Bicalutamide: Difference between revisions
Split content to Pharmacology of bicalutamide. |
|||
| Line 12: | Line 12: | ||
<!--Clinical data--> |
<!--Clinical data--> |
||
| pronounce = Bicalutamide:<br />{{IPAc-en|b|aɪ|k|ə|ˈ|l|uː|t|ə|m|aɪ|d}} {{respell|bye-kə|LOO|tə-myde}}<ref name="(PharmD.)Clark2009">{{cite book |first1=Richard |last1=Finkel |first2=Michelle Alexia |last2=Clark |first3=Luigi X. |last3=Cubeddu | name-list-format = vanc |title=Pharmacology |url=https://books.google.com/books?id=Q4hG2gRhy7oC&pg=PA481 |year=2009 |publisher=Lippincott Williams & Wilkins |isbn=978-0-7817-7155-9 |pages=481–}}</ref><br />Casodex:<br />{{IPAc-en|ˈ|k|eɪ|s|oʊ|d|ɛ|k|s}} {{respell|KAY|soh-deks}}<ref name="SiftonStaff2002">{{cite book |vauthors=Sifton DW, ((PDR Staff)) |title=PDR Drug Guide for Mental Health Professionals |url=https://books.google.com/books?id=Nd9sAAAAMAAJ |year=2002 |publisher=Thomson/PDR |isbn=978-1-56363-457-4}}</ref> |
| pronounce = Bicalutamide:<br />{{IPAc-en|b|aɪ|k|ə|ˈ|l|uː|t|ə|m|aɪ|d}} {{respell|bye-kə|LOO|tə-myde}}<ref name="(PharmD.)Clark2009">{{cite book |first1=Richard |last1=Finkel |first2=Michelle Alexia |last2=Clark |first3=Luigi X. |last3=Cubeddu | name-list-format = vanc |title=Pharmacology |url=https://books.google.com/books?id=Q4hG2gRhy7oC&pg=PA481 |year=2009 |publisher=Lippincott Williams & Wilkins |isbn=978-0-7817-7155-9 |pages=481–}}</ref><br />Casodex:<br />{{IPAc-en|ˈ|k|eɪ|s|oʊ|d|ɛ|k|s}} {{respell|KAY|soh-deks}}<ref name="SiftonStaff2002">{{cite book |vauthors=Sifton DW, ((PDR Staff)) |title=PDR Drug Guide for Mental Health Professionals |url=https://books.google.com/books?id=Nd9sAAAAMAAJ |year=2002 |publisher=Thomson/PDR |isbn=978-1-56363-457-4}}</ref> |
||
| tradename = Casodex |
| tradename = Casodex, others |
||
| Drugs.com = {{drugs.com|monograph|bicalutamide}} |
| Drugs.com = {{drugs.com|monograph|bicalutamide}} |
||
| MedlinePlus = a697047 |
| MedlinePlus = a697047 |
||
| Line 104: | Line 104: | ||
===Available forms=== |
===Available forms=== |
||
[[File:Bicalutamide Teva 50 mg tablets.jpg|thumb|right|230px|Bicalutamide [[Teva Pharmaceutical Industries|Teva]] 50 mg tablets.<ref>{{cite web |url=https://www.tevagenerics.com/product/bicalutamide-tablets-usp |title=Bicalutamide Tablets, USP |publisher=Teva Pharmaceuticals USA, Inc. |deadurl=no |archiveurl=https://web.archive.org/web/20160917110946/https://www.tevagenerics.com/product/bicalutamide-tablets-usp |archivedate=17 September 2016 |df=dmy-all}}</ref>]] |
<!--[[File:Bicalutamide Teva 50 mg tablets.jpg|thumb|right|230px|Bicalutamide [[Teva Pharmaceutical Industries|Teva]] 50 mg tablets.<ref>{{cite web |url=https://www.tevagenerics.com/product/bicalutamide-tablets-usp |title=Bicalutamide Tablets, USP |publisher=Teva Pharmaceuticals USA, Inc. |deadurl=no |archiveurl=https://web.archive.org/web/20160917110946/https://www.tevagenerics.com/product/bicalutamide-tablets-usp |archivedate=17 September 2016 |df=dmy-all}}</ref>]] |
||
--> |
|||
Bicalutamide is available for the treatment of prostate cancer in most developed countries,<ref name="IndexNominum2000">{{cite book |editor=Swiss Pharmaceutical Society |title=Index Nominum 2000: International Drug Directory |url=https://books.google.com/books?id=5GpcTQD_L2oC&pg=PA123 |date=January 2000 |publisher=Taylor & Francis |isbn=978-3-88763-075-1 |pages=123– |deadurl=no |archiveurl=https://web.archive.org/web/20160424054101/https://books.google.com/books?id=5GpcTQD_L2oC&pg=PA123 |archivedate=24 April 2016 |df=dmy-all}}</ref><ref name="Drugs.com-2">{{cite web |title=Bicalutamide – International Drug Names |url=https://www.drugs.com/international/bicalutamide.html |publisher=Drugs.com |accessdate=13 August 2016 |deadurl=no |archiveurl=https://web.archive.org/web/20160918143637/https://www.drugs.com/international/bicalutamide.html |archivedate=18 September 2016 |df=dmy-all}}</ref><ref name="Martindale2011">{{cite book |first=Sean C. |last=Sweetman | name-list-format = vanc |title=Martindale: The Complete Drug Reference |url=https://books.google.com/books?id=r_qfcQAACAAJ |year=2011 |publisher=Pharmaceutical Press |isbn=978-0-85369-933-0 |pages=750–751}}</ref> including over 80 countries worldwide.<ref name=Ak1999>{{cite journal |vauthors=Akaza H |title=[A new anti-androgen, bicalutamide (Casodex), for the treatment of prostate cancer—basic clinical aspects] |language=Japanese |journal=Gan to Kagaku Ryoho. Cancer & Chemotherapy |volume=26 |issue=8 |pages=1201–7 |year=1999 |pmid=10431591 |doi= |url=}}</ref><ref name="AstraZeneca1999">{{cite web |title=1999 Annual Report and Form 20-F |url=https://ddd.uab.cat/pub/infanu/40172/iaASTZENa1999ieng.pdf |publisher=AstraZeneca |accessdate=1 July 2017}}</ref> Bicalutamide is available in 50 mg, 80 mg (in Japan),<ref name="SuzukiKamiya2008">{{cite journal |vauthors=Suzuki H, Kamiya N, Imamoto T, Kawamura K, Yano M, Takano M, Utsumi T, Naya Y, Ichikawa T |title=Current topics and perspectives relating to hormone therapy for prostate cancer |journal=International Journal of Clinical Oncology |volume=13 |issue=5 |pages=401–10 |date=October 2008 |pmid=18946750 |doi=10.1007/s10147-008-0830-y}}</ref> and 150 mg tablets for [[oral administration]].<ref name="WhiteBradnam2015">{{cite book |first1=Rebecca |last1=White |first2=Vicky |last2=Bradnam | name-list-format = vanc |title=Handbook of Drug Administration via Enteral Feeding Tubes |edition=3rd |url=https://books.google.com/books?id=yyikBwAAQBAJ&pg=PA133 |date=11 March 2015 |publisher=Pharmaceutical Press |isbn=978-0-85711-162-3 |pages=133–}}</ref><ref name="MortonHall2001">{{cite book |first1=Ian |last1=Morton |first2=Judith |last2=Hall | name-list-format = vanc |title=The Avery Complete Guide to Medicines |url=https://books.google.com/books?id=0MlN61X5ogkC&focus=searchwithinvolume&q=bicalutamide |year=2001 |publisher=Avery |isbn=978-1-58333-105-7 |pages=105–106}}</ref> The drug is registered for use as a 150 mg/day monotherapy for the treatment of {{abbr|LAPC|locally advanced prostate cancer}} in at least 55 countries,<ref name="Cockshott2004" /> with the {{abbr|U.S.|United States}} being a notable exception where it is registered only for use at a dosage of 50 mg/day in combination with castration.<ref name="ChabnerLongo2010">{{cite book |first1=Bruce A. |last1=Chabner |first2=Dan L. |last2=Longo | name-list-format = vanc |title=Cancer Chemotherapy and Biotherapy: Principles and Practice |url=https://books.google.com/books?id=WL4arNFsQa8C&pg=PA680 |date=8 November 2010 |publisher=Lippincott Williams & Wilkins |isbn=978-1-60547-431-1 |pages=679–680 |quote=From a structural standpoint, antiandrogens are classified as steroidal, including cyproterone [acetate] (Androcur) and megestrol [acetate], or nonsteroidal, including flutamide (Eulexin, others), bicalutamide (Casodex), and nilutamide (Nilandron). The steroidal antiandrogens are rarely used.}}</ref> No other [[pharmaceutical formulation|formulations]] or [[routes of administration]] are available or used.<ref name="WhiteBradnam2015" /> All formulations of bicalutamide are specifically indicated for the treatment of prostate cancer alone or in combination with surgical or medication castration.<ref name="LemkeWilliams2008" /> A [[combination drug|combined formulation]] of bicalutamide and the [[GnRH agonist|{{abbr|GnRH|gonadotropin-releasing hormone}} agonist]] [[goserelin]] in which goserelin is provided as a [[subcutaneous tissue|subcutaneous]] [[implant (medicine)|implant]] for [[injection (medicine)|injection]] and bicalutamide is included as 50 mg tablets for oral ingestion is marketed in Australia and [[New Zealand]] under the brand name ZolaCos CP (Zoladex–Cosudex Combination Pack).<ref name="Martindale2011" /><ref name="Drugs.com-3">{{cite web |title=Zolacos CP |url=https://www.drugs.com/international/zolacos-cp.html |work=Drugs.com |deadurl=no |archiveurl=https://web.archive.org/web/20160920130215/https://www.drugs.com/international/zolacos-cp.html |archivedate=20 September 2016 |df=dmy-all}}</ref><ref name="ZolacosCPLabelAu">{{cite web |title=Zolacos CP | archive-url = https://web.archive.org/web/20160917215734/https://www.betterhealth.vic.gov.au/~/media/bhc/files/medicine%20guides%20library/07/cmi7435.pdf |url=https://www.betterhealth.vic.gov.au/~/media/bhc/files/medicine%20guides%20library/07/cmi7435.pdf |archive-date=17 September 2016 | dead-url = yes |publisher=MIMS/myDr |date=April 2007}}</ref><ref name="ZolacosCPLabelNZ">{{cite web |url=http://www.medsafe.govt.nz/profs/datasheet/z/ZolaCosCP.pdf |title=ZOLACOS CP |work=New Zealand Data Sheet |date=25 July 2016 |deadurl=no |archiveurl=https://web.archive.org/web/20160919034509/http://www.medsafe.govt.nz/profs/datasheet/z/ZolaCosCP.pdf |archivedate=19 September 2016 |df=dmy-all}}</ref> |
Bicalutamide is available for the treatment of prostate cancer in most developed countries,<ref name="IndexNominum2000">{{cite book |editor=Swiss Pharmaceutical Society |title=Index Nominum 2000: International Drug Directory |url=https://books.google.com/books?id=5GpcTQD_L2oC&pg=PA123 |date=January 2000 |publisher=Taylor & Francis |isbn=978-3-88763-075-1 |pages=123– |deadurl=no |archiveurl=https://web.archive.org/web/20160424054101/https://books.google.com/books?id=5GpcTQD_L2oC&pg=PA123 |archivedate=24 April 2016 |df=dmy-all}}</ref><ref name="Drugs.com-2">{{cite web |title=Bicalutamide – International Drug Names |url=https://www.drugs.com/international/bicalutamide.html |publisher=Drugs.com |accessdate=13 August 2016 |deadurl=no |archiveurl=https://web.archive.org/web/20160918143637/https://www.drugs.com/international/bicalutamide.html |archivedate=18 September 2016 |df=dmy-all}}</ref><ref name="Martindale2011">{{cite book |first=Sean C. |last=Sweetman | name-list-format = vanc |title=Martindale: The Complete Drug Reference |url=https://books.google.com/books?id=r_qfcQAACAAJ |year=2011 |publisher=Pharmaceutical Press |isbn=978-0-85369-933-0 |pages=750–751}}</ref> including over 80 countries worldwide.<ref name=Ak1999>{{cite journal |vauthors=Akaza H |title=[A new anti-androgen, bicalutamide (Casodex), for the treatment of prostate cancer—basic clinical aspects] |language=Japanese |journal=Gan to Kagaku Ryoho. Cancer & Chemotherapy |volume=26 |issue=8 |pages=1201–7 |year=1999 |pmid=10431591 |doi= |url=}}</ref><ref name="AstraZeneca1999">{{cite web |title=1999 Annual Report and Form 20-F |url=https://ddd.uab.cat/pub/infanu/40172/iaASTZENa1999ieng.pdf |publisher=AstraZeneca |accessdate=1 July 2017}}</ref> Bicalutamide is available in 50 mg, 80 mg (in Japan),<ref name="SuzukiKamiya2008">{{cite journal |vauthors=Suzuki H, Kamiya N, Imamoto T, Kawamura K, Yano M, Takano M, Utsumi T, Naya Y, Ichikawa T |title=Current topics and perspectives relating to hormone therapy for prostate cancer |journal=International Journal of Clinical Oncology |volume=13 |issue=5 |pages=401–10 |date=October 2008 |pmid=18946750 |doi=10.1007/s10147-008-0830-y}}</ref> and 150 mg tablets for [[oral administration]].<ref name="WhiteBradnam2015">{{cite book |first1=Rebecca |last1=White |first2=Vicky |last2=Bradnam | name-list-format = vanc |title=Handbook of Drug Administration via Enteral Feeding Tubes |edition=3rd |url=https://books.google.com/books?id=yyikBwAAQBAJ&pg=PA133 |date=11 March 2015 |publisher=Pharmaceutical Press |isbn=978-0-85711-162-3 |pages=133–}}</ref><ref name="MortonHall2001">{{cite book |first1=Ian |last1=Morton |first2=Judith |last2=Hall | name-list-format = vanc |title=The Avery Complete Guide to Medicines |url=https://books.google.com/books?id=0MlN61X5ogkC&focus=searchwithinvolume&q=bicalutamide |year=2001 |publisher=Avery |isbn=978-1-58333-105-7 |pages=105–106}}</ref> The drug is registered for use as a 150 mg/day monotherapy for the treatment of {{abbr|LAPC|locally advanced prostate cancer}} in at least 55 countries,<ref name="Cockshott2004" /> with the {{abbr|U.S.|United States}} being a notable exception where it is registered only for use at a dosage of 50 mg/day in combination with castration.<ref name="ChabnerLongo2010">{{cite book |first1=Bruce A. |last1=Chabner |first2=Dan L. |last2=Longo | name-list-format = vanc |title=Cancer Chemotherapy and Biotherapy: Principles and Practice |url=https://books.google.com/books?id=WL4arNFsQa8C&pg=PA680 |date=8 November 2010 |publisher=Lippincott Williams & Wilkins |isbn=978-1-60547-431-1 |pages=679–680 |quote=From a structural standpoint, antiandrogens are classified as steroidal, including cyproterone [acetate] (Androcur) and megestrol [acetate], or nonsteroidal, including flutamide (Eulexin, others), bicalutamide (Casodex), and nilutamide (Nilandron). The steroidal antiandrogens are rarely used.}}</ref> No other [[pharmaceutical formulation|formulations]] or [[routes of administration]] are available or used.<ref name="WhiteBradnam2015" /> All formulations of bicalutamide are specifically indicated for the treatment of prostate cancer alone or in combination with surgical or medication castration.<ref name="LemkeWilliams2008" /> A [[combination drug|combined formulation]] of bicalutamide and the [[GnRH agonist|{{abbr|GnRH|gonadotropin-releasing hormone}} agonist]] [[goserelin]] in which goserelin is provided as a [[subcutaneous tissue|subcutaneous]] [[implant (medicine)|implant]] for [[injection (medicine)|injection]] and bicalutamide is included as 50 mg tablets for oral ingestion is marketed in Australia and [[New Zealand]] under the brand name ZolaCos CP (Zoladex–Cosudex Combination Pack).<ref name="Martindale2011" /><ref name="Drugs.com-3">{{cite web |title=Zolacos CP |url=https://www.drugs.com/international/zolacos-cp.html |work=Drugs.com |deadurl=no |archiveurl=https://web.archive.org/web/20160920130215/https://www.drugs.com/international/zolacos-cp.html |archivedate=20 September 2016 |df=dmy-all}}</ref><ref name="ZolacosCPLabelAu">{{cite web |title=Zolacos CP | archive-url = https://web.archive.org/web/20160917215734/https://www.betterhealth.vic.gov.au/~/media/bhc/files/medicine%20guides%20library/07/cmi7435.pdf |url=https://www.betterhealth.vic.gov.au/~/media/bhc/files/medicine%20guides%20library/07/cmi7435.pdf |archive-date=17 September 2016 | dead-url = yes |publisher=MIMS/myDr |date=April 2007}}</ref><ref name="ZolacosCPLabelNZ">{{cite web |url=http://www.medsafe.govt.nz/profs/datasheet/z/ZolaCosCP.pdf |title=ZOLACOS CP |work=New Zealand Data Sheet |date=25 July 2016 |deadurl=no |archiveurl=https://web.archive.org/web/20160919034509/http://www.medsafe.govt.nz/profs/datasheet/z/ZolaCosCP.pdf |archivedate=19 September 2016 |df=dmy-all}}</ref> |
||
==Contraindications== |
==Contraindications== |
||
In individuals with severe, though not mild-to-moderate [[hepatic impairment]], there is evidence that the elimination of bicalutamide is slowed, and hence, caution may be warranted in these patients as circulating levels of bicalutamide may be increased.<ref name="Cockshott2004" /><ref name="SkeelKhleif2011">{{cite book |first1=Roland T. |last1=Skeel |first2=Samir N. |last2=Khleif |name-list-format=vanc |title=Handbook of Cancer Chemotherapy |url=https://books.google.com/books?id=6Nz_87OLrtcC&pg=PA724 |year=2011 |publisher=Lippincott Williams & Wilkins |pages=724– |deadurl=no |archiveurl=https://web.archive.org/web/20160529144852/https://books.google.com/books?id=6Nz_87OLrtcC&pg=PA724 |archivedate=29 May 2016 |df=dmy-all}}</ref> In severe hepatic impairment, the elimination half-life of the active (''R'')-[[enantiomer]] of bicalutamide is increased by about 1.75-fold (76% increase; elimination half-life of 5.9 and 10.4 days for normal and impaired patients, respectively).<ref name="Wellington2006" /><ref>{{cite book |title=Mosby's GenRx: A Comprehensive Reference for Generic and Brand Prescription Drugs |url=https://books.google.com/books?id=QxsobYYgm8oC |year=2001 |publisher=Mosby |isbn=978-0-323-00629-3 |pages=289–290}}</ref><ref name="PDR2004">{{cite book |first=Thomson |last=PDR | name-list-format = vanc |title=Physicians' Desk Reference |url=https://books.google.com/books?id=_sf2G6ZPDKAC |year=2004 |publisher=Thomson PDR |isbn=978-1-56363-471-0}}</ref> The elimination half-life of bicalutamide is unchanged in [[renal impairment]].<ref name="ChabnerLongo2010" /> |
|||
===Hepatic impairment=== |
|||
In individuals with severe, though not mild-to-moderate [[hepatic impairment]], there is evidence that the elimination of bicalutamide is slowed, and hence, caution may be warranted in these patients.<ref name="Cockshott2004" /><ref name="SkeelKhleif2011">{{cite book |first1=Roland T. |last1=Skeel |first2=Samir N. |last2=Khleif |name-list-format=vanc |title=Handbook of Cancer Chemotherapy |url=https://books.google.com/books?id=6Nz_87OLrtcC&pg=PA724 |year=2011 |publisher=Lippincott Williams & Wilkins |pages=724– |deadurl=no |archiveurl=https://web.archive.org/web/20160529144852/https://books.google.com/books?id=6Nz_87OLrtcC&pg=PA724 |archivedate=29 May 2016 |df=dmy-all}}</ref> In severe hepatic impairment, the elimination half-life of the active (''R'')-[[enantiomer]] of bicalutamide is increased by about 1.75-fold (76% increase; elimination half-life of 5.9 and 10.4 days for normal and impaired patients, respectively).<ref name="Wellington2006" /><ref>{{cite book |title=Mosby's GenRx: A Comprehensive Reference for Generic and Brand Prescription Drugs |url=https://books.google.com/books?id=QxsobYYgm8oC |year=2001 |publisher=Mosby |isbn=978-0-323-00629-3 |pages=289–290}}</ref><ref name="PDR2004">{{cite book |first=Thomson |last=PDR | name-list-format = vanc |title=Physicians' Desk Reference |url=https://books.google.com/books?id=_sf2G6ZPDKAC |year=2004 |publisher=Thomson PDR |isbn=978-1-56363-471-0}}</ref> The elimination half-life of bicalutamide is unchanged in [[renal impairment]].<ref name="ChabnerLongo2010" /> |
|||
===Pregnancy and breastfeeding=== |
|||
Bicalutamide is [[Pregnancy category#United States|pregnancy category X]], or "contraindicated in pregnancy", in the {{abbr|U.S.|United States}},<ref name="FDALabel" /> and [[Pregnancy category#Australia|pregnancy category D]], the second most restricted rating, in Australia.<ref name="TGALabel" /> As such, it is contraindicated in women during pregnancy, and women who are sexually active and who can or may become pregnant are strongly recommended to take bicalutamide only in combination with adequate [[contraception]].<ref name="IswaranImai1997" /><ref name="Smith2013" /> It is unknown whether bicalutamide is excreted in [[breast milk]], but many drugs are excreted in breast milk, and for this reason, bicalutamide treatment is similarly not recommended while [[breastfeeding]].<ref name="Dart2004" /><ref name="FDALabel" /> |
Bicalutamide is [[Pregnancy category#United States|pregnancy category X]], or "contraindicated in pregnancy", in the {{abbr|U.S.|United States}},<ref name="FDALabel" /> and [[Pregnancy category#Australia|pregnancy category D]], the second most restricted rating, in Australia.<ref name="TGALabel" /> As such, it is contraindicated in women during pregnancy, and women who are sexually active and who can or may become pregnant are strongly recommended to take bicalutamide only in combination with adequate [[contraception]].<ref name="IswaranImai1997" /><ref name="Smith2013" /> It is unknown whether bicalutamide is excreted in [[breast milk]], but many drugs are excreted in breast milk, and for this reason, bicalutamide treatment is similarly not recommended while [[breastfeeding]].<ref name="Dart2004" /><ref name="FDALabel" /> |
||
Because bicalutamide blocks the {{abbr|AR|androgen receptor}}, like all antiandrogens, it can interfere with the androgen-mediated [[sexual differentiation]] of the [[genitalia]] (and brain) during [[prenatal development]].<ref name="IswaranImai1997">{{cite journal |vauthors=Iswaran TJ, Imai M, Betton GR, Siddall RA |title=An overview of animal toxicology studies with bicalutamide (ICI 176,334) |journal=The Journal of Toxicological Sciences |volume=22 |issue=2 |pages=75–88 |date=May 1997 |pmid=9198005 |doi=10.2131/jts.22.2_75}}</ref><ref name="Smith2013">{{cite book |first1=Robert E. |last1=Smith |name-list-format=vanc |title=Medicinal Chemistry – Fusion of Traditional and Western Medicine |url=https://books.google.com/books?id=RkDcAwAAQBAJ&pg=PA306 |date=4 April 2013 |publisher=Bentham Science Publishers |isbn=978-1-60805-149-6 |pages=306– |deadurl=no |archiveurl=https://web.archive.org/web/20160529034219/https://books.google.com/books?id=RkDcAwAAQBAJ&pg=PA306 |archivedate=29 May 2016 |df=dmy-all}}</ref><ref>{{cite book |title=Sex Differences in the Human Brain, their underpinnings and implications |url=https://books.google.com/books?id=JFpq6hYQRhQC&pg=PA44 |date=3 December 2010 |publisher=Elsevier |isbn=978-0-444-53631-0 |pages=44–45 |deadurl=no |archiveurl=https://web.archive.org/web/20160526221656/https://books.google.com/books?id=JFpq6hYQRhQC |archivedate=26 May 2016 |df=dmy-all}}</ref><ref name="Paoletti2012">{{cite book |first=Rodolfo |last=Paoletti | name-list-format = vanc |title=Chemistry and Brain Development: Proceedings of the Advanced Study Institute on “Chemistry of Brain Development,” held in Milan, Italy, September 9–19, 1970 |url=https://books.google.com/books?id=8YbgBwAAQBAJ&pg=PA218 |date=6 December 2012 |publisher=Springer Science & Business Media |isbn=978-1-4684-7236-3 |pages=218–}}</ref> In pregnant rats given bicalutamide at a dosage of 10 mg/kg/day (resulting in circulating drug levels approximately equivalent to two-thirds of human therapeutic concentrations) and above, feminization of male offspring, such as reduced [[anogenital distance]] and [[hypospadias]], as well as impotence, were observed.<ref name="FDALabel" /> No other teratogenic effects were observed in rats or rabbits receiving up to very high dosages of bicalutamide (that corresponded to up to approximately two times human therapeutic levels), and no [[teratogen]]ic effects of any sort were observed in female rat offspring at any dosage.<ref name="FDALabel" /> As such, bicalutamide is a selective reproductive teratogen in males, and may have the potential to produce [[undervirilization]]/sexually [[ambiguous genitalia]] in male [[fetus]]es.<ref name="IswaranImai1997" /><ref name="Smith2013" /> |
|||
==Side effects== |
==Side effects== |
||
{{Main|Side effects of bicalutamide}} |
{{Main|Side effects of bicalutamide}} |
||
The [[side effect]] profile of bicalutamide is highly dependent on sex; that is, on whether the person is male or female. In men, due to [[hypoandrogenism|androgen deprivation]], a variety of side effects of varying severity may occur during bicalutamide treatment, with [[mastodynia|breast pain/tenderness]] and [[gynecomastia]] ([[breast development]]/[[mammoplasia|enlargement]]) being the most common.<ref name="Lehne2013">{{cite book |first=Richard A. |last=Lehne | name-list-format = vanc |title=Pharmacology for Nursing Care |url=https://books.google.com/books?id=_4SwO2dHcAIC&pg=PA1297 |year=2013 |publisher=Elsevier Health Sciences |isbn=1-4377-3582-7 |pages=1297–}}</ref><ref name="WirthHakenberg2007">{{cite journal |vauthors=Wirth MP, Hakenberg OW, Froehner M |title=Antiandrogens in the treatment of prostate cancer |journal=European Urology |volume=51 |issue=2 |pages=306–13; discussion 314 |date=February 2007 |pmid=17007995 |doi=10.1016/j.eururo.2006.08.043}}</ref> In addition breast changes, physical [[feminization (biology)|feminization]] and [[demasculinization]] in general, including reduced [[body hair]] growth, decreased [[muscle mass]] and [[muscle strength|strength]], [[gynoid fat distribution|feminine]] changes in [[body fat percentage|fat mass]] and [[fat distribution|distribution]], and reduced [[human penis size|penile length]], may also occur in men.<ref name="Lehne2013" /><ref name="Higano2003">{{cite journal |vauthors=Higano CS |title=Side effects of androgen deprivation therapy: monitoring and minimizing toxicity |journal=Urology |volume=61 |issue=2 Suppl 1 |pages=32–8 |date=February 2003 |pmid=12667885 |doi=10.1016/S0090-4295(02)02397-X}}</ref><ref name="pmid20626600" /><ref name="pmid23008326">{{cite journal |vauthors=Higano CS |title=Sexuality and intimacy after definitive treatment and subsequent androgen deprivation therapy for prostate cancer |journal=Journal of Clinical Oncology |volume=30 |issue=30 |pages=3720–5 |year=2012 |pmid=23008326 |doi=10.1200/JCO.2012.41.8509 |url=}}</ref> Other side effects that have been observed in men and that are similarly related to androgen deprivation include [[hot flash]]es, [[sexual dysfunction]] (e.g., loss of [[libido]], [[erectile dysfunction]]), depression, [[fatigue (medical)|fatigue]], [[weakness]], [[anemia]], and decreased [[Ejaculation#Volume|semen/ejaculate volume]].<ref name="Lehne2013" /><ref name="Kolvenbag1996">{{cite journal |vauthors=Kolvenbag GJ, Blackledge GR |title=Worldwide activity and safety of bicalutamide: a summary review |journal=Urology |volume=47 |issue=1A Suppl |pages=70–9; discussion 80–4 |date=January 1996 |pmid=8560681 |doi= 10.1016/s0090-4295(96)80012-4|quote=Bicalutamide is a new antiandrogen that offers the convenience of once-daily administration, demonstrated activity in prostate cancer, and an excellent safety profile. Because it is effective and offers better tolerability than flutamide, bicalutamide represents a valid first choice for antiandrogen therapy in combination with castration for the treatment of patients with advanced prostate cancer.}}</ref><ref name="ResnickThompson2000">{{cite book |first1=Martin I. |last1=Resnick |first2=Ian Murchie |last2=Thompson |name-list-format=vanc |title=Advanced Therapy of Prostate Disease |url=https://books.google.com/books?id=9AKuf7rzfjcC&pg=PA379 |year=2000 |publisher=PMPH-USA |isbn=978-1-55009-102-1 |pages=379– |deadurl=no |archiveurl=https://web.archive.org/web/20160610095331/https://books.google.com/books?id=9AKuf7rzfjcC&pg=PA379 |archivedate=10 June 2016 |df=dmy-all}}</ref> In women, on the other hand, due to the little biological importance of androgens in this sex,<ref name="pmid28343552">{{cite journal |vauthors=Kathryn Korkidakis A, Reid RL |title=Testosterone in Women: Measurement and Therapeutic Use |journal=Journal of Obstetrics and Gynaecology Canada |volume=39 |issue=3 |pages=124–130 |year=2017 |pmid=28343552 |doi=10.1016/j.jogc.2017.01.006 |url=}}</ref><ref name="pmid26358173">{{cite journal |vauthors=Davis SR, Wahlin-Jacobsen S |title=Testosterone in women--the clinical significance |journal=The Lancet Diabetes & Endocrinology |volume=3 |issue=12 |pages=980–92 |year=2015 |pmid=26358173 |doi=10.1016/S2213-8587(15)00284-3 |url=}}</ref> the side effects of pure antiandrogens or {{abbr|NSAAs|nonsteroidal antiandrogens}} are minimal, and bicalutamide has been found to be very well-tolerated.<ref name="Shapiro2012" /> General side effects of bicalutamide that may occur in either sex include [[diarrhea]], [[constipation]], [[abdominal pain]], [[nausea]], [[dry skin]],<ref name="JamnickyNam2012">{{cite book |first1=Leah |last1=Jamnicky |first2=Robert |last2=Nam | name-list-format = vanc |title=Canadian Guide to Prostate Cancer |url=https://books.google.com/books?id=EFJhvLJeWX4C&pg=PT177 |date=5 November 2012 |publisher=John Wiley & Sons |isbn=978-1-118-51565-5 |pages=177–}}</ref> [[pruritus|itching]], and [[rash]].<ref name="Kolvenbag1996" /><ref name="Dart2004" /><ref name="pmid7579554">{{cite journal |vauthors=Lunglmayr G |title=Efficacy and tolerability of Casodex in patients with advanced prostate cancer. International Casodex Study Group |journal=Anti-Cancer Drugs |volume=6 |issue=4 |pages=508–13 |date=August 1995 |pmid=7579554 |doi=10.1097/00001813-199508000-00003}}</ref><ref name="pmid10388026">{{cite journal |vauthors=McLeod DG |title=Tolerability of Nonsteroidal Antiandrogens in the Treatment of Advanced Prostate Cancer |journal=The Oncologist |volume=2 |issue=1 |pages=18–27 |year=1997 |pmid=10388026 |doi=}}</ref><ref name="MDMD2008">{{cite book |first1=Lisa M |last1=DeAngelis |first2=Jerome B |last2=Posner |name-list-format=vanc |title=Neurologic Complications of Cancer |url=https://books.google.com/books?id=mpZ8Dp2KdHMC&pg=PA479 |date=12 September 2008 |publisher=Oxford University Press, USA |isbn=978-0-19-971055-3 |pages=479– |deadurl=no |archiveurl=https://web.archive.org/web/20160507051525/https://books.google.com/books?id=mpZ8Dp2KdHMC&pg=PA479 |archivedate=7 May 2016 |df=dmy-all}}</ref> The drug is well-tolerated at higher dosages than the 50 mg/day dosage, with rare additional side effects.<ref name="ChabnerLongo2010" /> |
The [[side effect]] profile of bicalutamide is highly dependent on sex; that is, on whether the person is male or female. In men, due to [[hypoandrogenism|androgen deprivation]], a variety of side effects of varying severity may occur during bicalutamide treatment, with [[mastodynia|breast pain/tenderness]] and [[gynecomastia]] ([[breast development]]/[[mammoplasia|enlargement]]) being the most common.<ref name="Lehne2013">{{cite book |first=Richard A. |last=Lehne | name-list-format = vanc |title=Pharmacology for Nursing Care |url=https://books.google.com/books?id=_4SwO2dHcAIC&pg=PA1297 |year=2013 |publisher=Elsevier Health Sciences |isbn=1-4377-3582-7 |pages=1297–}}</ref><ref name="WirthHakenberg2007">{{cite journal |vauthors=Wirth MP, Hakenberg OW, Froehner M |title=Antiandrogens in the treatment of prostate cancer |journal=European Urology |volume=51 |issue=2 |pages=306–13; discussion 314 |date=February 2007 |pmid=17007995 |doi=10.1016/j.eururo.2006.08.043}}</ref> In addition breast changes, physical [[feminization (biology)|feminization]] and [[demasculinization]] in general, including reduced [[body hair]] growth, decreased [[muscle mass]] and [[muscle strength|strength]], [[gynoid fat distribution|feminine]] changes in [[body fat percentage|fat mass]] and [[fat distribution|distribution]], and reduced [[human penis size|penile length]], may also occur in men.<ref name="Lehne2013" /><ref name="Higano2003">{{cite journal |vauthors=Higano CS |title=Side effects of androgen deprivation therapy: monitoring and minimizing toxicity |journal=Urology |volume=61 |issue=2 Suppl 1 |pages=32–8 |date=February 2003 |pmid=12667885 |doi=10.1016/S0090-4295(02)02397-X}}</ref><ref name="pmid20626600" /><ref name="pmid23008326">{{cite journal |vauthors=Higano CS |title=Sexuality and intimacy after definitive treatment and subsequent androgen deprivation therapy for prostate cancer |journal=Journal of Clinical Oncology |volume=30 |issue=30 |pages=3720–5 |year=2012 |pmid=23008326 |doi=10.1200/JCO.2012.41.8509 |url=}}</ref> Other side effects that have been observed in men and that are similarly related to androgen deprivation include [[hot flash]]es, [[sexual dysfunction]] (e.g., loss of [[libido]], [[erectile dysfunction]]), depression, [[fatigue (medical)|fatigue]], [[weakness]], [[anemia]], and decreased [[Ejaculation#Volume|semen/ejaculate volume]].<ref name="Lehne2013" /><ref name="Kolvenbag1996">{{cite journal |vauthors=Kolvenbag GJ, Blackledge GR |title=Worldwide activity and safety of bicalutamide: a summary review |journal=Urology |volume=47 |issue=1A Suppl |pages=70–9; discussion 80–4 |date=January 1996 |pmid=8560681 |doi= 10.1016/s0090-4295(96)80012-4|quote=Bicalutamide is a new antiandrogen that offers the convenience of once-daily administration, demonstrated activity in prostate cancer, and an excellent safety profile. Because it is effective and offers better tolerability than flutamide, bicalutamide represents a valid first choice for antiandrogen therapy in combination with castration for the treatment of patients with advanced prostate cancer.}}</ref><ref name="ResnickThompson2000">{{cite book |first1=Martin I. |last1=Resnick |first2=Ian Murchie |last2=Thompson |name-list-format=vanc |title=Advanced Therapy of Prostate Disease |url=https://books.google.com/books?id=9AKuf7rzfjcC&pg=PA379 |year=2000 |publisher=PMPH-USA |isbn=978-1-55009-102-1 |pages=379– |deadurl=no |archiveurl=https://web.archive.org/web/20160610095331/https://books.google.com/books?id=9AKuf7rzfjcC&pg=PA379 |archivedate=10 June 2016 |df=dmy-all}}</ref> In women, on the other hand, due to the little biological importance of androgens in this sex,<ref name="pmid28343552">{{cite journal |vauthors=Kathryn Korkidakis A, Reid RL |title=Testosterone in Women: Measurement and Therapeutic Use |journal=Journal of Obstetrics and Gynaecology Canada |volume=39 |issue=3 |pages=124–130 |year=2017 |pmid=28343552 |doi=10.1016/j.jogc.2017.01.006 |url=}}</ref><ref name="pmid26358173">{{cite journal |vauthors=Davis SR, Wahlin-Jacobsen S |title=Testosterone in women--the clinical significance |journal=The Lancet Diabetes & Endocrinology |volume=3 |issue=12 |pages=980–92 |year=2015 |pmid=26358173 |doi=10.1016/S2213-8587(15)00284-3 |url=}}</ref> the side effects of pure antiandrogens or {{abbr|NSAAs|nonsteroidal antiandrogens}} are minimal, and bicalutamide has been found to be very well-tolerated.<ref name="Shapiro2012" /> General side effects of bicalutamide that may occur in either sex include [[diarrhea]], [[constipation]], [[abdominal pain]], [[nausea]], [[dry skin]],<ref name="JamnickyNam2012">{{cite book |first1=Leah |last1=Jamnicky |first2=Robert |last2=Nam | name-list-format = vanc |title=Canadian Guide to Prostate Cancer |url=https://books.google.com/books?id=EFJhvLJeWX4C&pg=PT177 |date=5 November 2012 |publisher=John Wiley & Sons |isbn=978-1-118-51565-5 |pages=177–}}</ref> [[pruritus|itching]], and [[rash]].<ref name="Kolvenbag1996" /><ref name="Dart2004" /><ref name="pmid7579554">{{cite journal |vauthors=Lunglmayr G |title=Efficacy and tolerability of Casodex in patients with advanced prostate cancer. International Casodex Study Group |journal=Anti-Cancer Drugs |volume=6 |issue=4 |pages=508–13 |date=August 1995 |pmid=7579554 |doi=10.1097/00001813-199508000-00003}}</ref><ref name="pmid10388026">{{cite journal |vauthors=McLeod DG |title=Tolerability of Nonsteroidal Antiandrogens in the Treatment of Advanced Prostate Cancer |journal=The Oncologist |volume=2 |issue=1 |pages=18–27 |year=1997 |pmid=10388026 |doi=}}</ref><ref name="MDMD2008">{{cite book |first1=Lisa M |last1=DeAngelis |first2=Jerome B |last2=Posner |name-list-format=vanc |title=Neurologic Complications of Cancer |url=https://books.google.com/books?id=mpZ8Dp2KdHMC&pg=PA479 |date=12 September 2008 |publisher=Oxford University Press, USA |isbn=978-0-19-971055-3 |pages=479– |deadurl=no |archiveurl=https://web.archive.org/web/20160507051525/https://books.google.com/books?id=mpZ8Dp2KdHMC&pg=PA479 |archivedate=7 May 2016 |df=dmy-all}}</ref> The drug is well-tolerated at higher dosages than the 50 mg/day dosage, with rare additional side effects.<ref name="ChabnerLongo2010" /> |
||
| Line 130: | Line 126: | ||
==Interactions== |
==Interactions== |
||
===Cytochrome P450 enzymes=== |
|||
Bicalutamide is almost exclusively [[metabolized]] by [[CYP3A4]].<ref name="LemkeWilliams2008" /> As such, its levels in the body may be altered by [[enzyme inhibitor|inhibitors]] and [[enzyme inducer|inducers]] of CYP3A4.<ref name="Skidmore-Roth2013">{{cite book |first=Linda |last=Skidmore-Roth | name-list-format = vanc |title=Mosby's 2014 Nursing Drug Reference – Elsevieron VitalSource |url=https://books.google.com/books?id=ISYiAQAAQBAJ&pg=PA194 |date=17 April 2013 |publisher=Elsevier Health Sciences |isbn=978-0-323-22267-9 |pages=193–194}}</ref> (For a list of CYP3A4 inhibitors and inducers, see [[CYP3A4#CYP3A4 ligands|here]].) However, in spite of the fact bicalutamide is metabolized by CYP3A4, there is no evidence of clinically significant [[drug interaction]]s when bicalutamide at a dosage of 150 mg/day or less is co-administered with drugs that inhibit or induce [[cytochrome P450]] [[enzyme]] activity.<ref name="Wellington2006" /> |
Bicalutamide is almost exclusively [[metabolized]] by [[CYP3A4]].<ref name="LemkeWilliams2008" /> As such, its levels in the body may be altered by [[enzyme inhibitor|inhibitors]] and [[enzyme inducer|inducers]] of CYP3A4.<ref name="Skidmore-Roth2013">{{cite book |first=Linda |last=Skidmore-Roth | name-list-format = vanc |title=Mosby's 2014 Nursing Drug Reference – Elsevieron VitalSource |url=https://books.google.com/books?id=ISYiAQAAQBAJ&pg=PA194 |date=17 April 2013 |publisher=Elsevier Health Sciences |isbn=978-0-323-22267-9 |pages=193–194}}</ref> (For a list of CYP3A4 inhibitors and inducers, see [[CYP3A4#CYP3A4 ligands|here]].) However, in spite of the fact bicalutamide is metabolized by CYP3A4, there is no evidence of clinically significant [[drug interaction]]s when bicalutamide at a dosage of 150 mg/day or less is co-administered with drugs that inhibit or induce [[cytochrome P450]] [[enzyme]] activity.<ref name="Wellington2006" /> |
||
===Plasma binding proteins=== |
|||
Because bicalutamide circulates at relatively high concentrations and is highly protein-bound, it has the potential to displace other highly protein-bound drugs like [[warfarin]], [[phenytoin]], [[theophylline]], and [[aspirin]] from [[binding protein|plasma binding proteins]].<ref name="WirthHakenberg2007" /><ref name="Kolvenbag1996" /> This could, in turn, result in increased free concentrations of such drugs and increased effects and/or side effects, potentially necessitating dosage adjustments.<ref name="WirthHakenberg2007" /> Bicalutamide has specifically been found to displace [[coumarin]] [[anticoagulant]]s like warfarin from their plasma binding proteins (namely [[human serum albumin|albumin]]) ''[[in vitro]]'', potentially resulting in an increased anticoagulant effect, and for this reason, close monitoring of [[prothrombin]] time and dosage adjustment as necessary is recommended when bicalutamide is used in combination with these drugs.<ref name="Weber2015">{{cite book |first=Georg F. |last=Weber | name-list-format = vanc |title=Molecular Therapies of Cancer |url=https://books.google.com/books?id=dhs_CgAAQBAJ&pg=PA318 |date=22 July 2015 |publisher=Springer |isbn=978-3-319-13278-5 |pages=318– |quote=Compared to flutamide and nilutamide, bicalutamide has a 2-fold increased affinity for the Androgen Receptor, a longer half-life, and substantially reduced toxicities. Based on a more favorable safety profile relative to flutamide, bicalutamide is indicated for use in combination therapy with a Gonadotropin Releasing Hormone analog for the treatment of advanced metastatic prostate carcinoma.}}</ref><ref name="Mosby2001">{{cite book |title=Mosby's GenRx: A Comprehensive Reference for Generic and Brand Prescription Drugs |url=https://books.google.com/books?id=QxsobYYgm8oC |year=2001 |publisher=Mosby |isbn=978-0-323-00629-3 |page=290 |quote=In vitro studies have shown bicalutamide can displace coumarin anticoagulants, such as warfarin, from their protein-binding sites. It is recommended that if bicalutamide is started in patients already receiving coumarin anticoagulants, prothrombin times should be closely monitored and adjustment of the anticoagulant dose may be necessary.}}</ref><ref name="SprattoWoods2008">{{cite book |first1=George |last1=Spratto |first2=Adrienne |last2=Woods | name-list-format = vanc |title=2009 Edition Delmar's Nurse's Drug Handbook |url=https://books.google.com/books?id=8MoIHiUja_oC&pg=PA175 |date=2 July 2008 |publisher=Cengage Learning |isbn=1-4283-6106-5 |pages=175–}}</ref> However, in spite of this, no conclusive evidence of an interaction between bicalutamide and other drugs was found in clinical trials of nearly 3,000 patients.<ref name="Kolvenbag1996" /> |
Because bicalutamide circulates at relatively high concentrations and is highly protein-bound, it has the potential to displace other highly protein-bound drugs like [[warfarin]], [[phenytoin]], [[theophylline]], and [[aspirin]] from [[binding protein|plasma binding proteins]].<ref name="WirthHakenberg2007" /><ref name="Kolvenbag1996" /> This could, in turn, result in increased free concentrations of such drugs and increased effects and/or side effects, potentially necessitating dosage adjustments.<ref name="WirthHakenberg2007" /> Bicalutamide has specifically been found to displace [[coumarin]] [[anticoagulant]]s like warfarin from their plasma binding proteins (namely [[human serum albumin|albumin]]) ''[[in vitro]]'', potentially resulting in an increased anticoagulant effect, and for this reason, close monitoring of [[prothrombin]] time and dosage adjustment as necessary is recommended when bicalutamide is used in combination with these drugs.<ref name="Weber2015">{{cite book |first=Georg F. |last=Weber | name-list-format = vanc |title=Molecular Therapies of Cancer |url=https://books.google.com/books?id=dhs_CgAAQBAJ&pg=PA318 |date=22 July 2015 |publisher=Springer |isbn=978-3-319-13278-5 |pages=318– |quote=Compared to flutamide and nilutamide, bicalutamide has a 2-fold increased affinity for the Androgen Receptor, a longer half-life, and substantially reduced toxicities. Based on a more favorable safety profile relative to flutamide, bicalutamide is indicated for use in combination therapy with a Gonadotropin Releasing Hormone analog for the treatment of advanced metastatic prostate carcinoma.}}</ref><ref name="Mosby2001">{{cite book |title=Mosby's GenRx: A Comprehensive Reference for Generic and Brand Prescription Drugs |url=https://books.google.com/books?id=QxsobYYgm8oC |year=2001 |publisher=Mosby |isbn=978-0-323-00629-3 |page=290 |quote=In vitro studies have shown bicalutamide can displace coumarin anticoagulants, such as warfarin, from their protein-binding sites. It is recommended that if bicalutamide is started in patients already receiving coumarin anticoagulants, prothrombin times should be closely monitored and adjustment of the anticoagulant dose may be necessary.}}</ref><ref name="SprattoWoods2008">{{cite book |first1=George |last1=Spratto |first2=Adrienne |last2=Woods | name-list-format = vanc |title=2009 Edition Delmar's Nurse's Drug Handbook |url=https://books.google.com/books?id=8MoIHiUja_oC&pg=PA175 |date=2 July 2008 |publisher=Cengage Learning |isbn=1-4283-6106-5 |pages=175–}}</ref> However, in spite of this, no conclusive evidence of an interaction between bicalutamide and other drugs was found in clinical trials of nearly 3,000 patients.<ref name="Kolvenbag1996" /> |
||
==Pharmacology== |
==Pharmacology== |
||
{{Main|Pharmacology of bicalutamide}} |
|||
===Pharmacodynamics=== |
===Pharmacodynamics=== |
||
====Antiandrogenic activity==== |
====Antiandrogenic activity==== |
||
Bicalutamide acts as a highly [[binding selectivity|selective]] [[competitive antagonist|competitive]] [[silent antagonist|silent]] [[receptor antagonist|antagonist]] of the {{abbr|AR|androgen receptor}} ({{abbrlink|IC<sub>50</sub>|half-maximal inhibitory concentration}} = 159–243 nM), the major [[biological target]] of the [[androgen]] [[sex hormone]]s [[testosterone]] and {{abbrlink|DHT|dihydrotestosterone}}, and hence is an [[antiandrogen]].<ref name="SinghGauthier2000" /><ref name="Balaji2016">{{cite book |first=K.C. |last=Balaj|name-list-format=vanc |title=Managing Metastatic Prostate Cancer In Your Urological Oncology Practice |url=https://books.google.com/books?id=1U4WDAAAQBAJ&pg=PA25 |date=25 April 2016 |publisher=Springer |isbn=978-3-319-31341-2 |pages=24–25 |deadurl=no |archiveurl=https://web.archive.org/web/20170908222331/https://books.google.com/books?id=1U4WDAAAQBAJ&pg=PA25 |archivedate=8 September 2017 |df=dmy-all}}</ref><ref name="MasielloCheng2002">{{cite journal |vauthors=Masiello D, Cheng S, Bubley GJ, Lu ML, Balk SP |title=Bicalutamide functions as an androgen receptor antagonist by assembly of a transcriptionally inactive receptor |journal=The Journal of Biological Chemistry |volume=277 |issue=29 |pages=26321–6 |date=July 2002 |pmid=12015321 |doi=10.1074/jbc.M203310200}}</ref><ref name="Denis2012">{{cite book |first=Louis |last=Denis | name-list-format = vanc |title=Antiandrogens in Prostate Cancer: A Key to Tailored Endocrine Treatment |url=https://books.google.com/books?id=jqZDBQAAQBAJ&pg=PT128 |date=6 December 2012 |publisher=Springer Science & Business Media |isbn=978-3-642-45745-6 |pages=128, 158, 203}}</ref> The [[biological activity|activity]] of bicalutamide lies in the (''R'')-isomer.<ref name="SchellensMcLeod2005" /> Due to its selectivity for the {{abbr|AR|androgen receptor}}, bicalutamide does not bind to other [[steroid hormone receptor]]s and hence has no [[off-target activity|off-target]] hormonal activity (e.g., [[progestogen]]ic, [[glucocorticoid]], [[antimineralocorticoid]]).<ref name="Becker2001">{{cite book |first=Kenneth L. |last=Becker |name-list-format=vanc |title=Principles and Practice of Endocrinology and Metabolism |url=https://books.google.com/books?id=FVfzRvaucq8C&pg=PA1208 |year=2001 |publisher=Lippincott Williams & Wilkins |isbn=978-0-7817-1750-2 |pages=1119, 1196, 1208 |deadurl=no |archiveurl=https://web.archive.org/web/20170908222331/https://books.google.com/books?id=FVfzRvaucq8C&pg=PA1208 |archivedate=8 September 2017 |df=dmy-all}}</ref><ref name="FurrTucker1996">{{cite journal |vauthors=Furr BJ, Tucker H |title=The preclinical development of bicalutamide: pharmacodynamics and mechanism of action |journal=Urology |volume=47 |issue=1A Suppl |pages=13–25; discussion 29–32 |date=January 1996 |pmid=8560673 |doi=10.1016/S0090-4295(96)80003-3}}</ref><ref name="SchellensMcLeod2005">{{cite book |first1=Jan H. M. |last1=Schellens |first2=Howard L. |last2=McLeod |first3=David R. |last3=Newell |name-list-format=vanc |title=Cancer Clinical Pharmacology |url=https://books.google.com/books?id=co8Sgu9N0FMC&pg=PA229 |date=5 May 2005 |publisher=OUP Oxford |isbn=978-0-19-262966-1 |pages=229–230 |deadurl=no |archiveurl=https://web.archive.org/web/20160610134202/https://books.google.com/books?id=co8Sgu9N0FMC&pg=PA229 |archivedate=10 June 2016 |df=dmy-all}}</ref><ref name="BagatellBremner2003">{{cite book |first1=Carrie |last1=Bagatelle |first2=William J. |last2=Bremner | name-list-format = vanc |title=Androgens in Health and Disease |url=https://books.google.com/books?id=vDcBCAAAQBAJ&pg=PA25 |date=27 May 2003 |publisher=Springer Science & Business Media |isbn=978-/.1-59259-388-0 |pages=25–}}</ref> It also does not [[enzyme inhibitor|inhibit]] [[5α-reductase]] nor is known to inhibit other androgen [[steroidogenic]] [[enzyme]]s (e.g., [[CYP17A1]]).<ref name="Furr1995" /> Although it does not bind to the [[estrogen receptor]]s (ERs), bicalutamide can increase [[estrogen]] levels secondary to {{abbr|AR|androgen receptor}} blockade when used as a monotherapy in males, and hence can have some ''indirect'' [[estrogen]]ic effects in males.<ref name="pmid18231613">{{cite journal |vauthors=Guise TA, Oefelein MG, Eastham JA, Cookson MS, Higano CS, Smith MR |title=Estrogenic side effects of androgen deprivation therapy |journal=Reviews in Urology |volume=9 |issue=4 |pages=163–80 |year=2007 |pmid=18231613 |pmc=2213888 |doi=}}</ref> Bicalutamide neither suppresses nor inhibits androgen [[biosynthesis|production]] in the body (i.e., it does not act as an [[antigonadotropin]] or [[androgen steroidogenesis inhibitor]] or lower androgen levels) and hence exclusively mediates its antiandrogenic effects by antagonizing the {{abbr|AR|androgen receptor}}.<ref name="Dart2004" /><ref name="Becker2001" /><ref name="SchellensMcLeod2005" /> In addition to the classical [[nuclear receptor|nuclear]] {{abbr|AR|androgen receptor}}, bicalutamide has been assessed at the [[membrane androgen receptor]]s (mARs) and found to act as a potent antagonist of ZIP9 (IC<sub>50</sub> = 66.3 nM), whereas it does not appear to interact with [[GPRC6A]].<ref name="pmid28943399">{{cite journal | vauthors = Bulldan A, Malviya VN, Upmanyu N, Konrad L, Scheiner-Bobis G | title = Testosterone/bicalutamide antagonism at the predicted extracellular androgen binding site of ZIP9 | journal = Biochim. Biophys. Acta | volume = 1864 | issue = 12 | pages = 2402–2414 | year = 2017 | pmid = 28943399 | doi = 10.1016/j.bbamcr.2017.09.012 | url = }}</ref><ref name="pmid20947496">{{cite journal | vauthors = Pi M, Parrill AL, Quarles LD | title = GPRC6A mediates the non-genomic effects of steroids | journal = J. Biol. Chem. | volume = 285 | issue = 51 | pages = 39953–64 | year = 2010 | pmid = 20947496 | pmc = 3000977 | doi = 10.1074/jbc.M110.158063 | url = }}</ref> |
|||
[[File:W741L AR LBD-R-bicalutamide complex.png|350px|thumb|right|[[Crystal structure]] of W741L (pos. 741, W➞L) [[mutant protein|mutant]] {{abbrlink|AR|androgen receptor}} {{abbrlink|LBD|ligand-binding domain}} and (''R'')-bicalutamide [[protein–ligand complex]].<ref name="pmid15833816" />]] |
|||
The [[affinity (pharmacology)|affinity]] of bicalutamide for the {{abbr|AR|androgen receptor}} is relatively low as it is approximately 50 times lower than that of {{abbr|DHT|dihydrotestosterone}}, which is 2.5- to 10-fold as potent as an {{abbr|AR|androgen receptor}} agonist as testosterone in [[bioassay]]s and is the main [[endogenous]] [[ligand (biochemistry)|ligand]] of the [[receptor (biochemistry)|receptor]] in the [[prostate gland]].<ref name="Furr2009">{{cite journal |vauthors=Furr BJ |title=Research on reproductive medicine in the pharmaceutical industry |journal=Human Fertility |volume=1 |issue=1 |pages=56–63 |year=2009 |pmid=11844311 |doi=10.1080/1464727982000198131}}</ref><ref name="Denis2012" /> However, typical clinical dosages of bicalutamide result in circulating levels of the drug that are thousands of times higher than those of testosterone and {{abbr|DHT|dihydrotestosterone}}, allowing it to efficaciously prevent them from binding to and activating the receptor.<ref name="FiggChau2010" /><ref name="FurrTucker1996" /><ref name="pmid8717469">{{cite journal |vauthors=Furr BJ |title=The development of Casodex (bicalutamide): preclinical studies |journal=European Urology |volume=29 Suppl 2 |issue= |pages=83–95 |year=1996 |pmid=8717469 |doi=}}</ref><ref name="FDALabel" /><ref name="TGALabel" /><ref name="DenisMahler1996" /><ref name="Wellington2006" /><ref name="pmid15838655" /> This is especially true in the case of surgical or medical castration, in which testosterone levels in the circulation are approximately 95% reduced and {{abbr|DHT|dihydrotestosterone}} levels in the prostate gland are about 50 to 60% reduced.<ref name="Denis2012" /><ref name="LuoMartel1997">{{cite journal |vauthors=Luo S, Martel C, Chen C, Labrie C, Candas B, Singh SM, Labrie F |title=Daily dosing with flutamide or Casodex exerts maximal antiandrogenic activity |journal=Urology |volume=50 |issue=6 |pages=913–9 |date=December 1997 |pmid=9426723 |doi=10.1016/S0090-4295(97)00393-2}}</ref> In women, levels of testosterone are substantially lower than in men (20- to 40-fold),<ref name="MelmedPolonsky2015" /> so much smaller doses of bicalutamide (e.g., 25 mg/day in the hirsutism studies) are necessary.<ref name="WilliamsBigby2009" /><ref name="pmid24455796" /><ref name="MorettiGuccione2016">{{cite | title = Efficacy and Safety of Myo-Inositol Supplementation in the Treatment of Obese Hirsute PCOS Women: Comparative Evaluation with OCP+Bicalutamide Therapy | authors = Costanzo Giulio Moretti, Laura Guccione, Paola Di Giacinto, Amalia Cannuccia, Chiara Meleca, Giulia Lanzolla, Aikaterini Andreadi, Davide Lauro | year = 2016 | url = http://press.endocrine.org/doi/abs/10.1210/endo-meetings.2016.RE.5.SUN-153 | doi = 10.1210/endo-meetings.2016.RE.5.SUN-153}}</ref><ref name="MahlerVerhelst1998" /> |
|||
Bicalutamide acts as a highly selective [[competitive antagonist|competitive]] [[silent antagonist]] of the {{abbr|AR|androgen receptor}} ({{abbrlink|IC<sub>50</sub>|half-maximal inhibitory concentration}} = 159–243 nM), the major biological target of the androgen sex hormones testosterone and {{abbr|DHT|dihydrotestosterone}}.<ref name="SinghGauthier2000" /><ref name="Balaji2016">{{cite book |first=K.C. |last=Balaj|name-list-format=vanc |title=Managing Metastatic Prostate Cancer In Your Urological Oncology Practice |url=https://books.google.com/books?id=1U4WDAAAQBAJ&pg=PA25 |date=25 April 2016 |publisher=Springer |isbn=978-3-319-31341-2 |pages=24–25 |deadurl=no |archiveurl=https://web.archive.org/web/20170908222331/https://books.google.com/books?id=1U4WDAAAQBAJ&pg=PA25 |archivedate=8 September 2017 |df=dmy-all}}</ref><ref name="MasielloCheng2002">{{cite journal |vauthors=Masiello D, Cheng S, Bubley GJ, Lu ML, Balk SP |title=Bicalutamide functions as an androgen receptor antagonist by assembly of a transcriptionally inactive receptor |journal=The Journal of Biological Chemistry |volume=277 |issue=29 |pages=26321–6 |date=July 2002 |pmid=12015321 |doi=10.1074/jbc.M203310200}}</ref><ref name="Denis2012">{{cite book |first=Louis |last=Denis | name-list-format = vanc |title=Antiandrogens in Prostate Cancer: A Key to Tailored Endocrine Treatment |url=https://books.google.com/books?id=jqZDBQAAQBAJ&pg=PT128 |date=6 December 2012 |publisher=Springer Science & Business Media |isbn=978-3-642-45745-6 |pages=128, 158, 203}}</ref> It has no capacity to activate the {{abbr|AR|androgen receptor}} under normal [[physiology|physiological]] circumstances (see [[#Paradoxical stimulation of late-stage prostate cancer|below]]).<ref name="Furr1995" /> In addition to competitive antagonism of the {{abbr|AR|androgen receptor}}, bicalutamide has been found to accelerate the [[downregulation and upregulation|degradation]] of the {{abbr|AR|androgen receptor}}, and this action may also be involved in its activity as an antiandrogen.<ref name="pmid10828827">{{cite journal |vauthors=Waller AS, Sharrard RM, Berthon P, Maitland NJ |title=Androgen receptor localisation and turnover in human prostate epithelium treated with the antiandrogen, casodex |journal=Journal of Molecular Endocrinology |volume=24 |issue=3 |pages=339–51 |date=June 2000 |pmid=10828827 |doi=10.1677/jme.0.0240339}}</ref> The activity of bicalutamide lies in the (''R'')-[[isomer]], which binds to the {{abbr|AR|androgen receptor}} with an [[affinity (pharmacology)|affinity]] that is about 30-fold higher than that of the (''S'')-isomer.<ref name="SchellensMcLeod2005" /> Levels of the (''R'')-isomer also notably are 100-fold higher than those of the (''S'')-isomer at steady-state.<ref name="LemkeWilliams2012" /><ref name="ButlerGovindan2010" /> |
|||
Blockade of the {{abbr|AR|androgen receptor}} by bicalutamide in the [[pituitary gland]] and [[hypothalamus]] results in prevention of the [[negative feedback]] of androgens on the [[hypothalamic–pituitary–gonadal axis|hypothalamic–pituitary–gonadal]] (HPG) [[hypothalamic–pituitary–gonadal axis|axis]] in males and consequent disinhibition of pituitary [[luteinizing hormone]] (LH) [[secretion]].<ref name="IversenMelezinek2001" /> This, in turn, results in an increase in circulating {{abbr|LH|luteinizing hormone}} levels and activation of the gonadal production of testosterone and by extension production of estradiol.<ref name="pmid7537602">{{cite journal |vauthors=Eri LM, Haug E, Tveter KJ |title=Effects on the endocrine system of long-term treatment with the non-steroidal anti-androgen Casodex in patients with benign prostatic hyperplasia |journal=British Journal of Urology |volume=75 |issue=3 |pages=335–40 |date=March 1995 |pmid=7537602 |doi=10.1111/j.1464-410X.1995.tb07345.x}}</ref> Levels of testosterone have been found to increase 1.5- to 2-fold (59–97% increase) and levels of estradiol about 1.5- to 2.5-fold (65–146% increase) in men treated with 150 mg/day bicalutamide monotherapy.<ref name="IIIBarbieri2013a" /><ref name="MarcusFeldman2007">{{cite book |first1=Robert |last1=Marcus |first2=David |last2=Feldman |first3=Dorothy |last3=Nelson |first4=Clifford J. |last4=Rosen | name-list-format = vanc |title=Osteoporosis |url=https://books.google.com/books?id=blFlkDHffW8C&pg=PA1354 |date=8 November 2007 |publisher=Academic Press |isbn=978-0-08-055347-4 |pages=1354– |deadurl=no |archiveurl=https://web.archive.org/web/20160611031603/https://books.google.com/books?id=blFlkDHffW8C&pg=PA1354 |archivedate=11 June 2016 |df=dmy-all}}</ref><ref name="MahlerVerhelst1998">{{cite journal |vauthors=Mahler C, Verhelst J, Denis L |title=Clinical pharmacokinetics of the antiandrogens and their efficacy in prostate cancer |journal=Clinical Pharmacokinetics |volume=34 |issue=5 |pages=405–17 |date=May 1998 |pmid=9592622 |doi=10.2165/00003088-199834050-00005}}</ref> In addition to testosterone and estradiol, there are smaller increases in concentrations of {{abbr|DHT|dihydrotestosterone}}, [[sex hormone-binding globulin]], and [[prolactin]].<ref name="MahlerVerhelst1998" /> Estradiol levels with bicalutamide monotherapy are similar to those in the low-normal [[premenopause|premenopausal]] female range while testosterone levels generally remain in the high end of normal male range.<ref name="MarcusFeldman2007" /><ref name="WeinKavoussi2011">{{cite book |first1=Alan J. |last1=Wein |first2=Louis R. |last2=Kavoussi |first3=Andrew C. |last3=Novick |first4=Alan W. |last4=Partin |first5=Craig A. |last5=Peters |name-list-format=vanc |title=Campbell-Walsh Urology: Expert Consult Premium Edition: Enhanced Online Features and Print, 4-Volume Set |url=https://books.google.com/books?id=fu3BBwAAQBAJ&pg=PA2939 |date=25 August 2011 |publisher=Elsevier Health Sciences |isbn=978-1-4160-6911-9 |pages=2938–2939, 2946 |deadurl=no |archiveurl=https://web.archive.org/web/20160505225217/https://books.google.com/books?id=fu3BBwAAQBAJ&pg=PA2939 |archivedate=5 May 2016 |df=dmy-all}}</ref><ref name="Becker2001" /> Testosterone concentrations do not typically exceed the normal male range due to negative feedback on the {{abbr|HPG|hypothalamic–pituitary–gonadal}} axis by the increased concentrations of estradiol.<ref name="IversenMelezinek2001" /> Bicalutamide influences the {{abbr|HPG|hypothalamic–pituitary–gonadal}} axis and increases hormone levels only in men and not also in women.<ref name="Diamanti-KandarakisNestler2009" /><ref name="CarrellPeterson2010">{{cite book |first1=Douglas T. |last1=Carrell |first2=C. Matthew |last2=Peterson |name-list-format=vanc |title=Reproductive Endocrinology and Infertility: Integrating Modern Clinical and Laboratory Practice |url=https://books.google.com/books?id=lcBEheiufVcC&pg=PA163 |date=23 March 2010 |publisher=Springer Science & Business Media |isbn=978-1-4419-1436-1 |pages=163– |deadurl=no |archiveurl=https://web.archive.org/web/20140704201613/http://books.google.com/books?id=lcBEheiufVcC&pg=PA163 |archivedate=4 July 2014 |df=dmy-all}}</ref><ref name="BouchardCaraty1993">{{cite book |first1=P. |last1=Bouchard |first2=A. |last2=Caraty | name-list-format = vanc |title=GnRH, GnRH Analogs, Gonadotropins and Gonadal Peptides |url=https://books.google.com/books?id=uctURfWwTb4C&pg=PA455 |date=15 November 1993 |publisher=CRC Press |isbn=978-0-203-09205-7 |pages=455–456 |quote=[...] when male levels of androgens are achieved in plasma, their effects on gonadotropin secretion are similar in women and men. [...] administration of flutamide in a group of normally-cycling women produced a clinical improvement of acne and hirsutism without any significant hormonal change. [...] All these data emphasize that physiological levels of androgens have no action on the regulation of gonadotropins in normal women. [...] Androgens do not directly play a role in gonadotropin regulation [in women].}}</ref> This is due to the much lower levels of androgens in women and their lack of basal suppression of the {{abbr|HPG|hypothalamic–pituitary–gonadal}} axis in this sex.<ref name="Diamanti-KandarakisNestler2009" /><ref name="CarrellPeterson2010" /><ref name="BouchardCaraty1993" /> As evidenced by its effectiveness in the treatment of prostate cancer and other androgen-dependent conditions, the antiandrogenic actions of bicalutamide greatly exceed any impact of the increased levels of testosterone it results in.<ref name="ChabnerLongo2010" /> However, the elevated levels of estradiol remain unopposed by bicalutamide and are responsible for the gynecomastia and feminizing side effects it causes in men.<ref name="pmid18062751">{{cite journal |vauthors=Sieber PR |title=Treatment of bicalutamide-induced breast events |journal=Expert Review of Anticancer Therapy |volume=7 |issue=12 |pages=1773–9 |date=December 2007 |pmid=18062751 |doi=10.1586/14737140.7.12.1773}}</ref> |
|||
Owing to its selectivity for the {{abbr|AR|androgen receptor}}, unlike {{abbr|SAAs|steroidal antiandrogens}} such as {{abbr|CPA|cyproterone acetate}} and megestrol acetate, bicalutamide does not bind to other [[steroid hormone receptor]]s (including the {{abbrlink|ERs|estrogen receptors}}, {{abbrlink|PRs|progesterone receptors}}, {{abbrlink|GR|glucocorticoid receptor}}, or {{abbrlink|MR|mineralocorticoid receptor}}), and for this reason, has no additional, off-target [[hormonal]] activity ([[estrogen (medication)|estrogen]]ic or [[antiestrogen]]ic, [[progestogen]]ic or [[antiprogestogen]]ic, [[glucocorticoid]] or [[antiglucocorticoid]], or [[mineralocorticoid]] or [[antimineralocorticoid]]).<ref name="Becker2001">{{cite book |first=Kenneth L. |last=Becker |name-list-format=vanc |title=Principles and Practice of Endocrinology and Metabolism |url=https://books.google.com/books?id=FVfzRvaucq8C&pg=PA1208 |year=2001 |publisher=Lippincott Williams & Wilkins |isbn=978-0-7817-1750-2 |pages=1119, 1196, 1208 |deadurl=no |archiveurl=https://web.archive.org/web/20170908222331/https://books.google.com/books?id=FVfzRvaucq8C&pg=PA1208 |archivedate=8 September 2017 |df=dmy-all}}</ref><ref name="FurrTucker1996">{{cite journal |vauthors=Furr BJ, Tucker H |title=The preclinical development of bicalutamide: pharmacodynamics and mechanism of action |journal=Urology |volume=47 |issue=1A Suppl |pages=13–25; discussion 29–32 |date=January 1996 |pmid=8560673 |doi=10.1016/S0090-4295(96)80003-3}}</ref><ref name="SchellensMcLeod2005">{{cite book |first1=Jan H. M. |last1=Schellens |first2=Howard L. |last2=McLeod |first3=David R. |last3=Newell |name-list-format=vanc |title=Cancer Clinical Pharmacology |url=https://books.google.com/books?id=co8Sgu9N0FMC&pg=PA229 |date=5 May 2005 |publisher=OUP Oxford |isbn=978-0-19-262966-1 |pages=229–230 |deadurl=no |archiveurl=https://web.archive.org/web/20160610134202/https://books.google.com/books?id=co8Sgu9N0FMC&pg=PA229 |archivedate=10 June 2016 |df=dmy-all}}</ref><ref name="BagatellBremner2003">{{cite book |first1=Carrie |last1=Bagatelle |first2=William J. |last2=Bremner | name-list-format = vanc |title=Androgens in Health and Disease |url=https://books.google.com/books?id=vDcBCAAAQBAJ&pg=PA25 |date=27 May 2003 |publisher=Springer Science & Business Media |isbn=978-/.1-59259-388-0 |pages=25–}}</ref> In addition, it does not inhibit [[5α-reductase]] and is not known to inhibit other enzymes involved in androgen [[steroidogenesis]] (e.g., [[CYP17A1]]).<ref name="Furr1995" /> Although bicalutamide does not bind to the {{abbr|ERs|estrogen receptors}}, it can increase estrogen levels secondary to blockade of the {{abbr|AR|androgen receptor}} when used as a monotherapy in males, and for this reason, the medication can indirectly activate the {{abbr|ERs|estrogen receptors}} to a degree and hence have some ''indirect'' estrogenic effects in men.<ref name="pmid18231613">{{cite journal |vauthors=Guise TA, Oefelein MG, Eastham JA, Cookson MS, Higano CS, Smith MR |title=Estrogenic side effects of androgen deprivation therapy |journal=Reviews in Urology |volume=9 |issue=4 |pages=163–80 |year=2007 |pmid=18231613 |pmc=2213888 |doi=}}</ref> Also in contrast to {{abbr|SAAs|steroidal antiandrogens}}, bicalutamide neither inhibits nor suppresses androgen production in the body (i.e., it does not act as an [[antigonadotropin]] or [[steroidogenesis inhibitor]]),<ref name="Dart2004" /> and instead exclusively mediates its antiandrogen effects by blocking androgen [[Receptor (biochemistry)#Binding and activation|binding]] and subsequent [[Receptor (biochemistry)#Binding and activation|receptor activation]] at the level of the {{abbr|AR|androgen receptor}}.<ref name="Becker2001" /><ref name="SchellensMcLeod2005" /> |
|||
{{abbr|NSAA|nonsteroidal antiandrogen}} monotherapy, including with bicalutamide, shows a number of tolerability differences from methods of androgen deprivation therapy that incorporate surgical or medical castration. For example, the rates of hot flashes, depression, fatigue, and sexual dysfunction are all much higher with {{abbr|GnRH|gonadotropin-releasing hormone}} analogues than with {{abbr|NSAA|nonsteroidal antiandrogen}} monotherapy. It is thought that this is because {{abbr|GnRH|gonadotropin-releasing hormone}} analogues suppress estrogen production in addition to androgen production, resulting in [[estrogen deficiency]].<ref name="WibowoSchellhammer2011">{{cite journal |vauthors=Wibowo E, Schellhammer P, Wassersug RJ |title=Role of estrogen in normal male function: clinical implications for patients with prostate cancer on androgen deprivation therapy |journal=The Journal of Urology |volume=185 |issue=1 |pages=17–23 |date=January 2011 |pmid=21074215 |doi=10.1016/j.juro.2010.08.094}}</ref><ref name="MotofeiRowland2011">{{cite journal |vauthors=Motofei IG, Rowland DL, Popa F, Kreienkamp D, Paunica S |title=Preliminary study with bicalutamide in heterosexual and homosexual patients with prostate cancer: a possible implication of androgens in male homosexual arousal |journal=BJU International |volume=108 |issue=1 |pages=110–5 |date=July 2011 |pmid=20955264 |doi=10.1111/j.1464-410X.2010.09764.x}}</ref><ref name="pmid23484454">{{cite journal |vauthors=Wibowo E, Wassersug RJ |title=The effect of estrogen on the sexual interest of castrated males: Implications to prostate cancer patients on androgen-deprivation therapy |journal=Critical Reviews in Oncology/Hematology |volume=87 |issue=3 |pages=224–38 |date=September 2013 |pmid=23484454 |doi=10.1016/j.critrevonc.2013.01.006}}</ref> In contrast, {{abbr|NSAA|nonsteroidal antiandrogen}} monotherapy does not decrease estrogen levels and in fact increases them, resulting in an excess of estrogens that compensates for androgen deficiency and allows for a preservation of mood, energy, and sexual function.<ref name="WibowoSchellhammer2011" /><ref name="MotofeiRowland2011" /><ref name="pmid23484454" /> [[Neurosteroid]]s that are produced from testosterone like [[3α-androstanediol]] and [[3β-androstanediol]] may also be involved.<ref name="King2008">{{cite journal |vauthors=King SR |title=Emerging roles for neurosteroids in sexual behavior and function |journal=Journal of Andrology |volume=29 |issue=5 |pages=524–33 |year=2008 |pmid=18567641 |doi=10.2164/jandrol.108.005660}}</ref><ref name="pmid7803627">{{cite journal |vauthors=Morali G, Oropeza MV, Lemus AE, Perez-Palacios G |title=Mechanisms regulating male sexual behavior in the rat: role of 3 alpha- and 3 beta-androstanediols |journal=Biology of Reproduction |volume=51 |issue=3 |pages=562–71 |date=September 1994 |pmid=7803627 |doi=10.1095/biolreprod51.3.562}}</ref><ref name="King2008" /><ref name="pmid7803627" /><ref name="pmid20646182">{{cite journal |vauthors=Sánchez Montoya EL, Hernández L, Barreto-Estrada JL, Ortiz JG, Jorge JC |title=The testosterone metabolite 3α-diol enhances female rat sexual motivation when infused in the nucleus accumbens shell |journal=The Journal of Sexual Medicine |volume=7 |issue=11 |pages=3598–609 |date=November 2010 |pmid=20646182 |pmc=4360968 |doi=10.1111/j.1743-6109.2010.01937.x}}</ref><ref name="Chedrese2009">{{cite book |first=P. Jorge |last=Chedrese | name-list-format = vanc |title=Reproductive Endocrinology: A Molecular Approach |url=https://books.google.com/books?id=3FJXUN6Vh44C&pg=PA233 |date=13 June 2009 |publisher=Springer Science & Business Media |isbn=978-0-387-88186-7 |pages=233– |deadurl=no |archiveurl=https://web.archive.org/web/20170905040216/https://books.google.com/books?id=3FJXUN6Vh44C |archivedate=5 September 2017 |df=dmy-all}}</ref><ref name="Chedrese2009" /><ref name="pmid20552051">{{cite journal |vauthors=Frye CA, Edinger KL, Lephart ED, Walf AA |title=3alpha-androstanediol, but not testosterone, attenuates age-related decrements in cognitive, anxiety, and depressive behavior of male rats |journal=Frontiers in Aging Neuroscience |volume=2 |issue= |pages=15 |year=2010 |pmid=20552051 |pmc=2874398 |doi=10.3389/fnagi.2010.00015}}</ref><ref name="HuangZhu2008">{{cite journal |vauthors=Huang Q, Zhu H, Fischer DF, Zhou JN |title=An estrogenic effect of 5alpha-androstane-3beta, 17beta-diol on the behavioral response to stress and on CRH regulation |journal=Neuropharmacology |volume=54 |issue=8 |pages=1233–8 |date=June 2008 |pmid=18457850 |doi=10.1016/j.neuropharm.2008.03.016}}</ref><ref name="FryeKoonce2008">{{cite journal |vauthors=Frye CA, Koonce CJ, Edinger KL, Osborne DM, Walf AA |title=Androgens with activity at estrogen receptor beta have anxiolytic and cognitive-enhancing effects in male rats and mice |journal=Hormones and Behavior |volume=54 |issue=5 |pages=726–34 |date=November 2008 |pmid=18775724 |pmc=3623974 |doi=10.1016/j.yhbeh.2008.07.013}}</ref> In the specific case of sexual dysfunction, an additional possibility for the difference is that without concomitant suppression of androgen production, blockade of the {{abbr|AR|androgen receptor}} by the bicalutamide in the brain is incomplete and insufficient to markedly influence sexual function.{{Citation needed|date=November 2017}} |
|||
In addition to the classical nuclear {{abbr|AR|androgen receptor}}, bicalutamide has also been identified as a potent antagonist of [[ZIP9]], a [[membrane androgen receptor]] (mAR) and [[zinc transporter protein]], with an {{abbr|IC<sub>50</sub>|half-maximal inhibitory concentration}} of 66.3 nM (relative to K<sub>d</sub> = 17.9 nM for testosterone).<ref name="pmid28943399">{{cite journal | vauthors = Bulldan A, Malviya VN, Upmanyu N, Konrad L, Scheiner-Bobis G | title = Testosterone/bicalutamide antagonism at the predicted extracellular androgen binding site of ZIP9 | journal = Biochim. Biophys. Acta | volume = 1864 | issue = 12 | pages = 2402–2414 | year = 2017 | pmid = 28943399 | doi = 10.1016/j.bbamcr.2017.09.012 | url = }}</ref> This protein appears to be involved in prostate cancer and [[breast cancer]].<ref name="pmid28479083">{{cite journal | vauthors = Thomas P, Converse A, Berg HA | title = ZIP9, a novel membrane androgen receptor and zinc transporter protein | journal = Gen. Comp. Endocrinol. | volume = | issue = | pages = | year = 2017 | pmid = 28479083 | doi = 10.1016/j.ygcen.2017.04.016 | url = }}</ref> Bicalutamide failed to affect testosterone signaling mediated by [[GPRC6A]], another {{abbr|mAR|membrane androgen receptor}}, on the other hand.<ref name="pmid20947496">{{cite journal | vauthors = Pi M, Parrill AL, Quarles LD | title = GPRC6A mediates the non-genomic effects of steroids | journal = J. Biol. Chem. | volume = 285 | issue = 51 | pages = 39953–64 | year = 2010 | pmid = 20947496 | pmc = 3000977 | doi = 10.1074/jbc.M110.158063 | url = }}</ref> |
|||
Under normal circumstances, bicalutamide has no capacity to activate the {{abbr|AR|androgen receptor}}.<ref name="pmid25797385">{{cite journal |vauthors=Bambury RM, Scher HI |title=Enzalutamide: Development from bench to bedside |journal=Urologic Oncology |volume=33 |issue=6 |pages=280–8 |date=June 2015 |pmid=25797385 |doi=10.1016/j.urolonc.2014.12.017}}</ref><ref name="BamburyRathkopf2015">{{cite journal |vauthors=Bambury RM, Rathkopf DE |title=Novel and next-generation androgen receptor-directed therapies for prostate cancer: Beyond abiraterone and enzalutamide |journal=Urologic Oncology |volume=34 |issue=8 |pages=348–55 |date=August 2016 |pmid=26162486 |doi=10.1016/j.urolonc.2015.05.025}}</ref> However, in prostate cancer, [[genetic mutation|mutation]]s and overexpression of the {{abbr|AR|androgen receptor}} can accumulate in prostate gland cells which can convert bicalutamide from an antagonist of the {{abbr|AR|androgen receptor}} into an [[agonist]].<ref name="pmid25797385" /><ref name="pmid24100689">{{cite journal |vauthors=Pinto Á |title=Beyond abiraterone: new hormonal therapies for metastatic castration-resistant prostate cancer |journal=Cancer Biology & Therapy |volume=15 |issue=2 |pages=149–55 |date=February 2014 |pmid=24100689 |pmc=3928129 |doi=10.4161/cbt.26724}}</ref> This can result in paradoxical stimulation of prostate cancer growth with bicalutamide and is responsible for the phenomenon of the [[antiandrogen withdrawal syndrome]], where antiandrogen discontinuation paradoxically slows the rate of prostate cancer growth.<ref name="pmid25797385" /><ref name="pmid24100689" /> |
|||
====Drug levels, androgen levels, and efficacy==== |
|||
Although the affinity of bicalutamide for the {{abbr|AR|androgen receptor}} is approximately 50 times lower than that of {{abbr|DHT|dihydrotestosterone}} ({{abbr|IC<sub>50</sub>|half-maximal inhibitory concentration}} ≈ 3.8 nM),<ref name="Furr2009">{{cite journal |vauthors=Furr BJ |title=Research on reproductive medicine in the pharmaceutical industry |journal=Human Fertility |volume=1 |issue=1 |pages=56–63 |year=2009 |pmid=11844311 |doi=10.1080/1464727982000198131}}</ref><ref name="Denis2012" /> the main [[endogenous]] [[ligand (biochemistry)|ligand]] of the receptor in the prostate gland, sufficiently high relative concentrations of bicalutamide (1,000-fold excess)<ref name="FiggChau2010">{{cite book |first1=William |last1=Figg |first2=Cindy H. |last2=Chau |first3=Eric J. |last3=Small | name-list-format = vanc |title=Drug Management of Prostate Cancer |url=https://books.google.com/books?id=4KDrjeWA5-UC&pg=PA56 |date=14 September 2010 |publisher=Springer Science & Business Media |isbn=978-1-60327-829-4 |pages=56, 71–72, 75, 93}}</ref> are effective in preventing activation of the {{abbr|AR|androgen receptor}} by androgens like {{abbr|DHT|dihydrotestosterone}} and testosterone and subsequent [[downregulation and upregulation|upregulation]] of the [[gene transcription|transcription]] of androgen-responsive [[gene]]s.<ref name="FurrTucker1996" /><ref name="pmid8717469">{{cite journal |vauthors=Furr BJ |title=The development of Casodex (bicalutamide): preclinical studies |journal=European Urology |volume=29 Suppl 2 |issue= |pages=83–95 |year=1996 |pmid=8717469 |doi=}}</ref> At steady-state, relative to the normal adult male range for testosterone levels (300–1,000 ng/dL),<ref name="ChappleSteers2011">{{cite book |first1=Christopher R. |last1=Chapple |first2=William D. |last2=Steers | name-list-format = vanc |title=Practical Urology: Essential Principles and Practice: Essential Principles and Practice |url=https://books.google.com/books?id=A9m8TkdCUqEC&pg=PA225 |date=10 May 2011 |publisher=Springer Science & Business Media |isbn=978-1-84882-034-0 |pages=225– |quote=Normal reference ranges for serum total testosterone in adult men is generally considered to be 300–1,000 ng/dL (10–35 nmol/L).}}</ref> circulating concentrations of bicalutamide at 50 mg/day are 600 to 2,500 times higher and at 150 mg/day 1,500 to 8,000 times higher than circulating testosterone levels, while bicalutamide concentrations, relative to the mean testosterone levels present in men who have been surgically castrated (15 ng/dL),<ref name="GentilePanebianco2014">{{cite book |first1=Vincenzo |last1=Gentile |first2=Valeria |last2=Panebianco |first3=Alessandro |last3=Sciarra | name-list-format = vanc |title=Multidisciplinary Management of Prostate Cancer: The Role of the Prostate Cancer Unit |url=https://books.google.com/books?id=Kn3BBAAAQBAJ&pg=PA106 |date=11 April 2014 |publisher=Springer Science & Business Media |isbn=978-3-319-04385-2 |pages=106– |quote=The standard castrate level is <50 ng/dl. It was defined more than 40 years ago, when testosterone level testing was limited. However, current testing methods using chemiluminescence have found that the mean value of testosterone after surgical castration is 15 ng/dL.}}</ref> are 42,000 times higher than testosterone levels at 50 mg/day.<ref name="FDALabel" /><ref name="TGALabel" /><ref name="DenisMahler1996" /><ref name="Wellington2006" /><ref name="pmid15838655" /> |
|||
In transgender women, breast development is a desired effect of antiandrogen and/or estrogen treatment.<ref name="WierckxGooren2014" /><ref name="OrentreichDurr1974">{{cite journal |last1=Orentreich |first1=Norman |last2=Durr |first2=Nancy P | name-list-format = vanc |title=Mammogenesis in Transsexuals |journal=Journal of Investigative Dermatology |volume=63 |issue=1 |year=1974 |pages=142–6 |doi=10.1111/1523-1747.ep12678272 |pmid=4365991}}</ref> Breast development and gynecomastia induced by bicalutamide in people who are biologically male is thought to be mediated by increased activation of the {{abbr|ER|estrogen receptor}} secondary to blockade of the {{abbr|AR|androgen receptor}} (resulting in disinhibition of the {{abbr|ER|estrogen receptor}} in breast tissue) and increased levels of estradiol.<ref name="JamesonGroot2015" /><ref name="IIIBarbieri2013b">{{cite book |first1=Jerome F. |last1=Strauss III |first2=Robert L. |last2=Barbieri | name-list-format = vanc |title=Yen and Jaffe's Reproductive Endocrinology |url=https://books.google.com/books?id=KZ95AAAAQBAJ&pg=PA236 |date=13 September 2013 |publisher=Elsevier Health Sciences |isbn=978-1-4557-2758-2 |pages=236–237 |deadurl=no |archiveurl=https://web.archive.org/web/20170114164554/https://books.google.com/books?id=KZ95AAAAQBAJ&pg=PA236 |archivedate=14 January 2017 |df=dmy-all}}</ref><ref name="WilsonNizet2015">{{cite book |first1=Christopher B. |last1=Wilson |first2=Victor |last2=Nizet |first3=Yvonne |last3=Maldonado |first4=Jerome O. |last4=Klein |first5=Jack S. |last5=Remington | name-list-format = vanc |title=Remington and Klein's Infectious Diseases of the Fetus and Newborn Infant |url=https://books.google.com/books?id=VuZ1BwAAQBAJ&pg=PA190 |year=2015 |publisher=Elsevier Health Sciences |isbn=978-0-323-24147-2 |pages=190– |deadurl=no |archiveurl=https://web.archive.org/web/20170114165129/https://books.google.com/books?id=VuZ1BwAAQBAJ&pg=PA190 |archivedate=14 January 2017 |df=dmy-all}}</ref> In addition to [[fat deposition]], [[connective tissue]] growth, and [[lactiferous duct|ductal]] development, bicalutamide has been found to produce moderate [[mammary alveolus|lobuloalveolar]] development of the breasts.<ref name="KanhaiHage2000">{{cite journal |vauthors=Kanhai RC, Hage JJ, van Diest PJ, Bloemena E, Mulder JW |title=Short-term and long-term histologic effects of castration and estrogen treatment on breast tissue of 14 male-to-female transsexuals in comparison with two chemically castrated men |journal=The American Journal of Surgical Pathology |volume=24 |issue=1 |pages=74–80 |date=January 2000 |pmid=10632490 |doi=10.1097/00000478-200001000-00009}}</ref><ref name="Lawrence2007">{{cite book | editor-first1 = Ilan H. | editor-last1 = Meyer | editor-first2 = Mary E.| editor-last2 = Northridge |title=The Health of Sexual Minorities Public Health Perspectives on Lesbian, Gay, Bisexual and Transgender Populations |date=2006 |publisher=Springer |location=New York |isbn=978-0-387-28871-0 |chapter=Transgender Health Concerns |first=Anne A. |last=Lawrence | name-list-format = vanc |pages=476 |doi=10.1007/978-0-387-31334-4_19}}</ref><ref name="Rosen2009">{{cite book |first=Paul Peter |last=Rosen | name-list-format = vanc |title=Rosen's Breast Pathology |url=https://books.google.com/books?id=_swaovkfRMMC&pg=PA31 |year=2009 |publisher=Lippincott Williams & Wilkins |location=Philadelphia |isbn=978-0-7817-7137-5 |pages=31– |edition=3}}</ref> However, full lobuloalveolar maturation necessary for [[lactation]] and [[breastfeeding]] will not occur without progestogen treatment.<ref name="KanhaiHage2000" /><ref name="Lawrence2007" /><ref name="Rosen2009" /> |
|||
Whereas testosterone is the major circulating androgen, {{abbr|DHT|dihydrotestosterone}} is the major androgen in the prostate gland.<ref name="ChungIsaacs2007">{{cite book |first1=Leland W. K. |last1=Chung |first2=William B. |last2=Isaacs |first3=Jonathan W. |last3=Simons | name-list-format = vanc |title=Prostate Cancer: Biology, Genetics, and the New Therapeutics |url=https://books.google.com/books?id=9lBjngzdgtcC&pg=PA365 |date=10 November 2007 |publisher=Springer Science & Business Media |isbn=978-1-59745-224-3 |pages=365– |deadurl=no |archiveurl=https://web.archive.org/web/20160520012455/https://books.google.com/books?id=9lBjngzdgtcC |archivedate=20 May 2016 |df=dmy-all}}</ref> {{abbr|DHT|dihydrotestosterone}} levels in circulation are relatively low and only approximately 10% of those of circulating testosterone levels.<ref name="ChungIsaacs2007" /> Conversely, local concentrations of {{abbr|DHT|dihydrotestosterone}} in the prostate gland are 5- to 10-fold higher than circulating levels of {{abbr|DHT|dihydrotestosterone}}.<ref name="MelmedPolonsky2015" /><ref name="Becker2001" /> This is due to high expression of 5α-reductase in the prostate gland, which very efficiently catalyzes the formation of {{abbr|DHT|dihydrotestosterone}} from testosterone<ref name="MelmedPolonsky2015" /> such that over 90% of intraprostatic testosterone is converted into {{abbr|DHT|dihydrotestosterone}}.<ref name="Bruskewitz2012">{{cite book |first=Reginald |last=Bruskewitz | name-list-format = vanc |title=Atlas of the Prostate |url=https://books.google.com/books?id=pluvBQAAQBAJ&pg=PA190 |date=6 December 2012 |publisher=Springer Science & Business Media |isbn=978-1-4615-6505-5 |pages=5,190}}</ref><ref name="NieschlagBehre2012">{{cite book |first1=Eberhard |last1=Nieschlag |first2=Hermann M. |last2=Behre | name-list-format = vanc |title=Testosterone: Action – Deficiency – Substitution |url=https://books.google.com/books?id=jn3nCAAAQBAJ&pg=PA276 |date=6 December 2012 |publisher=Springer Science & Business Media |isbn=978-3-642-72185-4 |pages=130, 276}}</ref> Relative to testosterone, {{abbr|DHT|dihydrotestosterone}} is 2.5- to 10-fold as potent as an {{abbr|AR|androgen receptor}} agonist in [[bioassay]]s, and hence, is a much stronger androgen in comparison.<ref name="MozayaniRaymon2011">{{cite book |first1=Ashram |last1=Mozayani |first2=Lionel |last2=Raymon |name-list-format = vanc |title=Handbook of Drug Interactions: A Clinical and Forensic Guide |url=https://books.google.com/books?id=NhBJ6kg_uP0C&pg=PA656 |date=18 September 2011 |publisher=Springer Science & Business Media |isbn=978-1-61779-222-9 |pages=656–}}</ref> As such, {{abbr|AR|androgen receptor}} signaling is exceptionally high in the prostate gland, and the effectiveness of bicalutamide monotherapy in the treatment of prostate cancer, which is roughly equivalent to that of {{abbr|GnRH|gonadotropin-releasing hormone}} analogues,<ref name="ChabnerLongo2010" /><ref name="FiggChau2010" /><ref name="MydloGodec2015">{{cite book |first1=Jack H. |last1=Mydlo |first2=Ciril J. |last2=Godec | name-list-format = vanc |title=Prostate Cancer: Science and Clinical Practice |url=https://books.google.com/books?id=292cBAAAQBAJ&pg=PA530 |date=29 September 2015 |publisher=Elsevier Science |isbn=978-0-12-800592-7 |pages=516–521, 534–540 |deadurl=no |archiveurl=https://web.archive.org/web/20170908222331/https://books.google.com/books?id=292cBAAAQBAJ&pg=PA530 |archivedate=8 September 2017 |df=dmy-all}}</ref><ref name="IIIBarbieri2013a" /> is a reflection of its capacity to strongly and efficaciously antagonize the {{abbr|AR|androgen receptor}} at clinically used dosages. On the other hand, {{abbr|GnRH|gonadotropin-releasing hormone}} analogues achieve only a 50 to 60% reduction in levels of {{abbr|DHT|dihydrotestosterone}} in the prostate gland,<ref name="Denis2012" /><ref name="LuoMartel1997">{{cite journal |vauthors=Luo S, Martel C, Chen C, Labrie C, Candas B, Singh SM, Labrie F |title=Daily dosing with flutamide or Casodex exerts maximal antiandrogenic activity |journal=Urology |volume=50 |issue=6 |pages=913–9 |date=December 1997 |pmid=9426723 |doi=10.1016/S0090-4295(97)00393-2}}</ref> and the combination of a {{abbr|GnRH|gonadotropin-releasing hormone}} analogue and bicalutamide is significantly more effective than either modality alone in the treatment of prostate cancer.<ref name="SinghGauthier2000" /><ref name="WirthHakenberg2007" /> |
|||
Bicalutamide monotherapy seems to have minimal effect on [[spermatogenesis]], [[testicle|testicular]] [[ultrastructure]], and [[male fertility]].<ref name="MorganteGradini2001" /><ref name="Mulhall2013">{{cite book |first=John P. |last=Mulhall |name-list-format=vanc |title=Fertility Preservation in Male Cancer Patients |url=https://books.google.com/books?id=97wgAwAAQBAJ&pg=PA84 |date=21 February 2013 |publisher=Cambridge University Press |isbn=978-1-139-61952-3 |pages=84– |deadurl=no |archiveurl=https://web.archive.org/web/20160429171718/https://books.google.com/books?id=97wgAwAAQBAJ&pg=PA84 |archivedate=29 April 2016 |df=dmy-all}}</ref><ref name="IswaranImai1997" /><ref name="MorganteGradini2001">{{cite journal |vauthors=Morgante E, Gradini R, Realacci M, Sale P, D'Eramo G, Perrone GA, Cardillo MR, Petrangeli E, Russo M, Di Silverio F |title=Effects of long-term treatment with the anti-androgen bicalutamide on human testis: an ultrastructural and morphometric study |journal=Histopathology |volume=38 |issue=3 |pages=195–201 |date=March 2001 |pmid=11260298 |doi=10.1046/j.1365-2559.2001.01077.x}}</ref> This seems to be because testosterone levels in the testes (where ~95% of testosterone in males is produced) are extremely high (up to 200-fold higher than circulating levels) and only a small fraction (less than 10%) of the normal levels of testosterone in the testes are actually necessary to maintain spermatogenesis.<ref name="SchillComhaire2006">{{cite book |first1=Wolf-Bernhard |last1=Schill |first2=Frank H. |last2=Comhaire |first3=Timothy B. |last3=Hargreave | name-list-format = vanc |title=Andrology for the Clinician |url=https://books.google.com/books?id=5Ts_AAAAQBAJ&pg=PA76 |date=26 August 2006 |publisher=Springer Science & Business Media |isbn=978-3-540-33713-3 |pages=76– |deadurl=no |archiveurl=https://web.archive.org/web/20160526220017/https://books.google.com/books?id=5Ts_AAAAQBAJ&pg=PA76 |archivedate=26 May 2016 |df=dmy-all}}</ref><ref name="NieschlagBehre2012" /><ref name="NieschlagBehre2012" /><ref name="Cheng2009">{{cite book |first=C.Y. |last=Cheng | name-list-format = vanc |title=Molecular Mechanisms in Spermatogenesis |url=https://books.google.com/books?id=tdpVNN80_r0C&pg=PA258 |date=24 October 2009 |publisher=Springer Science & Business Media |isbn=978-0-387-09597-4 |pages=258–}}</ref> As a result, bicalutamide seems to not be able to compete with testosterone in this sole part of the body to an extent sufficient to considerably interfere with androgen signaling and function.<ref name="SchillComhaire2006" /><ref name="NieschlagBehre2012" /><ref name="NieschlagBehre2012" /><ref name="Cheng2009" /> However, suppression of gonadal androgen production, such as by taking an estrogen, progestogen, or {{abbr|GnRH|gonadotropin-releasing hormone}} analogue with bicalutamide, can compromise this due to their own adverse effects on spermatogenesis and fertility.<ref name="Johnson2003">{{cite book |first=Leonard R. |last=Johnson | name-list-format = vanc |title=Essential Medical Physiology |url=https://books.google.com/books?id=Ql10m-_q3nMC&pg=PA731 |date=14 October 2003 |publisher=Academic Press |isbn=978-0-08-047270-6 |pages=731– |deadurl=no |archiveurl=https://web.archive.org/web/20170215093206/https://books.google.com/books?id=Ql10m-_q3nMC&pg=PA731 |archivedate=15 February 2017 |df=dmy-all}}</ref><ref name="JonesReiter2016" /><ref name="PayneHardy2007">{{cite book |first1=Anita H. |last1=Payne |first2=Matthew P. |last2=Hardy | name-list-format = vanc |title=The Leydig Cell in Health and Disease |url=https://books.google.com/books?id=x4ttqKIAOg0C&pg=PA422 |date=28 October 2007 |publisher=Springer Science & Business Media |isbn=978-1-59745-453-7 |pages=422–431 |quote=Estrogens are highly efficient inhibitors of the hypothalamic-hypophyseal-testicular axis (212–214). Aside from their negative feedback action at the level of the hypothalamus and pituitary, direct inhibitory effects on the testis are likely (215,216). [...] The histology of the testes [with estrogen treatment] showed disorganization of the seminiferous tubules, vacuolization and absence of lumen, and compartmentalization of spermatogenesis.}}</ref><ref name="WakelinMaibach2002">{{cite book |first1=Sarah H. |last1=Wakelin |first2=Howard I. |last2=Maibach |first3=Clive B. |last3=Archer | name-list-format = vanc |title=Systemic Drug Treatment in Dermatology: A Handbook |url=https://books.google.com/books?id=F1ZiAgAAQBAJ&pg=PA32 |date=1 June 2002 |publisher=CRC Press |isbn=978-1-84076-013-2 |pages=32– |quote=[Cyproterone acetate] inhibits spermatogenesis and produces reversible infertility (but is not a male contraceptive). |deadurl=no |archiveurl=https://web.archive.org/web/20140725205131/http://books.google.com/books?id=F1ZiAgAAQBAJ&pg=PA32 |archivedate=25 July 2014 |df=dmy-all}}</ref><ref name="pmid8005205">{{cite journal |vauthors=Neumann F |title=The antiandrogen cyproterone acetate: discovery, chemistry, basic pharmacology, clinical use and tool in basic research |journal=Exp. Clin. Endocrinol. |volume=102 |issue=1 |pages=1–32 |year=1994 |pmid=8005205 |doi=10.1055/s-0029-1211261 |url= |quote=Spermatogenesis is also androgen-dependent and is inhibited by CPA, meaning that patients treated with high doses of CPA are sterile (Figure 23). All the effects of CPA are fully reversible.}}</ref><ref name="Salam2003">{{cite book |first=Muhammad A. |last=Salam | name-list-format =vanc |title=Principles & Practice of Urology: A Comprehensive Text |url=https://books.google.com/books?id=y50kTcCCfEcC&pg=PA684 |year=2003 |publisher=Universal-Publishers |isbn=978-1-58112-412-5 |pages=684– |quote=Estrogens act primarily through negative feedback at the hypothalamic-pituitary level to reduce LH secretion and testicular androgen synthesis. [...] Interestingly, if the treatment with estrogens is discontinued after 3 yr. of uninterrupted exposure, serum testosterone may remain at castration levels for up to another 3 yr. This prolonged suppression is thought to result from a direct effect of estrogens on the Leydig cells.}}</ref> |
|||
In women, total testosterone levels are 20-fold and free testosterone levels 40-fold lower relative to men.<ref name="MelmedPolonsky2015" /> In addition, whereas bicalutamide monotherapy can increase testosterone levels by up to 2-fold in men,<ref name="IIIBarbieri2013a" /><ref name="MarcusFeldman2007" /> the drug does not increase testosterone levels in women (see [[#Influences on hormone levels|below]]).<ref name="Diamanti-KandarakisNestler2009">{{cite book |first1=Evanthia |last1=Diamanti-Kandarakis |first2=John E. |last2=Nestler |first3=Dimities |last3=Pandas |first4=Renato |last4=Pasquale | name-list-format = vanc |title=Insulin Resistance and Polycystic Ovarian Syndrome: Pathogenesis, Evaluation, and Treatment |url=https://books.google.com/books?id=7ej6ZgqiFEsC&pg=PA75 |date=21 December 2009 |publisher=Springer Science & Business Media |isbn=978-1-59745-310-3 |pages=75– |deadurl=no |archiveurl=https://web.archive.org/web/20160519021821/https://books.google.com/books?id=7ej6ZgqiFEsC&pg=PA75 |archivedate=19 May 2016 |df=dmy-all}}</ref><ref name="CarrellPeterson2010" /><ref name="BouchardCaraty1993" /> For these reasons, much lower dosages of bicalutamide (e.g., 25 mg/day in the hirsutism studies) may be used in women with comparable antiandrogen effectiveness.<ref name="WilliamsBigby2009" /><ref name="pmid24455796" /><ref name="MorettiGuccione2016">{{cite | title = Efficacy and Safety of Myo-Inositol Supplementation in the Treatment of Obese Hirsute PCOS Women: Comparative Evaluation with OCP+Bicalutamide Therapy | authors = Costanzo Giulio Moretti, Laura Guccione, Paola Di Giacinto, Amalia Cannuccia, Chiara Meleca, Giulia Lanzolla, Aikaterini Andreadi, Davide Lauro | year = 2016 | url = http://press.endocrine.org/doi/abs/10.1210/endo-meetings.2016.RE.5.SUN-153 | doi = 10.1210/endo-meetings.2016.RE.5.SUN-153}}</ref><ref name="MahlerVerhelst1998" /> |
|||
====Influences on hormone levels==== |
|||
[[File:Bicalutamide and the hypothalamic-pituitary-glandular axes.png|thumb|right|300px|Bicalutamide, the [[hypothalamic–pituitary hormone|hypothalamic–pituitary–glandular axes]], and sex hormone production.<ref name="pmid14748655">{{cite journal |vauthors=Fradet Y |title=Bicalutamide (Casodex) in the treatment of prostate cancer |journal=Expert Review of Anticancer Therapy |volume=4 |issue=1 |pages=37–48 |date=February 2004 |pmid=14748655 |doi=10.1586/14737140.4.1.37 |quote=In contrast, the incidence of diarrhea was comparable between the bicalutamide and placebo groups (6.3 vs. 6.4%, respectively) in the EPC program [71].}}</ref>]] |
|||
In men, blockade of the {{abbr|AR|androgen receptor}} by bicalutamide in the [[pituitary gland]] and [[hypothalamus]] prevents the [[negative feedback]] of androgens on the [[hypothalamic–pituitary–gonadal axis|hypothalamic–pituitary–gonadal]] (HPG) [[hypothalamic–pituitary–gonadal axis|axis]], resulting in an increase in {{abbr|LH|luteinizing hormone}} secretion and levels.<ref name="IversenMelezinek2001" /> [[Follicle-stimulating hormone]] (FSH) levels, in contrast, remain essentially unchanged.<ref name="Jr.Lawrence2015">{{cite book |first1=Vincent T. |last1=DeVita Jr. |first2=Theodore S. |last2=Lawrence |first3=Steven A. |last3=Rosenberg | name-list-format = vanc |title=DeVita, Hellman, and Rosenberg's Cancer: Principles & Practice of Oncology |url=https://books.google.com/books?id=HEAYBgAAQBAJ&pg=PT1142 |date=7 January 2015 |publisher=Wolters Kluwer Health |isbn=978-1-4698-9455-3 |pages=1142–}}</ref> The increase in {{abbr|LH|luteinizing hormone}} levels leads to an elevation in androgen and estrogen levels.<ref name="pmid7537602">{{cite journal |vauthors=Eri LM, Haug E, Tveter KJ |title=Effects on the endocrine system of long-term treatment with the non-steroidal anti-androgen Casodex in patients with benign prostatic hyperplasia |journal=British Journal of Urology |volume=75 |issue=3 |pages=335–40 |date=March 1995 |pmid=7537602 |doi=10.1111/j.1464-410X.1995.tb07345.x}}</ref> At a dosage of 150 mg/day, bicalutamide has been found to increase testosterone levels by about 1.5- to 2-fold (59–97% increase) and estradiol levels by about 1.5- to 2.5-fold (65–146% increase).<ref name="IIIBarbieri2013a" /><ref name="MarcusFeldman2007">{{cite book |first1=Robert |last1=Marcus |first2=David |last2=Feldman |first3=Dorothy |last3=Nelson |first4=Clifford J. |last4=Rosen | name-list-format = vanc |title=Osteoporosis |url=https://books.google.com/books?id=blFlkDHffW8C&pg=PA1354 |date=8 November 2007 |publisher=Academic Press |isbn=978-0-08-055347-4 |pages=1354– |deadurl=no |archiveurl=https://web.archive.org/web/20160611031603/https://books.google.com/books?id=blFlkDHffW8C&pg=PA1354 |archivedate=11 June 2016 |df=dmy-all}}</ref><ref name="MahlerVerhelst1998">{{cite journal |vauthors=Mahler C, Verhelst J, Denis L |title=Clinical pharmacokinetics of the antiandrogens and their efficacy in prostate cancer |journal=Clinical Pharmacokinetics |volume=34 |issue=5 |pages=405–17 |date=May 1998 |pmid=9592622 |doi=10.2165/00003088-199834050-00005}}</ref> Levels of {{abbr|DHT|dihydrotestosterone}} are also increased to a lesser extent (by 25%), and concentrations of [[sex hormone-binding globulin]] (SHBG) and [[prolactin]] increase as well (by 8% and 40%, respectively) secondary to the increase in estradiol levels.<ref name="MahlerVerhelst1998" /> The estradiol concentrations produced in men by bicalutamide monotherapy are said to approximate the low-normal estradiol levels of a [[premenopausal]] woman,<ref name="MarcusFeldman2007" /> while testosterone levels generally remain in the high end of the normal male range and rarely exceed it.<ref name="WeinKavoussi2011">{{cite book |first1=Alan J. |last1=Wein |first2=Louis R. |last2=Kavoussi |first3=Andrew C. |last3=Novick |first4=Alan W. |last4=Partin |first5=Craig A. |last5=Peters |name-list-format=vanc |title=Campbell-Walsh Urology: Expert Consult Premium Edition: Enhanced Online Features and Print, 4-Volume Set |url=https://books.google.com/books?id=fu3BBwAAQBAJ&pg=PA2939 |date=25 August 2011 |publisher=Elsevier Health Sciences |isbn=978-1-4160-6911-9 |pages=2938–2939, 2946 |deadurl=no |archiveurl=https://web.archive.org/web/20160505225217/https://books.google.com/books?id=fu3BBwAAQBAJ&pg=PA2939 |archivedate=5 May 2016 |df=dmy-all}}</ref><ref name="Becker2001" /> Dosages of bicalutamide of 10 mg, 30 mg, and 50 mg per day have been found to produce a "moderate" effect on sex hormone levels in men with prostate cancer (notably providing indication that the drug has clinically-relevant antiandrogen effects in males at a dosage as low as 10 mg/day).<ref name="pmid2515147">{{cite journal |vauthors=Lunglmayr G |title=Casodex (ICI 176,334), a new, non-steroidal anti-androgen. Early clinical results |journal=Hormone Research |volume=32 Suppl 1 |issue= |pages=77–81 |year=1989 |pmid=2515147 |doi=10.1159/000181316}}</ref> It is important to note that bicalutamide increases androgen and estrogen levels only in men and not in women; this is because androgen levels are comparatively far lower in women and in turn exert little to no basal suppression of the {{abbr|HPG|hypothalamic–pituitary–gonadal}} axis.<ref name="Diamanti-KandarakisNestler2009" /><ref name="CarrellPeterson2010">{{cite book |first1=Douglas T. |last1=Carrell |first2=C. Matthew |last2=Peterson |name-list-format=vanc |title=Reproductive Endocrinology and Infertility: Integrating Modern Clinical and Laboratory Practice |url=https://books.google.com/books?id=lcBEheiufVcC&pg=PA163 |date=23 March 2010 |publisher=Springer Science & Business Media |isbn=978-1-4419-1436-1 |pages=163– |deadurl=no |archiveurl=https://web.archive.org/web/20140704201613/http://books.google.com/books?id=lcBEheiufVcC&pg=PA163 |archivedate=4 July 2014 |df=dmy-all}}</ref><ref name="BouchardCaraty1993">{{cite book |first1=P. |last1=Bouchard |first2=A. |last2=Caraty | name-list-format = vanc |title=GnRH, GnRH Analogs, Gonadotropins and Gonadal Peptides |url=https://books.google.com/books?id=uctURfWwTb4C&pg=PA455 |date=15 November 1993 |publisher=CRC Press |isbn=978-0-203-09205-7 |pages=455–456 |quote=[...] when male levels of androgens are achieved in plasma, their effects on gonadotropin secretion are similar in women and men. [...] administration of flutamide in a group of normally-cycling women produced a clinical improvement of acne and hirsutism without any significant hormonal change. [...] All these data emphasize that physiological levels of androgens have no action on the regulation of gonadotropins in normal women. [...] Androgens do not directly play a role in gonadotropin regulation [in women].}}</ref> |
|||
The reason that testosterone levels are elevated but almost always remain in the normal male range with bicalutamide monotherapy is thought to be due to the concomitantly increased levels of estradiol, as estradiol is potently antigonadotropic and limits secretion of {{abbr|LH|luteinizing hormone}}.<ref name="IversenMelezinek2001" /> In fact, estradiol is a much stronger inhibitor of gonadotropin secretion than is testosterone, and even though circulating concentrations of estradiol are far lower than those of testosterone in men, it is said that estradiol is nonetheless likely the major feedback regulator of gonadotropin secretion in this sex.<ref name="JamesonKretser2013">{{cite book |first1=J. Larry |last1=Jameson |first2=David M. |last2=de Kretser |first3=John C. |last3=Marshall |first4=Leslie J. |last4=De Groot | name-list-format = vanc |title=Endocrinology Adult and Pediatric: Reproductive Endocrinology |url=https://books.google.com/books?id=Np8xxP6pcdUC&pg=RA1-PT476 |date=7 May 2013 |publisher=Elsevier Health Sciences |isbn=978-0-323-22152-8 |pages= |quote=Nonsteroidal antiandrogens (e.g., flutamide and nilutamide) are also used, but they increase gonadotropin secretion, causing increased secretion of testosterone and estradiol.119 The latter is desirable in this context, as it has feminizing effects. |deadurl=no |archiveurl=https://web.archive.org/web/20140725230829/http://books.google.com/books?id=Np8xxP6pcdUC&pg=RA1-PT476 |archivedate=25 July 2014 |df=dmy-all}}</ref> In accordance, [[clomifene]], a {{abbr|SERM|selective estrogen receptor modulator}} with antiestrogenic activity, has been found to increase testosterone levels to as much as 250% of initial values in men with [[hypogonadism]],<ref name="BachNajari2016">{{cite journal |last1=Bach |first1=Phil Vu |last2=Najari |first2=Bobby B. |last3=Kashanian |first3=James A. | name-list-format = vanc |title=Adjunct Management of Male Hypogonadism |journal=Current Sexual Health Reports |year=2016 |issn=1548-3584 |doi=10.1007/s11930-016-0089-7}}</ref> and a study of clomifene treatment in normal men observed increases in {{abbr|FSH|follicle-stimulating hormone}} and {{abbr|LH|luteinizing hormone}} levels of 70–360% and 200–700%, respectively, with increases in testosterone levels that were similar to the increases seen with the gonadotropins.<ref name="pmid5135636">{{cite journal |vauthors=Santen RJ, Leonard JM, Sherins RJ, Gandy HM, Paulsen CA |title=Short- and long-term effects of clomiphene citrate on the pituitary-testicular axis |journal=J. Clin. Endocrinol. Metab. |volume=33 |issue=6 |pages=970–9 |year=1971 |pmid=5135636 |doi=10.1210/jcem-33-6-970 |url= |quote=Increase in serum LH levels ranged from 200–700% during the initial 21 days of clomiphene administration but then plateaued. Serum FSH levels exhibited a similar plateau after 35 days, with maximum titers 70–360% over control. The range in serum testosterone increments after 7 and 51 days of clomiphene administration was similar to that observed in serum gonadotrophin levels.}}</ref><ref name="Martini2012">{{cite book |first=Luciano |last=Martini | name-list-format = vanc |title=Clinical Neuroendocrinology |url=https://books.google.com/books?id=ieY0MWOZON8C&pg=PA239 |date=2 December 2012 |publisher=Elsevier |isbn=978-0-323-14429-2 |page=239 |quote=From the studies of Santen et al. (1971), it seems that a longer period of administration (51 days in their study) would cause an even greater rise in FSH and LH (70–360% and 200–700%, respectively).}}</ref> In addition to systemic or circulating estradiol, local aromatization of testosterone into estradiol in the hypothalamus and pituitary gland may contribute to suppression of gonadotropin secretion.<ref name="JamesonKretser2013" /> |
|||
Bicalutamide more than blocks the effects of the increased testosterone levels that it induces in men, which is evidenced by the fact that monotherapy with the drug is about as effective as {{abbr|GnRH|gonadotropin-releasing hormone}} analogue therapy in the treatment of prostate cancer.<ref name="ChabnerLongo2010" /> However, in contrast, the effects of the elevated estrogen levels remain unopposed by bicalutamide, and this is largely responsible for the feminizing side effects (e.g., gynecomastia) of the drug in men.<ref name="pmid18062751">{{cite journal |vauthors=Sieber PR |title=Treatment of bicalutamide-induced breast events |journal=Expert Review of Anticancer Therapy |volume=7 |issue=12 |pages=1773–9 |date=December 2007 |pmid=18062751 |doi=10.1586/14737140.7.12.1773}}</ref> |
|||
====Differences from castration==== |
|||
It has been proposed that the increase in estrogen levels caused by {{abbr|NSAAs|nonsteroidal antiandrogens}} like bicalutamide compensates for androgen blockade in the brain, which may explain differences in the side effect profiles of these drugs relative to {{abbr|GnRH|gonadotropin-releasing hormone}} analogues/castration, {{abbr|CAB|combined androgen blockade}}, and {{abbr|CPA|cyproterone acetate}} (which, in contrast, decrease both androgen and estrogen levels).<ref name="WibowoSchellhammer2011">{{cite journal |vauthors=Wibowo E, Schellhammer P, Wassersug RJ |title=Role of estrogen in normal male function: clinical implications for patients with prostate cancer on androgen deprivation therapy |journal=The Journal of Urology |volume=185 |issue=1 |pages=17–23 |date=January 2011 |pmid=21074215 |doi=10.1016/j.juro.2010.08.094}}</ref><ref name="MotofeiRowland2011">{{cite journal |vauthors=Motofei IG, Rowland DL, Popa F, Kreienkamp D, Paunica S |title=Preliminary study with bicalutamide in heterosexual and homosexual patients with prostate cancer: a possible implication of androgens in male homosexual arousal |journal=BJU International |volume=108 |issue=1 |pages=110–5 |date=July 2011 |pmid=20955264 |doi=10.1111/j.1464-410X.2010.09764.x}}</ref><ref name="pmid23484454">{{cite journal |vauthors=Wibowo E, Wassersug RJ |title=The effect of estrogen on the sexual interest of castrated males: Implications to prostate cancer patients on androgen-deprivation therapy |journal=Critical Reviews in Oncology/Hematology |volume=87 |issue=3 |pages=224–38 |date=September 2013 |pmid=23484454 |doi=10.1016/j.critrevonc.2013.01.006}}</ref> In the case of sexual interest and function, this notion is supported by a variety of findings including animal studies showing that [[hypoestrogenism|estrogen deficiency]] results in diminished sexual behavior, treatment with tamoxifen resulting in significantly lowered libido in 30% of men receiving it for male breast cancer, and estrogen administration restoring libido and the frequency of [[sexual intercourse]] in men with [[congenital estrogen deficiency]], among others.<ref name="WibowoSchellhammer2011" /><ref name="MotofeiRowland2011" /><ref name="pmid23484454" /><ref name="SimpsonJones2007">{{cite journal |vauthors=Simpson ER, Jones ME |title=Of mice and men: the many guises of estrogens |journal=Ernst Schering Foundation Symposium Proceedings |volume=2006/1 |issue=1 |pages=45–67 |year=2007 |pmid=17824171 |doi=10.1007/2789_2006_016}}</ref> |
|||
Several metabolites of testosterone and {{abbr|DHT|dihydrotestosterone}}, including estradiol, [[3α-androstanediol]], and [[3β-androstanediol]], are estrogens (mainly potent {{abbrlink|ERβ|estrogen receptor beta}} agonists in the cases of the latter two), and 3α-androstanediol is additionally a potent GABA<sub>A</sub> receptor-potentiating neurosteroid.<ref name="King2008">{{cite journal |vauthors=King SR |title=Emerging roles for neurosteroids in sexual behavior and function |journal=Journal of Andrology |volume=29 |issue=5 |pages=524–33 |year=2008 |pmid=18567641 |doi=10.2164/jandrol.108.005660}}</ref><ref name="pmid7803627">{{cite journal |vauthors=Morali G, Oropeza MV, Lemus AE, Perez-Palacios G |title=Mechanisms regulating male sexual behavior in the rat: role of 3 alpha- and 3 beta-androstanediols |journal=Biology of Reproduction |volume=51 |issue=3 |pages=562–71 |date=September 1994 |pmid=7803627 |doi=10.1095/biolreprod51.3.562}}</ref> Due to the fact that bicalutamide does not lower testosterone levels, the levels of these metabolites would not be expected to be lowered either, unlike with therapies such as {{abbr|GnRH|gonadotropin-releasing hormone}} analogues. (Indeed, testosterone, {{abbr|DHT|dihydrotestosterone}}, and estradiol levels are actually raised by bicalutamide treatment, and for this reason, levels of 3α- and 3β-androstanediol might be elevated to some degree similarly.) These metabolites of testosterone have been found to have {{abbr|AR|androgen receptor}}-independent positive effects on sexual motivation,<ref name="King2008" /><ref name="pmid7803627" /><ref name="pmid20646182">{{cite journal |vauthors=Sánchez Montoya EL, Hernández L, Barreto-Estrada JL, Ortiz JG, Jorge JC |title=The testosterone metabolite 3α-diol enhances female rat sexual motivation when infused in the nucleus accumbens shell |journal=The Journal of Sexual Medicine |volume=7 |issue=11 |pages=3598–609 |date=November 2010 |pmid=20646182 |pmc=4360968 |doi=10.1111/j.1743-6109.2010.01937.x}}</ref><ref name="Chedrese2009">{{cite book |first=P. Jorge |last=Chedrese | name-list-format = vanc |title=Reproductive Endocrinology: A Molecular Approach |url=https://books.google.com/books?id=3FJXUN6Vh44C&pg=PA233 |date=13 June 2009 |publisher=Springer Science & Business Media |isbn=978-0-387-88186-7 |pages=233– |deadurl=no |archiveurl=https://web.archive.org/web/20170905040216/https://books.google.com/books?id=3FJXUN6Vh44C |archivedate=5 September 2017 |df=dmy-all}}</ref> and may explain the preservation of sexual interest and function by bicalutamide and other {{abbr|NSAAs|nonsteroidal antiandrogens}}.<ref name="WibowoSchellhammer2011" /> They also have [[antidepressant]], [[anxiolytic]], and [[nootropic|cognitive-enhancing]] effects,<ref name="Chedrese2009" /><ref name="pmid20552051">{{cite journal |vauthors=Frye CA, Edinger KL, Lephart ED, Walf AA |title=3alpha-androstanediol, but not testosterone, attenuates age-related decrements in cognitive, anxiety, and depressive behavior of male rats |journal=Frontiers in Aging Neuroscience |volume=2 |issue= |pages=15 |year=2010 |pmid=20552051 |pmc=2874398 |doi=10.3389/fnagi.2010.00015}}</ref><ref name="HuangZhu2008">{{cite journal |vauthors=Huang Q, Zhu H, Fischer DF, Zhou JN |title=An estrogenic effect of 5alpha-androstane-3beta, 17beta-diol on the behavioral response to stress and on CRH regulation |journal=Neuropharmacology |volume=54 |issue=8 |pages=1233–8 |date=June 2008 |pmid=18457850 |doi=10.1016/j.neuropharm.2008.03.016}}</ref><ref name="FryeKoonce2008">{{cite journal |vauthors=Frye CA, Koonce CJ, Edinger KL, Osborne DM, Walf AA |title=Androgens with activity at estrogen receptor beta have anxiolytic and cognitive-enhancing effects in male rats and mice |journal=Hormones and Behavior |volume=54 |issue=5 |pages=726–34 |date=November 2008 |pmid=18775724 |pmc=3623974 |doi=10.1016/j.yhbeh.2008.07.013}}</ref> and may account for the lower incidence of depression with bicalutamide and other {{abbr|NSAAs|nonsteroidal antiandrogens}} relative to other antiandrogen therapies. |
|||
====Paradoxical stimulation of late-stage prostate cancer==== |
|||
Though a pure, or silent antagonist of the {{abbr|AR|androgen receptor}} under normal circumstances, bicalutamide, as well as other earlier antiandrogens like flutamide and nilutamide, have been found to possess weak [[partial agonist]] properties in the setting of {{abbr|AR|androgen receptor}} overexpression and agonist activity in the case of certain mutations in the [[ligand-binding domain]] (LBD) of the {{abbr|AR|androgen receptor}}.<ref name="pmid25797385">{{cite journal |vauthors=Bambury RM, Scher HI |title=Enzalutamide: Development from bench to bedside |journal=Urologic Oncology |volume=33 |issue=6 |pages=280–8 |date=June 2015 |pmid=25797385 |doi=10.1016/j.urolonc.2014.12.017}}</ref><ref name="BamburyRathkopf2015">{{cite journal |vauthors=Bambury RM, Rathkopf DE |title=Novel and next-generation androgen receptor-directed therapies for prostate cancer: Beyond abiraterone and enzalutamide |journal=Urologic Oncology |volume=34 |issue=8 |pages=348–55 |date=August 2016 |pmid=26162486 |doi=10.1016/j.urolonc.2015.05.025}}</ref> As both of these circumstances can eventually occur in prostate cancer, resistance to bicalutamide usually develops and the drug has the potential to paradoxically stimulate tumor growth when this happens.<ref name="pmid25797385" /><ref name="pmid24100689">{{cite journal |vauthors=Pinto Á |title=Beyond abiraterone: new hormonal therapies for metastatic castration-resistant prostate cancer |journal=Cancer Biology & Therapy |volume=15 |issue=2 |pages=149–55 |date=February 2014 |pmid=24100689 |pmc=3928129 |doi=10.4161/cbt.26724}}</ref> This is the mechanism of the phenomenon of [[antiandrogen withdrawal syndrome]], where antiandrogen discontinuation paradoxically slows the rate of tumor growth.<ref name="pmid24100689" /> The newer drug enzalutamide has been shown not to have agonistic properties in the context of overexpression of the {{abbr|AR|androgen receptor}}, though certain mutations in the {{abbr|AR|androgen receptor}} can still convert it from an antagonist to agonist.<ref name="pmid25797385" /> |
|||
====Induction of breast development==== |
|||
{{See also|Breast development|Hormonal breast enhancement}} |
|||
In transgender women, [[breast development]] is a desired effect of antiandrogen and/or estrogen treatment.<ref name="WierckxGooren2014" /><ref name="OrentreichDurr1974">{{cite journal |last1=Orentreich |first1=Norman |last2=Durr |first2=Nancy P | name-list-format = vanc |title=Mammogenesis in Transsexuals |journal=Journal of Investigative Dermatology |volume=63 |issue=1 |year=1974 |pages=142–6 |doi=10.1111/1523-1747.ep12678272 |pmid=4365991}}</ref> Bicalutamide induces breast development (or gynecomastia) in biologically male individuals by two mechanisms: 1) blocking androgen signaling in breast tissue; and 2) increasing estrogen levels.<ref name="JamesonGroot2015"/> Estrogen is responsible for the induction of breast development under normal circumstances, while androgens powerfully suppress estrogen-induced breast growth.<ref name="IIIBarbieri2013b">{{cite book |first1=Jerome F. |last1=Strauss III |first2=Robert L. |last2=Barbieri | name-list-format = vanc |title=Yen and Jaffe's Reproductive Endocrinology |url=https://books.google.com/books?id=KZ95AAAAQBAJ&pg=PA236 |date=13 September 2013 |publisher=Elsevier Health Sciences |isbn=978-1-4557-2758-2 |pages=236–237 |deadurl=no |archiveurl=https://web.archive.org/web/20170114164554/https://books.google.com/books?id=KZ95AAAAQBAJ&pg=PA236 |archivedate=14 January 2017 |df=dmy-all}}</ref><ref name="WilsonNizet2015">{{cite book |first1=Christopher B. |last1=Wilson |first2=Victor |last2=Nizet |first3=Yvonne |last3=Maldonado |first4=Jerome O. |last4=Klein |first5=Jack S. |last5=Remington | name-list-format = vanc |title=Remington and Klein's Infectious Diseases of the Fetus and Newborn Infant |url=https://books.google.com/books?id=VuZ1BwAAQBAJ&pg=PA190 |year=2015 |publisher=Elsevier Health Sciences |isbn=978-0-323-24147-2 |pages=190– |deadurl=no |archiveurl=https://web.archive.org/web/20170114165129/https://books.google.com/books?id=VuZ1BwAAQBAJ&pg=PA190 |archivedate=14 January 2017 |df=dmy-all}}</ref> It has been found that very low levels of estrogen can induce breast development in the presence of low or no androgen signaling.<ref name="IIIBarbieri2013b" /><ref name="YenJaffe2001">{{cite book |first1=Samuel S. C. |last1=Yen |first2=Robert B. |last2=Jaffe |first3=Robert L. |last3=Barbieri | name-list-format = vanc |title=Endocrinología de la reproducción: fisiología, fisiopatología y manejo clínico |url=https://books.google.com/books?id=eeb9izSYxMsC&pg=PA303 |year=2001 |publisher=Ed. Medic Panamericana |isbn=978-950-06-2538-8 |pages=303–}}</ref><ref name="PinskyErickson1999">{{cite book |first1=Leonard |last1=Pinsky |first2=Robert P. |last2=Ericsson |first3=R. Neil |last3=Schimke | name-list-format = vanc |title=Genetic Disorders of Human Sexual Development |url=https://books.google.com/books?id=yVTJkOqw_50C&pg=PA215 |year=1999 |publisher=Oxford University Press |isbn=978-0-19-510907-8 |pages=215–}}</ref> In accordance, bicalutamide not only induces gynecomastia at a high rate when given to men as a monotherapy,<ref name="JamesonGroot2015" /> it results in a higher incidence of gynecomastia in combination with a {{abbr|GnRH|gonadotropin-releasing hormone}} analogue relative to {{abbr|GnRH|gonadotropin-releasing hormone}} analogue treatment alone (in spite of the presence of only castrate levels of estrogen in both cases).<ref name="WassersugOliffe2009">{{cite journal |vauthors=Wassersug RJ, Oliffe JL |title=The social context for psychological distress from iatrogenic gynecomastia with suggestions for its management |journal=The Journal of Sexual Medicine |volume=6 |issue=4 |pages=989–1000 |date=April 2009 |pmid=19175864 |doi=10.1111/j.1743-6109.2008.01053.x |quote=By themselves, the LH-RH agonists do not produce much gynecomastia (ie, estimates as low as 4.4%) [13], but in conjunction with the typically prescribed antiandrogens (flutamide, bicalutamide, and nilutamide), gynecomastia is more common (49–68%) [13].}}</ref> |
|||
A study of men treated with {{abbr|NSAA|nonsteroidal antiandrogen}} (flutamide or bicalutamide) monotherapy for prostate cancer found that {{abbr|NSAAs|nonsteroidal antiandrogens}} induced full [[lactiferous duct|ductal development]] and moderate [[lobuloalveolar]] development of the breasts from a [[histology|histological]] standpoint.<ref name="KanhaiHage2000">{{cite journal |vauthors=Kanhai RC, Hage JJ, van Diest PJ, Bloemena E, Mulder JW |title=Short-term and long-term histologic effects of castration and estrogen treatment on breast tissue of 14 male-to-female transsexuals in comparison with two chemically castrated men |journal=The American Journal of Surgical Pathology |volume=24 |issue=1 |pages=74–80 |date=January 2000 |pmid=10632490 |doi=10.1097/00000478-200001000-00009}}</ref><ref name="Lawrence2007">{{cite book | editor-first1 = Ilan H. | editor-last1 = Meyer | editor-first2 = Mary E.| editor-last2 = Northridge |title=The Health of Sexual Minorities Public Health Perspectives on Lesbian, Gay, Bisexual and Transgender Populations |date=2006 |publisher=Springer |location=New York |isbn=978-0-387-28871-0 |chapter=Transgender Health Concerns |first=Anne A. |last=Lawrence | name-list-format = vanc |pages=476 |doi=10.1007/978-0-387-31334-4_19}}</ref><ref name="Rosen2009">{{cite book |first=Paul Peter |last=Rosen | name-list-format = vanc |title=Rosen's Breast Pathology |url=https://books.google.com/books?id=_swaovkfRMMC&pg=PA31 |year=2009 |publisher=Lippincott Williams & Wilkins |location=Philadelphia |isbn=978-0-7817-7137-5 |pages=31– |edition=3}}</ref> The study also found that, in contrast, treatment of transgender women with estrogen and {{abbr|CPA|cyproterone acetate}} (which is progestogenic in addition to antiandrogenic, unlike {{abbr|NSAAs|nonsteroidal antiandrogens}}) resulted in full lobuloalevolar development, as well as pregnancy-like [[breast hyperplasia]] in two of the subjects.<ref name="KanhaiHage2000" /><ref name="Rosen2009" /> In addition, it was observed that the lobuloalveolar maturation reversed upon discontinuation of {{abbr|CPA|cyproterone acetate}} after [[sex reassignment surgery]] (that is, surgical castration) in these individuals.<ref name="KanhaiHage2000" /> It was concluded that progestogen in addition to antiandrogen/estrogen treatment is required for the induction of full female-like histological breast development (i.e., that includes complete lobuloalveolar maturation), and that continued progestogen treatment is necessary to maintain such maturation.<ref name="KanhaiHage2000" /><ref name="Lawrence2007" /> It should be noted however that although these findings may have important implications in the contexts of [[lactation]] and breastfeeding, epithelial tissue accounts for approximately only 10% of breast volume (with the bulk of the breasts (80–90%) being represented by [[stroma (animal tissue)|stromal]] or [[adipose tissue|adipose]] tissue),<ref name="pmid16728564">{{cite journal |vauthors=Lorincz AM, Sukumar S |title=Molecular links between obesity and breast cancer |journal=Endocrine-related Cancer |volume=13 |issue=2 |pages=279–92 |year=2006 |pmid=16728564 |doi=10.1677/erc.1.00729 |url= |quote=Adipocytes make up the bulk of the human breast, with epithelial cells accounting for only approximately 10% of human breast volume.}}</ref><ref name="pmid11149569">{{cite journal |vauthors=Howard BA, Gusterson BA |title=Human breast development |journal=Journal of Mammary Gland Biology and Neoplasia |volume=5 |issue=2 |pages=119–37 |year=2000 |pmid=11149569 |doi= |url= |quote=In the stroma, there is an increase in the amount of fibrous and fatty tissue, with the adult nonlactating breast consisting of 80% or more of stroma.}}</ref><ref name="Sperling2014">{{cite book |first=Mark A. |last=Sperling | name-list-format = vanc |title=Pediatric Endocrinology |url=https://books.google.com/books?id=GgXnAgAAQBAJ&pg=PA598 |date=10 April 2014 |publisher=Elsevier Health Sciences |isbn=978-1-4557-5973-6 |pages=598– |quote=Estrogen stimulates the nipples to grow, mammary terminal duct branching to progress to the stage at which ductules are formed, and fatty stromal growth to increase until it constitutes about 85% of the mass of the breast. [...] Lobulation appears around menarche, when multiple blind saccular buds form by branching of the terminal ducts. These effects are due to the presence of progesterone. [...] Full alveolar development normally only occurs during pregnancy under the influence of additional progesterone and prolactin.}}</ref><ref name="pmid22206682">{{cite journal |vauthors=Hagisawa S, Shimura N, Arisaka O |title=Effect of excess estrogen on breast and external genitalia development in growth hormone deficiency |journal=Journal of Pediatric and Adolescent Gynecology |volume=25 |issue=3 |pages=e61–3 |year=2012 |pmid=22206682 |doi=10.1016/j.jpag.2011.11.005 |url= |quote=Estrogen stimulates growth of the nipples, progression of mammary duct branching to the stage at which ductiles are formed, and fatty stromal growth until it constitutes about 85% of the mass of the breast.}}</ref> and it is uncertain to what extent, if any, that development of lobuloalveolar structures (a form of [[epithelium|epithelial]] tissue) contributes to breast size and/or shape.<ref name="WierckxGooren2014" /> |
|||
====Effects on spermatogenesis and fertility==== |
|||
[[Spermatogenesis]] and [[male fertility]] are dependent on {{abbr|FSH|follicle-stimulating hormone}}, {{abbr|LH|luteinizing hormone}}, and high levels of testosterone within the testicles.<ref name="MelmedPolonsky2015">{{cite book |vauthors=Melmed S, Polonsky KS, Reed Larsen P, Kronenberg HM |title=Williams Textbook of Endocrinology |url=https://books.google.com/books?id=YZ8_CwAAQBAJ&pg=PA704 |date=30 November 2015 |publisher=Elsevier Health Sciences |isbn=978-0-323-29738-7 |pages=704–708, 711, 1104}}</ref><ref name="Aiman2012">{{cite book |author=J. Aiman |title=Infertility: Diagnosis and Management |url=https://books.google.com/books?id=D4_TBwAAQBAJ&pg=PA182 |date=6 December 2012 |publisher=Springer Science & Business Media |isbn=978-1-4613-8265-2 |pages=182–}}</ref> {{abbr|LH|Luteinizing hormone}} does not seem to be involved in spermatogenesis outside of its role in inducing production of testosterone by the [[Leydig cell]]s in the [[seminiferous tubule]]s (which make up approximately 80%<ref name="Krohmer2009">{{cite book |first=Randolph W. |last=Kroemer | name-list-format = vanc |title=The Reproductive System |url=https://books.google.com/books?id=GDVfveqBmrcC&pg=PA51 |year=2009 |publisher=Infobase Publishing |isbn=978-1-4381-3083-5 |pages=51–}}</ref> of the bulk of the testes),<ref name="pmid4062226">{{cite journal |vauthors=Fody EP, Walker EM |title=Effects of drugs on the male and female reproductive systems |journal=Ann. Clin. Lab. Sci. |volume=15 |issue=6 |pages=451–8 |year=1985 |pmid=4062226 |doi= |url=}}</ref> whereas this is not the case for {{abbr|FSH|follicle-stimulating hormone}}, which is importantly involved.<ref name="pmid15804862">{{cite journal |vauthors=Liu YX |title=Control of spermatogenesis in primate and prospect of male contraception |journal=Arch. Androl. |volume=51 |issue=2 |pages=77–92 |year=2005 |pmid=15804862 |doi=10.1080/01485010490485768 |url=}}</ref><ref name="pmid19682538">{{cite journal |vauthors=Cheng CY, Wong EW, Yan HH, Mruk DD |title=Regulation of spermatogenesis in the microenvironment of the seminiferous epithelium: new insights and advances |journal=Mol. Cell. Endocrinol. |volume=315 |issue=1–2 |pages=49–56 |year=2010 |pmid=19682538 |pmc=3516447 |doi=10.1016/j.mce.2009.08.004 |url=}}</ref> In accordance with the fact that the testes are the source of 95% of circulating testosterone in the body, local levels of testosterone inside of the testes are extremely high, ranging from 20- to 200-fold higher than circulating concentrations.<ref name="SchillComhaire2006">{{cite book |first1=Wolf-Bernhard |last1=Schill |first2=Frank H. |last2=Comhaire |first3=Timothy B. |last3=Hargreave | name-list-format = vanc |title=Andrology for the Clinician |url=https://books.google.com/books?id=5Ts_AAAAQBAJ&pg=PA76 |date=26 August 2006 |publisher=Springer Science & Business Media |isbn=978-3-540-33713-3 |pages=76– |deadurl=no |archiveurl=https://web.archive.org/web/20160526220017/https://books.google.com/books?id=5Ts_AAAAQBAJ&pg=PA76 |archivedate=26 May 2016 |df=dmy-all}}</ref><ref name="NieschlagBehre2012" /> Moreover, high levels of testosterone within the testes are required for spermatogenesis,<ref name="Aiman2012" /> although only a small fraction (5–10%) of normal levels appears to actually be necessary for spermatogenesis.<ref name="NieschlagBehre2012" /><ref name="Cheng2009">{{cite book |first=C.Y. |last=Cheng | name-list-format = vanc |title=Molecular Mechanisms in Spermatogenesis |url=https://books.google.com/books?id=tdpVNN80_r0C&pg=PA258 |date=24 October 2009 |publisher=Springer Science & Business Media |isbn=978-0-387-09597-4 |pages=258–}}</ref> |
|||
Unlike with antigonadotropic antiandrogens like {{abbr|CPA|cyproterone acetate}} and {{abbr|GnRH|gonadotropin-releasing hormone}} analogues, it has been reported that bicalutamide monotherapy (at 50 mg/day) has very little effect on the [[ultrastructure]] of the testes and on [[sperm]] maturation in humans even after long-term therapy (>4 years).<ref name="MorganteGradini2001">{{cite journal |vauthors=Morgante E, Gradini R, Realacci M, Sale P, D'Eramo G, Perrone GA, Cardillo MR, Petrangeli E, Russo M, Di Silverio F |title=Effects of long-term treatment with the anti-androgen bicalutamide on human testis: an ultrastructural and morphometric study |journal=Histopathology |volume=38 |issue=3 |pages=195–201 |date=March 2001 |pmid=11260298 |doi=10.1046/j.1365-2559.2001.01077.x}}</ref> This may be explained by the extremely high local levels of testosterone in the testes, in that it is likely that systemic bicalutamide therapy is unable to achieve concentrations of the drug within the testes that are able to considerably block androgen signaling in this part of the body.<ref name="MorganteGradini2001" /> This is particularly so considering that bicalutamide increases circulating testosterone levels, and by extension gonadal testosterone production, by up to two-fold in males,<ref name="pmid7537602" /> and that only a small fraction of normal intratesticular testosterone levels, and by extension androgen action, appears to be necessary to maintain spermatogenesis.<ref name="NieschlagBehre2012" /><ref name="Cheng2009" /> |
|||
In contrast to bicalutamide and other pure antiandrogens or {{abbr|NSAAs|nonsteroidal antiandrogens}}, antigonadotropic antiandrogens suppress gonadotropin secretion, which in turn diminishes testosterone production by the testes as well as the maintenance of the testes by {{abbr|FSH|follicle-stimulating hormone}}, resulting in [[atrophy]] and loss of their function.<ref name="Johnson2003">{{cite book |first=Leonard R. |last=Johnson | name-list-format = vanc |title=Essential Medical Physiology |url=https://books.google.com/books?id=Ql10m-_q3nMC&pg=PA731 |date=14 October 2003 |publisher=Academic Press |isbn=978-0-08-047270-6 |pages=731– |deadurl=no |archiveurl=https://web.archive.org/web/20170215093206/https://books.google.com/books?id=Ql10m-_q3nMC&pg=PA731 |archivedate=15 February 2017 |df=dmy-all}}</ref> As such, bicalutamide and other {{abbr|NSAAs|nonsteroidal antiandrogens}} may uniquely have the potential to preserve testicular function and spermatogenesis and thus male fertility relative to alternative therapies.<ref name="MorganteGradini2001" /><ref name="Mulhall2013">{{cite book |first=John P. |last=Mulhall |name-list-format=vanc |title=Fertility Preservation in Male Cancer Patients |url=https://books.google.com/books?id=97wgAwAAQBAJ&pg=PA84 |date=21 February 2013 |publisher=Cambridge University Press |isbn=978-1-139-61952-3 |pages=84– |deadurl=no |archiveurl=https://web.archive.org/web/20160429171718/https://books.google.com/books?id=97wgAwAAQBAJ&pg=PA84 |archivedate=29 April 2016 |df=dmy-all}}</ref> In accordance with this notion, a study found that prolonged, high-dose bicalutamide treatment had minimal effects on fertility in male rats.<ref name="IswaranImai1997" /> However, another study found that low-dose bicalutamide administration resulted in testicular atrophy and reduced the [[germ cell]] count in the testes of male rats by almost 50%, though the rate of successful [[fertilization]] and pregnancy following [[mating]] was not assessed.<ref>{{cite journal |url=http://applications.emro.who.int/imemrf/Pak_Armed_Forces_Med_J/Pak_Armed_Forces_Med_J_2011_61_3_325_329.pdf |vauthors=Khursheed A, Minhas LA, Diaz WA |title=Histomorphometric study of effects of bicalutamide on spermatogenesis in male rats |journal=Pakistan Armed Forces Medical Journal |date=September 2011 |issue=3 |deadurl=no |archiveurl=https://web.archive.org/web/20160623201722/http://applications.emro.who.int/imemrf/Pak_Armed_Forces_Med_J/Pak_Armed_Forces_Med_J_2011_61_3_325_329.pdf |archivedate=23 June 2016 |df=dmy-all}}</ref> |
|||
Treatment of men with [[exogenous]] testosterone or other {{abbr|AAS|anabolic–androgenic steroid}} results in suppression of gonadotropin secretion and gonadal testosterone production due to their antigonadotropic effects or activation of the {{abbr|AR|androgen receptor}} in the pituitary gland, resulting in inhibition or abolition of spermatogenesis and fertility:<ref name="DohleSmit2003">{{cite journal |vauthors=Dohle GR, Smit M, Weber RF |title=Androgens and male fertility |journal=World Journal of Urology |volume=21 |issue=5 |pages=341–5 |date=November 2003 |pmid=14566423 |doi=10.1007/s00345-003-0365-9}}</ref> |
|||
{{Quotation|''Treatment of an infertile man with testosterone does [not] improve spermatogenesis, since exogenous administrated testosterone and its metabolite estrogen will suppress both {{abbr|GnRH|gonadotropin-releasing hormone}} production by the hypothalamus and luteinizing hormone production by the pituitary gland and subsequently suppress testicular testosterone production. Also, high levels of testosterone are needed inside the testis and this can never be accomplished by oral or parenteral administration of androgens. Suppression of testosterone production by the leydig cells will result in a deficient spermatogenesis, as can be seen in men taking anabolic–androgenic steroids.''<ref name="DohleSmit2003" />}} |
|||
In contrast, pure {{abbr|AR|androgen receptor}} antagonists would, in theory, result in the opposite (although reduced semen volume and sexual dysfunction may occur):<ref name="Basu2011">{{cite book |vauthors=Basu SC |title=Male Reproductive Dysfunction |url=https://books.google.com/books?id=8VMO3Vpqi0cC&pg=PA323 |date=15 December 2011 |publisher=Jaypee Brothers Medical Publishers Pvt. Ltd. |isbn=978-93-5025-703-6 |pages=323–}}</ref> |
|||
{{Quotation|''It is theoretically a sound hypothesis that the spermatogenesis can be increased by indirectly stimulating {{abbr|FSH|follicle-stimulating hormone}} and {{abbr|LH|luteinizing hormone}} secretions from the pituitary gland. However, for this to fructify, it requires the use of testosterone antagonist to nullify the negative feedback effect of circulating testosterone on the release of {{abbr|FSH|follicle-stimulating hormone}} and {{abbr|LH|luteinizing hormone}}, thus augmenting the secretion of testosterone and spermatogenesis. Unfortunately, a testosterone antagonist will be unacceptable to males, as it may reduce secondary sexual functions including erection and ejaculation that is vital for the successful fertilization.''<ref name="Basu2011" />}} |
|||
Although bicalutamide alone would appear to have minimal detrimental effect on spermatogenesis and male fertility, other hormonal agents that bicalutamide may be combined with, including {{abbr|GnRH|gonadotropin-releasing hormone}} analogues and particularly estrogens (as in transgender hormone therapy), can have a considerable detrimental effect on fertility.<ref name="JonesReiter2016" /><ref name="PayneHardy2007">{{cite book |first1=Anita H. |last1=Payne |first2=Matthew P. |last2=Hardy | name-list-format = vanc |title=The Leydig Cell in Health and Disease |url=https://books.google.com/books?id=x4ttqKIAOg0C&pg=PA422 |date=28 October 2007 |publisher=Springer Science & Business Media |isbn=978-1-59745-453-7 |pages=422–431 |quote=Estrogens are highly efficient inhibitors of the hypothalamic-hypophyseal-testicular axis (212–214). Aside from their negative feedback action at the level of the hypothalamus and pituitary, direct inhibitory effects on the testis are likely (215,216). [...] The histology of the testes [with estrogen treatment] showed disorganization of the seminiferous tubules, vacuolization and absence of lumen, and compartmentalization of spermatogenesis.}}</ref> This is largely a consequence of their antigonadotropic activity.<ref name="PayneHardy2007" /> Antigonadotropic agents like high-dose {{abbr|CPA|cyproterone acetate}},<ref name="WakelinMaibach2002">{{cite book |first1=Sarah H. |last1=Wakelin |first2=Howard I. |last2=Maibach |first3=Clive B. |last3=Archer | name-list-format = vanc |title=Systemic Drug Treatment in Dermatology: A Handbook |url=https://books.google.com/books?id=F1ZiAgAAQBAJ&pg=PA32 |date=1 June 2002 |publisher=CRC Press |isbn=978-1-84076-013-2 |pages=32– |quote=[Cyproterone acetate] inhibits spermatogenesis and produces reversible infertility (but is not a male contraceptive). |deadurl=no |archiveurl=https://web.archive.org/web/20140725205131/http://books.google.com/books?id=F1ZiAgAAQBAJ&pg=PA32 |archivedate=25 July 2014 |df=dmy-all}}</ref><ref name="pmid8005205">{{cite journal |vauthors=Neumann F |title=The antiandrogen cyproterone acetate: discovery, chemistry, basic pharmacology, clinical use and tool in basic research |journal=Exp. Clin. Endocrinol. |volume=102 |issue=1 |pages=1–32 |year=1994 |pmid=8005205 |doi=10.1055/s-0029-1211261 |url= |quote=Spermatogenesis is also androgen-dependent and is inhibited by CPA, meaning that patients treated with high doses of CPA are sterile (Figure 23). All the effects of CPA are fully reversible.}}</ref> high-dose androgens (e.g., [[testosterone ester]]s), and {{abbr|GnRH|gonadotropin-releasing hormone}} antagonists (though notably not {{abbr|GnRH|gonadotropin-releasing hormone}} agonists) produce hypogonadism and high rates of severe or complete infertility (e.g., severe [[oligospermia]] or complete [[azoospermia]]) in men.<ref name="PayneHardy2007" /> However, these effects are fully and often rapidly reversible with their discontinuation, even after prolonged treatment.<ref name="PayneHardy2007" /><ref name="pmid8005205" /> In contrast, while estrogens at sufficiently high dosages similarly are able to produce hypogonadism and to abolish or severely impair spermatogenesis,<ref name="JonesReiter2016">{{cite journal |last1=Jones |first1=C. A. |last2=Reiter |first2=L. |last3=Greenblatt |first3=E. | name-list-format = vanc |title=Fertility preservation in transgender patients |journal=International Journal of Transgenderism |volume=17 |issue=2 |year=2016 |pages=76–82 |issn=1553-2739 |doi=10.1080/15532739.2016.1153992 |quote=Traditionally, patients have been advised to cryopreserve sperm prior to starting cross-sex hormone therapy as there is a potential for a decline in sperm motility with high-dose estrogen therapy over time (Lubbert et al., 1992). However, this decline in fertility due to estrogen therapy is controversial due to limited studies.}}</ref> this is not necessarily reversible in the case of estrogens and can be long-lasting after prolonged exposure.<ref name="PayneHardy2007" /><ref name="Salam2003">{{cite book |first=Muhammad A. |last=Salam | name-list-format =vanc |title=Principles & Practice of Urology: A Comprehensive Text |url=https://books.google.com/books?id=y50kTcCCfEcC&pg=PA684 |year=2003 |publisher=Universal-Publishers |isbn=978-1-58112-412-5 |pages=684– |quote=Estrogens act primarily through negative feedback at the hypothalamic-pituitary level to reduce LH secretion and testicular androgen synthesis. [...] Interestingly, if the treatment with estrogens is discontinued after 3 yr. of uninterrupted exposure, serum testosterone may remain at castration levels for up to another 3 yr. This prolonged suppression is thought to result from a direct effect of estrogens on the Leydig cells.}}</ref> The difference is attributed to an apparently unique, direct adverse effect of high concentrations of estrogens on the Leydig cells of the testes.<ref name="PayneHardy2007" /><ref name="Salam2003" /> |
|||
====Other activities==== |
====Other activities==== |
||
Bicalutamide has been found to act as an [[enzyme inhibitor|inhibitor]] or [[enzyme inducer|inducer]] of certain [[cytochrome P450]] [[enzyme]]s including [[CYP3A4]], [[CYP2C9]], [[CYP2C19]], and [[CYP2D6]] in [[preclinical research]], but no evidence of this has been found in humans treated with up to 150 mg/day.<ref name="Cockshott2004" /> It has also been identified ''[[in vitro]]'' as a strong inhibitor of [[CYP27A1]] (cholesterol 27-hydroxylase) and as an inhibitor of [[CYP46A1]] (cholesterol 24-hydroxylase), but this has yet to be assessed or confirmed ''[[in vivo]]'' or in humans and the clinical significance remains unknown.<ref name="pmid26082378">{{cite journal |vauthors=Mast N, Lin JB, Pikuleva IA |title=Marketed Drugs Can Inhibit Cytochrome P450 27A1, a Potential New Target for Breast Cancer Adjuvant Therapy |journal=Molecular Pharmacology |volume=88 |issue=3 |pages=428–36 |date=September 2015 |pmid=26082378 |doi=10.1124/mol.115.099598 |pmc=4551053}}</ref><ref name="MastZheng2013">{{cite journal |vauthors=Mast N, Zheng W, Stout CD, Pikuleva IA |title=Binding of a cyano- and fluoro-containing drug bicalutamide to cytochrome P450 46A1: unusual features and spectral response |journal=The Journal of Biological Chemistry |volume=288 |issue=7 |pages=4613–24 |date=February 2013 |pmid=23288837 |doi=10.1074/jbc.M112.438754 |pmc=3576067}}</ref> Bicalutamide has been found to be a [[P-glycoprotein]] (ABCB1) inhibitor.<ref name="ZhuLiu2015">{{cite journal |vauthors=Zhu Y, Liu C, Armstrong C, Lou W, Sandher A, Gao AC |title=Antiandrogens Inhibit ABCB1 Efflux and ATPase Activity and Reverse Docetaxel Resistance in Advanced Prostate Cancer |journal=Clinical Cancer Research |volume=21 |issue=18 |pages=4133–42 |date=September 2015 |pmid=25995342 |doi=10.1158/1078-0432.CCR-15-0269 |pmc=4573793}}</ref><ref name="Fenner2015">{{cite journal |vauthors=Fenner A |title=Prostate cancer: Antiandrogens reverse docetaxel resistance via ABCB1 inhibition |journal=Nature Reviews. Urology |volume=12 |issue=7 |pages=361 |date=July 2015 |pmid=26057062 |doi=10.1038/nrurol.2015.135}}</ref><ref name="pmid26309896">{{cite journal |vauthors=Armstrong CM, Gao AC |title=Drug resistance in castration resistant prostate cancer: resistance mechanisms and emerging treatment strategies |journal=American Journal of Clinical and Experimental Urology |volume=3 |issue=2 |pages=64–76 |year=2015 |pmid=26309896 |pmc=4539108 |doi=}}</ref> Like other first-generation {{abbr|NSAAs|nonsteroidal antiandrogens}} and enzalutamide, it has been found to act as a weak [[negative allosteric modulator|non-competitive inhibitor]] of [[GABAA receptor|GABA<sub>A</sub> receptor]]-mediated [[electric current|current]]s ''in vitro'' (IC<sub>50</sub> = 5.2 μM). However, unlike enzalutamide, bicalutamide has not been found to be associated with [[seizure]]s or other related adverse [[central nervous system|central]] effects, so the clinical relevance of this finding is uncertain.<ref name="FosterCar2011">{{cite journal |vauthors=Foster WR, Car BD, Shi H, Levesque PC, Obermeier MT, Gan J, Arezzo JC, Powlin SS, Dinchuk JE, Balog A, Salvati ME, Attar RM, Gottardis MM |title=Drug safety is a barrier to the discovery and development of new androgen receptor antagonists |journal=The Prostate |volume=71 |issue=5 |pages=480–8 |date=April 2011 |pmid=20878947 |doi=10.1002/pros.21263}}</ref><ref name="BarrishCarter2010">{{cite book |first1=Joel |last1=Barrish |first2=Percy |last2=Carter |first3=Peter |last3=Cheng | name-list-format = vanc |title=Accounts in Drug Discovery: Case Studies in Medicinal Chemistry |url=https://books.google.com/books?id=GlrOSAvRlJsC&pg=PA127 |year=2010 |publisher=Royal Society of Chemistry |isbn=978-1-84973-126-3 |pages=127–}}</ref> |
|||
It has been reported that bicalutamide may have the potential to inhibit the [[enzyme]]s [[CYP3A4]] and, to a lesser extent, [[CYP2C9]], [[CYP2C19]], and [[CYP2D6]], based on ''[[in vitro]]'' research.<ref name="Cockshott2004" /> However, no relevant inhibition of CYP3A4 has been observed ''in vivo'' with bicalutamide at a dose of 150 mg (using [[midazolam]] as a specific marker of CYP3A4 activity).<ref name="Cockshott2004" /> In animals, bicalutamide has been found to be an [[enzyme inducer|inducer]] of certain [[cytochrome P450]] enzymes.<ref name="Cockshott2004" /> However, dosages of 150 mg/day or less have shown no evidence of this in humans.<ref name="Cockshott2004" /> |
|||
Bicalutamide has been identified as a strong [[CYP27A1]] (cholesterol 27-hydroxylase) inhibitor ''in vitro''.<ref name="pmid26082378">{{cite journal |vauthors=Mast N, Lin JB, Pikuleva IA |title=Marketed Drugs Can Inhibit Cytochrome P450 27A1, a Potential New Target for Breast Cancer Adjuvant Therapy |journal=Molecular Pharmacology |volume=88 |issue=3 |pages=428–36 |date=September 2015 |pmid=26082378 |doi=10.1124/mol.115.099598 |pmc=4551053}}</ref> CYP27A1 converts [[cholesterol]] into [[27-hydroxycholesterol]], an [[oxysterol]] that has multiple biological functions including direct, tissue-specific activation of the {{abbr|ER|estrogen receptor}} (it has been characterized as a selective estrogen receptor modulator) and the [[liver X receptor]].<ref name="pmid26082378" /> 27-Hydroxycholesterol has been found to increase {{abbr|ER|estrogen receptor}}-positive breast cancer cell growth via its estrogenic action, and hence, it has been proposed that bicalutamide and other CYP27A1 inhibitors may be effective as [[adjuvant therapy|adjuvant therapies]] to [[aromatase inhibitor]]s in the treatment of {{abbr|ER|estrogen receptor}}-positive breast cancer.<ref name="pmid26082378" /> In addition to CYP27A1, bicalutamide has been found to bind to and inhibit [[CYP46A1]] (cholesterol 24-hydroxylase) ''in vitro'', but this has yet to be assessed and confirmed ''in vivo''.<ref name="MastZheng2013">{{cite journal |vauthors=Mast N, Zheng W, Stout CD, Pikuleva IA |title=Binding of a cyano- and fluoro-containing drug bicalutamide to cytochrome P450 46A1: unusual features and spectral response |journal=The Journal of Biological Chemistry |volume=288 |issue=7 |pages=4613–24 |date=February 2013 |pmid=23288837 |doi=10.1074/jbc.M112.438754 |pmc=3576067}}</ref> |
|||
Bicalutamide, as well as enzalutamide, have been found to act as [[transporter blocker|inhibitors]] of [[P-glycoprotein]] efflux and [[ATPase]] activity.<ref name="ZhuLiu2015">{{cite journal |vauthors=Zhu Y, Liu C, Armstrong C, Lou W, Sandher A, Gao AC |title=Antiandrogens Inhibit ABCB1 Efflux and ATPase Activity and Reverse Docetaxel Resistance in Advanced Prostate Cancer |journal=Clinical Cancer Research |volume=21 |issue=18 |pages=4133–42 |date=September 2015 |pmid=25995342 |doi=10.1158/1078-0432.CCR-15-0269 |pmc=4573793}}</ref><ref name="Fenner2015">{{cite journal |vauthors=Fenner A |title=Prostate cancer: Antiandrogens reverse docetaxel resistance via ABCB1 inhibition |journal=Nature Reviews. Urology |volume=12 |issue=7 |pages=361 |date=July 2015 |pmid=26057062 |doi=10.1038/nrurol.2015.135}}</ref><ref name="pmid26309896">{{cite journal |vauthors=Armstrong CM, Gao AC |title=Drug resistance in castration resistant prostate cancer: resistance mechanisms and emerging treatment strategies |journal=American Journal of Clinical and Experimental Urology |volume=3 |issue=2 |pages=64–76 |year=2015 |pmid=26309896 |pmc=4539108 |doi=}}</ref> This action may reverse [[docetaxel]] resistance in prostate cancer cells by reducing [[membrane transport|transport]] of the drug out of these cells.<ref name="ZhuLiu2015" /><ref name="Fenner2015" /><ref name="pmid26309896" /> |
|||
All of the {{abbr|NSAAs|nonsteroidal antiandrogens}} approved for the treatment of prostate cancer have been found to possess an off-target action of acting as weak [[non-competitive inhibition|non-competitive inhibitors]] of human GABA<sub>A</sub> receptor currents ''in vitro'' to varying extents.<ref name="FosterCar2011">{{cite journal |vauthors=Foster WR, Car BD, Shi H, Levesque PC, Obermeier MT, Gan J, Arezzo JC, Powlin SS, Dinchuk JE, Balog A, Salvati ME, Attar RM, Gottardis MM |title=Drug safety is a barrier to the discovery and development of new androgen receptor antagonists |journal=The Prostate |volume=71 |issue=5 |pages=480–8 |date=April 2011 |pmid=20878947 |doi=10.1002/pros.21263}}</ref><ref name="BarrishCarter2010">{{cite book |first1=Joel |last1=Barrish |first2=Percy |last2=Carter |first3=Peter |last3=Cheng | name-list-format = vanc |title=Accounts in Drug Discovery: Case Studies in Medicinal Chemistry |url=https://books.google.com/books?id=GlrOSAvRlJsC&pg=PA127 |year=2010 |publisher=Royal Society of Chemistry |isbn=978-1-84973-126-3 |pages=127–}}</ref> The IC<sub>50</sub> values are 44 μM for flutamide (as hydroxyflutamide), 21 μM for nilutamide, 5.2 μM for bicalutamide, and 3.6 μM for enzalutamide.<ref name="FosterCar2011" /> In addition, flutamide, nilutamide, and enzalutamide have been found to cause [[convulsion]]s and/or death in mice at sufficiently high doses.<ref name="FosterCar2011" /> Bicalutamide was notably not found to do this, but this was likely simply due to the limited [[central nervous system]] penetration of bicalutamide in this species.<ref name="FosterCar2011" /> In any case, enzalutamide is the only approved {{abbr|NSAA|nonsteroidal antiandrogen}} that has been found to be associated with a significantly increased incidence of seizures and other associated side effects clinically, so the relevance of the aforementioned findings with regard to bicalutamide and the other {{abbr|NSAAs|nonsteroidal antiandrogens}} is unclear.<ref name="FosterCar2011" /> |
|||
===Pharmacokinetics=== |
===Pharmacokinetics=== |
||
Though its absolute [[bioavailability]] in humans is unknown, bicalutamide is known to be extensively and well-[[absorption (pharmacokinetics)|absorbed]].<ref name="Cockshott2004" /><ref name="Dart2004" /> Its absorption is not affected by [[food]].<ref name="Dart2004" /><ref name="Weber2015" /> The absorption of bicalutamide is linear at doses up to 150 mg/day and is saturable at doses above this, with no further increases in [[steady state (pharmacokinetics)|steady-state levels]] of bicalutamide occurring at doses above 300 mg/day.<ref name="Cockshott2004" /><ref name="Wellington2006" /><ref name="KolvenbagBlackledge1998">{{cite journal |vauthors=Kolvenbag GJ, Blackledge GR, Gotting-Smith K |title=Bicalutamide (Casodex) in the treatment of prostate cancer: history of clinical development |journal=The Prostate |volume=34 |issue=1 |pages=61–72 |date=January 1998 |pmid=9428389 |doi=10.1002/(SICI)1097-0045(19980101)34:1<61::AID-PROS8>3.0.CO;2-N}}</ref><ref name="TYRRElLIversen2006">{{cite journal |vauthors=Tyrrell CJ, Iversen P, Tammela T, Anderson J, Björk T, Kaisary AV, Morris T |title=Tolerability, efficacy and pharmacokinetics of bicalutamide 300 mg, 450 mg or 600 mg as monotherapy for patients with locally advanced or metastatic prostate cancer, compared with castration |journal=BJU International |volume=98 |issue=3 |pages=563–72 |date=September 2006 |pmid=16771791 |doi=10.1111/j.1464-410X.2006.06275.x}}</ref> Whereas absorption of (''R'')-bicalutamide is slow, (''S'')-bicalutamide is much more rapidly absorbed.<ref name="Cockshott2004" /> Steady-state concentrations of the drug are reached after 4 to 12 months of treatment independently of dosage, with a 10- to 20-fold progressive accumulation in levels of (''R'')-bicalutamide.<ref name="Wellington2006" /><ref name="pmid8717470">{{cite journal |vauthors=Blackledge GR |title=Clinical progress with a new antiandrogen, Casodex (bicalutamide) |journal=European Urology |volume=29 Suppl 2 |issue= |pages=96–104 |year=1996 |pmid=8717470 |doi= |url= |quote=Casodex is associated with significantly less gastrointestinal effects (diarrhoea) than the nonsteroidal antiandrogen flutamide (Eulexin, Schering-Plough International). Casodex is not associated with alcohol intolerance, pneumonitis and ocular defects which have been seen with the antiandrogen nilutamide (Anandron, Roussel).}}</ref><ref name="Jr.Lawrence2015" /><ref name="DenisMahler1996">{{cite journal |vauthors=Denis L, Mahler C |title=Pharmacodynamics and pharmacokinetics of bicalutamide: defining an active dosing regimen |journal=Urology |volume=47 |issue=1A Suppl |pages=26–8; discussion 29–32 |date=January 1996 |pmid=8560674 |doi=10.1016/S0090-4295(96)80004-5}}</ref> The long time to steady-state levels is the result of bicalutamide's very long [[elimination half-life]].<ref name="DenisMahler1996" /> Although it takes a long time for bicalutamide to reach steady-state concentrations, it appears to have antiandrogenic efficacy equivalent to that of flutamide (which has a much shorter elimination half-life and reaches steady-state levels much faster) by the end of the first day of treatment.<ref name="pmid8717470" /> Levels of (''R'')-bicalutamide [[Cmax (pharmacology)|peak]] at 31 to 39 hours after a dose.<ref name="Wellington2006" /><ref name="FDALabel" /> |
|||
The pharmacokinetics of bicalutamide are unaffected by food, [[ageing|age]], [[human body weight|body weight]], renal impairment, and mild-to-moderate hepatic impairment.<ref name="Cockshott2004" /><ref name="DenisMahler1996" /> However, it has been observed that steady-state concentrations of bicalutamide are higher in Japanese individuals than in [[Caucasian race|Caucasians]], indicating that [[ethnicity]] may be associated with differences in the pharmacokinetics of bicalutamide in some instances.<ref name="Cockshott2004" /> |
|||
The [[distribution (pharmacology)|tissue distribution]] of bicalutamide is not well-characterized.<ref name="ChuJr.2012">{{cite book |first1=Edward |last1=Chu |first2=Vincent T. |last2=DeVita Jr. |name-list-format = vanc |title=Physicians' Cancer Chemotherapy Drug Manual 2013 |url=https://books.google.com/books?id=E_Q8eIxYlHcC&pg=PA51 |date=28 December 2012 |publisher=Jones & Bartlett Publishers |isbn=978-1-284-04039-5 |pages=51–}}</ref> The amount of bicalutamide in [[semen]] that could potentially be transferred to a female partner during [[sexual intercourse]] is low and is not thought to be important.<ref name="TGALabel" /> Based on [[animal research|animal studies]] with rats and dogs it was thought that bicalutamide could not cross the [[blood–brain barrier]] and hence could not enter the brain.<ref name="HelsenVan den Broeck2014">{{cite journal |vauthors=Helsen C, Van den Broeck T, Voet A, Prekovic S, Van Poppel H, Joniau S, Claessens F |title=Androgen receptor antagonists for prostate cancer therapy |journal=Endocrine-Related Cancer |volume=21 |issue=4 |pages=T105-18 |date=August 2014 |pmid=24639562 |doi=10.1530/ERC-13-0545}}</ref><ref name="FurrTucker1996" /><ref name="Furr1989">{{cite journal |vauthors=Furr BJ |title="Casodex" (ICI 176,334)--a new, pure, peripherally-selective anti-androgen: preclinical studies |journal=Hormone Research |volume=32 Suppl 1 |issue=1 |pages=69–76 |year=1989 |pmid=2533159 |doi=10.1159/000181315}}</ref><ref name="FurrValcaccia1987">{{cite journal |vauthors=Furr BJ, Valcaccia B, Curry B, Woodburn JR, Chesterson G, Tucker H |title=ICI 176,334: a novel non-steroidal, peripherally selective antiandrogen |journal=The Journal of Endocrinology |volume=113 |issue=3 |pages=R7-9 |date=June 1987 |pmid=3625091 |doi=10.1677/joe.0.113R007}}</ref> As such, it was initially thought to be a [[peripherally selective drug|peripherally selective]] antiandrogen.<ref name="HelsenVan den Broeck2014" /><ref name="FurrTucker1996" /> However, subsequent clinical studies found that this was not also the case for humans, indicating species differences; bicalutamide crosses into the human brain and, in accordance, produces effects and side effects consistent with central antiandrogenic action.<ref name="Cockshott2004" /><ref name="IversenMelezinek2001" /><ref name="SolowaySchellhammer1995">{{cite journal |vauthors=Soloway MS, Schellhammer PF, Smith JA, Chodak GW, Vogelzang NJ, Kennealey GT |title=Bicalutamide in the treatment of advanced prostatic carcinoma: a phase II noncomparative multicenter trial evaluating safety, efficacy and long-term endocrine effects of monotherapy |journal=The Journal of Urology |volume=154 |issue=6 |pages=2110–4 |date=December 1995 |pmid=7500470 |doi=10.1016/S0022-5347(01)66709-0}}</ref><ref name="GaoDalton2007">{{cite journal |vauthors=Gao W, Dalton JT |title=Expanding the therapeutic use of androgens via selective androgen receptor modulators (SARMs) |journal=Drug Discovery Today |volume=12 |issue=5–6 |pages=241–8 |date=March 2007 |pmid=17331889 |pmc=2072879 |doi=10.1016/j.drudis.2007.01.003}}</ref><ref name="Cockshott2004" /><ref name="GaoDalton2007" /><ref name="pmid16896883" /> Bicalutamide is highly [[plasma protein binding|plasma protein bound]] (96.1% for racemic bicalutamide, 99.6% for (''R'')-bicalutamide) and is bound mainly to [[human serum albumin|albumin]], with negliglble binding to {{abbr|SHBG|sex hormone-binding globulin}} and [[corticosteroid-binding globulin]].<ref name="LemkeWilliams2008" /><ref name="Cockshott2004" /><ref name="ChuJr.2012" /><ref name="Furr1995">{{cite journal |vauthors=Furr BJ |title=Casodex: preclinical studies and controversies |journal=Annals of the New York Academy of Sciences |volume=761 |issue=1 |pages=79–96 |date=June 1995 |pmid=7625752 |doi=10.1111/j.1749-6632.1995.tb31371.x}}</ref> |
|||
====Absorption==== |
|||
Bicalutamide is extensively and well-absorbed following [[oral administration]],<ref name="Cockshott2004" /> and its absorption is not affected by food.<ref name="Dart2004" /><ref name="Weber2015" /> The [[Bioavailability#Absolute bioavailability|absolute bioavailability]] of bicalutamide in humans is unknown due to its very low [[solubility|water solubility]] and hence lack of an assessable [[intravenous]] formulation.<ref name="Cockshott2004" /><ref name="Dart2004" /> However, the absolute bioavailability of bicalutamide has been found to be high in animals at low doses (72% in rats at 1 mg/kg; 100% in dogs at 0.1 mg/kg), but diminishes with increasing doses such that the bioavailability of bicalutamide is low at high doses (10% in rats at 250 mg/kg; 31% in dogs at 100 mg/kg).<ref name="Cockshott2004" /> In accordance, [[absorption (pharmacokinetics)|absorption]] of (''R'')-bicalutamide in humans is slow and extensive but saturable,<ref name="Wellington2006" /> with steady-state levels increasing linearly at a dosage of up to 150 mg/day and non-linearly at higher dosages.<ref name="Cockshott2004" /> |
|||
Bicalutamide is [[metabolism|metabolized]] in the [[liver]].<ref name="LemkeWilliams2008" /><ref name="Weber2015" /> (''R'')-Bicalutamide is metabolized slowly and almost exclusively via [[hydroxylation]] by [[CYP3A4]] into (''R'')-hydroxybicalutamide.<ref name="Weber2015" /><ref name="Cockshott2004" /><ref name="LemkeWilliams2008" /><ref name="LemkeWilliams2012" /> This [[metabolite]] is then [[glucuronidation|glucuronidated]] by [[UGT1A9]].<ref name="Weber2015" /><ref name="Cockshott2004" /><ref name="GrosseCampeau2013">{{cite journal |vauthors=Grosse L, Campeau AS, Caron S, Morin FA, Meunier K, Trottier J, Caron P, Verreault M, Barbier O |title=Enantiomer selective glucuronidation of the non-steroidal pure anti-androgen bicalutamide by human liver and kidney: role of the human UDP-glucuronosyltransferase (UGT)1A9 enzyme |journal=Basic & Clinical Pharmacology & Toxicology |volume=113 |issue=2 |pages=92–102 |date=August 2013 |pmid=23527766 |pmc=3815647 |doi=10.1111/bcpt.12071 |quote=}}</ref><ref name="Schellhammer2005" /> In contrast to (''R'')-bicalutamide, (''S'')-bicalutamide is metabolized rapidly and mainly by glucuronidation (without hydroxylation).<ref name="Weber2015" /> None of the metabolites of bicalutamide are known to be active and levels of the metabolites are low in plasma, where unchanged biclautamide predominates.<ref name="LemkeWilliams2008" /><ref name="pmid8997470" /><ref name="Cockshott2004" /> Due to the stereoselective metabolism of bicalutamide, (''R'')-bicalutamide has a far longer terminal half-life than (''S'')-bicalutamide and its levels are about 10- to 20-fold higher in comparison following a single dose and 100-fold higher at steady-state.<ref name="Wellington2006" /><ref name="LemkeWilliams2012">{{cite book |first1=Thomas L. |last1=Lemke |first2=David A. |last2=Williams |name-list-format=vanc |title=Foye's Principles of Medicinal Chemistry |url=https://books.google.com/books?id=Sd6ot9ul-bUC&pg=PA1372 |date=24 January 2012 |publisher=Lippincott Williams & Wilkins |isbn=978-1-60913-345-0 |pages=1372–1373 |deadurl=no |archiveurl=https://web.archive.org/web/20160503223616/https://books.google.com/books?id=Sd6ot9ul-bUC&pg=PA1372 |archivedate=3 May 2016 |df=dmy-all}}</ref><ref name="ButlerGovindan2010">{{cite book |first1=Sara K. |last1=Butler |first2=Ramaswamy |last2=Govindan | name-list-format = vanc |title=Essential Cancer Pharmacology: The Prescriber's Guide |url=https://books.google.com/books?id=ZC0oMwt1ZKgC&pg=PA49 |date=25 October 2010 |publisher=Lippincott Williams & Wilkins |isbn=978-1-60913-704-5 |pages=49–}}</ref> (''R'')-Bicalutamide has a relatively long elimination half-life of 5.8 days with a single dose and 7 to 10 days following repeated administration.<ref name="JordanFurr2010">{{cite book |first1=Virgil Craig |last1=Jordan |first2=B. J. A. |last2=Furr |name-list-format=vanc |title=Hormone Therapy in Breast and Prostate Cancer |url=https://books.google.com/books?id=dM0uvBnxiN0C&pg=PA350 |date=5 February 2010 |publisher=Springer Science & Business Media |isbn=978-1-59259-152-7 |pages=350– |deadurl=no |archiveurl=https://web.archive.org/web/20160529061703/https://books.google.com/books?id=dM0uvBnxiN0C&pg=PA350 |archivedate=29 May 2016 |df=dmy-all}}</ref> The long amount of time that (''R'')-bicalutamide stays in the body allows for convenient once-daily dosing.<ref name="JordanFurr2010" /> |
|||
At higher dosages of 100 to 200 mg/day, absorption of bicalutamide is approximately linear, with a small but increasing departure from linearity above 150 mg/day.<ref name="KolvenbagBlackledge1998">{{cite journal |vauthors=Kolvenbag GJ, Blackledge GR, Gotting-Smith K |title=Bicalutamide (Casodex) in the treatment of prostate cancer: history of clinical development |journal=The Prostate |volume=34 |issue=1 |pages=61–72 |date=January 1998 |pmid=9428389 |doi=10.1002/(SICI)1097-0045(19980101)34:1<61::AID-PROS8>3.0.CO;2-N}}</ref> In terms of [[geometric mean]] steady-state concentrations of (''R'')-bicalutamide, the departures from linearity were 4%, 13%, 17%, and 32% with dosages of 100, 150, 200, and 300 mg/day, respectively.<ref name="Cockshott2004" /> There is a plateau in steady-state levels of (''R'')-bicalutamide with bicalutamide dosages above 300 mg/day, and, accordingly, dosages of bicalutamide of 300 to 600 mg/day result in similar circulating concentrations of (''R'')-bicalutamide and similar degrees clinically of efficacy, tolerability, and toxicity.<ref name="Cockshott2004" /><ref name="TYRRElLIversen2006">{{cite journal |vauthors=Tyrrell CJ, Iversen P, Tammela T, Anderson J, Björk T, Kaisary AV, Morris T |title=Tolerability, efficacy and pharmacokinetics of bicalutamide 300 mg, 450 mg or 600 mg as monotherapy for patients with locally advanced or metastatic prostate cancer, compared with castration |journal=BJU International |volume=98 |issue=3 |pages=563–72 |date=September 2006 |pmid=16771791 |doi=10.1111/j.1464-410X.2006.06275.x}}</ref> Relative to 150 mg/day bicalutamide, levels of (''R'')-bicalutamide are about 15% higher at a dosage of 200 mg/day and about 50% higher at a dosage of 300 mg/day.<ref name="TYRRElLIversen2006" /> In contrast to (''R'')-bicalutamide, the inactive enantiomer (''S'')-bicalutamide is much more rapidly absorbed (as well as cleared from circulation).<ref name="Cockshott2004" /> |
|||
Bicalutamide is [[elimination (pharmacology)|eliminated]] in similar proportions in [[feces]] (43%) and [[urine]] (34%), while its metabolites are eliminated roughly equally in [[urine]] and [[bile]].<ref name="LemkeWilliams2008" /><ref name="Weber2015" /><ref name="pmid14748655" /><ref name="pmid22495777" /> Bicalutamide is [[excretion|excreted]] to a substantial extent in unmetabolized form, and both bicalutamide and its metabolites are eliminated mainly as [[glucuronide]] [[conjugation (biochemistry)|conjugate]]s.<ref name="SchellensMcLeod2005" /> The glucuronide conjugates of bicalutamide and its metabolites are eliminated from the circulation rapidly, unlike unconjugated bicalutamide.<ref name="Cockshott2004" /><ref name="Weber2015" /><ref name="AndersonKnoben2001" /> |
|||
{| class="wikitable floatright" |
|||
|+ <small>Pharmacokinetics of bicalutamide<br />pertaining to circulating concentrations</small> |
|||
|- |
|||
! !! 50 mg !! 150 mg |
|||
|- |
|||
| '''[[Cmax (pharmacology)|C<sub>max</sub>]]''' || 0.77 μg/mL<br />(1.8 μmol/L) || 1.4 μg/mL<br />(3.3 μmol/L) |
|||
|- |
|||
| '''[[tmax (pharmacology)|t<sub>max</sub>]]''' || 31 hours || 39 hours |
|||
|- |
|||
| '''[[Steady state (pharmacokinetics)|C<sub>ss</sub>]]''' || 8.9 μg/mL<br />(21 μmol/L) || 22–28.5 μg/mL<br />(51–66.3 μmol/L) |
|||
|- |
|||
| '''[[Steady state (pharmacokinetics)|t<sub>ss</sub>]]''' || 4–12 weeks || 4–12 weeks |
|||
|- class="sortbottom" |
|||
| colspan="3" | <center>All values are for (R)-bicalutamide</center> |
|||
|} |
|||
The pharmacokinetics of bicalutamide are not affected by consumption of food, a person's age or body weight, [[renal impairment]], or mild-to-moderate [[hepatic impairment]].<ref name="Cockshott2004" /><ref name="DenisMahler1996" /> However, steady-state levels of bicalutamide are higher in [[Japanese people|Japanese individuals]] than in [[white people]].<ref name="Cockshott2004" /> |
|||
Steady-state concentrations of the drug are reached after 4 to 12 weeks of administration independently of dosage, with an approximate 10- to 20-fold progressive accumulation of circulating levels of (''R'')-bicalutamide.<ref name="Wellington2006" /><ref name="pmid8717470">{{cite journal |vauthors=Blackledge GR |title=Clinical progress with a new antiandrogen, Casodex (bicalutamide) |journal=European Urology |volume=29 Suppl 2 |issue= |pages=96–104 |year=1996 |pmid=8717470 |doi= |url= |quote=Casodex is associated with significantly less gastrointestinal effects (diarrhoea) than the nonsteroidal antiandrogen flutamide (Eulexin, Schering-Plough International). Casodex is not associated with alcohol intolerance, pneumonitis and ocular defects which have been seen with the antiandrogen nilutamide (Anandron, Roussel).}}</ref><ref name="Jr.Lawrence2015" /><ref name="DenisMahler1996">{{cite journal |vauthors=Denis L, Mahler C |title=Pharmacodynamics and pharmacokinetics of bicalutamide: defining an active dosing regimen |journal=Urology |volume=47 |issue=1A Suppl |pages=26–8; discussion 29–32 |date=January 1996 |pmid=8560674 |doi=10.1016/S0090-4295(96)80004-5}}</ref> In spite of the relatively long time to reach steady-state (which is a product of its long elimination half-life),<ref name="DenisMahler1996" /> there is evidence that the achieved {{abbr|AR|androgen receptor}} blockade of bicalutamide is equivalent to that of flutamide by the end of the first day of treatment.<ref name="pmid8717470" /> With single 50 mg and 150 mg doses of bicalutamide, mean [[Cmax (pharmacology)|peak concentrations]] (C<sub>max</sub>) of (''R'')-bicalutamide are 0.77 μg/mL (1.8 μmol/L) (at 31 hours) and 1.4 μg/mL (3.3 μmol/L) (at 39 hours), respectively.<ref name="Wellington2006" /><ref name="FDALabel" /> At steady-state, mean circulating concentrations (C<sub>ss</sub>) of (''R'')-bicalutamide with 50 mg/day and 150 mg/day bicalutamide are 8.9 μg/mL (21 μmol/L) and 22 μg/mL (51 μmol/L), respectively.<ref name="Wellington2006" /><ref name="FDALabel" /><ref name="TGALabel" /><ref name="DenisMahler1996" /> In another 150 mg/day bicalutamide study, mean circulating concentrations of (''R'')-bicalutamide were 19.4 μg/mL (45.1 μmol/L) and 28.5 μg/mL (66.3 μmol/L) on days 28 and 84 (weeks 4 and 12) of treatment, respectively.<ref name="pmid15838655">{{cite journal |vauthors=Boccardo F, Rubagotti A, Conti G, Potenzoni D, Manganelli A, Del Monaco D |title=Exploratory study of drug plasma levels during bicalutamide 150 mg therapy co-administered with tamoxifen or anastrozole for prophylaxis of gynecomastia and breast pain in men with prostate cancer |journal=Cancer Chemotherapy and Pharmacology |volume=56 |issue=4 |pages=415–20 |year=2005 |pmid=15838655 |doi=10.1007/s00280-005-1016-1 |url=https://www.researchgate.net/profile/Alessandrarubagottiunigeit_Alessandra51/publication/7897958_Exploratory_study_of_drug_plasma_levels_during_bicalutamide_150_mg_therapy_co-administered_with_tamoxifen_or_anastrozole_for_prophylaxis_of_gynecomastia_and_breast_pain_in_men_with_prostate_cancer/links/0c960528c993b1b5f5000000.pdf}}</ref> |
|||
====Distribution==== |
|||
The [[tissue (biology)|tissue]] [[distribution (pharmacology)|distribution]] of bicalutamide is not well-characterized.<ref name="ChuJr.2012">{{cite book |first1=Edward |last1=Chu |first2=Vincent T. |last2=DeVita Jr. |name-list-format = vanc |title=Physicians' Cancer Chemotherapy Drug Manual 2013 |url=https://books.google.com/books?id=E_Q8eIxYlHcC&pg=PA51 |date=28 December 2012 |publisher=Jones & Bartlett Publishers |isbn=978-1-284-04039-5 |pages=51–}}</ref> However, it has been reported that distribution studies with bicalutamide have shown that preferential (i.e., [[tissue selectivity|tissue-selective]]) accumulation in [[anabolic]] (e.g., [[muscle]]) tissues does not occur.<ref name="BunceCampbell2010">{{cite book |first1=Chris M. |last1=Bunce |first2=Moray J. |last2=Campbell |name-list-format=vanc |title=Nuclear Receptors: Current Concepts and Future Challenges |url=https://books.google.com/books?id=U_1I616STa4C&pg=PA160 |date=11 March 2010 |publisher=Springer Science & Business Media |isbn=978-90-481-3303-1 |pages=160, 167 |deadurl=no |archiveurl=https://web.archive.org/web/20160610112652/https://books.google.com/books?id=U_1I616STa4C&pg=PA160 |archivedate=10 June 2016 |df=dmy-all}}</ref> There are no available data on hepatic bicalutamide concentrations in humans, but a rat study found that oral bicalutamide treatment resulted in 4-fold higher concentrations of the drug in the liver relative to plasma (a common finding with orally administered drugs, due to transfer through the [[hepatic portal system]] prior to reaching [[circulatory system|circulation]]).<ref name="Cockshott2004" /><ref name="BealeCollins1996">{{cite book |first1=C.M. |last1=Beale |first2=P. |last2=Collins | name-list-format = vanc |title=The Cardioprotective Role of HRT: A Clinical Update |url=https://books.google.com/books?id=QwgZsblGLBgC&pg=PA14 |date=15 May 1996 |publisher=CRC Press |isbn=978-1-85070-740-0 |pages=14–}}</ref> In men receiving 150 mg/day bicalutamide, concentrations of (''R'')-bicalutamide in semen were 4.9 μg/mL (11 μmol/L), and the amount of the drug that could potentially be delivered to a female partner during [[sexual intercourse]] is regarded as low (estimated at 0.3 μg/kg) and below the amount that is required to induce changes in the offspring of laboratory animals.<ref name="TGALabel" /> Bicalutamide is highly [[plasma protein binding|protein-bound]] (96.1% for racemic bicalutamide, 99.6% for (''R'')-bicalutamide)), mainly to albumin.<ref name="LemkeWilliams2008" /><ref name="Cockshott2004" /><ref name="ChuJr.2012" /> It has negligible affinity for {{abbr|SHBG|sex hormone-binding globulin}} and no affinity for [[corticosteroid-binding globulin]].<ref name="Furr1995">{{cite journal |vauthors=Furr BJ |title=Casodex: preclinical studies and controversies |journal=Annals of the New York Academy of Sciences |volume=761 |issue=1 |pages=79–96 |date=June 1995 |pmid=7625752 |doi=10.1111/j.1749-6632.1995.tb31371.x}}</ref> |
|||
Based on [[animal testing|animal research]], it was initially thought that bicalutamide was unable to cross the [[blood–brain barrier]] into the central nervous system and hence would be a [[peripherally selective drug|peripherally-selective]] antiandrogen in humans.<ref name="HelsenVan den Broeck2014">{{cite journal |vauthors=Helsen C, Van den Broeck T, Voet A, Prekovic S, Van Poppel H, Joniau S, Claessens F |title=Androgen receptor antagonists for prostate cancer therapy |journal=Endocrine-Related Cancer |volume=21 |issue=4 |pages=T105-18 |date=August 2014 |pmid=24639562 |doi=10.1530/ERC-13-0545}}</ref><ref name="FurrTucker1996" /> This conclusion was drawn from the finding that bicalutamide does not increase {{abbr|LH|luteinizing hormone}} or testosterone levels in multiple tested animal species (including rats and dogs),<ref name="HelsenVan den Broeck2014" /><ref name="FurrTucker1996" /><ref name="Furr1989">{{cite journal |vauthors=Furr BJ |title="Casodex" (ICI 176,334)--a new, pure, peripherally-selective anti-androgen: preclinical studies |journal=Hormone Research |volume=32 Suppl 1 |issue=1 |pages=69–76 |year=1989 |pmid=2533159 |doi=10.1159/000181315}}</ref><ref name="FurrValcaccia1987">{{cite journal |vauthors=Furr BJ, Valcaccia B, Curry B, Woodburn JR, Chesterson G, Tucker H |title=ICI 176,334: a novel non-steroidal, peripherally selective antiandrogen |journal=The Journal of Endocrinology |volume=113 |issue=3 |pages=R7-9 |date=June 1987 |pmid=3625091 |doi=10.1677/joe.0.113R007}}</ref> as antiandrogens like flutamide normally do this by blocking {{abbr|ARs|androgen receptors}} in the pituitary gland and hypothalamus in the brain and thereby disinhibiting the {{abbr|HPG|hypothalamic–pituitary–gonadal}} axis.<ref name="IversenMelezinek2001">{{cite journal |vauthors=Iversen P, Melezinek I, Schmidt A |title=Nonsteroidal antiandrogens: a therapeutic option for patients with advanced prostate cancer who wish to retain sexual interest and function |journal=BJU International |volume=87 |issue=1 |pages=47–56 |date=January 2001 |pmid=11121992 |doi=10.1046/j.1464-410x.2001.00988.x}}</ref> In humans however, bicalutamide has been found to increase {{abbr|LH|luteinizing hormone}} and testosterone levels, and to a comparable extent relative to flutamide and nilutamide.<ref name="Cockshott2004" /><ref name="IversenMelezinek2001" /><ref name="SolowaySchellhammer1995">{{cite journal |vauthors=Soloway MS, Schellhammer PF, Smith JA, Chodak GW, Vogelzang NJ, Kennealey GT |title=Bicalutamide in the treatment of advanced prostatic carcinoma: a phase II noncomparative multicenter trial evaluating safety, efficacy and long-term endocrine effects of monotherapy |journal=The Journal of Urology |volume=154 |issue=6 |pages=2110–4 |date=December 1995 |pmid=7500470 |doi=10.1016/S0022-5347(01)66709-0}}</ref><ref name="GaoDalton2007">{{cite journal |vauthors=Gao W, Dalton JT |title=Expanding the therapeutic use of androgens via selective androgen receptor modulators (SARMs) |journal=Drug Discovery Today |volume=12 |issue=5–6 |pages=241–8 |date=March 2007 |pmid=17331889 |pmc=2072879 |doi=10.1016/j.drudis.2007.01.003}}</ref> As such, it appears that there are species differences in the central penetration of bicalutamide and that the drug does indeed cross the blood–brain barrier and affect central function in humans,<ref name="Cockshott2004" /><ref name="GaoDalton2007" /> as supported by potential side effects, in spite of increased testosterone levels, like hot flashes and diminished sexual interest in men.<ref name="pmid16896883">{{cite journal |vauthors=Mason M |title=What implications do the tolerability profiles of antiandrogens and other commonly used prostate cancer treatments have on patient care? |journal=Journal of Cancer Research and Clinical Oncology |volume=132 Suppl 1 |issue= |pages=S27-35 |date=August 2006 |pmid=16896883 |doi=10.1007/s00432-006-0134-4}}</ref> A newer {{abbr|NSAA|nonsteroidal antiandrogen}}, darolutamide, has been found to negligibly cross the blood–brain barrier in both animals ''and'' humans, and in accordance, unlike bicalutamide, does not increase {{abbr|LH|luteinizing hormone}} or testosterone levels in humans.<ref name="MoilanenRiikonen2015">{{cite journal |vauthors=Moilanen AM, Riikonen R, Oksala R, Ravanti L, Aho E, Wohlfahrt G, Nykänen PS, Törmäkangas OP, Palvimo JJ, Kallio PJ |title=Discovery of ODM-201, a new-generation androgen receptor inhibitor targeting resistance mechanisms to androgen signaling-directed prostate cancer therapies |journal=Scientific Reports |volume=5 |pages=12007 |year=2015 |pmid=26137992 |doi=10.1038/srep12007 |pmc=4490394}}</ref> |
|||
====Metabolism==== |
|||
The [[metabolism]] of bicalutamide is [[hepatic]] and [[stereoselectivity|stereoselective]].<ref name="LemkeWilliams2008" /><ref name="Weber2015" /> The inactive (''S'')-enantiomer is metabolized mainly by [[glucuronidation]] and is rapidly [[clearance (pharmacology)|cleared]] from circulation, while the active (''R'')-isomer is slowly [[hydroxylation|hydroxylated]] and then glucuronidated.<ref name="Weber2015" /> In accordance, the active (''R'')-enantiomer has a far longer elimination half-life than the (''S'')-isomer,<ref name="SchellensMcLeod2005" /> and circulating levels of (''R'')-bicalutamide are 10- to 20-fold<ref name="Wellington2006" /> and 100-fold higher than those of (''S'')-bicalutamide after a single dose and at steady-state, respectively.<ref name="LemkeWilliams2012">{{cite book |first1=Thomas L. |last1=Lemke |first2=David A. |last2=Williams |name-list-format=vanc |title=Foye's Principles of Medicinal Chemistry |url=https://books.google.com/books?id=Sd6ot9ul-bUC&pg=PA1372 |date=24 January 2012 |publisher=Lippincott Williams & Wilkins |isbn=978-1-60913-345-0 |pages=1372–1373 |deadurl=no |archiveurl=https://web.archive.org/web/20160503223616/https://books.google.com/books?id=Sd6ot9ul-bUC&pg=PA1372 |archivedate=3 May 2016 |df=dmy-all}}</ref><ref name="ButlerGovindan2010">{{cite book |first1=Sara K. |last1=Butler |first2=Ramaswamy |last2=Govindan | name-list-format = vanc |title=Essential Cancer Pharmacology: The Prescriber's Guide |url=https://books.google.com/books?id=ZC0oMwt1ZKgC&pg=PA49 |date=25 October 2010 |publisher=Lippincott Williams & Wilkins |isbn=978-1-60913-704-5 |pages=49–}}</ref> (''R'')-Bicalutamide is almost exclusively [[metabolism|metabolized]] via hydroxylation into (''R'')-hydroxybicalutamide by the [[cytochrome P450]] [[enzyme]] [[CYP3A4]].<ref name="Cockshott2004" /><ref name="LemkeWilliams2008" /><ref name="LemkeWilliams2012" /> Bicalutamide is also glucuronidated by [[UGT1A9]], a [[UDP-glucuronyltransferase]],<ref name="GrosseCampeau2013">{{cite journal |vauthors=Grosse L, Campeau AS, Caron S, Morin FA, Meunier K, Trottier J, Caron P, Verreault M, Barbier O |title=Enantiomer selective glucuronidation of the non-steroidal pure anti-androgen bicalutamide by human liver and kidney: role of the human UDP-glucuronosyltransferase (UGT)1A9 enzyme |journal=Basic & Clinical Pharmacology & Toxicology |volume=113 |issue=2 |pages=92–102 |date=August 2013 |pmid=23527766 |pmc=3815647 |doi=10.1111/bcpt.12071 |quote=}}</ref> into bicalutamide glucuronide, and (''R'')-hydroxybicalutamide glucuronide is formed from the metabolism of (''R'')-hydroxybicalutamide by UGT1A9.<ref name="Cockshott2004" /><ref name="GrosseCampeau2013" /><ref name="Schellhammer2005" /> Similar to the inactive (''S'')-enantiomer of bicalutamide, (''R'')-hydroxybicalutamide is glucuronidated and rapidly cleared from circulation.<ref name="AndersonKnoben2001">{{cite book |first1=Philip O. |last1=Anderson |first2=James E. |last2=Knoben |first3=William G. |last3=Troutman |name-list-format = vanc |title=Handbook of Clinical Drug Data |url=https://books.google.com/books?id=40UJmr_6WQ4C |date=22 August 2001 |publisher=McGraw Hill Professional |isbn=978-0-07-138942-6 |page=245 |quote=With an oral dose of 50 mg/day, bicalutamide attains a peak serum level of 8.9 mg/L (21 μmol/L) 31 hr after a dose at steady state. CI of (R)-bicalutamide is 0.32 L/hr. The active (R)-enantiomer of bicalutamide is oxidized to an inactive metabolite, which, like the inactive (S)-enantiomer, is glucuronidated and cleared rapidly by elimination in the urine and feces.165}}</ref> None of the metabolites of bicalutamide are known to be active.<ref name="LemkeWilliams2008" /><ref name="pmid8997470" /> Following administration of bicalutamide, only low concentrations of the metabolites are detectable in [[blood plasma]], while unchanged bicalutamide predominates.<ref name="Cockshott2004" /> (''R'')-Bicalutamide has a long [[biological half-life|elimination half-life]] of 5.8 days with a single dose,<ref name="Skidmore-Roth2013" /><ref name="WeinKavoussi2011" /> and an elimination half-life of 7 to 10 days with repeated administration, which allows for convenient once-daily dosing of bicalutamide.<ref name="JordanFurr2010">{{cite book |first1=Virgil Craig |last1=Jordan |first2=B. J. A. |last2=Furr |name-list-format=vanc |title=Hormone Therapy in Breast and Prostate Cancer |url=https://books.google.com/books?id=dM0uvBnxiN0C&pg=PA350 |date=5 February 2010 |publisher=Springer Science & Business Media |isbn=978-1-59259-152-7 |pages=350– |deadurl=no |archiveurl=https://web.archive.org/web/20160529061703/https://books.google.com/books?id=dM0uvBnxiN0C&pg=PA350 |archivedate=29 May 2016 |df=dmy-all}}</ref> |
|||
{{Bicalutamide metabolism|align=center|caption=This diagram illustrates the primary metabolic pathways involved in the metabolism of bicalutamide in humans.}} |
|||
====Elimination==== |
|||
Bicalutamide is [[elimination (pharmacology)|eliminated]] in [[feces]] (43%) and [[urine]] (34%),<ref name="LemkeWilliams2008" /><ref name="Weber2015" /> whereas its metabolites are eliminated in approximately equal proportions in urine and [[bile]].<ref name="pmid14748655" /><ref name="pmid22495777">{{cite journal |vauthors=Sharma K, Pawar GV, Giri S, Rajagopal S, Mullangi R |title=Development and validation of a highly sensitive LC-MS/MS-ESI method for the determination of bicalutamide in mouse plasma: application to a pharmacokinetic study |journal=Biomedical Chromatography |volume=26 |issue=12 |pages=1589–95 |year=2012 |pmid=22495777 |doi=10.1002/bmc.2736 |url=}}</ref> It is excreted to a substantial extent in its unmetabolized form, with both bicalutamide and its metabolites excreted mainly as [[glucuronide]] [[conjugation (biochemistry)|conjugates]].<ref name="SchellensMcLeod2005" /> |
|||
==Chemistry== |
==Chemistry== |
||
{{Multiple image |
|||
| direction = vertical |
|||
| width = 250 |
|||
| caption_align = center |
|||
| header = [[Chemical structure diagram|Chemical structure]] of bicalutamide |
|||
| footer = |
|||
| image1 = Bicalutamide.svg |
|||
| alt1 = |
|||
| caption1 = [[Skeletal formula]] of bicalutamide |
|||
| image2 = Bicalutamide 3D ball.png |
|||
| alt2 = |
|||
| caption2 = [[Ball-and-stick model]] of bicalutamide |
|||
| image3 = Bicalutamide 3D spacefill.png |
|||
| alt3 = |
|||
| caption3 = [[Space-filling model]] of bicalutamide |
|||
}} |
|||
Bicalutamide is a [[racemic mixture]] consisting of equal proportions of enantiomers (''R'')-bicalutamide ([[dextrorotatory]]) and (''S'')-bicalutamide ([[levorotatory]]).<ref name="FDALabel" /> Its [[systematic name]] ([[IUPAC nomenclature of organic chemistry|{{abbr|IUPAC|International Union of Pure and Applied Chemistry}}]]) is (''RS'')-''N''-[4-cyano-3-(trifluoromethyl)phenyl]-3-[(4-fluorophenyl)sulfonyl]-2-hydroxy-2-methylpropanamide.<ref name="Publishing2013" /><ref name="KomstaWaksmundzka-Hajnos2013">{{cite book |first1=Lukas |last1=Komsta |first2=Monika |last2=Waksmundzka-Hajnos |first3=Joseph |last3=Sherma | name-list-format = vanc |title=Thin Layer Chromatography in Drug Analysis |url=https://books.google.com/books?id=LSEtAgAAQBAJ&pg=PA652 |date=20 December 2013 |publisher=CRC Press |isbn=978-1-4665-0715-9 |pages=652–}}</ref> The compound has a [[chemical formula]] of C<sub>18</sub>H<sub>14</sub>F<sub>4</sub>N<sub>2</sub>O<sub>4</sub>S, a [[molecular weight]] of 430.373 g/mol, and is a fine white to off-white powder.<ref name="FDALabel" /><ref name="TGALabel">{{cite web |title=COSUDEX® (bicalutamide) 150 mg tablets |publisher=TGA |url=https://www.ebs.tga.gov.au/ebs/picmi/picmirepository.nsf/pdf?OpenAgent&id=CP-2010-PI-05200-3&d=2016081316114622483&d=2016083016114622483 |deadurl=no |archiveurl=https://web.archive.org/web/20160914231137/https://www.ebs.tga.gov.au/ebs/picmi/picmirepository.nsf/pdf?OpenAgent&id=CP-2010-PI-05200-3&d=2016081316114622483&d=2016083016114622483 |archivedate=14 September 2016 |df=dmy-all}}</ref> |
Bicalutamide is a [[racemic mixture]] consisting of equal proportions of enantiomers (''R'')-bicalutamide ([[dextrorotatory]]) and (''S'')-bicalutamide ([[levorotatory]]).<ref name="FDALabel" /> Its [[systematic name]] ([[IUPAC nomenclature of organic chemistry|{{abbr|IUPAC|International Union of Pure and Applied Chemistry}}]]) is (''RS'')-''N''-[4-cyano-3-(trifluoromethyl)phenyl]-3-[(4-fluorophenyl)sulfonyl]-2-hydroxy-2-methylpropanamide.<ref name="Publishing2013" /><ref name="KomstaWaksmundzka-Hajnos2013">{{cite book |first1=Lukas |last1=Komsta |first2=Monika |last2=Waksmundzka-Hajnos |first3=Joseph |last3=Sherma | name-list-format = vanc |title=Thin Layer Chromatography in Drug Analysis |url=https://books.google.com/books?id=LSEtAgAAQBAJ&pg=PA652 |date=20 December 2013 |publisher=CRC Press |isbn=978-1-4665-0715-9 |pages=652–}}</ref> The compound has a [[chemical formula]] of C<sub>18</sub>H<sub>14</sub>F<sub>4</sub>N<sub>2</sub>O<sub>4</sub>S, a [[molecular weight]] of 430.373 g/mol, and is a fine white to off-white powder.<ref name="FDALabel" /><ref name="TGALabel">{{cite web |title=COSUDEX® (bicalutamide) 150 mg tablets |publisher=TGA |url=https://www.ebs.tga.gov.au/ebs/picmi/picmirepository.nsf/pdf?OpenAgent&id=CP-2010-PI-05200-3&d=2016081316114622483&d=2016083016114622483 |deadurl=no |archiveurl=https://web.archive.org/web/20160914231137/https://www.ebs.tga.gov.au/ebs/picmi/picmirepository.nsf/pdf?OpenAgent&id=CP-2010-PI-05200-3&d=2016081316114622483&d=2016083016114622483 |archivedate=14 September 2016 |df=dmy-all}}</ref> |
||
| Line 271: | Line 172: | ||
===Analogues=== |
===Analogues=== |
||
====First-generation {{abbr|NSAAs|nonsteroidal antiandrogens}}==== |
|||
{{See also|Discovery and development of antiandrogens}} |
{{See also|Discovery and development of antiandrogens}} |
||
First-generation {{abbr|NSAAs|nonsteroidal antiandrogens}} including bicalutamide, flutamide, and nilutamide are all synthetic, nonsteroidal anilide derivatives and [[structural analog]]ues of each other.<ref name="MohlerBohl2009">{{cite journal |vauthors=Mohler ML, Bohl CE, Jones A, Coss CC, Narayanan R, He Y, Hwang DJ, Dalton JT, Miller DD |title=Nonsteroidal selective androgen receptor modulators (SARMs): dissociating the anabolic and androgenic activities of the androgen receptor for therapeutic benefit |journal=Journal of Medicinal Chemistry |volume=52 |issue=12 |pages=3597–617 |date=June 2009 |pmid=19432422 |doi=10.1021/jm900280m |quote="[C]linically relevant antiandrogens currently are nonsteroidal anilide derivatives. Antiandrogens used for prostate cancer include the monoarylpropionamide flutamide (1) (a prodrug of hydroxyflutamide (2)),29–31 the hydantoin nilutamide(3),32–34 and the diarylpropionamide bicalutamide (4) (Chart1).35–37"}}</ref> Bicalutamide is a diarylpropionamide while flutamide is a monoarylpropionamide and nilutamide is a [[hydantoin]].<ref name="MohlerBohl2009" /> Bicalutamide and flutamide, though not nilutamide, can also be classified as [[toluidide]]s.<ref name="LemkeWilliams2012" /> All three of the compounds share a common 3-[[trifluoromethyl]][[aniline]] moiety.<ref name="BéguéBonnet-Delpon2008">{{cite book |first1=Jean-Pierre |last1=Bégué |first2=Daniele |last2=Bonnet-Delpon | name-list-format = vanc |title=Bioorganic and Medicinal Chemistry of Fluorine |url=https://books.google.com/books?id=QMVSvZ-R7I0C&pg=PA327 |date=2 June 2008 |publisher=John Wiley & Sons |isbn=978-0-470-28187-1 |pages=327–}}</ref> Bicalutamide is a modification of flutamide in which a 4-[[fluoro]][[phenyl group|phenyl]][[sulfonyl]] moiety has been added and the nitro group on the original phenyl ring has been replaced with a cyano group.<ref name="BallKamalian2016">{{cite journal |vauthors=Ball AL, Kamalian L, Alfirevic A, Lyon JJ, Chadwick AE |title=Identification of the Additional Mitochondrial Liabilities of 2-Hydroxyflutamide When Compared With its Parent Compound, Flutamide in HepG2 Cells |journal=Toxicological Sciences |date=July 2016 |pmid=27413113 |doi=10.1093/toxsci/kfw126 |pages=kfw126}}</ref> [[Topilutamide]], also known as fluridil, is another {{abbr|NSAA|nonsteroidal antiandrogen}} that is closely related structurally to the first-generation {{abbr|NSAAs|nonsteroidal antiandrogens}}, but, in contrast to them, is not used in the treatment of prostate cancer and is instead used exclusively as a [[topical]] antiandrogen in the treatment of androgenic alopecia.<ref name="pmid16821162" /><ref name="AvramRogers2009">{{cite book |first1=Marc R. |last1=Avram |first2=Nicole E. |last2=Rogers | name-list-format = vanc |title=Hair Transplantation |url=https://books.google.com/books?id=j1XF1bnABFcC&pg=PA11 |date=30 November 2009 |publisher=Cambridge University Press |isbn=978-1-139-48339-1 |pages=11–}}</ref><ref name="HaberStough2006">{{cite book |first1=Robert S. |last1=Haber |first2=Dowling Bluford |last2=Stough |name-list-format=vanc |title=Hair Transplantation |url=https://books.google.com/books?id=PXJMqrbk-fAC&pg=PA6 |accessdate=28 May 2012 |year=2006 |publisher=Elsevier Health Sciences |isbn=978-1-4160-3104-8 |pages=6–7 |deadurl=no |archiveurl=https://web.archive.org/web/20140704201433/http://books.google.com/books?id=PXJMqrbk-fAC&pg=PA6 |archivedate=4 July 2014 |df=dmy-all}}</ref> |
First-generation {{abbr|NSAAs|nonsteroidal antiandrogens}} including bicalutamide, flutamide, and nilutamide are all synthetic, nonsteroidal anilide derivatives and [[structural analog]]ues of each other.<ref name="MohlerBohl2009">{{cite journal |vauthors=Mohler ML, Bohl CE, Jones A, Coss CC, Narayanan R, He Y, Hwang DJ, Dalton JT, Miller DD |title=Nonsteroidal selective androgen receptor modulators (SARMs): dissociating the anabolic and androgenic activities of the androgen receptor for therapeutic benefit |journal=Journal of Medicinal Chemistry |volume=52 |issue=12 |pages=3597–617 |date=June 2009 |pmid=19432422 |doi=10.1021/jm900280m |quote="[C]linically relevant antiandrogens currently are nonsteroidal anilide derivatives. Antiandrogens used for prostate cancer include the monoarylpropionamide flutamide (1) (a prodrug of hydroxyflutamide (2)),29–31 the hydantoin nilutamide(3),32–34 and the diarylpropionamide bicalutamide (4) (Chart1).35–37"}}</ref> Bicalutamide is a diarylpropionamide while flutamide is a monoarylpropionamide and nilutamide is a [[hydantoin]].<ref name="MohlerBohl2009" /> Bicalutamide and flutamide, though not nilutamide, can also be classified as [[toluidide]]s.<ref name="LemkeWilliams2012" /> All three of the compounds share a common 3-[[trifluoromethyl]][[aniline]] moiety.<ref name="BéguéBonnet-Delpon2008">{{cite book |first1=Jean-Pierre |last1=Bégué |first2=Daniele |last2=Bonnet-Delpon | name-list-format = vanc |title=Bioorganic and Medicinal Chemistry of Fluorine |url=https://books.google.com/books?id=QMVSvZ-R7I0C&pg=PA327 |date=2 June 2008 |publisher=John Wiley & Sons |isbn=978-0-470-28187-1 |pages=327–}}</ref> Bicalutamide is a modification of flutamide in which a 4-[[fluoro]][[phenyl group|phenyl]][[sulfonyl]] moiety has been added and the nitro group on the original phenyl ring has been replaced with a cyano group.<ref name="BallKamalian2016">{{cite journal |vauthors=Ball AL, Kamalian L, Alfirevic A, Lyon JJ, Chadwick AE |title=Identification of the Additional Mitochondrial Liabilities of 2-Hydroxyflutamide When Compared With its Parent Compound, Flutamide in HepG2 Cells |journal=Toxicological Sciences |date=July 2016 |pmid=27413113 |doi=10.1093/toxsci/kfw126 |pages=kfw126}}</ref> [[Topilutamide]], also known as fluridil, is another {{abbr|NSAA|nonsteroidal antiandrogen}} that is closely related structurally to the first-generation {{abbr|NSAAs|nonsteroidal antiandrogens}}, but, in contrast to them, is not used in the treatment of prostate cancer and is instead used exclusively as a [[topical]] antiandrogen in the treatment of androgenic alopecia.<ref name="pmid16821162" /><ref name="AvramRogers2009">{{cite book |first1=Marc R. |last1=Avram |first2=Nicole E. |last2=Rogers | name-list-format = vanc |title=Hair Transplantation |url=https://books.google.com/books?id=j1XF1bnABFcC&pg=PA11 |date=30 November 2009 |publisher=Cambridge University Press |isbn=978-1-139-48339-1 |pages=11–}}</ref><ref name="HaberStough2006">{{cite book |first1=Robert S. |last1=Haber |first2=Dowling Bluford |last2=Stough |name-list-format=vanc |title=Hair Transplantation |url=https://books.google.com/books?id=PXJMqrbk-fAC&pg=PA6 |accessdate=28 May 2012 |year=2006 |publisher=Elsevier Health Sciences |isbn=978-1-4160-3104-8 |pages=6–7 |deadurl=no |archiveurl=https://web.archive.org/web/20140704201433/http://books.google.com/books?id=PXJMqrbk-fAC&pg=PA6 |archivedate=4 July 2014 |df=dmy-all}}</ref> |
||
{{Hidden begin|toggle=left|title=Structures}} |
{{Hidden begin|toggle=left|title=Structures of first-generation NSAAs}} |
||
{{Multiple image |
{{Multiple image |
||
| direction = horizontal |
| direction = horizontal |
||
| Line 311: | Line 210: | ||
{{Hidden end}} |
{{Hidden end}} |
||
====Second-generation {{abbr|NSAAs|nonsteroidal antiandrogens}}==== |
|||
The second-generation {{abbr|NSAAs|nonsteroidal antiandrogens}} enzalutamide and apalutamide were derived from and are analogues of the first-generation {{abbr|NSAAs|nonsteroidal antiandrogens}},<ref name="Weber2015" /><ref name="KawaharaMiyamoto2014">{{cite journal |last1=Kawahara |first1=Takashi |last2=Minamoto |first2=Hiroshi | name-list-format = vanc |title=Androgen Receptor Antagonists in the Treatment of Prostate Cancer |journal=Clinical Immunology, Endocrine & Metabolic Drugs |volume=1 |issue=1 |year=2014 |pages=11–19 |doi=10.2174/22127070114019990002}}</ref> while another second-generation {{abbr|NSAA|nonsteroidal antiandrogen}}, darolutamide, is said to be structurally distinct and chemically unrelated to the other {{abbr|NSAAs|nonsteroidal antiandrogens}}.<ref name="pmid26137992">{{cite journal |vauthors=Moilanen AM, Riikonen R, Oksala R, Ravanti L, Aho E, Wohlfahrt G, Nykänen PS, Törmäkangas OP, Palvimo JJ, Kallio PJ |title=Discovery of ODM-201, a new-generation androgen receptor inhibitor targeting resistance mechanisms to androgen signaling-directed prostate cancer therapies |journal=Sci Rep |volume=5 |issue= |pages=12007 |year=2015 |pmid=26137992 |pmc=4490394 |doi=10.1038/srep12007 |url=}}</ref> Enzalutamide is a modification of bicalutamide in which the inter-ring linking [[side chain|chain]] has been altered and [[cyclic compound|cyclized]] into a 5,5-di[[methyl group|methyl]]-4-[[oxygen|oxo]]-2-[[thioxo]] [[imidazolidine]] moiety. In apalutamide, the 5,5-dimethyl groups of the imidazolidine ring of enzalutamide are cyclized to form an accessory [[cyclobutane]] ring and one of its phenyl rings is replaced with a [[pyridine]] ring. |
The second-generation {{abbr|NSAAs|nonsteroidal antiandrogens}} enzalutamide and apalutamide were derived from and are analogues of the first-generation {{abbr|NSAAs|nonsteroidal antiandrogens}},<ref name="Weber2015" /><ref name="KawaharaMiyamoto2014">{{cite journal |last1=Kawahara |first1=Takashi |last2=Minamoto |first2=Hiroshi | name-list-format = vanc |title=Androgen Receptor Antagonists in the Treatment of Prostate Cancer |journal=Clinical Immunology, Endocrine & Metabolic Drugs |volume=1 |issue=1 |year=2014 |pages=11–19 |doi=10.2174/22127070114019990002}}</ref> while another second-generation {{abbr|NSAA|nonsteroidal antiandrogen}}, darolutamide, is said to be structurally distinct and chemically unrelated to the other {{abbr|NSAAs|nonsteroidal antiandrogens}}.<ref name="pmid26137992">{{cite journal |vauthors=Moilanen AM, Riikonen R, Oksala R, Ravanti L, Aho E, Wohlfahrt G, Nykänen PS, Törmäkangas OP, Palvimo JJ, Kallio PJ |title=Discovery of ODM-201, a new-generation androgen receptor inhibitor targeting resistance mechanisms to androgen signaling-directed prostate cancer therapies |journal=Sci Rep |volume=5 |issue= |pages=12007 |year=2015 |pmid=26137992 |pmc=4490394 |doi=10.1038/srep12007 |url=}}</ref> Enzalutamide is a modification of bicalutamide in which the inter-ring linking [[side chain|chain]] has been altered and [[cyclic compound|cyclized]] into a 5,5-di[[methyl group|methyl]]-4-[[oxygen|oxo]]-2-[[thioxo]] [[imidazolidine]] moiety. In apalutamide, the 5,5-dimethyl groups of the imidazolidine ring of enzalutamide are cyclized to form an accessory [[cyclobutane]] ring and one of its phenyl rings is replaced with a [[pyridine]] ring. |
||
{{Hidden begin|toggle=left|title=Structures}} |
{{Hidden begin|toggle=left|title=Structures of second-generation NSAAs}} |
||
{{Multiple image |
{{Multiple image |
||
| direction = horizontal |
| direction = horizontal |
||
| Line 341: | Line 239: | ||
{{Hidden end}} |
{{Hidden end}} |
||
====Arylpropionamide {{abbr|SARMs|selective androgen receptor modulators}}==== |
|||
The first nonsteroidal androgens (the arylpropionamides) were discovered via [[molecular modification|structural modification]] of bicalutamide.<ref name="SegalNarayanan2006">{{cite journal |vauthors=Segal S, Narayanan R, Dalton JT |title=Therapeutic potential of the SARMs: revisiting the androgen receptor for drug discovery |journal=Expert Opinion on Investigational Drugs |volume=15 |issue=4 |pages=377–87 |date=April 2006 |pmid=16548787 |doi=10.1517/13543784.15.4.377 |quote="Structural modifications of bicalutamide led to the discovery of the first nonsteroidal androgens (the aryl propionamides) in 1998. Lead compounds in this class (denoted S1 and S4 in published literature) not only bind to the AR with high affinity (low nanomolar range), but also demonstrate tissue selectivity in animal models [46,50]."}}</ref> Unlike bicalutamide (which is purely antiandrogenic), these compounds show tissue-selective androgenic effects and were classified as [[selective androgen receptor modulator]]s (SARMs).<ref name="SegalNarayanan2006" /> Lead {{abbr|SARMs|selective androgen receptor modulator}} of this series included [[acetothiolutamide]], [[enobosarm]] (ostarine; S-22), and [[andarine]] (acetamidoxolutamide or androxolutamide; S-4).<ref name="MohlerBohl2009" /><ref name="SegalNarayanan2006" /><ref name="Yin2002">{{cite journal |vauthors=Yin D, Gao W, Kearbey JD, Xu H, Chung K, He Y, Marhefka CA, Veverka KA, Miller DD, Dalton JT |title=Pharmacodynamics of selective androgen receptor modulators |journal=The Journal of Pharmacology and Experimental Therapeutics |volume=304 |issue=3 |pages=1334–40 |date=March 2003 |pmid=12604714 |pmc=2040238 |doi=10.1124/jpet.102.040840}}</ref> They are very close to bicalutamide structurally, with the key differences being that the linker sulfone of bicalutamide has been replaced with an [[ether]] or [[thioether]] group to confer agonism of the {{abbr|AR|androgen receptor}} and the 4-fluoro atom of the pertinent phenyl ring has been substituted with an [[acetamide|acetamido]] or cyano group to eliminate [[reactivity (chemistry)|reactivity]] at the position.<ref name="OttowWeinmann2008">{{cite book |first1=Eckhardt |last1=Ottow |first2=Hilmar |last2=Weinmann | name-list-format = vanc |title=Nuclear Receptors as Drug Targets |url=https://books.google.com/books?id=iATfLbPgRugC&pg=PA257 |date=8 September 2008 |publisher=John Wiley & Sons |isbn=978-3-527-62330-3 |pages=257–258}}</ref> |
The first nonsteroidal androgens (the arylpropionamides) were discovered via [[molecular modification|structural modification]] of bicalutamide.<ref name="SegalNarayanan2006">{{cite journal |vauthors=Segal S, Narayanan R, Dalton JT |title=Therapeutic potential of the SARMs: revisiting the androgen receptor for drug discovery |journal=Expert Opinion on Investigational Drugs |volume=15 |issue=4 |pages=377–87 |date=April 2006 |pmid=16548787 |doi=10.1517/13543784.15.4.377 |quote="Structural modifications of bicalutamide led to the discovery of the first nonsteroidal androgens (the aryl propionamides) in 1998. Lead compounds in this class (denoted S1 and S4 in published literature) not only bind to the AR with high affinity (low nanomolar range), but also demonstrate tissue selectivity in animal models [46,50]."}}</ref> Unlike bicalutamide (which is purely antiandrogenic), these compounds show tissue-selective androgenic effects and were classified as [[selective androgen receptor modulator]]s (SARMs).<ref name="SegalNarayanan2006" /> Lead {{abbr|SARMs|selective androgen receptor modulator}} of this series included [[acetothiolutamide]], [[enobosarm]] (ostarine; S-22), and [[andarine]] (acetamidoxolutamide or androxolutamide; S-4).<ref name="MohlerBohl2009" /><ref name="SegalNarayanan2006" /><ref name="Yin2002">{{cite journal |vauthors=Yin D, Gao W, Kearbey JD, Xu H, Chung K, He Y, Marhefka CA, Veverka KA, Miller DD, Dalton JT |title=Pharmacodynamics of selective androgen receptor modulators |journal=The Journal of Pharmacology and Experimental Therapeutics |volume=304 |issue=3 |pages=1334–40 |date=March 2003 |pmid=12604714 |pmc=2040238 |doi=10.1124/jpet.102.040840}}</ref> They are very close to bicalutamide structurally, with the key differences being that the linker sulfone of bicalutamide has been replaced with an [[ether]] or [[thioether]] group to confer agonism of the {{abbr|AR|androgen receptor}} and the 4-fluoro atom of the pertinent phenyl ring has been substituted with an [[acetamide|acetamido]] or cyano group to eliminate [[reactivity (chemistry)|reactivity]] at the position.<ref name="OttowWeinmann2008">{{cite book |first1=Eckhardt |last1=Ottow |first2=Hilmar |last2=Weinmann | name-list-format = vanc |title=Nuclear Receptors as Drug Targets |url=https://books.google.com/books?id=iATfLbPgRugC&pg=PA257 |date=8 September 2008 |publisher=John Wiley & Sons |isbn=978-3-527-62330-3 |pages=257–258}}</ref> |
||
{{Hidden begin|toggle=left|title=Structures}} |
{{Hidden begin|toggle=left|title=Structures of arylpropionamide SARMs}} |
||
{{Multiple image |
{{Multiple image |
||
| direction = horizontal |
| direction = horizontal |
||
| Line 371: | Line 268: | ||
{{Hidden end}} |
{{Hidden end}} |
||
A few [[radiolabeling|radiolabeled]] derivatives of bicalutamide have been developed for potential use as [[radiotracer]]s in [[medical imaging]].<ref name="pmid17328524">{{cite journal |vauthors=Parent EE, Dence CS, Jenks C, Sharp TL, Welch MJ, Katzenellenbogen JA |title=Synthesis and biological evaluation of [18F]bicalutamide, 4-[76Br]bromobicalutamide, and 4-[76Br]bromo-thiobicalutamide as non-steroidal androgens for prostate cancer imaging |journal=J. Med. Chem. |volume=50 |issue=5 |pages=1028–40 |year=2007 |pmid=17328524 |doi=10.1021/jm060847r |url=}}</ref><ref name="DierckxOtte2014">{{cite book |first1=Rudi A.J.O. |last1=Dierckx |first2=Andreas |last2=Otte |first3=Erik F.J. |last3=de Vries |first4=Aren |last4=van Waarde |first5=Paul G.M. |last5=Luiten | name-list-format = vanc |title=PET and SPECT of Neurobiological Systems |url=https://books.google.com/books?id=LN64BAAAQBAJ&pg=PA394 |date=15 February 2014 |publisher=Springer Science & Business Media |isbn=978-3-642-42014-6 |pages=394–}}</ref> They include [<sup>18</sup>F]bicalutamide, 4-[<sup>76</sup>Br]bromobicalutamide, and [<sup>76</sup>Br]bromo-thiobicalutamide.<ref name="pmid17328524" /><ref name="DierckxOtte2014" /> The latter two were found to have substantially increased affinity for the {{abbr|AR|androgen receptor}} relative to that of bicautamide.<ref name="pmid17328524" /> However, none of these agents have been evaluated in humans.<ref name="pmid17328524" /><ref name="DierckxOtte2014" /> |
|||
====Radiotracers for medical imaging==== |
|||
A few [[radiolabeling|radiolabeled]] derivatives of bicalutamide have been developed for potential use as [[radiotracer]]s in [[medical imaging]].<ref name="pmid17328524">{{cite journal |vauthors=Parent EE, Dence CS, Jenks C, Sharp TL, Welch MJ, Katzenellenbogen JA |title=Synthesis and biological evaluation of [18F]bicalutamide, 4-[76Br]bromobicalutamide, and 4-[76Br]bromo-thiobicalutamide as non-steroidal androgens for prostate cancer imaging |journal=J. Med. Chem. |volume=50 |issue=5 |pages=1028–40 |year=2007 |pmid=17328524 |doi=10.1021/jm060847r |url=}}</ref><ref name="DierckxOtte2014">{{cite book |first1=Rudi A.J.O. |last1=Dierckx |first2=Andreas |last2=Otte |first3=Erik F.J. |last3=de Vries |first4=Aren |last4=van Waarde |first5=Paul G.M. |last5=Luiten | name-list-format = vanc |title=PET and SPECT of Neurobiological Systems |url=https://books.google.com/books?id=LN64BAAAQBAJ&pg=PA394 |date=15 February 2014 |publisher=Springer Science & Business Media |isbn=978-3-642-42014-6 |pages=394–}}</ref> They include [<sup>18</sup>F]bicalutamide, 4-[<sup>76</sup>Br]bromobicalutamide, and |
|||
[<sup>76</sup>Br]bromo-thiobicalutamide.<ref name="pmid17328524" /><ref name="DierckxOtte2014" /> The latter two were found to have substantially increased affinity for the {{abbr|AR|androgen receptor}} relative to that of bicautamide.<ref name="pmid17328524" /> However, none of these agents have been evaluated in humans.<ref name="pmid17328524" /><ref name="DierckxOtte2014" /> |
|||
====5''N''-Bicalutamide==== |
|||
[[5N-Bicalutamide|5''N''-Bicalutamide]], or 5-azabicalutamide, is a minor structural modification of bicalutamide which acts as a [[irreversible antagonist|reversible covalent antagonist]] of the {{abbr|AR|androgen receptor}} and has approximately 150-fold higher affinity for the {{abbr|AR|androgen receptor}} and about 20-fold greater functional inhibition of the {{abbr|AR|androgen receptor}} relative to bicalutamide.<ref name="pmid28981251">{{cite journal | vauthors = de Jesus Cortez F, Nguyen P, Truillet C, Tian B, Kuchenbecker KM, Evans MJ, Webb P, Jacobson MP, Fletterick RJ, England PM | title = Development of 5N-Bicalutamide, a High-Affinity Reversible Covalent Antiandrogen | journal = ACS Chem. Biol. | volume = | issue = | pages = | year = 2017 | pmid = 28981251 | doi = 10.1021/acschembio.7b00702 | url = }}</ref><ref name="US20170101384">Pamela, M., Fletterick, R. J., Kuchenbecker, K., & de Jesus Cortez, F. (2016). U.S. Patent Application No. 15/382,942. https://www.google.com/patents/US20170101384</ref> It is among the most potent {{abbr|AR|androgen receptor}} antagonists ever to have been developed and is being researched for potential use in the treatment of antiandrogen-resistant prostate cancer.<ref name="pmid28981251" /> |
[[5N-Bicalutamide|5''N''-Bicalutamide]], or 5-azabicalutamide, is a minor structural modification of bicalutamide which acts as a [[irreversible antagonist|reversible covalent antagonist]] of the {{abbr|AR|androgen receptor}} and has approximately 150-fold higher affinity for the {{abbr|AR|androgen receptor}} and about 20-fold greater functional inhibition of the {{abbr|AR|androgen receptor}} relative to bicalutamide.<ref name="pmid28981251">{{cite journal | vauthors = de Jesus Cortez F, Nguyen P, Truillet C, Tian B, Kuchenbecker KM, Evans MJ, Webb P, Jacobson MP, Fletterick RJ, England PM | title = Development of 5N-Bicalutamide, a High-Affinity Reversible Covalent Antiandrogen | journal = ACS Chem. Biol. | volume = | issue = | pages = | year = 2017 | pmid = 28981251 | doi = 10.1021/acschembio.7b00702 | url = }}</ref><ref name="US20170101384">Pamela, M., Fletterick, R. J., Kuchenbecker, K., & de Jesus Cortez, F. (2016). U.S. Patent Application No. 15/382,942. https://www.google.com/patents/US20170101384</ref> It is among the most potent {{abbr|AR|androgen receptor}} antagonists ever to have been developed and is being researched for potential use in the treatment of antiandrogen-resistant prostate cancer.<ref name="pmid28981251" /> |
||
===Synthesis=== |
===Synthesis=== |
||
A number of [[chemical synthesis|chemical syntheses]] of bicalutamide have been published in the literature.<ref name="Publishing2013" /><ref name="pmid3361581">{{cite journal |vauthors=Tucker H, Crook JW, Chesterson GJ |title=Nonsteroidal antiandrogens. Synthesis and structure-activity relationships of 3-substituted derivatives of 2-hydroxypropionanilides |journal=Journal of Medicinal Chemistry |volume=31 |issue=5 |pages=954–9 |year=1988 |pmid=3361581 |doi=10.1021/jm00400a011 |url=}}</ref><ref name="JamesEkwuribe2002">{{cite journal |last1=James |first1=Kenneth D. |last2=Ekwuribe |first2=Nnochiri N. | name-list-format = vanc |title=A Two-step Synthesis of the Anti-cancer Drug (R,S)-Bicalutamide |journal=Synthesis |volume=2002 |issue=7 |year=2002 |pages=850–2 |doi=10.1055/s-2002-28508}}</ref><ref>{{cite patent |country=US |number=2006/0041161 |status=application |title=Procedure for the synthesis of bicalutamide |pubdate=23 February 2006 |fdate=24 May 2005 |pridate=17 June 2004 |inventor=Pizzetti E, Vigano E, Lussana M, Landonio E |url=https://worldwide.espacenet.com/publicationDetails/biblio?II=0&ND=3&adjacent=true&locale=en_EP&FT=D&date=20060223&CC=US&NR=2006041161A1&KC=A1}}</ref><ref name="ChandShukla2012">{{cite journal |last1=Chand |first1=M. |last2=Shukla |first2=Anil Kumar | name-list-format = vanc |title=Novel Synthesis of Bicalutamide Drug Substance and their Impurities using Imidazolium Type of Ionic Liquid |journal=SSRN Electronic Journal |year=2012 |doi=10.2139/ssrn.2160199}}</ref> The procedure of the first published |
A number of [[chemical synthesis|chemical syntheses]] of bicalutamide have been published in the literature.<ref name="Publishing2013" /><ref name="pmid3361581">{{cite journal |vauthors=Tucker H, Crook JW, Chesterson GJ |title=Nonsteroidal antiandrogens. Synthesis and structure-activity relationships of 3-substituted derivatives of 2-hydroxypropionanilides |journal=Journal of Medicinal Chemistry |volume=31 |issue=5 |pages=954–9 |year=1988 |pmid=3361581 |doi=10.1021/jm00400a011 |url=}}</ref><ref name="JamesEkwuribe2002">{{cite journal |last1=James |first1=Kenneth D. |last2=Ekwuribe |first2=Nnochiri N. | name-list-format = vanc |title=A Two-step Synthesis of the Anti-cancer Drug (R,S)-Bicalutamide |journal=Synthesis |volume=2002 |issue=7 |year=2002 |pages=850–2 |doi=10.1055/s-2002-28508}}</ref><ref>{{cite patent |country=US |number=2006/0041161 |status=application |title=Procedure for the synthesis of bicalutamide |pubdate=23 February 2006 |fdate=24 May 2005 |pridate=17 June 2004 |inventor=Pizzetti E, Vigano E, Lussana M, Landonio E |url=https://worldwide.espacenet.com/publicationDetails/biblio?II=0&ND=3&adjacent=true&locale=en_EP&FT=D&date=20060223&CC=US&NR=2006041161A1&KC=A1}}</ref><ref name="ChandShukla2012">{{cite journal |last1=Chand |first1=M. |last2=Shukla |first2=Anil Kumar | name-list-format = vanc |title=Novel Synthesis of Bicalutamide Drug Substance and their Impurities using Imidazolium Type of Ionic Liquid |journal=SSRN Electronic Journal |year=2012 |doi=10.2139/ssrn.2160199}}</ref> The procedure of the first published synthesis of bicalutamide can be seen below.<ref name="pmid3361581" /> |
||
{{Hidden begin|toggle=left|title=Synthesis}} |
{{Hidden begin|toggle=left|title=Synthesis (Tucker et al., 1988)}} |
||
[[File:Bicalutamide synthesis.png|thumb|center|650px|Where the starting material is [[4-cyano-3-(trifluoromethyl)aniline]] (also known as 4-amino-2-(trifluoromethyl)benzonitrile), DMA is [[dimethylacetamide]], and ''m''CPBA is [[meta-Chloroperoxybenzoic acid|''meta''-chloroperoxybenzoic acid]].]] |
[[File:Bicalutamide synthesis.png|thumb|center|650px|Where the starting material is [[4-cyano-3-(trifluoromethyl)aniline]] (also known as 4-amino-2-(trifluoromethyl)benzonitrile), DMA is [[dimethylacetamide]], and ''m''CPBA is [[meta-Chloroperoxybenzoic acid|''meta''-chloroperoxybenzoic acid]].]] |
||
{{Hidden end}} |
{{Hidden end}} |
||
| Line 401: | Line 295: | ||
===Names=== |
===Names=== |
||
====Generic names==== |
|||
''Bicalutamide'' is the [[generic term|generic name]] of the drug in English and French and its {{abbrlink|INN|International Nonproprietary Name|INN}}, {{abbrlink|USAN|United States Adopted Name}}, {{abbrlink|USP|United States Pharmacopeia}},<ref name="KEGG">{{cite web |url=http://www.kegg.jp/entry/D00961 |title=Bicalutamide |work=Kyoto Encyclopedia of Genes and Genomes (KEGG) |deadurl=no |archiveurl=https://web.archive.org/web/20161126002030/http://www.kegg.jp/entry/D00961 |archivedate=26 November 2016 |df=dmy-all}}</ref> {{abbrlink|BAN|British Approved Name}}, {{abbrlink|DCF|Dénomination Commune Française}}, {{abbrlink|AAN|Australian Approved Name}},<ref name="TGALabel" /> and {{abbrlink|JAN|Japanese Accepted Name}}.<ref name="Drugs.com-2" /><ref name="MortonHall2012">{{cite book |first1=I.K. |last1=Morton |first2=Judith M. |last2=Hal |name-list-format=vanc |title=Concise Dictionary of Pharmacological Agents: Properties and Synonyms |url=https://books.google.com/books?id=tsjrCAAAQBAJ&pg=PA51 |date=6 December 2012 |publisher=Springer Science & Business Media |isbn=978-94-011-4439-1 |pages=51– |deadurl=no |archiveurl=https://web.archive.org/web/20160514090313/https://books.google.com/books?id=tsjrCAAAQBAJ&pg=PA51 |archivedate=14 May 2016 |df=dmy-all}}</ref><ref name="IndexNominum2000" /><ref name="GanellinTriggle1996">{{cite book |first1=C.R. |last1=Ganellin |first2=David J. |last2=Triggle | name-list-format = vanc |title=Dictionary of Pharmacological Agents |url=https://books.google.com/books?id=Z_mfTTIApVEC&pg=PA570 |date=21 November 1996 |publisher=CRC Press |isbn=978-0-412-46630-4 |pages=570– |deadurl=no |archiveurl=https://web.archive.org/web/20160507003409/https://books.google.com/books?id=Z_mfTTIApVEC&pg=PA570 |archivedate=7 May 2016 |df=dmy-all}}</ref> It is also referred to as ''bicalutamidum'' in [[Latin]], ''bicalutamida'' in Spanish and [[Portuguese language|Portuguese]], ''bicalutamid'' in German, and ''bikalutamid'' in Russian and other [[Slavic languages]].<ref name="Drugs.com-2" /><ref name="IndexNominum2000" /> The "-lutamide" suffix corresponds to that for {{abbr|NSAAs|nonsteroidal antiandrogens}}.<ref name="WHO2013">http://www.who.int/medicines/services/inn/StemBook_2013_Final.pdf</ref><ref name="NLM-DrugPortal">https://druginfo.nlm.nih.gov/drugportal/name/endswith/lutamide</ref> Bicalutamide is also known by its former [[Code name#Project code name|developmental code name]] {{abbr|ICI|Imperial Chemical Industries}}-176,334.<ref name="MortonHall2012" /><ref name="IndexNominum2000" /><ref name="Drugs.com-2" /> |
''Bicalutamide'' is the [[generic term|generic name]] of the drug in English and French and its {{abbrlink|INN|International Nonproprietary Name|INN}}, {{abbrlink|USAN|United States Adopted Name}}, {{abbrlink|USP|United States Pharmacopeia}},<ref name="KEGG">{{cite web |url=http://www.kegg.jp/entry/D00961 |title=Bicalutamide |work=Kyoto Encyclopedia of Genes and Genomes (KEGG) |deadurl=no |archiveurl=https://web.archive.org/web/20161126002030/http://www.kegg.jp/entry/D00961 |archivedate=26 November 2016 |df=dmy-all}}</ref> {{abbrlink|BAN|British Approved Name}}, {{abbrlink|DCF|Dénomination Commune Française}}, {{abbrlink|AAN|Australian Approved Name}},<ref name="TGALabel" /> and {{abbrlink|JAN|Japanese Accepted Name}}.<ref name="Drugs.com-2" /><ref name="MortonHall2012">{{cite book |first1=I.K. |last1=Morton |first2=Judith M. |last2=Hal |name-list-format=vanc |title=Concise Dictionary of Pharmacological Agents: Properties and Synonyms |url=https://books.google.com/books?id=tsjrCAAAQBAJ&pg=PA51 |date=6 December 2012 |publisher=Springer Science & Business Media |isbn=978-94-011-4439-1 |pages=51– |deadurl=no |archiveurl=https://web.archive.org/web/20160514090313/https://books.google.com/books?id=tsjrCAAAQBAJ&pg=PA51 |archivedate=14 May 2016 |df=dmy-all}}</ref><ref name="IndexNominum2000" /><ref name="GanellinTriggle1996">{{cite book |first1=C.R. |last1=Ganellin |first2=David J. |last2=Triggle | name-list-format = vanc |title=Dictionary of Pharmacological Agents |url=https://books.google.com/books?id=Z_mfTTIApVEC&pg=PA570 |date=21 November 1996 |publisher=CRC Press |isbn=978-0-412-46630-4 |pages=570– |deadurl=no |archiveurl=https://web.archive.org/web/20160507003409/https://books.google.com/books?id=Z_mfTTIApVEC&pg=PA570 |archivedate=7 May 2016 |df=dmy-all}}</ref> It is also referred to as ''bicalutamidum'' in [[Latin]], ''bicalutamida'' in Spanish and [[Portuguese language|Portuguese]], ''bicalutamid'' in German, and ''bikalutamid'' in Russian and other [[Slavic languages]].<ref name="Drugs.com-2" /><ref name="IndexNominum2000" /> The "-lutamide" suffix corresponds to that for {{abbr|NSAAs|nonsteroidal antiandrogens}}.<ref name="WHO2013">http://www.who.int/medicines/services/inn/StemBook_2013_Final.pdf</ref><ref name="NLM-DrugPortal">https://druginfo.nlm.nih.gov/drugportal/name/endswith/lutamide</ref> Bicalutamide is also known by its former [[Code name#Project code name|developmental code name]] {{abbr|ICI|Imperial Chemical Industries}}-176,334.<ref name="MortonHall2012" /><ref name="IndexNominum2000" /><ref name="Drugs.com-2" /> |
||
====Brand names==== |
|||
Bicalutamide is marketed by AstraZeneca in oral tablet form under the brand names Casodex, Cosudex, Calutide, Calumid, and Kalumid in many countries.<ref name="Drugs.com-2" /><ref name="IndexNominum2000" /><ref name="HuangJo2009">{{cite book | editor-first1 = De-Shuang | editor-last1 = Huang | editor-first2 = Kang-Hyun | editor-last2 = Jo | editor-first3 = Hong-Hee | editor-last3 = Lee | editor-first4 = Hee-Jun | editor-last4 = Kang | editor-first5 = Vitoantonio | editor-last5 = Bevilacqua |title=Emerging Intelligent Computing Technology and Applications: 5th International Conference on Intelligent Computing, ICIC 2009 Ulsan, South Korea, September 16–19, 2009 Proceedings |url=https://books.google.com/books?id=gRFtCQAAQBAJ&pg=PA120 |date=19 September 2009 |publisher=Springer |isbn=978-3-642-04070-2 |pages=120– |chapter=Parallel Genetic Algorithms for Crystal Structure Prediction: Successes and Failures in Predicting Bicalutamide Polymorphs |first1=Marta B. |last1=Ferraro |first2=Anita M. |last2=Orendt |first3=Julio C. |last3=Facelli | name-list-format = vanc |doi=10.1007/978-3-642-04070-2_14}}</ref><ref name="DhasIge2015">{{cite journal |last1=Dhas |first1=Namdev L. |last2=Ige |first2=Pradum P. |last3=Kudarha |first3=Ritu R. | name-list-format = vanc |title=Design, optimization and in-vitro study of folic acid conjugated-chitosan functionalized PLGA nanoparticle for delivery of bicalutamide in prostate cancer |journal=Powder Technology |volume=283 |year=2015 |pages=234–245 |doi=10.1016/j.powtec.2015.04.053}}</ref> It is also marketed under the brand names Bicadex, Bical, Bicalox, Bicamide, Bicatlon, Bicusan, Binabic, Bypro, Calutol, and Ormandyl among others in various countries.<ref name="Drugs.com-2" /> The drug is sold under a large number of generic trade names such as Apo-Bicalutamide, Bicalutamide Accord, Bicalutamide Actavis, Bicalutamide Bluefish, Bicalutamide Kabi, Bicalutamide Sandoz, and Bicalutamide Teva as well.<ref name="Drugs.com-2" /> A combination formulation of bicalutamide and goserelin is marketed by AstraZeneca in Australia and New Zealand under the brand name ZolaCos-CP.<ref name="Martindale2011" /><ref name="Drugs.com-3" /><ref name="ZolacosCPLabelAu" /><ref name="ZolacosCPLabelNZ" /> |
Bicalutamide is marketed by AstraZeneca in oral tablet form under the brand names Casodex, Cosudex, Calutide, Calumid, and Kalumid in many countries.<ref name="Drugs.com-2" /><ref name="IndexNominum2000" /><ref name="HuangJo2009">{{cite book | editor-first1 = De-Shuang | editor-last1 = Huang | editor-first2 = Kang-Hyun | editor-last2 = Jo | editor-first3 = Hong-Hee | editor-last3 = Lee | editor-first4 = Hee-Jun | editor-last4 = Kang | editor-first5 = Vitoantonio | editor-last5 = Bevilacqua |title=Emerging Intelligent Computing Technology and Applications: 5th International Conference on Intelligent Computing, ICIC 2009 Ulsan, South Korea, September 16–19, 2009 Proceedings |url=https://books.google.com/books?id=gRFtCQAAQBAJ&pg=PA120 |date=19 September 2009 |publisher=Springer |isbn=978-3-642-04070-2 |pages=120– |chapter=Parallel Genetic Algorithms for Crystal Structure Prediction: Successes and Failures in Predicting Bicalutamide Polymorphs |first1=Marta B. |last1=Ferraro |first2=Anita M. |last2=Orendt |first3=Julio C. |last3=Facelli | name-list-format = vanc |doi=10.1007/978-3-642-04070-2_14}}</ref><ref name="DhasIge2015">{{cite journal |last1=Dhas |first1=Namdev L. |last2=Ige |first2=Pradum P. |last3=Kudarha |first3=Ritu R. | name-list-format = vanc |title=Design, optimization and in-vitro study of folic acid conjugated-chitosan functionalized PLGA nanoparticle for delivery of bicalutamide in prostate cancer |journal=Powder Technology |volume=283 |year=2015 |pages=234–245 |doi=10.1016/j.powtec.2015.04.053}}</ref> It is also marketed under the brand names Bicadex, Bical, Bicalox, Bicamide, Bicatlon, Bicusan, Binabic, Bypro, Calutol, and Ormandyl among others in various countries.<ref name="Drugs.com-2" /> The drug is sold under a large number of generic trade names such as Apo-Bicalutamide, Bicalutamide Accord, Bicalutamide Actavis, Bicalutamide Bluefish, Bicalutamide Kabi, Bicalutamide Sandoz, and Bicalutamide Teva as well.<ref name="Drugs.com-2" /> A combination formulation of bicalutamide and goserelin is marketed by AstraZeneca in Australia and New Zealand under the brand name ZolaCos-CP.<ref name="Martindale2011" /><ref name="Drugs.com-3" /><ref name="ZolacosCPLabelAu" /><ref name="ZolacosCPLabelNZ" /> |
||
=== |
===Cost and generics=== |
||
Bicalutamide is a [[prescription drug]].<ref name="MortonHall2001" /> It is not specifically a [[controlled substance]] in any country and therefore is not an [[illegal drug]].<ref name="AHFS2016" /> However, the [[pharmaceutical manufacturing|manufacture]], [[legal drug trade|sale]], [[drug distribution|distribution]], and [[drug possession|possession]] of prescription drugs are all still subject to [[regulation of therapeutic goods|legal regulation]] throughout the world.<ref name="YagielaDowd2010">{{cite book |first1=John A. |last1=Yagiela |first2=Frank J. |last2=Dowd |first3=Bart |last3=Johnson |first4=Angelo |last4=Mariotti |first5=Enid A. |last5=Neidle | name-list-format = vanc |title=Pharmacology and Therapeutics for Dentistry |url=https://books.google.com/books?id=utVOHYuhxioC&pg=PA851 |date=19 March 2010 |publisher=Elsevier Health Sciences |isbn=0-323-07824-9 |pages=851–}}</ref><ref name="HeplerSegal2003">{{cite book |first1=Charles D. |last1=Hepler |first2=Richard |last2=Segal | name-list-format = vanc |title=Preventing Medication Errors and Improving Drug Therapy Outcomes: A Management Systems Approach |url=https://books.google.com/books?id=pvpZeDkaaIEC&pg=PA136 |date=25 February 2003 |publisher=CRC Press |isbn=978-0-203-01073-0 |pages=136–137}}</ref><ref name="DukesDukes1998">{{cite book |first1=Graham |last1=Dukes |first2=Maurice Nelson Graham |last2=Dukes |first3=Mark |last3=Mildred |first4=Barbara |last4=Swartz | name-list-format = vanc |title=Responsibility for Drug-induced Injury: A Reference Book for Lawyers, the Health Professions and Manufacturers |url=https://books.google.com/books?id=EQ3CZ1NaoQgC&pg=PA241 |date=January 1998 |publisher=IOS Press |isbn=978-90-5199-387-5 |pages=241–8}}</ref> |
|||
===Cost=== |
|||
Bicalutamide is off-patent and available as a generic, and its cost is very low in comparison to a number of other similar medications (from {{currency|10.00|USD|linked=no}} to {{currency|15.44|USD|linked=no}} for a 30-day supply of once-daily 50 mg tablets).<ref name="Drugs.com-1">{{cite web |url=http://www.drugs.com/price-guide/bicalutamide |title=Bicalutamide Prices, Coupons and Patient Assistance Programs |publisher=Drugs.com |accessdate=31 August 2015 |deadurl=no |archiveurl=https://web.archive.org/web/20150906121626/http://www.drugs.com/price-guide/bicalutamide |archivedate=6 September 2015 |df=dmy-all}}</ref><ref name="NADAC2016" /> Brand name Casodex costs {{currency|556.17|USD|linked=no}} for a 30-day supply of once-daily 50 mg tablets {{as of|2017|lc=y}}.<ref name="Drugs.com-4">{{cite web |url=https://www.drugs.com/price-guide/casodex |title=Casodex Prices, Coupons and Patient Assistance Programs |work=Drugs.com |deadurl=no |archiveurl=https://web.archive.org/web/20160417050012/http://www.drugs.com/price-guide/casodex |archivedate=17 April 2016 |df=dmy-all}}</ref> Unlike bicalutamide, the newer {{abbr|NSAA|nonsteroidal antiandrogen}} enzalutamide is still [[chemical patent|on-patent]], and for this reason, is far more expensive in comparison ({{currency|7,450|USD|linked=no}} for a 30-day supply {{as of|2015|lc=y}}).<ref name="RamadanKabbara2015">{{cite journal |vauthors=Ramadan WH, Kabbara WK, Al Basiouni Al Masri HS |title=Enzalutamide for patients with metastatic castration-resistant prostate cancer |journal=OncoTargets and Therapy |volume=8 |pages=871–6 |year=2015 |pmid=25945058 |doi=10.2147/OTT.S80488 |pmc=4407758}}</ref> |
Bicalutamide is off-patent and available as a generic, and its cost is very low in comparison to a number of other similar medications (from {{currency|10.00|USD|linked=no}} to {{currency|15.44|USD|linked=no}} for a 30-day supply of once-daily 50 mg tablets).<ref name="Drugs.com-1">{{cite web |url=http://www.drugs.com/price-guide/bicalutamide |title=Bicalutamide Prices, Coupons and Patient Assistance Programs |publisher=Drugs.com |accessdate=31 August 2015 |deadurl=no |archiveurl=https://web.archive.org/web/20150906121626/http://www.drugs.com/price-guide/bicalutamide |archivedate=6 September 2015 |df=dmy-all}}</ref><ref name="NADAC2016" /> Brand name Casodex costs {{currency|556.17|USD|linked=no}} for a 30-day supply of once-daily 50 mg tablets {{as of|2017|lc=y}}.<ref name="Drugs.com-4">{{cite web |url=https://www.drugs.com/price-guide/casodex |title=Casodex Prices, Coupons and Patient Assistance Programs |work=Drugs.com |deadurl=no |archiveurl=https://web.archive.org/web/20160417050012/http://www.drugs.com/price-guide/casodex |archivedate=17 April 2016 |df=dmy-all}}</ref> Unlike bicalutamide, the newer {{abbr|NSAA|nonsteroidal antiandrogen}} enzalutamide is still [[chemical patent|on-patent]], and for this reason, is far more expensive in comparison ({{currency|7,450|USD|linked=no}} for a 30-day supply {{as of|2015|lc=y}}).<ref name="RamadanKabbara2015">{{cite journal |vauthors=Ramadan WH, Kabbara WK, Al Basiouni Al Masri HS |title=Enzalutamide for patients with metastatic castration-resistant prostate cancer |journal=OncoTargets and Therapy |volume=8 |pages=871–6 |year=2015 |pmid=25945058 |doi=10.2147/OTT.S80488 |pmc=4407758}}</ref> |
||
| Line 456: | Line 344: | ||
Between January 2007 and December 2009 (a period of three years), 1,232,143 prescriptions of bicalutamide were dispensed in the {{abbr|U.S.|United States}}, or about 400,000 prescriptions per year.<ref name="HHS2010" /> During that time, bicalutamide accounted for about 87.2% of the {{abbr|NSAA|nonsteroidal antiandrogen}} market, while flutamide accounted for 10.5% of it and nilutamide for 2.3% of it.<ref name="HHS2010" /> Approximately 96% of bicalutamide prescriptions were written for diagnosis codes that clearly indicated [[neoplasm]].<ref name="HHS2010" /> About 1,200, or 0.1% of bicalutamide prescriptions were dispensed to pediatric patients (age 0–16).<ref name="HHS2010" /> |
Between January 2007 and December 2009 (a period of three years), 1,232,143 prescriptions of bicalutamide were dispensed in the {{abbr|U.S.|United States}}, or about 400,000 prescriptions per year.<ref name="HHS2010" /> During that time, bicalutamide accounted for about 87.2% of the {{abbr|NSAA|nonsteroidal antiandrogen}} market, while flutamide accounted for 10.5% of it and nilutamide for 2.3% of it.<ref name="HHS2010" /> Approximately 96% of bicalutamide prescriptions were written for diagnosis codes that clearly indicated [[neoplasm]].<ref name="HHS2010" /> About 1,200, or 0.1% of bicalutamide prescriptions were dispensed to pediatric patients (age 0–16).<ref name="HHS2010" /> |
||
===Regulation=== |
|||
Bicalutamide is a [[prescription drug]].<ref name="MortonHall2001" /> It is not specifically a [[controlled substance]] in any country and therefore is not an [[illegal drug]].<ref name="AHFS2016" /> However, the [[pharmaceutical manufacturing|manufacture]], [[legal drug trade|sale]], [[drug distribution|distribution]], and [[drug possession|possession]] of prescription drugs are all still subject to [[regulation of therapeutic goods|legal regulation]] throughout the world.<ref name="YagielaDowd2010">{{cite book |first1=John A. |last1=Yagiela |first2=Frank J. |last2=Dowd |first3=Bart |last3=Johnson |first4=Angelo |last4=Mariotti |first5=Enid A. |last5=Neidle | name-list-format = vanc |title=Pharmacology and Therapeutics for Dentistry |url=https://books.google.com/books?id=utVOHYuhxioC&pg=PA851 |date=19 March 2010 |publisher=Elsevier Health Sciences |isbn=0-323-07824-9 |pages=851–}}</ref><ref name="HeplerSegal2003">{{cite book |first1=Charles D. |last1=Hepler |first2=Richard |last2=Segal | name-list-format = vanc |title=Preventing Medication Errors and Improving Drug Therapy Outcomes: A Management Systems Approach |url=https://books.google.com/books?id=pvpZeDkaaIEC&pg=PA136 |date=25 February 2003 |publisher=CRC Press |isbn=978-0-203-01073-0 |pages=136–137}}</ref><ref name="DukesDukes1998">{{cite book |first1=Graham |last1=Dukes |first2=Maurice Nelson Graham |last2=Dukes |first3=Mark |last3=Mildred |first4=Barbara |last4=Swartz | name-list-format = vanc |title=Responsibility for Drug-induced Injury: A Reference Book for Lawyers, the Health Professions and Manufacturers |url=https://books.google.com/books?id=EQ3CZ1NaoQgC&pg=PA241 |date=January 1998 |publisher=IOS Press |isbn=978-90-5199-387-5 |pages=241–8}}</ref> |
|||
==Research== |
==Research== |
||
===Prostate cancer=== |
|||
A phase II clinical trial of bicalutamide with [[everolimus]] in {{abbr|mCRPC|metastatic castration-resistant prostate cancer}} has been conducted.<ref name="pmid27019001">{{cite journal |vauthors=Chow H, Ghosh PM, deVere White R, Evans CP, Dall'Era MA, Yap SA, Li Y, Beckett LA, Lara PN, Pan CX |title=A phase 2 clinical trial of everolimus plus bicalutamide for castration-resistant prostate cancer |journal=Cancer |volume=122 |issue=12 |pages=1897–904 |year=2016 |pmid=27019001 |doi=10.1002/cncr.29927 |laysummary=http://www.cancernetwork.com/news/bicalutamide-everolimus-combo-promising-crpc |laysource=Cancer Network}}</ref> Bicalutamide has also been studied in combination with the [[5α-reductase inhibitor]]s [[finasteride]] and [[dutasteride]] in prostate cancer.<ref name="pmid15138573">{{cite journal |vauthors=Wang LG, Mencher SK, McCarron JP, Ferrari AC |title=The biological basis for the use of an anti-androgen and a 5-alpha-reductase inhibitor in the treatment of recurrent prostate cancer: Case report and review |journal=Oncology Reports |volume=11 |issue=6 |pages=1325–9 |year=2004 |pmid=15138573 |doi= |url=}}</ref><ref name="pmid15151957">{{cite journal |vauthors=Tay MH, Kaufman DS, Regan MM, Leibowitz SB, George DJ, Febbo PG, Manola J, Smith MR, Kaplan ID, Kantoff PW, Oh WK |title=Finasteride and bicalutamide as primary hormonal therapy in patients with advanced adenocarcinoma of the prostate |journal=Annals of Oncology |volume=15 |issue=6 |pages=974–8 |year=2004 |pmid=15151957 |doi=10.1093/annonc/mdh221 |url=}}</ref><ref name="pmid16844453">{{cite journal |vauthors=Merrick GS, Butler WM, Wallner KE, Galbreath RW, Allen ZA, Kurko B |title=Efficacy of neoadjuvant bicalutamide and dutasteride as a cytoreductive regimen before prostate brachytherapy |journal=Urology |volume=68 |issue=1 |pages=116–20 |year=2006 |pmid=16844453 |doi=10.1016/j.urology.2006.01.061 |url=}}</ref><ref name="pmid19796455">{{cite journal |vauthors=Sartor O, Gomella LG, Gagnier P, Melich K, Dann R |title=Dutasteride and bicalutamide in patients with hormone-refractory prostate cancer: the Therapy Assessed by Rising PSA (TARP) study rationale and design |journal=The Canadian Journal of Urology |volume=16 |issue=5 |pages=4806–12 |year=2009 |pmid=19796455 |doi= |url=}}</ref><ref name="pmid26048455">{{cite journal |vauthors=Chu FM, Sartor O, Gomella L, Rudo T, Somerville MC, Hereghty B, Manyak MJ |title=A randomised, double-blind study comparing the addition of bicalutamide with or without dutasteride to GnRH analogue therapy in men with non-metastatic castrate-resistant prostate cancer |journal=European Journal of Cancer |volume=51 |issue=12 |pages=1555–69 |year=2015 |pmid=26048455 |doi=10.1016/j.ejca.2015.04.028 |url=}}</ref><ref name="pmid26702991">{{cite journal |vauthors=Gaudet M, Vigneault É, Foster W, Meyer F, Martin AG |title=Randomized non-inferiority trial of Bicalutamide and Dutasteride versus LHRH agonists for prostate volume reduction prior to I-125 permanent implant brachytherapy for prostate cancer |journal=Radiotherapy and Oncology : Journal of the European Society for Therapeutic Radiology and Oncology |volume=118 |issue=1 |pages=141–7 |year=2016 |pmid=26702991 |doi=10.1016/j.radonc.2015.11.022 |url=}}</ref><ref name="pmid27330919">{{cite journal |vauthors=Dijkstra S, Witjes WP, Roos EP, Vijverberg PL, Geboers AD, Bruins JL, Smits GA, Vergunst H, Mulders PF |title=The AVOCAT study: Bicalutamide monotherapy versus combined bicalutamide plus dutasteride therapy for patients with locally advanced or metastatic carcinoma of the prostate-a long-term follow-up comparison and quality of life analysis |journal=SpringerPlus |volume=5 |issue= |pages=653 |year=2016 |pmid=27330919 |pmc=4870485 |doi=10.1186/s40064-016-2280-8 |url=}}</ref> |
|||
===Benign prostatic hyperplasia=== |
|||
Bicalutamide has been studied in the treatment of [[benign prostatic hyperplasia]] (BPH) in a 24-week trial of 15 patients at a dosage of 50 mg/day.<ref name="Becker2001-2">{{cite book |first=Kenneth L. |last=Becker | name-list-format = vanc |title=Principles and Practice of Endocrinology and Metabolism |url=https://books.google.com/books?id=FVfzRvaucq8C&pg=PA1209 |year=2001 |publisher=Lippincott Williams & Wilkins |isbn=978-0-7817-1750-2 |page=1209 |deadurl=no |archiveurl=https://web.archive.org/web/20140628110255/http://books.google.com/books?id=FVfzRvaucq8C |archivedate=28 June 2014 |df=dmy-all}}</ref><ref name="pmid7694413">{{cite journal |vauthors=Lepor H |title=Medical therapy for benign prostatic hyperplasia |journal=Urology |volume=42 |issue=5 |pages=483–501 |year=1993 |pmid=7694413 |doi=10.1016/0090-4295(93)90258-c |url= |quote=The clinically significant adverse events reported in the casodex group included breast tenderness (93%), breast enlargement (54%), and sexual dysfunction (60%). In none of the patients in the placebo group did any of these adverse events develop. None of the subjects discontinued therapy owing to an adverse event.}}</ref> Prostate volume decreased by 26% in patients taking bicalutamide and [[dysuria|urinary irritative]] symptom scores significantly decreased.<ref name="Becker2001-2" /><ref name="pmid7694413" /> Conversely, peak [[urine flow rate]]s and [[urodynamic testing|urine pressure flow]] examinations were not significantly different between bicalutamide and placebo.<ref name="Becker2001-2" /><ref name="pmid7694413" /> The decrease in prostate volume achieved with bicalutamide was comparable to that observed with the 5α-reductase inhibitor finasteride, which is approved for the treatment of BPH.<ref name="pmid9101011">{{cite journal |vauthors=Lee M, Sharifi R |title=Benign prostatic hyperplasia: diagnosis and treatment guideline |journal=Ann Pharmacother |volume=31 |issue=4 |pages=481–6 |year=1997 |pmid=9101011 |doi=10.1177/106002809703100415 |url=}}</ref><ref name="pmid9135028">{{cite journal |vauthors=Kenny B, Ballard S, Blagg J, Fox D |title=Pharmacological options in the treatment of benign prostatic hyperplasia |journal=J. Med. Chem. |volume=40 |issue=9 |pages=1293–315 |year=1997 |pmid=9135028 |doi=10.1021/jm960697s |url=}}</ref> Breast tenderness (93%), gynecomastia (54%), and sexual dysfunction (60%) were all reported as side effects of bicalutamide at the dosage used in the study, although no treatment discontinuations due to adverse effects occurred and sexual functioning was maintained in 75% of patients.<ref name="pmid7694413" /><ref name="Kolvenbag1996" /> |
Bicalutamide has been studied in the treatment of [[benign prostatic hyperplasia]] (BPH) in a 24-week trial of 15 patients at a dosage of 50 mg/day.<ref name="Becker2001-2">{{cite book |first=Kenneth L. |last=Becker | name-list-format = vanc |title=Principles and Practice of Endocrinology and Metabolism |url=https://books.google.com/books?id=FVfzRvaucq8C&pg=PA1209 |year=2001 |publisher=Lippincott Williams & Wilkins |isbn=978-0-7817-1750-2 |page=1209 |deadurl=no |archiveurl=https://web.archive.org/web/20140628110255/http://books.google.com/books?id=FVfzRvaucq8C |archivedate=28 June 2014 |df=dmy-all}}</ref><ref name="pmid7694413">{{cite journal |vauthors=Lepor H |title=Medical therapy for benign prostatic hyperplasia |journal=Urology |volume=42 |issue=5 |pages=483–501 |year=1993 |pmid=7694413 |doi=10.1016/0090-4295(93)90258-c |url= |quote=The clinically significant adverse events reported in the casodex group included breast tenderness (93%), breast enlargement (54%), and sexual dysfunction (60%). In none of the patients in the placebo group did any of these adverse events develop. None of the subjects discontinued therapy owing to an adverse event.}}</ref> Prostate volume decreased by 26% in patients taking bicalutamide and [[dysuria|urinary irritative]] symptom scores significantly decreased.<ref name="Becker2001-2" /><ref name="pmid7694413" /> Conversely, peak [[urine flow rate]]s and [[urodynamic testing|urine pressure flow]] examinations were not significantly different between bicalutamide and placebo.<ref name="Becker2001-2" /><ref name="pmid7694413" /> The decrease in prostate volume achieved with bicalutamide was comparable to that observed with the 5α-reductase inhibitor finasteride, which is approved for the treatment of BPH.<ref name="pmid9101011">{{cite journal |vauthors=Lee M, Sharifi R |title=Benign prostatic hyperplasia: diagnosis and treatment guideline |journal=Ann Pharmacother |volume=31 |issue=4 |pages=481–6 |year=1997 |pmid=9101011 |doi=10.1177/106002809703100415 |url=}}</ref><ref name="pmid9135028">{{cite journal |vauthors=Kenny B, Ballard S, Blagg J, Fox D |title=Pharmacological options in the treatment of benign prostatic hyperplasia |journal=J. Med. Chem. |volume=40 |issue=9 |pages=1293–315 |year=1997 |pmid=9135028 |doi=10.1021/jm960697s |url=}}</ref> Breast tenderness (93%), gynecomastia (54%), and sexual dysfunction (60%) were all reported as side effects of bicalutamide at the dosage used in the study, although no treatment discontinuations due to adverse effects occurred and sexual functioning was maintained in 75% of patients.<ref name="pmid7694413" /><ref name="Kolvenbag1996" /> |
||
A phase II clinical trial of bicalutamide with [[everolimus]] in {{abbr|mCRPC|metastatic castration-resistant prostate cancer}} has been conducted.<ref name="pmid27019001">{{cite journal |vauthors=Chow H, Ghosh PM, deVere White R, Evans CP, Dall'Era MA, Yap SA, Li Y, Beckett LA, Lara PN, Pan CX |title=A phase 2 clinical trial of everolimus plus bicalutamide for castration-resistant prostate cancer |journal=Cancer |volume=122 |issue=12 |pages=1897–904 |year=2016 |pmid=27019001 |doi=10.1002/cncr.29927 |laysummary=http://www.cancernetwork.com/news/bicalutamide-everolimus-combo-promising-crpc |laysource=Cancer Network}}</ref> Bicalutamide has also been studied in combination with the [[5α-reductase inhibitor]]s [[finasteride]] and [[dutasteride]] in prostate cancer.<ref name="pmid15138573">{{cite journal |vauthors=Wang LG, Mencher SK, McCarron JP, Ferrari AC |title=The biological basis for the use of an anti-androgen and a 5-alpha-reductase inhibitor in the treatment of recurrent prostate cancer: Case report and review |journal=Oncology Reports |volume=11 |issue=6 |pages=1325–9 |year=2004 |pmid=15138573 |doi= |url=}}</ref><ref name="pmid15151957">{{cite journal |vauthors=Tay MH, Kaufman DS, Regan MM, Leibowitz SB, George DJ, Febbo PG, Manola J, Smith MR, Kaplan ID, Kantoff PW, Oh WK |title=Finasteride and bicalutamide as primary hormonal therapy in patients with advanced adenocarcinoma of the prostate |journal=Annals of Oncology |volume=15 |issue=6 |pages=974–8 |year=2004 |pmid=15151957 |doi=10.1093/annonc/mdh221 |url=}}</ref><ref name="pmid16844453">{{cite journal |vauthors=Merrick GS, Butler WM, Wallner KE, Galbreath RW, Allen ZA, Kurko B |title=Efficacy of neoadjuvant bicalutamide and dutasteride as a cytoreductive regimen before prostate brachytherapy |journal=Urology |volume=68 |issue=1 |pages=116–20 |year=2006 |pmid=16844453 |doi=10.1016/j.urology.2006.01.061 |url=}}</ref><ref name="pmid19796455">{{cite journal |vauthors=Sartor O, Gomella LG, Gagnier P, Melich K, Dann R |title=Dutasteride and bicalutamide in patients with hormone-refractory prostate cancer: the Therapy Assessed by Rising PSA (TARP) study rationale and design |journal=The Canadian Journal of Urology |volume=16 |issue=5 |pages=4806–12 |year=2009 |pmid=19796455 |doi= |url=}}</ref><ref name="pmid26048455">{{cite journal |vauthors=Chu FM, Sartor O, Gomella L, Rudo T, Somerville MC, Hereghty B, Manyak MJ |title=A randomised, double-blind study comparing the addition of bicalutamide with or without dutasteride to GnRH analogue therapy in men with non-metastatic castrate-resistant prostate cancer |journal=European Journal of Cancer |volume=51 |issue=12 |pages=1555–69 |year=2015 |pmid=26048455 |doi=10.1016/j.ejca.2015.04.028 |url=}}</ref><ref name="pmid26702991">{{cite journal |vauthors=Gaudet M, Vigneault É, Foster W, Meyer F, Martin AG |title=Randomized non-inferiority trial of Bicalutamide and Dutasteride versus LHRH agonists for prostate volume reduction prior to I-125 permanent implant brachytherapy for prostate cancer |journal=Radiotherapy and Oncology : Journal of the European Society for Therapeutic Radiology and Oncology |volume=118 |issue=1 |pages=141–7 |year=2016 |pmid=26702991 |doi=10.1016/j.radonc.2015.11.022 |url=}}</ref><ref name="pmid27330919">{{cite journal |vauthors=Dijkstra S, Witjes WP, Roos EP, Vijverberg PL, Geboers AD, Bruins JL, Smits GA, Vergunst H, Mulders PF |title=The AVOCAT study: Bicalutamide monotherapy versus combined bicalutamide plus dutasteride therapy for patients with locally advanced or metastatic carcinoma of the prostate-a long-term follow-up comparison and quality of life analysis |journal=SpringerPlus |volume=5 |issue= |pages=653 |year=2016 |pmid=27330919 |pmc=4870485 |doi=10.1186/s40064-016-2280-8 |url=}}</ref> Bicalutamide has been tested for the treatment of {{abbr|AR|androgen receptor}}-positive {{abbr|ER|estrogen receptor}}/[[progesterone receptor|{{abbr|PR|progesterone receptor}}]]-negative locally advanced and [[metastatic breast cancer]] in a phase II study for this indication.<ref>{{cite journal |url=http://meetinglibrary.asco.org/content/94715-114 |title=Targeting the androgen receptor (AR) in women with AR+ ER-/PR- metastatic breast cancer (MBC) |journal=J Clin Oncol |year=2012 |issue=suppl |page=abstract 1006 |author=Translational Breast Cancer Research Consortium (TBCRC) |deadurl=no |archiveurl=https://web.archive.org/web/20150710035954/http://meetinglibrary.asco.org/content/94715-114 |archivedate=10 July 2015 |df=dmy-all}}</ref><ref>{{ClinicalTrialsGov|NCT00468715|Bicalutamide in Treating Patients With Metastatic Breast Cancer}}</ref><ref>{{cite journal |vauthors=Gucalp A, Tolaney S, Isakoff SJ, Ingle JN, Liu MC, Carey LA, Blackwell K, Rugo H, Nabell L, Forero A, Stearns V, Doane AS, Danso M, Moynahan ME, Momen LF, Gonzalez JM, Akhtar A, Giri DD, Patil S, Feigin KN, Hudis CA, Traina TA |title=Phase II trial of bicalutamide in patients with androgen receptor-positive, estrogen receptor-negative metastatic Breast Cancer |journal=Clinical Cancer Research |volume=19 |issue=19 |pages=5505–12 |date=October 2013 |pmid=23965901 |pmc=4086643 |doi=10.1158/1078-0432.CCR-12-3327 |author23=Translational Breast Cancer Research Consortium (TBCRC 011)}}</ref> Enzalutamide is also being investigated for this type of cancer.<ref name="CaiazzaMurray2016">{{cite journal |vauthors=Caiazza F, Murray A, Madden SF, Synnott NC, Ryan EJ, O'Donovan N, Crown J, Duffy MJ |title=Preclinical evaluation of the AR inhibitor enzalutamide in triple-negative breast cancer cells |journal=Endocrine-Related Cancer |volume=23 |issue=4 |pages=323–34 |date=April 2016 |pmid=26932782 |doi=10.1530/ERC-16-0068}}</ref><ref>{{cite journal |vauthors=Traina TA, etal |title=Results from a phase 2 study of enzalutamide (ENZA), an androgen receptor (AR) inhibitor, in advanced AR+ triple-negative breast cancer (TNBC). |journal=Journal of Clinical Oncology |volume=33 |date=2015 |issue=suppl |page=abstr 1003 |url=http://meetinglibrary.asco.org/content/150040-156 |deadurl=no |archiveurl=https://web.archive.org/web/20160530074130/http://meetinglibrary.asco.org/content/150040-156 |archivedate=30 May 2016 |df=dmy-all}}</ref> Bicalutamide has also been studied in a phase II clinical trial for [[ovarian cancer]].<ref name="pmid17918264">{{cite journal |vauthors=Levine D, Park K, Juretzka M, Esch J, Hensley M, Aghajanian C, Lewin S, Konner J, Derosa F, Spriggs D, Iasonos A, Sabbatini P |title=A phase II evaluation of goserelin and bicalutamide in patients with ovarian cancer in second or higher complete clinical disease remission |journal=Cancer |volume=110 |issue=11 |pages=2448–56 |date=December 2007 |pmid=17918264 |doi=10.1002/cncr.23072}}</ref> |
|||
==={{abbr|AR|Androgen receptor}}-positive breast cancer=== |
|||
Bicalutamide has been tested for the treatment of {{abbr|AR|androgen receptor}}-positive {{abbr|ER|estrogen receptor}}/[[progesterone receptor|{{abbr|PR|progesterone receptor}}]]-negative locally advanced and [[metastatic breast cancer]] in a phase II study for this indication.<ref>{{cite journal |url=http://meetinglibrary.asco.org/content/94715-114 |title=Targeting the androgen receptor (AR) in women with AR+ ER-/PR- metastatic breast cancer (MBC) |journal=J Clin Oncol |year=2012 |issue=suppl |page=abstract 1006 |author=Translational Breast Cancer Research Consortium (TBCRC) |deadurl=no |archiveurl=https://web.archive.org/web/20150710035954/http://meetinglibrary.asco.org/content/94715-114 |archivedate=10 July 2015 |df=dmy-all}}</ref><ref>{{ClinicalTrialsGov|NCT00468715|Bicalutamide in Treating Patients With Metastatic Breast Cancer}}</ref><ref>{{cite journal |vauthors=Gucalp A, Tolaney S, Isakoff SJ, Ingle JN, Liu MC, Carey LA, Blackwell K, Rugo H, Nabell L, Forero A, Stearns V, Doane AS, Danso M, Moynahan ME, Momen LF, Gonzalez JM, Akhtar A, Giri DD, Patil S, Feigin KN, Hudis CA, Traina TA |title=Phase II trial of bicalutamide in patients with androgen receptor-positive, estrogen receptor-negative metastatic Breast Cancer |journal=Clinical Cancer Research |volume=19 |issue=19 |pages=5505–12 |date=October 2013 |pmid=23965901 |pmc=4086643 |doi=10.1158/1078-0432.CCR-12-3327 |author23=Translational Breast Cancer Research Consortium (TBCRC 011)}}</ref> Enzalutamide is also being investigated for this type of cancer.<ref name="CaiazzaMurray2016">{{cite journal |vauthors=Caiazza F, Murray A, Madden SF, Synnott NC, Ryan EJ, O'Donovan N, Crown J, Duffy MJ |title=Preclinical evaluation of the AR inhibitor enzalutamide in triple-negative breast cancer cells |journal=Endocrine-Related Cancer |volume=23 |issue=4 |pages=323–34 |date=April 2016 |pmid=26932782 |doi=10.1530/ERC-16-0068}}</ref><ref>{{cite journal |vauthors=Traina TA, etal |title=Results from a phase 2 study of enzalutamide (ENZA), an androgen receptor (AR) inhibitor, in advanced AR+ triple-negative breast cancer (TNBC). |journal=Journal of Clinical Oncology |volume=33 |date=2015 |issue=suppl |page=abstr 1003 |url=http://meetinglibrary.asco.org/content/150040-156 |deadurl=no |archiveurl=https://web.archive.org/web/20160530074130/http://meetinglibrary.asco.org/content/150040-156 |archivedate=30 May 2016 |df=dmy-all}}</ref> |
|||
===Ovarian cancer=== |
|||
Bicalutamide has been studied in a phase II clinical trial for [[ovarian cancer]].<ref name="pmid17918264">{{cite journal |vauthors=Levine D, Park K, Juretzka M, Esch J, Hensley M, Aghajanian C, Lewin S, Konner J, Derosa F, Spriggs D, Iasonos A, Sabbatini P |title=A phase II evaluation of goserelin and bicalutamide in patients with ovarian cancer in second or higher complete clinical disease remission |journal=Cancer |volume=110 |issue=11 |pages=2448–56 |date=December 2007 |pmid=17918264 |doi=10.1002/cncr.23072}}</ref> |
|||
==Veterinary use== |
==Veterinary use== |
||
| Line 510: | Line 392: | ||
[[Category:Antiandrogens]] |
[[Category:Antiandrogens]] |
||
[[Category:AstraZeneca]] |
[[Category:AstraZeneca]] |
||
[[Category:Bicalutamide]] |
|||
[[Category:Hair loss medications]] |
[[Category:Hair loss medications]] |
||
[[Category:Hair removal]] |
[[Category:Hair removal]] |
||
Revision as of 09:02, 23 November 2017
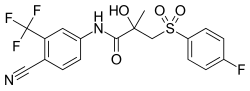 | |
 | |
| Clinical data | |
|---|---|
| Pronunciation | Bicalutamide: ⫽baɪkəˈluːtəmaɪd⫽ bye-kə-LOO-tə-myde[1] Casodex: ⫽ˈkeɪsoʊdɛks⫽ KAY-soh-deks[2] |
| Trade names | Casodex, others |
| Other names | ICI-176,334; ZD-176,334 |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a697047 |
| License data |
|
| Pregnancy category |
|
| Routes of administration | By mouth[3] |
| Drug class | Nonsteroidal antiandrogen |
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Bioavailability | Well-absorbed; absolute bioavailability unknown[4] |
| Protein binding | Racemate: 96.1%[3] (R)-Isomer: 99.6%[3] (Mainly to albumin)[3] |
| Metabolism | Liver (extensively):[5][10] • Hydroxylation (CYP3A4) • Glucuronidation (UGT1A9) |
| Metabolites | • Bicalutamide glucuronide • Hydroxybicalutamide • Hydroxybicalutamide gluc. (All inactive)[5][3][6][7] |
| Elimination half-life | Acute: 5.8 days[8] Chronic: 7–10 days[9] |
| Excretion | Feces: 43%[5] Urine: 34%[5] |
| Identifiers | |
| |
| CAS Number |
|
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| PDB ligand | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.126.100 |
| Chemical and physical data | |
| Formula | C18H14F4N2O4S |
| Molar mass | 430.373 g/mol g·mol−1 |
| 3D model (JSmol) | |
| Chirality | Racemic mixture (of (R)- and (S)-enantiomers) |
| Melting point | 191 to 193 °C (376 to 379 °F) (experimental) |
| Boiling point | 650 °C (1,202 °F) (predicted) |
| Solubility in water | 0.005 mg/mL (20 °C) |
| |
| |
| | |
Bicalutamide, sold under the brand name Casodex among others, is an antiandrogen medication that is primarily used to treat prostate cancer.[11] It is typically used together with a gonadotropin-releasing hormone (GnRH) analogue or surgical removal of the testicles to treat metastatic prostate cancer.[12][11][13] Bicalutamide may also be used to treat excessive hair growth in women,[14] as a component of hormone therapy for transgender women,[15] to treat early puberty in boys,[16] and to prevent priapism.[17] It is taken by mouth.[11]
Common side effects in men include breast enlargement, breast tenderness, and hot flashes.[11] Other side effects in men include feminization and sexual dysfunction.[18] While the medication appears to produce few side effects in women, its use in women is not recommended by the Food and Drug Administration (FDA).[19][11] Use during pregnancy may harm the baby.[11] Bicalutamide causes elevated liver enzymes in around 1% of people.[20][21] Rarely, it has been associated with cases of liver damage,[11] lung toxicity,[4] and sensitivity to light.[22][23] Although the risk of adverse liver changes is small, monitoring of liver enzymes is recommended during treatment.[11]
Bicalutamide is a member of the nonsteroidal antiandrogen (NSAA) group of medications.[4] It works by blocking the androgen receptor (AR), the biological target of the androgen sex hormones testosterone and dihydrotestosterone (DHT).[24] It does not lower androgen levels.[4] The medication can have some estrogen-like effects in men.[25][26][27] Bicalutamide is well-absorbed, and its absorption is not affected by food.[3] The elimination half-life of the medication is around one week.[3][11] It is believed to cross the blood–brain barrier and affect both the body and brain.[3]
Bicalutamide was patented in 1982 and approved for medical use in 1995.[28] It is on the World Health Organization's List of Essential Medicines, the most effective and safe medicines needed in a health system.[29] Bicalutamide is available as a generic medication.[30] The wholesale cost in the developing world is about US$7.07 to US$144.22 per month.[31] In the United States it costs about US$10 and above per month.[32] The drug is sold in more than 80 countries, including most developed countries.[33][34][35] It is the most widely used antiandrogen in the treatment of prostate cancer, and has been prescribed to millions of men with the disease.[36][37][38][39]
Medical uses
Bicalutamide is mainly used in and is only approved for the following indications:[40]
- Metastatic prostate cancer (mPC) in men in combination with a gonadotropin-releasing hormone (GnRH) analogue or orchiectomy at moderate doses[5][41]
- Locally advanced prostate cancer (LAPC) in men as a monotherapy in high doses[5][3][21][42]
It can also be and is used to a lesser extent for the following off-label (non-approved) indications:
- Androgen-dependent skin and hair conditions such as acne, seborrhea, hirsutism, and pattern hair loss (androgenic alopecia) in women at low doses, generally in combination with an oral contraceptive[14][43][44][45][46]
- Hyperandrogenism such as due to polycystic ovary syndrome (PCOS) or congenital adrenal hyperplasia (CAH) in women
- Hormone therapy for transgender women in combination with an estrogen (e.g., estradiol)[15][47][48][49][50]
- Precocious puberty in boys in moderate doses, especially due to familial male-limited precocious puberty (testotoxicosis)[51][52][53][54][55][16]
- Priapism in men at low to very low doses[56][57][58][59][4][8][17]
It has been suggested for but has uncertain effectiveness in the following indications:
- Hypersexuality and paraphilias, particularly in combination with chemical castration[60][61][62][63][64][65]
Available forms
Bicalutamide is available for the treatment of prostate cancer in most developed countries,[66][33][67] including over 80 countries worldwide.[34][35] Bicalutamide is available in 50 mg, 80 mg (in Japan),[68] and 150 mg tablets for oral administration.[69][70] The drug is registered for use as a 150 mg/day monotherapy for the treatment of LAPC in at least 55 countries,[3] with the U.S. being a notable exception where it is registered only for use at a dosage of 50 mg/day in combination with castration.[71] No other formulations or routes of administration are available or used.[69] All formulations of bicalutamide are specifically indicated for the treatment of prostate cancer alone or in combination with surgical or medication castration.[5] A combined formulation of bicalutamide and the GnRH agonist goserelin in which goserelin is provided as a subcutaneous implant for injection and bicalutamide is included as 50 mg tablets for oral ingestion is marketed in Australia and New Zealand under the brand name ZolaCos CP (Zoladex–Cosudex Combination Pack).[67][72][73][74]
Contraindications
In individuals with severe, though not mild-to-moderate hepatic impairment, there is evidence that the elimination of bicalutamide is slowed, and hence, caution may be warranted in these patients as circulating levels of bicalutamide may be increased.[3][75] In severe hepatic impairment, the elimination half-life of the active (R)-enantiomer of bicalutamide is increased by about 1.75-fold (76% increase; elimination half-life of 5.9 and 10.4 days for normal and impaired patients, respectively).[21][76][77] The elimination half-life of bicalutamide is unchanged in renal impairment.[71]
Bicalutamide is pregnancy category X, or "contraindicated in pregnancy", in the U.S.,[20] and pregnancy category D, the second most restricted rating, in Australia.[78] As such, it is contraindicated in women during pregnancy, and women who are sexually active and who can or may become pregnant are strongly recommended to take bicalutamide only in combination with adequate contraception.[79][80] It is unknown whether bicalutamide is excreted in breast milk, but many drugs are excreted in breast milk, and for this reason, bicalutamide treatment is similarly not recommended while breastfeeding.[4][20]
Side effects
The side effect profile of bicalutamide is highly dependent on sex; that is, on whether the person is male or female. In men, due to androgen deprivation, a variety of side effects of varying severity may occur during bicalutamide treatment, with breast pain/tenderness and gynecomastia (breast development/enlargement) being the most common.[81][82] In addition breast changes, physical feminization and demasculinization in general, including reduced body hair growth, decreased muscle mass and strength, feminine changes in fat mass and distribution, and reduced penile length, may also occur in men.[81][83][18][84] Other side effects that have been observed in men and that are similarly related to androgen deprivation include hot flashes, sexual dysfunction (e.g., loss of libido, erectile dysfunction), depression, fatigue, weakness, anemia, and decreased semen/ejaculate volume.[81][85][86] In women, on the other hand, due to the little biological importance of androgens in this sex,[87][88] the side effects of pure antiandrogens or NSAAs are minimal, and bicalutamide has been found to be very well-tolerated.[19] General side effects of bicalutamide that may occur in either sex include diarrhea, constipation, abdominal pain, nausea, dry skin,[89] itching, and rash.[85][4][90][91][92] The drug is well-tolerated at higher dosages than the 50 mg/day dosage, with rare additional side effects.[71]
Bicalutamide monotherapy has been associated with abnormal liver function tests such as elevated liver enzymes in 3.4% of men relative to 1.9% for standard care.[21][93] Hepatic changes such as marked increases in liver enzymes or hepatitis that necessitated discontinuation of bicalutamide have occurred in approximately 0.3 to 1% of men in clinical trials.[20][27] Monitoring of liver function during treatment is recommended, particularly in the first few months.[21][81] In men of advanced age with prostate cancer, bicalutamide monotherapy has been associated with an increase in non-prostate cancer mortality, in part due to an increase in the rate of heart failure.[94][21] These mortality-related effects are thought to be a consequence of androgen deprivation, rather than a specific drug-related toxicity of bicalutamide.[95]
Five cases of hepatotoxicity or liver failure, two of which resulted in death, have been reported with bicalutamide.[96][97] Symptoms that may indicate liver dysfunction include nausea, vomiting, abdominal pain, fatigue, anorexia, "flu-like" symptoms, dark urine, and jaundice.[20] Bicalutamide has also been associated with several case reports of interstitial pneumonitis, which can potentially progress to pulmonary fibrosis.[98][99][100] Symptoms that may indicate lung dysfunction include dyspnea (difficult breathing or shortness of breath), cough, and pharyngitis (inflammation of the pharynx, resulting in sore throat).[101] Both hepatotoxicity and interstitial pneumonitis are said to be extremely rare events with bicalutamide.[96][102][103] A few cases of photosensitivity have been reported with bicalutamide.[22] Hypersensitivity reactions (drug allergy) like angioedema and hives have also uncommonly been reported in association with bicalutamide.[20]
Overdose
A single oral dose of bicalutamide in humans that results in symptoms of overdose or that is considered to be life-threatening has not been established.[20][104] Dosages of up to 600 mg/day have been well-tolerated in clinical trials,[105] and it is notable that there is a saturation of absorption with bicalutamide such that circulating levels of its active (R)-enantiomer do not further increase above a dosage of 300 mg/day.[3][105] Overdose is considered to be unlikely to be life-threatening with bicalutamide or other first-generation NSAAs (i.e., flutamide and nilutamide).[106] A massive overdose of nilutamide (13 grams, or 43 times the normal maximum 300 mg/day clinical dosage) in a 79-year-old man was uneventful, producing no clinical signs or symptoms or toxicity.[107] There is no specific antidote for bicalutamide or NSAA overdose, and treatment should be based on symptoms.[20][104]
Interactions
Bicalutamide is almost exclusively metabolized by CYP3A4.[5] As such, its levels in the body may be altered by inhibitors and inducers of CYP3A4.[8] (For a list of CYP3A4 inhibitors and inducers, see here.) However, in spite of the fact bicalutamide is metabolized by CYP3A4, there is no evidence of clinically significant drug interactions when bicalutamide at a dosage of 150 mg/day or less is co-administered with drugs that inhibit or induce cytochrome P450 enzyme activity.[21]
Because bicalutamide circulates at relatively high concentrations and is highly protein-bound, it has the potential to displace other highly protein-bound drugs like warfarin, phenytoin, theophylline, and aspirin from plasma binding proteins.[82][85] This could, in turn, result in increased free concentrations of such drugs and increased effects and/or side effects, potentially necessitating dosage adjustments.[82] Bicalutamide has specifically been found to displace coumarin anticoagulants like warfarin from their plasma binding proteins (namely albumin) in vitro, potentially resulting in an increased anticoagulant effect, and for this reason, close monitoring of prothrombin time and dosage adjustment as necessary is recommended when bicalutamide is used in combination with these drugs.[108][109][110] However, in spite of this, no conclusive evidence of an interaction between bicalutamide and other drugs was found in clinical trials of nearly 3,000 patients.[85]
Pharmacology
Pharmacodynamics
Antiandrogenic activity
Bicalutamide acts as a highly selective competitive silent antagonist of the AR (IC50 = 159–243 nM), the major biological target of the androgen sex hormones testosterone and DHT, and hence is an antiandrogen.[24][111][112][113] The activity of bicalutamide lies in the (R)-isomer.[114] Due to its selectivity for the AR, bicalutamide does not bind to other steroid hormone receptors and hence has no off-target hormonal activity (e.g., progestogenic, glucocorticoid, antimineralocorticoid).[115][116][114][40] It also does not inhibit 5α-reductase nor is known to inhibit other androgen steroidogenic enzymes (e.g., CYP17A1).[117] Although it does not bind to the estrogen receptors (ERs), bicalutamide can increase estrogen levels secondary to AR blockade when used as a monotherapy in males, and hence can have some indirect estrogenic effects in males.[118] Bicalutamide neither suppresses nor inhibits androgen production in the body (i.e., it does not act as an antigonadotropin or androgen steroidogenesis inhibitor or lower androgen levels) and hence exclusively mediates its antiandrogenic effects by antagonizing the AR.[4][115][114] In addition to the classical nuclear AR, bicalutamide has been assessed at the membrane androgen receptors (mARs) and found to act as a potent antagonist of ZIP9 (IC50 = 66.3 nM), whereas it does not appear to interact with GPRC6A.[119][120]
The affinity of bicalutamide for the AR is relatively low as it is approximately 50 times lower than that of DHT, which is 2.5- to 10-fold as potent as an AR agonist as testosterone in bioassays and is the main endogenous ligand of the receptor in the prostate gland.[121][113] However, typical clinical dosages of bicalutamide result in circulating levels of the drug that are thousands of times higher than those of testosterone and DHT, allowing it to efficaciously prevent them from binding to and activating the receptor.[122][116][123][20][78][124][21][125] This is especially true in the case of surgical or medical castration, in which testosterone levels in the circulation are approximately 95% reduced and DHT levels in the prostate gland are about 50 to 60% reduced.[113][126] In women, levels of testosterone are substantially lower than in men (20- to 40-fold),[127] so much smaller doses of bicalutamide (e.g., 25 mg/day in the hirsutism studies) are necessary.[14][43][128][27]
Blockade of the AR by bicalutamide in the pituitary gland and hypothalamus results in prevention of the negative feedback of androgens on the hypothalamic–pituitary–gonadal (HPG) axis in males and consequent disinhibition of pituitary luteinizing hormone (LH) secretion.[129] This, in turn, results in an increase in circulating LH levels and activation of the gonadal production of testosterone and by extension production of estradiol.[130] Levels of testosterone have been found to increase 1.5- to 2-fold (59–97% increase) and levels of estradiol about 1.5- to 2.5-fold (65–146% increase) in men treated with 150 mg/day bicalutamide monotherapy.[25][26][27] In addition to testosterone and estradiol, there are smaller increases in concentrations of DHT, sex hormone-binding globulin, and prolactin.[27] Estradiol levels with bicalutamide monotherapy are similar to those in the low-normal premenopausal female range while testosterone levels generally remain in the high end of normal male range.[26][131][115] Testosterone concentrations do not typically exceed the normal male range due to negative feedback on the HPG axis by the increased concentrations of estradiol.[129] Bicalutamide influences the HPG axis and increases hormone levels only in men and not also in women.[132][133][134] This is due to the much lower levels of androgens in women and their lack of basal suppression of the HPG axis in this sex.[132][133][134] As evidenced by its effectiveness in the treatment of prostate cancer and other androgen-dependent conditions, the antiandrogenic actions of bicalutamide greatly exceed any impact of the increased levels of testosterone it results in.[71] However, the elevated levels of estradiol remain unopposed by bicalutamide and are responsible for the gynecomastia and feminizing side effects it causes in men.[135]
NSAA monotherapy, including with bicalutamide, shows a number of tolerability differences from methods of androgen deprivation therapy that incorporate surgical or medical castration. For example, the rates of hot flashes, depression, fatigue, and sexual dysfunction are all much higher with GnRH analogues than with NSAA monotherapy. It is thought that this is because GnRH analogues suppress estrogen production in addition to androgen production, resulting in estrogen deficiency.[136][137][138] In contrast, NSAA monotherapy does not decrease estrogen levels and in fact increases them, resulting in an excess of estrogens that compensates for androgen deficiency and allows for a preservation of mood, energy, and sexual function.[136][137][138] Neurosteroids that are produced from testosterone like 3α-androstanediol and 3β-androstanediol may also be involved.[139][140][139][140][141][142][142][143][144][145] In the specific case of sexual dysfunction, an additional possibility for the difference is that without concomitant suppression of androgen production, blockade of the AR by the bicalutamide in the brain is incomplete and insufficient to markedly influence sexual function.[citation needed]
Under normal circumstances, bicalutamide has no capacity to activate the AR.[146][147] However, in prostate cancer, mutations and overexpression of the AR can accumulate in prostate gland cells which can convert bicalutamide from an antagonist of the AR into an agonist.[146][148] This can result in paradoxical stimulation of prostate cancer growth with bicalutamide and is responsible for the phenomenon of the antiandrogen withdrawal syndrome, where antiandrogen discontinuation paradoxically slows the rate of prostate cancer growth.[146][148]
In transgender women, breast development is a desired effect of antiandrogen and/or estrogen treatment.[49][149] Breast development and gynecomastia induced by bicalutamide in people who are biologically male is thought to be mediated by increased activation of the ER secondary to blockade of the AR (resulting in disinhibition of the ER in breast tissue) and increased levels of estradiol.[16][150][151] In addition to fat deposition, connective tissue growth, and ductal development, bicalutamide has been found to produce moderate lobuloalveolar development of the breasts.[152][153][154] However, full lobuloalveolar maturation necessary for lactation and breastfeeding will not occur without progestogen treatment.[152][153][154]
Bicalutamide monotherapy seems to have minimal effect on spermatogenesis, testicular ultrastructure, and male fertility.[155][156][79][155] This seems to be because testosterone levels in the testes (where ~95% of testosterone in males is produced) are extremely high (up to 200-fold higher than circulating levels) and only a small fraction (less than 10%) of the normal levels of testosterone in the testes are actually necessary to maintain spermatogenesis.[157][158][158][159] As a result, bicalutamide seems to not be able to compete with testosterone in this sole part of the body to an extent sufficient to considerably interfere with androgen signaling and function.[157][158][158][159] However, suppression of gonadal androgen production, such as by taking an estrogen, progestogen, or GnRH analogue with bicalutamide, can compromise this due to their own adverse effects on spermatogenesis and fertility.[160][161][162][163][164][165]
Other activities
Bicalutamide has been found to act as an inhibitor or inducer of certain cytochrome P450 enzymes including CYP3A4, CYP2C9, CYP2C19, and CYP2D6 in preclinical research, but no evidence of this has been found in humans treated with up to 150 mg/day.[3] It has also been identified in vitro as a strong inhibitor of CYP27A1 (cholesterol 27-hydroxylase) and as an inhibitor of CYP46A1 (cholesterol 24-hydroxylase), but this has yet to be assessed or confirmed in vivo or in humans and the clinical significance remains unknown.[166][167] Bicalutamide has been found to be a P-glycoprotein (ABCB1) inhibitor.[168][169][170] Like other first-generation NSAAs and enzalutamide, it has been found to act as a weak non-competitive inhibitor of GABAA receptor-mediated currents in vitro (IC50 = 5.2 μM). However, unlike enzalutamide, bicalutamide has not been found to be associated with seizures or other related adverse central effects, so the clinical relevance of this finding is uncertain.[171][172]
Pharmacokinetics
Though its absolute bioavailability in humans is unknown, bicalutamide is known to be extensively and well-absorbed.[3][4] Its absorption is not affected by food.[4][108] The absorption of bicalutamide is linear at doses up to 150 mg/day and is saturable at doses above this, with no further increases in steady-state levels of bicalutamide occurring at doses above 300 mg/day.[3][21][173][105] Whereas absorption of (R)-bicalutamide is slow, (S)-bicalutamide is much more rapidly absorbed.[3] Steady-state concentrations of the drug are reached after 4 to 12 months of treatment independently of dosage, with a 10- to 20-fold progressive accumulation in levels of (R)-bicalutamide.[21][174][175][124] The long time to steady-state levels is the result of bicalutamide's very long elimination half-life.[124] Although it takes a long time for bicalutamide to reach steady-state concentrations, it appears to have antiandrogenic efficacy equivalent to that of flutamide (which has a much shorter elimination half-life and reaches steady-state levels much faster) by the end of the first day of treatment.[174] Levels of (R)-bicalutamide peak at 31 to 39 hours after a dose.[21][20]
The tissue distribution of bicalutamide is not well-characterized.[176] The amount of bicalutamide in semen that could potentially be transferred to a female partner during sexual intercourse is low and is not thought to be important.[78] Based on animal studies with rats and dogs it was thought that bicalutamide could not cross the blood–brain barrier and hence could not enter the brain.[177][116][178][179] As such, it was initially thought to be a peripherally selective antiandrogen.[177][116] However, subsequent clinical studies found that this was not also the case for humans, indicating species differences; bicalutamide crosses into the human brain and, in accordance, produces effects and side effects consistent with central antiandrogenic action.[3][129][180][181][3][181][182] Bicalutamide is highly plasma protein bound (96.1% for racemic bicalutamide, 99.6% for (R)-bicalutamide) and is bound mainly to albumin, with negliglble binding to SHBG and corticosteroid-binding globulin.[5][3][176][117]
Bicalutamide is metabolized in the liver.[5][108] (R)-Bicalutamide is metabolized slowly and almost exclusively via hydroxylation by CYP3A4 into (R)-hydroxybicalutamide.[108][3][5][183] This metabolite is then glucuronidated by UGT1A9.[108][3][10][7] In contrast to (R)-bicalutamide, (S)-bicalutamide is metabolized rapidly and mainly by glucuronidation (without hydroxylation).[108] None of the metabolites of bicalutamide are known to be active and levels of the metabolites are low in plasma, where unchanged biclautamide predominates.[5][6][3] Due to the stereoselective metabolism of bicalutamide, (R)-bicalutamide has a far longer terminal half-life than (S)-bicalutamide and its levels are about 10- to 20-fold higher in comparison following a single dose and 100-fold higher at steady-state.[21][183][184] (R)-Bicalutamide has a relatively long elimination half-life of 5.8 days with a single dose and 7 to 10 days following repeated administration.[9] The long amount of time that (R)-bicalutamide stays in the body allows for convenient once-daily dosing.[9]
Bicalutamide is eliminated in similar proportions in feces (43%) and urine (34%), while its metabolites are eliminated roughly equally in urine and bile.[5][108][185][186] Bicalutamide is excreted to a substantial extent in unmetabolized form, and both bicalutamide and its metabolites are eliminated mainly as glucuronide conjugates.[114] The glucuronide conjugates of bicalutamide and its metabolites are eliminated from the circulation rapidly, unlike unconjugated bicalutamide.[3][108][187]
The pharmacokinetics of bicalutamide are not affected by consumption of food, a person's age or body weight, renal impairment, or mild-to-moderate hepatic impairment.[3][124] However, steady-state levels of bicalutamide are higher in Japanese individuals than in white people.[3]
Chemistry
Bicalutamide is a racemic mixture consisting of equal proportions of enantiomers (R)-bicalutamide (dextrorotatory) and (S)-bicalutamide (levorotatory).[20] Its systematic name (IUPAC) is (RS)-N-[4-cyano-3-(trifluoromethyl)phenyl]-3-[(4-fluorophenyl)sulfonyl]-2-hydroxy-2-methylpropanamide.[188][189] The compound has a chemical formula of C18H14F4N2O4S, a molecular weight of 430.373 g/mol, and is a fine white to off-white powder.[20][78]
The acid dissociation constant (pKa') of bicalutamide is approximately 12.[78] It is a highly lipophilic compound (log P = 2.92).[3][190] At 37 °C (98.6 °F), or normal human body temperature, bicalutamide is practically insoluble in water (4.6 mg/L), acid (4.6 mg/L at pH 1), and alkali (3.7 mg/L at pH 8).[20][78] In organic solvents, it is slightly soluble in chloroform and absolute ethanol, sparingly soluble in methanol, and freely soluble in acetone and tetrahydrofuran.[20][78]
Bicalutamide is a synthetic and nonsteroidal compound which was derived from flutamide.[191] It can be classified as and has variously been referred to as an anilide (N-phenylamide; or aniline), a diarylpropionamide, and a toluidide.[191][183]
Analogues
First-generation NSAAs including bicalutamide, flutamide, and nilutamide are all synthetic, nonsteroidal anilide derivatives and structural analogues of each other.[191] Bicalutamide is a diarylpropionamide while flutamide is a monoarylpropionamide and nilutamide is a hydantoin.[191] Bicalutamide and flutamide, though not nilutamide, can also be classified as toluidides.[183] All three of the compounds share a common 3-trifluoromethylaniline moiety.[192] Bicalutamide is a modification of flutamide in which a 4-fluorophenylsulfonyl moiety has been added and the nitro group on the original phenyl ring has been replaced with a cyano group.[193] Topilutamide, also known as fluridil, is another NSAA that is closely related structurally to the first-generation NSAAs, but, in contrast to them, is not used in the treatment of prostate cancer and is instead used exclusively as a topical antiandrogen in the treatment of androgenic alopecia.[194][195][196]
The second-generation NSAAs enzalutamide and apalutamide were derived from and are analogues of the first-generation NSAAs,[108][197] while another second-generation NSAA, darolutamide, is said to be structurally distinct and chemically unrelated to the other NSAAs.[198] Enzalutamide is a modification of bicalutamide in which the inter-ring linking chain has been altered and cyclized into a 5,5-dimethyl-4-oxo-2-thioxo imidazolidine moiety. In apalutamide, the 5,5-dimethyl groups of the imidazolidine ring of enzalutamide are cyclized to form an accessory cyclobutane ring and one of its phenyl rings is replaced with a pyridine ring.
The first nonsteroidal androgens (the arylpropionamides) were discovered via structural modification of bicalutamide.[199] Unlike bicalutamide (which is purely antiandrogenic), these compounds show tissue-selective androgenic effects and were classified as selective androgen receptor modulators (SARMs).[199] Lead SARMs of this series included acetothiolutamide, enobosarm (ostarine; S-22), and andarine (acetamidoxolutamide or androxolutamide; S-4).[191][199][200] They are very close to bicalutamide structurally, with the key differences being that the linker sulfone of bicalutamide has been replaced with an ether or thioether group to confer agonism of the AR and the 4-fluoro atom of the pertinent phenyl ring has been substituted with an acetamido or cyano group to eliminate reactivity at the position.[201]
A few radiolabeled derivatives of bicalutamide have been developed for potential use as radiotracers in medical imaging.[202][203] They include [18F]bicalutamide, 4-[76Br]bromobicalutamide, and [76Br]bromo-thiobicalutamide.[202][203] The latter two were found to have substantially increased affinity for the AR relative to that of bicautamide.[202] However, none of these agents have been evaluated in humans.[202][203]
5N-Bicalutamide, or 5-azabicalutamide, is a minor structural modification of bicalutamide which acts as a reversible covalent antagonist of the AR and has approximately 150-fold higher affinity for the AR and about 20-fold greater functional inhibition of the AR relative to bicalutamide.[204][205] It is among the most potent AR antagonists ever to have been developed and is being researched for potential use in the treatment of antiandrogen-resistant prostate cancer.[204]
Synthesis
A number of chemical syntheses of bicalutamide have been published in the literature.[188][206][207][208][209] The procedure of the first published synthesis of bicalutamide can be seen below.[206]
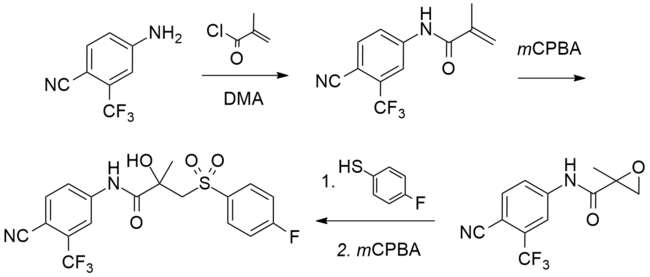
History
Bicalutamide as well as all of the other currently marketed NSAAs were derived from structural modification of flutamide, which itself was originally synthesized as a bacteriostatic agent in 1967 at Schering Plough Corporation and was subsequently and serendipitously found to possess antiandrogenic activity.[210][211][212] Bicalutamide was discovered by Tucker and colleagues at Imperial Chemical Industries in the 1980s and was selected for development from a group of over 1,000 synthesized compounds.[117][213][188] It was first patented in 1982[214] and was first reported in the scientific literature in June 1987.[215]
Bicalutamide was first studied in a phase I clinical trial in 1987[85] and the results of the first phase II clinical trial in prostate cancer were published in 1990.[216] The pharmaceutical division of ICI was split out into an independent company called Zeneca in 1993, and in April and May 1995, Zeneca (now AstraZeneca, after merging with Astra AB in 1999) began pre-approval marketing of bicalutamide for the treatment of prostate cancer in the U.S..[217] It was first launched in the U.K. in May 1995,[218] and was subsequently approved by the U.S. FDA on 4 October 1995, for the treatment of prostate cancer at a dosage of 50 mg/day in combination with a GnRH analogue.[219][220]
Following its introduction for use in combination with a GnRH analogue, bicalutamide was developed as a monotherapy at a dosage of 150 mg/day for the treatment of prostate cancer, and was approved for this indication in Europe, Canada, and a number of other countries in the early 2000s.[21][113][221][222] This application of bicalutamide was also under review by the FDA in the U.S. in 2002,[223] but ultimately was not approved in this country.[71] In Japan, bicalutamide is licensed at a dosage of 80 mg/day alone or in combination with a GnRH analogue for prostate cancer.[68] The unique 80 mg dosage of bicalutamide used in Japan was selected for development in this country on the basis of observed pharmacokinetic differences with bicalutamide in Japanese men.[224]
Subsequent to negative findings of bicalutamide monotherapy for LPC in the EPC trial, approval of bicalutamide for use specifically in the treatment of LPC was withdrawn in a number of countries[225] including the U.K. (in October or November 2003)[226] and several other European countries and Canada (in August 2003).[21][227][228] In addition, the U.S. and Canada explicitly recommended against the use of 150 mg/day bicalutamide for this indication.[229] The drug is effective for, remains approved for, and continues to be used in the treatment of LAPC and mPC, on the other hand.[21]
The patent protection of bicalutamide expired in the U.S. in March 2009 and the drug has subsequently been available as a generic,[230] at greatly reduced cost.[231]
Bicalutamide was the fourth antiandrogen (and the third NSAA) to be introduced for the treatment of prostate cancer, following the SAA CPA in 1973[232] and the NSAAs flutamide in 1983 (1989 in the U.S.)[188][233] and nilutamide in 1989 (1996 in the U.S.).[192][234][235] It has been followed by abiraterone acetate in 2011 and enzalutamide in 2012, and may also be followed by in-development drugs such as apalutamide, darolutamide, and seviteronel.[236]
Society and culture
Names
Bicalutamide is the generic name of the drug in English and French and its INN, USAN, USP,[237] BAN, DCF, AAN,[78] and JAN.[33][238][66][239] It is also referred to as bicalutamidum in Latin, bicalutamida in Spanish and Portuguese, bicalutamid in German, and bikalutamid in Russian and other Slavic languages.[33][66] The "-lutamide" suffix corresponds to that for NSAAs.[240][241] Bicalutamide is also known by its former developmental code name ICI-176,334.[238][66][33]
Bicalutamide is marketed by AstraZeneca in oral tablet form under the brand names Casodex, Cosudex, Calutide, Calumid, and Kalumid in many countries.[33][66][242][243] It is also marketed under the brand names Bicadex, Bical, Bicalox, Bicamide, Bicatlon, Bicusan, Binabic, Bypro, Calutol, and Ormandyl among others in various countries.[33] The drug is sold under a large number of generic trade names such as Apo-Bicalutamide, Bicalutamide Accord, Bicalutamide Actavis, Bicalutamide Bluefish, Bicalutamide Kabi, Bicalutamide Sandoz, and Bicalutamide Teva as well.[33] A combination formulation of bicalutamide and goserelin is marketed by AstraZeneca in Australia and New Zealand under the brand name ZolaCos-CP.[67][72][73][74]
Cost and generics
Bicalutamide is off-patent and available as a generic, and its cost is very low in comparison to a number of other similar medications (from US$10 to US$15.44 for a 30-day supply of once-daily 50 mg tablets).[244][32] Brand name Casodex costs US$556.17 for a 30-day supply of once-daily 50 mg tablets as of 2017[update].[245] Unlike bicalutamide, the newer NSAA enzalutamide is still on-patent, and for this reason, is far more expensive in comparison (US$7,450 for a 30-day supply as of 2015[update]).[246]
The patent protection of all three of the first-generation NSAAs has expired and flutamide and bicalutamide are both available as relatively inexpensive generics.[247][248] Nilutamide, on the other hand, has always been a poor third competitor to flutamide and bicalutamide and, in relation to this fact, has not been developed as a generic and is only available as brand name Nilandron, at least in the U.S.[247][248]
Bicalutamide is far less expensive than GnRH analogues, which, in spite of some having been off-patent many years, have been reported (in 2013) to typically cost US$10,000–$15,000 per year (or about US$1,000 per month) of treatment.[249][250]
Sales and usage
| Year | Sales | Year | Sales | |
|---|---|---|---|---|
| 1995 | ~$15m | 2006 | $1206m | |
| 1996 | $109m | 2007* | $1335m | |
| 1997 | $200m | 2008 | $1258m | |
| 1998 | $245m | 2009 | $844m | |
| 1999 | $340m | 2010 | $579m | |
| 2000 | $433m | 2011 | $550m | |
| 2001 | $569m | 2012 | $454m | |
| 2002 | $644m | 2013 | $376m | |
| 2003 | $854m | 2014 | $320m | |
| 2004 | $1012m | 2015 | $267m | |
| 2005 | $1123m | 2016 | $247m | |
| Total sales: $13.0 billion (as of end 2016) | ||||
| * First generic availability[251] | ||||
| References:[252][253][35][254][255][256][257][258][259] | ||||
Sales of bicalutamide (as Casodex) worldwide peaked at US$1.3 billion in 2007,[256] and it has been described as a "billion-dollar-a-year" drug prior to losing its patent protection starting in 2007.[38][251][194] In 2014, despite the introduction of abiraterone acetate in 2011 and enzalutamide in 2012, bicalutamide was still the most commonly prescribed drug in the treatment of metastatic castration-resistant prostate cancer (mCRPC).[38] Moreover, in spite of being off-patent, bicalutamide was said to still generate a few hundred million dollars in sales per year for AstraZeneca.[38] Total worldwide sales of brand name Casodex were approximately US$13.0 billion as of the end of 2016.[252][253][35][254][255][256][257][258][259]
Between January 2007 and December 2009 (a period of three years), 1,232,143 prescriptions of bicalutamide were dispensed in the U.S., or about 400,000 prescriptions per year.[39] During that time, bicalutamide accounted for about 87.2% of the NSAA market, while flutamide accounted for 10.5% of it and nilutamide for 2.3% of it.[39] Approximately 96% of bicalutamide prescriptions were written for diagnosis codes that clearly indicated neoplasm.[39] About 1,200, or 0.1% of bicalutamide prescriptions were dispensed to pediatric patients (age 0–16).[39]
Regulation
Bicalutamide is a prescription drug.[70] It is not specifically a controlled substance in any country and therefore is not an illegal drug.[11] However, the manufacture, sale, distribution, and possession of prescription drugs are all still subject to legal regulation throughout the world.[260][261][262]
Research
Bicalutamide has been studied in the treatment of benign prostatic hyperplasia (BPH) in a 24-week trial of 15 patients at a dosage of 50 mg/day.[263][264] Prostate volume decreased by 26% in patients taking bicalutamide and urinary irritative symptom scores significantly decreased.[263][264] Conversely, peak urine flow rates and urine pressure flow examinations were not significantly different between bicalutamide and placebo.[263][264] The decrease in prostate volume achieved with bicalutamide was comparable to that observed with the 5α-reductase inhibitor finasteride, which is approved for the treatment of BPH.[265][266] Breast tenderness (93%), gynecomastia (54%), and sexual dysfunction (60%) were all reported as side effects of bicalutamide at the dosage used in the study, although no treatment discontinuations due to adverse effects occurred and sexual functioning was maintained in 75% of patients.[264][85]
A phase II clinical trial of bicalutamide with everolimus in mCRPC has been conducted.[267] Bicalutamide has also been studied in combination with the 5α-reductase inhibitors finasteride and dutasteride in prostate cancer.[268][269][270][271][272][273][274] Bicalutamide has been tested for the treatment of AR-positive ER/PR-negative locally advanced and metastatic breast cancer in a phase II study for this indication.[275][276][277] Enzalutamide is also being investigated for this type of cancer.[278][279] Bicalutamide has also been studied in a phase II clinical trial for ovarian cancer.[280]
Veterinary use
Bicalutamide may be used to treat hyperandrogenism and associated benign prostatic hyperplasia secondary to hyperadrenocorticism (caused by excessive adrenal androgens) in male ferrets.[281][282][283] However, it has not been formally assessed in controlled studies for this purpose.[283][284]
See also
References
- ^ Finkel, Richard; Clark, Michelle Alexia; Cubeddu, Luigi X. (2009). Pharmacology. Lippincott Williams & Wilkins. pp. 481–. ISBN 978-0-7817-7155-9.
{{cite book}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ Sifton DW, PDR Staff (2002). PDR Drug Guide for Mental Health Professionals. Thomson/PDR. ISBN 978-1-56363-457-4.
- ^ a b c d e f g h i j k l m n o p q r s t u v w x y z Cockshott ID (2004). "Bicalutamide: clinical pharmacokinetics and metabolism". Clinical Pharmacokinetics. 43 (13): 855–878. doi:10.2165/00003088-200443130-00003. PMID 15509184.
These data indicate that direct glucuronidation is the main metabolic pathway for the rapidly cleared (S)-bicalutamide, whereas hydroxylation followed by glucuronidation is a major metabolic pathway for the slowly cleared (R)-bicalutamide.
- ^ a b c d e f g h i j Dart, Richard C. (2004). Medical Toxicology. Lippincott Williams & Wilkins. pp. 497, 521. ISBN 978-0-7817-2845-4. Archived from the original on 11 May 2016.
{{cite book}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help); Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ a b c d e f g h i j k l m Lemke, Thomas L.; Williams, David A. (2008). Foye's Principles of Medicinal Chemistry. Lippincott Williams & Wilkins. pp. 121, 1288, 1290. ISBN 978-0-7817-6879-5. Archived from the original on 8 September 2017.
{{cite book}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help); Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ a b Dole EJ, Holdsworth MT (1997). "Nilutamide: an antiandrogen for the treatment of prostate cancer". The Annals of Pharmacotherapy. 31 (1): 65–75. doi:10.1177/106002809703100112. PMID 8997470.
page 67: Currently, information is not available regarding the activity of the major urinary metabolites of bicalutamide, bicalutamide glucuronide, and hydroxybicalutamide glucuronide.
- ^ a b Schellhammer PF (September 2002). "An evaluation of bicalutamide in the treatment of prostate cancer". Expert Opinion on Pharmacotherapy. 3 (9): 1313–28. doi:10.1517/14656566.3.9.1313. PMID 12186624.
The clearance of bicalutamide occurs pre- dominantly by hepatic metabolism and glucuronidation, with excretion of the resulting inactive metabolites in the urine and faces.
- ^ a b c Skidmore-Roth, Linda (17 April 2013). Mosby's 2014 Nursing Drug Reference – Elsevieron VitalSource. Elsevier Health Sciences. pp. 193–194. ISBN 978-0-323-22267-9.
{{cite book}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ a b c Jordan, Virgil Craig; Furr, B. J. A. (5 February 2010). Hormone Therapy in Breast and Prostate Cancer. Springer Science & Business Media. pp. 350–. ISBN 978-1-59259-152-7. Archived from the original on 29 May 2016.
{{cite book}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help); Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ a b Grosse L, Campeau AS, Caron S, Morin FA, Meunier K, Trottier J, Caron P, Verreault M, Barbier O (August 2013). "Enantiomer selective glucuronidation of the non-steroidal pure anti-androgen bicalutamide by human liver and kidney: role of the human UDP-glucuronosyltransferase (UGT)1A9 enzyme". Basic & Clinical Pharmacology & Toxicology. 113 (2): 92–102. doi:10.1111/bcpt.12071. PMC 3815647. PMID 23527766.
- ^ a b c d e f g h i j "Bicalutamide". The American Society of Health-System Pharmacists. Archived from the original on 29 December 2016. Retrieved 8 December 2016.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ Wass, John A.H.; Stewart, Paul M. (28 July 2011). Oxford Textbook of Endocrinology and Diabetes. OUP Oxford. pp. 1625–. ISBN 978-0-19-923529-2. Archived from the original on 11 May 2016.
{{cite book}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help); Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ Shergill, Iqbal; Arya, Manit; Grange, Philippe R.; Mundy, A. R. (2010). Medical Therapy in Urology. Springer Science & Business Media. p. 40. ISBN 9781848827042. Archived from the original on 28 October 2014.
{{cite book}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help); Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ a b c Williams, Hywel; Bigby, Michael; Diepgen, Thomas; Herxheimer, Andrew; Naldi, Luigi; Rzany, Berthold (22 January 2009). Evidence-Based Dermatology. John Wiley & Sons. pp. 529–. ISBN 978-1-4443-0017-8. Archived from the original on 2 May 2016.
{{cite book}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help); Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ a b Gooren, LJ (31 March 2011). "Clinical practice. Care of transsexual persons". The New England Journal of Medicine. 364 (13): 1251–7. doi:10.1056/nejmcp1008161. PMID 21449788.
- ^ a b c Jameson, J. Larry; De Groot, Leslie J. (25 February 2015). Edndocrinology: Adult and Pediatric. Elsevier Health Sciences. pp. 2425–2426, 2139. ISBN 978-0-323-32195-2.
{{cite book}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ a b Yuan J, Desouza R, Westney OL, Wang R (2008). "Insights of priapism mechanism and rationale treatment for recurrent priapism". Asian Journal of Andrology. 10 (1): 88–101. doi:10.1111/j.1745-7262.2008.00314.x. PMID 18087648.
- ^ a b Elliott S, Latini DM, Walker LM, Wassersug R, Robinson JW (2010). "Androgen deprivation therapy for prostate cancer: recommendations to improve patient and partner quality of life". The Journal of Sexual Medicine. 7 (9): 2996–3010. doi:10.1111/j.1743-6109.2010.01902.x. PMID 20626600.
- ^ a b Shapiro, Jerry (12 November 2012). Hair Disorders: Current Concepts in Pathophysiology, Diagnosis and Management, An Issue of Dermatologic Clinics. Elsevier Health Sciences. pp. 187–. ISBN 1-4557-7169-4.
{{cite book}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ a b c d e f g h i j k l m n "Casodex® (bicalutamide) Tablets" (PDF). FDA. Archived from the original (PDF) on 27 February 2017.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ a b c d e f g h i j k l m n o Wellington K, Keam SJ (2006). "Bicalutamide 150mg: a review of its use in the treatment of locally advanced prostate cancer" (PDF). Drugs. 66 (6): 837–50. doi:10.2165/00003495-200666060-00007. PMID 16706554. Archived from the original (PDF) on 28 August 2016.
{{cite journal}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ a b Lee K, Oda Y, Sakaguchi M, Yamamoto A, Nishigori C (May 2016). "Drug-induced photosensitivity to bicalutamide – case report and review of the literature". Photodermatology, Photoimmunology & Photomedicine. 32 (3): 161–4. doi:10.1111/phpp.12230. PMID 26663090.
- ^ Lee K, et al. (2016). "Drug-induced photosensitivity to bicalutamide – case report and review of the literature". Reactions Weekly. 1612 (1): 37–37. doi:10.1007/s40278-016-19790-1.
- ^ a b Singh SM, Gauthier S, Labrie F (February 2000). "Androgen receptor antagonists (antiandrogens): structure-activity relationships". Current Medicinal Chemistry. 7 (2): 211–47. doi:10.2174/0929867003375371. PMID 10637363.
- ^ a b Strauss III, Jerome F.; Barbieri, Robert L. (28 August 2013). Yen & Jaffe's Reproductive Endocrinology: Physiology, Pathophysiology, and Clinical Management. Elsevier Health Sciences. pp. 688–. ISBN 978-1-4557-5972-9.
Bone density improves in men receiving bicalutamide, most likely secondary to the 146% increase in estradiol and the fact that estradiol is the major mediator of bone density in men.
{{cite book}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ a b c Marcus, Robert; Feldman, David; Nelson, Dorothy; Rosen, Clifford J. (8 November 2007). Osteoporosis. Academic Press. pp. 1354–. ISBN 978-0-08-055347-4. Archived from the original on 11 June 2016.
{{cite book}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help); Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ a b c d e Mahler C, Verhelst J, Denis L (May 1998). "Clinical pharmacokinetics of the antiandrogens and their efficacy in prostate cancer". Clinical Pharmacokinetics. 34 (5): 405–17. doi:10.2165/00003088-199834050-00005. PMID 9592622.
- ^ Fischer, Janos; Ganellin, C. Robin (2006). Analogue-based Drug Discovery. John Wiley & Sons. p. 515. ISBN 9783527607495.
{{cite book}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ "WHO Model List of Essential Medicines (19th List)" (PDF). World Health Organization. April 2015. Archived from the original (PDF) on 13 December 2016. Retrieved 8 December 2016.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ Hamilton, Richart (2015). Tarascon Pocket Pharmacopoeia 2015 Deluxe Lab-Coat Edition. Jones & Bartlett Learning. p. 381. ISBN 9781284057560.
- ^ "Bicalutamide". International Drug Price Indicator Guide. Retrieved 8 December 2016.
- ^ a b "NADAC as of 2016-12-07 | Data.Medicaid.gov". Centers for Medicare and Medicaid Services. Archived from the original on 21 December 2016. Retrieved 17 January 2017.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ a b c d e f g h "Bicalutamide – International Drug Names". Drugs.com. Archived from the original on 18 September 2016. Retrieved 13 August 2016.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ a b Akaza H (1999). "[A new anti-androgen, bicalutamide (Casodex), for the treatment of prostate cancer—basic clinical aspects]". Gan to Kagaku Ryoho. Cancer & Chemotherapy (in Japanese). 26 (8): 1201–7. PMID 10431591.
- ^ a b c d "1999 Annual Report and Form 20-F" (PDF). AstraZeneca. Retrieved 1 July 2017.
- ^ Mukherji D, Pezaro CJ, De-Bono JS (February 2012). "MDV3100 for the treatment of prostate cancer". Expert Opinion on Investigational Drugs. 21 (2): 227–33. doi:10.1517/13543784.2012.651125. PMID 22229405.
- ^ Pchejetski, Dmitri; Alshaker, Heba; Stebbing, Justin (2014). "Castrate-resistant prostate cancer: the future of antiandrogens". Trends in Urology & Men's Health. 5 (1): 7–10. doi:10.1002/tre.371.
{{cite journal}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ a b c d Campbell, Todd (22 January 2014). "Slowing Sales for Johnson & Johnson's Zytiga May Be Good News for Medivation". The Motley Fool. Archived from the original on 26 August 2016. Retrieved 20 July 2016.
[...] the most commonly prescribed treatment for metastatic castration resistant prostate cancer: bicalutamide. That was sold as AstraZeneca's billion-dollar-a-year drug Casodex before losing patent protection in 2008. AstraZeneca still generates a few hundred million dollars in sales from Casodex, [...]
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help); Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ a b c d e Chang, Stephen (10 March 2010), Bicalutamide BPCA Drug Use Review in the Pediatric Population (PDF), U.S. Department of Health and Human Service, archived from the original (PDF) on 24 October 2016, retrieved 20 July 2016
{{citation}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help); Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ a b Bagatelle, Carrie; Bremner, William J. (27 May 2003). Androgens in Health and Disease. Springer Science & Business Media. pp. 25–. ISBN 978-/.1-59259-388-0.
{{cite book}}: Check|isbn=value: invalid character (help); Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ Klotz L, Schellhammer P (March 2005). "Combined androgen blockade: the case for bicalutamide". Clinical Prostate Cancer. 3 (4): 215–9. doi:10.3816/cgc.2005.n.002. PMID 15882477.
- ^ Schellhammer PF, Sharifi R, Block NL, Soloway MS, Venner PM, Patterson AL, Sarosdy MF, Vogelzang NJ, Schellenger JJ, Kolvenbag GJ (September 1997). "Clinical benefits of bicalutamide compared with flutamide in combined androgen blockade for patients with advanced prostatic carcinoma: final report of a double-blind, randomized, multicenter trial. Casodex Combination Study Group". Urology. 50 (3): 330–6. doi:10.1016/S0090-4295(97)00279-3. PMID 9301693.
- ^ a b Erem C (2013). "Update on idiopathic hirsutism: diagnosis and treatment". Acta Clinica Belgica. 68 (4): 268–74. doi:10.2143/ACB.3267. PMID 24455796.
- ^ Ascenso A, Marques HC (January 2009). "Acne in the adult". Mini Reviews in Medicinal Chemistry. 9 (1): 1–10. doi:10.2174/138955709787001730. PMID 19149656.
- ^ Kaur S, Verma P, Sangwan A, Dayal S, Jain VK (2016). "Etiopathogenesis and Therapeutic Approach to Adult Onset Acne". Indian Journal of Dermatology. 61 (4): 403–7. doi:10.4103/0019-5154.185703. PMC 4966398. PMID 27512185.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Lotti, Francesco; Maggi, Mario (2015). "Hormonal Treatment for Skin Androgen-Related Disorders". European Handbook of Dermatological Treatments: 1451–1464. doi:10.1007/978-3-662-45139-7_142.
{{cite journal}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ Bourgeois AL, Auriche P, Palmaro A, Montastruc JL, Bagheri H (February 2016). "Risk of hormonotherapy in transgender people: Literature review and data from the French Database of Pharmacovigilance". Annales d'Endocrinologie. 77 (1): 14–21. doi:10.1016/j.ando.2015.12.001. PMID 26830952.
Drugs for cross-gender hormonal replacement therapy used in the male to female (MtoF) transsexual population. [...] Non-steroidal anti-androgens Bicalutamide, flutamide, nilutamide
- ^ Ho CK (December 2011). "Testosterone testing in adult males". The Malaysian Journal of Pathology. 33 (2): 71–81. PMID 22299206.
Anti-androgens such as flutamide, bicalutamide and cyproterone acetate are also used in patients with prostate cancer and sometimes in male-to-female transgender individuals [...]
- ^ a b Wierckx K, Gooren L, T'Sjoen G (May 2014). "Clinical review: Breast development in trans women receiving cross-sex hormones". The Journal of Sexual Medicine. 11 (5): 1240–7. doi:10.1111/jsm.12487. PMID 24618412.
Other agents with anti-androgenic properties used [in the treatment of transgender women] are nonsteroidal androgen receptor blockers, such as flutamide and bicalutamide [...]
- ^ Deutsch, Madeline (17 June 2016), Guidelines for the Primary and Gender-Affirming Care of Transgender and Gender Nonbinary People (PDF) (2nd ed.), University of California, San Francisco: Center of Excellence for Transgender Health, p. 28
{{citation}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ Kliegman, Robert M.; Stanton, Bonita; St. Geme, Joseph; Schor, Nina F (17 April 2015). Nelson Textbook of Pediatrics. Elsevier Health Sciences. pp. 2661–. ISBN 978-0-323-26352-8.
{{cite book}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ Kreher NC, Pescovitz OH, Delameter P, Tiulpakov A, Hochberg Z (September 2006). "Treatment of familial male-limited precocious puberty with bicalutamide and anastrozole". The Journal of Pediatrics. 149 (3): 416–20. doi:10.1016/j.jpeds.2006.04.027. PMID 16939760.
- ^ Reiter EO, Mauras N, McCormick K, Kulshreshtha B, Amrhein J, De Luca F, O'Brien S, Armstrong J, Melezinkova H (October 2010). "Bicalutamide plus anastrozole for the treatment of gonadotropin-independent precocious puberty in boys with testotoxicosis: a phase II, open-label pilot study (BATT)". Journal of Pediatric Endocrinology & Metabolism. 23 (10): 999–1009. doi:10.1515/jpem.2010.161. PMID 21158211.
- ^ Styne, Dennis M. (25 April 2016). "Disorders of Puberty". Pediatric Endocrinology: A Clinical Handbook. Springer. pp. 197–. ISBN 978-3-319-18371-8.
Antiandrogens are used [...] in conditions such as premature Leydig cell and germ cell maturation in boys to decrease androgen effects if the source of androgens cannot be removed.
{{cite book}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ Lenz AM, Shulman D, Eugster EA, Rahhal S, Fuqua JS, Pescovitz OH, Lewis KA (September 2010). "Bicalutamide and third-generation aromatase inhibitors in testotoxicosis". Pediatrics. 126 (3): e728-33. doi:10.1542/peds.2010-0596. PMC 4096839. PMID 20713483.
- ^ Levey HR, Kutlu O, Bivalacqua TJ (2012). "Medical management of ischemic stuttering priapism: a contemporary review of the literature". Asian Journal of Andrology. 14 (1): 156–63. doi:10.1038/aja.2011.114. PMC 3753435. PMID 22057380.
- ^ Broderick GA, Kadioglu A, Bivalacqua TJ, Ghanem H, Nehra A, Shamloul R (2010). "Priapism: pathogenesis, epidemiology, and management". The Journal of Sexual Medicine. 7 (1 Pt 2): 476–500. doi:10.1111/j.1743-6109.2009.01625.x. PMID 20092449.
- ^ Chow K, Payne S (2008). "The pharmacological management of intermittent priapismic states". BJU International. 102 (11): 1515–21. doi:10.1111/j.1464-410X.2008.07951.x. PMID 18793304.
- ^ Dahm P, Rao DS, Donatucci CF (2002). "Antiandrogens in the treatment of priapism". Urology. 59 (1): 138. doi:10.1016/S0090-4295(01)01492-3. PMID 11796309.
- ^ Gooren LJ (2011). "Clinical review: Ethical and medical considerations of androgen deprivation treatment of sex offenders". The Journal of Clinical Endocrinology & Metabolism. 96 (12): 3628–37. doi:10.1210/jc.2011-1540. PMID 21956411.
- ^ Giltay EJ, Gooren LJ (2009). "Potential side effects of androgen deprivation treatment in sex offenders". The Journal of the American Academy of Psychiatry and the Law. 37 (1): 53–8. PMID 19297634.
- ^ Khan O, Mashru A (2016). "The efficacy, safety and ethics of the use of testosterone-suppressing agents in the management of sex offending". Current Opinion in Endocrinology, Diabetes and Obesity. 23 (3): 271–8. doi:10.1097/MED.0000000000000257. PMID 27032060.
- ^ Dangerous Sex Offenders: A Task Force Report of the American Psychiatric Association. American Psychiatric Pub. 1999. pp. 111–. ISBN 978-0-89042-280-9.
- ^ Houts FW, Taller I, Tucker DE, Berlin FS (2011). "Androgen deprivation treatment of sexual behavior". Advances in Psychosomatic Medicine. 31: 149–63. doi:10.1159/000330196. PMID 22005210.
- ^ Rousseau L, Couture M, Dupont A, Labrie F, Couture N (1990). "Effect of combined androgen blockade with an LHRH agonist and flutamide in one severe case of male exhibitionism". The Canadian Journal of Psychiatry. 35 (4): 338–41. doi:10.1177/070674379003500412. PMID 2189544.
- ^ a b c d e Swiss Pharmaceutical Society, ed. (January 2000). Index Nominum 2000: International Drug Directory. Taylor & Francis. pp. 123–. ISBN 978-3-88763-075-1. Archived from the original on 24 April 2016.
{{cite book}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ a b c Sweetman, Sean C. (2011). Martindale: The Complete Drug Reference. Pharmaceutical Press. pp. 750–751. ISBN 978-0-85369-933-0.
{{cite book}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ a b Suzuki H, Kamiya N, Imamoto T, Kawamura K, Yano M, Takano M, Utsumi T, Naya Y, Ichikawa T (October 2008). "Current topics and perspectives relating to hormone therapy for prostate cancer". International Journal of Clinical Oncology. 13 (5): 401–10. doi:10.1007/s10147-008-0830-y. PMID 18946750.
- ^ a b White, Rebecca; Bradnam, Vicky (11 March 2015). Handbook of Drug Administration via Enteral Feeding Tubes (3rd ed.). Pharmaceutical Press. pp. 133–. ISBN 978-0-85711-162-3.
{{cite book}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ a b Morton, Ian; Hall, Judith (2001). The Avery Complete Guide to Medicines. Avery. pp. 105–106. ISBN 978-1-58333-105-7.
{{cite book}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ a b c d e Chabner, Bruce A.; Longo, Dan L. (8 November 2010). Cancer Chemotherapy and Biotherapy: Principles and Practice. Lippincott Williams & Wilkins. pp. 679–680. ISBN 978-1-60547-431-1.
From a structural standpoint, antiandrogens are classified as steroidal, including cyproterone [acetate] (Androcur) and megestrol [acetate], or nonsteroidal, including flutamide (Eulexin, others), bicalutamide (Casodex), and nilutamide (Nilandron). The steroidal antiandrogens are rarely used.
{{cite book}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ a b "Zolacos CP". Drugs.com. Archived from the original on 20 September 2016.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ a b "Zolacos CP" (PDF). MIMS/myDr. April 2007. Archived from the original (PDF) on 17 September 2016.
{{cite web}}: Unknown parameter|dead-url=ignored (|url-status=suggested) (help) - ^ a b "ZOLACOS CP" (PDF). New Zealand Data Sheet. 25 July 2016. Archived from the original (PDF) on 19 September 2016.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ Skeel, Roland T.; Khleif, Samir N. (2011). Handbook of Cancer Chemotherapy. Lippincott Williams & Wilkins. pp. 724–. Archived from the original on 29 May 2016.
{{cite book}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help); Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ Mosby's GenRx: A Comprehensive Reference for Generic and Brand Prescription Drugs. Mosby. 2001. pp. 289–290. ISBN 978-0-323-00629-3.
- ^ PDR, Thomson (2004). Physicians' Desk Reference. Thomson PDR. ISBN 978-1-56363-471-0.
{{cite book}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ a b c d e f g h "COSUDEX® (bicalutamide) 150 mg tablets". TGA. Archived from the original on 14 September 2016.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ a b Cite error: The named reference
IswaranImai1997was invoked but never defined (see the help page). - ^ Cite error: The named reference
Smith2013was invoked but never defined (see the help page). - ^ a b c d Lehne, Richard A. (2013). Pharmacology for Nursing Care. Elsevier Health Sciences. pp. 1297–. ISBN 1-4377-3582-7.
{{cite book}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ a b c Wirth MP, Hakenberg OW, Froehner M (February 2007). "Antiandrogens in the treatment of prostate cancer". European Urology. 51 (2): 306–13, discussion 314. doi:10.1016/j.eururo.2006.08.043. PMID 17007995.
- ^ Higano CS (February 2003). "Side effects of androgen deprivation therapy: monitoring and minimizing toxicity". Urology. 61 (2 Suppl 1): 32–8. doi:10.1016/S0090-4295(02)02397-X. PMID 12667885.
- ^ Higano CS (2012). "Sexuality and intimacy after definitive treatment and subsequent androgen deprivation therapy for prostate cancer". Journal of Clinical Oncology. 30 (30): 3720–5. doi:10.1200/JCO.2012.41.8509. PMID 23008326.
- ^ a b c d e f Kolvenbag GJ, Blackledge GR (January 1996). "Worldwide activity and safety of bicalutamide: a summary review". Urology. 47 (1A Suppl): 70–9, discussion 80–4. doi:10.1016/s0090-4295(96)80012-4. PMID 8560681.
Bicalutamide is a new antiandrogen that offers the convenience of once-daily administration, demonstrated activity in prostate cancer, and an excellent safety profile. Because it is effective and offers better tolerability than flutamide, bicalutamide represents a valid first choice for antiandrogen therapy in combination with castration for the treatment of patients with advanced prostate cancer.
- ^ Resnick, Martin I.; Thompson, Ian Murchie (2000). Advanced Therapy of Prostate Disease. PMPH-USA. pp. 379–. ISBN 978-1-55009-102-1. Archived from the original on 10 June 2016.
{{cite book}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help); Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ Kathryn Korkidakis A, Reid RL (2017). "Testosterone in Women: Measurement and Therapeutic Use". Journal of Obstetrics and Gynaecology Canada. 39 (3): 124–130. doi:10.1016/j.jogc.2017.01.006. PMID 28343552.
- ^ Davis SR, Wahlin-Jacobsen S (2015). "Testosterone in women--the clinical significance". The Lancet Diabetes & Endocrinology. 3 (12): 980–92. doi:10.1016/S2213-8587(15)00284-3. PMID 26358173.
- ^ Jamnicky, Leah; Nam, Robert (5 November 2012). Canadian Guide to Prostate Cancer. John Wiley & Sons. pp. 177–. ISBN 978-1-118-51565-5.
{{cite book}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ Lunglmayr G (August 1995). "Efficacy and tolerability of Casodex in patients with advanced prostate cancer. International Casodex Study Group". Anti-Cancer Drugs. 6 (4): 508–13. doi:10.1097/00001813-199508000-00003. PMID 7579554.
- ^ McLeod DG (1997). "Tolerability of Nonsteroidal Antiandrogens in the Treatment of Advanced Prostate Cancer". The Oncologist. 2 (1): 18–27. PMID 10388026.
- ^ DeAngelis, Lisa M; Posner, Jerome B (12 September 2008). Neurologic Complications of Cancer. Oxford University Press, USA. pp. 479–. ISBN 978-0-19-971055-3. Archived from the original on 7 May 2016.
{{cite book}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help); Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ See WA, Wirth MP, McLeod DG, Iversen P, Klimberg I, Gleason D, et al. (August 2002). "Bicalutamide as immediate therapy either alone or as adjuvant to standard care of patients with localized or locally advanced prostate cancer: first analysis of the early prostate cancer program". The Journal of Urology. 168 (2): 429–35. doi:10.1016/S0022-5347(05)64652-6. PMID 12131282.
- ^ Iversen P, Johansson JE, Lodding P, Lukkarinen O, Lundmo P, Klarskov P, Tammela TL, Tasdemir I, Morris T, Carroll K (November 2004). "Bicalutamide (150 mg) versus placebo as immediate therapy alone or as adjuvant to therapy with curative intent for early nonmetastatic prostate cancer: 5.3-year median followup from the Scandinavian Prostate Cancer Group Study Number 6". The Journal of Urology. 172 (5 Pt 1): 1871–6. doi:10.1097/01.ju.0000139719.99825.54. PMID 15540741.
- ^ Iversen P, Johansson JE, Lodding P, Kylmälä T, Lundmo P, Klarskov P, Tammela TL, Tasdemir I, Morris T, Armstrong J (2006). "Bicalutamide 150 mg in addition to standard care for patients with early non-metastatic prostate cancer: updated results from the Scandinavian Prostate Cancer Period Group-6 Study after a median follow-up period of 7.1 years". Scandinavian Journal of Urology and Nephrology. 40 (6): 441–52. doi:10.1080/00365590601017329. PMID 17130095.
- ^ a b Hussain S, Haidar A, Bloom RE, Zayouna N, Piper MH, Jafri SM (2014). "Bicalutamide-induced hepatotoxicity: A rare adverse effect". The American Journal of Case Reports. 15: 266–70. doi:10.12659/AJCR.890679. PMC 4068966. PMID 24967002.
- ^ Yun GY, Kim SH, Kim SW, Joo JS, Kim JS, Lee ES, Lee BS, Kang SH, Moon HS, Sung JK, Lee HY, Kim KH (April 2016). "Atypical onset of bicalutamide-induced liver injury". World Journal of Gastroenterology. 22 (15): 4062–5. doi:10.3748/wjg.v22.i15.4062. PMC 4823258. PMID 27099451.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Dart, Richard C. (2004). Medical Toxicology. Lippincott Williams & Wilkins. pp. 497–. ISBN 978-0-7817-2845-4. Archived from the original on 11 May 2016.
{{cite book}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help); Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ Masago T, Watanabe T, Nemoto R, Motoda K (December 2011). "Interstitial pneumonitis induced by bicalutamide given for prostate cancer". International Journal of Clinical Oncology. 16 (6): 763–5. doi:10.1007/s10147-011-0239-x. PMID 21537882.
- ^ Aronson, Jeffrey K (4 March 2014). Side Effects of Drugs Annual: A worldwide yearly survey of new data in adverse drug reactions. Newnes. pp. 740–. ISBN 978-0-444-62636-3. Archived from the original on 6 May 2016.
{{cite book}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help); Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ Daba MH, El-Tahir KE, Al-Arifi MN, Gubara OA (June 2004). "Drug-induced pulmonary fibrosis". Saudi Medical Journal. 25 (6): 700–6. PMID 15195196.
- ^ Thole Z, Manso G, Salgueiro E, Revuelta P, Hidalgo A (2004). "Hepatotoxicity induced by antiandrogens: a review of the literature". Urologia Internationalis. 73 (4): 289–95. doi:10.1159/000081585. PMID 15604569.
- ^ Ricci F, Buzzatti G, Rubagotti A, Boccardo F (November 2014). "Safety of antiandrogen therapy for treating prostate cancer". Expert Opinion on Drug Safety. 13 (11): 1483–99. doi:10.1517/14740338.2014.966686. PMID 25270521.
- ^ a b Nurse Practitioner's Drug Handbook. Springhouse Corp. 2000.
- ^ a b c Tyrrell CJ, Iversen P, Tammela T, Anderson J, Björk T, Kaisary AV, Morris T (September 2006). "Tolerability, efficacy and pharmacokinetics of bicalutamide 300 mg, 450 mg or 600 mg as monotherapy for patients with locally advanced or metastatic prostate cancer, compared with castration". BJU International. 98 (3): 563–72. doi:10.1111/j.1464-410X.2006.06275.x. PMID 16771791.
- ^ Henry Winter Griffith (2008). Complete Guide to Prescription & Nonprescription Drugs 2009. HP Books. pp. 62–. ISBN 978-0-399-53463-8.
Overdose unlikely to threaten life [with NSAAs].
- ^ Genrx (1999). 1999 Mosby's GenRx. Mosby. ISBN 978-0-323-00625-5.
A 79-year-old man attempted suicide by ingesting 13g of nilutamide (i.e., 43 times the maximum recommended dose). Despite immediate gastric lavage and oral administration of activated charcoal, plasma nilutamide levels peaked at 6 times the normal range 2 hours after ingestion. There were no clinical signs or symptoms or changes in parameters such as transaminases or chest x-ray. Maintenance treatment (150 mg/day) was resumed 30 days later.
- ^ a b c d e f g h i Weber, Georg F. (22 July 2015). Molecular Therapies of Cancer. Springer. pp. 318–. ISBN 978-3-319-13278-5.
Compared to flutamide and nilutamide, bicalutamide has a 2-fold increased affinity for the Androgen Receptor, a longer half-life, and substantially reduced toxicities. Based on a more favorable safety profile relative to flutamide, bicalutamide is indicated for use in combination therapy with a Gonadotropin Releasing Hormone analog for the treatment of advanced metastatic prostate carcinoma.
{{cite book}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ Mosby's GenRx: A Comprehensive Reference for Generic and Brand Prescription Drugs. Mosby. 2001. p. 290. ISBN 978-0-323-00629-3.
In vitro studies have shown bicalutamide can displace coumarin anticoagulants, such as warfarin, from their protein-binding sites. It is recommended that if bicalutamide is started in patients already receiving coumarin anticoagulants, prothrombin times should be closely monitored and adjustment of the anticoagulant dose may be necessary.
- ^ Spratto, George; Woods, Adrienne (2 July 2008). 2009 Edition Delmar's Nurse's Drug Handbook. Cengage Learning. pp. 175–. ISBN 1-4283-6106-5.
{{cite book}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ Balaj, K.C. (25 April 2016). Managing Metastatic Prostate Cancer In Your Urological Oncology Practice. Springer. pp. 24–25. ISBN 978-3-319-31341-2. Archived from the original on 8 September 2017.
{{cite book}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help); Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ Masiello D, Cheng S, Bubley GJ, Lu ML, Balk SP (July 2002). "Bicalutamide functions as an androgen receptor antagonist by assembly of a transcriptionally inactive receptor". The Journal of Biological Chemistry. 277 (29): 26321–6. doi:10.1074/jbc.M203310200. PMID 12015321.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ a b c d Denis, Louis (6 December 2012). Antiandrogens in Prostate Cancer: A Key to Tailored Endocrine Treatment. Springer Science & Business Media. pp. 128, 158, 203. ISBN 978-3-642-45745-6.
{{cite book}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ a b c d Schellens, Jan H. M.; McLeod, Howard L.; Newell, David R. (5 May 2005). Cancer Clinical Pharmacology. OUP Oxford. pp. 229–230. ISBN 978-0-19-262966-1. Archived from the original on 10 June 2016.
{{cite book}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help); Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ a b c Becker, Kenneth L. (2001). Principles and Practice of Endocrinology and Metabolism. Lippincott Williams & Wilkins. pp. 1119, 1196, 1208. ISBN 978-0-7817-1750-2. Archived from the original on 8 September 2017.
{{cite book}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help); Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ a b c d Furr BJ, Tucker H (January 1996). "The preclinical development of bicalutamide: pharmacodynamics and mechanism of action". Urology. 47 (1A Suppl): 13–25, discussion 29–32. doi:10.1016/S0090-4295(96)80003-3. PMID 8560673.
- ^ a b c Furr BJ (June 1995). "Casodex: preclinical studies and controversies". Annals of the New York Academy of Sciences. 761 (1): 79–96. doi:10.1111/j.1749-6632.1995.tb31371.x. PMID 7625752.
- ^ Guise TA, Oefelein MG, Eastham JA, Cookson MS, Higano CS, Smith MR (2007). "Estrogenic side effects of androgen deprivation therapy". Reviews in Urology. 9 (4): 163–80. PMC 2213888. PMID 18231613.
- ^ Bulldan A, Malviya VN, Upmanyu N, Konrad L, Scheiner-Bobis G (2017). "Testosterone/bicalutamide antagonism at the predicted extracellular androgen binding site of ZIP9". Biochim. Biophys. Acta. 1864 (12): 2402–2414. doi:10.1016/j.bbamcr.2017.09.012. PMID 28943399.
- ^ Pi M, Parrill AL, Quarles LD (2010). "GPRC6A mediates the non-genomic effects of steroids". J. Biol. Chem. 285 (51): 39953–64. doi:10.1074/jbc.M110.158063. PMC 3000977. PMID 20947496.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Furr BJ (2009). "Research on reproductive medicine in the pharmaceutical industry". Human Fertility. 1 (1): 56–63. doi:10.1080/1464727982000198131. PMID 11844311.
- ^ Cite error: The named reference
FiggChau2010was invoked but never defined (see the help page). - ^ Furr BJ (1996). "The development of Casodex (bicalutamide): preclinical studies". European Urology. 29 Suppl 2: 83–95. PMID 8717469.
- ^ a b c d Denis L, Mahler C (January 1996). "Pharmacodynamics and pharmacokinetics of bicalutamide: defining an active dosing regimen". Urology. 47 (1A Suppl): 26–8, discussion 29–32. doi:10.1016/S0090-4295(96)80004-5. PMID 8560674.
- ^ Cite error: The named reference
pmid15838655was invoked but never defined (see the help page). - ^ Luo S, Martel C, Chen C, Labrie C, Candas B, Singh SM, Labrie F (December 1997). "Daily dosing with flutamide or Casodex exerts maximal antiandrogenic activity". Urology. 50 (6): 913–9. doi:10.1016/S0090-4295(97)00393-2. PMID 9426723.
- ^ Cite error: The named reference
MelmedPolonsky2015was invoked but never defined (see the help page). - ^ Efficacy and Safety of Myo-Inositol Supplementation in the Treatment of Obese Hirsute PCOS Women: Comparative Evaluation with OCP+Bicalutamide Therapy, 2016, doi:10.1210/endo-meetings.2016.RE.5.SUN-153
{{citation}}: Cite uses deprecated parameter|authors=(help) - ^ a b c Cite error: The named reference
IversenMelezinek2001was invoked but never defined (see the help page). - ^ Eri LM, Haug E, Tveter KJ (March 1995). "Effects on the endocrine system of long-term treatment with the non-steroidal anti-androgen Casodex in patients with benign prostatic hyperplasia". British Journal of Urology. 75 (3): 335–40. doi:10.1111/j.1464-410X.1995.tb07345.x. PMID 7537602.
- ^ Wein, Alan J.; Kavoussi, Louis R.; Novick, Andrew C.; Partin, Alan W.; Peters, Craig A. (25 August 2011). Campbell-Walsh Urology: Expert Consult Premium Edition: Enhanced Online Features and Print, 4-Volume Set. Elsevier Health Sciences. pp. 2938–2939, 2946. ISBN 978-1-4160-6911-9. Archived from the original on 5 May 2016.
{{cite book}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help); Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ a b Cite error: The named reference
Diamanti-KandarakisNestler2009was invoked but never defined (see the help page). - ^ a b Carrell, Douglas T.; Peterson, C. Matthew (23 March 2010). Reproductive Endocrinology and Infertility: Integrating Modern Clinical and Laboratory Practice. Springer Science & Business Media. pp. 163–. ISBN 978-1-4419-1436-1. Archived from the original on 4 July 2014.
{{cite book}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help); Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ a b Bouchard, P.; Caraty, A. (15 November 1993). GnRH, GnRH Analogs, Gonadotropins and Gonadal Peptides. CRC Press. pp. 455–456. ISBN 978-0-203-09205-7.
[...] when male levels of androgens are achieved in plasma, their effects on gonadotropin secretion are similar in women and men. [...] administration of flutamide in a group of normally-cycling women produced a clinical improvement of acne and hirsutism without any significant hormonal change. [...] All these data emphasize that physiological levels of androgens have no action on the regulation of gonadotropins in normal women. [...] Androgens do not directly play a role in gonadotropin regulation [in women].
{{cite book}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ Sieber PR (December 2007). "Treatment of bicalutamide-induced breast events". Expert Review of Anticancer Therapy. 7 (12): 1773–9. doi:10.1586/14737140.7.12.1773. PMID 18062751.
- ^ a b Wibowo E, Schellhammer P, Wassersug RJ (January 2011). "Role of estrogen in normal male function: clinical implications for patients with prostate cancer on androgen deprivation therapy". The Journal of Urology. 185 (1): 17–23. doi:10.1016/j.juro.2010.08.094. PMID 21074215.
- ^ a b Motofei IG, Rowland DL, Popa F, Kreienkamp D, Paunica S (July 2011). "Preliminary study with bicalutamide in heterosexual and homosexual patients with prostate cancer: a possible implication of androgens in male homosexual arousal". BJU International. 108 (1): 110–5. doi:10.1111/j.1464-410X.2010.09764.x. PMID 20955264.
- ^ a b Wibowo E, Wassersug RJ (September 2013). "The effect of estrogen on the sexual interest of castrated males: Implications to prostate cancer patients on androgen-deprivation therapy". Critical Reviews in Oncology/Hematology. 87 (3): 224–38. doi:10.1016/j.critrevonc.2013.01.006. PMID 23484454.
- ^ a b King SR (2008). "Emerging roles for neurosteroids in sexual behavior and function". Journal of Andrology. 29 (5): 524–33. doi:10.2164/jandrol.108.005660. PMID 18567641.
- ^ a b Morali G, Oropeza MV, Lemus AE, Perez-Palacios G (September 1994). "Mechanisms regulating male sexual behavior in the rat: role of 3 alpha- and 3 beta-androstanediols". Biology of Reproduction. 51 (3): 562–71. doi:10.1095/biolreprod51.3.562. PMID 7803627.
- ^ Sánchez Montoya EL, Hernández L, Barreto-Estrada JL, Ortiz JG, Jorge JC (November 2010). "The testosterone metabolite 3α-diol enhances female rat sexual motivation when infused in the nucleus accumbens shell". The Journal of Sexual Medicine. 7 (11): 3598–609. doi:10.1111/j.1743-6109.2010.01937.x. PMC 4360968. PMID 20646182.
- ^ a b Chedrese, P. Jorge (13 June 2009). Reproductive Endocrinology: A Molecular Approach. Springer Science & Business Media. pp. 233–. ISBN 978-0-387-88186-7. Archived from the original on 5 September 2017.
{{cite book}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help); Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ Frye CA, Edinger KL, Lephart ED, Walf AA (2010). "3alpha-androstanediol, but not testosterone, attenuates age-related decrements in cognitive, anxiety, and depressive behavior of male rats". Frontiers in Aging Neuroscience. 2: 15. doi:10.3389/fnagi.2010.00015. PMC 2874398. PMID 20552051.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Huang Q, Zhu H, Fischer DF, Zhou JN (June 2008). "An estrogenic effect of 5alpha-androstane-3beta, 17beta-diol on the behavioral response to stress and on CRH regulation". Neuropharmacology. 54 (8): 1233–8. doi:10.1016/j.neuropharm.2008.03.016. PMID 18457850.
- ^ Frye CA, Koonce CJ, Edinger KL, Osborne DM, Walf AA (November 2008). "Androgens with activity at estrogen receptor beta have anxiolytic and cognitive-enhancing effects in male rats and mice". Hormones and Behavior. 54 (5): 726–34. doi:10.1016/j.yhbeh.2008.07.013. PMC 3623974. PMID 18775724.
- ^ a b c Bambury RM, Scher HI (June 2015). "Enzalutamide: Development from bench to bedside". Urologic Oncology. 33 (6): 280–8. doi:10.1016/j.urolonc.2014.12.017. PMID 25797385.
- ^ Bambury RM, Rathkopf DE (August 2016). "Novel and next-generation androgen receptor-directed therapies for prostate cancer: Beyond abiraterone and enzalutamide". Urologic Oncology. 34 (8): 348–55. doi:10.1016/j.urolonc.2015.05.025. PMID 26162486.
- ^ a b Pinto Á (February 2014). "Beyond abiraterone: new hormonal therapies for metastatic castration-resistant prostate cancer". Cancer Biology & Therapy. 15 (2): 149–55. doi:10.4161/cbt.26724. PMC 3928129. PMID 24100689.
- ^ Orentreich, Norman; Durr, Nancy P (1974). "Mammogenesis in Transsexuals". Journal of Investigative Dermatology. 63 (1): 142–6. doi:10.1111/1523-1747.ep12678272. PMID 4365991.
{{cite journal}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ Strauss III, Jerome F.; Barbieri, Robert L. (13 September 2013). Yen and Jaffe's Reproductive Endocrinology. Elsevier Health Sciences. pp. 236–237. ISBN 978-1-4557-2758-2. Archived from the original on 14 January 2017.
{{cite book}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help); Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ Wilson, Christopher B.; Nizet, Victor; Maldonado, Yvonne; Klein, Jerome O.; Remington, Jack S. (2015). Remington and Klein's Infectious Diseases of the Fetus and Newborn Infant. Elsevier Health Sciences. pp. 190–. ISBN 978-0-323-24147-2. Archived from the original on 14 January 2017.
{{cite book}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help); Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ a b Kanhai RC, Hage JJ, van Diest PJ, Bloemena E, Mulder JW (January 2000). "Short-term and long-term histologic effects of castration and estrogen treatment on breast tissue of 14 male-to-female transsexuals in comparison with two chemically castrated men". The American Journal of Surgical Pathology. 24 (1): 74–80. doi:10.1097/00000478-200001000-00009. PMID 10632490.
- ^ a b Lawrence, Anne A. (2006). "Transgender Health Concerns". In Meyer, Ilan H.; Northridge, Mary E. (eds.). The Health of Sexual Minorities Public Health Perspectives on Lesbian, Gay, Bisexual and Transgender Populations. New York: Springer. p. 476. doi:10.1007/978-0-387-31334-4_19. ISBN 978-0-387-28871-0.
{{cite book}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ a b Rosen, Paul Peter (2009). Rosen's Breast Pathology (3 ed.). Philadelphia: Lippincott Williams & Wilkins. pp. 31–. ISBN 978-0-7817-7137-5.
{{cite book}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ a b Morgante E, Gradini R, Realacci M, Sale P, D'Eramo G, Perrone GA, Cardillo MR, Petrangeli E, Russo M, Di Silverio F (March 2001). "Effects of long-term treatment with the anti-androgen bicalutamide on human testis: an ultrastructural and morphometric study". Histopathology. 38 (3): 195–201. doi:10.1046/j.1365-2559.2001.01077.x. PMID 11260298.
- ^ Mulhall, John P. (21 February 2013). Fertility Preservation in Male Cancer Patients. Cambridge University Press. pp. 84–. ISBN 978-1-139-61952-3. Archived from the original on 29 April 2016.
{{cite book}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help); Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ a b Schill, Wolf-Bernhard; Comhaire, Frank H.; Hargreave, Timothy B. (26 August 2006). Andrology for the Clinician. Springer Science & Business Media. pp. 76–. ISBN 978-3-540-33713-3. Archived from the original on 26 May 2016.
{{cite book}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help); Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ a b c d Cite error: The named reference
NieschlagBehre2012was invoked but never defined (see the help page). - ^ a b Cheng, C.Y. (24 October 2009). Molecular Mechanisms in Spermatogenesis. Springer Science & Business Media. pp. 258–. ISBN 978-0-387-09597-4.
{{cite book}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ Johnson, Leonard R. (14 October 2003). Essential Medical Physiology. Academic Press. pp. 731–. ISBN 978-0-08-047270-6. Archived from the original on 15 February 2017.
{{cite book}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help); Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ Cite error: The named reference
JonesReiter2016was invoked but never defined (see the help page). - ^ Payne, Anita H.; Hardy, Matthew P. (28 October 2007). The Leydig Cell in Health and Disease. Springer Science & Business Media. pp. 422–431. ISBN 978-1-59745-453-7.
Estrogens are highly efficient inhibitors of the hypothalamic-hypophyseal-testicular axis (212–214). Aside from their negative feedback action at the level of the hypothalamus and pituitary, direct inhibitory effects on the testis are likely (215,216). [...] The histology of the testes [with estrogen treatment] showed disorganization of the seminiferous tubules, vacuolization and absence of lumen, and compartmentalization of spermatogenesis.
{{cite book}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ Wakelin, Sarah H.; Maibach, Howard I.; Archer, Clive B. (1 June 2002). Systemic Drug Treatment in Dermatology: A Handbook. CRC Press. pp. 32–. ISBN 978-1-84076-013-2. Archived from the original on 25 July 2014.
[Cyproterone acetate] inhibits spermatogenesis and produces reversible infertility (but is not a male contraceptive).
{{cite book}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help); Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ Neumann F (1994). "The antiandrogen cyproterone acetate: discovery, chemistry, basic pharmacology, clinical use and tool in basic research". Exp. Clin. Endocrinol. 102 (1): 1–32. doi:10.1055/s-0029-1211261. PMID 8005205.
Spermatogenesis is also androgen-dependent and is inhibited by CPA, meaning that patients treated with high doses of CPA are sterile (Figure 23). All the effects of CPA are fully reversible.
- ^ Salam, Muhammad A. (2003). Principles & Practice of Urology: A Comprehensive Text. Universal-Publishers. pp. 684–. ISBN 978-1-58112-412-5.
Estrogens act primarily through negative feedback at the hypothalamic-pituitary level to reduce LH secretion and testicular androgen synthesis. [...] Interestingly, if the treatment with estrogens is discontinued after 3 yr. of uninterrupted exposure, serum testosterone may remain at castration levels for up to another 3 yr. This prolonged suppression is thought to result from a direct effect of estrogens on the Leydig cells.
{{cite book}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ Mast N, Lin JB, Pikuleva IA (September 2015). "Marketed Drugs Can Inhibit Cytochrome P450 27A1, a Potential New Target for Breast Cancer Adjuvant Therapy". Molecular Pharmacology. 88 (3): 428–36. doi:10.1124/mol.115.099598. PMC 4551053. PMID 26082378.
- ^ Mast N, Zheng W, Stout CD, Pikuleva IA (February 2013). "Binding of a cyano- and fluoro-containing drug bicalutamide to cytochrome P450 46A1: unusual features and spectral response". The Journal of Biological Chemistry. 288 (7): 4613–24. doi:10.1074/jbc.M112.438754. PMC 3576067. PMID 23288837.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Zhu Y, Liu C, Armstrong C, Lou W, Sandher A, Gao AC (September 2015). "Antiandrogens Inhibit ABCB1 Efflux and ATPase Activity and Reverse Docetaxel Resistance in Advanced Prostate Cancer". Clinical Cancer Research. 21 (18): 4133–42. doi:10.1158/1078-0432.CCR-15-0269. PMC 4573793. PMID 25995342.
- ^ Fenner A (July 2015). "Prostate cancer: Antiandrogens reverse docetaxel resistance via ABCB1 inhibition". Nature Reviews. Urology. 12 (7): 361. doi:10.1038/nrurol.2015.135. PMID 26057062.
- ^ Armstrong CM, Gao AC (2015). "Drug resistance in castration resistant prostate cancer: resistance mechanisms and emerging treatment strategies". American Journal of Clinical and Experimental Urology. 3 (2): 64–76. PMC 4539108. PMID 26309896.
- ^ Foster WR, Car BD, Shi H, Levesque PC, Obermeier MT, Gan J, Arezzo JC, Powlin SS, Dinchuk JE, Balog A, Salvati ME, Attar RM, Gottardis MM (April 2011). "Drug safety is a barrier to the discovery and development of new androgen receptor antagonists". The Prostate. 71 (5): 480–8. doi:10.1002/pros.21263. PMID 20878947.
- ^ Barrish, Joel; Carter, Percy; Cheng, Peter (2010). Accounts in Drug Discovery: Case Studies in Medicinal Chemistry. Royal Society of Chemistry. pp. 127–. ISBN 978-1-84973-126-3.
{{cite book}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ Kolvenbag GJ, Blackledge GR, Gotting-Smith K (January 1998). "Bicalutamide (Casodex) in the treatment of prostate cancer: history of clinical development". The Prostate. 34 (1): 61–72. doi:10.1002/(SICI)1097-0045(19980101)34:1<61::AID-PROS8>3.0.CO;2-N. PMID 9428389.
- ^ a b Blackledge GR (1996). "Clinical progress with a new antiandrogen, Casodex (bicalutamide)". European Urology. 29 Suppl 2: 96–104. PMID 8717470.
Casodex is associated with significantly less gastrointestinal effects (diarrhoea) than the nonsteroidal antiandrogen flutamide (Eulexin, Schering-Plough International). Casodex is not associated with alcohol intolerance, pneumonitis and ocular defects which have been seen with the antiandrogen nilutamide (Anandron, Roussel).
- ^ Cite error: The named reference
Jr.Lawrence2015was invoked but never defined (see the help page). - ^ a b Chu, Edward; DeVita Jr., Vincent T. (28 December 2012). Physicians' Cancer Chemotherapy Drug Manual 2013. Jones & Bartlett Publishers. pp. 51–. ISBN 978-1-284-04039-5.
{{cite book}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ a b Helsen C, Van den Broeck T, Voet A, Prekovic S, Van Poppel H, Joniau S, Claessens F (August 2014). "Androgen receptor antagonists for prostate cancer therapy". Endocrine-Related Cancer. 21 (4): T105-18. doi:10.1530/ERC-13-0545. PMID 24639562.
- ^ Furr BJ (1989). ""Casodex" (ICI 176,334)--a new, pure, peripherally-selective anti-androgen: preclinical studies". Hormone Research. 32 Suppl 1 (1): 69–76. doi:10.1159/000181315. PMID 2533159.
- ^ Furr BJ, Valcaccia B, Curry B, Woodburn JR, Chesterson G, Tucker H (June 1987). "ICI 176,334: a novel non-steroidal, peripherally selective antiandrogen". The Journal of Endocrinology. 113 (3): R7-9. doi:10.1677/joe.0.113R007. PMID 3625091.
- ^ Soloway MS, Schellhammer PF, Smith JA, Chodak GW, Vogelzang NJ, Kennealey GT (December 1995). "Bicalutamide in the treatment of advanced prostatic carcinoma: a phase II noncomparative multicenter trial evaluating safety, efficacy and long-term endocrine effects of monotherapy". The Journal of Urology. 154 (6): 2110–4. doi:10.1016/S0022-5347(01)66709-0. PMID 7500470.
- ^ a b Gao W, Dalton JT (March 2007). "Expanding the therapeutic use of androgens via selective androgen receptor modulators (SARMs)". Drug Discovery Today. 12 (5–6): 241–8. doi:10.1016/j.drudis.2007.01.003. PMC 2072879. PMID 17331889.
- ^ Cite error: The named reference
pmid16896883was invoked but never defined (see the help page). - ^ a b c d Lemke, Thomas L.; Williams, David A. (24 January 2012). Foye's Principles of Medicinal Chemistry. Lippincott Williams & Wilkins. pp. 1372–1373. ISBN 978-1-60913-345-0. Archived from the original on 3 May 2016.
{{cite book}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help); Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ Butler, Sara K.; Govindan, Ramaswamy (25 October 2010). Essential Cancer Pharmacology: The Prescriber's Guide. Lippincott Williams & Wilkins. pp. 49–. ISBN 978-1-60913-704-5.
{{cite book}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ Cite error: The named reference
pmid14748655was invoked but never defined (see the help page). - ^ Cite error: The named reference
pmid22495777was invoked but never defined (see the help page). - ^ Cite error: The named reference
AndersonKnoben2001was invoked but never defined (see the help page). - ^ a b c d McPherson, Edwin M. (22 October 2013). Pharmaceutical Manufacturing Encyclopedia (3rd ed.). William Andrew Publishing. pp. 627, 1695. ISBN 978-0-8155-1856-3. Archived from the original on 9 June 2016.
{{cite book}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help); Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ Komsta, Lukas; Waksmundzka-Hajnos, Monika; Sherma, Joseph (20 December 2013). Thin Layer Chromatography in Drug Analysis. CRC Press. pp. 652–. ISBN 978-1-4665-0715-9.
{{cite book}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ Sancheti PP, Vyas VM, Shah M, Karekar P, Pore YV (2008). "Spectrophotometric estimation of bicalutamide in tablets". Indian Journal of Pharmaceutical Sciences. 70 (6): 810–2. doi:10.4103/0250-474X.49131. PMC 3040883. PMID 21369450.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ a b c d e Mohler ML, Bohl CE, Jones A, Coss CC, Narayanan R, He Y, Hwang DJ, Dalton JT, Miller DD (June 2009). "Nonsteroidal selective androgen receptor modulators (SARMs): dissociating the anabolic and androgenic activities of the androgen receptor for therapeutic benefit". Journal of Medicinal Chemistry. 52 (12): 3597–617. doi:10.1021/jm900280m. PMID 19432422.
[C]linically relevant antiandrogens currently are nonsteroidal anilide derivatives. Antiandrogens used for prostate cancer include the monoarylpropionamide flutamide (1) (a prodrug of hydroxyflutamide (2)),29–31 the hydantoin nilutamide(3),32–34 and the diarylpropionamide bicalutamide (4) (Chart1).35–37
- ^ a b Bégué, Jean-Pierre; Bonnet-Delpon, Daniele (2 June 2008). Bioorganic and Medicinal Chemistry of Fluorine. John Wiley & Sons. pp. 327–. ISBN 978-0-470-28187-1.
{{cite book}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ Ball AL, Kamalian L, Alfirevic A, Lyon JJ, Chadwick AE (July 2016). "Identification of the Additional Mitochondrial Liabilities of 2-Hydroxyflutamide When Compared With its Parent Compound, Flutamide in HepG2 Cells". Toxicological Sciences: kfw126. doi:10.1093/toxsci/kfw126. PMID 27413113.
- ^ a b Hermkens PH, Kamp S, Lusher S, Veeneman GH (July 2006). "Non-steroidal steroid receptor modulators". IDrugs. 9 (7): 488–94. PMID 16821162.
- ^ Avram, Marc R.; Rogers, Nicole E. (30 November 2009). Hair Transplantation. Cambridge University Press. pp. 11–. ISBN 978-1-139-48339-1.
{{cite book}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ Haber, Robert S.; Stough, Dowling Bluford (2006). Hair Transplantation. Elsevier Health Sciences. pp. 6–7. ISBN 978-1-4160-3104-8. Archived from the original on 4 July 2014. Retrieved 28 May 2012.
{{cite book}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help); Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ Kawahara, Takashi; Minamoto, Hiroshi (2014). "Androgen Receptor Antagonists in the Treatment of Prostate Cancer". Clinical Immunology, Endocrine & Metabolic Drugs. 1 (1): 11–19. doi:10.2174/22127070114019990002.
{{cite journal}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ Moilanen AM, Riikonen R, Oksala R, Ravanti L, Aho E, Wohlfahrt G, Nykänen PS, Törmäkangas OP, Palvimo JJ, Kallio PJ (2015). "Discovery of ODM-201, a new-generation androgen receptor inhibitor targeting resistance mechanisms to androgen signaling-directed prostate cancer therapies". Sci Rep. 5: 12007. doi:10.1038/srep12007. PMC 4490394. PMID 26137992.
- ^ a b c Segal S, Narayanan R, Dalton JT (April 2006). "Therapeutic potential of the SARMs: revisiting the androgen receptor for drug discovery". Expert Opinion on Investigational Drugs. 15 (4): 377–87. doi:10.1517/13543784.15.4.377. PMID 16548787.
Structural modifications of bicalutamide led to the discovery of the first nonsteroidal androgens (the aryl propionamides) in 1998. Lead compounds in this class (denoted S1 and S4 in published literature) not only bind to the AR with high affinity (low nanomolar range), but also demonstrate tissue selectivity in animal models [46,50].
- ^ Yin D, Gao W, Kearbey JD, Xu H, Chung K, He Y, Marhefka CA, Veverka KA, Miller DD, Dalton JT (March 2003). "Pharmacodynamics of selective androgen receptor modulators". The Journal of Pharmacology and Experimental Therapeutics. 304 (3): 1334–40. doi:10.1124/jpet.102.040840. PMC 2040238. PMID 12604714.
- ^ Ottow, Eckhardt; Weinmann, Hilmar (8 September 2008). Nuclear Receptors as Drug Targets. John Wiley & Sons. pp. 257–258. ISBN 978-3-527-62330-3.
{{cite book}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ a b c d Parent EE, Dence CS, Jenks C, Sharp TL, Welch MJ, Katzenellenbogen JA (2007). "Synthesis and biological evaluation of [18F]bicalutamide, 4-[76Br]bromobicalutamide, and 4-[76Br]bromo-thiobicalutamide as non-steroidal androgens for prostate cancer imaging". J. Med. Chem. 50 (5): 1028–40. doi:10.1021/jm060847r. PMID 17328524.
- ^ a b c Dierckx, Rudi A.J.O.; Otte, Andreas; de Vries, Erik F.J.; van Waarde, Aren; Luiten, Paul G.M. (15 February 2014). PET and SPECT of Neurobiological Systems. Springer Science & Business Media. pp. 394–. ISBN 978-3-642-42014-6.
{{cite book}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ a b de Jesus Cortez F, Nguyen P, Truillet C, Tian B, Kuchenbecker KM, Evans MJ, Webb P, Jacobson MP, Fletterick RJ, England PM (2017). "Development of 5N-Bicalutamide, a High-Affinity Reversible Covalent Antiandrogen". ACS Chem. Biol. doi:10.1021/acschembio.7b00702. PMID 28981251.
- ^ Pamela, M., Fletterick, R. J., Kuchenbecker, K., & de Jesus Cortez, F. (2016). U.S. Patent Application No. 15/382,942. https://www.google.com/patents/US20170101384
- ^ a b Tucker H, Crook JW, Chesterson GJ (1988). "Nonsteroidal antiandrogens. Synthesis and structure-activity relationships of 3-substituted derivatives of 2-hydroxypropionanilides". Journal of Medicinal Chemistry. 31 (5): 954–9. doi:10.1021/jm00400a011. PMID 3361581.
- ^ James, Kenneth D.; Ekwuribe, Nnochiri N. (2002). "A Two-step Synthesis of the Anti-cancer Drug (R,S)-Bicalutamide". Synthesis. 2002 (7): 850–2. doi:10.1055/s-2002-28508.
{{cite journal}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ US application 2006/0041161, Pizzetti E, Vigano E, Lussana M, Landonio E, "Procedure for the synthesis of bicalutamide", published 23 February 2006
- ^ Chand, M.; Shukla, Anil Kumar (2012). "Novel Synthesis of Bicalutamide Drug Substance and their Impurities using Imidazolium Type of Ionic Liquid". SSRN Electronic Journal. doi:10.2139/ssrn.2160199.
{{cite journal}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ Diamanti-Kandarakis E (September 1999). "Current aspects of antiandrogen therapy in women". Current Pharmaceutical Design. 5 (9): 707–23. PMID 10495361.
Several trials demonstrated complete clearing of acne with flutamide [62,77]. Flutamide used in combination with an [oral contraceptive], at a dose of 500mg/d, flutamide caused a dramatic decrease (80%) in total acne, seborrhea and hair loss score after only 3 months of therapy [53]. When used as a monotherapy in lean and obese PCOS, it significantly improves the signs of hyperandrogenism, hirsutism and particularly acne [48]. [...] flutamide 500mg/d combined with an [oral contraceptive] caused an increase in cosmetically acceptable hair density, in sex of seven women suffering from diffuse androgenetic alopecia [53].
- ^ Denis, Louis J; Griffiths, Keith; Kaisary, Amir V; Murphy, Gerald P (1 March 1999). Textbook of Prostate Cancer: Pathology, Diagnosis and Treatment: Pathology, Diagnosis and Treatment. CRC Press. pp. 55, 279–280. ISBN 978-1-85317-422-3. Archived from the original on 3 June 2016.
{{cite book}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help); Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ Elks, J. (14 November 2014). The Dictionary of Drugs: Chemical Data: Chemical Data, Structures and Bibliographies. Springer. pp. 573–. ISBN 978-1-4757-2085-3. Archived from the original on 15 May 2016.
{{cite book}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help); Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ Cadilla R, Turnbull P (2006). "Selective androgen receptor modulators in drug discovery: medicinal chemistry and therapeutic potential". Curr Top Med Chem. 6 (3): 245–70. doi:10.2174/156802606776173456. PMID 16515480.
- ^ Engel, Jürgen; Kleemann, Axel; Kutscher, Bernhard; Reichert, Dietmar (2009). Pharmaceutical Substances: Syntheses, Patents and Applications of the most relevant APIs (5th ed.). Thieme. pp. 153–154. ISBN 978-3-13-179275-4.
{{cite book}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ Furr BJ, Valcaccia B, Curry B, Woodburn JR, Chesterson G, Tucker H (June 1987). "ICI 176,334: a novel non-steroidal, peripherally selective antiandrogen". The Journal of Endocrinology. 113 (3): R7-9. doi:10.1677/joe.0.113r007. PMID 3625091.
- ^ Newling DW (1990). "The response of advanced prostatic cancer to a new non-steroidal antiandrogen: results of a multicenter open phase II study of Casodex. European/Australian Co-operative Group". European Urology. 18 Suppl 3: 18–21. PMID 2094607.
- ^ The United States Patents Quarterly. Associated Industry Publications. 1997.
- ^ Chaurasiya, Akash; Singh, Ajeet Kumar; Upadhyay, Satish Chandra; Asati, Dinesh; Ahmad, Farhan Jalees; Mukherjee, Rama; Khar, Roop Krishen (2012). "Lipidic Nanocarrier for Oral Bioavailability Enhancement of an Anticancer Agent: Formulation Design and Evaluation". Advanced Science Letters. 11 (1): 43–52. doi:10.1166/asl.2012.2170. ISSN 1936-6612.
{{cite journal}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ Klotz L (May 2006). "Combined androgen blockade: an update". The Urologic Clinics of North America. 33 (2): 161–6, v–vi. doi:10.1016/j.ucl.2005.12.001. PMID 16631454.
- ^ Gohil K (August 2015). "Exciting Therapies Ahead in Prostate Cancer". P & T. 40 (8): 530–1. PMC 4517537. PMID 26236143.
- ^ Kolvenbag GJ, Iversen P, Newling DW (2001). "Antiandrogen monotherapy: a new form of treatment for patients with prostate cancer". Urology. 58 (2 Suppl 1): 16–23. doi:10.1016/s0090-4295(01)01237-7. PMID 11502439.
- ^ Carswell CI, Figgitt DP (2002). "Bicalutamide: in early-stage prostate cancer". Drugs. 62 (17): 2471–79, discussion 2480–1. doi:10.2165/00003495-200262170-00006. PMID 12421104.
- ^ Jasmin, Claude; Capanna, Rodolfo; Coia, Lawrence; Coleman, Robert; Saillant, Gerard (27 September 2005). Textbook of Bone Metastases. John Wiley & Sons. pp. 493–. ISBN 978-0-470-01160-7.
{{cite book}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ Usami M, Akaza H, Arai Y, Hirano Y, Kagawa S, Kanetake H, Naito S, Sumiyoshi Y, Takimoto Y, Terai A, Yoshida H, Ohashi Y (2007). "Bicalutamide 80 mg combined with a luteinizing hormone-releasing hormone agonist (LHRH-A) versus LHRH-A monotherapy in advanced prostate cancer: findings from a phase III randomized, double-blind, multicenter trial in Japanese patients". Prostate Cancer Prostatic Dis. 10 (2): 194–201. doi:10.1038/sj.pcan.4500934. PMID 17199134.
In most countries, bicalutamide is given at a dose of 50 mg when used in combination with an LHRH-A. However, based on pharmacokinetic and pharmacodynamic data, the approved dose of bicalutamide in Japanese men is 80 mg per day.
- ^ Shahani R, Fleshner NE, Zlotta AR (2007). "Pharmacotherapy for prostate cancer: the role of hormonal treatment". Discovery Medicine. 7 (39): 118–24. PMID 18093474.
- ^ Bowsher, Winsor; Carter, Adam (15 April 2008). Challenges in Prostate Cancer. John Wiley & Sons. pp. 146–. ISBN 978-1-4051-7177-9.
{{cite book}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ United Nations (2005). Consolidated List of Products Whose Consumption And/or Sale Have Been Banned, Withdrawn, Severely Restricted Or Not Approved by Governments: Pharmaceuticals. United Nations Publications. pp. 4–. ISBN 978-92-1-130241-7.
- ^ Bono, Aldo V (2004). "Overview of Current Treatment Strategies in Prostate Cancer". European Urology Supplements. 3 (1): 2–7. doi:10.1016/j.eursup.2003.12.002.
The Canadian Health Authorities have withdrawn the approval for antiandrogen monotherapy with bicalutamide for the treatment of localised prostate cancer [5]. Several European countries have also withdrawn approval for bicalutamide for this indication.
{{cite journal}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ Nargund, Vinod H.; Raghavan, Derek; Sandler, Howard M. (17 January 2015). Urological Oncology. Springer. pp. 823–. ISBN 978-0-85729-482-1.
On the other hand, the 150 mg dose of bicalutamide has been associated with some safety concerns, such as a higher death rate when added to active surveillance in the early prostate cancer trialists group study [29], which has led the United States and Canada to recommend against prescribing the 150 mg dose [30].
{{cite book}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ Moul JW (August 2009). "Twenty years of controversy surrounding combined androgen blockade for advanced prostate cancer". Cancer. 115 (15): 3376–8. doi:10.1002/cncr.24393. PMID 19484788.
- ^ Kampel, Lewis J. (20 March 2012). Dx/Rx: Prostate Cancer. Jones & Bartlett Publishers. pp. 178–. ISBN 978-0-7637-9453-8.
{{cite book}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ Tobias, Jeffrey S.; Hochhauser, Daniel (3 October 2014). Cancer and its Management. Wiley. pp. 379–. ISBN 978-1-118-46871-5.
{{cite book}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ Neal, David E. (1994). Tumours in Urology. Springer Science & Business Media. pp. 233–. ISBN 978-1-4471-2086-5. Archived from the original on 27 April 2016.
{{cite book}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help); Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ Regitz-Zagrosek, Vera (2 October 2012). Sex and Gender Differences in Pharmacology. Springer Science & Business Media. pp. 575–. ISBN 978-3-642-30725-6. Archived from the original on 24 June 2016.
{{cite book}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help); Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ Bohl CE, Gao W, Miller DD, Bell CE, Dalton JT (April 2005). "Structural basis for antagonism and resistance of bicalutamide in prostate cancer". Proceedings of the National Academy of Sciences of the United States of America. 102 (17): 6201–6. doi:10.1073/pnas.0500381102. PMC 1087923. PMID 15833816.
- ^ Kolinsky M, de Bono JS (2016). "The Ongoing Challenges of Targeting the Androgen Receptor". European Urology. 69 (5): 841–3. doi:10.1016/j.eururo.2015.10.052. PMID 26585581.
- ^ "Bicalutamide". Kyoto Encyclopedia of Genes and Genomes (KEGG). Archived from the original on 26 November 2016.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ a b Morton, I.K.; Hal, Judith M. (6 December 2012). Concise Dictionary of Pharmacological Agents: Properties and Synonyms. Springer Science & Business Media. pp. 51–. ISBN 978-94-011-4439-1. Archived from the original on 14 May 2016.
{{cite book}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help); Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ Ganellin, C.R.; Triggle, David J. (21 November 1996). Dictionary of Pharmacological Agents. CRC Press. pp. 570–. ISBN 978-0-412-46630-4. Archived from the original on 7 May 2016.
{{cite book}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help); Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ http://www.who.int/medicines/services/inn/StemBook_2013_Final.pdf
- ^ https://druginfo.nlm.nih.gov/drugportal/name/endswith/lutamide
- ^ Ferraro, Marta B.; Orendt, Anita M.; Facelli, Julio C. (19 September 2009). "Parallel Genetic Algorithms for Crystal Structure Prediction: Successes and Failures in Predicting Bicalutamide Polymorphs". In Huang, De-Shuang; Jo, Kang-Hyun; Lee, Hong-Hee; Kang, Hee-Jun; Bevilacqua, Vitoantonio (eds.). Emerging Intelligent Computing Technology and Applications: 5th International Conference on Intelligent Computing, ICIC 2009 Ulsan, South Korea, September 16–19, 2009 Proceedings. Springer. pp. 120–. doi:10.1007/978-3-642-04070-2_14. ISBN 978-3-642-04070-2.
{{cite book}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ Dhas, Namdev L.; Ige, Pradum P.; Kudarha, Ritu R. (2015). "Design, optimization and in-vitro study of folic acid conjugated-chitosan functionalized PLGA nanoparticle for delivery of bicalutamide in prostate cancer". Powder Technology. 283: 234–245. doi:10.1016/j.powtec.2015.04.053.
{{cite journal}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ "Bicalutamide Prices, Coupons and Patient Assistance Programs". Drugs.com. Archived from the original on 6 September 2015. Retrieved 31 August 2015.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ "Casodex Prices, Coupons and Patient Assistance Programs". Drugs.com. Archived from the original on 17 April 2016.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ Ramadan WH, Kabbara WK, Al Basiouni Al Masri HS (2015). "Enzalutamide for patients with metastatic castration-resistant prostate cancer". OncoTargets and Therapy. 8: 871–6. doi:10.2147/OTT.S80488. PMC 4407758. PMID 25945058.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ a b Stuhan, Mary Ann (2 April 2013). Understanding Pharmacology for Pharmacy Technicians. ASHP. pp. 268–. ISBN 978-1-58528-360-6.
{{cite book}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ a b Allan GF, Sui Z (2003). "Therapeutic androgen receptor ligands". Nucl Recept Signal. 1: e009. doi:10.1621/nrs.01009. PMC 1402218. PMID 16604181.
- ^ Emans, S. Jean; Laufer, Marc R. (5 January 2012). Emans, Laufer, Goldstein's Pediatric and Adolescent Gynecology. Lippincott Williams & Wilkins. pp. 365–. ISBN 978-1-4511-5406-1. Archived from the original on 16 May 2016.
Therapy with GnRH analogs is expensive and requires intramuscular injections of depot formulations, the insert of a subcutaneous implant yearly, or, much less commonly, daily subcutaneous injections.
{{cite book}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help); Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ Hillard, Paula J. Adams (29 March 2013). Practical Pediatric and Adolescent Gynecology. John Wiley & Sons. pp. 182–. ISBN 978-1-118-53857-9.
Treatment is expensive, with costs typicall in the range of $10,000–$15,000 per year.
{{cite book}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ a b "Actavis Generic Prostate Cancer Drug Bicalutamide First to Market in UK, Germany, France". Press Release. AstraZeneca, Actavis. 10 July 2008.
- ^ a b "Hormonal Therapies" (PDF). Future Oncology. 2 (2–3): 306. June 1996.
- ^ a b "Zeneca of Britain Posts Strong Drug Profits". The New York Times. 12 March 1997.
- ^ a b "Annual Report and Form 20-F 2001" (PDF). AstraZeneca.
- ^ a b "Annual Report and Form 20-F 2004" (PDF). AstraZeneca.
- ^ a b c "Annual Report and Form 20-F 2007" (PDF). AstraZeneca.
- ^ a b "Annual Report and Form 20-F 2010" (PDF). AstraZeneca.
- ^ a b "Annual Report and Form 20-F 2013" (PDF). AstraZeneca.
- ^ a b "Annual Report and Form 20-F 2016" (PDF). AstraZeneca. Archived from the original (PDF) on 3 April 2017.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ Yagiela, John A.; Dowd, Frank J.; Johnson, Bart; Mariotti, Angelo; Neidle, Enid A. (19 March 2010). Pharmacology and Therapeutics for Dentistry. Elsevier Health Sciences. pp. 851–. ISBN 0-323-07824-9.
{{cite book}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ Hepler, Charles D.; Segal, Richard (25 February 2003). Preventing Medication Errors and Improving Drug Therapy Outcomes: A Management Systems Approach. CRC Press. pp. 136–137. ISBN 978-0-203-01073-0.
{{cite book}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ Dukes, Graham; Dukes, Maurice Nelson Graham; Mildred, Mark; Swartz, Barbara (January 1998). Responsibility for Drug-induced Injury: A Reference Book for Lawyers, the Health Professions and Manufacturers. IOS Press. pp. 241–8. ISBN 978-90-5199-387-5.
{{cite book}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ a b c Becker, Kenneth L. (2001). Principles and Practice of Endocrinology and Metabolism. Lippincott Williams & Wilkins. p. 1209. ISBN 978-0-7817-1750-2. Archived from the original on 28 June 2014.
{{cite book}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help); Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ a b c d Lepor H (1993). "Medical therapy for benign prostatic hyperplasia". Urology. 42 (5): 483–501. doi:10.1016/0090-4295(93)90258-c. PMID 7694413.
The clinically significant adverse events reported in the casodex group included breast tenderness (93%), breast enlargement (54%), and sexual dysfunction (60%). In none of the patients in the placebo group did any of these adverse events develop. None of the subjects discontinued therapy owing to an adverse event.
- ^ Lee M, Sharifi R (1997). "Benign prostatic hyperplasia: diagnosis and treatment guideline". Ann Pharmacother. 31 (4): 481–6. doi:10.1177/106002809703100415. PMID 9101011.
- ^ Kenny B, Ballard S, Blagg J, Fox D (1997). "Pharmacological options in the treatment of benign prostatic hyperplasia". J. Med. Chem. 40 (9): 1293–315. doi:10.1021/jm960697s. PMID 9135028.
- ^ Chow H, Ghosh PM, deVere White R, Evans CP, Dall'Era MA, Yap SA, Li Y, Beckett LA, Lara PN, Pan CX (2016). "A phase 2 clinical trial of everolimus plus bicalutamide for castration-resistant prostate cancer". Cancer. 122 (12): 1897–904. doi:10.1002/cncr.29927. PMID 27019001.
{{cite journal}}: Unknown parameter|laysource=ignored (help); Unknown parameter|laysummary=ignored (help) - ^ Wang LG, Mencher SK, McCarron JP, Ferrari AC (2004). "The biological basis for the use of an anti-androgen and a 5-alpha-reductase inhibitor in the treatment of recurrent prostate cancer: Case report and review". Oncology Reports. 11 (6): 1325–9. PMID 15138573.
- ^ Tay MH, Kaufman DS, Regan MM, Leibowitz SB, George DJ, Febbo PG, Manola J, Smith MR, Kaplan ID, Kantoff PW, Oh WK (2004). "Finasteride and bicalutamide as primary hormonal therapy in patients with advanced adenocarcinoma of the prostate". Annals of Oncology. 15 (6): 974–8. doi:10.1093/annonc/mdh221. PMID 15151957.
- ^ Merrick GS, Butler WM, Wallner KE, Galbreath RW, Allen ZA, Kurko B (2006). "Efficacy of neoadjuvant bicalutamide and dutasteride as a cytoreductive regimen before prostate brachytherapy". Urology. 68 (1): 116–20. doi:10.1016/j.urology.2006.01.061. PMID 16844453.
- ^ Sartor O, Gomella LG, Gagnier P, Melich K, Dann R (2009). "Dutasteride and bicalutamide in patients with hormone-refractory prostate cancer: the Therapy Assessed by Rising PSA (TARP) study rationale and design". The Canadian Journal of Urology. 16 (5): 4806–12. PMID 19796455.
- ^ Chu FM, Sartor O, Gomella L, Rudo T, Somerville MC, Hereghty B, Manyak MJ (2015). "A randomised, double-blind study comparing the addition of bicalutamide with or without dutasteride to GnRH analogue therapy in men with non-metastatic castrate-resistant prostate cancer". European Journal of Cancer. 51 (12): 1555–69. doi:10.1016/j.ejca.2015.04.028. PMID 26048455.
- ^ Gaudet M, Vigneault É, Foster W, Meyer F, Martin AG (2016). "Randomized non-inferiority trial of Bicalutamide and Dutasteride versus LHRH agonists for prostate volume reduction prior to I-125 permanent implant brachytherapy for prostate cancer". Radiotherapy and Oncology : Journal of the European Society for Therapeutic Radiology and Oncology. 118 (1): 141–7. doi:10.1016/j.radonc.2015.11.022. PMID 26702991.
- ^ Dijkstra S, Witjes WP, Roos EP, Vijverberg PL, Geboers AD, Bruins JL, Smits GA, Vergunst H, Mulders PF (2016). "The AVOCAT study: Bicalutamide monotherapy versus combined bicalutamide plus dutasteride therapy for patients with locally advanced or metastatic carcinoma of the prostate-a long-term follow-up comparison and quality of life analysis". SpringerPlus. 5: 653. doi:10.1186/s40064-016-2280-8. PMC 4870485. PMID 27330919.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Translational Breast Cancer Research Consortium (TBCRC) (2012). "Targeting the androgen receptor (AR) in women with AR+ ER-/PR- metastatic breast cancer (MBC)". J Clin Oncol (suppl): abstract 1006. Archived from the original on 10 July 2015.
{{cite journal}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ Clinical trial number NCT00468715 for "Bicalutamide in Treating Patients With Metastatic Breast Cancer" at ClinicalTrials.gov
- ^ Gucalp A, Tolaney S, Isakoff SJ, Ingle JN, Liu MC, Carey LA, Blackwell K, Rugo H, Nabell L, Forero A, Stearns V, Doane AS, Danso M, Moynahan ME, Momen LF, Gonzalez JM, Akhtar A, Giri DD, Patil S, Feigin KN, Hudis CA, Traina TA (October 2013). "Phase II trial of bicalutamide in patients with androgen receptor-positive, estrogen receptor-negative metastatic Breast Cancer". Clinical Cancer Research. 19 (19): 5505–12. doi:10.1158/1078-0432.CCR-12-3327. PMC 4086643. PMID 23965901.
- ^ Caiazza F, Murray A, Madden SF, Synnott NC, Ryan EJ, O'Donovan N, Crown J, Duffy MJ (April 2016). "Preclinical evaluation of the AR inhibitor enzalutamide in triple-negative breast cancer cells". Endocrine-Related Cancer. 23 (4): 323–34. doi:10.1530/ERC-16-0068. PMID 26932782.
- ^ Traina TA, et al. (2015). "Results from a phase 2 study of enzalutamide (ENZA), an androgen receptor (AR) inhibitor, in advanced AR+ triple-negative breast cancer (TNBC)". Journal of Clinical Oncology. 33 (suppl): abstr 1003. Archived from the original on 30 May 2016.
{{cite journal}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ Levine D, Park K, Juretzka M, Esch J, Hensley M, Aghajanian C, Lewin S, Konner J, Derosa F, Spriggs D, Iasonos A, Sabbatini P (December 2007). "A phase II evaluation of goserelin and bicalutamide in patients with ovarian cancer in second or higher complete clinical disease remission". Cancer. 110 (11): 2448–56. doi:10.1002/cncr.23072. PMID 17918264.
- ^ Bonagura, John D.; Twedt, David C. (1 December 2013). Kirk's Current Veterinary Therapy XV. Elsevier Health Sciences. p. 908. ISBN 978-0-323-22762-9.
{{cite book}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ Mitchell, Mark A.; Tully, Thomas N. (2009). Manual of Exotic Pet Practice. Elsevier Health Sciences. p. 363. ISBN 1-4160-0119-0.
{{cite book}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ a b Pilny, Anthony A. (9 February 2014). Endocrinology, An Issue of Veterinary Clinics: Exotic Animal Practice. Elsevier Health Sciences. pp. 16–17. ISBN 978-0-323-26419-8.
In ferrets, 5 mg/kg [of bicalutamide] orally every 24 hours has been used clinically, but no controlled toxicologic or pharmacologic studies have been published at this time.
{{cite book}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ Fox, James G.; Marini, Robert P. (26 March 2014). Biology and Diseases of the Ferret. Wiley. p. 980. ISBN 978-1-118-78273-6.
Other agents have been proposed for medical management of [adrenal-associated endocrinopathy] but have not been studied. Possibly medications include the androgen receptor blockers flutamide and bicalutamide, the anti-androgen finasteride, estrogen-inhibiting anastrozole, and another GnRH analog, goserelin. [...] None of these drugs have been tested in controlled clinical trials in ferrets.
{{cite book}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help)
Further reading
- Tucker H, Crook JW, Chesterson GJ (1988). "Nonsteroidal antiandrogens. Synthesis and structure-activity relationships of 3-substituted derivatives of 2-hydroxypropionanilides". J. Med. Chem. 31 (5): 954–9. doi:10.1021/jm00400a011. PMID 3361581.
- Furr BJ (June 1995). "Casodex: preclinical studies and controversies". Annals of the New York Academy of Sciences. 761 (1): 79–96. doi:10.1111/j.1749-6632.1995.tb31371.x. PMID 7625752.
- Furr BJ, Tucker H (January 1996). "The preclinical development of bicalutamide: pharmacodynamics and mechanism of action". Urology. 47 (1A Suppl): 13–25, discussion 29–32. doi:10.1016/S0090-4295(96)80003-3. PMID 8560673.
- Blackledge GR (1996). "Clinical progress with a new antiandrogen, Casodex (bicalutamide)". European Urology. 29 Suppl 2: 96–104. PMID 8717470.
- Kolvenbag GJ, Blackledge GR (January 1996). "Worldwide activity and safety of bicalutamide: a summary review". Urology. 47 (1A Suppl): 70–9, discussion 80–4. doi:10.1016/s0090-4295(96)80012-4. PMID 8560681.
- Fradet Y (February 2004). "Bicalutamide (Casodex) in the treatment of prostate cancer". Expert Review of Anticancer Therapy. 4 (1): 37–48. doi:10.1586/14737140.4.1.37. PMID 14748655.
- Schellhammer PF, Davis JW (March 2004). "An evaluation of bicalutamide in the treatment of prostate cancer". Clinical Prostate Cancer. 2 (4): 213–9. doi:10.3816/CGC.2004.n.002. PMID 15072604.
- Cockshott ID (2004). "Bicalutamide: clinical pharmacokinetics and metabolism". Clinical Pharmacokinetics. 43 (13): 855–78. doi:10.2165/00003088-200443130-00003. PMID 15509184.
- Wellington K, Keam SJ (2006). "Bicalutamide 150mg: a review of its use in the treatment of locally advanced prostate cancer". Drugs. 66 (6): 837–50. doi:10.2165/00003495-200666060-00007. PMID 16706554.
External links
- 27-Hydroxylase inhibitors
- Alcohols
- Anilides
- Anti-acne preparations
- Antiandrogens
- AstraZeneca
- Hair loss medications
- Hair removal
- Hepatotoxins
- Hormonal antineoplastic drugs
- Nitriles
- Progonadotropins
- Prostate cancer
- Sulfones
- Transgender and medicine
- Trifluoromethyl compounds
- Veterinary drugs
- World Health Organization essential medicines
- RTT









