Herpes simplex virus: Difference between revisions
m Journal cites, added 1 DOI, added 1 PMID using AWB (9627) |
|||
| Line 85: | Line 85: | ||
|- |
|- |
||
| <small> [[UL4]] || <small>UL4 [http://www.uniprot.org/uniprot/P10188] || <small>unknown |
| <small> [[UL4]] || <small>UL4 [http://www.uniprot.org/uniprot/P10188] || <small>unknown |
||
| |<small> [[UL41]] || <small>UL41; VHS [http://www.uniprot.org/uniprot/P10225] || <small>Tegument protein; Virion host shutoff<ref name="pmid12083325">{{cite journal |author=Matis J, Kúdelová M |title=Early shutoff of host protein synthesis in cells infected with herpes simplex viruses |journal=Acta Virol. |volume=45 |issue=5–6 |pages=269–77 |year=2001 |pmid=12083325 |doi=}}</ref> |
| |<small> [[UL41]] || <small>UL41; VHS [http://www.uniprot.org/uniprot/P10225] || <small>Tegument protein; Virion host shutoff<ref name="pmid12083325">{{cite journal |author=Matis J, Kúdelová M |title=Early shutoff of host protein synthesis in cells infected with herpes simplex viruses |journal=Acta Virol. |volume=45 |issue=5–6 |pages=269–77 |year=2001 |pmid=12083325 |doi=10.2217/fvl.11.24}}</ref> |
||
|- |
|- |
||
| <small>[[UL5]] || <small>UL5 [http://www.expasy.org/uniprot/Q2MGV2] || <small> [[DNA replication]] |
| <small>[[UL5]] || <small>UL5 [http://www.expasy.org/uniprot/Q2MGV2] || <small> [[DNA replication]] |
||
| Line 191: | Line 191: | ||
==Evolution== |
==Evolution== |
||
The Herpes simplex 1 genomes can be classified into six clades.<ref name=Kolb2013>Kolb AW, Ané C, Brandt CR (2013) Using HSV-1 genome phylogenetics to track past human migrations |
The Herpes simplex 1 genomes can be classified into six clades.<ref name=Kolb2013>Kolb AW, Ané C, Brandt CR (2013) Using HSV-1 genome phylogenetics to track past human migrations" ''PLoS One'' 8(10) e76267. {{DOI|10.1371/journal.pone.0076267}}</ref> Four of these occur in East Africa with one clade in East Asian and another in Europe/North America. This suggests that this virus may have originated in East Africa. The [[most recent common ancestor]] of the Eurasian strains appears to have evolved ~60,000 years ago.<ref name=Bowden2006>Bowden R, Sakaoka H, Ward R, Donnelly P (2006) Patterns of Eurasian HSV-1 molecular diversity and inferences of human migrations" ''Infect Genet Evol'' 6(1) 63-74 </ref> The East Asian HSV-1 isolates have an unusual pattern that is currently best explained by the two waves of migration responsible for the peopling of Japan. |
||
The mutation rate has been estimated to be ~1.38×10<sup>-7</sup> subsitutions/site/year.<ref name=Kolb2013>Kolb AW, Ané C, Brandt CR (2013) Using HSV-1 genome phylogenetics to track past human migrations |
The mutation rate has been estimated to be ~1.38×10<sup>-7</sup> subsitutions/site/year.<ref name=Kolb2013>Kolb AW, Ané C, Brandt CR (2013) Using HSV-1 genome phylogenetics to track past human migrations" ''PLoS One'' 8(10) e76267. {{DOI|10.1371/journal.pone.0076267}}</ref> |
||
==Treatment and vaccine development== |
==Treatment and vaccine development== |
||
| Line 201: | Line 201: | ||
==Connection between facial sores and Alzheimer's disease== |
==Connection between facial sores and Alzheimer's disease== |
||
In the presence of a certain gene variation ([[Apolipoprotein E|APOE]]-epsilon4 allele carriers), a possible link between HSV-1 (i.e., the virus that causes cold sores or oral herpes) and [[Alzheimer's disease]] was reported in 1979.<ref>{{cite journal |author=Middleton PJ, Petric M, Kozak M, Rewcastle NB, McLachlan DR |title=Herpes-simplex viral genome and senile and presenile dementias of Alzheimer and Pick |journal=Lancet |volume=315 |issue=8176 |pages=1038 |year=1980 |month=May |pmid=6103379 |doi=10.1016/S0140-6736(80)91490-7 |url=}}</ref> HSV-1 appears to be particularly damaging to the nervous system and increases one’s risk of developing Alzheimer’s disease. The virus interacts with the components and receptors of [[lipoproteins]], which may lead to the development of Alzheimer's disease.<ref name=Dobson1999>{{cite journal |author=Dobson CB, Itzhaki RF |title=Herpes simplex virus type 1 and Alzheimer's disease |journal=Neurobiol. Aging |volume=20 |issue=4 |pages=457–65 |year=1999 |pmid=10604441 |doi=10.1016/S0197-4580(99)00055-X |url=}}</ref> This research identifies HSVs as the [[pathogen]] most clearly linked to the establishment of Alzheimer’s.<ref name=Pyles2001>{{cite journal |author=Pyles RB |title=The association of herpes simplex virus and Alzheimer's disease: a potential synthesis of genetic and environmental factors |journal=Herpes |volume=8 |issue=3 |pages=64–8 |year=2001 |month=November |pmid=11867022 |doi= |url = http://www.ihmf.com/journal/download/83pyles(64)vol864.pdf |format=PDF}}</ref> According to a study done in 1997, without the presence of the gene allele, HSV-1 does not appear to cause any neurological damage or increase the risk of Alzheimer’s.<ref name=Itzhaki1997>{{cite journal |author=Itzhaki RF, Lin WR, Shang D, Wilcock GK, Faragher B, Jamieson GA |title=Herpes simplex virus type 1 in brain and risk of Alzheimer's disease |journal=Lancet |volume=349 |issue=9047 |pages=241–4 |year=1997 |month=January |pmid=9014911 |doi=10.1016/S0140-6736(96)10149-5 |url=}}</ref> However, a more recent prospective study from 2008 with a cohort of several thousand people showed a high correlation between seropositivity for HSV and Alzheimer's disease, without direct correlation to the APOE-epsilon4 allele.<ref>{{cite journal|last=Letenneur|first=L|coauthors=Pérès, K, Fleury, H, Garrigue, I, Barberger-Gateau, P, Helmer, C, Orgogozo, JM, Gauthier, S, Dartigues, JF|title=Seropositivity to herpes simplex virus antibodies and risk of Alzheimer's disease: a population-based cohort study.|journal=PLoS ONE|year=2008|volume=3|issue=11|pages=e3637|pmid=18982063|doi=10.1371/journal.pone.0003637|pmc=2572852}}</ref> In 2011 Manchester University scientists showed that treating HSV1-infected cells with antiviral agents decreased the accumulation of ß-amyloid and P-tau, and also decreased HSV1 replication as expected.<ref>Wozniak MA, Frost AL, Preston CM, Itzhaki RF (2011) [http://www.plosone.org/article/info%3Adoi%2F10.1371%2Fjournal.pone.0025152 Antivirals Reduce the Formation of Key Alzheimer's Disease Molecules in Cell Cultures Acutely Infected with Herpes Simplex Virus Type 1] |
In the presence of a certain gene variation ([[Apolipoprotein E|APOE]]-epsilon4 allele carriers), a possible link between HSV-1 (i.e., the virus that causes cold sores or oral herpes) and [[Alzheimer's disease]] was reported in 1979.<ref>{{cite journal |author=Middleton PJ, Petric M, Kozak M, Rewcastle NB, McLachlan DR |title=Herpes-simplex viral genome and senile and presenile dementias of Alzheimer and Pick |journal=Lancet |volume=315 |issue=8176 |pages=1038 |year=1980 |month=May |pmid=6103379 |doi=10.1016/S0140-6736(80)91490-7 |url=}}</ref> HSV-1 appears to be particularly damaging to the nervous system and increases one’s risk of developing Alzheimer’s disease. The virus interacts with the components and receptors of [[lipoproteins]], which may lead to the development of Alzheimer's disease.<ref name=Dobson1999>{{cite journal |author=Dobson CB, Itzhaki RF |title=Herpes simplex virus type 1 and Alzheimer's disease |journal=Neurobiol. Aging |volume=20 |issue=4 |pages=457–65 |year=1999 |pmid=10604441 |doi=10.1016/S0197-4580(99)00055-X |url=}}</ref> This research identifies HSVs as the [[pathogen]] most clearly linked to the establishment of Alzheimer’s.<ref name=Pyles2001>{{cite journal |author=Pyles RB |title=The association of herpes simplex virus and Alzheimer's disease: a potential synthesis of genetic and environmental factors |journal=Herpes |volume=8 |issue=3 |pages=64–8 |year=2001 |month=November |pmid=11867022 |doi= |url = http://www.ihmf.com/journal/download/83pyles(64)vol864.pdf |format=PDF}}</ref> According to a study done in 1997, without the presence of the gene allele, HSV-1 does not appear to cause any neurological damage or increase the risk of Alzheimer’s.<ref name=Itzhaki1997>{{cite journal |author=Itzhaki RF, Lin WR, Shang D, Wilcock GK, Faragher B, Jamieson GA |title=Herpes simplex virus type 1 in brain and risk of Alzheimer's disease |journal=Lancet |volume=349 |issue=9047 |pages=241–4 |year=1997 |month=January |pmid=9014911 |doi=10.1016/S0140-6736(96)10149-5 |url=}}</ref> However, a more recent prospective study from 2008 with a cohort of several thousand people showed a high correlation between seropositivity for HSV and Alzheimer's disease, without direct correlation to the APOE-epsilon4 allele.<ref>{{cite journal|last=Letenneur|first=L|coauthors=Pérès, K, Fleury, H, Garrigue, I, Barberger-Gateau, P, Helmer, C, Orgogozo, JM, Gauthier, S, Dartigues, JF|title=Seropositivity to herpes simplex virus antibodies and risk of Alzheimer's disease: a population-based cohort study.|journal=PLoS ONE|year=2008|volume=3|issue=11|pages=e3637|pmid=18982063|doi=10.1371/journal.pone.0003637|pmc=2572852}}</ref> In 2011 Manchester University scientists showed that treating HSV1-infected cells with antiviral agents decreased the accumulation of ß-amyloid and P-tau, and also decreased HSV1 replication as expected.<ref>Wozniak MA, Frost AL, Preston CM, Itzhaki RF (2011) [http://www.plosone.org/article/info%3Adoi%2F10.1371%2Fjournal.pone.0025152 Antivirals Reduce the Formation of Key Alzheimer's Disease Molecules in Cell Cultures Acutely Infected with Herpes Simplex Virus Type 1]" ''PLoS ONE'' 6(10) e25152. {{DOI|10.1371/journal.pone.0025152}}</ref> |
||
==Multiplicity reactivation== |
==Multiplicity reactivation== |
||
| Line 211: | Line 211: | ||
{{Main|Oncolytic herpes virus}} |
{{Main|Oncolytic herpes virus}} |
||
Herpes simplex virus is considered as a potential therapy for cancer and has been extensively clinically tested to assess its [[oncolytic]] (cancer killing) ability.<ref>{{cite journal|last=Varghese|first=Susan|coauthors=Rabkin, Samuel D|title=Oncolytic herpes simplex virus vectors for cancer virotherapy|journal=Cancer Gene Therapy|date=1 December 2002|volume=9|issue=12|pages=967–978|doi=10.1038/sj.cgt.7700537|url=http://www.nature.com/cgt/journal/v9/n12/full/7700537a.html}}</ref> |
Herpes simplex virus is considered as a potential therapy for cancer and has been extensively clinically tested to assess its [[oncolytic]] (cancer killing) ability.<ref>{{cite journal|last=Varghese|first=Susan|coauthors=Rabkin, Samuel D|title=Oncolytic herpes simplex virus vectors for cancer virotherapy|journal=Cancer Gene Therapy|date=1 December 2002|volume=9|issue=12|pages=967–978|doi=10.1038/sj.cgt.7700537|url=http://www.nature.com/cgt/journal/v9/n12/full/7700537a.html|pmid=12522436}}</ref> |
||
==Use in neuronal connection tracing== |
==Use in neuronal connection tracing== |
||
Revision as of 19:36, 18 November 2013
| Herpes simplex virus | |
|---|---|

| |
| TEM micrograph of a herpes simplex virus. | |
| Virus classification | |
| Group: | Group I (dsDNA)
|
| Order: | |
| Family: | |
| Subfamily: | |
| Genus: | |
| Species | |
| |
Herpes simplex virus 1 and 2 (HSV-1 and HSV-2), also known as Human herpes virus 1 and 2 (HHV-1 and -2), are two members of the herpes virus family, Herpesviridae, that infect humans.[1] Both HSV-1 (which produces most cold sores) and HSV-2 (which produces most genital herpes) are ubiquitous and contagious. They can be spread when an infected person is producing and shedding the virus. Herpes Simplex can be spread through contact with saliva, such as sharing drinks.
Symptoms of herpes simplex virus infection include watery blisters in the skin or mucous membranes of the mouth, lips or genitals.[1] Lesions heal with a scab characteristic of herpetic disease. Sometimes, the viruses cause very mild or atypical symptoms during outbreaks. However, as neurotropic and neuroinvasive viruses, HSV-1 and -2 persist in the body by becoming latent and hiding from the immune system in the cell bodies of neurons. After the initial or primary infection, some infected people experience sporadic episodes of viral reactivation or outbreaks. In an outbreak, the virus in a nerve cell becomes active and is transported via the neuron's axon to the skin, where virus replication and shedding occur and cause new sores.[2]
Transmission
HSV-1 and -2 are transmitted by contact with an infected area of the skin during re-activations of the virus. Although less likely, the herpes viruses can be transmitted during latency.[citation needed] Transmission is likely to occur during symptomatic re-activation of the virus that causes visible and typical skin sores. Asymptomatic reactivation means that the virus causes atypical, subtle or hard to notice symptoms that are not identified as an active herpes infection. Daily genital swab samples show that HSV-2 is found in a median of 12-28% of days among those who have had an outbreak and 10% of days among those suffering from asymptomatic infection, with many of these episodes occurring without visible outbreak ("subclinical shedding").[3] For HSV-2, subclinical shedding may account for most of the transmission, and one study found that infection occurred after a median of 40 sex acts.[3] Atypical symptoms are often attributed to other causes such as a yeast infection.[4][5] HSV-1 is often acquired orally during childhood. It may also be sexually transmitted, including contact with saliva, such as kissing and mouth-to-genital contact (oral sex).[6] HSV-2 is primarily a sexually transmitted infection but rates of HSV-1 genital infections are increasing.[4]
Both viruses may also be transmitted vertically during childbirth, although the real risk is very low.[7] The risk of infection is minimal if the mother has no symptoms or exposed blisters during delivery. The risk is considerable when the mother gets the virus for the first time during late pregnancy.[8]
Herpes simplex viruses can affect areas of skin exposed to contact with an infected person. An example of this is herpetic whitlow which is a herpes infection on the fingers. This was a common affliction of dental surgeons prior to the routine use of gloves when conducting treatment on patients.
Microbiology
Viral structure
Animal herpes viruses all share some common properties. The structure of herpes viruses consists of a relatively large double-stranded, linear DNA genome encased within an icosahedral protein cage called the capsid, which is wrapped in a lipid bilayer called the envelope. The envelope is joined to the capsid by means of a tegument. This complete particle is known as the virion.[9] HSV-1 and HSV-2 each contain at least 74 genes (or open reading frames, ORFs) within their genomes,[10] although speculation over gene crowding allows as many as 84 unique protein coding genes by 94 putative ORFs.[11] These genes encode a variety of proteins involved in forming the capsid, tegument and envelope of the virus, as well as controlling the replication and infectivity of the virus. These genes and their functions are summarized in the table below.
The genomes of HSV1 and HSV2 are complex and contain two unique regions called the long unique region (UL) and the short unique region (US). Of the 74 known ORFs, UL contains 56 viral genes, whereas US contains only 12.[10] Transcription of HSV genes is catalyzed by RNA polymerase II of the infected host.[10] Immediate early genes, which encode proteins that regulate the expression of early and late viral genes, are the first to be expressed following infection. Early gene expression follows, to allow the synthesis of enzymes involved in DNA replication and the production of certain envelope glycoproteins. Expression of late genes occurs last; this group of genes predominantly encode proteins that form the virion particle.[10]
Five proteins from (UL) form the viral capsid; UL6, UL18, UL35, UL38 and the major capsid protein UL19.[9]
Cellular entry
Entry of HSV into the host cell involves interactions of several glycoproteins on the surface of the enveloped virus, with receptors on the surface of the host cell. The envelope covering the virus particle, when bound to specific receptors on the cell surface, will fuse with the host cell membrane and create an opening, or pore, through which the virus enters the host cell.
The sequential stages of HSV entry are analogous to those of other viruses. At first, complementary receptors on the virus and the cell surface bring the viral and cell membranes into proximity. In an intermediate state, the two membranes begin to merge, forming a hemifusion state. Finally, a stable entry pore is formed through which the viral envelope contents are introduced to the host cell.[12] In the case of a herpes virus, initial interactions occur when a viral envelope glycoprotein called glycoprotein C (gC) binds to a cell surface particle called heparan sulfate. A second glycoprotein, glycoprotein D (gD), binds specifically to at least one of three known entry receptors. These include herpesvirus entry mediator(HVEM), nectin-1 and 3-O sulfated heparan sulfate. The receptor provides a strong, fixed attachment to the host cell. These interactions bring the membrane surfaces into mutual proximity and allow for other glycoproteins embedded in the viral envelope to interact with other cell surface molecules. Once bound to the HVEM, gD changes its conformation and interacts with viral glycoproteins H (gH) and L (gL), which form a complex. The interaction of these membrane proteins results in the hemifusion state. Afterward, gB interaction with the gH/gL complex creates an entry pore for the viral capsid.[12] Glycoprotein B interacts with glycosaminoglycans on the surface of the host cell.
Genetic inoculation
After the viral capsid enters the cellular cytoplasm, it is transported to the cell nucleus. Once attached to the nucleus at a nuclear entry pore, the capsid ejects its DNA contents via the capsid portal. The capsid portal is formed by twelve copies of portal protein, UL6, arranged as a ring; the proteins contain a leucine zipper sequence of amino acids which allow them to adhere to each other.[13] Each icosahedral capsid contains a single portal, located in one vertex.[14][15] The DNA exits the capsid in a single linear segment.[16]
Immune evasion
HSV evades the immune system through interference with MHC class I presentation of antigen on the cell surface. It achieves this through blockade of the transporter associated with antigen processing (TAP) induced by the secretion of ICP-47 by HSV.[17] In the host cell, TAP transports digested viral antigen epitopes from the cytosol to the endoplasmic reticulum, allowing these epitopes to be combined with MHC class I molecules and presented on the surface of the cell. Viral epitope presentation with MHC class I is a requirement for activation of cytotoxic T-lymphocytes (CTLs), the major effectors of the cell-mediated immune response against virally-infected cells. ICP-47 prevents initiation of a CTL-response against HSV, allowing the virus to survive for a protracted period in the host.
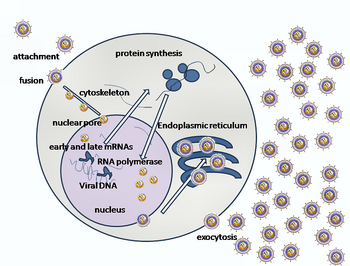
Replication

Following infection of a cell, a cascade of herpes virus proteins, called immediate-early, early, and late, are produced. Research using flow cytometry on another member of the herpes virus family, Kaposi's sarcoma-associated herpesvirus, indicates the possibility of an additional lytic stage, delayed-late.[18] These stages of lytic infection, particularly late lytic, are distinct from the latency stage. In the case of HSV-1, no protein products are detected during latency, whereas they are detected during the lytic cycle.
The early proteins transcribed are used in the regulation of genetic replication of the virus. On entering the cell, an α-TIF protein joins the viral particle and aids in immediate-early transcription. The virion host shutoff protein (VHS or UL41) is very important to viral replication.[19] This enzyme shuts off protein synthesis in the host, degrades host mRNA, helps in viral replication, and regulates gene expression of viral proteins. The viral genome immediately travels to the nucleus but the VHS protein remains in the cytoplasm.[20][21]
The late proteins are used in to form the capsid and the receptors on the surface of the virus. Packaging of the viral particles — including the genome, core and the capsid - occurs in the nucleus of the cell. Here, concatemers of the viral genome are separated by cleavage and are placed into pre-formed capsids. HSV-1 undergoes a process of primary and secondary envelopment. The primary envelope is acquired by budding into the inner nuclear membrane of the cell. This then fuses with the outer nuclear membrane releasing a naked capsid into the cytoplasm. The virus acquires its final envelope by budding into cytoplasmic vesicles.[22]
Latent infection
HSVs may persist in a quiescent but persistent form known as latent infection, notably in neural ganglia.[1] HSV-1 tends to reside in the trigeminal ganglia, while HSV-2 tends to reside in the sacral ganglia, but note that these are tendencies only, not fixed behavior. During such latent infection of a cell, HSVs express Latency Associated Transcript (LAT) RNA. LAT is known to regulate the host cell genome and interferes with natural cell death mechanisms. By maintaining the host cells, LAT expression preserves a reservoir of the virus, which allows subsequent, usually symptomatic, periodic recurrences or "outbreaks" characteristic of non-latency. Whether or not recurrences are noticeable (symptomatic), viral shedding occurs to produce further infections (usually in a new host, if any). A protein found in neurons may bind to herpes virus DNA and regulate latency. Herpes virus DNA contains a gene for a protein called ICP4, which is an important transactivator of genes associated with lytic infection in HSV-1.[23] Elements surrounding the gene for ICP4 bind a protein known as the human neuronal protein Neuronal Restrictive Silencing Factor (NRSF) or human Repressor Element Silencing Transcription Factor (REST). When bound to the viral DNA elements, histone deacetylation occurs atop the ICP4 gene sequence to prevent initiation of transcription from this gene, thereby preventing transcription of other viral genes involved in the lytic cycle.[23][24] Another HSV protein reverses the inhibition of ICP4 protein synthesis. ICP0 dissociates NRSF from the ICP4 gene and thus prevents silencing of the viral DNA.[25]
The virus can be reactivated by illnesses such as colds and influenza, eczema, emotional and physical stress, gastric upset, fatigue or injury, by menstruation and possibly exposure to bright sunlight.
Viral genome
Template:Genome header | UL1 || Glycoprotein L [1] || Surface and membrane | | UL38 || UL38; VP19C [2] || Capsid assembly and DNA maturation |- | UL2 || UL2 [3] || Uracil-DNA glycosylase | | UL39 || UL39 [4] || Ribonucleotide reductase (Large subunit) |- | UL3 || UL3 [5] || unknown | | UL40 || UL40 [6] || Ribonucleotide reductase (Small subunit) |- | UL4 || UL4 [7] || unknown | | UL41 || UL41; VHS [8] || Tegument protein; Virion host shutoff[19] |- | UL5 || UL5 [9] || DNA replication | | UL42 || UL42 [10] || DNA polymerase processivity factor |- | UL6 || Portal protein UL-6 || Twelve of these proteins constitute the capsid portal ring through which DNA enters and exits the capsid.[13][14][15] | | UL43 || UL43 [11] || Membrane protein |- | UL7 || UL7 [12] || Virion maturation | | UL44 || Glycoprotein C [13] || Surface and membrane |- | UL8 || UL8 [14] || DNA helicase/primase complex-associated protein | | UL45 || UL45 [15] || Membrane protein; C-type lectin[26] |- | UL9 || UL9 [16] || Replication origin-binding protein | | UL46 ||VP11/12 [17] || Tegument proteins |- | UL10 || Glycoprotein M [18] || Surface and membrane | | UL47 || UL47; VP13/14 [19] || Tegument protein |- | UL11 || UL11 [20] || virion exit and secondary envelopment | UL48 || VP16 (Alpha-TIF) [21] || Virion maturation; activate IE genes by interacting with the cellular transcription factors Oct-1 and HCF. Binds to the sequence 5'TAATGARAT3'. |- | UL12 || UL12 [22] || Alkaline exonuclease | | UL49 || UL49A [23] || Envelope protein |- | UL13 || UL13 [24] || Serine-threonine protein kinase | |UL50 || UL50 [25] || dUTP diphosphatase |- | UL14 || UL14 [26] || Tegument protein | | UL51 || UL51 [27] || Tegument protein |- | UL15 || Terminase [28] || Processing and packaging of DNA | |UL52 || UL52 [29] || DNA helicase/primase complex protein |- | UL16 || UL16 [30] || Tegument protein | |UL53 || Glycoprotein K [31] || Surface and membrane |- | UL17 || UL17 [32] || Processing and packaging DNA | |UL54 || IE63; ICP27 [33] || Transcriptional regulation |- | UL18 || VP23 [34] || Capsid protein | |UL55 || UL55 [35] || Unknown |- | UL19 || VP5 [36] || Major capsid protein | |UL56 || UL56 [37] || Unknown |- | UL20 || UL20 [38] || Membrane protein | |US1 || ICP22; IE68 [39] || Viral replication |- | UL21 || UL21 [40] || Tegument protein[27] | |US2 || US2 [41] || Unknown |- | UL22 || Glycoprotein H [42] || Surface and membrane | |US3 || US3 [43] || Serine/threonine-protein kinase |- | UL23 || Thymidine kinase [44] || Peripheral to DNA replication | |US4 || Glycoprotein G [45] || Surface and membrane |- | UL24 || UL24 [46] || unknown | |US5 || Glycoprotein J [47] || Surface and membrane |- | UL25 || UL25 [48] || Processing and packaging DNA | |US6 || Glycoprotein D [49] || Surface and membrane |- | UL26 || P40; VP24; VP22A [50] || Capsid protein | |US7 || Glycoprotein I [51] || Surface and membrane |- | UL27 || Glycoprotein B [52] || Surface and membrane | |US8 || Glycoprotein E [53] || Surface and membrane |- | UL28 || ICP18.5 [54] || Processing and packaging DNA | |US9 || US9 [55] || Tegument protein |- | UL29 || UL29; ICP8 [56] || Major DNA-binding protein | |US10 || US10 [57] || Capsid/Tegument protein |- | UL30 || DNA polymerase [58] || DNA replication | |US11 || US11; Vmw21 [59] || Binds DNA and RNA |- | UL31 || UL31 [60] || Nuclear matrix protein | |US12 || ICP47; IE12 [61] || Inhibits MHC class I pathway by preventing binding of antigen to TAP |- | UL32 || UL32 [62] || Envelope glycoprotein | |RS1 || ICP4; IE175 [63] || Major transcriptional activator. Essential for progression beyond the immediate-early phase of infection. IEG transcription repressor. |- | UL33 || UL33 [64] || Processing and packaging DNA | |ICP0 || ICP0; IE110; α0 [65] || E3 ubiquitin ligase that activates viral gene transcription by opposing chromatinization of the viral genome and counteracts intrinsic- and interferon-based antiviral responses.[28] |- | UL34 || UL34 [66] || Inner nuclear membrane protein | |LRP1 || LRP1 [67] || Latency-related protein |- | UL35 || VP26 [68] || Capsid protein | |LRP2 || LRP2 [69] || Latency-related protein |- | UL36 || UL36 [70] || Large tegument protein | |RL1 || RL1; ICP34.5 [71] || Neurovirulence factor. Antagonizes PKR by de-phosphorylating eIF4a. Binds to BECN1 and inactivates autophagy. |- | |UL37 || UL37 [72] || Capsid assembly | | LAT || none [73] || Latency-associated transcript |}
Evolution
The Herpes simplex 1 genomes can be classified into six clades.[29] Four of these occur in East Africa with one clade in East Asian and another in Europe/North America. This suggests that this virus may have originated in East Africa. The most recent common ancestor of the Eurasian strains appears to have evolved ~60,000 years ago.[30] The East Asian HSV-1 isolates have an unusual pattern that is currently best explained by the two waves of migration responsible for the peopling of Japan.
The mutation rate has been estimated to be ~1.38×10-7 subsitutions/site/year.[29]
Treatment and vaccine development
- For more details on treatment of herpes simplex virus, see Herpes simplex.
Herpes viruses establish lifelong infections, and the virus cannot yet be eradicated from the body. Treatment usually involves general-purpose antiviral drugs that interfere with viral replication, reduce the physical severity of outbreak-associated lesions, and lower the chance of transmission to others. Studies of vulnerable patient populations have indicated that daily use of antivirals such as acyclovir[31] and valacyclovir can reduce reactivation rates.[5]
Connection between facial sores and Alzheimer's disease
In the presence of a certain gene variation (APOE-epsilon4 allele carriers), a possible link between HSV-1 (i.e., the virus that causes cold sores or oral herpes) and Alzheimer's disease was reported in 1979.[32] HSV-1 appears to be particularly damaging to the nervous system and increases one’s risk of developing Alzheimer’s disease. The virus interacts with the components and receptors of lipoproteins, which may lead to the development of Alzheimer's disease.[33] This research identifies HSVs as the pathogen most clearly linked to the establishment of Alzheimer’s.[34] According to a study done in 1997, without the presence of the gene allele, HSV-1 does not appear to cause any neurological damage or increase the risk of Alzheimer’s.[35] However, a more recent prospective study from 2008 with a cohort of several thousand people showed a high correlation between seropositivity for HSV and Alzheimer's disease, without direct correlation to the APOE-epsilon4 allele.[36] In 2011 Manchester University scientists showed that treating HSV1-infected cells with antiviral agents decreased the accumulation of ß-amyloid and P-tau, and also decreased HSV1 replication as expected.[37]
Multiplicity reactivation
Multiplicity reactivation (MR) is the process by which viral genomes containing inactivating damage interact within an infected cell to form a viable viral genome. MR was originally discovered with the bacterial virus bacteriophage T4, but was subsequently also found with pathogenic viruses including influenza virus, HIV-1, adenovirus simian virus 40, vaccinia virus, reovirus, poliovirus and herpes simplex virus.[38]
When HSV particles are exposed to doses of a DNA damaging agent that would be lethal in single infections, but are then allowed to undergo multiple infection (i.e. two or more viruses per host cell), MR is observed. Enhanced survival of HSV-1 due to MR occurs upon exposure to different DNA damaging agents, including methyl methanesulfonate,[39] trimethylpsoralen (which causes inter-strand DNA cross-links,[40][41] and UV light.[42] After treatment of genetically marked HIV with trimethylpsoralen, recombination between the marked viruses increases, suggesting that trimethylpsoralen damages stimulate recombination.[40] MR of HSV appears to partially depend on the host cell recombinational repair machinery since skin fibroblast cells defective in a component of this machinery (i.e. cells from Bloom’s syndrome patients) are deficient in MR.[42] These observations suggest that MR in HSV infections involves genetic recombination between damaged viral genomes resulting in production of viable progeny viruses. HSV-1, upon infecting host cells, induces inflammation and oxidative stress.[43] Thus it appears that the HSV genome may be subjected to oxidative DNA damage during infection, and that MR may enhance viral survival and virulence under these conditions.
Use as an anti-cancer agent
Herpes simplex virus is considered as a potential therapy for cancer and has been extensively clinically tested to assess its oncolytic (cancer killing) ability.[44]
Use in neuronal connection tracing
Herpes simplex virus is also used as a transneuronal tracer defining connections among neurons by virtue of traversing synapses[45]
References
- ^ a b c Ryan KJ, Ray CG (editors) (2004). Sherris Medical Microbiology (4th ed.). McGraw Hill. pp. 555–62. ISBN 0-8385-8529-9.
{{cite book}}:|author=has generic name (help) - ^ "Herpes simplex". DermNet NZ — New Zealand Dermatological Society. 2006-09-16. Retrieved 2006-10-15.
- ^ a b Johnston C, Koelle DM, Wald A (2011). "HSV-2: in pursuit of a vaccine". J Clin Invest. 121 (12): 4600–9. doi:10.1172/JCI57148. PMID 22133885.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ a b Gupta R, Warren T, Wald A (2007). "Genital herpes". Lancet. 370 (9605): 2127–37. doi:10.1016/S0140-6736(07)61908-4. PMID 18156035.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ a b Koelle DM, Corey L (2008). "Herpes simplex: insights on pathogenesis and possible vaccines". Annual Review of Medicine. 59: 381–95. doi:10.1146/annurev.med.59.061606.095540. PMID 18186706.
- ^ "EVERYTHING YOU NEED TO KNOW ABOUT HERPES".
- ^ Corey L, Wald A (2009). "Maternal and Neonatal HSV Infections". New England Journal of Medicine. 361 (14): 1376–85. doi:10.1056/NEJMra0807633. PMC 2780322. PMID 19797284.
- ^ Kimberlin DW (2007). "Herpes simplex virus infections of the newborn". Semin. Perinatol. 31 (1): 19–25. doi:10.1053/j.semperi.2007.01.003. PMID 17317423.
- ^ a b Mettenleiter TC, Klupp BG, Granzow H (2006). "Herpesvirus assembly: a tale of two membranes". Curr. Opin. Microbiol. 9 (4): 423–9. doi:10.1016/j.mib.2006.06.013. PMID 16814597.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ a b c d McGeoch DJ, Rixon FJ, Davison AJ (2006). "Topics in herpesvirus genomics and evolution". Virus Res. 117 (1): 90–104. doi:10.1016/j.virusres.2006.01.002. PMID 16490275.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Rajcáni J, Andrea V, Ingeborg R (2004). "Peculiarities of herpes simplex virus (HSV) transcription: an overview". Virus Genes. 28 (3): 293–310. doi:10.1023/B:VIRU.0000025777.62826.92. PMID 15266111.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ a b Subramanian RP, Geraghty RJ (2007). "Herpes simplex virus type 1 mediates fusion through a hemifusion intermediate by sequential activity of glycoproteins D, H, L, and B". Proc. Natl. Acad. Sci. U.S.A. 104 (8): 2903–8. doi:10.1073/pnas.0608374104. PMC 1815279. PMID 17299053.
- ^ a b
Cardone G, Winkler DC, Trus BL, Cheng N, Heuser JE, Newcomb WW, Brown JC, Steven AC (2007). "Visualization of the Herpes Simplex Virus Portal in situ by Cryo-electron Tomography". Virology. 361 (2): 426–34. doi:10.1016/j.virol.2006.10.047. PMC 1930166. PMID 17188319.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) Cite error: The named reference "pmid17188319" was defined multiple times with different content (see the help page). - ^ a b Trus BL, Cheng N, Newcomb WW, Homa FL, Brown JC, Steven AC (2004). "Structure and Polymorphism of the UL6 Portal Protein of Herpes Simplex Virus Type 1". Journal of Virology. 78 (22): 12668–71. doi:10.1128/JVI.78.22.12668-12671.2004. PMC 525097. PMID 15507654.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ a b
Nellissery JK, Szczepaniak R, Lamberti C, Weller SK (2007-06-20). "A Putative Leucine Zipper within the Herpes Simplex Virus Type 1 UL6 Protein Is Required for Portal Ring Formation". Journal Virology. 81 (17): 8868–77. doi:10.1128/JVI.00739-07. PMC 1951442. PMID 17581990.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Newcomb WW, Booy FP, Brown JC (2007). "Uncoating the Herpes Simplex Virus Genome". J. Mol. Biol. 370 (4): 633–42. doi:10.1016/j.jmb.2007.05.023. PMC 1975772. PMID 17540405.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Abbas et al (2009) Cellular and Molecular Immunology, Elsevier Inc.
- ^ Adang LA, Parsons CH, Kedes DH (2006). "Asynchronous Progression through the Lytic Cascade and Variations in Intracellular Viral Loads Revealed by High-Throughput Single-Cell Analysis of Kaposi's Sarcoma-Associated Herpesvirus Infection". J. Virol. 80 (20): 10073–82. doi:10.1128/JVI.01156-06. PMC 1617294. PMID 17005685.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ a b Matis J, Kúdelová M (2001). "Early shutoff of host protein synthesis in cells infected with herpes simplex viruses". Acta Virol. 45 (5–6): 269–77. doi:10.2217/fvl.11.24. PMID 12083325.
- ^ Taddeo B, Roizman B (2006). "The Virion Host Shutoff Protein (UL41) of Herpes Simplex Virus 1 Is an Endoribonuclease with a Substrate Specificity Similar to That of RNase A". J. Virol. 80 (18): 9341–5. doi:10.1128/JVI.01008-06. PMC 1563938. PMID 16940547.
- ^ Skepper JN, Whiteley A, Browne H, Minson A (2001). "Herpes Simplex Virus Nucleocapsids Mature to Progeny Virions by an Envelopment → Deenvelopment → Reenvelopment Pathway". J. Virol. 75 (12): 5697–702. doi:10.1128/JVI.75.12.5697-5702.2001. PMC 114284. PMID 11356979.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Granzow H, Klupp BG, Fuchs W, Veits J, Osterrieder N, Mettenleiter TC (2001). "Egress of Alphaherpesviruses: Comparative Ultrastructural Study". J. Virol. 75 (8): 3675–84. doi:10.1128/JVI.75.8.3675-3684.2001. PMC 114859. PMID 11264357.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ a b Pinnoji RC, Bedadala GR, George B, Holland TC, Hill JM, Hsia SC (2007). "Repressor element-1 silencing transcription factor/neuronal restrictive silencer factor (REST/NRSF) can regulate HSV-1 immediate-early transcription via histone modification". Virol. J. 4: 56. doi:10.1186/1743-422X-4-56. PMC 1906746. PMID 17555596.
{{cite journal}}: CS1 maint: multiple names: authors list (link) CS1 maint: unflagged free DOI (link) - ^ Bedadala GR, Pinnoji RC, Hsia SC (2007). "Early growth response gene 1 (Egr-1) regulates HSV-1 ICP4 and ICP22 gene expression". Cell Res. 17 (6): 546–55. doi:10.1038/cr.2007.44. PMID 17502875.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Roizman B, Gu H, Mandel G (2005). "The first 30 minutes in the life of a virus: unREST in the nucleus". Cell Cycle. 4 (8): 1019–21. doi:10.4161/cc.4.8.1902. PMID 16082207.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Wyrwicz LS, Ginalski K, Rychlewski L (2007). "HSV-1 UL45 encodes a carbohydrate binding C-type lectin protein". Cell Cycle. 7 (2): 269–71. doi:10.4161/cc.7.2.5324. PMID 18256535.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Vittone V, Diefenbach E, Triffett D, Douglas MW, Cunningham AL, Diefenbach RJ (2005). "Determination of Interactions between Tegument Proteins of Herpes Simplex Virus Type 1". J. Virol. 79 (15): 9566–71. doi:10.1128/JVI.79.15.9566-9571.2005. PMC 1181608. PMID 16014918.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Smith MC, Boutell C, Davido DJ (2011). "HSV-1 ICP0: paving the way for viral replication". Future Virology. 6 (4): 421–429. doi:10.2217/fvl.11.24. PMID 12083325.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ a b Kolb AW, Ané C, Brandt CR (2013) Using HSV-1 genome phylogenetics to track past human migrations" PLoS One 8(10) e76267. doi:10.1371/journal.pone.0076267
- ^ Bowden R, Sakaoka H, Ward R, Donnelly P (2006) Patterns of Eurasian HSV-1 molecular diversity and inferences of human migrations" Infect Genet Evol 6(1) 63-74
- ^ Kimberlin, M.D., David W (10/6/2011). "Oral Acyclovir Suppression and Neurodevelopment after Neonatal Herpes". New England Journal of Medicine. 365 (14): 1284–1292. doi:10.1056/NEJMoa1003509. Retrieved 5 May 2013.
{{cite journal}}: Check date values in:|date=(help); Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|month=ignored (help)CS1 maint: date and year (link) - ^ Middleton PJ, Petric M, Kozak M, Rewcastle NB, McLachlan DR (1980). "Herpes-simplex viral genome and senile and presenile dementias of Alzheimer and Pick". Lancet. 315 (8176): 1038. doi:10.1016/S0140-6736(80)91490-7. PMID 6103379.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Dobson CB, Itzhaki RF (1999). "Herpes simplex virus type 1 and Alzheimer's disease". Neurobiol. Aging. 20 (4): 457–65. doi:10.1016/S0197-4580(99)00055-X. PMID 10604441.
- ^ Pyles RB (2001). "The association of herpes simplex virus and Alzheimer's disease: a potential synthesis of genetic and environmental factors" (PDF). Herpes. 8 (3): 64–8. PMID 11867022.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Itzhaki RF, Lin WR, Shang D, Wilcock GK, Faragher B, Jamieson GA (1997). "Herpes simplex virus type 1 in brain and risk of Alzheimer's disease". Lancet. 349 (9047): 241–4. doi:10.1016/S0140-6736(96)10149-5. PMID 9014911.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Letenneur, L (2008). "Seropositivity to herpes simplex virus antibodies and risk of Alzheimer's disease: a population-based cohort study". PLoS ONE. 3 (11): e3637. doi:10.1371/journal.pone.0003637. PMC 2572852. PMID 18982063.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help)CS1 maint: unflagged free DOI (link) - ^ Wozniak MA, Frost AL, Preston CM, Itzhaki RF (2011) Antivirals Reduce the Formation of Key Alzheimer's Disease Molecules in Cell Cultures Acutely Infected with Herpes Simplex Virus Type 1" PLoS ONE 6(10) e25152. doi:10.1371/journal.pone.0025152
- ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 18295550, please use {{cite journal}} with
|pmid=18295550instead. - ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 6289091, please use {{cite journal}} with
|pmid=6289091instead. - ^ a b Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 6272987, please use {{cite journal}} with
|pmid=6272987instead. - ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 2541311, please use {{cite journal}} with
|pmid=2541311instead. - ^ a b Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 225021, please use {{cite journal}} with
|pmid=225021instead. - ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 11118355, please use {{cite journal}} with
|pmid=11118355instead. - ^ Varghese, Susan (1 December 2002). "Oncolytic herpes simplex virus vectors for cancer virotherapy". Cancer Gene Therapy. 9 (12): 967–978. doi:10.1038/sj.cgt.7700537. PMID 12522436.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Norgren, R. B., Jr., & Lehman, M. N. (1998). "Herpes simplex virus as a transneuronal tracer. [Review]". Neurosci Biobehav Rev. 22 (6): 695–708. PMID 9809305.
{{cite journal}}: CS1 maint: multiple names: authors list (link)
