DDT

| |
| |
| |
| Names | |
|---|---|
| IUPAC name
1,1,1-trichloro-2,2-di(4-chlorophenyl)ethane
| |
| Identifiers | |
3D model (JSmol)
|
|
| ChEBI | |
| ChEMBL | |
| ChemSpider | |
| ECHA InfoCard | 100.000.023 |
| KEGG | |
PubChem CID
|
|
| UNII | |
CompTox Dashboard (EPA)
|
|
| |
| |
| Properties | |
| C 14H 9Cl 5 | |
| Molar mass | 354.49 g/mol |
| Density | 0.99 g/cm³[1] |
| Melting point | 108.5 °C |
| Boiling point | 260 °C (decomp.) |
| Hazards | |
| Occupational safety and health (OHS/OSH): | |
Main hazards
|
T, N |
| Lethal dose or concentration (LD, LC): | |
LD50 (median dose)
|
113 mg/kg (rat) |
Except where otherwise noted, data are given for materials in their standard state (at 25 °C [77 °F], 100 kPa).
| |
DDT (dichlorodiphenyltrichloroethane) is an organochlorine insecticide which is a white, crystalline solid, tasteless and almost odorless chemical compound. Technical DDT has been formulated in almost every conceivable form including solutions in xylene or petroleum distillates, emulsifiable concentrates, water-wettable powders, granules, aerosols, smoke candles, and charges for vaporisers and lotions.[2]
First synthesized in 1874, DDT's insecticidal properties were not discovered until 1939, and it was used with great success in the second half of World War II to control malaria and typhus among civilians and troops. The Swiss chemist Paul Hermann Müller was awarded the Nobel Prize in Physiology or Medicine in 1948 "for his discovery of the high efficiency of DDT as a contact poison against several arthropods."[3] After the war, DDT was made available for use as an agricultural insecticide, and soon its production and use skyrocketed.[4]
In 1962, Silent Spring by American biologist Rachel Carson was published. The book catalogued the environmental impacts of the indiscriminate spraying of DDT in the US and questioned the logic of releasing large amounts of chemicals into the environment without fully understanding their effects on ecology or human health. The book suggested that DDT and other pesticides may cause cancer[citation needed] and that their agricultural use was a threat to wildlife, particularly birds. Its publication was one of the signature events in the birth of the environmental movement, and resulted in a large public outcry that eventually led to DDT being banned in the US in 1972.[5] DDT was subsequently banned for agricultural use worldwide under the Stockholm Convention, but its limited use in disease vector control continues to this day and remains controversial.[6][7]
Along with the passage of the Endangered Species Act, the US ban on DDT is cited by scientists as a major factor in the comeback of the bald eagle, the national bird of the United States, from near-extinction in the contiguous US.[8]
Properties and chemistry
DDT is similar in structure to the insecticide methoxychlor and the acaricide dicofol. It is highly hydrophobic, nearly insoluble in water but has a good solubility in most organic solvents, fats, and oils. DDT does not occur naturally, but is produced by the reaction of chloral (CCl
3CHO) with chlorobenzene (C
6H
5Cl) in the presence of sulfuric acid, which acts as a catalyst. Trade names that DDT has been marketed under include Anofex (Geigy Chemical Corp.), Cezarex, Chlorophenothane, Clofenotane, Dicophane, Dinocide, Gesarol (Syngenta Crop.), Guesapon, Guesarol, Gyron (Ciba-Geigy Corp. - now Novartis), Ixodex, Neocid (Reckitt & Colman, Ltd), Neocidol (Ciba-Geigy Corp. - now Novartis), and Zerdane.[4]
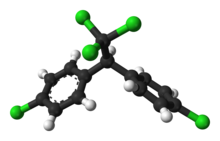
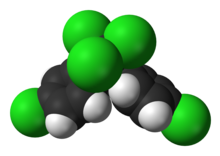
Isomers and related compounds

Commercial DDT is a mixture of several closely–related compounds. The major component (77%) is the p,p' isomer which is pictured at the top of this article. The o,p' isomer (pictured to the right) is also present in significant amounts (15%). Dichlorodiphenyldichloroethylene (DDE) and dichlorodiphenyldichloroethane (DDD) make up the balance. DDE and DDD are also the major metabolites and breakdown products in the environment.[4] The term "total DDT" is often used to refer to the sum of all DDT related compounds (p,p'-DDT, o,p'-DDT, DDE, and DDD) in a sample.
Production and use statistics
From 1950 to 1980, DDT was extensively used in agriculture—more than 40,000 tonnes were used each year worldwide[9]—and it has been estimated that a total of 1.8 million tonnes have been produced globally since the 1940s.[1] In the U.S., where it was manufactured by Ciba,[10] Montrose Chemical Company, Pennwalt[11] and Velsicol Chemical Corporation,[12] production peaked in 1963 at 82,000 tonnes per year.[4] More than 600,000 tonnes (1.35 billion lbs) were applied in the U.S. before the 1972 ban. Usage peaked in 1959 at about 36,000 tonnes.[13]
In 2009, 3314 tonnes were produced for the control of malaria and visceral leishmaniasis. India is the only country still manufacturing DDT, with China having ceased production in 2007.[14] India is the largest consumer.[15]
Mechanism of insecticide action
In insects it opens sodium ion channels in neurons, causing them to fire spontaneously, which leads to spasms and eventual death. Insects with certain mutations in their sodium channel gene are resistant to DDT and other similar insecticides. DDT resistance is also conferred by up-regulation of genes expressing cytochrome P450 in some insect species.[16]
In humans, however, it may affect health through genotoxicity or endocrine disruption. See Effects on human health.
History


DDT was first synthesized in 1874 by Othmar Zeidler under the supervision of Adolf von Baeyer.[4] [17] It was further described in 1929 in a dissertation by W. Bausch and in two subsequent publications in 1930[18][19]. The insecticide properties of "mutliple chlorinated aliphatic or fat-aromatic alcohols with at least one trichloromethane group" were described in a patent in 1934 by Wolfgang von Leuthold.[20] But DDT's insecticidal properties were not discovered until 1939 by the Swiss scientist Paul Hermann Müller, who was awarded the 1948 Nobel Prize in Physiology and Medicine for his efforts.[3]
Use in the 1940s and 1950s
DDT is the best-known of several chlorine-containing pesticides used in the 1940s and 1950s. With pyrethrum in short supply, DDT was used extensively during World War II by the Allies to control the insect vectors of typhus — nearly eliminating the disease in many parts of Europe. In the South Pacific, it was sprayed aerially for malaria and dengue fever control with spectacular effects. While DDT's chemical and insecticidal properties were important factors in these victories, advances in application equipment coupled with a high degree of organization and sufficient manpower were also crucial to the success of these programs.[21] In 1945, it was made available to farmers as an agricultural insecticide,[4] and it played a minor role in the final elimination of malaria in Europe and North America.[6] By the time DDT was introduced in the U.S., the disease had already been brought under control by a variety of other means.[22] One CDC physician involved in the United States' DDT spraying campaign said of the effort that "we kicked a dying dog."[23]
In 1955, the World Health Organization commenced a program to eradicate malaria worldwide, relying largely on DDT. The program was initially highly successful, eliminating the disease in "Taiwan, much of the Caribbean, the Balkans, parts of northern Africa, the northern region of Australia, and a large swath of the South Pacific"[24] and dramatically reducing mortality in Sri Lanka and India.[25] However widespread agricultural use led to resistant insect populations. In many areas, early victories partially or completely reversed, and in some cases rates of transmission even increased.[26] The program was successful in eliminating malaria only in areas with "high socio-economic status, well-organized healthcare systems, and relatively less intensive or seasonal malaria transmission".[27]
DDT was less effective in tropical regions due to the continuous life cycle of mosquitoes and poor infrastructure. It was not applied at all in sub-Saharan Africa due to these perceived difficulties. Mortality rates in that area never declined to the same dramatic extent, and now constitute the bulk of malarial deaths worldwide, especially following the disease's resurgence as a result of resistance to drug treatments and the spread of the deadly malarial variant caused by Plasmodium falciparum. The goal of eradication was abandoned in 1969, and attention was focused on controlling and treating the disease. Spraying programs (especially using DDT) were curtailed due to concerns over safety and environmental effects, as well as problems in administrative, managerial and financial implementation, but mostly because mosquitoes were developing resistance to DDT.[26] Efforts shifted from spraying to the use of bednets impregnated with insecticides and other interventions.[27][28]
Silent Spring and the U.S. ban
As early as the 1940s, scientists in the U.S. had begun expressing concern over possible hazards associated with DDT, and in the 1950s the government began tightening some of the regulations governing its use.[13] However, these early events received little attention, and it was not until 1957, when the New York Times reported an unsuccessful struggle to restrict DDT use in Nassau County, New York, that the issue came to the attention of the popular naturalist-author, Rachel Carson. William Shawn, editor of The New Yorker, urged her to write a piece on the subject, which developed into her famous book Silent Spring, published in 1962. The book argued that pesticides, including DDT, were poisoning both wildlife and the environment and were also endangering human health.[5]
Silent Spring was a best seller, and public reaction to it launched the modern environmental movement in the United States. The year after it appeared, President Kennedy ordered his Science Advisory Committee to investigate Carson's claims. The report the committee issued "add[ed] up to a fairly thorough-going vindication of Rachel Carson’s Silent Spring thesis," in the words of the journal Science,[29] and recommended a phaseout of "persistent toxic pesticides".[30] DDT became a prime target of the growing anti-chemical and anti-pesticide movements, and in 1967 a group of scientists and lawyers founded the Environmental Defense Fund (EDF) with the specific goal of winning a ban on DDT. Victor Yannacone, Charles Wurster, Art Cooley and others associated with inception of EDF had all witnessed bird kills or declines in bird populations and suspected that DDT was the cause. In their campaign against the chemical, EDF petitioned the government for a ban and filed a series of lawsuits.[31] Around this time, toxicologist David Peakall was measuring DDE levels in the eggs of peregrine falcons and California condors and finding that increased levels corresponded with thinner shells.
In response to an EDF suit, the U.S. District Court of Appeals in 1971 ordered the EPA to begin the de-registration procedure for DDT. After an initial six-month review process, William Ruckelshaus, the Agency's first Administrator rejected an immediate suspension of DDT's registration, citing studies from the EPA's internal staff stating that DDT was not an imminent danger to human health and wildlife.[13] However, the findings of these staff members were criticized, as they were performed mostly by economic entomologists inherited from the United States Department of Agriculture, who many environmentalists felt were biased towards agribusiness and tended to minimize concerns about human health and wildlife. The decision not to ban thus created public controversy.[21]
The EPA then held seven months of hearings in 1971–1972, with scientists giving evidence both for and against the use of DDT. In the summer of 1972, Ruckelshaus announced the cancellation of most uses of DDT—an exemption allowed for public health uses under some conditions.[13] Immediately after the cancellation was announced, both EDF and the DDT manufacturers filed suit against the EPA, with the industry seeking to overturn the ban, and EDF seeking a comprehensive ban. The cases were consolidated, and in 1973 the U.S. Court of Appeals for the District of Columbia ruled that the EPA had acted properly in banning DDT.[13]
The U.S. DDT ban took place amidst a growing public mistrust of industry, with the Surgeon General issuing a report on smoking in 1964, the Cuyahoga River catching fire in 1969, the fiasco surrounding the use of diethylstilbestrol (DES), and the well-publicized decline in the bald eagle population.[30]
Some uses of DDT continued under the public health exemption. For example, in June 1979, the California Department of Health Services was permitted to use DDT to suppress flea vectors of bubonic plague.[32] DDT also continued to be produced in the US for foreign markets until as late as 1985, when over 300 tons were exported.[1]
Restrictions on usage
In the 1970s and 1980s, agricultural use was banned in most developed countries, beginning with Hungary in 1968[33] then in Norway and Sweden in 1970, Germany and the United States in 1972, but not in the United Kingdom until 1984. Vector control use has not been banned, but it has been largely replaced by less persistent alternative insecticides.
The Stockholm Convention, which took effect in 2004, outlawed several persistent organic pollutants, and restricted DDT use to vector control. The Convention has been ratified by more than 170 countries and is endorsed by most environmental groups. Recognizing that total elimination in many malaria-prone countries is currently unfeasible because there are few affordable or effective alternatives, public health use is exempt from the ban pending acceptable alternatives. Malaria Foundation International states, "The outcome of the treaty is arguably better than the status quo going into the negotiations...For the first time, there is now an insecticide which is restricted to vector control only, meaning that the selection of resistant mosquitoes will be slower than before."[34]
Despite the worldwide ban, agricultural use continues in India[35][dead link] North Korea, and possibly elsewhere.[15]
Today, about 3-4,000 tonnes each year are produced for vector control.[14] DDT is applied to the inside walls of homes to kill or repel mosquitoes. This intervention, called indoor residual spraying (IRS), greatly reduces environmental damage. It also reduces the incidence of DDT resistance.[36] For comparison, treating 40 hectares (99 acres) of cotton during a typical U.S. growing season requires the same amount of chemical as roughly 1,700 homes.[37]
Environmental impact

DDT is a persistent organic pollutant that is readily adsorbed to soils and sediments, which can act both as sinks and as long-term sources of exposure contributing to terrestrial organisms.[2] Depending on conditions, its soil half life can range from 22 days to 30 years. Routes of loss and degradation include runoff, volatilization, photolysis and aerobic and anaerobic biodegradation. Due to hydrophobic properties, in aquatic ecosystems DDT and its metabolites are absorbed by aquatic organisms and adsorbed on suspended particles, leaving little DDT dissolved in the water itself. Its breakdown products and metabolites, DDE and DDD, are also highly persistent and have similar chemical and physical properties.[1] DDT and its breakdown products are transported from warmer regions of the world to the Arctic by the phenomenon of global distillation, where they then accumulate in the region's food web.[38]
Because of its lipophilic properties, DDT has a high potential to bioaccumulate, especially in predatory birds.[39] DDT, DDE, and DDD magnify through the food chain, with apex predators such as raptor birds concentrating more chemicals than other animals in the same environment. They are very lipophilic and are stored mainly in body fat. DDT and DDE are very resistant to metabolism; in humans, their half-lives are 6 and up to 10 years, respectively. In the United States, these chemicals were detected in almost all human blood samples tested by the Centers for Disease Control in 2005, though their levels have sharply declined since most uses were banned in the US.[40] Estimated dietary intake has also declined,[40] although FDA food tests commonly detect it.[41]
Marine macroalgae (seaweed) help reduce soil toxicity by up to 80% within six weeks.[42]
Effects on wildlife and eggshell thinning
DDT is toxic to a wide range of living organisms, including marine animals such as crayfish, daphnids, sea shrimp and many species of fish. It is less toxic to mammals, but may be moderately toxic to some amphibian species, especially in the larval stage. DDT, through its metabolite DDE, caused eggshell thinning and resulted in severe population declines in multiple North American and European bird of prey species.[43] Eggshell thinning lowers the reproductive rate of certain bird species by causing egg breakage and embryo deaths. DDE related eggshell thinning is considered a major reason for the decline of the bald eagle,[8] brown pelican,[44] peregrine falcon, and osprey.[1] However, different groups of birds vary greatly in their sensitivity to these chemicals.[2] Birds of prey, waterfowl, and song birds are more susceptible to eggshell thinning than chickens and related species, and DDE appears to be more potent than DDT.[1] Even in 2010, more than forty years after the U.S. ban, California condors which feed on sea lions at Big Sur which in turn feed in the Palos Verdes Shelf area of the Montrose Chemical Superfund site seemed to be having continued thin-shell problems. Scientists with the Ventana Wildlife Society and others are intensifying studies and remediations of the condors' problems.[45]
The biological thinning mechanism is not entirely known, but there is strong evidence that p,p'-DDE inhibits calcium ATPase in the membrane of the shell gland and reduces the transport of calcium carbonate from blood into the eggshell gland. This results in a dose-dependent thickness reduction.[1][46][47][48] There is also evidence that o,p'-DDT disrupts female reproductive tract development, impairing eggshell quality later.[49] Multiple mechanisms may be at work, or different mechanisms may operate in different species.[1] Some studies show that although DDE levels have fallen dramatically, eggshell thickness remains 10–12 percent thinner than before DDT was first used.[50]
Effects on human health
Potential mechanisms of action on humans are genotoxicity and endocrine disruption. DDT can be directly genotoxic,[51] but may also induce enzymes to produce other genotoxic intermediates and DNA adducts.[51] It is an endocrine disruptor; The DDT metabolite DDE acts as an antiandrogen (but not as an estrogen). p,p'-DDT, DDT's main component, has little or no androgenic or estrogenic activity.[51] Minor component o,p'-DDT has weak estrogenic activity.
Acute toxicity
DDT is classified as "moderately toxic" by the United States National Toxicology Program (NTP)[52] and "moderately hazardous" by the World Health Organization (WHO), based on the rat oral LD50 of 113 mg/kg.[53] DDT has on rare occasions been administered orally as a treatment for barbiturate poisoning.[54]
Chronic toxicity
Diabetes
DDT and DDE have been linked to diabetes. A number of studies from the US, Canada, and Sweden have found that the prevalence of the disease in a population increases with serum DDT or DDE levels.[55][56][57][58][59][60]
Developmental toxicity
DDT and DDE, like other organochlorines, have been shown to have xenoestrogenic activity, meaning they are chemically similar enough to estrogens to trigger hormonal responses in animals. This endocrine disrupting activity has been observed in mice and rat toxicological studies, and available epidemiological evidence indicates that these effects may be occurring in humans as a result of DDT exposure. The US Environmental Protection Agency states that DDT exposure damages the reproductive system and reduces reproductive success. These effects may cause developmental and reproductive toxicity:
- A review article in The Lancet states, "research has shown that exposure to DDT at amounts that would be needed in malaria control might cause preterm birth and early weaning ... toxicological evidence shows endocrine-disrupting properties; human data also indicate possible disruption in semen quality, menstruation, gestational length, and duration of lactation."[28]
- Human epidemiological studies suggest that exposure is a risk factor for premature birth and low birth weight, and may harm a mother's ability to breast feed.[61] Some 21st-century researchers argue that these effects may increase infant deaths, offsetting any anti-malarial benefits.[62] A 2008 study, however, failed to confirm the association between exposure and difficulty breastfeeding.[63]
- Several recent studies demonstrate a link between in utero exposure to DDT or DDE and developmental neurotoxicity in humans. For example, a 2006 University of California, Berkeley study suggests that children exposed while in the womb have a greater chance of development problems,[64] and other studies have found that even low levels of DDT or DDE in umbilical cord serum at birth are associated with decreased attention at infancy[65] and decreased cognitive skills at 4 years of age.[66] Similarly, Mexican researchers have linked first trimester DDE exposure to retarded psychomotor development.[67]
- Other studies document decreases in semen quality among men with high exposures (generally from IRS).[68][69][70]
- Studies generally find that high blood DDT or DDE levels do not increase time to pregnancy (TTP.)[71] There is some evidence that the daughters of highly exposed women may have more difficulty getting pregnant (i.e. increased TTP).[72]
- DDT is associated with early pregnancy loss, a type of miscarriage. A prospective cohort study of Chinese textile workers found "a positive, monotonic, exposure-response association between preconception serum total DDT and the risk of subsequent early pregnancy losses."[73] The median serum DDE level of study group was lower than that typically observed in women living in homes sprayed with DDT.[74]
- A Japanese study of congenital hypothyroidism concluded that in utero DDT exposure may affect thyroid hormone levels and "play an important role in the incidence and/or causation of cretinism."[75] Other studies have also found that DDT or DDE interfere with proper thyroid function.[76][77]
Other
Occupational exposure in agriculture and malaria control has been linked to neurological problems (i.e. Parkinsons)[78] and asthma.[79]
Carcinogenicity
In 2002 the Centers for Disease Control reported that "Overall, in spite of some positive associations for some cancers within certain subgroups of people, there is no clear evidence that exposure to DDT/DDE causes cancer in humans."[1] The NTP classifies it as "reasonably anticipated to be a carcinogen," the International Agency for Research on Cancer classifies it as a "possible" human carcinogen, and the EPA classifies DDT, DDE, and DDD as class B2 "probable" carcinogens. These evaluations are based mainly on the results of animal studies.[1][28]
More recent evidence from epidemiological studies (i.e. studies in human populations) indicates that DDT causes cancers of the liver,[28][40] pancreas[28][40] and breast.[40] There is mixed evidence that it contributes to leukemia,[40] lymphoma[40][80] and testicular cancer.[28][40][81] Other epidemiological studies suggest that DDT/DDE does not cause multiple myeloma,[28] or cancers of the prostate,[28] endometrium,[28][40] rectum,[28][40] lung,[40] bladder,[40] or stomach.[40]
Breast cancer
The question of whether DDT or DDE are risk factors of breast cancer has been repeatedly studied. While individual studies conflict, the most recent reviews of all the evidence conclude that pre-puberty exposure increases the risk of subsequent breast cancer.[40][82] Until recently, almost all studies measured DDT or DDE blood levels at the time of breast cancer diagnosis or after. This study design has been criticized, since the levels at diagnosis do not necessarily correspond to levels when the cancer started.[83] Taken as a whole such studies "do not support the hypothesis that exposure to DDT is an important risk factor for breast cancer."[51] The studies of this design have been extensively reviewed.[28][84][85]
In contrast, a study published in 2007 strongly associated early exposure (the p,p'- isomer) and breast cancer later in life. Unlike previous studies, this prospective cohort study collected blood samples from young mothers in the 1960s while DDT was still in use, and their breast cancer status was then monitored over the years. In addition to suggesting that the p,p'- isomer is the more significant risk factor, the study also suggests that the timing of exposure is critical. For the subset of women born more than 14 years before agricultural use, there was no association between DDT and breast cancer. However, for younger women—exposed earlier in life—the third who were exposed most to p,p'-DDT had a fivefold increase in breast cancer incidence over the least exposed third, after correcting for the protective effect of o,p'-DDT.[51][86][87] These results are supported by animal studies.[40]
Use against malaria
Malaria remains a major public health challenge in many countries. 2008 WHO estimates were 243 million cases, and 863,000 deaths. About 89% of these deaths occur in Africa, and mostly to children under the age of 5.[88] DDT is one of many tools that public health officials use to fight the disease. Its use in this context has been called everything from a "miracle weapon [that is] like Kryptonite to the mosquitoes,"[89] to "toxic colonialism."[90]
Before DDT, eliminating mosquito breeding grounds by drainage or poisoning with Paris green or pyrethrum was sometimes successful in fighting malaria. In parts of the world with rising living standards, the elimination of malaria was often a collateral benefit of the introduction of window screens and improved sanitation.[24] Today, a variety of usually simultaneous interventions is the norm. These include antimalarial drugs to prevent or treat infection; improvements in public health infrastructure to quickly diagnose, sequester, and treat infected individuals; bednets and other methods intended to keep mosquitoes from biting humans; and vector control strategies[88] such as larvaciding with insecticides, ecological controls such as draining mosquito breeding grounds or introducing fish to eat larvae, and indoor residual spraying with insecticides, possibly including DDT. IRS involves the treatment of all interior walls and ceilings with insecticides, and is particularly effective against mosquitoes, since many species rest on an indoor wall before or after feeding. DDT is one of 12 WHO–approved IRS insecticides. How much of a role DDT should play in this mix of strategies is still controversial.[91]
WHO's anti-malaria campaign of the 1950s and 1960s relied heavily on DDT and the results were promising, though temporary. Experts tie the resurgence of malaria to multiple factors, including poor leadership, management and funding of malaria control programs; poverty; civil unrest; and increased irrigation. The evolution of resistance to first-generation drugs (e.g. chloroquine) and to insecticides exacerbated the situation.[15][92] Resistance was largely fueled by often unrestricted agricultural use. Resistance and the harm both to humans and the environment led many governments to restrict or curtail the use of DDT in vector control as well as agriculture.[26] In 2006 the WHO reversed a longstanding policy against DDT by recommending that it be used as an indoor pesticide in regions where malaria is a major problem.[93]
Once the mainstay of anti-malaria campaigns, as of 2008 only 12 countries used DDT, including India and some southern African states,[88] though the number is expected to rise.[15]
Effectiveness of DDT against malaria
When it was first introduced in World War II, DDT was very effective in reducing malaria morbidity and mortality.[21] The WHO's anti-malaria campaign, which consisted mostly of spraying DDT, was initially very successful as well. For example, in Sri Lanka, the program reduced cases from about 3 million per year before spraying to just 18 in 1963[94][95] and 29 in 1964. Thereafter the program was halted to save money and malaria rebounded to 600,000 cases in 1968 and the first quarter of 1969. The country resumed DDT vector control but the mosquitoes had acquired resistance in the interim, presumably because of continued agricultural use. The program switched to malathion, which though more expensive, proved effective.[25]
Today, DDT remains on the WHO's list of insecticides recommended for IRS. Since the appointment of Arata Kochi as head of its anti-malaria division, WHO's policy has shifted from recommending IRS only in areas of seasonal or episodic transmission of malaria, to also advocating it in areas of continuous, intense transmission.[96] The WHO has reaffirmed its commitment to eventually phasing out DDT, aiming "to achieve a 30% cut in the application of DDT world-wide by 2014 and its total phase-out by the early 2020s if not sooner" while simultaneously combating malaria. The WHO plans to implement alternatives to DDT to achieve this goal.[97]
South Africa is one country that continues to use DDT under WHO guidelines. In 1996, the country switched to alternative insecticides and malaria incidence increased dramatically. Returning to DDT and introducing new drugs brought malaria back under control.[98] According to DDT advocate Donald Roberts, malaria cases increased in South America after countries in that continent stopped using DDT. Research data shows a significantly strong negative relationship between DDT residual house sprayings and malaria rates. In a research from 1993 to 1995, Ecuador increased its use of DDT and resulted in a 61% reduction in malaria rates, while each of the other countries that gradually decreased its DDT use had large increase in malaria rates.[37]
Mosquito resistance
Resistance has greatly reduced DDT's effectiveness. WHO guidelines require that absence of resistance must be confirmed before using the chemical.[99] Resistance is largely due to agricultural use, in much greater quantities than required for disease prevention. According to one study that attempted to quantify the lives saved by banning agricultural use and thereby slowing the spread of resistance, "it can be estimated that at current rates each kilo of insecticide added to the environment will generate 105 new cases of malaria."[26]
Resistance was noted early in spray campaigns. Paul Russell, a former head of the Allied Anti-Malaria campaign, observed in 1956 that "resistance has appeared after six or seven years."[24] DDT has lost much of its effectiveness in Sri Lanka, Pakistan, Turkey and Central America, and it has largely been replaced by organophosphate or carbamate insecticides, e.g. malathion or bendiocarb.[100]
In many parts of India, DDT has also largely lost its effectiveness.[101] Agricultural uses were banned in 1989, and its anti-malarial use has been declining. Urban use has halted completely.[102] Nevertheless, DDT is still manufactured and used,[103] and one study had concluded that "DDT is still a viable insecticide in indoor residual spraying owing to its effectivity in well supervised spray operation and high excito-repellency factor."[104]
Studies of malaria-vector mosquitoes in KwaZulu-Natal Province, South Africa found susceptibility to 4% DDT (the WHO susceptibility standard), in 63% of the samples, compared to the average of 86.5% in the same species caught in the open. The authors concluded that "Finding DDT resistance in the vector An. arabiensis, close to the area where we previously reported pyrethroid-resistance in the vector An. funestus Giles, indicates an urgent need to develop a strategy of insecticide resistance management for the malaria control programmes of southern Africa."[105]
DDT can still be effective against resistant mosquitoes,[106] and the avoidance of DDT-sprayed walls by mosquitoes is an additional benefit of the chemical.[104] For example, a 2007 study reported that resistant mosquitoes avoided treated huts. The researchers argued that DDT was the best pesticide for use in IRS (even though it did not afford the most protection from mosquitoes out of the three test chemicals) because the others pesticides worked primarily by killing or irritating mosquitoes—encouraging the development of resistance to these agents.[106] Others argue that the avoidance behavior slows the eradication of the disease.[107] Unlike other insecticides such as pyrethroids, DDT requires long exposure to accumulate a lethal dose; however its irritant property shortens contact periods. "For these reasons, when comparisons have been made, better malaria control has generally been achieved with pyrethroids than with DDT."[100] In India, with its outdoor sleeping habits and frequent night duties, "the excito-repellent effect of DDT, often reported useful in other countries, actually promotes outdoor transmission."[108]
Residents' concerns
For IRS to be effective, at least 80% of homes and barns in an area must be sprayed.[99] Lower coverage rates can jeopardize program effectiveness. Many residents resist DDT spraying, objecting to the lingering smell, stains on walls, and may exacerbate problems with other insect pests.[100][107][109] Pyrethroid insecticides (e.g. deltamethrin and lambda-cyhalothrin) can overcome some of these issues, increasing participation.[100]
Human exposure
People living in areas where DDT is used for IRS have high levels of the chemical and its breakdown products in their bodies. Compared to contemporaries living where DDT is not used, South Africans living in sprayed homes have levels that are several orders of magnitude greater.[40] Breast milk in regions where DDT is used against malaria greatly exceeds the allowable standards for breast-feeding infants.[110][111][112] These levels are associated with neurological abnormalities in babies.[100][110][111]
Most studies of DDT's human health effects have been conducted in developed countries where DDT is not used and exposure is relatively low. Many experts urge that alternatives be used instead of IRS.[28][40] Epidemiologist Brenda Eskenazi argues, "We know DDT can save lives by repelling and killing disease-spreading mosquitoes. But evidence suggests that people living in areas where DDT is used are exposed to very high levels of the pesticide. The only published studies on health effects conducted in these populations have shown profound effects on male fertility. Clearly, more research is needed on the health of populations where indoor residual spraying is occurring, but in the meantime, DDT should really be the last resort against malaria rather than the first line of defense."[113]
Illegal diversion to agriculture is also a concern, as it is almost impossible to prevent, and its subsequent use on crops is uncontrolled. For example, DDT use is widespread in Indian agriculture,[114] particularly mango production,[115] and is reportedly used by librarians to protect books.[116] Other examples include Ethiopia, where DDT intended for malaria control is reportedly being used in coffee production,[117] and Ghana where it is used for fishing."[118][119] The residues in crops at levels unacceptable for export have been an important factor in recent bans in several tropical countries.[100] Adding to this problem is a lack of skilled personnel and supervision.[107]
Criticism of restrictions on DDT use
Banning DDT killed more people than Hitler.
Critics claim that restricting DDT in vector control have caused unnecessary deaths due to malaria. Estimates range from hundreds of thousands,[121] to millions. Robert Gwadz of the National Institutes of Health said in 2007, "The ban on DDT may have killed 20 million children."[122] These arguments have been dismissed as "outrageous" by former WHO scientist Socrates Litsios. May Berenbaum, University of Illinois entomologist, says, "to blame environmentalists who oppose DDT for more deaths than Hitler is worse than irresponsible."[89] Investigative journalist Adam Sarvana and others characterize this notion as a "myth" promoted principally by Roger Bate of the pro-DDT advocacy group Africa Fighting Malaria (AFM).[123][124]
Criticisms of a DDT "ban" often specifically reference the 1972 US ban (with the erroneous implication that this constituted a worldwide ban and prohibited use of DDT in vector control). Reference is often made to Rachel Carson's Silent Spring even though she never pushed for a ban on DDT. John Quiggin and Tim Lambert wrote, "the most striking feature of the claim against Carson is the ease with which it can be refuted."[125] Carson actually devoted a page of her book to considering the relationship between DDT and malaria, warning of the evolution of DDT resistance in mosquitoes and concluding:
It is more sensible in some cases to take a small amount of damage in preference to having none for a time but paying for it in the long run by losing the very means of fighting [is the advice given in Holland by Dr Briejer in his capacity as director of the Plant Protection Service]. Practical advice should be "Spray as little as you possibly can" rather than "Spray to the limit of your capacity."
It has also been alleged that donor governments and agencies have refused to fund DDT spraying, or made aid contingent upon not using DDT. According to a report in the British Medical Journal, use of DDT in Mozambique "was stopped several decades ago, because 80% of the country's health budget came from donor funds, and donors refused to allow the use of DDT."[126] Roger Bate asserts, "many countries have been coming under pressure from international health and environment agencies to give up DDT or face losing aid grants: Belize and Bolivia are on record admitting they gave in to pressure on this issue from [USAID]."[127]
The United States Agency for International Development (USAID) has been the focus of much criticism. While the agency is currently funding the use of DDT in some African countries,[128] in the past it did not. When John Stossel accused USAID of not funding DDT because it wasn't "politically correct," Anne Peterson, the agency's assistant administrator for global health, replied that "I believe that the strategies we are using are as effective as spraying with DDT ... So, politically correct or not, I am very confident that what we are doing is the right strategy."[129] USAID's Kent R. Hill states that the agency has been misrepresented: "USAID strongly supports spraying as a preventative measure for malaria and will support the use of DDT when it is scientifically sound and warranted."[130] The Agency's website states that "USAID has never had a 'policy' as such either 'for' or 'against' DDT for IRS. The real change in the past two years [2006/07] has been a new interest and emphasis on the use of IRS in general—with DDT or any other insecticide—as an effective malaria prevention strategy in tropical Africa."[128] The website further explains that in many cases alternative malaria control measures were judged to be more cost-effective that DDT spraying, and so were funded instead.[131]
Alternatives
Other insecticides
Advocates of increased use of DDT in IRS claim that alternative insecticides are more expensive, more toxic, or not as effective. As discussed above, susceptibility of mosquitoes to DDT varies geographically. The same is true for alternative insecticides, so its relative effectiveness varies. Toxicity and cost-effectiveness comparisons lack data. Relative insecticide costs vary by location and ease of access, the habits of the local mosquitoes, the degrees of resistance exhibited by the mosquitoes, and the habits and compliance of the population, among other factors. The choice of insecticide has little impact on the total cost of a round of spraying, since product costs are only a fraction of campaign costs. IRS coverage needs to be maintained throughout the malaria season, making DDT's relatively long life an important cost savings.
Organophosphate and carbamate insecticides, e.g. malathion and bendiocarb, respectively, are more expensive than DDT per kilogram and are applied at roughly the same dosage. Pyrethroids such as deltamethrin are also more expensive than DDT, but are applied more sparingly (0.02-0.3 g/m2 vs 1-2 g/m2), so the net cost per house is about the same over 6 months.[27]
Non-chemical vector control
Before DDT, malaria was successfully eradicated or curtailed in several tropical areas by removing or poisoning mosquito breeding grounds and larva habitats, for example by filling or applying oil to standing water. These methods have seen little application in Africa for more than half a century.[132]
The relative effectiveness of IRS (with DDT or alternative insecticides) versus other malaria control techniques (e.g. bednets or prompt access to anti-malarial drugs) varies greatly and is highly dependent on local conditions.[27]
A WHO study released in January 2008 found that mass distribution of insecticide-treated mosquito nets and artemisinin–based drugs cut malaria deaths in half in Rwanda and Ethiopia, countries with high malaria burdens. IRS with DDT did not play an important role in mortality reduction in these countries.[133][134]
Vietnam has enjoyed declining malaria cases and a 97% mortaility reduction after switching in 1991 from a poorly funded DDT-based campaign to a program based on prompt treatment, bednets, and pyrethroid group insecticides.[135]
In Mexico, effective and affordable chemical and non-chemical strategies against malaria have been so successful that the Mexican DDT manufacturing plant ceased production due to lack of demand.[136]
While the increased numbers of malaria victims since DDT usage collapsed document its value, many other factors contributed to the rise in cases.
A review of fourteen studies on the subject in sub-Saharan Africa, covering insecticide-treated nets, residual spraying, chemoprophylaxis for children, chemoprophylaxis or intermittent treatment for pregnant women, a hypothetical vaccine, and changing front–line drug treatment, found decision making limited by the gross lack of information on the costs and effects of many interventions, the very small number of cost-effectiveness analyses available, the lack of evidence on the costs and effects of packages of measures, and the problems in generalizing or comparing studies that relate to specific settings and use different methodologies and outcome measures. The two cost-effectiveness estimates of DDT residual spraying examined were not found to provide an accurate estimate of the cost-effectiveness of DDT spraying; furthermore, the resulting estimates may not be good predictors of cost-effectiveness in current programs.[137]
However, a study in Thailand found the cost per malaria case prevented of DDT spraying ($1.87 US) to be 21% greater than the cost per case prevented of lambda-cyhalothrin–treated nets ($1.54 US),[138] at very least casting some doubt on the unexamined assumption that DDT was the most cost-effective measure to use in all cases. The director of Mexico's malaria control program finds similar results, declaring that it is 25% cheaper for Mexico to spray a house with synthetic pyrethroids than with DDT.[136] However, another study in South Africa found generally lower costs for DDT spraying than for impregnated nets.[139]
A more comprehensive approach to measuring cost-effectiveness or efficacy of malarial control would not only measure the cost in dollars of the project, as well as the number of people saved, but would also consider ecological damage and negative aspects of insecticide use on human health. One preliminary study regarding the effect of DDT found that it is likely the detriment to human health approaches or exceeds the beneficial reductions in malarial cases, except perhaps in malarial epidemic situations. It is similar to the earlier mentioned study regarding estimated theoretical infant mortality caused by DDT and subject to the criticism also mentioned earlier.[140]
A study in the Solomon Islands found that "although impregnated bed nets cannot entirely replace DDT spraying without substantial increase in incidence, their use permits reduced DDT spraying."[141]
A comparison of four successful programs against malaria in Brazil, India, Eritrea, and Vietnam does not endorse any single strategy but instead states, "Common success factors included conducive country conditions, a targeted technical approach using a package of effective tools, data-driven decision-making, active leadership at all levels of government, involvement of communities, decentralized implementation and control of finances, skilled technical and managerial capacity at national and sub-national levels, hands-on technical and programmatic support from partner agencies, and sufficient and flexible financing."[142]
DDT resistant mosquitoes have generally proved susceptible to pyrethroids. Thus far, pyrethroid resistance in Anopheles has not been a major problem.[100]
See also
- DDT in Australia
- DDT in New Zealand
- DDT in the United States
- Mickey Slim, a short-lived cocktail that combined gin with a pinch of DDT.
- Operation Cat Drop
References
- ^ a b c d e f g h i j Toxicological Profile: for DDT, DDE, and DDE. Agency for Toxic Substances and Disease Registry, September 2002.
- ^ a b c DDT and Its Derivatives. Geneva: World Health Organisation. 1989. p. 83. ISBN 92-4-154283-7.
- ^ a b NobelPrize.org: The Nobel Prize in Physiology of Medicine 1948 Accessed July 26, 2007.
- ^ a b c d e f Environmental Health Criteria 9: DDT and its derivatives, World Health Organization, 1979.
- ^ a b Lear, Linda (1997). Rachel Carson: Witness for Nature. New York: Henry Hoyten.
- ^ a b Larson, Kim (December 1, 2007). "Bad Blood". On Earth (Winter 2008). Retrieved 2008-06-05.
- ^ Moyers, Bill (2007-09-21), Rachel Carson and DDT, retrieved 2011-03-05
- ^ a b
Stokstad E (2007). "Species conservation. Can the bald eagle still soar after it is delisted?". Science. 316 (5832): 1689–90. doi:10.1126/science.316.5832.1689. PMID 17588911.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Geisz HN, Dickhut RM, Cochran MA, Fraser WR, Ducklow HW (2005). "Melting Glaciers: A Probable Source of DDT to the Antarctic Marine Ecosystem". Environ. Sci. Technol. ASAP: 3958. doi:10.1021/es702919n. Retrieved 2008-05-07.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ DAVID, DAVID (July 4, 2008). "McIntosh residents file suit against Ciba". Archived from the original on 2010-11-18. Retrieved 2008-07-07.
{{cite news}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ Environmental Cleanup Site Information Database for Arkema (former Pennwalt) facility, Oregon DEQ, April 2009.
- ^ Rosemary, Rosemary (2008-01-27). "Tests shed light on how pCBSA got into St. Louis water". Morning Sun. Retrieved 2008-05-16. [dead link]
- ^ a b c d e DDT Regulatory History: A Brief Survey (to 1975), U.S. EPA, July 1975.
- ^ a b Report of the Third Expert Group Meeting on DDT, UNEP/POPS/DDT-EG.3/3, Stockholm Convention on Persistent Organic Pollutants, November 12, 2010. Available here.
- ^ a b c d van den Berg, Henk (October 23, 2008). "Global status of DDT and its alternatives for use in vector control to prevent disease". Stockholm Convention/United Nations Environment Programme. Archived from the original (PDF) on 2010-11-18. Retrieved 2008-11-22.
{{cite web}}: Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ Denholm I, Devine GJ, Williamson MS (2002). "Evolutionary genetics. Insecticide resistance on the move". Science. 297 (5590): 2222–3. doi:10.1126/science.1077266. PMID 12351778.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Augustin, Frank (1993). Zur Geschichte des Insektizids Dichlordiphenyltrichloräthan (DDT) unter besonderer Berücksichtigung der Leistung des Chemikers Paul Müller (1899 - 1965). Leipzig: Medizinische Fakultät der Universität Leipzig. pp. 1–77.
- ^ Attention: This template ({{cite doi}}) is deprecated. To cite the publication identified by doi:10.1002/prac.19301270114, please use {{cite journal}} (if it was published in a bona fide academic journal, otherwise {{cite report}} with
|doi=10.1002/prac.19301270114instead. - ^ {{Cite doi|10.1002/prac.19301270115
- ^ Wolfgang von Leuthold, Schädlingsbekämpfung. DRP Nr 673246, 27.4.1934
- ^ a b c Dunlap, Thomas R. (1981). DDT: Scientists, Citizens, and Public Policy. New Jersey: Princeton University Press. ISBN 978-0-691-04680-8.
- ^ Oreskes, Naomi; Erik M. Conway, Erik M (2010). Merchants of Doubt: How a Handful of Scientists Obscured the Truth on Issues from Tobacco Smoke to Global Warming (First ed.). San Francisco, CA: Bloomsbury Press. ISBN 978-1-59691-610-4.
- ^ Shah, Sonia “Don’t Blame Environmentalists for Malaria,” The Nation. April 2006.
- ^ a b c Gladwell, Malcolm (July 2, 2001). "The Mosquito Killer". The New Yorker.
- ^ a b Harrison, Gordon A (1978). Mosquitoes, Malaria, and Man: A History of the Hostilities Since 1880. Dutton. ISBN 978-0-525-16025-0.
- ^ a b c d Chapin G, Wasserstrom R (1981). "Agricultural production and malaria resurgence in Central America and India". Nature. 293 (5829): 181–5. doi:10.1038/293181a0. PMID 7278974.
- ^ a b c d Sadasivaiah, Shobha; Tozan, Yesim; Breman, Joel G. (1 December 2007). "Dichlorodiphenyltrichloroethane (DDT) for Indoor Residual Spraying in Africa: How Can It Be Used for Malaria Control?". Am. J. Trop. Med. Hyg. 77 (Suppl 6): 249–263.
- ^ a b c d e f g h i j k l Rogan WJ, Chen A (2005). "Health risks and benefits of bis(4-chlorophenyl)-1,1,1-trichloroethane (DDT)". Lancet. 366 (9487): 763–73. doi:10.1016/S0140-6736(05)67182-6. PMID 16125595.
- ^ Greenberg DS (1963). "Pesticides: White House Advisory Body Issues Report Recommending Steps to Reduce Hazard to Public". Science. 140 (3569): 878–9. doi:10.1126/science.140.3569.878. PMID 17810673.
{{cite journal}}: Unknown parameter|month=ignored (help) cited in Graham Jr., Frank. "Nature's Protector and Provocateur". Audubon Magazine. [dead link] - ^ a b Michaels, David (2008). Doubt is Their Product: How Industry's Assault on Science Threatens Your Health. New York: Oxford University Press. ISBN 978-0-19-530067-3.
- ^ "Sue the Bastards". TIME. October 18, 1971. Archived from the original on 2010-11-18.
{{cite news}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ "AEI - Short Publications - The Rise, Fall, Rise, and Imminent Fall of DDT". Archived from the original on 2010-11-18.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ "Selected passages from the history of the Hungarian plant protection administration on the 50th anniversary of establishing the county plant protection stations".
- ^ "MFI second page". Malaria Foundation International. Archived from the original on 2010-11-18. Retrieved 2006-03-15.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ "Concern over excessive DDT use in Jiribam fields". The Imphal Free Press. 2008-05-05. Retrieved 2008-05-05.
- ^ "Is DDT still effective and needed in malaria control?". Malaria Foundation International. Archived from the original on 2010-11-18. Retrieved 2006-03-15.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ a b Roberts, Donald R.; Laughlin, LL; Hsheih, P; Legters, LJ (1997). "DDT, global strategies, and a malaria control crisis in South America". Emerging Infectious Diseases. 3 (3): 295–302. doi:10.3201/eid0303.970305. PMC 2627649. PMID 9284373.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ "The Grasshopper Effect and Tracking Hazardous Air Pollutants". The Science and the Environment Bulletin (May/June 1998). Environment Canada.[dead link]
- ^ Connell, D.; et al. (1999). Introduction to Ecotoxicology. Blackwell Science. p. 68. ISBN 0-632-03852-7.
{{cite book}}: Explicit use of et al. in:|author=(help) - ^ a b c d e f g h i j k l m n o p q Eskenazi, Brenda (May 4, 2009). "The Pine River Statement: Human Health Consequences of DDT Use" (PDF). Environ. Health Perspect.
- ^ USDA, Pesticide Data Program Annual Summary Calendar Year 2005, November 2006.
- ^ D Kantachote, R Naidu, B Williams, N McClure, M Megharaj, I Singleton, D; Naidu, R; Williams, B; McClure, N; Megharaj, M; Singleton, I (2004). "Bioremediation of DDT-contaminated soil: enhancement by seaweed addition". Journal of Chemical Technology & Biotechnology. 79 (6): 632–8. doi:10.1002/jctb.1032. Retrieved 2009-05-26.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Vos JG, Dybing E, Greim HA, Ladefoged O, Lambré C, Tarazona JV; et al. (2000). "Health effects of endocrine-disrupting chemicals on wildlife, with special reference to the European situation". Crit Rev Toxicol. 30 (1): 71–133. doi:10.1080/10408440091159176. PMID 10680769.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ "Endangered and Threatened Wildlife and Plants; 12-Month Petition Finding and Proposed Rule To Remove the Brown Pelican (Pelecanus occidentalis) From the Federal List of Endangered and Threatened Wildlife; Proposed Rule," Fish and Wildlife Service, U.S. Department of the Interior, February 20, 2008. 73 FR 9407
- ^ Moir, John, "New Hurdle for California Condors May Be DDT From Years Ago", The New York Times, November 15, 2010. Retrieved 2010-11-15.
- ^ Walker C.H.; et al. (2006). Principles of ecotoxicology (3rd ed.). Boca Raton, FL: CRC/Taylor & Francis. ISBN 978-0-8493-3635-5.
{{cite book}}: Explicit use of et al. in:|author=(help) - ^ Guillette, Louis J., Jr. (2006). "Endocrine Disrupting Contaminants". Archived from the original (PDF) on 2010-11-18. Retrieved 2007-02-02.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help)CS1 maint: multiple names: authors list (link) - ^ Lundholm, C.E. (1997). "DDE-Induced eggshell thinning in birds". Comp Biochem Physiol C Pharmacol Toxicol Endocrinol. 118 (2): 113. doi:10.1016/S0742-8413(97)00105-9. PMID 9490182.
- ^ Holm L, Blomqvist A, Brandt I, Brunström B, Ridderstråle Y, Berg C (2006). "Embryonic exposure to o,p'-DDT causes eggshell thinning and altered shell gland carbonic anhydrase expression in the domestic hen". Environ. Toxicol. Chem. 25 (10): 2787–93. doi:10.1897/05-619R.1. PMID 17022422.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Division of Environmental Quality
- ^ a b c d e Cohn, BA (2007). "DDT and breast cancer in young women: new data on the significance of age at exposure". Environ. Health Perspect. 115 (10): 1406–14. doi:10.1289/ehp.10260. PMC 2022666. PMID 17938728.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|month=ignored (help) - ^ Pesticideinfo.org
- ^ World Health Organization, The WHO Recommended Classification of Pesticides by Hazard, 2005.
- ^ Rappolt, RT (1973). "Use of oral DDT in three human barbiturate intoxications: hepatic enzyme induction by reciprocal detoxicants". Clin Toxicol. 6 (2): 147–51. doi:10.3109/15563657308990512. PMID 4715198.
- ^ Jones, Oliver AH; Maguire, Mahon L; Griffin, Julian L (January 26, 2008). "Environmental pollution and diabetes: a neglected association" (PDF). Lancet. 371 (9609): 287–8. doi:10.1016/S0140-6736(08)60147-6. PMID 18294985.
- ^ Turyk, Mary (March 6, 2009). "Organochlorine Exposure and Incidence of Diabetes in a Cohort of Great Lakes Sport Fish Consumers". Environ. Health Perspect. Archived from the original on 2010-11-18.
{{cite journal}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ Codru, Neculai; Schymura, MJ; Negoita, S; Akwesasne Task Force on Environment; Rej, R; Carpenter, DO (2007). "Diabetes in Relation to Serum Levels of Polychlorinated Biphenyls and Chlorinated Pesticides in Adult Native Americans". Environ. Health Perspect. 115 (10): 1442–7. doi:10.1289/ehp.10315. PMC 2022671. PMID 17938733. Archived from the original (PDF) on 2010-11-18.
{{cite journal}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ Cox, Shanna; Niskar, AS; Narayan, KM; Marcus, M (2007). "Prevalence of Self-Reported Diabetes and Exposure to Organochlorine Pesticides among Mexican Americans: Hispanic Health and Nutrition Examination Survey, 1982–1984". Environ. Health Perspect. 115 (12): 1747–52. doi:10.1289/ehp.10258. PMC 2137130. PMID 18087594. Archived from the original (PDF) on 2010-11-18.
{{cite journal}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ Turyk M, Anderson H, Knobeloch L, Imm P, Persky V (2009). "Organochlorine exposure and incidence of diabetes in a cohort of Great Lakes sport fish consumers". Environ. Health Perspect. 117 (7): 1076–82. doi:10.1289/ehp.0800281. PMC 2717133. PMID 19654916.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Philibert, Aline (11 December 2009). "An Exploratory Study of Diabetes in a First Nation Community with Respect to Serum Concentrations of p,p'-DDE and PCBs and Fish Consumption". Int. J. Environ. Res. Public Health. 6 (12): 3179–89. doi:10.3390/ijerph6123179. PMC 2800343. PMID 20049255. Archived from the original on 2010-11-18.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|deadurl=ignored (|url-status=suggested) (help)CS1 maint: unflagged free DOI (link) - ^ Rogan WJ, Ragan NB (2003). "Evidence of effects of environmental chemicals on the endocrine system in children". Pediatrics. 112 (1 Pt 2): 247–52. doi:10.1542/peds.112.1.S1.247. PMID 12837917.
- ^ Chen A, Rogan WJ (2003). "Nonmalarial infant deaths and DDT use for malaria control". Emerging Infect. Dis. 9 (8): 960–4. PMC 3020610. PMID 12967494.
Roberts D, Curtis C, Tren R, Sharp B, Shiff C, Bate R (2004). "Malaria control and public health". Emerging Infect. Dis. 10 (6): 1170–1, author reply 1171–2. PMID 15224677.{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Cupul-Uicab, LA; Gladen, BC; Hernández-Avila, M; Weber, JP; Longnecker, MP (2008). "DDE, a Degradation Product of DDT, and Duration of Lactation in a Highly Exposed Area of Mexico". Environ. Health Perspect. 116 (2): 179–183. doi:10.1289/ehp.10550. PMC 2235222. PMID 18288315.
- ^ BBC (2006-07-05). "DDT 'link' to slow child progress". BBC News. Retrieved 2006-07-05.
- ^ Sagiv SK, Nugent JK, Brazelton TB; et al. (2008). "Prenatal organochlorine exposure and measures of behavior in infancy using the Neonatal Behavioral Assessment Scale (NBAS)". Environ. Health Perspect. 116 (5): 666–73. doi:10.1289/ehp.10553. PMC 2367684. PMID 18470320.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Ribas-Fitó N, Torrent M, Carrizo D (2006). "In utero exposure to background concentrations of DDT and cognitive functioning among preschoolers". Am. J. Epidemiol. 164 (10): 955–62. doi:10.1093/aje/kwj299. PMID 16968864.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Torres-Sánchez L, Rothenberg SJ, Schnaas L (2007). "In utero p, p'-DDE exposure and infant neurodevelopment: a perinatal cohort in Mexico". Environ. Health Perspect. 115 (3): 435–9. doi:10.1289/ehp.9566. PMC 1849908. PMID 17431495.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Jurewicz J, Hanke W, Radwan M, Bonde JP (2010). "Environmental factors and semen quality". Int J Occup Med Environ Health. 22 (4): 1–25. doi:10.2478/v10001-009-0036-1. PMID 20053623.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Aneck-Hahn NH, Schulenburg GW, Bornman MS, Farias P, de Jager C (2007). "Impaired semen quality associated with environmental DDT exposure in young men living in a malaria area in the Limpopo Province, South Africa". J. Androl. 28 (3): 423–34. doi:10.2164/jandrol.106.001701. PMID 17192596.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ De Jager C, Farias P, Barraza-Villarreal A (2006). "Reduced seminal parameters associated with environmental DDT exposure and p,p'-DDE concentrations in men in Chiapas, Mexico: a cross-sectional study". J. Androl. 27 (1): 16–27. doi:10.2164/jandrol.05121. PMID 16400073.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Harley KG, Marks AR, Bradman A, Barr DB, Eskenazi B (2008). "DDT Exposure, Work in Agriculture, and Time to Pregnancy Among Farmworkers in California". J. Occup. Environ. Med. 50 (12): 1335–42. doi:10.1097/JOM.0b013e31818f684d. PMC 2684791. PMID 19092487. Archived from the original on 2010-11-18.
{{cite journal}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Cohn BA, Cirillo PM, Wolff MS (2003). "DDT and DDE exposure in mothers and time to pregnancy in daughters". Lancet. 361 (9376): 2205–6. doi:10.1016/S0140-6736(03)13776-2. PMID 12842376.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Venners SA, Korrick S, Xu X (2005). "Preconception serum DDT and pregnancy loss: a prospective study using a biomarker of pregnancy". Am. J. Epidemiol. 162 (8): 709–16. doi:10.1093/aje/kwi275. PMID 16120699.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Longnecker MP (2005). "Invited Commentary: Why DDT matters now". Am. J. Epidemiol. 162 (8): 726–8. doi:10.1093/aje/kwi277. PMID 16120697.
- ^ Nagayama J, Kohno H, Kunisue T (2007). "Concentrations of organochlorine pollutants in mothers who gave birth to neonates with congenital hypothyroidism". Chemosphere. 68 (5): 972–6. doi:10.1016/j.chemosphere.2007.01.010. PMID 17307219.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Alvarez-Pedrerol M, Ribas-Fito N, Torrent M, Carrizo D, Grimalt JO, Sunyer J (2007). "Effects of PCBs, p,p'-DDT, p,p'-DDE, HCB and {beta}-HCH on thyroid function in preschoolers". Occup Environ Med. 65 (7): 452–7. doi:10.1136/oem.2007.032763. PMID 17933884.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Schell LM, Gallo MV, Denham M, Ravenscroft J, Decaprio AP, Carpenter DO (2008). "Relationship of Thyroid Hormone Levels to Levels of Polychlorinated Biphenyls, Lead, p, p'- DDE, and Other Toxicants in Akwesasne Mohawk Youth". Environ Health Perspect. 116 (6): 806–13. doi:10.1289/ehp.10490. PMC 2430238. PMID 18560538.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ van Wendel de Joode B, Wesseling C, Kromhout H, Monge P, Garcia M, Mergler D (2001). "Chronic nervous-system effects of long-term occupational exposure to DDT". Lancet. 357 (9261): 1014–6. doi:10.1016/S0140-6736(00)04249-5. PMID 11293598.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Anthony J Brown, Pesticide Exposure Linked to Asthma, Scientific American, September 17, 2007.
- ^ Spinelli, John J.; Ng, CH; Weber, JP; Connors, JM; Gascoyne, RD; Lai, AS; Brooks-Wilson, AR; Le, ND; Berry, BR (2007-12-15). "Organochlorines and risk of non-Hodgkin lymphoma". Int. J. Cancer. 121 (12): 2767–75. doi:10.1002/ijc.23005. PMID 17722095.
- ^ McGlynn, Katherine A.; Quraishi, Sabah M.; Graubard, BI; Weber, JP; Rubertone, MV; Erickson, RL (April 29, 2008). "Persistent Organochlorine Pesticides and Risk of Testicular Germ Cell Tumors". Journal of the National Cancer Institute. 100 (9): 663. doi:10.1093/jnci/djn101. PMID 18445826.
- ^ Clapp RW, Jacobs MM, Loechler EL (2008). "Environmental and occupational causes of cancer: new evidence 2005-2007". Rev Environ Health. 23 (1): 1–37. PMC 2791455. PMID 18557596.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Verner MA, Charbonneau M, López-Carrillo L, Haddad S (2008). "Physiologically based pharmacokinetic modeling of persistent organic pollutants for lifetime exposure assessment: a new tool in breast cancer epidemiologic studies". Environ. Health Perspect. 116 (7): 886–92. doi:10.1289/ehp.10917. PMC 2453156. PMID 18629310.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Brody JG, Moysich KB, Humblet O, Attfield KR, Beehler GP, Rudel RA (2007). "Environmental pollutants and breast cancer: epidemiologic studies". Cancer. 109 (12 Suppl): 2667–711. doi:10.1002/cncr.22655. PMID 17503436.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ López-Cervantes M, Torres-Sánchez L, Tobías A, López-Carrillo L (2004). "Dichlorodiphenyldichloroethane burden and breast cancer risk: a meta-analysis of the epidemiologic evidence". Environ. Health Perspect. 112 (2): 207–14. doi:10.1289/ehp.6492. PMC 1241830. PMID 14754575.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Douglas Fischer (August 8, 2007). "Exposure to DDT is linked to cancer". Contra Costa Times. Archived from the original on 2010-11-18.
{{cite news}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ Marla Cone (September 30, 2007). "Study suggests DDT, breast cancer link". LA Times. [dead link]
- ^ a b c 2009 WHO World Malaria Report 2009
- ^ a b Kirsten Weir (June 29, 2007). "Rachel Carson's birthday bashing". Salon.com. Retrieved 2007-07-01.
- ^ Paull, John (3 November 2007). "Toxic Colonialism". New Scientist (2628): 25.
- ^ Yakob, L., Dunning, R. & Yan, G. Indoor residual spray and insecticide-treated bednets for malaria control: theoretical synergisms and antagonisms. JRS Interface doi:10.1098/rsif.2010.0537
- ^ Feachem RG, Sabot OJ (2007). "Global malaria control in the 21st century: a historic but fleeting opportunity". JAMA. 297 (20): 2281–4. doi:10.1001/jama.297.20.2281. PMID 17519417.
- ^ "WHO Urges Use of DDT in Africa". Washington Post. September 16, 2006.
- ^ Garrett, Laurie. (1994). The Coming Plague. Virago Press. p. 51. ISBN 1-86049-211-8.
- ^ Malaria: A Disease Close to Eradication Grows, Aided by Political Tumult in Sri Lanka, Donald G. McNeil Jr, The New York Times, December 27, 2010.
- ^ WHO | WHO gives indoor use of DDT a clean bill of health for controlling malaria
- ^ Countries move toward more sustainable ways to roll back malaria
- ^ Yamey, Gavin (2004). "Roll Back Malaria: a failing global health campaign". BMJ. 328 (7448): 1086–1087. doi:10.1136/bmj.328.7448.1086. PMC 406307. PMID 15130956.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ a b Indoor Residual Spraying: Use of Indoor Residual Spraying for Scaling Up Global Malaria Control and Elimination. World Health Organization, 2006.
- ^ a b c d e f g Control of Malaria Vectors in Africa and Asia C.F.Curtis
- ^ Sharma, V.P. (1999). "Current scenario of malaria in India". Parassitologia. 41 (1–3): 349–53. PMID 10697882.
- ^ Agarwal, Ravi (2001). "No Future in DDT: A case study of India". Pesticide Safety News.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Art Fisher, Mark Walker, Pam Powell. "DDT and DDE: Sources of Exposure and How to Avoid Them" (PDF). Retrieved 2010-12-02.
{{cite web}}: CS1 maint: multiple names: authors list (link) - ^ a b Sharma SN, Shukla RP, Raghavendra K, Subbarao SK (2005). "Impact of DDT spraying on malaria transmission in Bareilly District, Uttar Pradesh, India". J Vector Borne Dis. 42 (2): 54–60. PMID 16161701.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Hargreaves K, Hunt RH, Brooke BD (2003). "Anopheles arabiensis and An. quadriannulatus resistance to DDT in South Africa". Med. Vet. Entomol. 17 (4): 417–22. doi:10.1111/j.1365-2915.2003.00460.x. PMID 14651656.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ a b Grieco JP, Achee NL, Chareonviriyaphap T (2007). "A new classification system for the actions of IRS chemicals traditionally used for malaria control". PLoS ONE. 2 (1): e716. doi:10.1371/journal.pone.0000716. PMC 1934935. PMID 17684562.
{{cite journal}}: CS1 maint: multiple names: authors list (link) CS1 maint: unflagged free DOI (link) - ^ a b c Mabaso ML, Sharp B, Lengeler C (2004). "Historical review of malarial control in southern African with emphasis on the use of indoor residual house-spraying". Trop. Med. Int. Health. 9 (8): 846–56. doi:10.1111/j.1365-3156.2004.01263.x. PMID 15303988.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Sharma, V. P. (2003). "DDT: The fallen angel" (PDF). Current Science. 85 (11): 1532–1537.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ In Malaria War, South Africa Turns To Pesticide Long Banned in the West, Roger Thurow, Wall Street Journal, July 26, 2001
- ^ a b Bouwman H, Sereda B, Meinhardt HM (2006). "Simultaneous presence of DDT and pyrethroid residues in human breast milk from a malaria endemic area in South Africa". Environ. Pollut. 144 (3): 902–17. doi:10.1016/j.envpol.2006.02.002. PMID 16564119.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ a b Ntow WJ, Tagoe LM, Drechsel P, Kelderman P, Gijzen HJ, Nyarko E (2008). "Accumulation of persistent organochlorine contaminants in milk and serum of farmers from Ghana". Environ. Res. 106 (1): 17–26. doi:10.1016/j.envres.2007.05.020. PMID 17931619.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Spicer PE, Kereu RK (1993). "Organochlorine insecticide residues in human breast milk: a survey of lactating mothers from a remote area in Papua New Guinea". Bull Environ Contam Toxicol. 50 (4): 540–6. PMID 8467139.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Science Daily (May 9, 2009). "Unprecedented Use Of DDT Concerns Experts". ScienceDaily.com. Retrieved 2009-05-30.
- ^ Jayashree, Jayashree (June 10, 2009). "Pesticide level in veggies, fruits rises". Economic Times. Retrieved 2009-06-10.
- ^ SANJANA (June 13, 2009). "A Whole Fruit". Tehelka Magazine. 6 (23).
- ^ Chakravartty, Anupam (June 8, 2009). "State public libraries gasp for breath". Indian Express. Retrieved 2009-06-08.
- ^ Katima, Jamidu (June 2009). "African NGOs outline commitment to malaria control without DDT". Pesticides News (84): 5.
- ^ Ghana News Agency (November 17, 2009). "Ministry moves to check unorthodox fishing methods". Ghana News Agency. Archived from the original on 2010-11-18. Retrieved 2009-11-18.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ Appiah, Samuel (27 April 2010). "Northern fisherfolks complain of committee's harassment". Joy Online. Retrieved 27 April 2010.
- ^ William Souder (September 4, 2012). "Rachel Carson Didn't Kill Millions of Africans". Slate. Retrieved September 5, 2012.
- ^ Kristof, Nicholas D. (2005). "I Have a Nightmare". New York Times. Section A, Page 15, Column 1.
{{cite news}}: Unknown parameter|month=ignored (help); Unknown parameter|nopp=ignored (|no-pp=suggested) (help) - ^ Finkel, Michael (July 2007). "Malaria". National Geographic.
- ^ Sarvana, Adam (May 28, 2009). "Bate and Switch: How a free-market magician manipulated two decades of environmental science". Natural Resources New Service. Retrieved 2009-06-02.
- ^ Gutstein, Donald (November 24, 2009). Not a Conspiracy Theory: How Business Propaganda Hijacks Democracy. Key Porter Books. ISBN 978-1-55470-191-9.. Relevant section excepted at: Gutstein, Donald (January 22, 2010). "Inside the DDT Propaganda Machine". The Tyee. Retrieved 22 January 2010.
- ^ Rehabilitating Carson, John Quiggin & Tim Lambert, Prospect, May 2008.
- ^ Sidley P (2000). "Malaria epidemic expected in Mozambique". BMJ. 320 (7236): 669. doi:10.1136/bmj.320.7236.669. PMC 1117705. PMID 10710569.
- ^ Bate, Roger (2001). "A Case of the DDTs: The war against the war against malaria". National Review. LIII (9). Archived from the original on 2010-11-18.
{{cite journal}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help); Unknown parameter|month=ignored (help) - ^ a b "USAID Health: Infectious Diseases, Malaria, Technical Areas, Prevention and Control, Indoor Residual Spraying". USAID. Archived from the original on 2010-11-18. Retrieved 2008-10-14.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ Stossel, John (November 16, 2007). "Excerpt: 'Myths, Lies, and Downright Stupidity'". ABC News. Retrieved 2008-10-14.
- ^ Kent R. Hill (2005). "USAID isn't against using DDT in worldwide malaria battle". Archived from the original on 2006-03-31. Retrieved 2006-04-03.
- ^ "USAID Health: Infectious Diseases, Malaria, News, Africa Malaria Day, USAID Support for Malaria Control in Countries Using DDT". 2005. Archived from the original on 2010-11-18. Retrieved 2006-03-15.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ Killeen GF, Fillinger U, Kiche I, Gouagna LC, Knols BG (2002). "Eradication of Anopheles gambiae from Brazil: lessons for malaria control in Africa?". Lancet Infect Dis. 2 (10): 618–27. doi:10.1016/S1473-3099(02)00397-3. PMID 12383612.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Impact of long-lasting insecticidal-treated nets (LLINs) and artemisinin-based combination therapies (ACTs) measured using surveillance data in four African countries. World Health Organization, January 31, 2008.
- ^ Malaria deaths halved in Rwanda and Ethiopia Better drugs, mosquito nets are the crucial tools, David Brown (Washington Post), SF Chronicle, A-12, February 1, 2008.
- ^ World Health Organization, "A story to be shared: The successful fight against malaria in Vietnam," November 6, 2000.
- ^ a b "DDT & Malaria". Archived from the original (PDF) on 2010-05-21. Retrieved 2009-03-11.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ C. A. Goodman and A. J. Mills (1999). "The evidence base on the cost-effectiveness of malaria control measures in Africa" (PDF). Health Policy and Planning. 14 (4): 301–312. doi:10.1093/heapol/14.4.301. PMID 10787646.
- ^ Kamolratanakul, P.; Butraporn, P; Prasittisuk, M; Prasittisuk, C; Indaratna, K (2001). "Cost-effectiveness and sustainability of lambdacyhalothrin-treated mosquito nets in comparison to DDT spraying for malaria control in western Thailand". American Journal of Tropical Medicine and Hygiene. 65 (4): 279–84. PMID 11693869.
- ^ Goodman CA, Mnzava AE, Dlamini SS, Sharp BL, Mthembu DJ, Gumede JK (2001). "Comparison of the cost and cost-effectiveness of insecticide-treated bednets and residual house-spraying in KwaZulu-Natal, South Africa". Trop. Med. Int. Health. 6 (4): 280–95. doi:10.1046/j.1365-3156.2001.00700.x. PMID 11348519.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Corin, S. E & Weaver, S.A. (2005). "A risk analysis model with an ecological perspective on DDT and malaria control in South Africa" (PDF). Journal of Rural and Tropical Public Health. 4 (4): 21–32.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Over, M; Bakote'e, B; Velayudhan, R; Wilikai, P; Graves, PM (2004). "Impregnated nets or DDT residual spraying? Field effectiveness of malaria prevention techniques in solomon islands, 1993-1999". Am. J. Trop. Med. Hyg. 71 (2 Suppl): 214–23. PMID 15331840.
- ^ Barat LM (2006). "Four malaria success stories: how malaria burden was successfully reduced in Brazil, Eritrea, India, and Vietnam". Am. J. Trop. Med. Hyg. 74 (1): 12–6. PMID 16407339.
External links
- Toxicity
- DDT Technical Fact Sheet - National Pesticide Information Center
- DDT General Fact Sheet - National Pesticide Information Center
- EXTOXNET: Pesticide Information Profiles—DDT
- Scorecard: The Pollution Information Site—DDT
- Interview with Barbara Cohn, PhD about DDT and breast cancer
- Pesticide residues in food 2000 : DDT
- Politics and DDT
- DDT, Eggshells, and Me Article from Reason magazine by Ronald Bailey.
- Rachel Carson, Mass Murderer?: The creation of an anti-environmental myth. Aaron Swartz, Extra!, September/October, 2007.
- Malaria and DDT
- "If Malaria's the Problem, DDT's Not the Only Answer", a Washington Post column by entomologist May Berenbaum
- 'Andrew Spielman, Harvard School of Public Health, discusses environmentally friendly control of Malaria and uses of DDT Freeview video provided by the Vega Science Trust
- Ugandan farmers push for DDT ban. Dated 31 May 2008 ABC News
