Ibuprofen: Difference between revisions
Filling out drugbox fields; PNG->SVG (1st); PNG->GIF (2nd) |
Removing dosing info as per WP:PHARMMOS. Filling out pharmacokinetic drugbox fields. |
||
| Line 22: | Line 22: | ||
<!--Pharmacokinetic data--> |
<!--Pharmacokinetic data--> |
||
| bioavailability = 87-100% (oral), 87% (rectal)<ref name = clinp>{{cite journal|last=Davies|first=NM|title=Clinical pharmacokinetics of ibuprofen. The first 30 years.|journal=Clinical Pharmacokinetics|date=February 1998|volume=34|issue=2|pages=101-54|doi=10.2165/00003088-199834020-00002|pmid=9515184}}</ref> |
|||
| bioavailability = 49–73% |
|||
| protein_bound = |
| protein_bound = 98%<ref name = clinp/> |
||
| metabolism = Hepatic ([[CYP2C9]]) |
| metabolism = Hepatic ([[CYP2C9]])<ref name = clinp/> |
||
| elimination_half-life = 1. |
| elimination_half-life = 1.3-3 hours<ref name = clinp/> |
||
| excretion = Urine (95%)<ref name = clinp/><ref name = TGA>{{cite web|title=PRODUCT INFORMATION BRUFEN® TABLETS AND SYRUP|work=TGA eBusiness Services|publisher=Abbott Australasia Pty Ltd|date=31 July 2012|accessdate=8 May 2014|url=https://www.ebs.tga.gov.au/ebs/picmi/picmirepository.nsf/pdf?OpenAgent&id=CP-2009-PI-00035-3|format=PDF}}</ref> |
|||
| excretion = Renal |
|||
<!--Identifiers--> |
<!--Identifiers--> |
||
| Line 74: | Line 74: | ||
==Medical uses== |
==Medical uses== |
||
Ibuprofen is used primarily for [[fever]], [[pain]], [[dysmenorrhea|painful periods]] and inflammatory diseases such as [[osteoarthritis]] and [[rheumatoid arthritis]].<ref>http://www.rxwiki.com/ibuprofen</ref><ref name=AHFS/> It is also used for [[pericarditis]] and [[patent ductus arteriosus]].<ref name="AHFS"/> |
Ibuprofen is used primarily for [[fever]], [[pain]], [[dysmenorrhea|painful periods]] and inflammatory diseases such as [[osteoarthritis]] and [[rheumatoid arthritis]].<ref>http://www.rxwiki.com/ibuprofen</ref><ref name=AHFS/> It is also used for [[pericarditis]] and [[patent ductus arteriosus]].<ref name="AHFS"/> |
||
===Dosage=== |
|||
Ibuprofen has a dose-dependent duration of action of around four to eight hours, which is longer than suggested by its short [[Biological half-life|half-life]]. A study concluded that the time to onset of analgesia (time to effect) is about 24.2 minutes using 400 mg of liquigel orally.<ref>http://www.ncbi.nlm.nih.gov/pubmed/11697757</ref> The recommended dose varies with body mass and indication. A dose of 200 mg per dose and 1200 mg per day is considered the maximum amount for over-the-counter use,{{Citation needed|reason=See dosage discussion on talk page|date=March 2014}} and a dose of 800 mg per dose and 3200 mg per day is considered the maximum amount for prescription use under a doctor's supervision.{{Citation needed|reason=See dosage discussion on talk page|date=March 2014}} Unlike aspirin, which breaks down in solution, ibuprofen is stable, thus it can be available in [[topical]] gel form, which is absorbed through the skin, and can be used for sports injuries, with less risk of digestive problems.<ref name=topical/> |
|||
===Ibuprofen lysine=== |
===Ibuprofen lysine=== |
||
| Line 87: | Line 84: | ||
==Adverse effects== |
==Adverse effects== |
||
Common adverse effects include: [[nausea]], [[dyspepsia]], gastrointestinal ulceration/bleeding, raised [[Liver function tests|liver enzymes]], [[diarrhea]], [[constipation]], [[nosebleed]], [[headache]], [[dizziness]], rash, salt and fluid retention, and [[hypertension]].<ref name="AMH2004-Rossi"/>{{ |
Common adverse effects include: [[nausea]], [[dyspepsia]], gastrointestinal ulceration/bleeding, raised [[Liver function tests|liver enzymes]], [[diarrhea]], [[constipation]], [[nosebleed]], [[headache]], [[dizziness]], rash, salt and fluid retention, and [[hypertension]].<ref name="AMH2004-Rossi"/> A study from 2010 has shown regular use of NSAIDs was associated with an increase in hearing loss.<ref>{{cite pmid | 20193831 }}</ref> |
||
A study from 2010 has shown regular use of NSAIDs was associated with an increase in hearing loss.<ref>{{cite pmid | 20193831 }}</ref> |
|||
Infrequent adverse effects include: esophageal ulceration, [[Congestive heart failure|heart failure]], [[hyperkalemia]], [[Renal failure|renal impairment]], confusion, and [[bronchospasm]].<ref name="AMH2004-Rossi"/> Ibuprofen can exacerbate asthma, sometimes fatally.<ref name="Lancet1987-Ayres"/> |
Infrequent adverse effects include: esophageal ulceration, [[Congestive heart failure|heart failure]], [[hyperkalemia]], [[Renal failure|renal impairment]], confusion, and [[bronchospasm]].<ref name="AMH2004-Rossi"/> Ibuprofen can exacerbate asthma, sometimes fatally.<ref name="Lancet1987-Ayres"/> |
||
Ibuprofen appears to have the lowest incidence of digestive [[adverse drug reaction]]s of all the nonselective NSAIDs.{{citation needed|date=February 2014}} However, this holds true only at lower doses of ibuprofen, so over-the-counter (OTC) preparations of ibuprofen are, in general, labeled to advise a maximum daily dose of 1,200 mg.<ref name=otcusa/> |
|||
Ibuprofen may be quantitated in blood, plasma, or serum to demonstrate the presence of the drug in a person having experienced an anaphylactic reaction, confirm a diagnosis of poisoning in hospitalized patients, or assist in a medicolegal death investigation. A nomogram relating ibuprofen plasma concentration, time since ingestion, and risk of developing renal toxicity in overdose patients has been published.<ref name=Baselt/> |
Ibuprofen may be quantitated in blood, plasma, or serum to demonstrate the presence of the drug in a person having experienced an anaphylactic reaction, confirm a diagnosis of poisoning in hospitalized patients, or assist in a medicolegal death investigation. A nomogram relating ibuprofen plasma concentration, time since ingestion, and risk of developing renal toxicity in overdose patients has been published.<ref name=Baselt/> |
||
===Cardiovascular risk=== |
===Cardiovascular risk=== |
||
Along with several other NSAIDs, chronic ibuprofen use has been found correlated with risk of [[hypertension]]<ref>{{cite pmid | 16103274 }}</ref> and [[myocardial infarction]] (heart attack),<ref>{{cite pmid | 15947398 }}</ref> particularly among those chronically using high doses. In older |
Along with several other NSAIDs, chronic ibuprofen use has been found correlated with risk of [[hypertension]]<ref>{{cite pmid | 16103274 }}</ref> and [[myocardial infarction]] (heart attack),<ref>{{cite pmid | 15947398 }}</ref> particularly among those chronically using high doses. In older hypertensive patients treated with [[hydrochlorothiazide]], ibuprofen in doses of 1800 mg per day was found to significantly increase systolic blood pressure.<ref>{{cite pmid | 8612107}}</ref> |
||
hypertensive patients treated with [[hydrochlorothiazide]], ibuprofen in doses of 1800 mg per day was found to significantly increase systolic blood pressure.<ref>{{cite pmid | 8612107}}</ref> |
|||
===Increased risk of kidney cancer=== |
===Increased risk of kidney cancer=== |
||
| Line 110: | Line 103: | ||
Drinking alcohol when taking ibuprofen may increase risk of stomach bleeding.<ref name=drugs/> |
Drinking alcohol when taking ibuprofen may increase risk of stomach bleeding.<ref name=drugs/> |
||
According to the [[Food and Drug Administration (United States)|US Food and Drug Administration]], "ibuprofen can interfere with the anti[[platelet]] effect of low-dose [[aspirin]] |
According to the [[Food and Drug Administration (United States)|US Food and Drug Administration]], "ibuprofen can interfere with the anti[[platelet]] effect of low-dose [[aspirin]], potentially rendering aspirin less effective when used for cardioprotection and [[stroke]] prevention." Allowing sufficient time between doses of ibuprofen and immediate-release (IR) aspirin can avoid this problem. The recommended elapsed time between a 400-mg dose of ibuprofen and a dose of aspirin depends on which is taken first. It would be 30 minutes or more for ibuprofen taken after IR aspirin, and 8 hours or more for ibuprofen taken before IR aspirin. However, this timing cannot be recommended for [[Enteric coating|enteric-coated]] aspirin. But, if ibuprofen is taken only occasionally without the recommended timing, the reduction of the cardioprotection and stroke prevention of a daily aspirin regimen is minimal.<ref name="FDA2006"/> |
||
===Erectile dysfunction risk=== |
===Erectile dysfunction risk=== |
||
Revision as of 03:44, 8 May 2014
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Advil, Brufen, Motrin, Nurofen, and others |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a682159 |
| License data | |
| Pregnancy category |
|
| Routes of administration | Oral, rectal, topical, and intravenous |
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Bioavailability | 87-100% (oral), 87% (rectal)[2] |
| Protein binding | 98%[2] |
| Metabolism | Hepatic (CYP2C9)[2] |
| Elimination half-life | 1.3-3 hours[2] |
| Excretion | Urine (95%)[2][3] |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| PDB ligand | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.036.152 |
| Chemical and physical data | |
| Formula | C13H18O2 |
| Molar mass | 206.29 g/mol g·mol−1 |
| 3D model (JSmol) | |
| Density | 1.03 gr/ml g/cm3 |
| Melting point | 76 °C (169 °F) |
| |
| |
| (verify) | |

Ibuprofen (INN) (/ˈaɪbjuːproʊfɛn/ or /aɪbjuːˈproʊfən/ EYE-bew-PROH-fən; from isobutylphenylpropanoic acid) is a nonsteroidal anti-inflammatory drug (NSAID) used for relieving pain, helping with fever,[4] and reducing inflammation.
Ibuprofen has an antiplatelet effect, though it is relatively mild and somewhat short-lived compared with aspirin or prescription antiplatelet drugs. In general, ibuprofen also has a vasodilation effect.[5]
Ibuprofen was derived from propanoic acid by the research arm of Boots Company during the 1960s[6] and patented in 1961. Originally marketed as Brufen, ibuprofen is available under a variety of popular trademarks, including Motrin, Nurofen, Advil, Nuprin and many others.[7] Generic formulations are available as well. It is on the World Health Organization's List of Essential Medicines, a list of the most important medication needed in a basic health system.[8]
Medical uses
Ibuprofen is used primarily for fever, pain, painful periods and inflammatory diseases such as osteoarthritis and rheumatoid arthritis.[9][10] It is also used for pericarditis and patent ductus arteriosus.[10]
Ibuprofen lysine
In Europe, Australia, and New Zealand, ibuprofen lysine (the lysine salt of ibuprofen, sometimes called "ibuprofen lysinate" even though the lysine is in cationic form) is licensed for treatment of the same conditions as ibuprofen. The lysine salt increases water solubility, allowing intravenous use, and is indicated for closure of a patent ductus arteriosus in premature infants weighing between 500 and 1,500 grams (1 and 3 lb), who are no more than 32 weeks gestational age when usual medical management (e.g., fluid restriction, diuretics, respiratory support, etc.) is ineffective.[11]
With regard to this indication, ibuprofen lysine is an effective alternative to intravenous indomethacin, and may be advantageous in terms of kidney function.[12] Ibuprofen lysine has been shown to have a more rapid onset of action compared to acid ibuprofen.[13]
In UK Ibuprofen Lysine is marketed as express pain relief, tension headache relief and more commonly migraine relief medicine. Usually available in packing of 16 342 mg tablets the pack is marketed OTC by most superstores and pharmacies as their own branded product including, but not limited to, Asda, Tesco and Superdrug.[14]
Adverse effects
Common adverse effects include: nausea, dyspepsia, gastrointestinal ulceration/bleeding, raised liver enzymes, diarrhea, constipation, nosebleed, headache, dizziness, rash, salt and fluid retention, and hypertension.[15] A study from 2010 has shown regular use of NSAIDs was associated with an increase in hearing loss.[16]
Infrequent adverse effects include: esophageal ulceration, heart failure, hyperkalemia, renal impairment, confusion, and bronchospasm.[15] Ibuprofen can exacerbate asthma, sometimes fatally.[17]
Ibuprofen may be quantitated in blood, plasma, or serum to demonstrate the presence of the drug in a person having experienced an anaphylactic reaction, confirm a diagnosis of poisoning in hospitalized patients, or assist in a medicolegal death investigation. A nomogram relating ibuprofen plasma concentration, time since ingestion, and risk of developing renal toxicity in overdose patients has been published.[18]
Cardiovascular risk
Along with several other NSAIDs, chronic ibuprofen use has been found correlated with risk of hypertension[19] and myocardial infarction (heart attack),[20] particularly among those chronically using high doses. In older hypertensive patients treated with hydrochlorothiazide, ibuprofen in doses of 1800 mg per day was found to significantly increase systolic blood pressure.[21]
Increased risk of kidney cancer
A 2011 study in the Archives of Internal Medicine reported a 51% increase in the rate of renal cell carcinoma, the most common form of kidney cancer, in nurses who regularly took ibuprofen and other NSAIDs, such as naproxen.[22]
Skin
Along with other NSAIDs, ibuprofen has been associated with the onset of bullous pemphigoid or pemphigoid-like blistering.[23] As with other NSAIDs, ibuprofen has been reported to be a photosensitising agent,[24] but it is considered a weak photosensitising agent compared to other members of the 2-arylpropionic acid class. Like other NSAIDs, ibuprofen is an extremely rare cause of the autoimmune disease Stevens-Johnson syndrome (SJS).[25][26]
Interactions
Drinking alcohol when taking ibuprofen may increase risk of stomach bleeding.[27]
According to the US Food and Drug Administration, "ibuprofen can interfere with the antiplatelet effect of low-dose aspirin, potentially rendering aspirin less effective when used for cardioprotection and stroke prevention." Allowing sufficient time between doses of ibuprofen and immediate-release (IR) aspirin can avoid this problem. The recommended elapsed time between a 400-mg dose of ibuprofen and a dose of aspirin depends on which is taken first. It would be 30 minutes or more for ibuprofen taken after IR aspirin, and 8 hours or more for ibuprofen taken before IR aspirin. However, this timing cannot be recommended for enteric-coated aspirin. But, if ibuprofen is taken only occasionally without the recommended timing, the reduction of the cardioprotection and stroke prevention of a daily aspirin regimen is minimal.[28]
Erectile dysfunction risk
A 2005 study linked long-term (over three months) use of NSAIDs, including ibuprofen, with a 140% higher risk of erectile dysfunction.[29][30] The study, conducted at Kaiser Permanente and published in the Journal of Urology, reported, "regular nonsteroidal anti-inflammatory drug use is associated with erectile dysfunction beyond what would be expected due to age and other conditions".[31] The director of research for Kaiser Permanente added, "There are many proven benefits of nonsteroidals in preventing heart disease and for other conditions. People shouldn't stop taking them based on this observational study. However, if a man is taking this class of drugs and has ED, it's worth a discussion with his doctor".[30]
Overdose
Ibuprofen overdose has become common since it was licensed for OTC use. Many overdose experiences are reported in the medical literature, although the frequency of life-threatening complications from ibuprofen overdose is low.[32] Human response in cases of overdose ranges from absence of symptoms to fatal outcome despite intensive-care treatment. Most symptoms are an excess of the pharmacological action of ibuprofen, and include abdominal pain, nausea, vomiting, drowsiness, dizziness, headache, tinnitus, and nystagmus. Rarely, more severe symptoms, such as gastrointestinal bleeding, seizures, metabolic acidosis, hyperkalaemia, hypotension, bradycardia, tachycardia, atrial fibrillation, coma, hepatic dysfunction, acute renal failure, cyanosis, respiratory depression, and cardiac arrest have been reported.[33] The severity of symptoms varies with the ingested dose and the time elapsed; however, individual sensitivity also plays an important role. Generally, the symptoms observed with an overdose of ibuprofen are similar to the symptoms caused by overdoses of other NSAIDs.
Correlation between severity of symptoms and measured ibuprofen plasma levels is weak. Toxic effects are unlikely at doses below 100 mg/kg, but can be severe above 400 mg/kg (around 150 tablets of 200 mg units for an average man);[34] however, large doses do not indicate the clinical course is likely to be lethal.[35] A precise lethal dose is difficult to determine, as it may vary with age, weight, and concomitant diseases of the individual patient.
Therapy is largely symptomatic. In cases presenting early, gastric decontamination is recommended. This is achieved using activated charcoal; charcoal adsorbs the drug before it can enter the systemic circulation. Gastric lavage is now rarely used, but can be considered if the amount ingested is potentially life-threatening, and it can be performed within 60 minutes of ingestion. Emesis is not recommended.[36] The majority of ibuprofen ingestions produce only mild effects and the management of overdose is straightforward. Standard measures to maintain normal urine output should be instituted and renal function monitored.[34] Since ibuprofen has acidic properties and is also excreted in the urine, forced alkaline diuresis is theoretically beneficial. However, because ibuprofen is highly protein-bound in the blood, renal excretion of unchanged drug is minimal. Forced alkaline diuresis is, therefore, of limited benefit.[37] Symptomatic therapy for hypotension, gastrointestinal bleeding, acidosis, and renal toxicity may be indicated. On occasion, close monitoring in an intensive-care unit for several days is necessary. A patient who survives the acute intoxication usually experiences no late sequelae.
Miscarriage
A Canadian study published in the Canadian Medical Association Journal of thousands of pregnant woman suggests those taking any type or amount of NSAIDs (including ibuprofen, diclofenac and naproxen) were 2.4 times more likely to miscarry than those not taking the drugs.[38] However, an Israeli study following thousands of women found no increased risk of miscarriage in the group of mothers using NSAIDs.[39]
Rhabdomyolysis
In a study by eHealthMe, Ibuprofen has been associated also with the development of rhabdomyolysis, especially in people with high blood cholesterol, hyperlipidaemia, high blood pressure, and depression.[40]
Mechanism of action
Nonsteroidal anti-inflammatory drugs such as ibuprofen work by inhibiting the enzyme cyclooxygenase (COX), which converts arachidonic acid to prostaglandin H2 (PGH2). PGH2, in turn, is converted by other enzymes to several other prostaglandins (which are mediators of pain, inflammation, and fever) and to thromboxane A2 (which stimulates platelet aggregation, leading to the formation of blood clots).
Like aspirin and indomethacin,[citation needed] ibuprofen is a nonselective COX inhibitor, in that it inhibits two isoforms of cyclooxygenase, COX-1 and COX-2. The analgesic, antipyretic, and anti-inflammatory activity of NSAIDs appears to operate mainly through inhibition of COX-2, whereas inhibition of COX-1 would be responsible for unwanted effects on the gastrointestinal tract.[41] However, the role of the individual COX isoforms in the analgesic, anti-inflammatory, and gastric damage effects of NSAIDs is uncertain and different compounds cause different degrees of analgesia and gastric damage.[42]
To achieve the beneficial effects of ibuprofen and other NSAIDs without gastrointestinal ulceration and bleeding, selective COX-2 inhibitors were developed to inhibit the COX-2 isoform without inhibition of COX-1.[43]
Chemistry
Ibuprofen is only very slightly soluble in water. Less than 1 mg of ibuprofen dissolves in 1 ml water (< 1 mg/ml).[44]
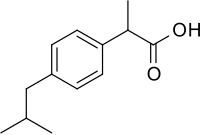
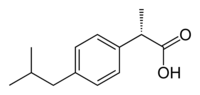
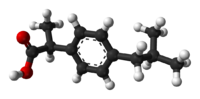
Stereochemistry
Ibuprofen is produced industrially as a racemate. The compound, like other 2-arylpropionate derivatives (including ketoprofen, flurbiprofen, naproxen, etc.), does contain a chiral center in the α-position of the propionate moiety. So two enantiomers of ibuprofen occur, with the potential for different biological effects and metabolism for each enantiomer. Indeed, the (S)-(+)-ibuprofen (dexibuprofen) was found to be the active form both in vitro and in vivo.
It was logical, then, to consider the potential for improving the selectivity and potency of ibuprofen formulations by marketing ibuprofen as a single-enantiomer product (as occurs with naproxen, another NSAID). Further in vivo testing, however, revealed the existence of an isomerase (alpha-methylacyl-CoA racemase), which converted (R)-ibuprofen to the active (S)-enantiomer.[45][46][47]
 |
 |
 |
 |
 |
 |
Synthesis
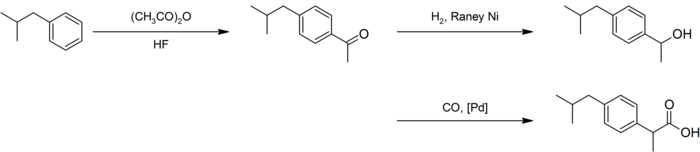
The synthesis of this compound is a popular case study in green chemistry. The original Boots synthesis of ibuprofen consisted of six steps, started with the Friedel-Crafts acetylation of isobutylbenzene. Reaction with ethyl chloroacetate (Darzens reaction) gave the α,β-epoxy ester, which was hydrolyzed and decarboxylated to the aldehyde. Reaction with hydroxylamine gave the oxime, which was converted to the nitrile, then hydrolyzed to the desired acid:[48][49]
An improved synthesis by BHC required only three steps. This improved synthesis won the Presidential Green Chemistry Challenge Greener Synthetic Pathways Award in 1997.[50]
After a similar acetylation, hydrogenation with Raney nickel gave the alcohol, which underwent palladium-catalyzed carbonylation:[48][51]
History
Ibuprofen was derived from propionic acid by the research arm of Boots Group during the 1960s.[6] It was discovered by Andrew RM Dunlop, with colleagues Stewart Adams, John Nicholson, Vonleigh Simmons, Jeff Wilson and Colin Burrows, and patented in 1961. The drug was launched as a treatment for rheumatoid arthritis in the United Kingdom in 1969, and in the United States in 1974. Adams initially tested his drug on a hangover.[52] He was subsequently awarded an OBE in 1987. Boots was awarded the Queen's Award for Technical Achievement for the development of the drug in 1987.[52]
Availability

Ibuprofen was made available under prescription in the United Kingdom in 1969, and in the United States in 1974.[53] In the years since, the good tolerability profile, along with extensive experience in the population, as well as in so-called phase IV trials (post-approval studies), has resulted in the availability of ibuprofen over the counter (OTC) in pharmacies worldwide, as well as in supermarkets and other general retailers.[citation needed]
North America
Ibuprofen is commonly available in the United States up to the FDA's 200 mg 1984 dose limit OTC, rarely used higher by prescription.[54]
In Canada, the OTC dose limit is 400 mg, with 600 mg and 800 mg routinely available by prescription.[citation needed]
In 2009, the first injectable formulation of ibuprofen was approved in the United States, under the trade name Caldolor.[55][56] Ibuprofen was the only parenteral for both pain and fever available in the country prior to the approval of Ofirmev (acetaminophen) injection by the FDA.[57]
Research
Ibuprofen is sometimes used for the treatment of acne, because of its anti-inflammatory properties,[58] and has been sold in Japan in topical form for adult acne.[59] As with other NSAIDs, ibuprofen may be useful in the treatment of severe orthostatic hypotension (low blood pressure when standing up).[60] In some studies, ibuprofen showed superior results compared to a placebo in the prophylaxis of Alzheimer's disease, when given in low doses over a long time.[61][62] Some of the aforementioned uses would be considered off-label uses in some countries.
Ibuprofen has been associated with a lower risk of Parkinson's disease, and may delay or prevent it. Aspirin, other NSAIDs, and paracetamol (acetaminophen) had no effect on the risk for Parkinson's.[63] In March 2011, researchers at Harvard Medical School announced in Neurology that ibuprofen had a neuroprotective effect against the risk of developing Parkinson's disease.[64][65][66] People regularly consuming ibuprofen were reported to have a 38% lower risk of developing Parkinson's disease, but no such effect was found for other pain relievers, such as aspirin and paracetamol. Use of ibuprofen to lower the risk of Parkinson's disease in the general population would not be problem-free, given the possibility of adverse effects on the urinary and digestive systems.[67]
References
- ^ "FDA-sourced list of all drugs with black box warnings (Use Download Full Results and View Query links.)". nctr-crs.fda.gov. FDA. Retrieved 22 Oct 2023.
- ^ a b c d e Davies, NM (February 1998). "Clinical pharmacokinetics of ibuprofen. The first 30 years". Clinical Pharmacokinetics. 34 (2): 101–54. doi:10.2165/00003088-199834020-00002. PMID 9515184.
- ^ "PRODUCT INFORMATION BRUFEN® TABLETS AND SYRUP" (PDF). TGA eBusiness Services. Abbott Australasia Pty Ltd. 31 July 2012. Retrieved 8 May 2014.
- ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 7767417 , please use {{cite journal}} with
|pmid= 7767417instead. - ^
Apstein CS,Vogel MM (January 22, 1982). "Coronary arterial vasodilator effect of ibuprofen". PMID 7053413.
{{cite journal}}: Cite journal requires|journal=(help) - ^ a b Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 1569234 , please use {{cite journal}} with
|pmid= 1569234instead. - ^ "PubMed Health - Ibuprofen". U.S. National Library of Medicine. 2010-10-01. Retrieved 2011-01-20.
- ^ "WHO Model List of EssentialMedicines" (PDF). World Health Organization. October 2013. Retrieved 22 April 2014.
- ^ http://www.rxwiki.com/ibuprofen
- ^ a b "Ibuprofen". The American Society of Health-System Pharmacists. Retrieved 3 April 2011.
- ^ "Neoprofen (ibuprofen lysine) injection. Package insert" (PDF). Ovation Pharmaceuticals.
- ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 14651538 , please use {{cite journal}} with
|pmid= 14651538instead. - ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 2777420 , please use {{cite journal}} with
|pmid= 2777420instead. - ^ [1]
- ^ a b Rossi, S., ed. (2004). Australian Medicines Handbook (2004 ed.). Australian Medicines Handbook. ISBN 0-9578521-4-2. OCLC 224121065.
- ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 20193831 , please use {{cite journal}} with
|pmid= 20193831instead. - ^
Ayres, JG, Fleming D, Whittington R. (1987). "Asthma death due to ibuprofen". Lancet.
{{cite web}}: CS1 maint: multiple names: authors list (link) - ^ Baselt, R. (2008). Disposition of Toxic Drugs and Chemicals in Man (8th ed.). Foster City, CA: Biomedical Publications. pp. 758–761.
- ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 16103274 , please use {{cite journal}} with
|pmid= 16103274instead. - ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 15947398 , please use {{cite journal}} with
|pmid= 15947398instead. - ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 8612107, please use {{cite journal}} with
|pmid= 8612107instead. - ^ Cortez, Michelle (September 12, 2011). "Commonly Used Pain Pills Increase Kidney Cancer Risk in Study". Bloomberg.
- ^ Chan, L. S. (2011). "Bullous Pemphigoid". eMedicine Reference. Medscape.
- ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 1531054 , please use {{cite journal}} with
|pmid= 1531054instead. - ^ Raksha MP, Marfatia YS (2008). "Clinical study of cutaneous drug eruptions in 200 patients". Indian J Dermatol Venereol Leprol. 74 (1): 80. doi:10.4103/0378-6323.38431. PMID 18193504.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 20101062, please use {{cite journal}} with
|pmid=20101062instead. - ^ "Ibuprofen". Drugs.com.
- ^ "Information for Healthcare Professionals: Concomitant Use of Ibuprofen and Aspirin". U.S. Food and Drug Administration (FDA). September 2006. Retrieved 2010-11-22.
- ^
Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 16600768 , please use {{cite journal}} with
|pmid= 16600768instead. - ^ a b "Non-steroidal anti-inflammatory drugs linked to increased risk of erectile dysfunction". sciencedaily.com. 2011-03-02. Retrieved 2011-06-07.
- ^ Mary Brophy Marcus (March 2011). "New study links pain relievers to erectile dysfunction". USA Today.
- ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 2188537 , please use {{cite journal}} with
|pmid= 2188537instead. - ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 3537613 , please use {{cite journal}} with
|pmid= 3537613instead. - ^ a b Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 12737366 , please use {{cite journal}} with
|pmid= 12737366instead. - ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 10696926 , please use {{cite journal}} with
|pmid= 10696926instead. - ^
Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 15214617 , please use {{cite journal}} with
|pmid= 15214617instead. - ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 3777588 , please use {{cite journal}} with
|pmid= 3777588instead. - ^ "Miscarriage risk doubled: drug study". theage.com.au. 2011-09-07. Retrieved 2011-09-07.
- ^ Sharon Daniel, Gideon Koren, Eitan Lunenfeld, Natalya Bilenko, Ronit Ratzon, Amalia Levy (2014). "Fetal exposure to nonsteroidal anti-inflammatory drugs and spontaneous abortions" Canadian Medical Association Journal
- ^ http://www.ehealthme.com/ds/ibuprofen/rhabdomyolysis
- ^
Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 19203472 , please use {{cite journal}} with
|pmid= 19203472instead. - ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 18363350 , please use {{cite journal}} with
|pmid= 18363350instead. - ^ "Pain Medications". eMedicine. 2006-02-13. Retrieved 2010-06-07.
- ^ Motrin (Ibuprofen) drug description - FDA-approved labeling for prescription drugs and medications at RxList
- ^
Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 1859831 , please use {{cite journal}} with
|pmid= 1859831instead. - ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 1352228 , please use {{cite journal}} with
|pmid= 1352228instead. - ^
Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 9106621 , please use {{cite journal}} with
|pmid= 9106621instead. - ^ a b "Ibuprofen — a case study in green chemistry" (pdf). Royal Society of Chemistry.
- ^ US patent 3385886, Stuart, N. J. & Sanders, A. S., issued 1968-05-28, assigned to Boots Pure Drug Company
- ^ "Presidential Green Chemistry Challenge: 1997 Greener Synthetic Pathways Award". United States EPA. Retrieved 2009-08-18.
- ^ Attention: This template ({{cite doi}}) is deprecated. To cite the publication identified by doi: 10.1021/ed100892p , please use {{cite journal}} (if it was published in a bona fide academic journal, otherwise {{cite report}} with
|doi= 10.1021/ed100892pinstead. - ^ a b Lambert, Victoria (2007-10-08). "Dr. Stewart Adams: 'I tested ibuprofen on my hangover'". The Daily Telegraph. London. Retrieved 2008-01-20.
- ^ "Written submission to the NDAC meeting on risks of NSAIDs presented by the International Ibuprofen Foundation". International Ibuprofen Foundation. August 2002. Retrieved 20 March 2014.
- ^ "Ibuprofen". U.S. Food and Drug Administration (FDA).
- ^ "Drug Approval Package: Caldolor (Ibuprofen) NDA #022348". U.S. Food and Drug Administration (FDA). March 11, 2010.
- ^ "FDA Approves Injectable Form of Ibuprofen" (Press release). U.S. Food and Drug Administration (FDA). June 11, 2009.
- ^ "FDA Approves Caldolor: Cumberland Pharmaceuticals Announces FDA Approval of Caldolor" (Press release). Drugs.com. June 11, 2009. Retrieved 2009-06-13.
- ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 6239884 , please use {{cite journal}} with
|pmid= 6239884instead. - ^ "In Japan, an OTC ibuprofen ointment (Fukidia) for alleviating adult acne has been launched". Inpharma. 1 (1530). Adis: 18. March 25, 2006. ISSN 1173-8324.
- ^
Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 7041104 , please use {{cite journal}} with
|pmid= 7041104instead. - ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 16195368 , please use {{cite journal}} with
|pmid= 16195368instead. - ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 18458226 , please use {{cite journal}} with
|pmid= 18458226instead. - ^
Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 16240369 , please use {{cite journal}} with
|pmid= 16240369instead. - ^
Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 21368281 , please use {{cite journal}} with
|pmid= 21368281instead. - ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 21555992 , please use {{cite journal}} with
|pmid= 21555992instead. - ^
Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 21368280 , please use {{cite journal}} with
|pmid= 21368280instead. - ^ Mary Brophy Marcus (March 2, 2011). "Ibuprofen may reduce risk of getting Parkinson's disease". USA Today.
Cite error: A list-defined reference named "essentialWHO" is not used in the content (see the help page).
Cite error: A list-defined reference named "WHOchild" is not used in the content (see the help page).
Cite error: A list-defined reference named "WHOmod" is not used in the content (see the help page).
Cite error: A list-defined reference named "WHOmodchild" is not used in the content (see the help page).