gestational age of 6 weeks). Retrieved 2007-08-28. A rotatable 3D version of this photo is available [http://www.3dpregnancy.com/rotatable/6-weeks-pregnant.html here], and a sketch is available [http://www.3dpregnancy.com/pictures/pregnancy-week-6.html here].</ref> |
|||
Image:10 weeks pregnant.png|Fetus at 8 weeks after fertilization<ref>[http://www.3dpregnancy.com/static/pregnancy-week-10.html 3D Pregnancy] (Image from gestational age of 10 weeks). Retrieved 2007-08-28. A rotatable 3D version of this photo is available [http://www.3dpregnancy.com/rotatable/10-weeks-pregnant.html here], and a sketch is available [http://www.3dpregnancy.com/pictures/pregnancy-week-10.html here].</ref> |
|||
Image:20 weeks pregnant.png|Fetus at 18 weeks after fertilization<ref>[http://www.3dpregnancy.com/static/pregnancy-week-20.html 3D Pregnancy] (Image from gestational age of 20 weeks). Retrieved 2007-08-28. A rotatable 3D version of this photo is available [http://www.3dpregnancy.com/rotatable/20-weeks-pregnant.html here], and a sketch is available [http://www.3dpregnancy.com/pictures/pregnancy-week-20.html here].</ref> |
|||
Image:40 weeks pregnant.png|Fetus at 38 weeks after fertilization<ref>[http://www.3dpregnancy.com/static/pregnancy-week-40.html 3D Pregnancy] (Image from gestational age of 40 weeks). Retrieved 2007-08-28. A rotatable 3D version of this photo is available [http://www.3dpregnancy.com/rotatable/40-weeks-pregnant.html here], and a sketch is available [http://www.3dpregnancy.com/pictures/pregnancy-week-40.html here].</ref> |
|||
</gallery></center> |
|||
<center><gallery> |
|||
Image:Month 1.svg|Relative size in 1st month (simplified illustration) |
|||
Image:Month 3.svg|Relative size in 3rd month (simplified illustration) |
|||
Image:Month 5.svg|Relative size in 5th month (simplified illustration) |
|||
Image:Month 9.svg|Relative size in 9th month (simplified illustration) |
|||
</gallery></center> |
|||
===Maternal changes=== |
|||
{{Main|Maternal physiological changes in pregnancy}} |
|||
[[File:Breast changes during pregnancy 1.png|thumb|400px|Breast changes as seen during pregnancy. Note the increase in size and darkening of the areola.]] |
|||
During pregnancy, the woman undergoes many [[physiology|physiological]] changes, which are entirely normal, including [[cardiovascular]], [[hematology|hematologic]], [[metabolism|metabolic]], [[renal]] and [[respiration (physiology)|respiratory]] changes that become very important in the event of complications. The body must change its physiological and homeostatic mechanisms in pregnancy to ensure the fetus is provided for. Increases in blood sugar, breathing and cardiac output are all required. Levels of progesterone and oestrogens rise continually throughout pregnancy, suppressing the hypothalamic axis and subsequently the menstrual cycle. |
|||
The [[fetus]] inside a pregnant woman may be viewed as an unusually successful [[allograft]], since it genetically differs from the woman.<ref name=clark>{{cite journal |author=Clark DA, Chaput A, Tutton D |title=Active suppression of host-vs-graft reaction in pregnant mice. VII. Spontaneous abortion of allogeneic CBA/J x DBA/2 fetuses in the uterus of CBA/J mice correlates with deficient non-T suppressor cell activity |journal=J. Immunol. |volume=136 |issue=5|pages=1668–75 |year=1986 |month=March |pmid=2936806 |url=http://www.jimmunol.org/cgi/pmidlookup?view=long&pmid=2936806}}</ref> The main reason for this success is an increased [[Immune tolerance in pregnancy|maternal immune tolerance]] during pregnancy. However, this increased immune tolerance in pregnancy can also cause an increased susceptibility to and severity of some [[infectious diseases]]. |
|||
Pregnancy is typically broken into three periods, or trimesters, each of about three months.<ref>[http://www.collinsdictionary.com/dictionary/english/trimester trimester]. CollinsDictionary.com. Collins English Dictionary – Complete & Unabridged 11th Edition. Retrieved 26 November 2012. |
|||
</ref><ref>[http://www.thefreedictionary.com/trimester thefreedictionary.com > trimester] Citing: |
|||
*The American Heritage® Dictionary of the English Language, Fourth Edition, copyright 2000 |
|||
</ref> Obstetricians define each trimester as lasting for 14 weeks, resulting in a total duration of 42 weeks, although the average duration of pregnancy is actually about 40 weeks.<ref>Cunningham, et al., (2010). Williams Textbook of Obstetrics, chapter 8.</ref> While there are no hard and fast rules, these distinctions are useful in describing the changes that take place over time. |
|||
====First trimester==== |
|||
[[Image:2917 Size of Uterus Throughout Pregnancy-02.jpg|200px|thumb|right|The uterus as it changes in size over the duration of the trimesters.]] |
|||
[[Minute ventilation]] is increased by 40% in the first trimester.<ref name="pmid11316633">{{cite journal|last=Campbell|first=LA|coauthors=Klocke, RA|title=Implications for the pregnant patient|journal=American Journal of Respiratory and Critical Care Medicine|date=April 2001|volume=163|issue=5|pages=1051–54|pmid=11316633|doi=10.1164/ajrccm.163.5.16353}}</ref> The womb will grown to the size of a lemon by eight weeks. Many [[symptoms and discomforts of pregnancy]] (further described in later sections) appear in the first trimester.<ref>http://www.nhs.uk/conditions/pregnancy-and-baby/pages/pregnancy-weeks-4-5-6-7-8.aspx#close</ref> |
|||
====Second trimester==== |
|||
[[File:Pregnancy 26 weeks 1.jpg|upright|thumb|By the end of the second trimester, the expanding uterus has created a visible "baby bump". Although the breasts have been developing internally since the beginning of the pregnancy, most of the visible changes appear after this point.]] |
|||
Weeks 13 to 28 of the pregnancy are called the second trimester. Most women feel more energized in this period, and begin to put on weight as the symptoms of morning sickness subside and eventually fade away. The uterus, the muscular organ that holds the developing fetus, can expand up to 20 times its normal size during pregnancy. |
|||
Although the [[fetus]] begins to move and takes a recognizable human shape during the first trimester, it is not until the second trimester that movement of the fetus, often referred to as "[[quickening]]", can be felt. This typically happens in the fourth month, more specifically in the 20th to 21st week, or by the 19th week if the woman has been pregnant before. However, it is not uncommon for some women not to feel the fetus move until much later. During the second trimester, most women begin to wear [[maternity clothes]]. |
|||
====Third trimester==== |
|||
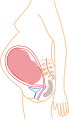
[[Image:Bumm 123 lg.jpg|thumb|400|right|The uterus expands making up a larger and larger portion of the woman's stomach. At left anterior view with months labeled, at right lateral view labeling the last 4 weeks. During the final stages of gestation before childbirth the fetus and uterus will drop to a lower position on the stomach.]] |
|||
Final weight gain takes place, which is the most weight gain throughout the pregnancy. The woman's belly will transform in shape as the belly drops due to the fetus turning in a downward position ready for birth. During the second trimester, the woman's belly would have been very upright, whereas in the third trimester it will drop down quite low, and the woman will be able to lift her belly up and down. The fetus begins to move regularly, and is felt by the woman. Fetal movement can become quite strong and be disruptive to the woman. The woman's [[navel]] will sometimes become convex, "popping" out, due to her expanding [[abdomen]]. |
|||
[[Head engagement]], where the fetal head descends into [[cephalic presentation]], relieves pressure on the upper abdomen with renewed ease in breathing. However, it severely reduces bladder capacity, increases pressure on the pelvic floor and the rectum. |
|||
It is also during the third trimester that maternal activity and sleep positions may affect fetal development due to restricted blood flow. For instance, the enlarged uterus may impede blood flow by compressing the lower pressured [[vena cava]], with the left lateral laying positions appearing to providing better oxygenation to the infant.<ref name="pmid21673002">{{cite journal|last=Stacey|first=T|coauthors=Thompson, JM; Mitchell, EA; Ekeroma, AJ; Zuccollo, JM; McCowan, LM|title=Association between maternal sleep practices and risk of late stillbirth: a case-control study|journal=BMJ (Clinical research ed.)|date=2011 Jun 14|volume=342|pages=d3403|pmid=21673002|doi=10.1136/bmj.d3403|pmc=3114953}}</ref> |
|||
===Duration=== |
|||
Since these are spread over a significant period of time, the duration of pregnancy necessarily depends on the date selected as the starting point chosen. |
|||
As measured on a [[reference group]] of women with a [[menstrual cycle]] of exactly 28-days prior to pregnancy, and who had spontaneous onset of labor, the mean pregnancy length has been estimated to be 283.4 days of [[gestational age]] as timed from the first day of the [[last menstrual period]] as recalled by the mother, and 280.6 days when the gestational age was retrospectively estimated by [[obstetric ultrasound]] measurement of the [[fetal biparietal diameter]] (BPD) in the second trimester.<ref name=Kieler2003/> Other algorithms take into account a variety of other variables, such as whether this is the first or subsequent child (i.e., pregnant woman is a primipara or a [[multipara]], respectively), the mother's race, parental age, length of menstrual cycle, and menstrual regularity), but these are rarely used by healthcare professionals. In order to have a standard reference point, the normal pregnancy duration is generally assumed to be 280 days (or 40 weeks) of gestational age. |
|||
There is a [[standard deviation]] of 8–9 days surrounding due dates calculated with even the most accurate methods. This means that fewer than 5 percent of births occur on the day of being 40 weeks of gestational age; 50 percent of births are within a week of this duration, and about 80 percent are within 2 weeks.<ref name=Kieler2003>{{cite journal |author=Dr H. Kieler, O. Axelsson, S. Nilsson, U. Waldenströ|title=The length of human pregnancy as calculated by ultrasonographic measurement of the fetal biparietal diameter|journal=Ultrasound in Obstetrics & Gynecology|pages=353–357|volume=6|issue=5 |year=1995|doi=10.1046/j.1469-0705.1995.06050353.x|pmid=8590208}}</ref> For the estimation of due date, [[mobile app]]s essentially always give consistent estimations compared to each other and correct for [[leap year]], while pregnancy wheels made of paper can differ from each other by 7 days and generally do not correct for leap year.<ref>{{cite doi|10.1016/j.ajog.2013.09.013}}</ref> |
|||
The most common system used among healthcare professionals is [[Naegele's rule]], which was developed in the early 19th century. This calculates the expected due date from the first day of the last normal menstrual period (LMP or LNMP) regardless of factors known to make this inaccurate, such as a shorter or longer menstrual cycle length. Pregnancy most commonly lasts for 40 weeks according to this LNMP-based method, assuming that the woman has a predictable menstrual cycle length of close to 28 days and conceives on the 14th day of that cycle. |
|||
As measured from the day of [[ovulation]], the average time to birth has been estimated to be 268 days (38 weeks and two days), with a [[coefficient of variation]] of 3.7%.<ref>{{cite doi|10.1093/humrep/det297}}</ref> |
|||
Accurate dating of pregnancy is important, because it is used in calculating the results of various [[Prenatal diagnosis|prenatal tests]], (for example, in the [[triple test]]). A decision may be made to [[Induction (birth)|induce]] labour if a fetus is perceived to be overdue. Furthermore, if LMP and ultrasound dating predict different respective due dates, with the latter being later, this might signify slowed fetal growth and therefore require closer review. |
|||
The stage of pregnancy defined as the beginning of legal [[fetal viability]] varies around the world. It sometimes incorporates weight as well as gestational age.<ref name=AIHW-2012>{{cite web|last=Li|first=Z|title=Australia's Mothers and Babies 2010|url=http://www.aihw.gov.au/WorkArea/DownloadAsset.aspx?id=60129542372|work=Perinatal statistics series no. 27. Cat. no. PER 57|publisher=Australian Institute of Health and Welfare National Perinatal Statistics Unit, Australian Government|accessdate=4 July 2013|coauthors=Zeki, R; Hilder, L; Sullivan, EA|year=2012}}</ref> It ranges from 16 weeks in Norway, to 20 weeks in the US and Australia, 24 weeks in the UK and 26 weeks in Italy and Spain.<ref name="AIHW-2012"/><ref name=Mohangoo-2013>{{cite journal|last=Mohangoo|first=AD|coauthors=Blondel, B; Gissler, M; Velebil, P; Macfarlane, A; Zeitlin, J; Euro-Peristat Scientific, Committee|editor1-last=Wright|editor1-first=Linda|title=International comparisons of fetal and neonatal mortality rates in high-income countries: should exclusion thresholds be based on birth weight or gestational age?|journal=PLoS ONE|year=2013|volume=8|issue=5|pages=e64869|pmid=23700489|doi=10.1371/journal.pone.0064869|pmc=3658983}}</ref><ref name=RCOG-late-abortion>{{cite web|last=Royal College of Obstetricians and Gynaecologists UK|title=Further Issues Relating to Late Abortion, Fetal Viability and Registration of Births and Deaths|url=http://www.rcog.org.uk/womens-health/clinical-guidance/further-issues-relating-late-abortion-fetal-viability-and-registrati|publisher=Royal College of Obstetricians and Gynaecologists UK|accessdate=4 July 2013|month=April|year=2001}}</ref> |
|||
====Preterm, term and postterm==== |
|||
{{Further|Preterm birth|Postterm pregnancy}} |
|||
{{anchor|Term}} |
|||
Pregnancy is considered "at term" when gestation has lasted 37 complete weeks (occurring at the transition from the 37th to the 38th week of gestation), but is less than 42 weeks of gestational age (occurring at the transition from the 42nd week to the 43rd week of gestation, or between 259 and 294 days since LMP). The [[American College of Obstetricians and Gynecologists]] recommends the following categorization of term pregnancies:<ref name=acog2013>[http://www.acog.org/About_ACOG/News_Room/News_Releases/2013/Ob-Gyns_Redefine_Meaning_of_Term_Pregnancy Ob-Gyns Redefine Meaning of "Term Pregnancy"], from [[American College of Obstetricians and Gynecologists]]. October 22, 2013</ref> |
|||
*Early Term: Between 37 weeks 0 days and 38 weeks 6 days of [[gestational age]] |
|||
*Full Term: Between 39 weeks 0 days and 40 weeks 6 days of gestational age |
|||
*Late Term: Between 41 weeks 0 days and 41 weeks 6 days of gestational age |
|||
Events before completion of 37 weeks (259 days) are considered [[Premature birth|preterm]], and events after 42 weeks (294 days) are considered [[Postmature birth|postterm]].<ref name=acog2013/><ref>{{cite web |url=http://www.preventioninstitute.sk.ca/home/Program_Areas/Maternal__Infant_Health/Definitions/ |title=Definitions |accessdate=16 January 2008 |publisher=Saskatchewan Prevention Institute. }}</ref> When a pregnancy exceeds 42 weeks (294 days), the risk of complications for both the woman and the fetus increases significantly.<ref name="UpToDate">{{cite web |url=http://www.uptodate.com/contents/postterm-pregnancy-beyond-the-basics |title=Postterm Pregnancy (Beyond the Basics) |accessdate=24 August 2012 |last=Norwitz, MD, PhD |first=Errol R. |publisher=UpToDate, Inc.}}</ref><ref>{{cite web |url=http://www.medem.com/MedLB/article_detaillb.cfm?article_ID=ZZZRDLPH97C&sub_cat=2005 |title=What To Expect After Your Due Date |accessdate=16 January 2008 |author=The American College of Obstetricians and Gynecologists |month=April | year=2006 |work=Medem |publisher=Medem, Inc.}}</ref> Therefore, in an otherwise uncomplicated pregnancy, obstetricians usually prefer to [[induce labour]] at some stage between 41 and 42 weeks.<ref>{{cite web |url=http://www.rcog.org.uk/resources/public/pdf/rcog_induction_of_labour.pdf |title=Induction of labour – Evidence-based Clinical Guideline Number 9|accessdate=18 January 2008 |year=2001 |publisher=Royal College of Obstetricians and Gynaecologists|format=PDF |archiveurl = http://web.archive.org/web/20061230063449/http://www.rcog.org.uk/resources/public/pdf/rcog_induction_of_labour.pdf |archivedate = 30 December 2006}}</ref><ref>{{cite web |url=http://www.durhamobgyn.com/viewArticle?ID=336380 |title=Postdate Pregnancy |accessdate=18 January 2008 |last=Stovall, M.D. |first=Thomas G. |date=23 March 2004 |work=Durham Obstetrics and Gynecology |publisher=Durham Obstetrics and Gynecology}} {{Dead link|date=September 2010|bot=H3llBot}}</ref> |
|||
Birth before 39 weeks by [[Caesarean section]] section, even if considered "at term", results in an increased risk of complications and premature death, when not medically needed.<ref>{{cite web|title=Nonmedically Indicated Early-Term Deliveries|url=http://www.acog.org/Resources_And_Publications/Committee_Opinions/Committee_on_Obstetric_Practice/Nonmedically_Indicated_Early-Term_Deliveries|work=American College of Obstetricians and Gynecologists|accessdate=24 March 2013|year=2013}}</ref> This is from factors including underdeveloped lungs, infection due to underdeveloped immune system, feeding problems due to underdeveloped brain, and [[jaundice]] from underdeveloped liver. Some hospitals in the United States have noted a significant increase in [[neonatal intensive care unit]] patients when women schedule deliveries for convenience and are taking steps to reduce induction for non-medical reasons.<ref>{{cite web|url=http://www.npr.org/templates/transcript/transcript.php?storyId=138473097|title=Doctors To Pregnant Women: Wait At Least 39 Weeks|accessdate=20 August 2011|date=18 July 2011}}</ref> Complications from Caesarean section are more common than for live births. |
|||
Recent medical literature prefers the terminology ''preterm'' and ''postterm'' to ''premature'' and ''postmature.'' ''Preterm'' and ''postterm'' are unambiguously defined as above, whereas ''premature'' and ''postmature'' have historical meaning and relate more to the infant's size and state of development rather than to the stage of pregnancy.<ref>{{cite web |url=http://www.medterms.com/script/main/art.asp?articlekey=11895 |title=Definition of Premature birth |accessdate=16 January 2008 |publisher=Medicine.net}}</ref><ref>{{cite web |url=http://health.discovery.com/encyclopedias/illnesses.html?article=2728 |title=Premature Infant |accessdate=16 January 2008 |author=Lama Rimawi, MD |date=22 September 2006 |work=Disease & Conditions Encyclopedia |publisher=Discovery Communications, LLC.}}</ref> |
|||
===Childbirth=== |
|||
{{Main|Childbirth}} |
|||
Childbirth is the process whereby an infant is born. |
|||
A woman is considered to be in labour when she begins experiencing regular uterine contractions, accompanied by changes of her cervix – primarily effacement and dilation. While childbirth is widely experienced as painful, some women do report painless labours, while others find that concentrating on the birth helps to quicken labour and lessen the sensations. Most births are successful vaginal births, but sometimes complications arise and a woman may undergo a [[cesarean section]]. |
|||
During the time immediately after birth, both the mother and the baby are hormonally cued to bond, the mother through the release of [[oxytocin]], a hormone also released during [[breastfeeding]]. Studies show that skin-to-skin contact between a mother and her newborn immediately after birth is beneficial for both the mother and baby. A review done by the [[World Health Organization]] found that skin-to-skin contact between mothers and babies after birth reduces crying, improves mother-infant interaction, and helps mothers to breastfeed successfully. They recommend that [[neonates]] be allowed to bond with the mother during their first two hours after birth, the period that they tend to be more alert than in the following hours of early life.<ref>[http://apps.who.int/rhl/newborn/gpcom/en/index.html WHO | Early skin-to-skin contact for mothers and their healthy newborn infants<!-- Bot generated title -->]</ref> |
|||
===Postnatal period=== |
|||
{{Main|Postnatal}} |
|||
The postnatal period begins immediately after the birth of a child and then extends for about six weeks. During this period, the mother's body begins the return to prepregnancy conditions that includes changes in hormone levels and uterus size. |
|||
==Diagnosis== |
|||
The beginning of pregnancy may be detected either based on symptoms by the pregnant woman herself, or by using medical tests with or without the assistance of a medical professional. Approximately 1 in 475 women at 20 weeks, and 1 in 2500 women at delivery, refuse to acknowledge that they are pregnant, which is called ''[[denial of pregnancy]]''.<ref name="pmid21725094">{{cite journal|last=Jenkins|first=A|coauthors=Millar, S; Robins, J|title=Denial of pregnancy: a literature review and discussion of ethical and legal issues|journal=Journal of the Royal Society of Medicine|date=July 2011|volume=104|issue=7|pages=286–91|pmid=21725094|doi=10.1258/jrsm.2011.100376}}</ref> Some non-pregnant women have a very strong belief that they are pregnant along with some of the physical changes.<!-- <ref name=Gabbe2012> --> This condition is known as [[pseudocyesis]] or false pregnancy.<ref name=Gabbe2012>{{cite book|last=Gabbe|first=Steven|title=Obstetrics : normal and problem pregnancies|publisher=Elsevier/Saunders|location=Philadelphia|isbn=9781437719352|page=[http://books.google.ca/books?id=-3ufSTqeb6cC&pg=PA1184 1184]|edition=6th}}</ref> |
|||
===Physical signs=== |
|||
{{Further|Symptoms and discomforts of pregnancy}} |
|||
[[File:Linea nigra.jpg|thumb|[[Linea nigra]] in a woman at 22 weeks pregnant.]] |
|||
Most pregnant women experience a number of symptoms,<ref name="pregnancy symptoms">{{cite web | title = Pregnancy Symptoms | url = http://www.nhs.uk/livewell/sexandyoungpeople/pages/amipregnant.aspx | publisher = [[National Health Service (NHS)]] | date = 11 March 2010 | accessdate =11 March 2010 }}</ref> which can signify pregnancy. The symptoms can include nausea and vomiting, excessive tiredness and fatigue, [[Food craving|cravings]] for certain foods that are not normally sought out, and frequent urination particularly during the night. |
|||
A number of early [[medical sign]]s are associated with pregnancy.<ref name="mayo symptoms">{{cite web | title = Early symptoms of pregnancy: What happens right away | url = http://www.mayoclinic.com/health/symptoms-of-pregnancy/PR00102 | publisher = [[Mayo Clinic]] | date = 22 February 2007 | accessdate =22 August 2007 }}</ref><ref name="American Pregnancy Association">{{cite web |url=http://www.americanpregnancy.org/gettingpregnant/earlypregnancysymptoms.html |title=Pregnancy Symptoms – Early Signs of Pregnancy : American Pregnancy Association |accessdate=16 January 2008 }}</ref> These signs typically appear, if at all, within the first few weeks after conception. Although not all of these signs are universally present, nor are all of them diagnostic by themselves, taken together they make a presumptive diagnosis of pregnancy. These signs include the presence of [[human chorionic gonadotropin]] (hCG) in the blood and urine, missed [[menstrual cycle|menstrual period]], implantation bleeding that occurs at [[Implantation (human embryo)|implantation]] of the embryo in the uterus during the third or fourth week after last menstrual period, increased [[basal body temperature]] sustained for over 2 weeks after [[ovulation]], [[Chadwick's sign]] (darkening of the [[cervix]], [[vagina]], and [[vulva]]), [[Goodell's sign]] (softening of the vaginal portion of the cervix), [[Hegar's sign]] (softening of the [[uterus]] [[isthmus]]), and pigmentation of linea alba – [[Linea nigra]], (darkening of the skin in a midline of the [[abdomen]], caused by [[hyperpigmentation]] resulting from hormonal changes, usually appearing around the middle of pregnancy).<ref name="mayo symptoms"/><ref name="American Pregnancy Association"/> [[Breast tenderness]] is common during the first trimester, and is more common in women who are pregnant at a young age.<ref>[http://www.nlm.nih.gov/medlineplus/ency/article/003152.htm MedlinePlus > Breast pain] Update Date: 31 December 2008. Updated by: David C. Dugdale, Susan Storck. Also reviewed by David Zieve.</ref> Shortly after conception, the nipples and areolas begin to darken due to a temporary increase in hormones.<ref name="pregnancy video">{{cite web|url=http://sexperienceuk.channel4.com/education/about/pregnancy|title=Pregnancy video|accessdate=22 January 2009|publisher=Channel 4|year=2008}}</ref> This process continues throughout the pregnancy. |
|||
Despite all the signs, some women may not realize they are pregnant until they are far along in pregnancy. In some cases, a few have not been aware of their pregnancy until they begin [[Childbirth|labour]]. This can be caused by many factors, including irregular periods (quite common in teenagers), certain medications (not related to conceiving children), and [[obese]] women who disregard their weight gain. Others may be in [[Pregnancy denial|denial]] of their situation. |
|||
===Biomarkers=== |
|||
{{Further|Pregnancy test}} |
|||
Pregnancy detection can be accomplished using one or more various [[pregnancy test]]s,<ref name="pregnancy">{{cite web | title = NHS Pregnancy Planner | url = http://www.nhs.uk/Planners/Pregnancycareplanner | publisher = [[National Health Service (NHS)]] | date = 19 March 2010 | accessdate =19 March 2010 }}</ref> which detect hormones generated by the newly formed [[placenta]], serving as [[Biomarker (medicine)|biomarkers]] of pregnancy. Blood and urine tests can detect pregnancy 12 days after implantation.<ref>{{cite journal |doi=10.1007/BF02066422 |author=Qasim SM, Callan C, Choe JK |title=The predictive value of an initial serum beta human chorionic gonadotropin level for pregnancy outcome following in vitro fertilization |journal=Journal of Assisted Reproduction and Genetics |volume=13 |issue=9 |pages=705–8 |year=1996 |pmid=8947817 }}</ref> Blood pregnancy tests are more sensitive than urine tests (giving fewer false negatives).<ref>{{cite web |url=http://www.bestbets.org/bets/bet.php?id=936 |title=BestBets: Serum or Urine beta-hCG? }}</ref> Home [[pregnancy test]]s are [[urine]] tests, and normally detect a pregnancy 12 to 15 days after fertilization. A quantitative blood test can determine approximately the date the embryo was conceived. Testing 48 hours apart can provide useful information regarding how the pregnancy is doing. A single test of [[progesterone]] levels can also help determine how likely a fetus will survive in those with a [[threatened miscarriage]] (bleeding in early pregnancy).<ref name="pmid23045257">{{cite journal|last=Verhaegen|first=J|coauthors=Gallos, ID; van Mello, NM; Abdel-Aziz, M; Takwoingi, Y; Harb, H; Deeks, JJ; Mol, BW; Coomarasamy, A|title=Accuracy of single progesterone test to predict early pregnancy outcome in women with pain or bleeding: meta-analysis of cohort studies|journal=BMJ (Clinical research ed.)|date=2012 Sep 27|volume=345|pages=e6077|pmid=23045257|pmc=3460254|doi=10.1136/bmj.e6077}}</ref> |
|||
===Ultrasound=== |
|||
{{see also|Obstetric ultrasonography}} |
|||
[[Obstetric ultrasonography]] can detect some [[congenital disease]]s at an early stage, estimate the due date as well as detecting [[multiple pregnancy]].<ref name="pmid20393955">{{cite journal|last=Whitworth|first=M|coauthors=Bricker, L; Neilson, JP; Dowswell, T|editor1-last=Whitworth|editor1-first=Melissa|title=Ultrasound for fetal assessment in early pregnancy|journal=Cochrane database of systematic reviews (Online)|date=2010 Apr 14|issue=4|pages=CD007058|pmid=20393955|doi=10.1002/14651858.CD007058.pub2}}</ref> The resultant estimated due date of the fetus is slightly more accurate than methods based on last menstrual period.<ref>{{cite journal | title = Evaluation of ultrasound-estimated date of delivery in 17 450 spontaneous singleton births: do we need to modify Naegele's rule? | url = http://www.blackwell-synergy.com/doi/abs/10.1046/j.1469-0705.1999.14010023.x | journal = Ultrasound in Obstetrics and Gynecology | volume = 14 | issue = 1 | pages = 23–28 | last = Nguyen | first = T.H. | coauthors = ''et al.'' | year = 1999 | accessdate =18 August 2007 | doi = 10.1046/j.1469-0705.1999.14010023.x | format = abstract | pmid = 10461334 }}</ref> In those who are at low risk it is unclear if obstetric ultrasound before 24 weeks makes a significant difference in outcomes.<ref name=US1996/> Routine ultrasound imaging after 24 weeks gestation does not improve outcomes in either the mother or the baby and might increase the risk of a cesarean section.<ref name="pmid18843617">{{cite journal|last=Bricker|first=L|coauthors=Neilson, JP; Dowswell, T|editor1-last=Bricker|editor1-first=Leanne|title=Routine ultrasound in late pregnancy (after 24 weeks' gestation)|journal=Cochrane database of systematic reviews (Online)|date=2008 Oct 8|issue=4|pages=CD001451|pmid=18843617|doi=10.1002/14651858.CD001451.pub3}}</ref> It is thus is not recommended.<ref name=US1996>{{cite web|title=Screening for Ultrasonography in Pregnancy|url=http://www.uspreventiveservicestaskforce.org/uspstf/uspsuspg.htm|work=U.S. Preventive Services Task Force|accessdate=6 March 2013}}</ref> Modern [[3D ultrasound]] images provide greater detail for prenatal diagnosis than the older 2D ultrasound technology.<ref name="pmid17469450">{{cite journal|author=Dimitrova V, Markov D, Dimitrov R |title=[3D and 4D ultrasonography in obstetrics] |language=Bulgarian|journal=Akush Ginekol (Sofiia) |volume=46 |issue=2 |pages=31–40 |year=2007 |pmid=17469450 }}</ref> While 3D is popular with parents desiring a prenatal photograph as a keepsake,<ref name="pmid17265534">{{cite journal |author=Sheiner E, Hackmon R, Shoham-Vardi I, ''et al.'' |title=A comparison between acoustic output indices in 2D and 3D/4D ultrasound in obstetrics |journal=Ultrasound Obstet Gynecol |volume=29 |issue=3 |pages=326–8 |year=2007 |pmid=17265534|doi=10.1002/uog.3933}}</ref> both 2D and 3D are discouraged by the [[Food and Drug Administration|FDA]] for non-medical use,<ref>{{cite web |author=Rados C |title=FDA Cautions Against Ultrasound 'Keepsake' Images|url=http://www.fda.gov/FDAC/features/2004/104_images.html|archiveurl=http://web.archive.org/web/20090513041746/http://www.fda.gov/fdac/features/2004/104_images.html|archivedate=13 May 2009 |accessdate=28 February 2012 |publisher=FDA Consumer Magazine |date=January–February 2004}}</ref> but there are no definitive studies linking ultrasound to any adverse medical effects.<ref>{{cite news|author=Kempley R |title=The Grin Before They Bear It; Peek-a-Boo: Prenatal Portraits for the Ultrasound Set|url=http://www.highbeam.com/doc/1P2-279063.html |work=Washington Post |date=9 August 2003}}</ref> The following 3D ultrasound images were taken at different stages of pregnancy: |
|||
<center><gallery> |
|||
Image:Fetal movements 3D Ultrasound Dr. Wolfgang Moroder.theora.ogv| 3D Ultrasound of fetal movements at 12 weeks |
|||
Image:Ultrasound_image_of_a_fetus.jpg|75-mm fetus (about 14 weeks [[gestational age]]) |
|||
Image:Sucking his thumb and waving.jpg|Fetus at 17 weeks |
|||
Image:3dultrasound 20 weeks.jpg|Fetus at 20 weeks |
|||
</gallery></center> |
|||
== Management == |
|||
===Attending prenatal care=== |
|||
{{Main|Prenatal care|pre-conception counseling}} |
|||
Prenatal medical care is the medical and nursing care recommended for women [[Pre-conception counseling|before]] and [[prenatal care|during]] pregnancy. The aim of good prenatal care is to identify any potential problems early, to prevent them if possible (through recommendations on adequate nutrition, exercise, vitamin intake etc.), and to manage problems, possibly by directing the woman to appropriate specialists, hospitals, etc. if necessary. |
|||
===Nutrition=== |
|||
{{Main|Nutrition and pregnancy}} |
|||
A balanced, nutritious diet is an important aspect of a healthy pregnancy. Eating a healthy diet, balancing [[carbohydrates]], fat, and [[proteins]], and eating a variety of fruits and vegetables, usually ensures good nutrition. Those whose diets are affected by health issues, religious requirements, or ethical beliefs may choose to consult a health professional for specific advice. |
|||
Adequate periconceptional [[folic acid]] (also called folate or Vitamin B<sub>9</sub>) intake has been shown to decrease the risk of fetal neural tube defects such as [[spina bifida]], a serious [[birth defect]]. The neural tube develops during the first 28 days of pregnancy, explaining the necessity to guarantee adequate periconceptional folate intake.<ref name="pmid16303691">{{cite journal |author=Klusmann A, Heinrich B, Stöpler H, Gärtner J, Mayatepek E, Von Kries R |title=A decreasing rate of neural tube defects following the recommendations for periconceptional folic acid supplementation |journal=Acta Paediatr. |volume=94 |issue=11 |pages=1538–42 |year=2005 |pmid=16303691 |doi=10.1080/08035250500340396 |url=http://www.blackwell-synergy.com/openurl?genre=article&sid=nlm:pubmed&issn=0803-5253&date=2005&volume=94&issue=11&spage=1538 |accessdate=20 January 2008}}</ref><ref name="pmid11015508">{{cite journal |author=Stevenson RE, Allen WP, Pai GS, Best R, Seaver LH, Dean J, Thompson S |title=Decline in prevalence of neural tube defects in a high-risk region of the United States |journal=Pediatrics |volume=106 |issue=4 |pages=677–83 |year=2000 |pmid=11015508 |doi=10.1542/peds.106.4.677}}</ref> Folate (from ''folia'', leaf) is abundant in [[spinach]] (fresh, frozen, or canned), and is found in [[green vegetables|green leafy vegetables]] e.g. salads, beets, broccoli, asparagus, citrus fruits and melons, chickpeas (i.e. in the form of [[hummus]] or [[falafel]]), and [[Egg (food)|eggs]]. In the United States and Canada, most wheat products (flour, noodles) are fortified with folic acid.<ref name="pmid18185493">{{cite journal |title=Use of supplements containing folic acid among women of childbearing age—United States, 2007 |journal=MMWR Morb. Mortal. Wkly. Rep. |volume=57 |issue=1 |pages=5–8 |year=2008 |pmid=18185493 |author1= Centers for Disease Control and Prevention (CDC)}}</ref> |
|||
[[Docosahexaenoic acid|DHA omega-3]] is a major structural fatty acid in the brain and retina, and is naturally found in breast milk. It is important for the woman to consume adequate amounts of DHA during pregnancy and while nursing to support her well-being and the health of her infant. Developing infants cannot produce DHA efficiently, and must receive this vital nutrient from the woman through the placenta during pregnancy and in breast milk after birth.<ref name="pmid11724467">{{cite journal|last=Salem N|first=Jr|coauthors=Litman, B; Kim, HY; Gawrisch, K|title=Mechanisms of action of docosahexaenoic acid in the nervous system|journal=Lipids|date=September 2001|volume=36|issue=9|pages=945–59|pmid=11724467|doi=10.1007/s11745-001-0805-6}}</ref> |
|||
Several [[micronutrients]] are important for the health of the developing fetus, especially in areas of the world where insufficient nutrition is prevalent.<ref name="pmid17054223">{{cite journal |author=Haider BA, Bhutta ZA |title=Multiple-micronutrient supplementation for women during pregnancy |journal=Cochrane Database Syst Rev |issue=4 |pages=CD004905 |year=2006 |pmid=17054223 |doi=10.1002/14651858.CD004905.pub2 |editor1-last=Bhutta |editor1-first=Zulfiqar A}}</ref> In developed areas, such as Western Europe and the United States, certain nutrients such as [[Vitamin D]] and [[calcium]], required for bone development, may require supplementation.<ref name="pmid17476978">{{cite journal |author=Theobald HE |title=Eating for pregnancy and breast-feeding |journal=J Fam Health Care |volume=17 |issue=2 |pages=45–9 |year=2007 |pmid=17476978 }}</ref><ref name="pmid17625571">{{cite journal |author=Basile LA, Taylor SN, Wagner CL, Quinones L, Hollis BW |title=Neonatal vitamin D status at birth at latitude 32 degrees 72': evidence of deficiency |journal=J Perinatol |volume=27 |issue=9 |pages=568–71 |year=2007 |pmid=17625571 |doi=10.1038/sj.jp.7211796}}</ref><ref name="pmid3488981">{{cite journal |author=Kuoppala T, Tuimala R, Parviainen M, Koskinen T, Ala-Houhala M |title=Serum levels of vitamin D metabolites, calcium, phosphorus, magnesium and alkaline phosphatase in Finnish women throughout pregnancy and in cord serum at delivery |journal=Hum Nutr Clin Nutr |volume=40 |issue=4 |pages=287–93 |year=1986 |pmid=3488981 }}</ref> |
|||
Dangerous bacteria or parasites may contaminate foods, including ''[[Listeria]]'' and ''[[Toxoplasma gondii]]''. Careful washing of fruits and raw vegetables may remove these pathogens, as may thoroughly cooking leftovers, meat, or processed meat. Soft cheeses may contain ''Listeria''; if milk is raw, the risk may increase. Cat feces pose a particular risk of [[toxoplasmosis]]. Pregnant women are also more prone to ''[[Salmonella]]'' infections from eggs and poultry, which should be thoroughly cooked. Practicing good hygiene in the kitchen can reduce these risks.<ref name="Tarlow">{{cite journal|last=Tarlow|first=MJ|title=Epidemiology of neonatal infections|journal=The Journal of antimicrobial chemotherapy|date=August 1994|volume=34 Suppl A|pages=43–52|pmid=7844073}}</ref> |
|||
===Weight gain=== |
|||
The amount of healthy weight gain during a pregnancy varies.<ref name=AHRQ-weight>{{cite web|title=Outcomes of Maternal Weight Gain|url=http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0007502/|work=Evidence Reports/Technology Assessments, No. 168|publisher=Agency for Healthcare Research and Quality|accessdate=23 June 2013|author=Viswanathan M|coauthors=Siega-Riz, AM; Moos, M-K; et al|month=May|year=2008}}</ref> Weight gain is only partly related to the weight of the baby and growing placenta, and includes extra fluid for circulation, and the weight needed to provide nutrition for the growing fetus.<ref name=IQWiG-Weight>{{cite web|last=Institute for Quality and Efficiency in Health Care|title=Weight gain in pregnancy|url=http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0005004/|work=Fact sheet|publisher=Institute for Quality and Efficiency in Health Care|accessdate=23 June 2013}}</ref> Most needed weight gain occurs later in pregnancy.<ref name=IQWiG-Weight /> |
|||
The [[Institute of Medicine]] recommends an overall pregnancy weight gain for those of normal weight ([[body mass index]] of 18.5–24.9), of 11.3–15.9 kg (25–35 pounds) having a singleton pregnancy.<ref>{{cite web|url=http://iom.edu/Reports/2009/Weight-Gain-During-Pregnancy-Reexamining-the-Guidelines.aspx |title=Weight Gain During Pregnancy: Reexaminging the Guidelines, Report Brief |accessdate=29 July 2010| work=Institute of Medicine}}</ref> Women who are underweight (BMI of less than 18.5), should gain between 12.7–18 kg (28–40 lbs), while those who are [[overweight]] (BMI of 25–29.9) are advised to gain between 6.8–11.3 kg (15–25 lbs) and those who are [[obese]] (BMI>30) should gain between 5–9 kg (11–20 lbs).<ref name="pmid23262962">{{cite journal|last=American College of Obstetricians and Gynecologists|title=Weight Gain During Pregnancy|journal=Obstet Gynecol|year=2013|month=January|volume=121|issue=1|pages=210–12|pmid=23262962|doi=10.1097/01.AOG.0000425668.87506.4c}}</ref> |
|||
During pregnancy, insufficient or excessive weight gain can compromise the health of the mother and fetus.<ref name=IQWiG-Weight /> The most effective interventions for weight gain in underweight women is not clear.<ref name=IQWiG-Weight /> Being or becoming very overweight in pregnancy increases the risk of complications for mother and fetus, including cesarean section, [[gestational hypertension]], [[pre-eclampsia]], [[macrosomia]] and [[shoulder dystocia]].<ref name=AHRQ-weight /> It can make losing weight after the pregnancy difficult.<ref name=AHRQ-weight /><ref name=NIHR-weight /> |
|||
Around 50% of women of childbearing age in developed countries like the United Kingdom are overweight or obese before pregnancy.<ref name=NIHR-weight>{{cite web|last=Thangaratinam|first=S|title=Interventions to Reduce or Prevent Obesity in Pregnant Women: A Systematic Review|url=http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0050098/|work=Health Technology Assessment, No. 16.31|publisher=NIHR Evaluation, Trials and Studies Coordinating Centre|accessdate=23 June 2013|coauthors=Rogozińska, E; Jolly, K; et al|month=July|year=2012}}</ref> A systematic review found that diet is the most effective way to reduce weight gain and associated risks in pregnancy.<ref name=NIHR-weight /> The review did not find evidence of harm associated with diet control and exercise.<ref name=NIHR-weight /> |
|||
===Medication use=== |
|||
{{Main|Pharmaceutical drugs in pregnancy}} |
|||
Drugs used during pregnancy can have temporary or permanent effects on the fetus. Therefore many physicians would prefer not to prescribe for pregnant women, the major concern being over [[teratogen]]icity of the drugs. |
|||
Drugs have been classified into categories A,B,C,D and X based on the Food and Drug Administration (FDA) rating system to provide therapeutic guidance based on potential benefits and fetal risks. Drugs, including some [[multivitamins]], that have demonstrated no fetal risks after controlled studies in humans are classified as Category A. On the other hand drugs like [[thalidomide]] with proven fetal risks that outweigh all benefits are classified as Category X.<ref name="reena shaji">{{cite web|last=Shaji|first=Reena|title=Drugs in pregnancy and teratogenicity|url=http://www.lifehugger.com/doc/525/drugs-pregnancy-and-teratogenicity|publisher=LifeHugger|date=13 January 2009}}</ref> |
|||
=== Use of recreational drugs=== |
|||
Use of [[recreational drugs]] in pregnancy can cause various [[pregnancy complication]]s. |
|||
*[[Ethanol]] during pregnancy can cause [[fetal alcohol syndrome]] and [[fetal alcohol spectrum disorder]]. A number of studies have shown that light to moderate drinking during pregnancy might not pose a risk to the fetus, although no amount of alcohol during pregnancy can be guaranteed to be absolutely safe.<ref name="pmid20616979">{{cite journal|last=Ornoy|first=A|coauthors=Ergaz, Z|title=Alcohol abuse in pregnant women: effects on the fetus and newborn, mode of action and maternal treatment|journal=International journal of environmental research and public health|date=February 2010|volume=7|issue=2|pages=364–79|pmid=20616979|doi=10.3390/ijerph7020364|pmc=2872283}}</ref> |
|||
*[[Tobacco smoking and pregnancy]], when combined, can cause a wide range of behavioral, neurological, and physical difficulties.<ref name=Hackshaw>{{cite journal|last=Hackshaw|first=A|coauthors=Rodeck, C; Boniface, S|title=Maternal smoking in pregnancy and birth defects: a systematic review based on 173 687 malformed cases and 11.7 million controls|journal=Human reproduction update|date=2011 Sep-Oct|volume=17|issue=5|pages=589–604|pmid=21747128|doi=10.1093/humupd/dmr022|pmc=3156888}}</ref> Smoking during pregnancy causes twice the risk of [[premature rupture of membranes]], [[placental abruption]] and [[placenta previa]].<ref name="CDC preventing">Centers for Disease Control and Prevention. 2007. [http://www.cdc.gov/nccdphp/publications/factsheets/prevention/pdf/smoking.pdf Preventing Smoking and Exposure to Secondhand Smoke Before, During, and After Pregnancy].</ref> Also, it causes 30% higher odds of the baby being born prematurely.<ref name="CDC tobacco use">Centers for Disease Control and Prevention. 2009. Tobacco Use and Pregnancy: Home. |
|||
http://www.cdc.gov/reproductivehealth/tobaccousepregnancy/index.htm</ref> |
|||
*[[Prenatal cocaine exposure]] is associated with, for example, [[preterm birth|premature birth]], [[birth defect]]s and [[attention deficit disorder]]. |
|||
*[[Prenatal methamphetamine exposure]] can cause [[premature birth]] and [[congenital abnormalities]].<ref name=Fact>{{cite web|title=New Mother Fact Sheet: Methamphetamine Use During Pregnancy|url=http://www.ndmch.com|work=North Dakota Department of Health|accessdate=7 October 2011}}</ref> Other investigations have revealed short-term neonatal outcomes to include small deficits in infant neurobehavioral function and growth restriction when compared to control infants.<ref name=Grotta>{{cite journal|last=Grotta|first=Sheri|coauthors=LaGasse, Linda; Arria, Amelia; Derauf, Chris|title=Patterns of Methamphetamine Use During Pregnancy: Results from the IDEAL Study|journal=Matern Child Health J|date=30 June 2009|volume=14|issue=4|pages=519–527|pmid=19565330|pmc=2895902|doi=10.1007/s10995-009-0491-0}}</ref> Also, prenatal methamphetamine use is believed to have long-term effects in terms of brain development, which may last for many years.<ref name=Fact/> |
|||
*[[Cannabis in pregnancy]] is possibly associated with adverse effects on the child later in life. |
|||
=== Exposure to environmental toxins === |
|||
{{Main|Environmental toxins in pregnancy}} |
|||
Intrauterine exposure to [[environmental toxins in pregnancy]] has the potential to cause adverse effects on the [[prenatal development]] of the [[human embryogenesis|embryo]] or [[fetus]], as well as [[pregnancy complications]]. Potential effects of [[toxic]] substances and [[pollution]] include [[congenital abnormalities]]. Also, [[neuroplastic effects of pollution]] can give rise to [[neurodevelopmental disorder]]s for the child later in life. Conditions of particular severity in pregnancy include [[mercury poisoning]] and [[lead poisoning]]. To minimize exposure to environmental toxins, the ''American College of Nurse-Midwives'' recommends for example checking whether lead paint has been used if living in a home built before 1978, washing all [[produce]] thoroughly and buying [[Organic food|organic]] produce, as well as well as avoiding any cleaning supply labeled "toxic" or any product with a warning on the label.<ref>[http://www.midwife.org/ACNM/files/ccLibraryFiles/Filename/000000000688/Environmental%20Hazards%20During%20Pregnancy.pdf Environmental Hazards During Pregnancy] Volume 51, No. 1, January/February 2006.</ref> |
|||
=== Sexual activity === |
|||
{{main|Sexual activity during pregnancy}} |
|||
Most women can continue to engage in sexual activity throughout pregnancy.<ref>[http://www.mayoclinic.com/health/sex-during-pregnancy/HO00140 Sex during pregnancy: What's OK, what's not - MayoClinic.com<!-- Bot generated title -->]</ref> Most research suggests that during pregnancy both sexual desire and frequency of sexual relations decrease.<ref name="Bermudez">{{cite journal |
|||
|title=Influence of the Gestation Period on Sexual Desire |
|||
|journal=Psychology in Spain |
|||
|year=2001 |
|||
|author=M.P. Bermudez |
|||
|coauthors=A.I. Sanchez, G. Buela-Casal |
|||
|volume=5 |
|||
|issue=1 |
|||
|pages=14–16 |
|||
|url=http://www.psychologyinspain.com/content/full/2001/2.htm}}</ref><ref name="Fok">{{cite journal |
|||
|title=Sexual behavior and activity in Chinese pregnant women |
|||
|author=Wing Yee Fok |
|||
|coauthors=Louis Yik-Si Chan, Pong Mo Yuen |
|||
|journal=Acta Obstetricia et Gynecologica Scandinavica |
|||
|volume=84 |
|||
|issue=10 |
|||
|pages=934–938 |
|||
|year=2005 |
|||
|month=October |
|||
|pmid= 16167907 |
|||
|doi=10.1111/j.0001-6349.2005.00743.x}}</ref> In context of this overall decrease in desire, some studies indicate a second-trimester increase, preceding a decrease during the third trimester.<ref name="Reamy">{{cite journal |
|||
|title=Sexuality and pregnancy. A prospective study |
|||
|journal=J Reprod Med. |
|||
|year=1982 |
|||
|month=June |
|||
|volume=27 |
|||
|issue=6 |
|||
|pages=321–7 |
|||
|author=Reamy K |
|||
|coauthors=White SE, Daniell WC, Le Vine ES |
|||
|pmid=7120209}}</ref><ref>{{cite journal |
|||
|author=Malarewicz A, Szymkiewicz J, Rogala J |
|||
|title=[Sexuality of pregnant women] |
|||
|language=Polish |
|||
|journal=Ginekol. Pol. |
|||
|volume=77 |
|||
|issue=9 |
|||
|pages=733–9 |
|||
|year=2006 |
|||
|month=September |
|||
|pmid=17219804 }}</ref> |
|||
Some individuals are sexually attracted to pregnant women ([[pregnancy fetishism]], also known as [[maiesiophilia]]). |
|||
Sex during pregnancy is a low-risk behavior except when the healthcare provider advises that sexual intercourse be avoided for particular medical reasons. Otherwise, for a healthy pregnant woman who is not ill or weak, there is no ''safe'' or ''right'' way to have sex during pregnancy: it is enough to apply the common sense rule that both partners avoid putting pressure on the uterus, or a partner's full weight on a pregnant belly.<ref> |
|||
{{cite web |url=http://sexuality.about.com/od/sexualpositions/a/pregnantsexposi.htm |title=Pregnancy Sex Positions: ideas for comfortable sex positions during pregnancy |author= Cory Silverberg|date=19 September 2011 |publisher=About.com Guide }}</ref> |
|||
===Exercise=== |
|||
Regular aerobic exercise during pregnancy appears to improve (or maintain) physical fitness; however, the quality of the research is poor and the data was insufficient to infer important risks or benefits for the mother or infant.<ref>{{cite journal|last=Kramer|first=MS|coauthors=McDonald, SW|title=Aerobic exercise for women during pregnancy|journal=Cochrane database of systematic reviews (Online)|date=19 July 2006|volume=3|pages=CD000180|pmid=16855953 |doi=10.1002/14651858.CD000180.pub2|editor1-last=Kramer|editor1-first=Michael S|issue=3}}</ref> |
|||
The Clinical Practice Obstetrics Committee of Canada recommends that "All women without contraindications should be encouraged to participate in aerobic and strength-conditioning exercises as part of a healthy lifestyle during their pregnancy". Although an upper level of safe exercise intensity has not been established, women who were regular exercisers before pregnancy and who have uncomplicated, healthy pregnancies should be able to engage in high intensity exercise programs, such as jogging and aerobics for less than 45 minutes, with no adverse effects if they are mindful of the possibility that they may need to increase their energy intake and are careful to not become overheated. In the absence of either medical or obstetric complications, they advise an accumulation of 30 minutes a day of exercise on most if not all days of the week. In general, participation in a wide range of recreational activities appears to be safe, with the avoidance of those with a high risk of falling such as horseback riding or skiing or those that carry a risk of abdominal trauma, such as soccer or hockey.<ref name="pmid12547738">{{cite journal|last=Artal|first=R|coauthors=O'Toole, M|title=Guidelines of the American College of Obstetricians and Gynecologists for exercise during pregnancy and the postpartum period|journal=British journal of sports medicine|date=February 2003|volume=37|issue=1|pages=6–12; discussion 12|pmid=12547738|doi=10.1136/bjsm.37.1.6|pmc=1724598}}</ref> |
|||
The American College of Obstetricians and Gynecologists reports that in the past, the main concerns of exercise in pregnancy were focused on the fetus and any potential maternal benefit was thought to be offset by potential risks to the fetus. However, they write that more recent information suggests that in the uncomplicated pregnancy, fetal injuries are highly unlikely. They do, however, list several circumstances when a woman should contact her health care provider before continuing with an exercise program. Contraindications include: |
|||
Vaginal bleeding, [[dyspnea]] before exertion, dizziness, headache, chest pain, muscle weakness, preterm labor, decreased fetal movement, amniotic fluid leakage, and calf pain or swelling (to rule out [[thrombophlebitis]]).<ref name="pmid12547738" /> |
|||
==Symptoms and discomforts == |
|||
{{Main|Symptoms and discomforts of pregnancy}} |
|||
[[File:Melasmablemish.jpg|thumb|[[Melasma]] pigment changes to the face due to pregnancy]] |
|||
The [[symptoms and discomforts of pregnancy]] are those presentations and conditions that result from pregnancy but do not significantly interfere with [[activities of daily living]] or pose any significant threat to the health of the mother or baby, in contrast to [[pregnancy complication]]s. Still, there is often no clear separation between symptoms versus discomforts versus complications, and in some cases the same basic feature can manifest as either a discomfort or a complication depending on the severity. For example, mild nausea may merely be a discomfort ([[morning sickness]]), but if severe and with vomiting causing [[water-electrolyte imbalance]] it can be classified as a pregnancy complication ([[hyperemesis gravidarum]]). |
|||
Common symptoms and discomforts of pregnancy include: |
|||
*Tiredness. |
|||
*[[Constipation]] |
|||
*[[Pelvic girdle pain]] |
|||
*[[Back pain#Pregnancy|Back pain]] |
|||
*[[Braxton Hicks contractions]]. Occasional, irregular, and often painless contractions that occur several times per day. |
|||
*[[Edema]] (swelling). Common complaint in advancing pregnancy. Caused by compression of the [[inferior vena cava]] (IVC) and pelvic veins by the [[uterus]] leads to increased hydrostatic pressure in lower extremities. |
|||
*[[Increased urinary frequency]]. A common complaint referred by the gravida, caused by increased intravascular volume, elevated GFR ([[glomerular filtration rate]]), and compression of the [[urinary bladder|bladder]] by the expanding uterus. |
|||
*[[Urinary tract infection]]<ref>{{cite web|last=Merck|title=Urinary tract infections during pregnancy|url=http://www.merckmanuals.com/home/womens_health_issues/pregnancy_complicated_by_disease/urinary_tract_infections_during_pregnancy.html|work=Merck Manual Home Health Handbook}}</ref> |
|||
*[[Varicose veins]]. Common complaint caused by relaxation of the venous [[smooth muscle]] and increased intravascular pressure. |
|||
*[[Hemorrhoids|Haemorrhoids]] (piles) are swollen veins at or inside the anal area, resulting from impaired venous return, straining associated with constipation, or increased intra-abdominal pressure in later pregnancy.<ref name=CE-Vazquez>{{cite journal|last=Vazquez|first=JC|title=Constipation, haemorrhoids, and heartburn in pregnancy|journal=Clinical evidence|date=2010 Aug 3|volume=2010|pages=1411|pmid=21418682|pmc=3217736}}</ref> |
|||
*[[Regurgitation (digestion)|Regurgitation]], [[heartburn]], and [[nausea]]. |
|||
*[[Striae gravidarum]], pregnancy-related stretch marks |
|||
==Complications== |
|||
{{Main|Complications of pregnancy}} |
|||
Each year, according to the WHO, ill-health as a result of pregnancy is experienced (sometimes permanently) by more than 20 million women around the world. Furthermore, the "lives of eight million women are threatened, and more than 500,000 women are estimated to have died in 1995 as a result of causes related to pregnancy and childbirth."<ref name="WHO Reproductive Health and Research Publications: Making Pregnancy Safer">{{cite web|url=http://www.searo.who.int/EN/Section13/Section36/Section129/Section396_1450.htm|title=Reproductive Health and Research Publications: Making Pregnancy Safer|year=2009|publisher=World Health Organization Regional Office for South-East Asia|accessdate=7 December 2009}}</ref> |
|||
The following are some examples of pregnancy complications: |
|||
*[[Pregnancy induced hypertension]] |
|||
*[[Anemia]]<ref>{{cite web|last=Merck|title=Pregnancy complicated by disease|url=http://www.merckmanuals.com/home/womens_health_issues/pregnancy_complicated_by_disease/anemia_during_pregnancy.html|work=Merck Manual, Home Health Handbook|publisher=Merck Sharp & Dohme}}</ref> |
|||
*[[Postpartum depression]] |
|||
*[[Postpartum psychosis]] |
|||
*Thromboembolic disorders. The leading cause of death in pregnant women in the US.<ref>{{cite web|last=C. Blackwell|first=Sean|title=Thromboembolic Disorders During Pregnancy|url=http://www.merckmanuals.com/home/womens_health_issues/pregnancy_complicated_by_disease/thromboembolic_disorders_during_pregnancy.html|publisher=Merck Sharp & Dohme Corp|date=December 2008}}</ref> |
|||
*[[PUPPP]] skin disease that develop around the 32nd week. (Pruritic Urticarial Papules and Plaques of Pregnancy), red plaques, papules, itchiness around the belly button that spread all over the body except for the inside of hands and face. |
|||
*[[Ectopic pregnancy]], implantation of the embryo outside the uterus. |
|||
*[[Hyperemesis gravidarum]], excessive nausea that is more severe than [[morning sickness]]. |
|||
==Intercurrent diseases== |
|||
{{Main|Intercurrent disease in pregnancy}} |
|||
In addition to [[complications of pregnancy]] that can arise, a pregnant woman may have [[intercurrent diseases in pregnancy|intercurrent diseases]], that is, other diseases or conditions (not directly caused by the pregnancy) that may become worse or be a potential risk to the pregnancy. |
|||
*[[Diabetes mellitus and pregnancy]] deals with the interactions of [[diabetes mellitus]] (not restricted to [[gestational diabetes]]) and pregnancy. Risks for the child include miscarriage, growth restriction, growth acceleration, fetal obesity (macrosomia), polyhydramnios and birth defects. |
|||
*[[Systemic lupus erythematosus and pregnancy]] confers an increased rate of fetal death ''in utero'' and [[spontaneous abortion]] (miscarriage), as well as of [[neonatal lupus]]. |
|||
*[[Thyroid disease in pregnancy]] can, if uncorrected, cause adverse effects on fetal and maternal well-being. The deleterious effects of thyroid dysfunction can also extend beyond pregnancy and delivery to affect neurointellectual development in the early life of the child. Demand for thyroid hormones is increased during pregnancy which may cause a previously unnoticed thyroid disorder to worsen. |
|||
*[[Hypercoagulability in pregnancy]] is the propensity of pregnant women to develop [[thrombosis]] (blood clots). Pregnancy itself is a factor of [[hypercoagulability]] (pregnancy-induced hypercoagulability), as a physiologically adaptive mechanism to prevent [[postpartum hemorrhage|''post partum'' bleeding]].<ref name=gresele/> However, when combined with an additional underlying hypercoagulable states, the risk of thrombosis or embolism may become substantial.<ref name=gresele>Page 264 in: {{cite book |author=Gresele, Paolo |title=Platelets in hematologic and cardiovascular disorders: a clinical handbook |publisher=Cambridge University Press |location=Cambridge, UK |year=2008 |pages= |isbn=0-521-88115-3 |oclc= |doi= |accessdate=}}</ref> |
|||
==Epidemiology== |
|||
{{See also|Pregnancy rate|Advanced maternal age}} |
|||
The incidence of pregnancy among the female population, as well as the ages at which it occurs, differ significantly by country and region, and are often influenced by a multitude of factors, such as cultural, social and religious norms; access to contraception; and the prevalence of (higher) education. The total fertility rate (TFR) in 2013 was estimated to be highest in [[Niger]] (7.03 children born per woman) and lowest in [[Singapore]] (0.79 children/woman).<ref>https://www.cia.gov/library/publications/the-world-factbook/rankorder/2127rank.html</ref> |
|||
In Europe, the average childbearing age has been rising continuously for some time. In Western, Northern, and Southern Europe, first-time mothers are on average 26 to 29 years old, up from 23 to 25 years at the start of the 1970s. In a number of European countries (Spain), the mean age of women at first childbirth has now even crossed the 30-year threshold. |
|||
This process is not restricted to Europe. Asia, Japan and the United States are all seeing average age at first birth on the rise, and increasingly the process is spreading to countries in the developing world like China, Turkey and Iran. In the US, the age of first childbirth was 25.4 in 2010.<ref>[http://www.cdc.gov/nchs/data/nvsr/nvsr61/nvsr61_01.pdf National Vital Statistics Reports] from [[Centers for Disease Control and Prevention]] National Center for Health Statistics. Volume 61, Number 1 August 28, 2012: Births: Final Data for 2010</ref> |
|||
==Society and culture== |
|||
[[File:Venus of Willendorf 03.jpg|thumb|The "[[Venus of Willendorf]]"]] |
|||
<!-- This section has no references because it is mostly based on the German Wikipedia article. Most information here is common sense or should be easy to source. The section is intended to kickstart a more in-depth treatment. --> |
|||
In most cultures, pregnant women have a special status in society and receive particularly gentle care.<ref name=isbn_9780759110441 /> At the same time, they are subject to expectations that may exert great psychological pressure, such as having to produce a son and heir. In many traditional societies, pregnancy must be preceded by marriage, on pain of ostracism of mother and [[Legitimacy (law)|(illegitimate) child]]. |
|||
Depictions of pregnant women can serve as mystically connotated symbols of fertility. The so-called [[Venus of Willendorf]] with its exaggerated female sexual characteristics (huge breasts and belly, prominent [[mons pubis]]) has been interpreted as indicative of a [[rite|fertility cult]] in [[paleolithic Europe]]. |
|||
Overall, pregnancy is accompanied by numerous customs that are often subject to ethnological research, often rooted in [[traditional medicine]] or religion. The [[baby shower]] is an example of a modern custom. |
|||
Pregnancy is an important topic in [[sociology of the family]]. The prospective child is preliminarily placed into numerous [[social role]]s such as prospective heir or welfare recipient. (This may accelerate weddings.) The parents' relationship and the relation between parents and their surroundings are also affected. |
|||
[[File:Giotto - Scrovegni - -16- - Visitation.jpg|thumb|left|[[Giotto di Bondone]]<br />[[Visitation (Christianity)|Visitation]], circa 1305]] |
|||
===Arts=== |
|||
Due to the important role of the [[Mother of God]] in Christianity, the Western visual arts have a long tradition of depictions of pregnancy.<ref>{{cite book|last=Rossi|first=Timothy Verdon ; captions by Filippo|title=Mary in western art|year=2005|publisher=In Association with Hudson Hills Press|location=New York|isbn=0-9712981-9-X|pages=106|url=http://books.google.com/?id=qd7EZAFouDgC&pg=PA106&dq=097129819X+pregnancy#v=onepage&q&f=false}}</ref> |
|||
Pregnancy, and especially pregnancy of unmarried women, is also an important motif in literature. Notable examples include Hardy's [[Tess of the d'Urbervilles]] and Goethe's [[Faust: The First Part of the Tragedy|Faust]]. |
|||
===Infertility=== |
|||
{{main|Assisted reproductive technology}} |
|||
Modern reproductive medicine offers a choice of measures for couples who stay childless against their will: fertility treatment, [[artificial insemination]] and [[surrogacy]]. |
|||
===Abortion=== |
|||
{{main|Abortion}} |
|||
An abortion is the termination of an embryo or fetus, either naturally or via medical methods. When done electively, it is more often done within the first trimester than the second, and rarely in the third.<ref name=sharply /> Not using contraception, contraceptive failure, poor family planning or rape can lead to [[unintended pregnancy|undesired pregnancies]]. Legality of socially indicated abortions varies widely both internationally and through time. In most countries of Western Europe, abortions during the first trimester were a criminal offense a few decades ago but have since been legalized, sometimes subject to mandatory consultations. In Germany, for example, as of 2009 less than 3% of abortions had a medical indication. |
|||
===Legal protection=== |
|||
Many countries have various legal regulations in place to protect pregnant women and their children. [[Maternity Protection Convention, 2000|Maternity Protection Convention]] ensures that pregnant women are exempt from activities such as night shifts or carrying heavy stocks. [[Maternity leave]] typically provides paid leave from work during roughly the last trimester of pregnancy and for some time after birth. Notable extreme cases include Norway (8 months with full pay) and the United States (no paid leave at all except in some states). Moreover, many countries have laws against [[pregnancy discrimination]]. |
|||
==References== |
|||
{{Reflist|colwidth=30em|refs= |
|||
<ref name=isbn_9780759110441>{{cite book|last=Womack|first=Mari|title=The anthropology of health and healing.|year=2010|publisher=AltaMira Press|location=Plymouth|isbn=978-0-7591-1044-1|pages=133|url=http://books.google.com/?id=DvR53MCGx1YC&pg=PA133&dq=In+most+cultures,+pregnant+women+have+a+special+status+in+society#v=onepage&q=In%20most%20cultures%2C%20pregnant%20women%20have%20a%20special%20status%20in%20society&f=false}}</ref> |
|||
}} |
|||
==Further reading== |
|||
* {{cite web|title=Nutrition For The First Trimester Of Pregnancy|url=http://www.ideafit.com/fitness-library/nutrition-for-the-first-trimester-of-pregnancy|publisher=IDEA Health & Fitness Association|accessdate=9 December 2013}} |
|||
* {{cite journal|last=Bothwell|first=TH|title=Iron requirements in pregnancy and strategies to meet them|journal=The American journal of clinical nutrition|date=July 2000|volume=72|issue=1 Suppl|pages=257S–264S|pmid=10871591}} |
|||
* {{cite journal|last=O'Brien|first=KO|title=Bone calcium turnover during pregnancy and lactation in women with low calcium diets is associated with calcium intake and circulating insulin-like growth factor 1 concentrations1|journal=Am J Clin Nutr|date=February 2006|volume=83|issue=2|pages=317–323|pmid=16469990|url=http://ajcn.nutrition.org/content/83/2/317.full}} |
|||
==External links== |
|||
{{Commons category|Human pregnancy}} |
|||
* {{dmoz|Health/Reproductive_Health/Pregnancy_and_Birth}} |
|||
* [http://www.merckmanuals.com/home/womens_health_issues/pregnancy_complicated_by_disease/overview_of_disease_during_pregnancy.html Merck Manual Home Health Handbook] – further details on the diseases, disorders, etc., which may complicate pregnancy. |
|||
* [http://www.nhs.uk/Planners/pregnancycareplanner/Pages/PregnancyHome.aspx Pregnancy care planner] – NHS guide to having baby including preconception, pregnancy, labor, and birth. |
|||
{{Pregnancy}} |
|||
{{Pathology of pregnancy, childbirth and the puerperium}} |
|||
{{Pediatric conditions originating in the perinatal period}} |
|||
{{Reproductive health}} |
|||
{{Reproductive physiology}} |
|||
{{Humandevelopment}} |
|||
{{sex}} |
|||
[[Category:Human pregnancy| ]] |
|||
[[Category:Birth control]] |
|||
[[Category:Reproduction in mammals| ]] |
|||
[[Category:Obstetrics]] |
|||
[[Category:Family]] |
|||
[[Category:Fertility]] |
|||
{{Link FA|mk}} |
|||
{{Link FA|af}} |
|||
Revision as of 20:45, 29 December 2013
| Aparnaji/sandbox |
|---|
Pregnancy is the fertilization and development of one or more offspring, known as an embryo or fetus, in a woman's uterus. It is the common name for gestation in humans. A multiple pregnancy involves more than one embryo or fetus a single pregnancy, such as with twins. Childbirth usually occurs about 38 weeks after conception; in women who have a menstrual cycle length of four weeks, this is approximately 40 weeks from the start of the last normal menstrual period (LNMP). Human pregnancy is the most studied of all mammalian pregnancies. Conception can be achieved through sexual intercourse or assisted reproductive technology.
An embryo is the developing offspring during the first 8 weeks following conception, and subsequently the term fetus is used until birth.[1][2] In many societies' medical or legal definitions, human pregnancy is somewhat arbitrarily divided into three trimester periods, as a means to simplify reference to the different stages of prenatal development. The first trimester carries the highest risk of miscarriage (natural death of embryo or fetus). During the second trimester, the development of the fetus can be more easily monitored and diagnosed. The beginning of the third trimester often approximates the point of viability, or the ability of the fetus to survive, with or without medical help, outside of the uterus.[3]
In the United States and United Kingdom, 40% of pregnancies are unplanned, and between a quarter and half of those unplanned pregnancies were unwanted pregnancies.[4][5] Of those unintended pregnancies that occurred in the US, 60% of the women used birth control to some extent during the month pregnancy occurred.[6]
Terminology
One scientific term for the state of pregnancy is gravidity (adjective "gravid"), Latin for "heavy" and a pregnant female is sometimes referred to as a gravida.[7] Similarly, the term parity (abbreviated as "para") is used for the number of times a female has given birth, counting twins and other multiple births as one pregnancy, and usually including stillbirths. Medically, a woman who has never been pregnant is referred to as a nulligravida, a woman who is (or has been only) pregnant for the first time as a primigravida,[8] and a woman in subsequent pregnancies as a multigravida or multiparous.[7][9] Hence, during a second pregnancy a woman would be described as gravida 2, para 1 and upon live delivery as gravida 2, para 2. An in-progress pregnancy, as well as abortions, miscarriages, or stillbirths account for parity values being less than the gravida number. In the case of twins, triplets etc., gravida number and parity value are increased by one only. Women who have never carried a pregnancy achieving more than 20 weeks of gestation age are referred to as nulliparous.[10]
Physiology

Initiation

The most commonly used event to mark the initiation of pregnancy is the first day of the woman's last normal menstrual period, and the resulting fetal age is called the gestational age. This choice is a result of a lack of a convenient way to discern the point in time when the actual creation of the baby naturally happens. In case of in vitro fertilisation, gestational age is calculated by days from oocyte retrieval + 14 days.[11]
Still, already at the initiation of the preceding menstrual period the female body goes through changes to prepare for an upcoming conception, including a rise in follicle stimulating hormone that stimulates folliculogenesis and subsequently oogenesis in order to give rise to a mature egg cell, which is the female gamete. Fertilization is the event where the egg cell fuses with the male gamete, spermatozoon. In lay terms, it is more commonly known as "conception." After the point of fertilization, the fused product of the female and male gamete is referred to as a zygote or fertilized egg. The fusion of male and female gametes usually occurs following the act of sexual intercourse, resulting in spontaneous pregnancy. It can also occur by assisted reproductive technology such as artificial insemination and in vitro fertilisation, and may be undertaken as a voluntary choice or due to infertility.
The event of fertilization is sometimes used as a mark of the initiation of pregnancy, with the derived age being termed fertilization age, and is an alternative to gestational age. Fertilization usually occurs about two weeks before her next expected menstrual period, and if either date is unknown in an individual case it is a frequent practice to add 14 days to the fertilization age to get the gestational age and vice versa.
Development of embryo and fetus
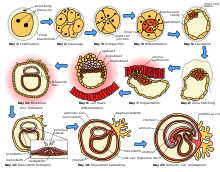
The sperm and the egg cell, which has been released from one of the female's two ovaries, unite in one of the two fallopian tubes. The fertilized egg, known as a zygote, then moves toward the uterus, a journey that can take up to a week to complete. Cell division begins approximately 24 to 36 hours after the male and female cells unite. Cell division continues at a rapid rate and the cells then develop into what is known as a blastocyst. The blastocyst arrives at the uterus and attaches to the uterine wall, a process known as implantation.
The development of the mass of cells that will become the baby is called embryogenesis during the first approximately 10 weeks of gestation. During this time, cells begin to differentiate into the various body systems. The basic outlines of the organ, body, and nervous systems are established. By the end of the embryonic stage, the beginnings of features such as fingers, eyes, mouth, and ears become visible. Also during this time, there is development of structures important to the support of the embryo, including the placenta and umbilical cord. The placenta connects the developing embryo to the uterine wall to allow nutrient uptake, waste elimination, and gas exchange via the mother's blood supply. The umbilical cord is the connecting cord from the embryo or fetus to the placenta.
After about 10 weeks of gestational age, the embryo becomes known as a fetus instead. At the beginning of the fetal stage, the risk of miscarriage decreases sharply,[12] When the fetal stage commences, a fetus is typically about 30 mm (1.2 inches) in length, and the heart can be seen beating via ultrasound; the fetus can be seen making various involuntary motions at this stage.[13] During continued fetal development, the early body systems and structures that were established in the embryonic stage continue to develop. Sex organs begin to appear during the third month of gestation. The fetus continues to grow in both weight and length, although the majority of the physical growth occurs in the last weeks of pregnancy.
Electrical brain activity is first detected between the 5th and 6th week of gestation, though this is still considered primitive neural activity rather than the beginning of conscious thought, something that develops much later in fetation. Synapses begin forming at 17 weeks, and at about week 28 begin to multiply at a rapid pace which continues until 3 to 4 months after birth.[14]
-
Relative size in 1st month (simplified illustration)
-
Relative size in 3rd month (simplified illustration)
-
Relative size in 5th month (simplified illustration)
-
Relative size in 9th month (simplified illustration)
Maternal changes

During pregnancy, the woman undergoes many physiological changes, which are entirely normal, including cardiovascular, hematologic, metabolic, renal and respiratory changes that become very important in the event of complications. The body must change its physiological and homeostatic mechanisms in pregnancy to ensure the fetus is provided for. Increases in blood sugar, breathing and cardiac output are all required. Levels of progesterone and oestrogens rise continually throughout pregnancy, suppressing the hypothalamic axis and subsequently the menstrual cycle.
The fetus inside a pregnant woman may be viewed as an unusually successful allograft, since it genetically differs from the woman.[19] The main reason for this success is an increased maternal immune tolerance during pregnancy. However, this increased immune tolerance in pregnancy can also cause an increased susceptibility to and severity of some infectious diseases.
Pregnancy is typically broken into three periods, or trimesters, each of about three months.[20][21] Obstetricians define each trimester as lasting for 14 weeks, resulting in a total duration of 42 weeks, although the average duration of pregnancy is actually about 40 weeks.[22] While there are no hard and fast rules, these distinctions are useful in describing the changes that take place over time.
First trimester
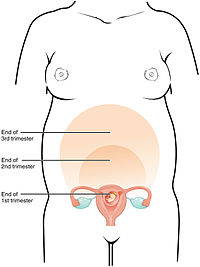
Minute ventilation is increased by 40% in the first trimester.[23] The womb will grown to the size of a lemon by eight weeks. Many symptoms and discomforts of pregnancy (further described in later sections) appear in the first trimester.[24]
Second trimester

Weeks 13 to 28 of the pregnancy are called the second trimester. Most women feel more energized in this period, and begin to put on weight as the symptoms of morning sickness subside and eventually fade away. The uterus, the muscular organ that holds the developing fetus, can expand up to 20 times its normal size during pregnancy.
Although the fetus begins to move and takes a recognizable human shape during the first trimester, it is not until the second trimester that movement of the fetus, often referred to as "quickening", can be felt. This typically happens in the fourth month, more specifically in the 20th to 21st week, or by the 19th week if the woman has been pregnant before. However, it is not uncommon for some women not to feel the fetus move until much later. During the second trimester, most women begin to wear maternity clothes.
Third trimester

Final weight gain takes place, which is the most weight gain throughout the pregnancy. The woman's belly will transform in shape as the belly drops due to the fetus turning in a downward position ready for birth. During the second trimester, the woman's belly would have been very upright, whereas in the third trimester it will drop down quite low, and the woman will be able to lift her belly up and down. The fetus begins to move regularly, and is felt by the woman. Fetal movement can become quite strong and be disruptive to the woman. The woman's navel will sometimes become convex, "popping" out, due to her expanding abdomen.
Head engagement, where the fetal head descends into cephalic presentation, relieves pressure on the upper abdomen with renewed ease in breathing. However, it severely reduces bladder capacity, increases pressure on the pelvic floor and the rectum.
It is also during the third trimester that maternal activity and sleep positions may affect fetal development due to restricted blood flow. For instance, the enlarged uterus may impede blood flow by compressing the lower pressured vena cava, with the left lateral laying positions appearing to providing better oxygenation to the infant.[25]
Duration
Since these are spread over a significant period of time, the duration of pregnancy necessarily depends on the date selected as the starting point chosen.
As measured on a reference group of women with a menstrual cycle of exactly 28-days prior to pregnancy, and who had spontaneous onset of labor, the mean pregnancy length has been estimated to be 283.4 days of gestational age as timed from the first day of the last menstrual period as recalled by the mother, and 280.6 days when the gestational age was retrospectively estimated by obstetric ultrasound measurement of the fetal biparietal diameter (BPD) in the second trimester.[26] Other algorithms take into account a variety of other variables, such as whether this is the first or subsequent child (i.e., pregnant woman is a primipara or a multipara, respectively), the mother's race, parental age, length of menstrual cycle, and menstrual regularity), but these are rarely used by healthcare professionals. In order to have a standard reference point, the normal pregnancy duration is generally assumed to be 280 days (or 40 weeks) of gestational age.
There is a standard deviation of 8–9 days surrounding due dates calculated with even the most accurate methods. This means that fewer than 5 percent of births occur on the day of being 40 weeks of gestational age; 50 percent of births are within a week of this duration, and about 80 percent are within 2 weeks.[26] For the estimation of due date, mobile apps essentially always give consistent estimations compared to each other and correct for leap year, while pregnancy wheels made of paper can differ from each other by 7 days and generally do not correct for leap year.[27]
The most common system used among healthcare professionals is Naegele's rule, which was developed in the early 19th century. This calculates the expected due date from the first day of the last normal menstrual period (LMP or LNMP) regardless of factors known to make this inaccurate, such as a shorter or longer menstrual cycle length. Pregnancy most commonly lasts for 40 weeks according to this LNMP-based method, assuming that the woman has a predictable menstrual cycle length of close to 28 days and conceives on the 14th day of that cycle.
As measured from the day of ovulation, the average time to birth has been estimated to be 268 days (38 weeks and two days), with a coefficient of variation of 3.7%.[28]
Accurate dating of pregnancy is important, because it is used in calculating the results of various prenatal tests, (for example, in the triple test). A decision may be made to induce labour if a fetus is perceived to be overdue. Furthermore, if LMP and ultrasound dating predict different respective due dates, with the latter being later, this might signify slowed fetal growth and therefore require closer review.
The stage of pregnancy defined as the beginning of legal fetal viability varies around the world. It sometimes incorporates weight as well as gestational age.[29] It ranges from 16 weeks in Norway, to 20 weeks in the US and Australia, 24 weeks in the UK and 26 weeks in Italy and Spain.[29][30][31]
Preterm, term and postterm
Pregnancy is considered "at term" when gestation has lasted 37 complete weeks (occurring at the transition from the 37th to the 38th week of gestation), but is less than 42 weeks of gestational age (occurring at the transition from the 42nd week to the 43rd week of gestation, or between 259 and 294 days since LMP). The American College of Obstetricians and Gynecologists recommends the following categorization of term pregnancies:[32]
- Early Term: Between 37 weeks 0 days and 38 weeks 6 days of gestational age
- Full Term: Between 39 weeks 0 days and 40 weeks 6 days of gestational age
- Late Term: Between 41 weeks 0 days and 41 weeks 6 days of gestational age
Events before completion of 37 weeks (259 days) are considered preterm, and events after 42 weeks (294 days) are considered postterm.[32][33] When a pregnancy exceeds 42 weeks (294 days), the risk of complications for both the woman and the fetus increases significantly.[34][35] Therefore, in an otherwise uncomplicated pregnancy, obstetricians usually prefer to induce labour at some stage between 41 and 42 weeks.[36][37]
Birth before 39 weeks by Caesarean section section, even if considered "at term", results in an increased risk of complications and premature death, when not medically needed.[38] This is from factors including underdeveloped lungs, infection due to underdeveloped immune system, feeding problems due to underdeveloped brain, and jaundice from underdeveloped liver. Some hospitals in the United States have noted a significant increase in neonatal intensive care unit patients when women schedule deliveries for convenience and are taking steps to reduce induction for non-medical reasons.[39] Complications from Caesarean section are more common than for live births.
Recent medical literature prefers the terminology preterm and postterm to premature and postmature. Preterm and postterm are unambiguously defined as above, whereas premature and postmature have historical meaning and relate more to the infant's size and state of development rather than to the stage of pregnancy.[40][41]
Childbirth
Childbirth is the process whereby an infant is born.
A woman is considered to be in labour when she begins experiencing regular uterine contractions, accompanied by changes of her cervix – primarily effacement and dilation. While childbirth is widely experienced as painful, some women do report painless labours, while others find that concentrating on the birth helps to quicken labour and lessen the sensations. Most births are successful vaginal births, but sometimes complications arise and a woman may undergo a cesarean section.
During the time immediately after birth, both the mother and the baby are hormonally cued to bond, the mother through the release of oxytocin, a hormone also released during breastfeeding. Studies show that skin-to-skin contact between a mother and her newborn immediately after birth is beneficial for both the mother and baby. A review done by the World Health Organization found that skin-to-skin contact between mothers and babies after birth reduces crying, improves mother-infant interaction, and helps mothers to breastfeed successfully. They recommend that neonates be allowed to bond with the mother during their first two hours after birth, the period that they tend to be more alert than in the following hours of early life.[42]
Postnatal period
The postnatal period begins immediately after the birth of a child and then extends for about six weeks. During this period, the mother's body begins the return to prepregnancy conditions that includes changes in hormone levels and uterus size.
Diagnosis
The beginning of pregnancy may be detected either based on symptoms by the pregnant woman herself, or by using medical tests with or without the assistance of a medical professional. Approximately 1 in 475 women at 20 weeks, and 1 in 2500 women at delivery, refuse to acknowledge that they are pregnant, which is called denial of pregnancy.[43] Some non-pregnant women have a very strong belief that they are pregnant along with some of the physical changes. This condition is known as pseudocyesis or false pregnancy.[44]
Physical signs

Most pregnant women experience a number of symptoms,[45] which can signify pregnancy. The symptoms can include nausea and vomiting, excessive tiredness and fatigue, cravings for certain foods that are not normally sought out, and frequent urination particularly during the night.
A number of early medical signs are associated with pregnancy.[46][47] These signs typically appear, if at all, within the first few weeks after conception. Although not all of these signs are universally present, nor are all of them diagnostic by themselves, taken together they make a presumptive diagnosis of pregnancy. These signs include the presence of human chorionic gonadotropin (hCG) in the blood and urine, missed menstrual period, implantation bleeding that occurs at implantation of the embryo in the uterus during the third or fourth week after last menstrual period, increased basal body temperature sustained for over 2 weeks after ovulation, Chadwick's sign (darkening of the cervix, vagina, and vulva), Goodell's sign (softening of the vaginal portion of the cervix), Hegar's sign (softening of the uterus isthmus), and pigmentation of linea alba – Linea nigra, (darkening of the skin in a midline of the abdomen, caused by hyperpigmentation resulting from hormonal changes, usually appearing around the middle of pregnancy).[46][47] Breast tenderness is common during the first trimester, and is more common in women who are pregnant at a young age.[48] Shortly after conception, the nipples and areolas begin to darken due to a temporary increase in hormones.[49] This process continues throughout the pregnancy.
Despite all the signs, some women may not realize they are pregnant until they are far along in pregnancy. In some cases, a few have not been aware of their pregnancy until they begin labour. This can be caused by many factors, including irregular periods (quite common in teenagers), certain medications (not related to conceiving children), and obese women who disregard their weight gain. Others may be in denial of their situation.
Biomarkers
Pregnancy detection can be accomplished using one or more various pregnancy tests,[50] which detect hormones generated by the newly formed placenta, serving as biomarkers of pregnancy. Blood and urine tests can detect pregnancy 12 days after implantation.[51] Blood pregnancy tests are more sensitive than urine tests (giving fewer false negatives).[52] Home pregnancy tests are urine tests, and normally detect a pregnancy 12 to 15 days after fertilization. A quantitative blood test can determine approximately the date the embryo was conceived. Testing 48 hours apart can provide useful information regarding how the pregnancy is doing. A single test of progesterone levels can also help determine how likely a fetus will survive in those with a threatened miscarriage (bleeding in early pregnancy).[53]
Ultrasound
Obstetric ultrasonography can detect some congenital diseases at an early stage, estimate the due date as well as detecting multiple pregnancy.[54] The resultant estimated due date of the fetus is slightly more accurate than methods based on last menstrual period.[55] In those who are at low risk it is unclear if obstetric ultrasound before 24 weeks makes a significant difference in outcomes.[56] Routine ultrasound imaging after 24 weeks gestation does not improve outcomes in either the mother or the baby and might increase the risk of a cesarean section.[57] It is thus is not recommended.[56] Modern 3D ultrasound images provide greater detail for prenatal diagnosis than the older 2D ultrasound technology.[58] While 3D is popular with parents desiring a prenatal photograph as a keepsake,[59] both 2D and 3D are discouraged by the FDA for non-medical use,[60] but there are no definitive studies linking ultrasound to any adverse medical effects.[61] The following 3D ultrasound images were taken at different stages of pregnancy:
-
3D Ultrasound of fetal movements at 12 weeks
-
75-mm fetus (about 14 weeks gestational age)
-
Fetus at 17 weeks
-
Fetus at 20 weeks
Management
Attending prenatal care
Prenatal medical care is the medical and nursing care recommended for women before and during pregnancy. The aim of good prenatal care is to identify any potential problems early, to prevent them if possible (through recommendations on adequate nutrition, exercise, vitamin intake etc.), and to manage problems, possibly by directing the woman to appropriate specialists, hospitals, etc. if necessary.
Nutrition
A balanced, nutritious diet is an important aspect of a healthy pregnancy. Eating a healthy diet, balancing carbohydrates, fat, and proteins, and eating a variety of fruits and vegetables, usually ensures good nutrition. Those whose diets are affected by health issues, religious requirements, or ethical beliefs may choose to consult a health professional for specific advice.
Adequate periconceptional folic acid (also called folate or Vitamin B9) intake has been shown to decrease the risk of fetal neural tube defects such as spina bifida, a serious birth defect. The neural tube develops during the first 28 days of pregnancy, explaining the necessity to guarantee adequate periconceptional folate intake.[62][63] Folate (from folia, leaf) is abundant in spinach (fresh, frozen, or canned), and is found in green leafy vegetables e.g. salads, beets, broccoli, asparagus, citrus fruits and melons, chickpeas (i.e. in the form of hummus or falafel), and eggs. In the United States and Canada, most wheat products (flour, noodles) are fortified with folic acid.[64]
DHA omega-3 is a major structural fatty acid in the brain and retina, and is naturally found in breast milk. It is important for the woman to consume adequate amounts of DHA during pregnancy and while nursing to support her well-being and the health of her infant. Developing infants cannot produce DHA efficiently, and must receive this vital nutrient from the woman through the placenta during pregnancy and in breast milk after birth.[65]
Several micronutrients are important for the health of the developing fetus, especially in areas of the world where insufficient nutrition is prevalent.[66] In developed areas, such as Western Europe and the United States, certain nutrients such as Vitamin D and calcium, required for bone development, may require supplementation.[67][68][69]
Dangerous bacteria or parasites may contaminate foods, including Listeria and Toxoplasma gondii. Careful washing of fruits and raw vegetables may remove these pathogens, as may thoroughly cooking leftovers, meat, or processed meat. Soft cheeses may contain Listeria; if milk is raw, the risk may increase. Cat feces pose a particular risk of toxoplasmosis. Pregnant women are also more prone to Salmonella infections from eggs and poultry, which should be thoroughly cooked. Practicing good hygiene in the kitchen can reduce these risks.[70]
Weight gain
The amount of healthy weight gain during a pregnancy varies.[71] Weight gain is only partly related to the weight of the baby and growing placenta, and includes extra fluid for circulation, and the weight needed to provide nutrition for the growing fetus.[72] Most needed weight gain occurs later in pregnancy.[72]
The Institute of Medicine recommends an overall pregnancy weight gain for those of normal weight (body mass index of 18.5–24.9), of 11.3–15.9 kg (25–35 pounds) having a singleton pregnancy.[73] Women who are underweight (BMI of less than 18.5), should gain between 12.7–18 kg (28–40 lbs), while those who are overweight (BMI of 25–29.9) are advised to gain between 6.8–11.3 kg (15–25 lbs) and those who are obese (BMI>30) should gain between 5–9 kg (11–20 lbs).[74]
During pregnancy, insufficient or excessive weight gain can compromise the health of the mother and fetus.[72] The most effective interventions for weight gain in underweight women is not clear.[72] Being or becoming very overweight in pregnancy increases the risk of complications for mother and fetus, including cesarean section, gestational hypertension, pre-eclampsia, macrosomia and shoulder dystocia.[71] It can make losing weight after the pregnancy difficult.[71][75]
Around 50% of women of childbearing age in developed countries like the United Kingdom are overweight or obese before pregnancy.[75] A systematic review found that diet is the most effective way to reduce weight gain and associated risks in pregnancy.[75] The review did not find evidence of harm associated with diet control and exercise.[75]
Medication use
Drugs used during pregnancy can have temporary or permanent effects on the fetus. Therefore many physicians would prefer not to prescribe for pregnant women, the major concern being over teratogenicity of the drugs.
Drugs have been classified into categories A,B,C,D and X based on the Food and Drug Administration (FDA) rating system to provide therapeutic guidance based on potential benefits and fetal risks. Drugs, including some multivitamins, that have demonstrated no fetal risks after controlled studies in humans are classified as Category A. On the other hand drugs like thalidomide with proven fetal risks that outweigh all benefits are classified as Category X.[76]
Use of recreational drugs
Use of recreational drugs in pregnancy can cause various pregnancy complications.
- Ethanol during pregnancy can cause fetal alcohol syndrome and fetal alcohol spectrum disorder. A number of studies have shown that light to moderate drinking during pregnancy might not pose a risk to the fetus, although no amount of alcohol during pregnancy can be guaranteed to be absolutely safe.[77]
- Tobacco smoking and pregnancy, when combined, can cause a wide range of behavioral, neurological, and physical difficulties.[78] Smoking during pregnancy causes twice the risk of premature rupture of membranes, placental abruption and placenta previa.[79] Also, it causes 30% higher odds of the baby being born prematurely.[80]
- Prenatal cocaine exposure is associated with, for example, premature birth, birth defects and attention deficit disorder.
- Prenatal methamphetamine exposure can cause premature birth and congenital abnormalities.[81] Other investigations have revealed short-term neonatal outcomes to include small deficits in infant neurobehavioral function and growth restriction when compared to control infants.[82] Also, prenatal methamphetamine use is believed to have long-term effects in terms of brain development, which may last for many years.[81]
- Cannabis in pregnancy is possibly associated with adverse effects on the child later in life.
Exposure to environmental toxins
Intrauterine exposure to environmental toxins in pregnancy has the potential to cause adverse effects on the prenatal development of the embryo or fetus, as well as pregnancy complications. Potential effects of toxic substances and pollution include congenital abnormalities. Also, neuroplastic effects of pollution can give rise to neurodevelopmental disorders for the child later in life. Conditions of particular severity in pregnancy include mercury poisoning and lead poisoning. To minimize exposure to environmental toxins, the American College of Nurse-Midwives recommends for example checking whether lead paint has been used if living in a home built before 1978, washing all produce thoroughly and buying organic produce, as well as well as avoiding any cleaning supply labeled "toxic" or any product with a warning on the label.[83]
Sexual activity
Most women can continue to engage in sexual activity throughout pregnancy.[84] Most research suggests that during pregnancy both sexual desire and frequency of sexual relations decrease.[85][86] In context of this overall decrease in desire, some studies indicate a second-trimester increase, preceding a decrease during the third trimester.[87][88] Some individuals are sexually attracted to pregnant women (pregnancy fetishism, also known as maiesiophilia).
Sex during pregnancy is a low-risk behavior except when the healthcare provider advises that sexual intercourse be avoided for particular medical reasons. Otherwise, for a healthy pregnant woman who is not ill or weak, there is no safe or right way to have sex during pregnancy: it is enough to apply the common sense rule that both partners avoid putting pressure on the uterus, or a partner's full weight on a pregnant belly.[89]
Exercise
Regular aerobic exercise during pregnancy appears to improve (or maintain) physical fitness; however, the quality of the research is poor and the data was insufficient to infer important risks or benefits for the mother or infant.[90]
The Clinical Practice Obstetrics Committee of Canada recommends that "All women without contraindications should be encouraged to participate in aerobic and strength-conditioning exercises as part of a healthy lifestyle during their pregnancy". Although an upper level of safe exercise intensity has not been established, women who were regular exercisers before pregnancy and who have uncomplicated, healthy pregnancies should be able to engage in high intensity exercise programs, such as jogging and aerobics for less than 45 minutes, with no adverse effects if they are mindful of the possibility that they may need to increase their energy intake and are careful to not become overheated. In the absence of either medical or obstetric complications, they advise an accumulation of 30 minutes a day of exercise on most if not all days of the week. In general, participation in a wide range of recreational activities appears to be safe, with the avoidance of those with a high risk of falling such as horseback riding or skiing or those that carry a risk of abdominal trauma, such as soccer or hockey.[91]
The American College of Obstetricians and Gynecologists reports that in the past, the main concerns of exercise in pregnancy were focused on the fetus and any potential maternal benefit was thought to be offset by potential risks to the fetus. However, they write that more recent information suggests that in the uncomplicated pregnancy, fetal injuries are highly unlikely. They do, however, list several circumstances when a woman should contact her health care provider before continuing with an exercise program. Contraindications include: Vaginal bleeding, dyspnea before exertion, dizziness, headache, chest pain, muscle weakness, preterm labor, decreased fetal movement, amniotic fluid leakage, and calf pain or swelling (to rule out thrombophlebitis).[91]
Symptoms and discomforts

The symptoms and discomforts of pregnancy are those presentations and conditions that result from pregnancy but do not significantly interfere with activities of daily living or pose any significant threat to the health of the mother or baby, in contrast to pregnancy complications. Still, there is often no clear separation between symptoms versus discomforts versus complications, and in some cases the same basic feature can manifest as either a discomfort or a complication depending on the severity. For example, mild nausea may merely be a discomfort (morning sickness), but if severe and with vomiting causing water-electrolyte imbalance it can be classified as a pregnancy complication (hyperemesis gravidarum).
Common symptoms and discomforts of pregnancy include:
- Tiredness.
- Constipation
- Pelvic girdle pain
- Back pain
- Braxton Hicks contractions. Occasional, irregular, and often painless contractions that occur several times per day.
- Edema (swelling). Common complaint in advancing pregnancy. Caused by compression of the inferior vena cava (IVC) and pelvic veins by the uterus leads to increased hydrostatic pressure in lower extremities.
- Increased urinary frequency. A common complaint referred by the gravida, caused by increased intravascular volume, elevated GFR (glomerular filtration rate), and compression of the bladder by the expanding uterus.
- Urinary tract infection[92]
- Varicose veins. Common complaint caused by relaxation of the venous smooth muscle and increased intravascular pressure.
- Haemorrhoids (piles) are swollen veins at or inside the anal area, resulting from impaired venous return, straining associated with constipation, or increased intra-abdominal pressure in later pregnancy.[93]
- Regurgitation, heartburn, and nausea.
- Striae gravidarum, pregnancy-related stretch marks
Complications
Each year, according to the WHO, ill-health as a result of pregnancy is experienced (sometimes permanently) by more than 20 million women around the world. Furthermore, the "lives of eight million women are threatened, and more than 500,000 women are estimated to have died in 1995 as a result of causes related to pregnancy and childbirth."[94]
The following are some examples of pregnancy complications:
- Pregnancy induced hypertension
- Anemia[95]
- Postpartum depression
- Postpartum psychosis
- Thromboembolic disorders. The leading cause of death in pregnant women in the US.[96]
- PUPPP skin disease that develop around the 32nd week. (Pruritic Urticarial Papules and Plaques of Pregnancy), red plaques, papules, itchiness around the belly button that spread all over the body except for the inside of hands and face.
- Ectopic pregnancy, implantation of the embryo outside the uterus.
- Hyperemesis gravidarum, excessive nausea that is more severe than morning sickness.
Intercurrent diseases
In addition to complications of pregnancy that can arise, a pregnant woman may have intercurrent diseases, that is, other diseases or conditions (not directly caused by the pregnancy) that may become worse or be a potential risk to the pregnancy.
- Diabetes mellitus and pregnancy deals with the interactions of diabetes mellitus (not restricted to gestational diabetes) and pregnancy. Risks for the child include miscarriage, growth restriction, growth acceleration, fetal obesity (macrosomia), polyhydramnios and birth defects.
- Systemic lupus erythematosus and pregnancy confers an increased rate of fetal death in utero and spontaneous abortion (miscarriage), as well as of neonatal lupus.
- Thyroid disease in pregnancy can, if uncorrected, cause adverse effects on fetal and maternal well-being. The deleterious effects of thyroid dysfunction can also extend beyond pregnancy and delivery to affect neurointellectual development in the early life of the child. Demand for thyroid hormones is increased during pregnancy which may cause a previously unnoticed thyroid disorder to worsen.
- Hypercoagulability in pregnancy is the propensity of pregnant women to develop thrombosis (blood clots). Pregnancy itself is a factor of hypercoagulability (pregnancy-induced hypercoagulability), as a physiologically adaptive mechanism to prevent post partum bleeding.[97] However, when combined with an additional underlying hypercoagulable states, the risk of thrombosis or embolism may become substantial.[97]
Epidemiology
The incidence of pregnancy among the female population, as well as the ages at which it occurs, differ significantly by country and region, and are often influenced by a multitude of factors, such as cultural, social and religious norms; access to contraception; and the prevalence of (higher) education. The total fertility rate (TFR) in 2013 was estimated to be highest in Niger (7.03 children born per woman) and lowest in Singapore (0.79 children/woman).[98]
In Europe, the average childbearing age has been rising continuously for some time. In Western, Northern, and Southern Europe, first-time mothers are on average 26 to 29 years old, up from 23 to 25 years at the start of the 1970s. In a number of European countries (Spain), the mean age of women at first childbirth has now even crossed the 30-year threshold.
This process is not restricted to Europe. Asia, Japan and the United States are all seeing average age at first birth on the rise, and increasingly the process is spreading to countries in the developing world like China, Turkey and Iran. In the US, the age of first childbirth was 25.4 in 2010.[99]
Society and culture

In most cultures, pregnant women have a special status in society and receive particularly gentle care.[100] At the same time, they are subject to expectations that may exert great psychological pressure, such as having to produce a son and heir. In many traditional societies, pregnancy must be preceded by marriage, on pain of ostracism of mother and (illegitimate) child.
Depictions of pregnant women can serve as mystically connotated symbols of fertility. The so-called Venus of Willendorf with its exaggerated female sexual characteristics (huge breasts and belly, prominent mons pubis) has been interpreted as indicative of a fertility cult in paleolithic Europe.
Overall, pregnancy is accompanied by numerous customs that are often subject to ethnological research, often rooted in traditional medicine or religion. The baby shower is an example of a modern custom.
Pregnancy is an important topic in sociology of the family. The prospective child is preliminarily placed into numerous social roles such as prospective heir or welfare recipient. (This may accelerate weddings.) The parents' relationship and the relation between parents and their surroundings are also affected.

Visitation, circa 1305
Arts
Due to the important role of the Mother of God in Christianity, the Western visual arts have a long tradition of depictions of pregnancy.[101]
Pregnancy, and especially pregnancy of unmarried women, is also an important motif in literature. Notable examples include Hardy's Tess of the d'Urbervilles and Goethe's Faust.
Infertility
Modern reproductive medicine offers a choice of measures for couples who stay childless against their will: fertility treatment, artificial insemination and surrogacy.
Abortion
An abortion is the termination of an embryo or fetus, either naturally or via medical methods. When done electively, it is more often done within the first trimester than the second, and rarely in the third.[12] Not using contraception, contraceptive failure, poor family planning or rape can lead to undesired pregnancies. Legality of socially indicated abortions varies widely both internationally and through time. In most countries of Western Europe, abortions during the first trimester were a criminal offense a few decades ago but have since been legalized, sometimes subject to mandatory consultations. In Germany, for example, as of 2009 less than 3% of abortions had a medical indication.
Legal protection
Many countries have various legal regulations in place to protect pregnant women and their children. Maternity Protection Convention ensures that pregnant women are exempt from activities such as night shifts or carrying heavy stocks. Maternity leave typically provides paid leave from work during roughly the last trimester of pregnancy and for some time after birth. Notable extreme cases include Norway (8 months with full pay) and the United States (no paid leave at all except in some states). Moreover, many countries have laws against pregnancy discrimination.
References
- ^ "Embryo definition". MedicineNet, Inc. 27 April 2011.
- ^ "Fetus definition". MedicineNet, Inc. 27 April 2011.
- ^ "Trimester definition". MedicineNet, Inc. 27 April 2011.
- ^ "40% of pregnancies 'unplanned'". BBC News. 16 March 2004.
- ^ Jayson, Sharon (20 May 2011). "Unplanned pregnancies in U.S. at 40 percent". PhysOrg.com.
- ^ The Johns Hopkins manual of gynecology and obstetrics (4th ed.). Philadelphia: Wolters Kluwer Health / Lippincott Williams & Wilkins. p. 232. ISBN 9781605474335.
{{cite book}}: Cite uses deprecated parameter|authors=(help) - ^ a b "definition of gravida". The Free Dictionary. Retrieved 17 January 2008.
- ^ Robinson, Victor, ed. (1939). "Primipara". The Modern Home Physician, A New Encyclopedia of Medical Knowledge. WM. H. Wise & Company (New York)., page 596.
- ^ "Definition of nulligravida". Merriam-Webster, Incorporated. Retrieved 9 March 2012.
- ^ "Nulliparous definition". MedicineNet, Inc. 18 November 2000.
- ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 10776011, please use {{cite journal}} with
|pmid=10776011instead. - ^ a b
- Lennart Nilsson, A Child is Born 91 (1990): at eight weeks, "the danger of a miscarriage … diminishes sharply."
- "Women's Health Information", Hearthstone Communications Limited: "The risk of miscarriage decreases dramatically after the 8th week as the weeks go by." Retrieved 2007-04-22.
- ^ Kalverboer, Alex Fedde; Gramsbergen, Albertus Arend (1 January 2001). Handbook of Brain and Behaviour in Human Development. Springer. pp. 1–. ISBN 978-0-7923-6943-1.
- ^ Illes, ed. by Judy (2008). Neuroethics : defining the issues in theory, practice, and policy (Repr. ed.). Oxford: Oxford University Press. p. 142. ISBN 9780198567219.
{{cite book}}:|first=has generic name (help) - ^ 3D Pregnancy (Image from gestational age of 6 weeks). Retrieved 2007-08-28. A rotatable 3D version of this photo is available here, and a sketch is available here.
- ^ 3D Pregnancy (Image from gestational age of 10 weeks). Retrieved 2007-08-28. A rotatable 3D version of this photo is available here, and a sketch is available here.
- ^ 3D Pregnancy (Image from gestational age of 20 weeks). Retrieved 2007-08-28. A rotatable 3D version of this photo is available here, and a sketch is available here.
- ^ 3D Pregnancy (Image from gestational age of 40 weeks). Retrieved 2007-08-28. A rotatable 3D version of this photo is available here, and a sketch is available here.
- ^ Clark DA, Chaput A, Tutton D (1986). "Active suppression of host-vs-graft reaction in pregnant mice. VII. Spontaneous abortion of allogeneic CBA/J x DBA/2 fetuses in the uterus of CBA/J mice correlates with deficient non-T suppressor cell activity". J. Immunol. 136 (5): 1668–75. PMID 2936806.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ trimester. CollinsDictionary.com. Collins English Dictionary – Complete & Unabridged 11th Edition. Retrieved 26 November 2012.
- ^ thefreedictionary.com > trimester Citing:
- The American Heritage® Dictionary of the English Language, Fourth Edition, copyright 2000
- ^ Cunningham, et al., (2010). Williams Textbook of Obstetrics, chapter 8.
- ^ Campbell, LA (April 2001). "Implications for the pregnant patient". American Journal of Respiratory and Critical Care Medicine. 163 (5): 1051–54. doi:10.1164/ajrccm.163.5.16353. PMID 11316633.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ http://www.nhs.uk/conditions/pregnancy-and-baby/pages/pregnancy-weeks-4-5-6-7-8.aspx#close
- ^ Stacey, T (2011 Jun 14). "Association between maternal sleep practices and risk of late stillbirth: a case-control study". BMJ (Clinical research ed.). 342: d3403. doi:10.1136/bmj.d3403. PMC 3114953. PMID 21673002.
{{cite journal}}: Check date values in:|date=(help); Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ a b Dr H. Kieler, O. Axelsson, S. Nilsson, U. Waldenströ (1995). "The length of human pregnancy as calculated by ultrasonographic measurement of the fetal biparietal diameter". Ultrasound in Obstetrics & Gynecology. 6 (5): 353–357. doi:10.1046/j.1469-0705.1995.06050353.x. PMID 8590208.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Attention: This template ({{cite doi}}) is deprecated. To cite the publication identified by doi:10.1016/j.ajog.2013.09.013, please use {{cite journal}} (if it was published in a bona fide academic journal, otherwise {{cite report}} with
|doi=10.1016/j.ajog.2013.09.013instead. - ^ Attention: This template ({{cite doi}}) is deprecated. To cite the publication identified by doi:10.1093/humrep/det297, please use {{cite journal}} (if it was published in a bona fide academic journal, otherwise {{cite report}} with
|doi=10.1093/humrep/det297instead. - ^ a b Li, Z (2012). "Australia's Mothers and Babies 2010". Perinatal statistics series no. 27. Cat. no. PER 57. Australian Institute of Health and Welfare National Perinatal Statistics Unit, Australian Government. Retrieved 4 July 2013.
{{cite web}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Mohangoo, AD (2013). Wright, Linda (ed.). "International comparisons of fetal and neonatal mortality rates in high-income countries: should exclusion thresholds be based on birth weight or gestational age?". PLoS ONE. 8 (5): e64869. doi:10.1371/journal.pone.0064869. PMC 3658983. PMID 23700489.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help)CS1 maint: unflagged free DOI (link) - ^ Royal College of Obstetricians and Gynaecologists UK (2001). "Further Issues Relating to Late Abortion, Fetal Viability and Registration of Births and Deaths". Royal College of Obstetricians and Gynaecologists UK. Retrieved 4 July 2013.
{{cite web}}: Unknown parameter|month=ignored (help) - ^ a b Ob-Gyns Redefine Meaning of "Term Pregnancy", from American College of Obstetricians and Gynecologists. October 22, 2013
- ^ "Definitions". Saskatchewan Prevention Institute. Retrieved 16 January 2008.
- ^ Norwitz, MD, PhD, Errol R. "Postterm Pregnancy (Beyond the Basics)". UpToDate, Inc. Retrieved 24 August 2012.
{{cite web}}: CS1 maint: multiple names: authors list (link) - ^ The American College of Obstetricians and Gynecologists (2006). "What To Expect After Your Due Date". Medem. Medem, Inc. Retrieved 16 January 2008.
{{cite web}}: Unknown parameter|month=ignored (help) - ^ "Induction of labour – Evidence-based Clinical Guideline Number 9" (PDF). Royal College of Obstetricians and Gynaecologists. 2001. Archived from the original (PDF) on 30 December 2006. Retrieved 18 January 2008.
- ^ Stovall, M.D., Thomas G. (23 March 2004). "Postdate Pregnancy". Durham Obstetrics and Gynecology. Durham Obstetrics and Gynecology. Retrieved 18 January 2008. [dead link]
- ^ "Nonmedically Indicated Early-Term Deliveries". American College of Obstetricians and Gynecologists. 2013. Retrieved 24 March 2013.
- ^ "Doctors To Pregnant Women: Wait At Least 39 Weeks". 18 July 2011. Retrieved 20 August 2011.
- ^ "Definition of Premature birth". Medicine.net. Retrieved 16 January 2008.
- ^ Lama Rimawi, MD (22 September 2006). "Premature Infant". Disease & Conditions Encyclopedia. Discovery Communications, LLC. Retrieved 16 January 2008.
- ^ WHO | Early skin-to-skin contact for mothers and their healthy newborn infants
- ^ Jenkins, A (July 2011). "Denial of pregnancy: a literature review and discussion of ethical and legal issues". Journal of the Royal Society of Medicine. 104 (7): 286–91. doi:10.1258/jrsm.2011.100376. PMID 21725094.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Gabbe, Steven. Obstetrics : normal and problem pregnancies (6th ed.). Philadelphia: Elsevier/Saunders. p. 1184. ISBN 9781437719352.
- ^ "Pregnancy Symptoms". National Health Service (NHS). 11 March 2010. Retrieved 11 March 2010.
- ^ a b "Early symptoms of pregnancy: What happens right away". Mayo Clinic. 22 February 2007. Retrieved 22 August 2007.
- ^ a b "Pregnancy Symptoms – Early Signs of Pregnancy : American Pregnancy Association". Retrieved 16 January 2008.
- ^ MedlinePlus > Breast pain Update Date: 31 December 2008. Updated by: David C. Dugdale, Susan Storck. Also reviewed by David Zieve.
- ^ "Pregnancy video". Channel 4. 2008. Retrieved 22 January 2009.
- ^ "NHS Pregnancy Planner". National Health Service (NHS). 19 March 2010. Retrieved 19 March 2010.
- ^ Qasim SM, Callan C, Choe JK (1996). "The predictive value of an initial serum beta human chorionic gonadotropin level for pregnancy outcome following in vitro fertilization". Journal of Assisted Reproduction and Genetics. 13 (9): 705–8. doi:10.1007/BF02066422. PMID 8947817.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ "BestBets: Serum or Urine beta-hCG?".
- ^ Verhaegen, J (2012 Sep 27). "Accuracy of single progesterone test to predict early pregnancy outcome in women with pain or bleeding: meta-analysis of cohort studies". BMJ (Clinical research ed.). 345: e6077. doi:10.1136/bmj.e6077. PMC 3460254. PMID 23045257.
{{cite journal}}: Check date values in:|date=(help); Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Whitworth, M (2010 Apr 14). Whitworth, Melissa (ed.). "Ultrasound for fetal assessment in early pregnancy". Cochrane database of systematic reviews (Online) (4): CD007058. doi:10.1002/14651858.CD007058.pub2. PMID 20393955.
{{cite journal}}: Check date values in:|date=(help); Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Nguyen, T.H. (1999). "Evaluation of ultrasound-estimated date of delivery in 17 450 spontaneous singleton births: do we need to modify Naegele's rule?" (abstract). Ultrasound in Obstetrics and Gynecology. 14 (1): 23–28. doi:10.1046/j.1469-0705.1999.14010023.x. PMID 10461334. Retrieved 18 August 2007.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ a b "Screening for Ultrasonography in Pregnancy". U.S. Preventive Services Task Force. Retrieved 6 March 2013.
- ^ Bricker, L (2008 Oct 8). Bricker, Leanne (ed.). "Routine ultrasound in late pregnancy (after 24 weeks' gestation)". Cochrane database of systematic reviews (Online) (4): CD001451. doi:10.1002/14651858.CD001451.pub3. PMID 18843617.
{{cite journal}}: Check date values in:|date=(help); Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Dimitrova V, Markov D, Dimitrov R (2007). "[3D and 4D ultrasonography in obstetrics]". Akush Ginekol (Sofiia) (in Bulgarian). 46 (2): 31–40. PMID 17469450.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Sheiner E, Hackmon R, Shoham-Vardi I; et al. (2007). "A comparison between acoustic output indices in 2D and 3D/4D ultrasound in obstetrics". Ultrasound Obstet Gynecol. 29 (3): 326–8. doi:10.1002/uog.3933. PMID 17265534.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Rados C (January–February 2004). "FDA Cautions Against Ultrasound 'Keepsake' Images". FDA Consumer Magazine. Archived from the original on 13 May 2009. Retrieved 28 February 2012.
- ^ Kempley R (9 August 2003). "The Grin Before They Bear It; Peek-a-Boo: Prenatal Portraits for the Ultrasound Set". Washington Post.
- ^ Klusmann A, Heinrich B, Stöpler H, Gärtner J, Mayatepek E, Von Kries R (2005). "A decreasing rate of neural tube defects following the recommendations for periconceptional folic acid supplementation". Acta Paediatr. 94 (11): 1538–42. doi:10.1080/08035250500340396. PMID 16303691. Retrieved 20 January 2008.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Stevenson RE, Allen WP, Pai GS, Best R, Seaver LH, Dean J, Thompson S (2000). "Decline in prevalence of neural tube defects in a high-risk region of the United States". Pediatrics. 106 (4): 677–83. doi:10.1542/peds.106.4.677. PMID 11015508.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Centers for Disease Control and Prevention (CDC) (2008). "Use of supplements containing folic acid among women of childbearing age—United States, 2007". MMWR Morb. Mortal. Wkly. Rep. 57 (1): 5–8. PMID 18185493.
- ^ Salem N, Jr (September 2001). "Mechanisms of action of docosahexaenoic acid in the nervous system". Lipids. 36 (9): 945–59. doi:10.1007/s11745-001-0805-6. PMID 11724467.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Haider BA, Bhutta ZA (2006). Bhutta, Zulfiqar A (ed.). "Multiple-micronutrient supplementation for women during pregnancy". Cochrane Database Syst Rev (4): CD004905. doi:10.1002/14651858.CD004905.pub2. PMID 17054223.
- ^ Theobald HE (2007). "Eating for pregnancy and breast-feeding". J Fam Health Care. 17 (2): 45–9. PMID 17476978.
- ^ Basile LA, Taylor SN, Wagner CL, Quinones L, Hollis BW (2007). "Neonatal vitamin D status at birth at latitude 32 degrees 72': evidence of deficiency". J Perinatol. 27 (9): 568–71. doi:10.1038/sj.jp.7211796. PMID 17625571.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Kuoppala T, Tuimala R, Parviainen M, Koskinen T, Ala-Houhala M (1986). "Serum levels of vitamin D metabolites, calcium, phosphorus, magnesium and alkaline phosphatase in Finnish women throughout pregnancy and in cord serum at delivery". Hum Nutr Clin Nutr. 40 (4): 287–93. PMID 3488981.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Tarlow, MJ (August 1994). "Epidemiology of neonatal infections". The Journal of antimicrobial chemotherapy. 34 Suppl A: 43–52. PMID 7844073.
- ^ a b c Viswanathan M (2008). "Outcomes of Maternal Weight Gain". Evidence Reports/Technology Assessments, No. 168. Agency for Healthcare Research and Quality. Retrieved 23 June 2013.
{{cite web}}: Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|month=ignored (help) - ^ a b c d Institute for Quality and Efficiency in Health Care. "Weight gain in pregnancy". Fact sheet. Institute for Quality and Efficiency in Health Care. Retrieved 23 June 2013.
- ^ "Weight Gain During Pregnancy: Reexaminging the Guidelines, Report Brief". Institute of Medicine. Retrieved 29 July 2010.
- ^ American College of Obstetricians and Gynecologists (2013). "Weight Gain During Pregnancy". Obstet Gynecol. 121 (1): 210–12. doi:10.1097/01.AOG.0000425668.87506.4c. PMID 23262962.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ a b c d Thangaratinam, S (2012). "Interventions to Reduce or Prevent Obesity in Pregnant Women: A Systematic Review". Health Technology Assessment, No. 16.31. NIHR Evaluation, Trials and Studies Coordinating Centre. Retrieved 23 June 2013.
{{cite web}}: Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|month=ignored (help) - ^ Shaji, Reena (13 January 2009). "Drugs in pregnancy and teratogenicity". LifeHugger.
- ^ Ornoy, A (February 2010). "Alcohol abuse in pregnant women: effects on the fetus and newborn, mode of action and maternal treatment". International journal of environmental research and public health. 7 (2): 364–79. doi:10.3390/ijerph7020364. PMC 2872283. PMID 20616979.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help)CS1 maint: unflagged free DOI (link) - ^ Hackshaw, A (2011 Sep-Oct). "Maternal smoking in pregnancy and birth defects: a systematic review based on 173 687 malformed cases and 11.7 million controls". Human reproduction update. 17 (5): 589–604. doi:10.1093/humupd/dmr022. PMC 3156888. PMID 21747128.
{{cite journal}}: Check date values in:|date=(help); Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Centers for Disease Control and Prevention. 2007. Preventing Smoking and Exposure to Secondhand Smoke Before, During, and After Pregnancy.
- ^ Centers for Disease Control and Prevention. 2009. Tobacco Use and Pregnancy: Home. http://www.cdc.gov/reproductivehealth/tobaccousepregnancy/index.htm
- ^ a b "New Mother Fact Sheet: Methamphetamine Use During Pregnancy". North Dakota Department of Health. Retrieved 7 October 2011.
- ^ Grotta, Sheri (30 June 2009). "Patterns of Methamphetamine Use During Pregnancy: Results from the IDEAL Study". Matern Child Health J. 14 (4): 519–527. doi:10.1007/s10995-009-0491-0. PMC 2895902. PMID 19565330.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Environmental Hazards During Pregnancy Volume 51, No. 1, January/February 2006.
- ^ Sex during pregnancy: What's OK, what's not - MayoClinic.com
- ^ M.P. Bermudez (2001). "Influence of the Gestation Period on Sexual Desire". Psychology in Spain. 5 (1): 14–16.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Wing Yee Fok (2005). "Sexual behavior and activity in Chinese pregnant women". Acta Obstetricia et Gynecologica Scandinavica. 84 (10): 934–938. doi:10.1111/j.0001-6349.2005.00743.x. PMID 16167907.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|month=ignored (help) - ^ Reamy K (1982). "Sexuality and pregnancy. A prospective study". J Reprod Med. 27 (6): 321–7. PMID 7120209.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|month=ignored (help) - ^ Malarewicz A, Szymkiewicz J, Rogala J (2006). "[Sexuality of pregnant women]". Ginekol. Pol. (in Polish). 77 (9): 733–9. PMID 17219804.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Cory Silverberg (19 September 2011). "Pregnancy Sex Positions: ideas for comfortable sex positions during pregnancy". About.com Guide.
- ^ Kramer, MS (19 July 2006). Kramer, Michael S (ed.). "Aerobic exercise for women during pregnancy". Cochrane database of systematic reviews (Online). 3 (3): CD000180. doi:10.1002/14651858.CD000180.pub2. PMID 16855953.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ a b Artal, R (February 2003). "Guidelines of the American College of Obstetricians and Gynecologists for exercise during pregnancy and the postpartum period". British journal of sports medicine. 37 (1): 6–12, discussion 12. doi:10.1136/bjsm.37.1.6. PMC 1724598. PMID 12547738.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Merck. "Urinary tract infections during pregnancy". Merck Manual Home Health Handbook.
- ^ Vazquez, JC (2010 Aug 3). "Constipation, haemorrhoids, and heartburn in pregnancy". Clinical evidence. 2010: 1411. PMC 3217736. PMID 21418682.
{{cite journal}}: Check date values in:|date=(help) - ^ "Reproductive Health and Research Publications: Making Pregnancy Safer". World Health Organization Regional Office for South-East Asia. 2009. Retrieved 7 December 2009.
- ^ Merck. "Pregnancy complicated by disease". Merck Manual, Home Health Handbook. Merck Sharp & Dohme.
- ^ C. Blackwell, Sean (December 2008). "Thromboembolic Disorders During Pregnancy". Merck Sharp & Dohme Corp.
- ^ a b Page 264 in: Gresele, Paolo (2008). Platelets in hematologic and cardiovascular disorders: a clinical handbook. Cambridge, UK: Cambridge University Press. ISBN 0-521-88115-3.
- ^ https://www.cia.gov/library/publications/the-world-factbook/rankorder/2127rank.html
- ^ National Vital Statistics Reports from Centers for Disease Control and Prevention National Center for Health Statistics. Volume 61, Number 1 August 28, 2012: Births: Final Data for 2010
- ^ Womack, Mari (2010). The anthropology of health and healing. Plymouth: AltaMira Press. p. 133. ISBN 978-0-7591-1044-1.
- ^ Rossi, Timothy Verdon ; captions by Filippo (2005). Mary in western art. New York: In Association with Hudson Hills Press. p. 106. ISBN 0-9712981-9-X.
{{cite book}}: CS1 maint: multiple names: authors list (link)
Further reading
- "Nutrition For The First Trimester Of Pregnancy". IDEA Health & Fitness Association. Retrieved 9 December 2013.
- Bothwell, TH (July 2000). "Iron requirements in pregnancy and strategies to meet them". The American journal of clinical nutrition. 72 (1 Suppl): 257S–264S. PMID 10871591.
- O'Brien, KO (February 2006). "Bone calcium turnover during pregnancy and lactation in women with low calcium diets is associated with calcium intake and circulating insulin-like growth factor 1 concentrations1". Am J Clin Nutr. 83 (2): 317–323. PMID 16469990.
External links
- Aparnaji/sandbox at Curlie
- Merck Manual Home Health Handbook – further details on the diseases, disorders, etc., which may complicate pregnancy.
- Pregnancy care planner – NHS guide to having baby including preconception, pregnancy, labor, and birth.


![Embryo at 4 weeks after fertilization[15]](http://upload.wikimedia.org/wikipedia/commons/a/aa/6_weeks_pregnant.png)
![Fetus at 8 weeks after fertilization[16]](http://upload.wikimedia.org/wikipedia/commons/c/c4/10_weeks_pregnant.png)
![Fetus at 18 weeks after fertilization[17]](http://upload.wikimedia.org/wikipedia/commons/3/3f/20_weeks_pregnant.png)
![Fetus at 38 weeks after fertilization[18]](http://upload.wikimedia.org/wikipedia/commons/e/ea/40_weeks_pregnant.png)