Hydroxycarbamide
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Apo-Hydroxyurea, Droxia, Hydrea, others |
| AHFS/Drugs.com | International Drug Names |
| MedlinePlus | a682004 |
| License data |
|
| Pregnancy category |
|
| Routes of administration | Oral |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Metabolism | Hepatic (to CO2 and urea) |
| Elimination half-life | 2-4 hours |
| Excretion | Renal and lungs |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| NIAID ChemDB | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.004.384 |
| Chemical and physical data | |
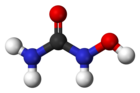
| Formula | CH4N2O2 |
| Molar mass | 76.0547 g/mol g·mol−1 |
| 3D model (JSmol) | |
| |
| |
| (verify) | |
Hydroxycarbamide (INN, BAN) or hydroxyurea (USAN, AAN) is an antineoplastic drug used in myeloproliferative disorders, specifically polycythemia vera and essential thrombocythemia. It is also used to reduce the rate of painful attacks in sickle-cell disease and has antiretroviral properties in diseases such as HIV/AIDS.
It is on the World Health Organization's List of Essential Medicines, a list of the most important medication needed in a basic health system.[2]
Medical uses
Hydroxycarbamide is used for the following indications:
- Myeloproliferative disease (primarily polycythemia vera and essential thrombocytosis). It has been found to be superior to anagrelide for the control of ET.[3]
- Sickle-cell disease[4] (breaks down cells that are prone to sickle, as well as increasing fetal hemoglobin content)
- AIDS as an adjunct to ddI in combination antiretroviral therapies[5]
- Second line treatment for psoriasis[6] (slows down the rapid division of skin cells)
- Psoriasis[7]
- Systemic mastocytosis[8]
- Chronic myelogenous leukemia (largely replaced by imatinib, but still in use for its cost-effectiveness)[9]
- Biochemical research as a DNA replication inhibitor[10] which causes deoxyribonucleotide depletion and results in DNA double strand breaks near replication forks (see DNA repair)
Side effects
Reported side-effects are: drowsiness, nausea, vomiting and diarrhea, constipation, mucositis, anorexia, stomatitis, bone marrow toxicity (dose-limiting toxicity; may take 7–21 days to recover after the drug has been discontinued), alopecia (hair loss), skin changes, abnormal liver enzymes, creatinine and blood urea nitrogen.[11]
Due to its effect on the bone marrow, regular monitoring of the full blood count is vital, as well as early response to possible infections. In addition, renal function, uric acid and electrolytes, as well as liver enzymes, are commonly checked.[12] Moreover, because of this, severe anemia and neutropenia are contraindicated.
Hydroxycarbamide has been used primarily for the treatment of myeloproliferative diseases, which has an inherent risk of transforming to acute myeloid leukemia. There has been a longstanding concern that hydroxycarbamide itself carries a leukemia risk, but large studies have shown that the risk is either absent or very small. Nevertheless, it has been a barrier for its wider use in patients with sickle-cell disease.[13]
Mechanism of action
Hydroxycarbamide decreases the production of deoxyribonucleotides[14] via inhibition of the enzyme ribonucleotide reductase by scavenging tyrosyl free radicals as they are involved in the reduction NDPs.[13]
In the treatment of sickle-cell disease, hydroxycarbamide increases the concentration of fetal hemoglobin. The precise mechanism of action is not yet clear, but it appears that hydroxycarbamide increases nitric oxide levels, causing soluble guanylyl cyclase activation with a resultant rise in cyclic GMP, and the activation of gamma globin chain synthesis necessary for fetal hemoglobin production (which inhibits the formation of sickle hemoglobin aggregates). A few red cell clones called F cells are progeny of a small pool of immature committed erythroid precursors (BFU-e) that retain the ability to produce HbF.[13][15]
Names
Brand names include: Hydrea, Litalir, Droxia, and Siklos
Natural occurrence
Hydroxyurea has been reported as endogenous in human blood plasma at concentrations of approximately 30 to 200 ng/mL.[16]
References
- ^ "FDA-sourced list of all drugs with black box warnings (Use Download Full Results and View Query links.)". nctr-crs.fda.gov. FDA. Retrieved 22 Oct 2023.
- ^ "WHO Model List of EssentialMedicines" (PDF). World Health Organization. October 2013. Retrieved 22 April 2014.
- ^ Harrison CN, Campbell PJ, Buck G, et al. (July 2005). "Hydroxyurea compared with anagrelide in high-risk essential thrombocythemia". N. Engl. J. Med. 353 (1): 33–45. doi:10.1056/NEJMoa043800. PMID 16000354.
- ^ Lanzkron S, Strouse JJ, Wilson R, et al. (June 2008). "Systematic review: Hydroxyurea for the treatment of adults with sickle cell disease". Ann. Intern. Med. 148 (12): 939–55. doi:10.7326/0003-4819-148-12-200806170-00221. PMC 3256736. PMID 18458272.
- ^ Frank I, Bosch RJ, Fiscus S, et al. (September 2004). "Activity, safety, and immunological effects of hydroxyurea added to didanosine in antiretroviral-naive and experienced HIV type 1-infected subjects: a randomized, placebo-controlled trial, ACTG 307". AIDS Res. Hum. Retroviruses. 20 (9): 916–26. doi:10.1089/aid.2004.20.916. PMID 15597521.
- ^ Sharma VK, Dutta B, Ramam M (2004). "Hydroxyurea as an alternative therapy for psoriasis". Indian J Dermatol Venereol Leprol. 70 (1): 13–7. PMID 17642550.
- ^ Rustin, MH (November 2012). "Long-term safety of biologics in the treatment of moderate-to-severe plaque psoriasis: review of current data". Br J Dermatol. 167 (Suppl 3): 3–11. doi:10.1111/j.1365-2133.2012.11208.x. PMID 23082810.
- ^ Escribano, L.; Álvarez-Twose, I. N.; Sánchez-Muñoz, L.; Garcia-Montero, A.; Núñez, R.; Almeida, J.; Jara-Acevedo, M.; Teodósio, C.; et al. (2009). "Prognosis in adult indolent systemic mastocytosis: A long-term study of the Spanish Network on Mastocytosis in a series of 145 patients". Journal of Allergy and Clinical Immunology. 124 (3): 514–521. doi:10.1016/j.jaci.2009.05.003. PMID 19541349.
- ^ Dalziel, K.; Round, A.; Stein, K.; Garside, R.; Price, A. (2004). "Effectiveness and cost-effectiveness of imatinib for first-line treatment of chronic myeloid leukaemia in chronic phase: A systematic review and economic analysis". Health technology assessment (Winchester, England). 8 (28): iii, ii1–120. PMID 15245690.
- ^ Koç A, Wheeler LJ, Mathews CK, Merrill GF (January 2004). "Hydroxyurea arrests DNA replication by a mechanism that preserves basal dNTP pools". J. Biol. Chem. 279 (1): 223–30. doi:10.1074/jbc.M303952200. PMID 14573610.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Liebelt, E.; Balk, S.; Faber, W.; Fisher, J.; Hughes, C.; Lanzkron, S.; Lewis, K.; Marchetti, F.; Mehendale, H.; Rogers, J. M.; Shad, A. T.; Skalko, R. G.; Stanek, E. J. (2007). "NTP-CERHR expert panel report on the reproductive and developmental toxicity of hydroxyurea". Birth defects research. Part B, Developmental and reproductive toxicology. 80 (4): 259–366. doi:10.1002/bdrb.20123. PMID 17712860.
- ^ Longe, Jacqueline L. (2002). Gale Encyclopedia Of Cancer: A Guide To Cancer And Its Treatments. Detroit: Thomson Gale. pp. 514–516. ISBN 978-1-4144-0362-5.
- ^ a b c Platt OS (2008). "Hydroxyurea for the treatment of sickle cell anemia". N. Engl. J. Med. 358 (13): 1362–9. doi:10.1056/NEJMct0708272. PMID 18367739.
- ^ "hydroxyurea" at Dorland's Medical Dictionary
- ^ Cokic VP, Smith RD, Beleslin-Cokic BB, et al. (2003). "Hydroxyurea induces fetal hemoglobin by the nitric oxide-dependent activation of soluble guanylyl cyclase". J Clin Invest. 111 (2): 231–9. doi:10.1172/JCI16672. PMC 151872. PMID 12531879.
- ^ Kettani, T; Gulbis, B; Ferster, A; Kumps, A (2009). "Plasma hydroxyurea determined by gas chromatography-mass spectrometry". Journal of Chromatography B. 877 (4): 446–450. doi:10.1016/j.jchromb.2008.12.048.
