Botulinum toxin
This article may require copy editing for grammar, style, cohesion, tone, or spelling. (December 2008) |
 | |
| Clinical data | |
|---|---|
| Routes of administration | IM (approved),SC, intradermal, into glands |
| ATC code | |
| Legal status | |
| Legal status | |
| Identifiers | |
| CAS Number | |
| PubChem CID | |
| DrugBank | |
| ECHA InfoCard | 100.088.372 |
| Chemical and physical data | |
| Formula | C6760H10447N1743O2010S32 |
| Molar mass | 149.322,3223 kDa g·mol−1 |
Botulinum toxin is a medication and a neurotoxic protein produced by the bacterium Clostridium botulinum, and is known to be very toxic[2][3] with an LD50 of roughly 0.005–0.05 µg/kg. Despite its deadly toxic effect, it is sometimes used in very small doses to treat muscle spasms.[4] Popularly known by its trade name, Botox, botulinum toxin is now commonly used in various settings for cosmetic procedures.[4]
History
Justinus Kerner described botulinum toxin as a "sausage poison" and "fatty poison",[5] as this bacterium often caused poisoning by growing in improperly handled or prepared meat products. It was Kerner who first conceived a possible therapeutic use of botulinum toxin physician, coined the name botulism. (In Latin, botulus means "sausage.") In 1897, Emile van Ermengem identified the bacterium Clostridium botulinum to be the producer of botulinum toxin.[6] In 1928, P. Tessmer Snipe and Hermann Sommer for the first time purified the toxin.[7] In 1949, Burgen's group discovered that botulinum toxin blocks neuromuscular transmission. In the late 1960s Alan Scott and Edward Schantz were the first to work on a standardized botulinum toxin preparation for therapeutic purposes.[8]
Other bacteria that produce botulinum toxin are Clostridium butyricum, C. baratii and C. argentinense.[9]
Alan Scott, a San Francisco ophthalmologist, first applied tiny doses of the toxin in a medicinal sense to treat "crossed eyes" (strabismus) and "uncontrollable blinking" (blepharospasm), but needed a partner to gain regulatory approval to market his discovery as a drug. Allergan renamed the drug Botox.
Botulinum toxin is neutralized at temperatures greater than 60 °C[10] (140°F). By 1973, Alan B. Scott, MD, of Smith-Kettlewell Institute used botulinum toxin type A (BTX-A) in monkey experiments, and, in 1980, he officially used BTX-A for the first time in humans to treat strabismus, a condition in which the eyes are not properly aligned with each other.
The possibility of using botox as a therapeutic agent was carried out in the early 1980’s, by groups of university-based ophthalmologists scattered throughout the U.S.A. and Canada. By 1985 a scientific protocol of injection sites and dosage had been empirically determined for treatment of blepharospasm (BLE) and strabismus. [11][12]Side effects had been evaluated and were deemed to be rare, mild and treatable. [13] The beneficial effects of the injection lasted only 4-6 months, so that BLE patients had to return to the clinics for re-injection two or three times a year.
In 1986 Dr. Alan Scott’s micro-manufacturer and distributor of botox was no longer able to supply the drug because of an inability to obtain product liability insurance. Patients became desperate as supplies of botox were gradually consumed, abandoning patients who would have been due for their next "fix". In an embarrassing scandal[14], for a period of four months American BLE patients had to arrange to have their injections performed by participating doctors at the Canadian eye centers until the liability issues could be resolved.
In December 1989, BTX-A (BOTOX) was approved by the U.S. Food and Drug Administration (FDA) for the treatment of strabismus, blepharospasm, and hemifacial spasm in patients over 12 years old. The cosmetic effect of BTX-A on wrinkles was originally documented by a plastic surgeon from Sacramento, California, Dr.Richard Clark, and published in Plastic and Reconstructive Surgery in 1989.[15] Similar effects had reportedly been observed by a number of independent groups (Brin, and the Columbia University group). Bushara and Park were the first to show that botulinum toxin injections inhibit sweating while treating patients with hemifacial spasm at Southend Hospital in England 1n 1993[16]. They further showed the efficacy of botulinum toxin in treating hyperhidrosis (excessive sweating). On April 15, 2002, the FDA announced the approval of botulinum toxin type A (BOTOX Cosmetic) to temporarily improve the appearance of moderate-to-severe frown lines between the eyebrows (glabellar lines). BTX-A was later approved for the treatment of excessive underarm sweating. The acceptance of BTX-A use for the treatment of spasticity and muscle pain disorders is growing, with approvals pending in many European countries and studies on headaches (including migraine), pro static symptoms, asthma, obesity and many other possible indications are ongoing. In June 2009 its use for treating spasticity led a UK doctor to successfully treat an Australian man who had been confined to a wheelchair following a stroke 20 years ago.[17]
In the United States, Botox is manufactured by Allergan, Inc. for both therapeutic and cosmetic use. Yet there are many other versions of the product being manufactured all over the world. For example, Dysport, a therapeutic formulation of the type A toxin developed and manufactured in Ireland, is licensed for the treatment of focal dystonias and certain cosmetic uses in many territories worldwide[citation needed]. Additionally, Lanzhou Institute (China) manufactures its own BTX-A product, producing 50U and 100U type A toxin[citation needed] and in 2009 yet another BTX-A product, Neuronox, was introduced by Medy-Tox Inc. (South Korea)[18].
Botulinum Toxin Type B (BTX-B) received FDA approval for treatment of cervical dystonia on December 21, 2000. Trade names for BTX-B are Myobloc in the United States, and Neurobloc in the European Union.[citation needed]
Since the original invention of Botox, a technique dubbed Microdroplet™ Botox™ was invented with the claim that it injects Botox more precisely and with more predictable results[19]. Other physicians debate whether the technique is anything more than using smaller needles and whether it merits a trademarked name[20].
Chemical overview and lethality
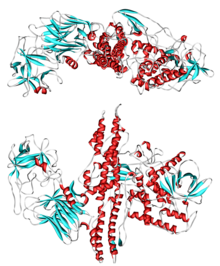
There are seven serologically distinct toxin types, designated A through G. Additionally, six of the seven toxin types have subtypes with five subtypes of BoNT A having been described. The toxin is a two-chain polypeptide with a 100-kDa heavy chain joined by a disulphide bond to a 50-kDa light chain. This light chain is an enzyme (a protease) that attacks one of the fusion proteins (SNAP-25, syntaxin or synaptobrevin) at a neuromuscular junction, preventing vesicles from anchoring to the membrane to release acetylcholine. By inhibiting acetylcholine release, the toxin interferes with nerve impulses and causes flaccid (sagging) paralysis of muscles in botulism, as opposed to the spastic paralysis seen in tetanus.
It is the most acutely toxic substance known, with a median lethal dose of about 1 ng/kg when introduced intravenously[21] and 3 ng/kg when inhaled[22]. This means that, depending on the method of introduction into the body, a mere 90–270 nanograms of botulinum toxin could be enough to kill an average 90 kg (200 lb) person.
Food-borne botulism usually results from ingestion of food that has become contaminated with spores (such as a perforated can) in an anaerobic environment, allowing the spores to germinate and grow. The growing (vegetative) bacteria produce toxin. It is the ingestion of preformed toxin that causes botulism, not the ingestion of the spores or the vegetative bacteria. Infant and wound botulism both result from infection with spores which subsequently germinate, resulting in production of toxin and the symptoms of botulism.
Proper refrigeration at temperatures below 3°C (38°F) prevents the growth of Clostridium botulinum. The organism is also susceptible to high salt and low pH levels. The toxin itself is rapidly destroyed by heat, such as in thorough cooking.[23] On the other hand, the spores which produce the toxin are heat-tolerant and will survive boiling water for an extended period of time.[24] Fortunately, ingestion of the spores is safe, except in infants, as the highly oxygenated and highly acidic environment of the digestive system prevents the spores from growing and producing the botulinum toxin.
Botulinum toxin has been recognized and feared as a potential bioterrorism toxic weapon. [25]. Intentional exposure to the toxin in a bioterrorism attack would most likely occur by poisoned food or water, or through breathing in the toxin.[26]
Medical uses
Although botulinum toxin is a lethal naturally occurring substance, when carefully isolated and purified, it can be used as an effective and powerful medication.[27] Researchers discovered in the 1950s that injecting overactive muscles with minute quantities of botulinum toxin type-A would result in decreased muscle activity by blocking the release of acetylcholine from the neuron by preventing the vesicle where the Acetylcholine is stored from binding to the membrane where the neurotransmitter can be released. This will render the muscle unable to contract for up to a period of three to four months.[citation needed]
In cosmetics, a Botox injection, consisting of a small dose of botulinum toxin, can be used to prevent formation of wrinkles by paralyzing facial muscles.[28] As of 2007, it is the most common cosmetic operation, with 4.6 million procedures in the United States, according to the American Society of Plastic Surgeons. Qualifications for Botox injectors vary by county, state and country. Botox Cosmetic providers include dermatologists, plastic surgeons, cosmetic physicians, nurses practitioners, nurses, physician assistants, and medical spas. The wrinkle preventing effect of Botox lasts for approximately 3-4 months[28][29], up to 6 months[29].
In addition to its cosmetic applications, Botox is currently used in the treatment e.g. spasms and dystonias, which it effectively suppresses for 60-70 days[30]. The main conditions are:
- Cervical dystonia (spasmodic torticollis) (a neuromuscular disorder involving the head and neck)[31]
- Blepharospasm (excessive blinking)[32]
- Severe primary axillary hyperhidrosis (excessive sweating)[33]
- Strabismus (Squints)
- Achalasia (failure of the lower oesophageal sphincter to relax)
- Local intradermal injection of BTX-A is helpful in chronic focal painful neuropathies. The analgesic effects are not dependent on changes in muscle tone.[34]
- Migraine and other headache disorders, although the evidence is conflicting in this indication[35]
Other uses of botulinum toxin type A that are widely known but not specifically approved by FDA (off-label uses) include treatment of:
- Pediatric incontinence,[36] incontinence due to overactive bladder,[37] and incontinence due to neurogenic bladder.[38]
- Anal fissure[39]
- Spastic disorders associated with injury or disease of the central nervous system including trauma, stroke, multiple sclerosis, Parkinson's disease, or cerebral palsy
- Focal dystonias affecting the limbs, face, jaw, or vocal cords
- TMJ pain disorders
- Diabetic neuropathy
- Wound healing
- Excessive salivation
- Vocal cord dysfunction (VCD) including spasmodic dysphonia and tremor
- Reduction of the Masseter muscle for decreasing the size of the lower jaw
Treatment and prevention of chronic headache[40] and chronic musculoskeletal pain[41] are emerging uses for botulinum toxin type A. In addition, there is evidence that Botox may aid in weight loss by increasing the gastric emptying time.[42]
Links to deaths
In September 2005, a paper published in the Journal of American Academy of Dermatology reported from the FDA saying that use of Botox has resulted in 28 deaths between 1989 and 2003, though none were attributed to cosmetic use.[43]
On February 8, 2008, the FDA announced that Botox has "been linked in some cases to adverse reactions, including respiratory failure and death, following treatment of a variety of conditions using a wide range of doses," due to its ability to spread to areas distant to the site of the injection.[44]
In January 2009, the Canadian government warned that botox can have the adverse effect of spreading to other parts of the body which could cause muscle weakness, swallowing difficulties, pneumonia, speech disorders and breathing problems.[45][46]
Several cases of death have been linked to the use of fake Botox,[47] one of the causes of death listed on the Spike TV show, "1000 Ways to Die".
Side effects
Side effects, which are generally minor and temporary[28], can be predicted from the mode of action (muscle paralysis) and chemical structure (protein) of the molecule, resulting broadly speaking in two major areas of side effects: paralysis of the wrong muscle group and allergic reaction. Bruising at the site of injection is a side effect not of the toxin, but rather the mode of administration. In cosmetic use, this can result in inappropriate facial expression such as drooping eyelid[28], double vision[28], uneven smile, or loss of the ability to close eyes. This will wear off in around six weeks. Bruising is prevented by the clinician applying pressure to the injection site, but may still occur, and will last around 7–10 days. When injecting the masseter muscle of the jaw, loss of muscle function will result in a loss or reduction of power to chew solid foods.[43] All cosmetic treatments are of limited duration, and can be as short a period as six weeks, but usually one sees an effective period of between three and eight months. At the extremely low doses used medicinally, botulinum toxin has a very low degree of toxicity.
Other adverse events from cosmetic use include headaches, dysphagia, flu-like syndromes, and allergic reactions.[43]
There has been a petition by Public Citizen to the FDA requesting regulatory action concerning the possible spread of botulinum toxin (Botox, Myobloc) from the site of injection to other parts of the body (HRG Publication #1834): Public Citizen
Individuals who are pregnant, have egg allergies or a neuromuscular disorder are advised to avoid Botox. [28]
Biochemical mechanism of toxicity

The heavy chain of the toxin is particularly important for targeting the toxin to specific types of axon terminals. The toxin must get inside the axon terminals in order to cause paralysis. Following the attachment of the toxin heavy chain to proteins on the surface of axon terminals, the toxin can be taken into neurons by endocytosis. The light chain is able to cleave endocytotic vesicles and reach the cytoplasm. The light chain of the toxin has protease activity. The type A toxin proteolytically degrades the SNAP-25 protein, a type of SNARE protein. The SNAP-25 protein is required for vesicle fusion that releases neurotransmitters from the axon endings (in particular Acetylcholine).[48] Botulinum toxin specifically cleaves these SNAREs, and so prevents neuro-secretory vesicles from docking/fusing with the nerve synapse plasma membrane and releasing their neurotransmitters.
Though it affects the nervous system, common nerve agent treatments (namely the injection of atropine and 2-pam-chloride) will increase mortality by enhancing botulin toxin's mechanism of toxicity[citation needed]. Attacks involving botulinum toxin are distinguishable from those involving nerve agent in that NBC detection equipment (such as M-8 paper or the ICAM) will not indicate a "positive" when a sample of the agent is tested. Furthermore, botulism symptoms develop relatively slowly, over several days compared to nerve agent effects, which can be instantaneous.
Documented outbreaks
This section needs expansion. You can help by adding to it. (March 2008) |
Bon Vivant incident
On July 2, 1971, the U.S. Food and Drug Administration (FDA) released a public warning after learning that a New York man had died and his wife had become seriously ill due to botulism after eating a can of Bon Vivant vichyssoise soup. The company began a recall of the 6,444 cans of vichyssoise soup made in the same batch as the can known to be contaminated. The FDA discovered that the company’s processing practices raised questions not only about these lots of the vichyssoise, but also about all other products packed by the company. The effectiveness check of the recall had revealed a number of swollen or otherwise suspect cans among Bon Vivant’s other products, so FDA extended the recall to include all Bon Vivant products. The FDA shut down the company’s Newark, New Jersey plant on July 7, 1971. Only five cans of Bon Vivant soup were found to be contaminated with the botulinum toxin, all in the initial batch of vichyssoise recalled and part of the first 324 cans tested. The ordeal destroyed public confidence in the company’s products and the Bon Vivant name. Bon Vivant filed for bankruptcy within a month of the announcement of the recall.[49]
Treatment of botulinum poisoning
If the symptoms of botulism are diagnosed early, an equine antitoxin, use of enemas, and extracorporeal removal of the gut contents can be used to treat the food-borne illness. Wound infections can be treated surgically. Information regarding methods of safe canning, and public education about the disease are methods of prevention. Tests to detect botulism include a brain scan, nerve conduction test, and a tensilon test for myasthenia gravis in order to differentiate botulism from other diseases that manifest in the same way. Electromyography (EMG) can be utilized to differentiate myasthenia gravis and Guillain-Barré syndrome, diseases that botulism often mimics. Toxicity testing of serum specimens, wound tissue cultures, and toxicity testing, and stool specimen cultures are the best methods for idientifying botulism. Laboratory tests of the patient’s serum or stool, which are then injected into mice are also indicative of botulism. ([50]
The case fatality rate for botulinum poisoning between 1950 and 1996 was 15.5%, down from approximately 60% over the previous 50 years.[51] Death is generally secondary to respiratory failure due to paralysis of the respiratory muscles, so treatment consists of antitoxin administration and artificial ventilation until the neurotoxins are excreted or metabolised. If initiated on time these treatments are quite effective, although antisera can not affect BoNT polypeptides that have already entered cells.[52] Occasionally, functional recovery may take several weeks to months or more.
There are two primary Botulinum Antitoxins available for treatment of botulism.
- Trivalent (A,B,E) Botulinum Antitoxin is derived from equine sources utilizing whole antibodies (Fab & Fc portions). This antitoxin is available from the local health department via the CDC in the USA.
- The second antitoxin is Heptavalent (A,B,C,D,E,F,G) Botulinum Antitoxin which is derived from "despeciated" equine IgG antibodies which have had the Fc portion cleaved off leaving the F(ab')2 portions. This is a less immunogenic antitoxin that is effective against all known strains of botulism where not contraindicated. This is available from the US Army. On June 1, 2006 the US Department of Health and Human Services awarded a $363 million contract with Cangene Corporation for 200,000 doses of Heptavalent Botulinum Antitoxin over five years for delivery into the Strategic National Stockpile beginning in 2007.[53].
See also
- Argireline—Botox Alternative
- Castleberry's Food Company
- Microbial toxins
- Wickham Laboratories
References
- ^ "FDA-sourced list of all drugs with black box warnings (Use Download Full Results and View Query links.)". nctr-crs.fda.gov. FDA. Retrieved 22 Oct 2023.
- ^ Montecucco C, Molgó J (2005). "Botulinal neurotoxins: revival of an old killer". Current opinion in pharmacology. 5 (3): 274–9. doi:10.1016/j.coph.2004.12.006. PMID 15907915.
- ^ Kukreja R and Singh BR (2009). "Botulinum Neurotoxins: Structure and Mechanism of Action". Microbial Toxins: Current Research and Future Trends. Caister Academic Press. ISBN 978-1-904455-44-8.
- ^ a b "BOTOX(registered) Injections for Muscle Spasms - Risks, Benefits, and Cost of Treatment". Docshop.com. Retrieved November 09, 2009.
{{cite web}}: Check date values in:|accessdate=(help) - ^ Frank J. Erbguth (2004). "Historical notes on botulism, Clostridium botulinum, botulinum toxin, and the idea of the therapeutic use of the toxin". Movement Disorders. 19 (S8). Movement Disorder Society (Wiley): S2–S6. doi:10.1002/mds.20003.
- ^ Van Ermengem EP (1897) Über einen neuen anaeroben Bacillus und seine Beziehungen zum Botulismus. Z Hyg Infektionskrankh 26:1–56
- ^ SNIPE PT., SOMMER H. Studies on botulinus toxin. Acid precipitation of botulinus toxin.J. Infect. Dis., 1928, 43, 152–60. http://www.jstor.org/pss/30083772
- ^ Dressler D.[Pharmacological aspects of therapeutic botulinum toxin preparations] Nervenarzt. 2006 Aug;77:912–21.
- ^ Schantz EJ, Johnson EA. Properties and use of botulinum toxin and other microbial neurotoxins in medicine. Microbiol Rev. 1992;56:80-99.
- ^ Irving, W. (2005). Instant notes: Medical Microbiology. Taylor & Francis. p. 160.
{{cite book}}:|journal=ignored (help) - ^ Michael Flanders, MD; Jack Wise, MD; et al. (1987). "Injection of type A Botulinum toxin into extraocular muscles for correction of strabismus". Canadian Journal of Ophthalmology. vol 22 (issue 4).
{{cite journal}}:|issue=has extra text (help);|volume=has extra text (help); Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ http://www.ncbi.nlm.nih.gov/pubmed/3607594
- ^ Scott AB. (1985). "Botulinum toxin therapy of eye muscle disorders: safety and effectiveness. Ophthalmic Procedures Assessment Recommendation". American Academy of Ophthalmology.
- ^ http://www.nytimes.com/1986/10/14/science/loss-of-drug-relegates-many-to-blindness-again.html
- ^ Clark, R.P., and Berris, C.E. Botulinum Toxin: A treatment for facial asymmetry caused by facial nerve paralysis. Plast. Reconst. Surg. 84: 353, 1989. DOI: 10.1097/01.prs.0000205566.47797.8d
- ^ K O Bushara, D M Park. Botulinum toxin and sweating. J Neurol Neurosurg Psychiatry 1994;57:1437-1438 doi:10.1136/jnnp.57.11.1437
- ^ http://www.meeja.com.au/articles/botox-injections-get-australian-man-out-of-wheelchair
- ^ Petrou, Ilya, M.D. "Medy-Tox Introduces Neuronox to the Botulinum Toxin Arena". The European Aesthetic Guide. Spring 2009.
- ^ Steinsapir, Kenneth, M.D. "[1]". Inventor of Microdroplet™ Botox.
- ^ Realself.com "[2]". "Can micro droplet approach in Botox prevent eyebrow from drooping?"
- ^ Arnon, Stephen S. et al., "Botulinum Toxin as a Biological Weapon". JAMA. vol 285. pp.1059–1070. 2001.
- ^ http://www.aahealth.org/physicianslink/bioterrorism_botulism_overview.asp
- ^ Licciardello JJ, Nickerson JT, Ribich CA, Goldblith SA (1967). "Thermal inactivation of type E botulinum toxin". Appl Microbiol. 15 (2): 249–56. PMC 546888. PMID 5339838.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Setlowa, Peter (April 2007). "I will survive: DNA protection in bacterial spores". Trends in Microbiology. 15 (4). Elsevier Ltd.: 172–180. doi:10.1016/j.tim.2007.02.004.
- ^ http://www.medscape.com/viewarticle/482812
- ^ http://www.health.ri.gov/environment/biot/botulism_public.php
- ^ Richard Barbano, MD, PhD, FAAN (2006). "Risks of erasing wrinkles: Buyer beware!". Neurology. 67: E17–E18. doi:10.1212/01.wnl.0000250411.93526.9e.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ a b c d e f Baylor College of Medicine > Botox for Wrinkles Last modified: September 30, 2009. By Dr. Ramsey Markus
- ^ a b Realself.com > How long does Botox last? Answers by Harold J. Kaplan, MD and William J. Hedden, MD. Retrieved on Jan 12, 2009
- ^ Bihari K (2005). "Safety, effectiveness, and duration of effect of BOTOX after switching from Dysport for blepharospasm, cervical dystonia, and hemifacial spasm dystonia, and hemifacial spasm". Curr Med Res Opin. 21 (3): 433–8. doi:10.1185/030079905X36396. PMID 15811212.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Brin MF, Lew MF, Adler CH, Comella CL, Factor SA, Jankovic J, O'Brien C, Murray JJ, Wallace JD, Willmer-Hulme A, Koller M (1999). "Safety and efficacy of NeuroBloc (botulinum toxin type B) in type A-resistant cervical dystonia". Neurology. 53 (7): 1431–8. PMID 10534247.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Shukla HD, Sharma SK (2005). "Clostridium botulinum: a bug with beauty and weapon". Crit. Rev. Microbiol. 31 (1): 11–8. doi:10.1080/10408410590912952. PMID 15839401.
- ^ Eisenach JH, Atkinson JL, Fealey RD (2005). "Hyperhidrosis: evolving therapies for a well-established phenomenon". Mayo Clin. Proc. 80 (5): 657–66. doi:10.4065/80.5.657. PMID 15887434.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Ranoux D, Attal N, Morain F, Bouhassira D (2008). "Botulinum toxin type A induces direct analgesic effects in chronic neuropathic pain". Annals of neurology. 64 (3): 274–83. doi:10.1002/ana.21427. PMID 18546285.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Naumann M, So Y, Argoff CE; et al. (2008). "Assessment: Botulinum neurotoxin in the treatment of autonomic disorders and pain (an evidence-based review): report of the Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology". Neurology. 70 (19): 1707–14. doi:10.1212/01.wnl.0000311390.87642.d8. PMID 18458231.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Schurch B, Corcos J (2005). "Botulinum toxin injections for paediatric incontinence". Current opinion in urology. 15 (4): 264–7. doi:10.1097/01.mou.0000172401.92761.86. PMID 15928517.
- ^ Duthie J, Wilson D, Herbison G, Wilson D (2007). "Botulinum toxin injections for adults with overactive bladder syndrome". 3: CD005493. doi:10.1002/14651858.CD005493.pub2. PMID 17636801.
{{cite journal}}: Cite journal requires|journal=(help)CS1 maint: multiple names: authors list (link) - ^ Akbar M, Abel R, Seyler TM, Gerner HJ, Möhring K (2007). "Repeated botulinum-A toxin injections in the treatment of myelodysplastic children and patients with spinal cord injuries with neurogenic bladder dysfunction". BJU Int. 100 (3): 639–45. doi:10.1111/j.1464-410X.2007.06977.x. PMID 17532858.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Trzciński R, Dziki A, Tchórzewski M (2002). "Injections of botulinum A toxin for the treatment of anal fissures". The European journal of surgery = Acta chirurgica. 168 (12): 720–3. PMID 15362583.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Panicker JN, Muthane UB (2003). "Botulinum toxins: pharmacology and its current therapeutic evidence for use". Neurology India. 51 (4): 455–60. PMID 14742921.
- ^ Charles PD (2004). "Botulinum neurotoxin serotype A: a clinical update on non-cosmetic uses". American journal of health-system pharmacy : AJHP : official journal of the American Society of Health-System Pharmacists. 61 (22 Suppl 6): S11–23. PMID 15598005.
- ^ Coskun H, Duran Y, Dilege E, Mihmanli M, Seymen H, Demirkol MO (2005). "Effect on gastric emptying and weight reduction of botulinum toxin-A injection into the gastric antral layer: an experimental study in the obese rat model". Obesity surgery : the official journal of the American Society for Bariatric Surgery and of the Obesity Surgery Society of Australia and New Zealand. 15 (8): 1137–43. doi:10.1381/0960892055002275. PMID 16197786.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ a b c Coté TR, Mohan AK, Polder JA, Walton MK, Braun MM (2005). "Botulinum toxin type A injections: adverse events reported to the US Food and Drug Administration in therapeutic and cosmetic cases". J. Am. Acad. Dermatol. 53 (3): 407–15. doi:10.1016/j.jaad.2005.06.011. PMID 16112345.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ FDA Notifies Public of Adverse Reactions Linked to Botox Use
- ^ http://www.cbc.ca/consumer/story/2009/01/13/botox.html
- ^ http://www.google.com/hostednews/afp/article/ALeqM5jjXaXXB231Ty8J7Sbi8yeN0EH5tA
- ^ Woman Dies From Fake Botox Injections
- ^ Foran PG, Mohammed N, Lisk GO; et al. (2003). "Evaluation of the therapeutic usefulness of botulinum neurotoxin B, C1, E, and F compared with the long lasting type A. Basis for distinct durations of inhibition of exocytosis in central neurons". J. Biol. Chem. 278 (2): 1363–71. doi:10.1074/jbc.M209821200. PMID 12381720.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) CS1 maint: unflagged free DOI (link) - ^ "An Examination of FDA's Recall Authority". Harvard Law School. Retrieved 2007-09-25.
The incident did not take a toll only on the company, however. Bon Vivant did not have adequate records and controls of production lots and distribution in order to trace the products quickly. The company also did not have the finances or manpower necessary to run a successful recall program. As a result, the FDA had to seize all the Bon Vivant soup throughout the country, more than a million cans in all. FDA said the seizure occupied 125 man years of FDA time, enough for 2,000 ordinary factory inspections for preventive purposes.
{{cite news}}: Cite has empty unknown parameter:|coauthors=(help) - ^ "Disease Listing, Botulism Manual, Additional Information". Retrieved 2010-01-21.
{{cite web}}: Text "CDC Bacterial, Mycotic Diseases" ignored (help) - ^ "Disease Listing, Botulism Manual, Additional Information". Retrieved 2007-08-14.
{{cite web}}: Text "CDC Bacterial, Mycotic Diseases" ignored (help) - ^ Turton, K., J. A. Chaddock, and K. R. Acharya. 2002. Botulinum and tetanus neurotoxins: structure, function and therapeutic utility. Trends in Biochemical Sciences 27:552-558.
- ^ "FEMA". Retrieved 2007-08-14.
External links
- A Poison that can Heal from the U.S. Food and Drug Administration
- Does Botox get into the brain? Troubling research contradicts earlier findings about the treatment
- BotDB: extensive resources on BoNT structures, inhibitors, kinetics, and literature
