Ebola
| Ebola | |
|---|---|
| Specialty | Infectious diseases |
Ebola virus disease (EVD) or Ebola hemorrhagic fever (EHF) is the human disease caused by the ebola virus. Symptoms typically start two days to three weeks after contracting the virus, with a fever, throat and muscle pains, and headaches. There is then typically nausea, vomiting, and diarrhea, along with decreased functioning of the liver and kidneys. At this point, some people begin to have problems with bleeding.[1]
The disease is usually acquired when a person comes into contact with the blood or bodily fluids of an infected animal such as a monkey or fruit bat. Fruit bats are believed to carry and spread the virus without being affected by it. Once infection of a human occurs, the disease may be spread from one person to another. Male survivors may be able to transmit the disease via their semen for nearly two months. To make the diagnosis, typically other diseases with similar symptoms such as malaria, cholera and other viral hemorrhagic fever are first excluded. The blood may then be tested for antibodies to the virus, or the viral RNA, or the virus itself, to confirm the diagnosis.[1]
Prevention includes decreasing the spread of the disease from infected monkeys and pigs to humans. This may be done by checking these types of animals for infection and killing and properly disposing of the bodies if the disease is discovered. Properly cooking meat and wearing protective clothing when handling meat may also be helpful, as is wearing protective clothing and washing hands when around a person who has the disease. Samples of bodily fluids and tissues from people with the disease should be handled with special caution.[1]
There is no specific treatment for the virus. Efforts to help persons who are infected include giving them either oral rehydration therapy or intravenous fluids.[1] The disease has a high mortality rate: often between 50% and 90% of those who are infected with the virus.[1][2] The disease was first identified in the Sudan and the Democratic Republic of the Congo. It typically occurs in outbreaks in tropical regions of Sub-Saharan Africa.[1] Between 1976, when it was first identified, and 2014, fewer than 1,000 people a year have been infected.[1][3] The largest outbreak to date is the ongoing 2014 West Africa Ebola outbreak, which is affecting Guinea, Sierra Leone, and Liberia. Efforts are ongoing to develop a vaccine; however, none exists as of 2014.[1]
Signs and symptoms
Manifestation of Ebola begins abruptly with a sudden onset of an influenza-like stage characterized by general malaise, fever with chills, sore throat, severe headache, weakness, joint pain, muscle pain, and chest pain.[4] Respiratory tract involvement is characterized by pharyngitis with sore throat, cough, dyspnea, and hiccups. The central nervous system is affected as judged by the development of severe headaches, agitation, confusion, fatigue, seizures, and sometimes coma.
Cutaneous presentation may include: maculopapular rash, petechiae, purpura, ecchymoses, and hematomas (especially around needle injection sites). In general, development of hemorrhagic symptoms is indicative of a negative prognosis. However, contrary to popular belief, hemorrhage does not lead to hypovolemia and is not the cause of death (total blood loss is low except during labor). Instead, death occurs due to multiple organ dysfunction syndrome (MODS) due to fluid redistribution, hypotension, disseminated intravascular coagulation, and focal tissue necroses.
The average time between contracting the infection and the onset of symptoms is 13 days, but can be as long as 25 days.[5]
Hemorrhage
All people infected show some extent of coagulopathy and impaired circulatory system symptomology.[6] Bleeding from mucous membranes and puncture sites is reported in 40–50% of cases,[7] while maculopapular rashes are evident in approximately 50% of cases.[6] Sources of bleeds include hematemesis, hemoptysis, melena, and aforementioned bleeding from mucous membranes (gastrointestinal tract, nose, vagina and gingiva). However diffuse bleeding (i.e. heavy) is rare; occurrence is usually exclusive to the gastrointestinal tract.[6][8]
Causes
EVD is caused by four of five viruses classified in the genus Ebolavirus, family Filoviridae, order Mononegavirales: Bundibugyo virus (BDBV), Ebola virus (EBOV), Sudan virus (SUDV), Taï Forest virus (TAFV). The fifth virus, Reston virus (RESTV), is thought not disease-causing in humans.
Transmission
EVD is believed to occur after an ebola virus is transmitted to a human index case via contact with an infected animal's bodily fluids. Human-to-human transmission occurs via direct contact with blood or bodily fluids from an infected person (including embalming of an infected dead person) or by contact with contaminated medical equipment, particularly needles and syringes. Medical workers who do not wear protective clothing, such as gloves and surgical masks, may also contract the disease.[9] In the past, explosive nosocomial transmission has occurred in under-equipped African hospitals due to the reuse of needles and lack of implementation of universal precautions.[citation needed] Aerosol transmission has not been observed during natural EVD outbreaks.[citation needed] The potential for widespread EVD epidemics is considered low due to the high case-fatality rate, the rapidity of demise of patients, and the often remote areas where infections occur.[citation needed]
Risk factors

Between 1976 and 1998, in 30,000 mammals, birds, reptiles, amphibians, and arthropods sampled from outbreak regions, no ebolavirus was detected apart from some genetic traces found in six rodents (Mus setulosus and Praomys) and one shrew (Sylvisorex ollula) collected from the Central African Republic.[11][12] Traces of EBOV were detected in the carcasses of gorillas and chimpanzees during outbreaks in 2001 and 2003, which later became the source of human infections. However, the high lethality from infection in these species makes them unlikely as a natural reservoir.[11]
Plants, arthropods, and birds have also been considered as possible reservoirs; however, bats are considered the most likely candidate.[13] Bats were known to reside in the cotton factory in which the index cases for the 1976 and 1979 outbreaks were employed, and they have also been implicated in Marburg virus infections in 1975 and 1980.[11] Of 24 plant species and 19 vertebrate species experimentally inoculated with EBOV, only bats became infected.[14]
The absence of clinical signs in these bats is characteristic of a reservoir species. In a 2002–2003 survey of 1,030 animals including 679 bats from Gabon and the Republic of the Congo, 13 fruit bats were found to contain EBOV RNA fragments.[15] As of 2005, three types of fruit bats (Hypsignathus monstrosus, Epomops franqueti, and Myonycteris torquata) have been identified as being in contact with EBOV. They are now suspected to represent the EBOV reservoir hosts.[16][17]
The existence of integrated genes of filoviruses in some genomes of small rodents, insectivorous bats, shrews, tenrecs, and marsupials indicates a history of infection with filoviruses in these groups as well.[18] However, infectious ebolaviruses have not yet been isolated from any nonhuman animal.
Bats drop partially eaten fruits and pulp, then terrestrial mammals such as gorillas and duikers feed on these fallen fruits. This chain of events forms a possible indirect means of transmission from the natural host to animal populations, which have led to research towards viral shedding in the saliva of bats. Fruit production, animal behavior, and other factors vary at different times and places that may trigger outbreaks among animal populations.[19] Transmission between natural reservoirs and humans are rare, and outbreaks are usually traceable to a single index case where an individual has handled the carcass of gorilla, chimpanzee, or duiker.[20] Fruit bats are also eaten by people in parts of West Africa where they are smoked, grilled or made into a spicy soup.[17][21] The virus then spreads person-to-person, especially within families, hospitals, and during some mortuary rituals where contact among individuals becomes more likely.[22]
The virus has been confirmed as transmitted through body fluids. Transmission through oral exposure and through conjunctiva exposure is likely[23] and has been confirmed in non-human primates.[24] Filoviruses are not naturally transmitted by aerosol. They are, however, highly infectious as breathable 0.8–1.2 micrometre droplets in laboratory conditions;[25] because of this potential route of infection, these viruses have been classified as Category A biological weapons.[26]
All epidemics of Ebola have occurred in sub-optimal hospital conditions, where practices of basic hygiene and sanitation are often either luxuries or unknown to caretakers and where disposable needles and autoclaves are unavailable or too expensive. In modern hospitals with disposable needles and knowledge of basic hygiene and barrier nursing techniques, Ebola has never spread on a large scale. In isolated settings such as a quarantined hospital or a remote village, most victims are infected shortly after the first case of infection is present. The quick onset of symptoms from the time the disease becomes contagious in an individual makes it easy to identify sick individuals and limits an individual's ability to spread the disease by traveling. Because bodies of the deceased are still infectious, some doctors had to take measures to properly dispose of dead bodies in a safe manner despite local traditional burial rituals.[27]
Virology
| Species name | Virus name (abbreviation) |
|---|---|
| Bundibugyo ebolavirus (accepted)[28] | Bundibugyo virus (BDBV; previously BEBOV) |
| Sudan ebolavirus | Sudan virus (SUDV; previously SEBOV) |
| Taï Forest ebolavirus | Taï Forest virus (TAFV; previously CIEBOV) |
| Zaire ebolavirus* | Ebola virus (EBOV; previously ZEBOV) |
| Table legend:
*: The type species accepted: Taxon that has been accepted by the Executive Committee of the ICTV but that has yet to be ratified. |
Genome

Like all mononegaviruses, ebolavirions contain linear nonsegmented, single-strand, non-infectious RNA genomes of negative polarity that possesses inverse-complementary 3' and 5' termini, do not possess a 5' cap, are not polyadenylated, and are not covalently linked to a protein.[29] Ebolavirus genomes are approximately 19 kilobase pairs long and contain seven genes in the order 3'-UTR-NP-VP35-VP40-GP-VP30-VP24-L-5'-UTR.[30] The genomes of the five different ebolaviruses (BDBV, EBOV, RESTV, SUDV, and TAFV) differ in sequence and the number and location of gene overlaps.
Structure
Like all filoviruses, ebolavirions are filamentous particles that may appear in the shape of a shepherd's crook or in the shape of a "U" or a "6", and they may be coiled, toroid, or branched.[30] In general, Ebolavirions are 80 nm in width, but vary somewhat in length. In general, the median particle length of ebolaviruses ranges from 974 to 1,086 nm (in contrast to marburgvirions, whose median particle length was measured at 795–828 nm), but particles as long as 14,000 nm have been detected in tissue culture.[31] Ebolavirions consist of seven structural proteins. At the center is the helical ribonucleocapsid, which consists of the genomic RNA wrapped around a polymer of nucleoproteins (NP). Associated with the ribonucleoprotein is the RNA-dependent RNA polymerase (L) with the polymerase cofactor (VP35) and a transcription activator (VP30). The ribonucleoprotein is embedded in a matrix, formed by the major (VP40) and minor (VP24) matrix proteins. These particles are surrounded by a lipid membrane derived from the host cell membrane. The membrane anchors a glycoprotein (GP1,2) that projects 7 to 10 nm spikes away from its surface. While nearly identical to marburgvirions in structure, ebolavirions are antigenically distinct.
Entry
Niemann–Pick C1 (NPC1) appears essential for Ebola infection. Two independent studies reported in the same issue of Nature showed that Ebola virus cell entry and replication requires the cholesterol transporter protein NPC1.[32][33] When cells from Niemann-Pick disease, type C1 patients (who have a mutated form of NPC1) were exposed to Ebola virus in the laboratory, the cells survived and appeared immune to the virus, further indicating that Ebola relies on NPC1 to enter cells. This might imply that genetic mutations in the NPC1 gene in humans could make some people resistant to one of the deadliest known viruses affecting humans. The same studies described similar results with Ebola's cousin in the filovirus group, Marburg virus, showing that it too needs NPC1 to enter cells.[32][33] Furthermore, NPC1 was shown critical to filovirus entry, because it mediates infection by binding directly to the viral envelope glycoprotein.[33] A later study confirmed these findings, and also showed that the second lysosomal domain of NPC1 mediates this binding.[34]
In one of the original studies, a small molecule was shown to inhibit Ebola virus infection by preventing the virus glycoprotein from binding to NPC1.[33][35] In the other study, mice that were heterozygous for NPC1 were shown to be protected from lethal challenge with mouse adapted Ebola virus.[32] Together, these studies suggest NPC1 may be potential therapeutic target for an Ebola anti-viral drug.
Replication
The ebolavirus life cycle begins with virion attachment to specific cell-surface receptors, followed by fusion of the virion envelope with cellular membranes and the concomitant release of the virus nucleocapsid into the cytosol. The viral RNA polymerase, encoded by the L gene, partially uncoats the nucleocapsid and transcribes the genes into positive-strand mRNAs, which are then translated into structural and nonstructural proteins. Ebolavirus RNA polymerase (L) binds to a single promoter located at the 3' end of the genome. Transcription either terminates after a gene or continues to the next gene downstream. This means that genes close to the 3' end of the genome are transcribed in the greatest abundance, whereas those toward the 5' end are least likely to be transcribed. The gene order is, therefore, a simple but effective form of transcriptional regulation. The most abundant protein produced is the nucleoprotein, whose concentration in the cell determines when L switches from gene transcription to genome replication. Replication results in full-length, positive-strand antigenomes that are, in turn, transcribed into negative-strand virus progeny genome copy. Newly synthesized structural proteins and genomes self-assemble and accumulate near the inside of the cell membrane. Virions bud off from the cell, gaining their envelopes from the cellular membrane they bud from. The mature progeny particles then infect other cells to repeat the cycle.[36]
Pathophysiology
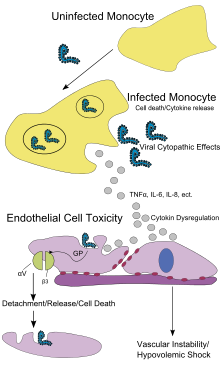
Endothelial cells, mononuclear phagocytes, and hepatocytes are the main targets of infection. After infection, a secreted glycoprotein (sGP) known as the Ebola virus glycoprotein (GP) is synthesized. Ebola replication overwhelms protein synthesis of infected cells and host immune defenses. The GP forms a trimeric complex, which binds the virus to the endothelial cells lining the interior surface of blood vessels. The sGP forms a dimeric protein that interferes with the signaling of neutrophils, a type of white blood cell, which allows the virus to evade the immune system by inhibiting early steps of neutrophil activation. These white blood cells also serve as carriers to transport the virus throughout the entire body to places such as the lymph nodes, liver, lungs, and spleen.[37] The presence of viral particles and cell damage resulting from budding causes the release of cytokines (to be specific, TNF-α, IL-6, IL-8, etc.), which are the signaling molecules for fever and inflammation. The cytopathic effect, from infection in the endothelial cells, results in a loss of vascular integrity. This loss in vascular integrity is furthered with synthesis of GP, which reduces specific integrins responsible for cell adhesion to the inter-cellular structure, and damage to the liver, which leads to coagulopathy.[38]
Diagnosis
EVD cannot be separated from Marburg virus disease based on symptoms. It can also easily be confused with many other diseases common in Equatorial Africa such as other viral hemorrhagic fevers, falciparum malaria, typhoid fever, shigellosis, rickettsial diseases such as typhus, cholera, gram-negative septicemia, borreliosis such as relapsing fever or EHEC enteritis. Other infectious diseases that should be included in the differential diagnosis include the following: leptospirosis, scrub typhus, plague, Q fever, candidiasis, histoplasmosis, trypanosomiasis, visceral leishmaniasis, hemorrhagic smallpox, measles, and fulminant viral hepatitis.[citation needed] Non-infectious diseases that can be confused with EVD are acute promyelocytic leukemia, hemolytic uremic syndrome, snake envenomation, clotting factor deficiencies/platelet disorders, thrombotic thrombocytopenic purpura, hereditary hemorrhagic telangiectasia, Kawasaki disease, and even warfarin intoxication.[39][40][41][42]
The most important method of diagnosis EVD is the medical history, especially travel and occupational history and the person's exposure to wildlife. EVD can be confirmed by isolating ebolaviruses from or by detection of ebolavirus antigen or genomic or subgenomic RNAs in patient blood or serum samples during the acute phase of EVD. Ebolavirus isolation is usually performed by inoculation of grivet kidney epithelial Vero E6 or MA-104 cell cultures or by inoculation of human adrenal carcinoma SW-13 cells, all of which react to infection with characteristic cytopathic effects.[43][44] Filovirions can easily be visualized and identified in cell culture by electron microscopy due to their unique filamentous shapes, but electron microscopy cannot differentiate the various filoviruses alone despite some overall length differences.[31] Immunofluorescence assays are used to confirm ebolavirus presence in cell cultures. During an outbreak, virus isolation and electron microscopy are most often not feasible options. The most common diagnostic methods are therefore RT-PCR[45][46][47][48][49][50][51] in conjunction with antigen-capture ELISA,[52][53][54][55][56] which can be performed in field or mobile hospitals and laboratories. Indirect immunofluorescence assays (IFAs) are not used for diagnosis of EVD in the field anymore.
Classification
The genera Ebolavirus and Marburgvirus were originally classified as the species of the now-obsolete Filovirus genus. In March 1998, the Vertebrate Virus Subcommittee proposed in the International Committee on Taxonomy of Viruses (ICTV) to change the Filovirus genus to the Filoviridae family with two specific genera: Ebola-like viruses and Marburg-like viruses. This proposal was implemented in Washington, DC on April 2001 and in Paris on July 2002. In 2000, another proposal was made in Washington, D.C., to change the "-like viruses" to "-virus" resulting in today's Ebolavirus and Marburgvirus.[57]

Rates of genetic change are 100 times slower than influenza A in humans, but on the same magnitude as those of hepatitis B. Extrapolating backwards using these rates indicates that Ebolavirus and Marburgvirus diverged several thousand years ago.[58] However, paleoviruses (genomic fossils) of filoviruses (Filoviridae) found in mammals indicate that the family itself is at least tens of millions of years old.[18] Fossilized viruses that are closely related to ebolaviruses have been found in the genome of the Chinese hamster.[59]
The five characterised Ebola species are:
- Zaire ebolavirus (EBOV; previously ZEBOV)
- Also known simply as the Zaire virus, ZEBOV has the highest case-fatality rate of the ebolaviruses, up to 90% in some epidemics, with an average case fatality rate of approximately 83% over 27 years. There have been more outbreaks of Zaire ebolavirus than of any other species. The first outbreak occurred on 26 August 1976 in Yambuku.[60] The first recorded case was Mabalo Lokela, a 44‑year-old schoolteacher. The symptoms resembled malaria, and subsequent patients received quinine. Transmission has been attributed to reuse of unsterilized needles and close personal contact.
- Sudan ebolavirus (SUDV; previously SEBOV)
- Like the Zaire virus, SEBOV emerged in 1976; it was at first assumed identical with the Zaire species.[61] SEBOV is believed to have broken out first among cotton factory workers in Nzara, Sudan (now South Sudan), with the first case reported as a worker exposed to a potential natural reservoir. The virus was not found in any of the local animals and insects that were tested in response. The carrier is still unknown. The lack of barrier nursing (or "bedside isolation") facilitated the spread of the disease. The most recent outbreak occurred in May, 2004. Twenty confirmed cases were reported in Yambio County, Sudan (now South Sudan), with five deaths resulting. The average fatality rates for SEBOV were 54% in 1976, 68% in 1979, and 53% in 2000 and 2001.
- Reston ebolavirus (RESTV; previously REBOV)
- Discovered during an outbreak of simian hemorrhagic fever virus (SHFV) in crab-eating macaques from Hazleton Laboratories (now Covance) in 1989. Since the initial outbreak in Reston, Virginia, it has since been found in non-human primates in Pennsylvania, Texas and Siena, Italy. In each case, the affected animals had been imported from a facility in the Philippines,[62] where the virus has also infected pigs.[63] Despite having a Biosafety status of Level‑4 and its apparent pathogenicity in monkeys, REBOV did not cause disease in exposed human laboratory workers.[64]
- Côte d'Ivoire ebolavirus (TAFV; previously CIEBOV)
- Also referred to as Taï Forest ebolavirus and by the English place name, "Ivory Coast", it was first discovered among chimpanzees from the Taï Forest in Côte d'Ivoire, Africa, in 1994. Necropsies showed blood within the heart was brown, no obvious marks were seen on the organs, and one necropsy showed lungs filled with blood. Studies of tissue taken from the chimpanzees showed results similar to human cases during the 1976 Ebola outbreaks in Zaire and Sudan. As more dead chimpanzees were discovered, many tested positive for Ebola using molecular techniques. Experts believed the source of the virus was the meat of infected Western Red Colobus monkeys, upon which the chimpanzees preyed. One of the scientists performing the necropsies on the infected chimpanzees contracted Ebola. She developed symptoms similar to those of dengue fever approximately a week after the necropsy, and was transported to Switzerland for treatment. She was discharged from the hospital after two weeks and had fully recovered six weeks after the infection.[65]
- Bundibugyo ebolavirus (BDBV; previously BEBOV)
- On 24 November 2007, the Uganda Ministry of Health confirmed an outbreak of Ebolavirus in the Bundibugyo District. After confirmation of samples tested by the United States National Reference Laboratories and the CDC, the World Health Organization confirmed the presence of the new species. On 20 February 2008, the Uganda Ministry officially announced the end of the epidemic in Bundibugyo, with the last infected person discharged on 8 January 2008.[66] An epidemiological study conducted by WHO and Uganda Ministry of Health scientists determined there were 116 confirmed and probable cases of the new Ebola species, and that the outbreak had a mortality rate of 34% (39 deaths). In 2012, there was an outbreak of Bundibugyo ebolavirus in a northeastern province of the Democratic Republic of the Congo. There were 15 confirmed cases and 10 fatalities.[67]
Prevention

Ebola viruses are highly infectious as well as contagious. Governments and individuals often quickly respond to quarantine the area while the lack of roads and transportation in many parts of Africa helps to contain the outbreak.[62] Airline crews are trained to spot the symptoms of Ebola in passengers flying from places where the virus is found. Crews are told to quarantine anyone who looks infected.[68]
As an outbreak of ebola progresses, bodily fluids from diarrhea, vomiting, and bleeding represent a hazard. Due to lack of proper equipment and hygienic practices, large-scale epidemics occur mostly in poor, isolated areas without modern hospitals or well-educated medical staff. Many areas where the infectious reservoir exists have just these characteristics. In such environments all that can be done is to immediately cease all needle-sharing or use without adequate sterilization procedures, isolate patients, and observe strict barrier nursing procedures with the use of a medical-rated disposable face mask, gloves, goggles, and a gown at all times, strictly enforced for all medical personnel and visitors.[69] The aim of all of these techniques is to avoid any person’s contact with the blood or secretions of any patient, including those who are deceased.[70]
Vaccines have protected nonhuman primates. Immunization takes six months, which impedes the counter-epidemic use of the vaccines. In 2003, a vaccine using an adenoviral (ADV) vector carrying the Ebola spike protein therefore was tested on crab-eating macaques. The monkeys twenty-eight days later were challenged with the virus and remained resistant.[71] A vaccine based on attenuated recombinant vesicular stomatitis virus (VSV) vector carrying either the Ebola glycoprotein or the Marburg glycoprotein in 2005 protected nonhuman primates,[72] opening clinical trials in humans.[73] The study by October completed the first human trial, over three months giving three vaccinations safely inducing an immune response. Individuals for a year were followed, and, in 2006, a study testing a faster-acting, single-shot vaccine began; this new study was completed in 2008.[74] Trying the vaccine on a strain of Ebola that more resembles the one that infects humans is the next step.[citation needed]
The Food and Drug Administration has approved no candidate vaccines,[75][76][77] the most promising whereof are DNA vaccines[78] or derive from adenoviruses,[71] vesicular stomatitis Indiana virus (VSIV)[79][80][81] or filovirus-like particles (VLPs)[82] because these candidates could protect nonhuman primates from ebolavirus-induced disease. DNA vaccines, adenovirus-based vaccines, and VSIV-based vaccines have entered clinical trials.[73][74][83][84]
Ebolaviruses are not transmitted by aerosol during natural EVD outbreaks. Without an approved vaccine, EVD prevention predominantly involves behavior modification, proper personal protective equipment, and sterilization/disinfection.
On 6 December 2011, the development of a successful vaccine against Ebola for mice was reported. Unlike the predecessors, it can be freeze-dried and thus stored for long periods in wait for an outbreak. The research is reported in Proceedings of National Academy of Sciences.[85]
Endemic zones
The natural maintenance hosts of ebolaviruses are unidentified: primary infection may not necessarily be preventable in nature. Fruit bats are believed the natural hosts (primary source needed, but see e.g., BBC). Thus, to avoid EVD, risk factors such as contact with bats, nonhuman primates, and bush meat should be avoided.
During outbreaks
The most straightforward prevention method during EVD outbreaks is not touching patients, their excretions, and body fluids, or possibly contaminated materials and utensils. Patients should be isolated, and medical staff should be trained and apply strict barrier nursing techniques (disposable face mask, gloves, goggles, and a gown at all times). Traditional burial rituals, especially those requiring embalming of bodies, should be discouraged or modified.[69]
In the laboratory
Ebola viruses are World Health Organization Risk Group 4 Pathogens, requiring Biosafety Level 4-equivalent containment. Laboratory researchers must be properly trained in BSL-4 practices and wear proper personal protective equipment.
Treatment

No ebolavirus-specific treatment exists. Treatment is primarily supportive in nature and includes minimizing invasive procedures, balancing fluids and electrolytes to counter dehydration, administration of anticoagulants early in infection to prevent or control disseminated intravascular coagulation, administration of procoagulants late in infection to control hemorrhaging, maintaining oxygen levels, pain management, and administration of antibiotics or antimycotics to treat secondary infections.[86][87][88]
According to Doctors Without Borders, early treatment may increase the survival chance, since there is no known cure. Treatment focuses on replenishing fluids, maintaining proper blood pressure, replacing lost blood, and treating related infections.[89]
Experimental therapies
Hyperimmune equine immunoglobulin raised against EBOV was used in Russia to treat a laboratory worker who accidentally infected herself with EBOV. The treatment, however, was unsuccessful in saving her life. [90][clarification needed] Experimentally, recombinant vesicular stomatitis Indiana virus (VSIV) expressing the glycoprotein of EBOV or SUDV has been used successfully in nonhuman primate models as post-exposure prophylaxis.[91][92][clarification needed] Such a recombinant post-exposure vaccine was also used to treat a German researcher who accidentally pricked herself with a possibly EBOV-contaminated needle. Treatment might have been successful as she survived. However, actual EBOV infection could never be demonstrated without a doubt.[93] Other promising experimental therapeutic regimens rely on antisense technology. Both small interfering RNAs (siRNAs) and phosphorodiamidate morpholino oligomers (PMOs) targeting the EBOV genome could prevent disease in nonhuman primates.[94][95]
Researchers from the U.S. Army Medical Research Institute of Infectious Diseases also found that FDA-approved estrogen receptor drugs used to treat infertility and breast cancer (clomiphene and toremifene) inhibit the progress of Ebola virus in infected mice.[96] Ninety percent of the mice treated with clomiphene and fifty percent of those treated with toremifene survived the tests.[97] The authors of the study concluded that given their oral availability and history of human use, these drugs would be excellent candidates for repurposing efforts to treat Ebola virus infection in remote geographical locations, either on their own or together with other antiviral drugs.
During an outbreak in the Democratic Republic of the Congo in 1995, seven of eight patients having received blood transfusions from convalescent individuals survived.[98] However, this potential treatment is considered controversial.[61]
Prognosis
The disease has a high mortality rate: often between 50 percent and 90 percent.[1][2] If an infected person survives, recovery may be quick and complete, or prolonged with long term problems, such as inflammation of the testicles, joint pains, muscle pains, skin peeling, or hair loss. Eye symptoms, such as light sensitivity, excess tearing, iritis, iridocyclitis, choroiditis and blindness have also been described. EBOV and SUDV may be able to persist in the semen of some survivors, which could give rise to infections and disease via sexual intercourse.[1]
Epidemiology
Outbreaks of EVD have occurred mainly in Africa.
| Year | Virus | Geographic Location | Human Deaths | Cases | CFR (case-fatality risk) |
|---|---|---|---|---|---|
| 1976 | SUDV | Juba, Maridi, Nzara, and Tembura, Sudan | 151 | 284 | 53% |
| 1976 | EBOV | Yambuku, Zaire | 280 | 318 | 88% |
| 1977 | EBOV | Bonduni, Zaire | 1 | 1 | 100% |
| 1979 | SUDV | Nzara, Sudan | 22 | 34 | 65% |
| 1988 | EBOV | Porton Down, United Kingdom [laboratory accident] | 0 | 1 | 0% |
| 1994 | TAFV | Taï National Park, Côte d'Ivoire | 0 | 1 | 0% |
| 1994–1995 | EBOV | Woleu-Ntem and Ogooué-Ivindo Provinces, Gabon | 32 | 52 | 62% |
| 1995 | EBOV | Kikwit, Zaire | 245 | 317 | 77% |
| 1996 | EBOV | Mayibout 2, Gabon | 21 | 31 | 68% |
| 1996 | EBOV | Sergiyev Posad, Russia [laboratory accident] | 1 | 1 | 100% |
| 1996–1997 | EBOV | Ogooué-Ivindo Province, Gabon; Cuvette-Ouest Department, Republic of the Congo | 46 | 62 | 74% |
| 2000–2001 | SUDV | Gulu, Mbarara, and Masindi Districts, Uganda | 224 | 425 | 53% |
| 2001–2002 | EBOV | Ogooué-Ivindo Province, Gabon; Cuvette-Ouest Department, Republic of the Congo | 97 | 124 | 78% |
| 2002 | EBOV | Ogooué-Ivindo Province, Gabon; Cuvette-Ouest Department, Republic of the Congo | 10 | 11 | 91% |
| 2002–2003 | EBOV | Cuvette-Ouest Department, Republic of the Congo; Ogooué-Ivindo Province, Gabon | 128 | 143 | 90% |
| 2003–2004 | EBOV | Cuvette-Ouest Department, Republic of the Congo | 29 | 35 | 83% |
| 2004 | EBOV | Koltsovo, Russia [laboratory accident] | 1 | 1 | 100% |
| 2004 | SUDV | Yambio County, Sudan | 7 | 17 | 41% |
| 2005 | EBOV | Cuvette-Ouest Department, Republic of the Congo | 9 | 11 | 82% |
| 2007 | EBOV | Kasai Occidental Province, Democratic Republic of the Congo | 186 | 264 | 71% |
| 2007–2008 | BDBV | Bundibugyo District, Uganda | 39 | 116 | 34% |
| 2008–2009 | EBOV | Kasai Occidental Province, Democratic Republic of the Congo | 15 | 32 | 47% |
| 2011 | SUDV | Luweero District, Uganda | 1 | 1 | 100% |
| 2012 | SUDV | Kibaale District, Western Uganda | 17 | 24 | 71% |
| 2012 | BDBV | Orientale Province, Democratic Republic of the Congo | 36 | 77 | 47% |
| 2014 | EBOV | Guinea, Sierra Leone, Liberia, Nigeria. [99] | 730 | 1323 | 55.1% |

While investigating an outbreak of Simian hemorrhagic fever virus (SHFV) in November 1989, an electron microscopist from USAMRIID discovered filoviruses similar in appearance to Ebola in tissue samples taken from crab-eating macaque imported from the Philippines to Hazleton Laboratories Reston, Virginia.[100]
Blood samples were taken from 178 animal handlers during the incident.[101] Of those, six animal handlers eventually seroconverted. When the handlers did not become ill, the CDC concluded that the virus had a very low pathogenicity to humans.[102]
Because of the virus's high mortality, it is a potential agent for biological warfare.[103]
Given the lethal nature of Ebola, and since no approved vaccine or treatment is available, it is classified as a biosafety level 4 agent, as well as a Category A bioterrorism agent by the Centers for Disease Control and Prevention. It has the potential to be weaponized for use in biological warfare.[104] The BBC reports in a study that frequent outbreaks of Ebola may have resulted in the deaths of 5,000 gorillas.[105]
2007 to 2011
As of 30 August 2007, 103 people (100 adults and three children) were infected by a suspected hemorrhagic fever outbreak in the village of Kampungu, Democratic Republic of the Congo. The outbreak started after the funerals of two village chiefs, and 217 people in four villages fell ill. The World Health Organization sent a team to take blood samples for analysis and confirmed that many of the cases are the result of Ebolavirus.[106][107] The Congo's last major Ebola epidemic killed 245 people in 1995 in Kikwit, about 200 miles (320 km) from the source of the August 2007 outbreak.[108]
On 30 November 2007, the Uganda Ministry of Health confirmed an outbreak of Ebola in the Bundibugyo District. After confirmation of samples tested by the United States National Reference Laboratories and the Centers for Disease Control, the World Health Organization confirmed the presence of a new species of Ebolavirus, which is now tentatively named Bundibugyo.[109] The epidemic came to an official end on 20 February 2008. While it lasted, 149 cases of this new strain were reported, and 37 of those led to deaths.
An International Symposium to explore the environment and filovirus, cell system and filovirus interaction, and filovirus treatment and prevention was held at Centre Culturel Français, Libreville, Gabon, during March 2008.[110] The virus appeared in southern Kasai Occidental on 27 November 2008,[111] and blood and stool samples were sent to laboratories in Gabon and South Africa for identification.
On 25 December 2008, a mysterious disease that had killed 11 and infected 21 people in southern Democratic Republic of Congo was identified as the Ebola virus.[112] Doctors Without Borders reported 11 deaths as of 29 December 2008 in the Western Kasai province of the Democratic Republic of Congo, stating that a further 24 cases were being treated. In January 2009, Angola closed down part of its border with DRC to prevent the spread of the outbreak.[113]
On 12 March 2009, an unidentified 45-year-old scientist from Germany accidentally pricked her finger with a needle used to inject Ebola into lab mice. She was given an experimental vaccine never before used on humans. Since the peak period for an outbreak during the 21-day Ebola incubation period has passed as of 2 April 2009, she has been declared healthy and safe. It remains unclear whether or not she was ever actually infected with the virus.[114]
In May 2011, a 12-year-old girl in Uganda died from Ebola (Sudan subspecies). No further cases were recorded.[115]
2012 outbreaks
In July 2012, the Ugandan Health Ministry confirmed 13 deaths due to an outbreak of the Ebola-Sudan variant[116] in the Kibaale District.[117] As of 28 July 2012, 14 out of 20 (70% mortality rate) had died in Kibaale.[118] On July 30, Stephen Byaruhanga, a health official in Kibaale District, said the Ebola outbreak has spread from one remote village to several villages.[119]
The World Health Organization's global and alert response network reported on August 3 that the suspected case count had risen to 53, including 16 deaths. Of these cases, five were confirmed by UVRI as Ebola cases. There have been no confirmed cases outside of Kibaale District except for a patient who was medically evacuated to Kampala District and has since died. WHO and CDC support is on the ground in Uganda supporting the government response. There have been no confirmed cases outside of Uganda.[120] Included among populations confirmed to be affected are prisoners in Kabbale prison. One of the inmates suspected of infection escaped from medical isolation on the same day.[121] Dr. Joaquim Saweka, the WHO representative to Uganda, also reported that the outbreak was then under control and that everyone known to have had contact with a known Ebola patient is now in isolation.[122]
On 8 August 2012, the Ugandan Ministry of Health has recorded 23 probable and confirmed cases, including 16 deaths. Ten cases were confirmed by the Uganda Virus Research Institute as Ebola. 185 people who came into contact with probable and confirmed Ebola cases are being followed up during the incubation period of 21 days.[123]
On 17 August 2012, the Ministry of Health of the Democratic Republic of the Congo reported an outbreak of the Ebola-Bundibugyo variant[124] in the eastern region.[125] By August 21, the WHO reported a total of 15 cases and 10 fatalities.[126] No evidence suggests that this outbreak connects to the Ugandan outbreak.[127] By 13 September 2012, the World Health Organisation revealed that the virus had claimed 32 lives and that the probable cause of the outbreak was tainted bush-meat hunted by local villagers around the towns of Isiro and Viadana.[128]
2014 outbreak
In February 2014, a strain of the Ebola Virus appeared in Guinea. This is the first Ebola virus outbreak registered in the region. As of April 10, 157 suspected and confirmed cases and 101 deaths have been reported in Guinea, 22 suspected cases in Liberia including 14 deaths, 8 suspected cases in Sierra Leone including 6 deaths, and 1 suspected case in Mali.[129][130] Investigations on these are under way.[131][132][133] By late June 2014 the death toll had reached 390 with over 600 cases reported.[134] By 23 July 2014, the World Health Organization had reported 1201 confirmed cases including 672 deaths since the epidemic began in March.[135]
History

Ebola virus first emerged in 1976 in outbreaks of Ebola hemorrhagic fever in Zaire[136] and Sudan.[137] The strain of Ebola that broke out in Zaire has one of the highest case fatality rates of any human virus, roughly 90%.[138]
The name of the disease originates from one of those first recorded outbreaks in 1976 in Yambuku, Democratic Republic of the Congo (then Zaire), which lies on the Ebola River.[136]
The Philippines and the United States had no previous cases of infection, and upon further isolation researchers concluded it was another strain of Ebola, or a new filovirus of Asian origin, which they named Reston ebolavirus (REBOV) after the location of the incident.
Some scientists also believe that the Plague of Athens, which wiped out about a third of its inhabitants during the Peloponnesian War, may have been caused by Ebola. However, these studies are conflicting, and point to other possible diseases such as typhoid.[139]
Other animals
In general, outbreaks of EVD among human populations result from handling infected wild animal carcasses. In general, declines in animal populations precede outbreaks among human populations. Since 2003, such declines have been monitored through surveillance of animal populations with the aim of predicting and preventing EVD outbreaks in humans.[140] Recovered carcasses from gorillas contain multiple Ebola virus strains, which suggest multiple introductions of the virus. Bodies decompose quickly and carcasses are not infectious after three to four days. Contact between gorilla groups is rare, suggesting transmission among gorilla groups is unlikely, and that outbreaks result from transmission between viral reservoir and animal populations.[141]
Outbreaks of EVD may have been responsible for an 88% decline in tracking indices of observed chimpanzee populations in 420 square kilometer Lossi Sanctuary between 2002 and 2003.[141] Transmission among chimpanzees through meat consumption constitutes a significant 5.2 (1.3–21.1 with 95% confidence) relative risk factor, while contact between individuals, such as touching dead bodies and grooming, do not.[142]
Domestic animals
Ebola virus can be transmitted to dogs and pigs.[143] While dogs may be asymptomatic, pigs tend to develop clinical disease.
Recent research
In late 2012, Canadian scientists discovered that the deadliest form of the virus could be transmitted by air between species.[144] They managed to prove that the virus was transmitted from pigs to monkeys without any direct contact between them, leading to fears that airborne transmission could be contributing to the wider spread of the disease in parts of Africa. Evidence was also found that pigs might be one of the reservoir hosts for the virus; the fruit bat has long been considered as the reservoir.[144] A 2013 study isolated antibodies from fruit bats in Bangladesh, against Ebola Zaire and Reston viruses, thus identifying potential virus hosts and signs of the filoviruses in Asia.[145]
See also
References
- ^ a b c d e f g h i j "Ebola virus disease Fact sheet N°103". World Health Organization. March 2014. Retrieved 12 April 2014.
- ^ a b C.M. Fauquet (2005). Virus taxonomy classification and nomenclature of viruses; 8th report of the International Committee on Taxonomy of Viruses. Oxford: Elsevier/Academic Press. p. 648. ISBN 9780080575483.
- ^ "Ebola Viral Disease Outbreak — West Africa, 2014". CDC. June 27, 2014. Retrieved 26 June 2014.
- ^ Nausea is accompanied by abdominal pain, diarrhea, and vomiting
- ^ Eichner M, Dowell SF, Firese N (2011). "Incubation Period of Ebola Hemorrhagic Virus Subtype Zaire OH AND BRETT". Osong Public Health and Research Perspectives. 2 (1): 3–7. doi:10.1016/j.phrp.2011.04.001. PMID 24159443.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ a b c Hoenen T, Groseth A, Falzarano D, Feldmann H (May 2006). "Ebola virus: unravelling pathogenesis to combat a deadly disease". Trends in Molecular Medicine. 12 (5): 206–215. doi:10.1016/j.molmed.2006.03.006. PMID 16616875.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ "Medscape: Ebola Virus, Clinical Presentation". Retrieved 2012-07-30.
- ^ Fisher-Hoch SP, Platt GS, Neild GH, Southee T, Baskerville A, Raymond RT, Lloyd G, Simpson DI (1985). "Pathophysiology of shock and hemorrhage in a fulminating viral infection (Ebola)". J. Infect. Dis. 152 (5): 887–894. doi:10.1093/infdis/152.5.887. PMID 4045253.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Mayo Clinic Staff, Ebola virus and Marburg virus: Causes
- ^ 25 people in Bakaklion, Cameroon killed due to eating of ape
- ^ a b c Pourrut X, Kumulungui B, Wittmann T, Moussavou G, Délicat A, Yaba P, Nkoghe D, Gonzalez JP, Leroy EM (2005). "The natural history of Ebola virus in Africa". Microbes and infection / Institut Pasteur. 7 (7–8): 1005–1014. doi:10.1016/j.micinf.2005.04.006. PMID 16002313.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Morvan JM, Deubel V, Gounon P, Nakouné E, Barrière P, Murri S, Perpète O, Selekon B, Coudrier D, Gautier-Hion A, Colyn M, Volehkov V (1999). "Identification of Ebola virus sequences present as RNA or DNA in organs of terrestrial small mammals of the Central African Republic". Microbes and Infection. 1 (14): 1193–1201. doi:10.1016/S1286-4579(99)00242-7. PMID 10580275.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ "Fruit bats may carry Ebola virus". BBC News. 2005-12-11. Retrieved 2008-02-25.
- ^ Swanepoel R, Leman PA, Burt FJ, Zachariades NA, Braack LE, Ksiazek TG, Rollin PE, Zaki SR, Peters CJ (Oct 1996). "Experimental inoculation of plants and animals with Ebola virus". Emerging Infectious Diseases. 2 (4): 321–325. doi:10.3201/eid0204.960407. ISSN 1080-6040. PMC 2639914. PMID 8969248.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Leroy EM, Kumulungui B, Pourrut X, Rouquet P, Hassanin A, Yaba P, Délicat A, Paweska JT, Gonzalez JP, Swanepoel R (2005). "Fruit bats as reservoirs of Ebola virus". Nature. 438 (7068): 575–576. Bibcode:2005Natur.438..575L. doi:10.1038/438575a. PMID 16319873.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Pourrut X, Délicat A, Rollin PE, Ksiazek TG, Gonzalez JP, Leroy EM (2007). "Spatial and temporal patterns of Zaire ebolavirus antibody prevalence in the possible reservoir bat species". The Journal of infectious diseases. Suppl 2 (s2): S176–S183. doi:10.1086/520541. PMID 17940947.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ a b Starkey, Jerome (5 April 2014) 90 killed as fruit bats spread Ebola virus across West Africa The Times (subscription may be needed), Retrieved 5 April 2014
- ^ a b Taylor DJ, Leach RW, Bruenn J (2010). "Filoviruses are ancient and integrated into mammalian genomes". BMC Evolutionary Biology. 10: 193. doi:10.1186/1471-2148-10-193. PMC 2906475. PMID 20569424.
{{cite journal}}: CS1 maint: multiple names: authors list (link) CS1 maint: unflagged free DOI (link) - ^ Gonzalez JP, Pourrut X, Leroy E (2007). "Ebolavirus and other filoviruses". Current topics in microbiology and immunology. Current Topics in Microbiology and Immunology. 315: 363–387. doi:10.1007/978-3-540-70962-6_15. ISBN 978-3-540-70961-9. PMID 17848072.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Peterson AT, Bauer JT, Mills JN (2004). "Ecologic and Geographic Distribution of Filovirus Disease". Emerging Infectious Diseases. 10 (1): 40–47. doi:10.3201/eid1001.030125. PMC 3322747. PMID 15078595.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ http://www.bbc.co.uk/news/world-africa-26735118
- ^ Questions and Answers about Ebola Hemorrhagic Fever. Centers for Disease Control and Prevention. 2009-03-25. Retrieved 2009-05-31.
- ^ Jaax N, Jahrling P, Geisbert T, Geisbert J, Steele K, McKee K, Nagley D, Johnson E, Jaax G, Peters C (Dec 1995). "Transmission of Ebola virus (Zaire strain) to uninfected control monkeys in a biocontainment laboratory". Lancet. 346 (8991–8992): 1669–1671. doi:10.1016/S0140-6736(95)92841-3. ISSN 0140-6736. PMID 8551825.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Jaax NK, Davis KJ, Geisbert TJ, Vogel P, Jaax GP, Topper M, Jahrling PB (Feb 1996). "Timed appearance of lymphocytic choriomeningitis virus after gastric inoculation of mice". Archives of pathology & laboratory medicine. 120 (2): 140–155. ISSN 0003-9985. PMID 8712894.
{{cite journal}}:|first2=missing|last2=(help);|first3=missing|last3=(help);|first4=missing|last4=(help);|first5=missing|last5=(help);|first6=missing|last6=(help);|first7=missing|last7=(help)CS1 maint: multiple names: authors list (link) - ^ Johnson E, Jaax N, White J, Jahrling P (Aug 1995). "Lethal experimental infections of rhesus monkeys by aerosolized Ebola virus". International journal of experimental pathology. 76 (4): 227–236. ISSN 0959-9673. PMC 1997182. PMID 7547435.
{{cite journal}}:|first2=missing|last2=(help);|first3=missing|last3=(help);|first4=missing|last4=(help)CS1 maint: multiple names: authors list (link) - ^ Leffel EK, Reed DS (2004). "Marburg and Ebola viruses as aerosol threats". Biosecurity and bioterrorism : biodefense strategy, practice, and science. 2 (3): 186–191. doi:10.1089/bsp.2004.2.186. ISSN 1538-7135. PMID 15588056.
{{cite journal}}: Cite has empty unknown parameter:|month=(help) - ^ Harden, Blaine (2001-02-18). "Dr. Matthew's Passion". New York Times Magazine. Retrieved 2008-02-25.
- ^ Kuhn JH, Becker S, Ebihara H, Geisbert TW, Johnson KM, Kawaoka Y, Lipkin WI, Negredo AI, Netesov SV, Nichol ST, Palacios G, Peters CJ, Tenorio A, Volchkov VE, Jahrling PB (2010). "Proposal for a revised taxonomy of the family Filoviridae: Classification, names of taxa and viruses, and virus abbreviations". Archives of Virology. 155 (12): 2083–103. doi:10.1007/s00705-010-0814-x. PMC 3074192. PMID 21046175.
{{cite journal}}: Unknown parameter|displayauthors=ignored (|display-authors=suggested) (help)CS1 maint: multiple names: authors list (link) - ^ Pringle, C. R. (2005). "Order Mononegavirales". In Fauquet, C. M.; Mayo, M. A.; Maniloff, J.; Desselberger, U.; Ball, L. A. (eds.). Virus Taxonomy – Eighth Report of the International Committee on Taxonomy of Viruses. San Diego, US: Elsevier/Academic Press. pp. 609–614. ISBN 0-12-370200-3Template:Inconsistent citations
{{cite book}}: Invalid|ref=harv(help)CS1 maint: postscript (link) - ^ a b Kiley MP, Bowen ET, Eddy GA, Isaäcson M, Johnson KM, McCormick JB, Murphy FA, Pattyn SR, Peters D, Prozesky OW, Regnery RL, Simpson DI, Slenczka W, Sureau P, van der Groen G, Webb PA, Wulff H (1982). "Filoviridae: A taxonomic home for Marburg and Ebola viruses?". Intervirology. 18 (1–2): 24–32. doi:10.1159/000149300. PMID 7118520.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ a b Geisbert TW, Jahrling PB (1995). "Differentiation of filoviruses by electron microscopy". Virus research. 39 (2–3): 129–150. PMID 8837880.
- ^ a b c Carette JE, Raaben M, Wong AC, Herbert AS, Obernosterer G, Mulherkar N, Kuehne AI, Kranzusch PJ, Griffin AM, Ruthel G, Dal Cin P, Dye JM, Whelan SP, Chandran K, Brummelkamp TR (September 2011). "Ebola virus entry requires the cholesterol transporter Niemann-Pick C1". Nature. 477 (7364): 340–3. Bibcode:2011Natur.477..340C. doi:10.1038/nature10348. PMC 3175325. PMID 21866103.
{{cite journal}}: Unknown parameter|laysource=ignored (help); Unknown parameter|laysummary=ignored (help)CS1 maint: multiple names: authors list (link) - ^ a b c d Côté M, Misasi J, Ren T, Bruchez A, Lee K, Filone CM, Hensley L, Li Q, Ory D, Chandran K, Cunningham J (September 2011). "Small molecule inhibitors reveal Niemann-Pick C1 is essential for Ebola virus infection". Nature. 477 (7364): 344–8. Bibcode:2011Natur.477..344C. doi:10.1038/nature10380. PMC 3230319. PMID 21866101.
{{cite journal}}: Unknown parameter|laysource=ignored (help); Unknown parameter|laysummary=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Miller EH, Obernosterer G, Raaben M, Herbert AS, Deffieu MS, Krishnan A, Ndungo E, Sandesara RG, Carette JE, Kuehne AI, Ruthel G, Pfeffer SR, Dye JM, Whelan SP, Brummelkamp TR, Chandran K (March 2012). "Ebola virus entry requires the host-programmed recognition of an intracellular receptor". The EMBO Journal. 31 (8): 1947–60. doi:10.1038/emboj.2012.53. PMC 3343336. PMID 22395071.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Flemming A (October 2011). "Achilles heel of Ebola viral entry". Nature Reviews Drug Discovery. 10 (10): 731. doi:10.1038/nrd3568. PMID 21959282.
- ^ Feldmann, H.; Geisbert, T. W.; Jahrling, P. B.; Klenk, H.-D.; Netesov, S. V.; Peters, C. J.; Sanchez, A.; Swanepoel, R.; Volchkov, V. E. (2005). "Family Filoviridae". In Fauquet, C. M.; Mayo, M. A.; Maniloff, J.; Desselberger, U.; Ball, L. A. (eds.). Virus Taxonomy – Eighth Report of the International Committee on Taxonomy of Viruses. San Diego, US: Elsevier/Academic Press. pp. 645–653. ISBN 0-12-370200-3Template:Inconsistent citations
{{cite book}}: Invalid|display-authors=9(help); Invalid|ref=harv(help)CS1 maint: postscript (link) - ^ Smith, Tara (2005). Ebola (Deadly Diseases and Epidemics). Chelsea House Publications. ISBN 0-7910-8505-8.
- ^ Sullivan N, Yang ZY, Nabel GJ (2003). "Ebola Virus Pathogenesis: Implications for Vaccines and Therapies" (Free full text). Journal of Virology. 77 (18): 9733–9737. doi:10.1128/JVI.77.18.9733-9737.2003. PMC 224575. PMID 12941881.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Gear JH (1989). "Clinical aspects of African viral hemorrhagic fevers". Reviews of infectious diseases. 11 Suppl 4: S777–S782. PMID 2665013.
- ^ Gear JH, Ryan J, Rossouw E (1978). "A consideration of the diagnosis of dangerous infectious fevers in South Africa". South African medical journal = Suid-Afrikaanse tydskrif vir geneeskunde. 53 (7): 235–237. PMID 565951.
{{cite journal}}: Missing pipe in:|journal=(help)CS1 maint: multiple names: authors list (link) - ^ Grolla A, Lucht A, Dick D, Strong JE, Feldmann H (2005). "Laboratory diagnosis of Ebola and Marburg hemorrhagic fever". Bulletin de la Societe de pathologie exotique (1990). 98 (3): 205–209. PMID 16267962.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Bogomolov BP (1998). "Differential diagnosis of infectious diseases with hemorrhagic syndrome". Terapevticheskii arkhiv. 70 (4): 63–68. PMID 9612907.
- ^ Ksiazek, Thomas G. (1991). "Laboratory diagnosis of filovirus infections in nonhuman primates". Lab Animal. 20 (7): 34–6.
- ^ van der Groen, G.; Webb, P.; Johnson, K.; Lange, J.; Lindsay, H.; Eliot, L. (1978). "Growth of Lassa and Ebola viruses in different cell lines". In Pattyn, S. R. (ed.). Ebola Virus Haemorrhagic Fever. Amsterdam, Netherlands: Elsevier/North-Holland Biomedical Press. pp. 255–260. ISBN 0-444-80060-3Template:Inconsistent citations
{{cite book}}: Invalid|ref=harv(help)CS1 maint: postscript (link) - ^ Sanchez A, Ksiazek TG, Rollin PE, Miranda ME, Trappier SG, Khan AS, Peters CJ, Nichol ST (1999). "Detection and Molecular Characterization of Ebola Viruses Causing Disease in Human and Nonhuman Primates". The Journal of Infectious Diseases. 179: S164–S169. doi:10.1086/514282. PMID 9988180.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Leroy EM, Baize S, Lu CY, McCormick JB, Georges AJ, Georges-Courbot MC, Lansoud-Soukate J, Fisher-Hoch SP (2000). "Diagnosis of Ebola haemorrhagic fever by RT-PCR in an epidemic setting". Journal of Medical Virology. 60 (4): 463–467. doi:10.1002/(SICI)1096-9071(200004)60:4<463::AID-JMV15>3.0.CO;2-M. PMID 10686031.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Drosten C, Göttig S, Schilling S, Asper M, Panning M, Schmitz H, Günther S (2002). "Rapid Detection and Quantification of RNA of Ebola and Marburg Viruses, Lassa Virus, Crimean-Congo Hemorrhagic Fever Virus, Rift Valley Fever Virus, Dengue Virus, and Yellow Fever Virus by Real-Time Reverse Transcription-PCR". Journal of clinical microbiology. 40 (7): 2323–2330. PMC 120575. PMID 12089242.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Gibb TR, Norwood DA, Woollen N, Henchal EA (2001). "Development and Evaluation of a Fluorogenic 5′ Nuclease Assay to Detect and Differentiate between Ebola Virus Subtypes Zaire and Sudan". Journal of Clinical Microbiology. 39 (11): 4125–4130. doi:10.1128/JCM.39.11.4125-4130.2001. PMC 88497. PMID 11682540.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Towner JS, Rollin PE, Bausch DG, Sanchez A, Crary SM, Vincent M, Lee WF, Spiropoulou CF, Ksiazek TG, Lukwiya M, Kaducu F, Downing R, Nichol ST (2004). "Rapid Diagnosis of Ebola Hemorrhagic Fever by Reverse Transcription-PCR in an Outbreak Setting and Assessment of Patient Viral Load as a Predictor of Outcome". Journal of Virology. 78 (8): 4330–4341. doi:10.1128/JVI.78.8.4330-4341.2004. PMC 374287. PMID 15047846.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Weidmann M, Mühlberger E, Hufert FT (2004). "Rapid detection protocol for filoviruses". Journal of Clinical Virology. 30 (1): 94–99. doi:10.1016/j.jcv.2003.09.004. PMID 15072761.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Zhai J, Palacios G, Towner JS, Jabado O, Kapoor V, Venter M, Grolla A, Briese T, Paweska J, Swanepoel R, Feldmann H, Nichol ST, Lipkin WI (2006). "Rapid Molecular Strategy for Filovirus Detection and Characterization". Journal of Clinical Microbiology. 45 (1): 224–226. doi:10.1128/JCM.01893-06. PMC 1828965. PMID 17079496.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Ksiazek TG, Rollin PE, Jahrling PB, Johnson E, Dalgard DW, Peters CJ (1992). "Enzyme immunosorbent assay for Ebola virus antigens in tissues of infected primates". Journal of clinical microbiology. 30 (4): 947–950. PMC 265191. PMID 1572982.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Niikura M, Ikegami T, Saijo M, Kurane I, Miranda ME, Morikawa S (2001). "Detection of Ebola Viral Antigen by Enzyme-Linked Immunosorbent Assay Using a Novel Monoclonal Antibody to Nucleoprotein". Journal of clinical microbiology. 39 (9): 3267–3271. PMC 88329. PMID 11526161.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Lucht A, Grunow R, Möller P, Feldmann H, Becker S (2003). "Development, characterization and use of monoclonal VP40-antibodies for the detection of Ebola virus". Journal of Virological Methods. 111 (1): 21–28. doi:10.1016/S0166-0934(03)00131-9. PMID 12821193.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Lucht A, Grunow R, Otterbein C, Möller P, Feldmann H, Becker S (2003). "Production of monoclonal antibodies and development of an antigen capture ELISA directed against the envelope glycoprotein GP of Ebola virus". Medical Microbiology and Immunology. 193 (4): 181–187. doi:10.1007/s00430-003-0204-z. PMID 14593476.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Yu JS, Liao HX, Gerdon AE, Huffman B, Scearce RM, McAdams M, Alam SM, Popernack PM, Sullivan NJ, Wright D, Cliffel DE, Nabel GJ, Haynes BF (2006). "Detection of Ebola virus envelope using monoclonal and polyclonal antibodies in ELISA, surface plasmon resonance and a quartz crystal microbalance immunosensor". Journal of Virological Methods. 137 (2): 219–228. doi:10.1016/j.jviromet.2006.06.014. PMID 16857271.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Büchen-Osmond, Cornelia (2006-04-25). "ICTVdB Virus Description – 01.025.0.02. Ebolavirus". International Committee on Taxonomy of Viruses. Retrieved 2009-06-02.
- ^ Suzuki Y, Gojobori T (1997). "The origin and evolution of Ebola and Marburg viruses". Molecular Biology and Evolution. 14 (8): 800–6. PMID 9254917.
- ^ Taylor DJ, Dittmar K, Ballinger MJ, Bruenn JA (2011). "Evolutionary maintenance of filovirus-like genes in bat genomes". BMC Evolutionary Biology. 11: 336. doi:10.1186/1471-2148-11-336. PMC 3229293. PMID 22093762.
{{cite journal}}: CS1 maint: multiple names: authors list (link) CS1 maint: unflagged free DOI (link) - ^ Isaacson, M; Sureau, P; Courteille, G; Pattyn, SR;. "Clinical Aspects of Ebola Virus Disease at the Ngaliema Hospital, Kinshasa, Zaire, 1976". Retrieved 2014-06-24.
{{cite journal}}: Cite journal requires|journal=(help); Invalid|ref=harv(help)CS1 maint: extra punctuation (link) CS1 maint: multiple names: authors list (link) - ^ a b Feldmann H, Geisbert TW (2011). "Ebola haemorrhagic fever". The Lancet. 377 (9768): 849–862. doi:10.1016/S0140-6736(10)60667-8. PMID 21084112.
- ^ a b Special Pathogens Branch CDC (2008-01-14). "Known Cases and Outbreaks of Ebola Hemorrhagic Fever". Center for Disease Control and Prevention. Retrieved 2008-08-02.
- ^ McNeil Jr, Donald G. (2009-01-24). "Pig-to-Human Ebola Case Suspected in Philippines". New York Times. Retrieved 2009-01-26.
- ^ McCormick & Fisher-Hoch 1999, p. 300
- ^ Waterman, Tara (1999). Ebola Cote D'Ivoire Outbreaks. Stanford University. Retrieved 2009-05-30.
- ^ "End of Ebola outbreak in Uganda" (Press release). World Health Organization. 2008-02-20.
- ^ Wamala, J; Lukwago, L; Malimbo, M; Nguku, P; Yoti, Z; Musenero, M; Amone, J; Mbabazi, W; Nanyunja, M; Zaramba, S; Opio, A; Lutwama, J; Talisuna, A; Okware, I; (2010). "Ebola Hemorrhagic Fever Associated with Novel Virus Strain, Uganda, 2007–2008". Emerging Infectious Disease. 16 (7). Retrieved 2010-06-24.
{{cite journal}}: Invalid|ref=harv(help)CS1 maint: extra punctuation (link) CS1 maint: multiple names: authors list (link) - ^ Ebola Virus: Symptoms, Treatment, and Prevention
- ^ a b Centers for Disease Control and Prevention and World Health Organization (1998). Infection Control for Viral Haemorrhagic Fevers in the African Health Care Setting (PDF). Atlanta, Georgia, US: Centers for Disease Control and Prevention. Retrieved 2013-02-08.
- ^ Center for Disease Control, Special Pathogens Branch. Questions and Answers about Ebola Hemorrhagic Fever (PDF). Atlanta, Georgia, US: Center for Disease Control.
- ^ a b Sullivan NJ, Geisbert TW, Geisbert JB, Xu L, Yang ZY, Roederer M, Koup RA, Jahrling PB, Nabel GJ (2003). "Accelerated vaccination for Ebola virus haemorrhagic fever in non-human primates". Nature. 424 (6949): 681–684. doi:10.1038/nature01876. PMID 12904795.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Jones SM, Feldmann H, Ströher U, Geisbert JB, Fernando L, Grolla A, Klenk HD, Sullivan NJ, Volchkov VE, Fritz EA, Daddario KM, Hensley LE, Jahrling PB, Geisbert TW (2005). "Live attenuated recombinant vaccine protects nonhuman primates against Ebola and Marburg viruses". Nature Medicine. 11 (7): 786–790. doi:10.1038/nm1258. PMID 15937495.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ a b Oplinger, Anne A. (2003-11-18). NIAID Ebola vaccine enters human trial. Bio-Medicine.
- ^ a b "Ebola/Marburg Vaccine Development" (Press release). National Institute of Allergy and Infectious Diseases. 2008-09-15.
- ^ Mikhaĭlov VV, Borisevich IV, Chernikova NK, Potryvaeva NV, Krasnianskiĭ VP (1994). "The evaluation in hamadryas baboons of the possibility for the specific prevention of Ebola fever". Voprosy virusologii. 39 (2): 82–84. PMID 8017061.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Lupton HW, Lambert RD, Bumgardner DL, Moe JB, Eddy GA (1980). "Inactivated vaccine for Ebola virus efficacious in guineapig model". Lancet. 2 (8207): 1294–1295. PMID 6108462.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Geisbert TW, Pushko P, Anderson K, Smith J, Davis KJ, Jahrling PB (2002). "Evaluation in nonhuman primates of vaccines against Ebola virus". Emerging Infectious Diseases. 8 (5): 503–507. PMID 11996686.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Xu L, Sanchez A, Yang Z, Zaki SR, Nabel EG, Nichol ST, Nabel GJ (1998). "Immunization for Ebola virus infection". Nature Medicine. 4 (1): 37–42. doi:10.1038/nm0198-037. PMID 9427604.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Geisbert TW, Daddario-Dicaprio KM, Geisbert JB, Reed DS, Feldmann F, Grolla A, Ströher U, Fritz EA, Hensley LE, Jones SM, Feldmann H (2008). "Vesicular stomatitis virus-based vaccines protect nonhuman primates against aerosol challenge with Ebola and Marburg viruses". Vaccine. 26 (52): 6894–6900. doi:10.1016/j.vaccine.2008.09.082. PMC 3398796. PMID 18930776.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Geisbert TW, Daddario-Dicaprio KM, Lewis MG, Geisbert JB, Grolla A, Leung A, Paragas J, Matthias L, Smith MA, Jones SM, Hensley LE, Feldmann H, Jahrling PB (2008). Kawaoka, Yoshihiro (ed.). "Vesicular Stomatitis Virus-Based Ebola Vaccine is Well-Tolerated and Protects Immunocompromised Nonhuman Primates". PLoS Pathogens. 4 (11): e1000225. doi:10.1371/journal.ppat.1000225. PMC 2582959. PMID 19043556.
{{cite journal}}: CS1 maint: multiple names: authors list (link) CS1 maint: unflagged free DOI (link) - ^ Geisbert TW, Geisbert JB, Leung A, Daddario-DiCaprio KM, Hensley LE, Grolla A, Feldmann H (2009). "Single-Injection Vaccine Protects Nonhuman Primates against Infection with Marburg Virus and Three Species of Ebola Virus". Journal of Virology. 83 (14): 7296–7304. doi:10.1128/JVI.00561-09. PMC 2704787. PMID 19386702.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Warfield KL, Swenson DL, Olinger GG, Kalina WV, Aman MJ, Bavari S (2007). "Ebola Virus‐Like Particle–Based Vaccine Protects Nonhuman Primates against Lethal Ebola Virus Challenge". The Journal of Infectious Diseases. 196: S430–S437. doi:10.1086/520583. PMID 17940980.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Martin JE, Sullivan NJ, Enama ME, Gordon IJ, Roederer M, Koup RA, Bailer RT, Chakrabarti BK, Bailey MA, Gomez PL, Andrews CA, Moodie Z, Gu L, Stein JA, Nabel GJ, Graham BS (2006). "A DNA Vaccine for Ebola Virus is Safe and Immunogenic in a Phase I Clinical Trial". Clinical and Vaccine Immunology. 13 (11): 1267–1277. doi:10.1128/CVI.00162-06. PMC 1656552. PMID 16988008.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Bush, L. (2005). "Crucell and NIH sign Ebola vaccine manufacturing contract". Pharmaceutical Technology. 29: 28Template:Inconsistent citations
{{cite journal}}: Invalid|ref=harv(help)CS1 maint: postscript (link) - ^ Phoolcharoen W, Dye JM, Kilbourne J, Piensook K, Pratt WD, Arntzen CJ, Chen Q, Mason HS, Herbst-Kralovetz MM (2011). "A nonreplicating subunit vaccine protects mice against lethal Ebola virus challenge". Proc. Natl. Acad. Sci. U.S.A. 108 (51): 20695–700. Bibcode:2011PNAS..10820695P. doi:10.1073/pnas.1117715108. PMC 3251076. PMID 22143779.
{{cite journal}}: Unknown parameter|laysource=ignored (help); Unknown parameter|laysummary=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Bausch DG, Feldmann H, Geisbert TW, Bray M, Sprecher AG, Boumandouki P, Rollin PE, Roth C (2007). "Outbreaks of Filovirus Hemorrhagic Fever: Time to Refocus on the Patient". The Journal of Infectious Diseases. 196: S136–S141. doi:10.1086/520542. PMID 17940941.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Jeffs B (2006). "A clinical guide to viral haemorrhagic fevers: Ebola, Marburg and Lassa". Tropical Doctor. 36 (1): 1–4. doi:10.1258/004947506775598914. PMID 16483416.
- ^ Nkoghé D, Formenty P, Nnégué S, Mvé MT, Hypolite I, Léonard P, Leroy E (2004). "Practical guidelines for the management of Ebola infected patients in the field". Medecine tropicale : revue du Corps de sante colonial. 64 (2): 199–204. PMID 15460155.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ "Sierra Leone Is Epicenter of Ebola as Guinea Clinic Shut". 2014-06-08. Retrieved 2014-07-30.
- ^ Akinfeeva LA, Aksyonova OI, Vasilevich IV, Ginko ZI, Zarkov KA, Zubavichene LR, Kuzovlev OP, Kuzubov VI, Lokteva LI, Ryabchikova YeI (2005). "A case of Ebola hemorrhagic fever". Infektsionnye Bolezni (3): 85–88.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Feldmann H, Jones SM, Daddario-DiCaprio KM, Geisbert JB, Ströher U, Grolla A, Bray M, Fritz EA, Fernando L, Feldmann F, Hensley LE, Geisbert TW (2007). "Effective Post-Exposure Treatment of Ebola Infection". PLoS Pathogens. 3 (1): e2. doi:10.1371/journal.ppat.0030002. PMC 1779298. PMID 17238284.
{{cite journal}}: CS1 maint: multiple names: authors list (link) CS1 maint: unflagged free DOI (link) - ^ Geisbert TW, Daddario-DiCaprio KM, Williams KJ, Geisbert JB, Leung A, Feldmann F, Hensley LE, Feldmann H, Jones SM (2008). "Recombinant Vesicular Stomatitis Virus Vector Mediates Postexposure Protection against Sudan Ebola Hemorrhagic Fever in Nonhuman Primates". Journal of Virology. 82 (11): 5664–5668. doi:10.1128/JVI.00456-08. PMC 2395203. PMID 18385248.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Tuffs A (2009). "Experimental vaccine may have saved Hamburg scientist from Ebola fever". BMJ. 338: b1223. doi:10.1136/bmj.b1223. PMID 19307268.
- ^ Geisbert TW, Lee AC, Robbins M, Geisbert JB, Honko AN, Sood V, Johnson JC, de Jong S, Tavakoli I, Judge A, Hensley LE, Maclachlan I (2010). "Postexposure protection of non-human primates against a lethal Ebola virus challenge with RNA interference: A proof-of-concept study". The Lancet. 375 (9729): 1896–1905. doi:10.1016/S0140-6736(10)60357-1. PMID 20511019.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Warren TK, Warfield KL, Wells J, Swenson DL, Donner KS, Van Tongeren SA, Garza NL, Dong L, Mourich DV, Crumley S, Nichols DK, Iversen PL, Bavari S (2010). "Advanced antisense therapies for postexposure protection against lethal filovirus infections". Nature Medicine. 16 (9): 991–994. doi:10.1038/nm.2202. PMID 20729866.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ "FDA-approved selective estrogen receptor modulators inhibit Ebola virus infection". Science Translation Medicine. 5 (190): 190ra79. 19 Jun 2013. doi:10.1126/scitranslmed.3005471. PMID 23785035.
- ^ Healthline – 20 June 2013 http://www.healthline.com/health-news/tech-breast-cancer-drugs-fight-ebola-virus-infection-062013
- ^ Mupapa K, Massamba M, Kibadi K, Kuvula K, Bwaka A, Kipasa M, Colebunders R, Muyembe-Tamfum JJ (1999). "Treatment of Ebola Hemorrhagic Fever with Blood Transfusions from Convalescent Patients". The Journal of Infectious Diseases. 179: S18–S23. doi:10.1086/514298. PMID 9988160.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ World Health Organization. "Ebola virus disease, West Africa – update 29 July 2014". Retrieved 2014-07-31.
- ^ McCormick & Fisher-Hoch 1999, pp. 277–279
- ^ Waterman, Tara (1999). Ebola Reston Outbreaks. Stanford University. Retrieved 2008-08-02.
- ^ McCormick & Fisher-Hoch 1999, pp. 298–299
- ^ Salvaggio MR, Baddley JW (2004). "Other viral bioweapons: Ebola and Marburg hemorrhagic fever". Dermatologic clinics. 22 (3): 291–302, vi. doi:10.1016/j.det.2004.03.003. PMID 15207310.
- ^ Borio L, Inglesby T, Peters CJ, Schmaljohn AL, Hughes JM, Jahrling PB, Ksiazek T, Johnson KM, Meyerhoff A, O'Toole T, Ascher MS, Bartlett J, Breman JG, Eitzen EM, Hamburg M, Hauer J, Henderson DA, Johnson RT, Kwik G, Layton M, Lillibridge S, Nabel GJ, Osterholm MT, Perl TM, Russell P, Tonat K (2002). "Hemorrhagic fever viruses as biological weapons: medical and public health management". Journal of the American Medical Association. 287 (18): 2391–405. doi:10.1001/jama.287.18.2391. PMID 11988060.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Ebola 'kills over 5,000 gorillas'. BBC. 2006-12-08. Retrieved 2009-05-31.
- ^ "Ebola Outbreak Confirmed in Congo". NewScientist.com. 2007-09-11. Retrieved 2008-02-25.
- ^ Ebola outbreak in Congo. CDC news. 2007-09-12. Retrieved 2009-05-31.
- ^ "Mystery DR Congo fever kills 100". BBC News. 2007-08-31. Retrieved 2008-02-25.
- ^ "Uganda: Deadly Ebola Outbreak Confirmed – UN". UN News Service. 2007-11-30. Retrieved 2008-02-25.
- ^ The IV International Symposium on Filoviruses. l'Institut de recherche pour le développement (IRD). Retrieved 2009-0-31.
{{cite book}}: Check date values in:|accessdate=(help) - ^ World Health Organization (2008-12-27). RD Congo: Fièvre hémorragique à virus Ebola au Kasaï Occidental, Rapport de situation No 1 des 26 & 27 décembre 2008 (in French). Relief Web. Retrieved 2009-06-02.
- ^ Ebola epidemic kills nine in central DR Congo: report. Agence France-Presse. 2008-12-25. Retrieved 2009-05-30.
- ^ Ebola alert shuts Angolan border. BBC. 2009-01-06. Retrieved 2009-05-31.
- ^ Eddyn, Melissan (2009-03-27). "Scientist Injects Self With Ebola". Associated Press. Retrieved 2009-05-02.
- ^ Malone, Barry (2011-06-17). "Uganda says Ebola outbreak is over". Reuters. Retrieved 2011-07-06.
- ^ Norway (2012-08-24). "Congo (DRC): Bushmeat blamed for Ebola outbreak – Norwegian Council for Africa". Afrika.no. Retrieved 2013-04-15.
- ^ "Outbreak of Ebola in Uganda kills 13". BBC News. July 28, 2012.
- ^ "Officials: Uganda Ebola outbreak kills 14 – Health | NBC News". MSNBC. 2012-07-28. Retrieved 2013-04-15.
- ^ "Ebola Outbreak Spreads". Associated Press – The Express. July 31, 2012.
{{cite news}}:|access-date=requires|url=(help) - ^ "WHO | Ebola in Uganda – update". Who.int. 2012-08-03. Retrieved 2013-04-15.
- ^ Prisoner with suspected case of Ebola escapes from hospital in Uganda – CNN.com
- ^ "WHO: Ebola Outbreak in Uganda is Under Control : US/World". Medical Daily. 2012-08-03. Retrieved 2013-04-15.
- ^ "Ebola in Uganda – update". WHO. Retrieved 2012-08-10.
- ^ "DRC Confirms Ebola Outbreak". Voanews.com. Retrieved 2013-04-15.
- ^ "WHO | Ebola outbreak in Democratic Republic of Congo". Who.int. 2012-08-17. Retrieved 2013-04-15.
- ^ "WHO | Ebola outbreak in Democratic Republic of Congo – update". Who.int. 2012-08-21. Retrieved 2013-04-15.
- ^ "Ebola outbreak in DRC – Disaster News Network". Disasternews.net. 2012-08-22. Retrieved 2013-04-15.
- ^ "Ebola virus claims 31 lives in Democratic Republic of the Congo". United States: CBS News. 2012. Retrieved 14 September 2012Template:Inconsistent citations
{{cite journal}}: Cite journal requires|journal=(help); Invalid|ref=harv(help)CS1 maint: postscript (link) - ^ "Outbreak of Ebola in Guinea and Liberia". Centers for Disease Control and Prevention. Retrieved 13 April 2014.
- ^ Ebola virus disease, West Africa (Situation as of 7 April 2014) – Guinea | ReliefWeb
- ^ EUROPA – PRESS RELEASES – Press release – Ebola in West Africa: European Union joins effort to stop spread of disease and releases €500 000 in immediate funding
- ^ United Nations News Centre – UN agency urges vigilance amid Ebola outbreak in Guinea, Sierra Leone and Liberia
- ^ Why Is This Ebola Outbreak Spreading?
- ^ WHO warns drastic action needed to combat Ebola outbreak | Big News Network.com
- ^ "Ebola virus disease, West Africa – update 25 July 2014". WHO: Outbreak news. 25 July 2014. Retrieved 30 July 2014.
- ^ a b Brown, Rob (18 July 2014) The virus detective who discovered Ebola in 1976 BBC News Magazine, Retrieved 18 July 2014
- ^ Bennett D, Brown D (May 1995). "Ebola virus". BMJ (Clinical research ed.). 310 (6991): 1344–1345. doi:10.1136/bmj.310.6991.1344. ISSN 0959-8138. PMC 2549737. PMID 7787519.
- ^ King, John W (April 2, 2008). "Ebola Virus". eMedicine. WebMd. Retrieved 2008-10-06.
- ^ "Plague of Athens".
- ^ Rouquet P, Froment JM, Bermejo M, Kilbourn A, Karesh W, Reed P, Kumulungui B, Yaba P, Délicat A, Rollin PE, Leroy EM (Feb 2005). "Wild animal mortality monitoring and human Ebola outbreaks, Gabon and Republic of Congo, 2001–2003" (Free full text). Emerging Infectious Diseases. 11 (2): 283–290. doi:10.3201/eid1102.040533. ISSN 1080-6040. PMC 3320460. PMID 15752448.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ a b Leroy EM, Rouquet P, Formenty P, Souquière S, Kilbourne A, Froment JM, Bermejo M, Smit S, Karesh W, Swanepoel R, Zaki SR, Rollin PE (2004). "Multiple Ebola virus transmission events and rapid decline of central African wildlife". Science. 303 (5656): 387–390. Bibcode:2004Sci...303..387L. doi:10.1126/science.1092528. PMID 14726594.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Formenty P, Boesch C, Wyers M, Steiner C, Donati F, Dind F, Walker F, Le Guenno B (1999). "Ebola virus outbreak among wild chimpanzees living in a rain forest of Côte d'Ivoire". The Journal of infectious diseases. 179. Suppl 1 (s1): S120–S126. doi:10.1086/514296. PMID 9988175.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Weingartl HM, Nfon C, Kobinger G (2013) Review of Ebola virus infections in domestic animals. Dev Biol (Basel). 2013;135:211–218
- ^ a b "Growing concerns over 'in the air' transmission of Ebola". United Kingdom: BBC News. 2012. Retrieved 16 November 2012Template:Inconsistent citations
{{cite journal}}: Cite journal requires|journal=(help); Invalid|ref=harv(help)CS1 maint: postscript (link) - ^ "Ebola Virus Antibodies in Fruit Bats, Bangladesh". Emerging Infectious Disease. 19 (2). CDC. 2013. doi:10.3201/eid1902.120524.
{{cite journal}}: Unknown parameter|authors=ignored (help)
- Bibliography
- Klenk, Hans-Dieter (January 1999). Marburg and Ebola Viruses (Current Topics in Microbiology and Immunology). Berlin: Springer-Verlag Telos. ISBN 978-3-540-64729-4.
{{cite book}}: CS1 maint: ref duplicates default (link) - Klenk, Hans-Dieter; Feldmann, Heinz (2004). Ebola and Marburg viruses: molecular and cellular biology (Limited preview). Wymondham, Norfolk, UK: Horizon Bioscience. ISBN 978-0-9545232-3-7.
{{cite book}}: CS1 maint: ref duplicates default (link) - Kuhn, Jens H. (2008). Filoviruses: A Compendium of 40 Years of Epidemiological, Clinical, and Laboratory Studies. Archives of Virology Supplement, vol. 20 (Limited preview). Vienna: SpringerWienNewYork. ISBN 978-3-211-20670-6.
{{cite book}}: CS1 maint: ref duplicates default (link) - McCormick, Joseph; Fisher-Hoch, Susan (1999) [1996]. Level 4: Virus Hunters of the CDC (Limited preview). Horvitz, Leslie Alan (Updated [3rd] ed.). Barnes & Noble. ISBN 978-0-7607-1208-5.
{{cite book}}: Unknown parameter|month=ignored (help)CS1 maint: ref duplicates default (link) - Pattyn, S. R. (1978). Ebola Virus Haemorrhagic Fever (Full free text) (1st ed.). Amsterdam: Elsevier/North-Holland Biomedical Press. ISBN 0-444-80060-3.
{{cite book}}: CS1 maint: ref duplicates default (link) - Ryabchikova, Elena I.; Price, Barbara B. (2004). Ebola and Marburg Viruses: A View of Infection Using Electron Microscopy. Columbus, Ohio: Battelle Press. ISBN 978-1-57477-131-2.
{{cite book}}: CS1 maint: ref duplicates default (link)
External links
- ViralZone: Ebola-like viruses – Virological repository from the Swiss Institute of Bioinformatics
- CDC: Ebola hemorrhagic fever – Centers for Disease Control and Prevention, Special Pathogens Branch
- WHO: Ebola haemorrhagic fever – World Health Organization, Global Alert and Response
- Virus Pathogen Database and Analysis Resource (ViPR): Filoviridae
- 3D macromolecular structures of the Ebola virus archived in the EM Data Bank(EMDB)
- Google Map of Ebola Outbreaks
- WHO recommended infection control measures
